Stay negat HIVe AIDS HIV AND AIDS Human














- Slides: 72
#Stay negat. HIVe -AIDS
HIV AND AIDS Human immunodeficiency virus infection and acquired immune deficiency syndrome is a spectrum of conditions caused by infection with the HIV virus. A syndrome in which there is severe loss of the body’s cellular immunity, greatly lowering the resistance to infections and malignancy.
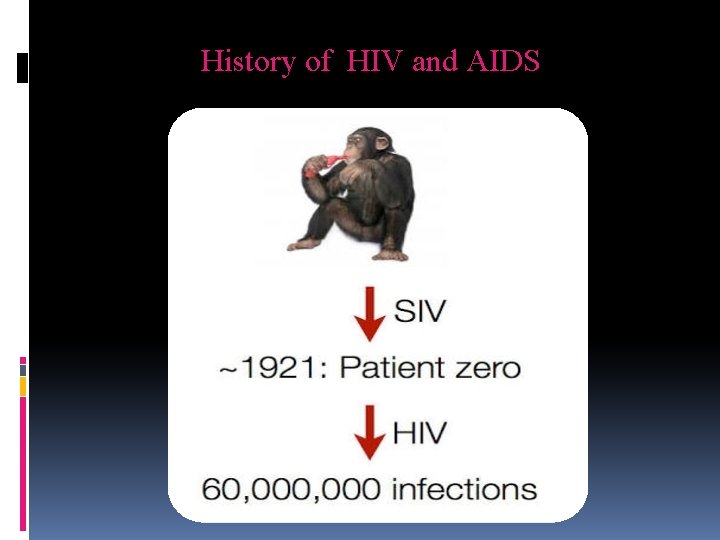
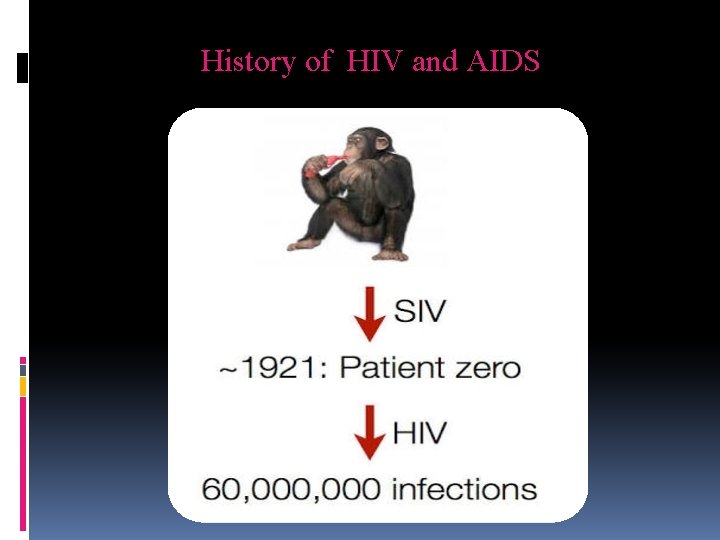
History of HIV and AIDS
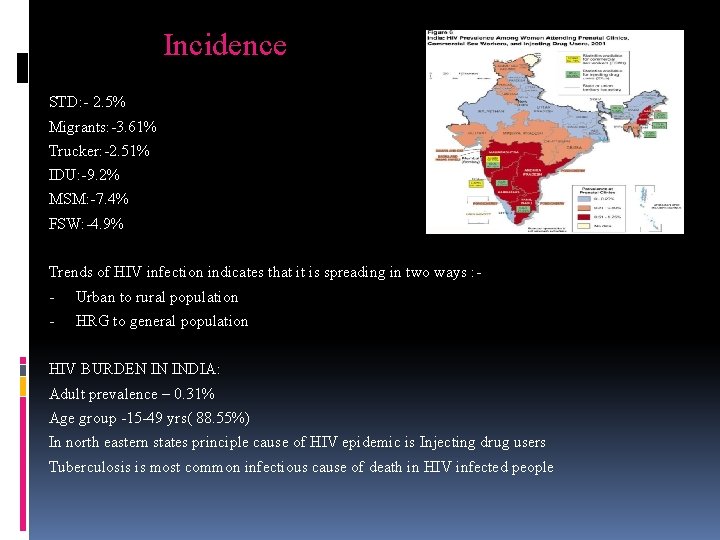
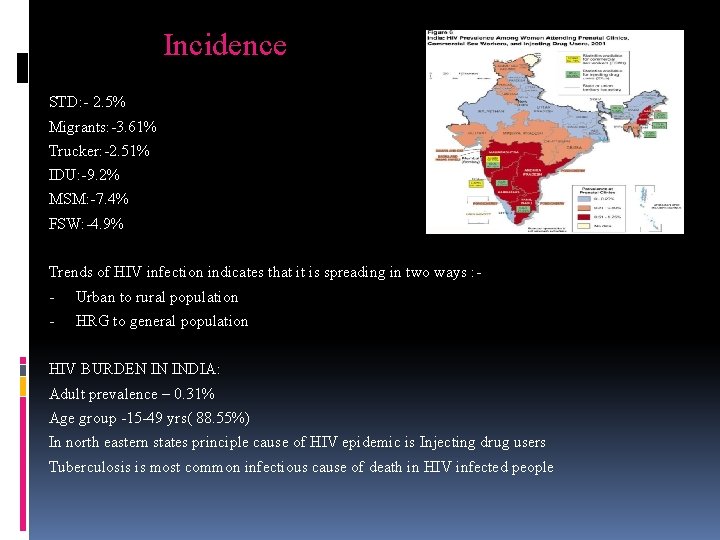
Incidence STD: - 2. 5% Migrants: -3. 61% Trucker: -2. 51% IDU: -9. 2% MSM: -7. 4% FSW: -4. 9% Trends of HIV infection indicates that it is spreading in two ways : - Urban to rural population - HRG to general population HIV BURDEN IN INDIA: Adult prevalence – 0. 31% Age group -15 -49 yrs( 88. 55%) In north eastern states principle cause of HIV epidemic is Injecting drug users Tuberculosis is most common infectious cause of death in HIV infected people
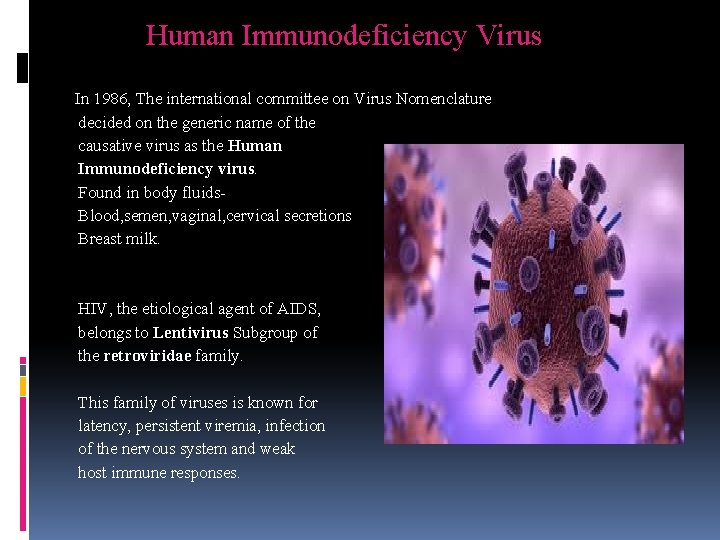
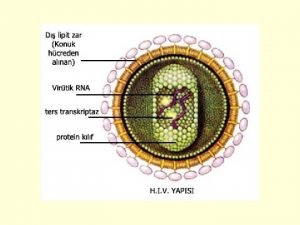
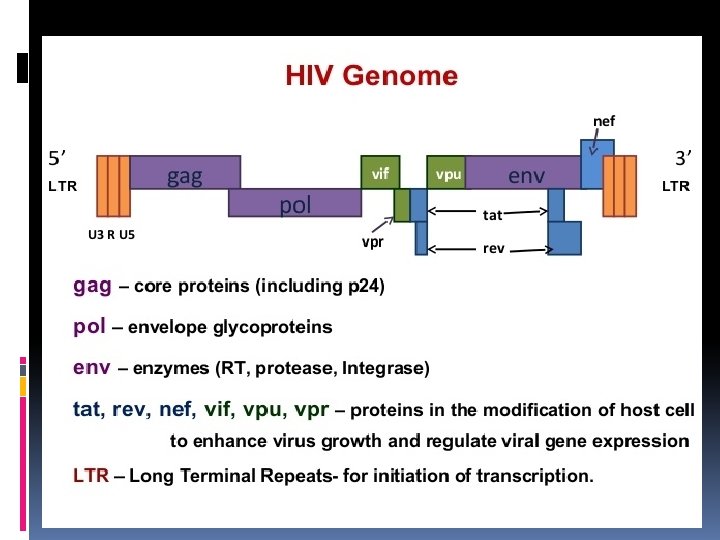
Human Immunodeficiency Virus In 1986, The international committee on Virus Nomenclature decided on the generic name of the causative virus as the Human Immunodeficiency virus. Found in body fluids. Blood, semen, vaginal, cervical secretions Breast milk. HIV, the etiological agent of AIDS, belongs to Lentivirus Subgroup of the retroviridae family. This family of viruses is known for latency, persistent viremia, infection of the nervous system and weak host immune responses.
