General principle of Psychopharmacology Alcohol 19 C paraldehyde






















































- Slides: 166
정신약물학 - General principle of Psychopharmacology- 권석준 신세계병원 신경정신과 과장
향정신성 약물 : 발달사 § § § § Alcohol, 아편, 코카인, 마리화나 19 C 중반 : paraldehyde, chloral hydrate 20 C 초 : barbiturate 1940년대 말 : lithium 1950년대 : chlorpromazine, haloperidol, Tricyclics 1960년대 : benzodiazepine 1980년대 : clozapine, SSRIs 1990년대 : risperidone, olanzapine

기존 약물 적응증 확대와 새로운 약물의 발견 및 개발. è“약물학적 분류”: 약리학적 작용 기전. l Beta-adrenergic receptor antagonist l BZD agonist: Benzodiazepine l Dopamine receptor antagonist l Monoamine oxidase inhibitor (MAOI) l Selective serotonin reuptake inhibitor (SSRI) l Tricyclic antidepressant (TCA) l Serotonin/dopamine antagonist (SDA)
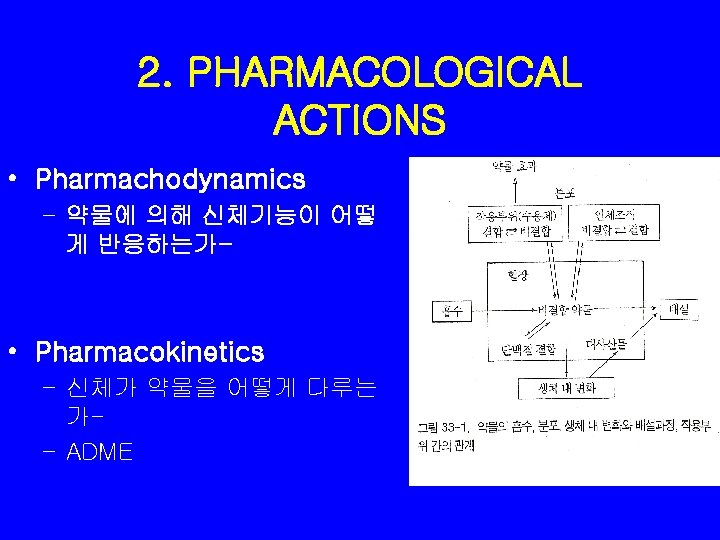
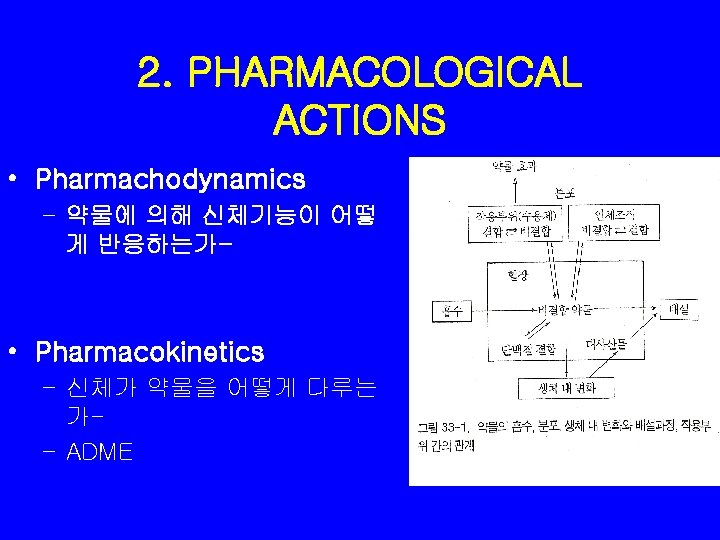
2. PHARMACOLOGICAL ACTIONS • Pharmachodynamics – 약물에 의해 신체기능이 어떻 게 반응하는가- • Pharmacokinetics – 신체가 약물을 어떻게 다루는 가– ADME
약력학 Pharmachodynamics • • Receptor mechanism Dose-response curve Therapeutic index Development of Tolerance, Dependence, Withdrawal
약동학 Pharmacokinetics • Absorption • Distribution and Bioavailability • Metabolism and Excretion 1. time of peak plasma concentration 2. drug's half-life 3. first pass effect 4. clearance
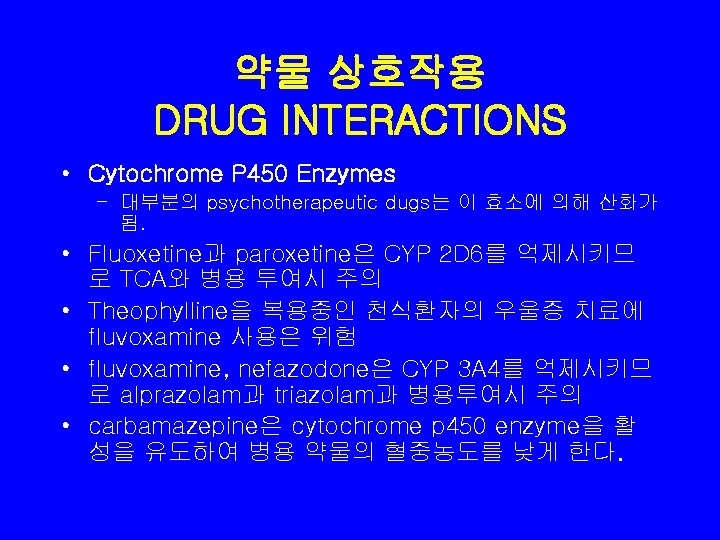
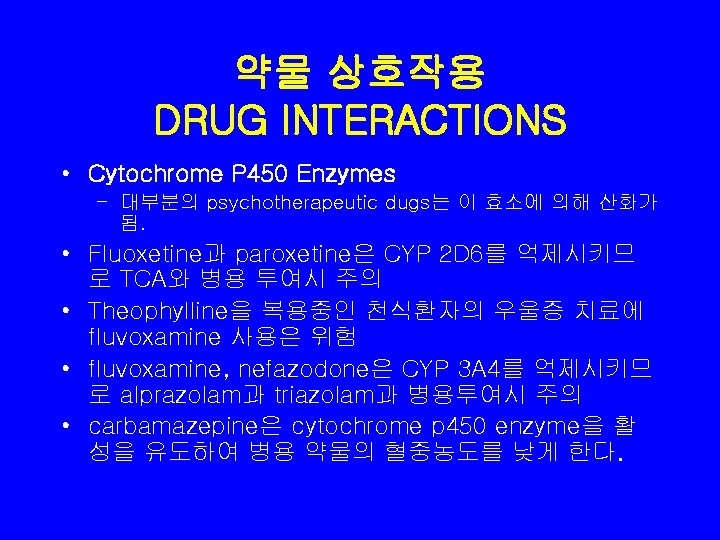
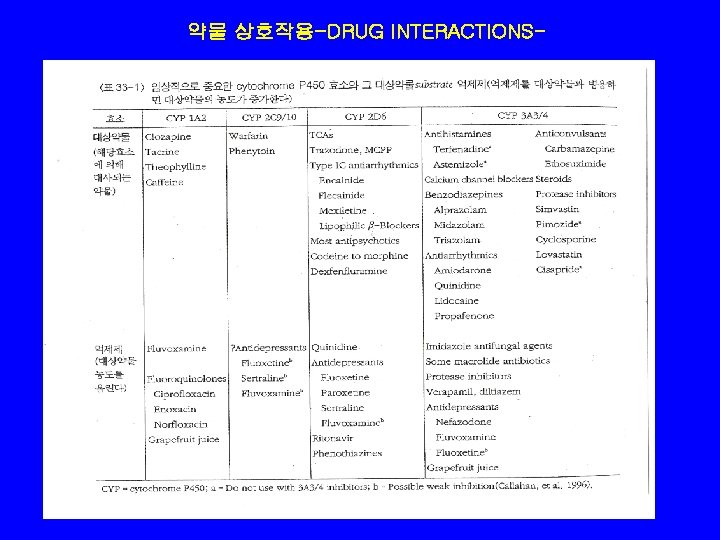
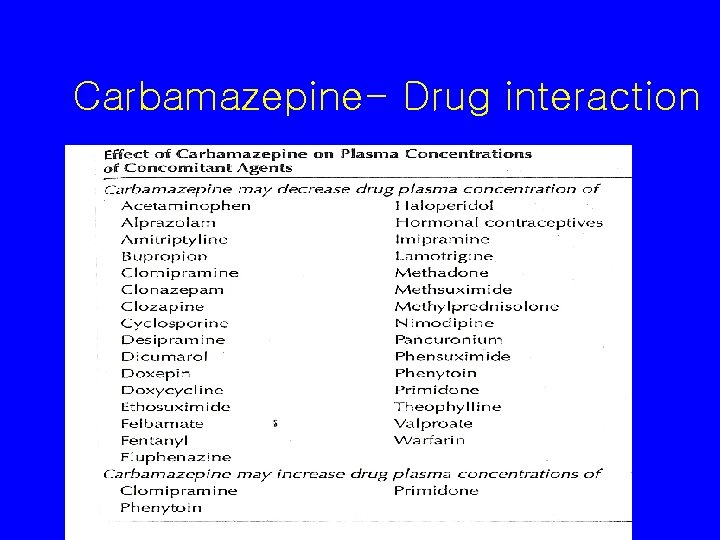
약물 상호작용 DRUG INTERACTIONS • Cytochrome P 450 Enzymes – 대부분의 psychotherapeutic dugs는 이 효소에 의해 산화가 됨. • Fluoxetine과 paroxetine은 CYP 2 D 6를 억제시키므 로 TCA와 병용 투여시 주의 • Theophylline을 복용중인 천식환자의 우울증 치료에 fluvoxamine 사용은 위험 • fluvoxamine, nefazodone은 CYP 3 A 4를 억제시키므 로 alprazolam과 triazolam과 병용투여시 주의 • carbamazepine은 cytochrome p 450 enzyme을 활 성을 유도하여 병용 약물의 혈중농도를 낮게 한다.
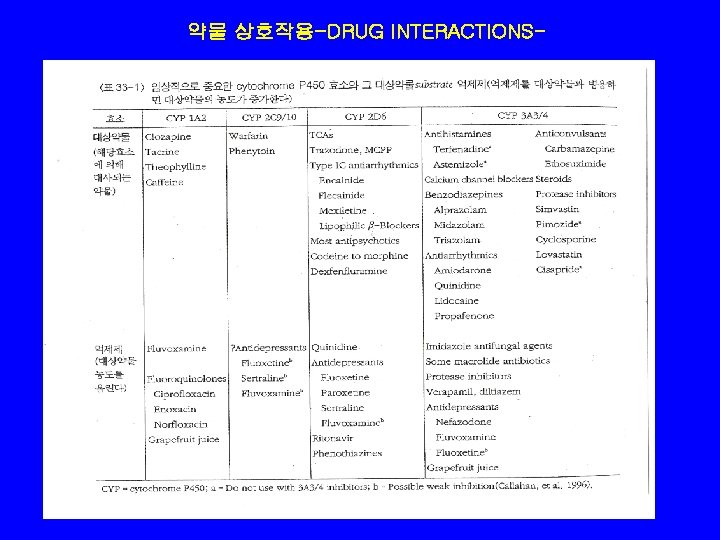
약물 상호작용-DRUG INTERACTIONS-


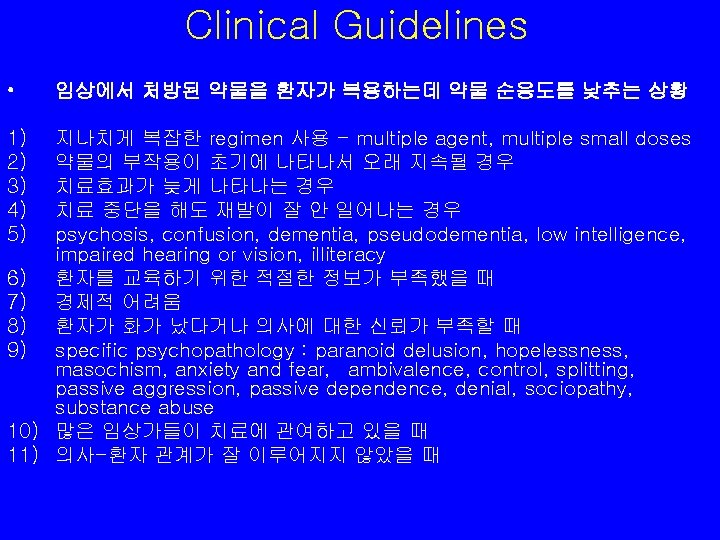
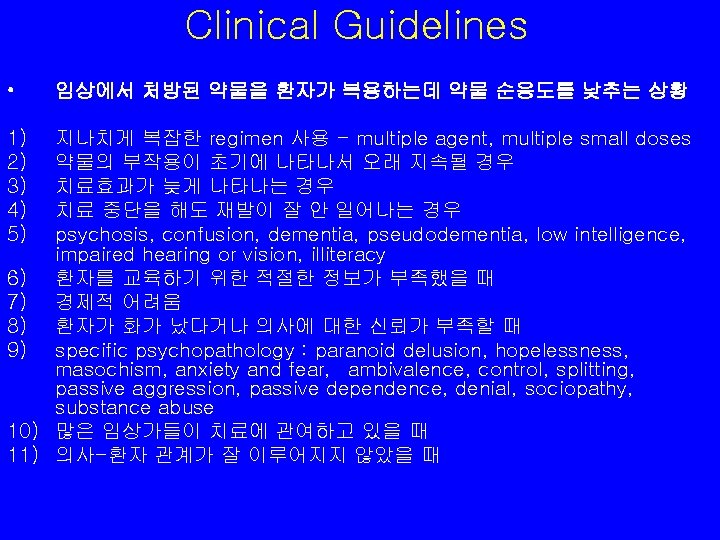
Clinical Guidelines • 1) 2) 3) 4) 5) 임상에서 처방된 약물을 환자가 복용하는데 약물 순응도를 낮추는 상황 지나치게 복잡한 regimen 사용 - multiple agent, multiple small doses 약물의 부작용이 초기에 나타나서 오래 지속될 경우 치료효과가 늦게 나타나는 경우 치료 중단을 해도 재발이 잘 안 일어나는 경우 psychosis, confusion, dementia, pseudodementia, low intelligence, impaired hearing or vision, illiteracy 6) 환자를 교육하기 위한 적절한 정보가 부족했을 때 7) 경제적 어려움 8) 환자가 화가 났다거나 의사에 대한 신뢰가 부족할 때 9) specific psychopathology : paranoid delusion, hopelessness, masochism, anxiety and fear, ambivalence, control, splitting, passive aggression, passive dependence, denial, sociopathy, substance abuse 10) 많은 임상가들이 치료에 관여하고 있을 때 11) 의사-환자 관계가 잘 이루어지지 않았을 때








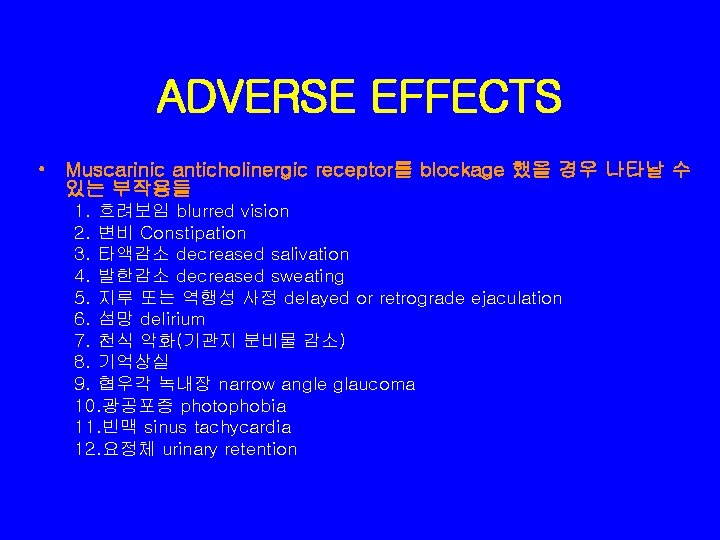
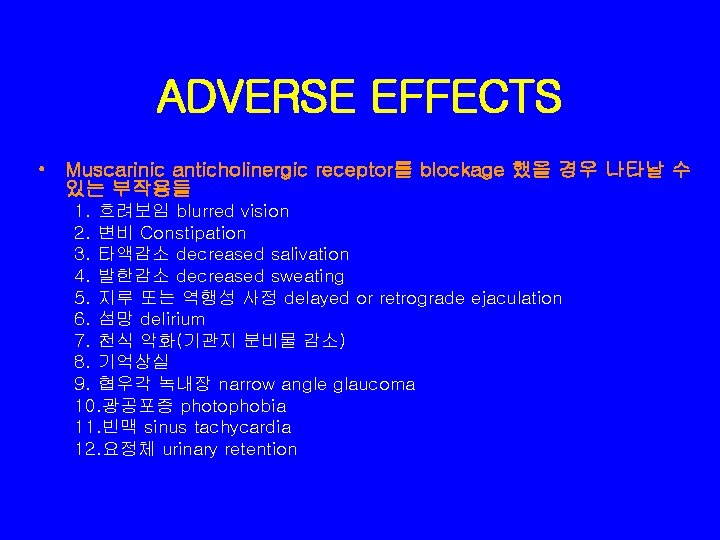
ADVERSE EFFECTS • Muscarinic anticholinergic receptor를 blockage 했을 경우 나타날 수 있는 부작용들 1. 흐려보임 blurred vision 2. 변비 Constipation 3. 타액감소 decreased salivation 4. 발한감소 decreased sweating 5. 지루 또는 역행성 사정 delayed or retrograde ejaculation 6. 섬망 delirium 7. 천식 악화(기관지 분비물 감소) 8. 기억상실 9. 협우각 녹내장 narrow angle glaucoma 10. 광공포증 photophobia 11. 빈맥 sinus tachycardia 12. 요정체 urinary retention
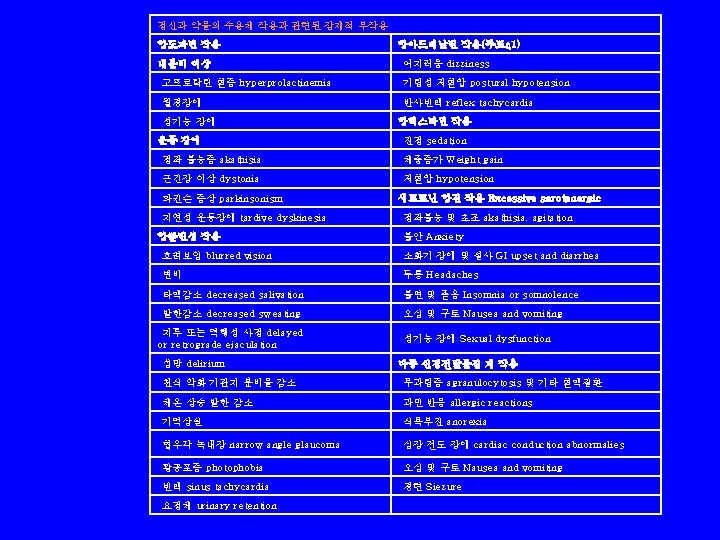
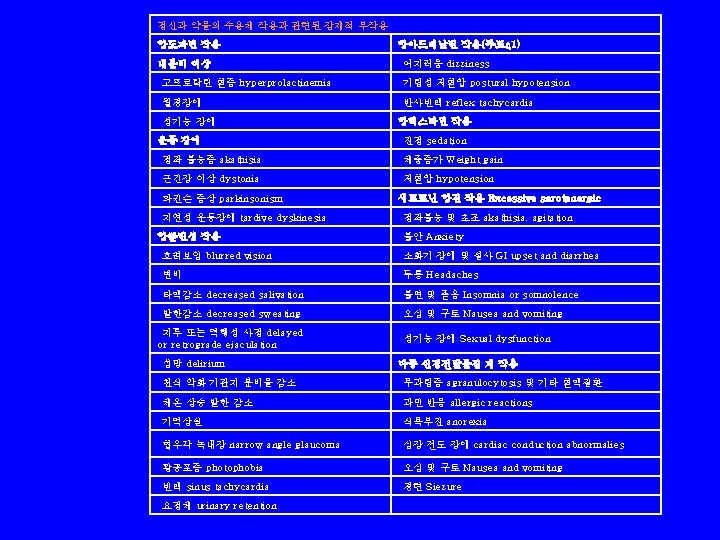
정신과 약물의 수용체 작용과 관련된 잠재적 부작용 항도파민 작용 항아드레날린 작용(주로α 1) 내분비 이상 어지러움 dizziness 고프로락틴 혈증 hyperprolactinemia 기립성 저혈압 postural hypotension 월경장애 반사빈맥 reflex tachycardia 성기능 장애 항히스타민 작용 운동 장애 진정 sedation 정좌 불능증 akathisia 체중증가 Weight gain 근긴장 이상 dystonia 저혈압 hypotension 파킨슨 증상 parkinsonism 세로토닌 항진 작용 Excessive serotonergic 지연성 운동장애 tardive dyskinesia 정좌불능 및 초조 akathisia, agitation 항콜린성 작용 불안 Anxiety 흐려보임 blurred vision 소화기 장애 및 설사 GI upset and diarrhea 변비 두통 Headaches 타액감소 decreased salivation 불면 및 졸음 Insomnia or somnolence 발한감소 decreased sweating 오심 및 구토 Nausea and vomiting 지루 또는 역행성 사정 delayed or retrograde ejaculation 성기능 장애 Sexual dysfunction 섬망 delirium 다중 신경전달물질 계 작용 천식 악화 기관지 분비물 감소 무과립증 agranulocytosis 및 기타 혈액질환 체온 상승 발한 감소 과민 반응 allergic reactions 기억상실 식욕부진 anorexia 협우각 녹내장 narrow angle glaucoma 심장 전도 장애 cardiac conduction abnormalies 광공포증 photophobia 오심 및 구토 Nausea and vomiting 빈맥 sinus tachycardia 경련 Siezure 요정체 urinary retention
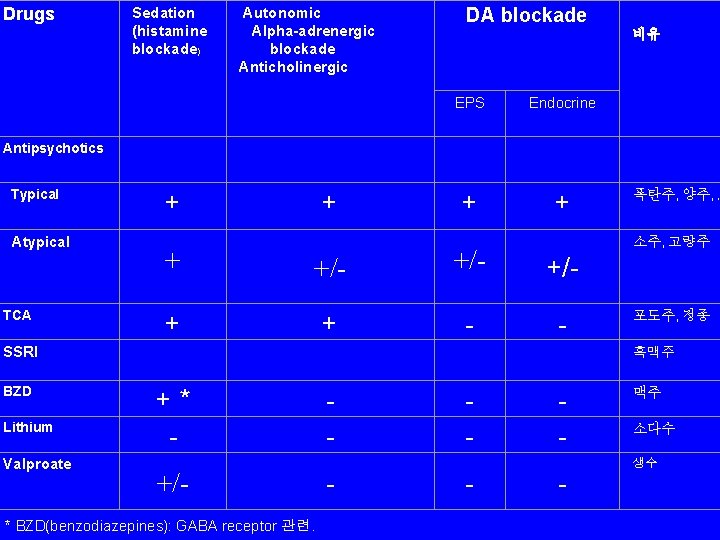
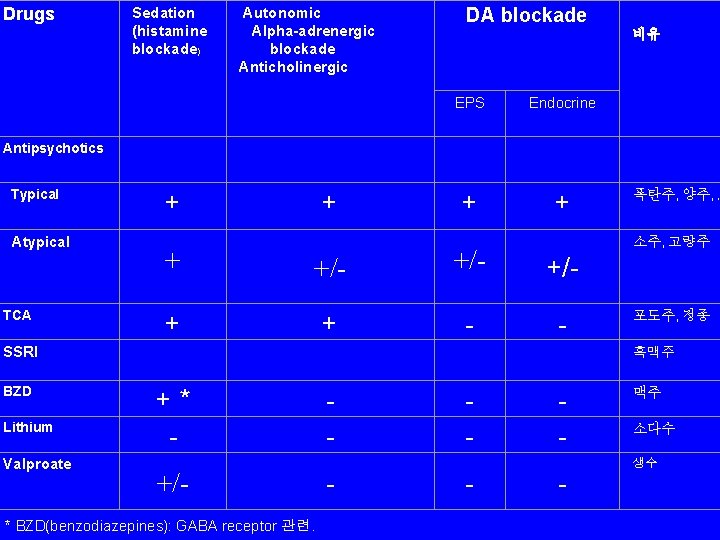
Drugs Antipsychotics Typical Atypical TCA SSRI BZD Lithium Valproate Sedation (histamine blockade) Autonomic Alpha-adrenergic blockade Anticholinergic DA blockade 비유 EPS Endocrine + + 폭탄주, 양주, , 소주, 고량주 + +/- +/- + + - - 포도주, 정종 흑맥주 +* - - 맥주 +/- - 생수 * BZD(benzodiazepines): GABA receptor 관련. 소다수
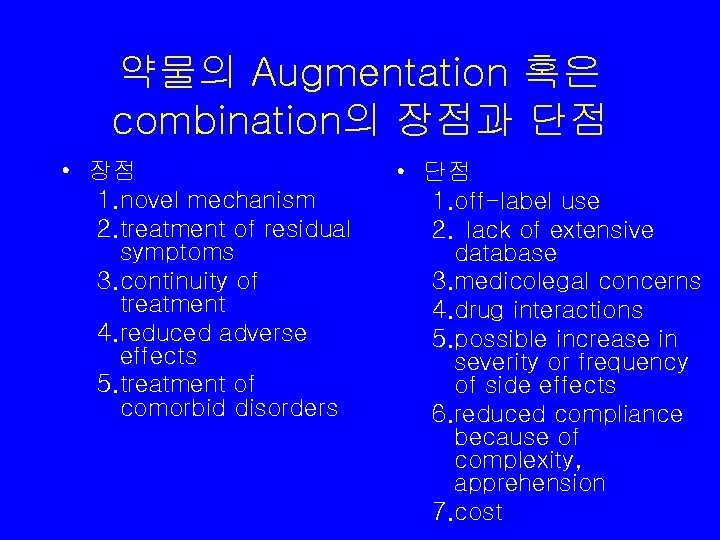
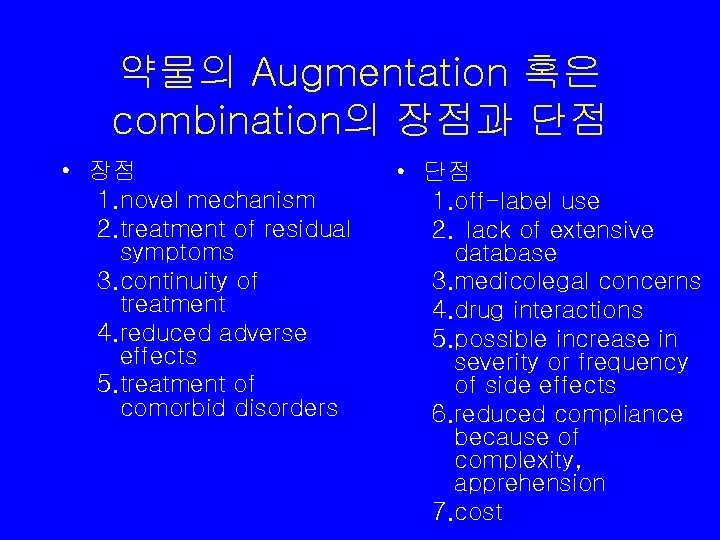
약물의 Augmentation 혹은 combination의 장점과 단점 • 장점 1. novel mechanism 2. treatment of residual symptoms 3. continuity of treatment 4. reduced adverse effects 5. treatment of comorbid disorders • 단점 1. off-label use 2. lack of extensive database 3. medicolegal concerns 4. drug interactions 5. possible increase in severity or frequency of side effects 6. reduced compliance because of complexity, apprehension 7. cost
Proper Treatment with Any Medication ( The “Four D’s) • • Diagnosis Drug Dose Duration


Terminology • Antipsychotics 항정신병 약물 • Major Tranquilizer – Cf. minor tranquilizer • Neuroleptics
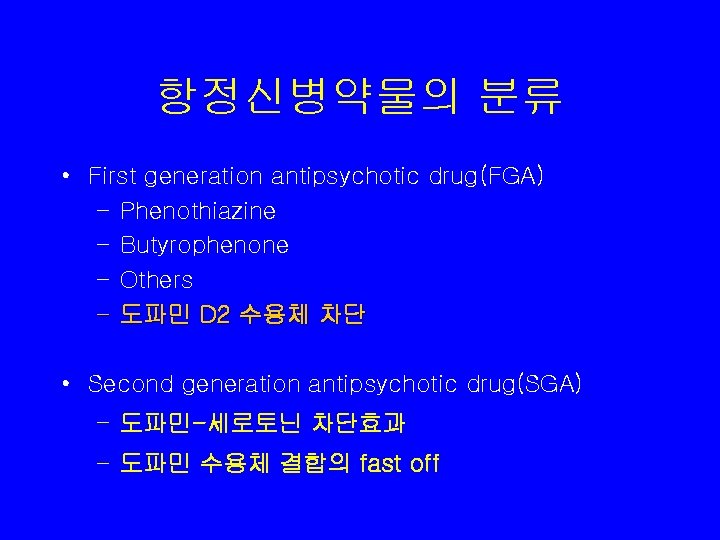
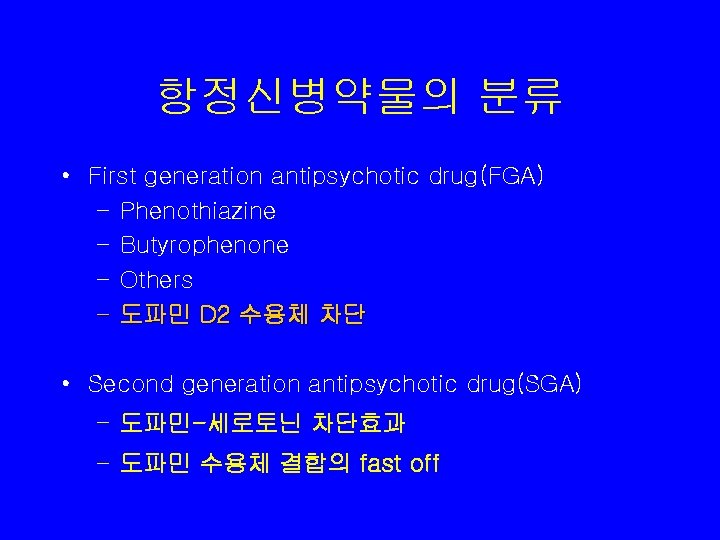
항정신병약물의 분류 • First generation antipsychotic drug(FGA) – Phenothiazine – Butyrophenone – Others – 도파민 D 2 수용체 차단 • Second generation antipsychotic drug(SGA) – 도파민-세로토닌 차단효과 – 도파민 수용체 결합의 fast off

