Fetal Alcohol Spectrum Disorder Caitlin Carew PGY3 Pediatrics



- Slides: 41
Fetal Alcohol Spectrum Disorder Caitlin Carew PGY-3 Pediatrics CHEO Telehealth Rounds March 31, 2017
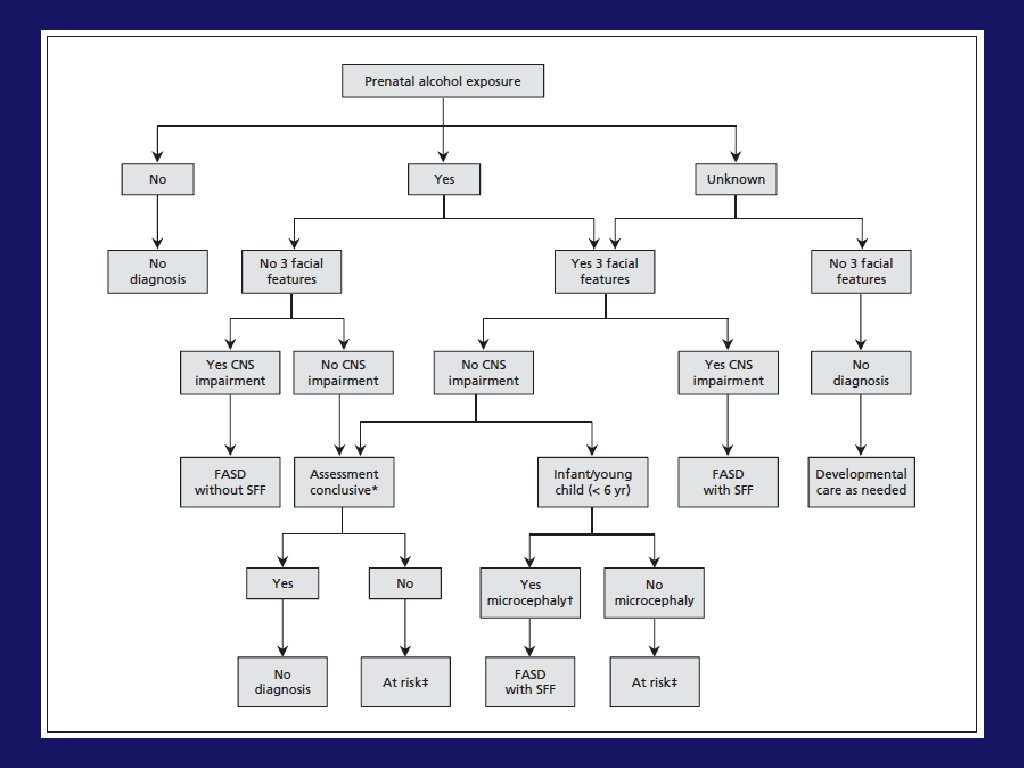
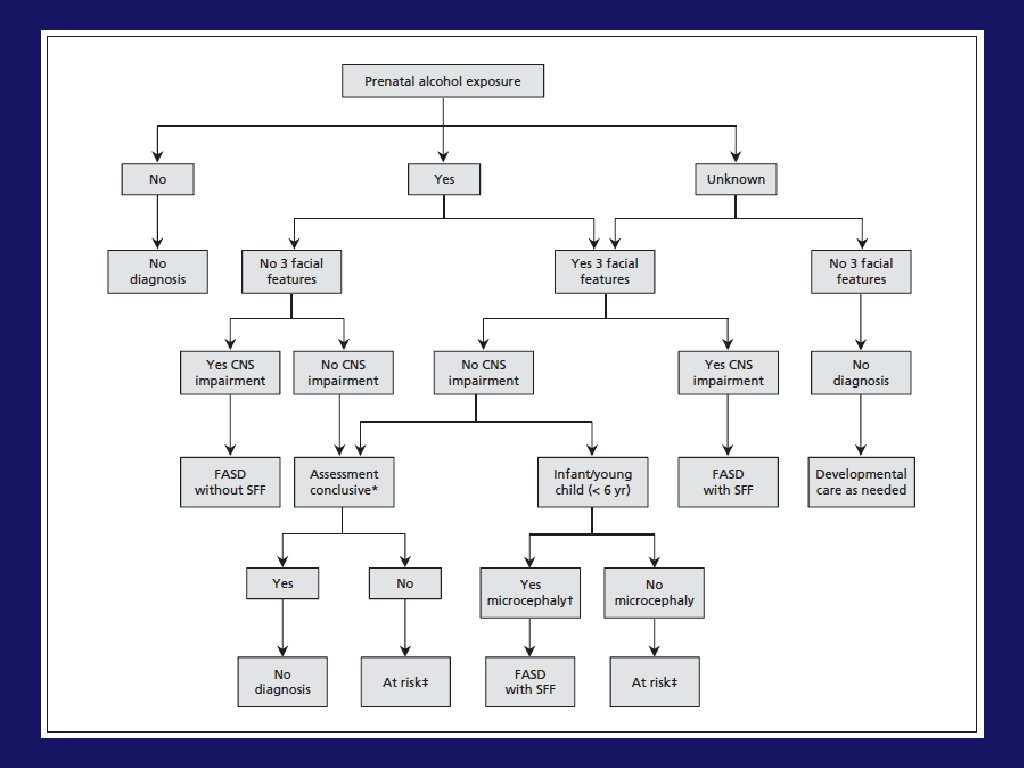
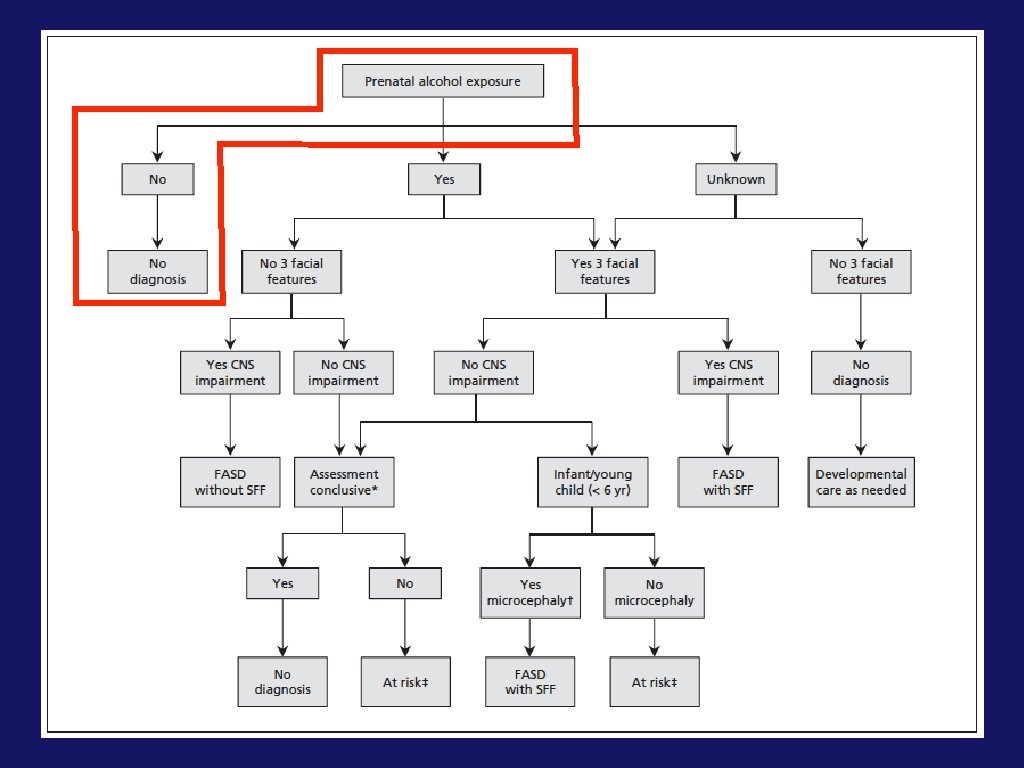
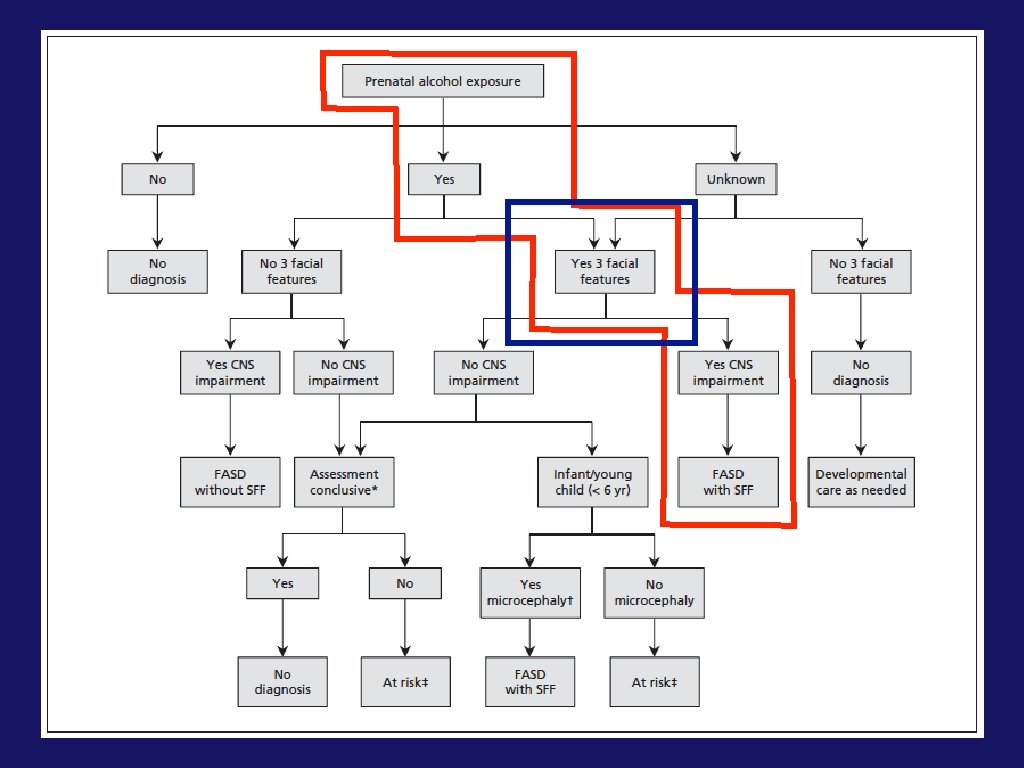
What is FASD? • A diagnostic term that describes a group of effects that result from prenatal exposure to alcohol
Prevalence of FASD • 2015 Canadian Guidelines estimate that 1/100 people meet diagnostic criteria for FASD
Etiology of FASD
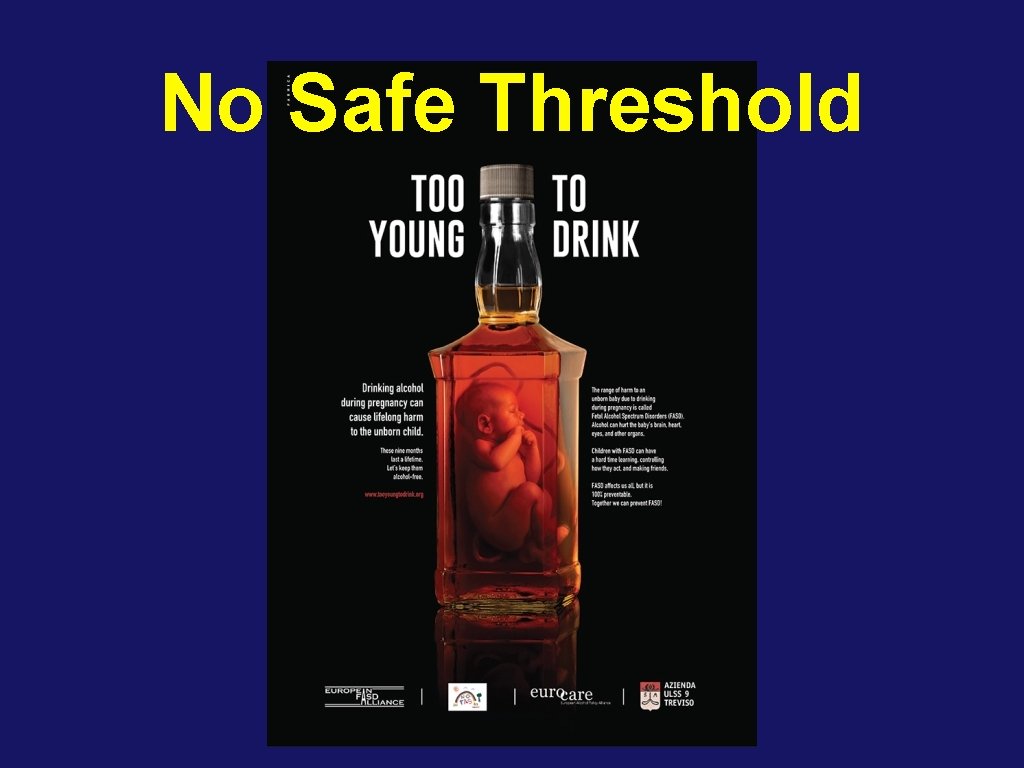
No Safe Threshold