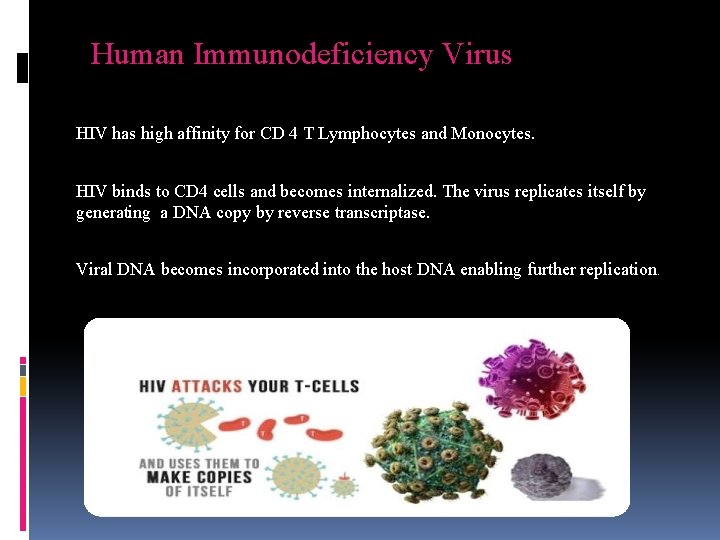
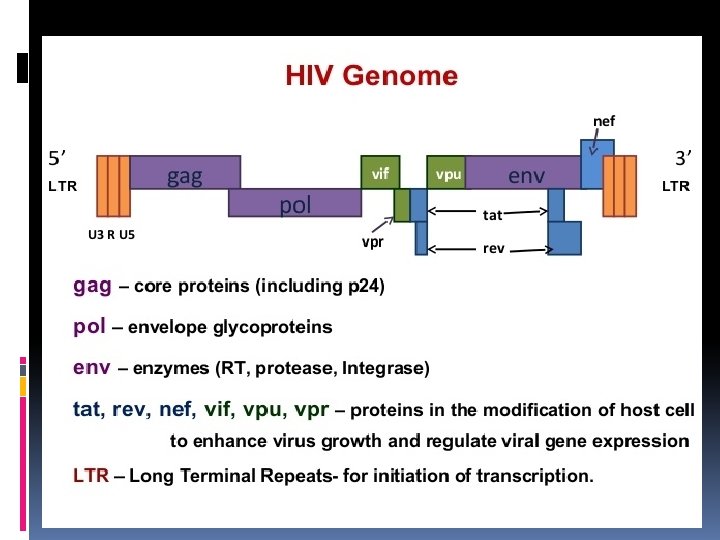
Human Immunodeficiency Virus HIV has high affinity for CD 4 T Lymphocytes and Monocytes. HIV binds to CD 4 cells and becomes internalized. The virus replicates itself by generating a DNA copy by reverse transcriptase. Viral DNA becomes incorporated into the host DNA enabling further replication.
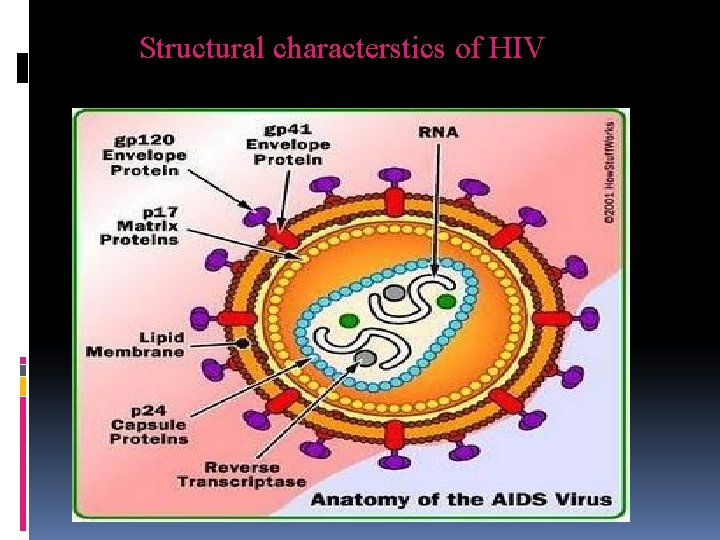
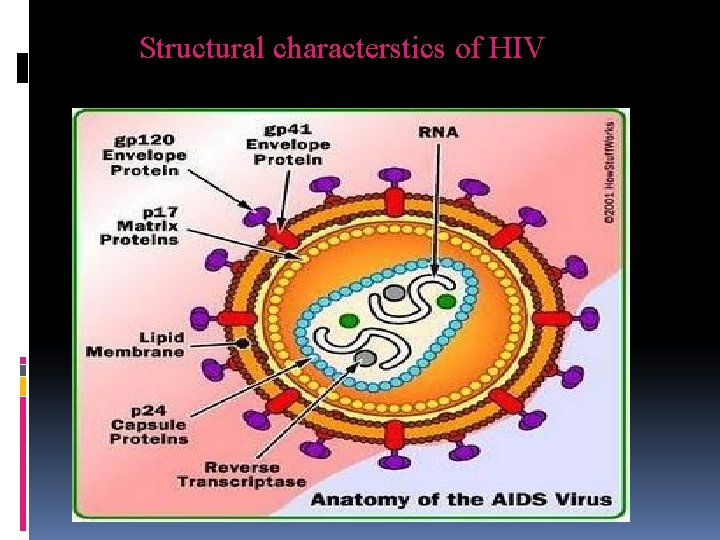
Structural characterstics of HIV
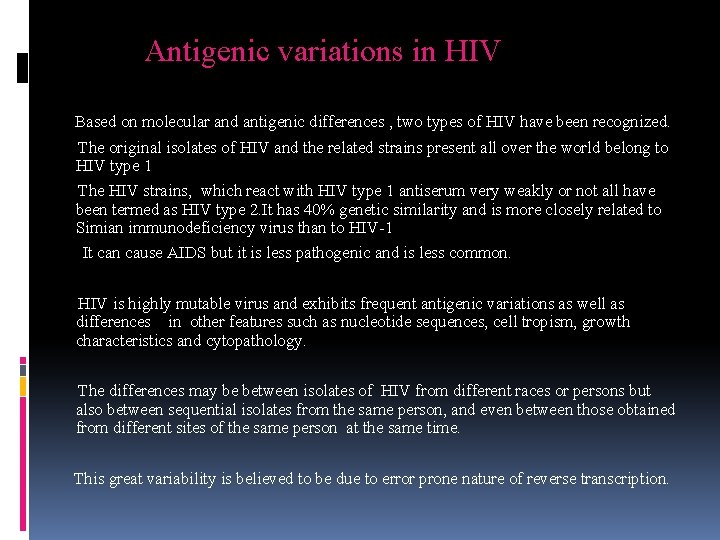
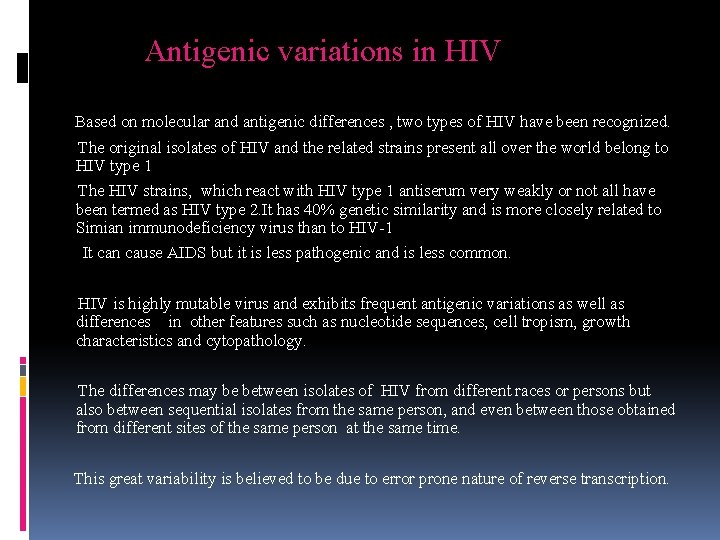
Antigenic variations in HIV Based on molecular and antigenic differences , two types of HIV have been recognized. The original isolates of HIV and the related strains present all over the world belong to HIV type 1 The HIV strains, which react with HIV type 1 antiserum very weakly or not all have been termed as HIV type 2. It has 40% genetic similarity and is more closely related to Simian immunodeficiency virus than to HIV-1 It can cause AIDS but it is less pathogenic and is less common. HIV is highly mutable virus and exhibits frequent antigenic variations as well as differences in other features such as nucleotide sequences, cell tropism, growth characteristics and cytopathology. The differences may be between isolates of HIV from different races or persons but also between sequential isolates from the same person, and even between those obtained from different sites of the same person at the same time. This great variability is believed to be due to error prone nature of reverse transcription.
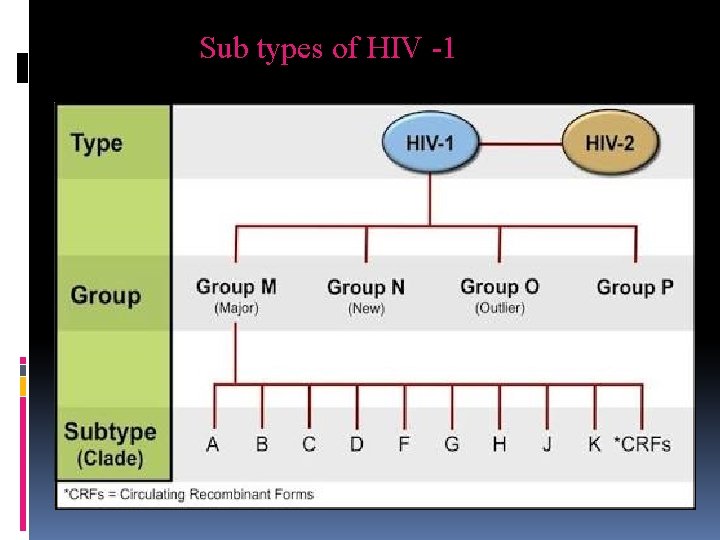
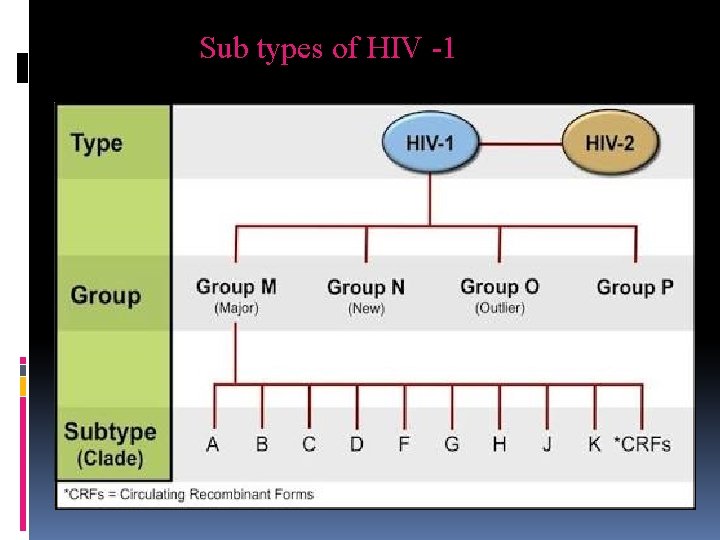
Sub types of HIV -1

How do you get HIV?


