Human immunodeficiency virus HIV is the causative organism






- Slides: 27

� Human immunodeficiency virus (HIV) is the causative organism of acquired immunodeficiency syndrome (AIDS) � HIV is a double stranded RNA virus belonging to the genus Lentivirus within the family Retroviridae
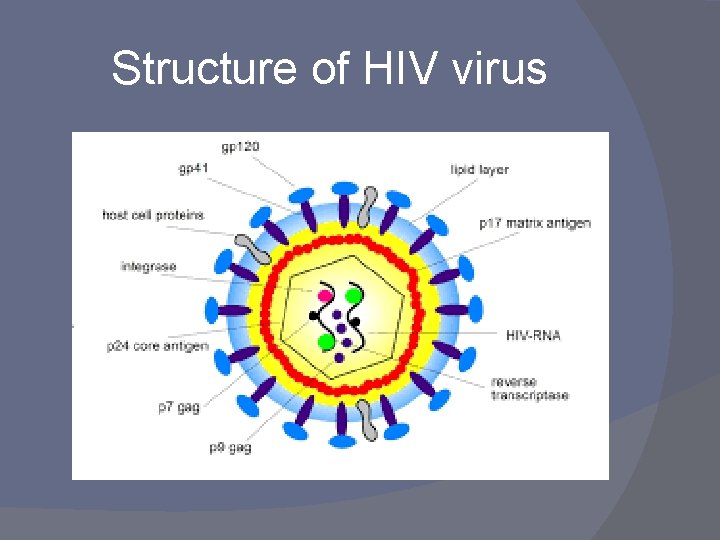
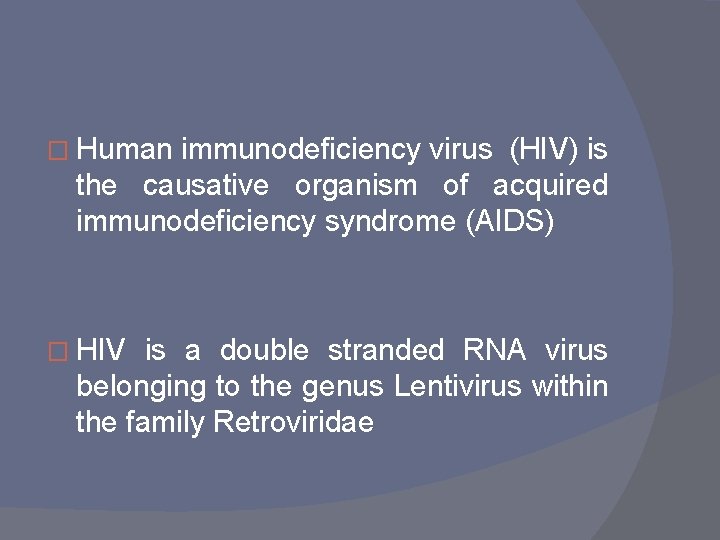
Structure of HIV virus
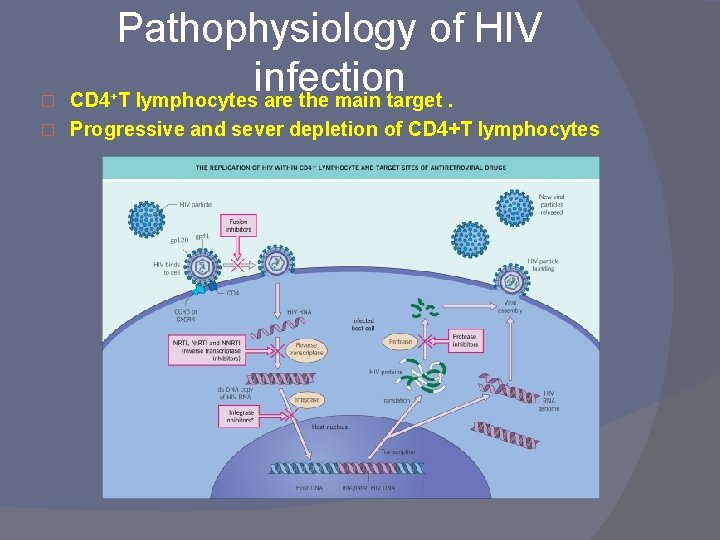
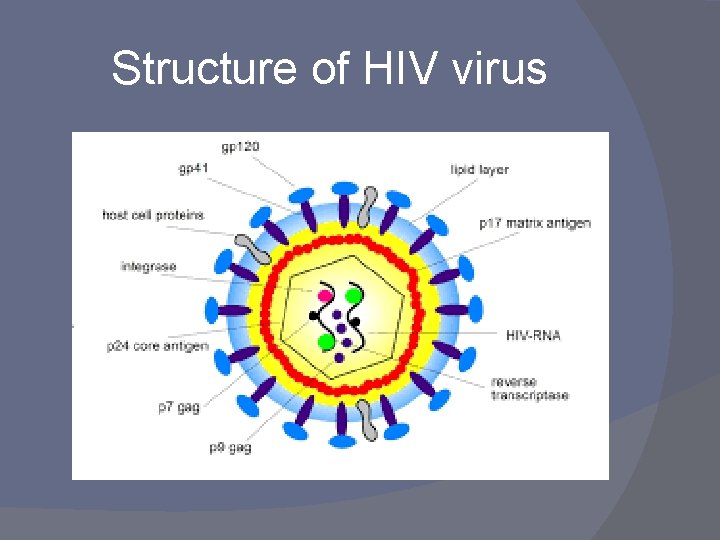
� Pathophysiology of HIV infection CD 4 T lymphocytes are the main target. � Progressive and sever depletion of CD 4+T lymphocytes +
Modes of transmission: � Sexual intercourse � Blood transfusion � Transplacental � Contaminated needle and syringes
