CERTIFIED CLINICAL TRAUMA PROFESSIONAL Trauma PTSD Grief Loss

























- Slides: 80
CERTIFIED CLINICAL TRAUMA PROFESSIONAL: Trauma, PTSD, Grief & Loss International Association of Trauma Professionals J. Eric Gentry, Ph. D, LMHC Board-Certified Expert in Traumatic Stress

Day I Welcome
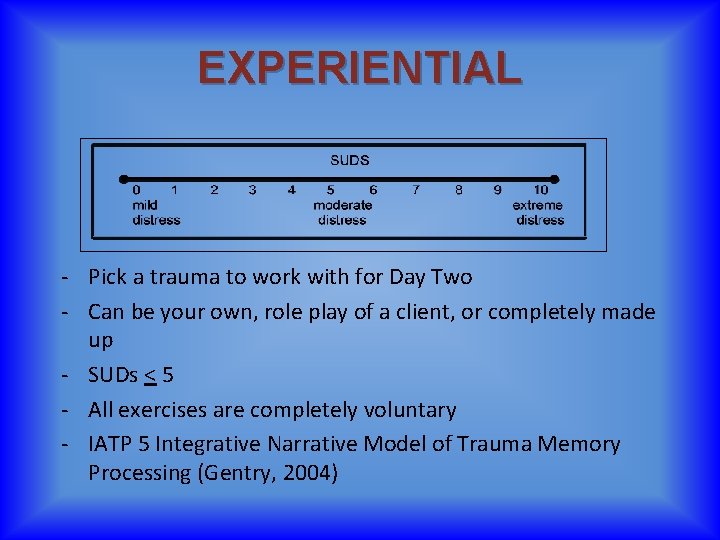
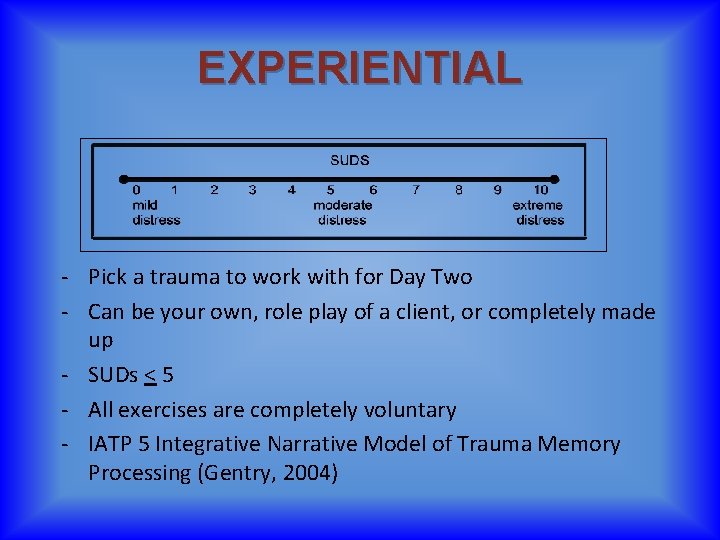
EXPERIENTIAL - Pick a trauma to work with for Day Two - Can be your own, role play of a client, or completely made up - SUDs < 5 - All exercises are completely voluntary - IATP 5 Integrative Narrative Model of Trauma Memory Processing (Gentry, 2004)
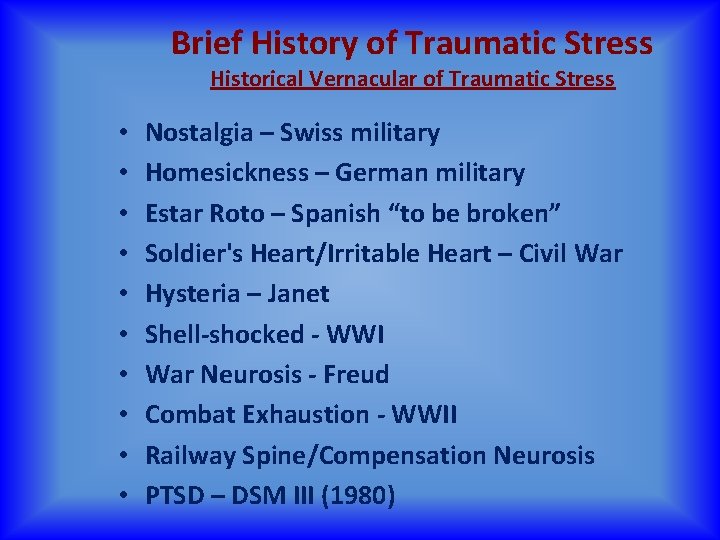
Brief History of Traumatic Stress Historical Vernacular of Traumatic Stress • • • Nostalgia – Swiss military Homesickness – German military Estar Roto – Spanish “to be broken” Soldier's Heart/Irritable Heart – Civil War Hysteria – Janet Shell-shocked - WWI War Neurosis - Freud Combat Exhaustion - WWII Railway Spine/Compensation Neurosis PTSD – DSM III (1980)

Brief History of Traumatic Stress 19 th Century
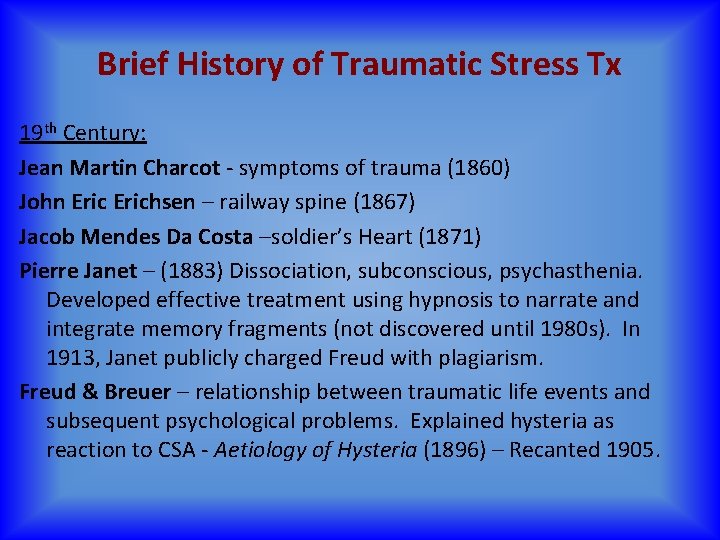
Brief History of Traumatic Stress Tx 19 th Century: Jean Martin Charcot - symptoms of trauma (1860) John Erichsen – railway spine (1867) Jacob Mendes Da Costa –soldier’s Heart (1871) Pierre Janet – (1883) Dissociation, subconscious, psychasthenia. Developed effective treatment using hypnosis to narrate and integrate memory fragments (not discovered until 1980 s). In 1913, Janet publicly charged Freud with plagiarism. Freud & Breuer – relationship between traumatic life events and subsequent psychological problems. Explained hysteria as reaction to CSA - Aetiology of Hysteria (1896) – Recanted 1905.
Brief History of Traumatic Stress Tx 20 th Century
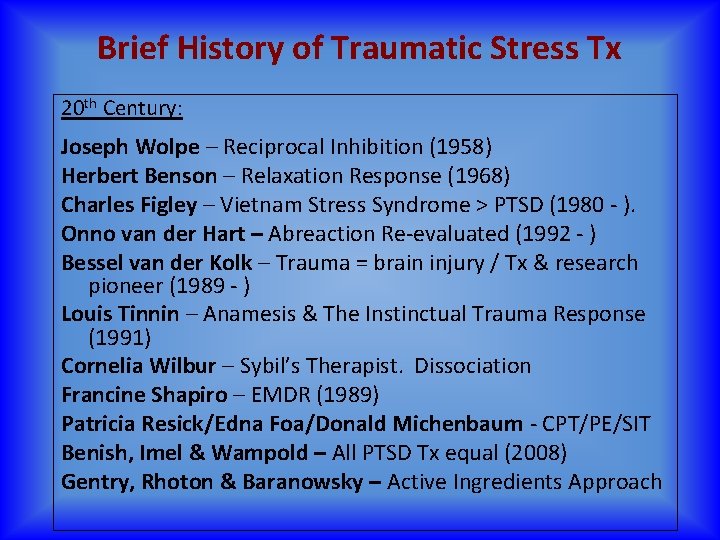
Brief History of Traumatic Stress Tx 20 th Century: Joseph Wolpe – Reciprocal Inhibition (1958) Herbert Benson – Relaxation Response (1968) Charles Figley – Vietnam Stress Syndrome > PTSD (1980 - ). Onno van der Hart – Abreaction Re-evaluated (1992 - ) Bessel van der Kolk – Trauma = brain injury / Tx & research pioneer (1989 - ) Louis Tinnin – Anamesis & The Instinctual Trauma Response (1991) Cornelia Wilbur – Sybil’s Therapist. Dissociation Francine Shapiro – EMDR (1989) Patricia Resick/Edna Foa/Donald Michenbaum - CPT/PE/SIT Benish, Imel & Wampold – All PTSD Tx equal (2008) Gentry, Rhoton & Baranowsky – Active Ingredients Approach
Trauma Treatment for the 21 st Century THE ACTIVE INGREDIENTS APPROACH International Association of Trauma Professionals 9
Clinical Excellence: Breaking it down • Systematic The process is based on an organized and structured “active ingredients” approach • Deliberate (no Automaticity) In order to be successful, we must develop a belief that a sustainable trauma informed and sensitive approach can permeate and be embraced across the organization. • Continuous A never-ending process…no matter how good we think we are doing, there is always room for improvement. Dr. Bob’s mantra: “sucking a little less each day” International Association of Trauma Professionals 10
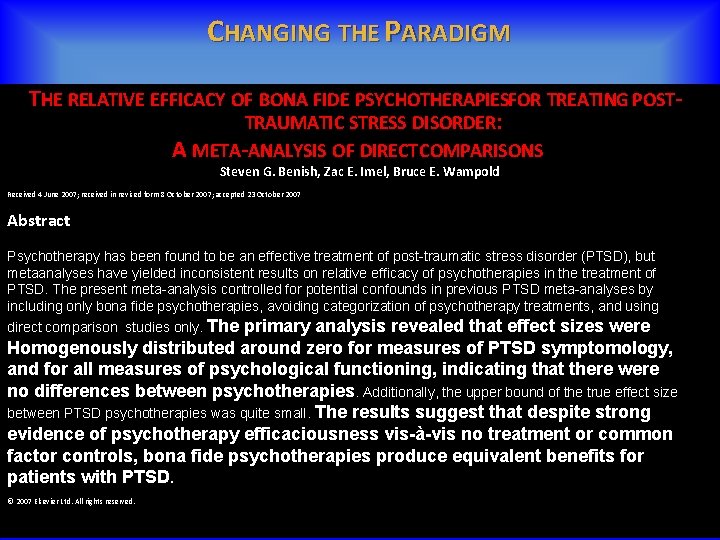
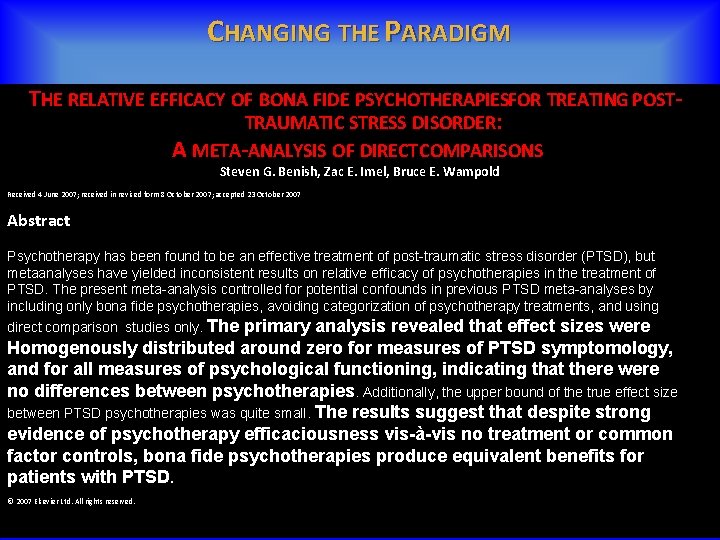
CHANGING THE PARADIGM THE RELATIVE EFFICACY OF BONA FIDE PSYCHOTHERAPIESFOR TREATING POSTTRAUMATIC STRESS DISORDER: A META-ANALYSIS OF DIRECT COMPARISONS Steven G. Benish, Zac E. Imel, Bruce E. Wampold Received 4 June 2007; received in revised form 8 October 2007; accepted 23 October 2007 Abstract Psychotherapy has been found to be an effective treatment of post-traumatic stress disorder (PTSD), but metaanalyses have yielded inconsistent results on relative efficacy of psychotherapies in the treatment of PTSD. The present meta-analysis controlled for potential confounds in previous PTSD meta-analyses by including only bona fide psychotherapies, avoiding categorization of psychotherapy treatments, and using direct comparison studies only. The primary analysis revealed that effect sizes were Homogenously distributed around zero for measures of PTSD symptomology, and for all measures of psychological functioning, indicating that there were no differences between psychotherapies. Additionally, the upper bound of the true effect size between PTSD psychotherapies was quite small. The results suggest that despite strong evidence of psychotherapy efficaciousness vis-à-vis no treatment or common factor controls, bona fide psychotherapies produce equivalent benefits for patients with PTSD. © 2007 Elsevier Ltd. All rights reserved.