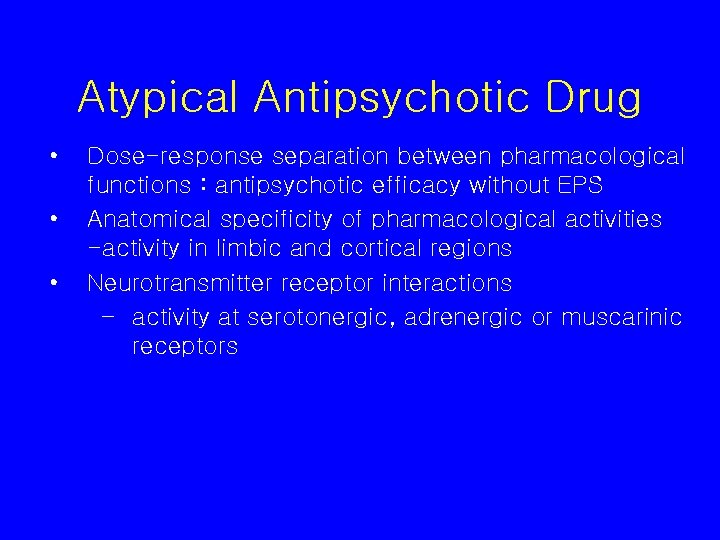
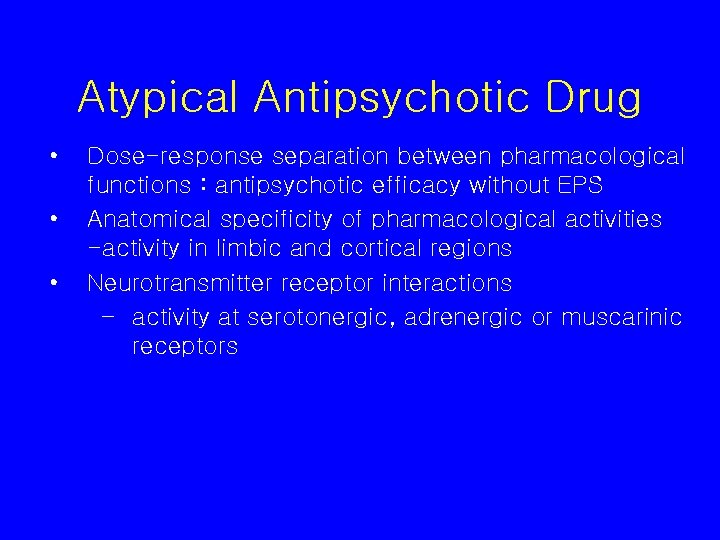
Atypical Antipsychotic Drug • • • Dose-response separation between pharmacological functions : antipsychotic efficacy without EPS Anatomical specificity of pharmacological activities -activity in limbic and cortical regions Neurotransmitter receptor interactions – activity at serotonergic, adrenergic or muscarinic receptors

Dopamine hypothesis • DA 활성 과잉 – “Antipsychotics reduce psychotic symptoms by decreasing dopamine activity. ” • Revised dopamine hypothesis – Negative symptom; mesocortical pathway의 DA 활성 저하 – Positive symptom ; Meso. Limbic pathway 의 DA 활성 과잉
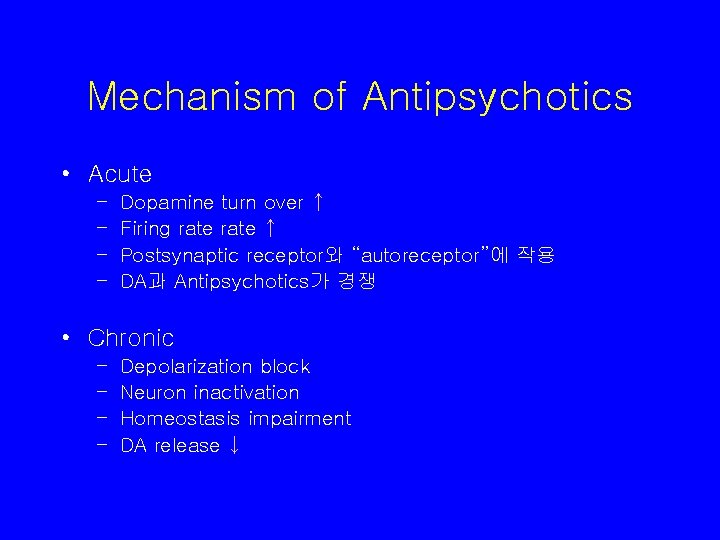
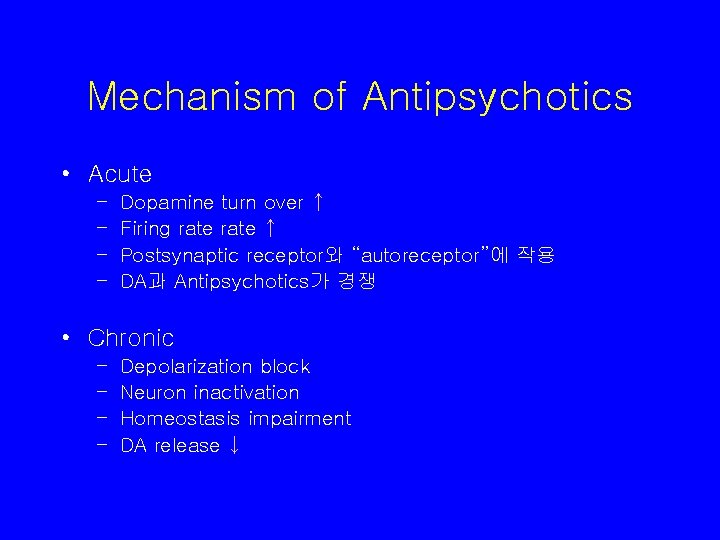
Mechanism of Antipsychotics • Acute – – Dopamine turn over ↑ Firing rate ↑ Postsynaptic receptor와 “autoreceptor”에 작용 DA과 Antipsychotics가 경쟁 • Chronic – – Depolarization block Neuron inactivation Homeostasis impairment DA release ↓
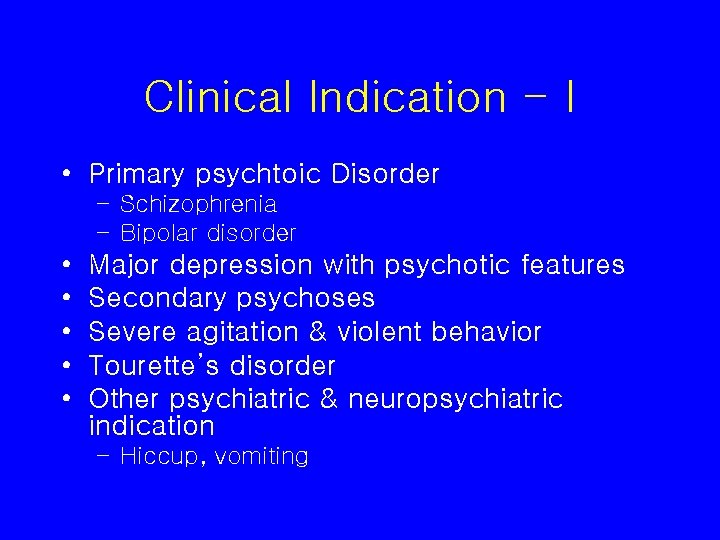
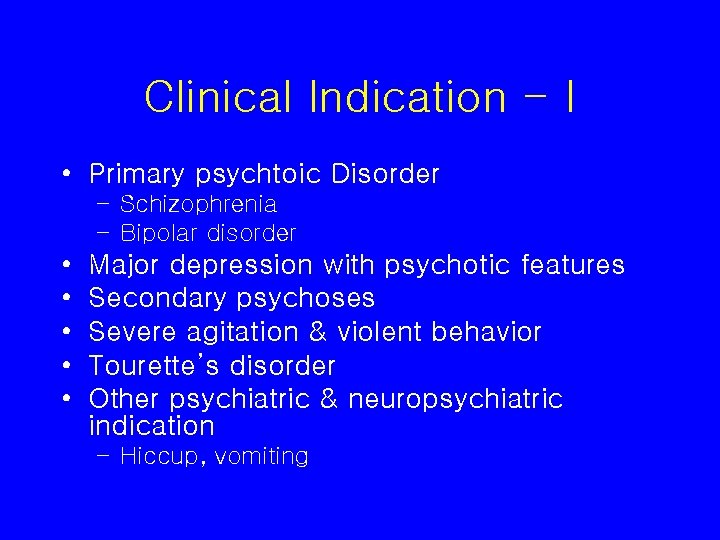
Clinical Indication - I • Primary psychtoic Disorder – Schizophrenia – Bipolar disorder • • • Major depression with psychotic features Secondary psychoses Severe agitation & violent behavior Tourette’s disorder Other psychiatric & neuropsychiatric indication – Hiccup, vomiting
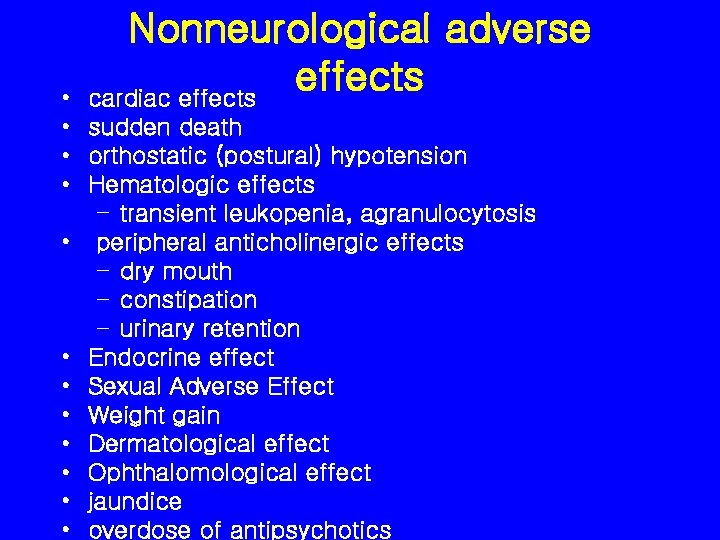
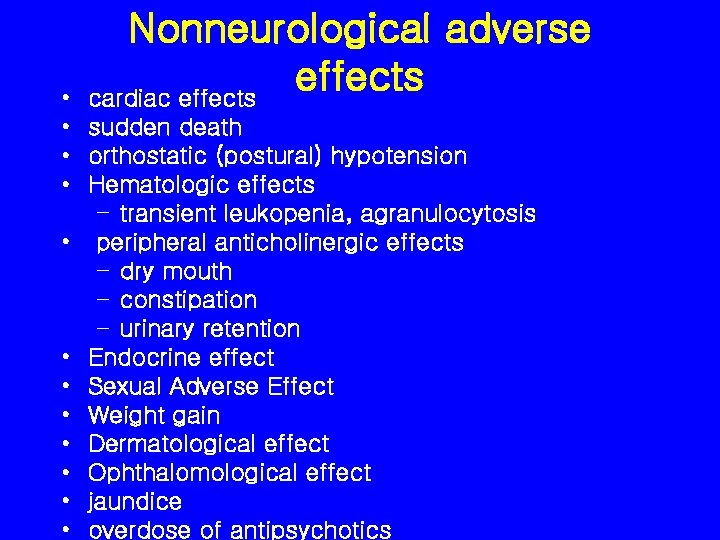
Nonneurological adverse effects cardiac effects • • sudden death • orthostatic (postural) hypotension • Hematologic effects – transient leukopenia, agranulocytosis • peripheral anticholinergic effects – dry mouth – constipation – urinary retention • Endocrine effect • Sexual Adverse Effect • Weight gain • Dermatological effect • Ophthalomological effect • jaundice • overdose of antipsychotics
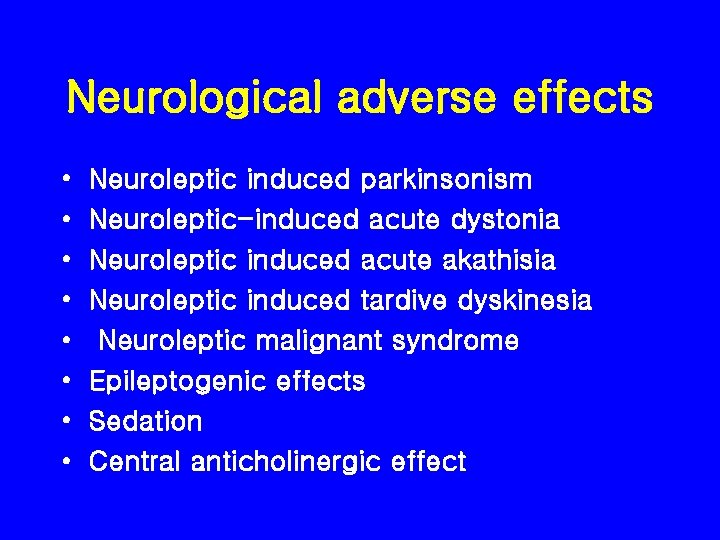
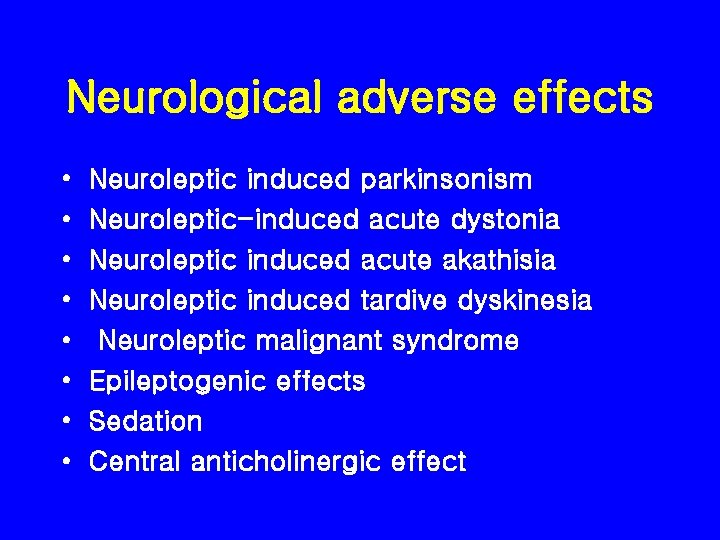
Neurological adverse effects • • Neuroleptic induced parkinsonism Neuroleptic-induced acute dystonia Neuroleptic induced acute akathisia Neuroleptic induced tardive dyskinesia Neuroleptic malignant syndrome Epileptogenic effects Sedation Central anticholinergic effect
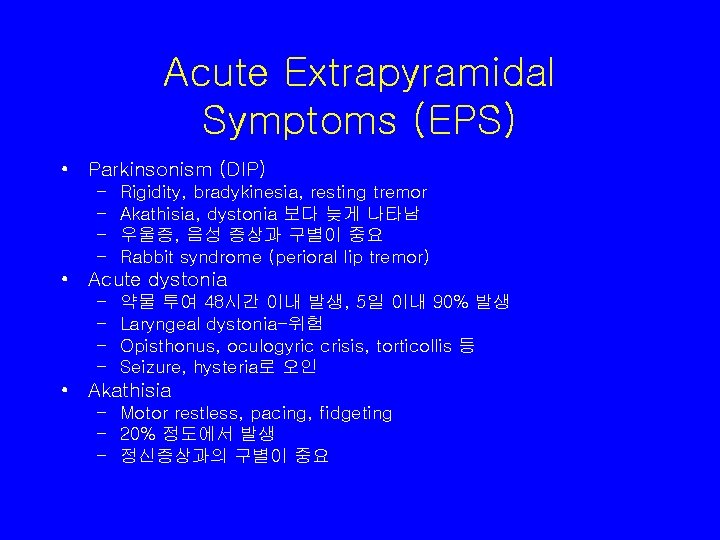
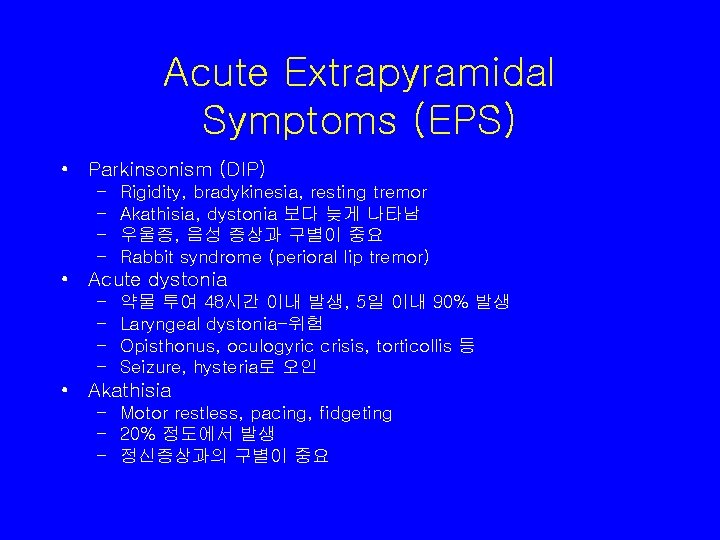
Acute Extrapyramidal Symptoms (EPS) • Parkinsonism (DIP) – – Rigidity, bradykinesia, resting tremor Akathisia, dystonia 보다 늦게 나타남 우울증, 음성 증상과 구별이 중요 Rabbit syndrome (perioral lip tremor) • Acute dystonia – – 약물 투여 48시간 이내 발생, 5일 이내 90% 발생 Laryngeal dystonia-위험 Opisthonus, oculogyric crisis, torticollis 등 Seizure, hysteria로 오인 • Akathisia – Motor restless, pacing, fidgeting – 20% 정도에서 발생 – 정신증상과의 구별이 중요




Neuroleptic induced tardive dyskinesia • Mechanism – Denervation supersensitivity 항정신병약 물의 장기 투여로 인한 도파민 수용체의 지 난친 감수성항진 – D 1 -D 2 imbalance – Free radical toxicity – GABA deficiency

TD 치료 • Antipsychotics의 중단 • Symptoms suppression – Valproic acid, clonazepam, diazepam – Propranolol, clonidine – Vitamine E, buspirone • Antipsychotics의 투여 – Atypical antipsychotics cf. Clozapine

Neuroleptic malignant syndrome • life threthning complication • motor & behavioral sx: muscular rigidity, akinesia, mutism, obtundation, agitation • autonomic sx: hyperpyrexia, sweating, pulse와 BP 증가 • lab finding: WBC증가, creatinine phosphokinase, liver enzyme, plasma myoblobin, myoglobinuria, ->renal failure • 경과: 24 -72 hr에 걸쳐 진전되고 치료 안하면 10 -14일까지도 지 속됨. 초기에 withdrawal or agitation 양상을 psychosis의 악화 로 잘못 판단하는 경우가 흔함. • risk: men, young • 사망률: 20 -30%, depot 사용시 그 이상일수 있음. • 발병기전은 Lithium 사용, 고역가 약물, 고용량, 약물의 빠른 증 량, 근육 주사, 탈수 등이 연관.








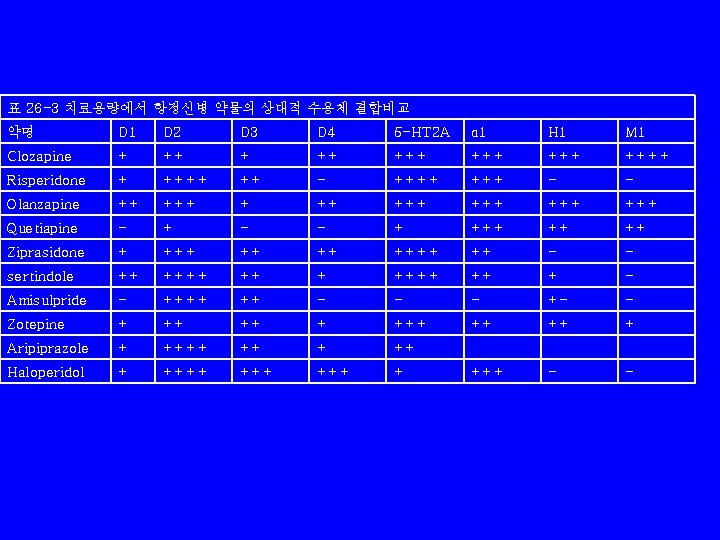
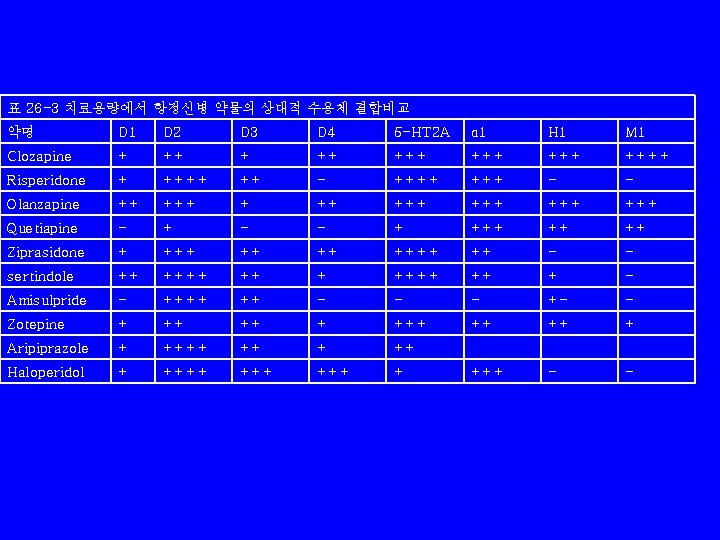
표 26 -3 치료용량에서 항정신병 약물의 상대적 수용체 결합비교 약명 D 1 D 2 D 3 D 4 5 -HT 2 A α 1 H 1 M 1 Clozapine + ++ +++ ++++ Risperidone + ++++ ++ - ++++ - - Olanzapine ++ +++ +++ +++ Quetiapine - + - - + ++ ++ Ziprasidone + ++ ++ ++ - - sertindole ++ ++++ ++ + - Amisulpride - ++++ ++ - - - +- - Zotepine + ++ ++ + Aripiprazole + ++++ ++ Haloperidol + +++ +++ - -
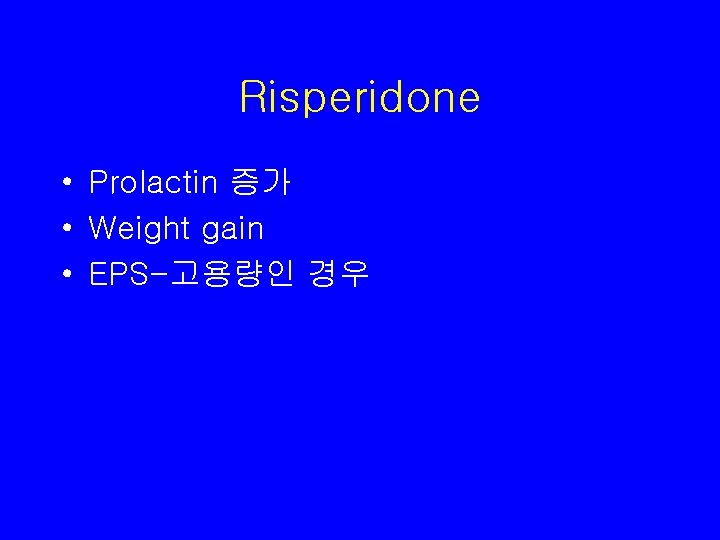
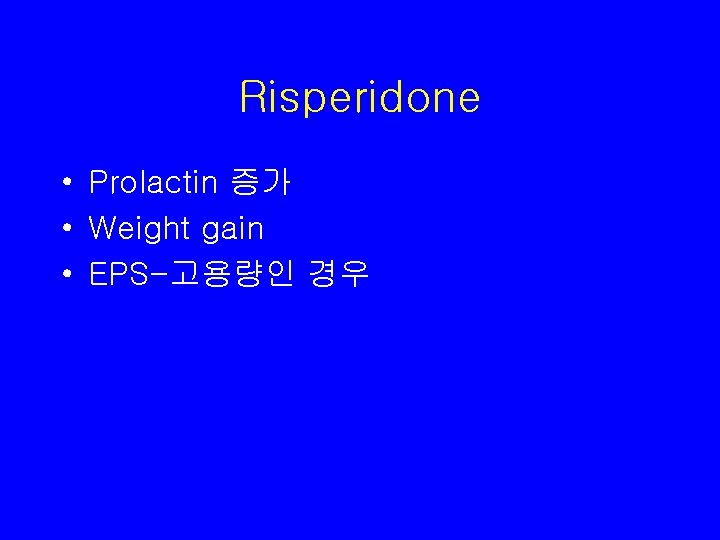
Risperidone • Prolactin 증가 • Weight gain • EPS-고용량인 경우
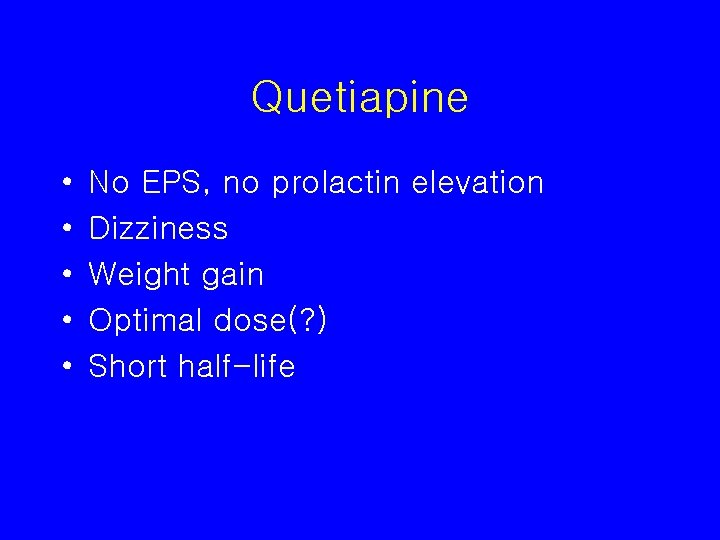
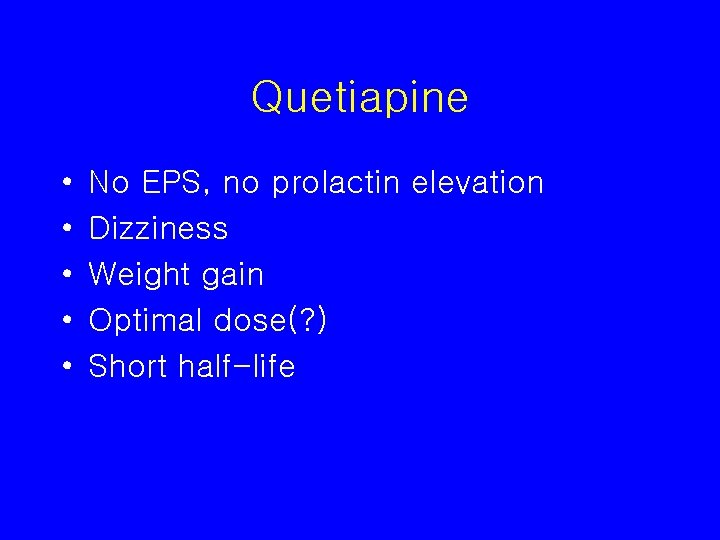
Quetiapine • • • No EPS, no prolactin elevation Dizziness Weight gain Optimal dose(? ) Short half-life

Amisulpride • 고용량에서 D 2 receptor Antagonistic acitivity • 저용량에서 Presynaptic D 2 autoreceptor Antagonistic activity
Ziprasidone • No weight gain • EKG abnormality • B. i. d. 로 복용
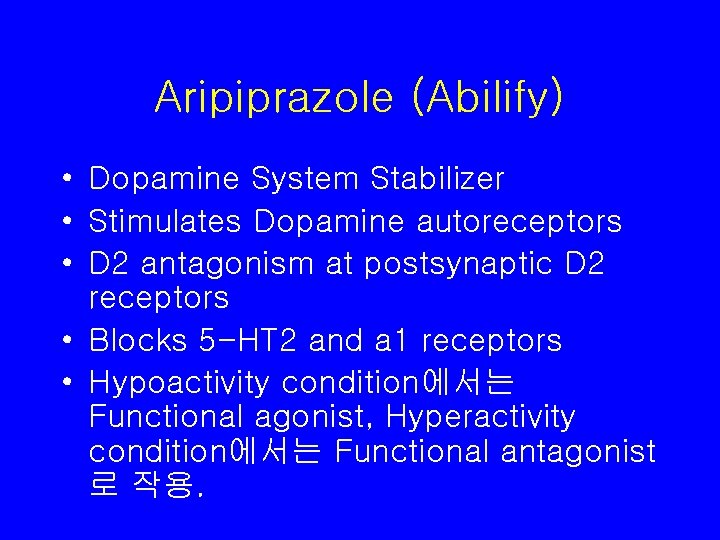
Aripiprazole (Abilify) • Dopamine System Stabilizer • Stimulates Dopamine autoreceptors • D 2 antagonism at postsynaptic D 2 receptors • Blocks 5 -HT 2 and a 1 receptors • Hypoactivity condition에서는 Functional agonist, Hyperactivity condition에서는 Functional antagonist 로 작용.