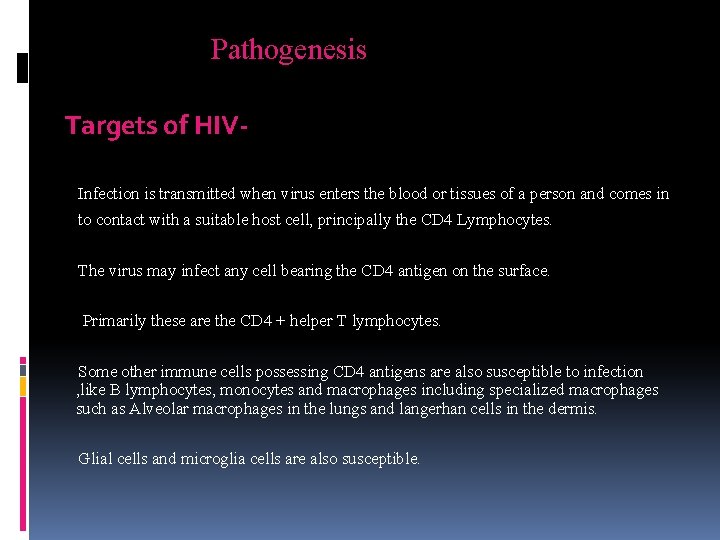
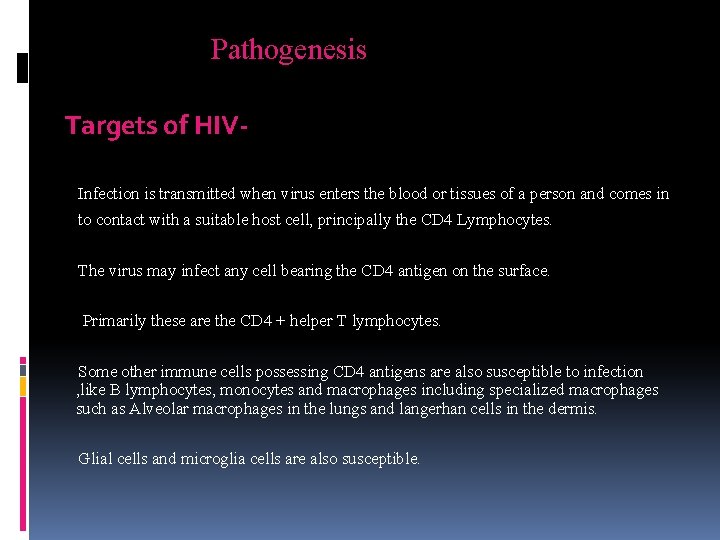
Pathogenesis Targets of HIVInfection is transmitted when virus enters the blood or tissues of a person and comes in to contact with a suitable host cell, principally the CD 4 Lymphocytes. The virus may infect any cell bearing the CD 4 antigen on the surface. Primarily these are the CD 4 + helper T lymphocytes. Some other immune cells possessing CD 4 antigens are also susceptible to infection , like B lymphocytes, monocytes and macrophages including specialized macrophages such as Alveolar macrophages in the lungs and langerhan cells in the dermis. Glial cells and microglia cells are also susceptible.
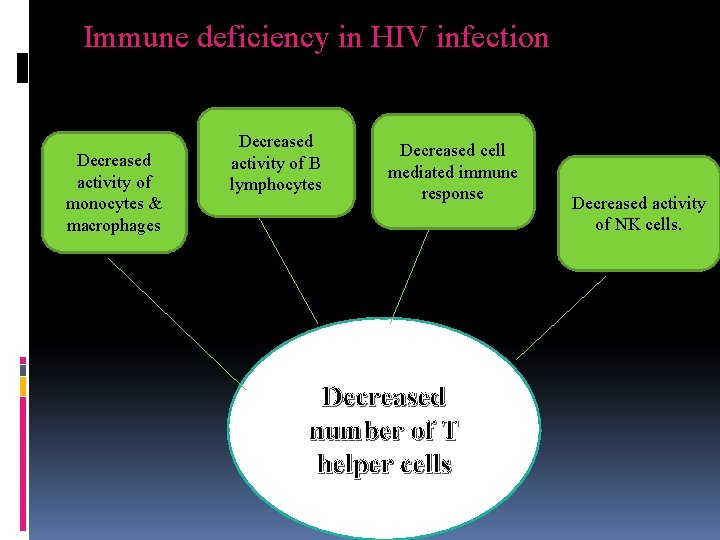
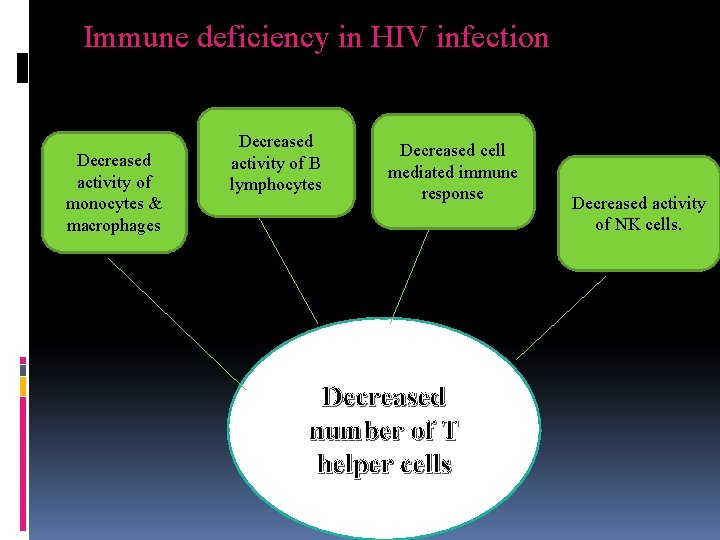
Immune deficiency in HIV infection Decreased activity of monocytes & macrophages Decreased activity of B lymphocytes Decreased cell mediated immune response Decreased number of T helper cells Decreased activity of NK cells.
INCUBATION PERIOD i. The incubation period is from HIV infection till development of AIDS. ii. It is from few months to 10 years or even more. iii. However it is estimated that 75% of people infected with HIV will develop AIDS at the end of 10 years.
Clinical Manifestations 1. Acute HIV infection. 2. Asymptomatic or Latent Infection. 3. Persistent generalized Lymphadenopathy (PGL) 4. AIDS related complex. 5. Full blown AIDS( Last stage).
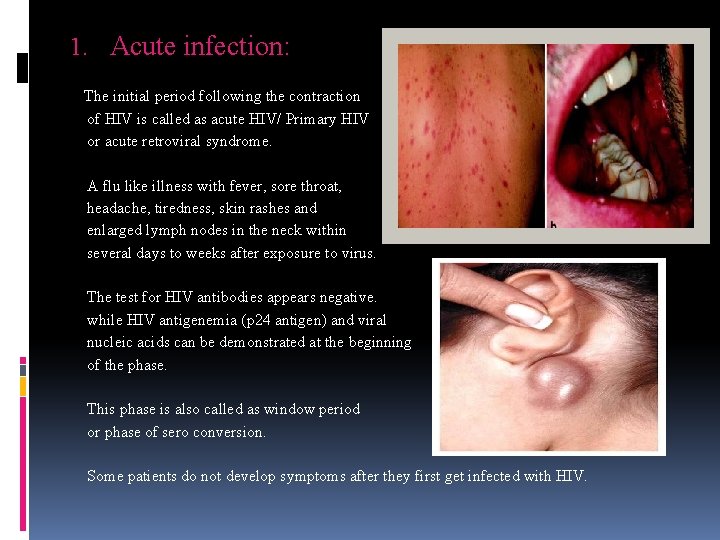
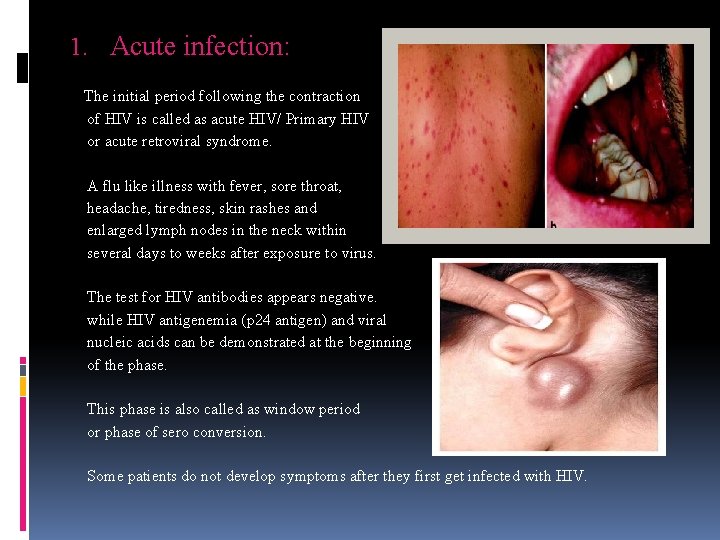
1. Acute infection: The initial period following the contraction of HIV is called as acute HIV/ Primary HIV or acute retroviral syndrome. A flu like illness with fever, sore throat, headache, tiredness, skin rashes and enlarged lymph nodes in the neck within several days to weeks after exposure to virus. The test for HIV antibodies appears negative. while HIV antigenemia (p 24 antigen) and viral nucleic acids can be demonstrated at the beginning of the phase. This phase is also called as window period or phase of sero conversion. Some patients do not develop symptoms after they first get infected with HIV.