Wampold & Imel (2015) “Given the evidence that treatments are about equally effective, that treatments delivered in clinical settings are effective (and as effective as that provided in clinical trials), that the manner in which treatments are provided are much more important than which treatment is provided, mandating particular treatments seems illogical. In addition, given the expense involved in “rolling out” evidence-based treatments in private practices, agencies, and in systems of care, it seems unwise to mandate any particular treatment. ”
Cloitre M, Courtois CA, Charuvastra A, Carapezza R, Stolbach BC, Green BL. (2011). Treatment of complex PTSD: results of the ISTSS expert clinician survey on best practices. J Trauma Stress. 2011 Dec; 24(6): 615 -27. doi: 10. 1002/jts. 20697. Epub 2011 Dec 6. • • • emotion regulation strategies narration of trauma memory cognitive restructuring anxiety and stress management interpersonal skills. International Association of Trauma Professionals 13

Psychotherapies for PTSD: what do they have in common? Schnyder, U. , Ehlers, A. , Elbert, T. , Foa, E. B. , Gersons, B. P. R. , Resick, P. A. , … Cloitre, M. (2015). European Journal of Psychotraumatology, 6, 10. 3402/ejpt. v 6. 28186. http: //doi. org/10. 3402/ejpt. v 6. 28186 • Psychoeducation • emotion regulation and coping skills • imaginal exposure • cognitive processing • restructuring • meaning making • emotions • memory processes International Association of Trauma Professionals 14
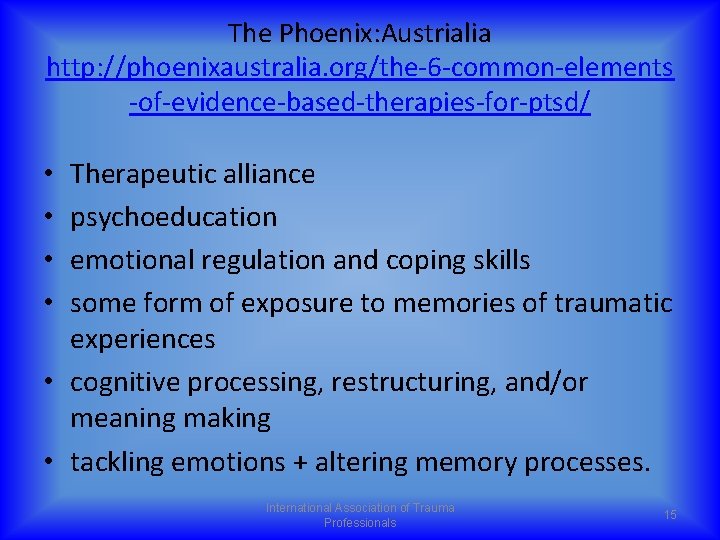
The Phoenix: Austrialia http: //phoenixaustralia. org/the-6 -common-elements -of-evidence-based-therapies-for-ptsd/ Therapeutic alliance psychoeducation emotional regulation and coping skills some form of exposure to memories of traumatic experiences • cognitive processing, restructuring, and/or meaning making • tackling emotions + altering memory processes. • • International Association of Trauma Professionals 15
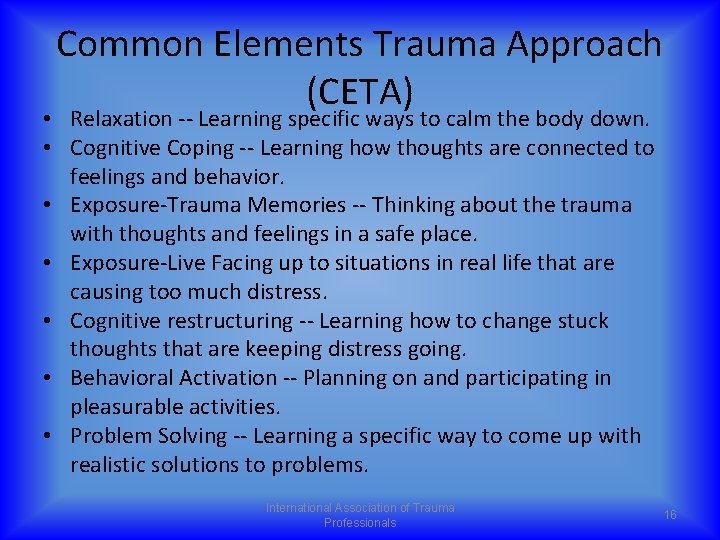
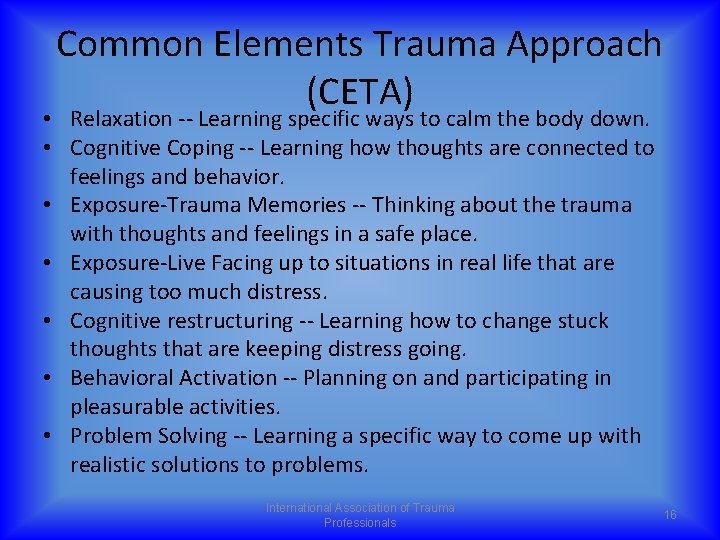
Common Elements Trauma Approach (CETA) • Relaxation -- Learning specific ways to calm the body down. • Cognitive Coping -- Learning how thoughts are connected to feelings and behavior. • Exposure-Trauma Memories -- Thinking about the trauma with thoughts and feelings in a safe place. • Exposure-Live Facing up to situations in real life that are causing too much distress. • Cognitive restructuring -- Learning how to change stuck thoughts that are keeping distress going. • Behavioral Activation -- Planning on and participating in pleasurable activities. • Problem Solving -- Learning a specific way to come up with realistic solutions to problems. International Association of Trauma Professionals 16

Trauma Competency: An Active Ingredients Approach to Treating PTSD Gentry, Baranowsky & Rhoton (in press). Journal of Counseling and Development • cognitive restructuring/psychoeducation • a deliberate and continually improving therapeutic relationship • relaxation and self-regulation • exposure via narrative of traumatic experiences International Association of Trauma Professionals 17
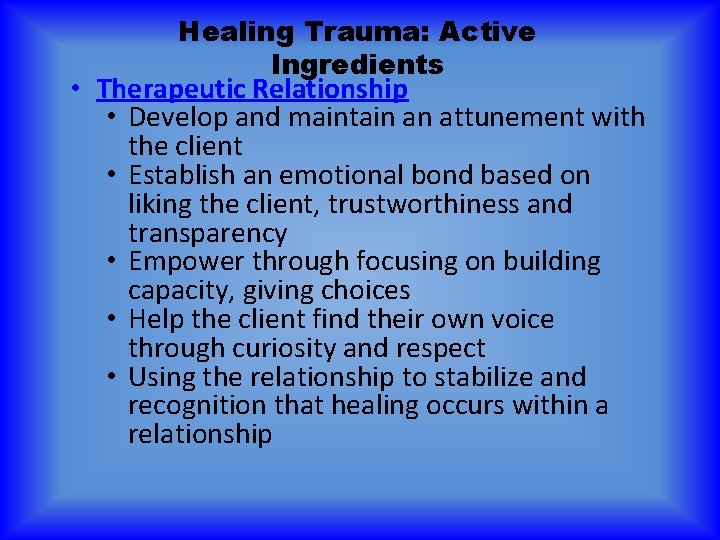
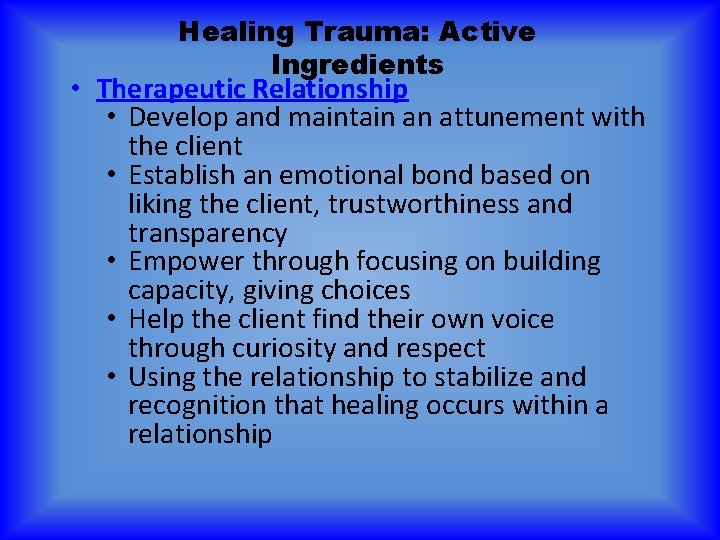
Healing Trauma: Active Ingredients • Therapeutic Relationship • Develop and maintain an attunement with the client • Establish an emotional bond based on liking the client, trustworthiness and transparency • Empower through focusing on building capacity, giving choices • Help the client find their own voice through curiosity and respect • Using the relationship to stabilize and recognition that healing occurs within a relationship
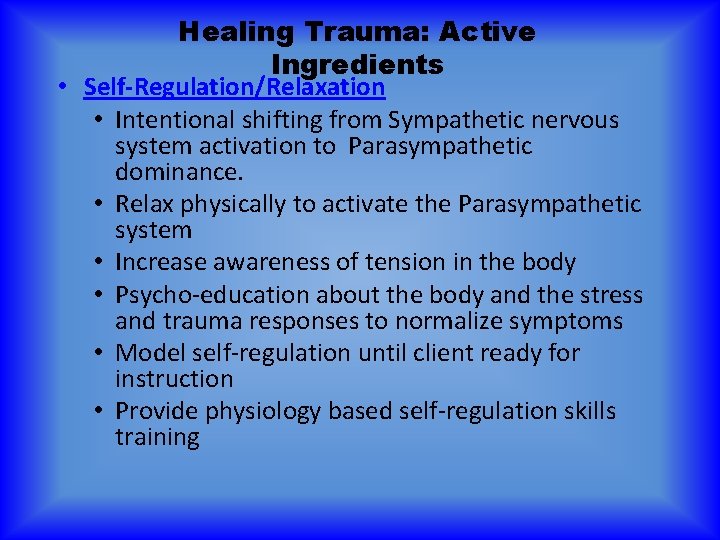
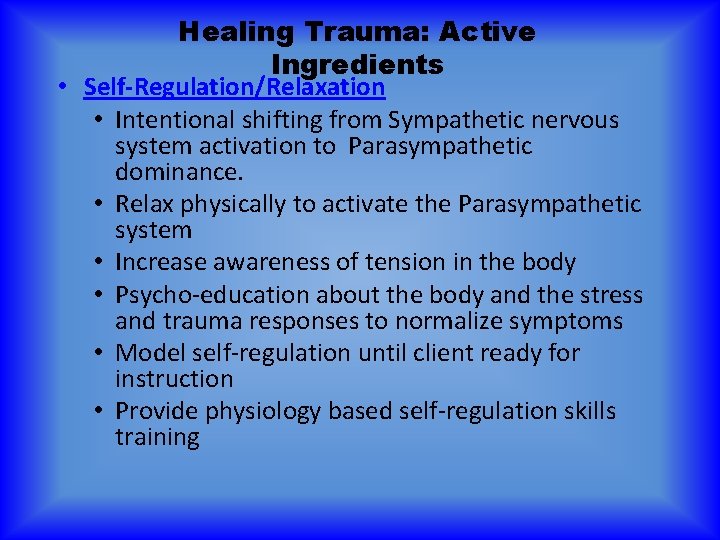
Healing Trauma: Active Ingredients • Self-Regulation/Relaxation • Intentional shifting from Sympathetic nervous system activation to Parasympathetic dominance. • Relax physically to activate the Parasympathetic system • Increase awareness of tension in the body • Psycho-education about the body and the stress and trauma responses to normalize symptoms • Model self-regulation until client ready for instruction • Provide physiology based self-regulation skills training
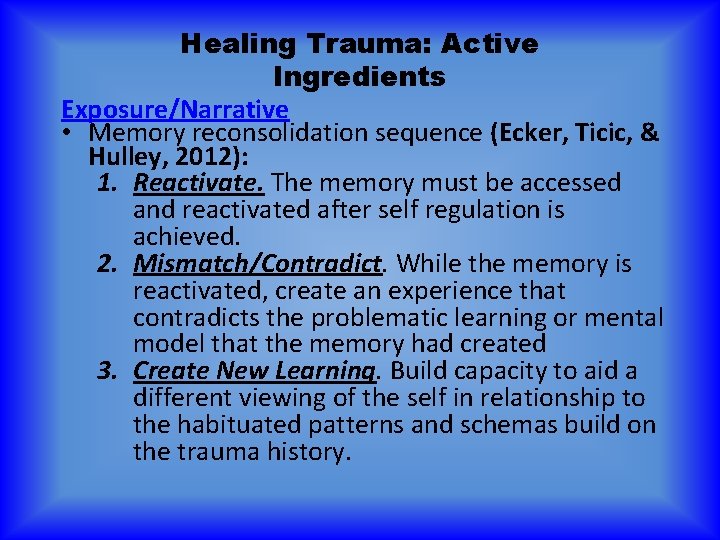
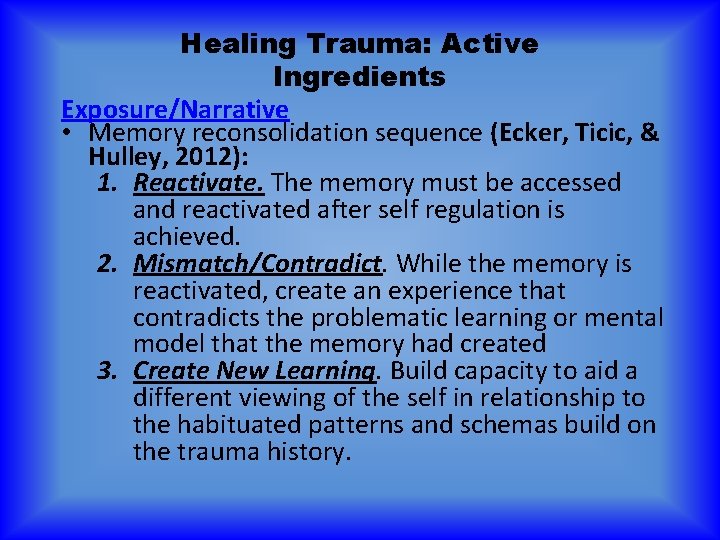
Healing Trauma: Active Ingredients Exposure/Narrative • Memory reconsolidation sequence (Ecker, Ticic, & Hulley, 2012): 1. Reactivate. The memory must be accessed and reactivated after self regulation is achieved. 2. Mismatch/Contradict. While the memory is reactivated, create an experience that contradicts the problematic learning or mental model that the memory had created 3. Create New Learning. Build capacity to aid a different viewing of the self in relationship to the habituated patterns and schemas build on the trauma history.
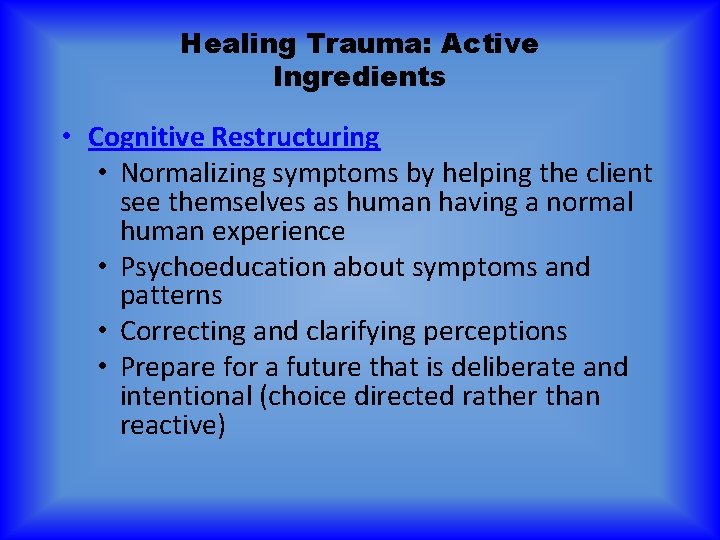
Healing Trauma: Active Ingredients • Cognitive Restructuring • Normalizing symptoms by helping the client see themselves as human having a normal human experience • Psychoeducation about symptoms and patterns • Correcting and clarifying perceptions • Prepare for a future that is deliberate and intentional (choice directed rather than reactive)
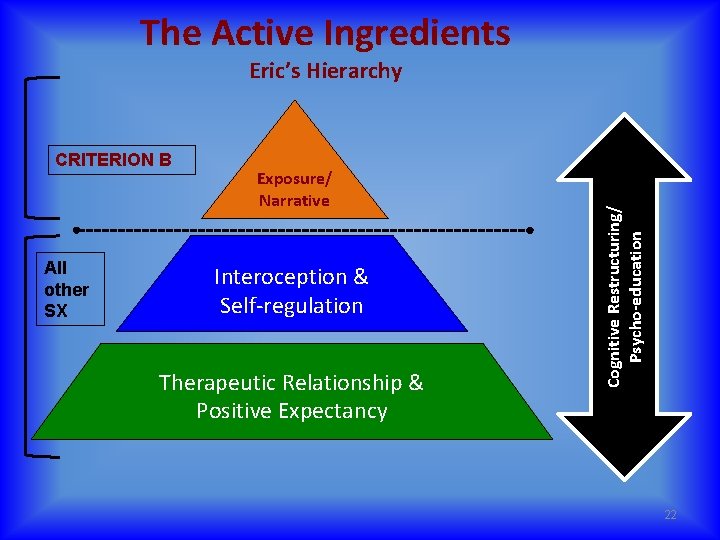
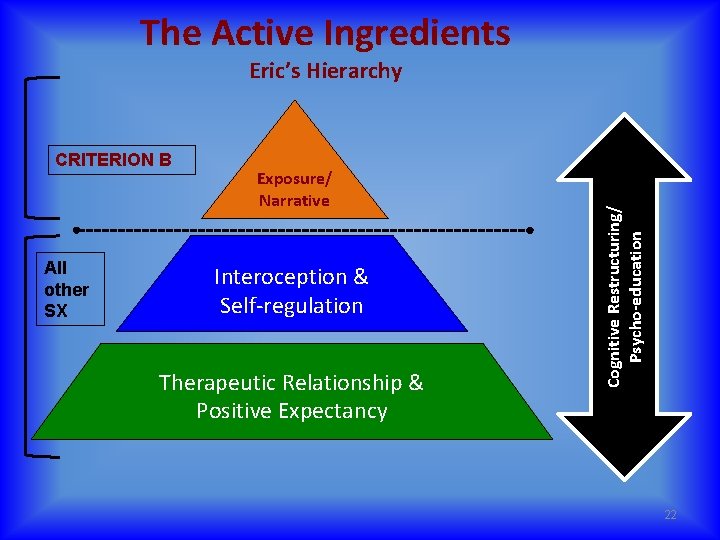
The Active Ingredients CRITERION B All other SX Exposure/ Narrative Interoception & Self-regulation Therapeutic Relationship & Positive Expectancy Cognitive Restructuring/ Psycho-education Eric’s Hierarchy 22

