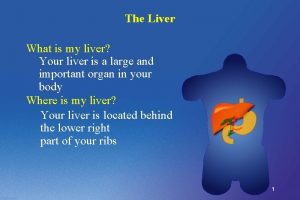
Liver trauma Introduction w The liver is the


















- Slides: 96
Liver trauma
Introduction w The liver is the most commonly injured abdominal organ after penetrating and blunt trauma w Blunt abdominal trauma-- most common cause of injuries, 95 % secondary to vehicle accident
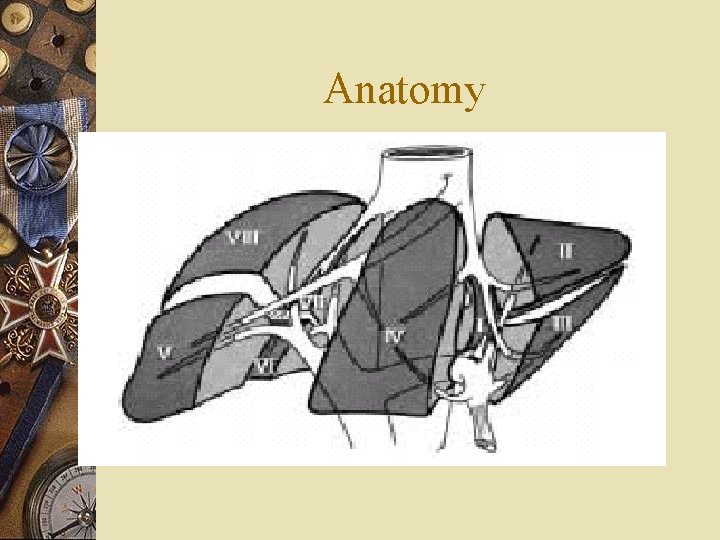
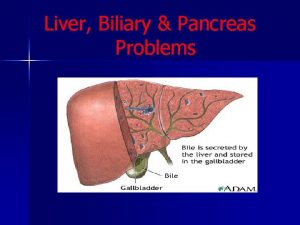
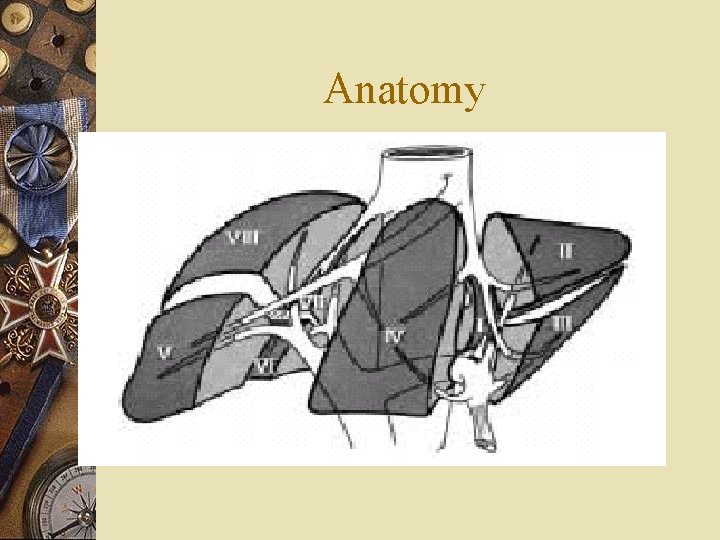
Anatomy