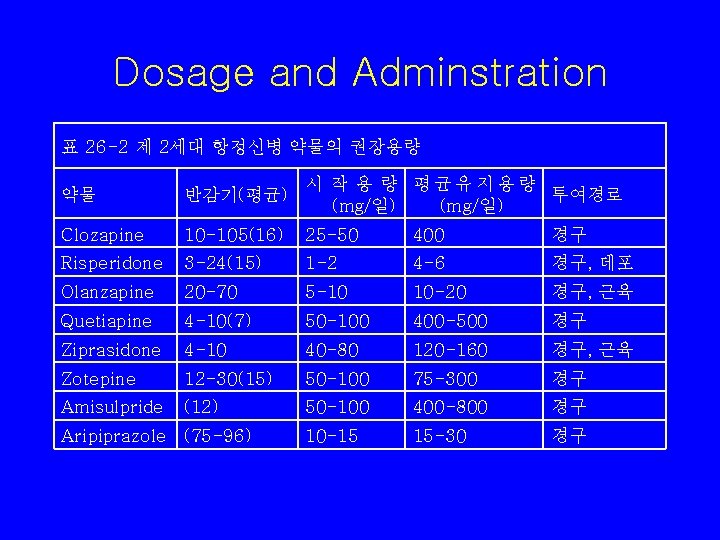
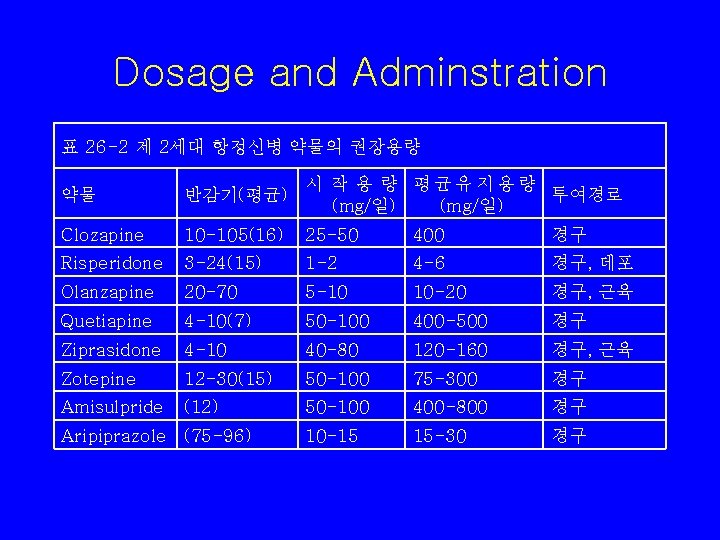
Dosage and Adminstration 표 26 -2 제 2세대 항정신병 약물의 권장용량 약물 반감기(평균) 시 작 용 량 평균유지용량 투여경로 (mg/일) Clozapine 10 -105(16) 25 -50 400 경구 Risperidone 3 -24(15) 1 -2 4 -6 경구, 데포 Olanzapine 20 -70 5 -10 10 -20 경구, 근육 Quetiapine 4 -10(7) 50 -100 400 -500 경구 Ziprasidone 4 -10 40 -80 120 -160 경구, 근육 Zotepine 12 -30(15) 50 -100 75 -300 경구 Amisulpride (12) 50 -100 400 -800 경구 10 -15 15 -30 경구 Aripiprazole (75 -96)

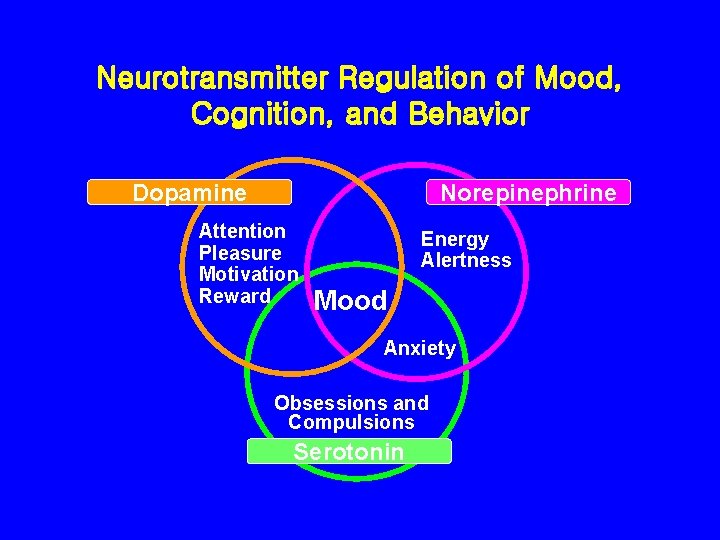
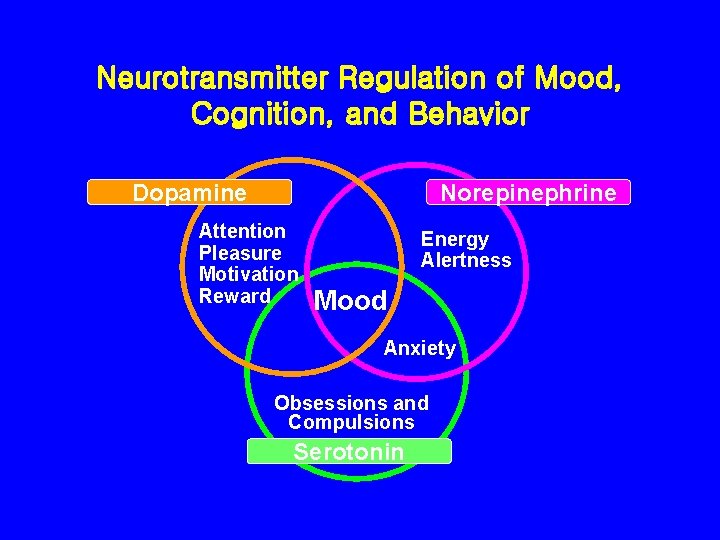
Neurotransmitter Regulation of Mood, Cognition, and Behavior Dopamine Norepinephrine Attention Pleasure Motivation Reward Energy Alertness Mood Anxiety Obsessions and Compulsions Serotonin Stahl. Essential Psychopharmacology 1996 Foote. Psychopharmacology 1995

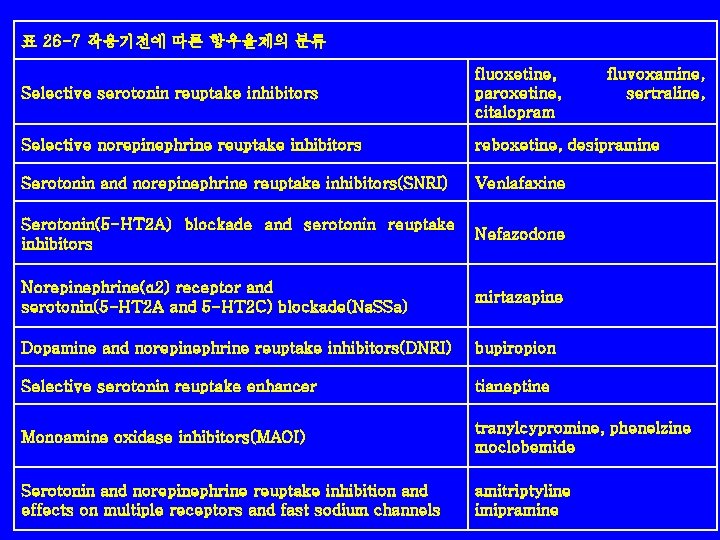
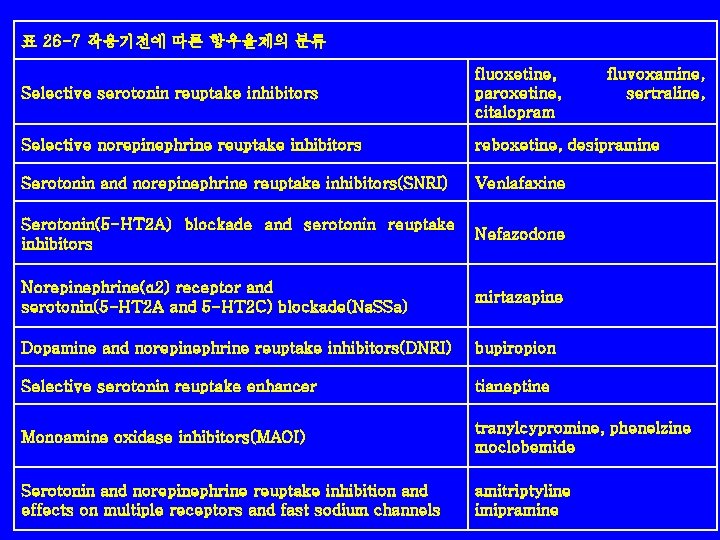
표 26 -7 작용기전에 따른 항우울제의 분류 Selective serotonin reuptake inhibitors fluoxetine, paroxetine, citalopram fluvoxamine, sertraline, Selective norepinephrine reuptake inhibitors reboxetine, desipramine Serotonin and norepinephrine reuptake inhibitors(SNRI) Venlafaxine Serotonin(5 -HT 2 A) blockade and serotonin reuptake inhibitors Nefazodone Norepinephrine(α 2) receptor and serotonin(5 -HT 2 A and 5 -HT 2 C) blockade(Na. SSa) mirtazapine Dopamine and norepinephrine reuptake inhibitors(DNRI) bupiropion Selective serotonin reuptake enhancer tianeptine Monoamine oxidase inhibitors(MAOI) tranylcypromine, phenelzine moclobemide Serotonin and norepinephrine reuptake inhibition and effects on multiple receptors and fast sodium channels amitriptyline imipramine
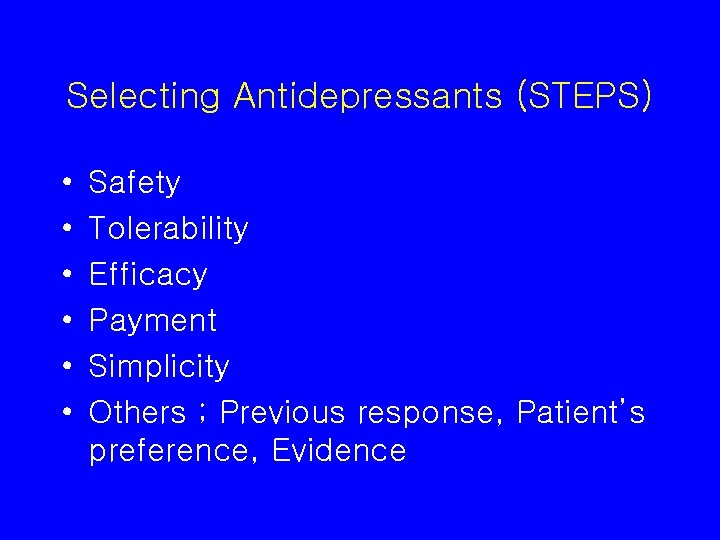
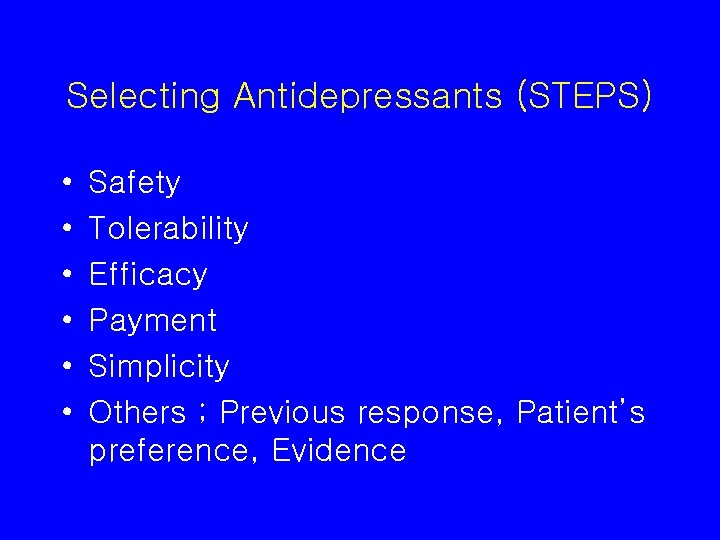
Selecting Antidepressants (STEPS) • • • Safety Tolerability Efficacy Payment Simplicity Others ; Previous response, Patient’s preference, Evidence

table 24 -2 Guidelines for choosing an antidepressant medication Unipolar depression All antidepresants are equally effective, Choose on the basis of previous response, side effects, comorbid medical and psychotic disorders Depression with melancholia features TCA Depression with atypical feature SSRI, MAOI Depression with psychotic feature Antidepressant plus antipsychotics, or ECT. Avoid Bupropion Bipolar depression Lithium, Lamotrigine Depression + OCD SSRI, Clomipramine Depression + Panic disorder SSRI, TCA, MAOI Depression + Seizure Avoids bupropion and TCAs Depression + Parkinson's Disease Bupropion Depression + Sexual Dysfunction Bupropion, nefazodone, mirtazapine
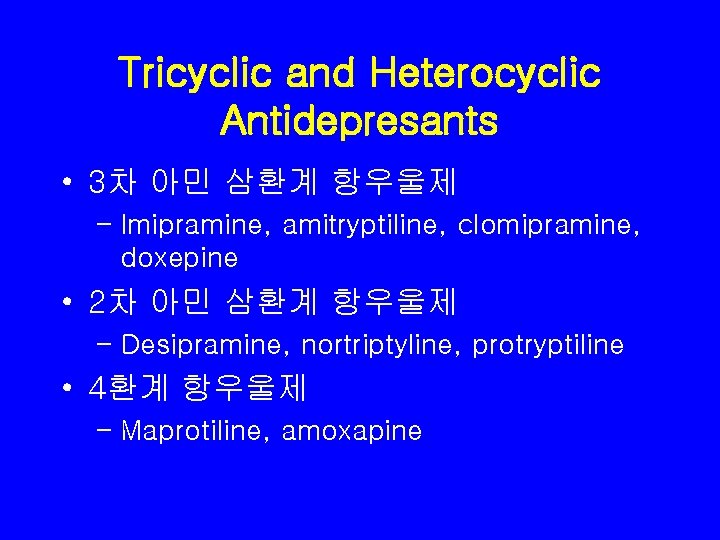
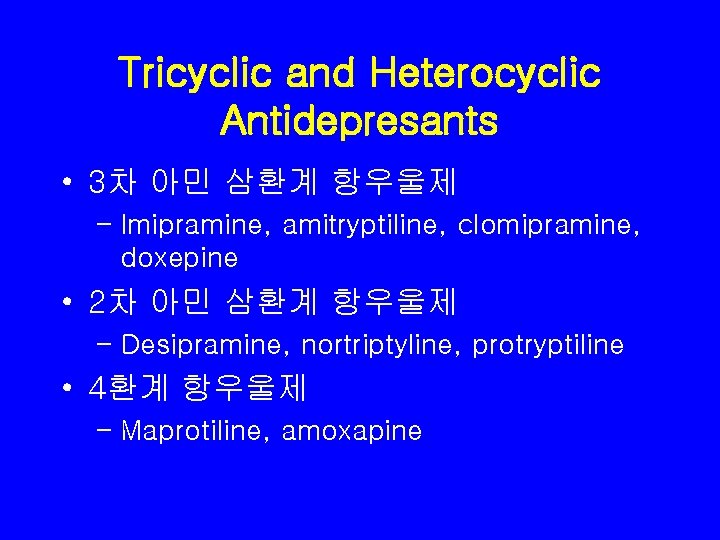
Tricyclic and Heterocyclic Antidepresants • 3차 아민 삼환계 항우울제 – Imipramine, amitryptiline, clomipramine, doxepine • 2차 아민 삼환계 항우울제 – Desipramine, nortriptyline, protryptiline • 4환계 항우울제 – Maprotiline, amoxapine
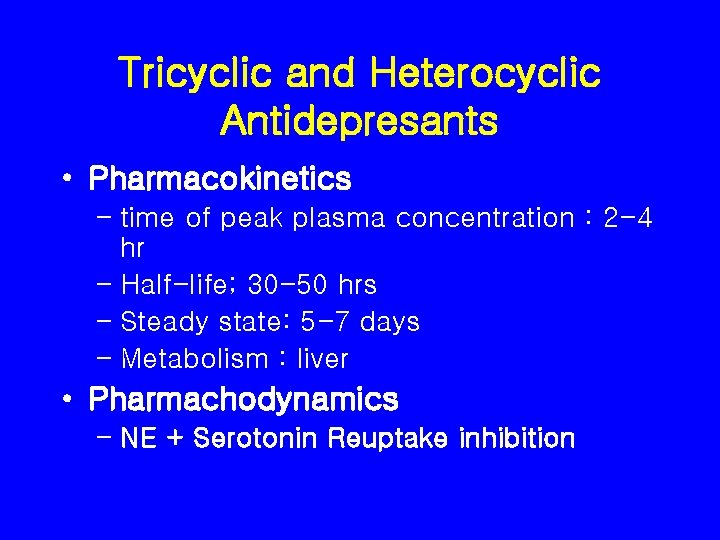
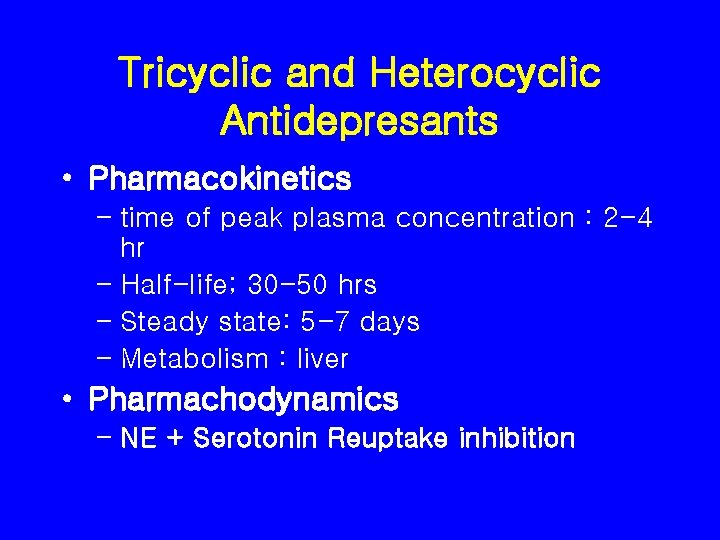
Tricyclic and Heterocyclic Antidepresants • Pharmacokinetics – time of peak plasma concentration : 2 -4 hr – Half-life; 30 -50 hrs – Steady state: 5 -7 days – Metabolism : liver • Pharmachodynamics – NE + Serotonin Reuptake inhibition
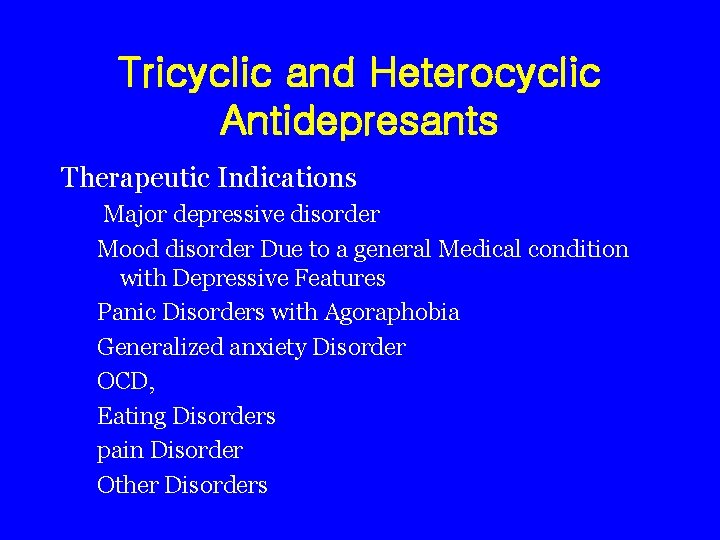
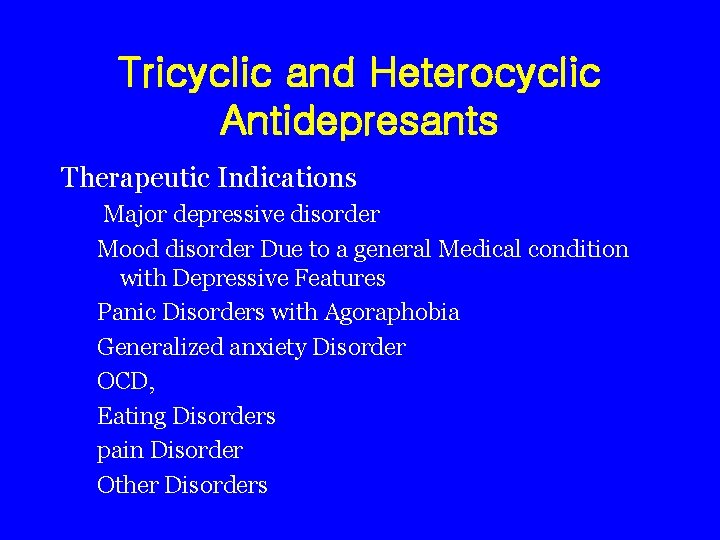
Tricyclic and Heterocyclic Antidepresants Therapeutic Indications Major depressive disorder Mood disorder Due to a general Medical condition with Depressive Features Panic Disorders with Agoraphobia Generalized anxiety Disorder OCD, Eating Disorders pain Disorder Other Disorders
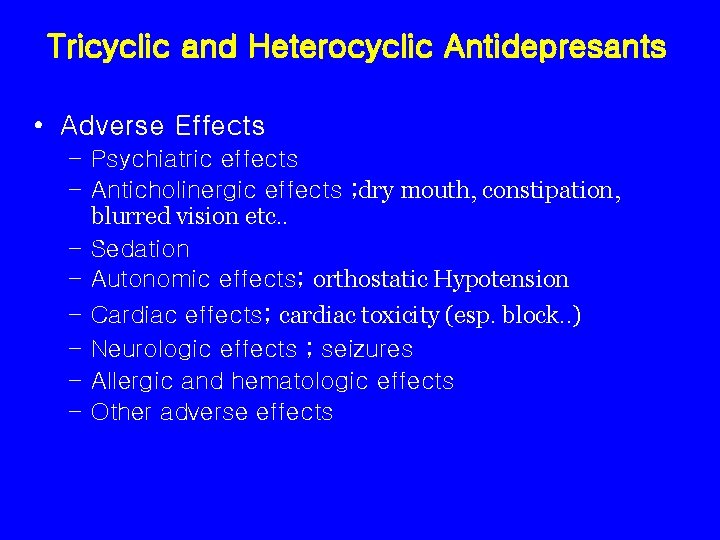
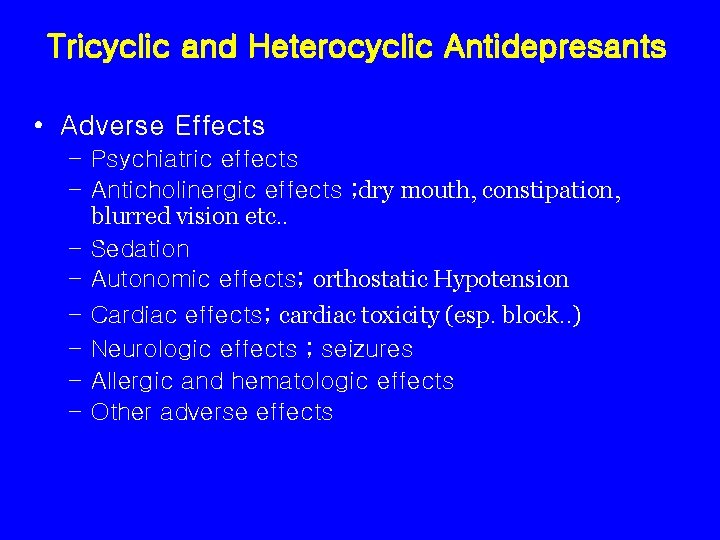
Tricyclic and Heterocyclic Antidepresants • Adverse Effects – Psychiatric effects – Anticholinergic effects ; dry mouth, constipation, blurred vision etc. . – Sedation – Autonomic effects; orthostatic Hypotension – Cardiac effects; cardiac toxicity (esp. block. . ) – Neurologic effects ; seizures – Allergic and hematologic effects – Other adverse effects

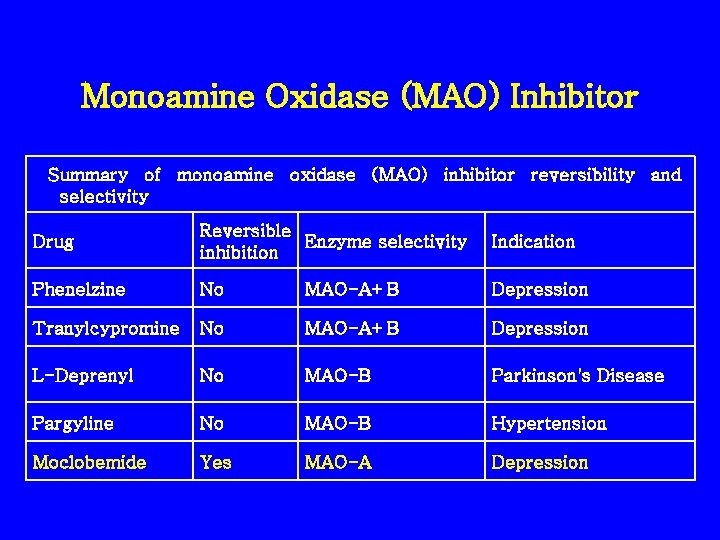
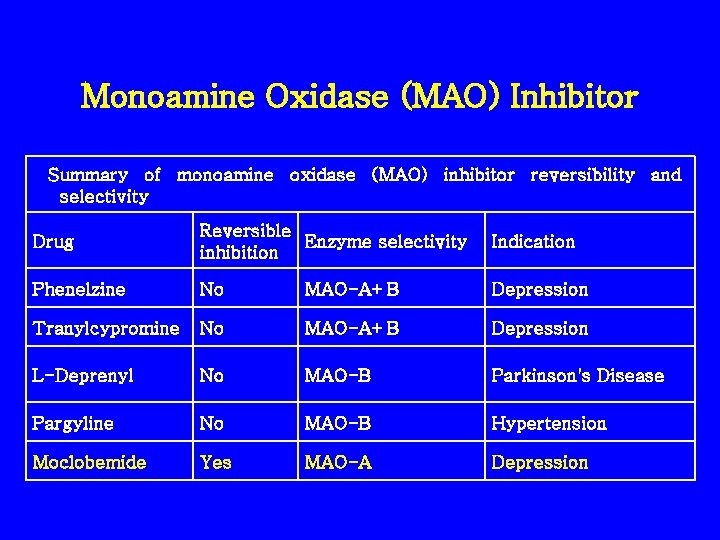
Monoamine Oxidase (MAO) Inhibitor Summary of monoamine oxidase (MAO) inhibitor reversibility and selectivity Drug Reversible Enzyme selectivity inhibition Indication Phenelzine No MAO-A+B Depression Tranylcypromine No MAO-A+B Depression L-Deprenyl No MAO-B Parkinson's Disease Pargyline No MAO-B Hypertension Moclobemide Yes MAO-A Depression

Selective Serotonin Reuptake Inhibitors • Fluoxetine (Prozac) • Paroxetine (Seroxat) • Sertraline (Zoloft) • Fluvoxamine (Dumirox) • Citalopram (Cipram)