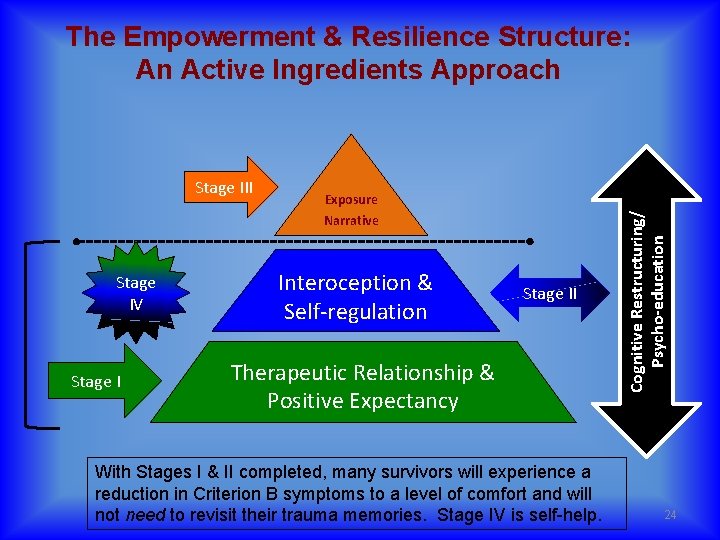
The Empowerment & Resilience Structure: An Active Ingredients Approach I. Preparation & Relationship II. Psychoeducation & Selfregulation III. Integration & Desensitization IV. Post Traumatic Growth & Resilience Rhoton & Gentry, 2014
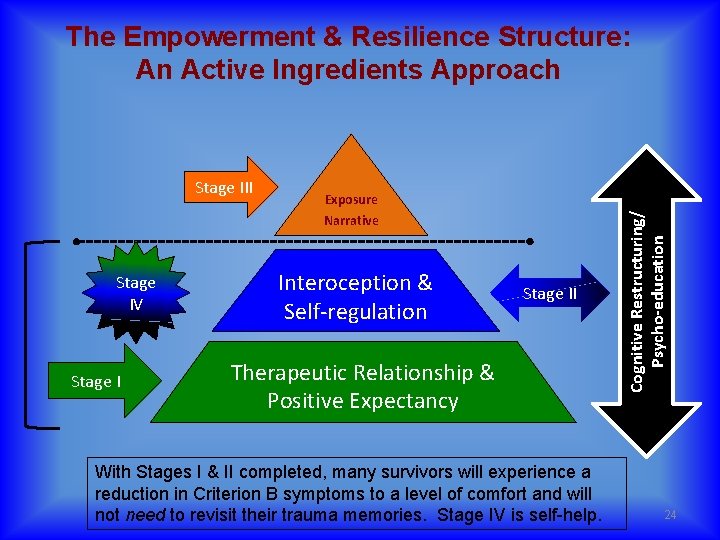
Stage III Stage IV Stage I Exposure Narrative Interoception & Self-regulation Stage II Therapeutic Relationship & Positive Expectancy With Stages I & II completed, many survivors will experience a reduction in Criterion B symptoms to a level of comfort and will not need to revisit their trauma memories. Stage IV is self-help. Cognitive Restructuring/ Psycho-education The Empowerment & Resilience Structure: An Active Ingredients Approach 24

Preparation & Relationship STAGE I International Association of Trauma Professionals 25

Stage I: Preparation & Relationship • Orientation and acculturation around therapy process (informed consent) • Develop Expectancy • Discovering capacities and strengths while instilling faith and hope in therapy process • Begin and continue Feedback Informed Therapy (FIT) • Formal and Informal assessments used to increase relationship and connection • Assessing patterns and developing global goals that will fine-tuned through the process International Association of Trauma Professionals 26
Resiliency “That which is to give light Must endure burning” - Viktor Frankl
Between stimulus and response there is a space. In that space is our power to choose our response. In our response lies our growth and our freedom. - Viktor Frankl

In 2013, Feedback Informed Treatment (FIT)– that is, formally using measures of progress and therapeutic alliance to guide care– was deemed an evidence-based practice by SAMHSA, and listed on the official NREPP website. It’s one of those good ideas. Research to date shows that FIT as much as doubles the effectiveness of behavioral health services, while decreasing costs, deterioration and dropout rates. SCOTT D MILLER - FEEDBACK-INFORMED THERAPY
Suggestions for Positive Outcomes www. scottdmiller. com 1. Collect empirical data evaluating the quality of therapeutic relationship 2. Generate honest feedback from client on methods to improve therapy (i. e. relational) 3. Be willing to change toward what works best for client—demonstrate that change


Psychoeducation & Skills-building STAGE II International Association of Trauma Professionals 32
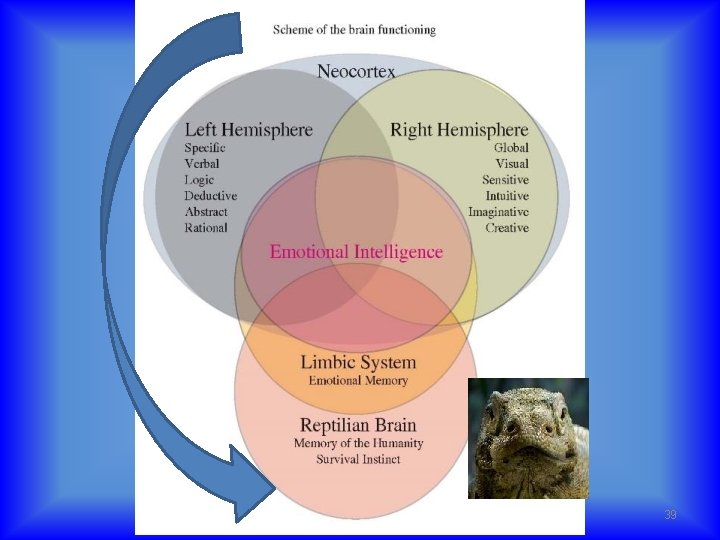
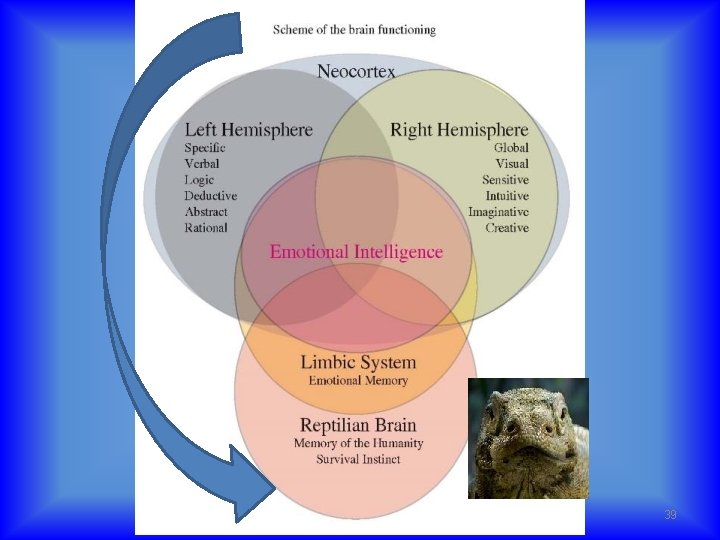
Stage II • Teach the mechanics of the threat response system • Creating a common language to enhance ease of discussion and relational connection • Teach impact of environment • Convert discussions of anger, sadness, fear etc, to physiological dysregulation • Normalize internal negative messages • Normalize perceptions of self, significant relationships and the world view • Normalize relationship, emotional and cognitive patterns. • Explore meaning of behaviors for the client • Tools for hope/and other self-regulation skills International Association of Trauma Professionals 33