Mechanism of injury(1) w Deceleration injury --producing a laceration of its relatively thin capsule and parenchyma at the sites of attachment to the diaphragm --usually tears between the post. sector(segments VI, VII ) and the ant. sectors(segments V, VIII ) of the R’t lobe
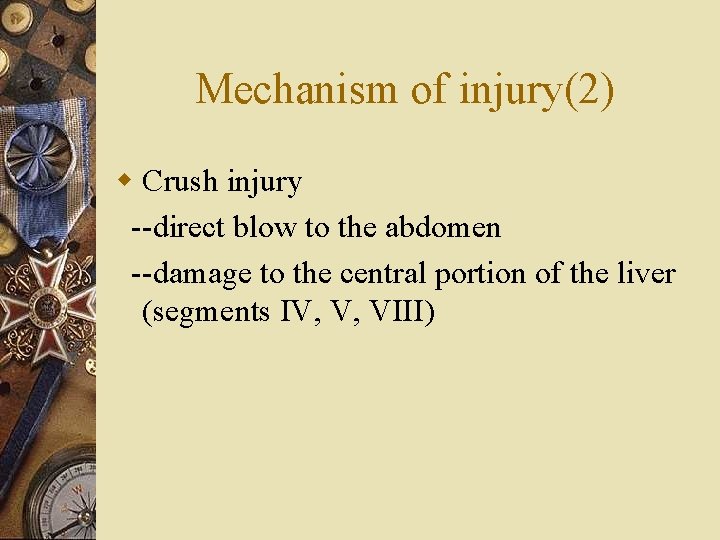
Mechanism of injury(2) w Crush injury --direct blow to the abdomen --damage to the central portion of the liver (segments IV, V, VIII)
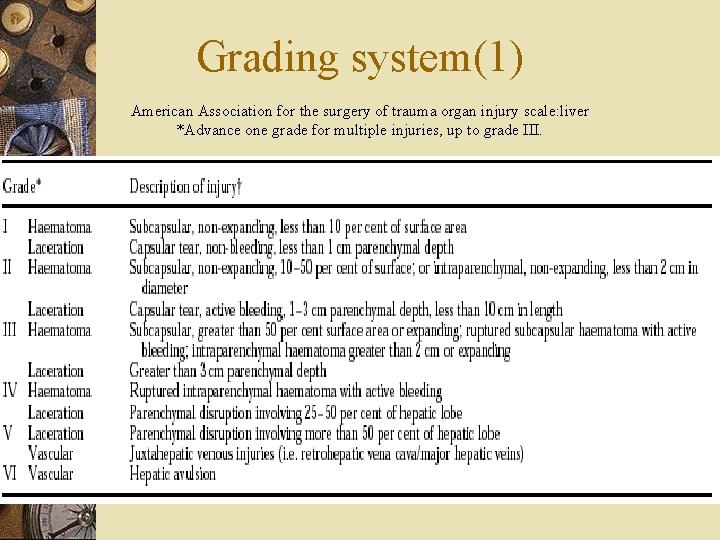
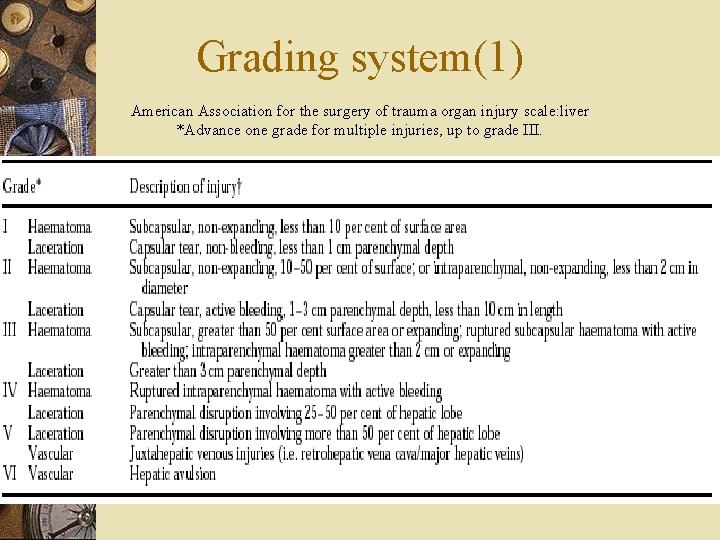
Grading system(1) American Association for the surgery of trauma organ injury scale: liver *Advance one grade for multiple injuries, up to grade III.
Grading system(2) w Grade I, II ---minor injuries, represent 80 -90% of all injuries, require minimal or no operative treatment w Grade III-V -- severe, require surgical intervention w Grade VI --incompatible with survival

Assessment and initial investigation w A conscious p’t, hemodynamically unstable with generalized peritonism laparotomy without investigation w Neurologically impaired or physical sign are equivocal →Diagnostic peritoneal lavage(DPL) and laparotomy performed if the test is positive w Hemodynamically stable →further radiological assessment
Diagnosis of liver injury w Diagnostic Peritoneal Lavage --fast, sensitive, accurate and simple to perform --invasive, cannot diagnose retroperitoneal injury w X-ray --nonspecific, but useful in showing the extent of associated skeletal trauma w Ultrasonography --fast, accurate, noninvasive, a good initial screening test --sensitivity 88%, specificity 99%, accuracy 97%
Ultrosonography
Computed tomography(1) w The standard evaluation method for stable p’t w Performed with Dilute water soluble oral contrast agent and intravenous contrast
Non-operative management w 86% of liver injuries stopped bleeding by the time of surgical exploration w 67% of operations performed are nontherapeutic w Standard method of pediatric p’t and many adults

Non-operative management w Criteria --hemodynamically stable --simple hepatic parenchyma laceration of inrahepatic hematoma --absence of active hemorrhage --hemoperitoneum of less than 500 ml --limited need for liver related blood transfusions (12 U) --absence of peritoneal sign --absence of other peritoneal injuries that would otherwise require an operation
Non-operative management w Criteria --good quality CT scans --experienced radiologist --intensive care setting w Currently believe that ultimate decisive factor should be the hemodynamic stability at presentation or after initial resuscitation
Non-operative management w Abdominal CT --no alteration in management is indicated unless there is change in patient’s clinical course w Resumption of normal activities --avoid delayed hemorrhage --avoid contact sports or heavy physical activity for 8 wks after liver injury of grades III-VI (3 wks-6 months)
Non-operative management w Role of interventional radiology in blunt liver injury --to document active haemorrhage in subcapsular haematomas, --as a salvage alternative to surgery in the face of continuous haemorrhage in patients who remain haemodynamically stable --in the diagnosis and treatment of haemobilia --in the treatment of retained collections or perihepatic sepsis (using percutaneous techniques).
Non-operative management --Arteriography is useful in selected patients after operative perihepatic packing who have postoperative evidence of ongoing haemorrhage. --Biliary endoscopy may be helpful in the diagnosis and treatment of complications secondary to complex liver injury Complication --delayed hemorrhage, biliary fistula and liver abscess, hemobilia and bilhemia, extrahepatic bile duct stricture