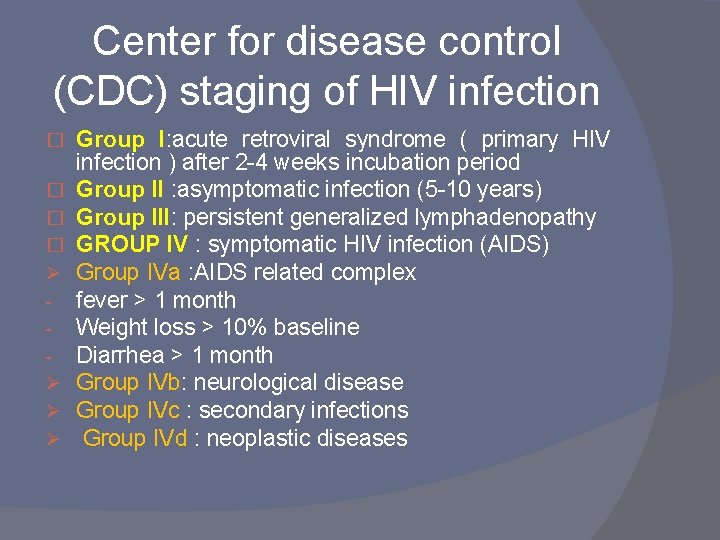
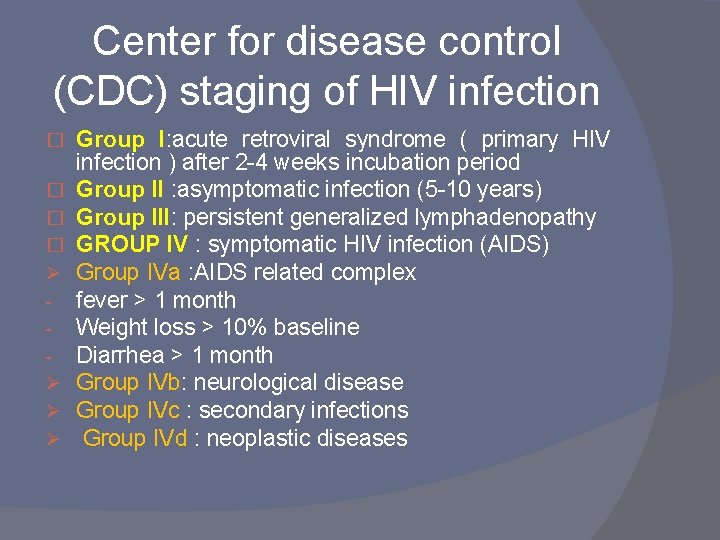
Center for disease control (CDC) staging of HIV infection � � Ø Ø Group I: acute retroviral syndrome ( primary HIV infection ) after 2 -4 weeks incubation period Group II : asymptomatic infection (5 -10 years) Group III: persistent generalized lymphadenopathy GROUP IV : symptomatic HIV infection (AIDS) Group IVa : AIDS related complex fever > 1 month Weight loss > 10% baseline Diarrhea > 1 month Group IVb: neurological disease Group IVc : secondary infections Group IVd : neoplastic diseases
Cutaneous manifestations of HIV infection Infection HIV related cutaneous disorders q Non infectious HIV related cutaneous disorders q Neoplastic HIV related cutaneous disorders q
