Etiology and Pathology Lesion Effects Demographics Deficits Stroke


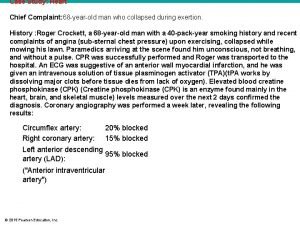
- Slides: 153
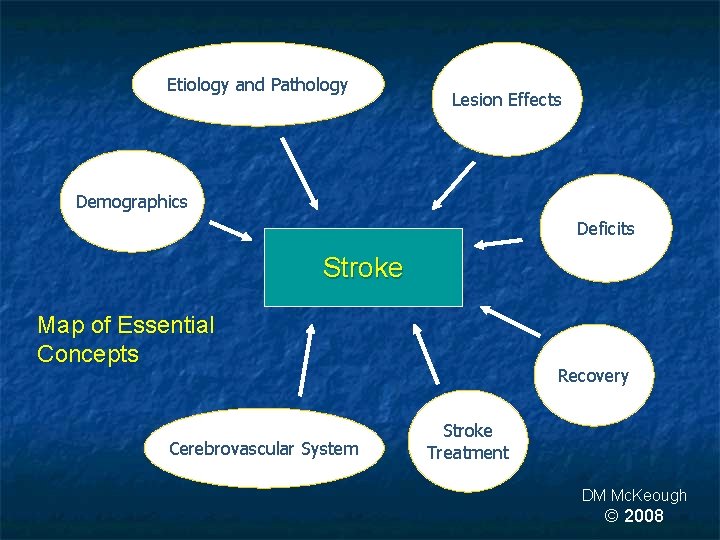
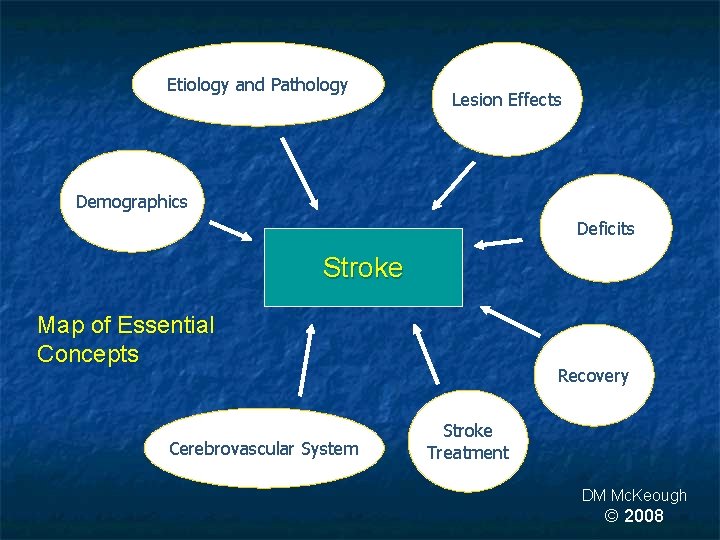
Etiology and Pathology Lesion Effects Demographics Deficits Stroke Map of Essential Concepts Cerebrovascular System Recovery Stroke Treatment DM Mc. Keough © 2008
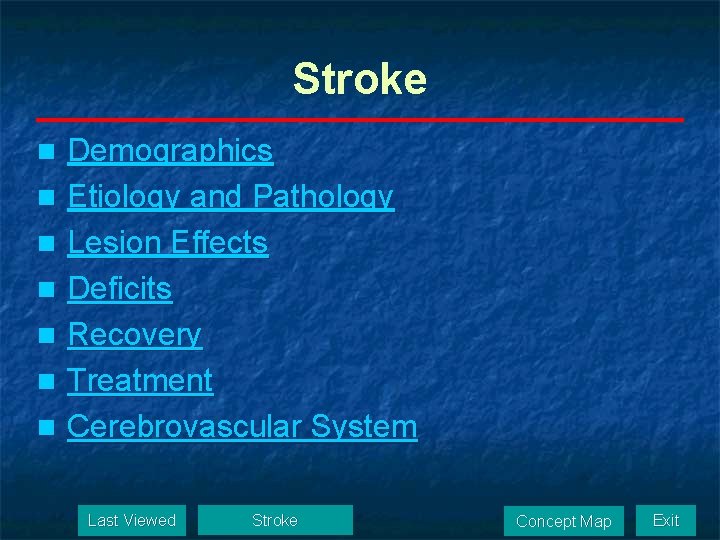
Stroke Demographics n Etiology and Pathology n Lesion Effects n Deficits n Recovery n Treatment n Cerebrovascular System n Last Viewed Stroke Concept Map Exit

Demographics n n n Brain Metabolism Oxygen Demands Hemiplegia Epidemiology Economic Costs Last Viewed Demographics Concept Map Exit
Brain Metabolism n Brain’s sole source of energy is aerobic or oxidative metabolism n Therefore, the brain requires a constant supply of O 2 and glucose, 24/ 7/ 365 Last Viewed Demographics Concept Map Exit
Oxygen Demands n n n At approximately 3 pounds, the brain accounts for roughly 2% of body mass Consumes 17% of cardiac output Responsible for 20% of oxygen consumption at rest Last Viewed Demographics Concept Map Exit
Hemiplegia n The hallmark of stroke is hemiplegia Hemiparesis + n Hemisensory impairment n n The great vulnerability of the brain to ischemic damage is due to its dependence on aerobic metabolism Last Viewed Demographics Concept Map Exit
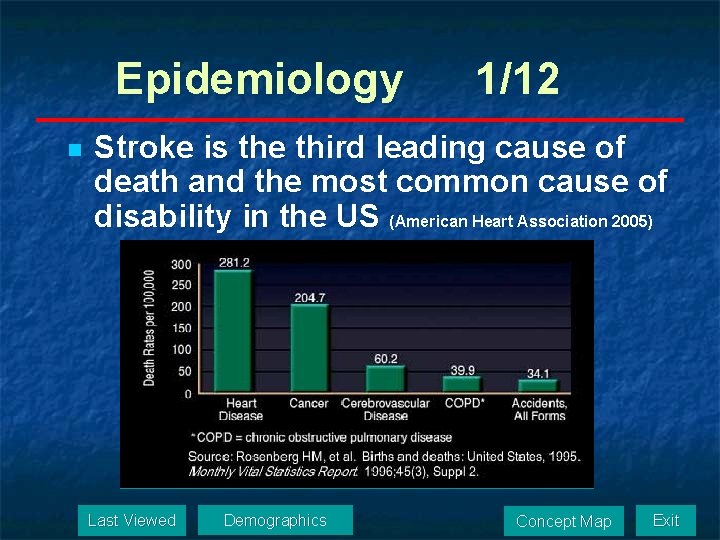
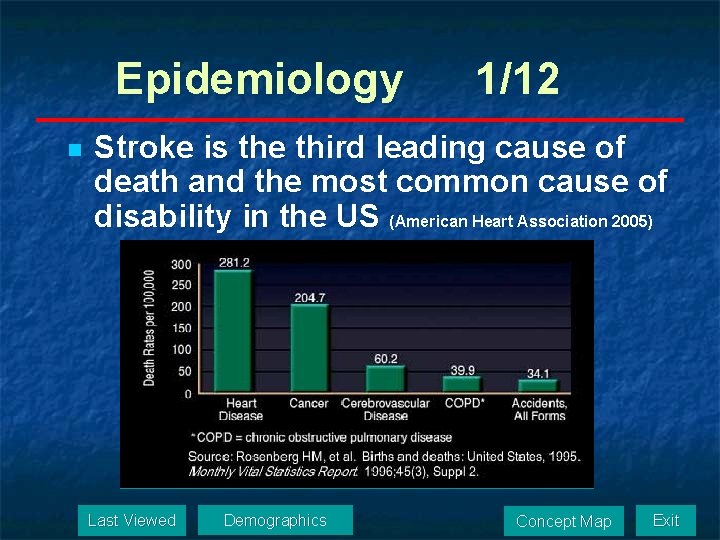
Epidemiology n 1/12 Stroke is the third leading cause of death and the most common cause of disability in the US (American Heart Association 2005) Last Viewed Demographics Concept Map Exit
Epidemiology 2/12 Incidence n Each year about 700, 000 people experience a new or recurrent stroke. (500, 000 are first attacks, and 200, 000 are recurrent attacks) (American Heart Association 2005) n Every 45 seconds someone in the US has a stroke (280 strokes during today’s class) Last Viewed Demographics Concept Map Exit
Epidemiology 3/12 Gender Distribution n Men > Women x 1. 25 Ethnic Distribution n African-Americans > Whites x 2 n Hispanic n Native Americans n Native Alaskans n Whites (American Heart Association 2005) Last Viewed Demographics Concept Map Exit
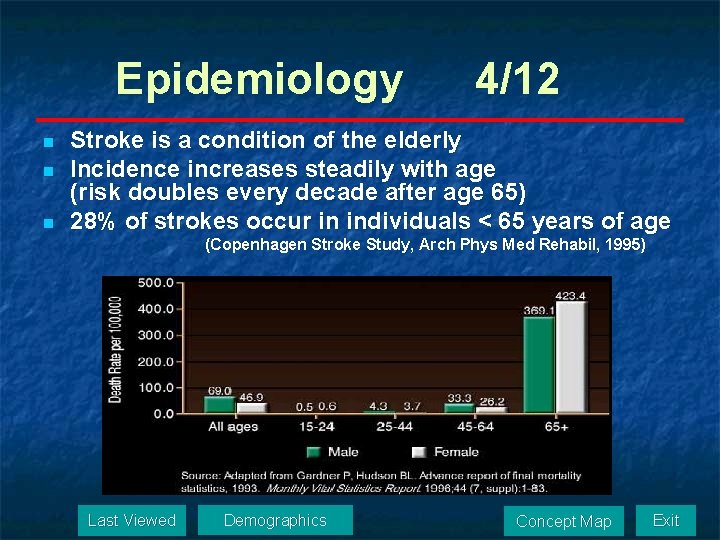
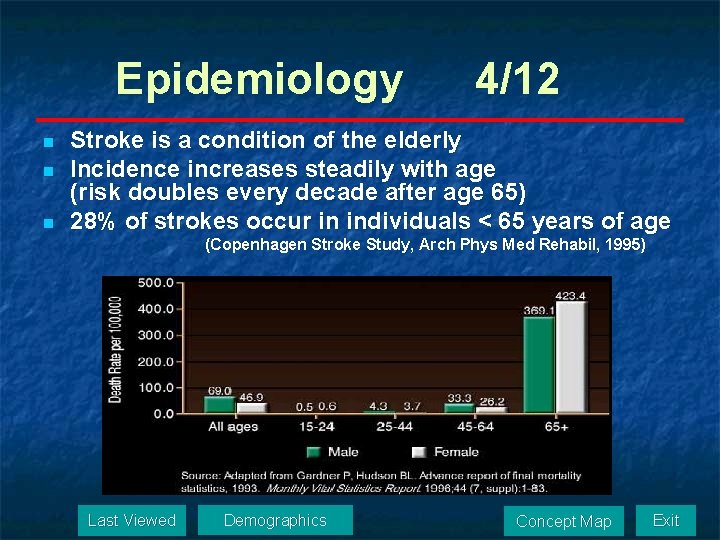
Epidemiology n n n 4/12 Stroke is a condition of the elderly Incidence increases steadily with age (risk doubles every decade after age 65) 28% of strokes occur in individuals < 65 years of age (Copenhagen Stroke Study, Arch Phys Med Rehabil, 1995) Last Viewed Demographics Concept Map Exit
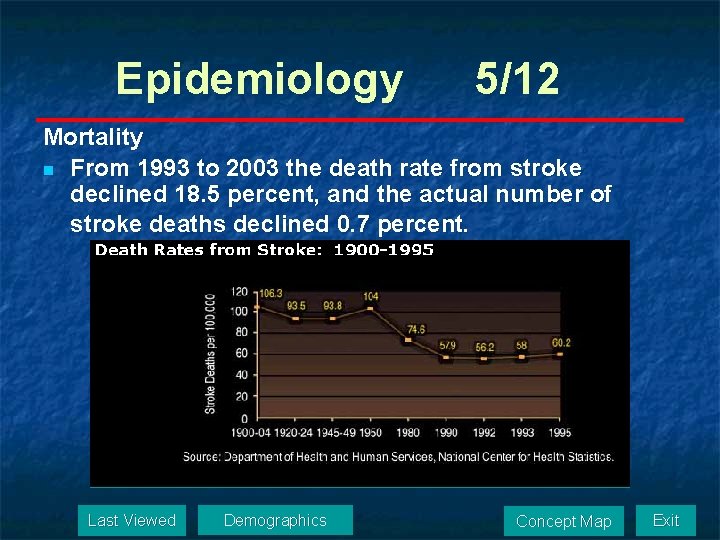
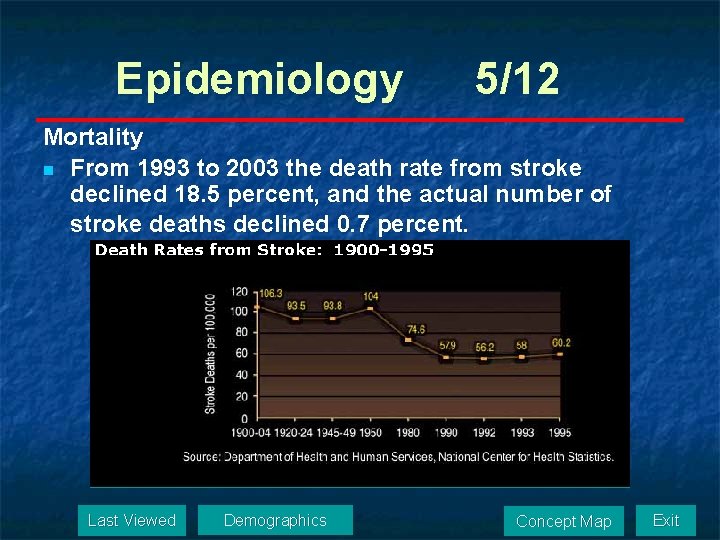
Epidemiology 5/12 Mortality n From 1993 to 2003 the death rate from stroke declined 18. 5 percent, and the actual number of stroke deaths declined 0. 7 percent. Last Viewed Demographics Concept Map Exit
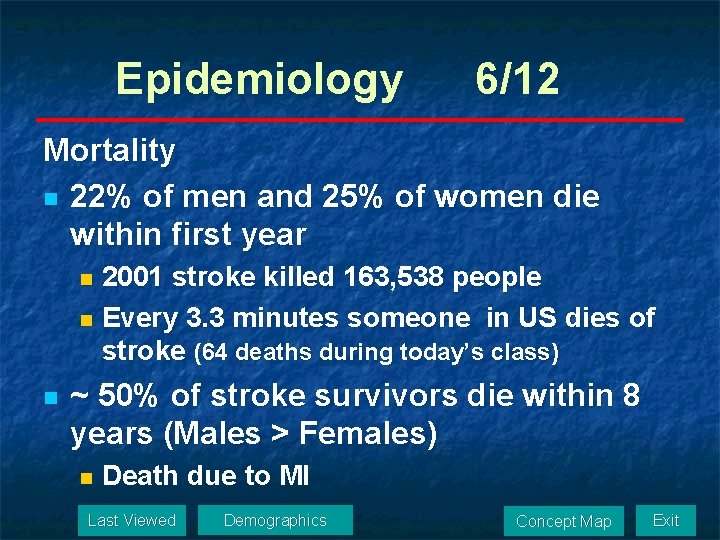
Epidemiology 6/12 Mortality n 22% of men and 25% of women die within first year 2001 stroke killed 163, 538 people n Every 3. 3 minutes someone in US dies of stroke (64 deaths during today’s class) n n ~ 50% of stroke survivors die within 8 years (Males > Females) n Death due to MI Last Viewed Demographics Concept Map Exit
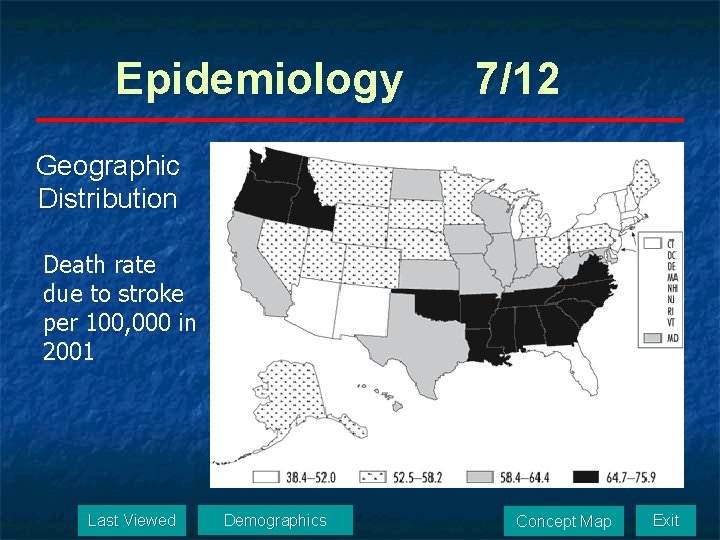
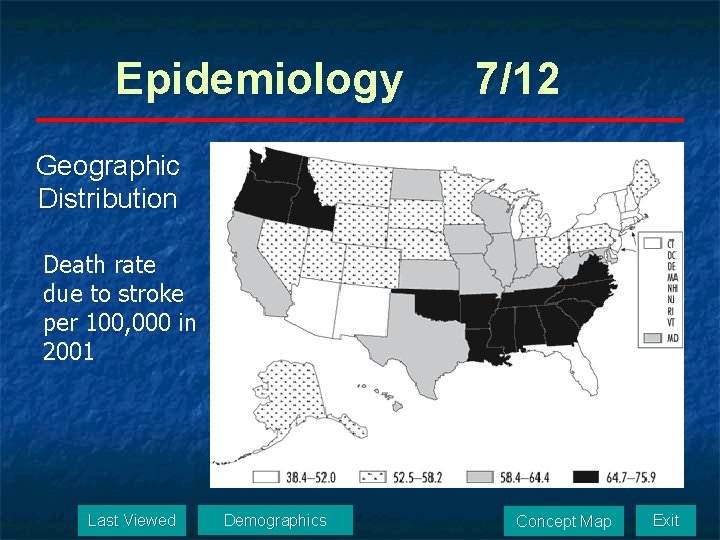
Epidemiology 7/12 Geographic Distribution Death rate due to stroke per 100, 000 in 2001 Last Viewed Demographics Concept Map Exit
Epidemiology 8/12 Mortality by type of stroke n Hemorrhagic 38% n Ischemic 12% (American Heart Association 2005) n Survival rates dramatically decreased by age and co-morbidity Hypertension n Heart disease n Diabetes (Post-Stroke Rehabilitation Guideline Panel 1995) n Last Viewed Demographics Concept Map Exit
Epidemiology 9/12 Recurrence n 14% per year, highest in first year n Risk of stroke increases 10 times after first stroke n Recurring strokes produce larger lesions (cumulative effects), greater cortical involvement, greater impairment, higher mortality n Outcome and pattern of recovery is similar to first-time stroke n Should receive similar rehab treatment as first -time stroke. Demographics Last Viewed Exit Concept Map
Epidemiology 10/12 Prevalence n About 5, 500, 000 stroke survivors are alive today n 2, 400, 000 are males and 3, 000 are females Last Viewed Demographics Concept Map Exit
Epidemiology 11/12 The following activity limitations were observed at six months post-stroke: 50 % had some one-sided paralysis n 35 % had depression n 30 % were unable to walk without some assistance n 26 % were dependent in activities of daily living (grooming, eating, bathing, etc) n 26 % were institutionalized in a nursing home n 19 % had aphasia (trouble speaking or Demographics Last Viewed Exit Concept Map understanding n
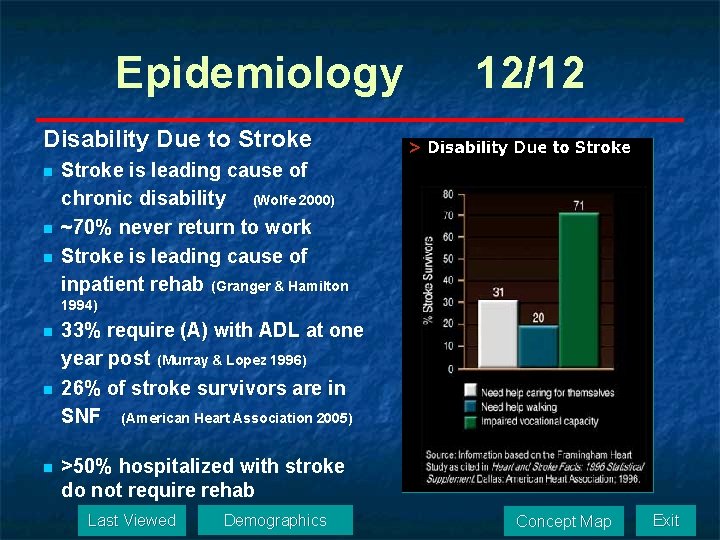
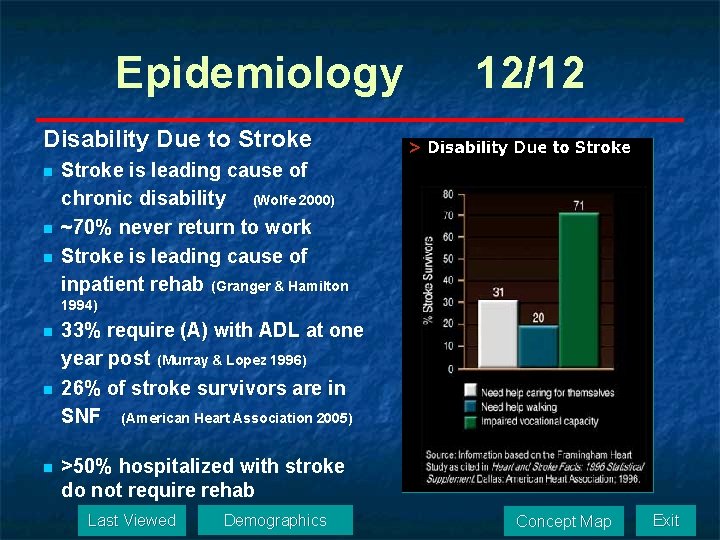
Epidemiology 12/12 Disability Due to Stroke n n n Stroke is leading cause of chronic disability (Wolfe 2000) ~70% never return to work Stroke is leading cause of inpatient rehab (Granger & Hamilton 1994) n n n 33% require (A) with ADL at one year post (Murray & Lopez 1996) 26% of stroke survivors are in SNF (American Heart Association 2005) >50% hospitalized with stroke do not require rehab Last Viewed Demographics Concept Map Exit
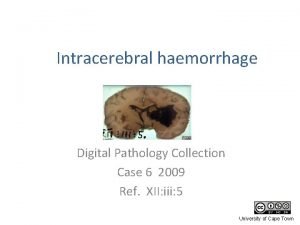
Economic Costs n n Estimated: $56. 8 billion per year in the US Life time costs: Thromboembolic stroke n Hemorrhagic stroke: n Subarachnoid n Intracerebral n Last Viewed Demographics $100, 000 $228, 000 $124, 000 Concept Map Exit
Etiology and Pathology n n n n n Etiology Common Occlusion Sites Risk Factors Stroke Prevention Predictors of Stroke Warning Signs Predictors of Good Outcome Predictors of Bad Outcome Nagi Model Pathophysiology Last Viewed Etiology and Pathology Concept Map Exit
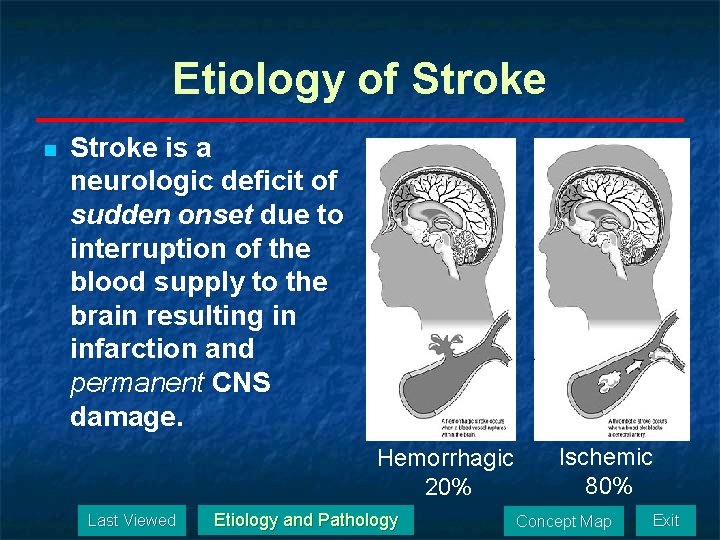
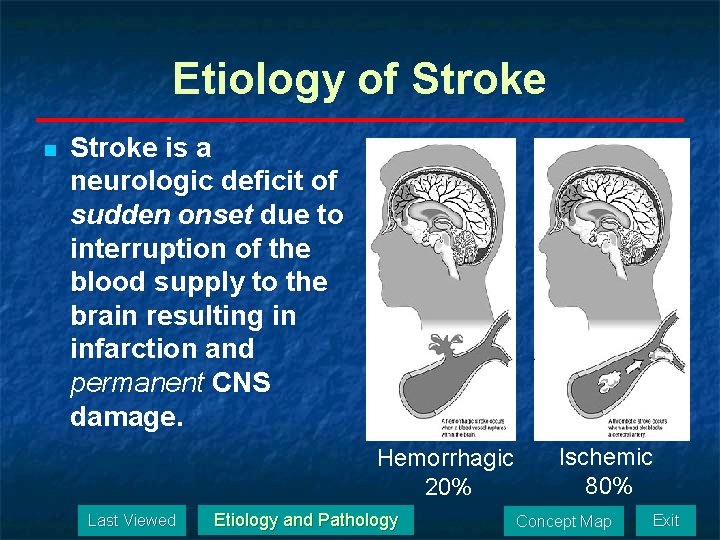
Etiology of Stroke n Stroke is a neurologic deficit of sudden onset due to interruption of the blood supply to the brain resulting in infarction and permanent CNS damage. Hemorrhagic 20% Last Viewed Etiology and Pathology Ischemic 80% Concept Map Exit
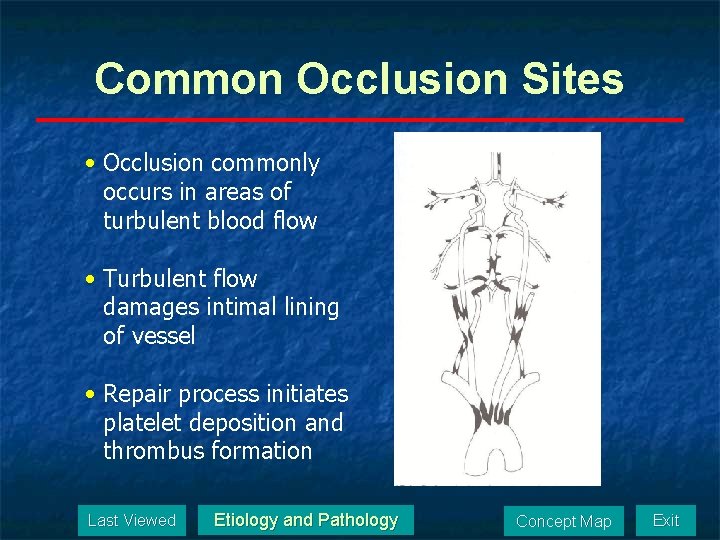
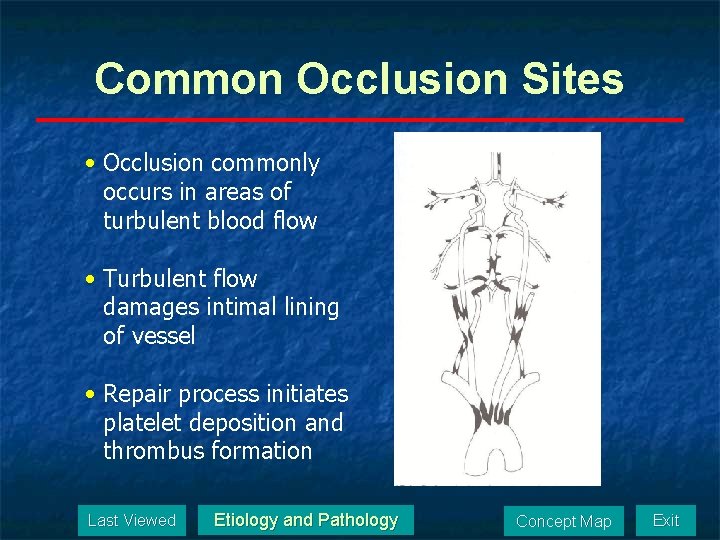
Common Occlusion Sites • Occlusion commonly occurs in areas of turbulent blood flow • Turbulent flow damages intimal lining of vessel • Repair process initiates platelet deposition and thrombus formation Last Viewed Etiology and Pathology Concept Map Exit
Risk Factors 1/3 § Non-modifiable Risk Factors § § § § Increased age Being male Race (e. g. , African-Americans) Diabetes mellitus Prior stroke/transient ischemic attacks Family history of stroke Asymptomatic carotid bruit § Less Well Documented (perhaps partly modifiable) § Geography/climate § Socioeconomic factors Last 1996. Viewed Facts. Source: American Stroke Association. Heart and Stroke Exit Etiology and Pathology Concept Map
Risk Factors 2/3 n Modifiable Risk Factor n Major n n n Secondary n n Hypertension Heart disease, especially atrial fibrillation Cigarette smoking Transient ischemic attacks Increased serum cholesterol / lipids Physical inactivity Obesity Less Well Documented n n Excessive alcohol intake / drug abuse Acute infection* * Not listed in the ASA publication Last Viewed Etiology and Pathology Concept Map Exit
Genetic Risk Factors for Stroke 3/3 n n Apolipoprotein E 4 Elevated homocysteine levels Factor V mutation Apolipoproteins -- important in the transport of lipids in plasma. Apolipoprotein E (Apo E) forms part of all plasma concentration is closely correlated with plasma triglyceride concentrations. The presence of the apolipoprotein-E 4 allele has also been associated with an increased risk for stroke; Last Viewed reports Exit Etiology and Concept Map however, are. Pathology conflicting.