Non-operative management w Morbidity and death --the incidence of associated abdominal injury ranges from 13% to 35% --the incidence of truly missed injury ranges from 0. 5% to 12% --the incidence of missed injury was 0. 2% when strict guidelines for conservative treatment were followed and CT was used routinely. --Wrong interpretation and poor quality of the initial scan is the most common cause --A radiologist and the attending trauma surgeon read the initial CT scan, which must be of excellent quality were recommended
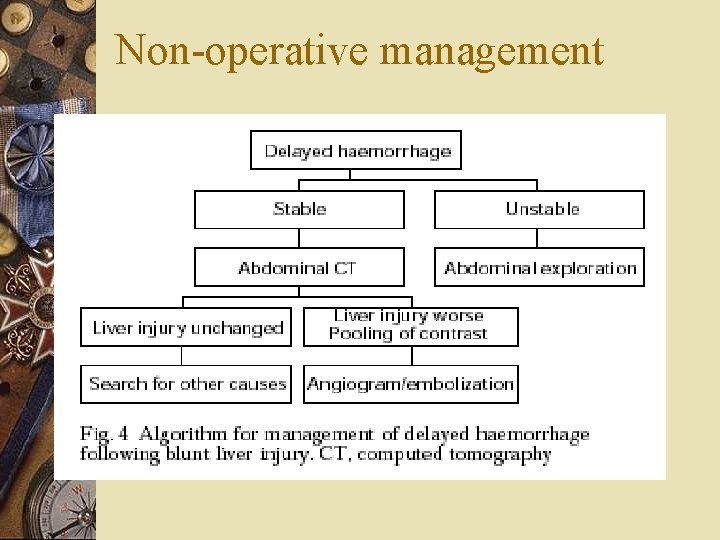
Non-operative management w Complication --Delayed hemorrhage ‧ most common, usual indication for a delayed operation ‧under strict guidelines, the incidence ranges from 0 -5%, and blood transfusions were required in fewer than 20% ‧ common errors: (1)assuming that the hemorrhage is not related to the liver (2)multiple(more than four)blood transfusions in the hope that it will stop (3)misreading CT and underestimating hemoperitoneum and active bleeding
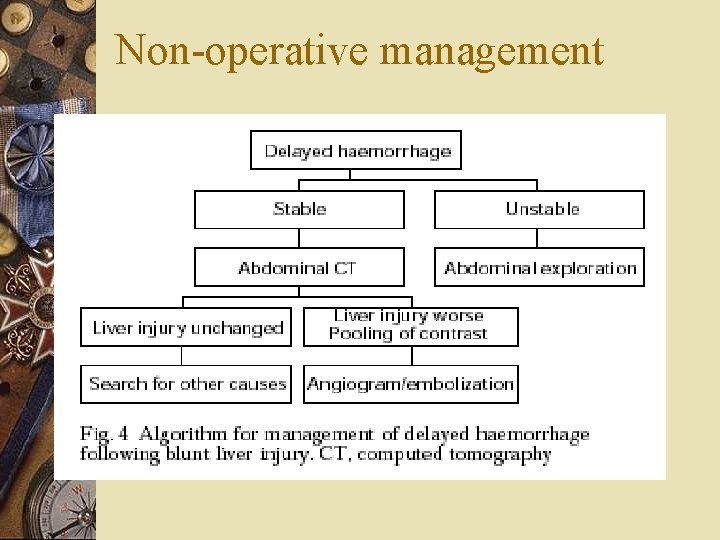
Non-operative management
Non-operative management w Complication --biliary fistula and liver abscess --Hemobilia ‧ 1%, iatrogenic causes most common ‧injury causes communication between the biliary tract and blood vessels ‧abdominal trauma, jaundice, RUQ colicky pain and blood in vomitus or stool point to this diagnosis ‧managed by percutaneous selective hepatic a. embolization or surgical intervention
Non-operative management w Complication --bilihemia ‧rare complication of severe decelerationon injury, in which the hepatic venules and the intrahepatic bile ducts rupture ‧excessive bilirubin level ‧endoscopic sphincterotomy and biliary endostenting --Extrahepatic bile duct stricture ‧ the incidence is higher than the past ‧no uniformity of treatment criteria
Non-operative management w Mortality rate --7 -13% with most resulting from associated injuries --0 -0. 4% resulting from liver itself

