PEPTIC ULCER DISEASE The lesion of peptic ulcer




- Slides: 37
PEPTIC ULCER DISEASE
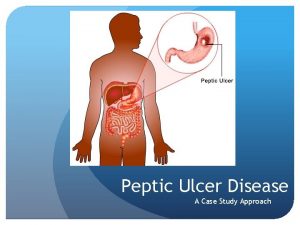
The lesion of peptic ulcer disease (PUD) is a disruption in the mucosal layer of the stomach or duodenum. An ulcer is distinguished from an erosion by its penetration through the muscularis mucosa or the muscular coating of the gastric or duodenal wall. Peptic ulcer disease results from the imbalance between defensive factors that protect the mucosa and offensive factors that disrupt this important barrier. Mucosal protective factors include the waterinsoluble mucous gel layer, local production of bicarbonate, regulation of gastric acid secretion, and adequate mucosal blood flow. Aggressive factors include the acid-pepsin environment, infection with Helicobacter pylori, and mucosal ischemia. Many differences are noted between children and adults with peptic ulcer disease, especially in clinical presentation, in the prevalence rates of different types of ulcer disease, and the prevalence rate of complications.
PATHOPHYSIOLOGY The 2 most important concepts in understanding the pathophysiology of peptic ulcer disease in children are the host factors that serve to protect the GI mucosa from ulceration and the inflammatory mediators and aggressive factors that contribute to mucosal inflammation and ulceration. Peptic ulcer disease in children is the result of an imbalance between mucosal defensive and aggressive factors. An overlying physiochemical barrier provides cytoprotection of the gastric mucosa. This barrier comprises water-insoluble gastric mucus, gastrically produced bicarbonate, an unstirred water layer, phospholipids, rapid shedding of cells resulting from epidermal growth factor, normal mucosal blood flow, prostaglandin-stimulated bicarbonate, mucus production, and inhibited acid secretion.
Contributors to mucosal inflammation and ulceration include endogenous factors, such as gastric acidity (approximates adult values by age 3 -4 y), acid-dependent pepsin and mucosal ischemia, and exogenous factors, such as drugs (eg, NSAIDs, aspirin, corticosteroids), alcohol, cigarette smoking, corrosive chemicals (eg, lye), and emotional stress. In patients with traumatic injuries, burns, sepsis, respiratory failure, or other critical systemic illnesses, many factors can contribute to erosions and ulcers, including mucosal ischemia, increased gastric acid and pepsin production, higher levels of endogenous catecholamines and steroids, and decreased prostaglandins and mucus production. Important mediators of mucosal inflammation and resultant ulceration include oxygen free radicals, lymphokines, platelets activating factors, tumor necrosis factor, leukotrienes, and monokines.

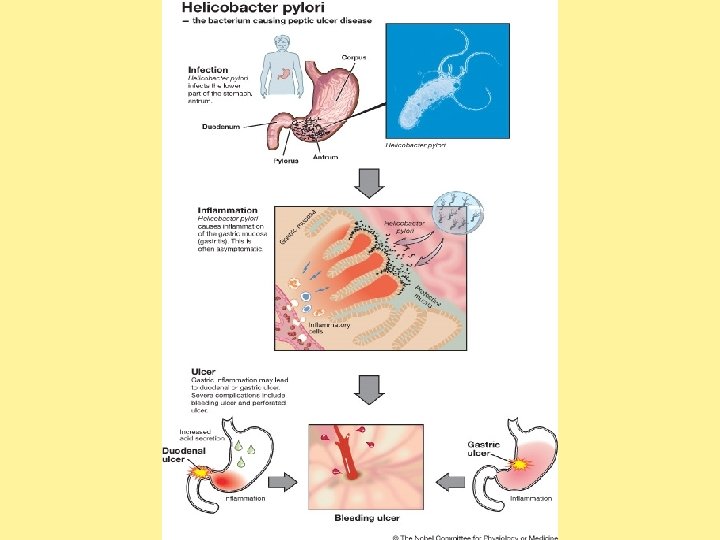
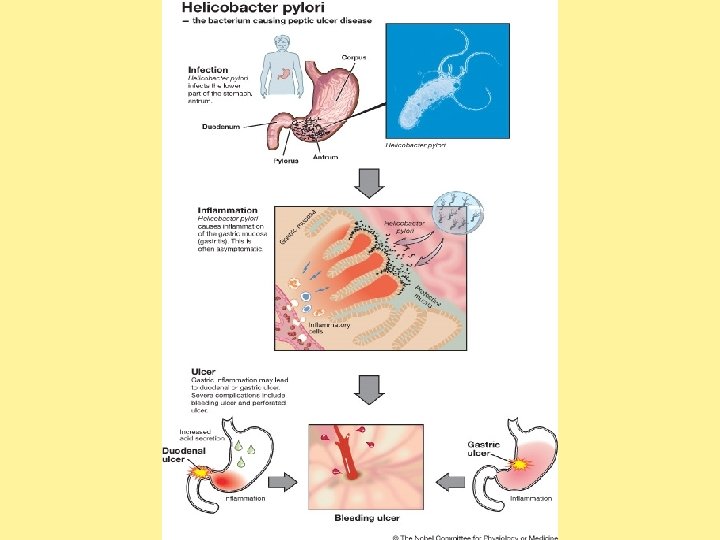
The gram-negative spirochete, H pylori, was first linked to gastritis in 1983. Since then, further study of H pylori has revealed that it is a major part of the triad, which includes acid and pepsin, that contributes to primary peptic ulcer disease. The unique microbiologic characteristics of this organism, such as urease production, allows it alkalinize its microenvironment and survive for years in the hostile acidic environment of the stomach, where it causes mucosal inflammation and, in some individuals, worsens the severity of peptic ulcer disease.