Making it Personal UNDERSTANDING TRAUMA
STRESS Cause and Effect Causes Effects

Are You 100% Safe Right Now?
The Body’s Radar System: Anterior Cingulate of the Cortex (ACC) 37

Anterior Cingulate Cortex Sensory input
39

Perceived Threat Physiological Brain Mechanics Other Effects ▲Heart Rate ▲ Basal Ganglia & Thalamic Fx ▲Obsession ▲ Breathing Rate ▼ Neo-cortical Fx ▲Compulsion ▼ Breathing Volume ▼Frontal Lobe activity ▼ Speed & Agility ▼Executive Fx ▼Fine motor control ▼Emotional regulation Centralized Circulation ▲ Muscle Tension ▼Temporal Lobe Activity ▼ Strength ▼Language (Werneke’s) ▼Speech (Broca’s) ▲ Energy ▼ Anterior Cingulate ▲ DIS-EASE Fight Constricted thoughts & behaviors Fatigue OR Flight

Neocortical FX ENERGY Stress & Reactivity THRESHOLD Compulsive Action Aggression or Avoidance Constricted Muscles International Association of Trauma Professionals 41
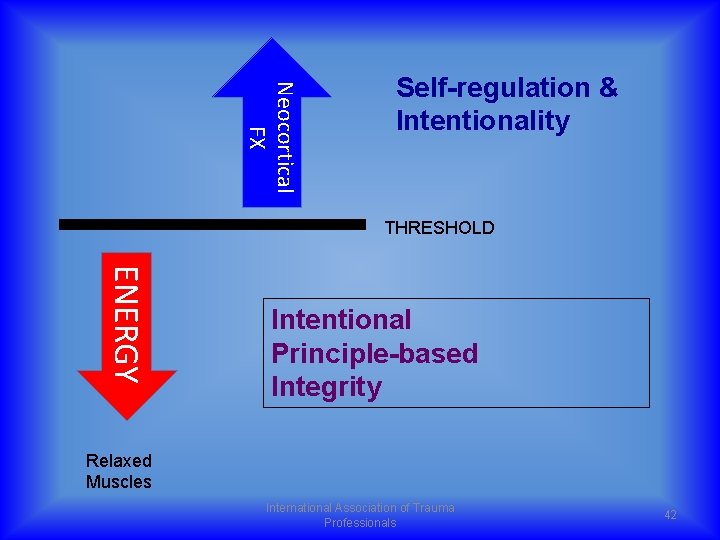
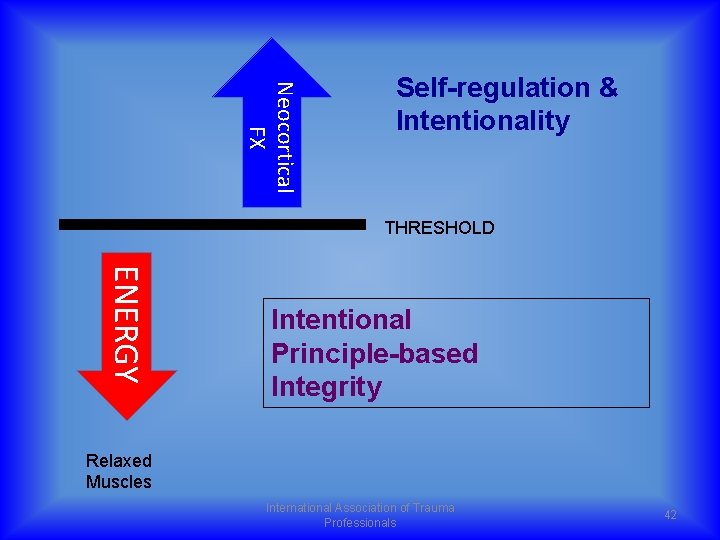
Neocortical FX Self-regulation & Intentionality THRESHOLD ENERGY Intentional Principle-based Integrity Relaxed Muscles International Association of Trauma Professionals 42
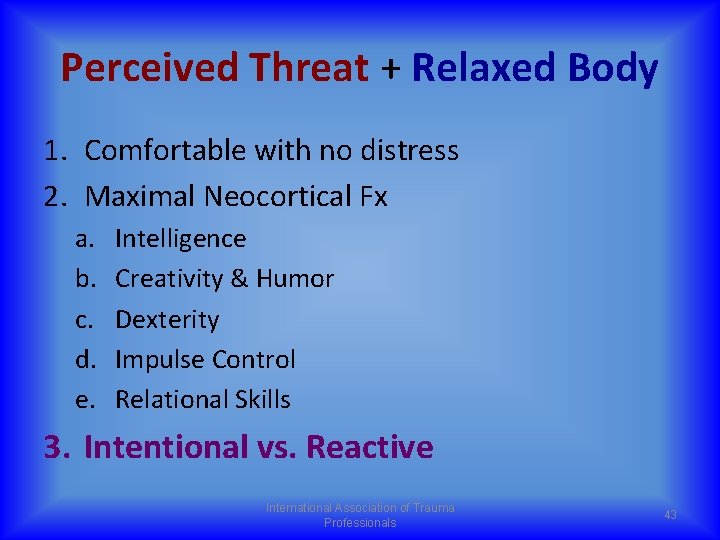
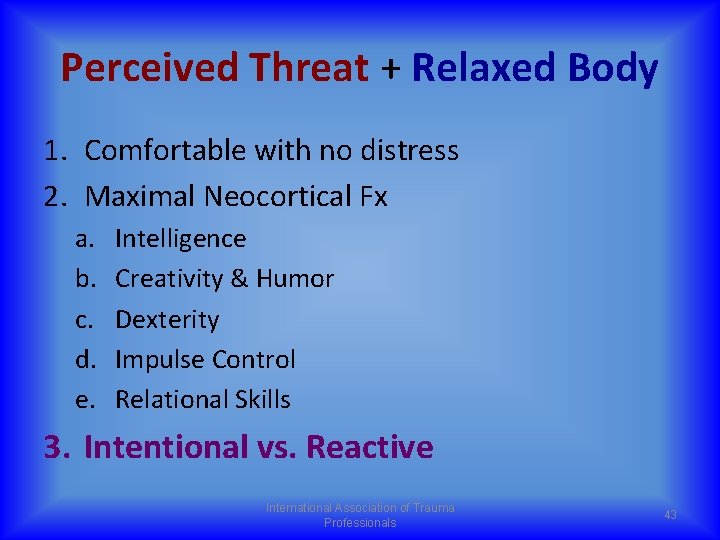
Perceived Threat + Relaxed Body 1. Comfortable with no distress 2. Maximal Neocortical Fx a. b. c. d. e. Intelligence Creativity & Humor Dexterity Impulse Control Relational Skills 3. Intentional vs. Reactive International Association of Trauma Professionals 43
Quick Write & Pair/Share 44
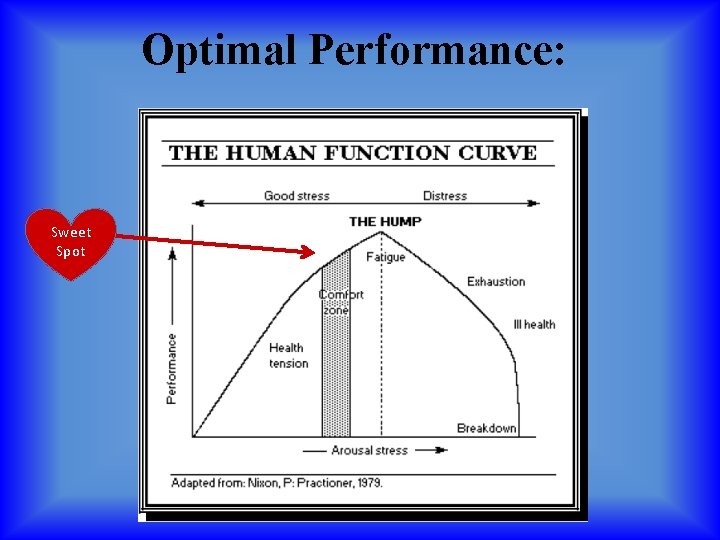
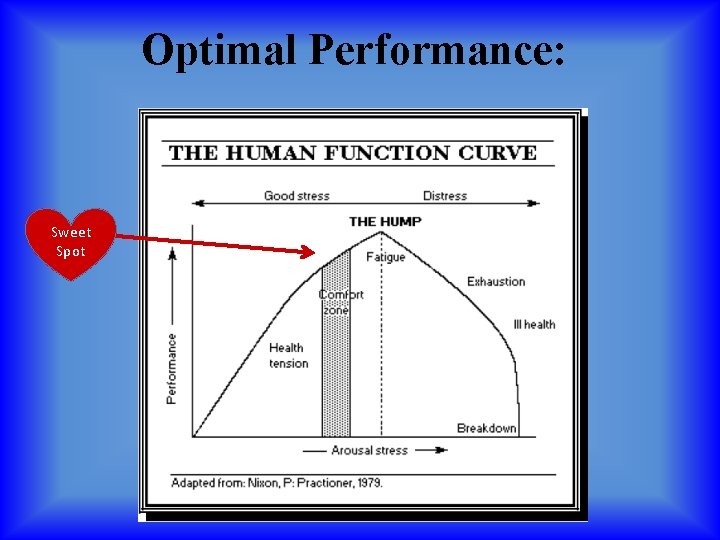
Optimal Performance: Sweet Spot
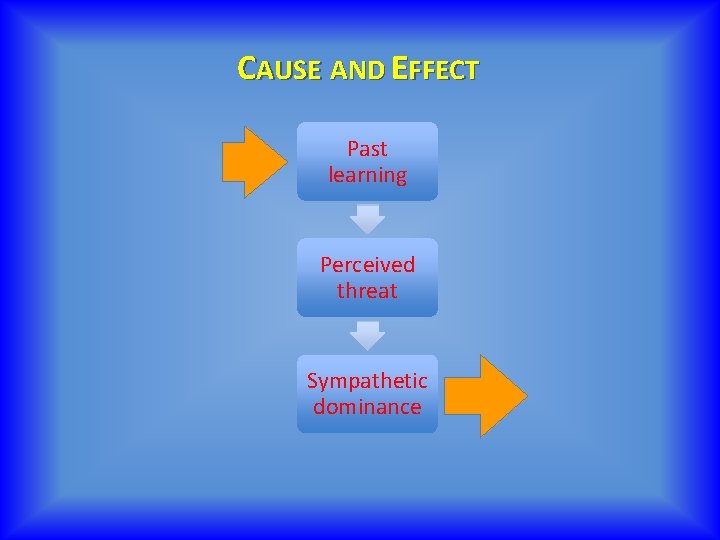
CAUSE AND EFFECT Past learning Perceived threat Sympathetic dominance
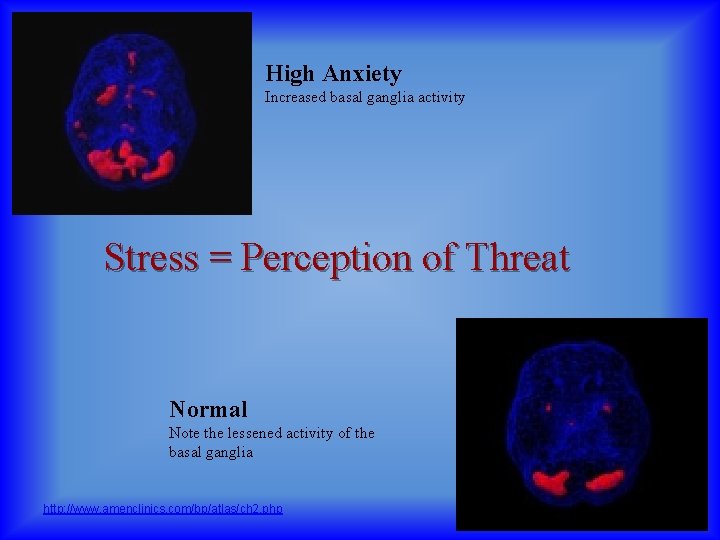
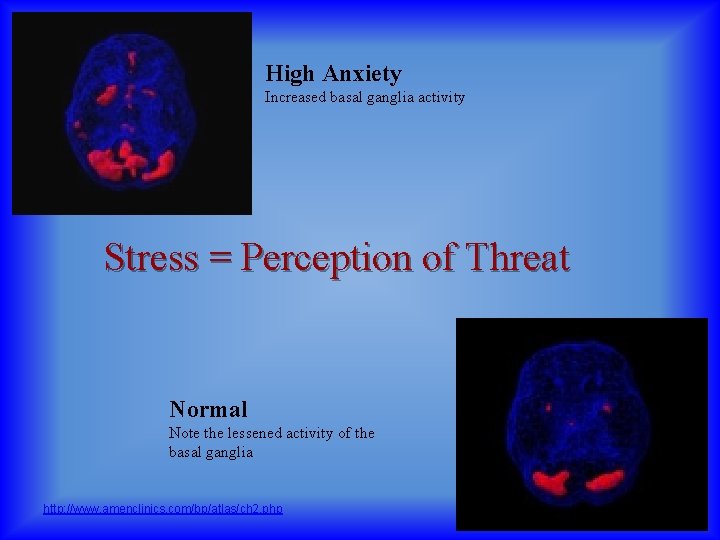
High Anxiety Increased basal ganglia activity Stress = Perception of Threat Normal Note the lessened activity of the basal ganglia http: //www. amenclinics. com/bp/atlas/ch 2. php
SELF-REGULATION Interoception & Balancing the ANS
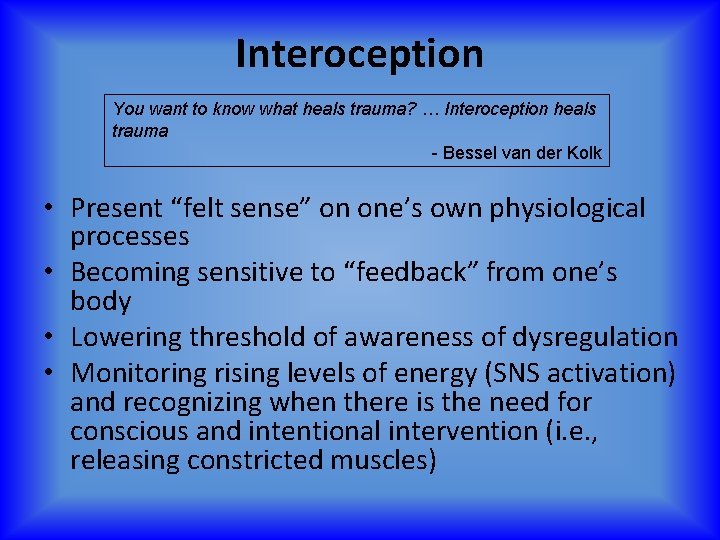
Interoception You want to know what heals trauma? … Interoception heals trauma - Bessel van der Kolk • Present “felt sense” on one’s own physiological processes • Becoming sensitive to “feedback” from one’s body • Lowering threshold of awareness of dysregulation • Monitoring rising levels of energy (SNS activation) and recognizing when there is the need for conscious and intentional intervention (i. e. , releasing constricted muscles)