Stroke Prevention 1/2 Exercise reduces the risk of stroke Intense exercise 27% Intense exercise: jogging 15 to 20 minutes a day on most days Moderate exercise 20% Moderate exercise: brisk walks of 30 minutes a day on most days J Stroke: Oct 2003 Last Viewed Etiology and Pathology Concept Map Exit
Stroke Prevention n n 2/2 “Clot Buster” (Tissue Plasminogen Activator, TPA, ) Recent research n n Tissue grafting Genetic engineering Last Viewed Etiology and Pathology Concept Map Exit
Predictors of Stroke n n Previous stroke Transient ischemic attacks: 35% of thrombotic strokes were preceded by TIA Last Viewed Etiology and Pathology Concept Map Exit
Warning Signs n Characterized by sudden onset focal neurological deficit n Warning signs: Call for medical assistance n Sudden numbness or weakness of the face, arm or leg, especially on one side of the body n Sudden confusion, trouble speaking or understanding n Sudden trouble seeing in one or both eyes n Sudden trouble walking, dizziness, loss of balance or coordination n Sudden, severe headache with no Last Viewed Etiology and Pathology (American Concept Map known cause Exit
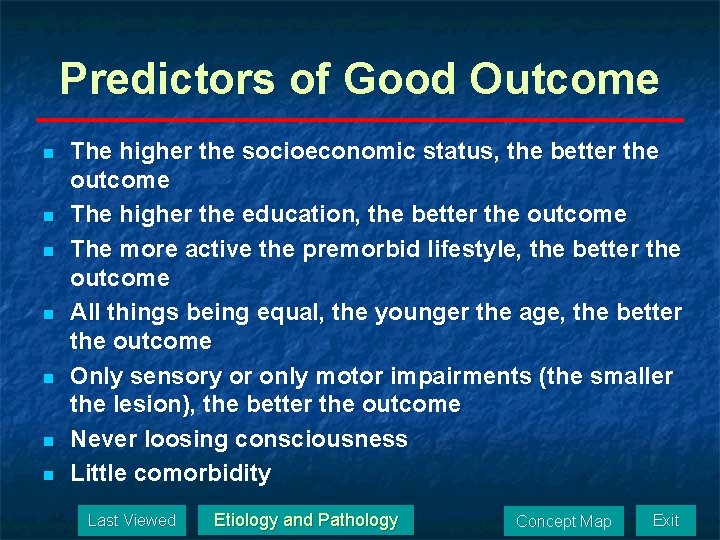
Predictors of Good Outcome n n n n The higher the socioeconomic status, the better the outcome The higher the education, the better the outcome The more active the premorbid lifestyle, the better the outcome All things being equal, the younger the age, the better the outcome Only sensory or only motor impairments (the smaller the lesion), the better the outcome Never loosing consciousness Little comorbidity Last Viewed Etiology and Pathology Concept Map Exit
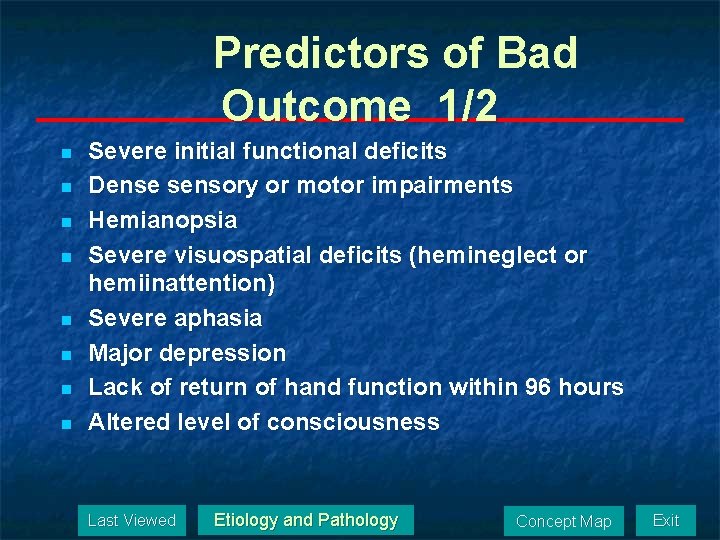
Predictors of Bad Outcome 1/2 n n n n Severe initial functional deficits Dense sensory or motor impairments Hemianopsia Severe visuospatial deficits (hemineglect or hemiinattention) Severe aphasia Major depression Lack of return of hand function within 96 hours Altered level of consciousness Last Viewed Etiology and Pathology Concept Map Exit
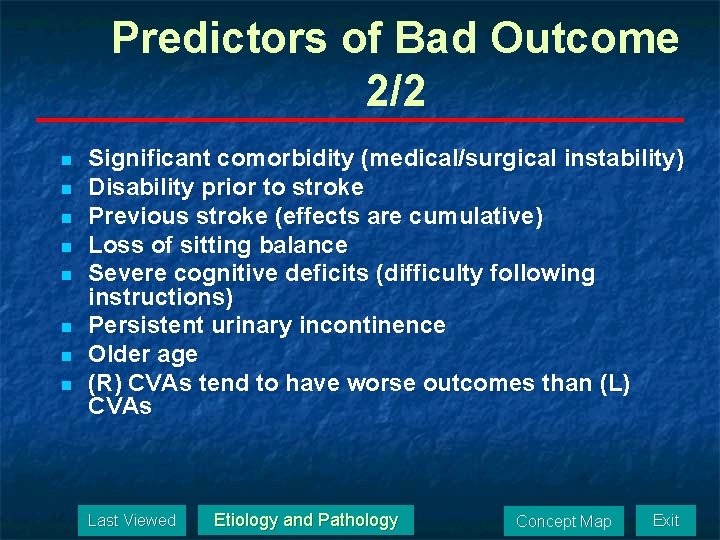
Predictors of Bad Outcome 2/2 n n n n Significant comorbidity (medical/surgical instability) Disability prior to stroke Previous stroke (effects are cumulative) Loss of sitting balance Severe cognitive deficits (difficulty following instructions) Persistent urinary incontinence Older age (R) CVAs tend to have worse outcomes than (L) CVAs Last Viewed Etiology and Pathology Concept Map Exit
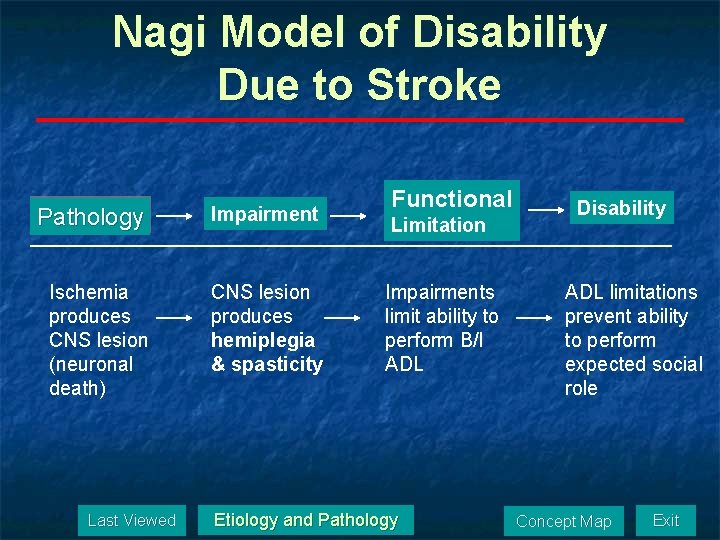
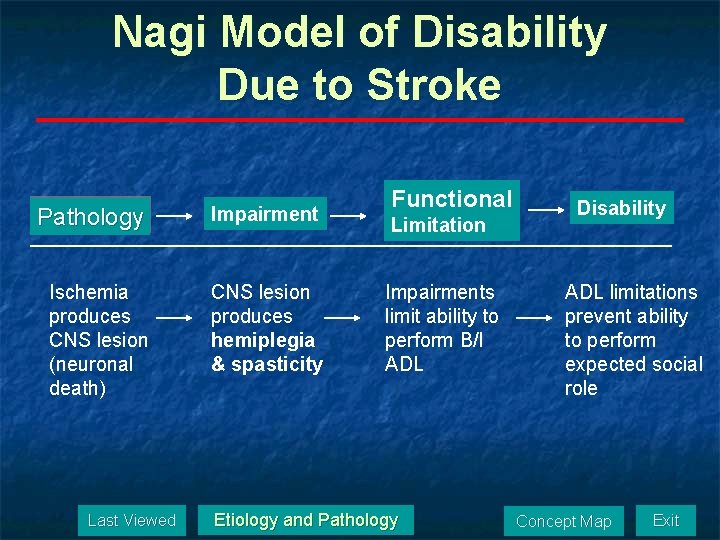
Nagi Model of Disability Due to Stroke Pathology Impairment Ischemia produces CNS lesion (neuronal death) CNS lesion produces hemiplegia & spasticity Last Viewed Functional Limitation Impairments limit ability to perform B/I ADL Etiology and Pathology Disability ADL limitations prevent ability to perform expected social role Concept Map Exit
Pathophysiology 1/10 n Transient ischemic attack (TIA) Caused by reversible ischemia (usually due to vasospasm). n Results in temporary functional impairment with no residual deficits. n ~35% of TIAs evolve into stroke within 1 -3 years n Last Viewed Etiology and Pathology Concept Map Exit
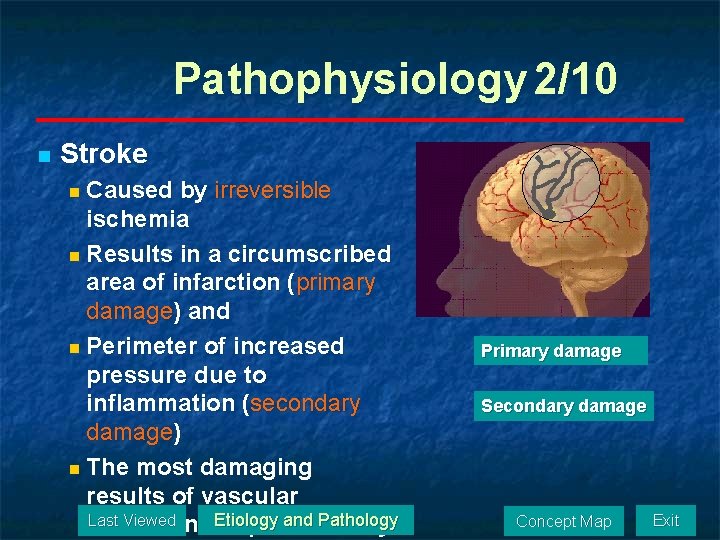
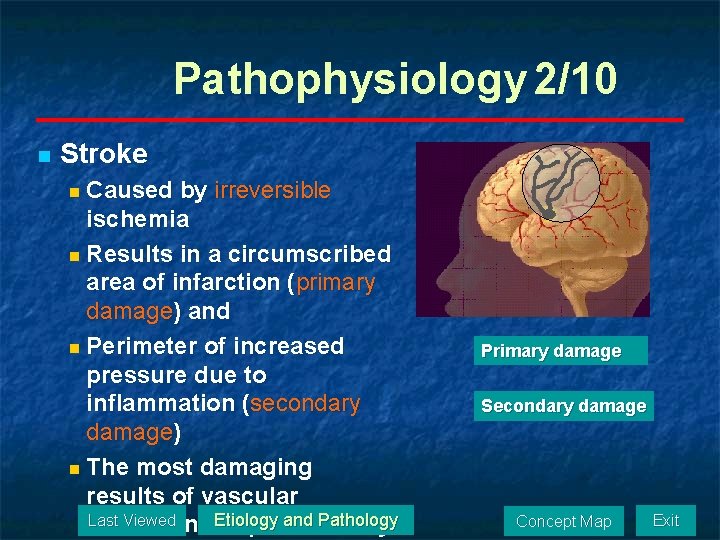
Pathophysiology 2/10 n Stroke n Caused by irreversible ischemia n Results in a circumscribed area of infarction (primary damage) and n Perimeter of increased pressure due to inflammation (secondary damage) n The most damaging results of vascular Last Viewed Etiology and Pathology occlusion are produced by Primary damage Secondary damage Concept Map Exit
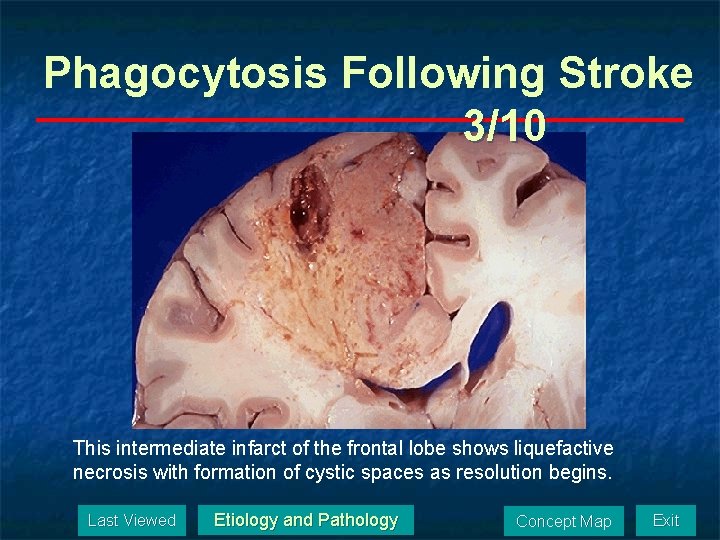
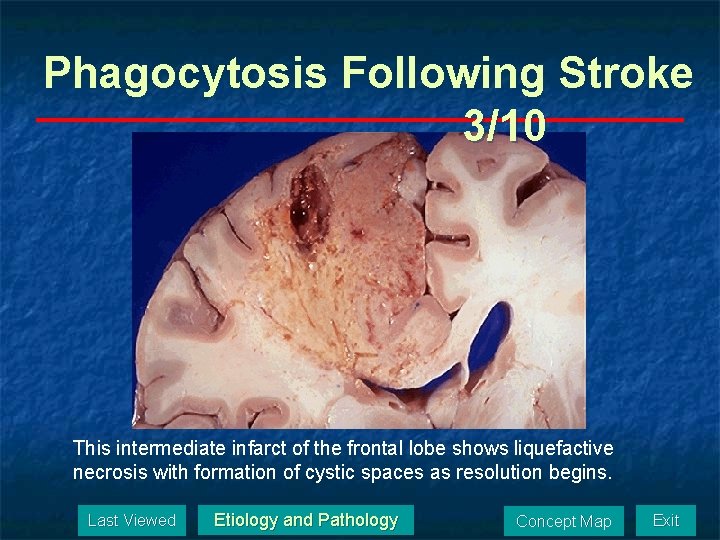
Phagocytosis Following Stroke 3/10 This intermediate infarct of the frontal lobe shows liquefactive necrosis with formation of cystic spaces as resolution begins. Last Viewed Etiology and Pathology Concept Map Exit
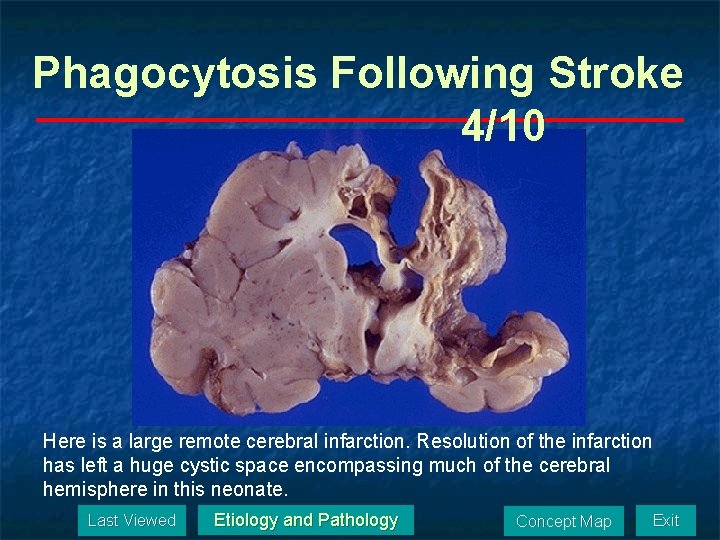
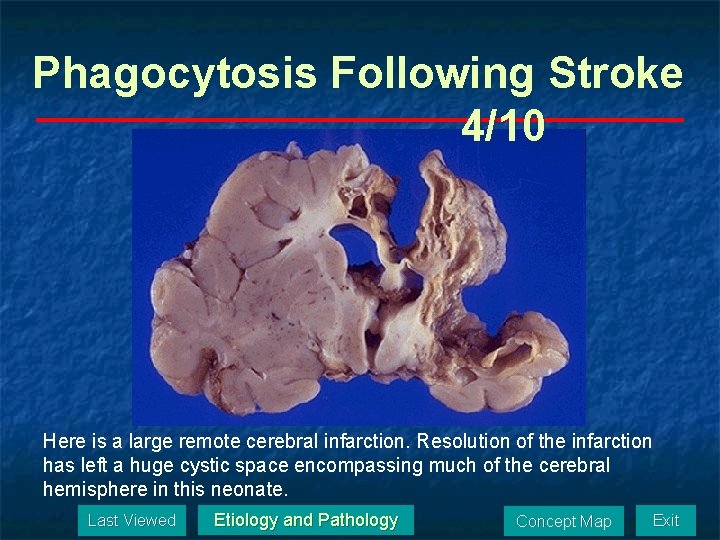
Phagocytosis Following Stroke 4/10 Here is a large remote cerebral infarction. Resolution of the infarction has left a huge cystic space encompassing much of the cerebral hemisphere in this neonate. Last Viewed Etiology and Pathology Concept Map Exit
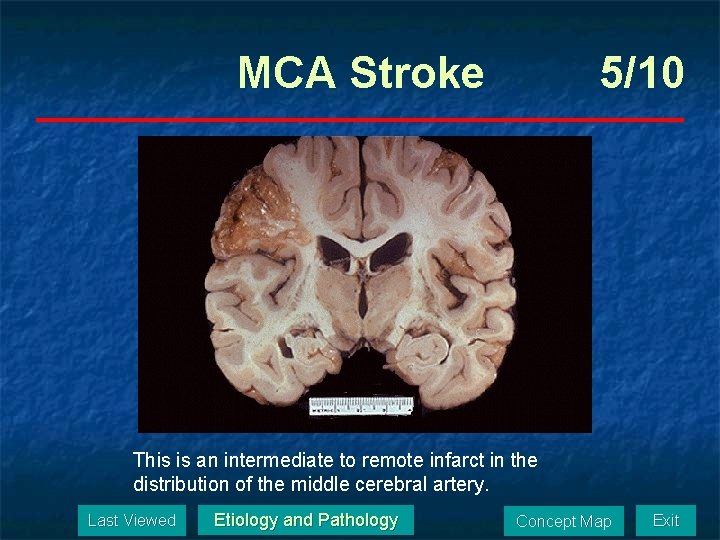
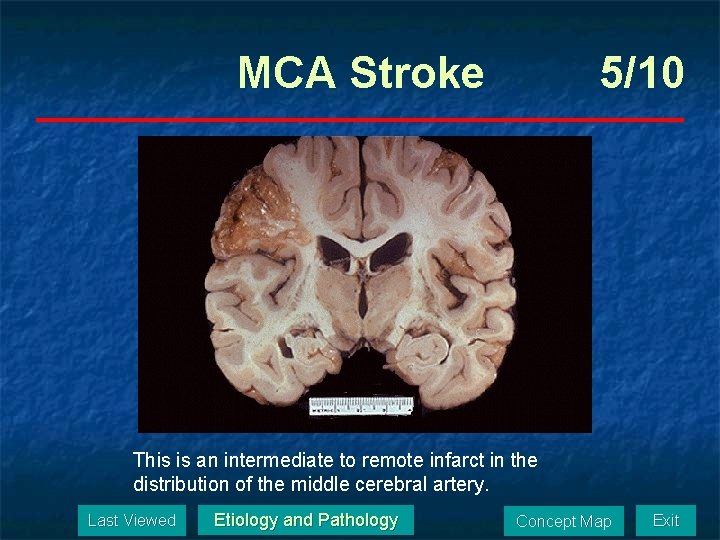
MCA Stroke 5/10 This is an intermediate to remote infarct in the distribution of the middle cerebral artery. Last Viewed Etiology and Pathology Concept Map Exit
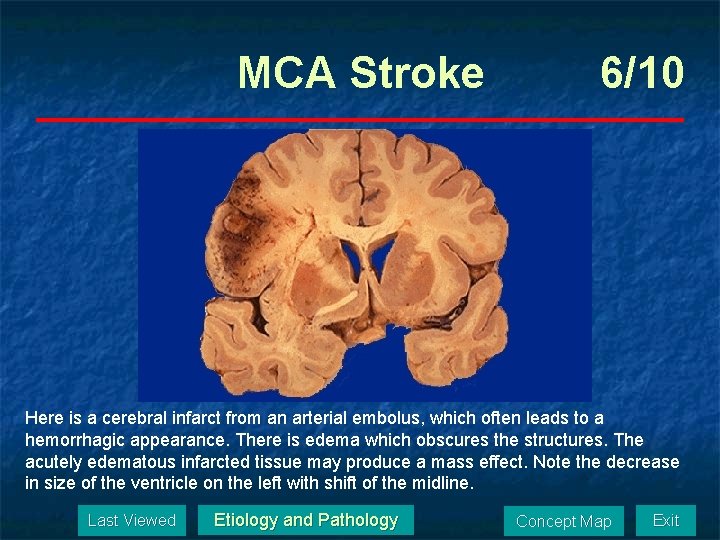
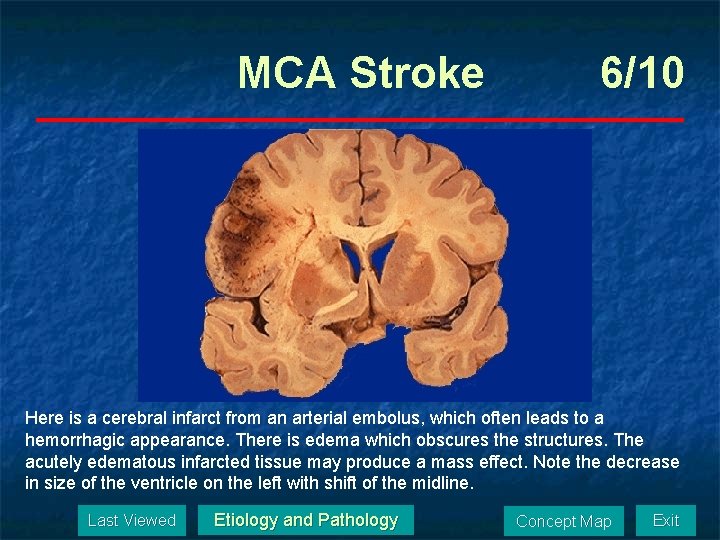
MCA Stroke 6/10 Here is a cerebral infarct from an arterial embolus, which often leads to a hemorrhagic appearance. There is edema which obscures the structures. The acutely edematous infarcted tissue may produce a mass effect. Note the decrease in size of the ventricle on the left with shift of the midline. Last Viewed Etiology and Pathology Concept Map Exit
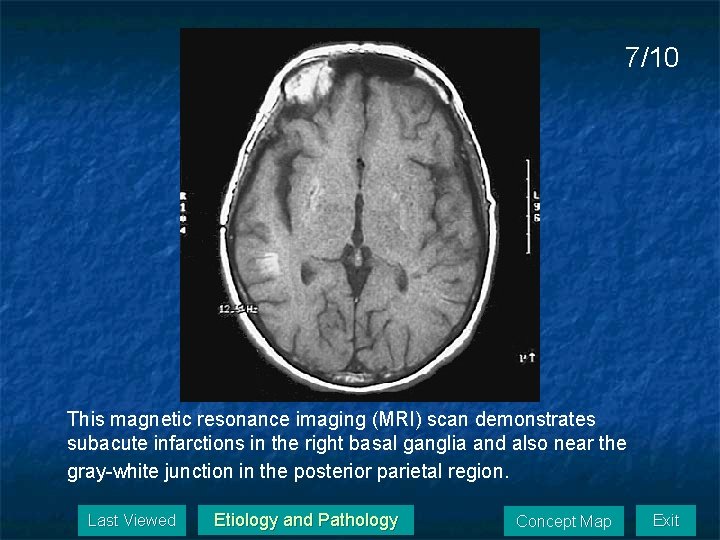
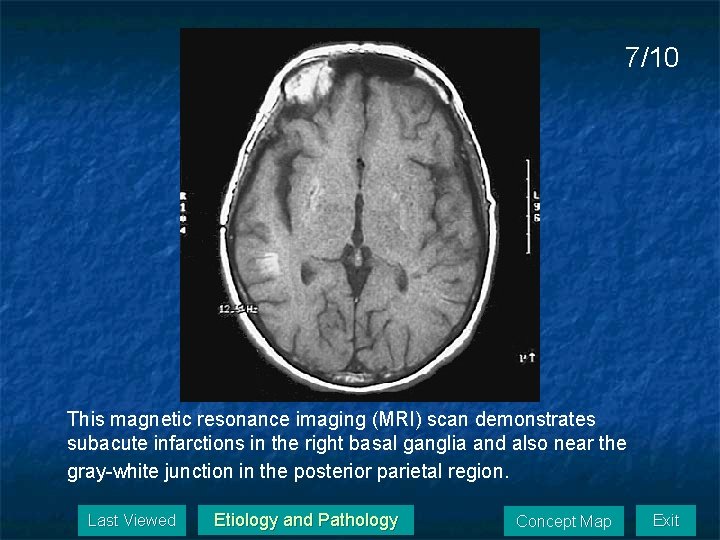
7/10 This magnetic resonance imaging (MRI) scan demonstrates subacute infarctions in the right basal ganglia and also near the gray-white junction in the posterior parietal region. Last Viewed Etiology and Pathology Concept Map Exit
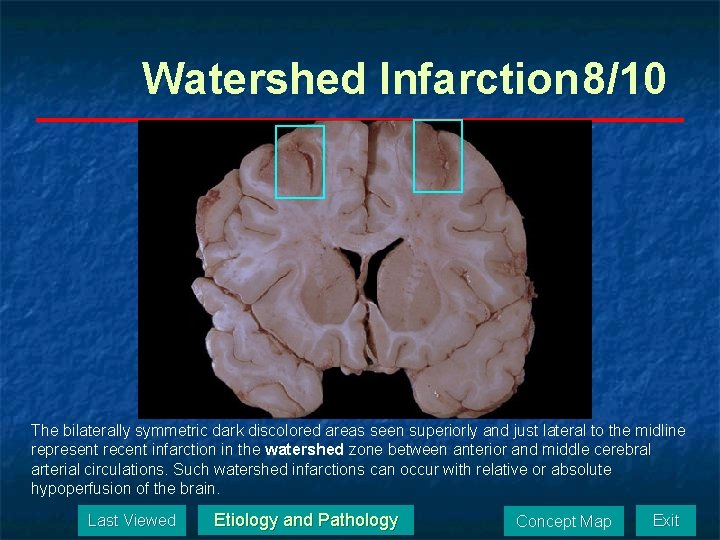
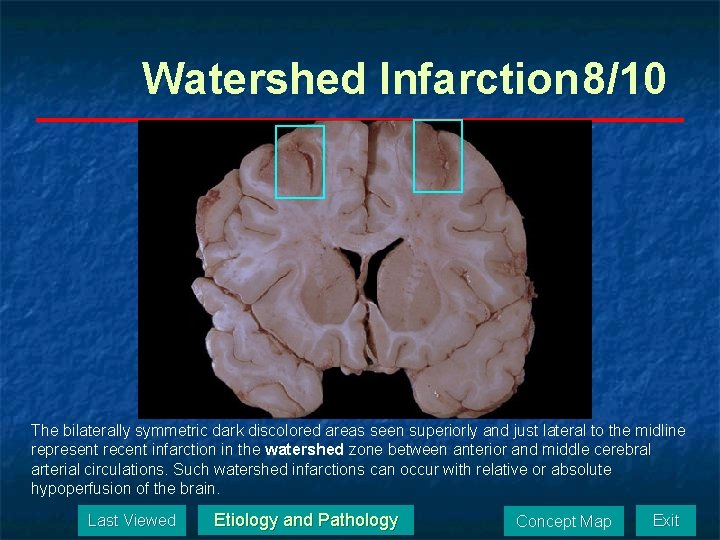
Watershed Infarction 8/10 The bilaterally symmetric dark discolored areas seen superiorly and just lateral to the midline represent recent infarction in the watershed zone between anterior and middle cerebral arterial circulations. Such watershed infarctions can occur with relative or absolute hypoperfusion of the brain. Last Viewed Etiology and Pathology Concept Map Exit
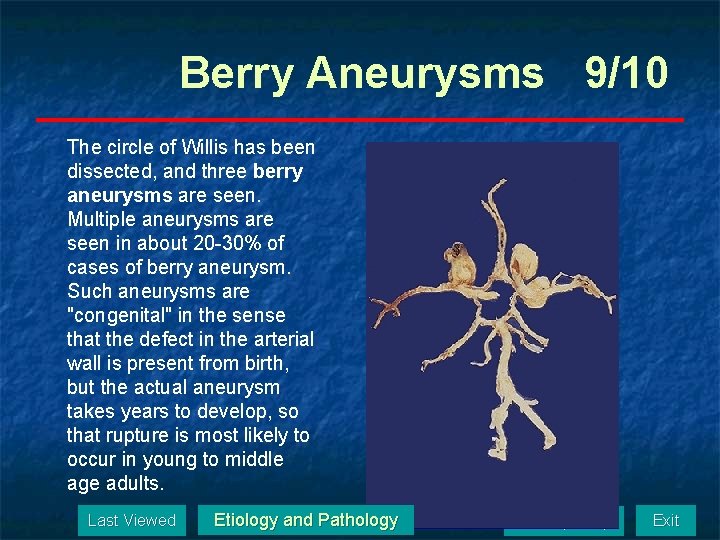
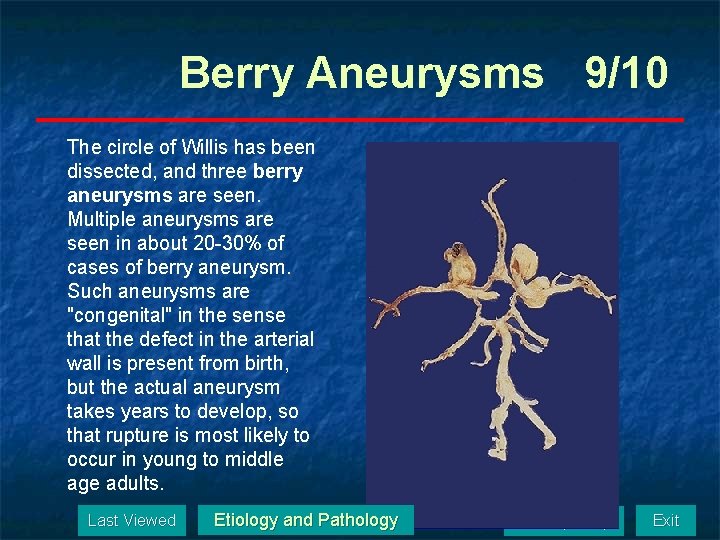
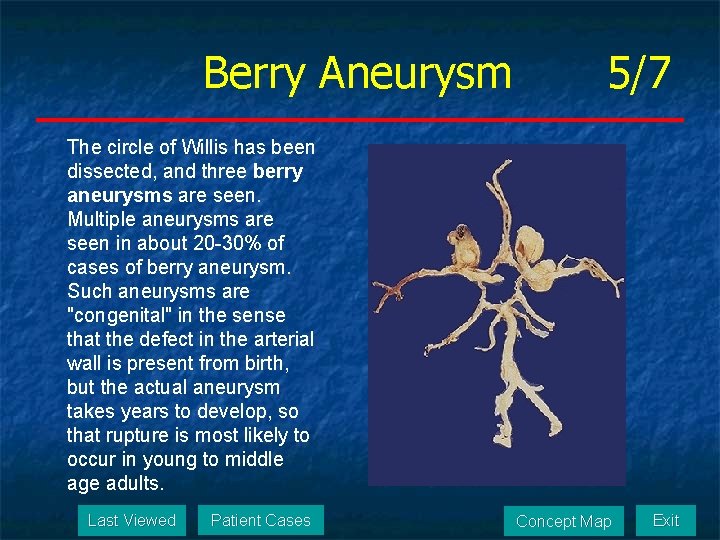
Berry Aneurysms 9/10 The circle of Willis has been dissected, and three berry aneurysms are seen. Multiple aneurysms are seen in about 20 -30% of cases of berry aneurysm. Such aneurysms are "congenital" in the sense that the defect in the arterial wall is present from birth, but the actual aneurysm takes years to develop, so that rupture is most likely to occur in young to middle age adults. Last Viewed Etiology and Pathology Concept Map Exit
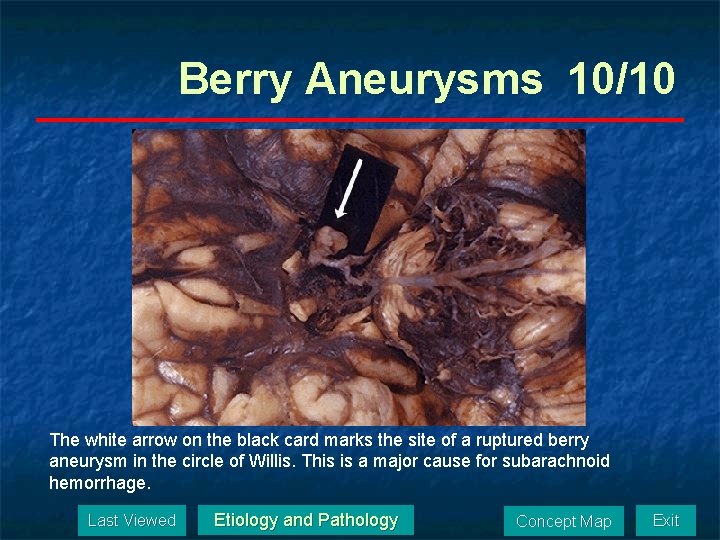
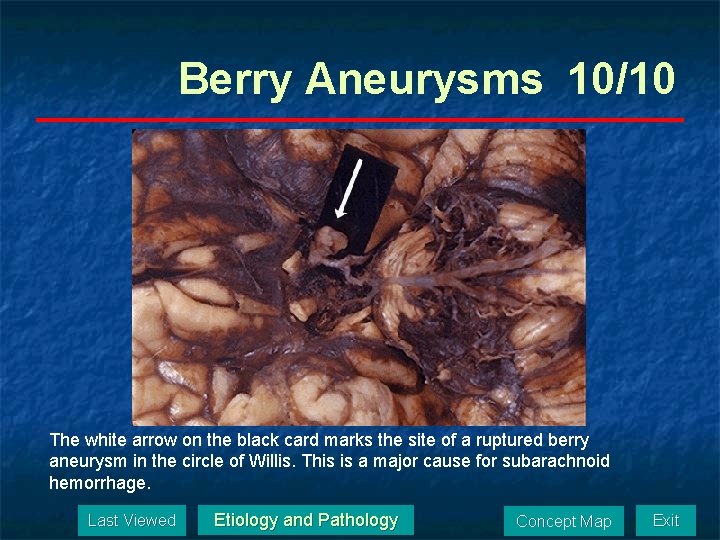
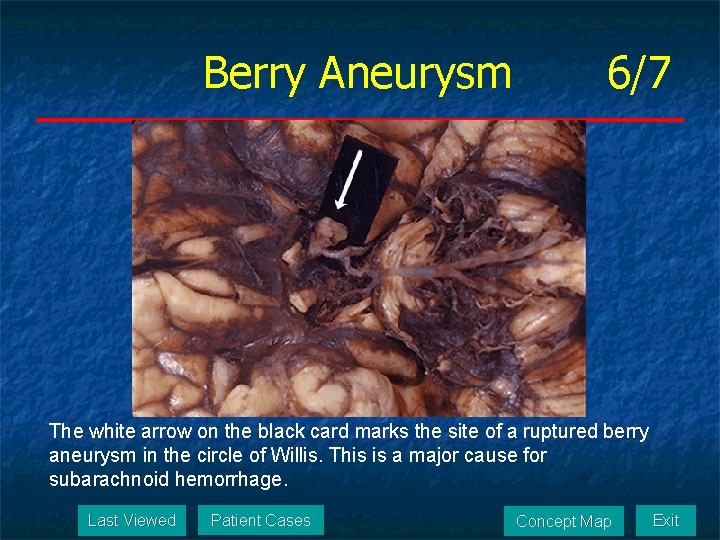
Berry Aneurysms 10/10 The white arrow on the black card marks the site of a ruptured berry aneurysm in the circle of Willis. This is a major cause for subarachnoid hemorrhage. Last Viewed Etiology and Pathology Concept Map Exit
Lesion Effects n n n Domains Affected by Stroke Hemispheric Effects Symptoms by Lesion Location Ideational Apraxia Motor Apraxia Last Viewed Lesion Effects Concept Map Exit
Domains Affected by Stroke n n n Motor Sensory Vision Language Cognition Affect Last Viewed Lesion Effects Concept Map Exit
Hemispheric Effects n n Hemispheric Specialization Dominant Hemisphere Stroke in the Nondominant Hemisphere Last Viewed Lesion Effects Concept Map Exit
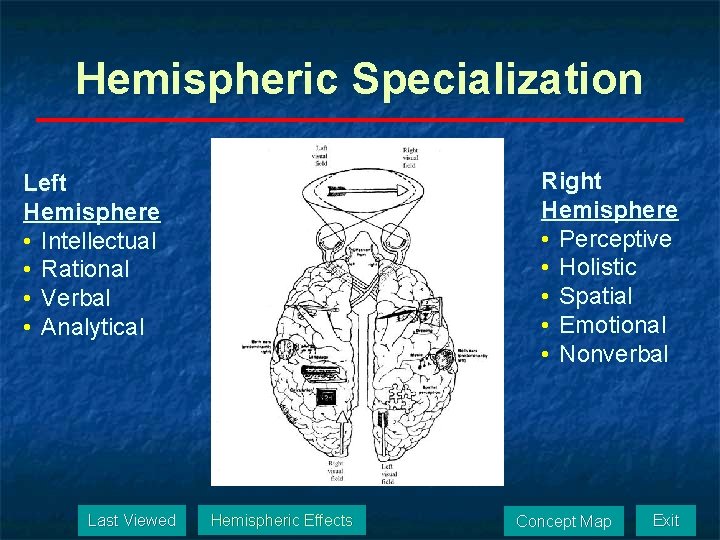
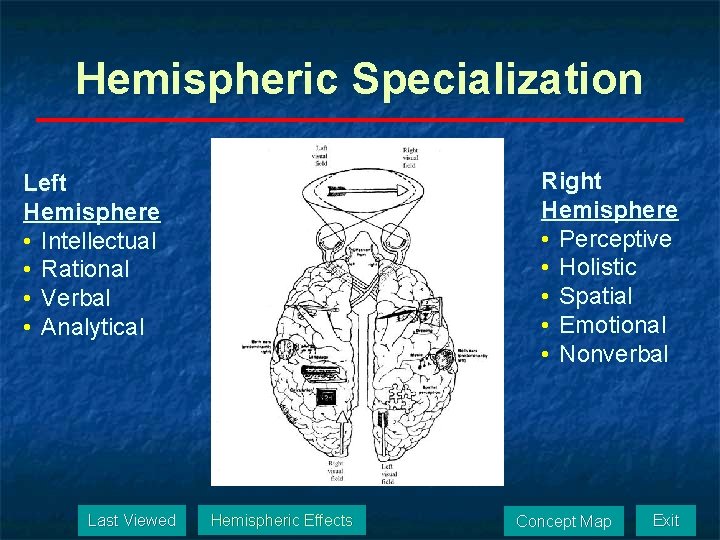