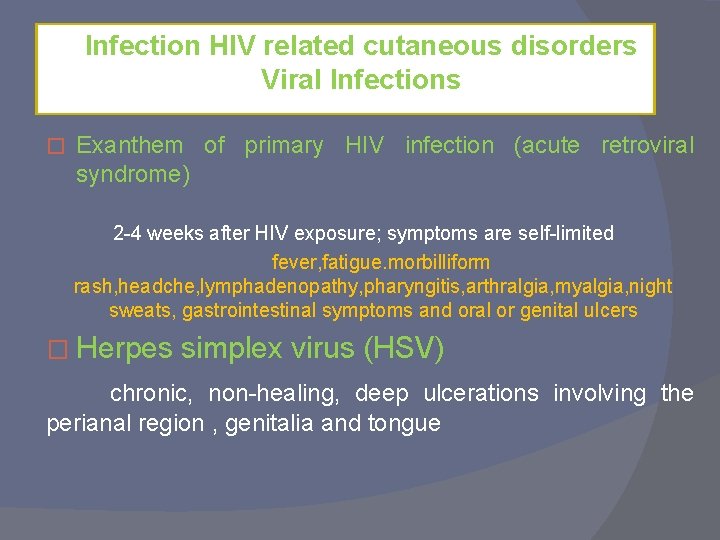
Infection HIV related cutaneous disorders Viral Infections � Exanthem of primary HIV infection (acute retroviral syndrome) 2 -4 weeks after HIV exposure; symptoms are self-limited fever, fatigue. morbilliform rash, headche, lymphadenopathy, pharyngitis, arthralgia, myalgia, night sweats, gastrointestinal symptoms and oral or genital ulcers � Herpes simplex virus (HSV) chronic, non-healing, deep ulcerations involving the perianal region , genitalia and tongue
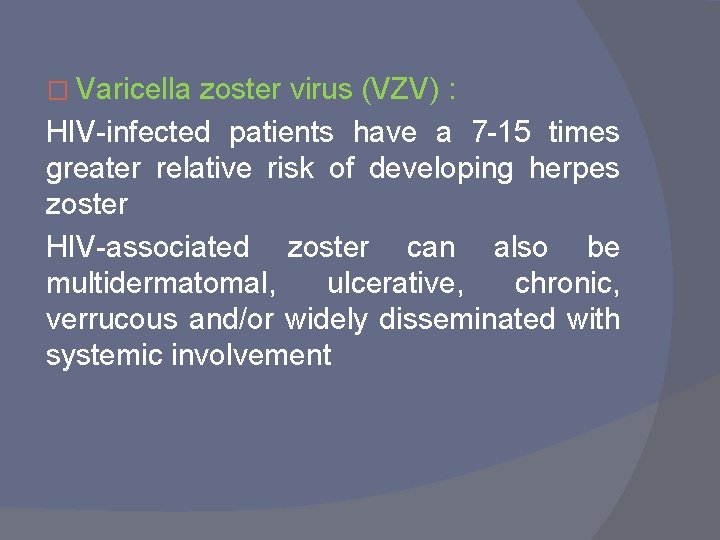
� Varicella zoster virus (VZV) : HIV-infected patients have a 7 -15 times greater relative risk of developing herpes zoster HIV-associated zoster can also be multidermatomal, ulcerative, chronic, verrucous and/or widely disseminated with systemic involvement