Interoception + Self-Regulation = Trauma Resolution Chill Developing “bodyfull-ness”

SKILLS Self-Regulation • • Body Scan/”Wet Noodle” Diaphragmatic Breathing Peripheral vision Pelvic floor relaxation 51
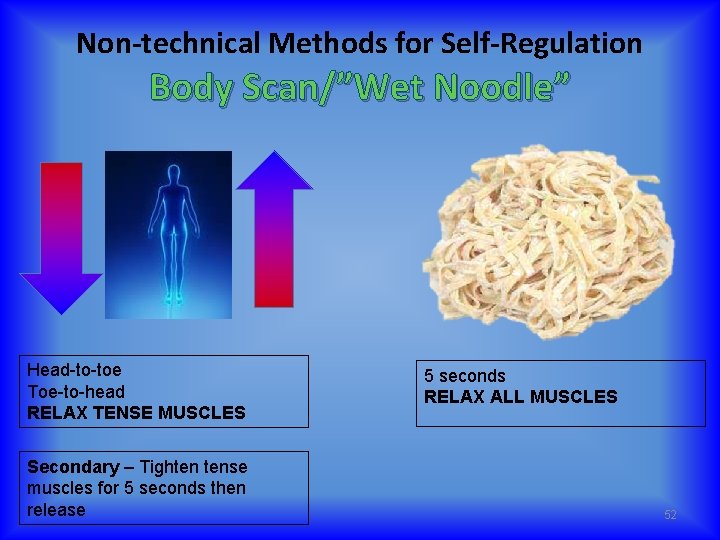
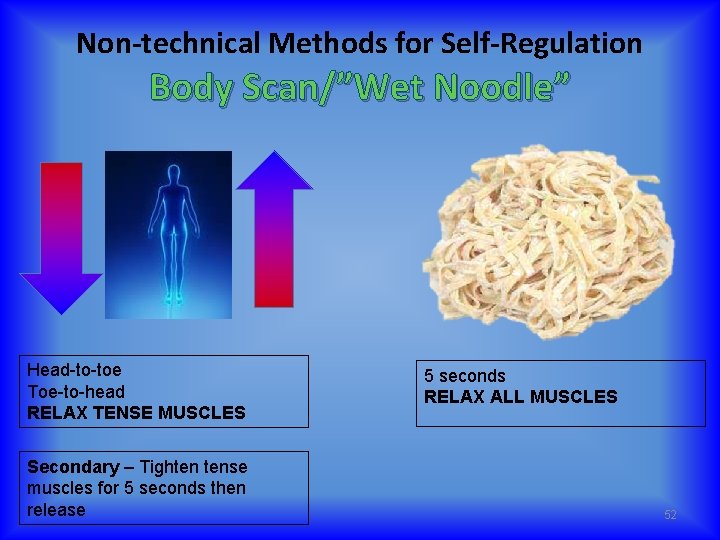
Non-technical Methods for Self-Regulation Body Scan/”Wet Noodle” Head-to-toe Toe-to-head RELAX TENSE MUSCLES Secondary – Tighten tense muscles for 5 seconds then release 5 seconds RELAX ALL MUSCLES 52
Self Regulation: Peripheral Vision • Focus on a spot straight ahead • Keeping your focus, widen your field of view and notice what you see in your peripheral vision 53
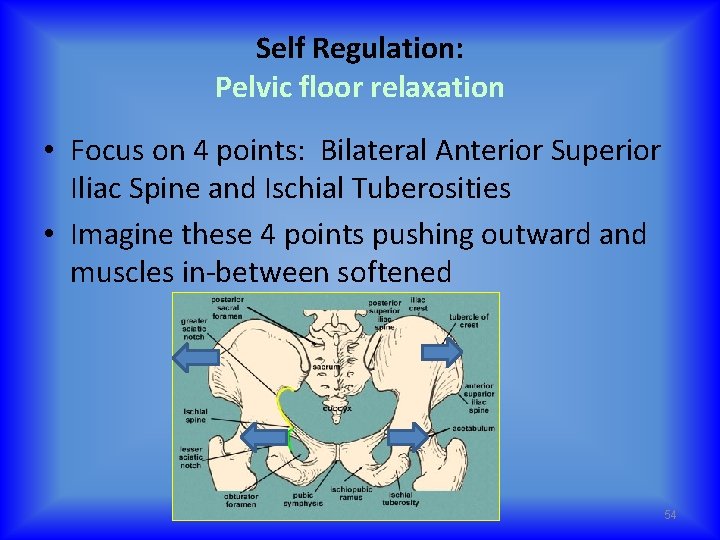
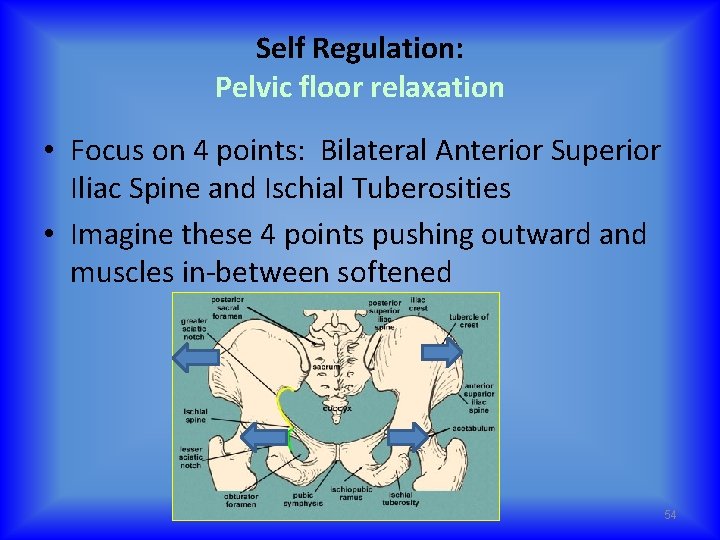
Self Regulation: Pelvic floor relaxation • Focus on 4 points: Bilateral Anterior Superior Iliac Spine and Ischial Tuberosities • Imagine these 4 points pushing outward and muscles in-between softened 54
Self-Regulation No Clenching
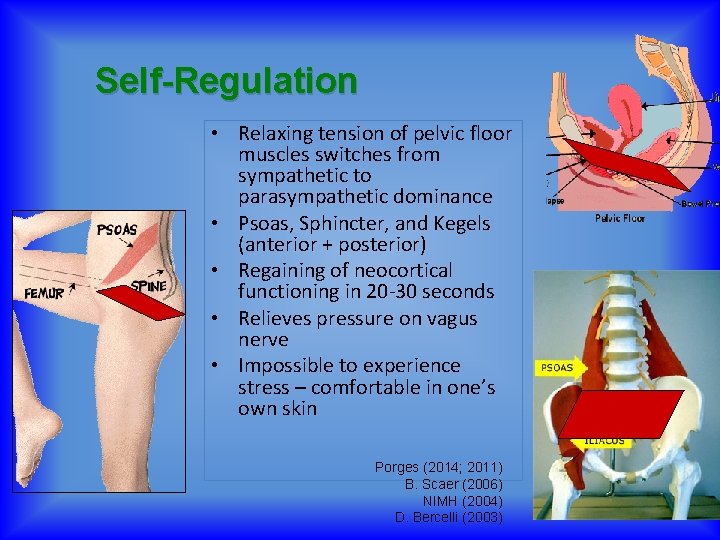
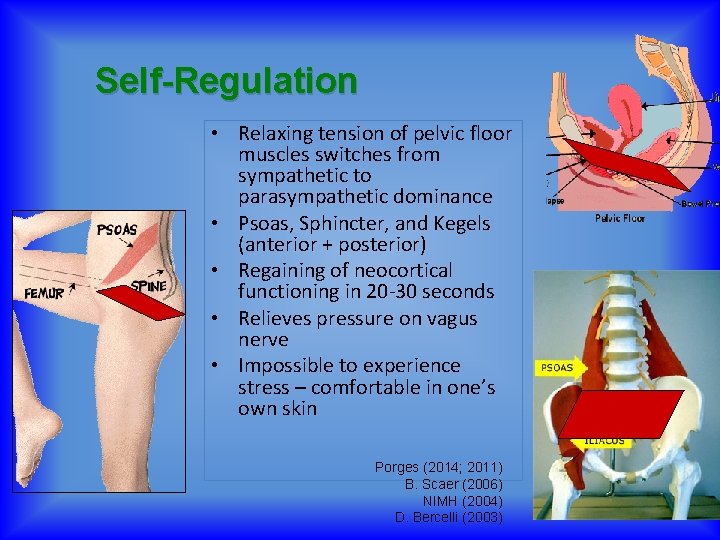
Self-Regulation • Relaxing tension of pelvic floor muscles switches from sympathetic to parasympathetic dominance • Psoas, Sphincter, and Kegels (anterior + posterior) • Regaining of neocortical functioning in 20 -30 seconds • Relieves pressure on vagus nerve • Impossible to experience stress – comfortable in one’s own skin Porges (2014; 2011) B. Scaer (2006) NIMH (2004) D. Bercelli (2003)
Who is squeezing the muscles in your body? STOP
DSM V POSTTRAUMATIC STRESS DISORDER
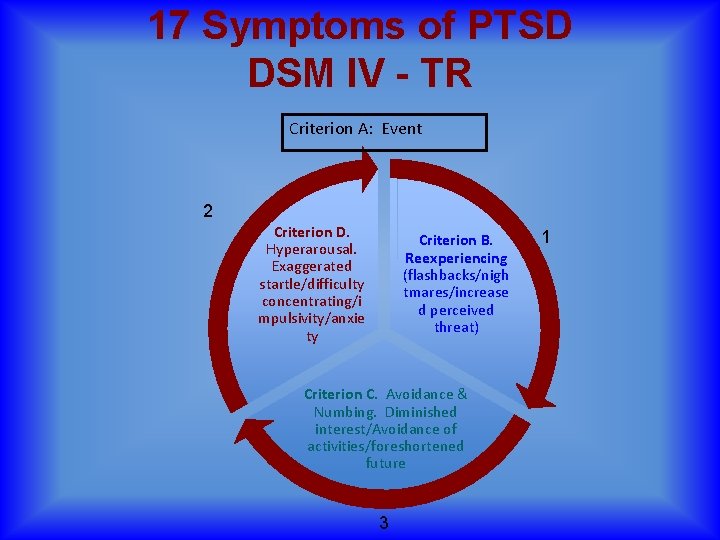
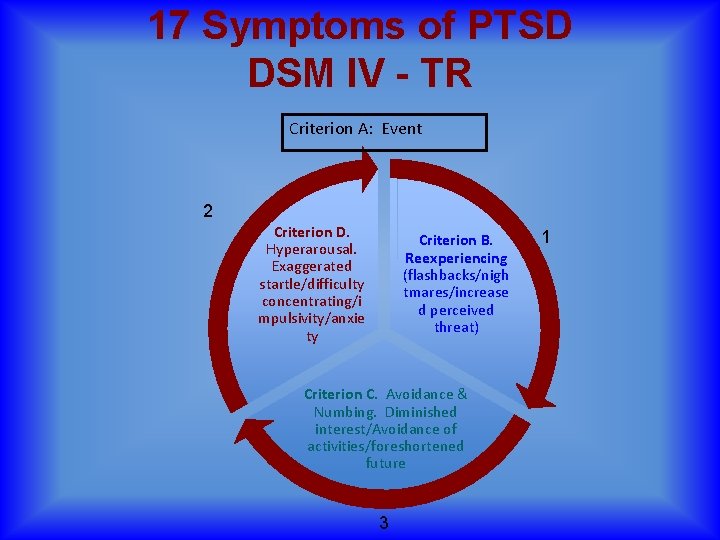
17 Symptoms of PTSD DSM IV - TR Criterion A: Event 2 Criterion D. Hyperarousal. Exaggerated startle/difficulty concentrating/i mpulsivity/anxie ty Criterion B. Reexperiencing (flashbacks/nigh tmares/increase d perceived threat) Criterion C. Avoidance & Numbing. Diminished interest/Avoidance of activities/foreshortened future 3 1
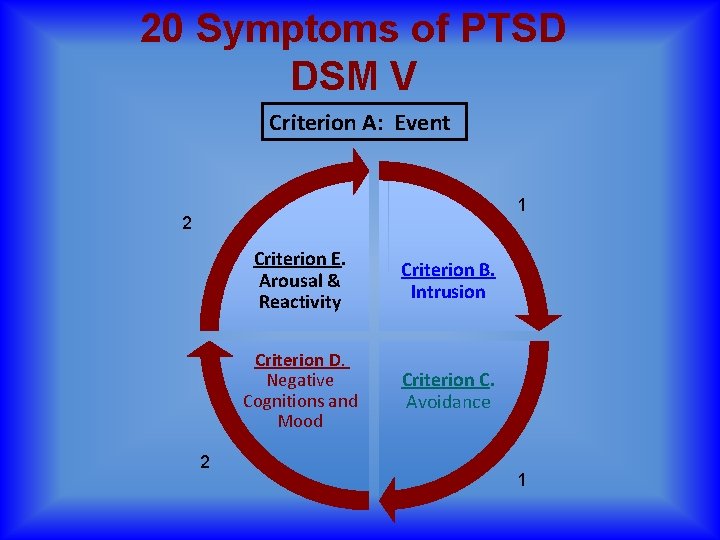
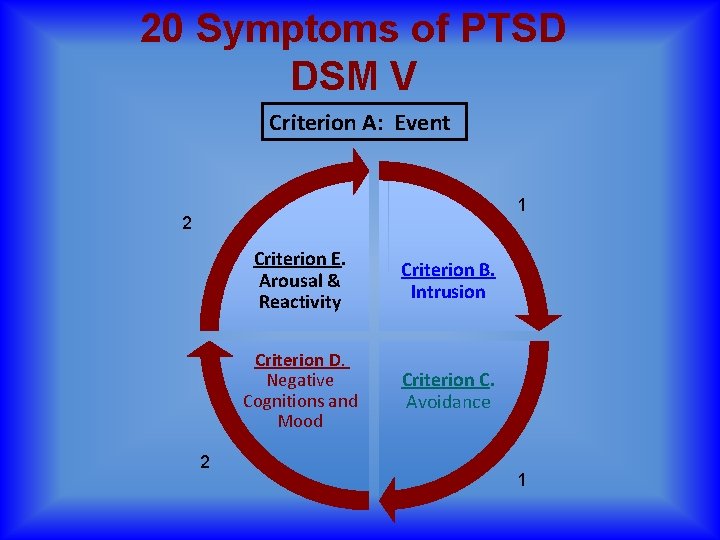
