Fetal Alcohol Spectrum Disorder Diagnosis Dilemmas and Hope








- Slides: 36
Fetal Alcohol Spectrum Disorder Diagnosis, Dilemmas and Hope Christine R. Wasson, Psychologist CDC & Dawa Z Samdup, Developmental Paediatrician CDC/Queens University Kingston
What Is Fetal Alcohol Syndrome? ¡ FAS refers to a group of features found in children born to women who drink in pregnancy ¡ These features included: • facial & other physical anomalies • pre- & post-natal growth deficiency • a variety of central nervous system (CNS)/brain abnormalities
Fetal Alcohol Spectrum Disorders (FASD) ¡ ¡ Umbrella term describing the range of effects that can occur in an individual whose mother drank alcohol during pregnancy (FAS, Partial FAS, Alcohol Related Neurodevelopment Disorder, Alcohol Related Birth Defects May include physical, mental, behavioral, and/or learning disabilities with possible lifelong implications “Invisible” disability + ¡
Fetal Alcohol Spectrum Disorders (FASD) Cont’d ¡ ¡ Diagnostic and Statistical Manual of Mental Disorders – Fifth Edition (DSM-5) Neurodevelopmental disorder associated with prenatal alcohol exposure - 315. 8 (F 88) Neurodevelopmental disorder associated with prenatal exposure is characterized by a range of developmental disabilities following exposure to alcohol in utero No set diagnostic criteria, diagnostic features, differential diagnosis or comorbidity are not discussed

How Does Alcohol Cause FAS/FASD? ¡ ¡ ¡ Exposure to alcohol in pregnancy decreased ‘sprouting’ of brain cells, which has a profound impact on subsequent cognitive development Interference with the 1 st growth spurt brain malformations, microcephaly, or cells in particular areas, e. g. corpus callosum or cerebellum A 2 nd growth spurt occurs at ~7 months. Exposure to toxins then behavioral/cognitive even with normal size brain
What Protects Some Kids & Not Others? Maternal drinking pattern ¡ Differences in maternal metabolism ¡ Differences in Genetic susceptibility ¡ Timing of alcohol consumption during pregnancy ¡ Variation in vulnerability of different brain regions ¡

How Common is FASD? ¡ ¡ 80% of women locally report drinking some alcohol Between 50%-75% of all pregnancies are unplanned and social drinking prior to knowledge of pregnancy is common (Riley, 2003) Estimate of FAS vary from 0. 5 to 3 per 1000 live birth in most populations, with higher rates in some communities (Stratton et al. , 1996) Estimates of alcohol-affected births are five to ten times as many

Why Diagnose? ¡ ¡ ¡ ¡ Supports a shift in understanding and reframing the meaning of presenting behaviours from “won’t” to “can’t” New understanding leads to new strategies at home and other environments Funding in school and daycare Opening doors for family services Better medical management Prevention of secondary disabilities (diagnosis before 6 years is protective factor) Prevention of future alcohol affected children