Non-operative management indications w In haemodynamically stable patients with blunt hepatic injury, an expeditious abdominal CT scan w haemodynamic stability rather than findings on CT determines which patients should be managed conservatively w in haemodynamically stable patients less treatment is probably the best treatment w most blunt hepatic injuries can be managed without operation with minimal morbidity and mortality rates
Operative management w Initial control of bleeding achieved with temporary tamponade using packs, portal triad occlusion(Pringle manoeuvre), bimanual compression of the liver or even manual compression abdominal aorta above celiac trunk w If hemorrhage is unaffected by portal triad occlusion(Pringle manoeuvre) by digital compression or vascular clamp, major vena cava injury or atypical vascular anatomy should be expected
Operative management w Hepatotomy with direct suture ligation --using the finger fracture technique, electrocautery or an ultrasonic dissector to expose damaged vessels and hepatic duct which ligated , clipped or repaired --low incidence of rebleeding, necrosis and sepsis --effectives following blunt liver trauma requires further evaluation
Operative management w Resection debridement --removal devitalized tissue --rapid compared with standard anatomical resection, which are more time consuming and remove more normal liver parenchyma --reduced risk of post-op sepsis secondary hemorrhage and bile leakage
Operative management Anatomical resection --reserved for deep laceration Perihepatic packing --Indication: coagulopathy, irreversible shock from blood loss (10 u), hypothermia(32 C), acidosis(PH 7. 2), bilobar injury, large nonexpanding hematoma, capsular avulsion, vena cava or hepatic vein injuries
Perihepatic packing
Operative management w Mesh rapping --new technique for grade III, IV laceration, tamponading large intrahepatic hematomas --not indicated where juxtacaval or hepatic vein injury is suspected
Mesh rapping
Operative management w Omental packing w Intrahepatic tamponade with penrose drains w Fibrin glue w Retrohepatic venous injuries --Total vascular exclusion --venous bypass --Atriocaval shunting --Liver transplantation
Operative management w Complication --Hemorrhage, sepsis --Biliary fistula --Respiratory problems --Liver failure --Hyperpyrexia --Acalculous cholecystitis --Pancreatic, duodenal of small bowel fistula --Drainage of intra-abdominal abscess or bilioma under ultrasonography or CT guidance and embolization of AV fistula and deep bleeding vessels
Conclusion w Optium results need a specialist team -experienced liver surgeon, and anaesthetist used to dealing with the coagulopathyof liver disease -interventional hepatobiliary radiologist and endoscpoist to manage post-op complication -rapid infusers, cell savers and venous bypass to deal with massive blood loss -Appropriate intensive care facilities -perihepatic packs to control hemorrhage -hepatotomy with direct suture ligation or resection debridement was preferred
Hydatid cyst of the liver
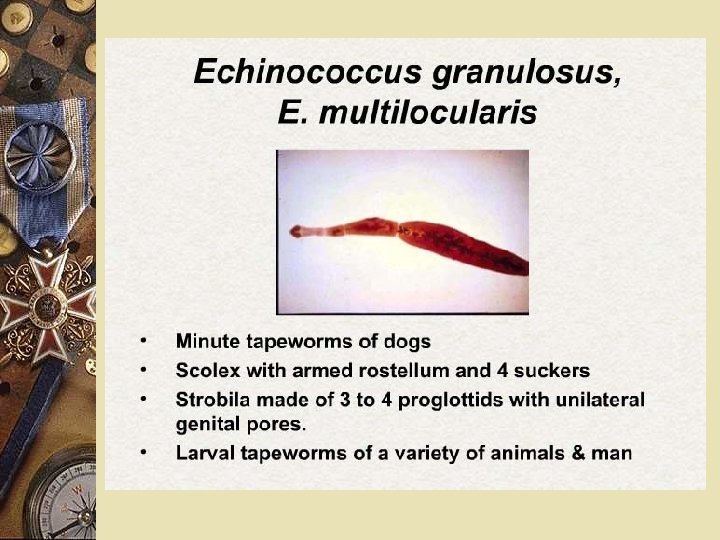
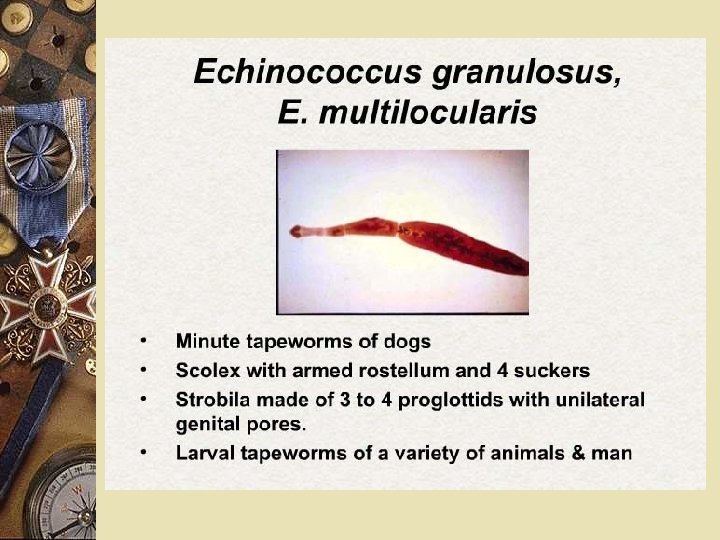
ETHIOLOGY q Taenia echinoccocus (cel mai frecvent) q. Taenia echnoccocus granularis – more severe due to exogenous vesiculation Multiple localisation: lung, brain, muscles


