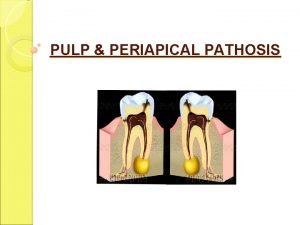
Periradicular Periapical Diseases Introduction u Periradicular tissues consist
- Slides: 22
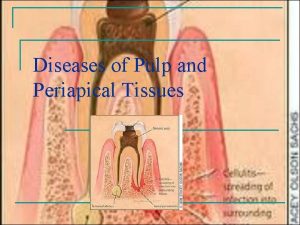
Periradicular/ Periapical Diseases
Introduction u Periradicular tissues consist of cementum, periodontal ligament, and alveolar bone. u The response of the periradicular tissues to various injuries is similar to that of other connective tissues elsewhere in the body- an immuno inflamatory response
Apical Periodontitis u Apical Periodontitis is a inflammatory lesion in the periodontal tissues that is caused mostly by bacterial elements derived from the infected root canal system of teeth. u Other causes: – Physical (overinstrumentation, overfilling) – Chemical (irrigants, intracanal medication, root canal filling materials) insults – traumatic injury
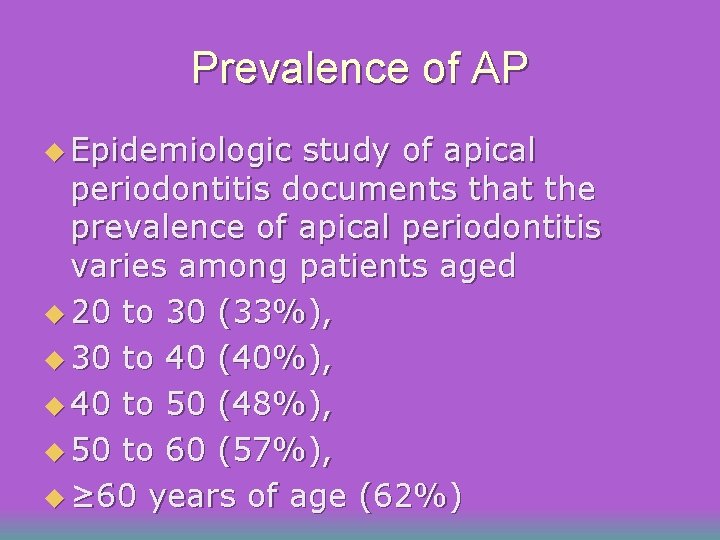
Prevalence of AP u Epidemiologic study of apical periodontitis documents that the prevalence of apical periodontitis varies among patients aged u 20 to 30 (33%), u 30 to 40 (40%), u 40 to 50 (48%), u 50 to 60 (57%), u ≥ 60 years of age (62%)
Types of apical periodontitis u Asymptomatic apical periodontitis u Symptomatic apical periodontitis u Acute apical abscess u Chronic apical abscess u Cellulitis u condensing osteitis
Histological classification u On a microscopic level, different structural frameworks of apical periodontitis can be identified. u These forms include: u Apical granuloma, u Apical abscess and u Apical cyst.