FREQUENCY Peptic ulcer disease has changed profoundly over the last few decades in Western countries in both children and adults. The proportion of H pylori –positive ulcers has declined, and the prevalence of H pylori –negative gastric ulcers and duodenal ulcers has grown. In a recent retrospective study from China, 6. 9% of children undergoing esophagogastroduodenoscopy had an ulcer; almost half of these cases (46. 5%) had no associated H pylori infection. 1 These data are different from that of other studies, in which only 20 -27% of childhood peptic ulcers were not associated with either NSAID use or H pylori infection. The prevalence of H pylori infection in developing countries is as high as 50 -100%. The prevalence of peptic ulcer disease is increasing in developing countries. In a retrospective review of 112 Taiwanese children undergoing upper GI endoscopy for upper GI bleeding,
CLINICAL HISTORY In children in whom peptic ulcer disease (PUD) is suspected, include the following in the history: Review of past illnesses and chronic medical conditions Family history of ulcer disease, including known H pylori infection, or conditions affecting the GI tract (eg, Crohn disease) Character, location, frequency, duration, severity, and exacerbating (especially meals in children) and alleviating factors of abdominal pain Vomiting and description of gastric material Bowel habits and description of stool (eg, profuse diarrhea seen in Zollinger-Ellison syndrome [ZES]) Prescribed and over-the-counter (OTC) medications, especially nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids Prior diagnostic testing and specific GI therapies Appetite, diet, and weight changes Family and social stressors Alcohol ingestion and smoking habits
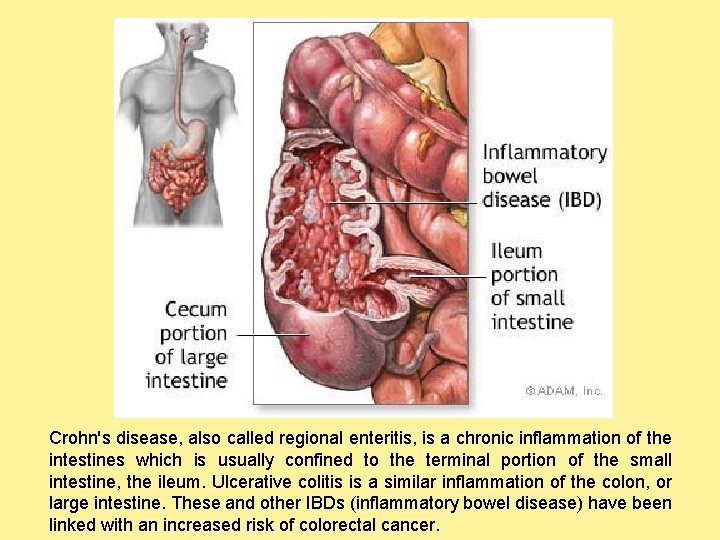
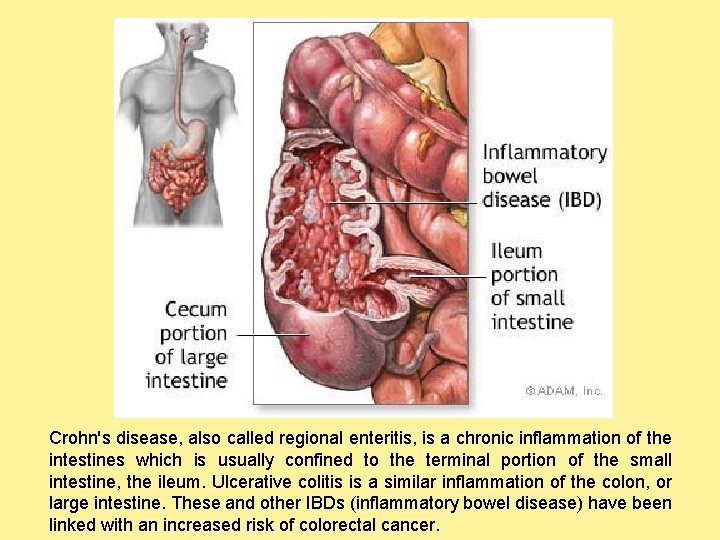
Crohn's disease, also called regional enteritis, is a chronic inflammation of the intestines which is usually confined to the terminal portion of the small intestine, the ileum. Ulcerative colitis is a similar inflammation of the colon, or large intestine. These and other IBDs (inflammatory bowel disease) have been linked with an increased risk of colorectal cancer.
