Tropical mycoses Piedra Classification of Mycoses The clinical

- Slides: 26
Tropical mycoses. Piedra.
Classification of Mycoses The clinical nomenclatures used for the mycoses are based on the • site of the infection, • route of acquisition of the pathogen, • type of virulence exhibited by the fungus.
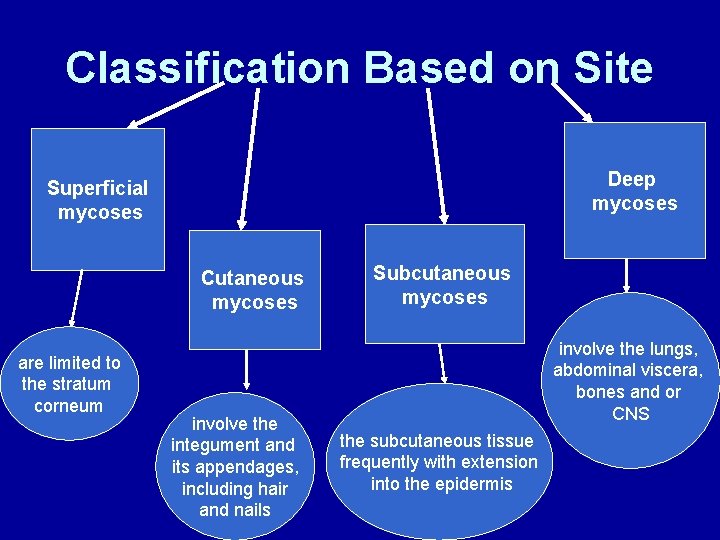
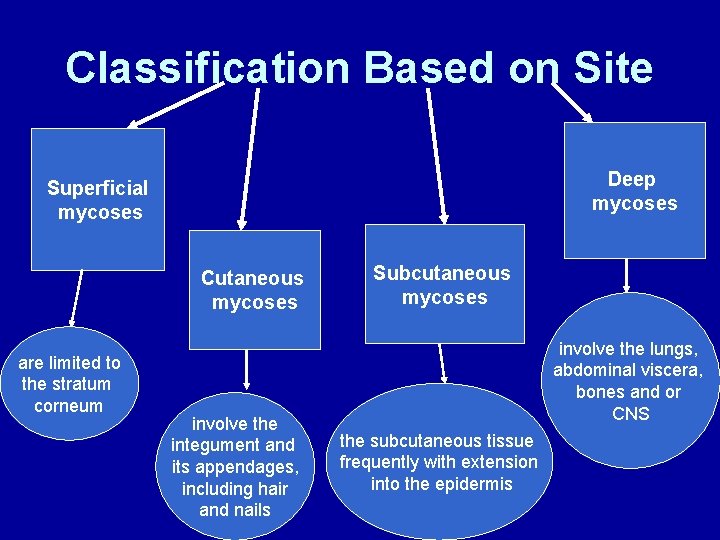
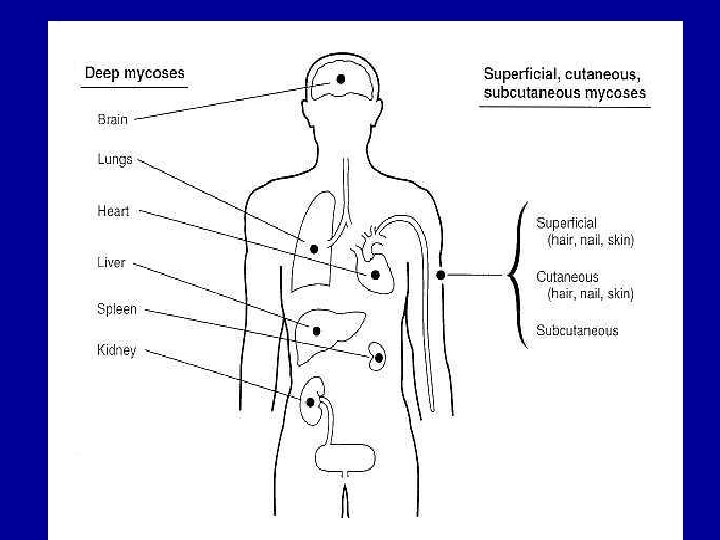
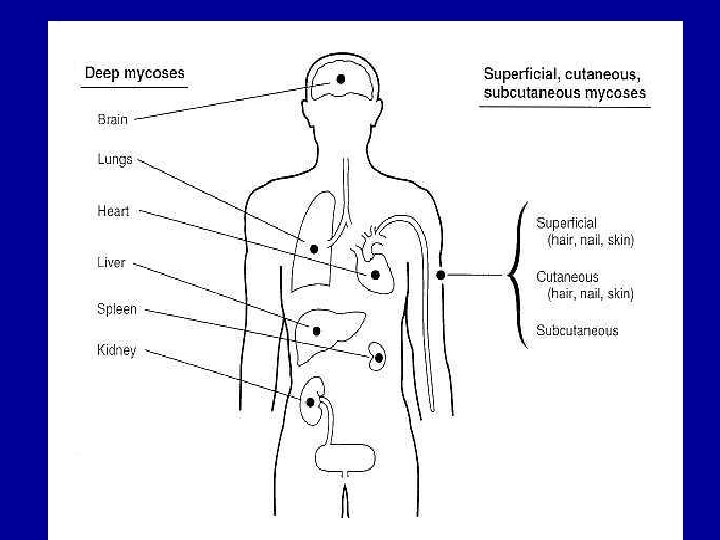
Classification Based on Site Deep mycoses Superficial mycoses Cutaneous mycoses are limited to the stratum corneum involve the integument and its appendages, including hair and nails Subcutaneous mycoses involve the lungs, abdominal viscera, bones and or CNS the subcutaneous tissue frequently with extension into the epidermis
Classification Based on Route of Acquisition • Infecting fungi may be either exogenous or endogenous. • If classified as exogenous, an infecting organism may be transmitted by airborne, cutaneous, or percutaneous routes. • Endogenous infection involves colonization by a member of the normal flora or reactivation of a previous infection.
Classification Based on Virulence • Fungi may be classified also according to virulence, as primary pathogens or as opportunistic pathogens. • Primary pathogens can establish infections in an immunologically normal hosts. • Opportunistic pathogens cause disease in individuals with compromised host defense mechanisms.
PIEDRA Synonyms: black piedra, white piedra, trichosporosis, asymptomatic superficial fungal infection of the hair shaft. Two varieties of piedra are recognized: black and white piedra. • Black piedra is a superficial fungal infection due to Piedraia hortae, which is characterized by formation of brown to black nodules that are very firmly attached to the hair shaft. Scalp hair is the most frequently infected area. • White piedra or trichosporosis is a superficial mycosis of the hair shaft, caused by the yeast Trichosporon beigelii. This disease is characterized by the presence of irregular white or brown nodules along the hair shaft. White piedra is a cosmopolitan infection being found in the hair of the beard, moustache, genitals.
Black piedra • Piedra, which means “stone” in Spanish, is an asymptomatic superficial fungal infection of the hair shaft. • In 1865, Beigel first described piedra in the human hair. • In 1911, Horta classified piedra into 2 types. The first is black piedra, the second is white piedra.
