Autism Next Steps The Day After the ASD










- Slides: 59
Autism Next Steps: The Day After the ASD Diagnosis Prachi Shah, MD Associate Professor, Pediatrics Division of Developmental-Behavioral Pediatrics Center for Human Growth and Development prachis@umich. edu
Objectives 1. To present the DSM-V diagnostic criteria and clinical symptoms of ASD 2. Discuss the diagnostic evaluation of children with suspected ASD 3. Discuss the medical / therapeutic treatments for children with suspected ASD 4. Discuss how to advocate for your patient with ASD in the school system
1. Clinical Presentation of ASD
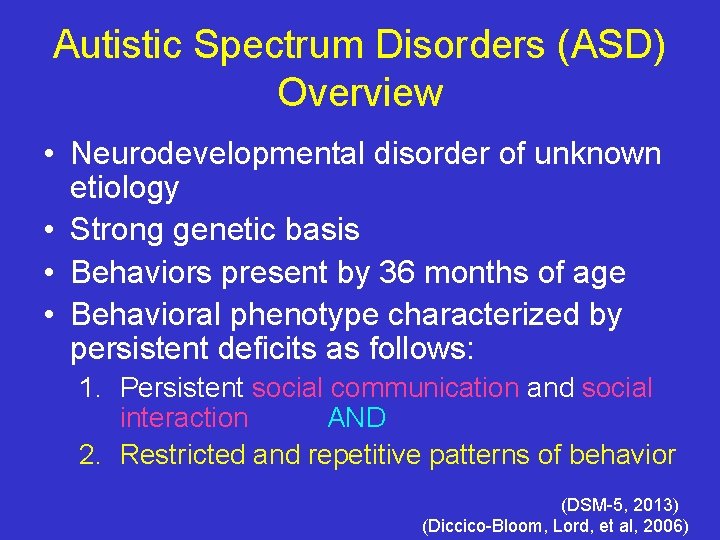
Autistic Spectrum Disorders (ASD) Overview • Neurodevelopmental disorder of unknown etiology • Strong genetic basis • Behaviors present by 36 months of age • Behavioral phenotype characterized by persistent deficits as follows: 1. Persistent social communication and social interaction AND 2. Restricted and repetitive patterns of behavior (DSM-5, 2013) (Diccico-Bloom, Lord, et al, 2006)
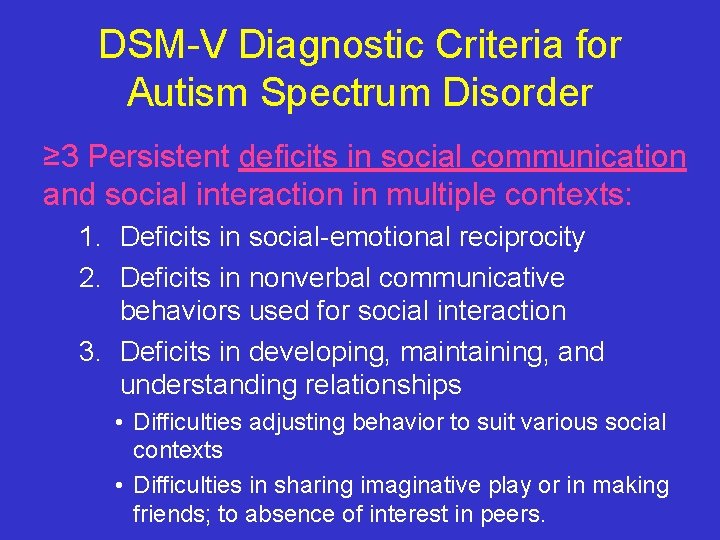
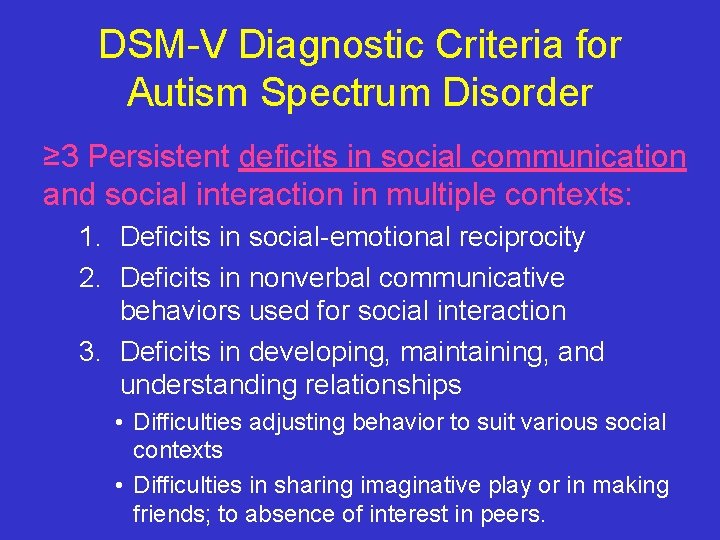
DSM-V Diagnostic Criteria for Autism Spectrum Disorder ≥ 3 Persistent deficits in social communication and social interaction in multiple contexts: 1. Deficits in social-emotional reciprocity 2. Deficits in nonverbal communicative behaviors used for social interaction 3. Deficits in developing, maintaining, and understanding relationships • Difficulties adjusting behavior to suit various social contexts • Difficulties in sharing imaginative play or in making friends; to absence of interest in peers.
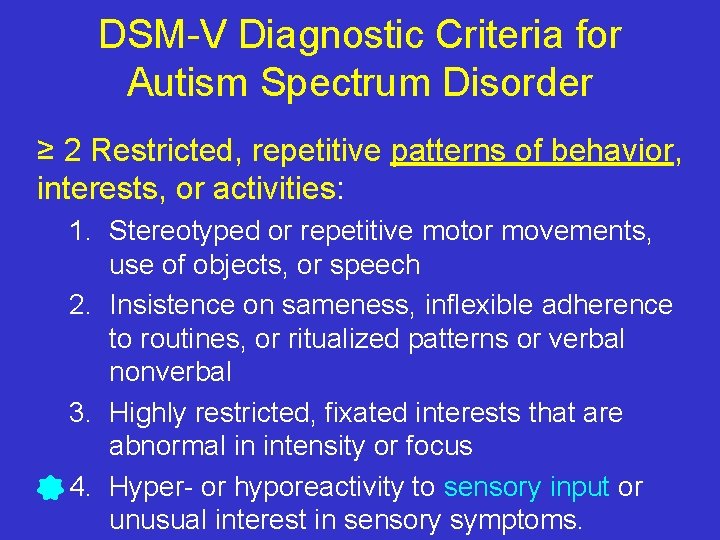
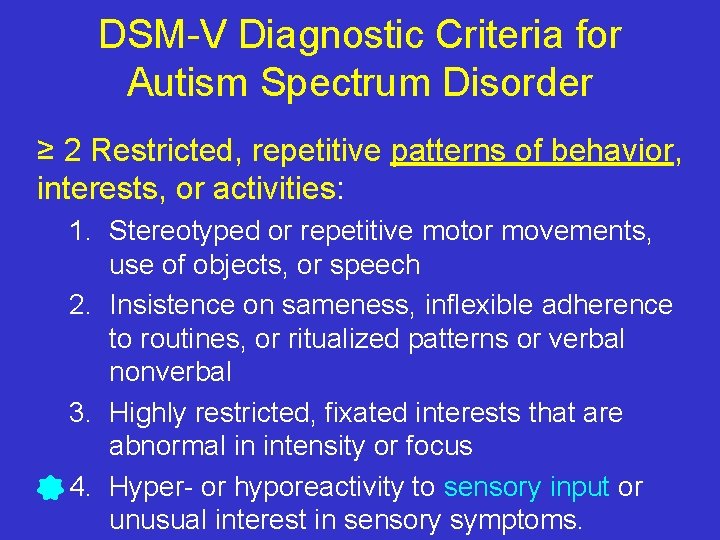
DSM-V Diagnostic Criteria for Autism Spectrum Disorder ≥ 2 Restricted, repetitive patterns of behavior, interests, or activities: 1. Stereotyped or repetitive motor movements, use of objects, or speech 2. Insistence on sameness, inflexible adherence to routines, or ritualized patterns or verbal nonverbal 3. Highly restricted, fixated interests that are abnormal in intensity or focus 4. Hyper- or hyporeactivity to sensory input or unusual interest in sensory symptoms.