Hemispheric Specialization Right Hemisphere • Perceptive • Holistic • Spatial • Emotional • Nonverbal Left Hemisphere • Intellectual • Rational • Verbal • Analytical Last Viewed Hemispheric Effects Concept Map Exit
Dominant Hemisphere n n Dominant = hemisphere with language (Broca, Wernicke) Left hemisphere is the dominant hemisphere in the vast majority of the population (95%) Last Viewed Hemispheric Effects Concept Map Exit
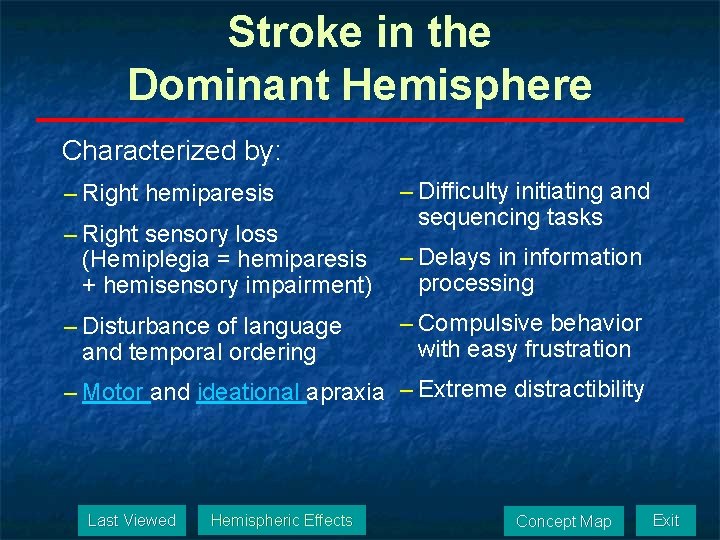
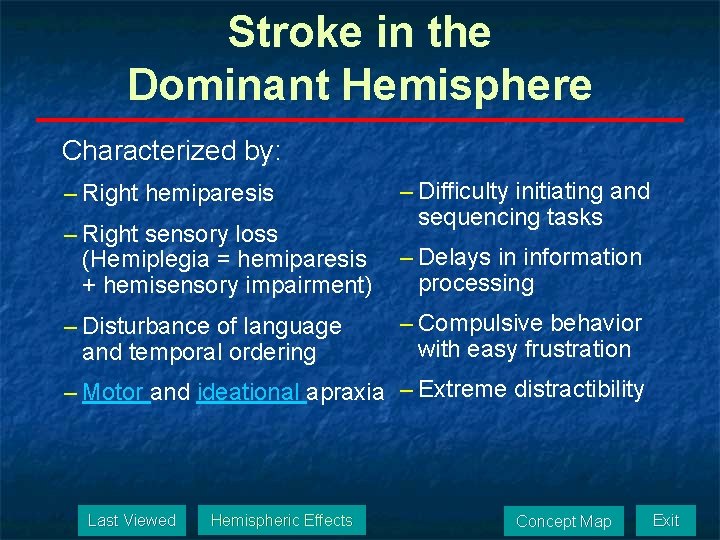
Stroke in the Dominant Hemisphere Characterized by: – Right hemiparesis – Right sensory loss (Hemiplegia = hemiparesis + hemisensory impairment) – Disturbance of language and temporal ordering – Difficulty initiating and sequencing tasks – Delays in information processing – Compulsive behavior with easy frustration – Motor and ideational apraxia – Extreme distractibility Last Viewed Hemispheric Effects Concept Map Exit
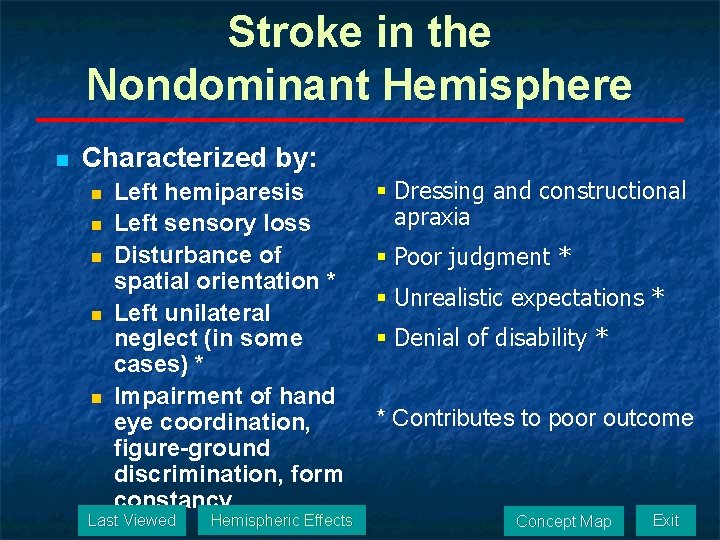
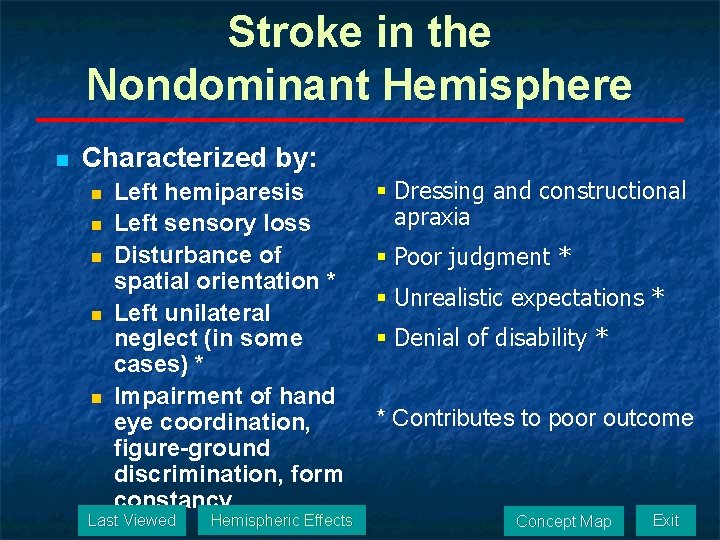
Stroke in the Nondominant Hemisphere n Characterized by: n n n Left hemiparesis Left sensory loss Disturbance of spatial orientation * Left unilateral neglect (in some cases) * Impairment of hand eye coordination, figure-ground discrimination, form constancy Last Viewed Hemispheric Effects § Dressing and constructional apraxia § Poor judgment * § Unrealistic expectations * § Denial of disability * * Contributes to poor outcome Concept Map Exit
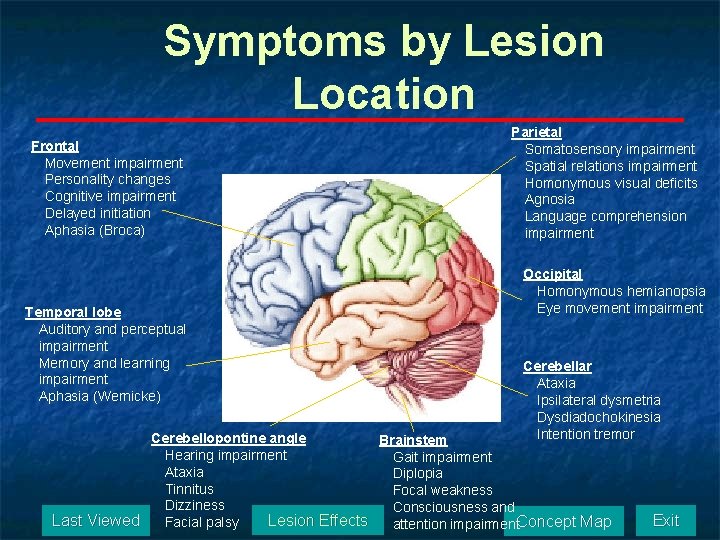
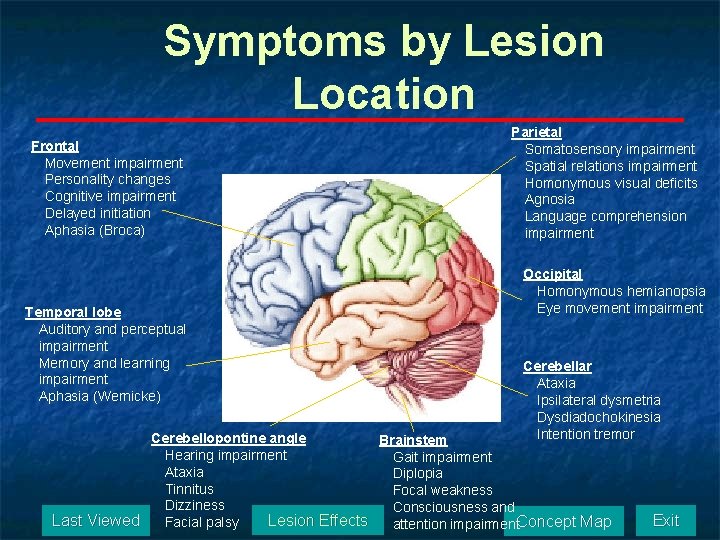
Symptoms by Lesion Location Frontal Movement impairment Personality changes Cognitive impairment Delayed initiation Aphasia (Broca) Temporal lobe Auditory and perceptual impairment Memory and learning impairment Aphasia (Wernicke) Parietal Somatosensory impairment Spatial relations impairment Homonymous visual deficits Agnosia Language comprehension impairment Occipital Homonymous hemianopsia Eye movement impairment Cerebellar Ataxia Ipsilateral dysmetria Dysdiadochokinesia Intention tremor Cerebellopontine angle Brainstem Hearing impairment Gait impairment Ataxia Diplopia Tinnitus Focal weakness Dizziness Consciousness and Lesion Effects Last Viewed Facial palsy attention impairment. Concept Map Exit
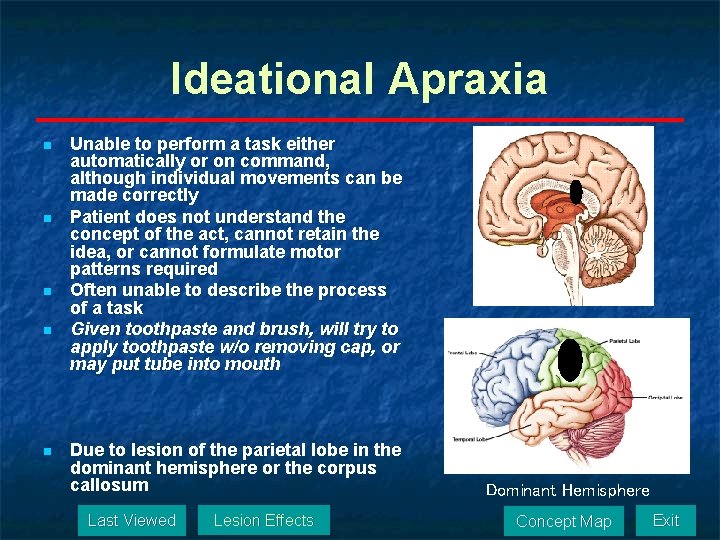
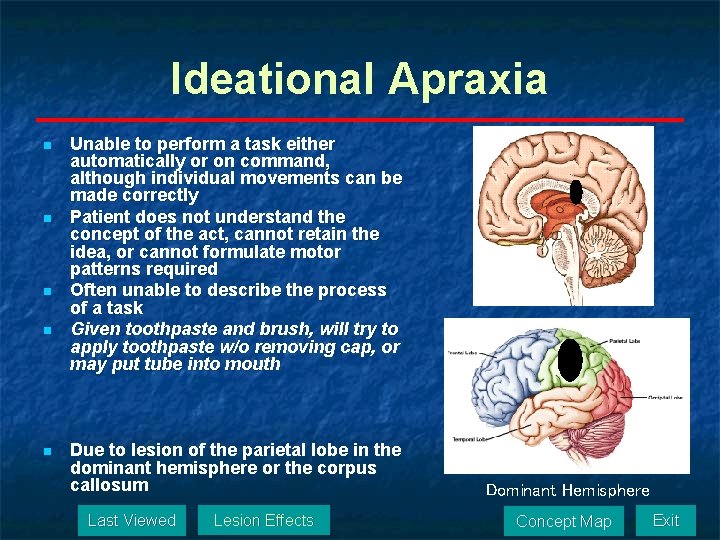
Ideational Apraxia n n n Unable to perform a task either automatically or on command, although individual movements can be made correctly Patient does not understand the concept of the act, cannot retain the idea, or cannot formulate motor patterns required Often unable to describe the process of a task Given toothpaste and brush, will try to apply toothpaste w/o removing cap, or may put tube into mouth Due to lesion of the parietal lobe in the dominant hemisphere or the corpus callosum Last Viewed Lesion Effects Dominant Hemisphere Concept Map Exit
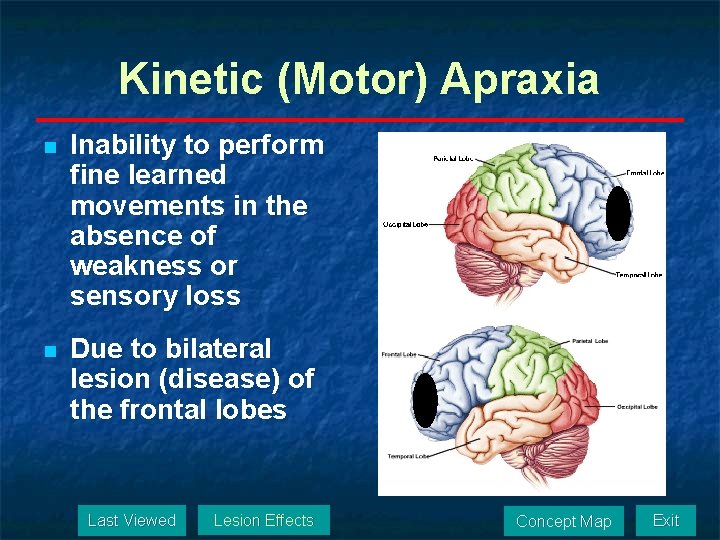
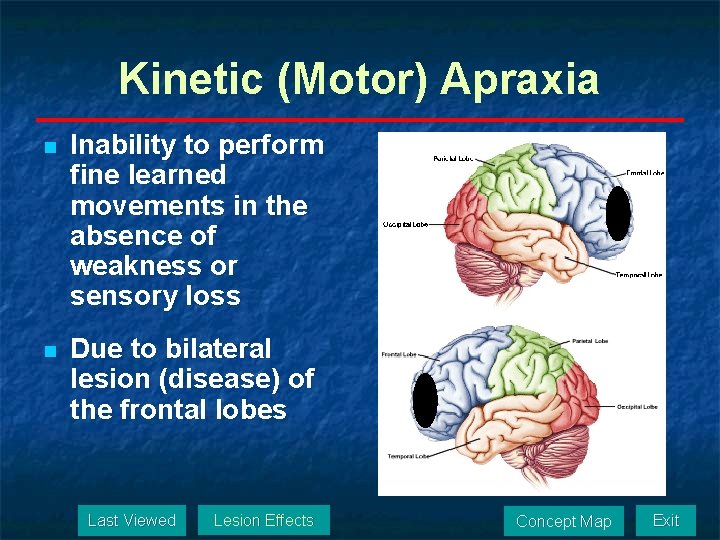
Kinetic (Motor) Apraxia n Inability to perform fine learned movements in the absence of weakness or sensory loss n Due to bilateral lesion (disease) of the frontal lobes Last Viewed Lesion Effects Concept Map Exit
Deficits n n Common Deficits Anatomic Substrate of Deficits Last Viewed Deficits Concept Map Exit
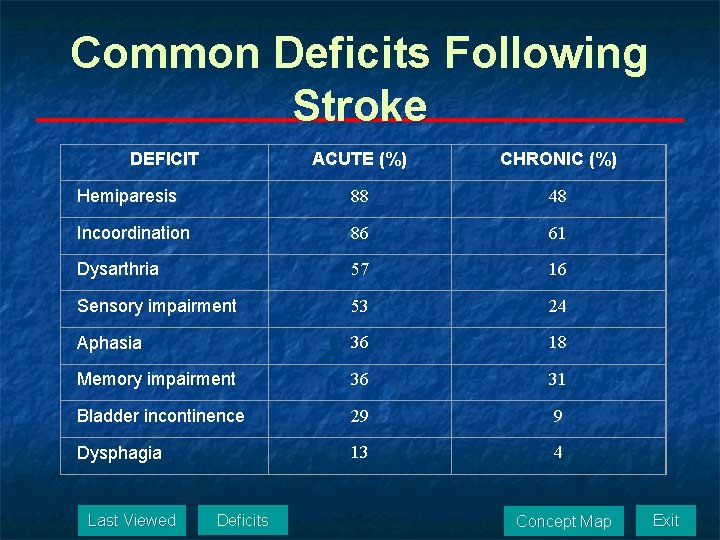
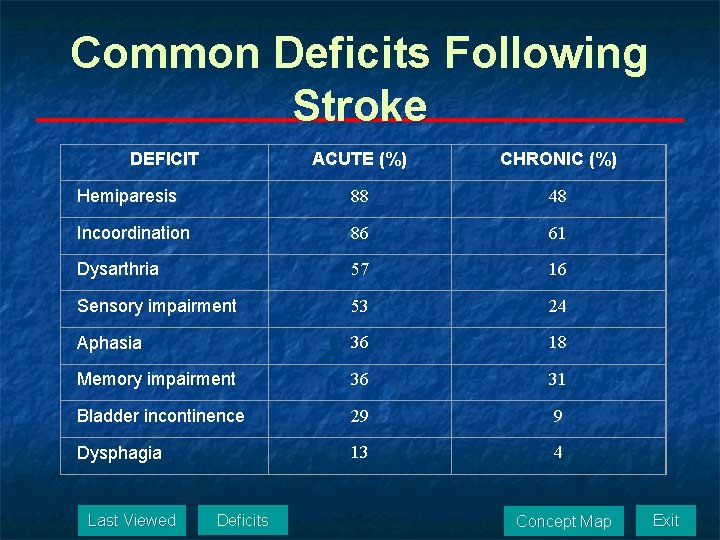
Common Deficits Following Stroke DEFICIT ACUTE (%) CHRONIC (%) Hemiparesis 88 48 Incoordination 86 61 Dysarthria 57 16 Sensory impairment 53 24 Aphasia 36 18 Memory impairment 36 31 Bladder incontinence 29 9 Dysphagia 13 4 Last Viewed Deficits Concept Map Exit
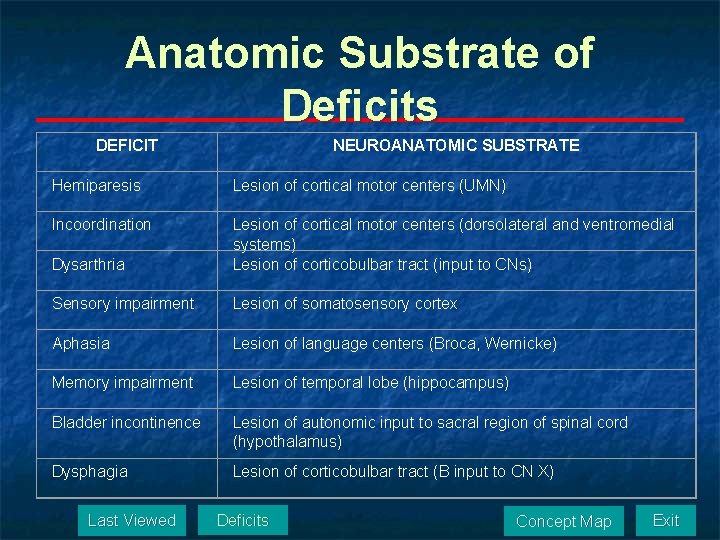
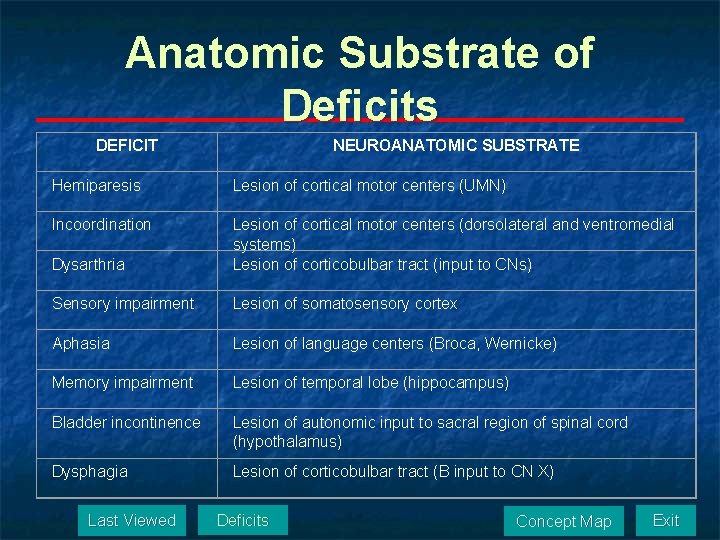
Anatomic Substrate of Deficits DEFICIT NEUROANATOMIC SUBSTRATE Hemiparesis Lesion of cortical motor centers (UMN) Incoordination Dysarthria Lesion of cortical motor centers (dorsolateral and ventromedial systems) Lesion of corticobulbar tract (input to CNs) Sensory impairment Lesion of somatosensory cortex Aphasia Lesion of language centers (Broca, Wernicke) Memory impairment Lesion of temporal lobe (hippocampus) Bladder incontinence Lesion of autonomic input to sacral region of spinal cord (hypothalamus) Dysphagia Lesion of corticobulbar tract (B input to CN X) Last Viewed Deficits Concept Map Exit
Recovery n n Natural History of Recovery With Intervention Pattern of Recovery Theories of Recovery Last Viewed Recovery Concept Map Exit
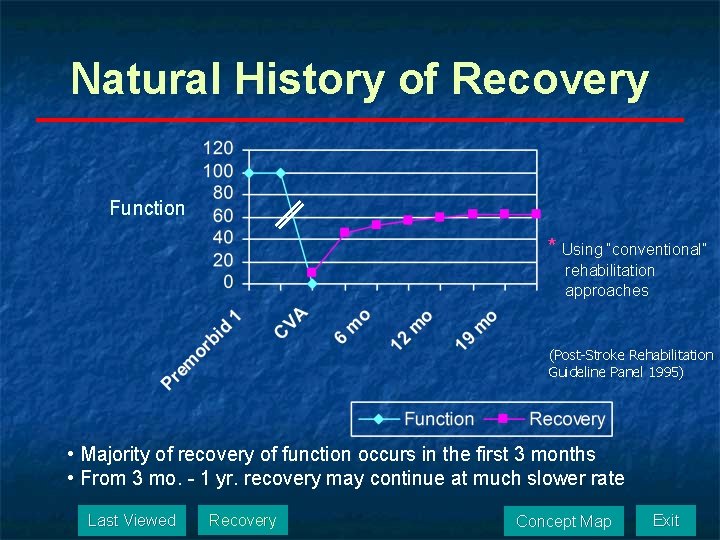
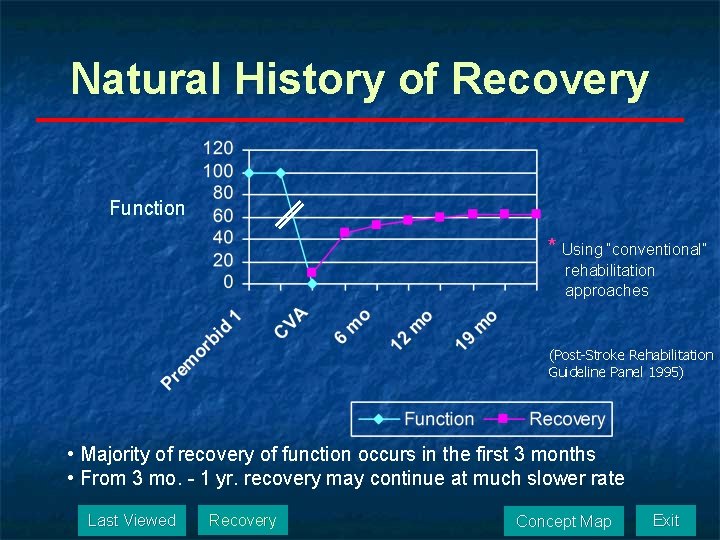
Natural History of Recovery Function * Using “conventional” rehabilitation approaches (Post-Stroke Rehabilitation Guideline Panel 1995) • Majority of recovery of function occurs in the first 3 months • From 3 mo. - 1 yr. recovery may continue at much slower rate Last Viewed Recovery Concept Map Exit
Recovery With Intervention Evidence-based Practice n Data now show that natural history of recovery can be changed by the right type of intervention n Constraint induced therapy (CIT) and weight supported treadmill training (WSTT) change the natural history of recovery n “Conventional” rehabilitation techniques do not change the natural history of recovery Last Viewed Recovery Concept Map Exit
Pattern of Recovery n Initially: hypotonia/ flaccidity n n Due to the interruption of UMN input to LMN Days to weeks later: hypertonia/ spasticity ? ? ? A leading question in stroke recovery n Due in part to n Decreased threshold in alpha LMN and n Denervation supersensitivity n Last Viewed Recovery Concept Map Exit
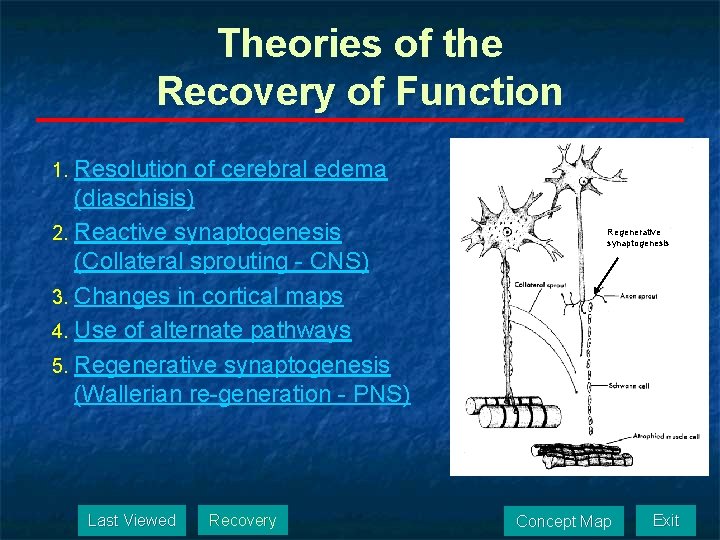
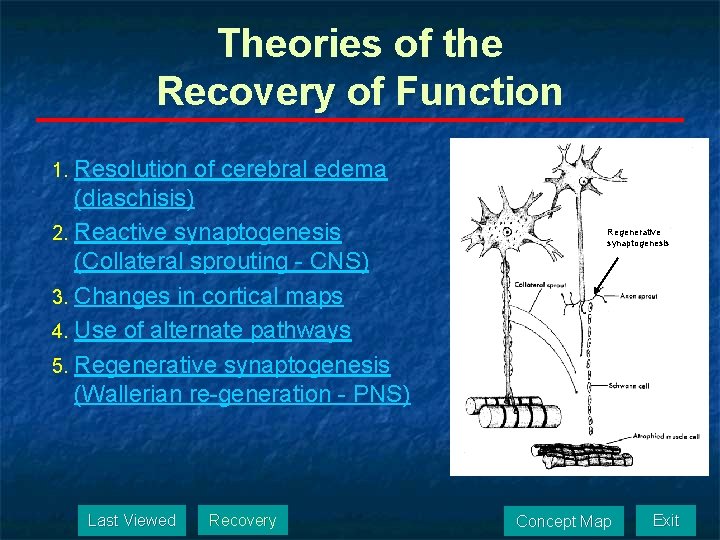
Theories of the Recovery of Function 1. Resolution of cerebral edema (diaschisis) 2. Reactive synaptogenesis (Collateral sprouting - CNS) 3. Changes in cortical maps 4. Use of alternate pathways 5. Regenerative synaptogenesis (Wallerian re-generation - PNS) Last Viewed Recovery Regenerative synaptogenesis Concept Map Exit
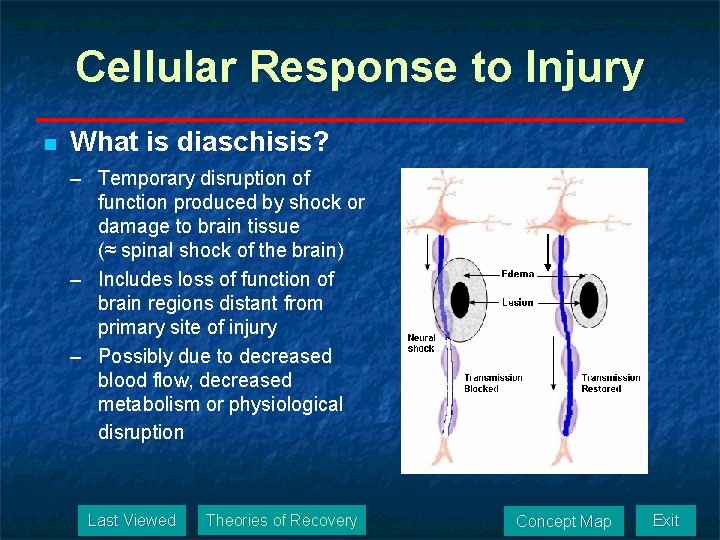
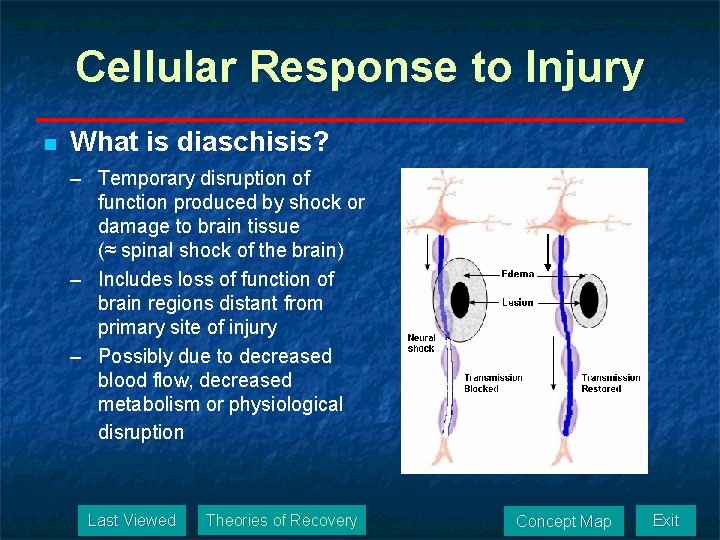
Cellular Response to Injury n What is diaschisis? – Temporary disruption of function produced by shock or damage to brain tissue (≈ spinal shock of the brain) – Includes loss of function of brain regions distant from primary site of injury – Possibly due to decreased blood flow, decreased metabolism or physiological disruption Last Viewed Theories of Recovery Concept Map Exit
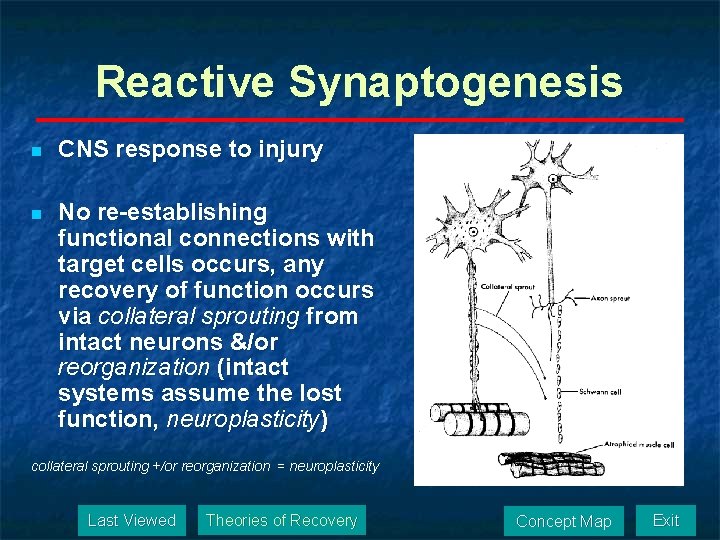
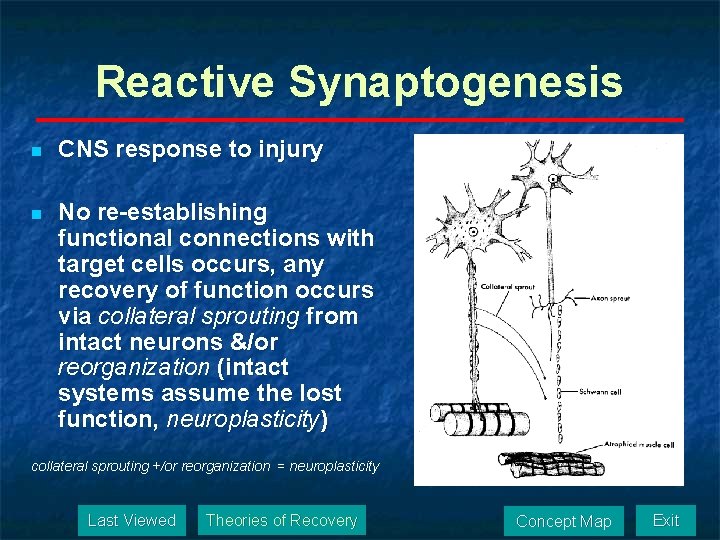
Reactive Synaptogenesis n CNS response to injury n No re-establishing functional connections with target cells occurs, any recovery of function occurs via collateral sprouting from intact neurons &/or reorganization (intact systems assume the lost function, neuroplasticity) collateral sprouting +/or reorganization = neuroplasticity Last Viewed Theories of Recovery Concept Map Exit
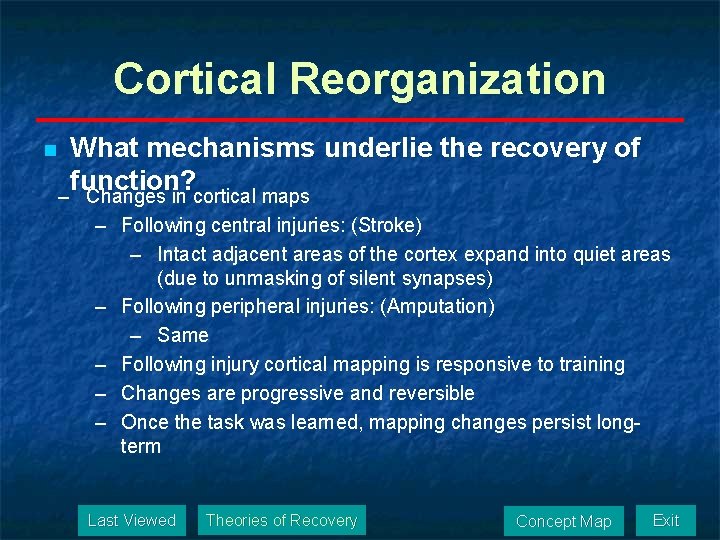
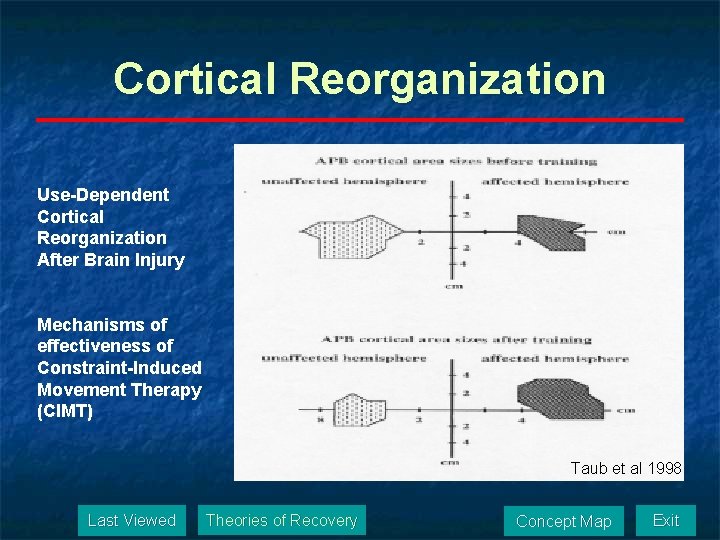