2. Asymptomatic or Latent infection v The initial symptoms are followed by a stage called Asymptomatic or latent infection v Typically there are few or no symptoms at first, near the end of this stage many people experience fever, weight loss, GIT problems and muscle pains, Generalized Lymphadenopathy, characterized by non painful enlargement of more than one group of lymph nodes for 3 -6 months. v This state may last from few months to more than 10 years. v During this phase the virus continues to multiply actively infects, and kills the cells of the immune system. CD 4 count is greater than 500 per microlitre. v The patients show positive antibody tests during this phase. v About 5 -10% of the infected appear to escape clinical AIDS for 15 years or more and are known as ‘ long term survivors’ or ‘long term non progressors’.

3. Persistent generalized lymphadenopathy (PGL) Ø This has been defined by presence of enlarged lymph nodes, atleast 1 cm in diameter , in two or more non contiguous extra inguinal sites, that persist for atleast three months, in the absence of any current illness or medication that may cause lymphadenopathy. Ø CD 4 count is less than 500 per microlitre Ø These are diagnostic of HIV when blood tests are positive for antibodies.
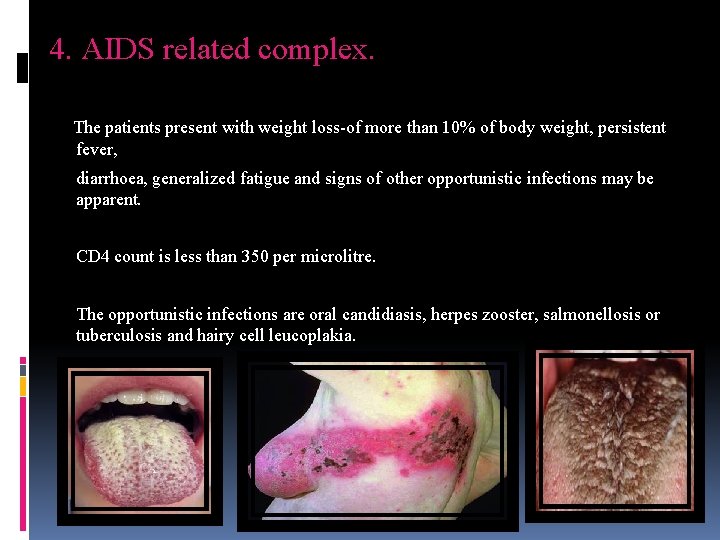
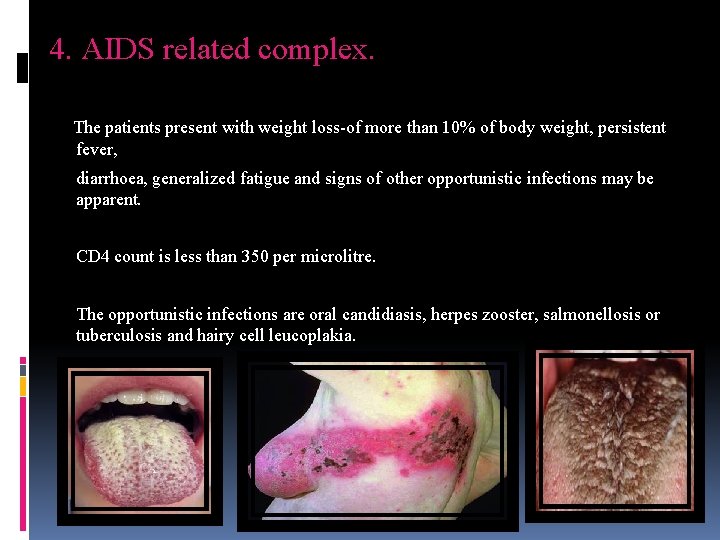
4. AIDS related complex. The patients present with weight loss-of more than 10% of body weight, persistent fever, diarrhoea, generalized fatigue and signs of other opportunistic infections may be apparent. CD 4 count is less than 350 per microlitre. The opportunistic infections are oral candidiasis, herpes zooster, salmonellosis or tuberculosis and hairy cell leucoplakia.

5. Full blown AIDS This is the end stage disease representing the irreversible break down of immune defense mechanisms. CD 4 count is less than 200 per microlitre. In addition to the opportunistic infections the patient may develop primary CNS Lymphomas And progressive multifocal leuko encephalopathy, dementia and other neurological abnormilities. Kaposi sarcoma, pneumocystis pneumonia and candidiasis of oesophagus, trachea are almost always observed in a majority of patients.

AIDS in children Infants who are seropositive at 18 months are infected Infants progress to AIDS more rapildy usually in 3 years. Transmission is usually perinatal 100% are HIV positive at birth THREE STAGESStage 1 -Asymptomatic, Generalized lymphadenopathy Stage 2 -Chronic diarrhoea, weight loss, fever, bacterial infections. Stage 3 -Oppotunistic infections, Failure to thrive, malignancy, septicaemia, meningitis
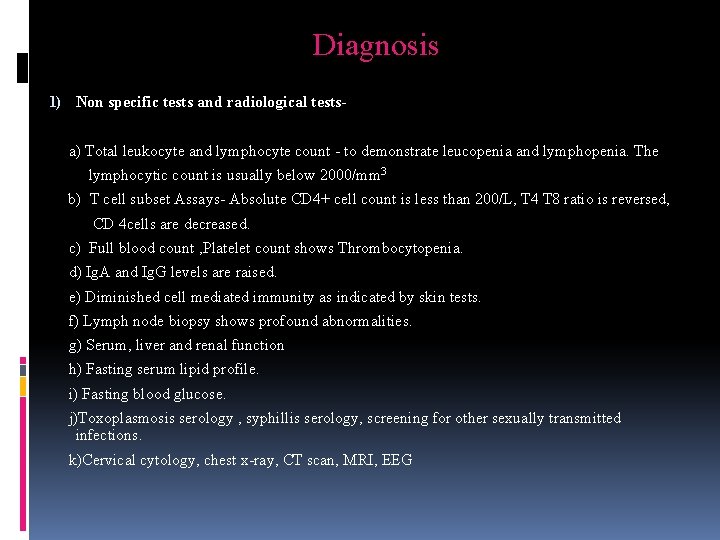
Diagnosis 1) Non specific tests and radiological tests- a) Total leukocyte and lymphocyte count - to demonstrate leucopenia and lymphopenia. The lymphocytic count is usually below 2000/mm 3 b) T cell subset Assays- Absolute CD 4+ cell count is less than 200/L, T 4 T 8 ratio is reversed, CD 4 cells are decreased. c) Full blood count , Platelet count shows Thrombocytopenia. d) Ig. A and Ig. G levels are raised. e) Diminished cell mediated immunity as indicated by skin tests. f) Lymph node biopsy shows profound abnormalities. g) Serum, liver and renal function h) Fasting serum lipid profile. i) Fasting blood glucose. j)Toxoplasmosis serology , syphillis serology, screening for other sexually transmitted infections. k)Cervical cytology, chest x-ray, CT scan, MRI, EEG
2) Specific tests for HIV infection- *HIV antigen *Antibodies *Viral nucleic acids or other components *Isolation of virus.
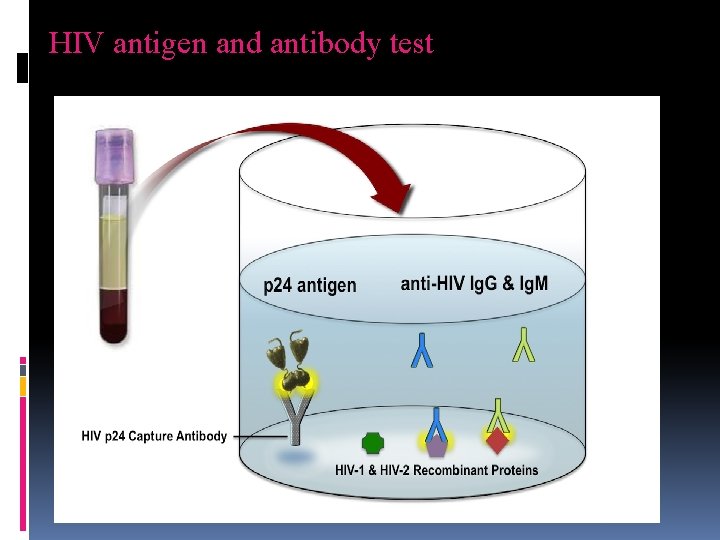
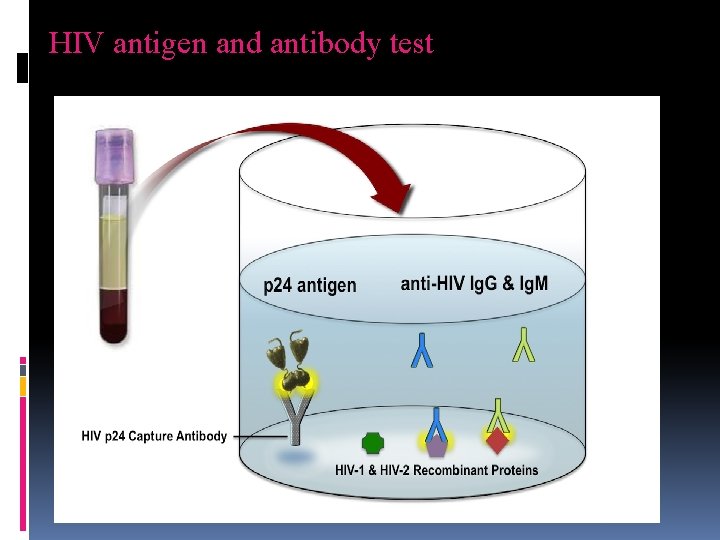
HIV antigen and antibody test
Screening tests ELISAFirst generation- whole viral lysates Second generation- glycopeptides Third generation- synthetic peptide Fourth generation- antigen + antibody Significance of ELISAAntibody can be detected in a majority of individuals within 6 -12 weeks after infection using the generation of assays. It can be detected within 3 -4 weeks when using the newer third generation ELISA. Due to their ability to detect p 24 antigen, the fourth generation ELISA can be of value in detecting early infection.