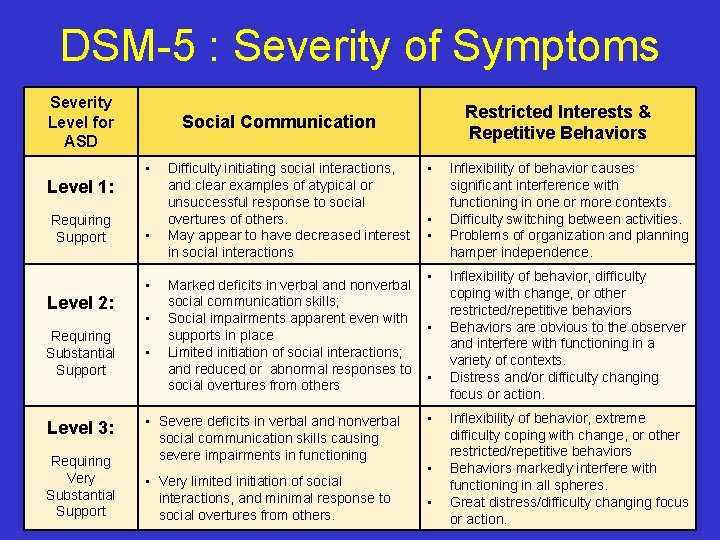
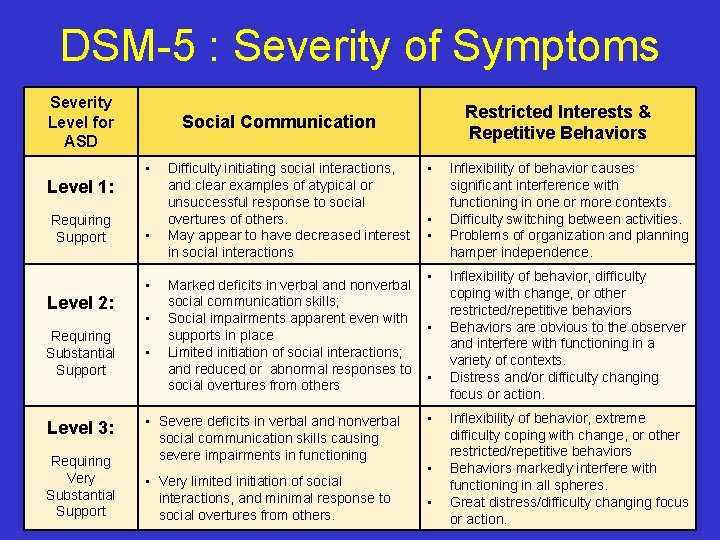
DSM-5 : Severity of Symptoms Severity Level for ASD • Level 1: Requiring Support • • Level 2: Requiring Substantial Support Level 3: Requiring Very Substantial Support Restricted Interests & Repetitive Behaviors Social Communication • • Difficulty initiating social interactions, • and clear examples of atypical or unsuccessful response to social overtures of others. • May appear to have decreased interest • in social interactions Inflexibility of behavior causes significant interference with functioning in one or more contexts. Difficulty switching between activities. Problems of organization and planning hamper independence. • Marked deficits in verbal and nonverbal social communication skills; Social impairments apparent even with • supports in place Limited initiation of social interactions; and reduced or abnormal responses to • social overtures from others Inflexibility of behavior, difficulty coping with change, or other restricted/repetitive behaviors Behaviors are obvious to the observer and interfere with functioning in a variety of contexts. Distress and/or difficulty changing focus or action. • Inflexibility of behavior, extreme difficulty coping with change, or other restricted/repetitive behaviors Behaviors markedly interfere with functioning in all spheres. Great distress/difficulty changing focus or action. • Severe deficits in verbal and nonverbal social communication skills causing severe impairments in functioning • Very limited initiation of social interactions, and minimal response to social overtures from others. • •
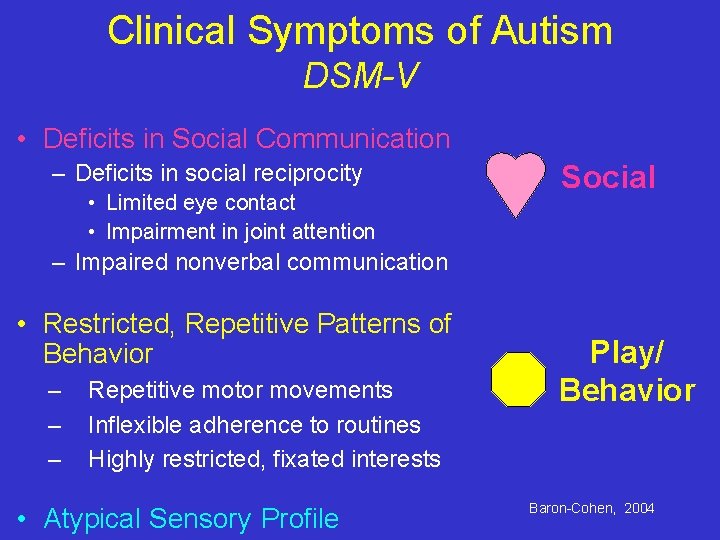
Clinical Symptoms of Autism DSM-V • Deficits in Social Communication – Deficits in social reciprocity • Limited eye contact • Impairment in joint attention Social – Impaired nonverbal communication • Restricted, Repetitive Patterns of Behavior – – – Repetitive motor movements Inflexible adherence to routines Highly restricted, fixated interests • Atypical Sensory Profile Play/ Behavior Baron-Cohen, 2004
A 6 -minute snapshot into the world of a child with ASD https: //www. youtube. com/watch? v=mc 1 H 0 a. Vqn 20
A 1 -minute snapshot of a child with high functioning ASD
2. The Diagnostic Evaluation of ASD