Risk Factors for FASD • Child Factors • Sibling with FASD • Lived/living in foster care • Current or past involvement with child protective services

Risk Factors for FASD • Maternal Factors • Low maternal educational attainment • Higher maternal age (>30) • Poor maternal nutrition in pregnancy • Higher gravidity and parity • History of miscarriages and stillbirths
Risk Factors for FASD • Maternal Factors Continued • Substance use including tobacco • Mental health disorders • Social isolation in pregnancy • Intimate partner violence • Poverty
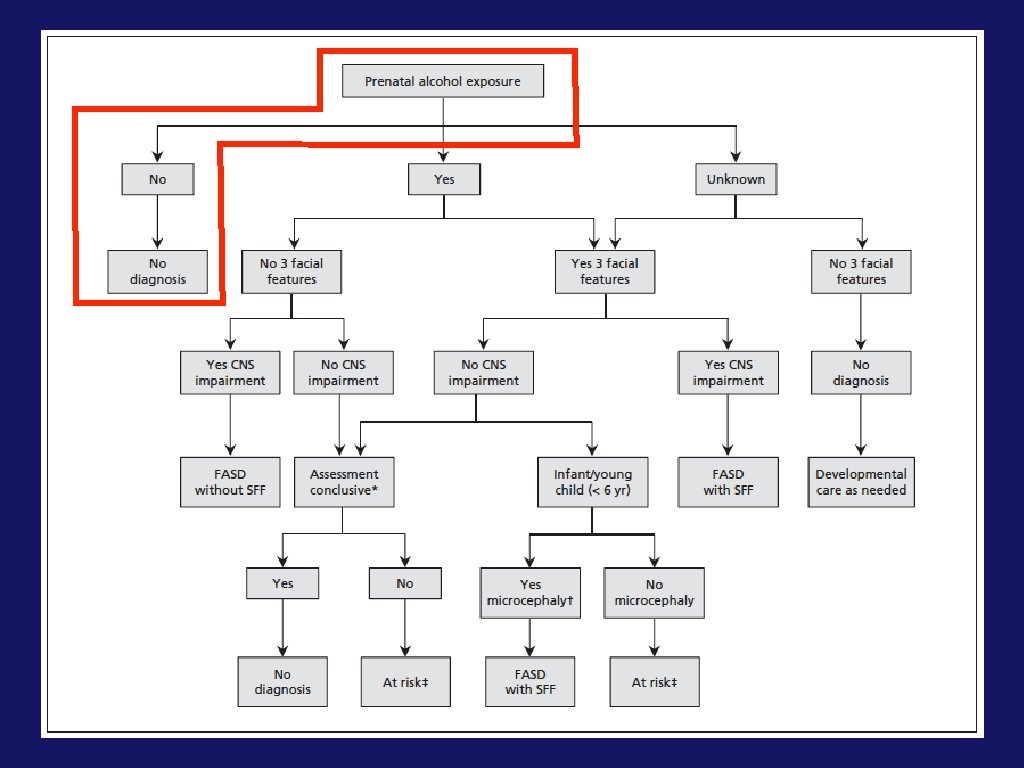
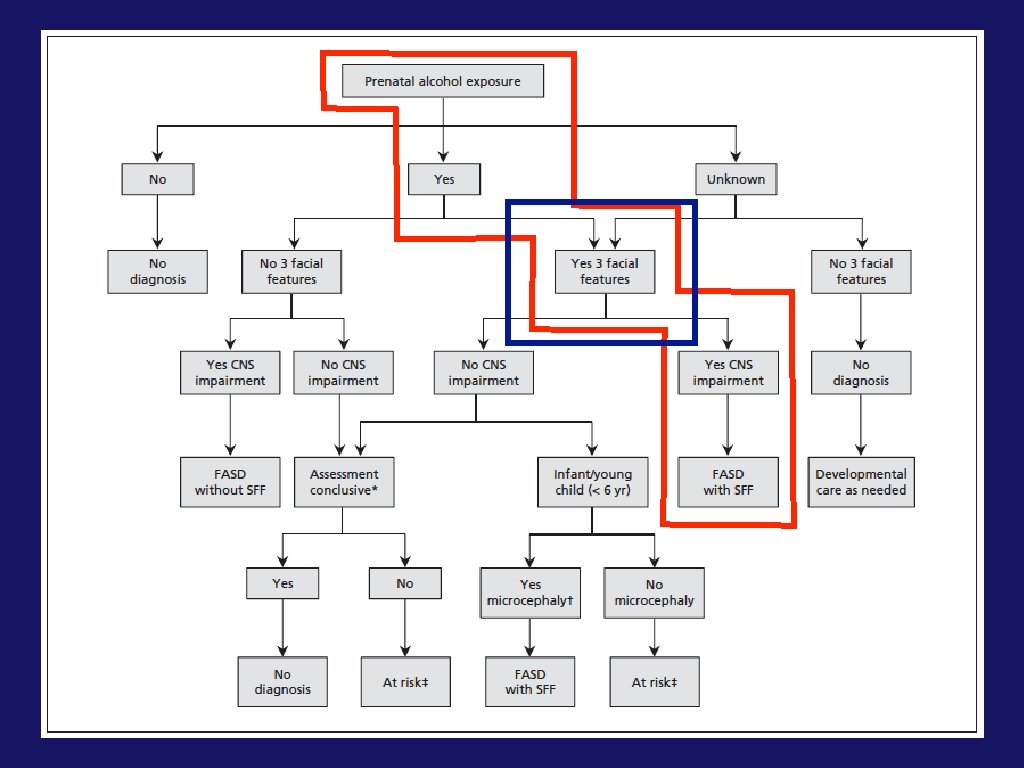
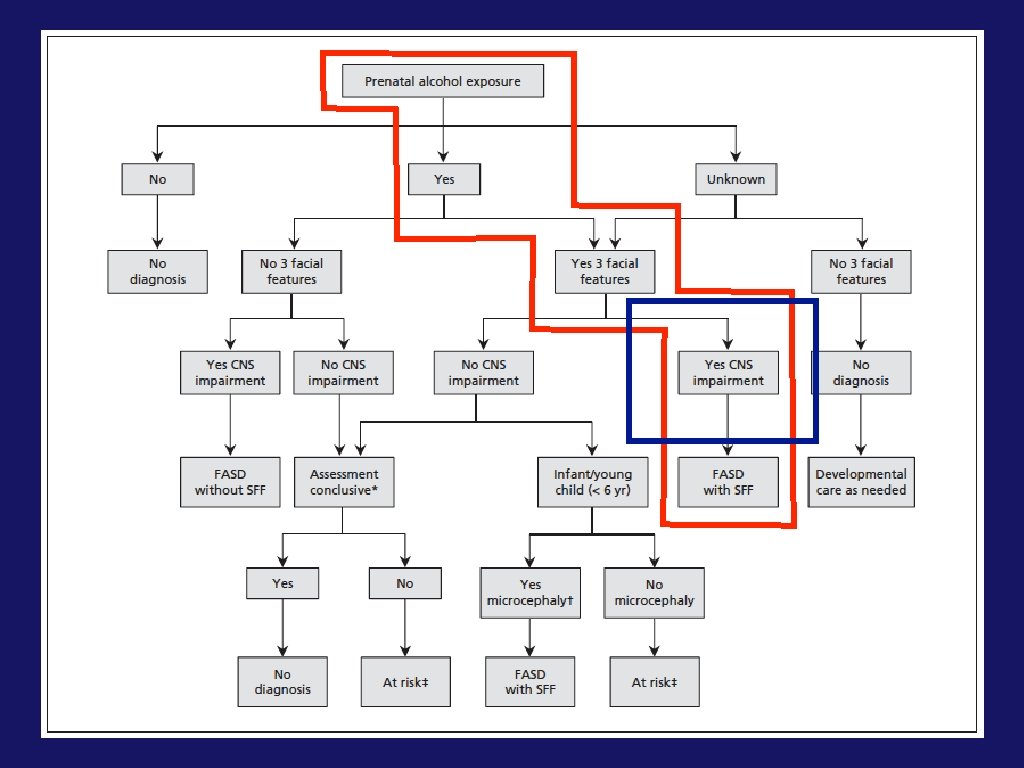
What is FASD?