20 Symptoms of PTSD DSM V Criterion A: Event 1 2 2 Criterion E. Arousal & Reactivity Criterion B. Intrusion Criterion D. Negative Cognitions and Mood Criterion C. Avoidance 1
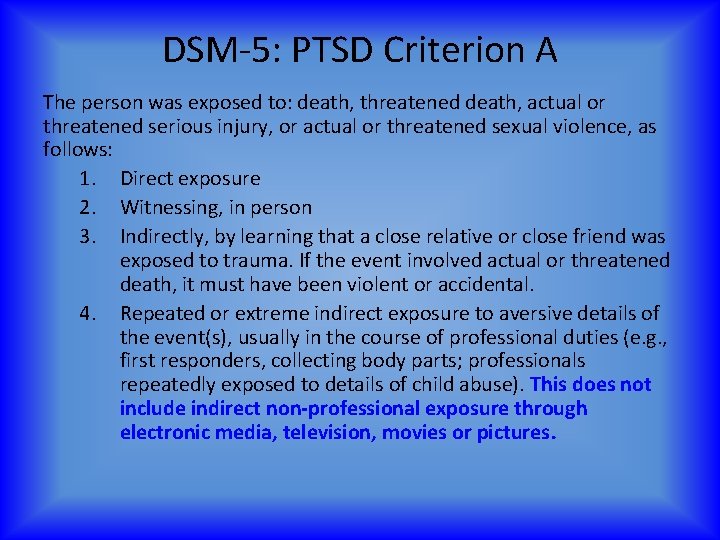
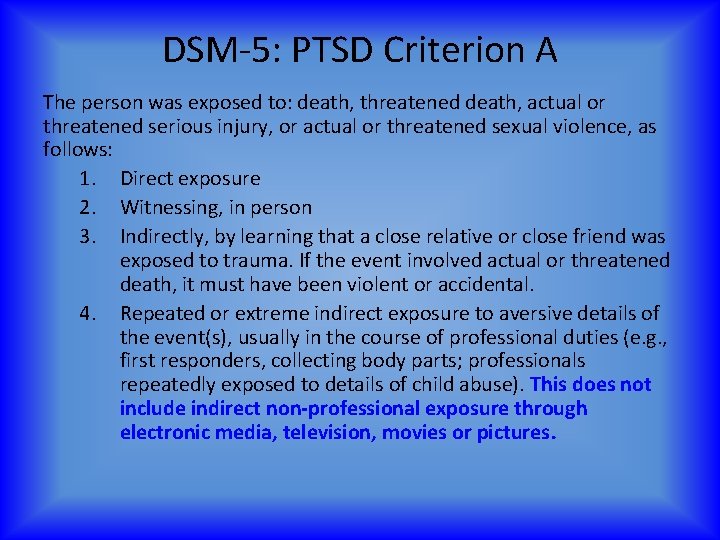
DSM-5: PTSD Criterion A The person was exposed to: death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence, as follows: 1. Direct exposure 2. Witnessing, in person 3. Indirectly, by learning that a close relative or close friend was exposed to trauma. If the event involved actual or threatened death, it must have been violent or accidental. 4. Repeated or extreme indirect exposure to aversive details of the event(s), usually in the course of professional duties (e. g. , first responders, collecting body parts; professionals repeatedly exposed to details of child abuse). This does not include indirect non-professional exposure through electronic media, television, movies or pictures.
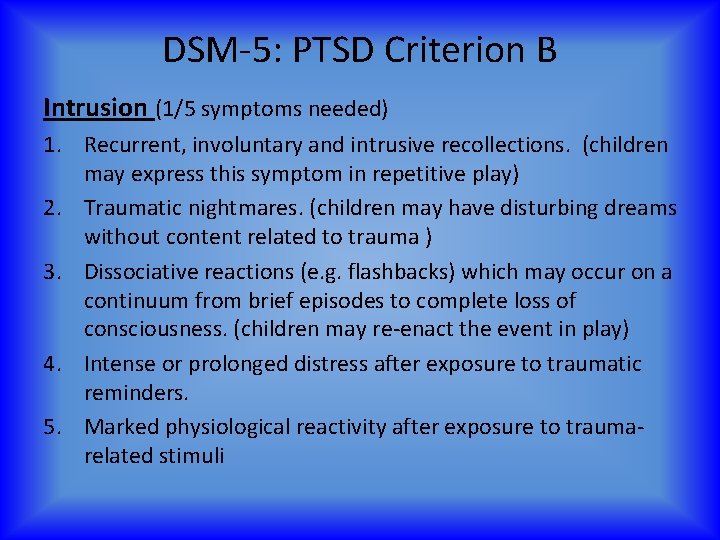
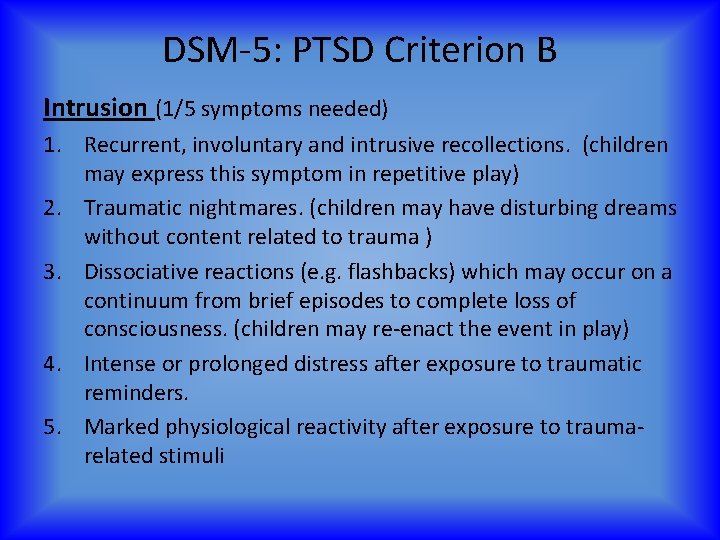
DSM-5: PTSD Criterion B Intrusion (1/5 symptoms needed) 1. Recurrent, involuntary and intrusive recollections. (children may express this symptom in repetitive play) 2. Traumatic nightmares. (children may have disturbing dreams without content related to trauma ) 3. Dissociative reactions (e. g. flashbacks) which may occur on a continuum from brief episodes to complete loss of consciousness. (children may re-enact the event in play) 4. Intense or prolonged distress after exposure to traumatic reminders. 5. Marked physiological reactivity after exposure to traumarelated stimuli
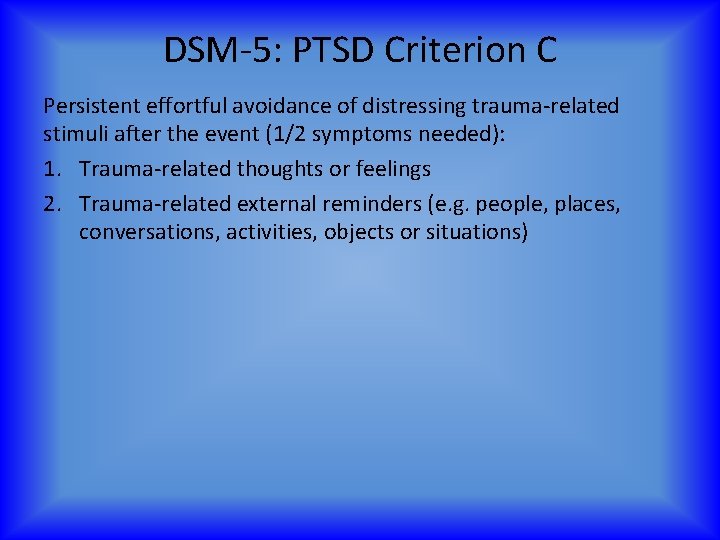
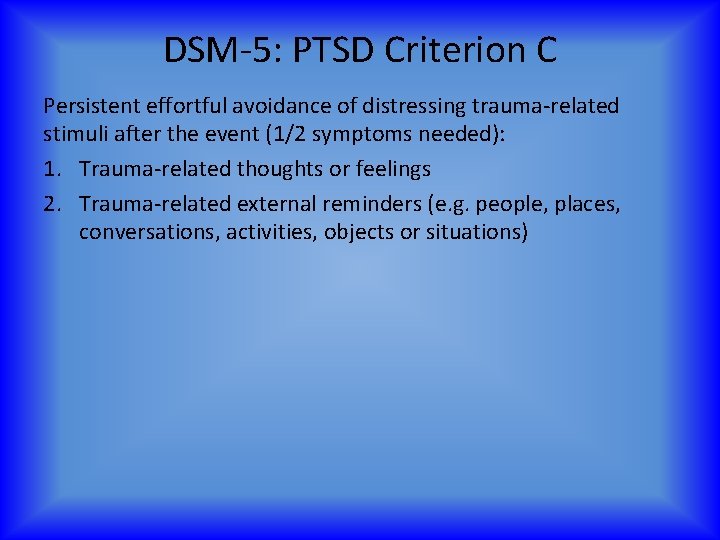
DSM-5: PTSD Criterion C Persistent effortful avoidance of distressing trauma-related stimuli after the event (1/2 symptoms needed): 1. Trauma-related thoughts or feelings 2. Trauma-related external reminders (e. g. people, places, conversations, activities, objects or situations)