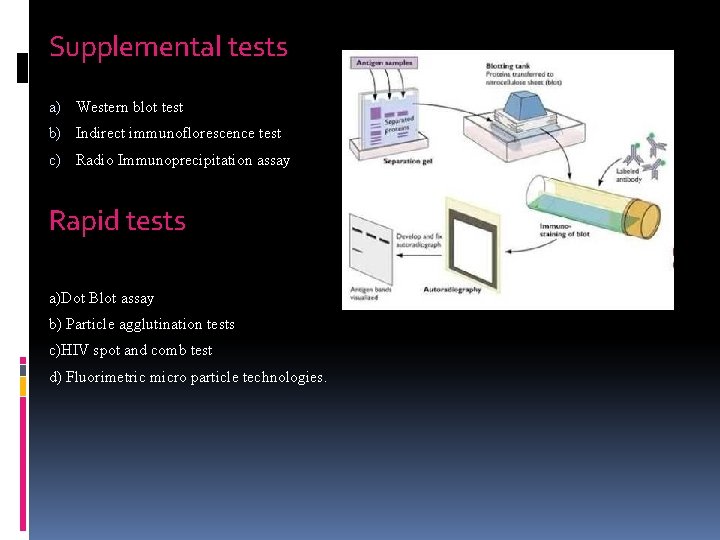
Supplemental tests a) Western blot test b) Indirect immunoflorescence test c) Radio Immunoprecipitation assay Rapid tests a)Dot Blot assay b) Particle agglutination tests c)HIV spot and comb test d) Fluorimetric micro particle technologies.
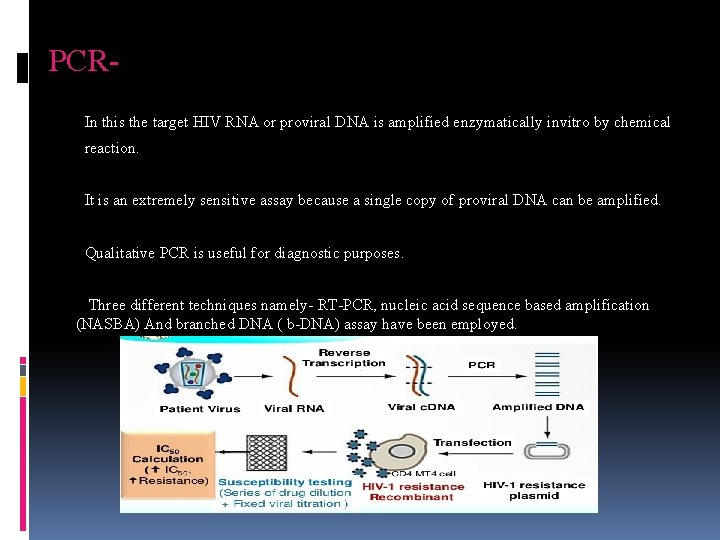
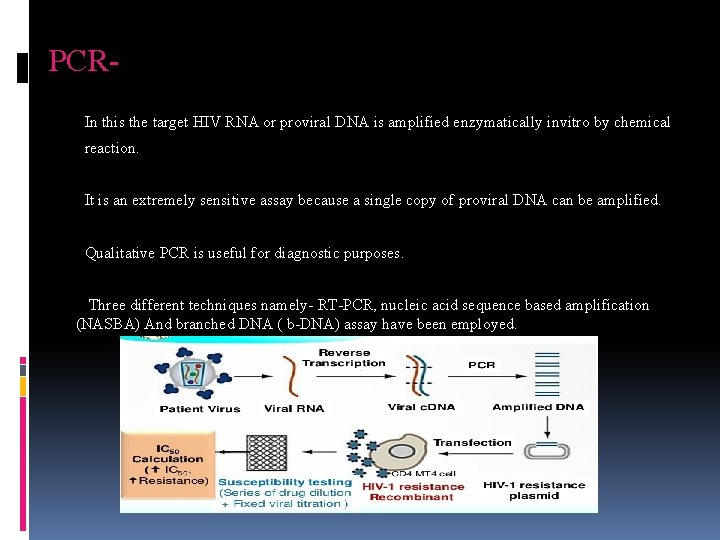
PCRIn this the target HIV RNA or proviral DNA is amplified enzymatically invitro by chemical reaction. It is an extremely sensitive assay because a single copy of proviral DNA can be amplified. Qualitative PCR is useful for diagnostic purposes. Three different techniques namely- RT-PCR, nucleic acid sequence based amplification (NASBA) And branched DNA ( b-DNA) assay have been employed.
Virus isolation is accompalished by the co cultivation of the patient’s lymphocytes with fresh peripheral blood cells of healthy donors or with suitable culture lines such as T lymphomas. The presence of the virus can be confirmed by reverse transcriptase assays, serological tests, or by changes in growth pattern of the indicator cells. Virus isolation is tedious and time consuming and successful in only 70 -90% of cases. Therefore virus isolation is mainly used for the characterization of the virus.
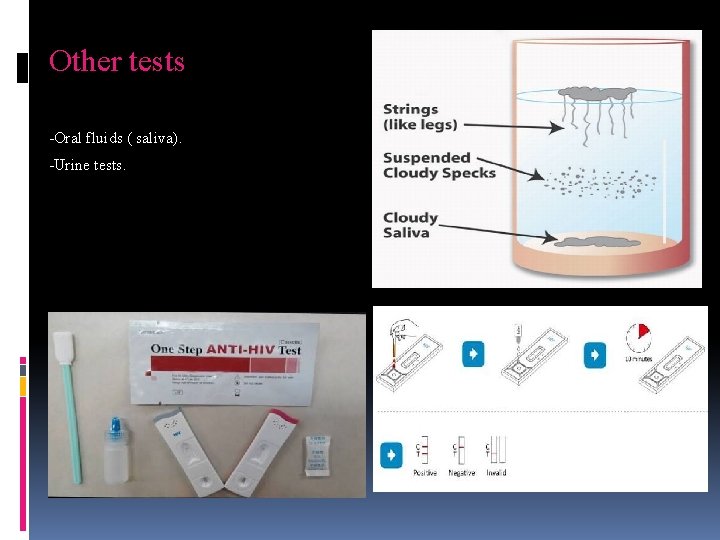
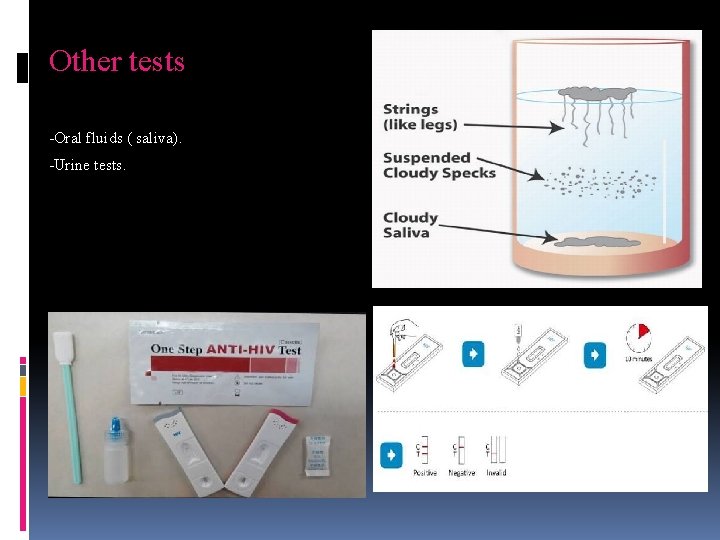
Other tests -Oral fluids ( saliva). -Urine tests.
Management 1) Immunotherapy. 2) Anti-HIV drugs. 3) Psychosocial counseling 4) Nutritious diet. Prevention 1) Avoidance of alcohol and smoking 2) Abstinence 3) Using condoms 4) Reducing number of sexual contacts.

Immunotherapy is transfusion based treatment designed to replace lost immunoglobulins needed to fight HIV infection , to provide cellular factors such as interlukins (IL-2) or to introduce selected or altered immune cells to attack cells harboring the virus. The results of trials using this latter approach however have been inconclusive, and no group has yet shown a survival benefit.

Anti HIV drug treatment 1) Reverse transcriptase inhibitors. They act at the pre – integration stage – before the viral RNA has been converted to DNA and enters the host cell nucleus to integrate into the cell chromosome. These drugs block the reverse transcription of viral RNA into viral DNA. There are two types of reverse transcriptase inhibitors, both of which accomplish the same objective: nucleoside and nucleotide analogues , and non-nucleoside reverse transcriptase inhibitors.
a) Nucleoside analogues. The most effective antiretroviral drugs introduced in 1987. They act by mimicking nucleic acids normally incorporated into viral DNA. They interfere with reverse transcriptase and thus prevent infection. Nucleotide analogues have the same action but are based around different sugar. Ex: Zidovudine ( AZT) (250 -300 mg b. i. d), didanosine( 400 mg once daily >60 kgs), Stavudine( 40 mg twice daily) etc.
b)Non- Nucleoside reverse transcriptase inhibitors- Directly inhibit reverse transcription and unlike nucleoside analogues. Ex: Nevirapine, ( 200 mg once daily and Delavirdine. (400 mg thrice daily).