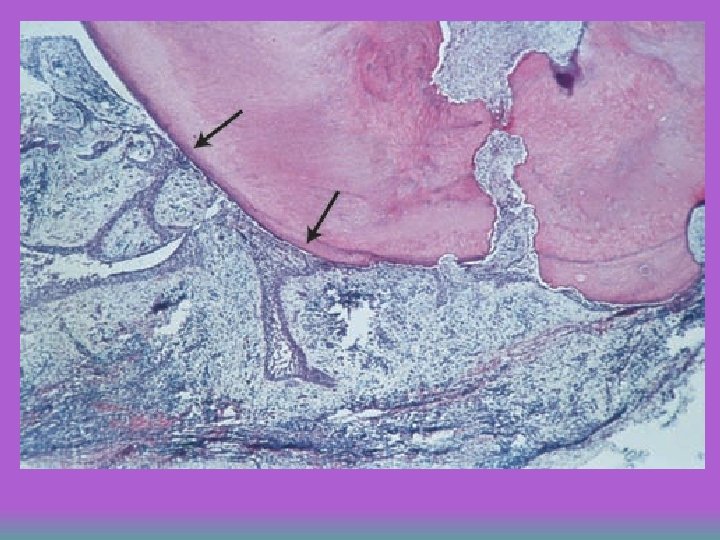
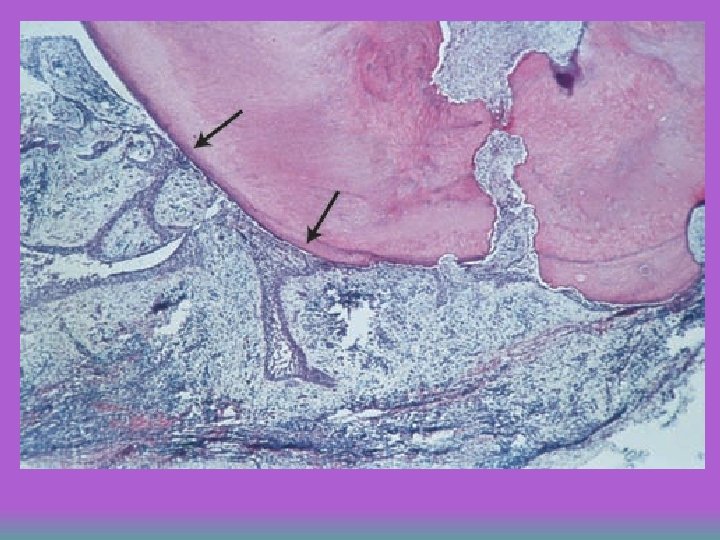
Apical granuloma Most common form of apical periodontitis and consists of an inflammatory lesion dominated by lymphocytes, macrophages and plasma cells u Numerous fibroblasts and connective tissue fibers are usually present with abundant capillaries u Epithelial cell proliferation is a common finding in longstanding apical granulomas and may occur in up to 50% of the lesions u
Apical abscess u Denotes the presence of pus within the lesion. u Abscess formation may reflect a shift in cellular dynamics within a preexisting apical granuloma or be a direct outcome of an acute primary infection
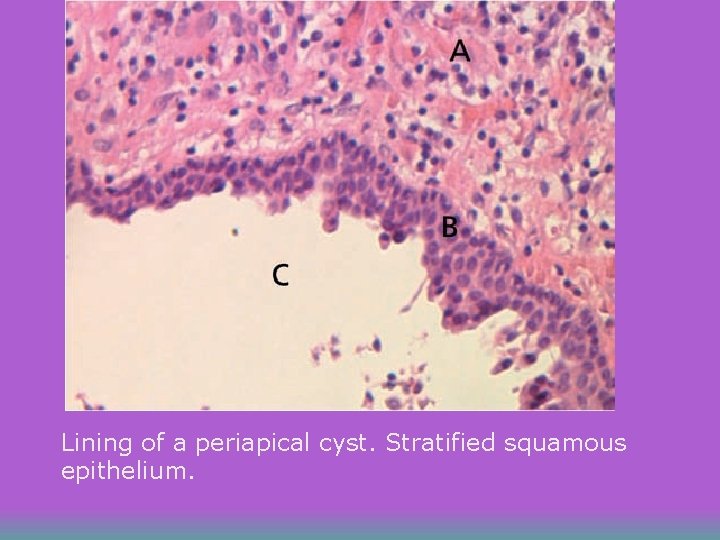