PATHOLOGY § Types of cysts: § unic vs. multiple § Structure Ø proligerous membrane - inside the mebrane: CUTICULA is the germinative strata, producing new daughter cysts Ø Adventiceal layer – compression and metaplazia of normal liver tiussue, forms the percyst which may impregnated with calcium salts. Ø content – typical transparent fluid, but may become stayne dwith bile
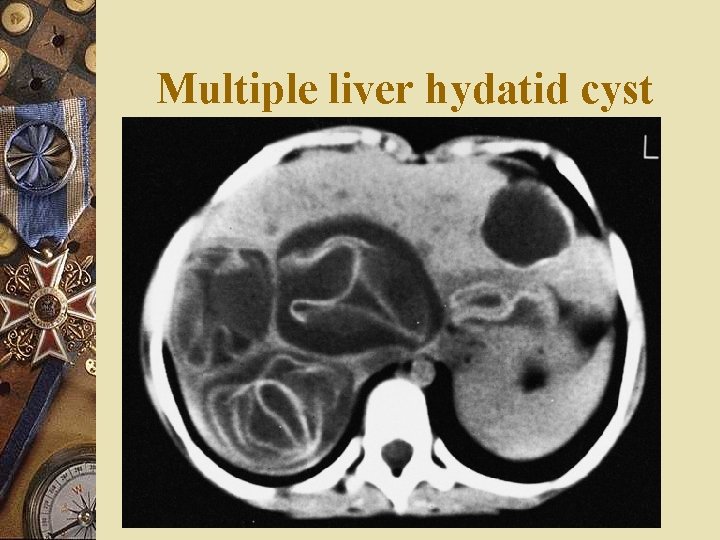
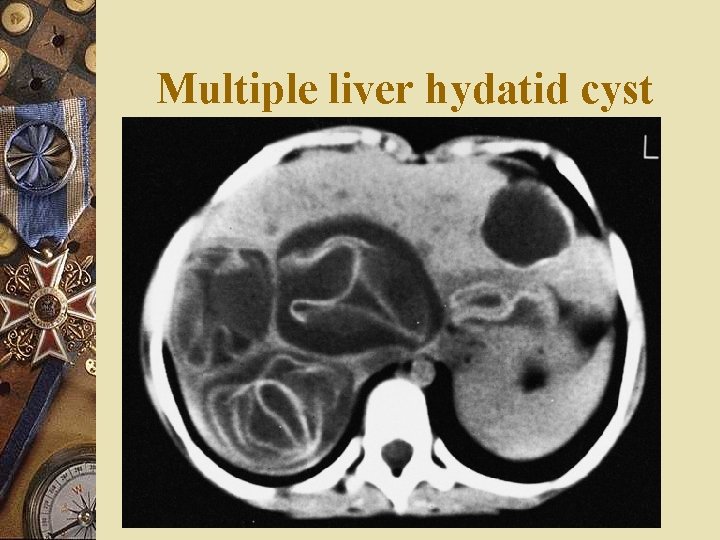
Multiple liver hydatid cyst
SYMPTOMS PRETUMORAL § No symptoms § Alergic reactions and eosinophylia PSEUDOTUMORAL – may become evident on liver surface and produce tumoral effect on adjacent organs: - post-superior – sdr. BUDD-CHIARI - ant-inferior duodenal compression - post-inferior – lombar expasnion may mimick renal problems, IVC compression

SYMPTOMS - centralc – may compress IVC or portal vein – portal hypertension - left lobe –may compress the splenic vein: segmentary portal hypertension COMPLICATIONS
COMPLICATIONS A. SISTEMIC 1. Alergic reactions – may produce even anaphylactic shock when suddenly ruptures 2. Septic complications – may become infected and behaves like liver abscess with billiary communications.
COMPLICATIONS B. LOCAL 1. Fissure: cyst may be evacuated in the billiary tree, main step to many comlpications 2. Rupture w Peritoneal cavity - usually with anaphylactic shock - may be symptom-less - during the operation Peritoneal echinoccocosis w Pleural cavity or pericardium w Bronchial tree: sudden pseudo-vomitus with salty taste, +/- alergic reactions. Risk to seed the opposite lung
TRATAMENT w No treatment- when the parasite is dead and cyst completely encapsulated w Medical treatment – antiparasitic, if the parasit may be accessed, as well as postoperative w Surgical treatment – most cases
STEPS TO FOLLOW 1. Parasite inactivation - injection in the cyst of a parasitic substance 2. Evacuation of the cyst 3. Extraction of the germinal membrane and daughter cysts 4. Manage the cavity. - care for billiary fistulas 5. LIVER RESECTION may be required