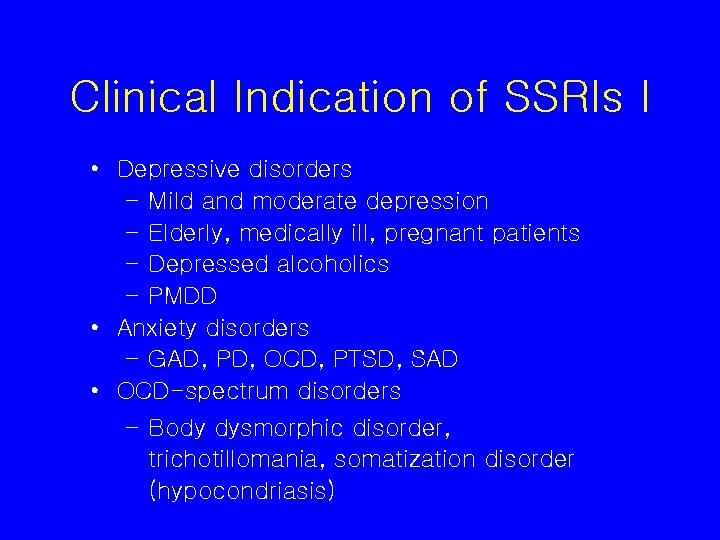
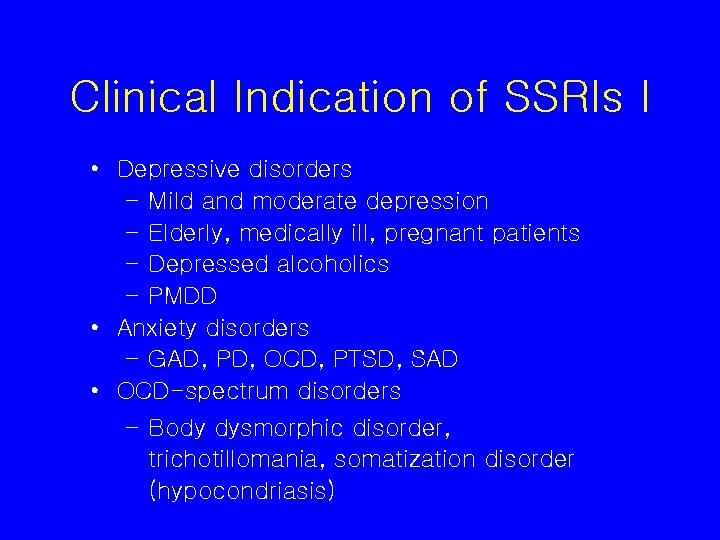
Clinical Indication of SSRIs I • Depressive disorders – Mild and moderate depression – Elderly, medically ill, pregnant patients – Depressed alcoholics – PMDD • Anxiety disorders – GAD, PD, OCD, PTSD, SAD • OCD-spectrum disorders – Body dysmorphic disorder, trichotillomania, somatization disorder (hypocondriasis)

Clinical Indication of SSRIs II • Eating disorder – Bulimia nervosa, Anorexia nervosa • • • Migraine, Chronic low back pain Perimenopausal hot flushes Affective incontinence Irritable bowel syndrome Premature ejaculation
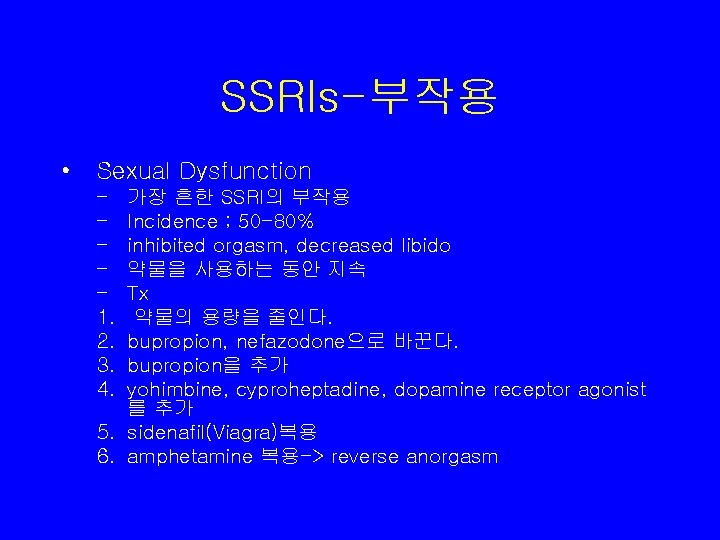
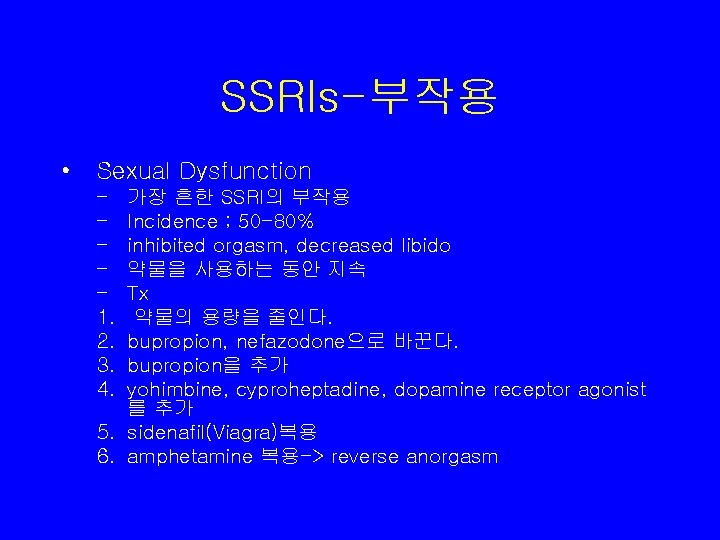
SSRIs-부작용 • Sexual Dysfunction – – – 1. 2. 3. 4. 가장 흔한 SSRI의 부작용 Incidence ; 50 -80% inhibited orgasm, decreased libido 약물을 사용하는 동안 지속 Tx 약물의 용량을 줄인다. bupropion, nefazodone으로 바꾼다. bupropion을 추가 yohimbine, cyproheptadine, dopamine receptor agonist 를 추가 5. sidenafil(Viagra)복용 6. amphetamine 복용-> reverse anorgasm

SSRIs-부작용 • Gastrointestinal Adverse Effects – m/c complaints; Nausea, diarrhea, anorexia, vomiting, dyspepsia – Fluoxetine induced weight loss and appetite loss ; 복용하 자 마자 바로 시작되고 20주에 peak를 이룬 이후에는 다시 baseline으로 돌아감 – Weight Gain; 1/3 에서 체중증가, Paroxetine이 anticholinergic activity를 가지며 가장 체중 증가와 연관된 SSRI임. • Headaches – Fluoxetine이 가장 두통과 연관됨 – 모든 SSRI가 migraine and tension-type headache 예방에 효과적임
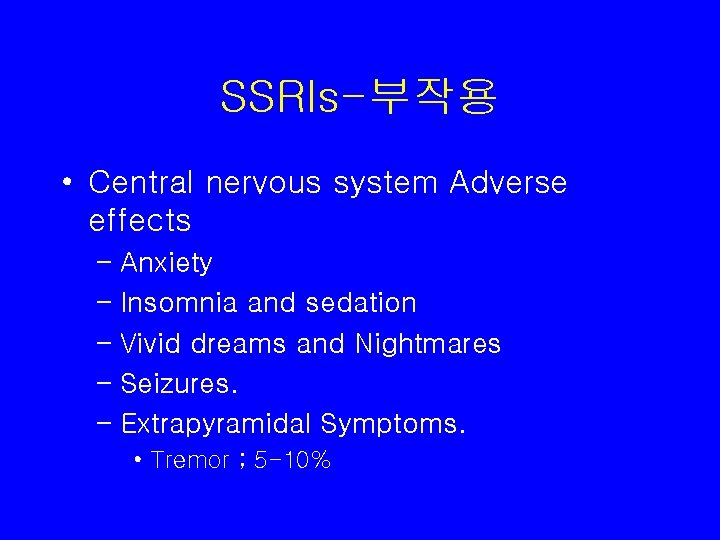
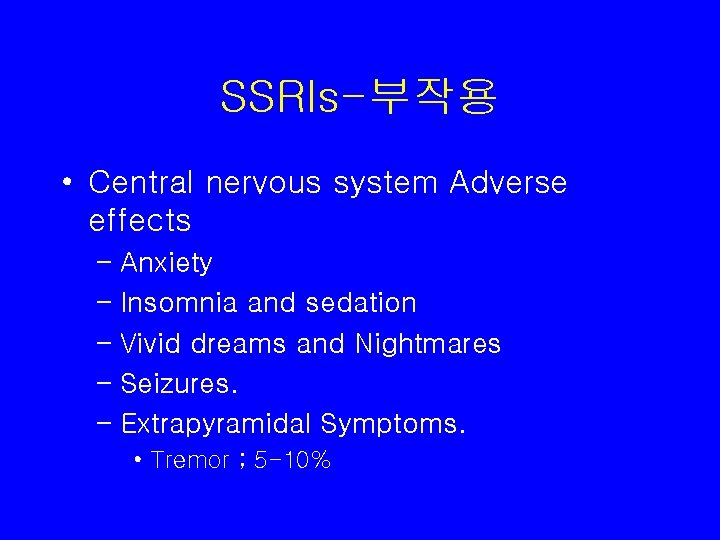
SSRIs-부작용 • Central nervous system Adverse effects – Anxiety – Insomnia and sedation – Vivid dreams and Nightmares – Seizures. – Extrapyramidal Symptoms. • Tremor ; 5 -10%
SSRIs-부작용 • • • Anticholinergic effects Hematological adverse Effects Electrolyte and Glucose Disturbance Endocrine and Allergic Reactions Galactorrhea
SSRIs-부작용 • Serotonin Syndrome – 심각하고 치명적 – SSRI와 MAOI, L-tryptophan, 또는 Lithium을 동 시에 투여하면 혈중 serotonin 농도를 독성 수준까 지 올림. – Sx; (1) diarrhea, (2) restlessness, (3) extreme agitation, hyperreflexia, autonomic instability (4) myoclonus, seizures, hyperthymia, uncontrollable shivering, and rigidity, and (5) delirium, coma, Status epilepticus, Cardiovascular collapse, Death.
SSRIs-부작용 • Serotonin Syndrome • 치료; – 유발 약물을 중단 – nitroglycerin, Cyproheptadine, methylsergide(Sansert), cooling blankets, chlorpromazine(Thorazine), dantrolene(Dantrium), Benzodiazepines, anticonvulsant, mechanical ventilation, & paralyzing agents 등 신속하고 포괄적인 지지적 인 처치.

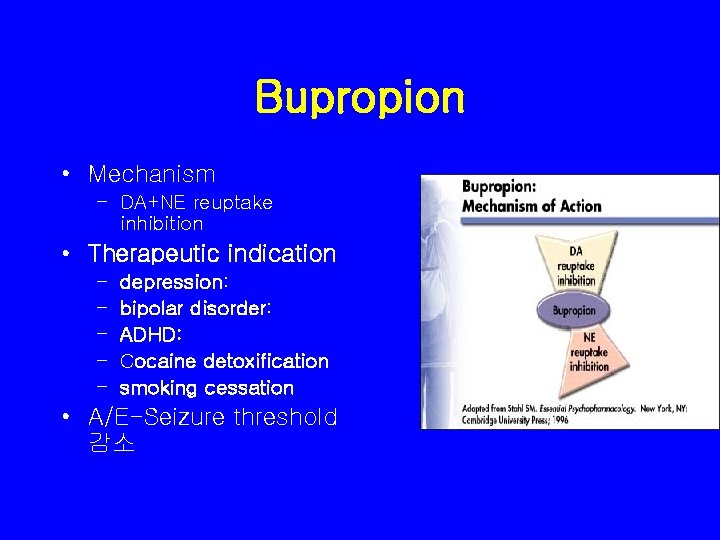
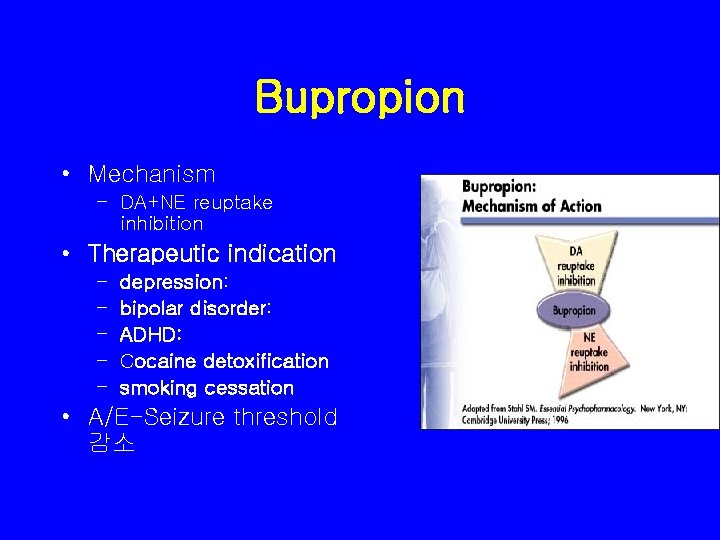
Bupropion • Mechanism – DA+NE reuptake inhibition • Therapeutic indication – – – depression: bipolar disorder: ADHD: Cocaine detoxification smoking cessation • A/E-Seizure threshold 감소
Trazodone • 5 -HT 2 antagonist + weak 5 -HT 2 Reuptake inhibition • No anticholinergic effect • Marked sedative effects • Half-life; 6 -11 hrs • Indication ; – Depression-수면의 질을 향상 – insomnia, esp. Insomnia d/t SSRIs – severe agitation in elderly patient • Side effects; Sedation, priapism, dizziness, orthostatic hypotension
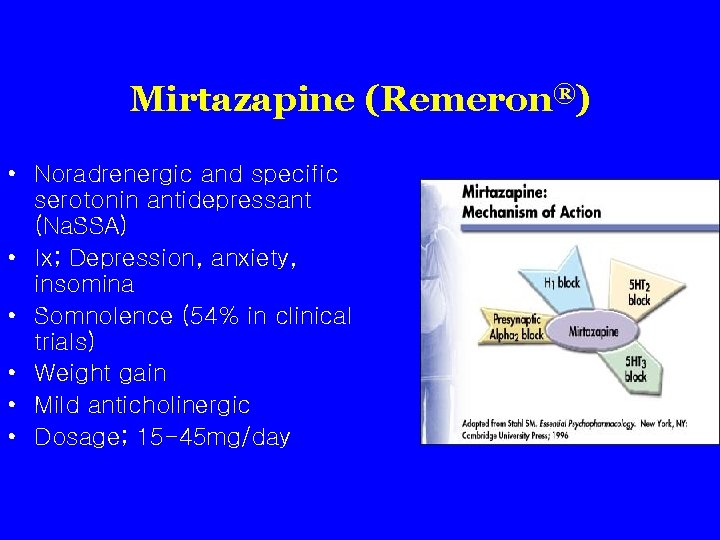
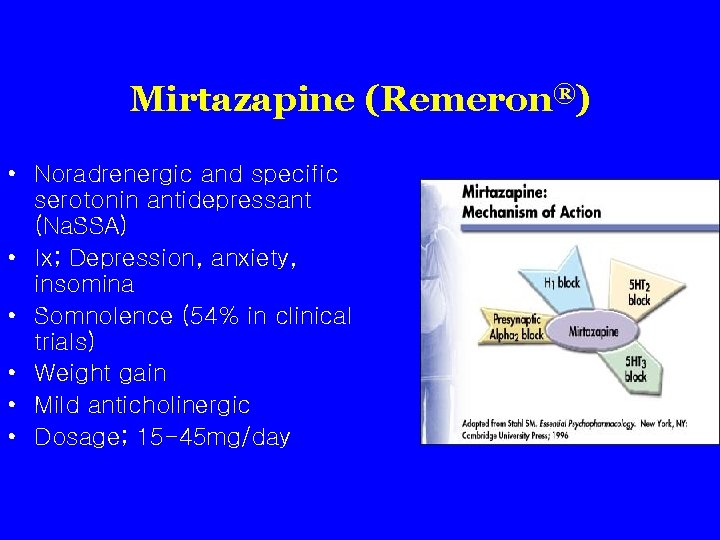
Mirtazapine (Remeron®) • Noradrenergic and specific serotonin antidepressant (Na. SSA) • Ix; Depression, anxiety, insomina • Somnolence (54% in clinical trials) • Weight gain • Mild anticholinergic • Dosage; 15 -45 mg/day
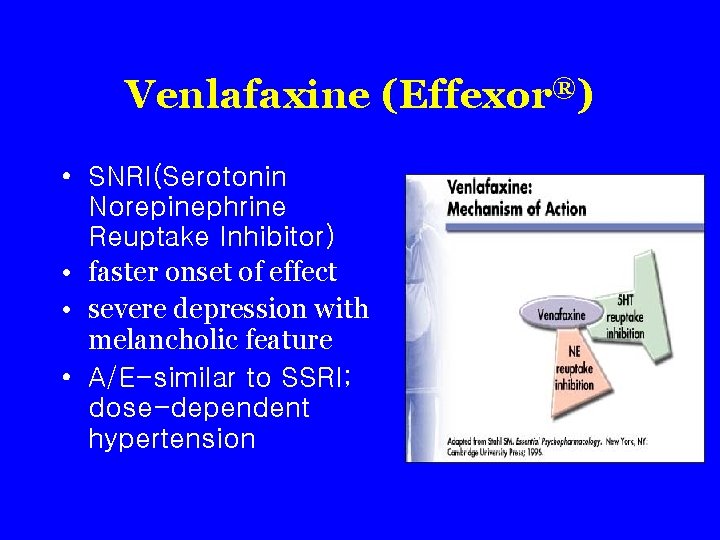
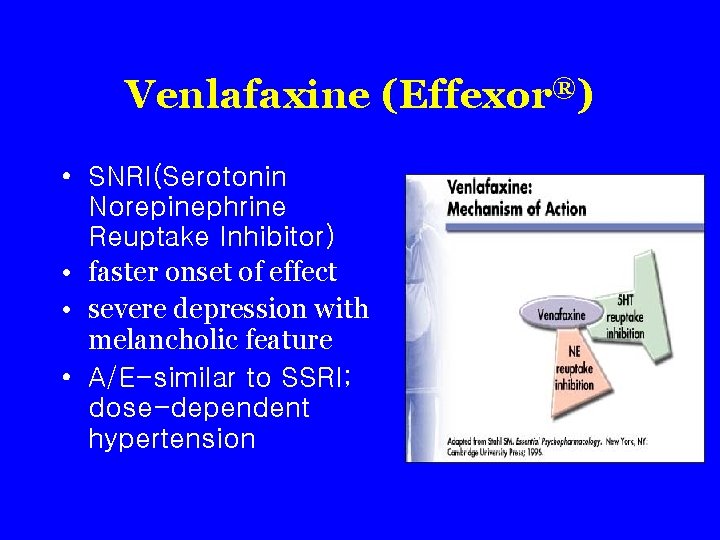
Venlafaxine (Effexor®) • SNRI(Serotonin Norepinephrine Reuptake Inhibitor) • faster onset of effect • severe depression with melancholic feature • A/E-similar to SSRI; dose-dependent hypertension
기분조절제 Mood Stabilizer
Mood Stabilizer : Definition • Narrow concept – Antimanic + antidepressive • Broad concept – Antimanic – Antidepressive – No switching
Mood Stabilizer : History • • • 1949 Li introduced 1950 s-60 s Li popular 19070 s Li; wonder drug 1980 s CBZ, VPA introduced 1990 s CBZ, VPA popular, Li goes down 2000 s APA Expert Conseus Guideline series Numerous systemic reviews Li revival, VPA popular; CBZ goes down New anti convulsant Atypical antipsychotics
Lithium
Lithium • Chemistry – Monovalent ion – Akali ion – 6 Li, 7 Li
Lithium • PHARMACOLOGICAL ACTIONS 1. Pharmacokinetics • • • Absorption; rapidly and completely absorbed Half-life : 24 hours Metabolism ; Renal
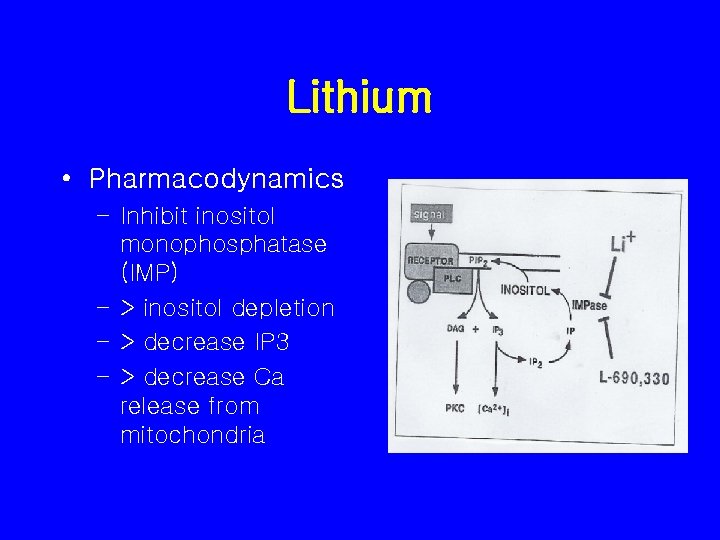
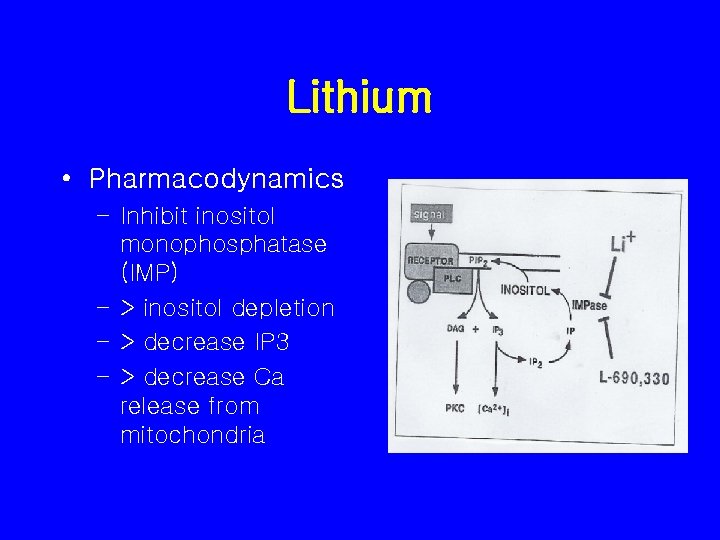
Lithium • Pharmacodynamics – Inhibit inositol monophosphatase (IMP) – > inositol depletion – > decrease IP 3 – > decrease Ca release from mitochondria
Lithium • Therapeutic indications – – – – Bipolar I disorder Schizoaffective disorder and Schizophrenia Major depression Aggression Alcohol use disorder Other Psychiatric disorder Nonpsychiatric medical conditions
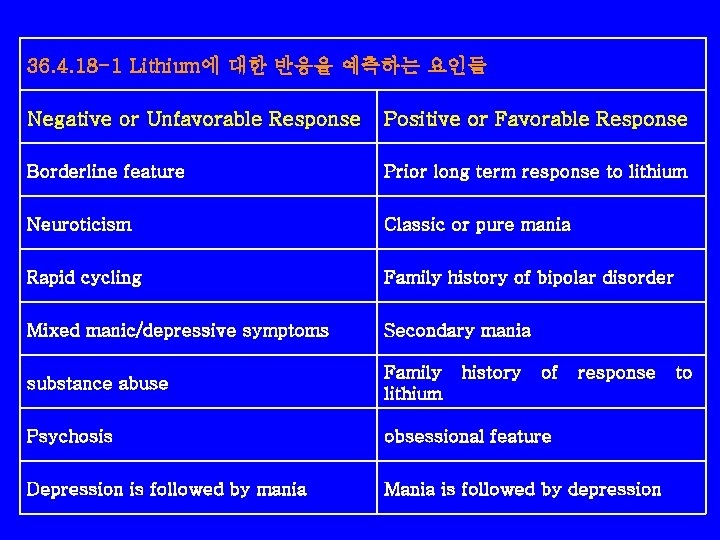
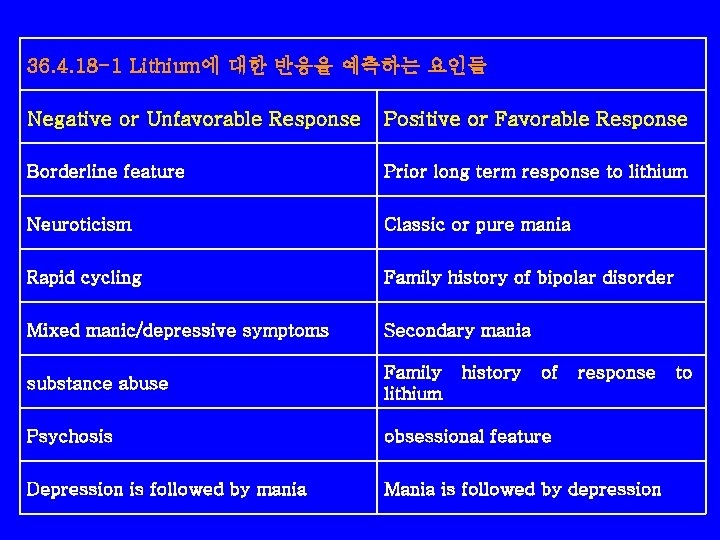
36. 4. 18 -1 Lithium에 대한 반응을 예측하는 요인들 Negative or Unfavorable Response Positive or Favorable Response Borderline feature Prior long term response to lithium Neuroticism Classic or pure mania Rapid cycling Family history of bipolar disorder Mixed manic/depressive symptoms Secondary mania substance abuse Family lithium Psychosis obsessional feature Depression is followed by mania Mania is followed by depression history of response to
Lithium • Adverse effects 1) Tremor 2) Cognitive effects 3) Renal effects 4) Thyroid effects 5) Li-induced hypothyroidism 6) Cardiac effects 7) Dermatological effects 8) Lithium intoxication
Lithium • Adverse effects – 많은 부작용을 가지고 있다. – 혈중농도에 따라 빈도와 정도가 다르다. – 농도를 30% 낮추면(0. 8 -1. 0 ->0. 5 -0. 8) 부작용 빈도가 90%에서 60%로 감소 • Most common side effects – Gastric distress – Weight gain – Tremor, fatigue, mild cognitive impairment
Lithium • Tremor – 8 -10 Hz – Outstretched hand (esp, fingers) – Worse during the times of peak drug levels – Tx • Divided dosage • Propranolol • Before bed time
Lithium • Cognitive effects – Dysphoria – Lack of spontaneity – Slowed reaction time – Impaired memory
Lithium • Renal effects – Polyuria with secondary polydipsia – ADH antagonistic effects – Insomnia, weight gain, dehydration, social occupational problem – Tx • Fluid replacement • Lowest effective dose • Single daily dose
Lithium • Thyroid effects – Transient mild abnormalities in TFT – Common early – Little or no clinical consequence – 50% of long-term tx: abnomal TRH response – 30% of long-term tx: TSH – Li-induced hypothyroidism
Lithium • Cardiac effects – T wave flattening or inversion ; benign – Sinus dysrhythmia, heart block, episode of syncope – Cix in sick sinus syndome – Rare: ventricular arrhythmia, CHF
Lithium • Dermatological effects – Dose-dependent – Acne and psoriasis – Rashes of varies types – Hair loss ; occasionally related to lithium -induced hypothyroidism
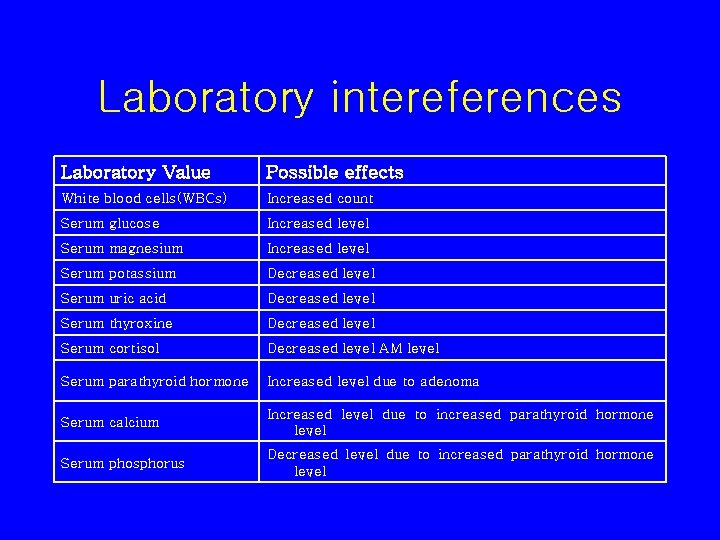
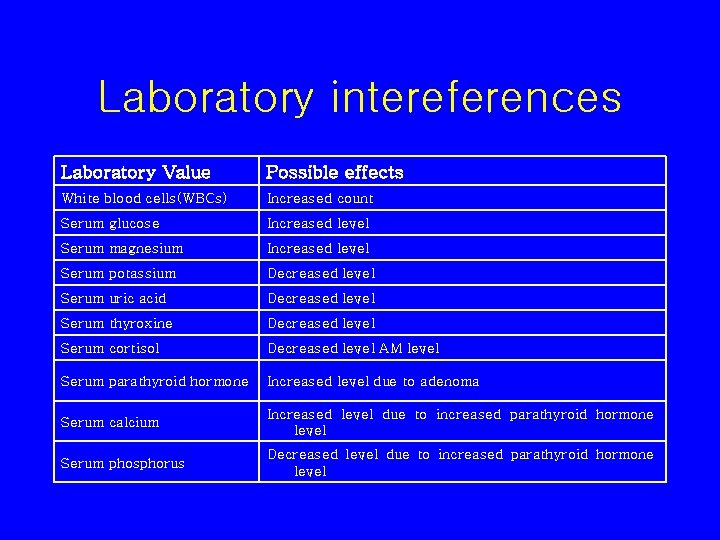
Laboratory intereferences Laboratory Value Possible effects White blood cells(WBCs) Increased count Serum glucose Increased level Serum magnesium Increased level Serum potassium Decreased level Serum uric acid Decreased level Serum thyroxine Decreased level Serum cortisol Decreased level AM level Serum parathyroid hormone Increased level due to adenoma Serum calcium Increased level due to increased parathyroid hormone level Serum phosphorus Decreased level due to increased parathyroid hormone level