Diagnostic “Gestalt” • Checking your Countertransference • “Ceiling Fan Question”
Observing Child Behavior : Important Diagnostic Keys
Diagnostic Evaluation of Children with Suspected ASD PEDIATRICS, Volume 120, Number 5, November 2007
The Role of the Physician • Screen – Using a validated screening tool • Suspect – Autism if a failed screen • Direct – Patient for a comprehensive ASD evaluation
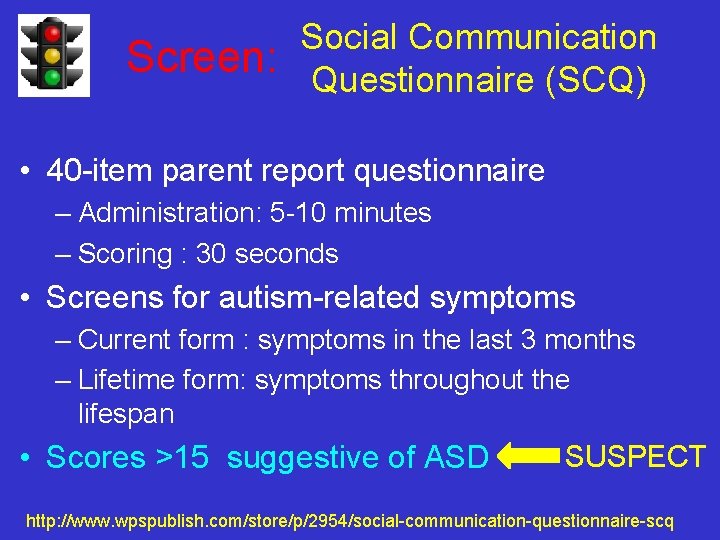
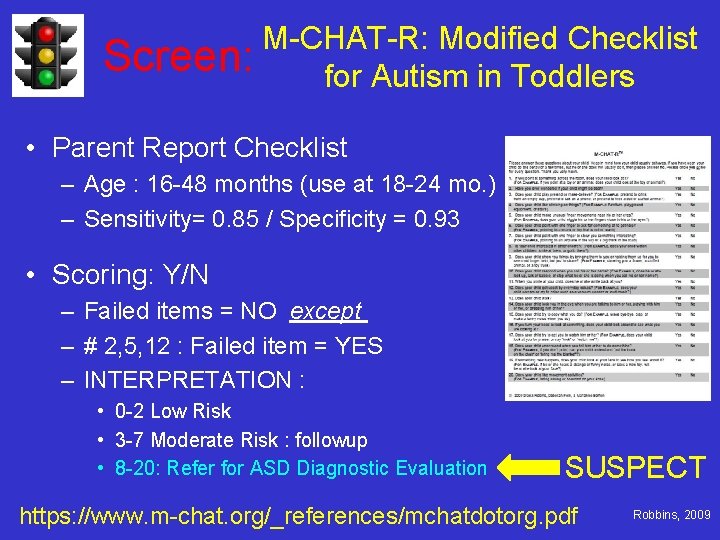
Actively Screen for ASD • American Academy of Pediatrics Guidelines – Screen for ASD at 18 and 24 months • http: //www. pediatrics. org/cgi/content/full/peds. 20072361 v 1 • Use a validated screening tool for Autism – Social Communication Questionnaire (SCQ) – Modified Checklist for Autism in Toddlers (MCHAT)
Social Communication Screen: Questionnaire (SCQ) • 40 -item parent report questionnaire – Administration: 5 -10 minutes – Scoring : 30 seconds • Screens for autism-related symptoms – Current form : symptoms in the last 3 months – Lifetime form: symptoms throughout the lifespan • Scores >15 suggestive of ASD SUSPECT http: //www. wpspublish. com/store/p/2954/social-communication-questionnaire-scq
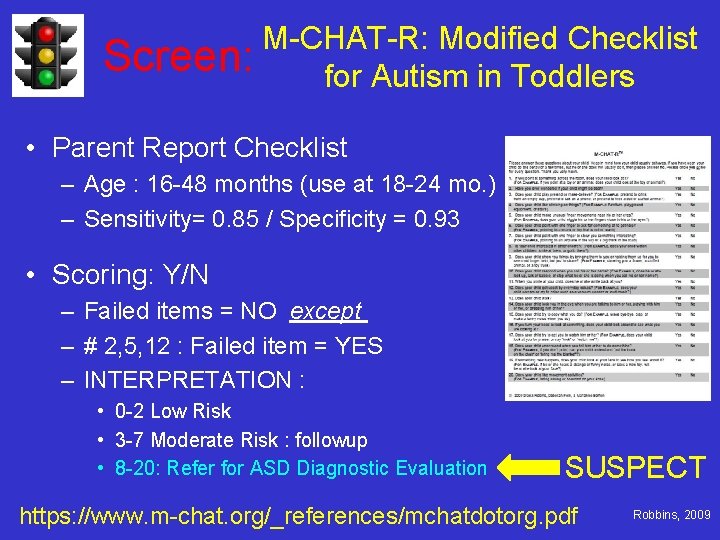
M-CHAT-R: Modified Checklist Screen: for Autism in Toddlers • Parent Report Checklist – Age : 16 -48 months (use at 18 -24 mo. ) – Sensitivity= 0. 85 / Specificity = 0. 93 • Scoring: Y/N – Failed items = NO except – # 2, 5, 12 : Failed item = YES – INTERPRETATION : • 0 -2 Low Risk • 3 -7 Moderate Risk : followup • 8 -20: Refer for ASD Diagnostic Evaluation SUSPECT https: //www. m-chat. org/_references/mchatdotorg. pdf Robbins, 2009
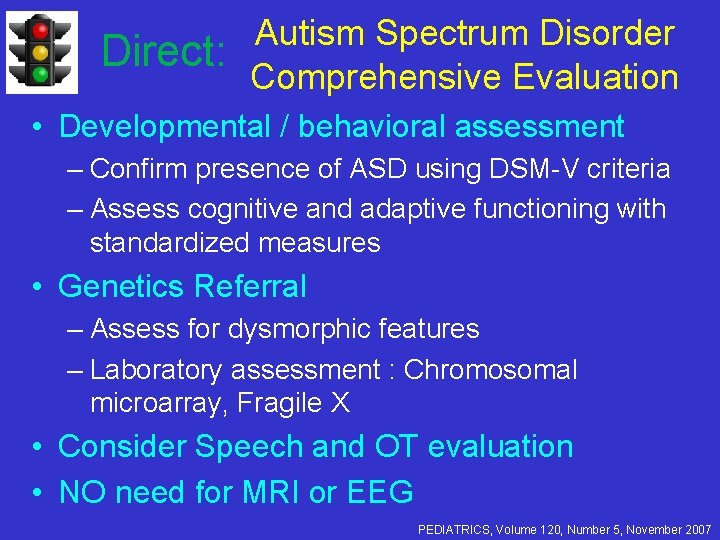
Direct: Autism Spectrum Disorder Comprehensive Evaluation • Developmental / behavioral assessment – Confirm presence of ASD using DSM-V criteria – Assess cognitive and adaptive functioning with standardized measures • Genetics Referral – Assess for dysmorphic features – Laboratory assessment : Chromosomal microarray, Fragile X • Consider Speech and OT evaluation • NO need for MRI or EEG PEDIATRICS, Volume 120, Number 5, November 2007

Autism and Michigan Legislation