Apical Cyst u An epithelium-lined cavity that contains fluid or semi-solid material and is commonly surrounded by dense connective tissue variably infiltrated by mononuclear leukocytes and PMNs. u Cyst cavity is most commonly lined with stratified squamous epithelium of varying thickness that originates from the epithelial rest cells of Malassez
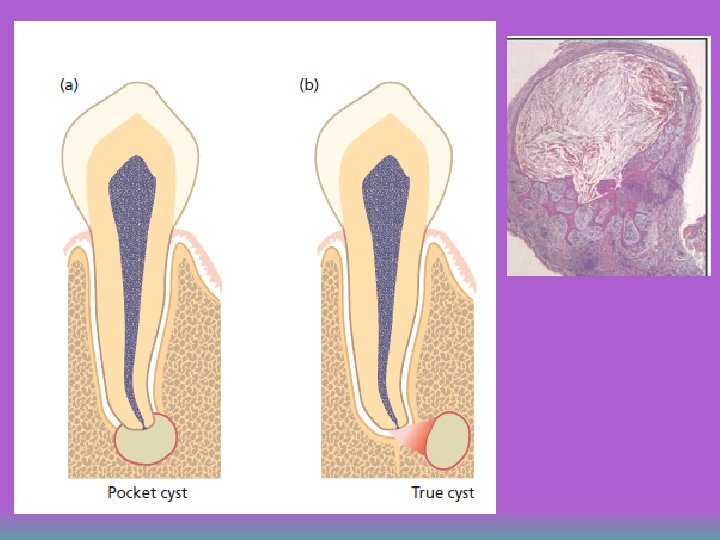
Apical cyst u Apical cysts are divided into – Pocket Cysts (Bay Cyst) – True Cysts A pocket cyst is an apical inflamatory saclike, epithelium lined cavity that is open to and continuous with the root canal space. u True apical cysts are located within the periapical granuloma with no apparent connection between their cavity and that of the root canal space u
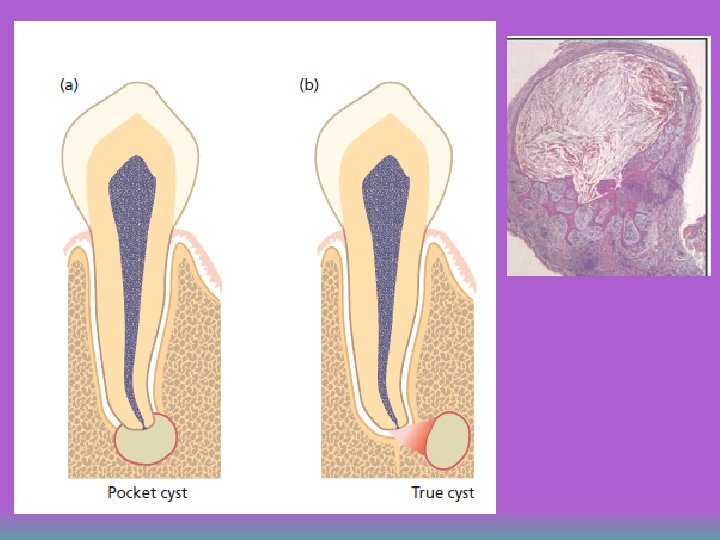
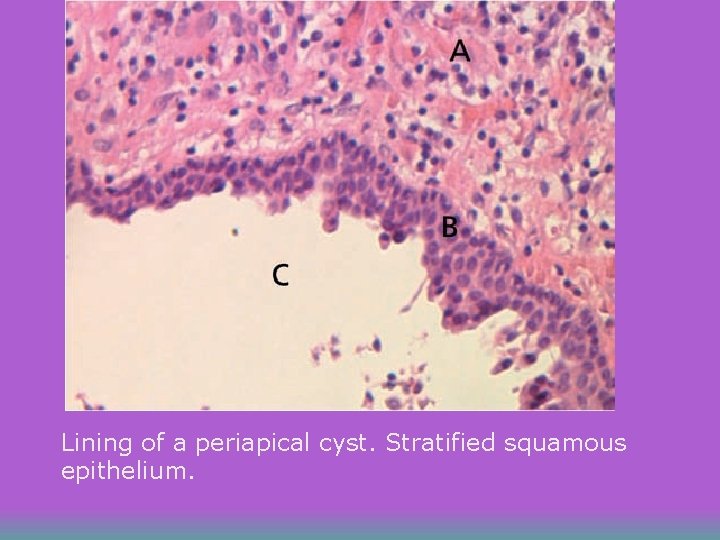
Lining of a periapical cyst. Stratified squamous epithelium.