Secondary Disabilities
Challenges To Diagnosis! ¡ ¡ ¡ ¡ Lack of history about biological parents Lack of diagnostic facilities Use of different diagnostic criteria Not all physician know how to make the diagnosis No school programs/solutions for diagnosed children No preparation/program in the correction system No facilities/plans for adults with FASD Limited investment for FASD by government
Diagnostic Criteria For FASD Prenatal exposure to Alcohol ¡ FAS Facial Features ¡ Growth deficiency ¡ CNS damage (brain dysfunction) ¡
Confirmation of Prenatal Exposure to Alcohol History – self report or by others close to biological mother ¡ Maternal biomarkers (e. g. , alcohol in blood/breath test; Liver enzymes) ¡ Neonatal Biomarkers (e. g. , measuring Fatty Acid Ethyl Esters/FAEEs in baby’s meconium) ¡
Growth Deficiency Intrauterine-Postnatal Growth ¡ Decelerating weight over time not due to nutrition or other know pathology ¡ Disproportional low weight to height ¡ Always consider parental weight, height, and head circumference ¡
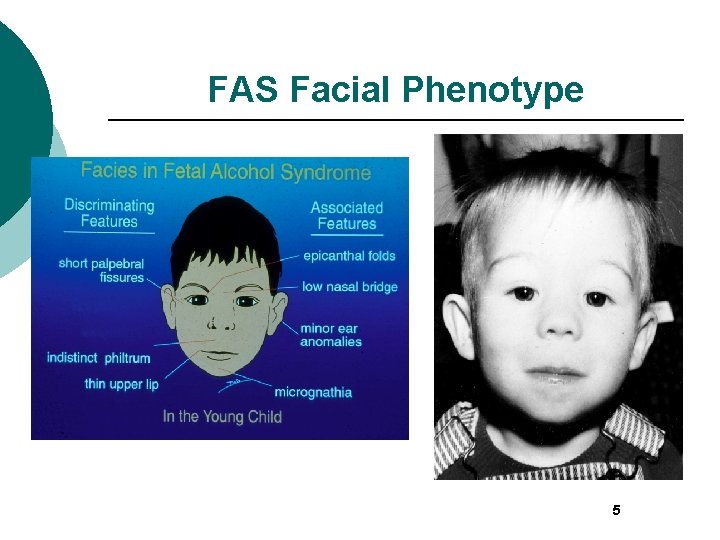
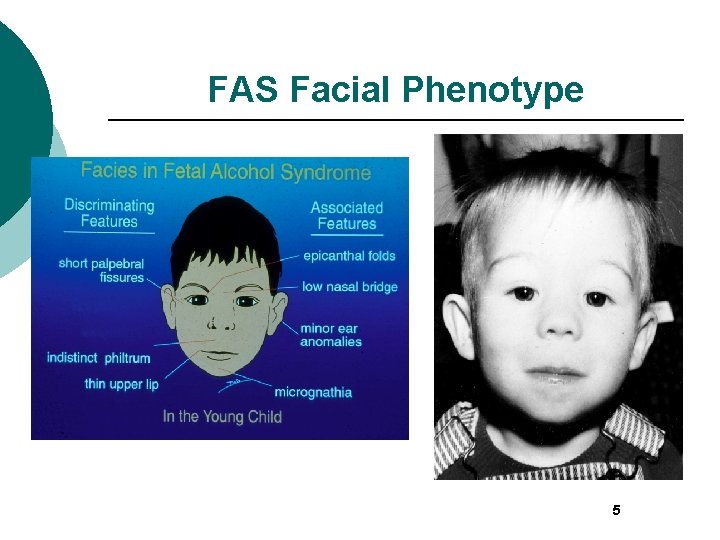
FAS Facial Phenotype 5

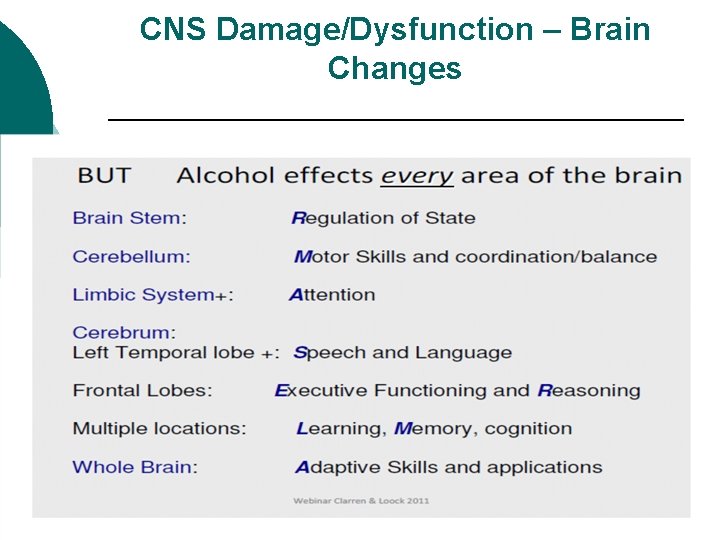
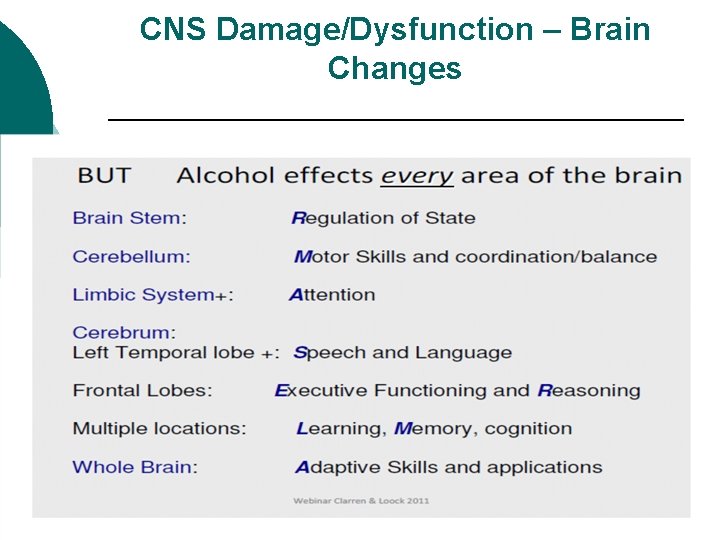
CNS Damage/Dysfunction – Brain Changes
CNS Damage/Dysfunction – Brain Changes ¡ Reasoning (IQ) ¡ Motor ¡ Attention ¡ Executive Function ¡ Learning ¡ Regulation of State ¡ Memory ¡ Speech/Language ¡ Adaptation
Typical Difficulties For Persons With an FASD Information Processing: ¡ Do not complete tasks or chores and may appear to be oppositional ¡ Have trouble determining what to do in a given situation ¡ Do not ask questions because they want to fit in ¡ Have trouble with changes in tasks and routine
Typical Difficulties For Persons With an FASD - Executive Function and Decision-Making ¡ ¡ Repeatedly break the rules Give in to peers pressure Tend not to learn from mistakes or natural consequences Frequently do not respond to reward systems (points, levels, stickers, etc. ) ¡ ¡ ¡ Have difficulty entertaining themselves Naïve, gullible (e. g. , may walk off with a stranger) Struggle with abstract concepts (e. g. , time, space, money, etc. ) I’m late!
Typical Difficulties For Persons With an FASD Self-Esteem and Personal Issues: ¡ ¡ ¡ Function unevenly in school, work, and development – Often feel “stupid” or like a failure Are seen as lazy, uncooperative, and unmotivated –Have often been told they’re not trying hard enough May have hygiene problems Are aware that they’re “different” from others Often grow up living in multiple homes and experience multiple losses
Typical Difficulties For Persons With an FASD Sensory: May be overly sensitive to bright lights, certain clothing, tastes and textures in food, loud sounds, etc. Physical: Have problems with balance and motor coordination (may seem “clumsy”).
Typical Strengths of Persons With an FASD ¡ Friendly and cheerful ¡ Determined ¡ Likable ¡ Have points of insight ¡ Desire to be liked ¡ Hard working ¡ Helpful ¡ ¡ Verbal Every day is a new day!
Clinical process for FASD Diagnosis at the Child Development Centre Hotel Dieu Hospital