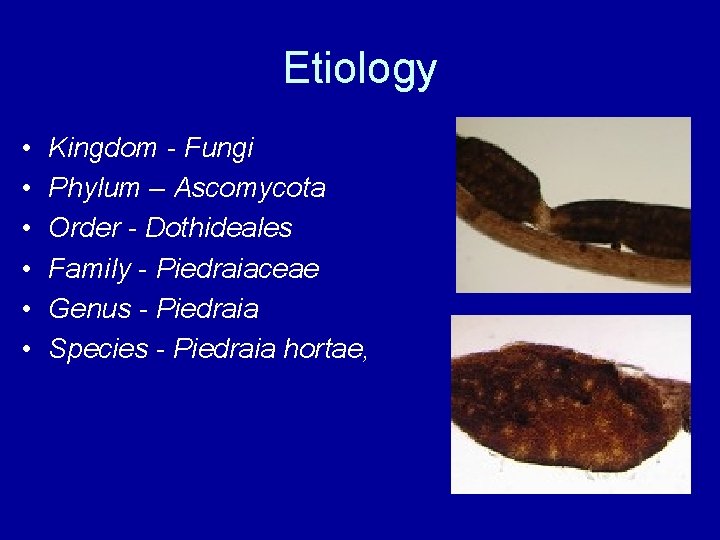
Etiology • • • Kingdom - Fungi Phylum – Ascomycota Order - Dothideales Family - Piedraiaceae Genus - Piedraia Species - Piedraia hortae,
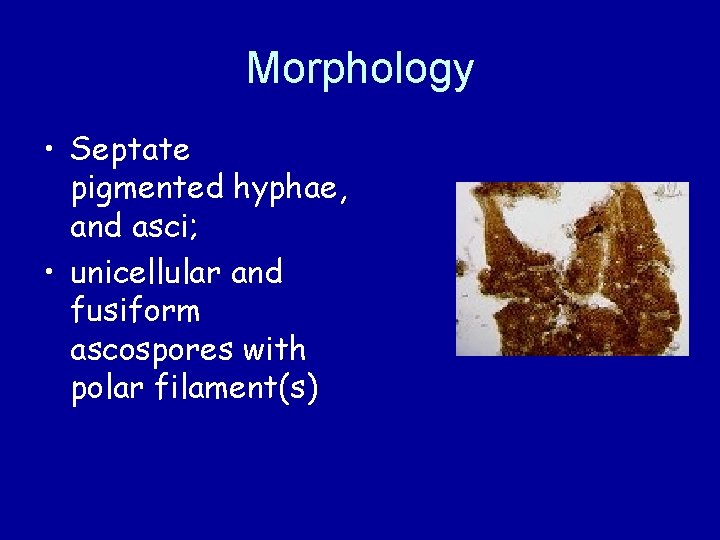
Morphology • Septate pigmented hyphae, and asci; • unicellular and fusiform ascospores with polar filament(s)
Epidemiology • The source of infection in black piedra, Piedraia hortae, appears to be in the soil; however, infection also has been traced to organisms in stagnant water and crops.
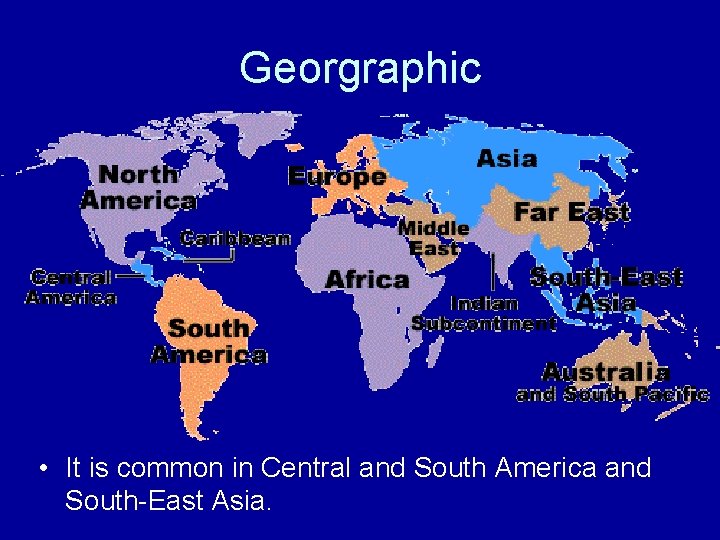
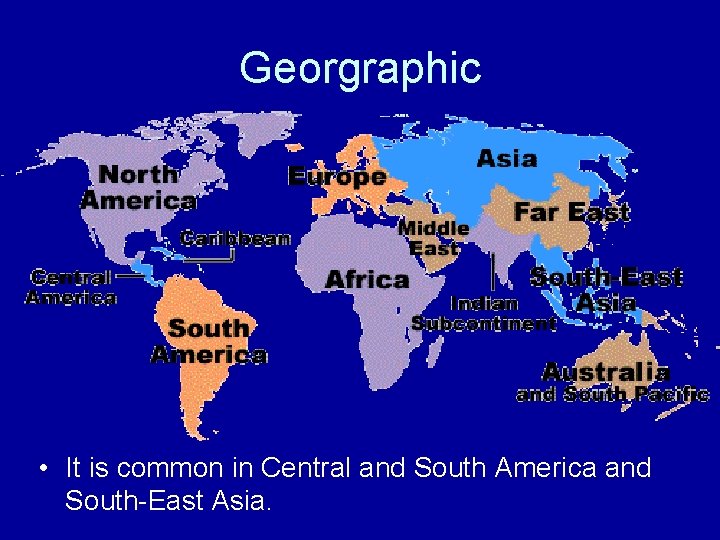
Georgraphic • It is common in Central and South America and South-East Asia.