Autism and Michigan Legislation Senate Bill 414 (PA 99): October 2012 • Coverage for treatment of ASD for children 0 -18 yo – 0 -6 years old : $50, 000/ year – 7 -12 years old : $40, 000/ year – 13 -18 years old : $30, 000/ ear • Requires diagnosis of ASD by MD or Psychologist • Covers evidence-based ASD related treatments – – Applied Behavioral Analysis (ABA) Pharmacy care Psychiatric / Psychological Care Therapies : PT/OT/ Speech

Direct: ASD Comprehensive Evaluation Michigan Requirements • Medical – Medical evaluation to confirm ASD Diagnosis – DBP; Neurologist; Geneticist • Behavioral – Behavioral assessment to confirm ASD diagnosis – Includes ADOS or ADI – Psychologist; Psychiatrist; DBP • Speech – Assess language and social pragmatics Services individualized based on patient’s needs
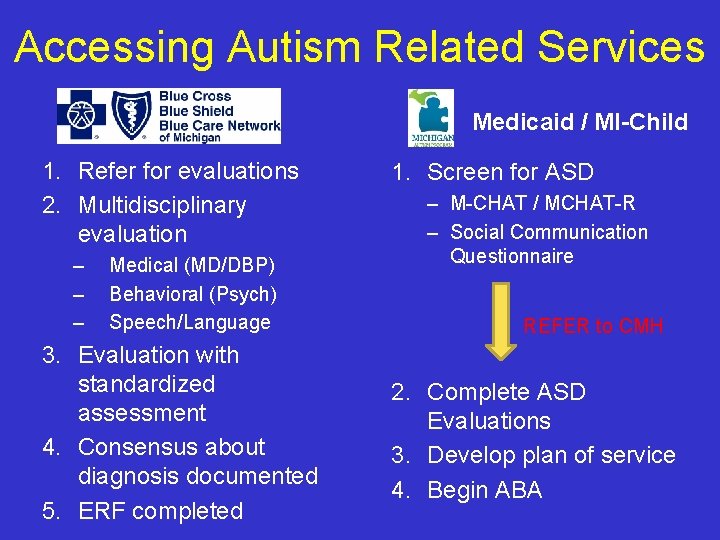
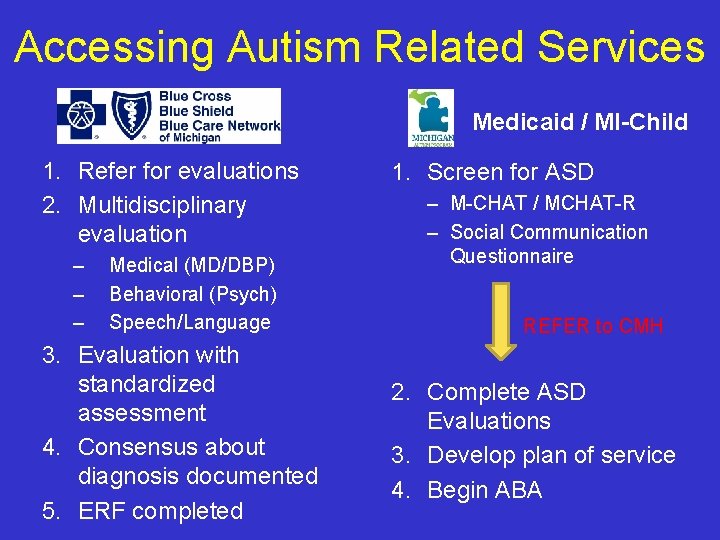
Accessing Autism Related Services Medicaid / MI-Child 1. Refer for evaluations 2. Multidisciplinary evaluation – – – Medical (MD/DBP) Behavioral (Psych) Speech/Language 3. Evaluation with standardized assessment 4. Consensus about diagnosis documented 5. ERF completed 1. Screen for ASD – M-CHAT / MCHAT-R – Social Communication Questionnaire REFER to CMH 2. Complete ASD Evaluations 3. Develop plan of service 4. Begin ABA

3. The Medical Management of ASD
Management of Children with Suspected ASD PEDIATRICS, Volume 120, Number 5, November 2007
Management of Children with ASD • Developmental / Behavioral Therapies – Speech Therapy; Occupational Therapy – ABA – Social skills training • Medication management for target symptoms – ADHD – Aggression – Sleep • Education Interventions – Interventions specific for ASD: 25 hrs/ wk, 12 mo. / year – Special Education services under the qualification of Autism / OHI PEDIATRICS, Volume 120, Number 5, November 2007

Goals of Therapy • Minimize Negative Symptoms – Sensory Symptoms – Difficult/ Rigid Behaviors – Difficulties with emotional regulation • Promote Skill Acquisition – Communication skills – Social skills – Play skills – Cognitive skills Individualize for the child’s strengths and weaknesses
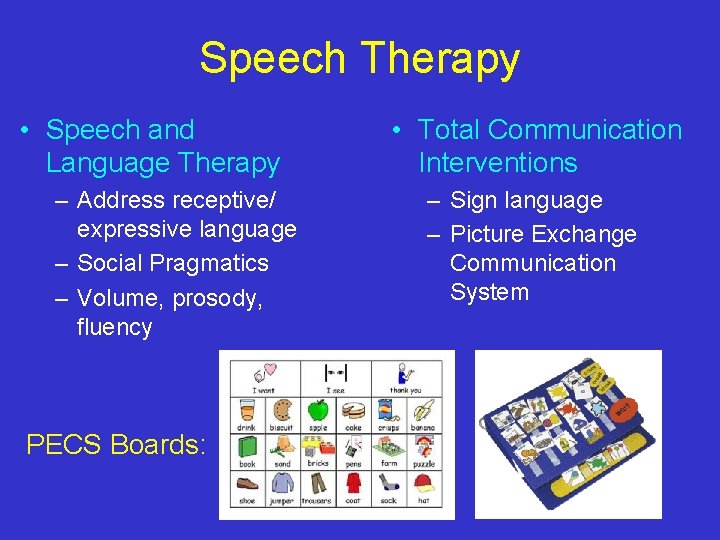
Speech Therapy • Speech and Language Therapy – Address receptive/ expressive language – Social Pragmatics – Volume, prosody, fluency PECS Boards: • Total Communication Interventions – Sign language – Picture Exchange Communication System