Abdominal pain is the most common symptom of childhood peptic ulcer disease. The pain is usually dull and vague. The pain is most likely to be dull and aching rather than sharp and burning, as adults describe. Food intake often causes the pain to worsen; this is the opposite of the adult pattern. The pain may be poorly localized or localized to the periumbilical or epigastric areas. In preschool-aged children, the pain is typically periumbilical and worsens after eating. Younger children may not localize pain and present with anorexia and irritability. After the age of 6 years, the child's description of pain may be similar to the description by adults. The classic pain of peptic ulcer disease (ie, pain that awakens the child, worsens with food, and is relieved by fasting) is described infrequently, but it helps in distinguishing GI pathology from psychogenic pathology when present. Frequent exacerbations and remissions of pain extend over weeks to months.
Vomiting in infants and toddlers may be associated with slow growth. Recurrent vomiting is also noted in preschool-aged and school-aged children. GI tract bleeding (eg, melena, hematochezia, hematemesis) may be another presentation in children. In infants and particularly neonates, serious underlying illness and stress ulceration most commonly manifest as acute perforation or hemorrhage. GI bleeding may lead to iron-deficiency anemia (IDA), and patients may present with vague complaints of fatigue, headache, dyspnea, or malaise. As many as 25% of children with duodenal ulcer have silent presentation with painless upper GI bleeding or iron deficiency anemia. For children with ulcer perforation, the symptoms are consistent with peritonitis and abrupt in onset.
PHYSICAL Children with peptic ulcer disease leading to complications (eg, severe blood loss in the GI tract, perforation, obstruction) can appear acutely ill and have evidence of hemodynamic instability or signs of an acute abdomen. Children with long-standing peptic ulcer disease from H pylori may become profoundly anemic from undetected chronic bleeding and have no complaints. H pylori
Include the following in the physical examination: Observation of the general appearance of the child Evaluation of vital signs Assessment of perfusion with attention to mental status, heart rate, pulses, and capillary refill Assessment of hydration status with attention to moisture of the mucous membranes and skin turgor Observation of any pallor of the skin and conjunctivae Thorough chest examination Careful inspection, auscultation, and palpation of the abdomen, with notation of any liver or spleen enlargement Rectal examination and stool guaiac testing Pelvic examination in sexually active female patients with pain Examination of the testicles and inguinal area in male patients Hemorrhage accompanies peptic ulcer disease in 15 -20% of patients. Acute abdomen resulting from perforation of the GI tract occurs in 5% of children with peptic ulcer disease.
CAUSES Primary peptic ulcer disease can be divided into the following: H pylori– associated disease H pylori– negative/idiopathic disease Hypersecretory states ZES, gastrin (G)-cell hyperplasia/hyperfunction systemic mastocytosis, cystic fibrosis, short bowel syndrome, and hyperparathyroidism. Genetic factors may be important, as indicated by the observation that as many as 50% of children with peptic ulcer disease have a first-degree or second-degree relative with peptic ulcer disease. In addition, a concordance rate that is 3 times higher in monozygotic than in dizygotic twins has been described, and children with blood group O have an increased incidence of peptic ulcer disease.

Emotional stress has been described as a factor that predisposes children to peptic ulcer disease. Alcohol has been documented to produce inflammation, erosions, and hemorrhage in the gastric mucosa in animal and adult human studies. Caffeine intake also predisposes children to peptic ulcer disease. Compared with people who do not smoke cigarettes, those who do are twice as likely to develop peptic ulcer disease. Smoking may lead to ulceration, slow healing, and an increased risk of recurrent disease.