Clinical symptoms: • Infections are usually localised to the scalp but may also be seen on hairs of the beard, moustache and pubic hair. • Black piedra mostly affects young adults and epidemics in families have been reported following the sharing of combs and hairbrushes. Infected hairs generally have a number of hard black nodules on the shaft. • Black piedra may be confused with trichorrhexis nodosa and trichonodosis but mycological examination will always confirm the diagnosis.
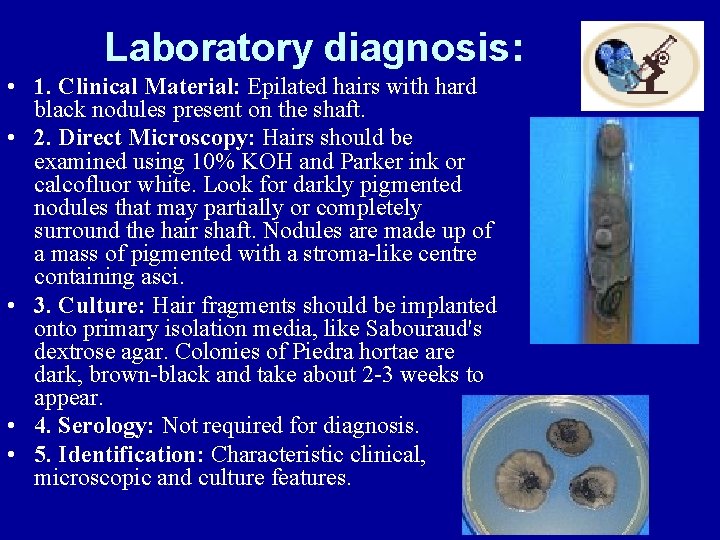
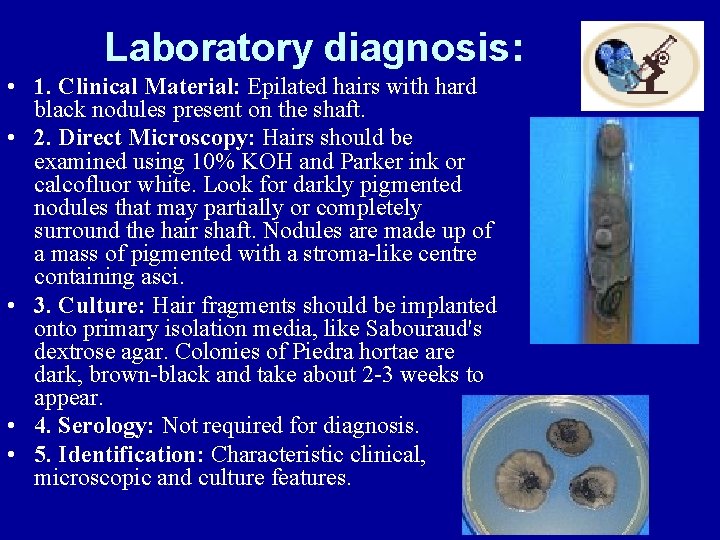
Laboratory diagnosis: • 1. Clinical Material: Epilated hairs with hard black nodules present on the shaft. • 2. Direct Microscopy: Hairs should be examined using 10% KOH and Parker ink or calcofluor white. Look for darkly pigmented nodules that may partially or completely surround the hair shaft. Nodules are made up of a mass of pigmented with a stroma-like centre containing asci. • 3. Culture: Hair fragments should be implanted onto primary isolation media, like Sabouraud's dextrose agar. Colonies of Piedra hortae are dark, brown-black and take about 2 -3 weeks to appear. • 4. Serology: Not required for diagnosis. • 5. Identification: Characteristic clinical, microscopic and culture features.