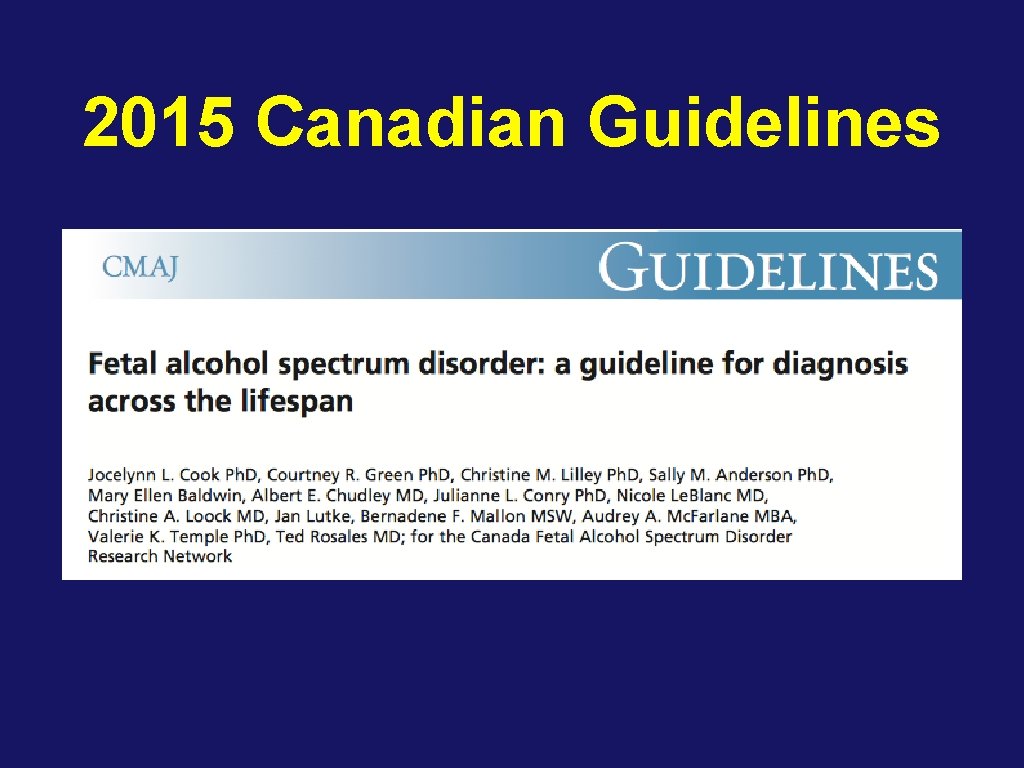
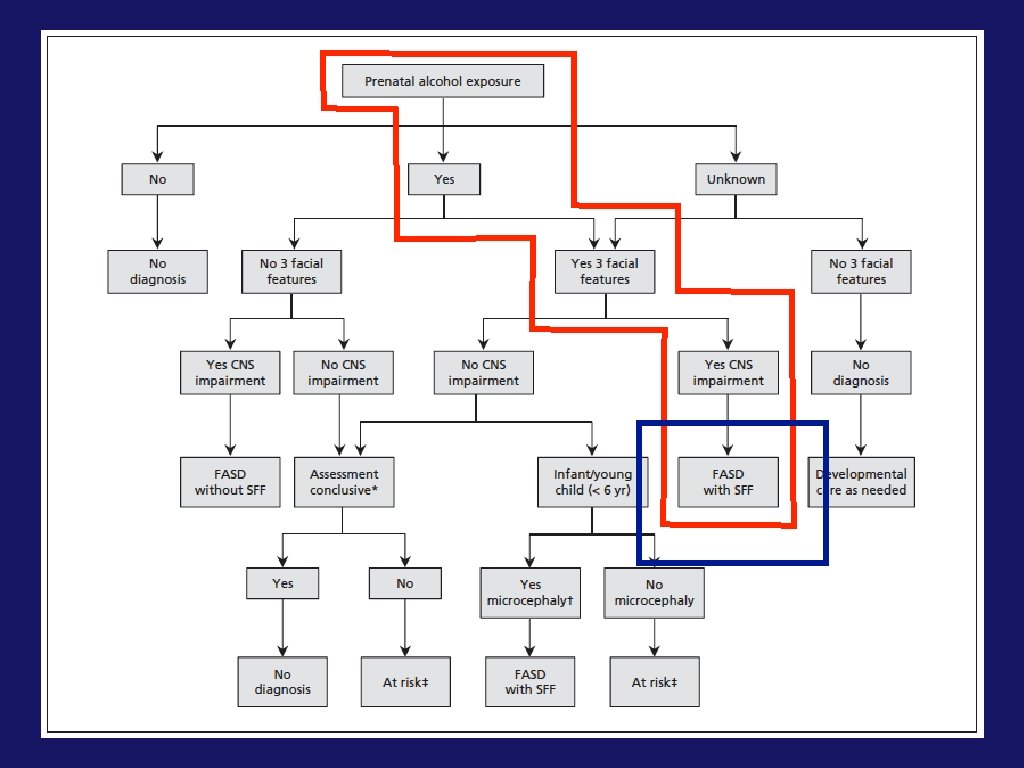
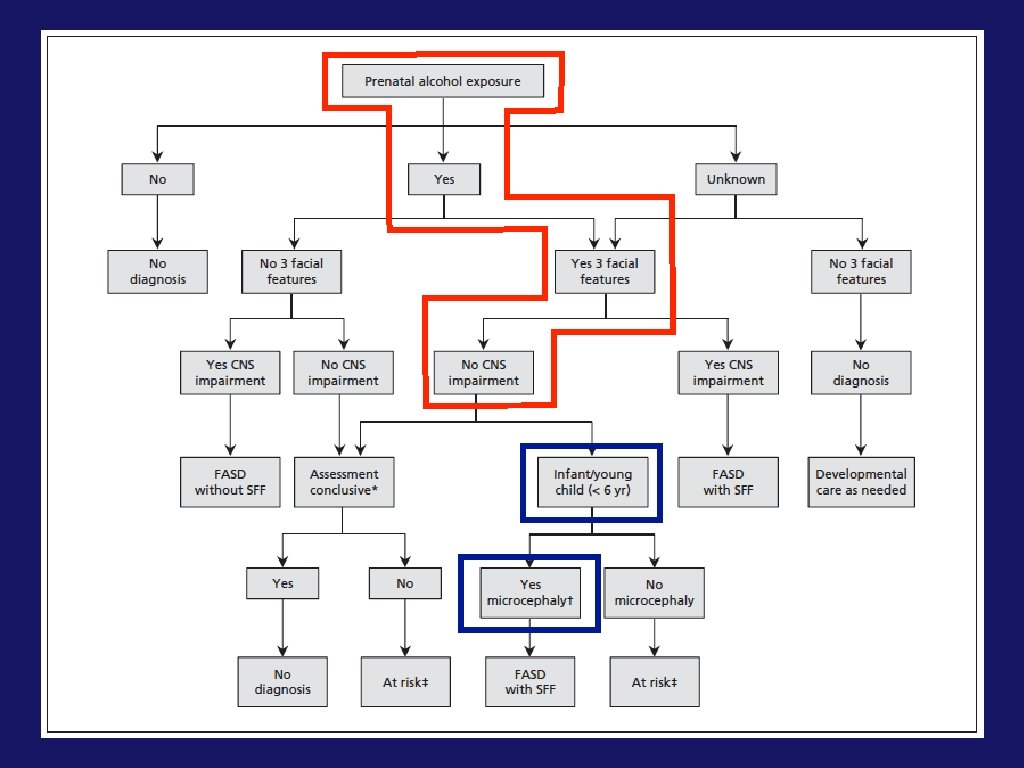
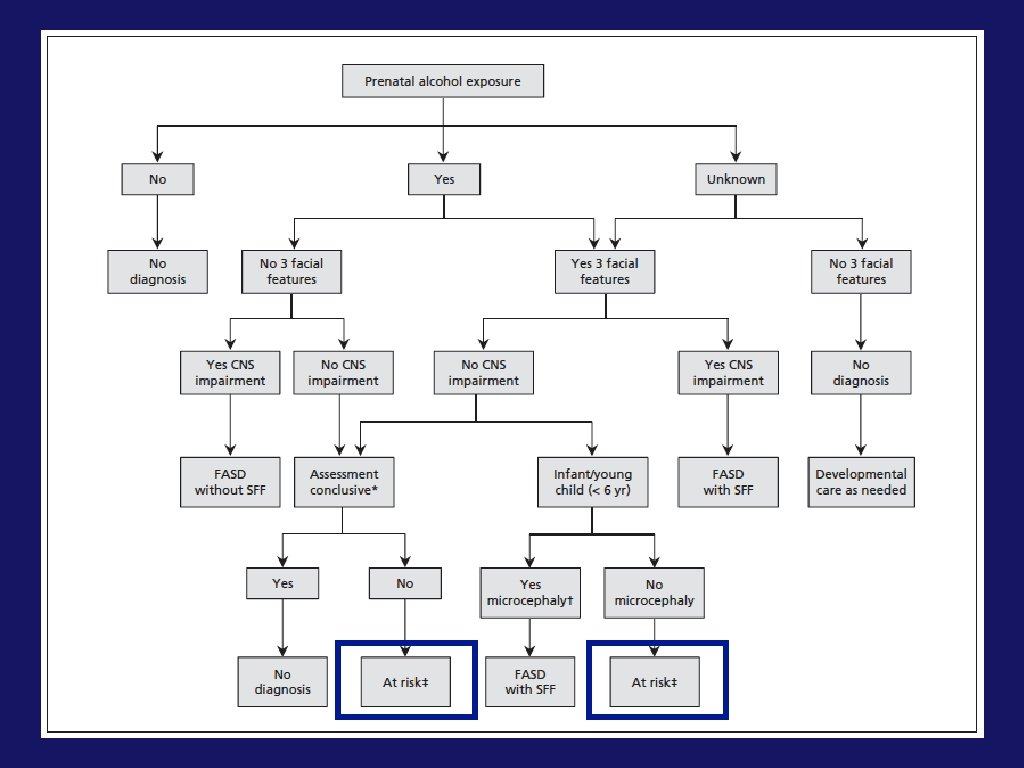
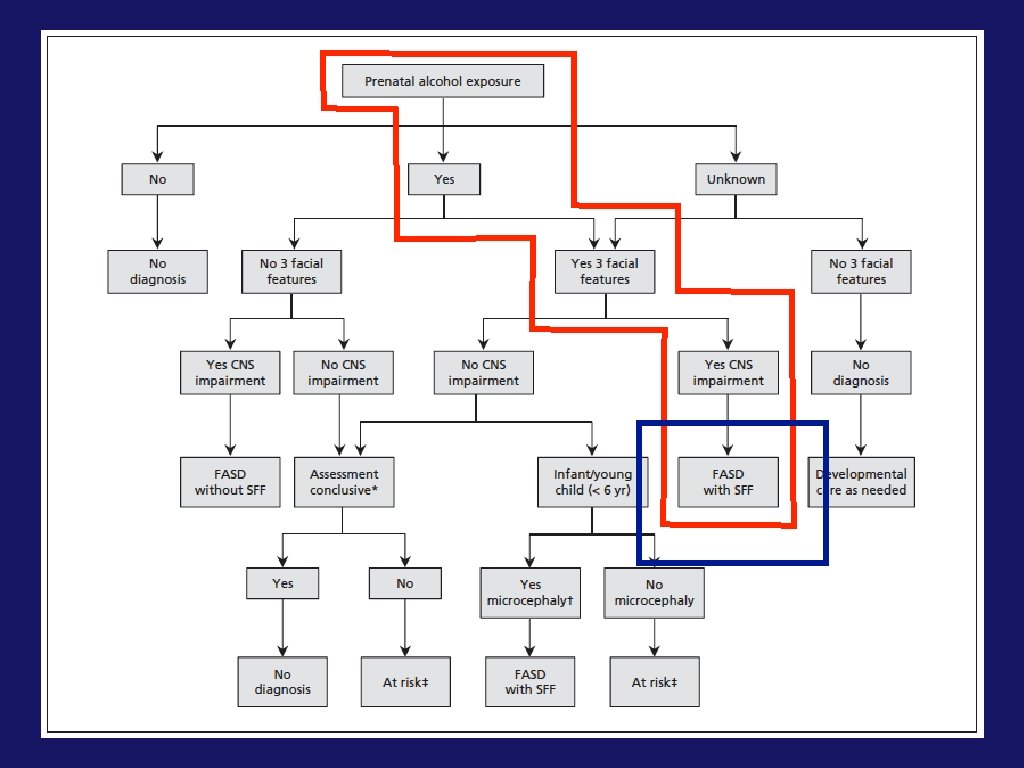
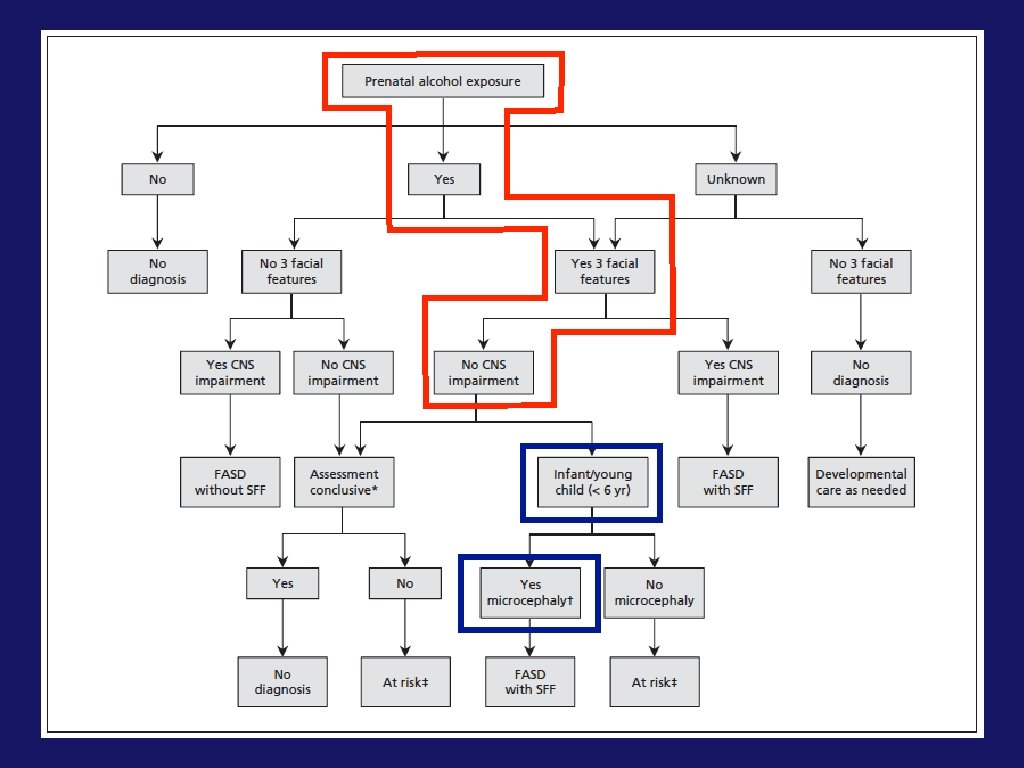
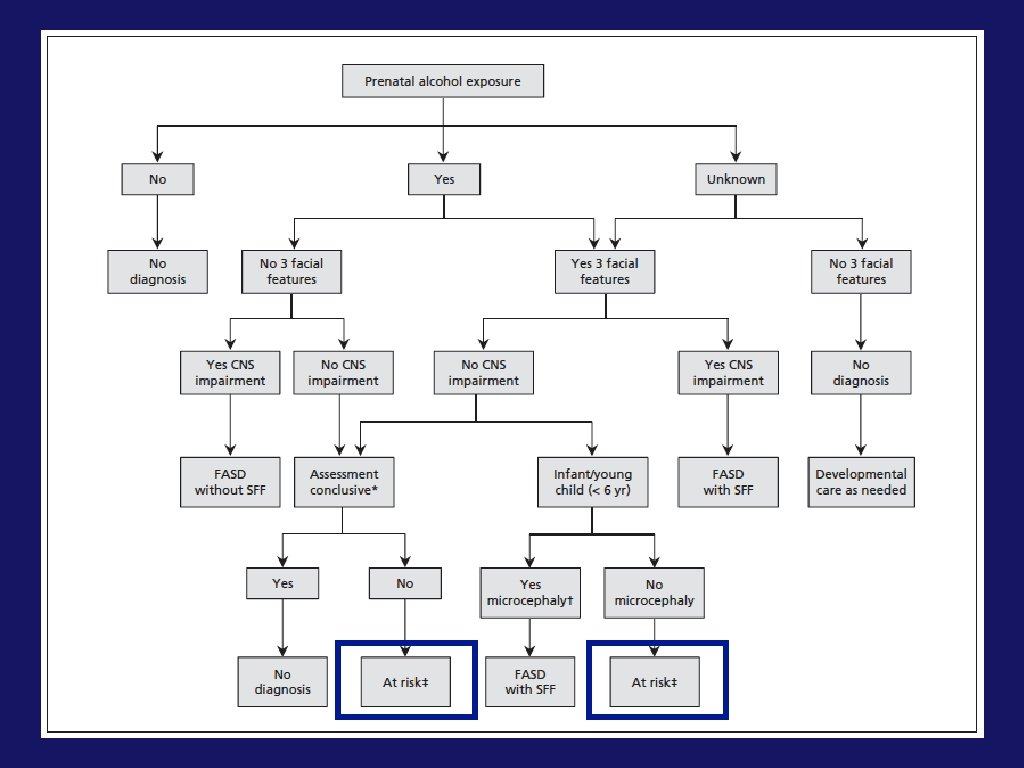
2015 Canadian Guidelines
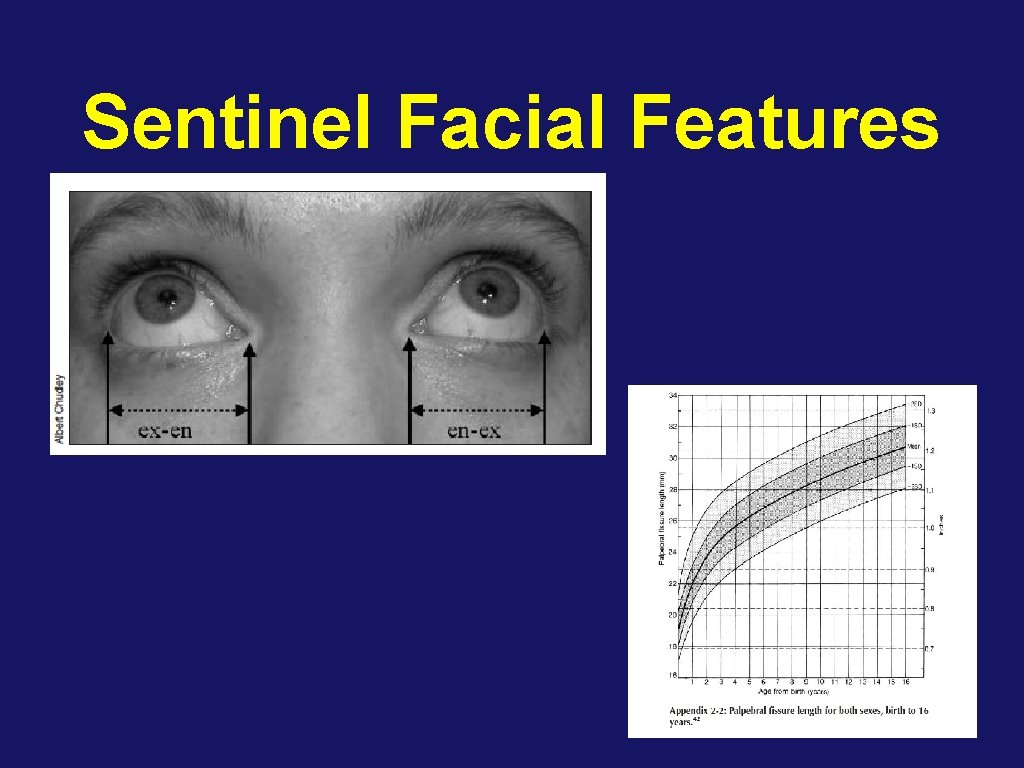
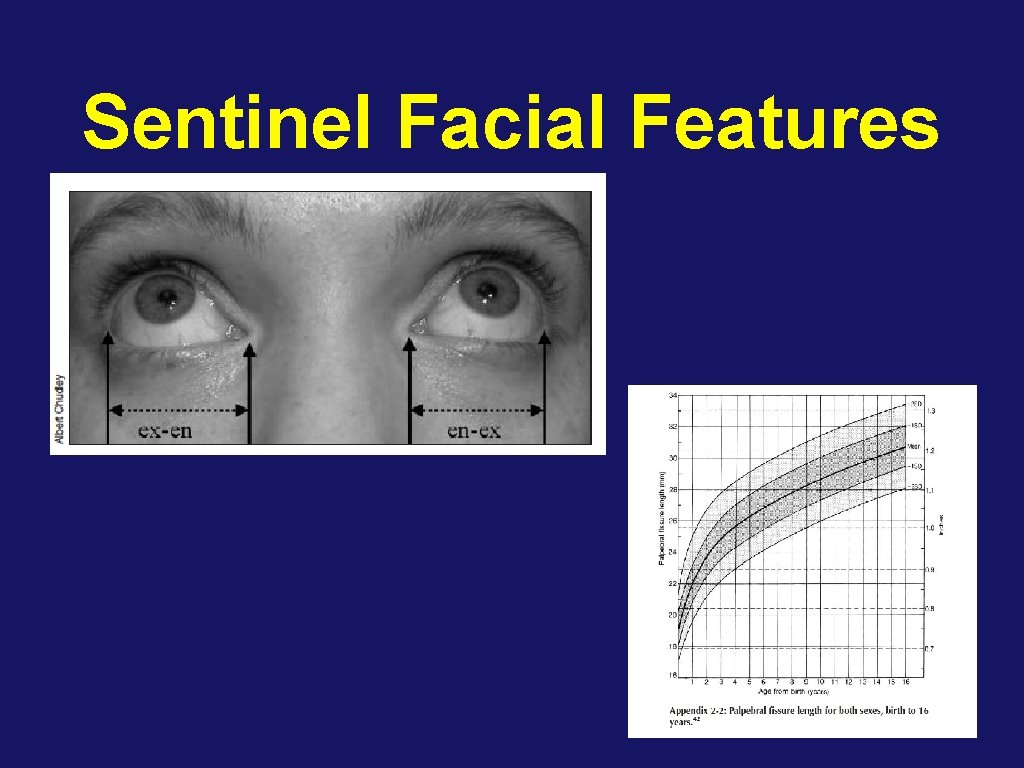
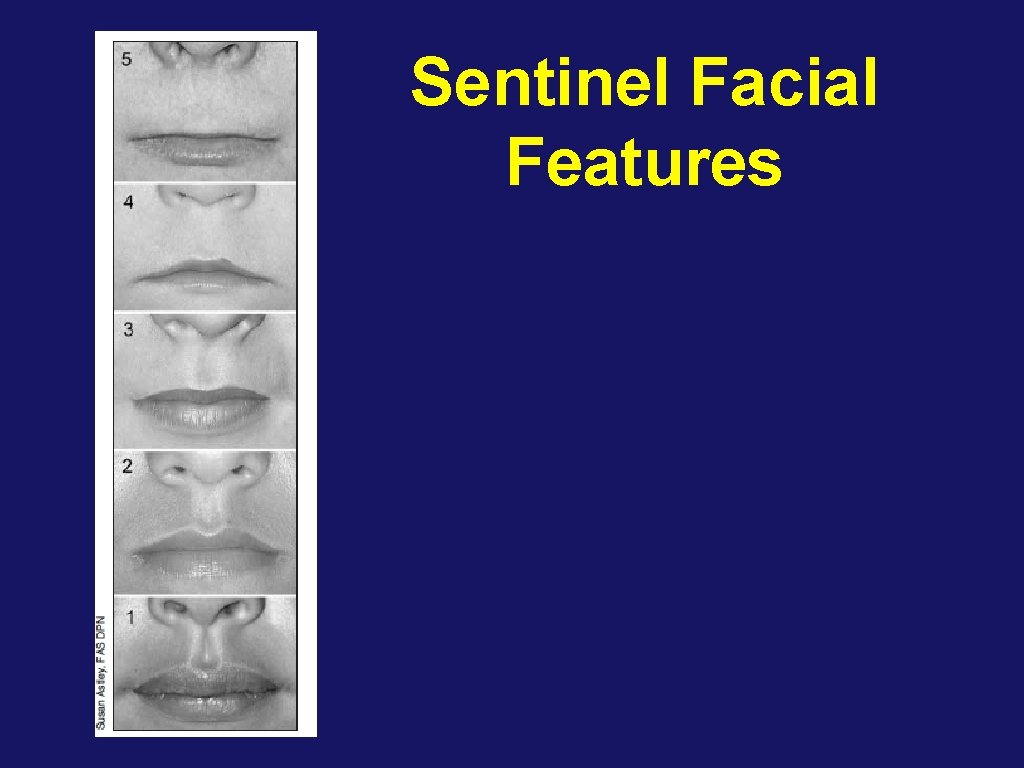
Sentinel Facial Features
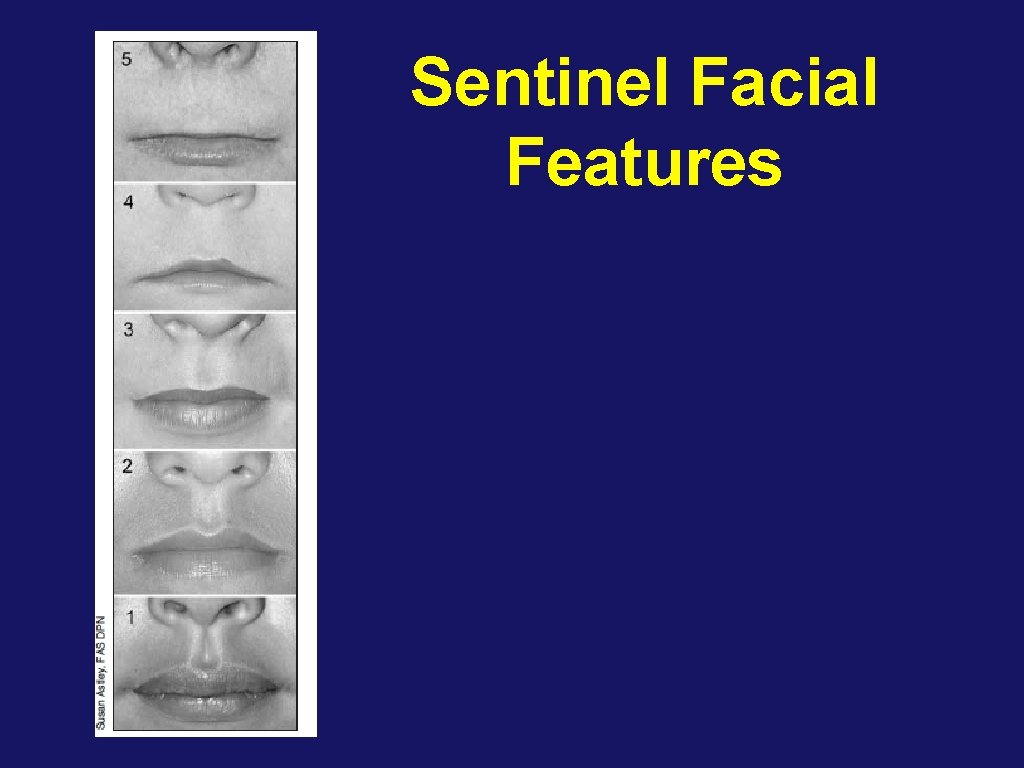
Sentinel Facial Features
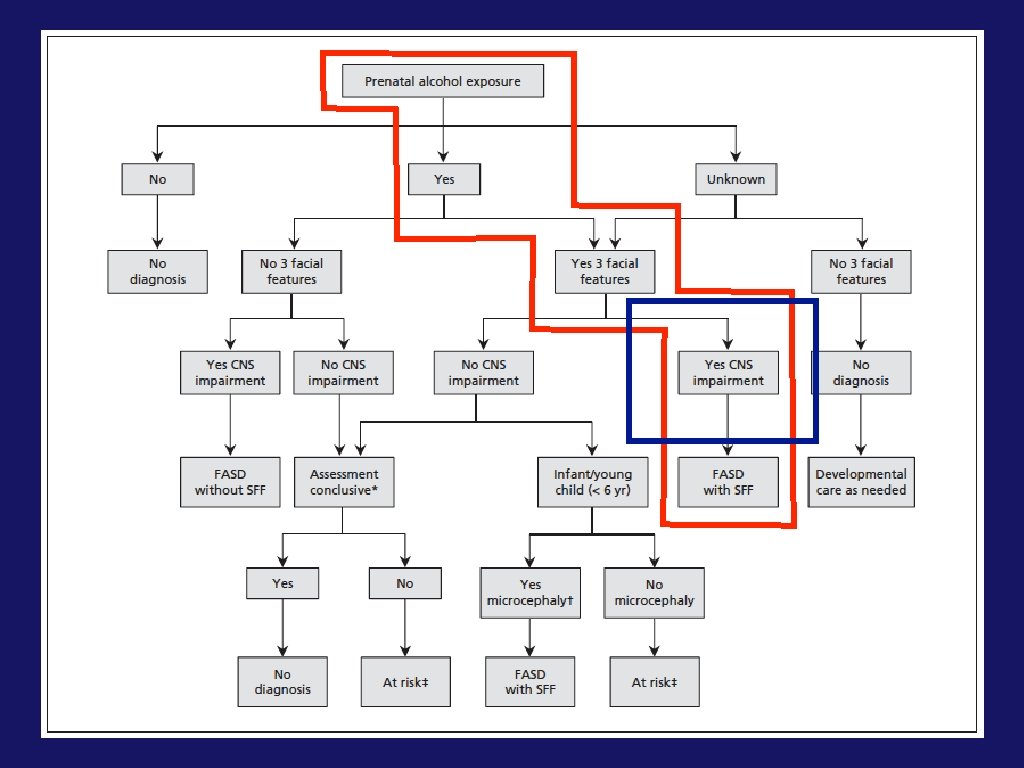
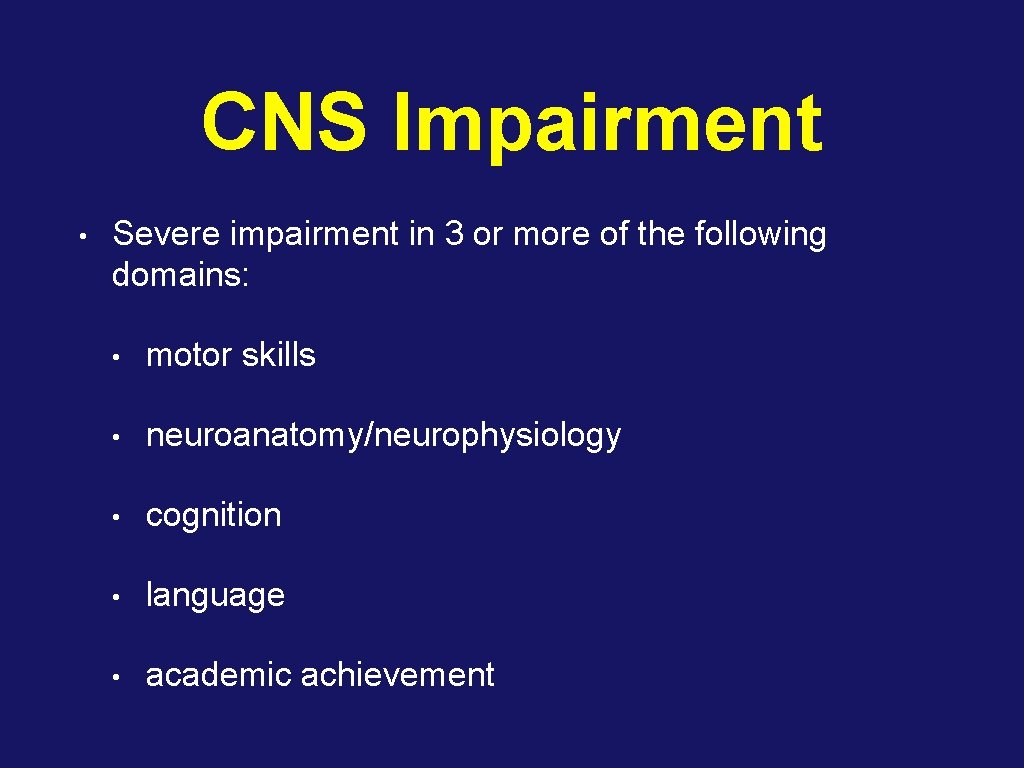
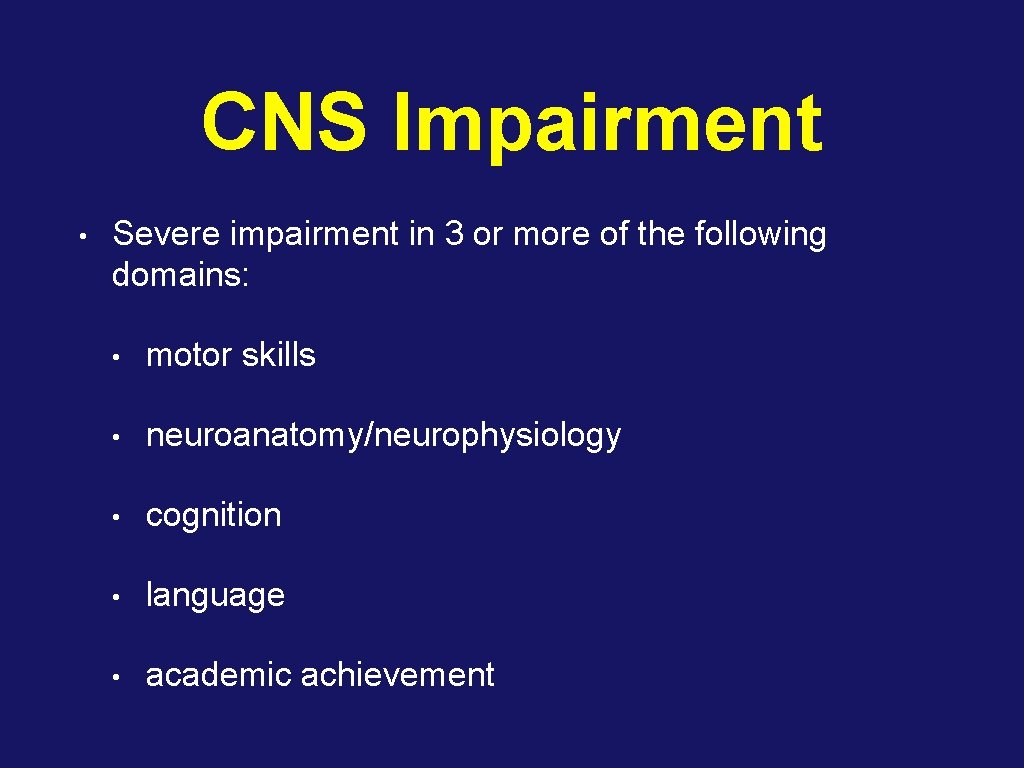
CNS Impairment • Severe impairment in 3 or more of the following domains: • motor skills • neuroanatomy/neurophysiology • cognition • language • academic achievement
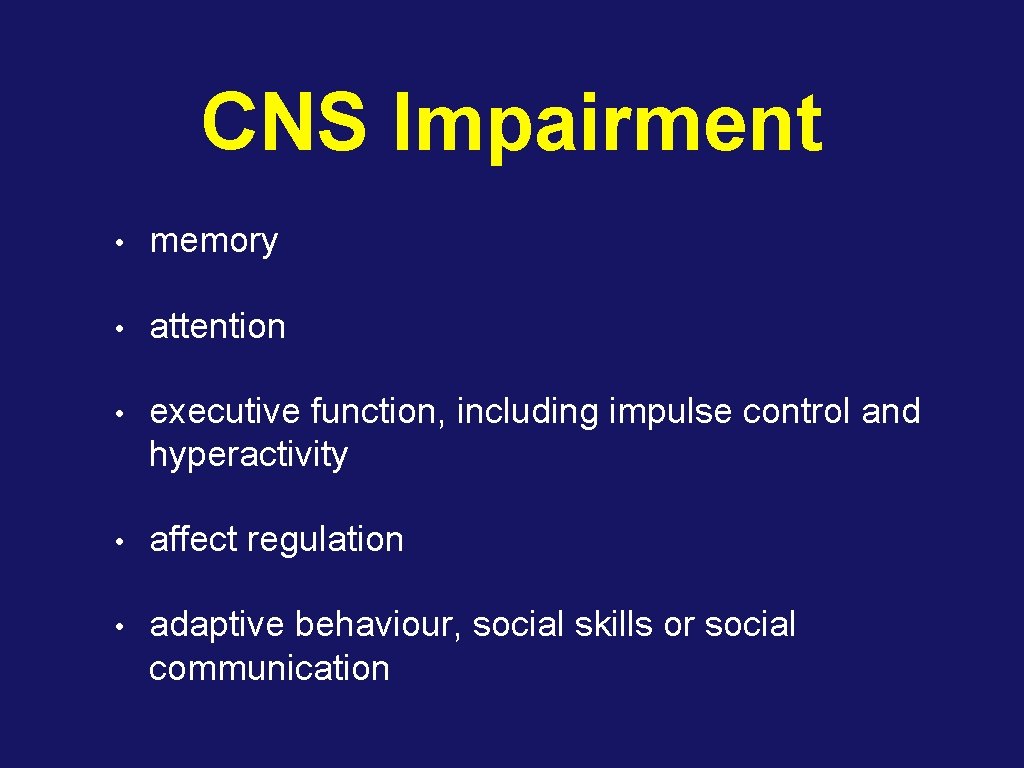
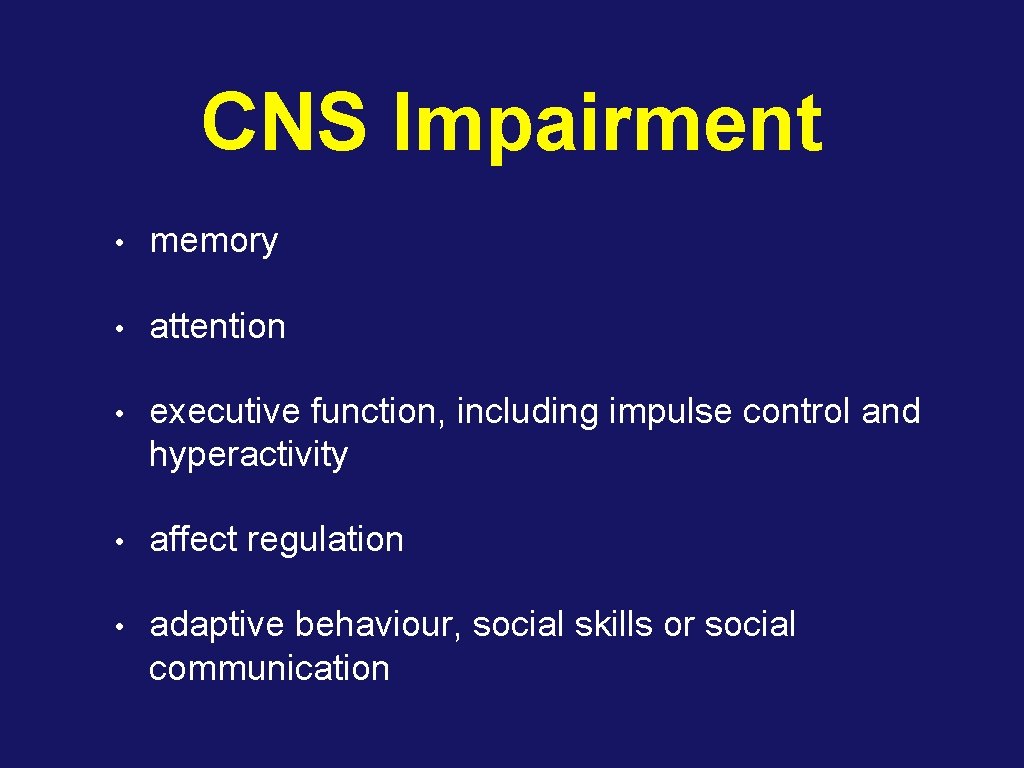
CNS Impairment • memory • attention • executive function, including impulse control and hyperactivity • affect regulation • adaptive behaviour, social skills or social communication
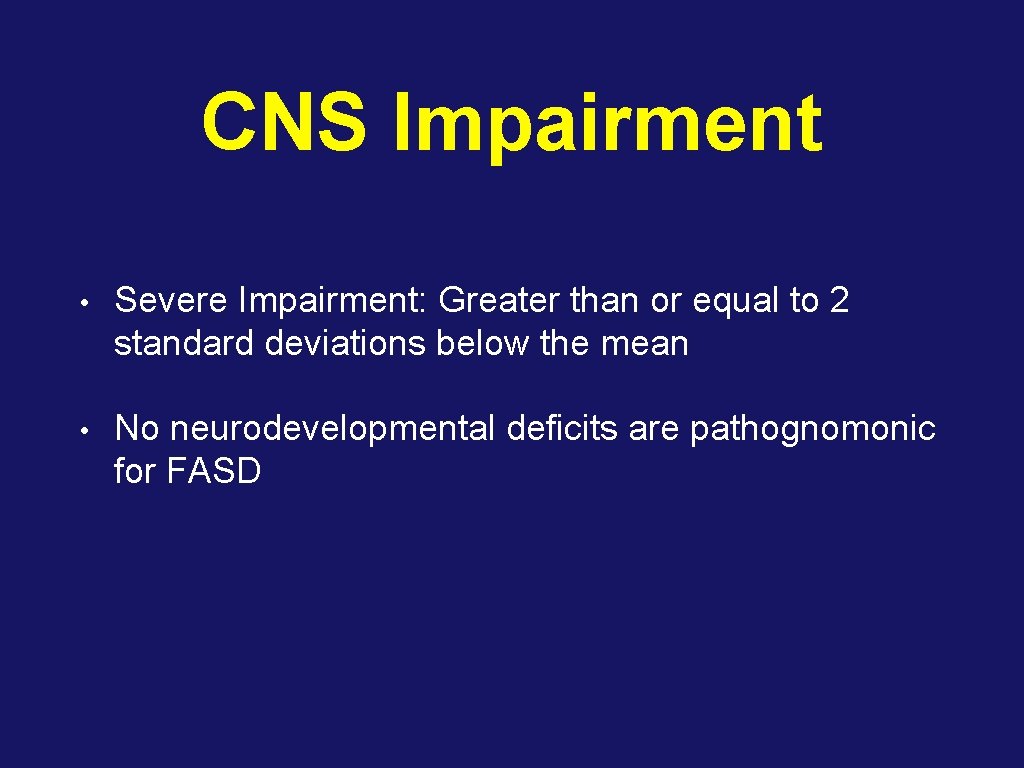