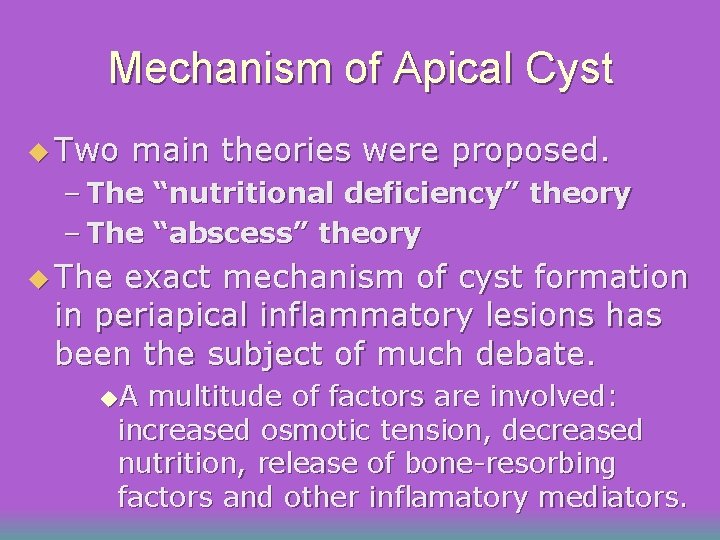
Mechanism of Apical Cyst u Two main theories were proposed. – The “nutritional deficiency” theory – The “abscess” theory u The exact mechanism of cyst formation in periapical inflammatory lesions has been the subject of much debate. u. A multitude of factors are involved: increased osmotic tension, decreased nutrition, release of bone-resorbing factors and other inflamatory mediators.
Symptomatic AP u History -symptoms of pulpitis or necrosis + pain on bite u Clinical examination: – pain on percussion u X-ray: – thickening of periodontal ligament space u Treatment: – root canal treatment, (adjustment of occlusion)