About the Child Development Centre (CDC) ¡ ¡ ¡ ¡ Located at Hotel Dieu Hospital One of 21 Children's Treatment Centres in the province. It serves children and youth with multiple disabilities Interdisciplinary teams that include the Medical, Social Work, Physiotherapy, Occupational therapy, Psychology, and Speech and Language disciplines. Work together with parents, teachers, community agencies to support the clients and their families to achieve an optimal level of independence in their home and community. More than 10, 000 patient visits are recorded by the CDC each year. The CDC is funded through the Ontario Ministry of Children and Youth. www. Kingston. CDC. ca
FASD Diagnosis vs. FASD Clinic ¡ ¡ CDC offers FASD diagnosis It is not a FASD clinic - Developmental paediatrician and psychologist Referrals have increased from 3 -4 to 810 in a year In 2013, 6 children were identified with FASD: 1 with FAS, 1 with partial FAS and 4 with ARND.
Referral Process A physician referral querying FASD; some knowledge of prenatal alcohol exposure ¡ Clients typically referred with a query of FASD range in age from 5 – 12 years of age ¡ All intakes for query FASD are reviewed by the Psychologist ¡
Steps 1) 2) 3) 4) 5) Parents/guardians may be contacted to ascertain what the presenting problems are The following information is collected: growth charts, Genetics testing, history about birth parents, details concerning maternal use of alcohol, and copies of all assessment reports (OT, PT, SLP) Typically children see the psychologist first for a comprehensive psychological assessment Children and parent/guardians are then booked in to see the Developmental Paediatrician for a comprehensive medical evaluation Typically the psychologist provides feedback to parents/guardians at the medical appointment