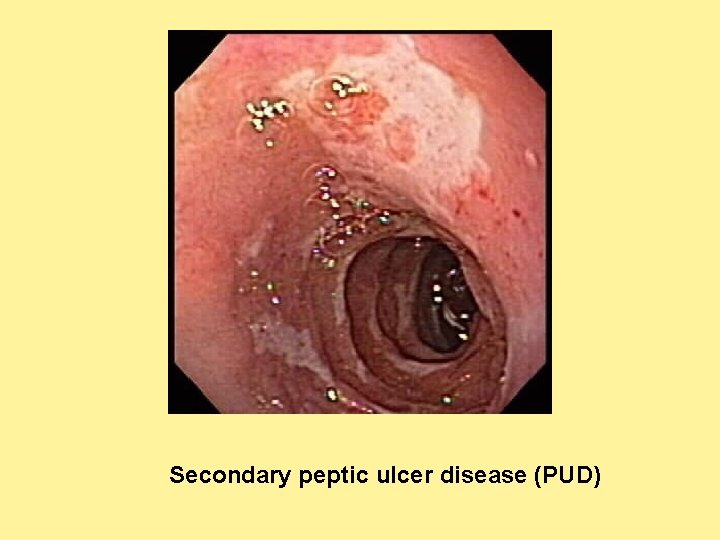
Secondary peptic ulcer disease Corticosteroids, NSAIDs, and aspirin use predispose children to ulceration. These drugs disrupt the mucosal permeability barrier, rendering the mucosa vulnerable to injury. As many as 30% of adults taking NSAIDS have GI adverse effects. Although the prevalence of NSAID gastropathy in children is unknown, it seems to be increasing, especially in children with chronic arthritis treated with NSAIDS. Recent case reports have demonstrated gastric ulceration from low-dose ibuprofen in children, even after 1 or 2 doses
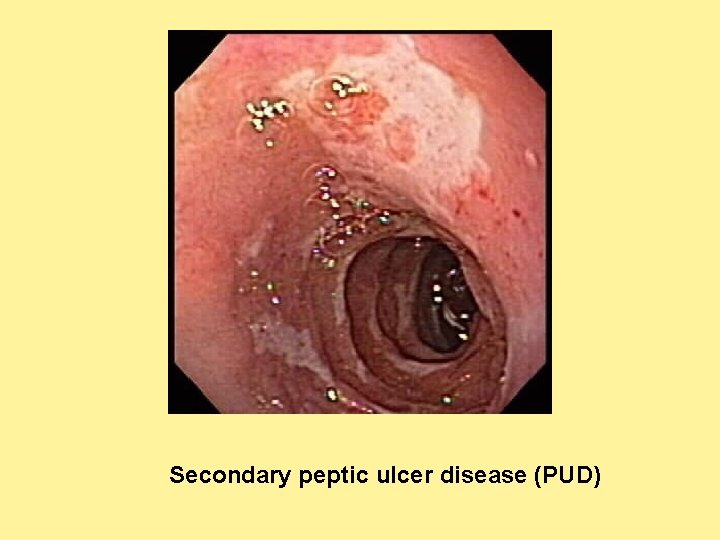
Secondary peptic ulcer disease (PUD)
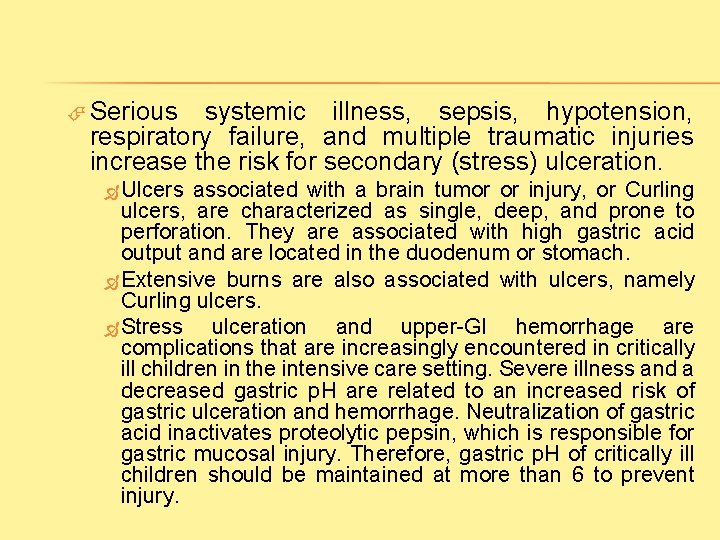
Serious systemic illness, sepsis, hypotension, respiratory failure, and multiple traumatic injuries increase the risk for secondary (stress) ulceration. Ulcers associated with a brain tumor or injury, or Curling ulcers, are characterized as single, deep, and prone to perforation. They are associated with high gastric acid output and are located in the duodenum or stomach. Extensive burns are also associated with ulcers, namely Curling ulcers. Stress ulceration and upper-GI hemorrhage are complications that are increasingly encountered in critically ill children in the intensive care setting. Severe illness and a decreased gastric p. H are related to an increased risk of gastric ulceration and hemorrhage. Neutralization of gastric acid inactivates proteolytic pepsin, which is responsible for gastric mucosal injury. Therefore, gastric p. H of critically ill children should be maintained at more than 6 to prevent injury.