Protease inhibitors block HIV replication after integration. These drugs inhibit the function of the protease needed to process the ‘ gag –pol’ polypeptide into proteins. Since protease inhibitors act after integration, they can obstruct infectious HIV production in both acutely and chronically infected T cells and macrophages. Saquinavir (1000 mg daily), Ritonavir ( 600 mg twice daily), Indinavir (800 mg twice daily) and Nelfinavir(1250 mg twice daily) are the licensed protease inhibitors used in the clinical practice.
Combination treatment Reverse transcriptase inhibitors and protease inhibitors are used in combination and has shown more effect than monotherapy in impeding the spread of HIV in the body and reducing viral loads. This combination of two reverse transcriptase inhibitors one of which is a thymidine analogue and a protease inhibitor blocks infection both before and after integration and in both activated and resting T cells. This combinational therapy is termed as highly active anti- retroviral therapy (HAART)
Management of HIV in pregnancy. Starts at 12 -14 weeks of pregnancy and continue during delivery. Zidovudine is the drug of choice with baby receiving for 6 weeks postpartum. Women who do not need treatment for themselves should be prescribed a short course of antiretroviral therapy initiated between 22 and 28 weeks of pregnancy to reduce vertical transmission. Efavirenz is contraindicated in pregnancy. ZDV regimen Antepartum- ZDV 300 mg bid Intrapartum-Iv dose of 2 mg/kg first hour followed by 1 mg/kg till delivery Post partum-ZDV syrup at 2 mg/kg q 6 h to new born.
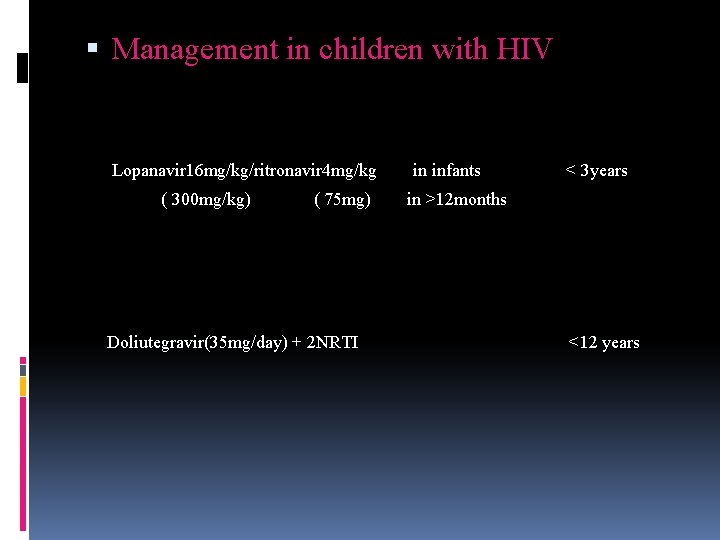
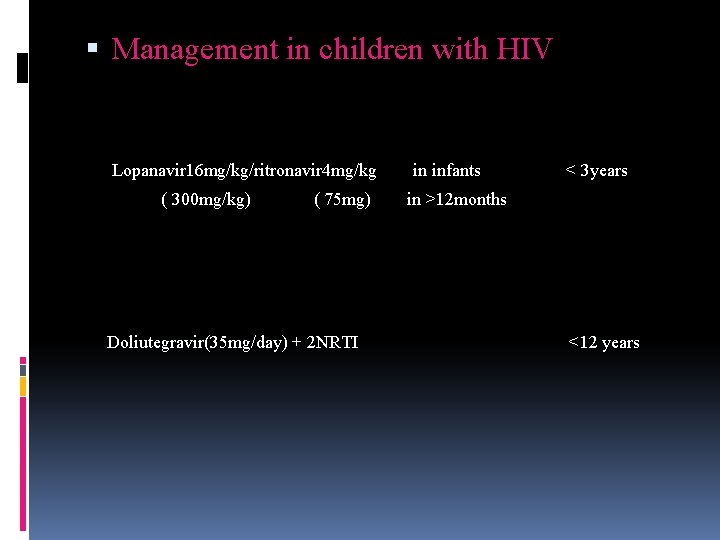
Management in children with HIV Lopanavir 16 mg/kg/ritronavir 4 mg/kg ( 300 mg/kg) ( 75 mg) Doliutegravir(35 mg/day) + 2 NRTI in infants < 3 years in >12 months <12 years

Approaches to HIV vaccine a)Preventive vaccine b)Perinatal vaccine c)Therapeutic vaccine Types -Live attenuated vaccine -Inactivated vaccine -Subunit vaccine -Synthetic peptide vaccine -DNA vaccines -Recombinant Vector vaccines
Development of vaccine HIV can mutate rapidly, thus it is not possible to design antibodies against all antigens. Antibody alone is not sufficient, cell mediated immunity may also be necessary. Virus enters the body not as free virions but also as infected cells, in which the virus or the provirus is protected against antibody or cell mediated lysis. Virus readily establishes life long latent infection hiding from antibodies.


Differential diagnosis. Primary herpes simplex infection. Burkitt lymphoma Mycobacterium avium complex (MAC)

Occupational risk from HIV-
Risk of transmission to surgeonsØ The surgeons are regularly exposed to blood which is the most infective medium for HIV transmission. Incidence of accidental exposure to infected patients blood is 6. 4% Ø Risk is greater when there are more HIV particles in blood. Ø materials- needle stick injury is 0. 3% and other sharps. Ø Risk of transmission in surgery is 1 in 28000 -50000 per hour of operations. Ø Risk is more when surgery lasts more than 3 hrs, > 300 ml blood loss , in intra-abdominal and gynaecological surgeries. Ø Injuries like cut or sharp instrument penetration. Ø Contact of eyes, nose, mouth or broken skin with blood or other body fluids.
Needle stick injuries 1. Passing of sharp instruments by hand 2. Prick while operating 3. Discarding needle 4. Administration of injection 5. Recapping needle 6. After IV cannula removal 7. While administrating local anaesthesia 8. Prick while focusing microscope 9. Paracentesis with 26 gauge needle.
Surgery in the management of clinical problems of HIV infection-Lymphadenopathy -Immune deficiency associated Thrombocytopenic purpura -Thoracic surgery -Abdominal lymphadenopathy and organomegaly -Biliary tract disease -Intracranial mass lesions -Anorectal surgery -Organ transplantation
Surgical treatment Screening Informed consent Operative risk in HIV/AIDS patients Occupational risks to the health care workers Variations in operative techniques. Universal and specific precautions. Ethics.
Consent. HIV patients fear social recognition and rejection, and frequently request surgeons to perform un necessary surgeries such as removal of ‘tell tale’ cervical lymph nodes or parotidectomy for DILS Some patients refuse surgery in desperate situations such as bowel perforation as they want to end the suffering. It should be emphasised to AIDS patients that they are more prone to perioperative complications.
Operative risk in HIV patients The preoperative physiological status is the most accurate predictor of postoperative outcome. While calculating the risk of operative mortality and morbidity the surgeon considers two aspects -The patho physiological state of the patient versus magnitude of the procedure. For ex- The patients with early HIV infection have an operative risk equal to HIV negative patients and therefore can be subjected to any major surgery. and - Operations in contaminated fields ex- Anorectum or oral cavity.
Anaesthesia in HIV patients General Anaesthesia should not be withheld on the grounds of HIV infection alone. Regional anaesthesia is safe Etomidate, Atracurium, remifentanyl and desflurane are preferred Midazolam and fentanyl are better avoided, Succinyl choline should be used with caution Preoperative assessment-Respiratory system -Cardiovascular system -Gastrointestinal system -Nervous system -IVDU group of diseases ( multisystem disease, poor venous access) Reducing the risk-Disposable equipments should be used, Laryngoscopes are exposed to contamination mainly, if heat-moisture exchange filter is used , (PALL BB 2215 MS) it is unnecessary to change the breathing circuit.
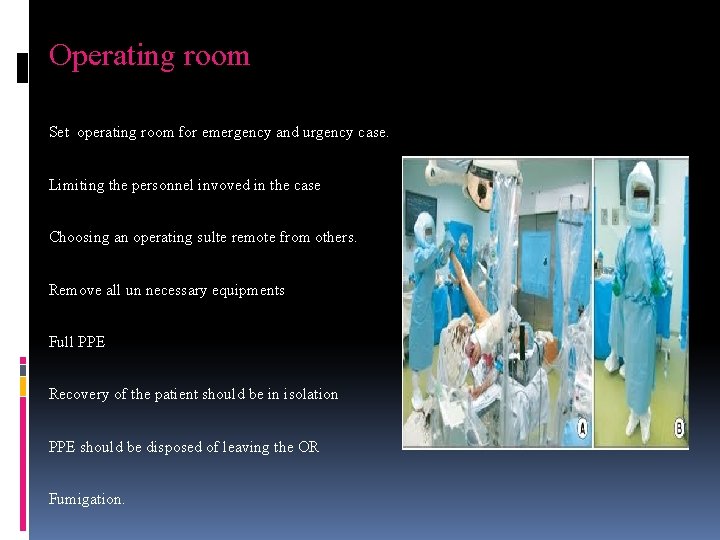
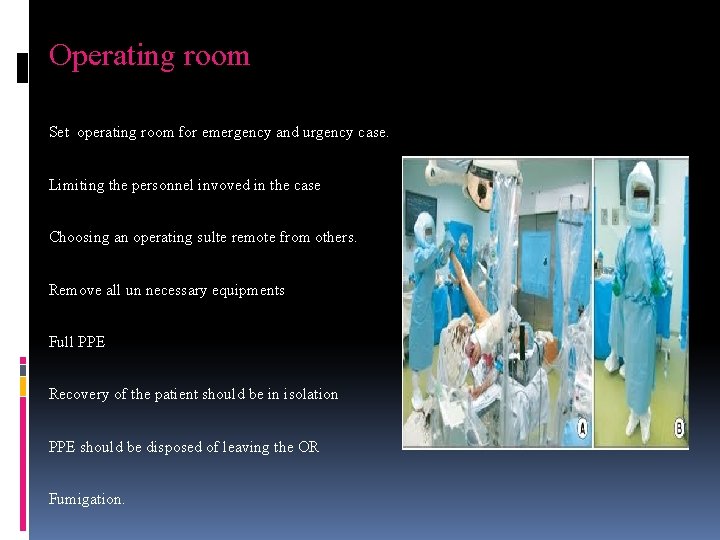
Operating room Set operating room for emergency and urgency case. Limiting the personnel invoved in the case Choosing an operating sulte remote from others. Remove all un necessary equipments Full PPE Recovery of the patient should be in isolation PPE should be disposed of leaving the OR Fumigation.