CNS Impairment • Severe Impairment: Greater than or equal to 2 standard deviations below the mean • No neurodevelopmental deficits are pathognomonic for FASD
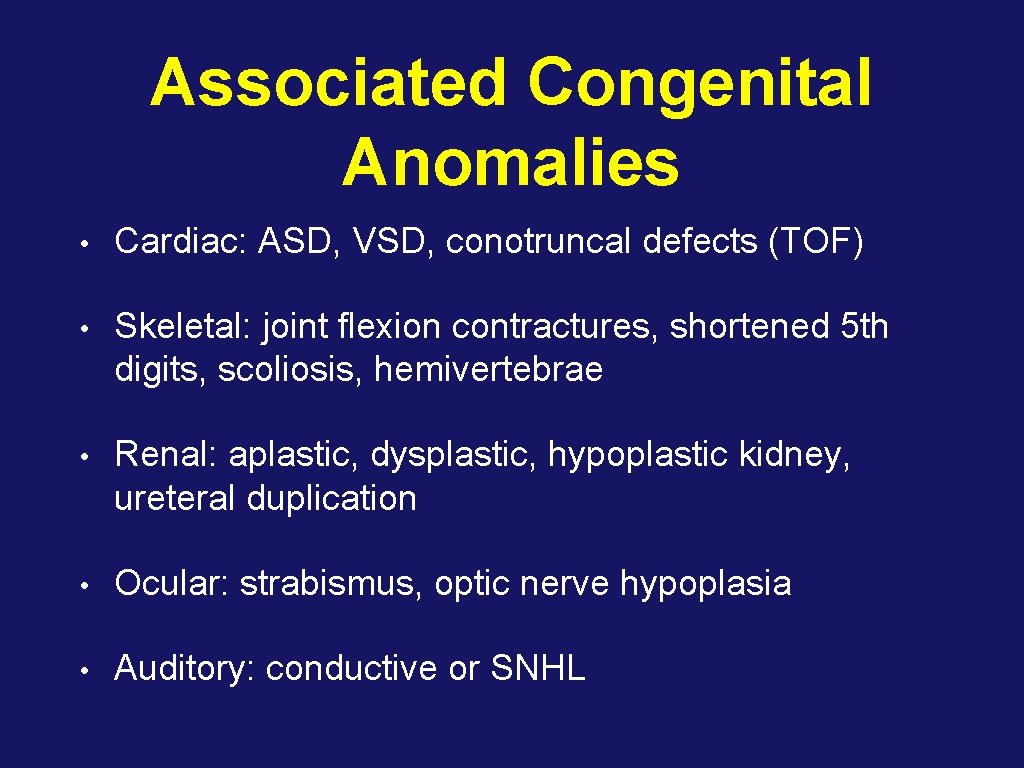
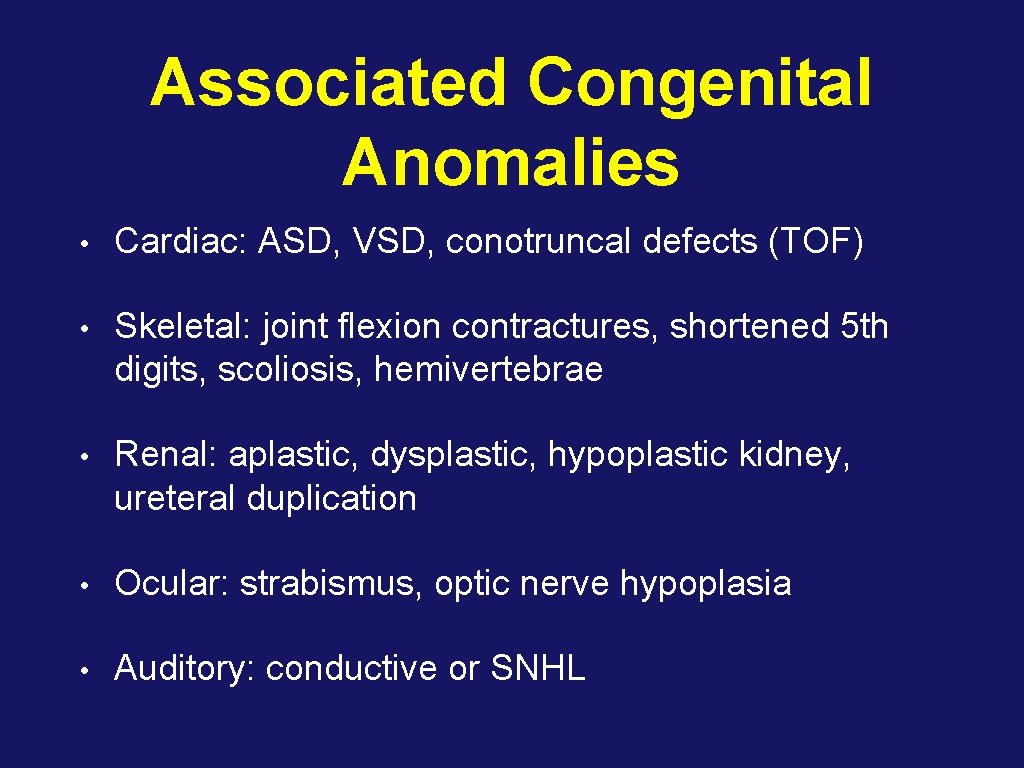
Associated Congenital Anomalies • Cardiac: ASD, VSD, conotruncal defects (TOF) • Skeletal: joint flexion contractures, shortened 5 th digits, scoliosis, hemivertebrae • Renal: aplastic, dysplastic, hypoplastic kidney, ureteral duplication • Ocular: strabismus, optic nerve hypoplasia • Auditory: conductive or SNHL
Management of FASD • An ounce of prevention…
Screen All Women • Abstainers • Low-risk drinkers • At-risk drinkers • Problem drinkers
T-ACE • Tolerance (2 or more drinks to feel effect) • Annoyed • Cut back • Eye opener
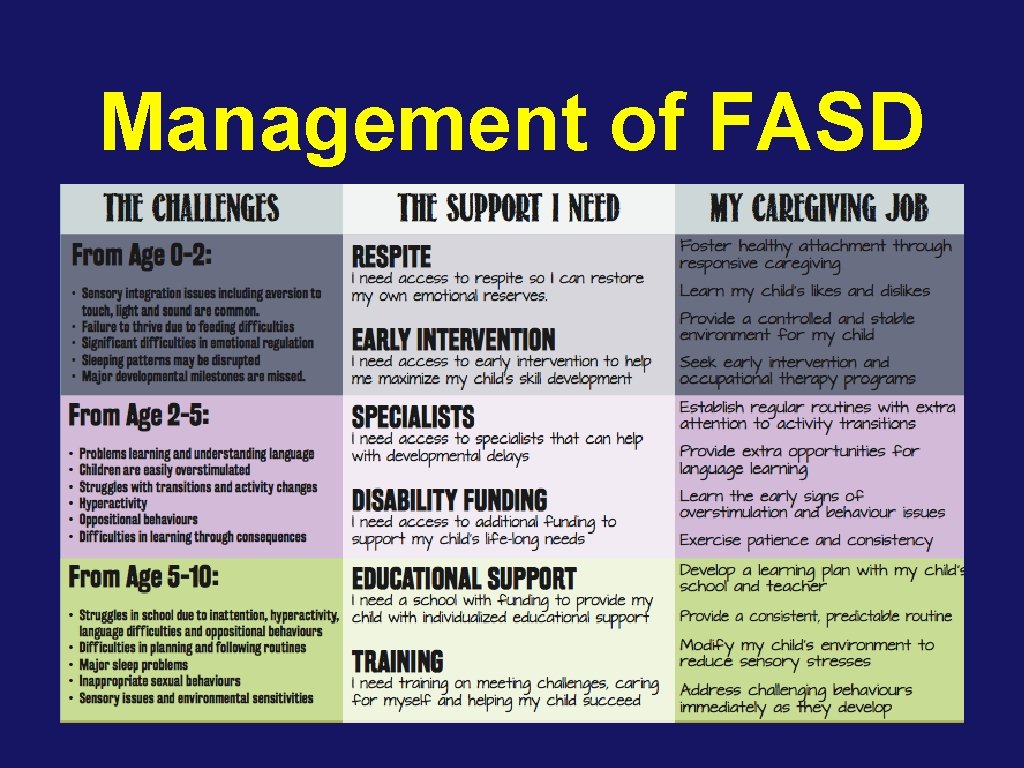
Management of FASD • Early diagnosis and intervention is important • Anticipatory guidance for parents
Management of FASD • Infancy: irritability, jitteriness • frequent, gentle handling • frequent eye contact and cuddling • avoid bouncing/sudden movements