Asymptomatic AP u u asymptomatic apical periodontitis may go unnoticed by the patient and is often discovered only by routine radiographic examination or by careful patient history. History : – asymptomatic or slight discomfort u Clinical examintaion: – little or no pain on percussion u X-ray: – interruption of lamina dura or apical radiolucency u Treatment: – root canal treatment
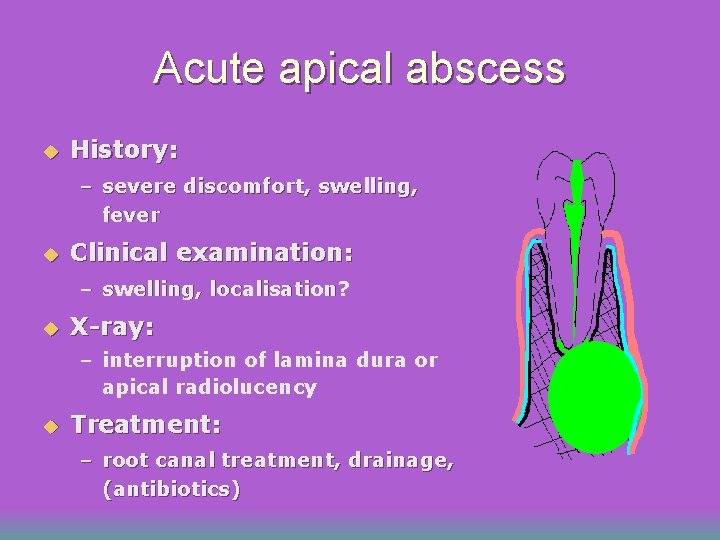
Acute apical abscess u History: – severe discomfort, swelling, fever u Clinical examination: – swelling, localisation? u X-ray: – interruption of lamina dura or apical radiolucency u Treatment: – root canal treatment, drainage, (antibiotics)
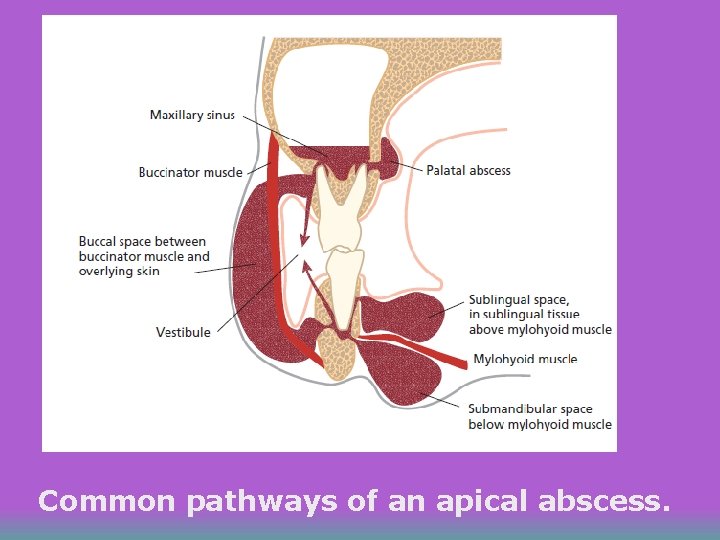