Variations in operative technique Simple techniques to reduce occupational hazards include. Cutting with electrocautey Avoidance of Hand – hand passage of sharps. Hands should never be used as tissue retractors. Avoid blood loss. Laporoscopic surgeries. Natural orifice trans-endoscopic surgery (NOTES) is on the horizon for major abdominal surgeries. Intraoperative tapling Banding of Haemorrhoids and varices.
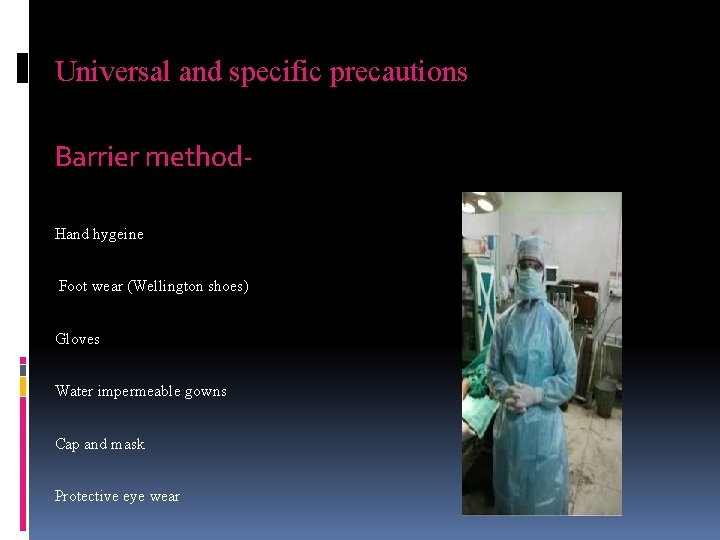
Universal and specific precautions Barrier method. Hand hygeine Foot wear (Wellington shoes) Gloves Water impermeable gowns Cap and mask Protective eye wear

Sharps precautions. Never to recap needles. Dispose of used needles and sharps immediatedly in sharp boxes. Sharp boxes: must be easily accessible, must not be overfilled, labelled or color coded Needle incinerators can be another safe way of disposal. Reusable sharps must be handled with care avoiding direct handling during processing.
How to deal with used materials after surgery Soiled linen : Soaking in 1: 100 hypochirite solution for 30 minutes Metal instruments: Wash with soap and water, soak in 2% Gluteraldehyde solution for 30 minutes, sharp instruments for 6 hrs Then they are autoclaved. Plastic tubing: Soaking in 2% Gluteraldehyde for 6 hours or ETO sterilisation.
Ethics. If a doctor proposes an operation the risks must be weighed against potential benefits of surgery. The occupational hazard is not only to the surgeon’s life but also to the lives of his/her spouse or intimate friends but if situation demands the surgeon should take calculated risk in order to improve the well-being of the patient. Referring the patients to colleagues on ground of contamination risk is unjustified To tell or not to tell? Clinical categories. Life threatning surgical correctable disease Surgical interventions for diagnosis and prophylaxis Surgery is must Find an alternative
Post operative complications in HIV patients: Septic Sequelae (Pelvic collections and wound infections). Postoperative pneumonia. Renal failure. Surgical infections. Tachycardia. Fever. Endometritis and wound infection.
Post operative care ICU for monitoring Ventilator support Blood transfusion. TPN and nasogastric tube is sufficient Chest tubes Urinary catheterization.
Stuck or splashed? Immediate actions required. Wash needle sticks and cuts with soap and water. Flush splashes. Irrigate eyes with clean water, saline or sterile irrigants for 15 minutes. Report the incident to your supervisor. Seek medical treatment as soon as possible.
-Prompt exposure Report regarding the time, nature etc of exposure should be reported. -Source HIV testing after proper consent, if known to be HIV positive then assess the health status and the possibility of drug resistance if on anti-retroviral therapy. -Recipient Baseline serological testing of HIV, HBV and HCV.
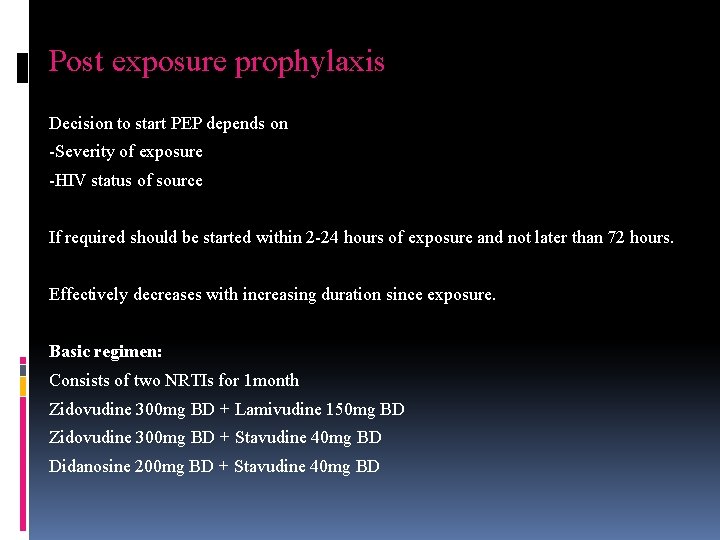
Post exposure prophylaxis Decision to start PEP depends on -Severity of exposure -HIV status of source If required should be started within 2 -24 hours of exposure and not later than 72 hours. Effectively decreases with increasing duration since exposure. Basic regimen: Consists of two NRTIs for 1 month Zidovudine 300 mg BD + Lamivudine 150 mg BD Zidovudine 300 mg BD + Stavudine 40 mg BD Didanosine 200 mg BD + Stavudine 40 mg BD
Expanded regimen Consists of 2 NRTIs + 1 PI for 1 month Any of the basic regimen + any of the following: Idinavir 800 mg TDS Ritonavir 100 mg BD Saquinavir 1000 mg BD Lopinavir 400 mg BD
HIV-AIDS- India’s Response National AIDS control programme (NACP)-1987 National AIDS control organization (NACO)-1992 OBJECTIVES – - Reduce new infections - Create awareness, Comprehensive care, support and treatment to all persons living with HIV/AIDS. - APPROACHES- - Core high risk groups - Bridge populations, with particular focus on clients of sex workers - Other vulnerable populations.
STRATEGIESPromotion of STI services Condom use Behaviour change communication AIDS helpline -1097 ‘University talk AIDS project’ Approaches- ABC (Abstinence, befaithful, condom), CNN –( Condom, Needle exchange, Negotiation). AIDS day- 1 st December.