Psychological Assessment ¡ ¡ Gets background history from parent/guardian Teacher interviews Review report cards (if available) Standardized measures & parent/teacher questionnaires are used to assess cognitive, adaptive, academic, sensory and behavioural functioning
Medical Evaluation ¡ ¡ Following the psychological assessment an appointment is scheduled for the child and parents/gurdians to see the developmental paeditrician A Developmental History is completed Comorbid disorders are checked for (e. g. , AHDH, Anxiety, Sleep Disorders) Physical Exam – FAS Facial Phenotype assessed
Diagnosis: The developmental pediatrician and psychologist review all available data ¡ The Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis are used ¡ The developmental pediatrician gives the diagnosis ¡
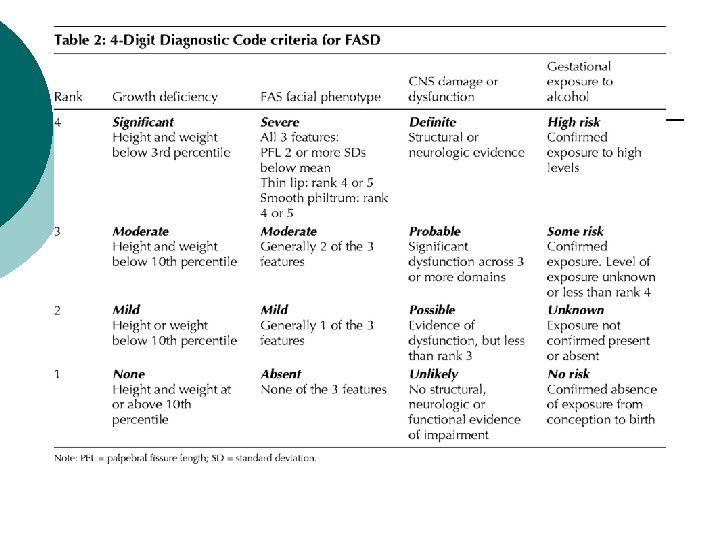
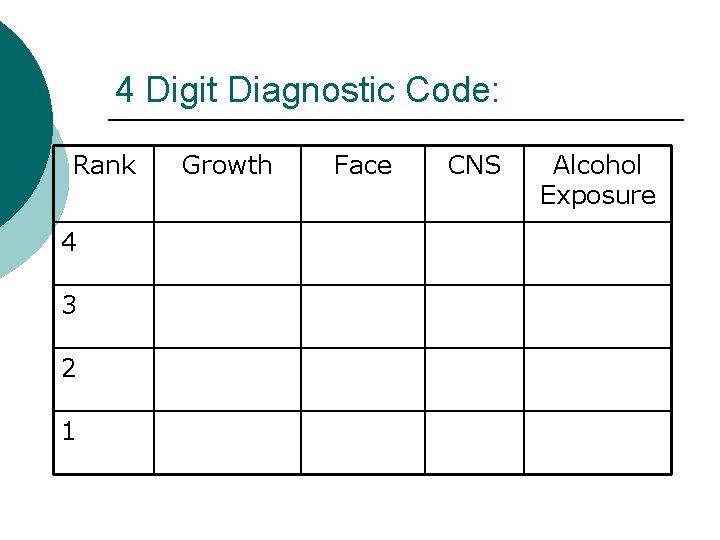
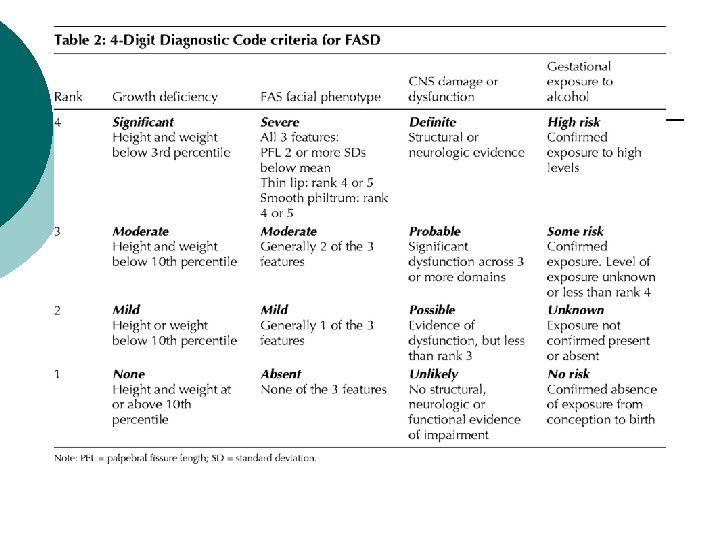
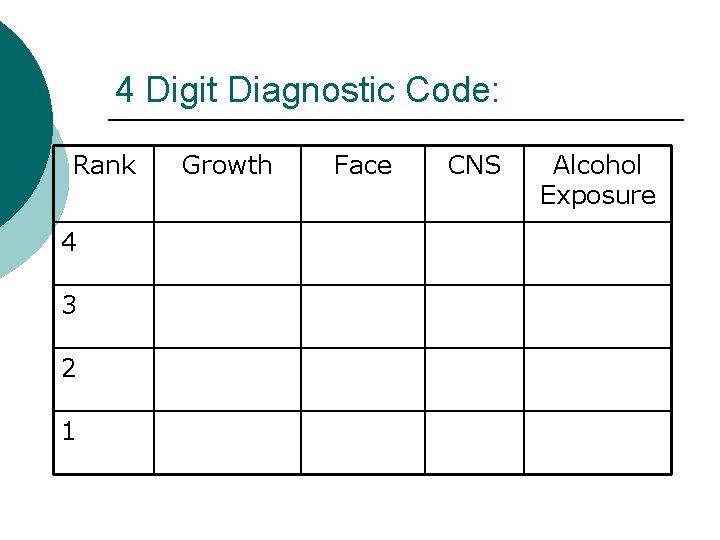
4 Digit Diagnostic Code: Rank 4 3 2 1 Growth Face CNS Alcohol Exposure