Lithium Contraindicated for patients with • Vomiting, diarrhea, severe disability, or dehydration • Cardiovascular disease • Renal damage • Pregnancy
LITHIUM Cautionary concerns include • Brain damage • Salt-restricted diet or diuretics • Elderly

혈중 농도에 따른 리툼의 중독증상 독성의 심한 정도 경도에서 중등도 독성 중등도에서 고도 독성 리툼농도 1. 5 -2. 0 m. Eq/L 2. 0 -2. 5 m. Eq/L >2. 5 m. Eq/L 위장관 증상 Vomiting Anorexia abdominal pain Persistent Nausea and Vomiting Dryness of mouth 신경계 증상 Ataxia Blurred vision Generalized convulsions Dizziness Muscle fasciculation Oligouria Failure slurred speech Clonic limb movement Death Nystagmus Convulsions Lethargy or Excitement Delirium Muscle weakness Syncope EEG change Circulatory failure and Renal

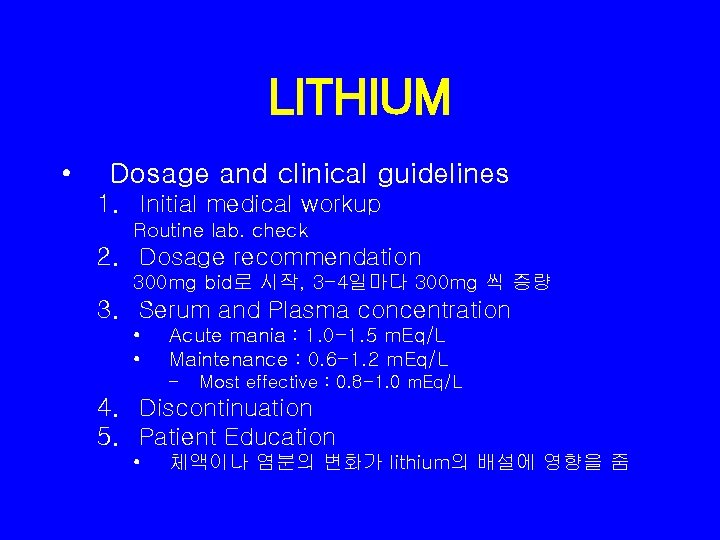
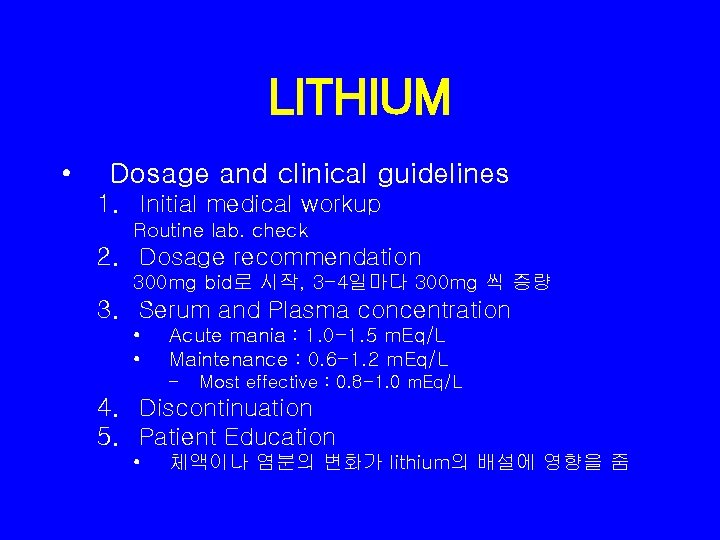
LITHIUM • Dosage and clinical guidelines 1. Initial medical workup Routine lab. check 2. Dosage recommendation 300 mg bid로 시작, 3 -4일마다 300 mg 씩 증량 3. Serum and Plasma concentration • • Acute mania : 1. 0 -1. 5 m. Eq/L Maintenance : 0. 6 -1. 2 m. Eq/L – Most effective : 0. 8 -1. 0 m. Eq/L 4. Discontinuation 5. Patient Education • 체액이나 염분의 변화가 lithium의 배설에 영향을 줌
Valproate • Chemistry – Simple, branched chain, carboxyl ndipropylacetic acid
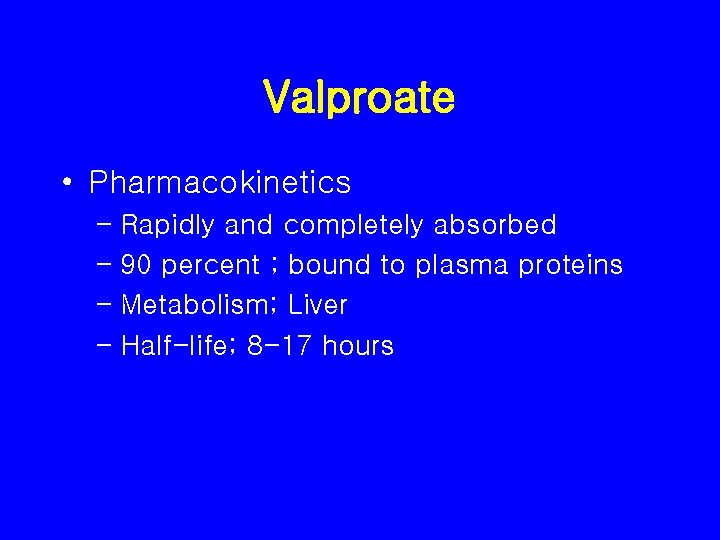
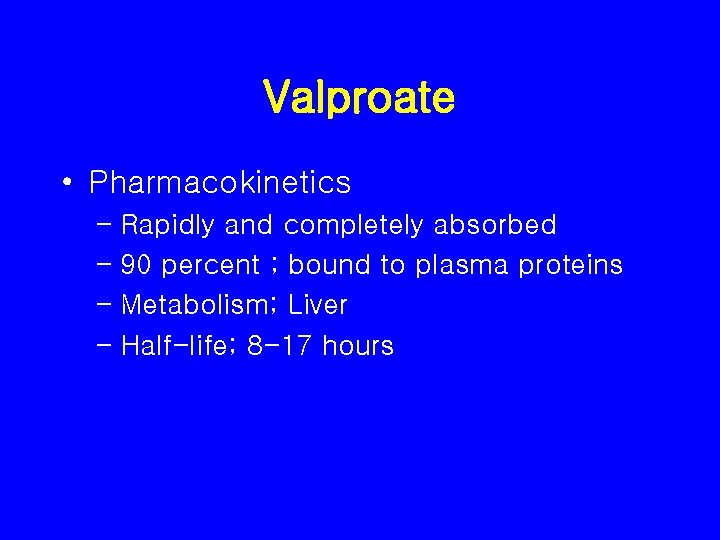
Valproate • Pharmacokinetics – Rapidly and completely absorbed – 90 percent ; bound to plasma proteins – Metabolism; Liver – Half-life; 8 -17 hours
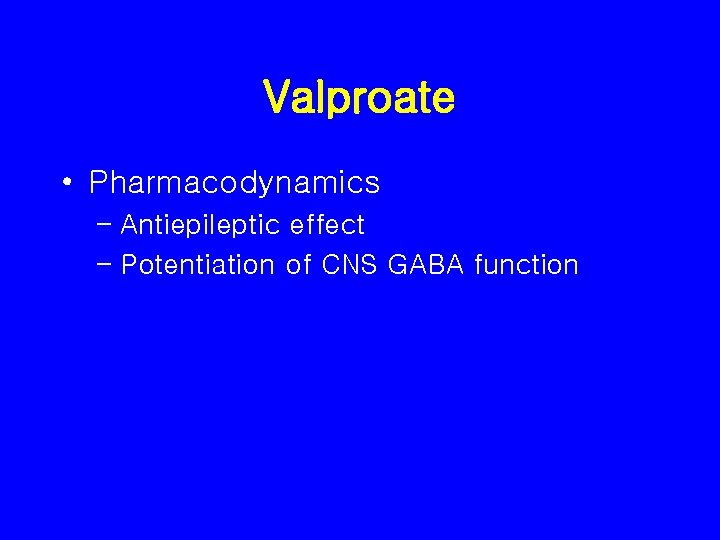
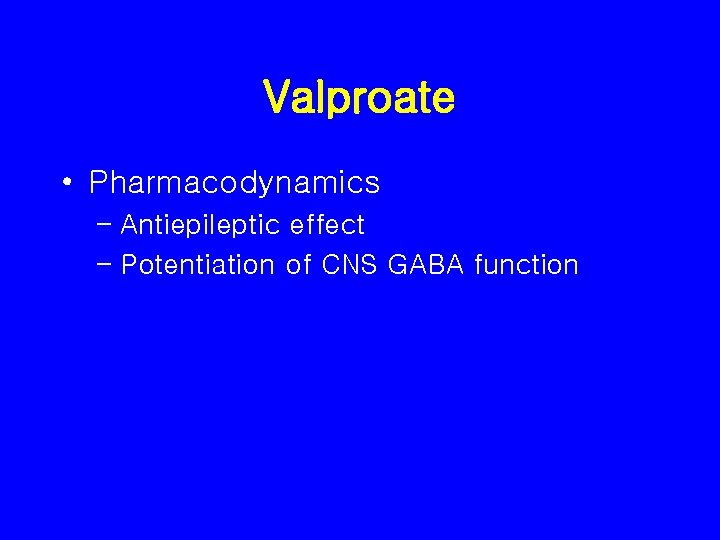
Valproate • Pharmacodynamics – Antiepileptic effect – Potentiation of CNS GABA function
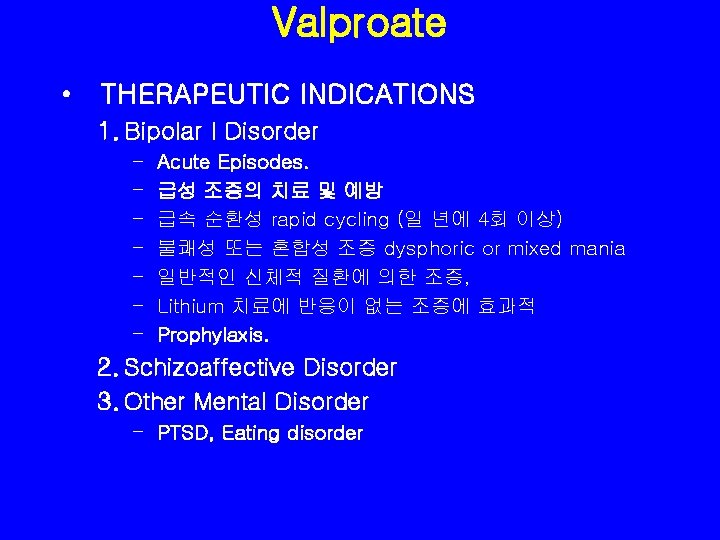
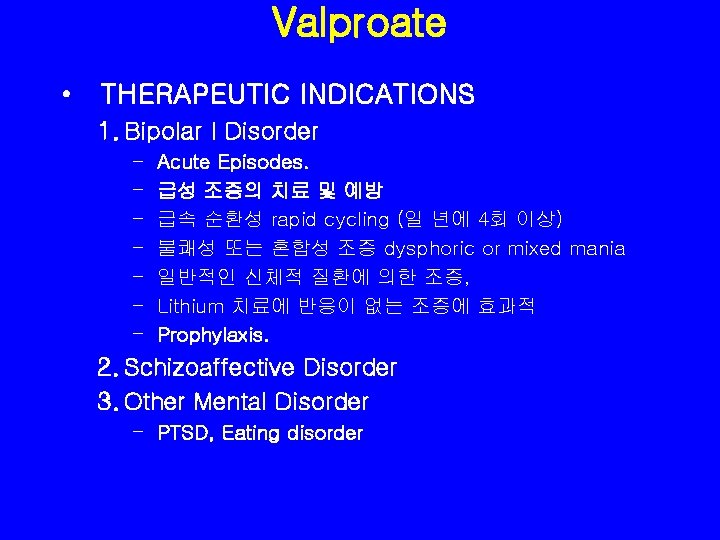
Valproate • THERAPEUTIC INDICATIONS 1. Bipolar I Disorder – – – – Acute Episodes. 급성 조증의 치료 및 예방 급속 순환성 rapid cycling (일 년에 4회 이상) 불쾌성 또는 혼합성 조증 dysphoric or mixed mania 일반적인 신체적 질환에 의한 조증, Lithium 치료에 반응이 없는 조증에 효과적 Prophylaxis. 2. Schizoaffective Disorder 3. Other Mental Disorder – PTSD, Eating disorder
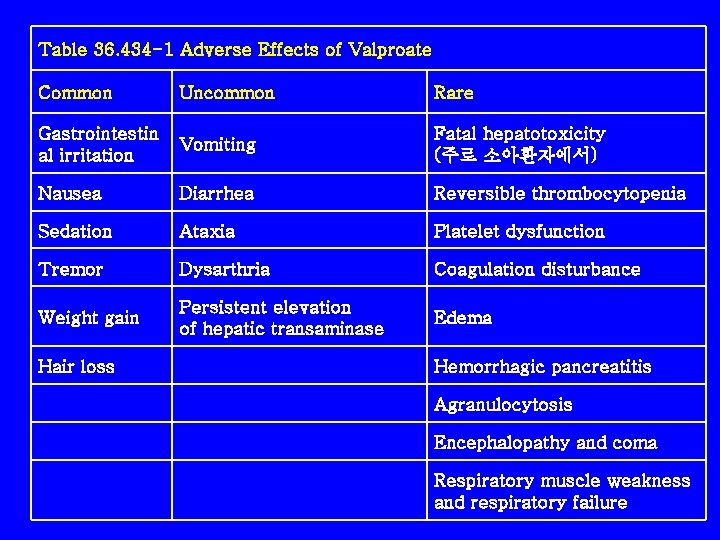
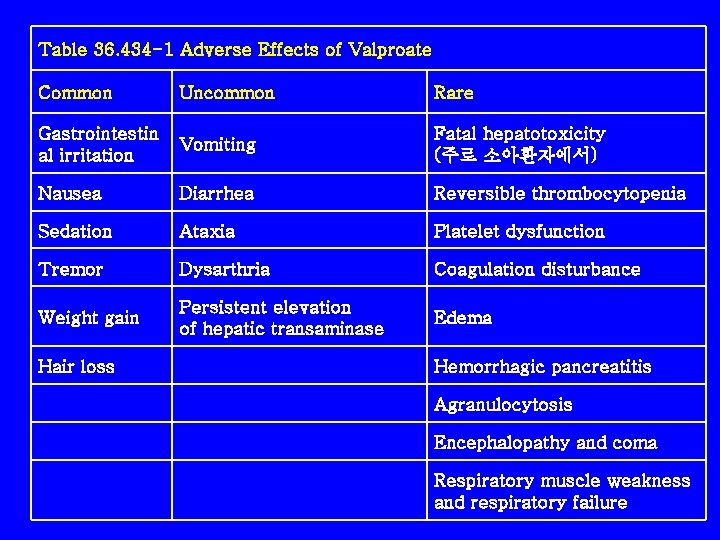
Table 36. 434 -1 Adverse Effects of Valproate Common Uncommon Rare Gastrointestin al irritation Vomiting Fatal hepatotoxicity (주로 소아환자에서) Nausea Diarrhea Reversible thrombocytopenia Sedation Ataxia Platelet dysfunction Tremor Dysarthria Coagulation disturbance Weight gain Persistent elevation of hepatic transaminase Edema Hair loss Hemorrhagic pancreatitis Agranulocytosis Encephalopathy and coma Respiratory muscle weakness and respiratory failure
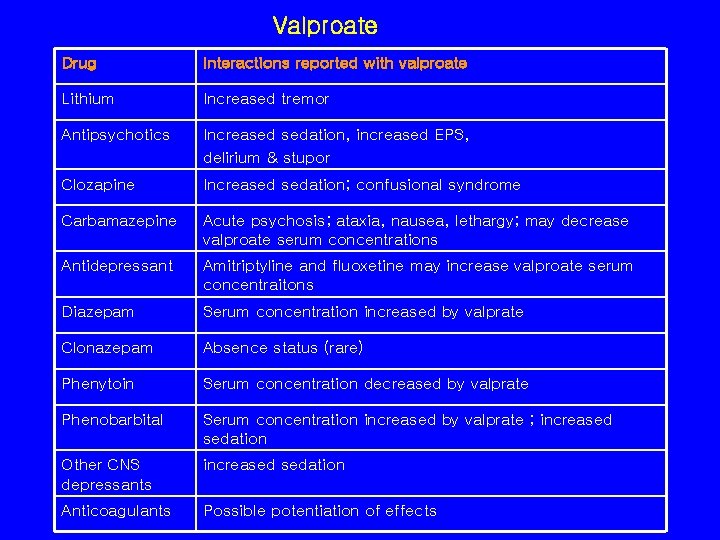
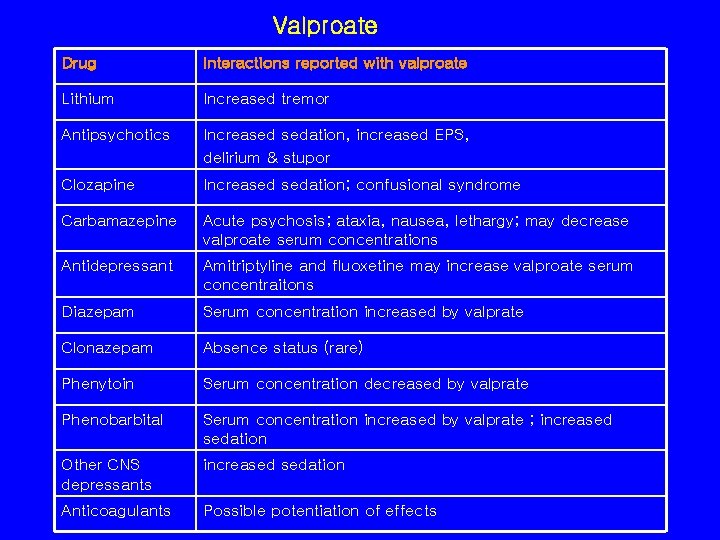
Valproate Drug Interactions reported with valproate Lithium Increased tremor Antipsychotics Increased sedation, increased EPS, delirium & stupor Clozapine Increased sedation; confusional syndrome Carbamazepine Acute psychosis; ataxia, nausea, lethargy; may decrease valproate serum concentrations Antidepressant Amitriptyline and fluoxetine may increase valproate serum concentraitons Diazepam Serum concentration increased by valprate Clonazepam Absence status (rare) Phenytoin Serum concentration decreased by valprate Phenobarbital Serum concentration increased by valprate ; increased sedation Other CNS depressants increased sedation Anticoagulants Possible potentiation of effects
Valproate • DOSAGE AND ADMINISTRATION – dose: 1 일 250 mg으로 시작, 3 -6일 뒤에 250 mg tid or 20 mg/kg – Therapeutic plasma levels: 50 -100 ng/m. L – Onset of action; 5 -15 days