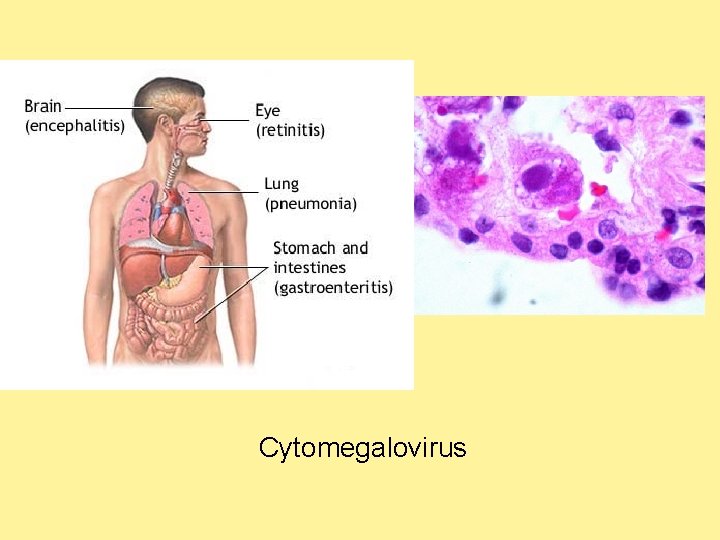
Other causes of secondary ulcers include the following: Allergic gastritis and eosinophilic gastritis Cytomegalovirus Graft versus host disease Uremic gastropathy Henoch-Schönlein gastritis Corrosive gastropathy Celiac disease Hepatic cirrhosis Bile gastropathy Autoimmune disease Exercise Crohn disease Other granulomatous gastritides (eg, sarcoidosis, histiocytosis X, tuberculosis) Phlegmonous gastritis and emphysematous gastritis Other infections, including Helicobacter heilmanni, herpes simplex, influenza, syphilis, Candida albicans , histoplasmosis, mucormycosis, and anisakiasis Radiation gastropathy
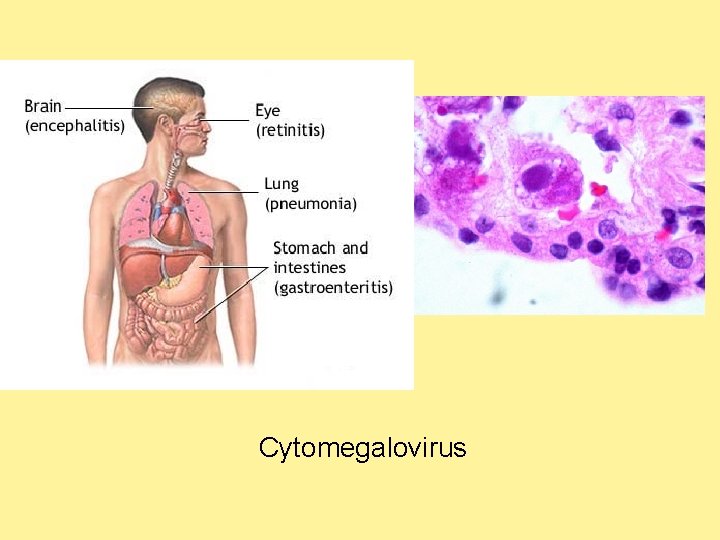
Cytomegalovirus
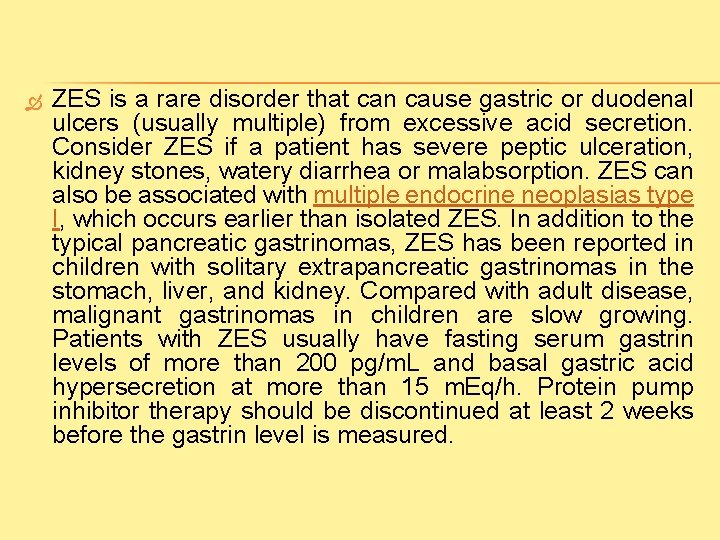
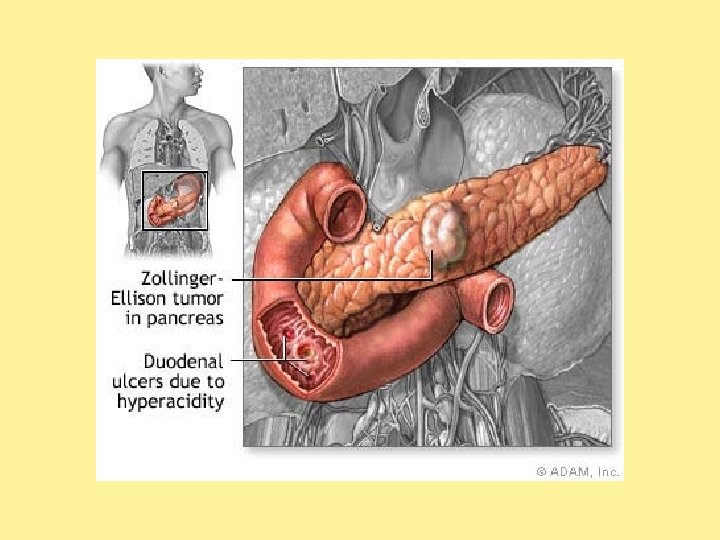
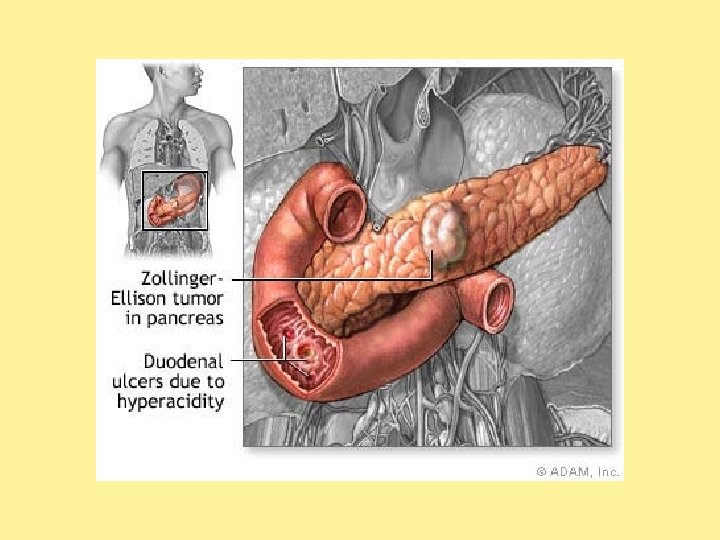
ZES is a rare disorder that can cause gastric or duodenal ulcers (usually multiple) from excessive acid secretion. Consider ZES if a patient has severe peptic ulceration, kidney stones, watery diarrhea or malabsorption. ZES can also be associated with multiple endocrine neoplasias type I, which occurs earlier than isolated ZES. In addition to the typical pancreatic gastrinomas, ZES has been reported in children with solitary extrapancreatic gastrinomas in the stomach, liver, and kidney. Compared with adult