Occupational / Physical Therapy • Address Fine/ Gross motor delay • Sensory integration disorder • Developmental Coordination Disorder

Behavioral Therapy: Applied Behavior Analysis • Uses positive reinforcement to encourage social and communicative behaviors • Breaks tasks down into small steps – Making eye contact when name is called – Pointing to indicate a request, joint attention – Trying a new food • Sets goals and assesses progress regularly • Should involve the family – either home-based or center -based education • Needs to be 12 months/year to prevent regression
ABA in a Nutshell
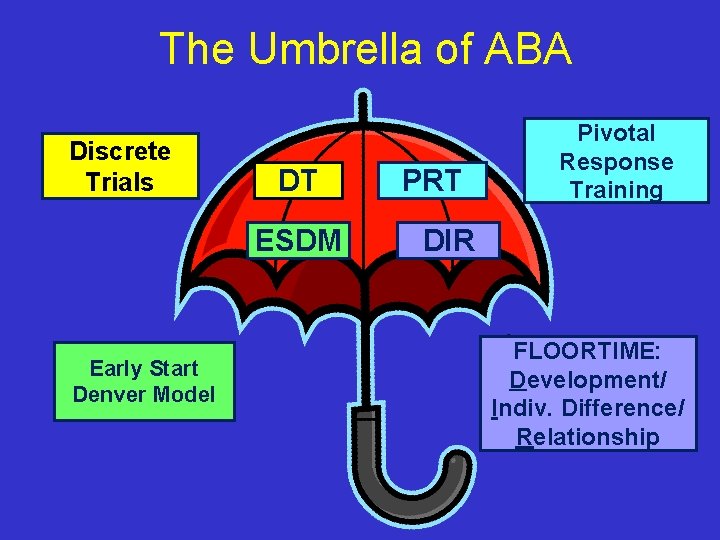
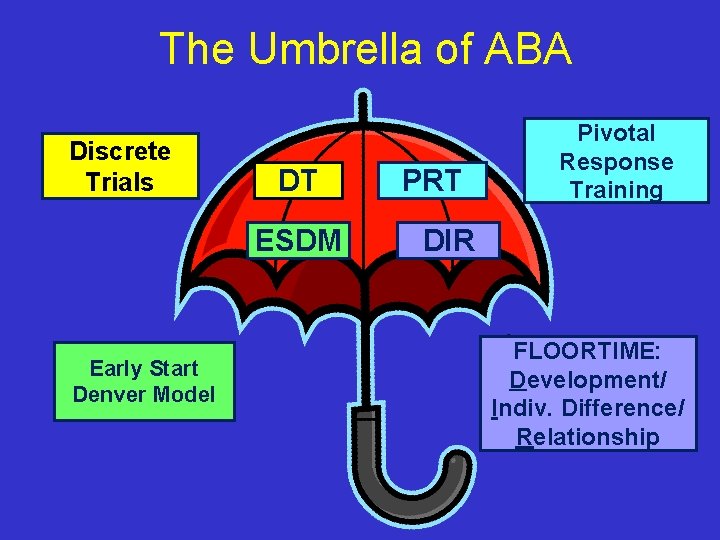
The Umbrella of ABA Discrete Trials DT ESDM Early Start Denver Model PRT Pivotal Response Training DIR FLOORTIME: Development/ Indiv. Difference/ Relationship
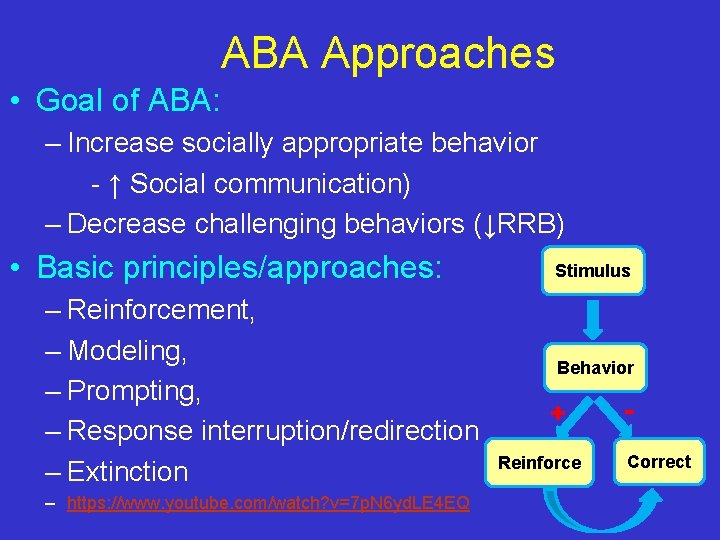
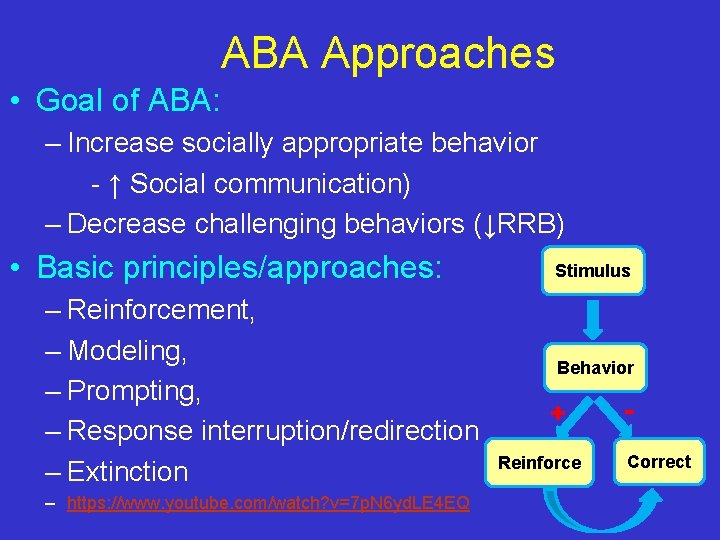
ABA Approaches • Goal of ABA: – Increase socially appropriate behavior - ↑ Social communication) – Decrease challenging behaviors (↓RRB) • Basic principles/approaches: – Reinforcement, – Modeling, – Prompting, – Response interruption/redirection – Extinction – https: //www. youtube. com/watch? v=7 p. N 6 yd. LE 4 EQ Stimulus Behavior + Reinforce Correct
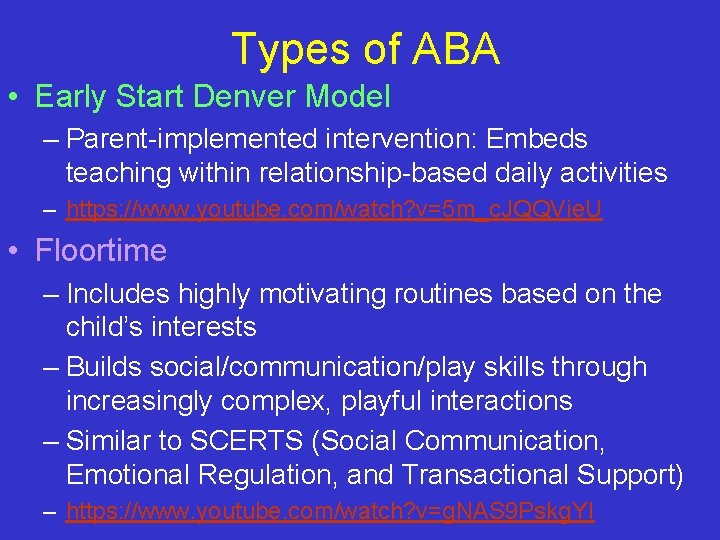
Types of ABA • Early Start Denver Model – Parent-implemented intervention: Embeds teaching within relationship-based daily activities – https: //www. youtube. com/watch? v=5 m_c. JQQVie. U • Floortime – Includes highly motivating routines based on the child’s interests – Builds social/communication/play skills through increasingly complex, playful interactions – Similar to SCERTS (Social Communication, Emotional Regulation, and Transactional Support) – https: //www. youtube. com/watch? v=g. NAS 9 Pskg. YI
Parent Coaching • Initiating, responding to, and sustaining play interactions • Making requests, answering questions, having conversations • Using body language to communicate needs and interests • Understanding emotions and what to do about them • Social attention, imitation, perspective taking • Taking turns, following someone else’s agenda/plan • Building flexibility, not getting “stuck” • Recognizing that rigid/repetitive behavior are an attempt to self-soothe or create a predictable world, increase under stress.