Carbamazepine
Carbamazepine-History • • Antiepileptic properties (1963) Trigeminal neuralgia ; FDA, March 1968 Temporal lobe epilepsy ; FDA, August 1974 Seizure disorders – Complex partial seizures – Generalized seizures thought to arise from the temporal lobe and limbic systems • Paroxysmal pain syndromes • Bipolar Disorder
Carbamazepine • Chemistry – 5 -H-dibenz(b, f)azepine-5 -carboxamide – Imipramine의 tricyclic structure와 유사.
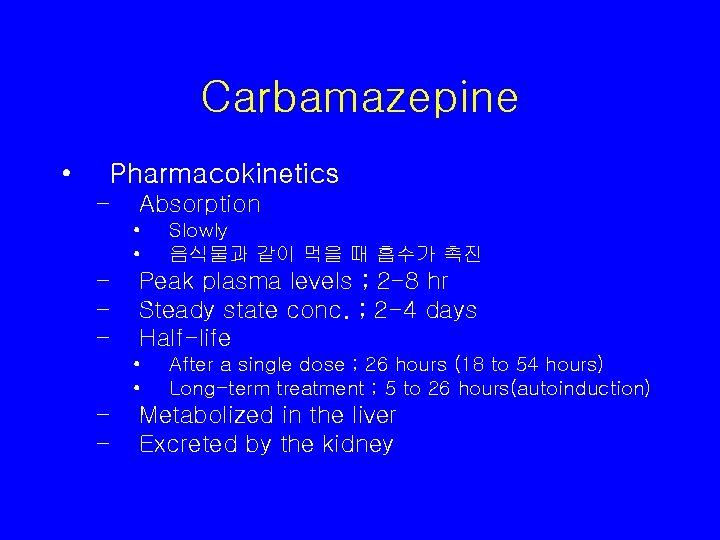
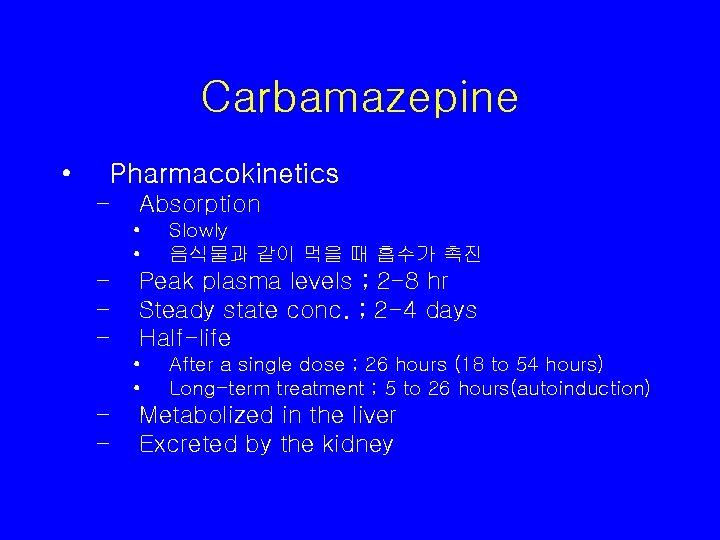
Carbamazepine • Pharmacokinetics – Absorption • • – – – Peak plasma levels ; 2 -8 hr Steady state conc. ; 2 -4 days Half-life • • – – Slowly 음식물과 같이 먹을 때 흡수가 촉진 After a single dose ; 26 hours (18 to 54 hours) Long-term treatment ; 5 to 26 hours(autoinduction) Metabolized in the liver Excreted by the kidney
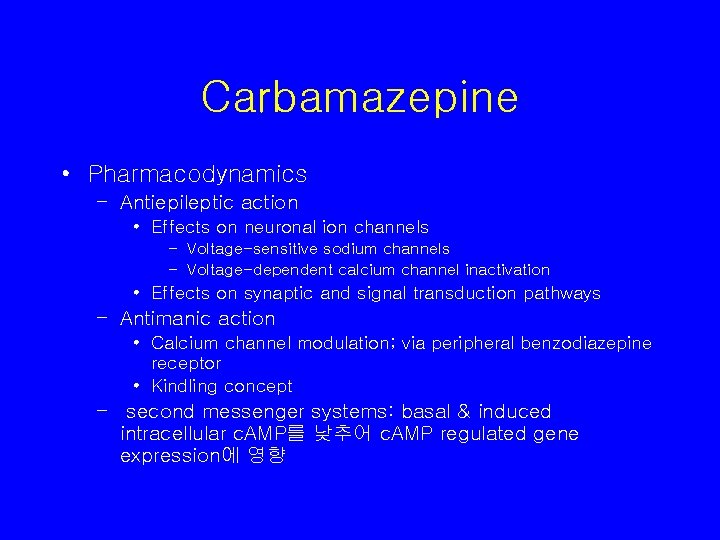
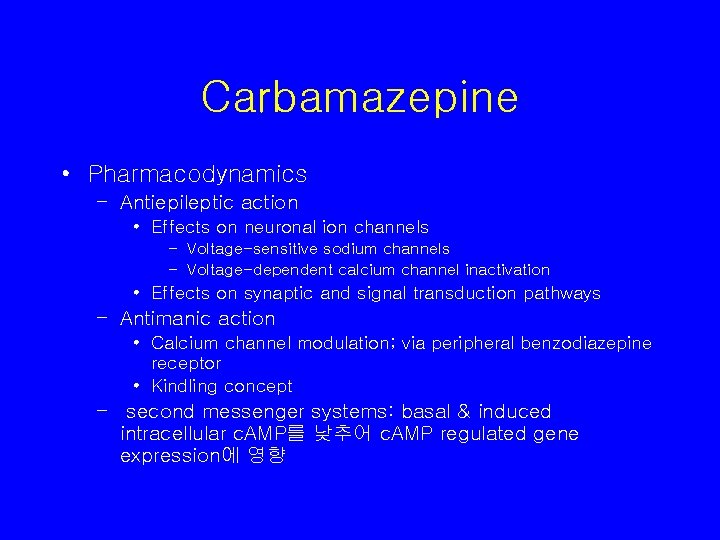
Carbamazepine • Pharmacodynamics – Antiepileptic action • Effects on neuronal ion channels – Voltage-sensitive sodium channels – Voltage-dependent calcium channel inactivation • Effects on synaptic and signal transduction pathways – Antimanic action • Calcium channel modulation; via peripheral benzodiazepine receptor • Kindling concept – second messenger systems: basal & induced intracellular c. AMP를 낮추어 c. AMP regulated gene expression에 영향
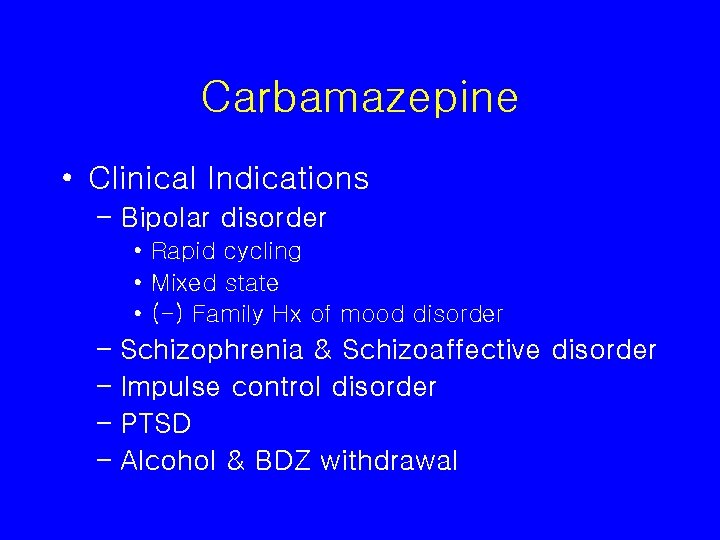
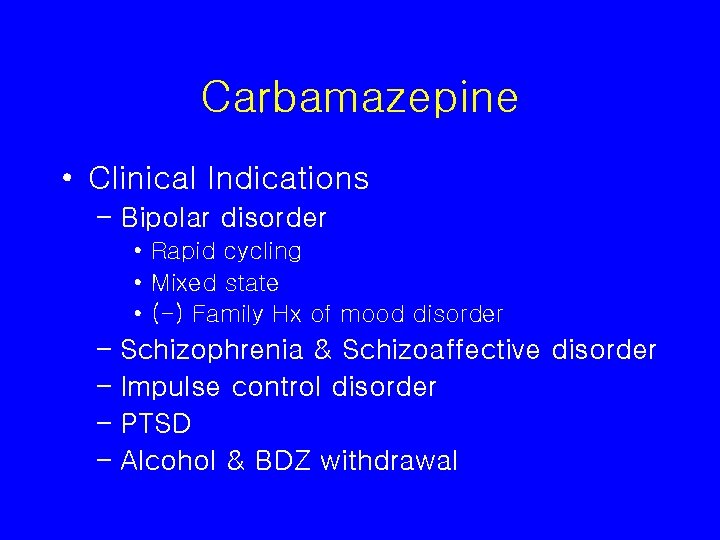
Carbamazepine • Clinical Indications – Bipolar disorder • Rapid cycling • Mixed state • (-) Family Hx of mood disorder – Schizophrenia & Schizoaffective disorder – Impulse control disorder – PTSD – Alcohol & BDZ withdrawal
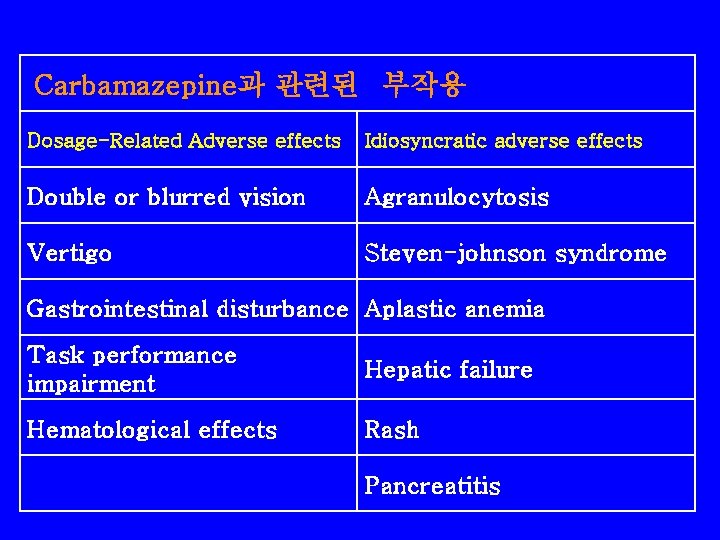
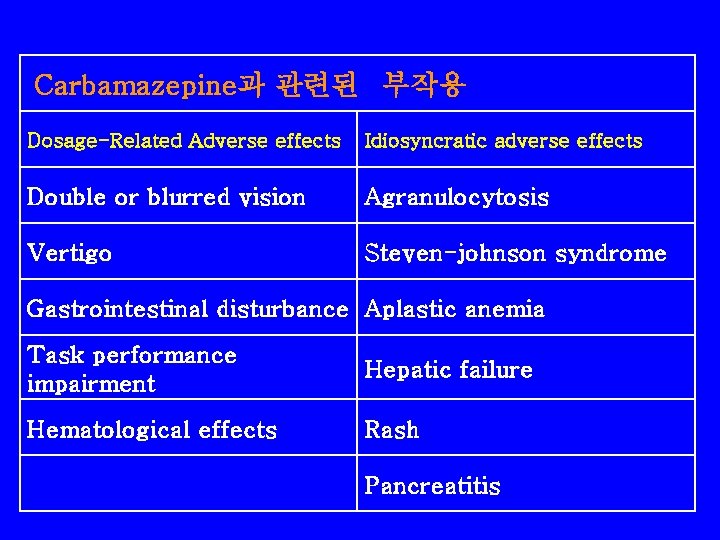
Carbamazepine과 관련된 부작용 Dosage-Related Adverse effects Idiosyncratic adverse effects Double or blurred vision Agranulocytosis Vertigo Steven-johnson syndrome Gastrointestinal disturbance Aplastic anemia Task performance impairment Hepatic failure Hematological effects Rash Pancreatitis
Carbamazepine • Blood dyscrasias – – – Mild leukopenia ; 1 -2 % Agraulocytosis ; 1/125, 000 Inhibitory action at the level of colony-stimulating factor Dosage can be reduced or discontinued CBC • Baseline • Weekly to stability • 6 to 12 months thereafter – Fever, sore throat, rash, petechia, bruising, easy bleeding – immediate medical evaluation
Carbamazepine • Hepatitis – Mild elevation in liver function tests – More persistent enzyme elevation • Rare • Drug discontinuation – Monitored at 6 -to 12 -months intervals
Carbamazepine • Exfoliative dermatitis – Carbamazepine-induced rashes • 12 -16% • Within the first 3 weeks • Benign and self-limiting – Serious adverse skin reaction ; 3 cases per million users per week • Exfoliative dermatitis, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis – Discontinuing carbamazepine with the onset of rash – Reexposed ; in most cases the rash returns, usually with a rapid onset – Crude relative risk of severe adverse cutaneous reactions • Similar for carbamazepine and valproic acid ; short peroids(<2 months) • Higher for carbamazepine ; longer periods
Carbamazepine • Gastrointestinal effects – Most common – Nausea, vomiting, gastric distress, constipation, diarrhea, anorexia
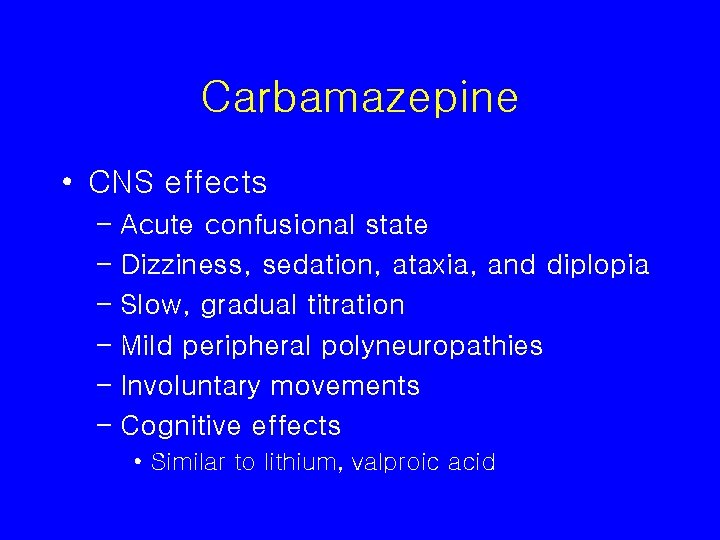
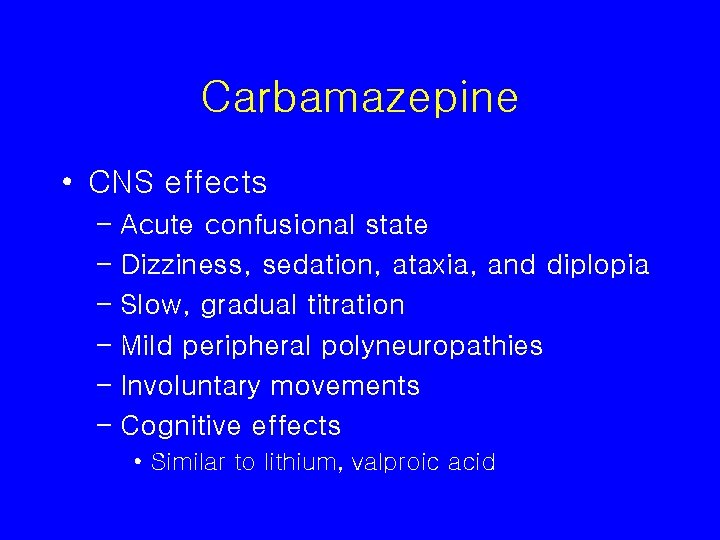
Carbamazepine • CNS effects – Acute confusional state – Dizziness, sedation, ataxia, and diplopia – Slow, gradual titration – Mild peripheral polyneuropathies – Involuntary movements – Cognitive effects • Similar to lithium, valproic acid
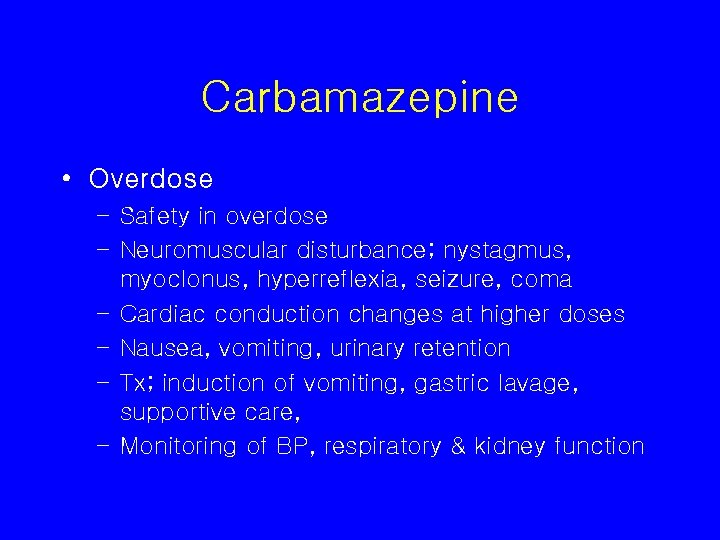
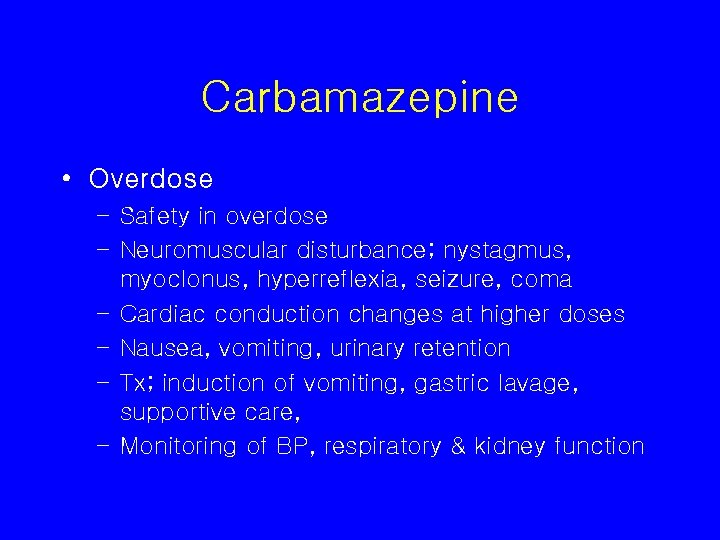
Carbamazepine • Overdose – Safety in overdose – Neuromuscular disturbance; nystagmus, myoclonus, hyperreflexia, seizure, coma – Cardiac conduction changes at higher doses – Nausea, vomiting, urinary retention – Tx; induction of vomiting, gastric lavage, supportive care, – Monitoring of BP, respiratory & kidney function
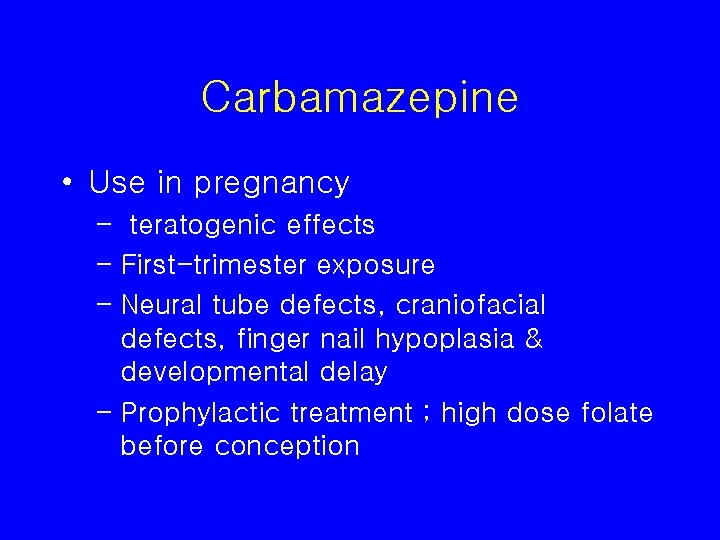
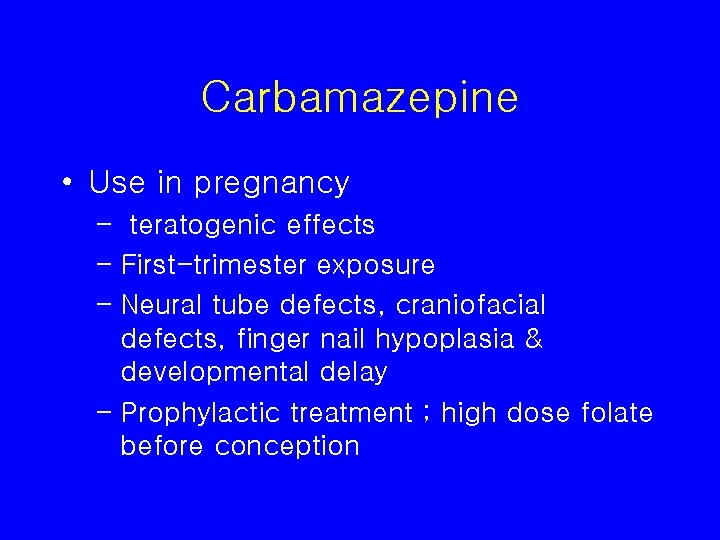
Carbamazepine • Use in pregnancy – teratogenic effects – First-trimester exposure – Neural tube defects, craniofacial defects, finger nail hypoplasia & developmental delay – Prophylactic treatment ; high dose folate before conception
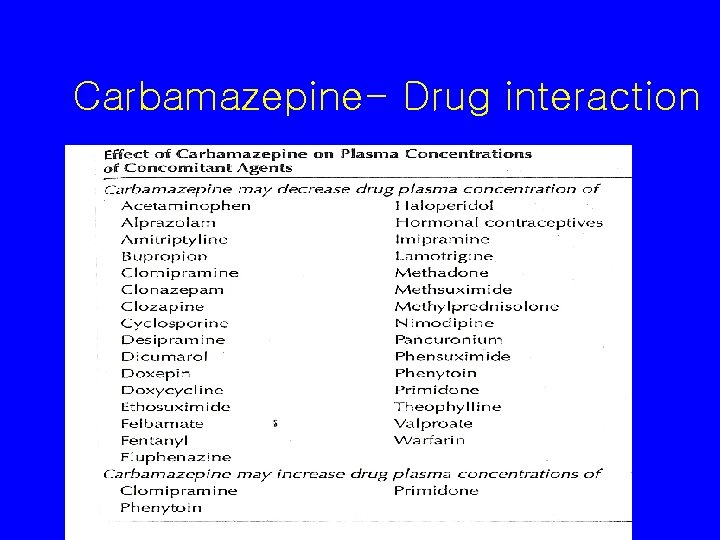
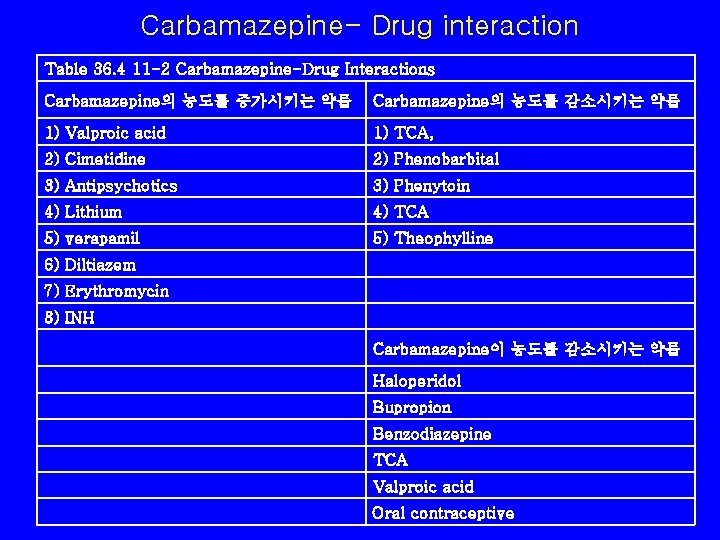
Carbamazepine- Drug interaction
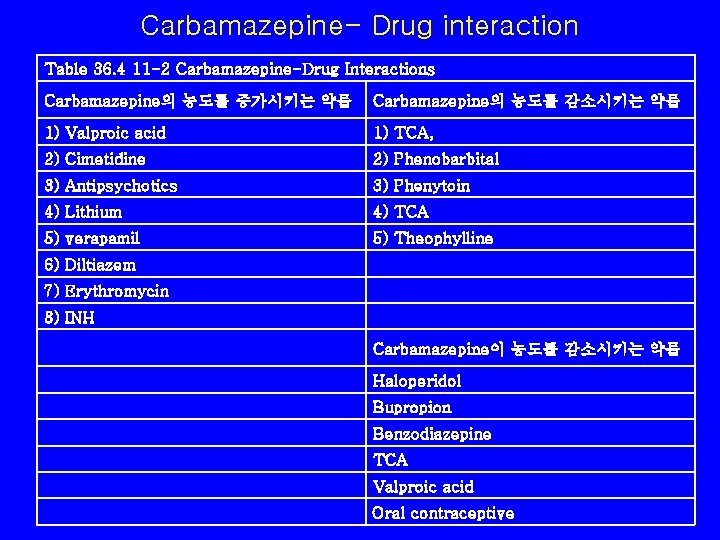
Carbamazepine- Drug interaction Table 36. 4 11 -2 Carbamazepine-Drug Interactions Carbamazepine의 농도를 증가시키는 약물 Carbamazepine의 농도를 감소시키는 약물 1) Valproic acid 1) TCA, 2) Cimetidine 2) Phenobarbital 3) Antipsychotics 3) Phenytoin 4) Lithium 4) TCA 5) verapamil 5) Theophylline 6) Diltiazem 7) Erythromycin 8) INH Carbamazepine이 농도를 감소시키는 약물 Haloperidol Bupropion Benzodiazepine TCA Valproic acid Oral contraceptive
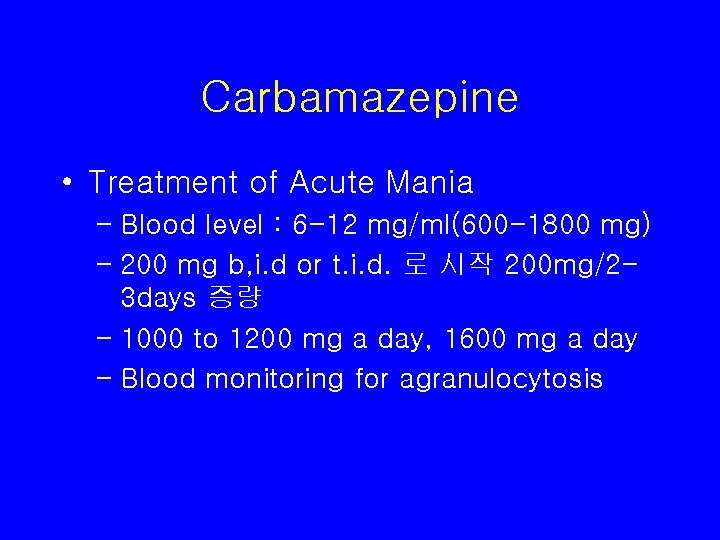
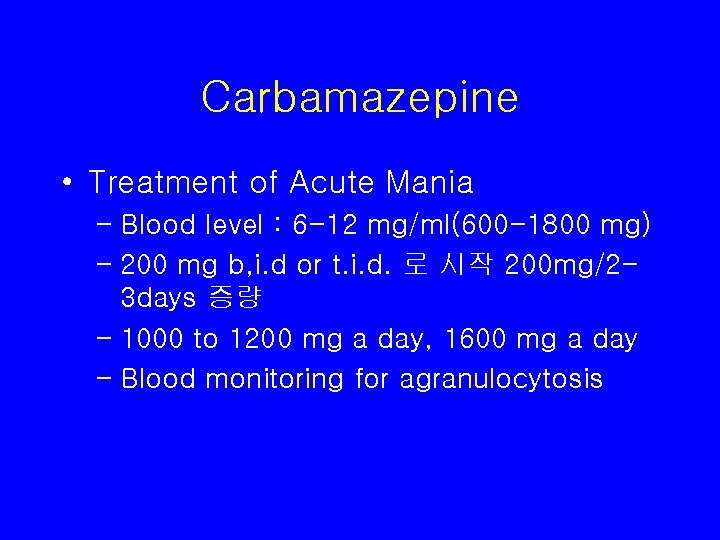
Carbamazepine • Treatment of Acute Mania – Blood level : 6 -12 mg/ml(600 -1800 mg) – 200 mg b, i. d or t. i. d. 로 시작 200 mg/23 days 증량 – 1000 to 1200 mg a day, 1600 mg a day – Blood monitoring for agranulocytosis


New anticonvulsants • Lamotrigine • Topiramate • Gabapentin
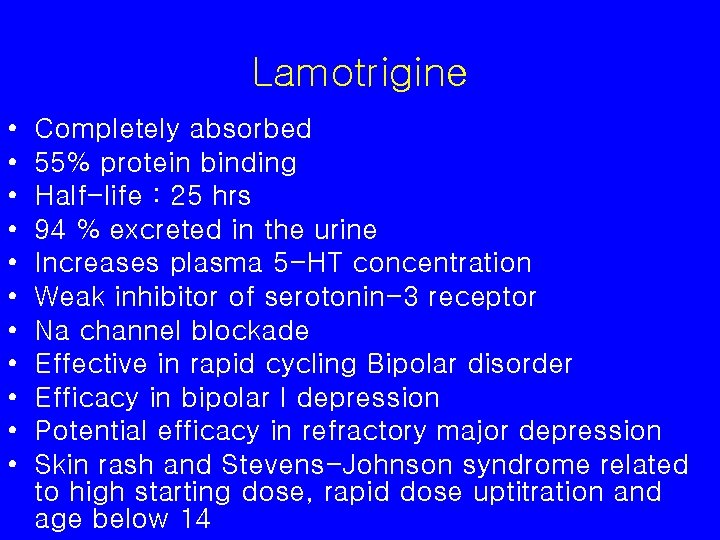
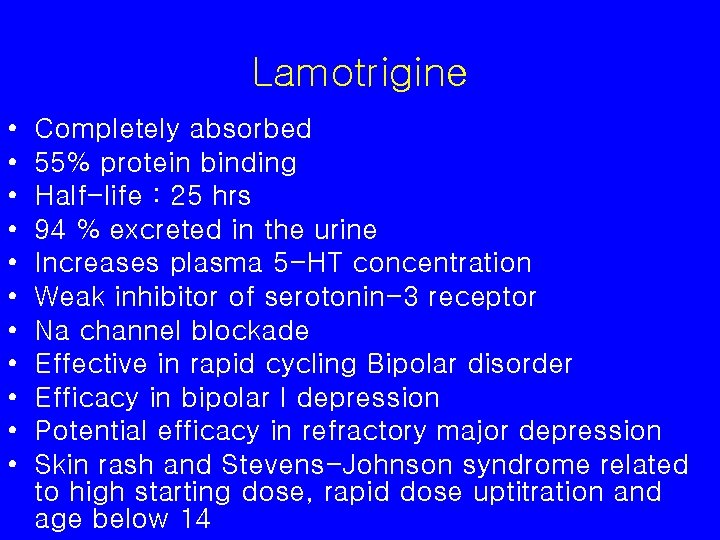
Lamotrigine • • • Completely absorbed 55% protein binding Half-life : 25 hrs 94 % excreted in the urine Increases plasma 5 -HT concentration Weak inhibitor of serotonin-3 receptor Na channel blockade Effective in rapid cycling Bipolar disorder Efficacy in bipolar I depression Potential efficacy in refractory major depression Skin rash and Stevens-Johnson syndrome related to high starting dose, rapid dose uptitration and age below 14
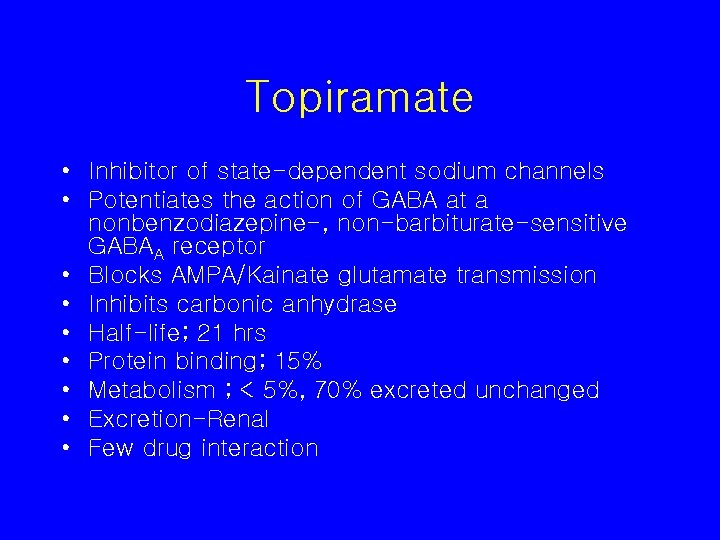
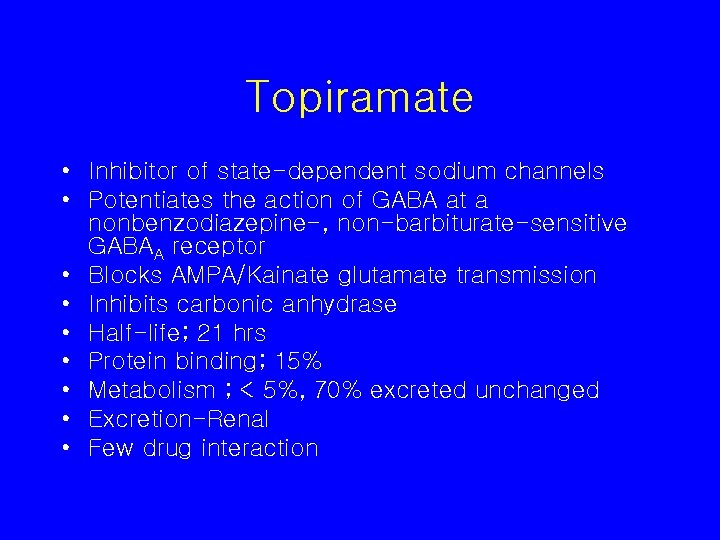
Topiramate • Inhibitor of state-dependent sodium channels • Potentiates the action of GABA at a nonbenzodiazepine-, non-barbiturate-sensitive GABAA receptor • Blocks AMPA/Kainate glutamate transmission • Inhibits carbonic anhydrase • Half-life; 21 hrs • Protein binding; 15% • Metabolism ; < 5%, 70% excreted unchanged • Excretion-Renal • Few drug interaction