Facts HIV is not airborne and cannot be caught by touching skin, sweat or saliva You cannot get HIV by holding hands or sharing drinks Mosquito’s do not inject other peoples blood when they bite and so cant spread HIV
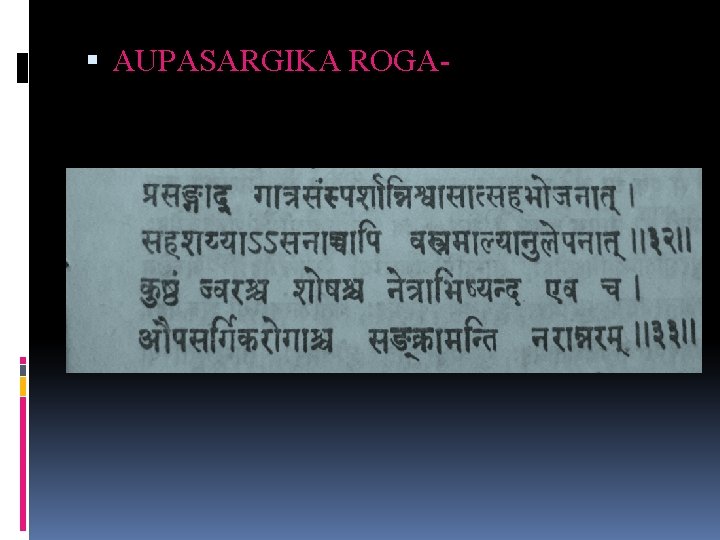
AUPASARGIKA ROGA-
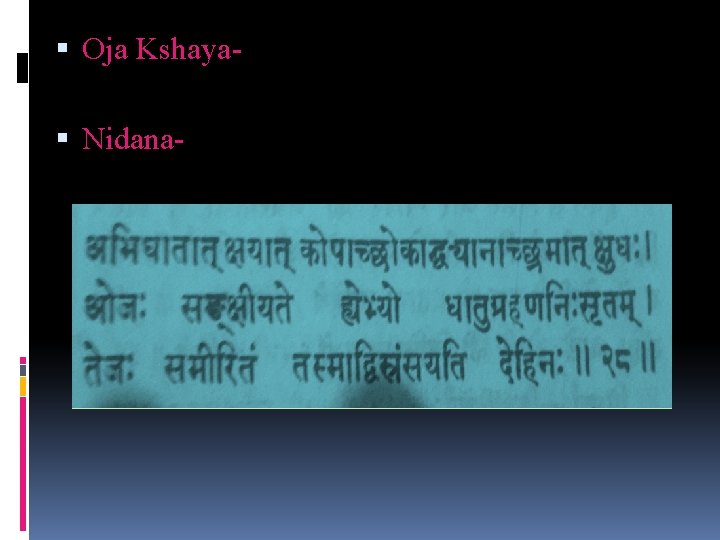
Oja Kshaya Nidana-
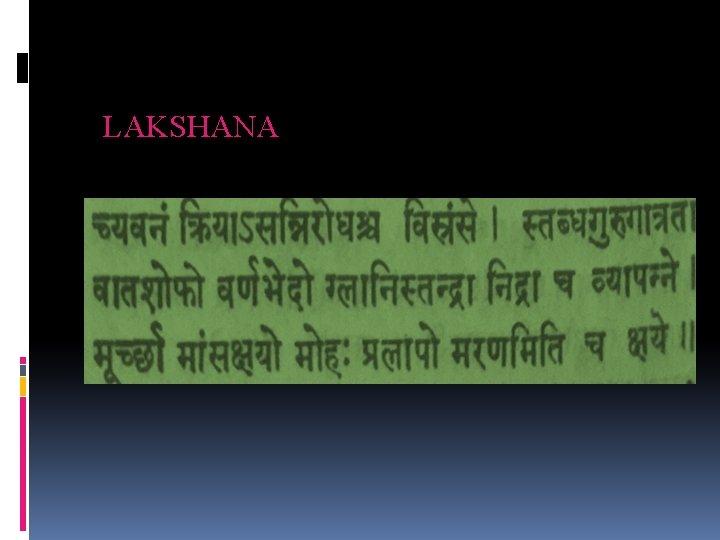
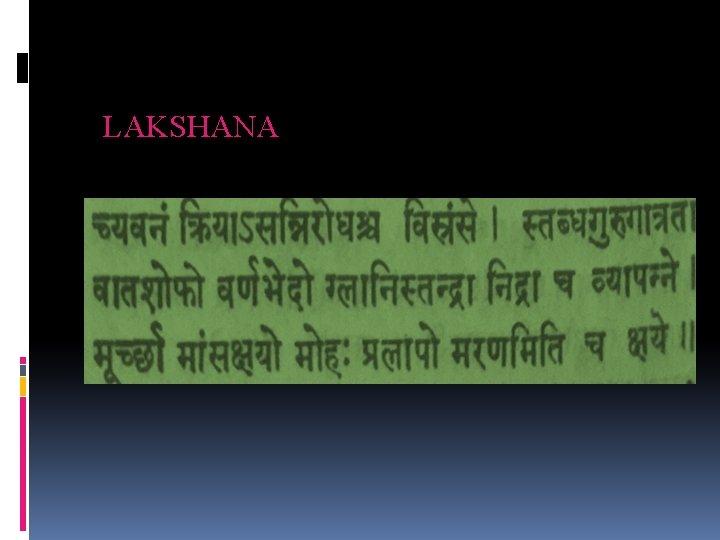
LAKSHANA
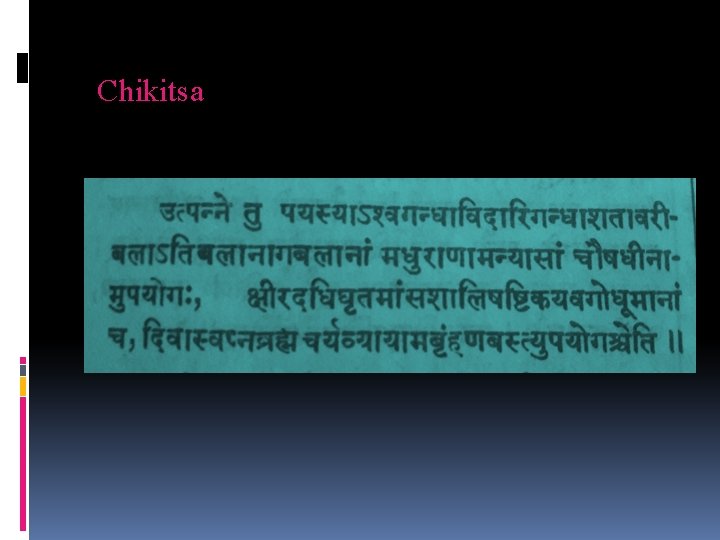
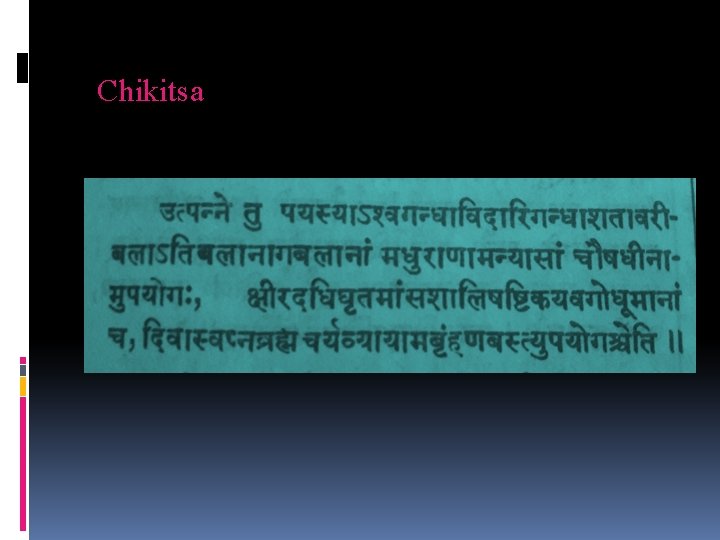
Chikitsa
 Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Test wiedzy o hiv
Test wiedzy o hiv Causative organism of hiv/aids
Causative organism of hiv/aids Name the five lesions associated with hiv/aids chapter 17
Name the five lesions associated with hiv/aids chapter 17 Kasus hiv aids
Kasus hiv aids I hope the days come easy
I hope the days come easy Where you go ill go
Where you go ill go Stay hungry stay foolish examples
Stay hungry stay foolish examples Good afternoon stay home stay safe
Good afternoon stay home stay safe So stay so stay 再知己
So stay so stay 再知己 To daffodils robert herrick analysis
To daffodils robert herrick analysis Stay hungry stay foolish significato
Stay hungry stay foolish significato Good morning stay safe
Good morning stay safe Stay hungry stay foolish significato
Stay hungry stay foolish significato Top bar hive plans pdf
Top bar hive plans pdf Hive architecture
Hive architecture Hive metrics
Hive metrics Introduction to pig
Introduction to pig Skew join in hive
Skew join in hive The hive dsrip
The hive dsrip Hive
Hive Animal/habitat analogy examples
Animal/habitat analogy examples Rest api for hortonworks hive
Rest api for hortonworks hive Zookeeper in hadoop ecosystem
Zookeeper in hadoop ecosystem Hive blockchain frankfort
Hive blockchain frankfort Hive provides data warehousing layer to data over hadoop
Hive provides data warehousing layer to data over hadoop Hive cbo
Hive cbo Apache hive data warehouse
Apache hive data warehouse Action and object analogies examples
Action and object analogies examples Define a kenya top bar hive
Define a kenya top bar hive Hive hdfs
Hive hdfs Introduction to poetry by billy collins analysis
Introduction to poetry by billy collins analysis Hive warehousing solution
Hive warehousing solution Hive architecture
Hive architecture Hive warehousing solution
Hive warehousing solution Africanized honey bee hive
Africanized honey bee hive Phil mulder
Phil mulder Michael bush top bar hive
Michael bush top bar hive Ostin law firm
Ostin law firm Apache atlas architecture
Apache atlas architecture Hive sql compliance
Hive sql compliance Ap 141
Ap 141 Triệu chứng nhiễm hiv
Triệu chứng nhiễm hiv Hiv reverse transcription
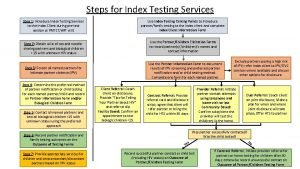
Hiv reverse transcription 10 steps of index testing
10 steps of index testing Prognas akreditasi
Prognas akreditasi Phdp in hiv
Phdp in hiv Kuchecheudzwa
Kuchecheudzwa Hcv window period
Hcv window period Why do the bodys antibodies fail to protect people from hiv
Why do the bodys antibodies fail to protect people from hiv Iris hiv
Iris hiv Hiv
Hiv Hiv risk factors
Hiv risk factors Asante hiv-1 rapid recency assay
Asante hiv-1 rapid recency assay Fiebig hiv
Fiebig hiv Hiv case-based surveillance in ethiopia
Hiv case-based surveillance in ethiopia Triệu chứng nhiễm hiv
Triệu chứng nhiễm hiv Basic hiv course
Basic hiv course Stakeholders in hiv prevention
Stakeholders in hiv prevention Hiv treatments
Hiv treatments What does hiv stand
What does hiv stand Aids 101
Aids 101 Hiv test window period
Hiv test window period Hiv stool color
Hiv stool color Procentowe ryzyko zakażenia hiv
Procentowe ryzyko zakażenia hiv Tes klamidia di prodia
Tes klamidia di prodia Hiv lifecycle
Hiv lifecycle Hiv pencere dönemi
Hiv pencere dönemi Hiv lifecycle
Hiv lifecycle Hiv
Hiv Incubation period of hiv
Incubation period of hiv Ciclo replicativo
Ciclo replicativo