TREATMENT - alternatives 1. LIVER RESECTION may be required 2. Ideal cystectomy 3. Percutaneous treatment – US control 4. Laparoscopic treatment 5. Albendazole
TOTAL CYSTECTOMY
TYPICAL EVOLUTION § Slow growth but no complications § Local complications – typical with billairy fistulas § Calcification of the membrane – associated with parasitic death

ECHINOCCOCUS MULTILOCULARIS PATHOLOGY - multiple cavities in liver parenchim, similar to a honey comb SYMPTOMS - hepato-splenomegaly associated with jaundice TREATMENT - parasitic inactivation with intracystic injection -liver transplantation
LIVER ABSCESS
LIVER ABSCESSES Classification Timing: - primary -secondary Evolution: -acute -chronic Ethiology - parasitic (amoebiene) - nonparasitic
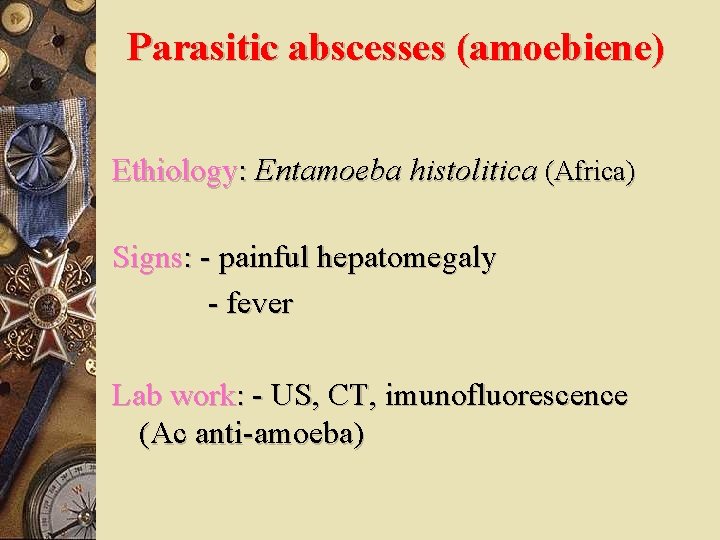
Parasitic abscesses (amoebiene) Ethiology: Entamoeba histolitica (Africa) Signs: - painful hepatomegaly - fever Lab work: - US, CT, imunofluorescence (Ac anti-amoeba)
Liver abscess (non parasitic) • After abdominal sepsis – apendicitis high fever, chils hepatomegaly, jaundice pleural effusion, US thrombosis or air in portal system • After billiary septic complications • After septicemic seeding

LAB WORK Laborator: - High WBC, very high levels or very low levels - ESR - Plain abdominal X-Ray, - US, CT Tratament: SOURCE + - antibyotics, - Percutaneous approach to evacuate and drain - Surgical drainage

Surgical treatment CLICK
LIVER TUMORS
CLASSIFICATION w BENIGN w MALIGNANANT
BENING LIVER TUMORS
HEPATOCYTIC ADENOMA w Well demarcated small, dark brown, with a clear tumoral wall w It may develop into a malignant tumor w Easy to confuse with a hepatoma which has to be ruled out
ADENOMA
Billiary adenoma w Originates in cells lining the billiary canaliculi w Small yellow tumor, but can also develop cystic w In superficial forms, metastasis must be ruled out