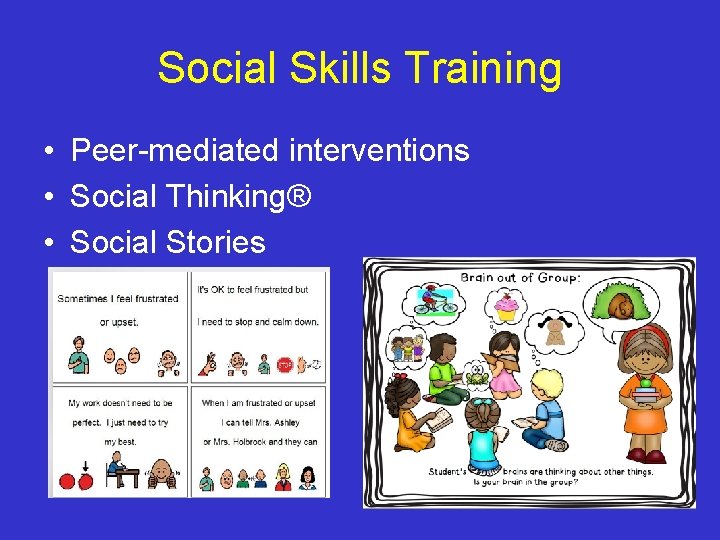
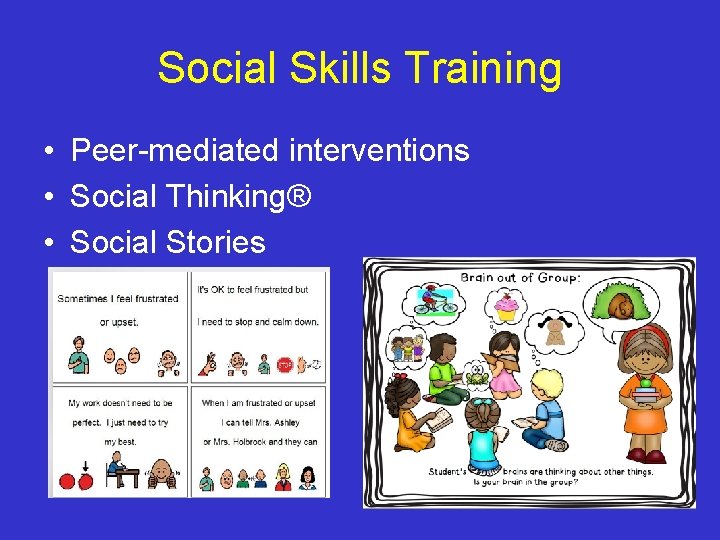
Social Skills Training • Peer-mediated interventions • Social Thinking® • Social Stories
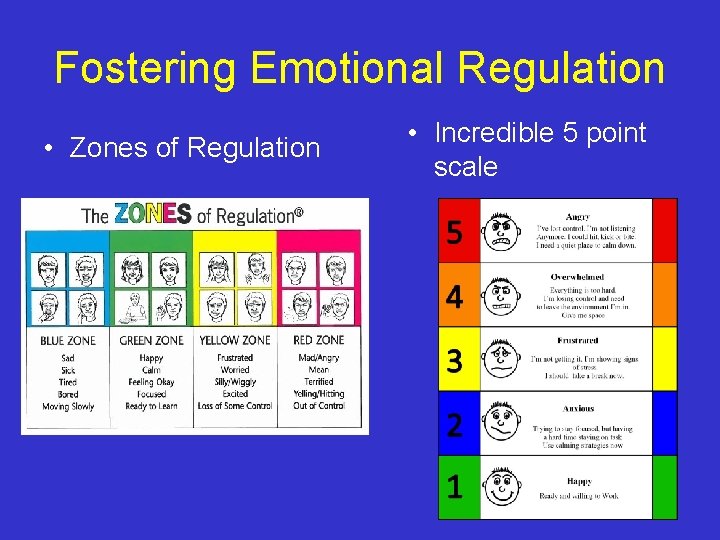
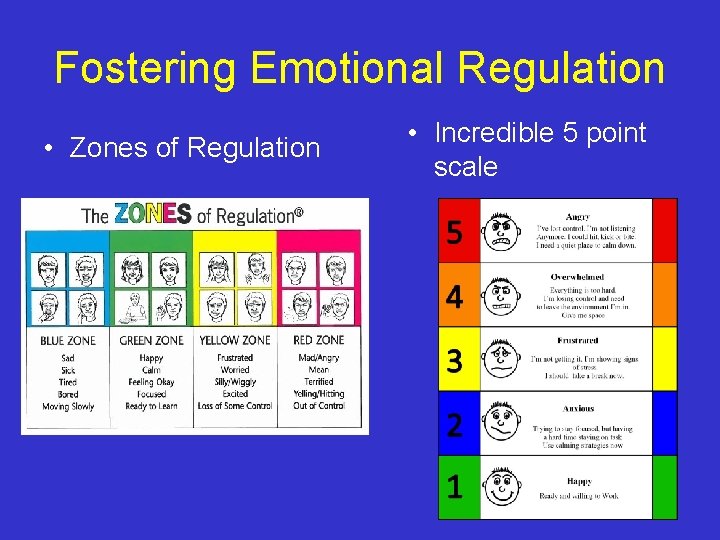
Fostering Emotional Regulation • Zones of Regulation • Incredible 5 point scale
Other Management • Medication – – To address co-morbid conditions Tenex for hyperactivity/aggression or unsafe behaviors SSRIs for anxiety or compulsive behaviors Stimulants for executive functioning. / hyperactivity • Biological therapies (limited to no evidence) – Restricted diets – Nutritional supplements and vitamins – Omega supplement
4. The Educational Management of ASD
3 -21 yo : Special Education Division of the Public Schools • IDEA Part B, requires that states provide a free appropriate public education in the least restrictive environment for children with disabilities ages 3 through 21; • State of Michigan provides it to the age of 25 years • Section 504 of the Rehabilitation Act requires that schools make “reasonable accommodations” to ensure that children are not denied a “free and appropriate public education because of a disability”
IDEA: Individuals with Disabilities Education Act 6 Principles of IDEA 1. 2. 3. 4. 5. Free and appropriate public education Appropriate Evaluation Individualized Education Program Least Restrictive Environment Parent and student participation in decision making 6. Procedural safeguards
IEP-101: Getting the process started • Parent or professional can refer • Request ‘evaluation for special education services’ in WRITING • Parents must sign consent • Evaluation completed within 30 school days of consent