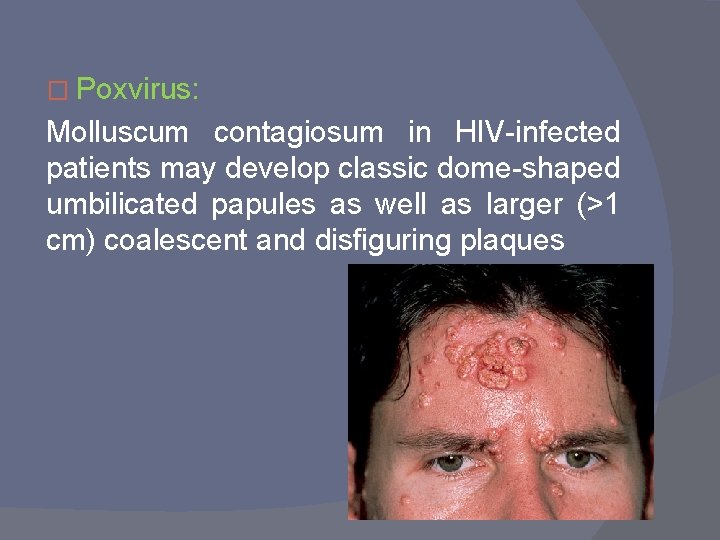
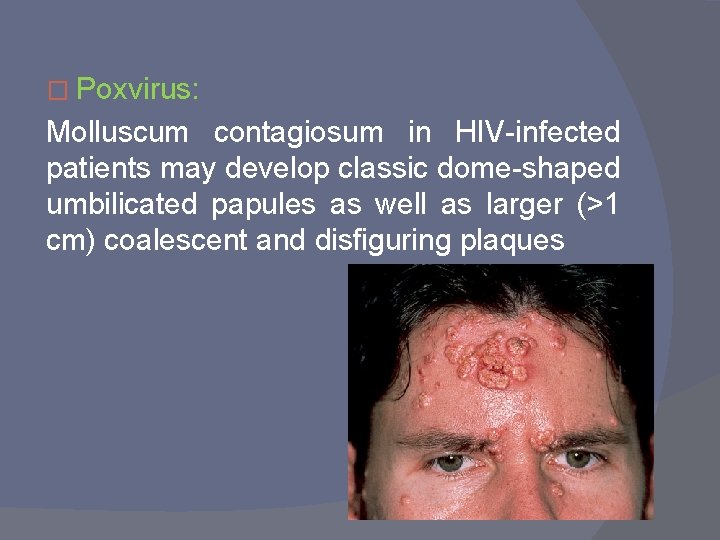
� Poxvirus: Molluscum contagiosum in HIV-infected patients may develop classic dome-shaped umbilicated papules as well as larger (>1 cm) coalescent and disfiguring plaques
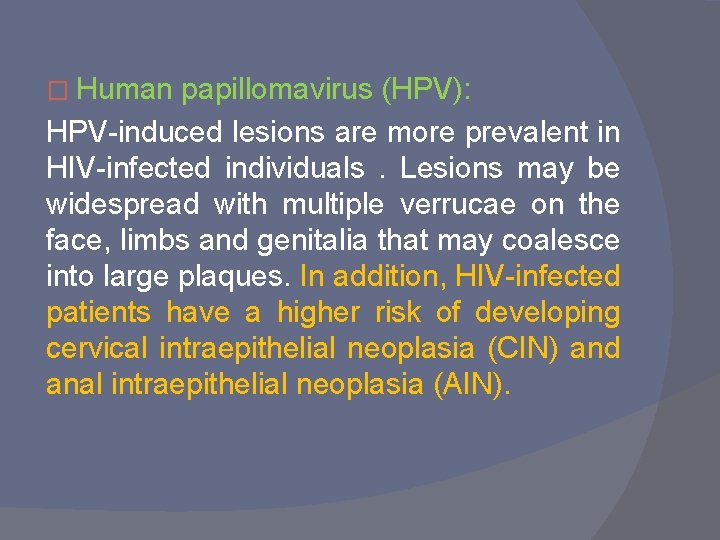
� Human papillomavirus (HPV): HPV-induced lesions are more prevalent in HIV-infected individuals. Lesions may be widespread with multiple verrucae on the face, limbs and genitalia that may coalesce into large plaques. In addition, HIV-infected patients have a higher risk of developing cervical intraepithelial neoplasia (CIN) and anal intraepithelial neoplasia (AIN).