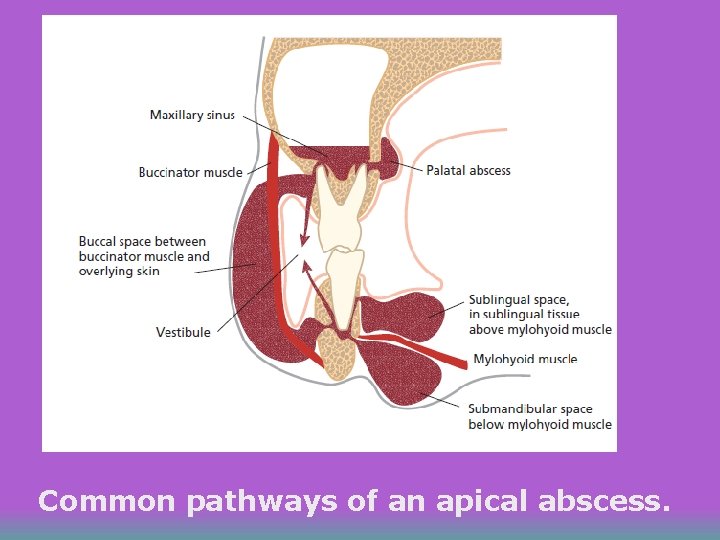
Common pathways of an apical abscess.
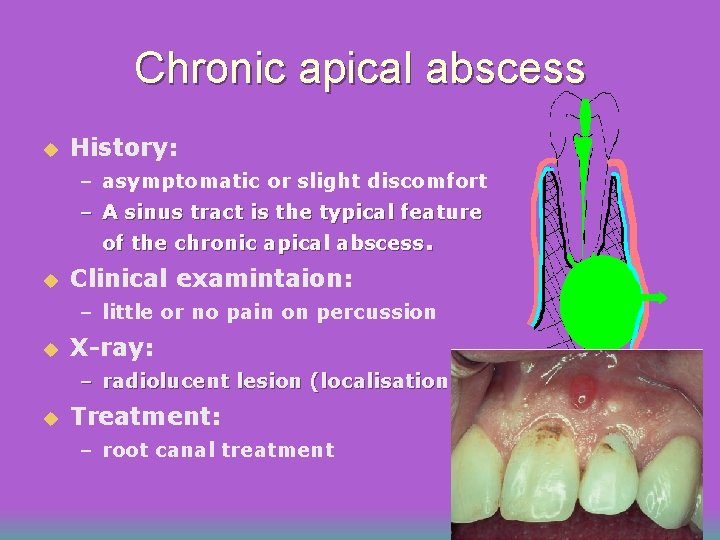
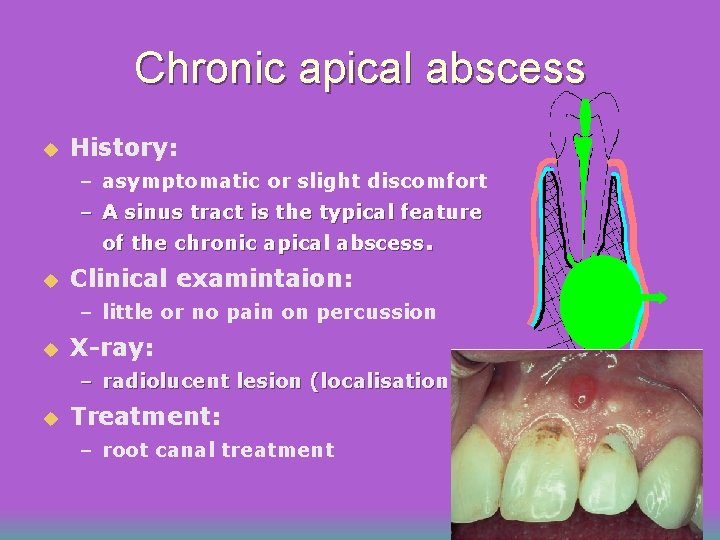
Chronic apical abscess u History: – asymptomatic or slight discomfort – A sinus tract is the typical feature of the chronic apical abscess. u Clinical examintaion: – little or no pain on percussion u X-ray: – radiolucent lesion (localisation) u Treatment: – root canal treatment
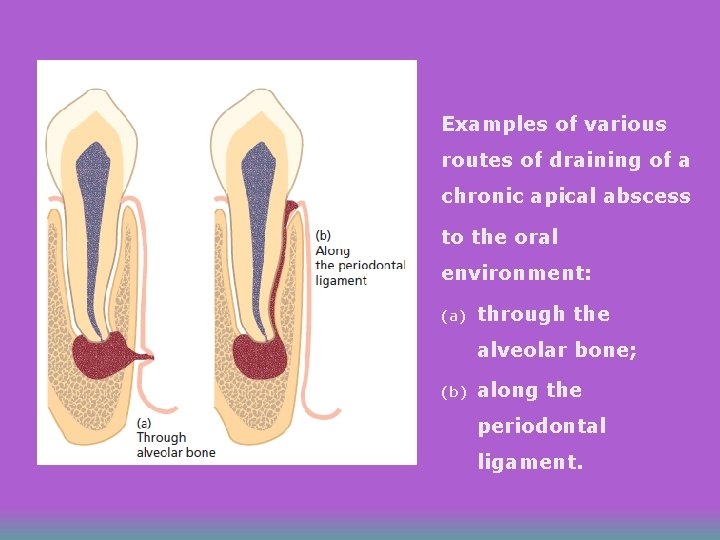
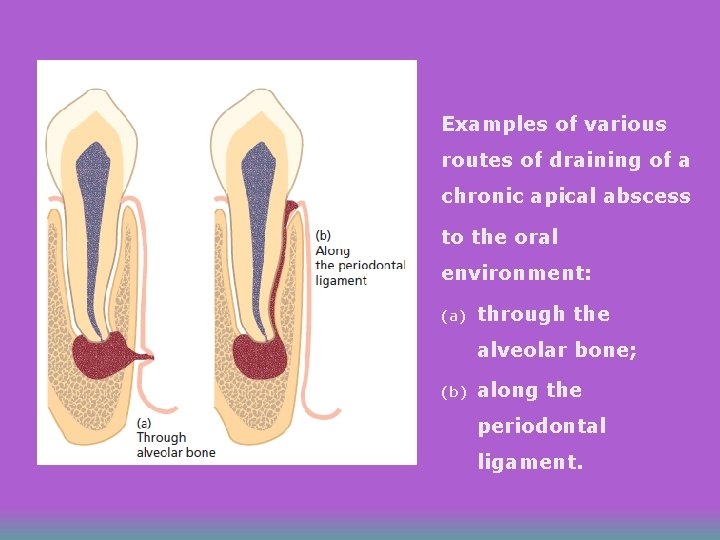
Examples of various routes of draining of a chronic apical abscess to the oral environment: (a) through the alveolar bone; (b) along the periodontal ligament.