Cortical Reorganization n What mechanisms underlie the recovery of function? – Changes in cortical maps – Following central injuries: (Stroke) – Intact adjacent areas of the cortex expand into quiet areas (due to unmasking of silent synapses) – Following peripheral injuries: (Amputation) – Same – Following injury cortical mapping is responsive to training – Changes are progressive and reversible – Once the task was learned, mapping changes persist longterm Last Viewed Theories of Recovery Concept Map Exit
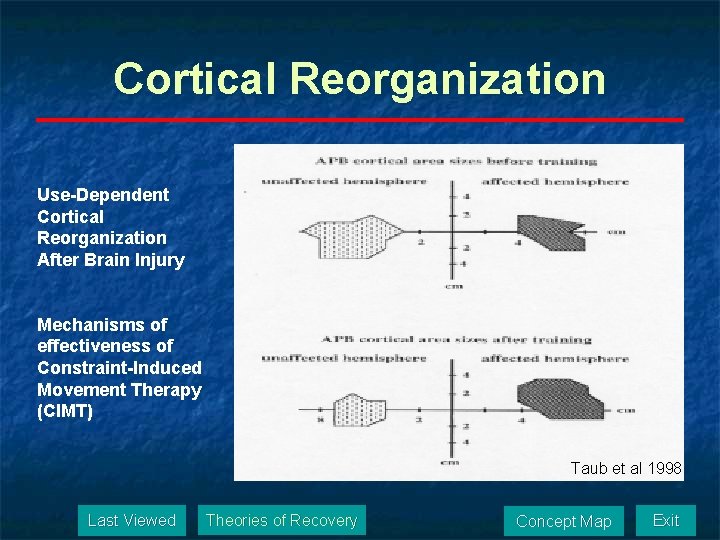
Cortical Reorganization Use-Dependent Cortical Reorganization After Brain Injury Mechanisms of effectiveness of Constraint-Induced Movement Therapy (CIMT) Taub et al 1998 Last Viewed Theories of Recovery Concept Map Exit
Alternate Pathways n What mechanisms underlie the recovery of function? – Ipsilateral motor tracts take over Last Viewed Theories of Recovery Concept Map Exit
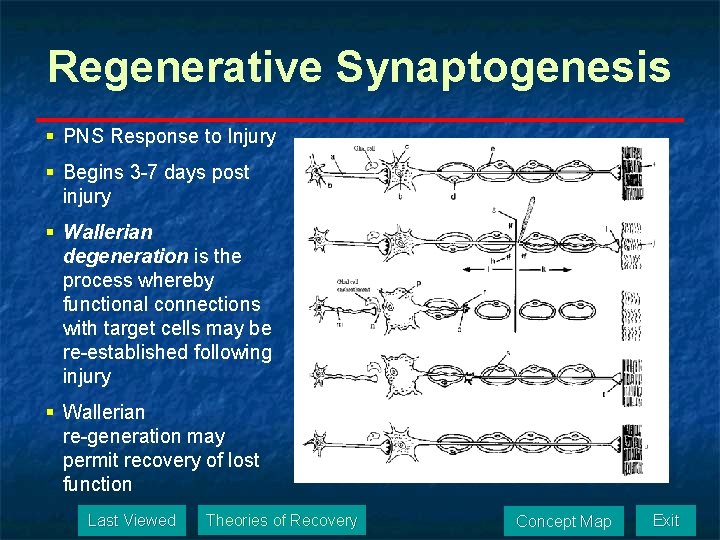
Regenerative Synaptogenesis § PNS Response to Injury § Begins 3 -7 days post injury § Wallerian degeneration is the process whereby functional connections with target cells may be re-established following injury § Wallerian re-generation may permit recovery of lost function Last Viewed Theories of Recovery Concept Map Exit
Stroke Treatment n n n Referral Patterns Treatment Efficacy “Unaffected" Upper Extremity Stroke Treatment Recovery of Locomotion Life Probability Tables Last Viewed Stroke Treatment Concept Map Exit
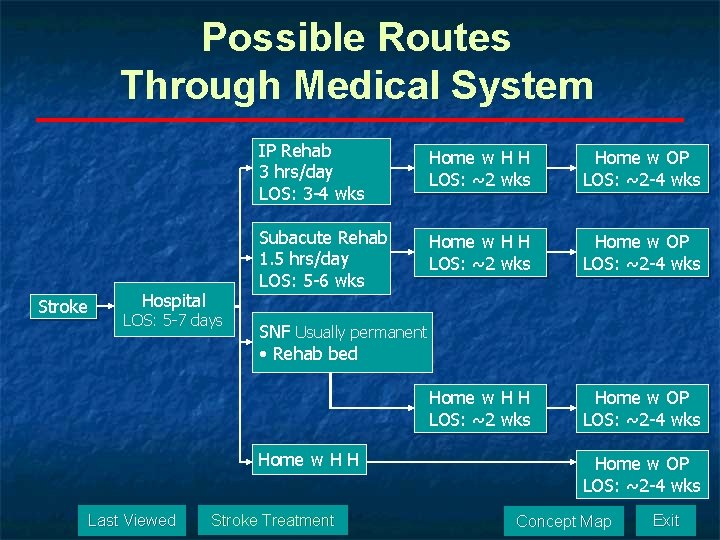
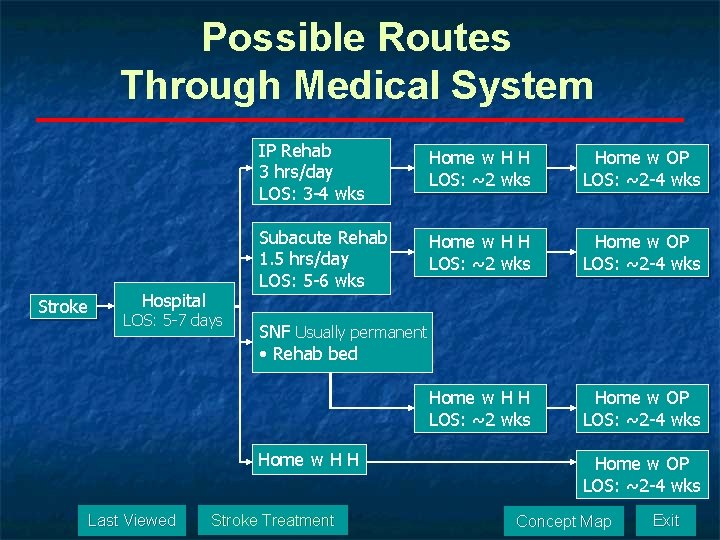
Possible Routes Through Medical System Stroke Hospital LOS: 5 -7 days IP Rehab 3 hrs/day LOS: 3 -4 wks Home w H H LOS: ~2 wks Home w OP LOS: ~2 -4 wks Subacute Rehab 1. 5 hrs/day LOS: 5 -6 wks Home w H H LOS: ~2 wks Home w OP LOS: ~2 -4 wks SNF Usually permanent • Rehab bed Home w H H Last Viewed Stroke Treatment Home w OP LOS: ~2 -4 wks Concept Map Exit
Treatment Efficacy n n Conventional therapy produces only a modest, temporary improvement in function (The Lancet Vol 359 No 9302, January 19, 2002) PT treatment effects are achieved through a neuroplastic reorganization of motor control centers (Treatment-Induced Cortical Reorganization After Stroke in Humans. Taub et al. , Stroke 2000; 31: 1210) Last Viewed Stroke Treatment Concept Map Exit
“Unaffected" Upper Extremity n Following stroke, the unaffected UE showed decreases in: functional independence due to decreased fine manual dexterity n activity level due to decreases in kinesthesia and gross dexterity n n There is no such thing as an “unaffected” extremity Last Viewed Stroke Treatment Concept Map Exit
Stroke Treatment n 1/2 Prevention n Reduce modifiable risk factors n n Vigorous exercise (J Stroke: Oct 2003) MD: antiplatlet or anticoagulant therapy Last Viewed Stroke Treatment Concept Map Exit
Stroke Treatment n 2/2 Acute phase MD: thrombolytic agents or acute anticoagulation drugs (TPA) may be successful in reversing primary impairments n PT: improve functional ability and prevent secondary impairments (deconditioning, pneumonia, UTI, pressure sores, DVT) n Last Viewed Stroke Treatment Concept Map Exit
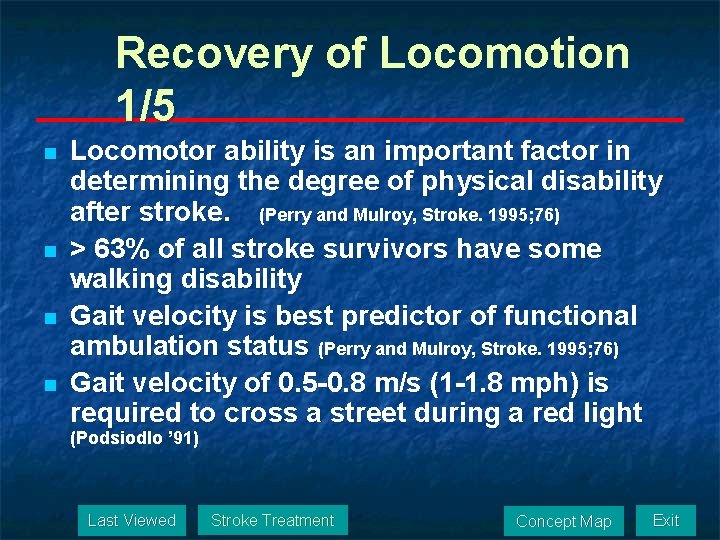
Recovery of Locomotion 1/5 n n Locomotor ability is an important factor in determining the degree of physical disability after stroke. (Perry and Mulroy, Stroke. 1995; 76) > 63% of all stroke survivors have some walking disability Gait velocity is best predictor of functional ambulation status (Perry and Mulroy, Stroke. 1995; 76) Gait velocity of 0. 5 -0. 8 m/s (1 -1. 8 mph) is required to cross a street during a red light (Podsiodlo ’ 91) Last Viewed Stroke Treatment Concept Map Exit
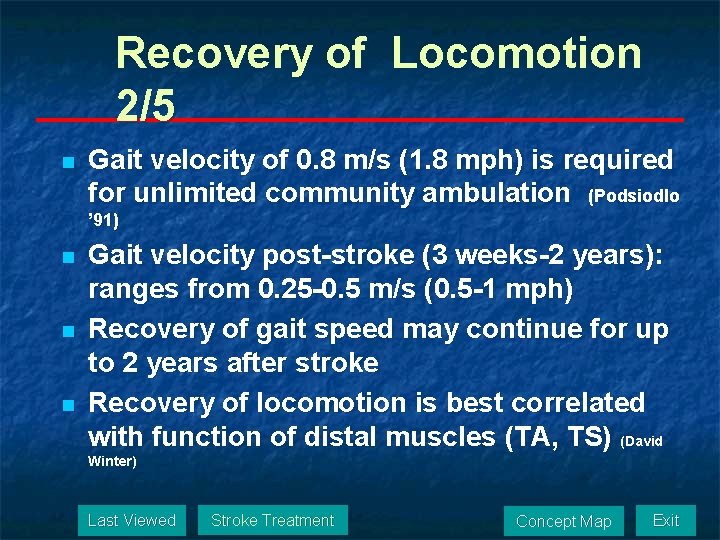
Recovery of Locomotion 2/5 n Gait velocity of 0. 8 m/s (1. 8 mph) is required for unlimited community ambulation (Podsiodlo ’ 91) n n n Gait velocity post-stroke (3 weeks-2 years): ranges from 0. 25 -0. 5 m/s (0. 5 -1 mph) Recovery of gait speed may continue for up to 2 years after stroke Recovery of locomotion is best correlated with function of distal muscles (TA, TS) (David Winter) Last Viewed Stroke Treatment Concept Map Exit
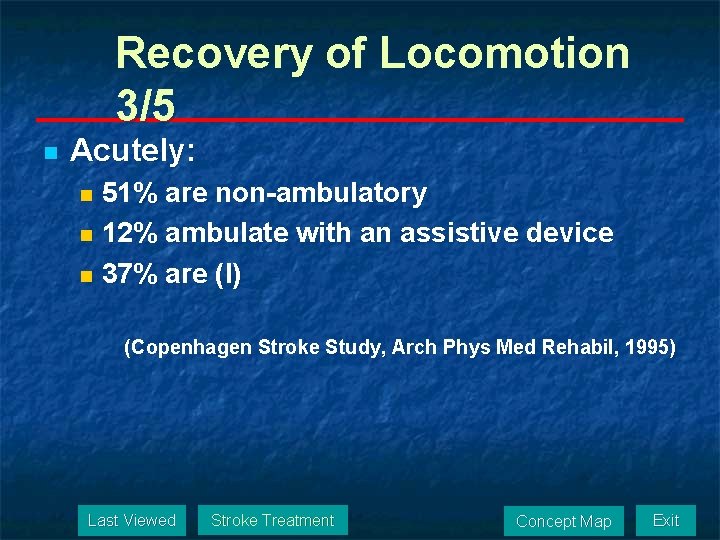
Recovery of Locomotion 3/5 n Acutely: 51% are non-ambulatory n 12% ambulate with an assistive device n 37% are (I) n (Copenhagen Stroke Study, Arch Phys Med Rehabil, 1995) Last Viewed Stroke Treatment Concept Map Exit
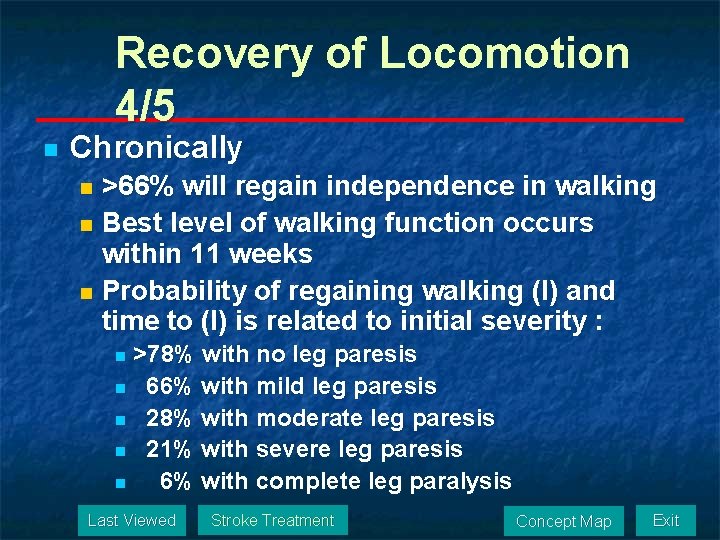
Recovery of Locomotion 4/5 n Chronically >66% will regain independence in walking n Best level of walking function occurs within 11 weeks n Probability of regaining walking (I) and time to (I) is related to initial severity : n >78% with no leg paresis n 66% with mild leg paresis n 28% with moderate leg paresis n 21% with severe leg paresis n 6% with complete leg paralysis n Last Viewed Stroke Treatment Concept Map Exit
Recovery of Locomotion 5/5 n Effects of Task-Specific Locomotor and Strength Training in Adults Who Were Ambulatory After Stroke: Results of the STEPS RCT n Phase II RCT to determine effects of combined task-specific and LE strength training to improve walking after stroke n Subjects: 80 adults 4 mo – 5 yrs post stroke n Method: BWSTT, CYCLE, LE-EX, UE-EX n n BWSTT/ UE-EX, CYCLE / UE-EX, BWSTT/CYCLE, BWSTT/ LE-EX Dosage: 4/wk x 6 wks (24 sessions) DV: Self-selected walking speed, fast walking speed, 6 MWT; pre- and post intervention and 6 mo post Results: n n BWSTT more effective than cycling in improving walking speed and maintaining gains at 6 mo. LE strength training, alternate days, produced no added benefit (Sullivan et al, (Phys Ther 2007; 87: 1580 -1602) Last Viewed Stroke Treatment Concept Map Exit
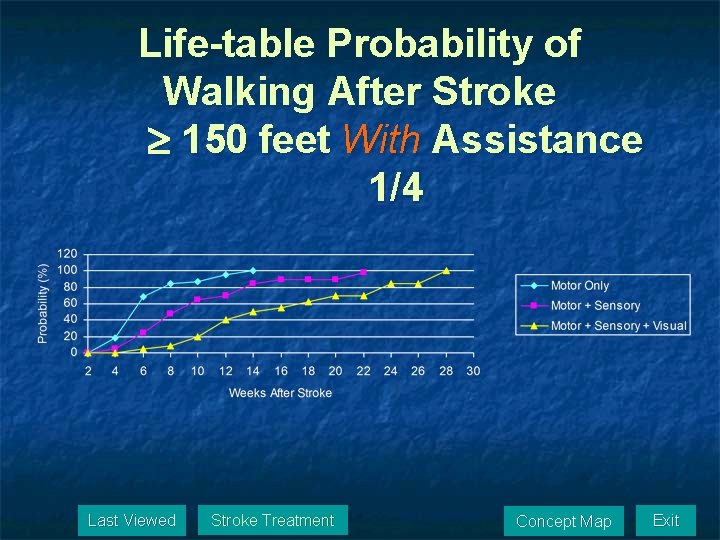
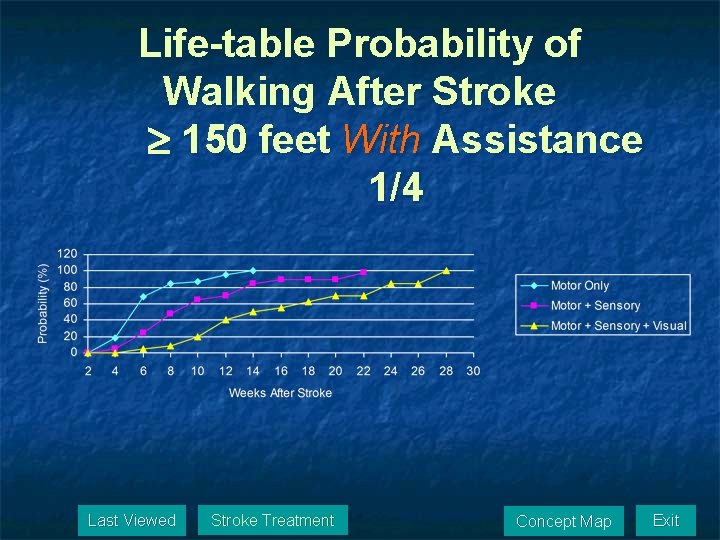
Life-table Probability of Walking After Stroke 150 feet With Assistance 1/4 Last Viewed Stroke Treatment Concept Map Exit
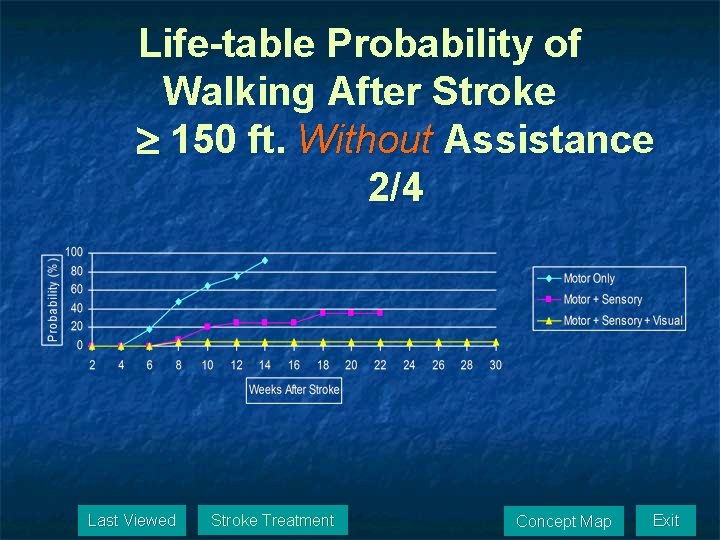
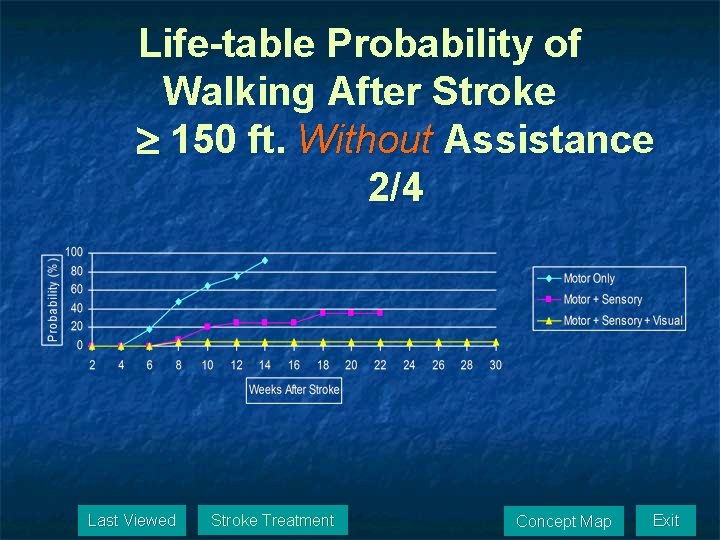
Life-table Probability of Walking After Stroke 150 ft. Without Assistance 2/4 Last Viewed Stroke Treatment Concept Map Exit
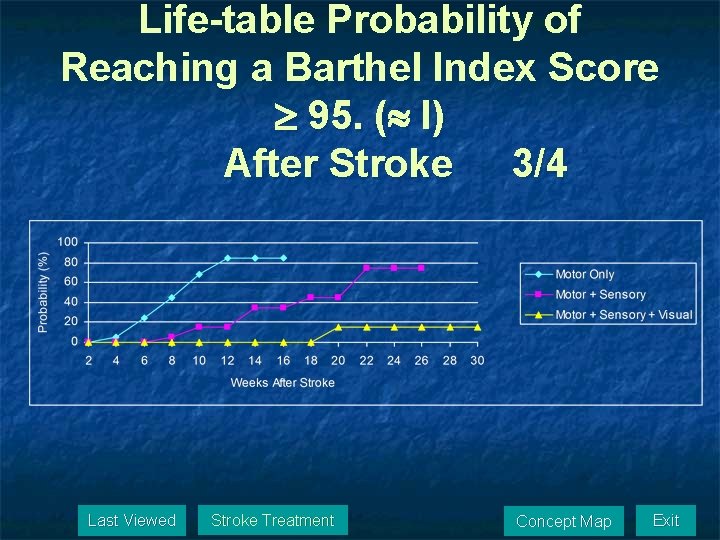
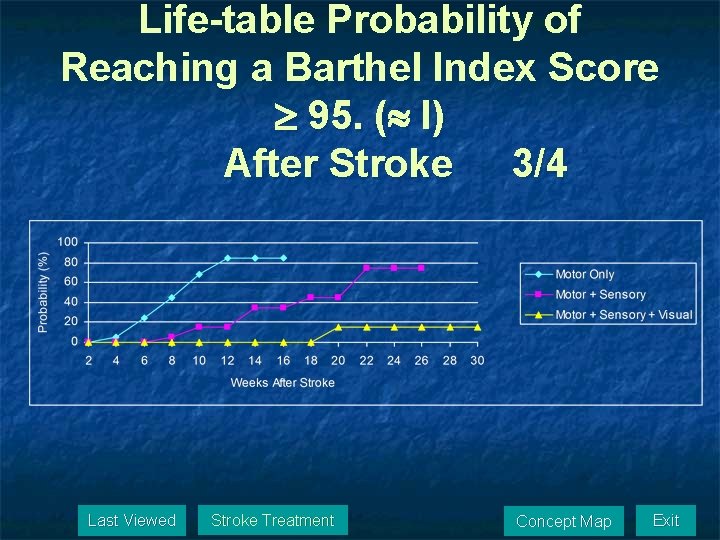
Life-table Probability of Reaching a Barthel Index Score 95. ( I) After Stroke 3/4 Last Viewed Stroke Treatment Concept Map Exit
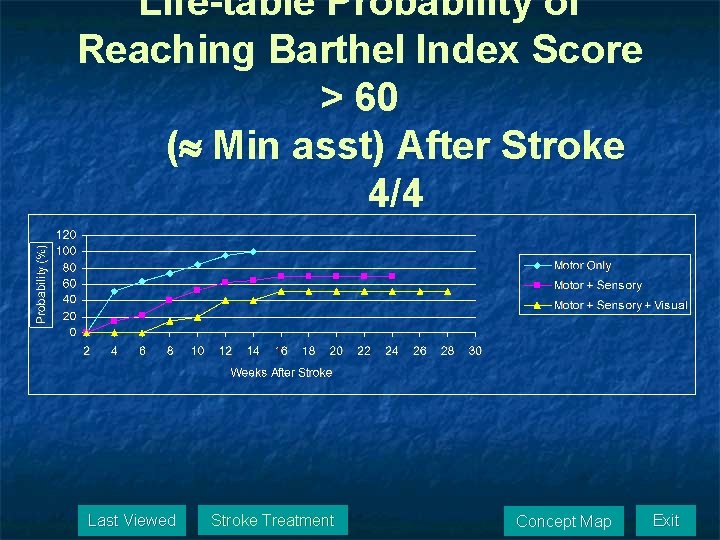
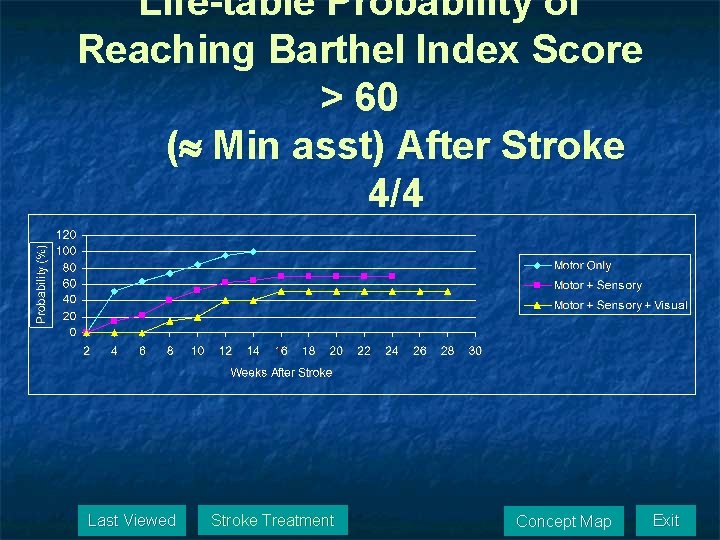
Life-table Probability of Reaching Barthel Index Score > 60 ( Min asst) After Stroke 4/4 Last Viewed Stroke Treatment Concept Map Exit
The Cerebrovascular System n n n Oxygen demands Metabolism Cerebrovascular disease Blood supply to the brain Carotid system Vertebrobasilar system Circle of Willis Perfusion Territories Cerebellar arteries Venous Drainage Blood supply to spinal cord Patient cases Last Viewed Posture & Balance Concept Map Exit
Oxygen Demands n The CNS (brain and spinal cord) is the best protected organ in the human body including mechanisms to protect its blood supply n At approximately 3 pounds, the brain accounts for about 2% of body mass n Consumes 17% of cardiac output n Responsible for 20% of oxygen consumption at rest Last Viewed Cerebrovascular System Concept Map Exit