Management of FASD • Young children: hyperactivity, inattention, cognitive impairment, emotional reactivity, learning disabilities, memory deficits, seizures • good structure and routine (transitions are hard) • teach acceptable interpersonal behaviour • maintain sense of self-worth
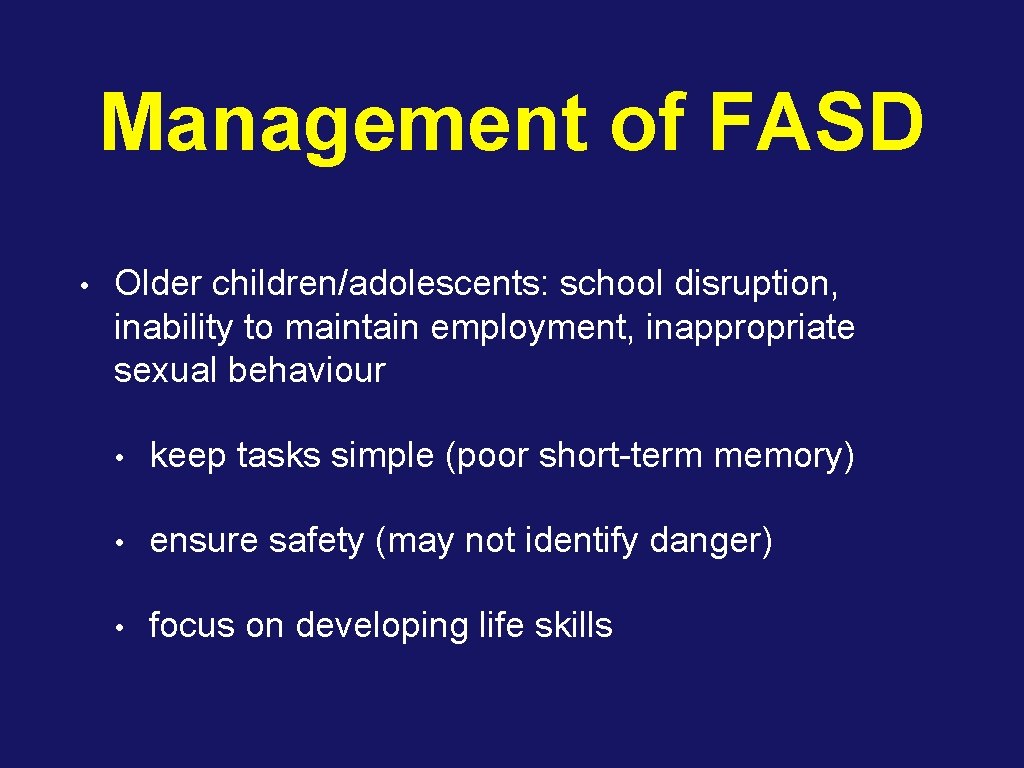
Management of FASD • Older children/adolescents: school disruption, inability to maintain employment, inappropriate sexual behaviour • keep tasks simple (poor short-term memory) • ensure safety (may not identify danger) • focus on developing life skills
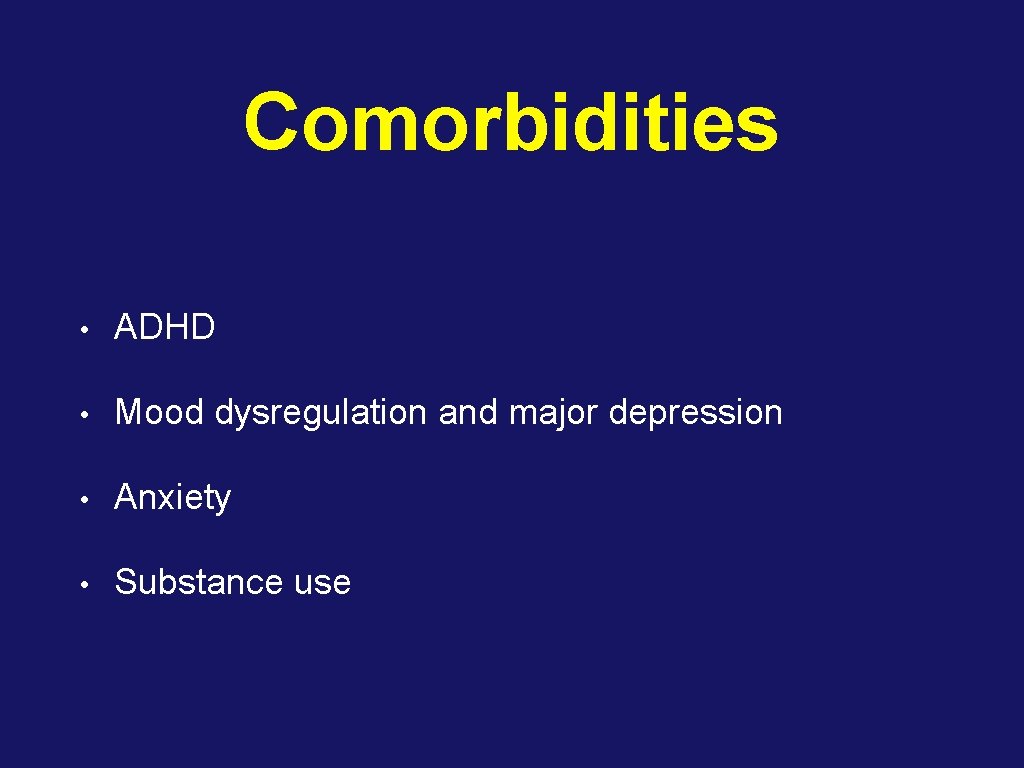
Comorbidities • ADHD • Mood dysregulation and major depression • Anxiety • Substance use
Referral • Patients will benefit from a multidisciplinary approach - consider referral to developmental pediatrics (OCTC in Ottawa)
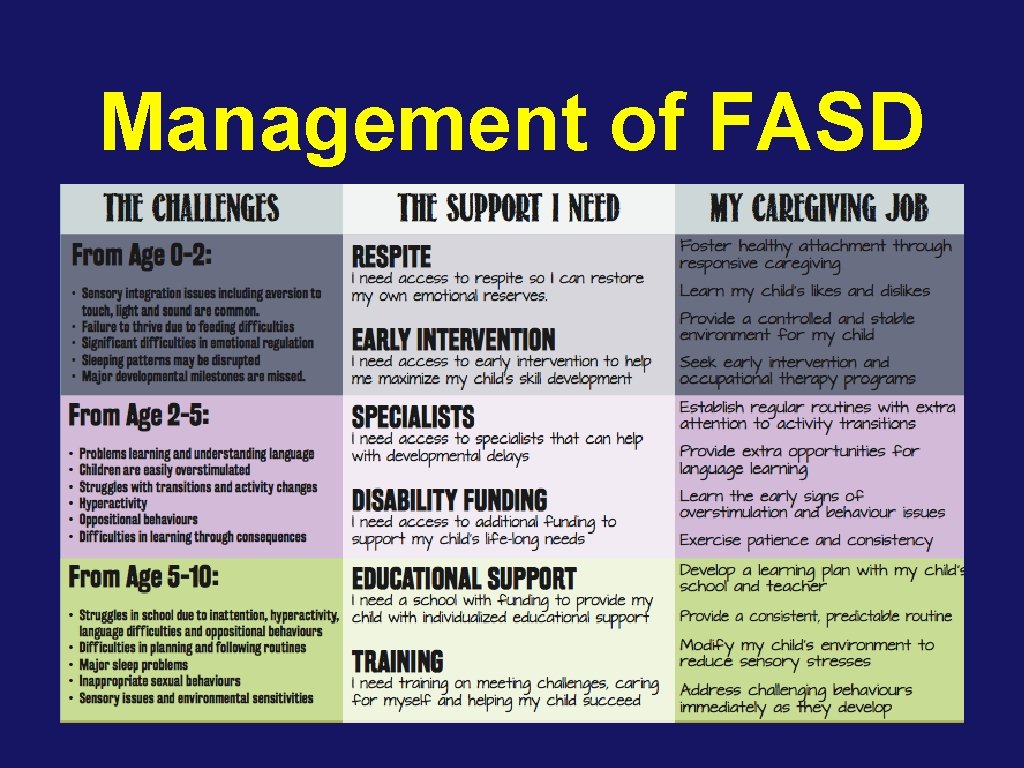
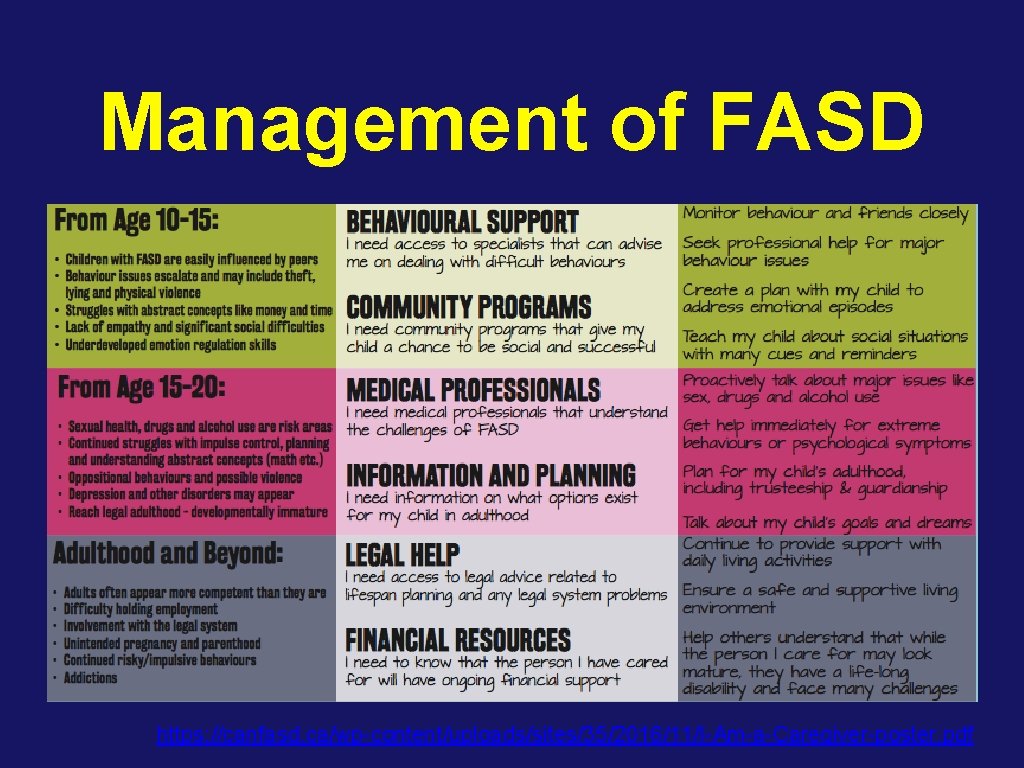
Management of FASD
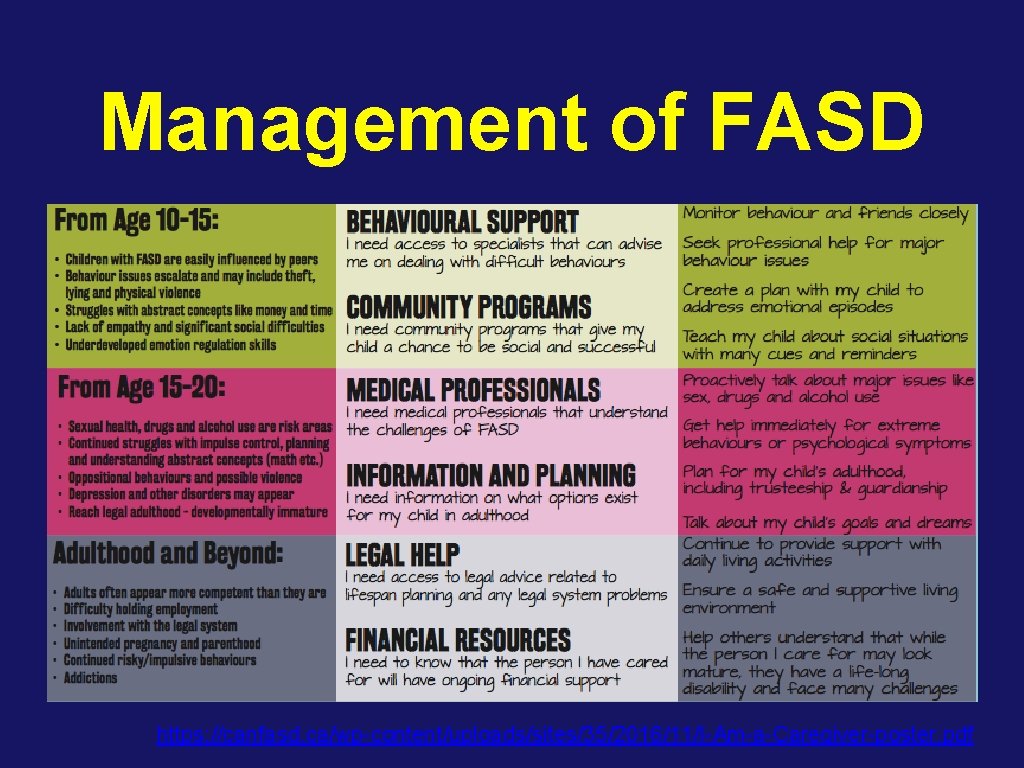
Management of FASD https: //canfasd. ca/wp-content/uploads/sites/35/2016/11/I-Am-a-Caregiver-poster. pdf
Prognosis • High prevalence of adverse outcomes • Inappropriate sexual behaviour • Suspension/expulsion/school drop out • Trouble with law • Confinement (prison, psychiatric, addiction rehab) • Alcohol/drug us