IEP-101: Evaluation • MUST include: – Educational history – Specialist assessments • MAY include: – Intelligence and achievement testing – Medical exam – Family history – Home visit
IEP-101: Content of an IEP • Individualized Education Plan • Parent and Teacher Concerns • Students’ current performance and strengths • Goals and benchmarks • Services, structure of day, transportation • Plan for evaluation – Annual review of IEP – Full re-evaluation every 3 years

Services Provided on an IEP • • Special education services in LRE Speech/language therapy Occupational therapy Psychological services/ individual counseling/ family counseling • Mobility Services (wheelchair ramp, elevator) • Communication services (facilitated communication, keyboarding) • Transportation
Special Education: Role of PCP • Referral – Provide letter template for parents – Walk them through the steps and key timelines • Communication – With teacher, with IEP team – May be present at evaluation – Document diagnoses as needed • Follow-up – Address at WCC – Advocate if need further support needed – Evaluate new concerns or suggested diagnoses
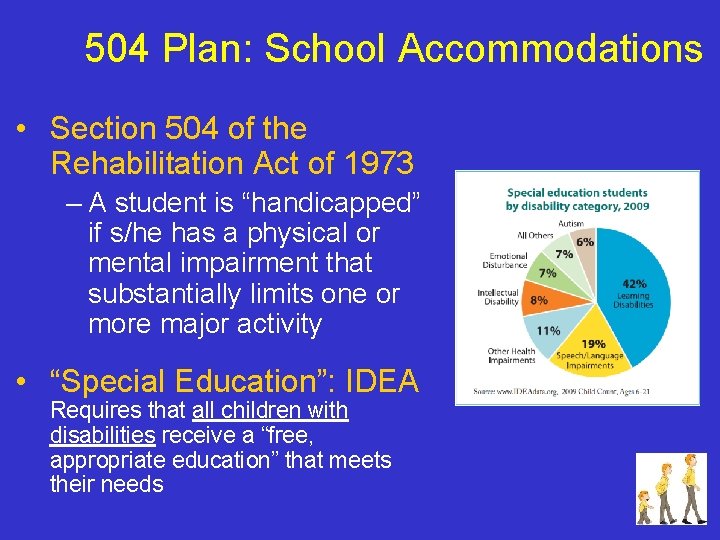
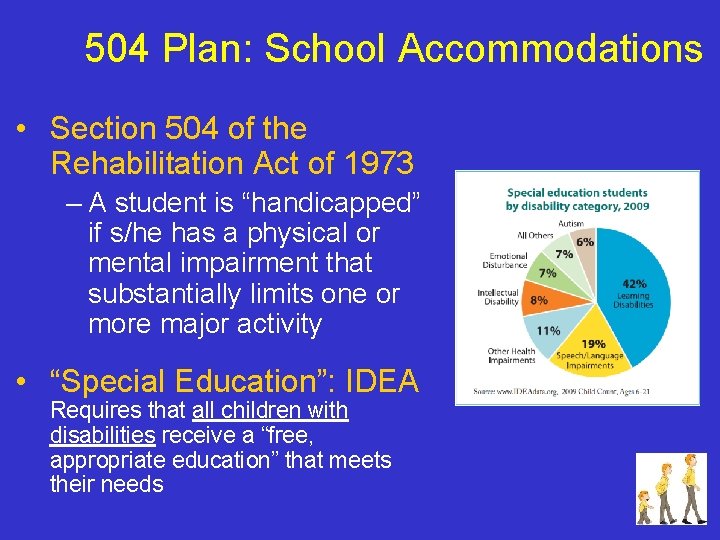
504 Plan: School Accommodations • Section 504 of the Rehabilitation Act of 1973 – A student is “handicapped” if s/he has a physical or mental impairment that substantially limits one or more major activity • “Special Education”: IDEA Requires that all children with disabilities receive a “free, appropriate education” that meets their needs
IEP Components for children with autism spectrum disorders
Basic IEP Components • Date (when is our next chance to easily suggest new services? ) • Qualifying diagnosis (make sure it’s correct) • Summary and Key Findings (gives sense of how well they know the child) • Accommodations • Goals (appropriate to child’s current functioning; include self-regulation, social skills, task independence) • Service Grid • Additional Info • Extended School Year (look for services in grid also)