Metabolism n Brain’s sole source of energy is aerobic or oxidative metabolism. n Therefore, the brain requires a constant supply of O 2 and glucose, 24 hours a day. Last Viewed Cerebrovascular System Concept Map Exit
Cerebrovascular Disease n While the blood supply to the brain is highly protected, cerebrovascular disease is the third leading cause of death in American adults and the number one cause of chronic functional disability requiring rehabilitative intervention. Last Viewed Cerebrovascular System Concept Map Exit
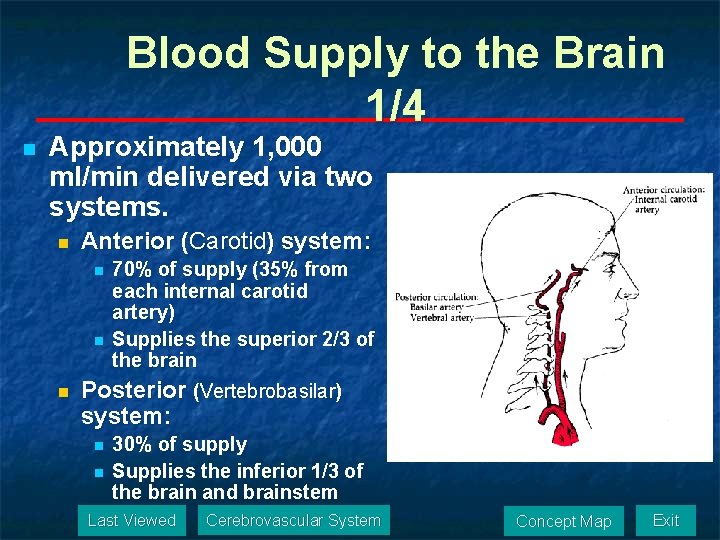
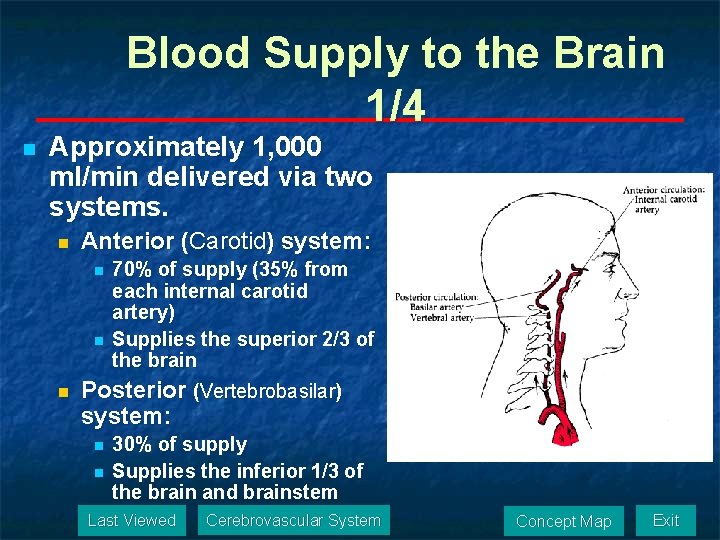
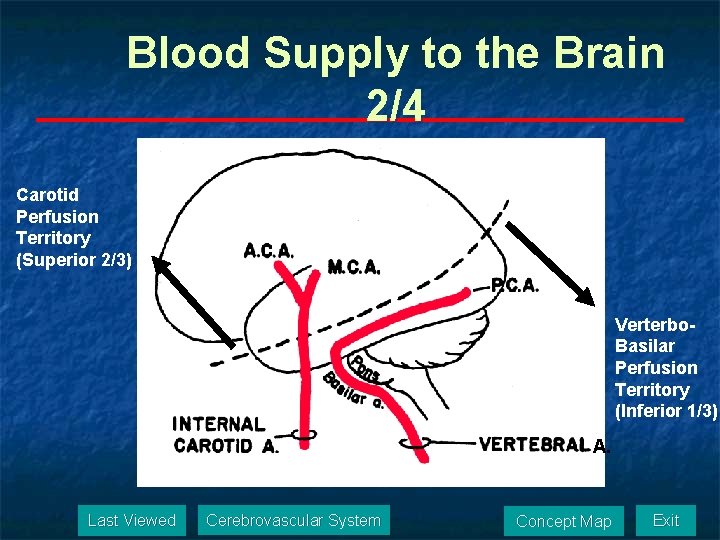
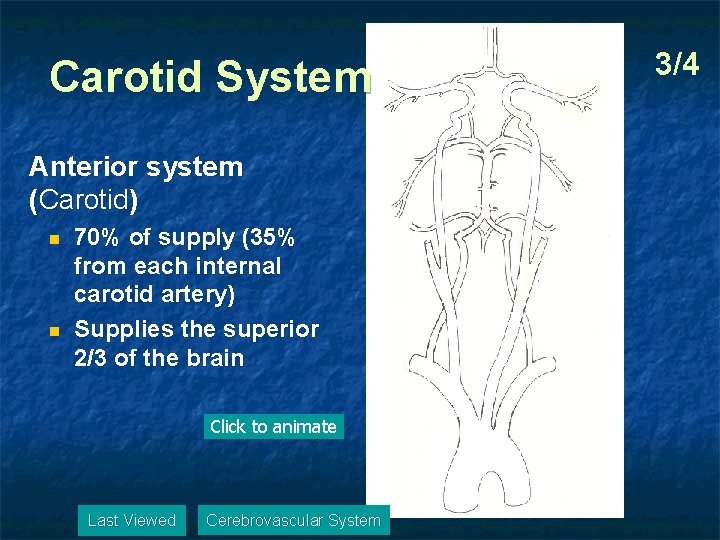
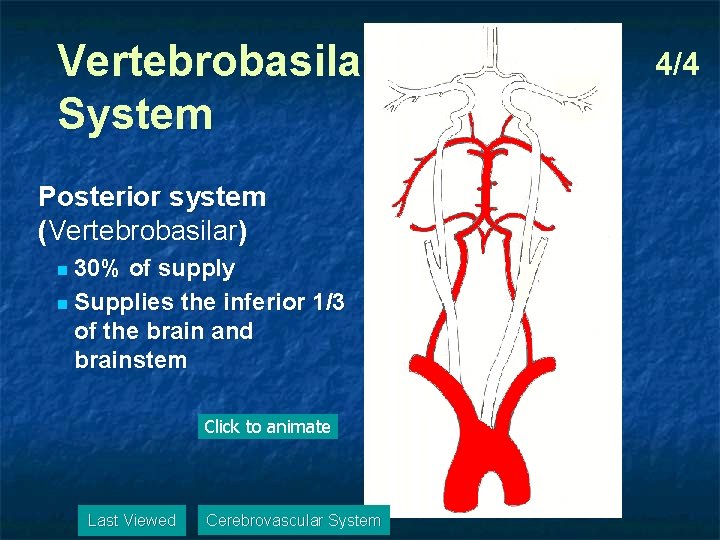
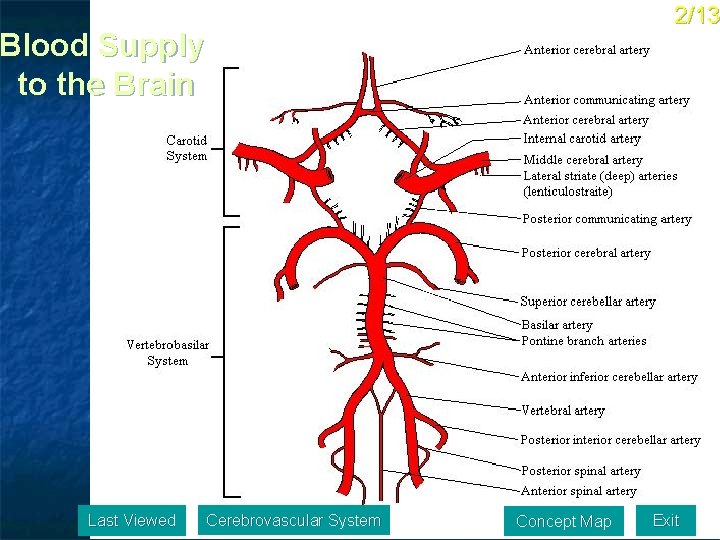
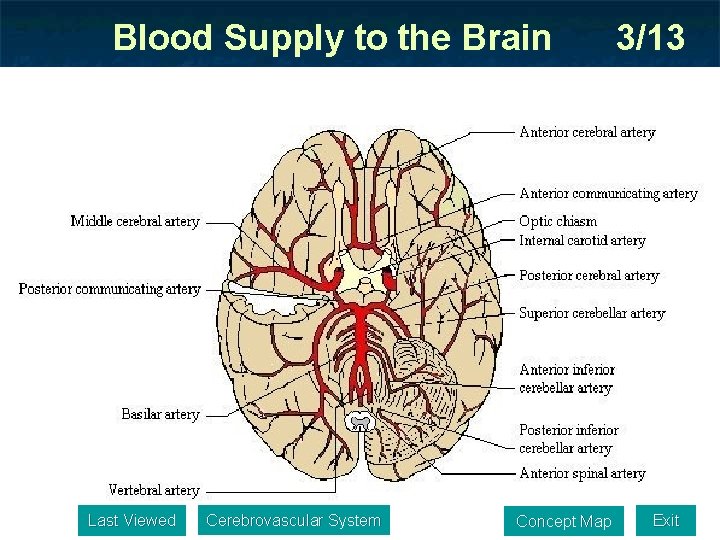
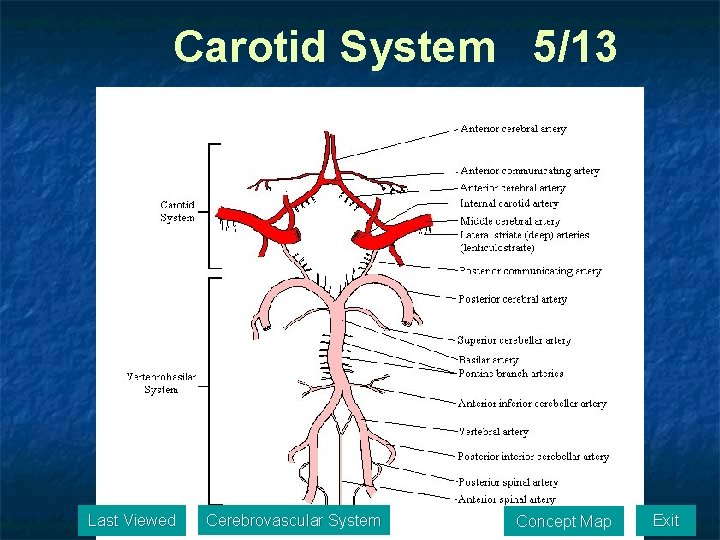
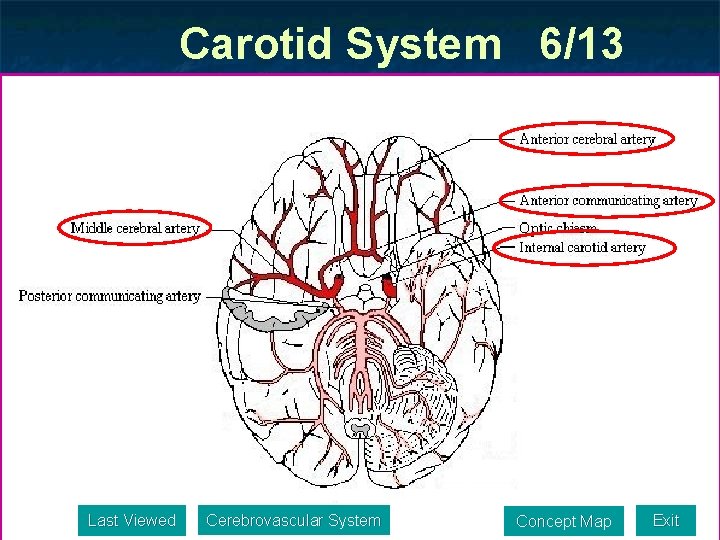
Blood Supply to the Brain 1/4 n Approximately 1, 000 ml/min delivered via two systems. n Anterior (Carotid) system: n n n 70% of supply (35% from each internal carotid artery) Supplies the superior 2/3 of the brain Posterior (Vertebrobasilar) system: n n 30% of supply Supplies the inferior 1/3 of the brain and brainstem Last Viewed Cerebrovascular System Concept Map Exit
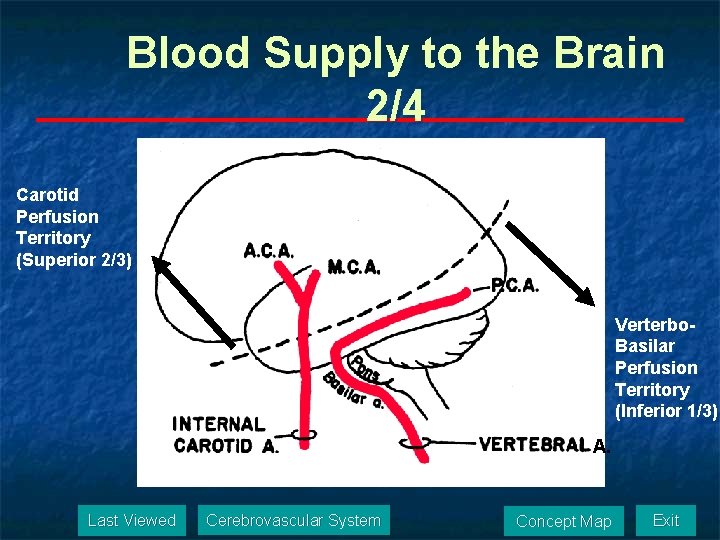
Blood Supply to the Brain 2/4 Carotid Perfusion Territory (Superior 2/3) Verterbo. Basilar Perfusion Territory (Inferior 1/3) A. Last Viewed Cerebrovascular System Concept Map Exit
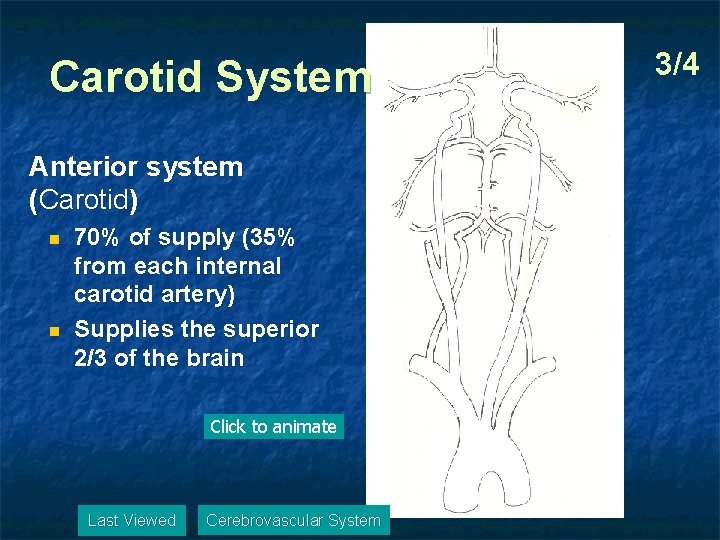
Carotid System Anterior system (Carotid) n n 70% of supply (35% from each internal carotid artery) Supplies the superior 2/3 of the brain Click to animate Last Viewed Cerebrovascular System 3/4
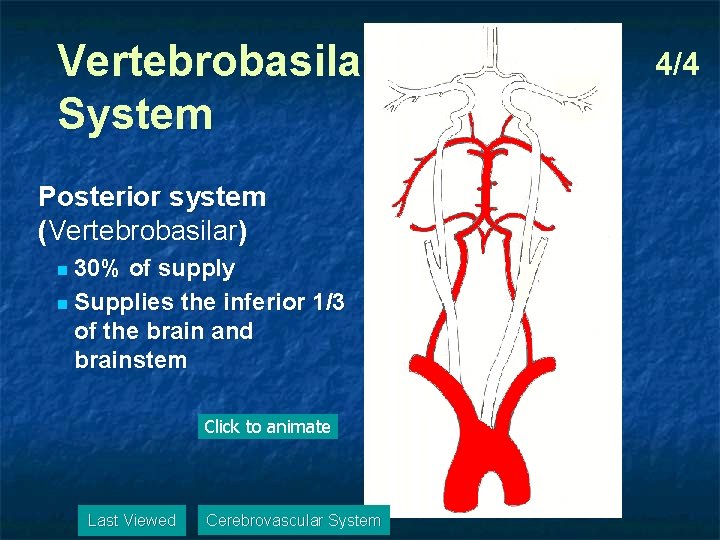
Vertebrobasilar System Posterior system (Vertebrobasilar) 30% of supply n Supplies the inferior 1/3 of the brain and brainstem n Click to animate Last Viewed Cerebrovascular System 4/4
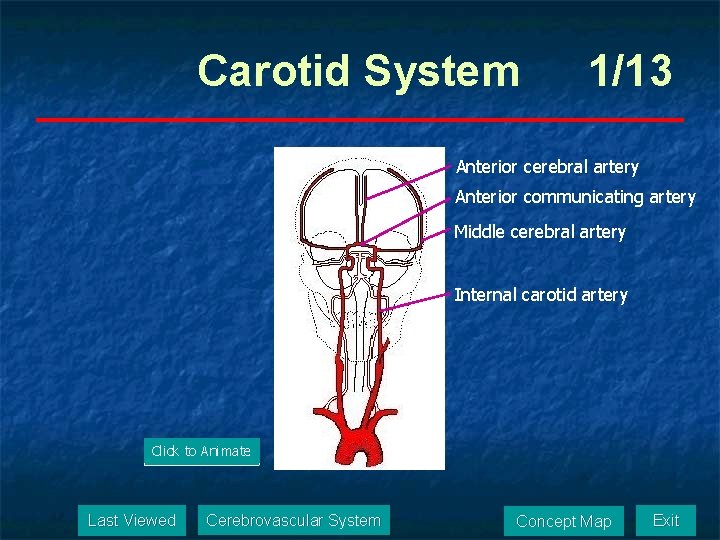
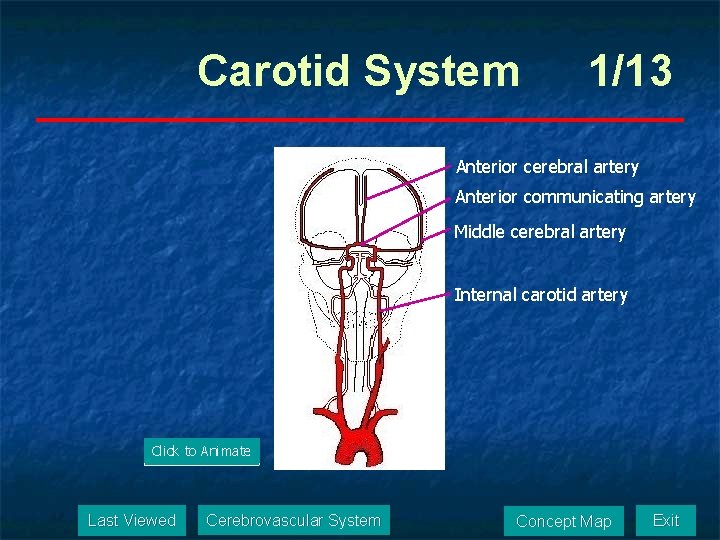
Carotid System 1/13 Anterior cerebral artery Anterior communicating artery Middle cerebral artery Internal carotid artery Click to Animate Last Viewed Cerebrovascular System Concept Map Exit
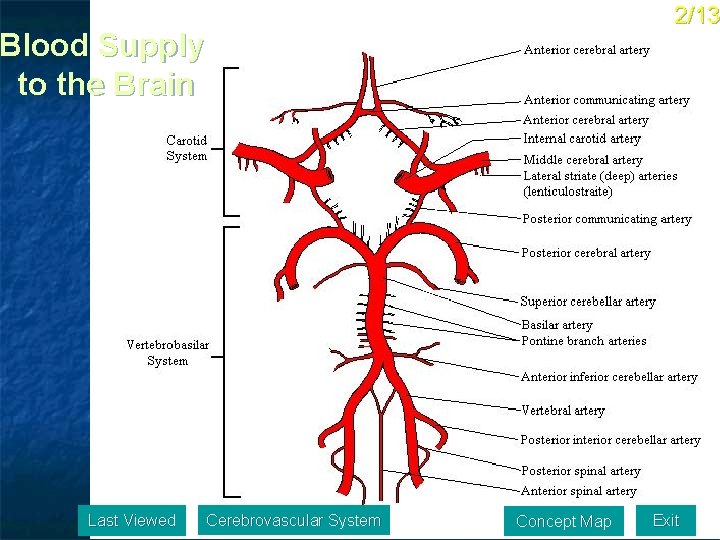
2/13 Blood Supply to the Brain Last Viewed Cerebrovascular System Concept Map Exit
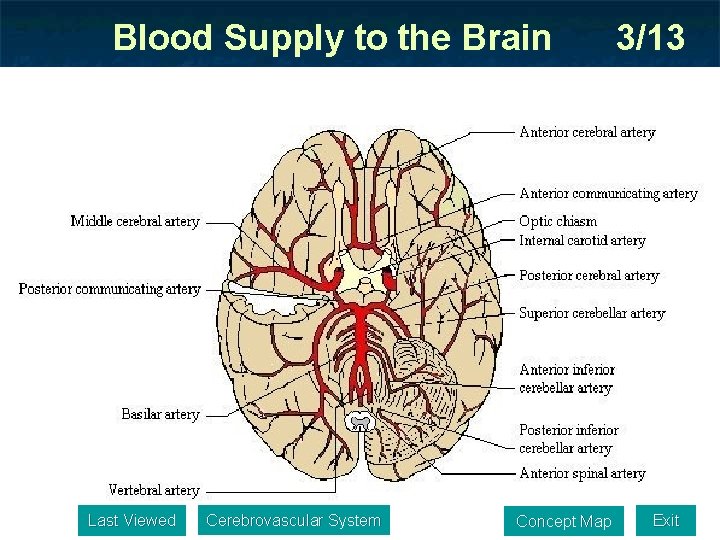
Blood Supply to the Brain Last Viewed Cerebrovascular System Concept Map 3/13 Exit
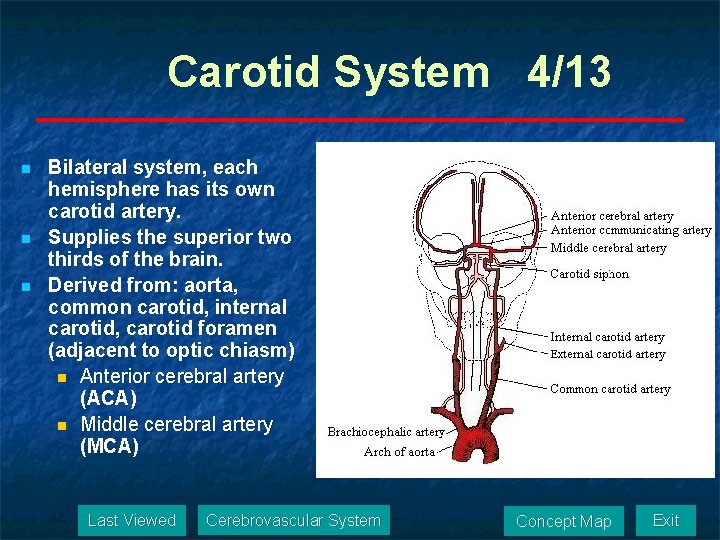
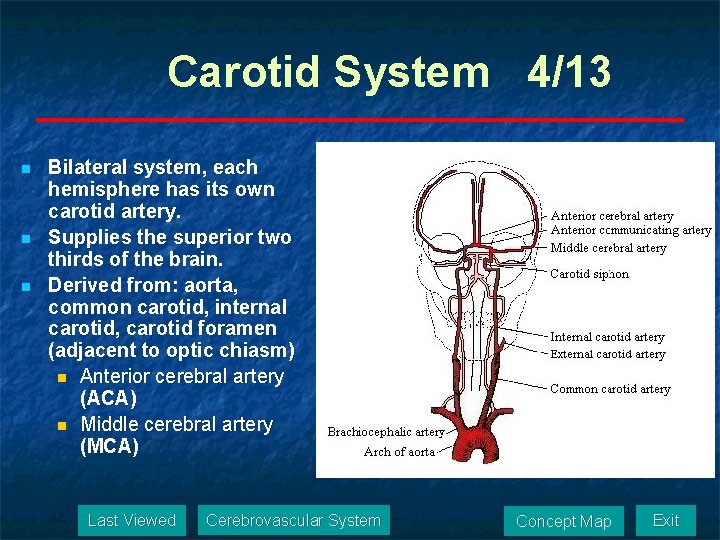
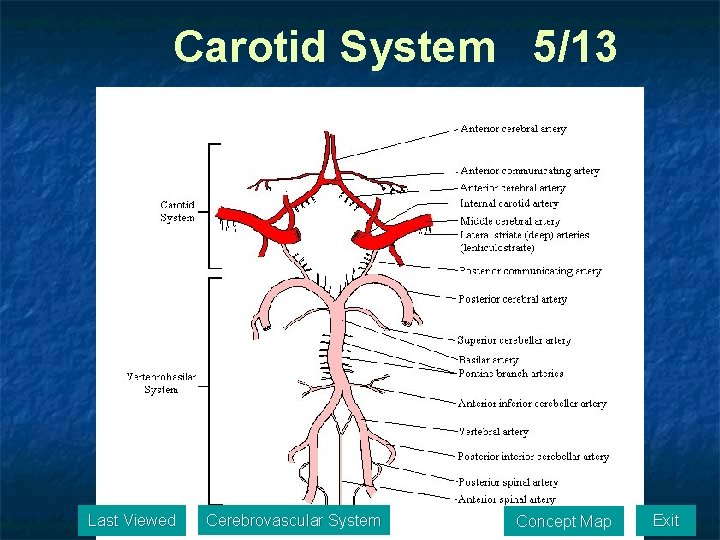
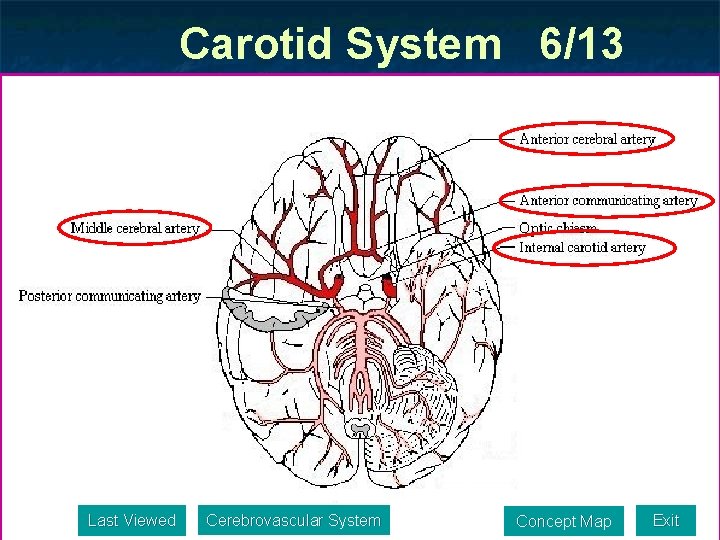
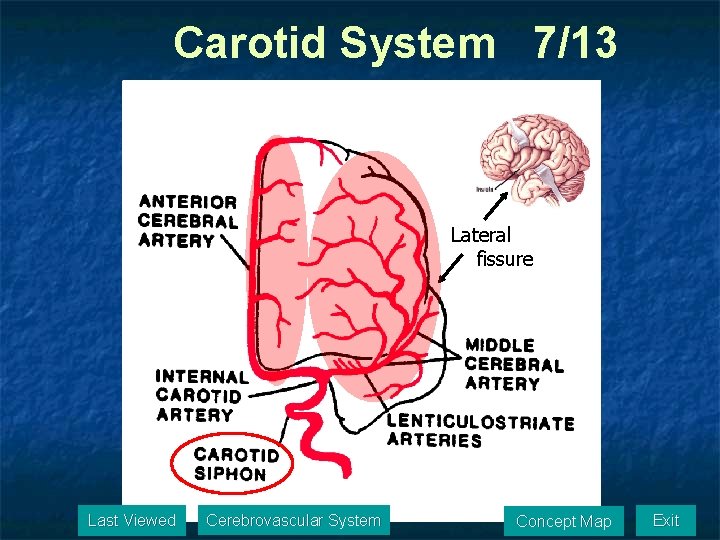
Carotid System 4/13 n n n Bilateral system, each hemisphere has its own carotid artery. Supplies the superior two thirds of the brain. Derived from: aorta, common carotid, internal carotid, carotid foramen (adjacent to optic chiasm) n Anterior cerebral artery (ACA) n Middle cerebral artery (MCA) Last Viewed Cerebrovascular System Concept Map Exit
Carotid System 5/13 Last Viewed Cerebrovascular System Concept Map Exit
Carotid System 6/13 Last Viewed Cerebrovascular System Concept Map Exit
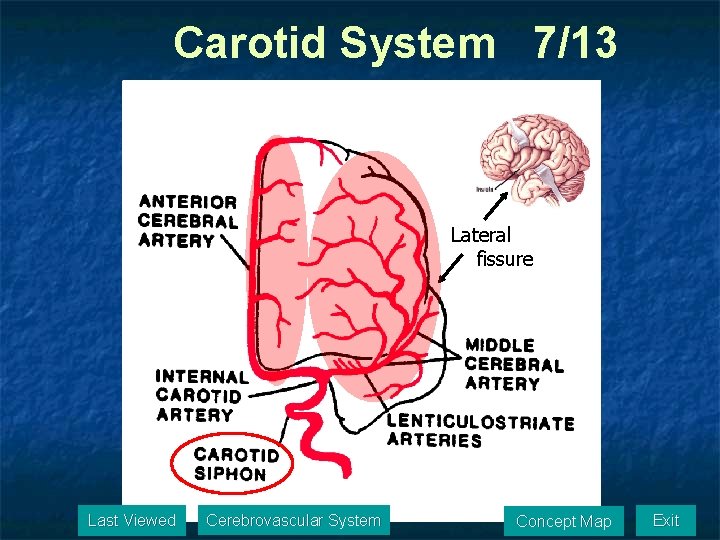
Carotid System 7/13 Lateral fissure Last Viewed Cerebrovascular System Concept Map Exit
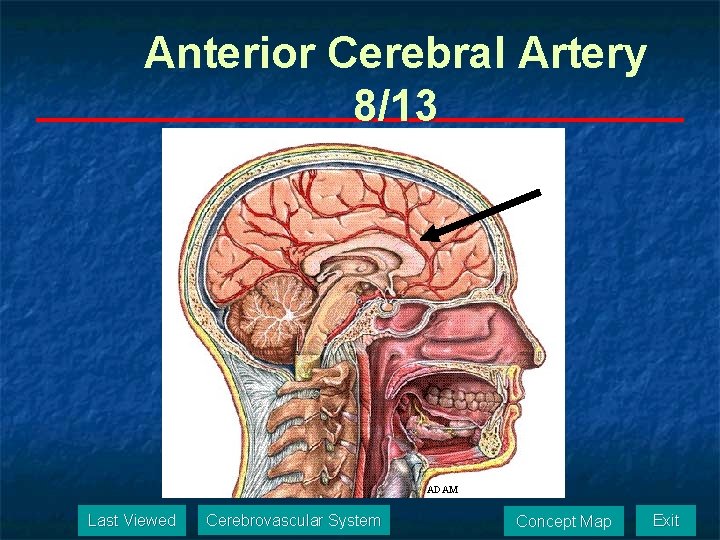
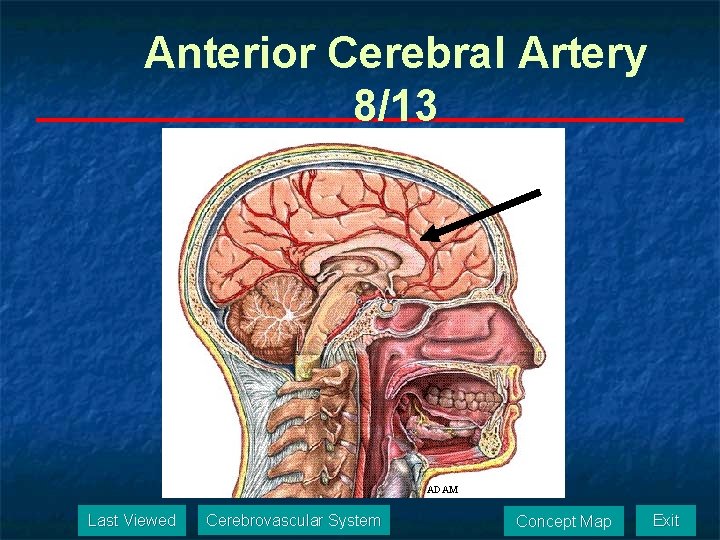
Anterior Cerebral Artery 8/13 ADAM Last Viewed Cerebrovascular System Concept Map Exit
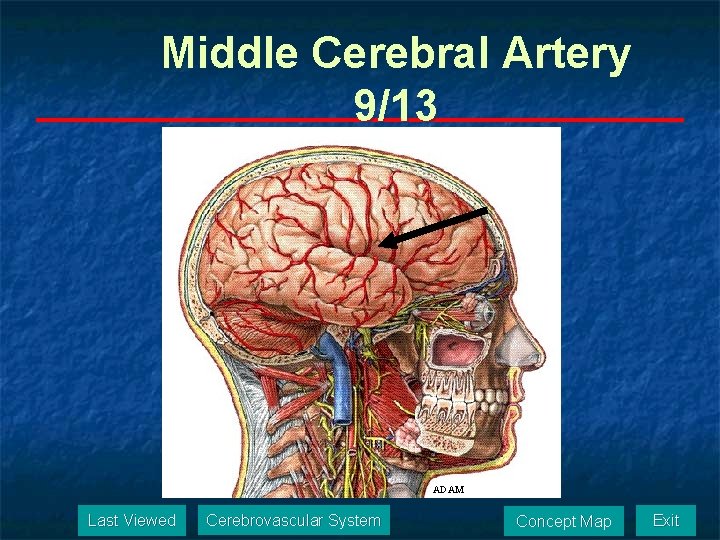
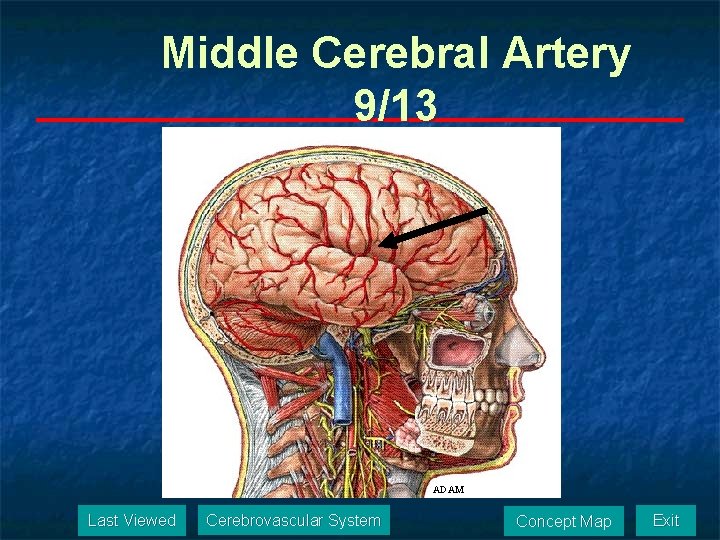
Middle Cerebral Artery 9/13 ADAM Last Viewed Cerebrovascular System Concept Map Exit
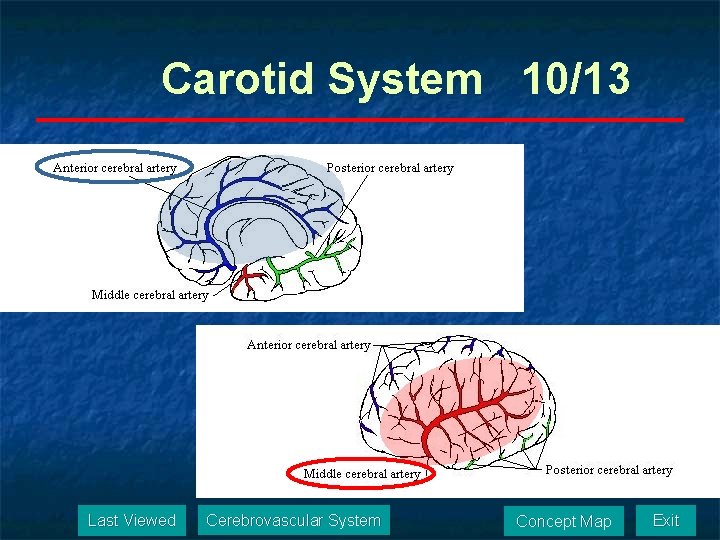
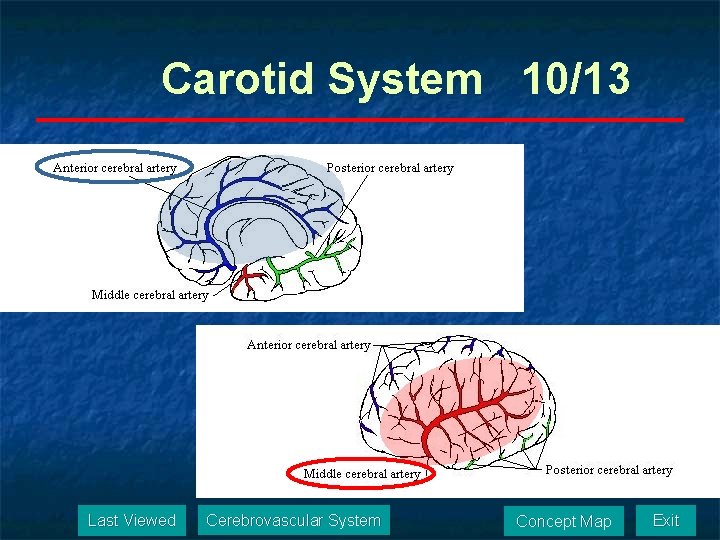
Carotid System 10/13 Last Viewed Cerebrovascular System Concept Map Exit
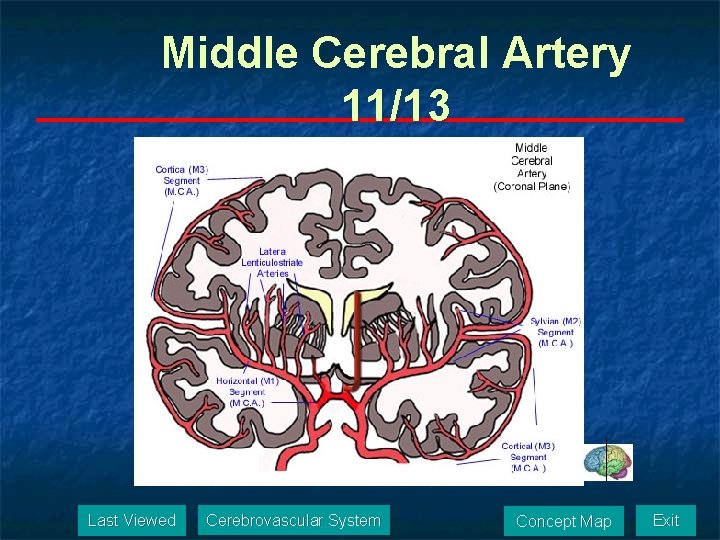
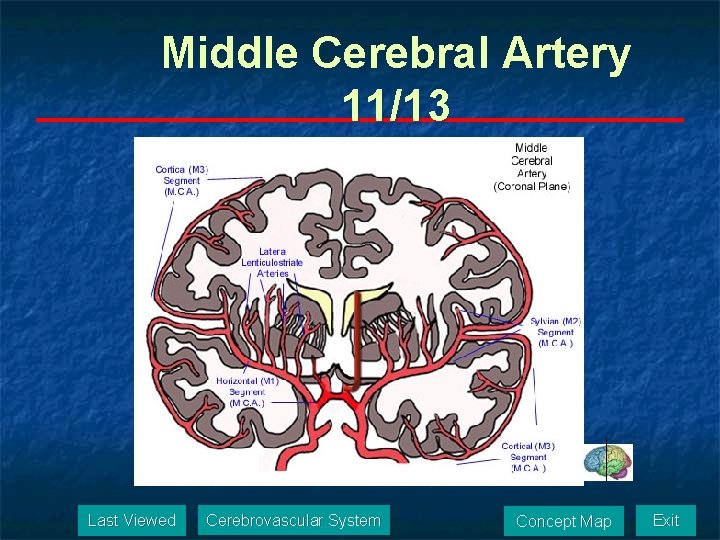
Middle Cerebral Artery 11/13 Last Viewed Cerebrovascular System Concept Map Exit
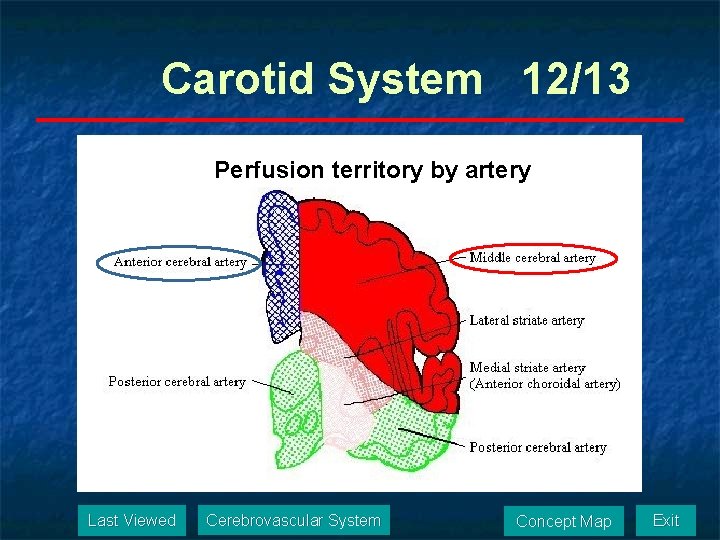
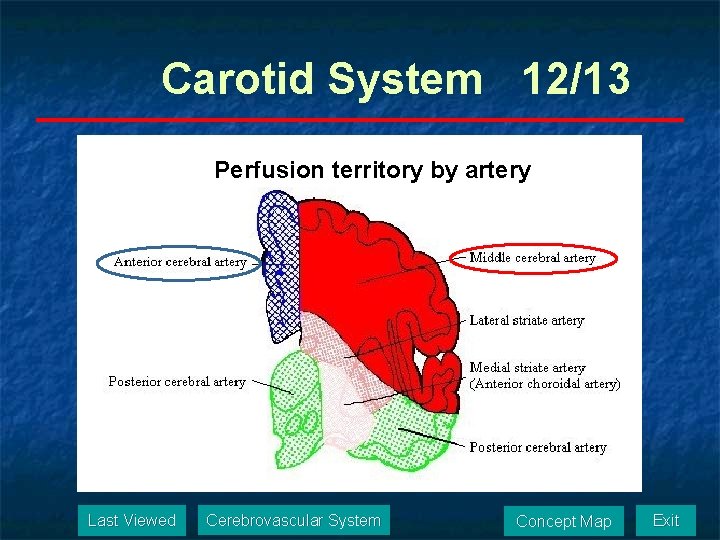
Carotid System 12/13 Perfusion territory by artery Last Viewed Cerebrovascular System Concept Map Exit
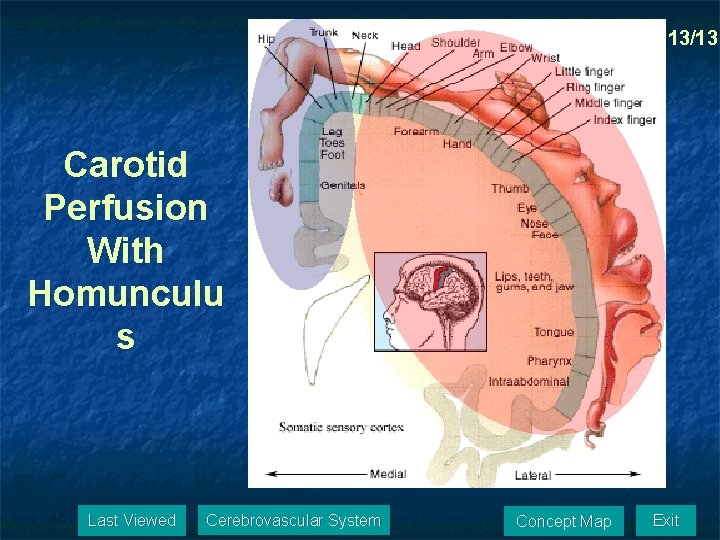
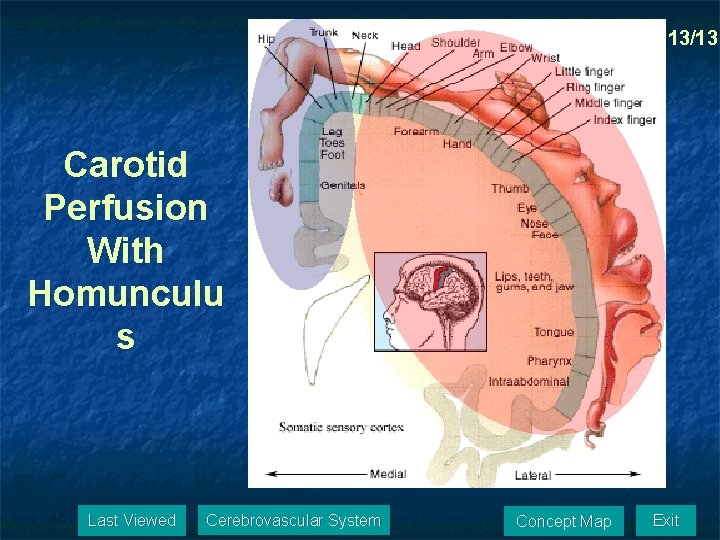
13/13 Carotid Perfusion With Homunculu s Last Viewed Cerebrovascular System Concept Map Exit
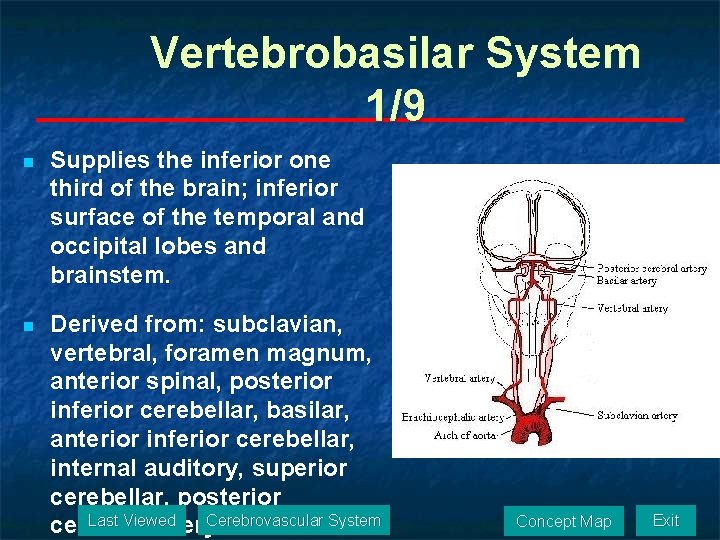
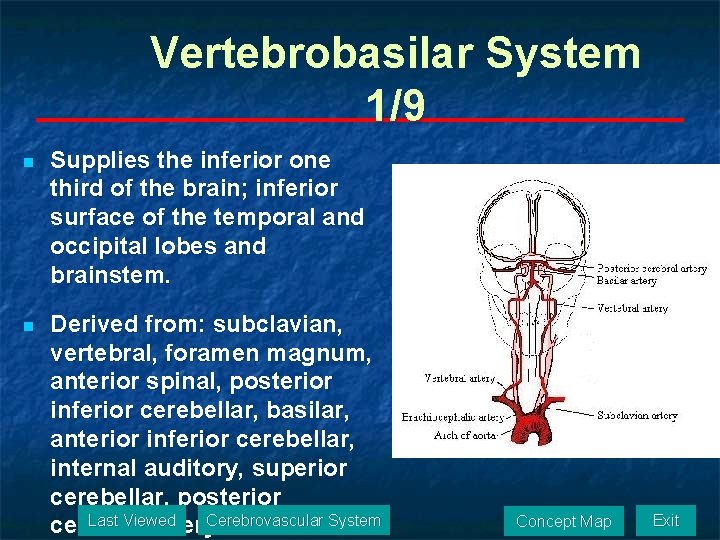
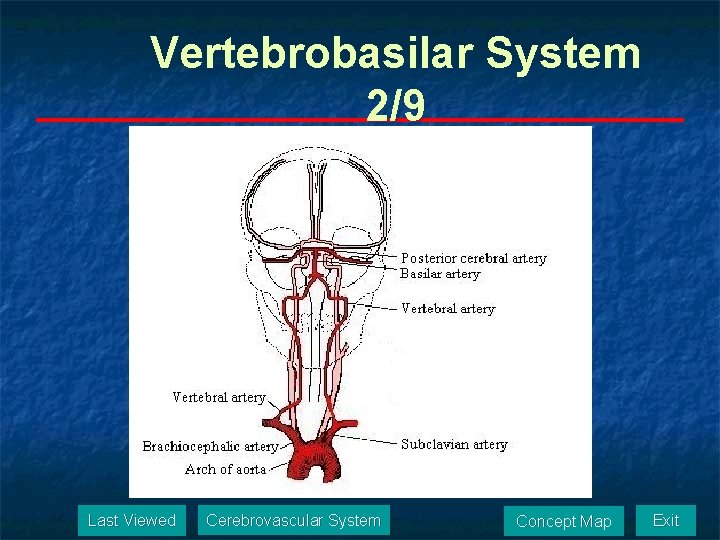
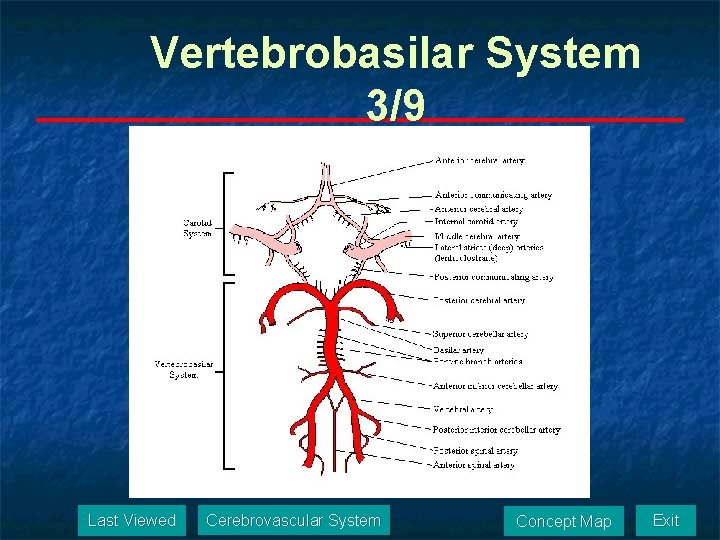
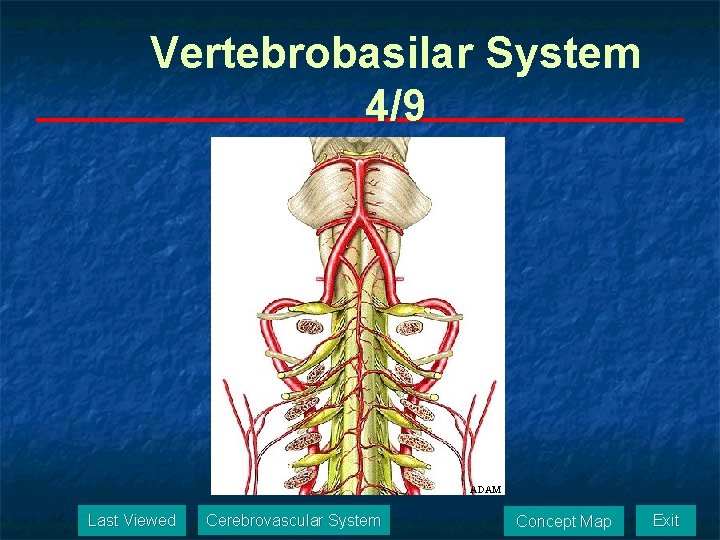
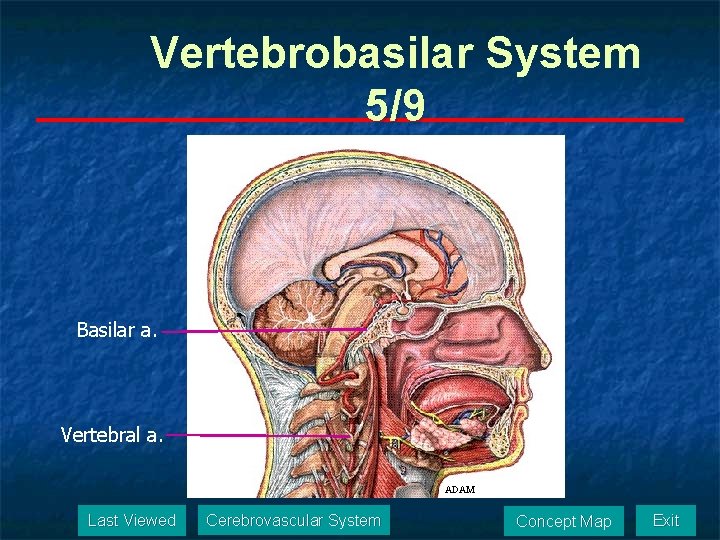
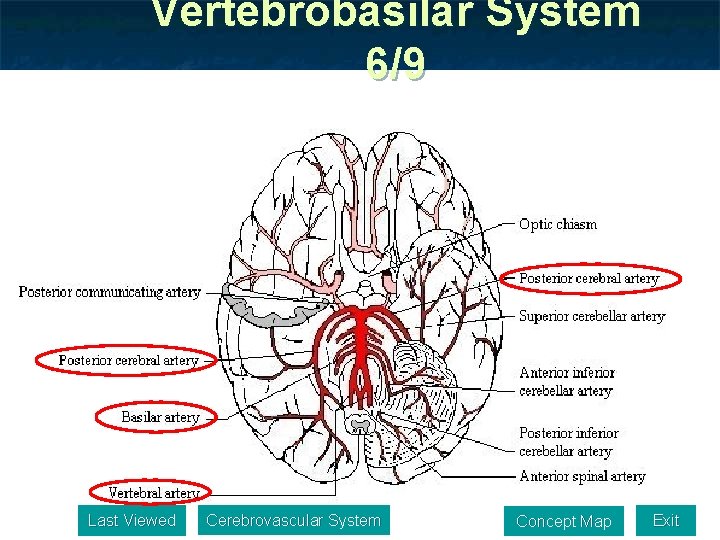
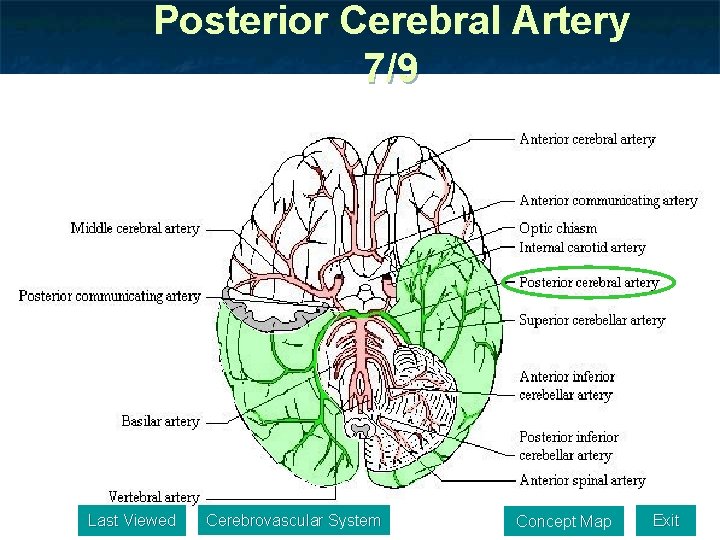
Vertebrobasilar System 1/9 n Supplies the inferior one third of the brain; inferior surface of the temporal and occipital lobes and brainstem. n Derived from: subclavian, vertebral, foramen magnum, anterior spinal, posterior inferior cerebellar, basilar, anterior inferior cerebellar, internal auditory, superior cerebellar, posterior Last Viewed cerebral artery. Cerebrovascular System Concept Map Exit
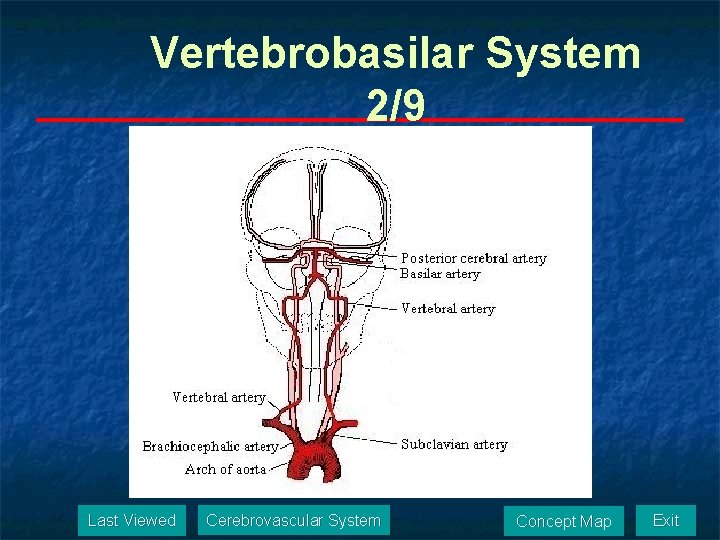
Vertebrobasilar System 2/9 Last Viewed Cerebrovascular System Concept Map Exit
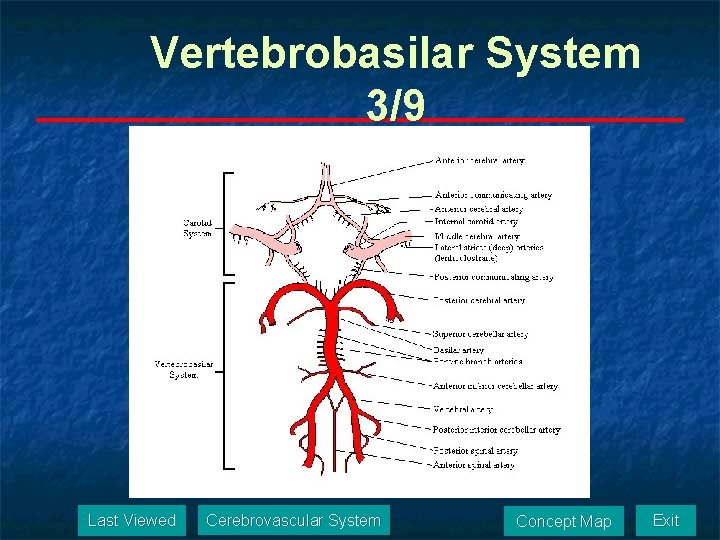
Vertebrobasilar System 3/9 Last Viewed Cerebrovascular System Concept Map Exit
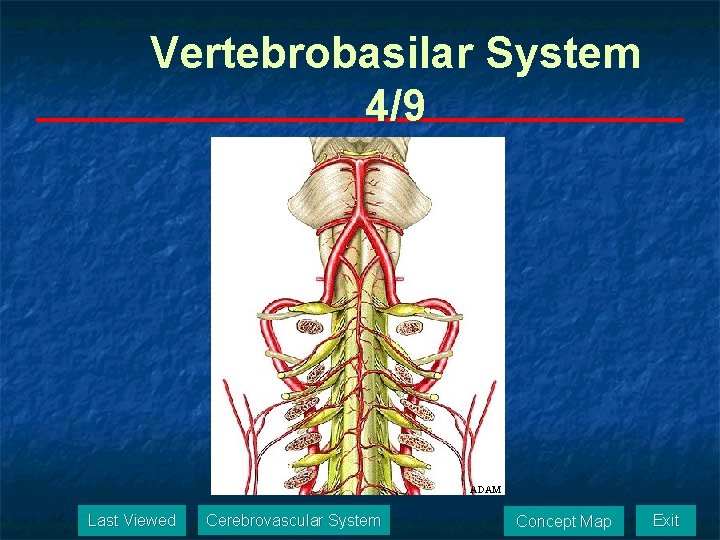
Vertebrobasilar System 4/9 ADAM Last Viewed Cerebrovascular System Concept Map Exit
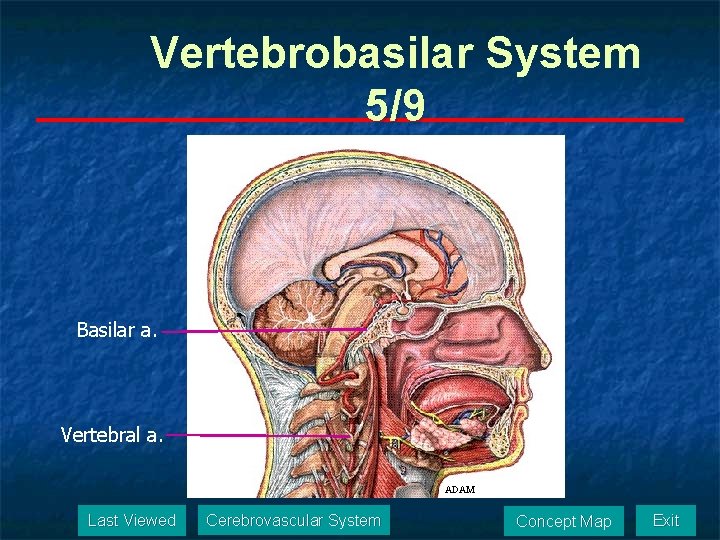
Vertebrobasilar System 5/9 Basilar a. Vertebral a. ADAM Last Viewed Cerebrovascular System Concept Map Exit
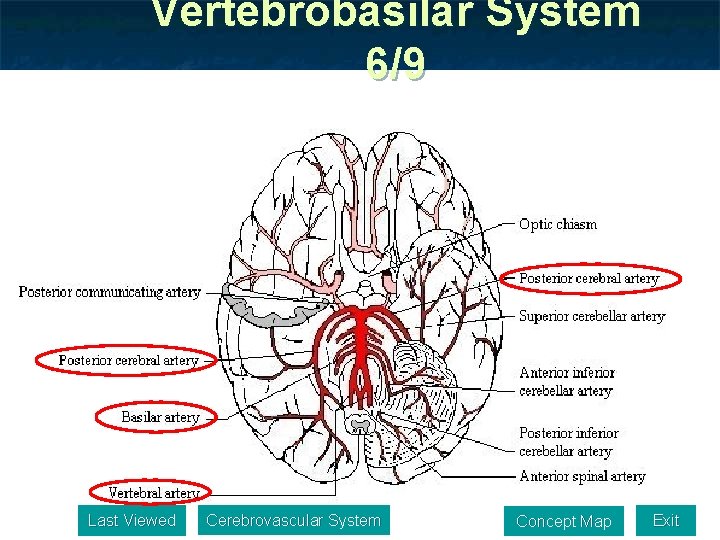
Vertebrobasilar System 6/9 Last Viewed Cerebrovascular System Concept Map Exit
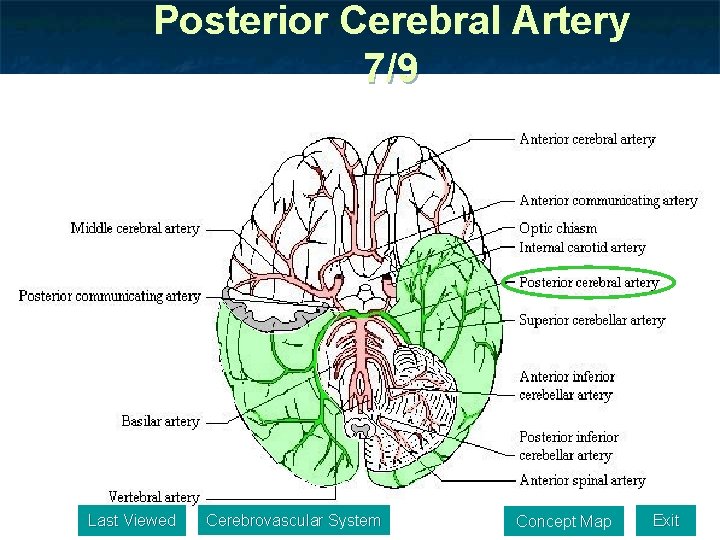
Posterior Cerebral Artery 7/9 Last Viewed Cerebrovascular System Concept Map Exit
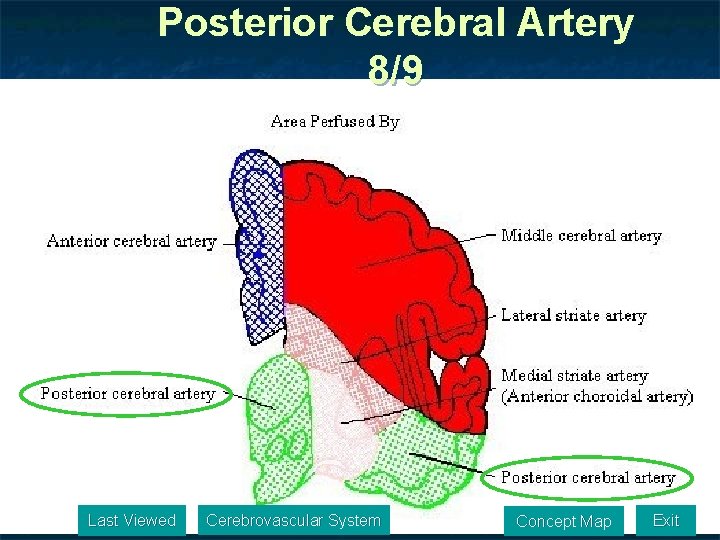
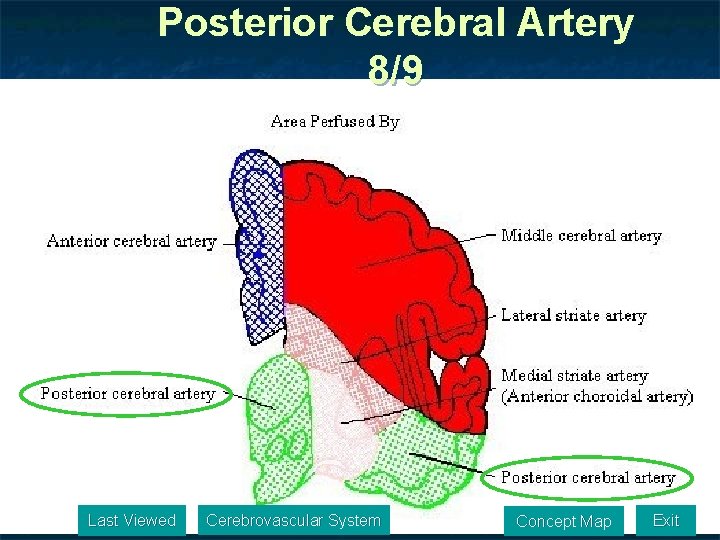
Posterior Cerebral Artery 8/9 Last Viewed Cerebrovascular System Concept Map Exit
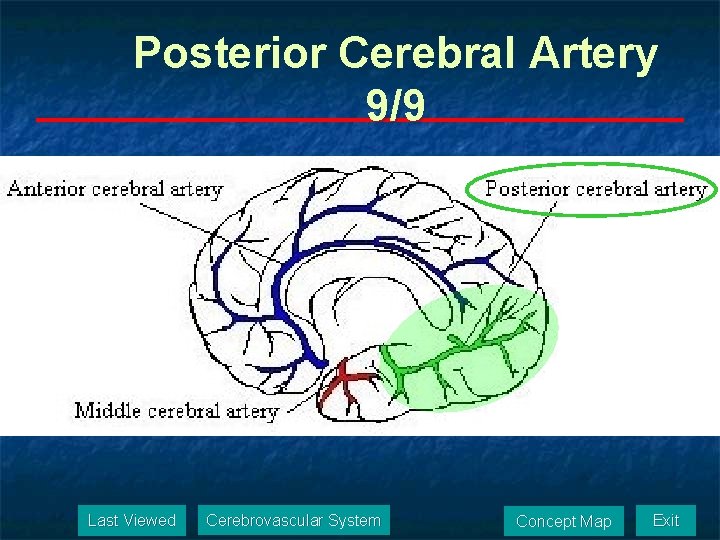
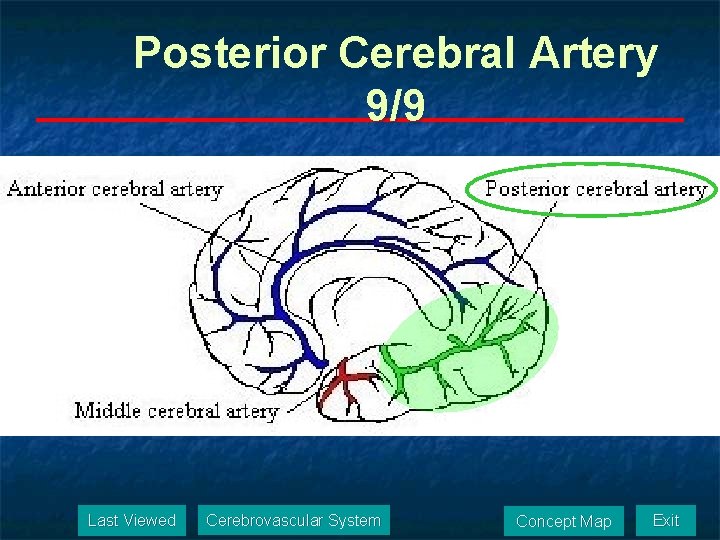
Posterior Cerebral Artery 9/9 Last Viewed Cerebrovascular System Concept Map Exit
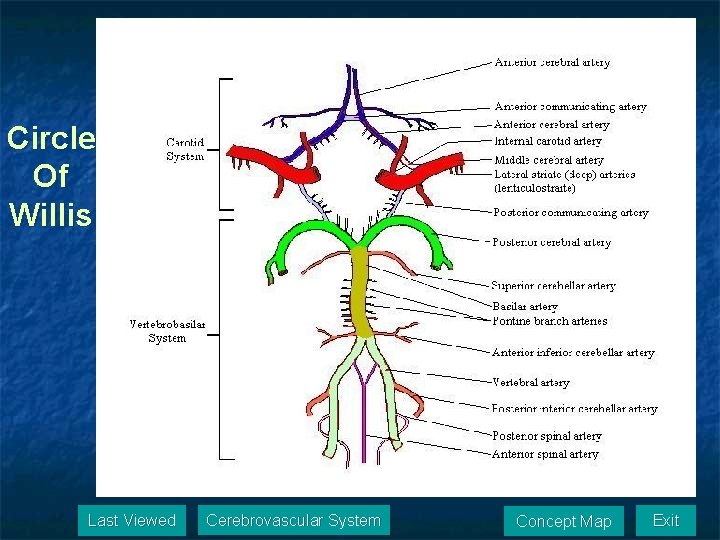
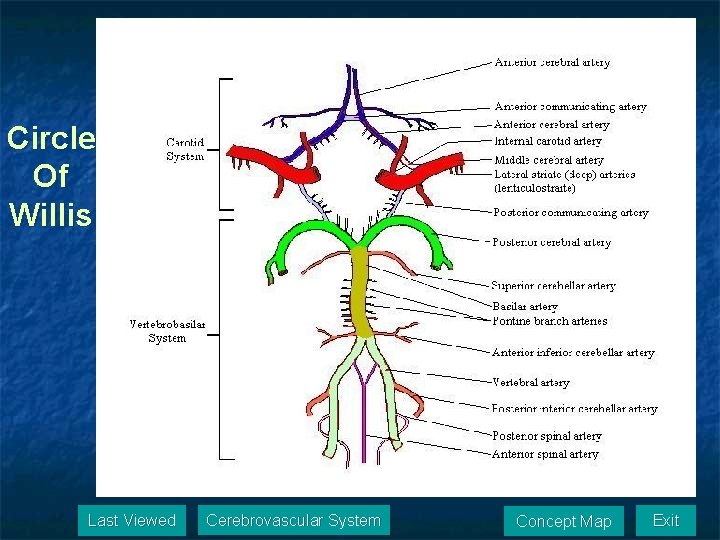
Circle Of Willis Last Viewed Cerebrovascular System Concept Map Exit
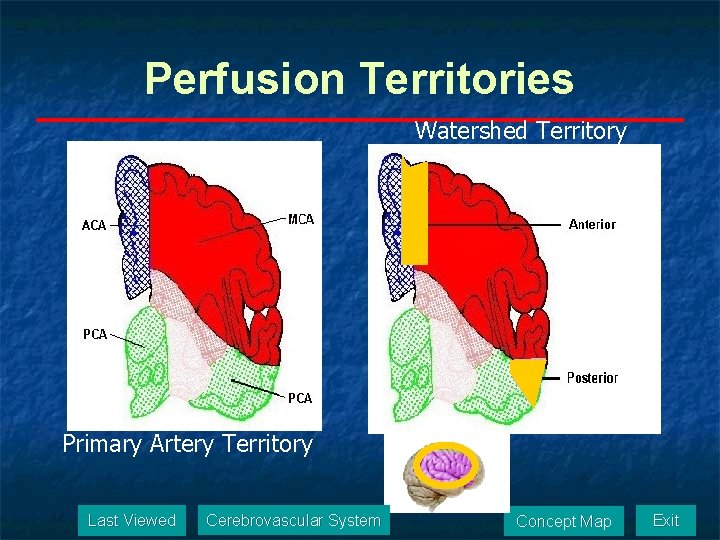
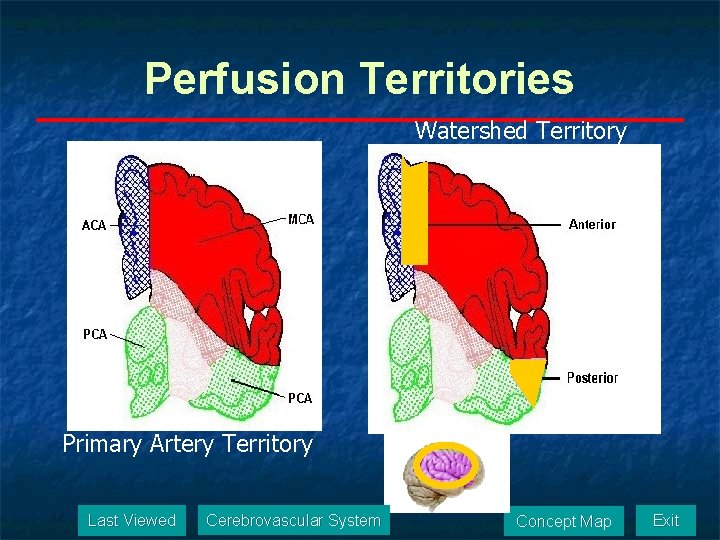
Perfusion Territories Watershed Territory Primary Artery Territory Last Viewed Cerebrovascular System Concept Map Exit
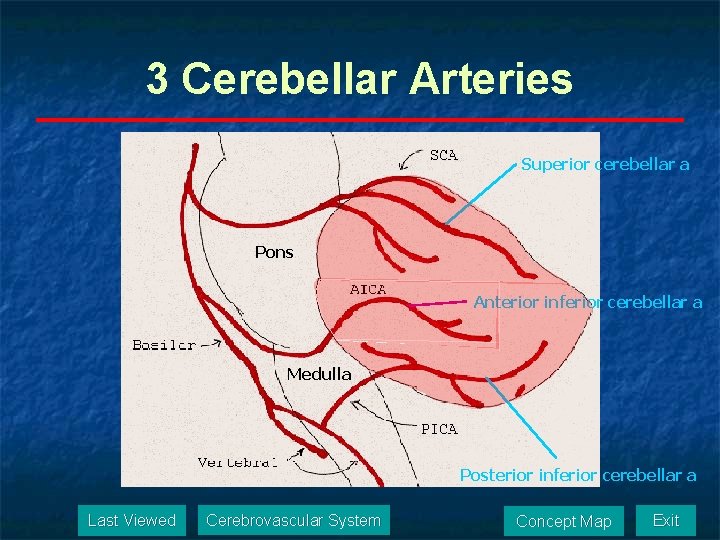
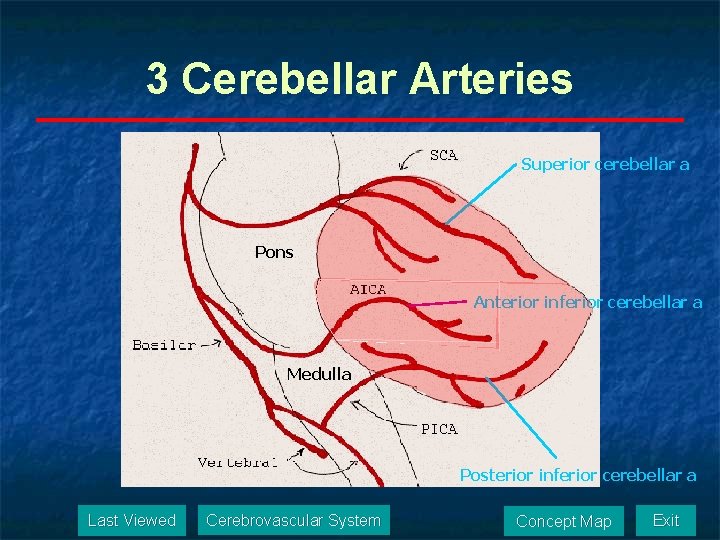
3 Cerebellar Arteries Superior cerebellar a Pons Anterior inferior cerebellar a Medulla Posterior inferior cerebellar a Last Viewed Cerebrovascular System Concept Map Exit
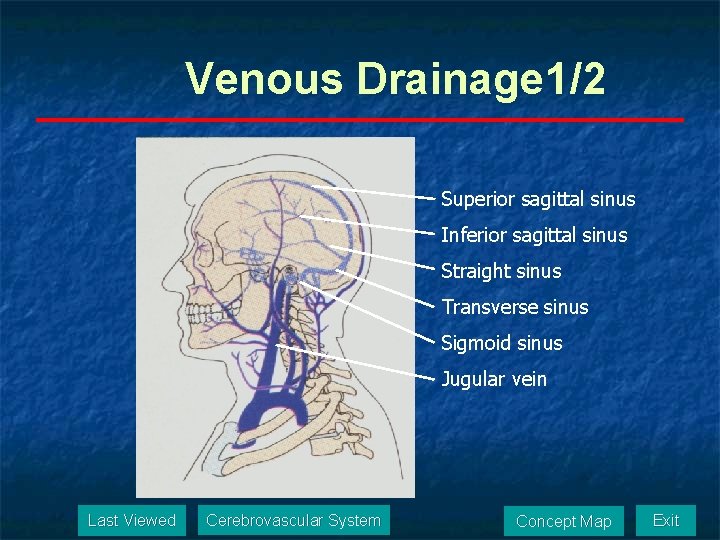
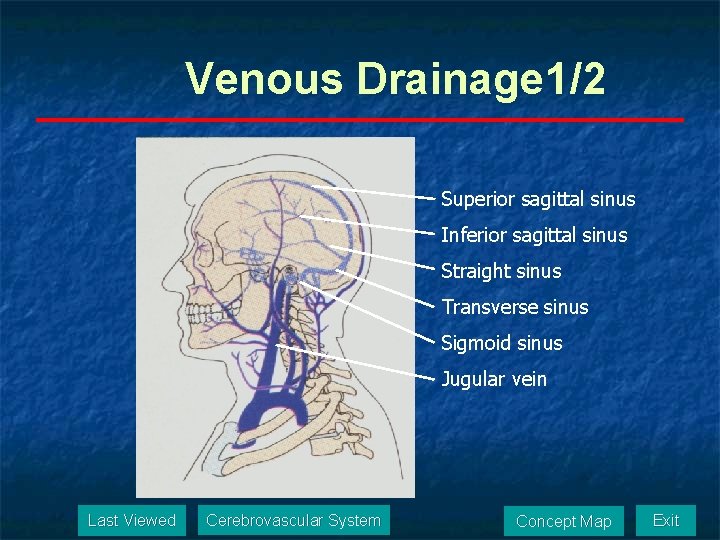
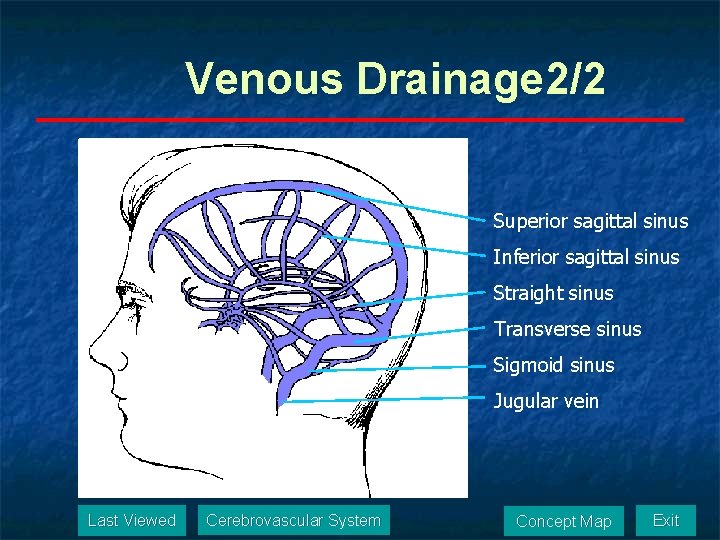
Venous Drainage 1/2 Superior sagittal sinus Inferior sagittal sinus Straight sinus Transverse sinus Sigmoid sinus Jugular vein Last Viewed Cerebrovascular System Concept Map Exit
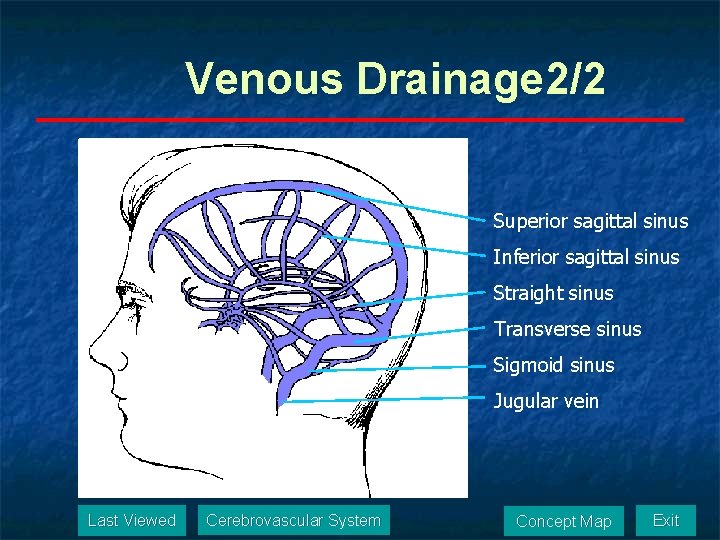
Venous Drainage 2/2 Superior sagittal sinus Inferior sagittal sinus Straight sinus Transverse sinus Sigmoid sinus Jugular vein Last Viewed Cerebrovascular System Concept Map Exit