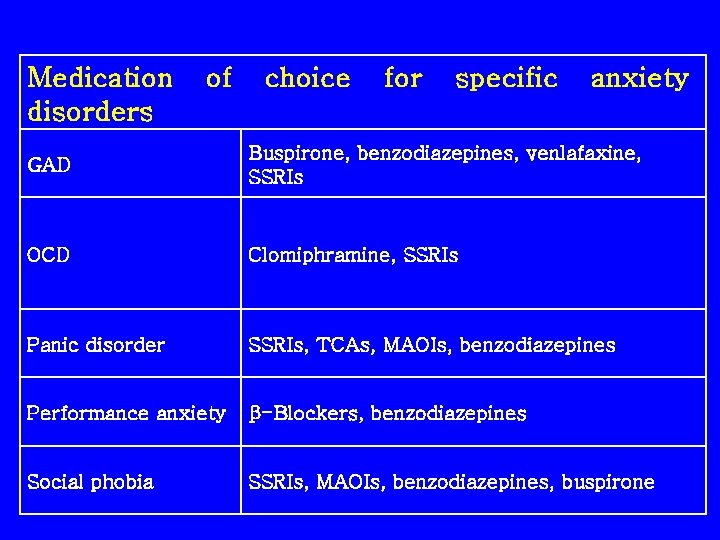
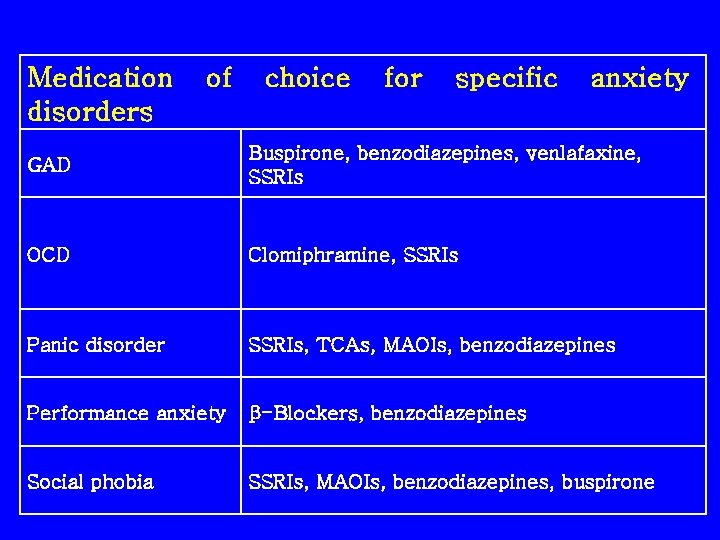
Medication disorders of choice for specific anxiety GAD Buspirone, benzodiazepines, venlafaxine, SSRIs OCD Clomiphramine, SSRIs Panic disorder SSRIs, TCAs, MAOIs, benzodiazepines Performance anxiety β-Blockers, benzodiazepines Social phobia SSRIs, MAOIs, benzodiazepines, buspirone
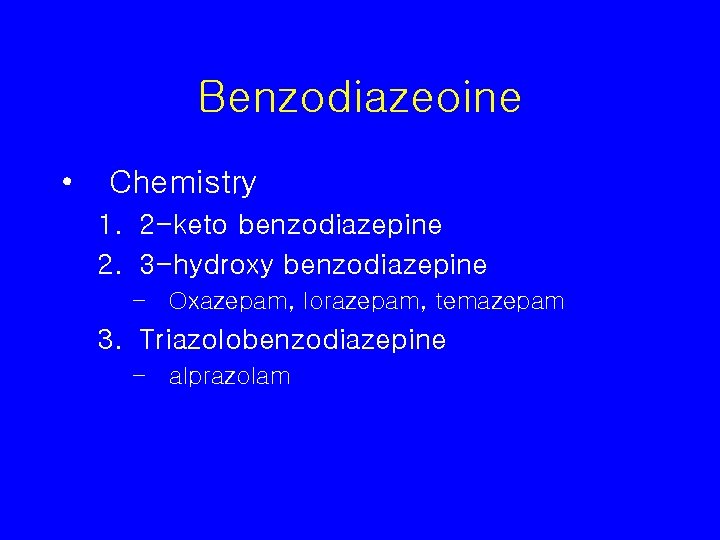
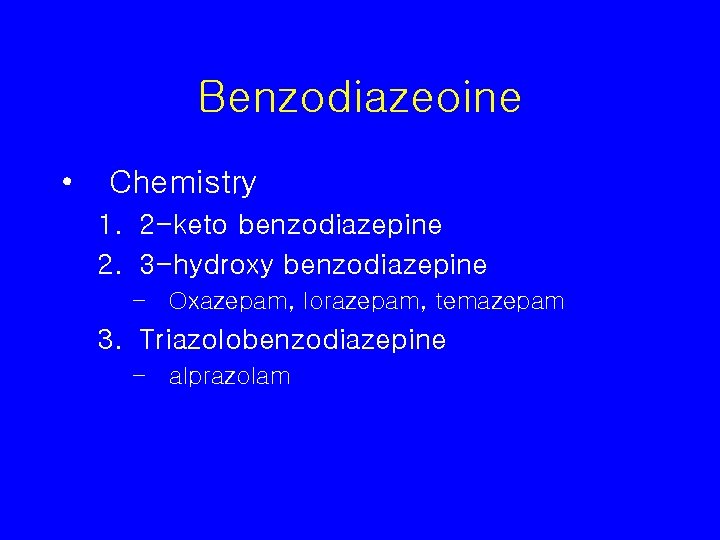
Benzodiazeoine • Chemistry 1. 2 -keto benzodiazepine 2. 3 -hydroxy benzodiazepine – Oxazepam, lorazepam, temazepam 3. Triazolobenzodiazepine – alprazolam
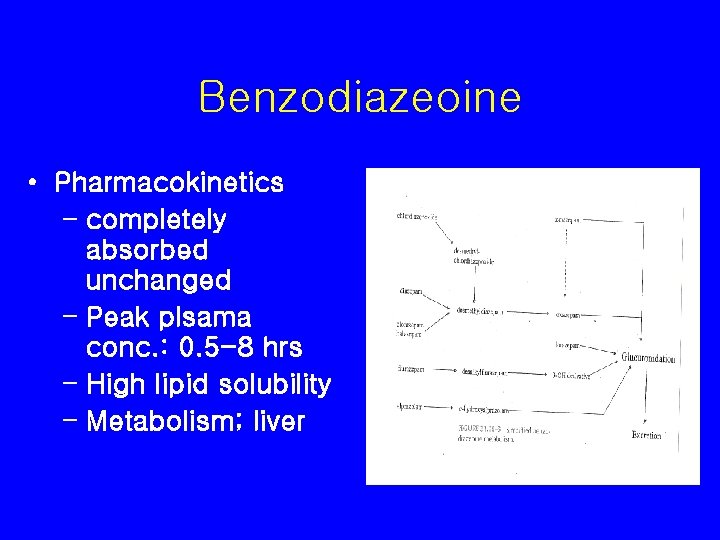
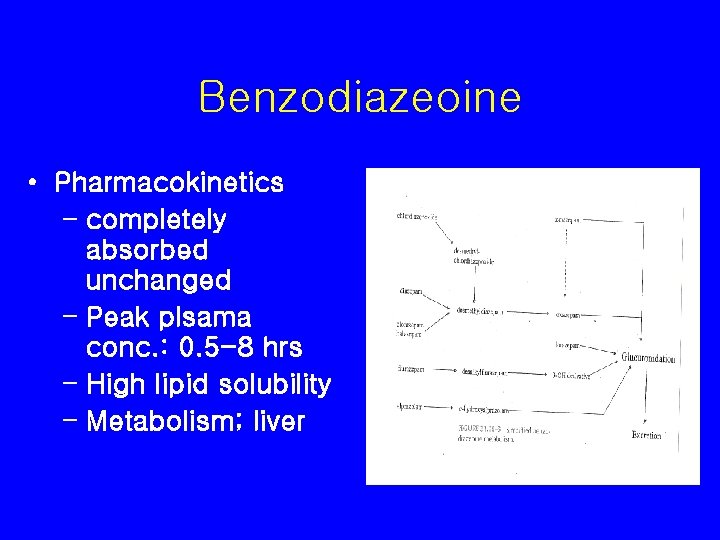
Benzodiazeoine • Pharmacokinetics – completely absorbed unchanged – Peak plsama conc. : 0. 5 -8 hrs – High lipid solubility – Metabolism; liver
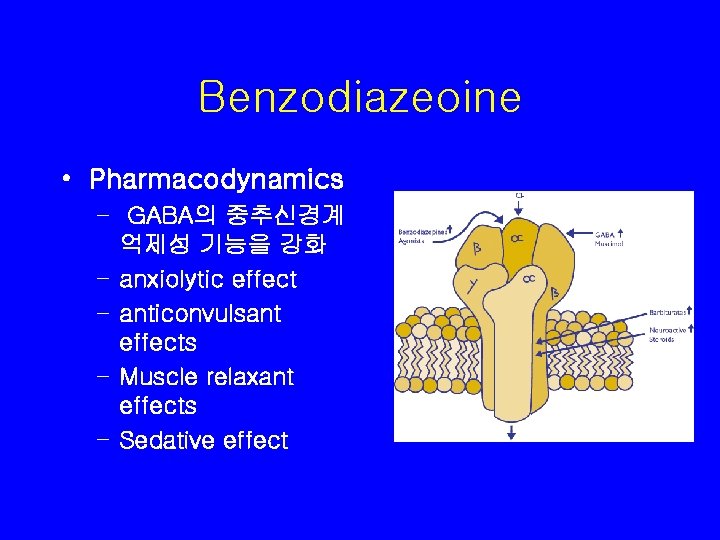
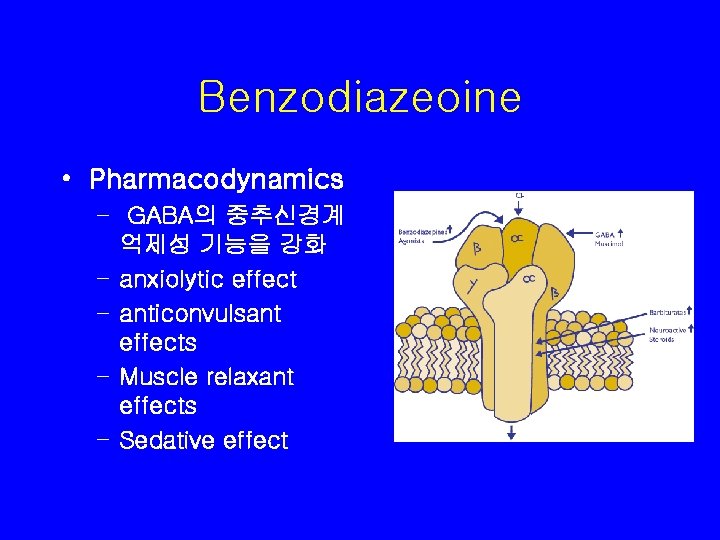
Benzodiazeoine • Pharmacodynamics – GABA의 중추신경계 억제성 기능을 강화 – anxiolytic effect – anticonvulsant effects – Muscle relaxant effects – Sedative effect
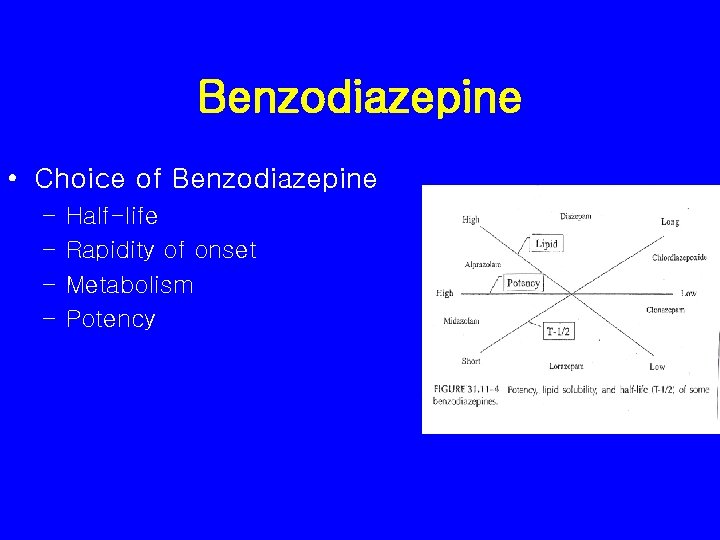
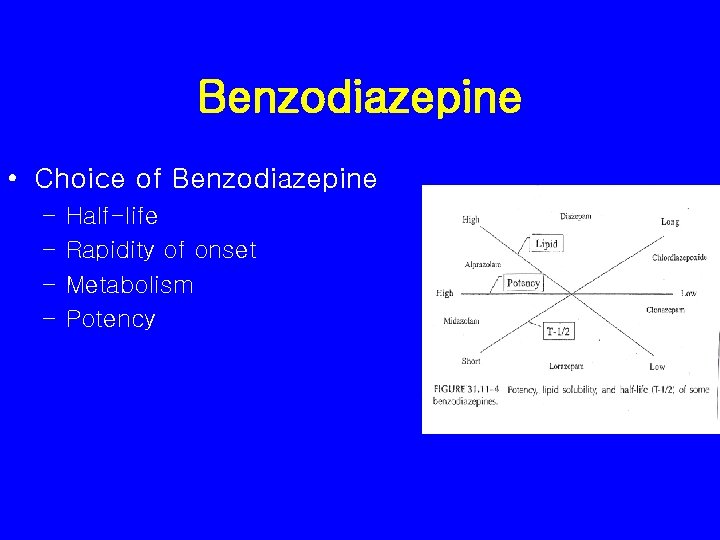
Benzodiazepine • Choice of Benzodiazepine – – Half-life Rapidity of onset Metabolism Potency
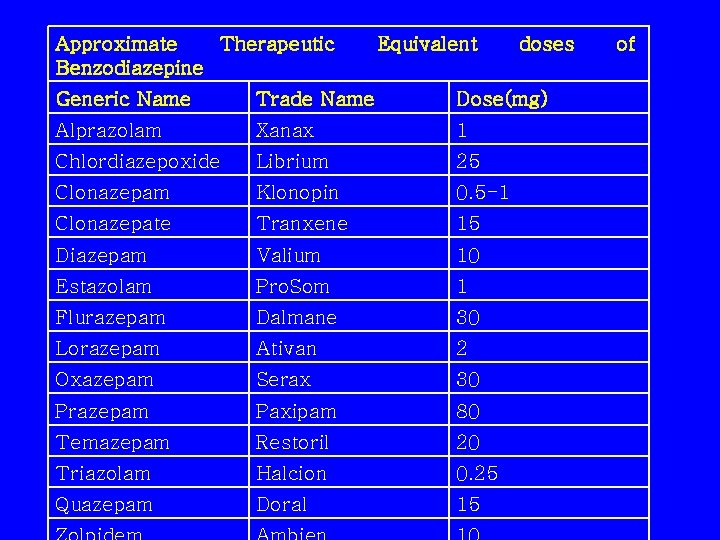
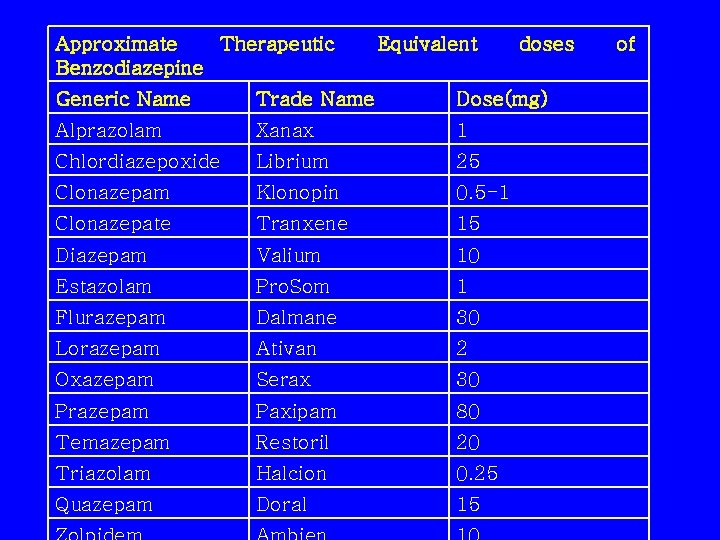
Approximate Therapeutic Benzodiazepine Equivalent doses Generic Name Trade Name Dose(mg) Alprazolam Xanax 1 Chlordiazepoxide Librium 25 Clonazepam Klonopin 0. 5 -1 Clonazepate Tranxene 15 Diazepam Valium 10 Estazolam Pro. Som 1 Flurazepam Dalmane 30 Lorazepam Ativan 2 Oxazepam Serax 30 Prazepam Paxipam 80 Temazepam Restoril 20 Triazolam Halcion 0. 25 Quazepam Doral 15 of
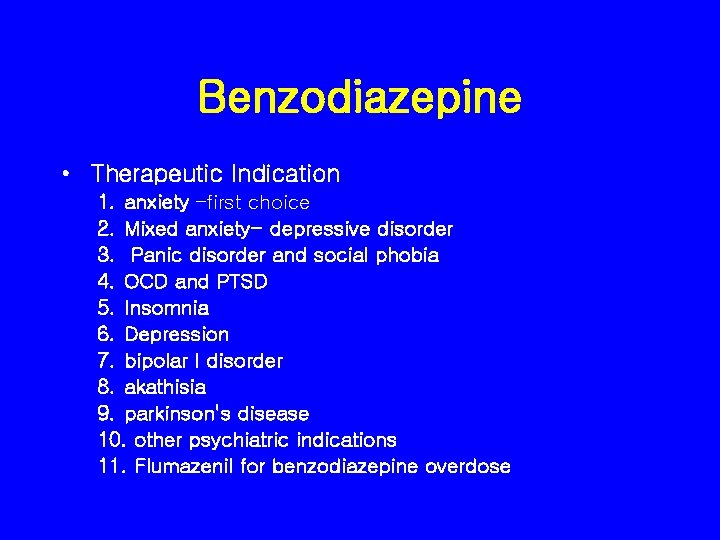
Benzodiazepine • Therapeutic Indication 1. anxiety –first choice 2. Mixed anxiety- depressive disorder 3. Panic disorder and social phobia 4. OCD and PTSD 5. Insomnia 6. Depression 7. bipolar I disorder 8. akathisia 9. parkinson's disease 10. other psychiatric indications 11. Flumazenil for benzodiazepine overdose
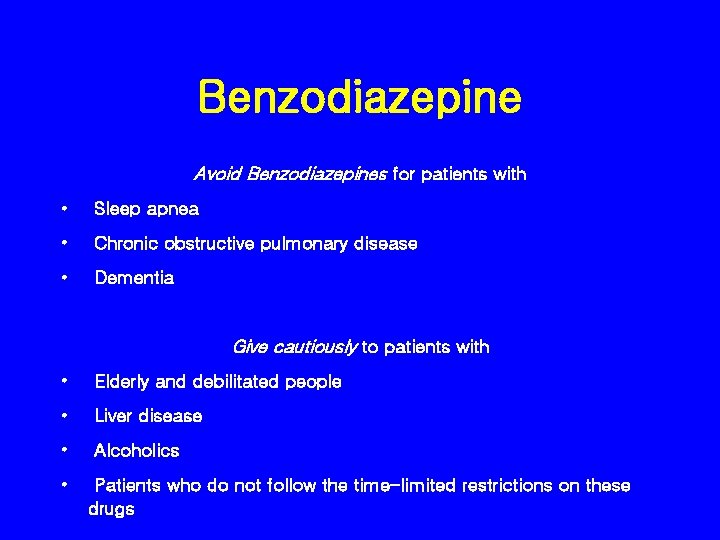
Benzodiazepine Avoid Benzodiazepines for patients with • Sleep apnea • Chronic obstructive pulmonary disease • Dementia Give cautiously to patients with • Elderly and debilitated people • Liver disease • Alcoholics • Patients who do not follow the time-limited restrictions on these drugs
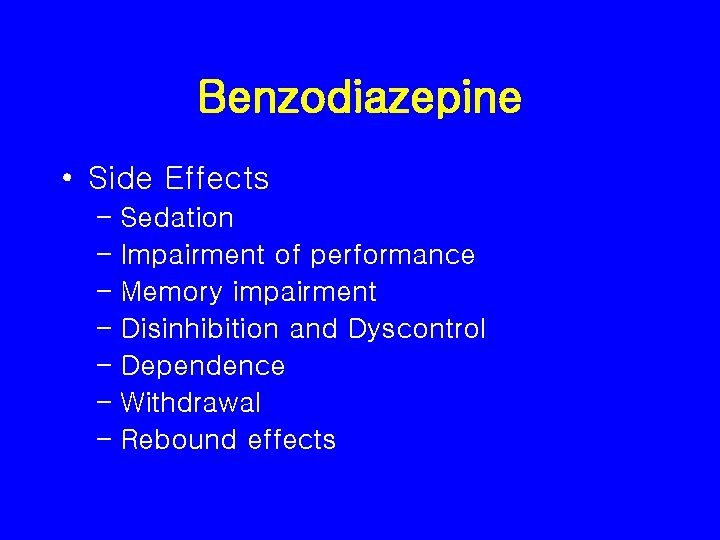
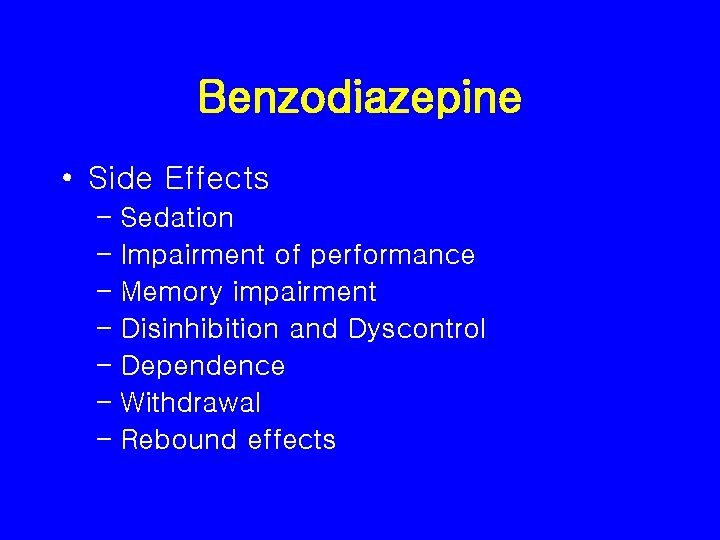
Benzodiazepine • Side Effects – Sedation – Impairment of performance – Memory impairment – Disinhibition and Dyscontrol – Dependence – Withdrawal – Rebound effects
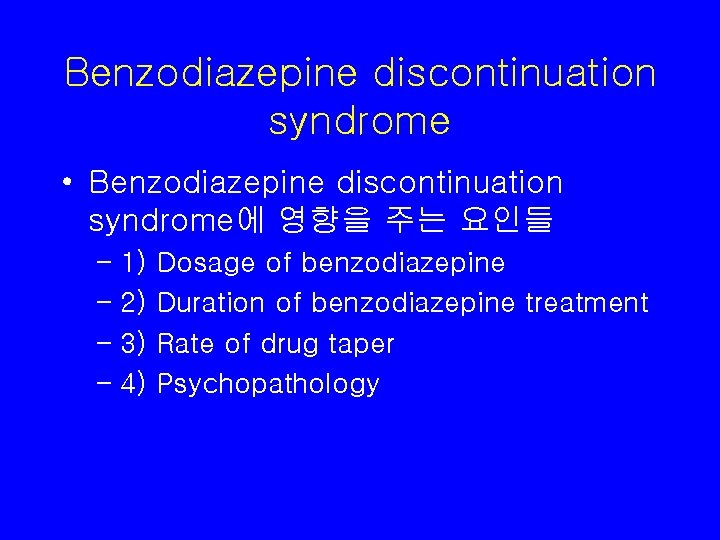
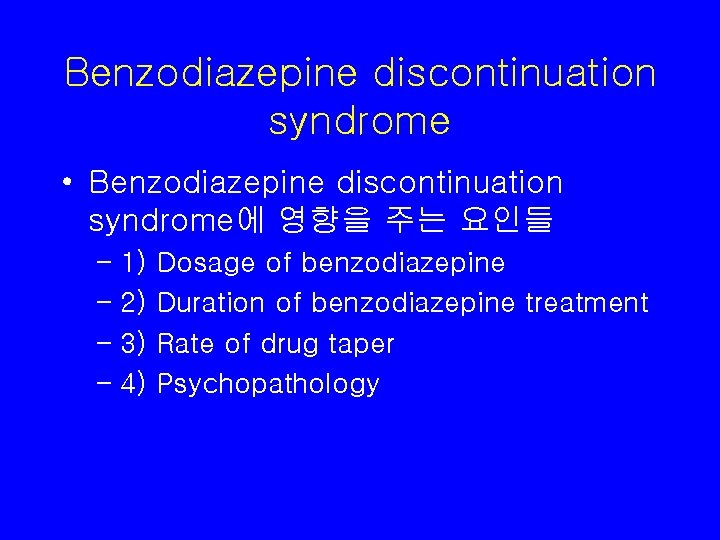
Benzodiazepine discontinuation syndrome • Benzodiazepine discontinuation syndrome에 영향을 주는 요인들 – 1) – 2) – 3) – 4) Dosage of benzodiazepine Duration of benzodiazepine treatment Rate of drug taper Psychopathology
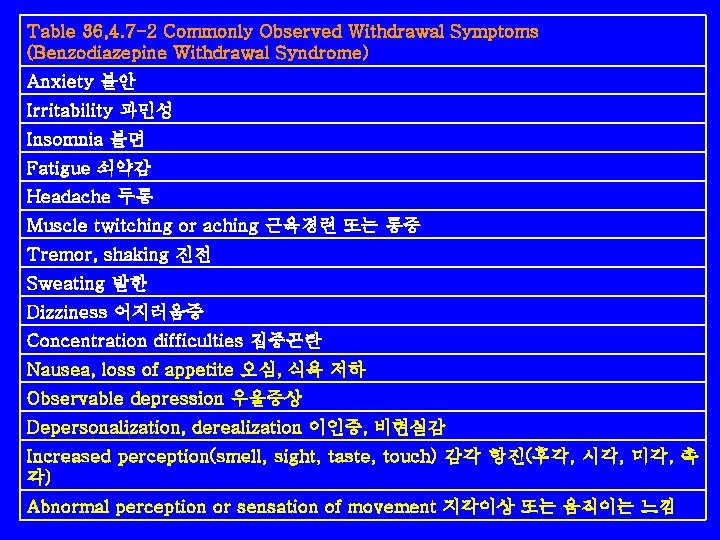
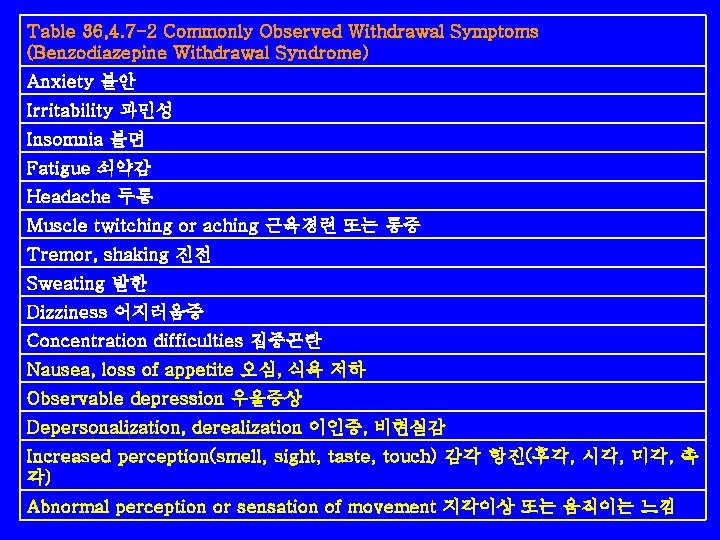
Table 36, 4. 7 -2 Commonly Observed Withdrawal Symptoms (Benzodiazepine Withdrawal Syndrome) Anxiety 불안 Irritability 과민성 Insomnia 불면 Fatigue 쇠약감 Headache 두통 Muscle twitching or aching 근육경련 또는 통증 Tremor, shaking 진전 Sweating 발한 Dizziness 어지러움증 Concentration difficulties 집중곤란 Nausea, loss of appetite 오심, 식욕 저하 Observable depression 우울증상 Depersonalization, derealization 이인증, 비현실감 Increased perception(smell, sight, taste, touch) 감각 항진(후각, 시각, 미각, 촉 각) Abnormal perception or sensation of movement 지각이상 또는 움직이는 느낌
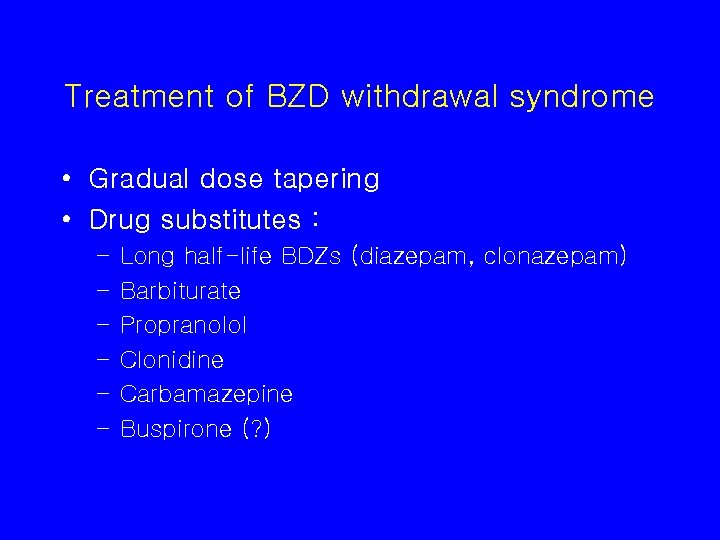
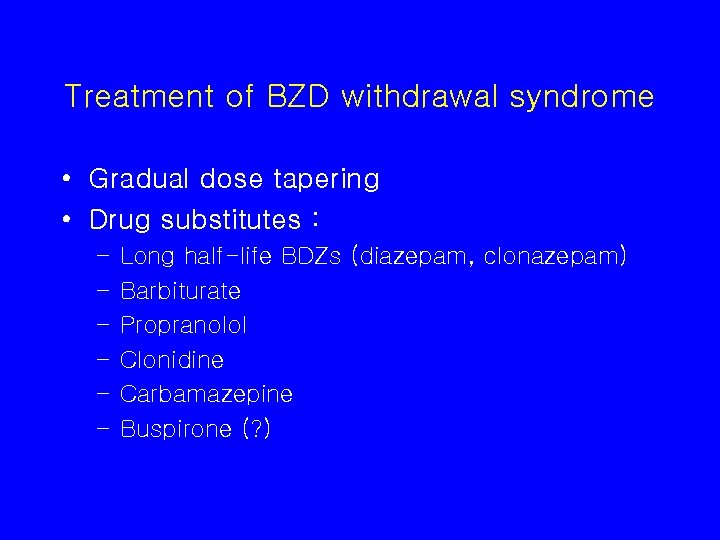
Treatment of BZD withdrawal syndrome • Gradual dose tapering • Drug substitutes : – – – Long half-life BDZs (diazepam, clonazepam) Barbiturate Propranolol Clonidine Carbamazepine Buspirone (? )
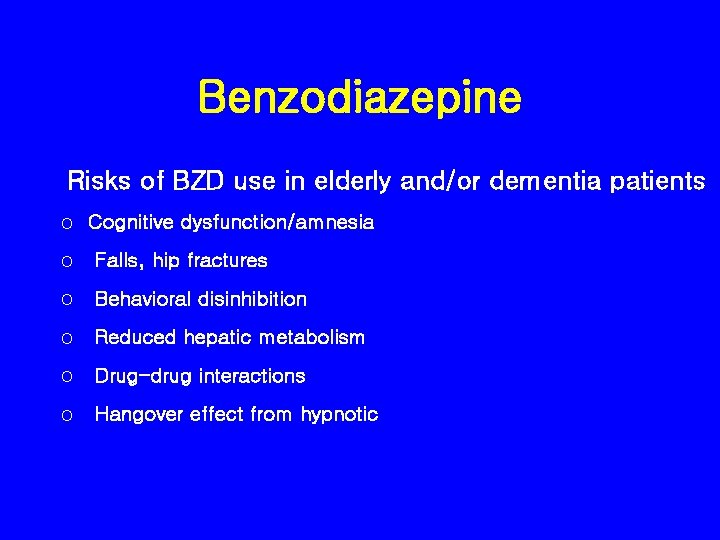
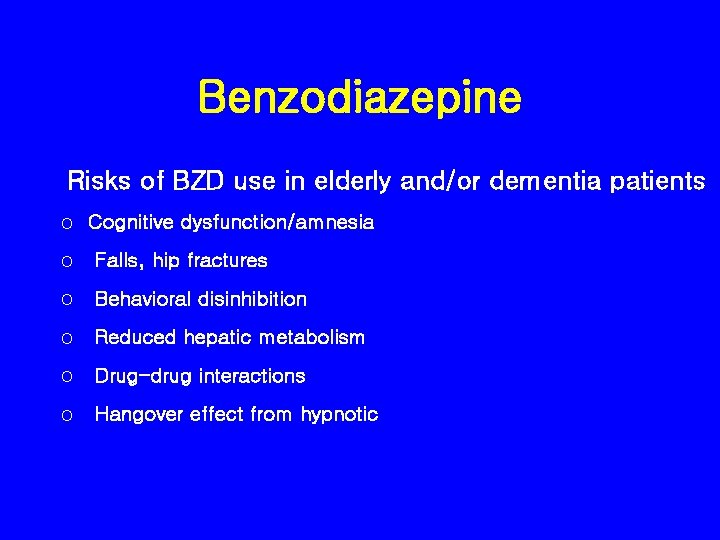
Benzodiazepine Risks of BZD use in elderly and/or dementia patients o Cognitive dysfunction/amnesia o Falls, hip fractures o Behavioral disinhibition o Reduced hepatic metabolism o Drug-drug interactions o Hangover effect from hypnotic

Benzodiazepine • 용량과 용법 dosage and administration – benzodiazepine • anxiety의 medical cause를 먼저 감별하고 low dosage로 시작, • continued Tx에 대해서는 monthly reevaluation 필요 – duration of treatment • chronic anxiety에 있어서의 long period 투여는 효과적이나 controversial – Discontinuation of therapy • 약을 끊을 때 : slow tapering -25%/week • withdrawal symptoms을 monitoring & psychological support가 중요 • carbamazepine을 병용 사용 : 금단증상을 짧게, 잘 견딜 수 있게 해준다. 400 -500 mg/d, • alprazolam의 경우 tapering에 어려움 : clonazepam으로 switch 후 tapering하면 좋음 – choice of drug & potency – drug combination • antipsychotics와 antidepressant 와 병용시 효과적