Treatment • The usual treatment is to shave or cut the hairs short, but this is often not considered acceptable, particularly by women. • Terbinafine - 250 mg a day for 6 weeks. • Topical salicylic acid, azol cremes
WHITE PIEDRA • Fungal infection of facial, axillary or genital hair.
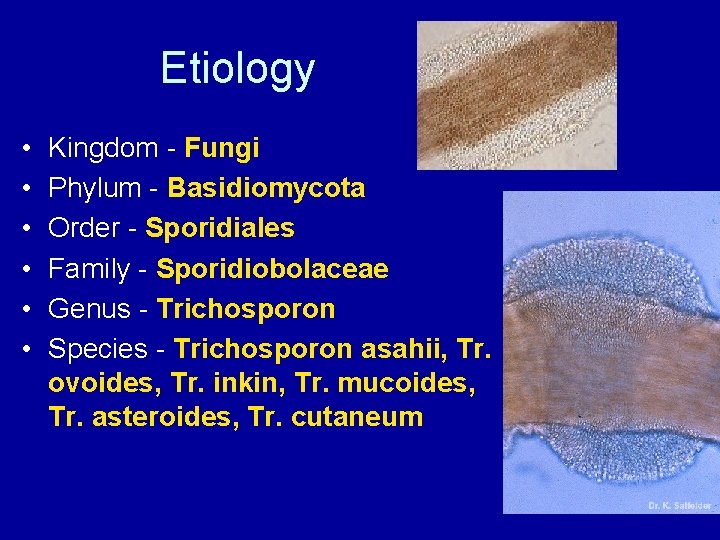
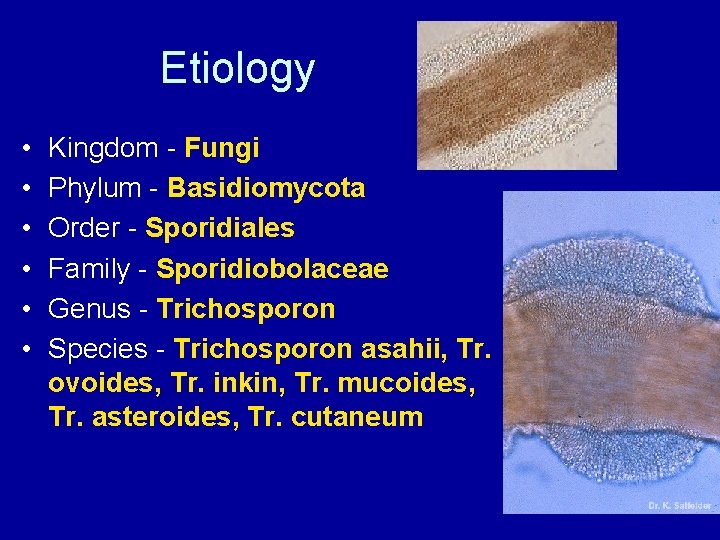
Etiology • • • Kingdom - Fungi Phylum - Basidiomycota Order - Sporidiales Family - Sporidiobolaceae Genus - Trichosporon Species - Trichosporon asahii, Tr. ovoides, Tr. inkin, Tr. mucoides, Tr. asteroides, Tr. cutaneum