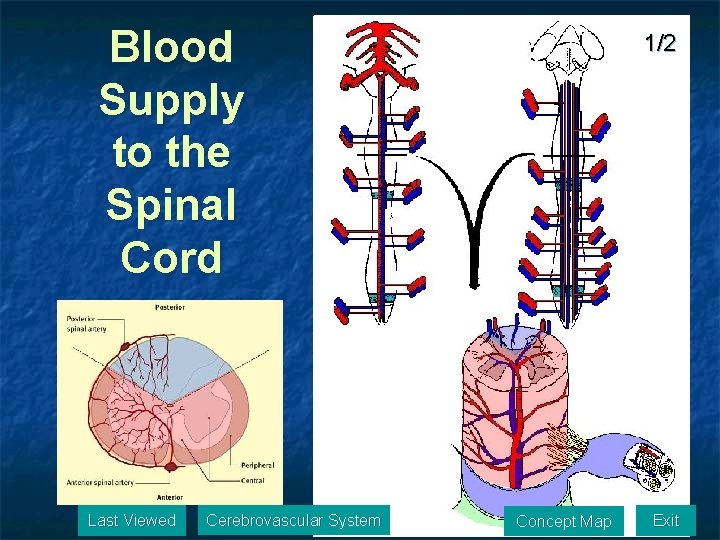
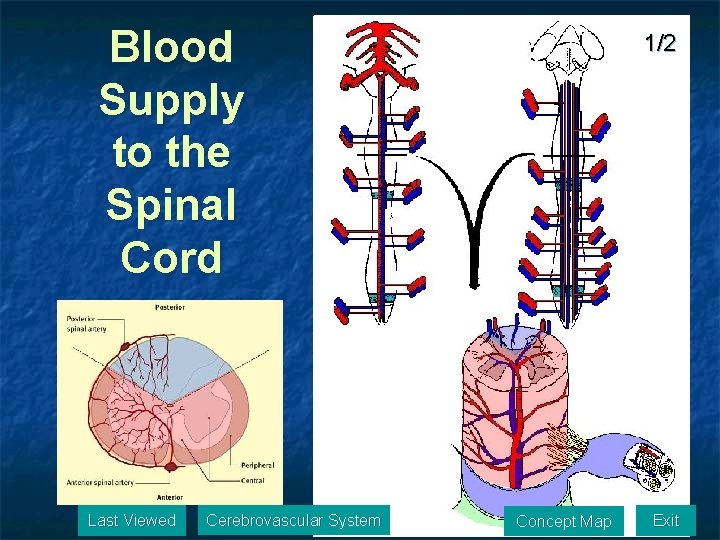
Blood Supply to the Spinal Cord Last Viewed Cerebrovascular System 1/2 Concept Map Exit
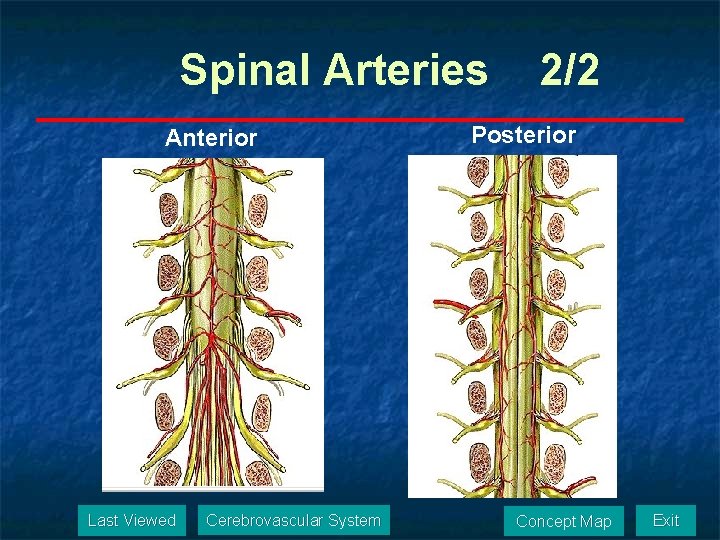
Spinal Arteries Anterior Last Viewed Cerebrovascular System 2/2 Posterior Concept Map Exit
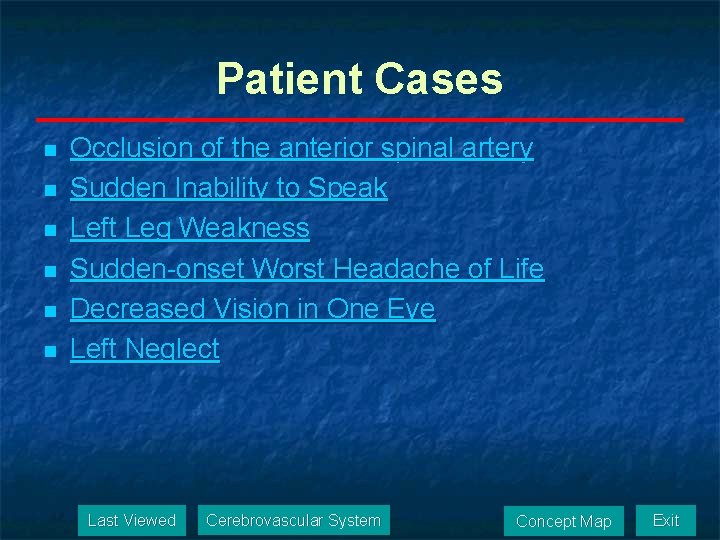
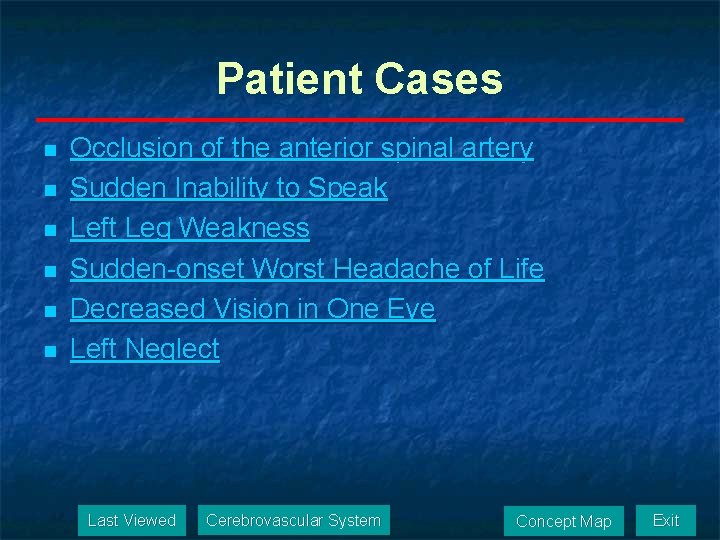
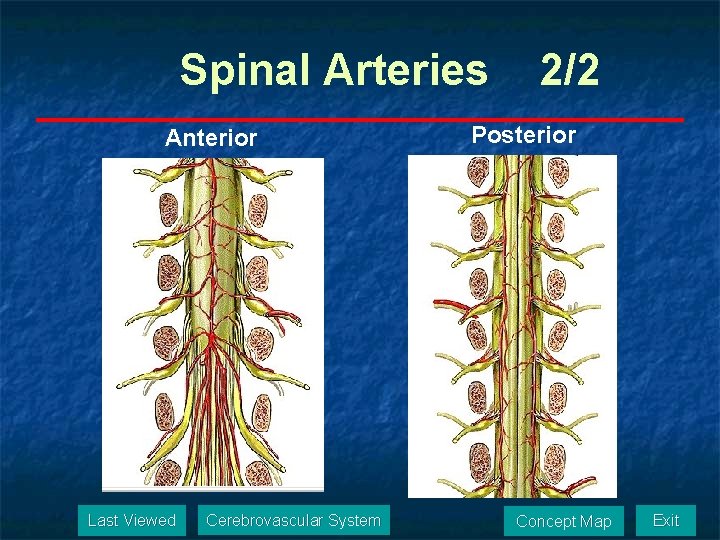
Patient Cases n n n Occlusion of the anterior spinal artery Sudden Inability to Speak Left Leg Weakness Sudden-onset Worst Headache of Life Decreased Vision in One Eye Left Neglect Last Viewed Cerebrovascular System Concept Map Exit
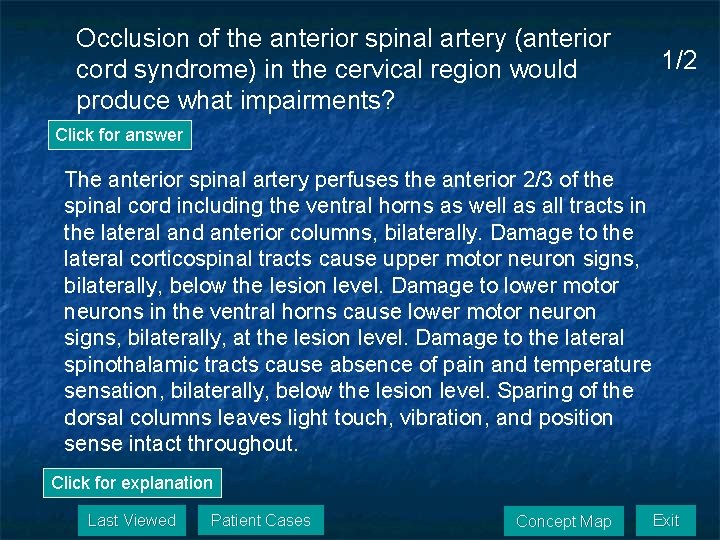
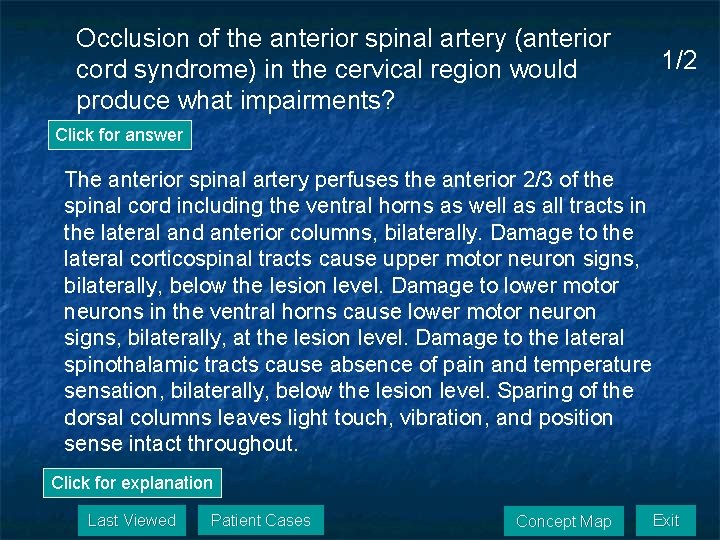
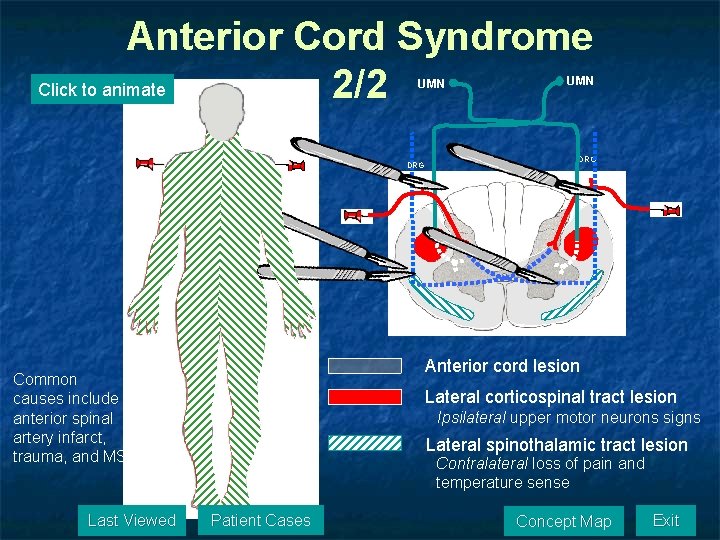
Occlusion of the anterior spinal artery (anterior cord syndrome) in the cervical region would produce what impairments? 1/2 Click for answer The anterior spinal artery perfuses the anterior 2/3 of the spinal cord including the ventral horns as well as all tracts in the lateral and anterior columns, bilaterally. Damage to the lateral corticospinal tracts cause upper motor neuron signs, bilaterally, below the lesion level. Damage to lower motor neurons in the ventral horns cause lower motor neuron signs, bilaterally, at the lesion level. Damage to the lateral spinothalamic tracts cause absence of pain and temperature sensation, bilaterally, below the lesion level. Sparing of the dorsal columns leaves light touch, vibration, and position sense intact throughout. Click for explanation Last Viewed Patient Cases Concept Map Exit
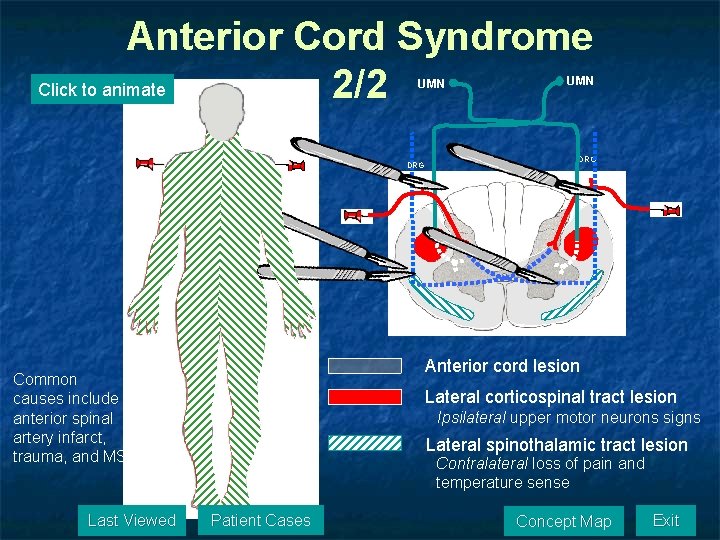
Anterior Cord Syndrome Click to animate 2/2 UMN DRG R Anterior cord lesion Common causes include anterior spinal artery infarct, trauma, and MS. Last Viewed L Lateral corticospinal tract lesion Ipsilateral upper motor neurons signs Lateral spinothalamic tract lesion Contralateral loss of pain and temperature sense Patient Cases Concept Map Exit
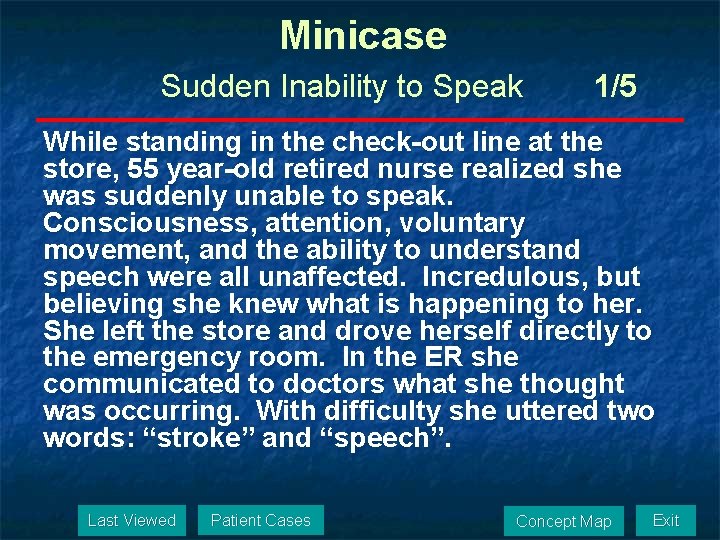
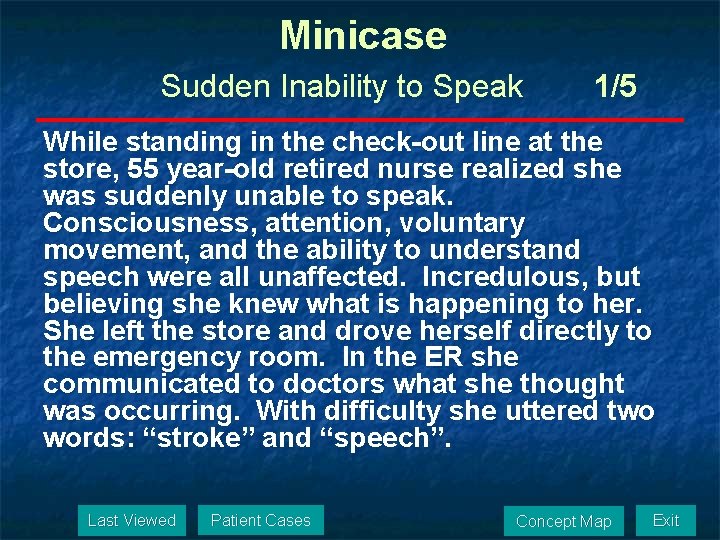
Minicase Sudden Inability to Speak 1/5 While standing in the check-out line at the store, 55 year-old retired nurse realized she was suddenly unable to speak. Consciousness, attention, voluntary movement, and the ability to understand speech were all unaffected. Incredulous, but believing she knew what is happening to her. She left the store and drove herself directly to the emergency room. In the ER she communicated to doctors what she thought was occurring. With difficulty she uttered two words: “stroke” and “speech”. Last Viewed Patient Cases Concept Map Exit
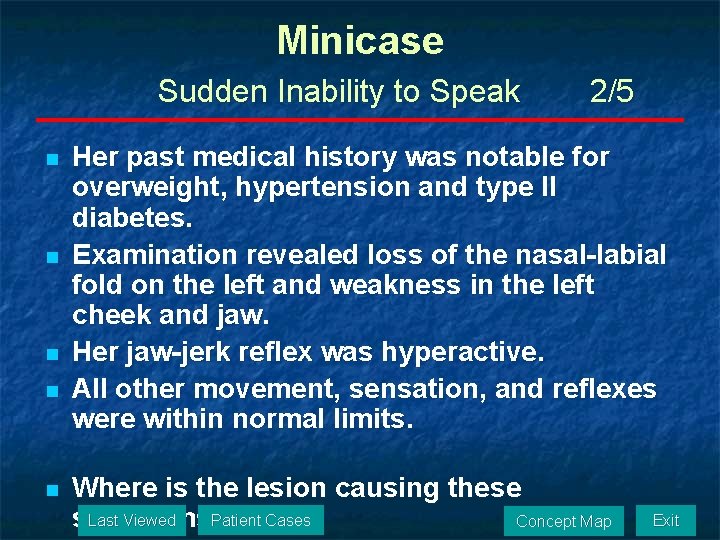
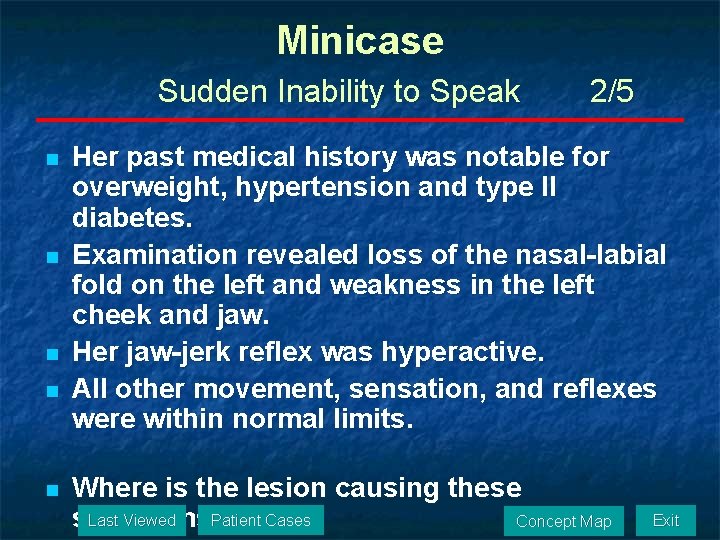
Minicase Sudden Inability to Speak n n n 2/5 Her past medical history was notable for overweight, hypertension and type II diabetes. Examination revealed loss of the nasal-labial fold on the left and weakness in the left cheek and jaw. Her jaw-jerk reflex was hyperactive. All other movement, sensation, and reflexes were within normal limits. Where is the lesion causing these Patient Cases Last Viewed Concept Map symptoms? Exit
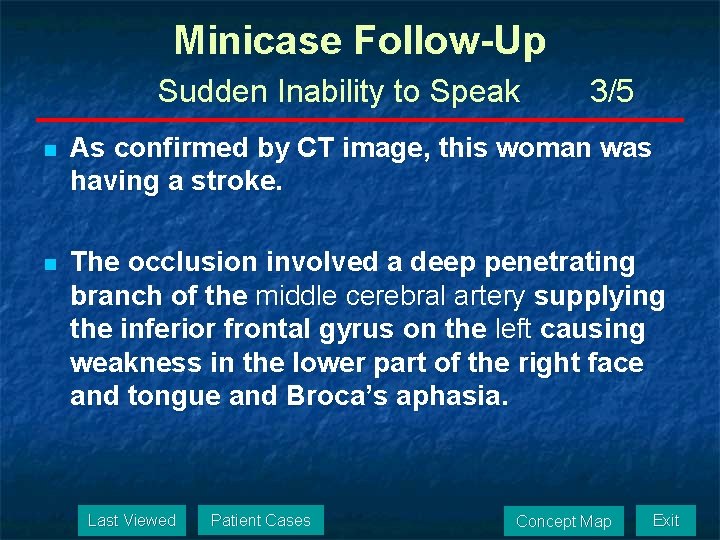
Minicase Follow-Up Sudden Inability to Speak 3/5 n As confirmed by CT image, this woman was having a stroke. n The occlusion involved a deep penetrating branch of the middle cerebral artery supplying the inferior frontal gyrus on the left causing weakness in the lower part of the right face and tongue and Broca’s aphasia. Last Viewed Patient Cases Concept Map Exit
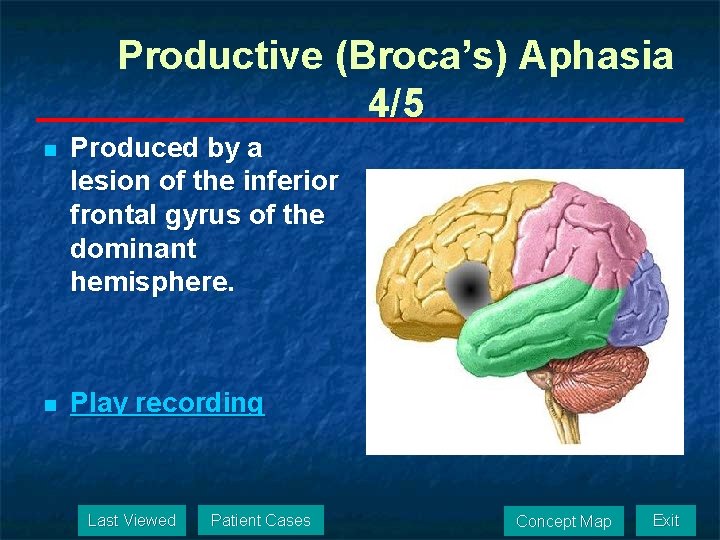
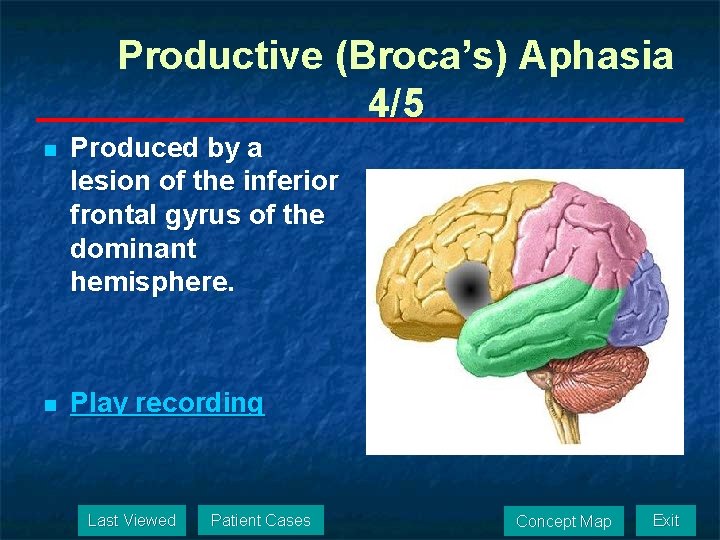
Productive (Broca’s) Aphasia 4/5 n Produced by a lesion of the inferior frontal gyrus of the dominant hemisphere. n Play recording Last Viewed Patient Cases Concept Map Exit
Minicase Follow-Up Sudden Inability to Speak 5/5 The key signs and symptoms in this case are: n Suddenly unable to speak n Consciousness, attention, voluntary movement, and the ability to understand speech were all unaffected n Loss of the nasal-labial fold on the left and weakness in the left cheek and jaw n Her jaw-jerk reflex was hyperactive Last Viewed Patient Cases Concept Map Exit
Minicase Left Leg Weakness 1/5 On attempting to stand after finishing breakfast, a 67 -year-old woman fell to the ground, hitting the table on the way down, because she was unable to support her body weight on her left leg. She called for help from her husband who was unable to get her off the floor and called for emergency assistance. Last Viewed Patient Cases Concept Map Exit
Minicase Left Leg Weakness 2/5 n n n Her past history was notable for obesity, hypertension, peripheral vascular disease, and smoking one pack per day for 52 years. She had hyperactive deep tendon reflexes in her left knee and ankle, and a positive Babinski sign in her left foot. The left leg was flaccid and she had no voluntary control of movement. She had mild impairment of light touch, pain, and temperature sensation in her left leg. Voluntary movement, reflexes, and sensation were intact in all other regions of the body. Where is the lesion causing these symptoms? Last Viewed Patient Cases Concept Map Exit
Minicase Follow-Up Left Leg Weakness 3/5 n n A head CT scan was done and the results suggested a probable right anterior cerebral artery infarct. Follow-up hear CT scan one month later confirmed the presence of a hypodense area on the anterior medial aspect of the right hemisphere consistent with a right anterior cerebral artery infarct Last Viewed Patient Cases Concept Map Exit

Minicase Follow-Up Left Leg Weakness 4/5 Last Viewed Patient Cases Concept Map Exit
Minicase Follow-Up Left Leg Weakness 5/5 The key signs and symptoms in this case are: n Unable to support her body weight on her left leg n Hyperactive deep tendon reflexes in her left knee and ankle, and a positive Babinski sign in her left foot n The left leg was flaccid and she had no voluntary control of movement n She had mild impairment of light touch, pain, and temperature sensation in her left leg n Voluntary movement, reflexes, and sensation were intact in all other regions of the body Last Viewed Patient Cases Concept Map Exit
Minicase Sudden-onset Worst Headache of Life 1/7 A 68 -year-old man suddenly developed “the worst of my life. ” On the morning of admission he was sitting watching TV when at 9: 00 am he suddenly developed an explosive headache worse than anything he had ever experienced. The headache began in the bifrontal area and over the next few minutes all over the head and down the neck. He denied loss of consciousness, nausea, vomiting or vision changes. Last Viewed Patient Cases Concept Map Exit
Minicase Sudden-onset Worst Headache of Life n n n 2/7 History was positive for severe diffuse atherosclerosis, including coronary disease and peripheral vascular disease requiring multiple bypass surgeries. He was obese and smoked two packs a day for 43 years. Examination was unremarkable except for mild nuchal rigidity. Last Viewed Patient Cases Concept Map Exit