Pharmacotherapy for General Anxiety Disorders • • Benzodiazepines Buspirone Selective Serotonin Reuptake Inhibitor Other Drugs – TCA, beta-blocker, Venlafaxine, Nefazodone
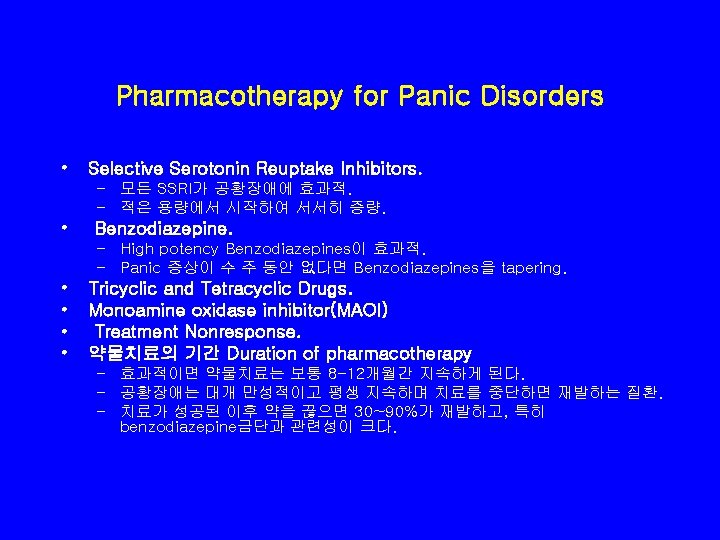
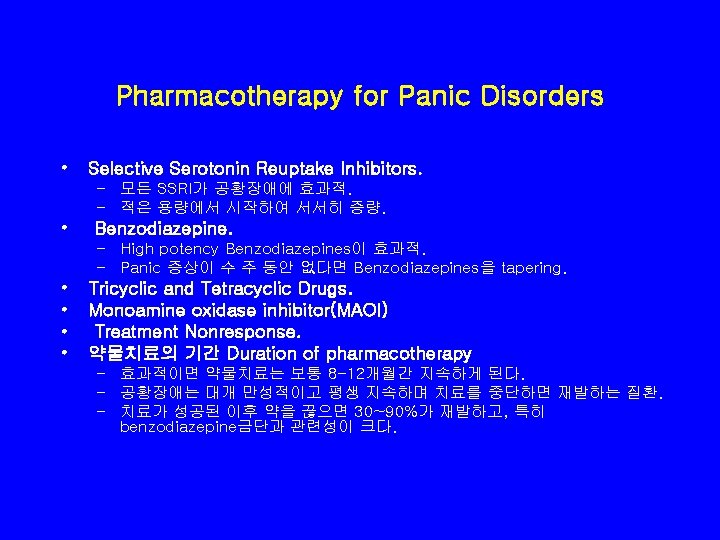
Pharmacotherapy for Panic Disorders • Selective Serotonin Reuptake Inhibitors. – 모든 SSRI가 공황장애에 효과적. – 적은 용량에서 시작하여 서서히 증량. • Benzodiazepine. – High potency Benzodiazepines이 효과적. – Panic 증상이 수 주 동안 없다면 Benzodiazepines을 tapering. • • Tricyclic and Tetracyclic Drugs. Monoamine oxidase inhibitor(MAOI) Treatment Nonresponse. 약물치료의 기간 Duration of pharmacotherapy – 효과적이면 약물치료는 보통 8 -12개월간 지속하게 된다. – 공황장애는 대개 만성적이고 평생 지속하며 치료를 중단하면 재발하는 질환. – 치료가 성공된 이후 약을 끊으면 30~90%가 재발하고, 특히 benzodiazepine금단과 관련성이 크다.
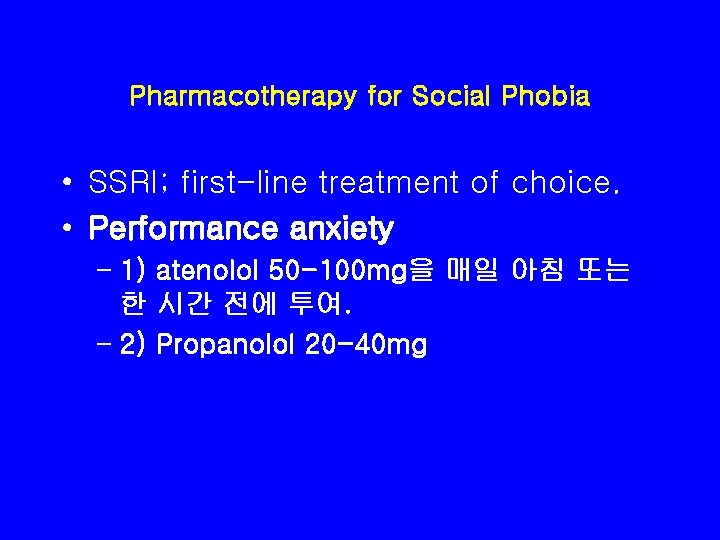
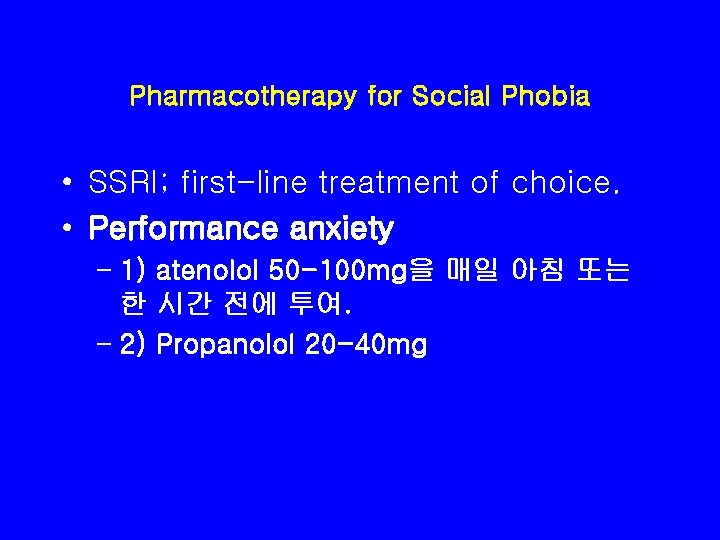
Pharmacotherapy for Social Phobia • SSRI; first-line treatment of choice. • Performance anxiety – 1) atenolol 50 -100 mg을 매일 아침 또는 한 시간 전에 투여. – 2) Propanolol 20 -40 mg
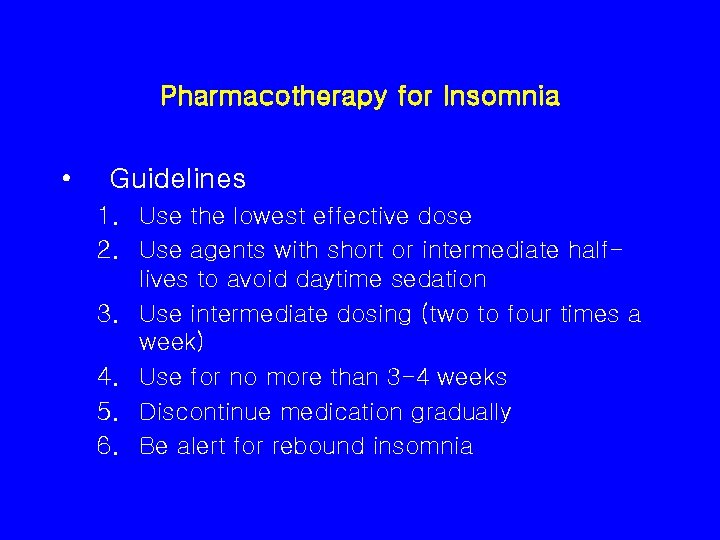
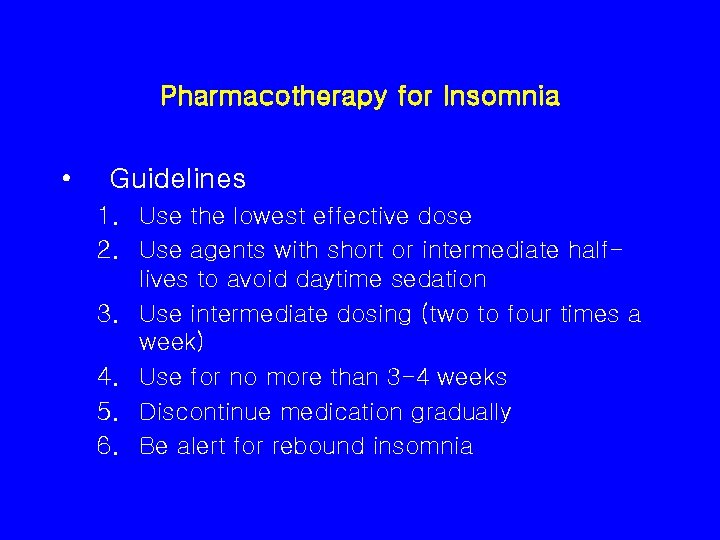
Pharmacotherapy for Insomnia • Guidelines 1. Use the lowest effective dose 2. Use agents with short or intermediate halflives to avoid daytime sedation 3. Use intermediate dosing (two to four times a week) 4. Use for no more than 3 -4 weeks 5. Discontinue medication gradually 6. Be alert for rebound insomnia

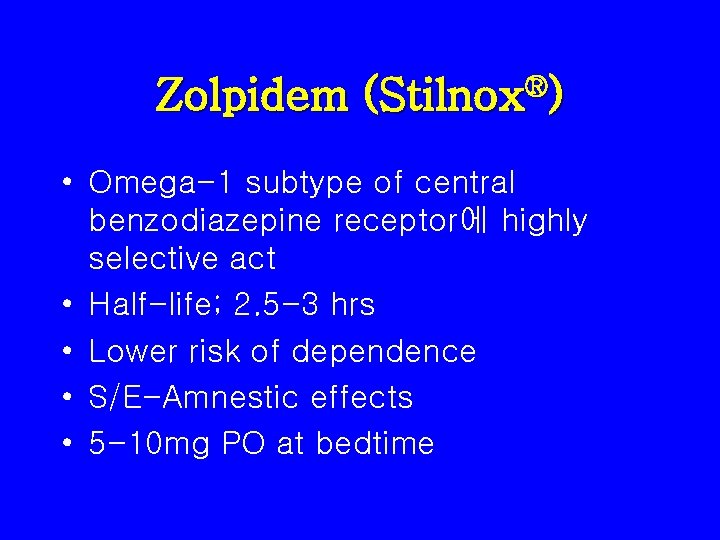
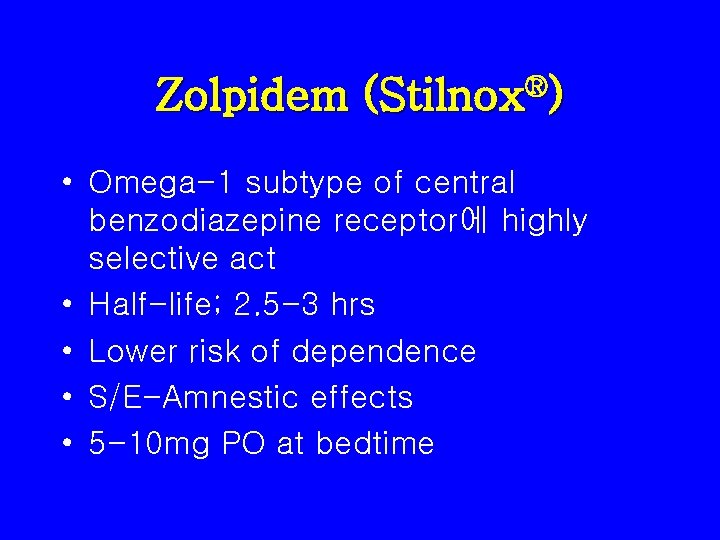
Zolpidem (Stilnox®) • Omega-1 subtype of central benzodiazepine receptor에 highly selective act • Half-life; 2. 5 -3 hrs • Lower risk of dependence • S/E-Amnestic effects • 5 -10 mg PO at bedtime
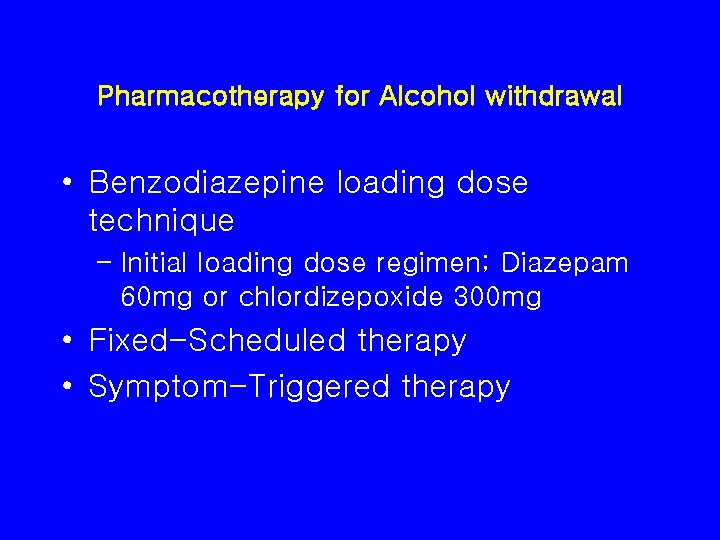
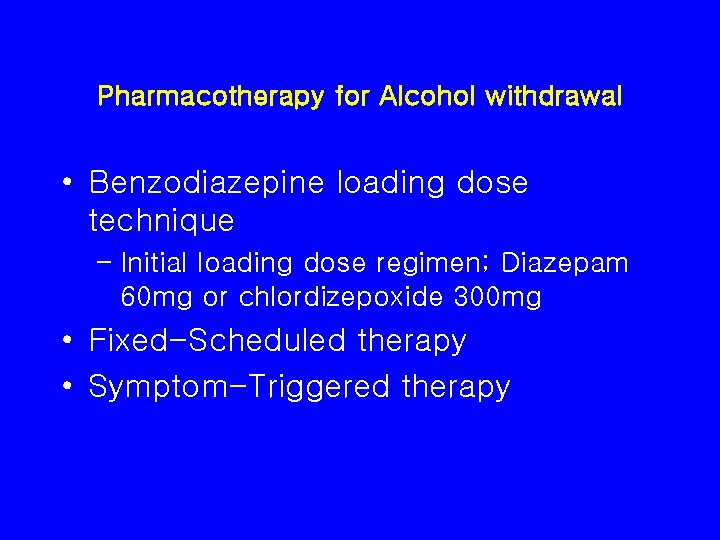
Pharmacotherapy for Alcohol withdrawal • Benzodiazepine loading dose technique – Initial loading dose regimen; Diazepam 60 mg or chlordizepoxide 300 mg • Fixed-Scheduled therapy • Symptom-Triggered therapy
인지기능개선제 Cognitive Enhancers
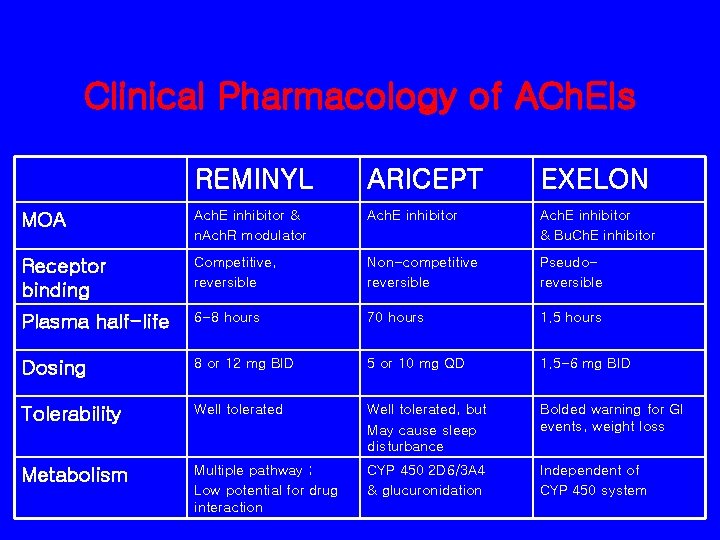
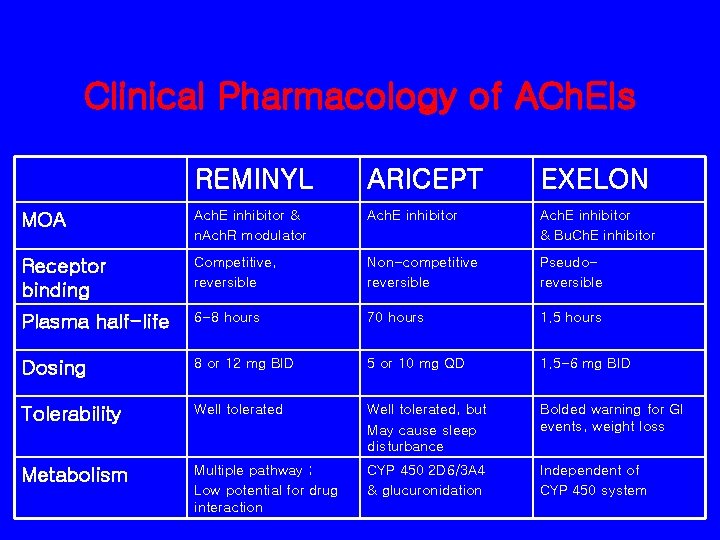
Clinical Pharmacology of ACh. EIs REMINYL ARICEPT EXELON MOA Ach. E inhibitor & n. Ach. R modulator Ach. E inhibitor & Bu. Ch. E inhibitor Receptor binding Competitive, reversible Non-competitive reversible Pseudoreversible Plasma half-life 6 -8 hours 70 hours 1. 5 hours Dosing 8 or 12 mg BID 5 or 10 mg QD 1. 5 -6 mg BID Tolerability Well tolerated, but May cause sleep disturbance Bolded warning for GI events, weight loss Metabolism Multiple pathway ; Low potential for drug interaction CYP 450 2 D 6/3 A 4 & glucuronidation Independent of CYP 450 system

기타 치매 약물 • • • Ginkgo biloba α-tocophenol (vitamine E) NSAIDs Hormone Therapy: Estrogen 혈관성 치매 – Aspirin, 고지혈증 치료제

 Cosmetic psychopharmacology
Cosmetic psychopharmacology Cosmetic psychopharmacology
Cosmetic psychopharmacology Psychopharmacology salary
Psychopharmacology salary Biological basis for understanding psychopharmacology
Biological basis for understanding psychopharmacology Nei master psychopharmacology
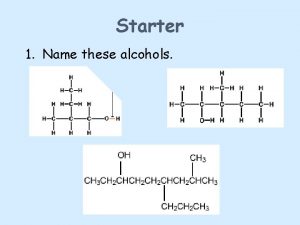
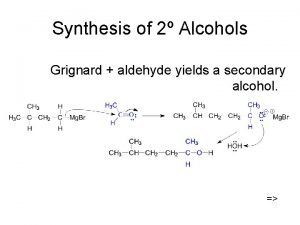
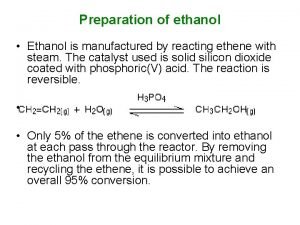
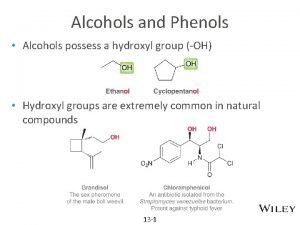
Nei master psychopharmacology Formation of alcohols
Formation of alcohols Oxidation of a primary alcohol
Oxidation of a primary alcohol Diferencia entre gran plano general y plano general
Diferencia entre gran plano general y plano general Where did general lee surrender to general grant?
Where did general lee surrender to general grant? General principle of greedy algorithm
General principle of greedy algorithm General principle of treatment of poisoning
General principle of treatment of poisoning Hillingdon arch
Hillingdon arch How much ethanol in alcohol
How much ethanol in alcohol Tlfb alcohol
Tlfb alcohol Recommended alcohol intake per day
Recommended alcohol intake per day Alcohol unscramble
Alcohol unscramble Alcohol flush syndrome
Alcohol flush syndrome Alcohol synthesis
Alcohol synthesis Sugar alcohol names
Sugar alcohol names Write a note on elimination reaction
Write a note on elimination reaction Edward wen
Edward wen Fetal alcohol syndrome celebrities
Fetal alcohol syndrome celebrities What is the ester
What is the ester Deshidratación de alcoholes
Deshidratación de alcoholes Ester ejemplos
Ester ejemplos Www.youtube.com
Www.youtube.com Are compounds pure substances
Are compounds pure substances Crystal violet iodine alcohol safranin
Crystal violet iodine alcohol safranin Neopentyl alcohol dehydration
Neopentyl alcohol dehydration Ingredientes del alcohol etílico
Ingredientes del alcohol etílico Functional group of aspirin
Functional group of aspirin Lucas reagent is
Lucas reagent is Formation of primary alcohol
Formation of primary alcohol Blood alcohol concentration (bac)
Blood alcohol concentration (bac) Alcohol thermometer
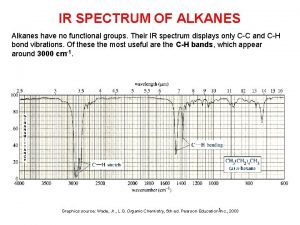
Alcohol thermometer Ir spectrum of alkanes
Ir spectrum of alkanes Alcohol rehab nuneaton
Alcohol rehab nuneaton Is a mixture of hydrocarbons.
Is a mixture of hydrocarbons. Alcohol delivery sunderland
Alcohol delivery sunderland Pancreazin
Pancreazin Adult with fetal alcohol syndrome
Adult with fetal alcohol syndrome Life expectancy fetal alcohol syndrome
Life expectancy fetal alcohol syndrome Fas
Fas Ester naming
Ester naming Alcohol secundario
Alcohol secundario Inhibitions drivers ed
Inhibitions drivers ed Blood alcohol concentration (bac)
Blood alcohol concentration (bac) Alcoholic ketoacidosis
Alcoholic ketoacidosis Conclusion on alcohol
Conclusion on alcohol Grupo funcional nitrogenado
Grupo funcional nitrogenado Long chain alcohol
Long chain alcohol Blood alcohol concentration (bac)
Blood alcohol concentration (bac) Chapter 8 toxicology poisons and alcohol
Chapter 8 toxicology poisons and alcohol Toxicology types
Toxicology types Alkyl halide solubility
Alkyl halide solubility Chapter 21 alcohol vocabulary practice
Chapter 21 alcohol vocabulary practice Ester functional group
Ester functional group Primary alcohol pcc
Primary alcohol pcc Upac
Upac Protonation of alcohol
Protonation of alcohol Alcohol to alkyl halide
Alcohol to alkyl halide Organic chemistry nomenclature
Organic chemistry nomenclature Jones reagent primary alcohol
Jones reagent primary alcohol Amide anhydride
Amide anhydride Hoeveel calorieën glas rose
Hoeveel calorieën glas rose Benzyl alcohol nmr
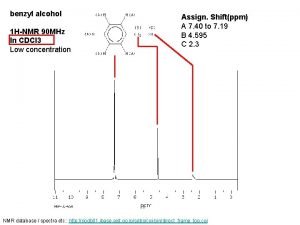
Benzyl alcohol nmr Is nh3 a nucleophile
Is nh3 a nucleophile Knockhardy chemistry
Knockhardy chemistry Alcohol from alkyl halide
Alcohol from alkyl halide What does na2cr2o7 do
What does na2cr2o7 do Ethanol with iodoform test
Ethanol with iodoform test Ethanol uses
Ethanol uses Alcohol toxicity
Alcohol toxicity Proh sub corr facil-alcohol/drug/phone/tobacco
Proh sub corr facil-alcohol/drug/phone/tobacco Alcohol straight up
Alcohol straight up Normal alcohol level
Normal alcohol level Iba alcohol
Iba alcohol Foetaal alcohol syndroom
Foetaal alcohol syndroom Alcohol formule
Alcohol formule Chapter 15 alcohol
Chapter 15 alcohol Alcohol ads targeting youth
Alcohol ads targeting youth Cage alcohol
Cage alcohol Carboxylic acid to ester
Carboxylic acid to ester Circle the acids and underline the bases
Circle the acids and underline the bases Tert butyl alcohol dehydration
Tert butyl alcohol dehydration Datos curiosos sobre el alcohol
Datos curiosos sobre el alcohol Site:slidetodoc.com
Site:slidetodoc.com Ethers naming
Ethers naming Ethanolamine production process
Ethanolamine production process Drugs and alcohol toolbox talk
Drugs and alcohol toolbox talk Hydroalcoholic solutions are:
Hydroalcoholic solutions are: Enfermedad causada por el alcohol
Enfermedad causada por el alcohol Bryce often acts so daring
Bryce often acts so daring Fetal alcohol syndrome face
Fetal alcohol syndrome face Pathophysiology of acute pancreatitis
Pathophysiology of acute pancreatitis Mateja grizelj
Mateja grizelj Harm reduction worksheets
Harm reduction worksheets Mesin pengganda yang menggunakan alcohol 100% adalah
Mesin pengganda yang menggunakan alcohol 100% adalah Advantages and disadvantages of alcohol thermometer
Advantages and disadvantages of alcohol thermometer Fetal alcohol syndrome life expectancy
Fetal alcohol syndrome life expectancy Primary alcohol pcc
Primary alcohol pcc Fetal alcohol spectrum disorder
Fetal alcohol spectrum disorder Alcohol chapter 1
Alcohol chapter 1 Nitrile to carboxylic acid
Nitrile to carboxylic acid Alcohol poisoning
Alcohol poisoning Hams alcohol taper
Hams alcohol taper Tadra is an acronym for
Tadra is an acronym for Alcohol rehab aboyne
Alcohol rehab aboyne Furfuryl alcohol resin
Furfuryl alcohol resin Effects of alcohol on the liver
Effects of alcohol on the liver Alcohol metabolism
Alcohol metabolism How exercise affect our consumption
How exercise affect our consumption Ethyl alcohol halal
Ethyl alcohol halal Leathermaking enzymes
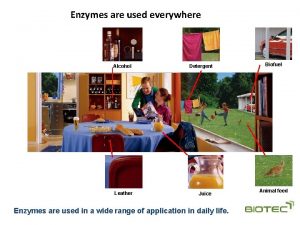
Leathermaking enzymes Stomach
Stomach Chapter 15 alcohol other drugs and driving
Chapter 15 alcohol other drugs and driving Conclusión sobre el alcohol
Conclusión sobre el alcohol Alcohol isopropilico
Alcohol isopropilico Exercise may alcohol consumption
Exercise may alcohol consumption Physical properties of alcohol
Physical properties of alcohol Nomenclature of ether
Nomenclature of ether Polyphagia alcohol withdrawal
Polyphagia alcohol withdrawal Alcohol behavior
Alcohol behavior Poppers alcohol
Poppers alcohol Effects of alcohol on the liver
Effects of alcohol on the liver 12 core functions of counseling
12 core functions of counseling Drug and alcohol jeopardy
Drug and alcohol jeopardy Dukoral alcohol
Dukoral alcohol Ash value definition
Ash value definition Teenage alcohol consumption
Teenage alcohol consumption Tabla de los aldehidos
Tabla de los aldehidos Alcohol bad for health
Alcohol bad for health Hoe maak je een reactieschema
Hoe maak je een reactieschema Alcohol is acidic or alkaline
Alcohol is acidic or alkaline Sabores indeseados en la cerveza
Sabores indeseados en la cerveza Intestifalk y alcohol
Intestifalk y alcohol Why is serving jugs of alcohol irresponsible
Why is serving jugs of alcohol irresponsible Alcohol + ammonia
Alcohol + ammonia Nucleofiele substitutie
Nucleofiele substitutie Chery alcohol
Chery alcohol Amfofilo
Amfofilo Define forensic toxicologist
Define forensic toxicologist A breath test reflects the alcohol concentration in the
A breath test reflects the alcohol concentration in the Caracteristicas del alcohol
Caracteristicas del alcohol Drug and alcohol information system (daisy)
Drug and alcohol information system (daisy) Alcohol is the mother of all evil
Alcohol is the mother of all evil Alcohol
Alcohol Rcoocor name
Rcoocor name Chapter 15 alcohol other drugs and driving
Chapter 15 alcohol other drugs and driving Centre county drug and alcohol
Centre county drug and alcohol Immune response controller crossword
Immune response controller crossword Fetal alcohol syndrome
Fetal alcohol syndrome Ultrapure vodka
Ultrapure vodka Caracteristicas del alcohol
Caracteristicas del alcohol Propylene glycol structure
Propylene glycol structure Alcohol fenol
Alcohol fenol What does pcc ch2cl2 do
What does pcc ch2cl2 do Alcohol en aymara
Alcohol en aymara With alcohol
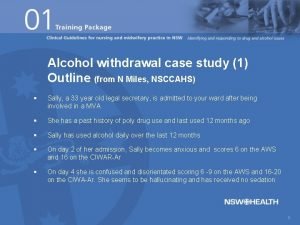
With alcohol Alcohol withdrawal case study
Alcohol withdrawal case study Alcohol is classified as
Alcohol is classified as Alcohol abuse
Alcohol abuse Alcohol is classified as a
Alcohol is classified as a Ciwa vragenlijst
Ciwa vragenlijst Why is alcohol considered a drug? *
Why is alcohol considered a drug? * Alcohol etilico
Alcohol etilico Oxidation of alcohol to aldehyde
Oxidation of alcohol to aldehyde