Epstein–Barr virus (EBV): Oral hairy leukoplakia is an early sign of HIV infection that develops in approximately 25% of infected individuals. q The usually asymptomatic lesions appear as corrugated white plaques with hair-like projections along the lateral aspect of the tongue. q Lesions have no malignant potential � q
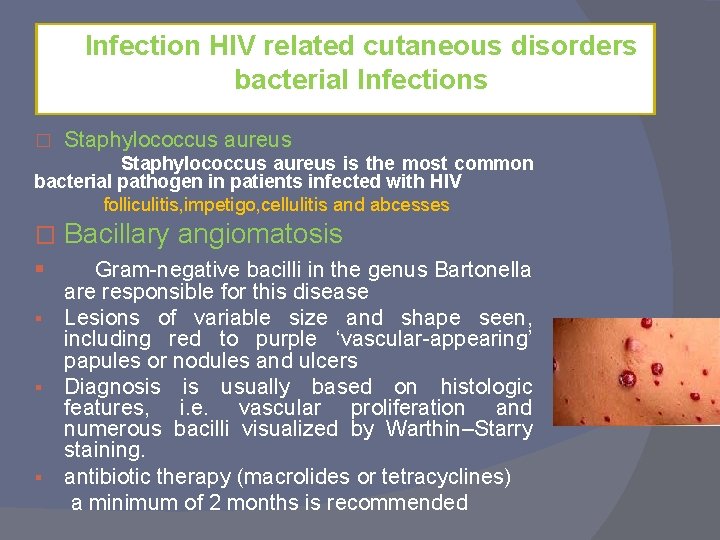
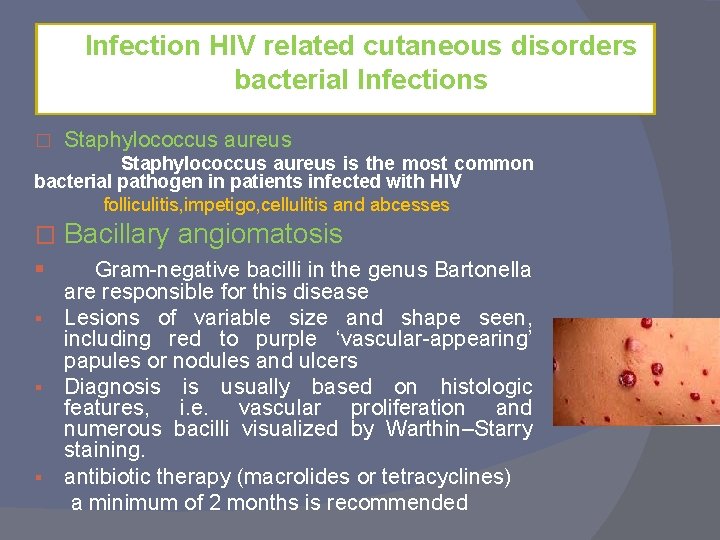
Infection HIV related cutaneous disorders bacterial Infections � Staphylococcus aureus is the most common bacterial pathogen in patients infected with HIV folliculitis, impetigo, cellulitis and abcesses � § Bacillary angiomatosis Gram-negative bacilli in the genus Bartonella are responsible for this disease § Lesions of variable size and shape seen, including red to purple ‘vascular-appearing’ papules or nodules and ulcers § Diagnosis is usually based on histologic features, i. e. vascular proliferation and numerous bacilli visualized by Warthin–Starry staining. § antibiotic therapy (macrolides or tetracyclines) a minimum of 2 months is recommended
Mycobacteria: Cutaneous tuberculosis can develop during advanced stages of HIV infection. Erythematous papules and nodules, ulcers, verrucous plaques and deep nodules can all be observed � Syphilis : Syphilis is caused by Treponema pallidum. Although the classic papulosquamous secondary lesions are often seen, unusual presentations may be observed in immunocompromised hosts, including rapidly progressive noduloulcerative forms, papular eruptions that mimic molluscum contagiosum, and lues maligna. Lues maligna is an aggressive, widespread variant of secondary syphilis with a prodrome of fever, headaches and myalgia, in association with a papulopustular eruption �
Infection HIV related cutaneous disorders fungal Infections Candidiasis is the fungal infection most frequently encountered in association with HIV infection Ninety percent of patients with AIDS will develop candidiasis of the oropharynx painful fissures at the oral commissures and persistent candidal infections of intertriginous zones are also seen in HIV-infected individuals. Other signs suggesting immune suppression include chronic paronychia, onychodystrophy, and refractory vaginal candidiasis. �
Dermatophytoses: Cutaneous involvement can be atypical in appearance, and lesions may be more widespread and resistant to therapy. � Systemic fungal infections : Disseminated cryptococcosis and histoplasmosis are seen most commonly, These infections present with a wide range of morphologies, including pustules, papulonodules, and less often, patches, plaques and mucocutaneous ulcerations � Pneumocystis jiroveci: Disseminated cutaneous P. jiroveci infection is extremely rare and may appear as molluscum contagiosum-like papules, bluish cellulitic plaques, and/or deeply seated abscesses in the external auditory canal or nares intravenous trimethoprim– sulfamethoxazole (TMP-SMX) is given for disseminated Pneumocystis infection �
Infection HIV related cutaneous disorders Parasitic Infections Leishmaniasis Multiple organs may be parasitized, and, when the skin is involved, the lesions typically present as ulcerated nodules (up to 2 cm in diameter) on the extremities; in atypical presentations, the lesions are disseminated. Erosions and ulcerations of the lips, palate and nasal mucosa can also be seen �

Infection HIV related cutaneous disorders Ectoparasitic Infections Scabies : it may be more sever and extensive in AIDS patients with involvement of atypical sites like face � Crusted scabies is more common with advanced immunosuppresion with thick crusted plaques on the hands and feet , subungual debris and gross nail thickening
Non infectious HIV related cutaneous disorders � Seborrheic dermatitis : Seborrheic dermatitis is the most common skin disorder to affect HIV-infected individuals (up to 85%) and is seen in all stages of the disease. Clinical findings may be similar to those seen in the general population, i. e. erythema and yellowish scale on the face as well as involvement of extrafacial locations such as the central chest and inguinal creases. However, exaggerated presentations with obvious facial plaques can also occur and should raise the possibility of HIV infection, as should a sudden onset or acute worsening of seborrheic dermatitis.