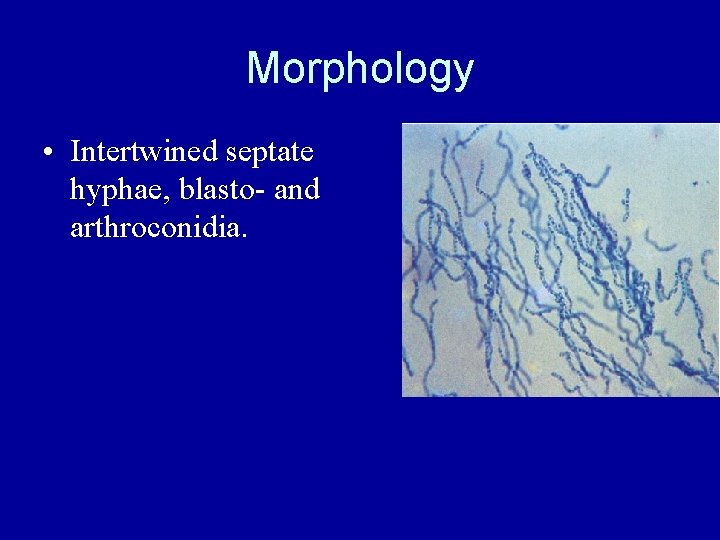
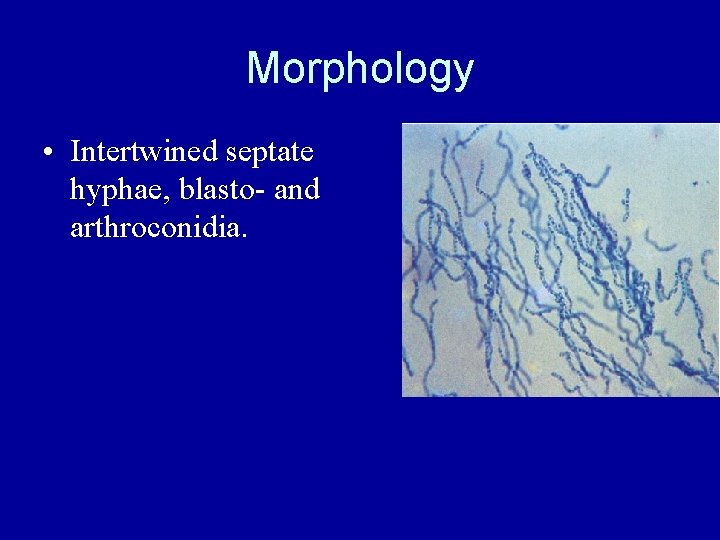
Morphology • Intertwined septate hyphae, blasto- and arthroconidia.
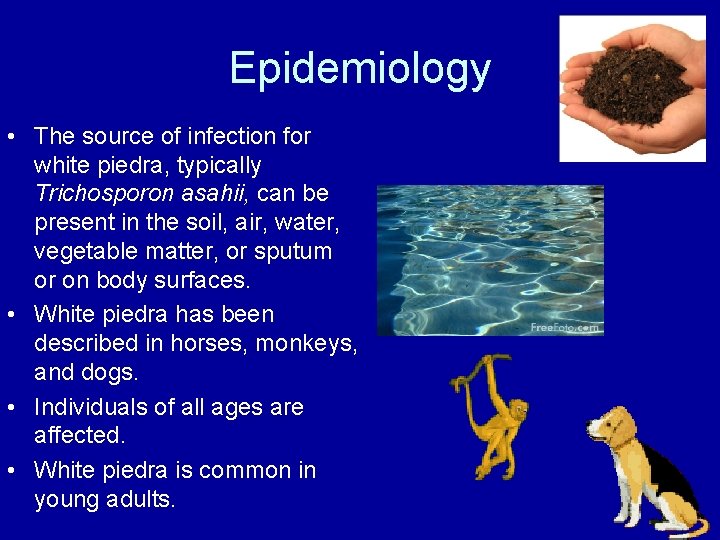
Epidemiology • The source of infection for white piedra, typically Trichosporon asahii, can be present in the soil, air, water, vegetable matter, or sputum or on body surfaces. • White piedra has been described in horses, monkeys, and dogs. • Individuals of all ages are affected. • White piedra is common in young adults.