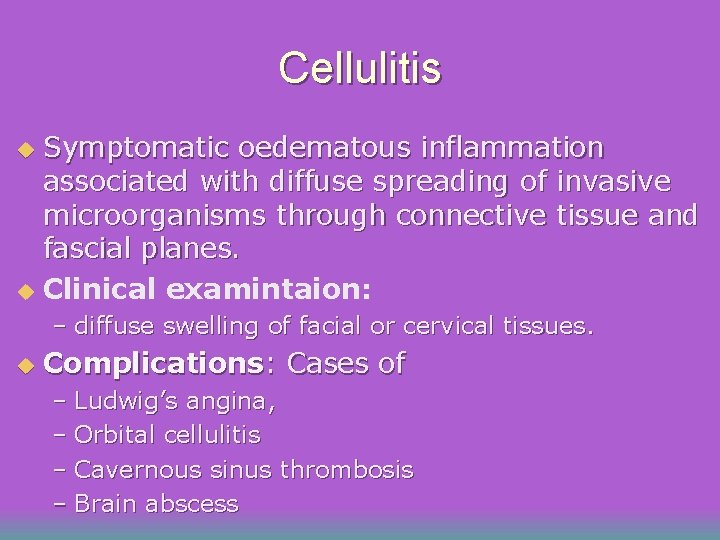
Cellulitis Symptomatic oedematous inflammation associated with diffuse spreading of invasive microorganisms through connective tissue and fascial planes. u Clinical examintaion: u – diffuse swelling of facial or cervical tissues. u Complications: Cases of – Ludwig’s angina, – Orbital cellulitis – Cavernous sinus thrombosis – Brain abscess
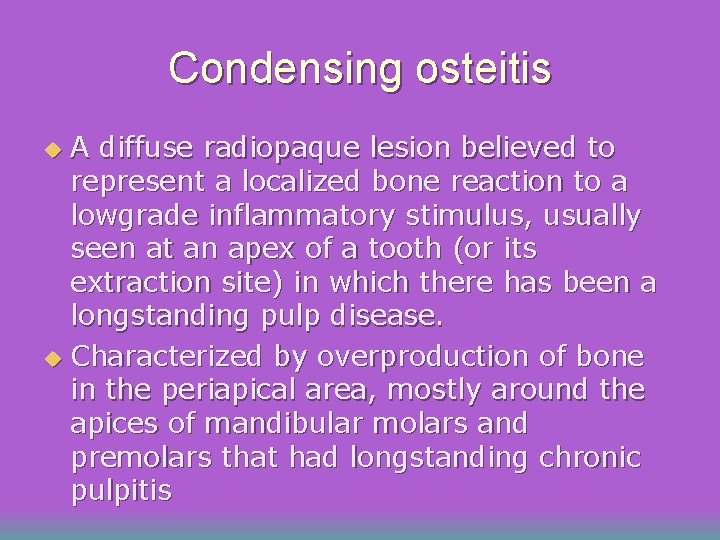
Condensing osteitis A diffuse radiopaque lesion believed to represent a localized bone reaction to a lowgrade inflammatory stimulus, usually seen at an apex of a tooth (or its extraction site) in which there has been a longstanding pulp disease. u Characterized by overproduction of bone in the periapical area, mostly around the apices of mandibular molars and premolars that had longstanding chronic pulpitis u
 Kronfeld mountain pass theory
Kronfeld mountain pass theory Who classification of periradicular diseases
Who classification of periradicular diseases Periradicular diseases
Periradicular diseases Body tissues chapter 3 cells and tissues
Body tissues chapter 3 cells and tissues The 4 tissues
The 4 tissues Body tissues chapter 3 cells and tissues
Body tissues chapter 3 cells and tissues Cells form tissues. tissues form __________.
Cells form tissues. tissues form __________. Chapter 3 cells and tissues
Chapter 3 cells and tissues Lateral periodontal cyst
Lateral periodontal cyst Faulty
Faulty Periapical
Periapical Odontoma compuesto
Odontoma compuesto Aot cyst
Aot cyst Placing reflex
Placing reflex Periapical granuloma
Periapical granuloma Periapical
Periapical Great britain countries
Great britain countries What does the united kingdom consist of
What does the united kingdom consist of What consists of the uk
What consists of the uk Safety net drop tests must consist of a
Safety net drop tests must consist of a Types of emulsion with example
Types of emulsion with example What does blood consist of
What does blood consist of A feeder consists of all circuit conductors located ____
A feeder consists of all circuit conductors located ____