Non infectious HIV related cutaneous disorders � Psoriasis: The overall incidence of psoriasis is probably not increased in the setting of HIV infection, although its clinical presentation can be sever. An ‘inverse’ distribution involving inguinal creases and genitalia may be observed it may be associated with significant nail dystrophy, arthritis. HIV-associated psoriasis may be refractory to topical therapies, systemic retinoids or phototherapy may be required Immunosuppressive agents such as methotrexate and cyclosporine should be avoided, if possible, in HIV-infected patients
Non infectious HIV related cutaneous disorders A generalized xerosis can be seen in HIV-infected patients and may be associated with refractory pruritus � generalized acquired ichthyosis with large plate-like scales may develop, beginning on the legs. ). � Pityriasis rubra pilaris can also occur in conjunction with HIV infection. � Papular pruritic eruption of AIDS Papular pruritic eruption (PPE) of AIDS is characterized by marked pruritus and a greater involvement of the extremities than the trunk or face. Some authors believe PPE represents an exaggerated response to arthropod antigens. Clinically, the lesions are symmetrically distributed, non-follicular papules, often with secondary changes (e. g. excoriations, formation of prurigo nodularis). �
Non infectious HIV related cutaneous disorders � Eosinophilic folliculitis is one of the most characteristic and common pruritic dermatoses associated with HIV disease One theory is that it is an exaggerated reaction to Malassezia yeast or other organisms normally present within the follicular infundibula in HIV-infected patients and is a reflection of abnormal Th 2/Th 1 immune responses. Excoriated follicular papules and rare intact pustules are found primarily on the face and upper trunk. Cultures are negative and peripheral eosinophilia may be present. CD 4+counts are usually <200 cells per cubic millimeter

Neoplastic HIV related cutaneous disorders Squamous and basal cell carcinoma: In HIV-infected individuals, as compared with the general population, these tumors appear earlier and more often in sites such as the trunk and extremities � Lymphomas: Unlike in immunocompetent patients, most lymphomas are non-Hodgkin B-cell type, Additional differences include a younger age of onset, more advanced stages and, most importantly, extranodal involvement at presentation, in particular the CNS, intestine and skin �
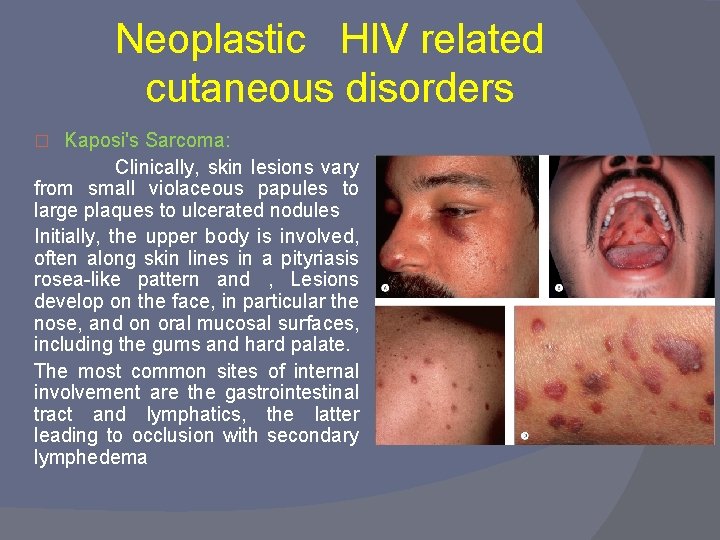
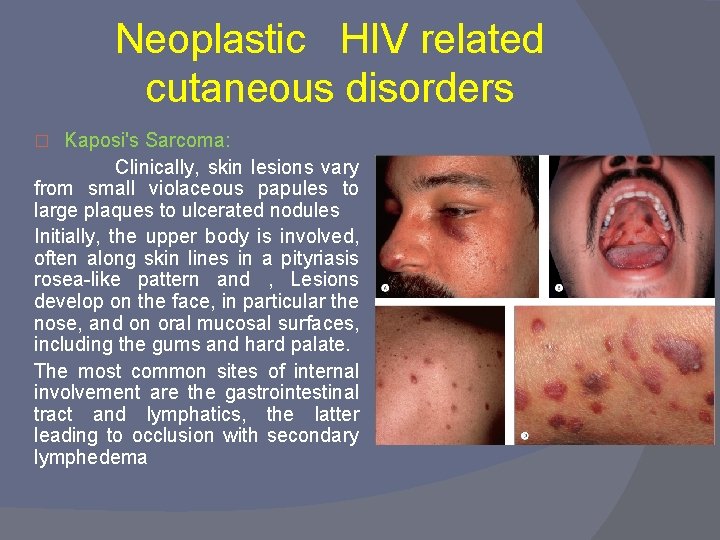