disease, malignant gastrinomas in children are slow growing. Patients with ZES usually have fasting serum gastrin levels of more than 200 pg/m. L and basal gastric acid hypersecretion at more than 15 m. Eq/h. Protein pump inhibitor therapy should be discontinued at least 2 weeks before the gastrin level is measured.
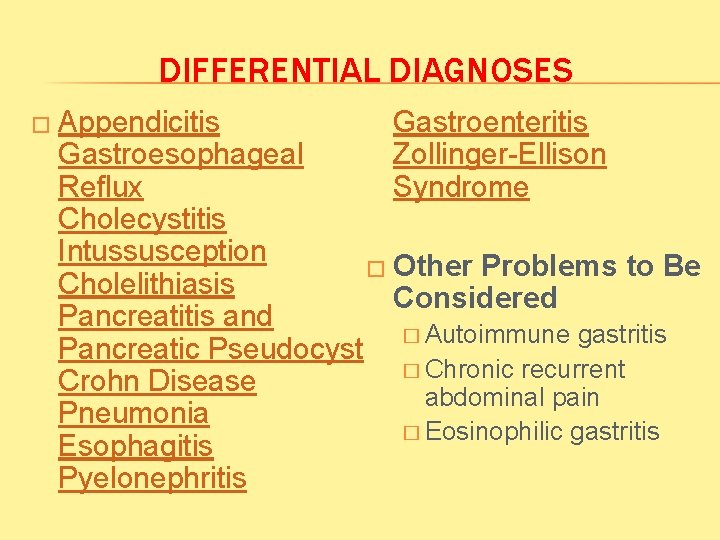
DIFFERENTIAL DIAGNOSES � Appendicitis Gastroenteritis Zollinger-Ellison Syndrome Gastroesophageal Reflux Cholecystitis Intussusception � Other Problems to Be Cholelithiasis Considered Pancreatitis and � Autoimmune gastritis Pancreatic Pseudocyst � Chronic recurrent Crohn Disease abdominal pain Pneumonia � Eosinophilic gastritis Esophagitis Pyelonephritis
LABORATORY STUDIES A minimum of laboratory studies may be indicated in children with mild peptic ulcer disease (PUD) symptoms and normal examination findings. The following laboratory data may be needed in children who are in unstable condition, in those who have severe or chronic or recurrent symptoms, or in those with serious complications of peptic ulcer disease. Hemoglobin and hematocrit tests: These may be indicated to diagnose anemia in the setting of chronic blood loss from the GI tract, to determine the severity of anemia in the setting of acute or massive GI bleeding, and to guide and monitor transfusion or iron therapy.