DSM-5: PTSD Criterion D Negative alterations in cognitions and mood that began or worsened after the traumatic event (2/7 symptoms needed) 1. Inability to recall key features of the traumatic event (usually dissociative amnesia; not due to head injury, alcohol or drugs) (C 3 in DSM-IV) 2. Persistent (& often distorted) negative beliefs and expectations about oneself or the world (e. g. “I am bad, ” “the world is completely dangerous”) (C 7 in DSM-IV) 3. Persistent distorted blame of self or others for causing the traumatic event or for resulting consequences (new) 4. Persistent negative trauma-related emotions (e. g. fear, horror, anger, guilt, or shame) (new)
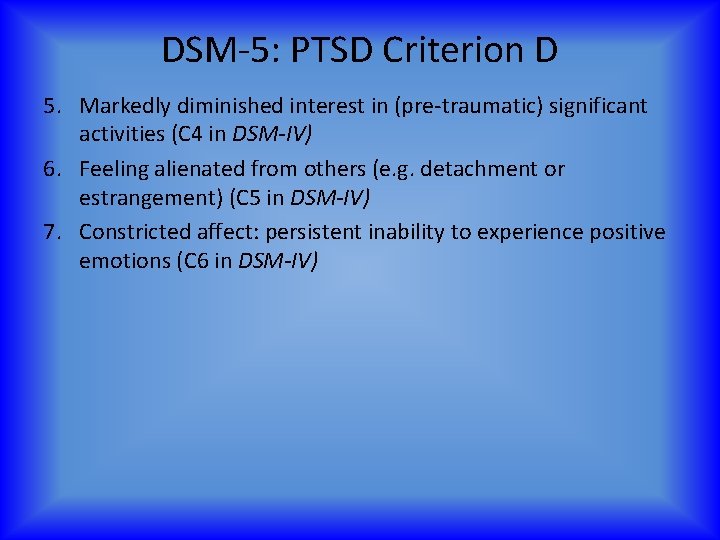
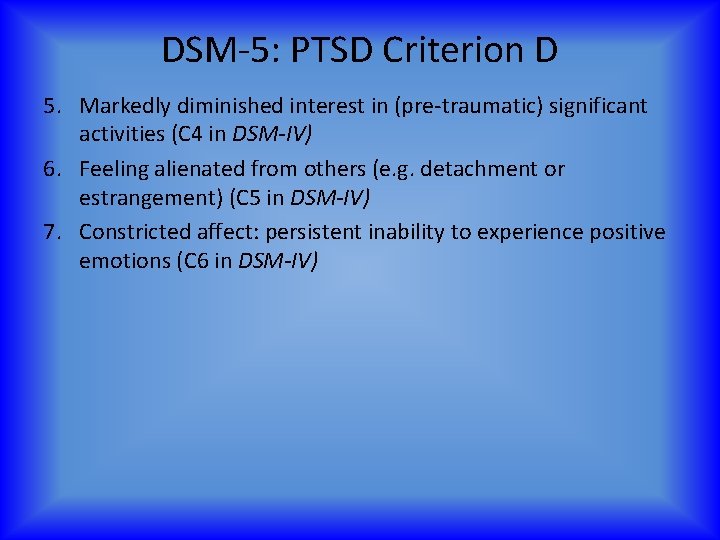
DSM-5: PTSD Criterion D 5. Markedly diminished interest in (pre-traumatic) significant activities (C 4 in DSM-IV) 6. Feeling alienated from others (e. g. detachment or estrangement) (C 5 in DSM-IV) 7. Constricted affect: persistent inability to experience positive emotions (C 6 in DSM-IV)
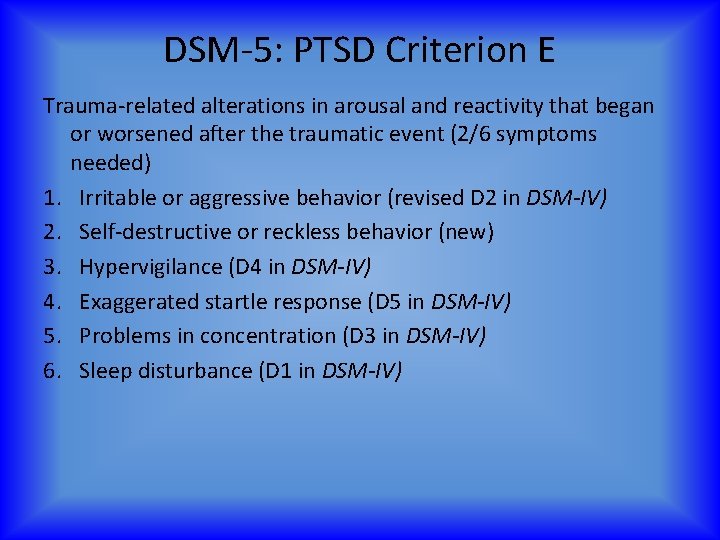
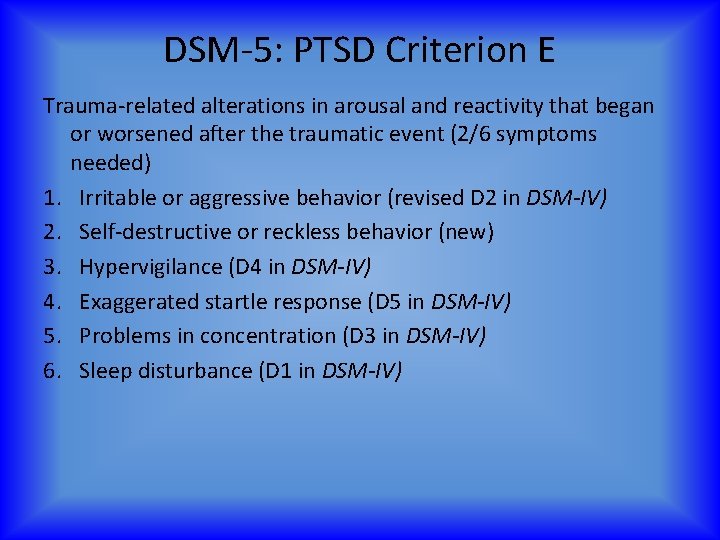
DSM-5: PTSD Criterion E Trauma-related alterations in arousal and reactivity that began or worsened after the traumatic event (2/6 symptoms needed) 1. Irritable or aggressive behavior (revised D 2 in DSM-IV) 2. Self-destructive or reckless behavior (new) 3. Hypervigilance (D 4 in DSM-IV) 4. Exaggerated startle response (D 5 in DSM-IV) 5. Problems in concentration (D 3 in DSM-IV) 6. Sleep disturbance (D 1 in DSM-IV)
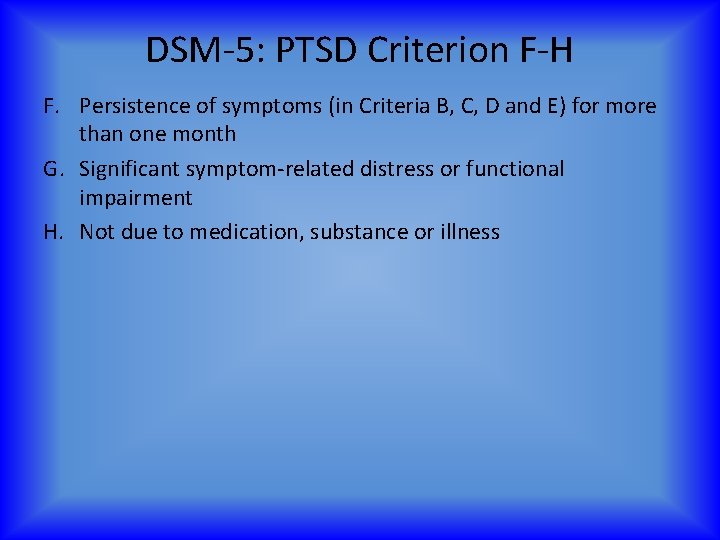
DSM-5: PTSD Criterion F-H F. Persistence of symptoms (in Criteria B, C, D and E) for more than one month G. Significant symptom-related distress or functional impairment H. Not due to medication, substance or illness
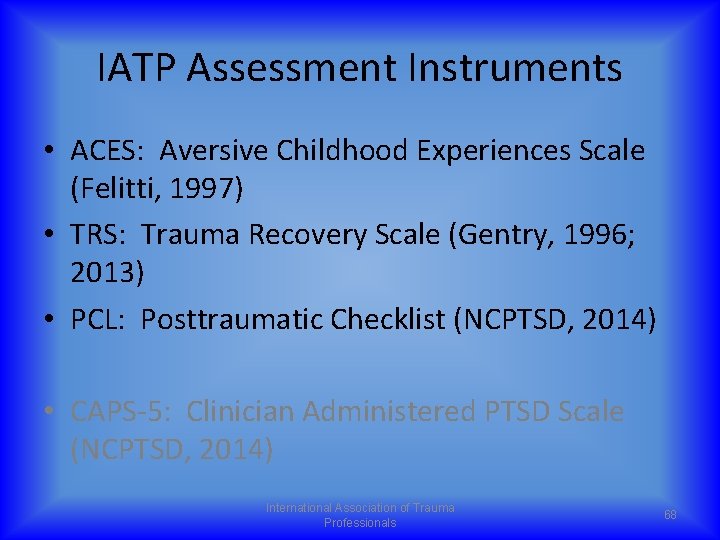
IATP Assessment Instruments • ACES: Aversive Childhood Experiences Scale (Felitti, 1997) • TRS: Trauma Recovery Scale (Gentry, 1996; 2013) • PCL: Posttraumatic Checklist (NCPTSD, 2014) • CAPS-5: Clinician Administered PTSD Scale (NCPTSD, 2014) International Association of Trauma Professionals 68
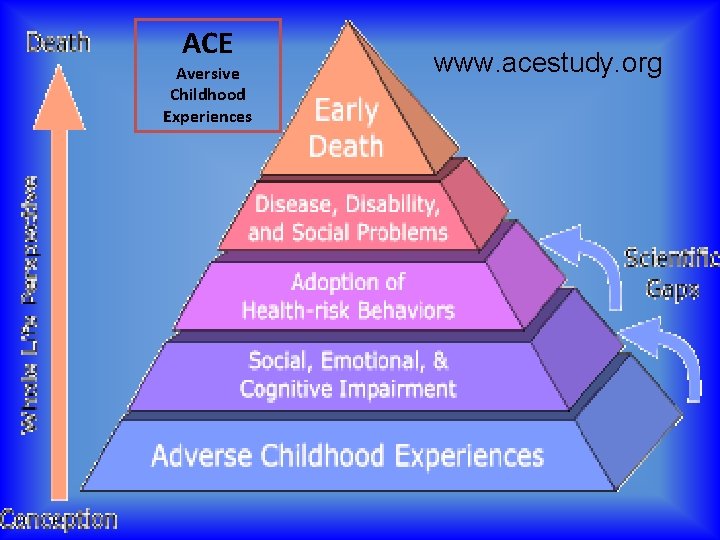
The Adverse Childhood Experiences Study (ACE) Collaboration between Kaiser Permanente’s Department of Preventive Medicine in San Diego and the Center for Disease Control and Prevention (CDC) 69
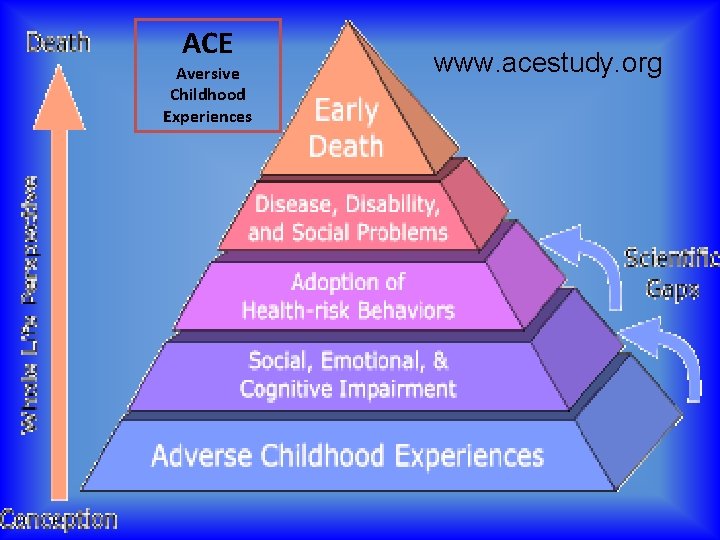
ACE Aversive Childhood Experiences www. acestudy. org

Why is This Important? Because ACEs are: • Surprisingly common • Occur in clusters • The basis for many common public health problems • Strong predictors of later social functioning, well-being, health risks, disease, and death

Top 10 risk factors for death in the USA ü smoking, ü severe obesity, ü physical inactivity, ü depression, ü suicide attempt, ü alcoholism, ü illicit drug use, ü injected drug use, ü 50+ sexual partners, ü history of STD