Post Assessment Practices ¡ ¡ ¡ ¡ The developmental paediatrician and psychologist provide feedback to parents/guardian together Psychologist often attends school conferences to share the finding of the assessment Developmental Pediatrician may continue to monitor if medication is prescribed Referral to behavioural programs (e. g. , Pathways for Children and Youth or Behavioural Services at Ongwanada) If significant sleep issues are present will refer young children to CHEO and if older to Kingston General Hospital for a sleep study Put families in touch with Queens University concerning different research initiatives Refer families to FASD Kingston Learning & Sharing Group
What’s Needed? ¡ ¡ More resources for other services (e. g. , SLP, OT and social work) Liaison person to translate test findings and educate school staff and to assist the family and school in working towards the recommendations Not enough psychologists in public sector to do testing More coordination of services among community partners
Hope ¡ ¡ ¡ Early identification and intervetnion reduces the risk of secondary disabilities considerably Community partners assisting in psychological assessments Collaboration of stakeholders, reseachers and community partners at the local, provincal and national level. Some of these include: • Neuro. Dev. Net • Queen’s University • Canada Fetal Alcohol Spectrum Disorder Research Network (Can. FASD) • FASD Ontario Network of Expertise (FASD ONE) • FASD Kingston Action Network
 Fetal alcohol spectrum disorder
Fetal alcohol spectrum disorder Popstrus
Popstrus Fetal alcohol syndrome face in adults
Fetal alcohol syndrome face in adults Life expectancy fetal alcohol syndrome
Life expectancy fetal alcohol syndrome Fetal alcohol syndrome ears
Fetal alcohol syndrome ears Fetal alcohol syndrome face
Fetal alcohol syndrome face Fetal alcohol syndrome life expectancy
Fetal alcohol syndrome life expectancy Fetal alcohol syndrome
Fetal alcohol syndrome Fetal alcohol syndrome
Fetal alcohol syndrome Orbital diagram for cu
Orbital diagram for cu Formation of alcohols
Formation of alcohols Oxidation primary alcohol
Oxidation primary alcohol Conversion disorder
Conversion disorder Types of nursing diagnosis
Types of nursing diagnosis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
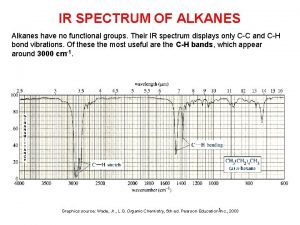
Medical diagnosis and nursing diagnosis difference Ir spectrum of nitrile
Ir spectrum of nitrile False dilemma definition
False dilemma definition School social work ethical dilemmas
School social work ethical dilemmas What is dilemma in ethics
What is dilemma in ethics 5 steps in resolving ethical dilemmas
5 steps in resolving ethical dilemmas Engineering ethical dilemmas
Engineering ethical dilemmas Ethical reasoning
Ethical reasoning Cpa ethical dilemmas
Cpa ethical dilemmas Historical ethical dilemmas
Historical ethical dilemmas Ethical dilemmas in early childhood education
Ethical dilemmas in early childhood education Leadership dilemmas grid solutions
Leadership dilemmas grid solutions Autism spectrum disorder authorization california
Autism spectrum disorder authorization california Types of autism spectrum disorder dsm 5
Types of autism spectrum disorder dsm 5 Types of autism spectrum disorder
Types of autism spectrum disorder Is autism genetic
Is autism genetic Autism spectrum disorder adhd
Autism spectrum disorder adhd Spectrum disorder
Spectrum disorder Spectrum disorder
Spectrum disorder Nursing diagnosis of somatoform disorder
Nursing diagnosis of somatoform disorder Post traumatic stress disorder
Post traumatic stress disorder