Prognosis • Factors associated with improved prognosis • Diagnosis before age 6 • Access to social services and educational supports • Stable living environment • Absence of exposure to abuse
Summary • New Canadian Guidelines for diagnosis of FASD • There is no safe amount of alcohol to consume in pregnancy • Prevention is key - screen all women of childbearing age for alcohol consumption habits and counsel on reducing intake • Management should be tailored to the individual child, but in general early diagnosis and intervention is associated with better outcomes
Thank You
References Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. Chudley AE, Conry J, Cook JL, Loock C, Rosales T, Le. Blanc N; Public Health Agency of Canada's National Advisory Committee on Fetal Alcohol Spectrum Disorder. CMAJ. 2005 Mar 1; 172(5 Suppl): S 1 -S 21. Fetal alcohol spectrum disorder: a guideline for diagnosis across the lifespan. Cook JL, Green CR, Lilley CM, Anderson SM, Baldwin ME, Chudley AE, Conry JL, Le. Blanc N, Loock CA, Lutke J, Mallon BF, Mc. Farlane AA, Temple VK, Rosales T; Canada Fetal Alcohol Spectrum Disorder Research Network. CMAJ. 2016 Feb 16; 188(3): 191 -7. Fetal alcohol syndrome. First Nations and Inuit Health Committee, Canadian Pediatric Society. Paediatr Child Health. 2002 Mar; 7(3): 161 -95.
 Fetal alcohol spectrum disorder
Fetal alcohol spectrum disorder Fas facial features
Fas facial features Fetal alcohol syndrome face
Fetal alcohol syndrome face Teetotal celebrities
Teetotal celebrities Alcohol
Alcohol Fasd
Fasd Fetal alcohol syndrome life expectancy
Fetal alcohol syndrome life expectancy Life expectancy fetal alcohol syndrome
Life expectancy fetal alcohol syndrome Fetal alcohol syndrome
Fetal alcohol syndrome Dr julye carew
Dr julye carew Dr julye carew
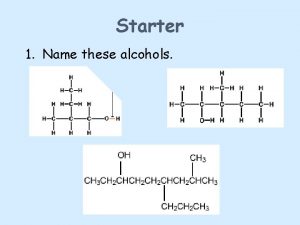
Dr julye carew High boiling point alcohols
High boiling point alcohols Primary and secondary alcohol oxidation
Primary and secondary alcohol oxidation Factitious disorder
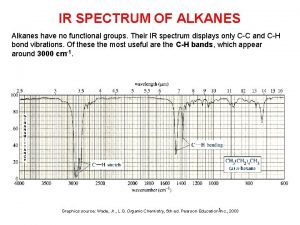
Factitious disorder Ir spectra of alkanes
Ir spectra of alkanes Types of autism spectrum disorder dsm 5
Types of autism spectrum disorder dsm 5 Spectrum disorder
Spectrum disorder Types of autism spectrum disorder
Types of autism spectrum disorder Spectrum disorder
Spectrum disorder Autism spectrum disorder
Autism spectrum disorder Autism spectrum disorder authorization california
Autism spectrum disorder authorization california Autism spectrum disorder adhd
Autism spectrum disorder adhd Absortpion
Absortpion Atomic size defination
Atomic size defination Caitlin puccio
Caitlin puccio Dr elise meoli
Dr elise meoli Caitlin lindsay
Caitlin lindsay Aefis uw madison
Aefis uw madison Ciasta mondrian caitlin freeman
Ciasta mondrian caitlin freeman Stanford children's administrative fellowship
Stanford children's administrative fellowship Esme caitlin
Esme caitlin I will always write back quotes
I will always write back quotes Caitlin crowley
Caitlin crowley Caitlin d. davidson
Caitlin d. davidson Caitlin bevers workshop
Caitlin bevers workshop Caitlin venus
Caitlin venus Caitlin driscoll
Caitlin driscoll Caitlin benson
Caitlin benson Caitlin coyle
Caitlin coyle Ataf ligament
Ataf ligament Caitlin grady
Caitlin grady Bronwyn and caitlin
Bronwyn and caitlin