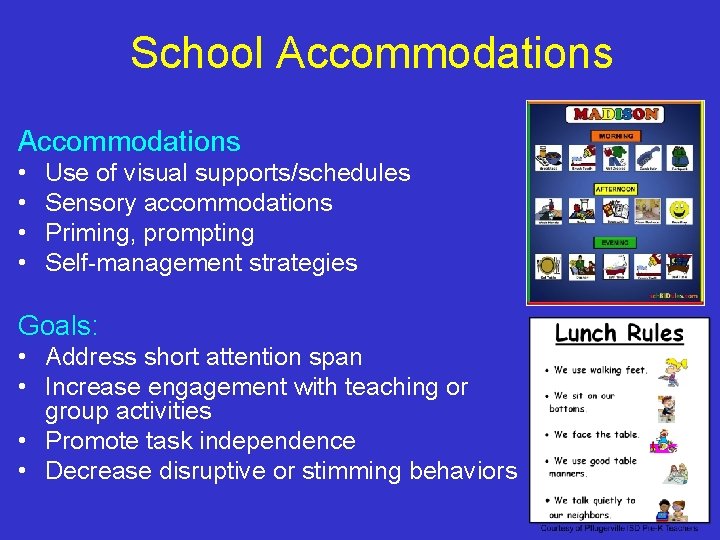
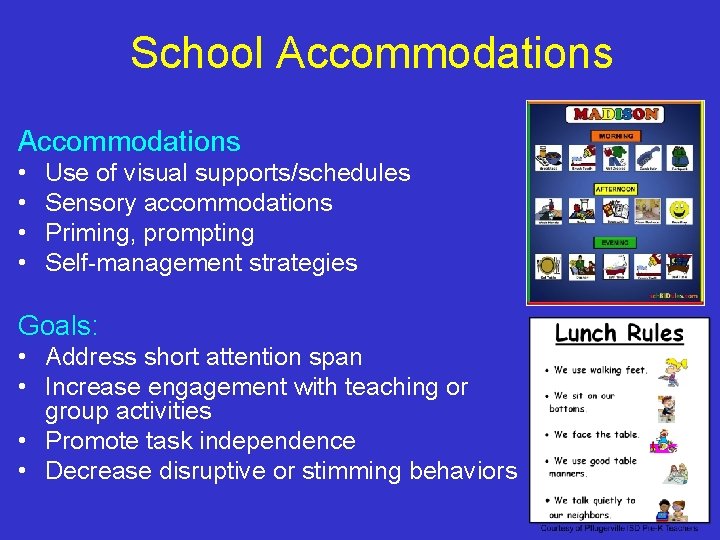
School Accommodations • • Use of visual supports/schedules Sensory accommodations Priming, prompting Self-management strategies Goals: • Address short attention span • Increase engagement with teaching or group activities • Promote task independence • Decrease disruptive or stimming behaviors

Sensory Accommodations for the Classroom
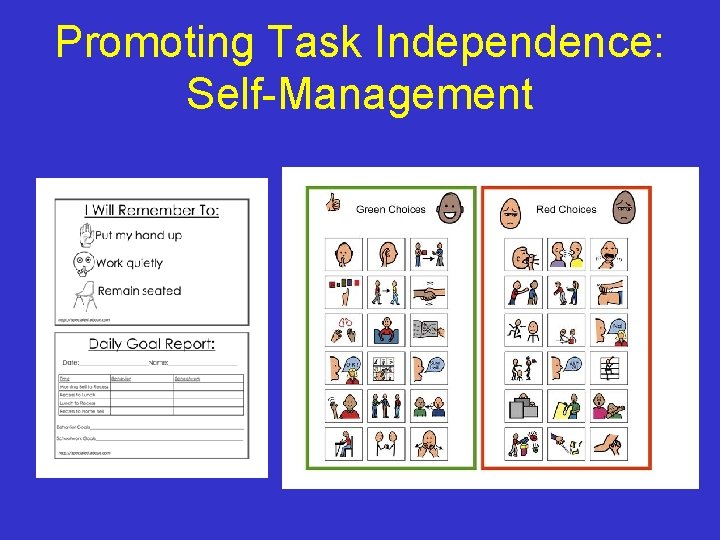
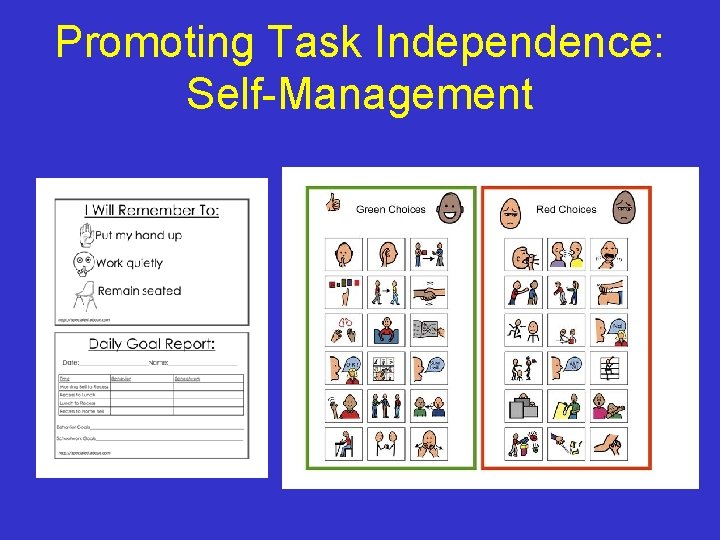
Promoting Task Independence: Self-Management
Communicating with Teachers
Service Grid • Consult for parents with specialists or teacher on regular basis • In home parent training • Autism teacher consultant • Direct services: – SLT – OT – Social skills group (SLP or SW) • Inclusion vs. sub separate placement • Summer services
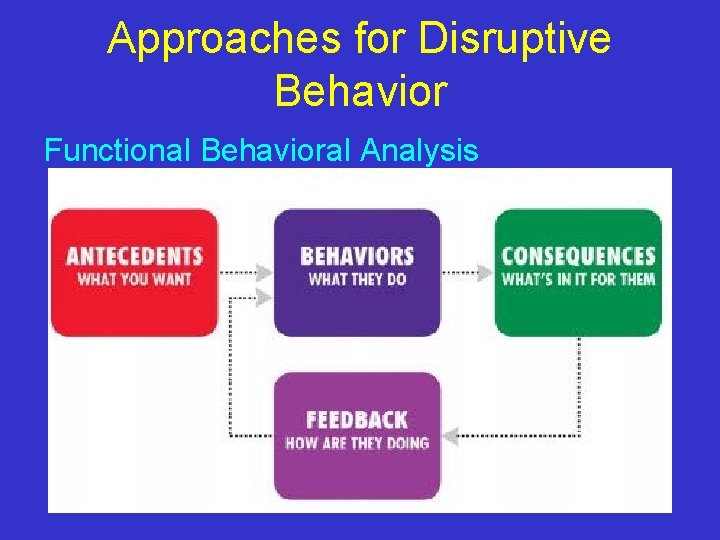
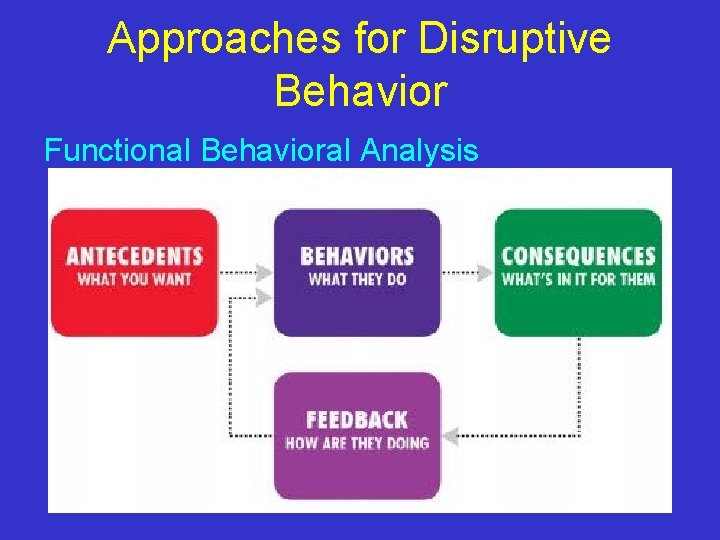
Approaches for Disruptive Behavior Functional Behavioral Analysis
Summing Up • Help parent arrange outpatient and schoolbased services to build skills in deficit areas: – Communication – Social/play – Behavior/emotions – Academics/independence • And help the parents themselves build confidence and skills to implement approaches at home, since this improves outcomes.
The Role of the Physician • Screen – Using a validated screening tool • Suspect – Autism if a failed screen • Direct – Patient for a comprehensive ASD evaluation
Autism A. L. A. R. M. • A: Autism is prevalent • L: Listen to parents • A: Act early • R: Refer • M: Monitor www. firstsigns. org

Thank you! prachis@umich. edu