Minicase Follow-Up Sudden-onset Worst Headache of Life n 3/7 Nuchal rigidity is often a sign of meningeal irritation caused by inflammation, infection, or hemorrhage in the subarachnoid space. Last Viewed Patient Cases Concept Map Exit
Minicase Follow-Up Sudden-onset Worst Headache of Life n n 4/7 The man underwent emergency head CT which demonstrated regions of hyperdensity in the subarachnoid space consistent with subarachnoid hemorrhage layering in the medial longitudinal fissure, lateral fissure, and around the brainstem. Next he was taken for an angiogram which clearly revealed an aneurysm arising from the region of the anterior communicating artery. Last Viewed Patient Cases Concept Map Exit
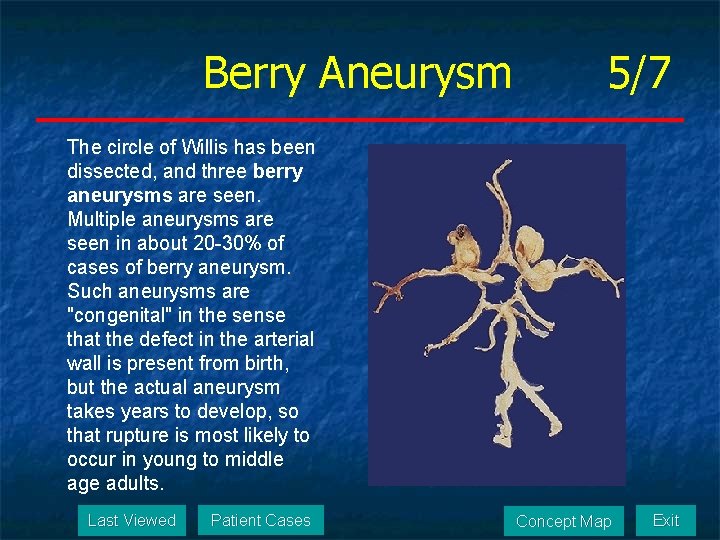
Berry Aneurysm 5/7 The circle of Willis has been dissected, and three berry aneurysms are seen. Multiple aneurysms are seen in about 20 -30% of cases of berry aneurysm. Such aneurysms are "congenital" in the sense that the defect in the arterial wall is present from birth, but the actual aneurysm takes years to develop, so that rupture is most likely to occur in young to middle age adults. Last Viewed Patient Cases Concept Map Exit
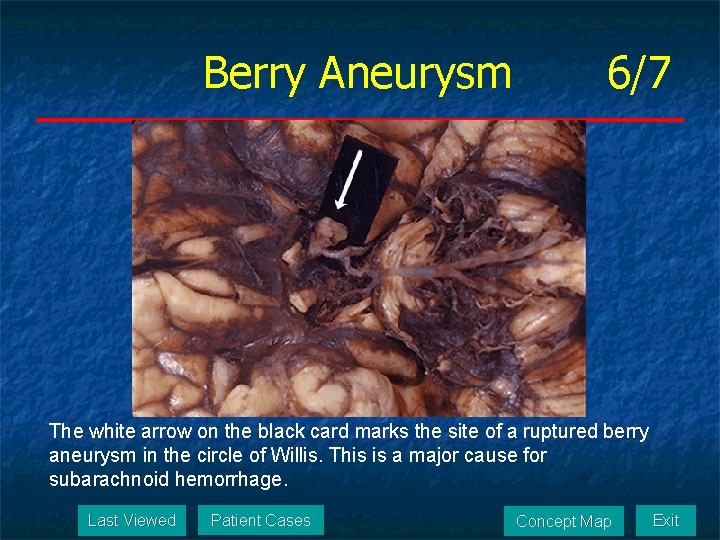
Berry Aneurysm 6/7 The white arrow on the black card marks the site of a ruptured berry aneurysm in the circle of Willis. This is a major cause for subarachnoid hemorrhage. Last Viewed Patient Cases Concept Map Exit
Minicase Follow-Up Sudden-onset Worst Headache of Life 7/7 The key signs and symptoms in this case are: n Suddenly developed “the worst of my life” n Headache began in the bifrontal area and over the next few minutes was all over the head and down the neck n Examination was unremarkable except for mild nuchal rigidity Last Viewed Patient Cases Concept Map Exit
Minicase Decreased Vision in One Eye 1/8 n A 63 -year-old woman went to an ophthalmologist complaining of episodes of decreased vision in her “right eye” over the past several weeks. Last Viewed Patient Cases Concept Map Exit
Minicase Decreased Vision in One Eye 2/8 n n n Her medical history was notable for type II diabetes, hypercholesterolemia, and coronary artery disease. About 5 -6 weeks ago the patient began having “episodes of sudden blurry wavy” appearance of her vision. She believed this was mostly in the right eye but never tried looking with only one eye at a time. Last Viewed Patient Cases Concept Map Exit
Minicase Decreased Vision in One Eye 3/8 n n n Episodes would last for 15 -20 minutes, resolved with no visual impairment, repeated 3 -4 times per week, and were never accompanied by pain. Previously she was able to recognize faces during the episodes but was unable to read. The current episode, that began two days ago, has resulted in persistent decreased vision on the right. Last Viewed Patient Cases Concept Map Exit
Minicase Decreased Vision in One Eye 4/8 n Neurologic examination revealed fluent speech. Pupils 3 mm, constricting to 2 mm bilaterally. Normal fundi. Visual acuity 20/30 right and 20/25 left. Visual field testing revealed a right homonymous hemianopia. Extraocular movements intact. Facial sensation intact to light touch and pinprick. Face symmetrical. Normal palate elevation. Normal shoulder shrug. Tongue midline. n Where is the lesion causing these symptoms? n n n n Last Viewed Patient Cases Concept Map Exit
Minicase Follow-Up Decreased Vision in One Eye 5/8 n n n The transient episodes of 15 -20 minutes of decreased right-sided vision occurring over several weeks, followed by a sudden-onset persistent deficit is suggestive of TIAs preceding a cerebral infarct. A right homonymous hemianopia can be caused by a lesion in the left hemisphere visual pathway anywhere from the left optic tract to the primary visual cortex. The patient’s age and past medical history raise the suspicion of cerebrovascular disease of the cause. Last Viewed Patient Cases Concept Map Exit
Minicase Follow-Up Decreased Vision in One Eye 6/8 n n The patient was sent to the hospital where an initial CT scan suggested a left posterior cerebral artery infarct, and a follow-up MRI confirmed the presence of a left PCS infarct involving the left primary visual cortex. An magnetic resonance angiogram (MRA) revealed several stenoses of the cerebral vessels compatible with diffuse intracranial atherosclerotic disease. She was treated with long-term oral anticoagulation. Her right hemianopia did not improve, but over time she learned to adapt to her visual deficit. Last Viewed Patient Cases Concept Map Exit
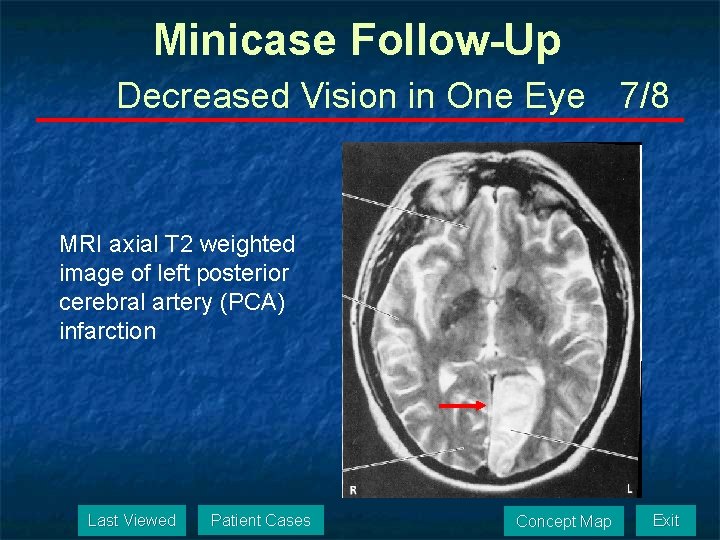
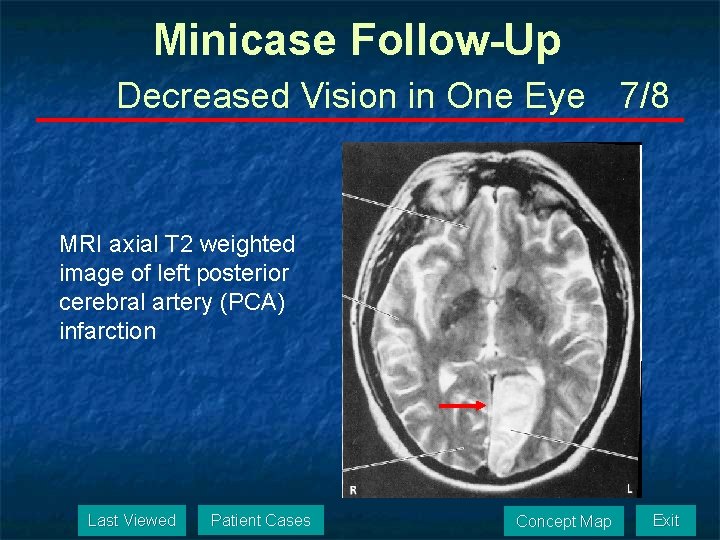
Minicase Follow-Up Decreased Vision in One Eye 7/8 MRI axial T 2 weighted image of left posterior cerebral artery (PCA) infarction Last Viewed Patient Cases Concept Map Exit
Minicase Follow-Up Decreased Vision in One Eye 8/8 The key signs and symptoms in this case are: n Episodes of sudden “blurry/ wavy” appearance of her vision in her “right eye” over the past several weeks n Right homonymous hemianopia Last Viewed Patient Cases Concept Map Exit
Minicase Left Neglect 1/5 n A 61 -year-old right-handed man was witnessed slumping to the floor in the grocery store. Last Viewed Patient Cases Concept Map Exit
Minicase Left Neglect 2/5 n n n On examination in the hospital he denied anything was wrong but said, “They called an ambulance because they said I had a stroke. ” He was unaware of having any impairment and wanted to go home. He had profound left visual field neglect , no blink to threat on the left, and no voluntary gaze to the left past midline. When trying to right, he moved the pen in the air off to the right of the page. When shown his left hand asked what it was, he replied “Someone’s hand. ” Last Viewed Patient Cases Concept Map Exit
Minicase Left Neglect 3/5 n n n When asked who’s hand it was he replied, “The doctor’s. ” He had a marked right gaze preference. He had marked weakness in the lower portion of the left face. Strength was 0/5 in the left arm and leg, the left plantar response was upgoing, and there was no response to pinprick on the left side. What lesion is causing this man’s symptoms? Last Viewed Patient Cases Concept Map Exit
Minicase Follow-Up Left Neglect 4/5 n n The patient exhibits several forms of neglect. In addition to anosognosia, he has left sensory neglect, to visual and tactile stimuli, as well as left motor neglect. These signs and symptoms are most commonly seen in patients with nondominant (usually right) parietal lobe lesions. Given the sudden onset of the deficits, involvement of the left arm and leg, the presence of sensory and motor deficits, and the patient’s age, the most likely cause is ischemic infarction of the right internal carotid artery. Last Viewed Patient Cases Concept Map Exit
Minicase Follow-Up Left Neglect 5/5 The key signs and symptoms in this case are: n Anosognosia n Left face, arm and leg plegia with positive Babinski’s sign n No blink to threat on the left n No voluntary gaze to the left past midline n No response to pinprick on the left Last Viewed Patient Cases Concept Map Exit
The End © DM Mc. Keough 2008 Last Viewed Patient Cases Concept Map