ACE Study Findings Of the 17, 000+ respondents… – More than 25% grew up in a household with an alcoholic or drug user – 25% had been beaten as children – Two-thirds had 1 adverse childhood event – 1 in 6 people had four or more ACES Source: Adverse Childhood Experiences (ACE) Study. Information available at http: //www. cdc. gov/ace/index. htm International Association of Trauma Professionals 73
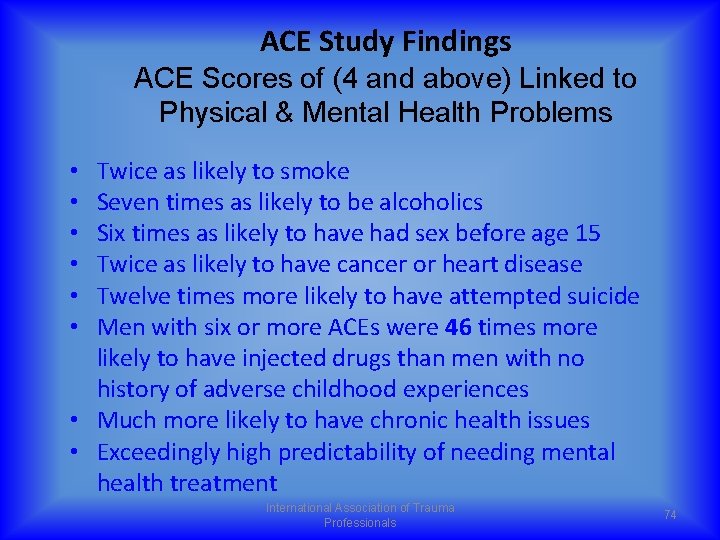
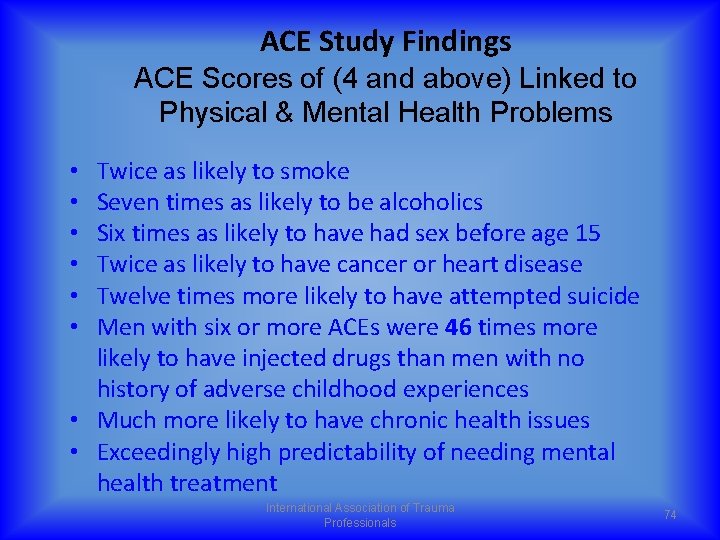
ACE Study Findings ACE Scores of (4 and above) Linked to Physical & Mental Health Problems Twice as likely to smoke Seven times as likely to be alcoholics Six times as likely to have had sex before age 15 Twice as likely to have cancer or heart disease Twelve times more likely to have attempted suicide Men with six or more ACEs were 46 times more likely to have injected drugs than men with no history of adverse childhood experiences • Much more likely to have chronic health issues • Exceedingly high predictability of needing mental health treatment • • • International Association of Trauma Professionals 74

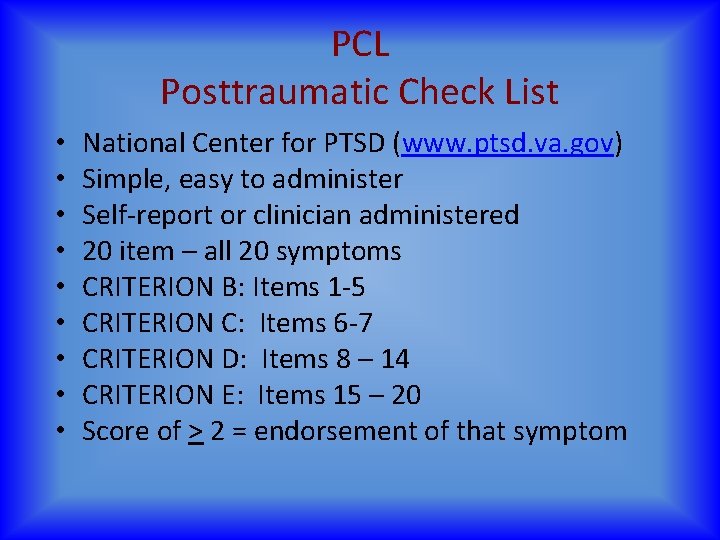
PCL Posttraumatic Check List • • • National Center for PTSD (www. ptsd. va. gov) Simple, easy to administer Self-report or clinician administered 20 item – all 20 symptoms CRITERION B: Items 1 -5 CRITERION C: Items 6 -7 CRITERION D: Items 8 – 14 CRITERION E: Items 15 – 20 Score of > 2 = endorsement of that symptom
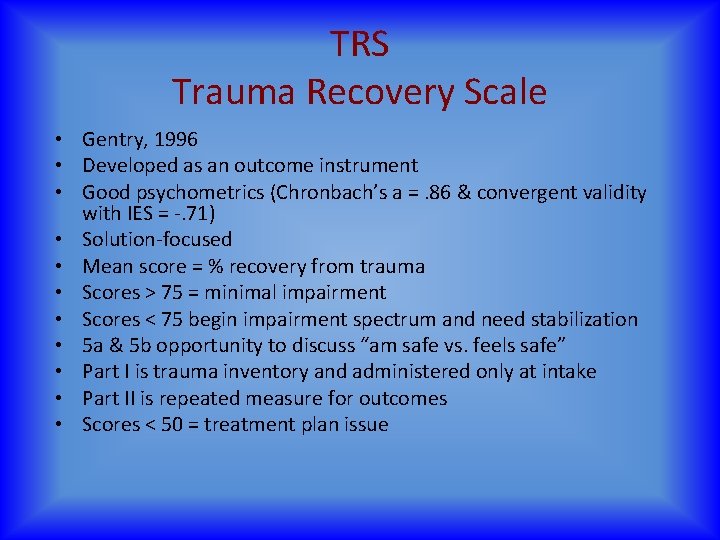
TRS Trauma Recovery Scale • Gentry, 1996 • Developed as an outcome instrument • Good psychometrics (Chronbach’s a =. 86 & convergent validity with IES = -. 71) • Solution-focused • Mean score = % recovery from trauma • Scores > 75 = minimal impairment • Scores < 75 begin impairment spectrum and need stabilization • 5 a & 5 b opportunity to discuss “am safe vs. feels safe” • Part I is trauma inventory and administered only at intake • Part II is repeated measure for outcomes • Scores < 50 = treatment plan issue

CAPS Clinician Administered PTSD Scale • • • National Center for PTSD (www. ptsd. va. gov) 20 item structured clinical interview Primarily for diagnosis Good psychometrics and inter-rater relaibilty “Gold Standard” for diagnosing PTSD (if diagnosis will be questioned or challanged) Clinician administered and clinician scored (not selfreport) Each symptom has a qualitative section used to derive quantitative evaluation of symptom Intensity x Frequency/2 = Severity score of > 2 = endorsement of that symptom
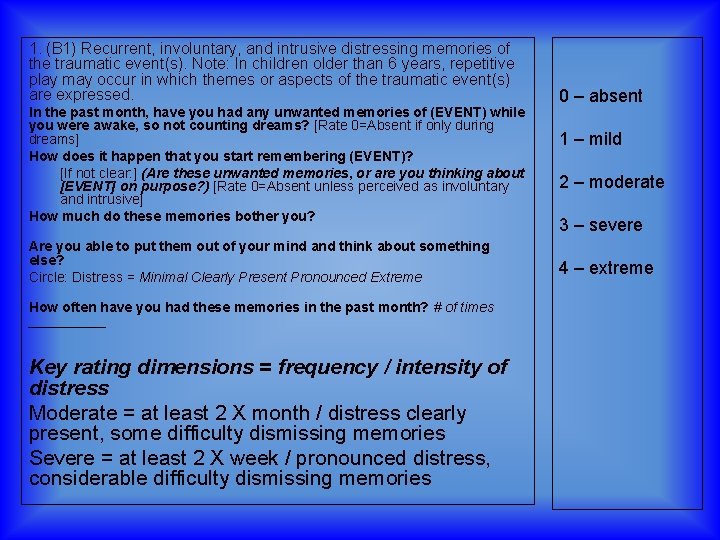
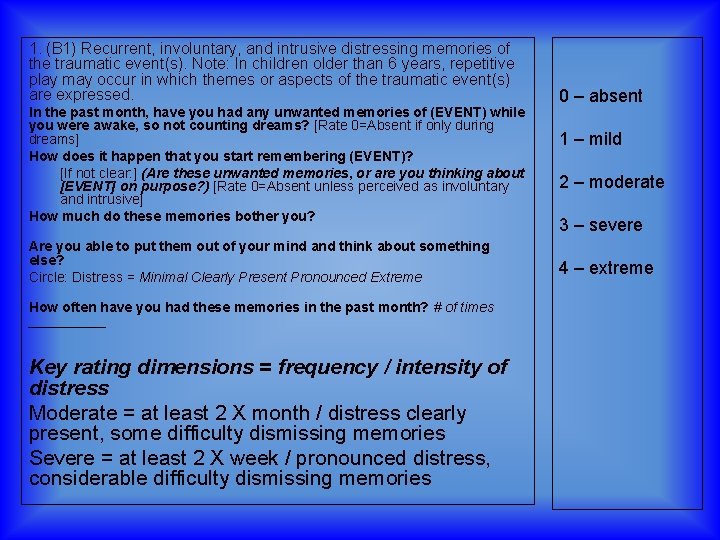
1. (B 1) Recurrent, involuntary, and intrusive distressing memories of the traumatic event(s). Note: In children older than 6 years, repetitive play may occur in which themes or aspects of the traumatic event(s) are expressed. In the past month, have you had any unwanted memories of (EVENT) while you were awake, so not counting dreams? [Rate 0=Absent if only during dreams] How does it happen that you start remembering (EVENT)? [If not clear: ] (Are these unwanted memories, or are you thinking about [EVENT] on purpose? ) [Rate 0=Absent unless perceived as involuntary and intrusive] How much do these memories bother you? Are you able to put them out of your mind and think about something else? Circle: Distress = Minimal Clearly Present Pronounced Extreme How often have you had these memories in the past month? # of times _____ Key rating dimensions = frequency / intensity of distress Moderate = at least 2 X month / distress clearly present, some difficulty dismissing memories Severe = at least 2 X week / pronounced distress, considerable difficulty dismissing memories 0 – absent 1 – mild 2 – moderate 3 – severe 4 – extreme

HOMEWORK 1. Notice the frequency in which you encounter perceived threats over the next 16 hours 2. Get and keep the muscles in your body relaxed all they way through your encounter with at least one perceived threat 3. Be prepared to discuss in the morning the difference between the time(s) you were able to selfregulate vs. the times you did not International Association of Trauma Professionals 80
 Certified clinical trauma professional
Certified clinical trauma professional Iatp 5 narrative model
Iatp 5 narrative model Personal response
Personal response Chapter 4 lesson 3 coping with loss and grief
Chapter 4 lesson 3 coping with loss and grief Chapter 36 loss and grief
Chapter 36 loss and grief Seven stages of grief
Seven stages of grief Normal loss treatment in process costing
Normal loss treatment in process costing Web accessibility specialist certification
Web accessibility specialist certification Certified business process professional
Certified business process professional What is citp certification
What is citp certification Incose asep exam
Incose asep exam Certified analytics professional cap
Certified analytics professional cap Certified professional public buyer
Certified professional public buyer Certified professional for lotus software
Certified professional for lotus software Ibf certification exam
Ibf certification exam Certified fisheries professional
Certified fisheries professional Abpmp certification
Abpmp certification Vo2r formula
Vo2r formula Physical security professional (psp)
Physical security professional (psp) Certified professional marketer
Certified professional marketer Cpp
Cpp Corning total rewards
Corning total rewards Certified training professional
Certified training professional What is incose
What is incose Microsoft certified trainer
Microsoft certified trainer Afp fp&a certification
Afp fp&a certification Nasbite cgbp
Nasbite cgbp What is cmrp certification
What is cmrp certification Csep exam questions
Csep exam questions Certified analytics professional cap
Certified analytics professional cap Certified software development professional
Certified software development professional Ptsd
Ptsd Causes of ptsd
Causes of ptsd Dual representation theory
Dual representation theory Circumcision ptsd
Circumcision ptsd Ptsd violent behavior
Ptsd violent behavior Psykoedukation ptsd
Psykoedukation ptsd Ptsd stages
Ptsd stages Ptsd spiritual warfare
Ptsd spiritual warfare Psychosis and ptsd
Psychosis and ptsd Toleransfönstret
Toleransfönstret Jamal and deborah therapy
Jamal and deborah therapy Va ptsd rating scale pdf
Va ptsd rating scale pdf Ptsd model ehlers and clark
Ptsd model ehlers and clark Cognitive processing therapy worksheets
Cognitive processing therapy worksheets Ptsd symptomer
Ptsd symptomer Evolution of ptsd
Evolution of ptsd Cptsd
Cptsd Ptsd seizures
Ptsd seizures Toleransevinduet
Toleransevinduet Simon armitage remains
Simon armitage remains Macbeth ptsd quotes
Macbeth ptsd quotes Anxiety goals nursing
Anxiety goals nursing Absent grief
Absent grief Emily dickinson grief
Emily dickinson grief Engels model of grief
Engels model of grief Ice breakers for grief support groups
Ice breakers for grief support groups Grief support
Grief support Tonkin model of grief
Tonkin model of grief Nothing gold can stay metaphor
Nothing gold can stay metaphor Adult attitude
Adult attitude Psalm 116 11
Psalm 116 11 Assura inc
Assura inc Grief wheel
Grief wheel Children grief
Children grief Disenfranchised grief losses
Disenfranchised grief losses Grief
Grief Types of grief
Types of grief Ambiguous loss
Ambiguous loss Ambiguous grief definition
Ambiguous grief definition Engels model of grief
Engels model of grief Do you think rowdy and junior will remain friends
Do you think rowdy and junior will remain friends Grief
Grief Grief is like an earthquake
Grief is like an earthquake A grief observed summary
A grief observed summary The three learned emotions are grief shame and
The three learned emotions are grief shame and Certified healthcare facility manager
Certified healthcare facility manager Microsoft certified reseller
Microsoft certified reseller Nc state bar certified paralegal
Nc state bar certified paralegal Testogenix reviews
Testogenix reviews Pbn certified
Pbn certified