Neoplastic HIV related cutaneous disorders Kaposi's Sarcoma: Clinically, skin lesions vary from small violaceous papules to large plaques to ulcerated nodules Initially, the upper body is involved, often along skin lines in a pityriasis rosea-like pattern and , Lesions develop on the face, in particular the nose, and on oral mucosal surfaces, including the gums and hard palate. The most common sites of internal involvement are the gastrointestinal tract and lymphatics, the latter leading to occlusion with secondary lymphedema �
� v v v Laboratory investigations : ELISA for the dettection of Ig. G antibody to envelope glycoprotien gp 120 Non-reactive results are obtained during a seronegative ‘window’ that usually lasts 1 -3 months after the initial infection. Thus, if HIV infection is strongly suspected, methods for detection of viral antigens rather than anti. HIV antibodies need to be employed HIV p 24 antigen test PCR for the detection of HIV nucleic acid CD 4 count is low , CD 4/CD 8 is less than one

� v v v Treatment : nucleoside reverse transcriptase inhibitors (zidovudine, lamivudine) non-nucleoside reverse transcriptase inhibitor (nevirapine) Protease inhibitors ( indinavir) Fusion inhibitor the most important was the development of a combination drug regimen known as HAART. Of the various HAART regimens, the most common ones comprise two nucleoside reverse transcriptase inhibitors (NRTIs) combined with either a protease inhibitor or a nonnucleoside reverse transcriptase inhibitor (NNRTI)

Thank you
 Causative organism of hiv/aids
Causative organism of hiv/aids Secondary immunodeficiency diseases
Secondary immunodeficiency diseases Severe combined immunodeficiency
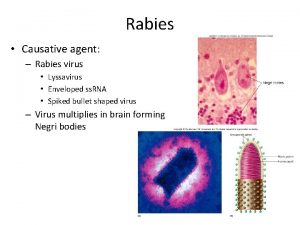
Severe combined immunodeficiency Rabies causative organism
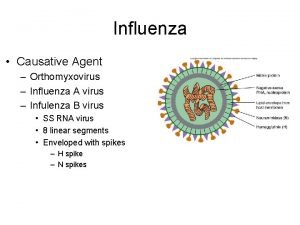
Rabies causative organism Influenza a causative agent
Influenza a causative agent Virus hiv
Virus hiv Hiv virus
Hiv virus Why does organism eat another organism
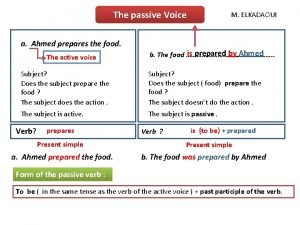
Why does organism eat another organism Causative verbs formula
Causative verbs formula Causative
Causative Causative passive
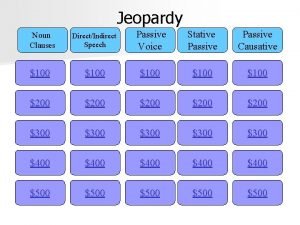
Causative passive Unit 15 class 11 english grammar
Unit 15 class 11 english grammar Causative have engleski
Causative have engleski Example of causative form
Example of causative form The teacher made juan leave the room
The teacher made juan leave the room Causative make
Causative make Causative have and get
Causative have and get Krashens theory
Krashens theory Stative passive voice
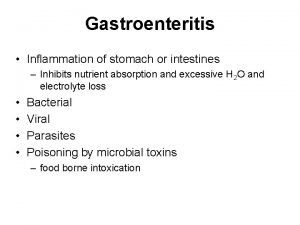
Stative passive voice Gastroenteritis
Gastroenteritis Passive voice about food
Passive voice about food Causative form
Causative form Causative agent malaria
Causative agent malaria Indirect speech passive voice
Indirect speech passive voice Kernig's sign
Kernig's sign Quang trung
Quang trung Where did hiv come from
Where did hiv come from Test wiedzy o hiv i aids z odpowiedziami
Test wiedzy o hiv i aids z odpowiedziami