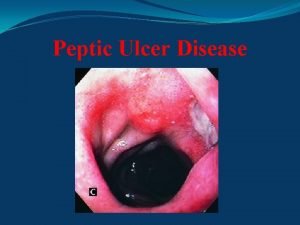
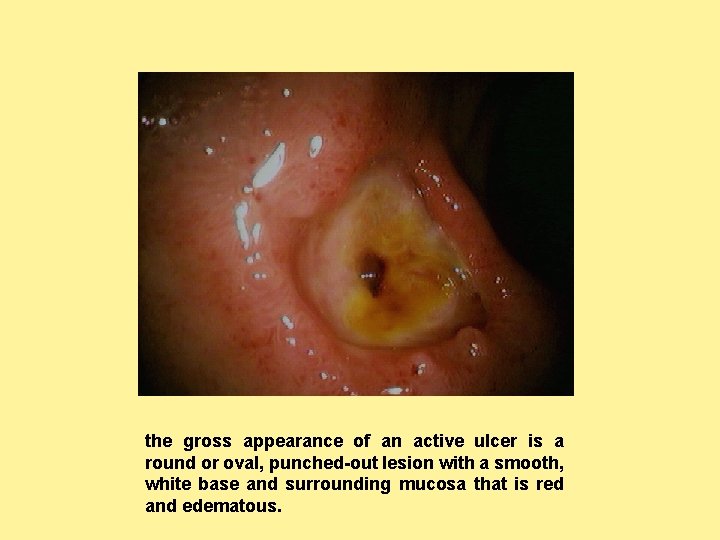
PROCEDURES Esophagogastroduodenoscopy (EGD) is the procedure of choice for detecting peptic ulcer disease in the pediatric population. EGD allows for direct visualization of the mucosa; for localization of the source of bleeding; and for the diagnosis of H pylori infection by analyzing biopsy specimens, performing cultures or detecting urease activity. Therapeutic endoscopy for acute bleeding (coagulation of a bleeding ulcer with a heater probe or injection with vasoconstricting agents) is another important indication for EGD. More than 90% of duodenal ulcers are found in the duodenal bulb. An erosion is small (<3 mm) and superficial defect in the mucosa. Consider nasogastric (NG) lavage in a child who is ill and in whom upper-GI hemorrhage is suspected because of hematemesis or melena.
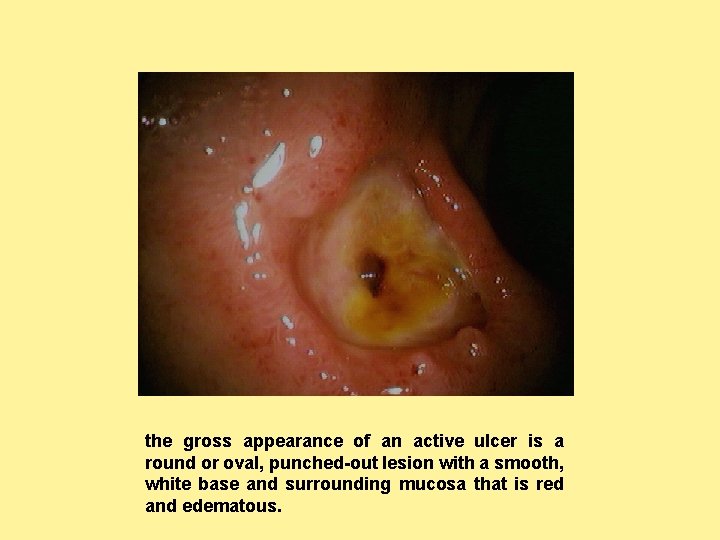
the gross appearance of an active ulcer is a round or oval, punched-out lesion with a smooth, white base and surrounding mucosa that is red and edematous.