Geographic White piedra is more common in temperate and semitropical climates, such as those in South America, Asia, Europe, Japan, and parts of the southern United States. White piedra is common in young adults. The presence of irregular, soft, white or light brown nodules, 1. 0 -1. 5 mm in length, firmly adhering to the hairs is characteristic of white piedra.
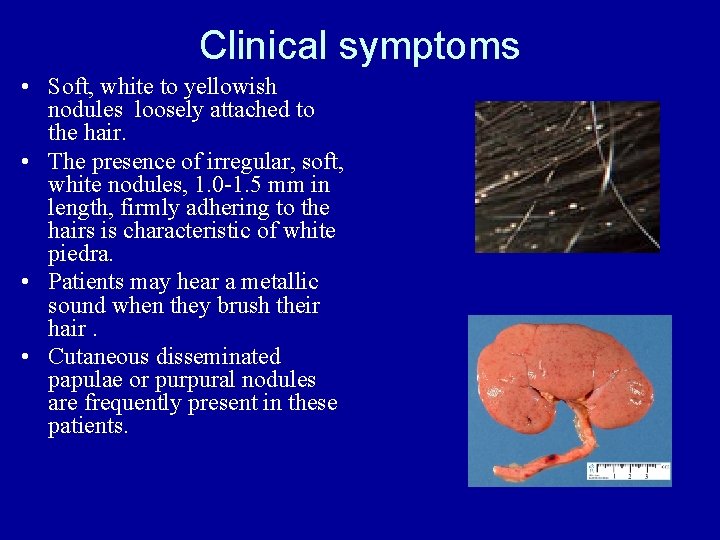
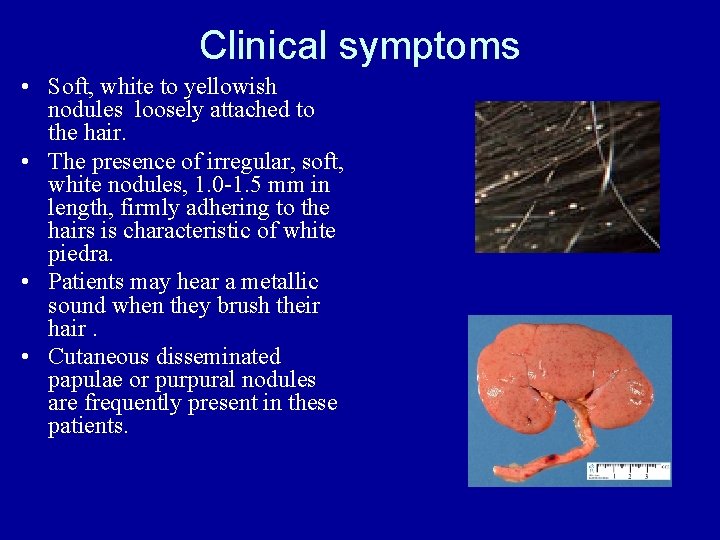
Clinical symptoms • Soft, white to yellowish nodules loosely attached to the hair. • The presence of irregular, soft, white nodules, 1. 0 -1. 5 mm in length, firmly adhering to the hairs is characteristic of white piedra. • Patients may hear a metallic sound when they brush their hair. • Cutaneous disseminated papulae or purpural nodules are frequently present in these patients.