 Anterior stroke vs posterior stroke
Anterior stroke vs posterior stroke Criminology etiology
Criminology etiology Multicausal model of addiction
Multicausal model of addiction Pef in asthma
Pef in asthma Status asthmaticus pathophysiology
Status asthmaticus pathophysiology Subcecal appendix
Subcecal appendix Difference between nursing bottle caries and rampant caries
Difference between nursing bottle caries and rampant caries Sample pes statements
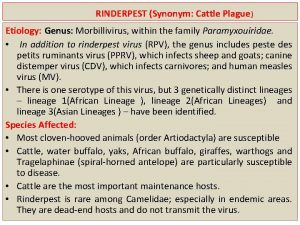
Sample pes statements Etiology
Etiology Etiology synonym
Etiology synonym Etiology
Etiology Classification of periradicular diseases
Classification of periradicular diseases Mild polyhydramnios range
Mild polyhydramnios range Lacunar infarct meaning
Lacunar infarct meaning Etiology synonym
Etiology synonym Conclusion of malaria
Conclusion of malaria Chitra pai
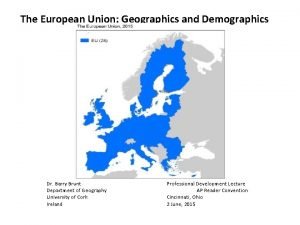
Chitra pai Demographics and the demand for higher education
Demographics and the demand for higher education Forever 21 swot analysis
Forever 21 swot analysis Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases Walmart shopper demographics
Walmart shopper demographics Uf demographics
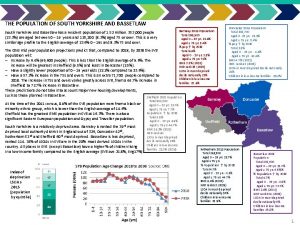
Uf demographics Yorkshire demographics
Yorkshire demographics Sfa demographics
Sfa demographics Orange county demographics
Orange county demographics Harvard demographics
Harvard demographics Sfa demographics
Sfa demographics Demographic cohort
Demographic cohort Nfl draft
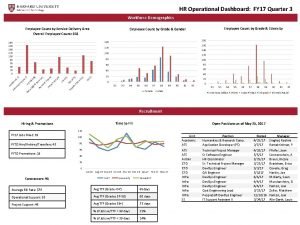
Nfl draft Hr demographics dashboard
Hr demographics dashboard Himachal pradesh map
Himachal pradesh map Bexley demographics
Bexley demographics Unlv demographics
Unlv demographics Lambert high school demographics
Lambert high school demographics Chinatown chicago demographics
Chinatown chicago demographics Demographics media studies
Demographics media studies Wine market council
Wine market council World of warcraft demographics
World of warcraft demographics South tyrol demographics
South tyrol demographics Favorable demographics
Favorable demographics Traffic director triage
Traffic director triage Demographics
Demographics Las vegas demographics
Las vegas demographics London demographics
London demographics Nascar
Nascar Ifta demographics
Ifta demographics Ut arlington va office
Ut arlington va office Lyons township high school demographics
Lyons township high school demographics Thomas barr cio
Thomas barr cio Nascar fan demographics
Nascar fan demographics Translingualism
Translingualism Automotive demographics
Automotive demographics Chipotle demographics
Chipotle demographics Heterogeneous hypoechoic lesion in liver
Heterogeneous hypoechoic lesion in liver Lateral spinothalamic tract
Lateral spinothalamic tract Tabes dorsalis
Tabes dorsalis Umnl and lmnl of facial nerve
Umnl and lmnl of facial nerve Pretectal area
Pretectal area Fractura de monteggia tratamiento fisioterapeutico
Fractura de monteggia tratamiento fisioterapeutico Lower
Lower Thalamus function
Thalamus function Lesions of vagus nerve
Lesions of vagus nerve Coarse echotexture
Coarse echotexture Optic tract lesions
Optic tract lesions Eduard baco
Eduard baco Signos duros y blandos de lesion vascular
Signos duros y blandos de lesion vascular Vascular
Vascular Patron colestasico
Patron colestasico Neocerebellum
Neocerebellum Subendocardio y subepicardio
Subendocardio y subepicardio Definicion de lesion celular
Definicion de lesion celular Verruga vulgar
Verruga vulgar 7th cranial nerve
7th cranial nerve Tejido vitalizado
Tejido vitalizado Infarto subendocardico y subepicardico
Infarto subendocardico y subepicardico Archi cerebellum
Archi cerebellum Endo perio lesion
Endo perio lesion Image en miroir ecg
Image en miroir ecg Do not touch lesions
Do not touch lesions Grado de lesion
Grado de lesion Lesion lamelar no penetrante
Lesion lamelar no penetrante Tafirol
Tafirol Hiato y diptongo reglas
Hiato y diptongo reglas Integridad tegumentaria
Integridad tegumentaria Quiste de menisco externo
Quiste de menisco externo Radiopaco radiolucido radiotransparente
Radiopaco radiolucido radiotransparente Nurografia
Nurografia Oftalmlogo
Oftalmlogo Lésion en verre dépoli
Lésion en verre dépoli Collar button ulcer
Collar button ulcer Lesion pacheco
Lesion pacheco Brain lesion
Brain lesion Granulomatous lesion
Granulomatous lesion Neuropatia periférica
Neuropatia periférica Dukes criteria
Dukes criteria Glumerolo
Glumerolo Edema lesion
Edema lesion Plet medium
Plet medium Parakeratin vs orthokeratin
Parakeratin vs orthokeratin Lesion
Lesion Atipicam
Atipicam Glossopharyngeal lesion
Glossopharyngeal lesion Breast lesion
Breast lesion Lesion longitudinal de menisco
Lesion longitudinal de menisco Tug lesion proximal tibia
Tug lesion proximal tibia Adnexal lesion
Adnexal lesion Sistema piramidal y extrapiramidal
Sistema piramidal y extrapiramidal Hpv us
Hpv us Hypervascular liver lesion
Hypervascular liver lesion Extradural lesion
Extradural lesion Lesion
Lesion Lésion
Lésion Diencepholon
Diencepholon Lésion
Lésion Lésion
Lésion Thalamus lesion
Thalamus lesion Lesion de primera y segunda motoneurona
Lesion de primera y segunda motoneurona Armanni ebstein lesion
Armanni ebstein lesion Apergaminamiento medicina legal
Apergaminamiento medicina legal Tipos de lesion celular irreversible
Tipos de lesion celular irreversible Lesion ap psychology
Lesion ap psychology Is emphysema additive or destructive
Is emphysema additive or destructive Introduction to cryptology
Introduction to cryptology Cryptology and pathology
Cryptology and pathology Chris concepts
Chris concepts Systemic pathology exam questions pdf
Systemic pathology exam questions pdf Introduction and importance of seed pathology
Introduction and importance of seed pathology Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Pathology of blood and urine ppt
Pathology of blood and urine ppt Fish and shellfish pathology
Fish and shellfish pathology Leeds pathology tests and tubes
Leeds pathology tests and tubes Stroke and turn clinic
Stroke and turn clinic Stab culture and stroke culture
Stab culture and stroke culture Explain stab culture and stroke culture
Explain stab culture and stroke culture Events of cardiac cycle class 11
Events of cardiac cycle class 11 Cardiac output and stroke volume
Cardiac output and stroke volume Cardiac output and stroke volume
Cardiac output and stroke volume Anaerobic culture method
Anaerobic culture method Lawn or carpet culture method
Lawn or carpet culture method Guidelines for adult stroke rehabilitation and recovery
Guidelines for adult stroke rehabilitation and recovery Cvds
Cvds Disadvantages picture
Disadvantages picture Branchless fruit laden tree appearance
Branchless fruit laden tree appearance Seed pathology definition
Seed pathology definition Banff pathology course
Banff pathology course Pathology job market
Pathology job market Pathology outline
Pathology outline Diagnostic report sample
Diagnostic report sample Wally langdon
Wally langdon Bronchial wall
Bronchial wall Pathology outline
Pathology outline Kidney pathology
Kidney pathology