HEMANGIOMA w Capillary w Cavernous w Vascular tumor, very frequent encountered w Small to large tumors located anywhere in the liver w Smooth surface, soft, dark-brown or violet in cavernous form (lakes of blood) w Symptoms generated by the size of tumor
LESION THAT MIMICK LIVER TUMORS 1. Focal nodular hyperplasia w w w Frequent in women 40 -50, associated with hormonal supplements and anti-baby pills Usual single lesion but may be multiple 2 pathological forms - solid type – the most frequent. Solid small tumor of hyperplastic hepatocytes. Scar like capsule that enteres and separates the tumor - telangiectatic form
2. Inflamatory pseudotumors w w w Inflammatory granulomas – due to infections propagated through the portal vein More frequent in children and young male adolescents Simptoms: fever, weight loss, billiary obstructions
w Pathology-inflammatory lesion progressively developing in association in pileflebitis w Differential diagnostic : liver malignancies (biopsy) w Treatament – antiinflamatory drugs w Prognostic good
3. Bening cystic tumor *Non – parasitic cysts - solitary : billiary / serosal; - multiple: polycystic disease - dg. US, CT Tratament - nothing - surgical unroofing - percutaneous evacuation
Polycystic disease
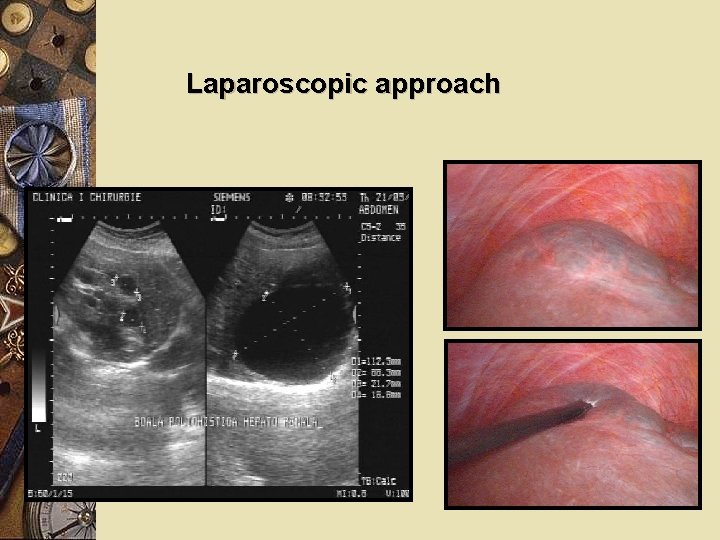
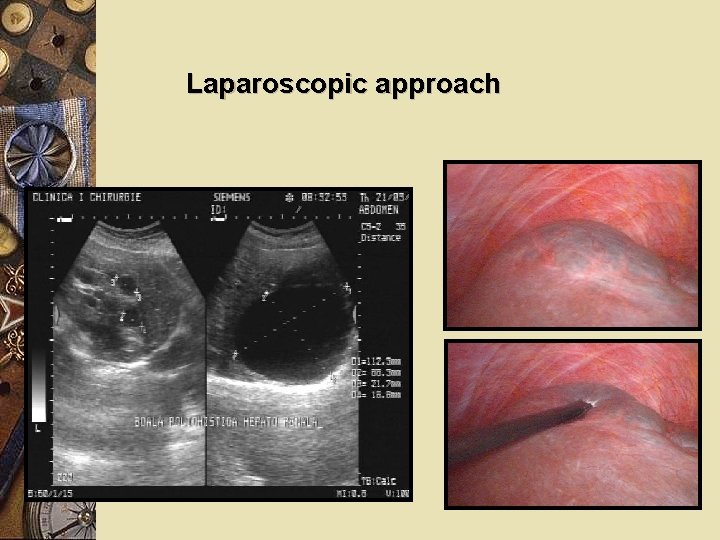
Laparoscopic approach
Malignant liver tumors • Primary liver tumors • Secondary liver tumors
Malignant liver tumors Incidence: more frequent in africa and far East, male patients Path: - Single tumor - Multiple tumors (liver cancer in chirotic livers)
HISTOLOGY ORIGIN w hepatocyt: – hepatocelular carcinoma – hepatoblastoma w Billiary canaliculi: cholangiocarcinoma w Mixt forms w Sarcomas
HEPATOCELULAR CARCINOMA w Adenocarcinoma developed from hepatocytes w More often unique tumor, brownish, soft w Centrifugal development produces compression of adjacent liver structures = pseudocapsule w May also develop bilobar and multicentric but diferentiation from metastasis
CLASIFICATION 1. INFILTRATING – develops on a normal liver without demarcation between tumor and normal tissue 2. EXPANDING– well encapsulated tumors, developed on chirrhotic liver 3. MIXT 4. DIFUSE – multiple nodule in liver chirrosis, nodules having no tendency to become confluent.

pedunculated tumor multifocal infiltrating
Spreading w Centrifugal – compressing adjecent liver tissue w Venos – anterograd şi retrograd w Limphatic – regional lymphnodes w Direct invasion of diaphragm
Hepatocelular carcinoma with satelite lesions
CLINICAL SIGNS SUBIECTIV w Discomfort in RUQ, but no pain w anorexia, weight loss w Low grade fever OBIECTIV w Hard hepatomegaly w jaundice w Sings of UGI bleeding w Ascites
LAB WORK w Anemia and increased ESR w High levels of AFP w Ultrasound imaging w CECT cu substanţă de contrast w MRI – indicaţii limitate w Angiography (CT angiography) – abnormal type o vascularisation w Laparoscopy +/- biopsy
PROGNOSTIC w Not very good in large tumors w With surgical treatment <10% survivaal at 5 y w MTS pleuropulmonary, bones, LN
COMPLICATIONS w Intraperitoneal rupture and hemoperitoneum w Necrosis + infections followed by septic complications w Compression of intra- or extrahepatic bile ducts and joundice w Hemobilia

TREATMENT w Systemic chemotherapy w Chemoembolisation w Arterial emolisation w Distruction with alchool injection, radofrequency, heat, etc w Radiotherapy w Cryosurgery w Surgical resection