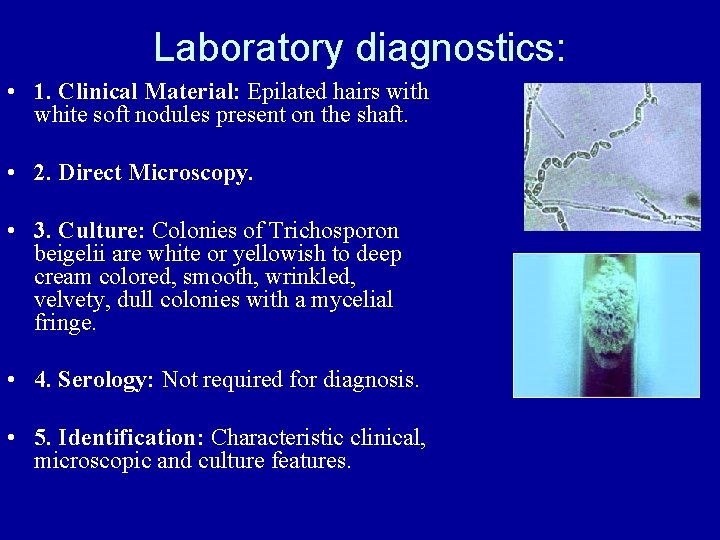
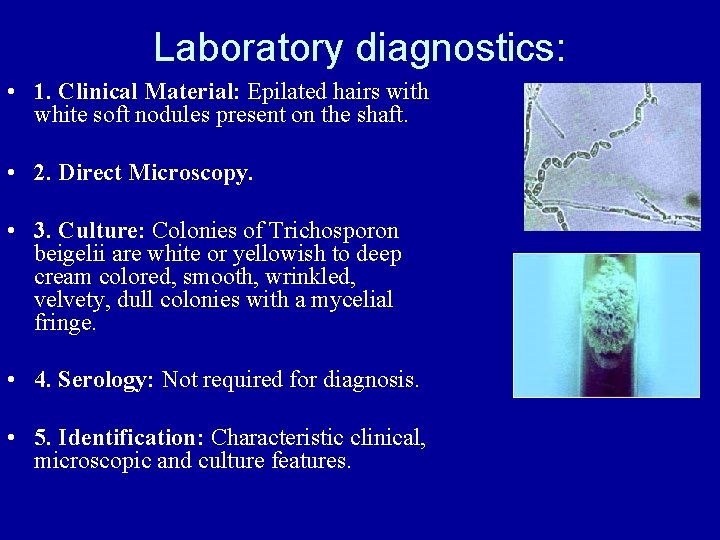
Laboratory diagnostics: • 1. Clinical Material: Epilated hairs with white soft nodules present on the shaft. • 2. Direct Microscopy. • 3. Culture: Colonies of Trichosporon beigelii are white or yellowish to deep cream colored, smooth, wrinkled, velvety, dull colonies with a mycelial fringe. • 4. Serology: Not required for diagnosis. • 5. Identification: Characteristic clinical, microscopic and culture features.

Treatment • Shaving the hairs is the simplest method of treatment. • Topical application of Ш an imidazole, Ш salycylic acid, Ш ciclopirox olamine, Ш selenium sulfide, Ш chlorhexidine solution, Ш Castellani paint, Ш zinc pyrithione, Ш Ketoconazole cream, Ш Econazole, Clotrimazole and amphotericin B lotion. • Oral therapy with either Ketoconazole or Terbinafine has also been used. However, relapse rates are high even after adequate therapy.
Prognosis: • The prognosis after treatment is good.
 Medically important fungi ppt
Medically important fungi ppt Zoonotic
Zoonotic Systemic mycoses
Systemic mycoses Tinea unguium
Tinea unguium Sofronio agustin
Sofronio agustin Astenopy
Astenopy Nsw health rto
Nsw health rto Piedraia hortae
Piedraia hortae Imagenes de tropezar con la misma piedra
Imagenes de tropezar con la misma piedra Slidetodoc.com
Slidetodoc.com Piedra angular cubo soma
Piedra angular cubo soma A una piedra se le imprime una velocidad inicial de 20m/s
A una piedra se le imprime una velocidad inicial de 20m/s Los socavones de pica leyenda
Los socavones de pica leyenda Las edades de la historia
Las edades de la historia Libro una mano ha sido cortada por completo
Libro una mano ha sido cortada por completo Merlín el encantador
Merlín el encantador Esporotricose
Esporotricose Molds unicellular or multicellular
Molds unicellular or multicellular Palabras que terminen con scopio
Palabras que terminen con scopio Escultura maya caracteristicas
Escultura maya caracteristicas Piedra branca
Piedra branca White piedra
White piedra Estructura de el burlador de sevilla
Estructura de el burlador de sevilla Consumir piedra
Consumir piedra Hidrogeologia
Hidrogeologia Piedra cúbica
Piedra cúbica Puente piedra
Puente piedra