TREATMENT w NEW DEVELOPMENTS – Radiotherapy using intratissular irradiation – Photodynamic therapy – Inteligent molecules: Anti VEGF
Cholangiocarcinoma w Origine: epithelium form billiary canaliculi w Ethiology: – Sclerosis cholangitis – Clonorchis sinensis w Pathology: glandular proliferation with mucin secretion, surrounded by dens stroma w Differential diagnostic with hepatoma: immunohystochemistry
CLINICAL DIAGNOSTIC w Non-specific symptoms LAB w US scan w CT w AFP, CEA, CA 19 -9 w Ac anti mytochondrial w FAlc
Cholangiocarcinoma
HEPATOMA ON CIRRHOTIC LIVER w Patients with high risk for hepatoma (B and C hepatitis) w Screenign: – AFP – US scan CT scan
TREATMENT w Destruction within oncologic limits (RF, Cryo, Heat) w Resection of tumor with free margins w Maintain enough liver tissue for sufficient liver function ***methods to increase the volume of the liver
Metastatic liver cancer second most common site for MTS
Primary tumors w Stomach w Pancreas w Genital (prostate, ovary, uterus) w Skin (malignant melanoma) w Breast
SYMPTOMS w May be asymptomatic w Symptoms generated by the primary w Symptoms generated by products produced by tumor or MTS w PLUS – Liver enlargment – Liver failure
LAB WORK w All imagistic evaluations work in different degrees w Monitoring programs after control of primary tumors w Tumoral markers w PET CT w FIND the primary

CT spiral:

TREATMENT and PROGNOSIS DEPEND ON THE PRIMARY TUMOR
TREATMENT w Surgical – usually addressed to single tumors. If adjacent hepatectomy – care for liver function w Destruction w Chemoembolisation w Systemic chemotherapy + inteligent molecules
 Dubin johnson syndrome
Dubin johnson syndrome Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Chúa yêu trần thế
Chúa yêu trần thế Các môn thể thao bắt đầu bằng tiếng đua
Các môn thể thao bắt đầu bằng tiếng đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính thế năng
Công thức tính thế năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Phép trừ bù
Phép trừ bù độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thế nào là giọng cùng tên
Thế nào là giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Fecboak
Fecboak Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot Số nguyên tố là gì
Số nguyên tố là gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Vicarious felidae
Vicarious felidae Trauma gestig behindert
Trauma gestig behindert Jenis jenis trauma thorax
Jenis jenis trauma thorax Tscyc screening form
Tscyc screening form Trauma sensitief lesgeven
Trauma sensitief lesgeven Trauma awareness and treatment center utah
Trauma awareness and treatment center utah 4 r's trauma informed care
4 r's trauma informed care Trauma informed care lgbtq
Trauma informed care lgbtq Miller classification
Miller classification Miemss trauma decision tree
Miemss trauma decision tree Examples of little t trauma
Examples of little t trauma Trauma bonding definition
Trauma bonding definition Trauma timeline template
Trauma timeline template Anita ravi md
Anita ravi md The golden hour ems
The golden hour ems Triune brain theory and trauma
Triune brain theory and trauma Trauma informed approach
Trauma informed approach Nethercutt trauma center
Nethercutt trauma center Psykoedukation ptsd
Psykoedukation ptsd Trauma bond
Trauma bond Neumotrax
Neumotrax National trauma data bank annual report 2020
National trauma data bank annual report 2020 Emergency management of maxillofacial trauma
Emergency management of maxillofacial trauma Escala abreviada de lesiones
Escala abreviada de lesiones Ocular trauma score
Ocular trauma score Adhd vs trauma
Adhd vs trauma I was not aware
I was not aware Rts trauma
Rts trauma Trauma-informed care activities for staff
Trauma-informed care activities for staff Types of physical trauma
Types of physical trauma Childhood trauma discussion questions
Childhood trauma discussion questions Criteri nexus trauma
Criteri nexus trauma Trauma informed physical environment
Trauma informed physical environment Tatalaksana trauma thorax
Tatalaksana trauma thorax Trauma-informed workplace assessment
Trauma-informed workplace assessment Revised trauma score italiano
Revised trauma score italiano Cpt trust star worksheet
Cpt trust star worksheet Holiday segar anak
Holiday segar anak Derrapamento
Derrapamento Cavitacion en trauma
Cavitacion en trauma Cinematica
Cinematica Lippincott williams & wilkins
Lippincott williams & wilkins Management of patients with neurologic trauma
Management of patients with neurologic trauma A 23 year old male experienced severe head trauma
A 23 year old male experienced severe head trauma International association of trauma professionals
International association of trauma professionals Certified clinical trauma professional
Certified clinical trauma professional Trauma-informed questions for clients
Trauma-informed questions for clients Pulmonary trauma
Pulmonary trauma Brute force trauma
Brute force trauma 4 r's trauma informed care
4 r's trauma informed care Revised trauma score
Revised trauma score Tarn database
Tarn database Robyn bradey vicarious trauma
Robyn bradey vicarious trauma Trauma dumping examples
Trauma dumping examples