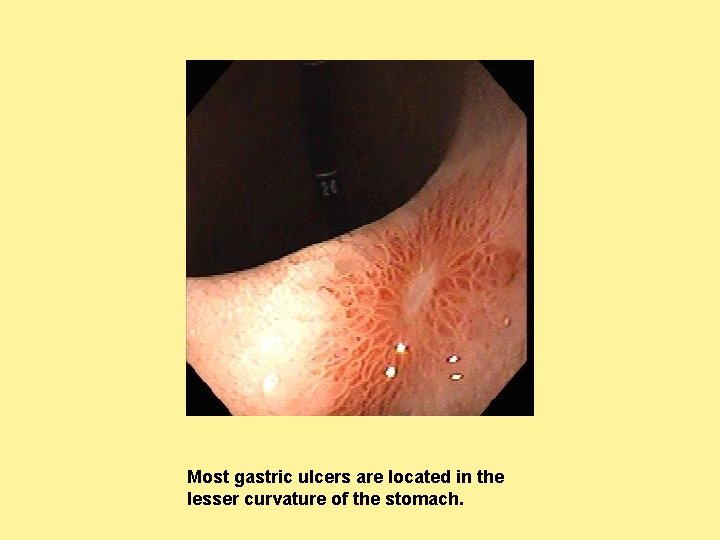
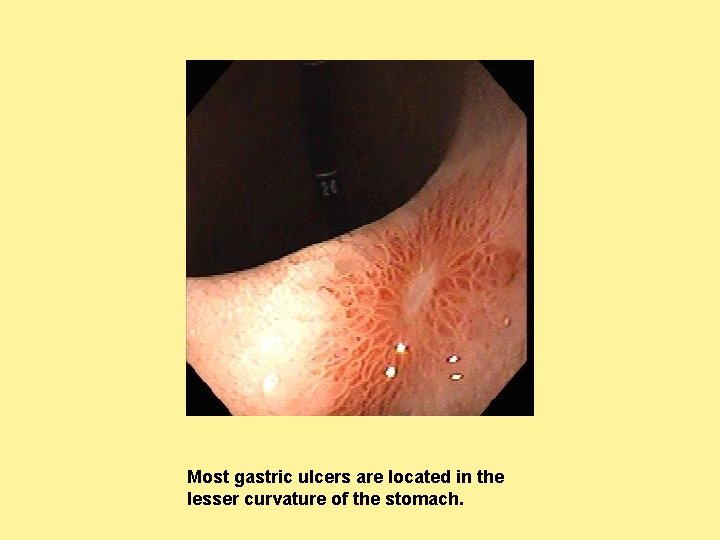
Most gastric ulcers are located in the lesser curvature of the stomach.
MEDICAL CARE In children with peptic ulcer disease (PUD) who appear to be well, in whom examination findings are normal and symptoms are mild, evaluation may be conducted on an outpatient basis. The eradication of H pylori relies on a multidrug regimen. Triple therapy is considered to be the standard treatment for children, including a proton pump inhibitor combined with 2 antibiotics. This regimen has been shown to be very effective in eradicating H pylori from the stomach. The current recommendation is treatment with amoxicillin, clarithromycin, and a proton pump inhibitor for 2 weeks.
Non-H pylori peptic ulcer disease is effectively treated with acid suppression; however, prospective studies are lacking. Complete healing and resolution of symptoms requires appropriate therapy for underlying etiology, as in Crohn disease. Proton pump inhibitors are increasingly used in the pediatric population, especially in children with gastroesophageal reflux disease (GERD), than before. Proton pump inhibitors provide consistent gastric p. H control, and patients do not develop tachyphylaxis with repeated dosing. A recent study in hospitalized adult patients revealed no significant difference among various proton pump inhibitors given through different routes (intravenous [IV] vs oral [PO]) on raising intragastric p. H levels above 6 for 72 hours after successful endoscopic hemostasis in patients with a bleeding peptic ulcer. 8 In addition standard -dose proton pump inhibitor infusion was as effective as a
The risk of adverse effects appear to be minimal with long -term administration. The number of gastrin-secreting cells (G cells) increases, as does the ratio of G cells to D cells. The clinical significance of this effect is unknown. Long-term studies have demonstrated hypergastrinemia and enterochromaffinlike cell hyperplasia in children receiving continuous proton pump inhibitor therapy, but this has not affected histologic findings or caused an increase risk for carcinoid formation. Small gastric polyps may develop in some patients during proton pump inhibitor maintenance therapy. These polyps usually develop in the gastric corpus and are hyperplastic or benign fundic gland cysts. Rebound acid hypersecretion arises from the trophic effects of the proton pump inhibitor–induced hypergastrinemia; 44% of previously asymptomatic subjects experienced clinically significant heartburn, acid reflux, or dyspepsia after discontinuing a 2 -month course of esomeprazole at 40 mg/d compared with 15% after placebo.
Sucralfate is an aluminum salt of sulfated sucrose, which, in the presence of acid p. H, forms a complex, pastelike substance that adheres to the damaged mucosal area. It forms a protective coating that acts as a barrier between the lining and gastric acid, pepsin, and bile salts. Misoprostol is a synthetic prostaglandin E 1 analog with gastric antisecretory and cytoprotective properties. It is effective in adults for the prophylaxis and treatment of nonsteroidal anti-inflammatory drug (NSAID)-induced gastropathy. Studies on the benefits of misoprostol administration in children are limited.
Optimal management of severe or refractory peptic ulcer disease requires a multidisciplinary team approach, using primary care providers, gastroenterologists, and general surgeons. Medical management has become the cornerstone of therapy. Identification and eradication of recurrent H pylori infection can heal ulceration and also prevent recurrence. Severe, intractable, or recurrent peptic ulcer disease with associated complications mandates a careful evaluation to determine potential etiologies like gastrinomas or Crohn disease
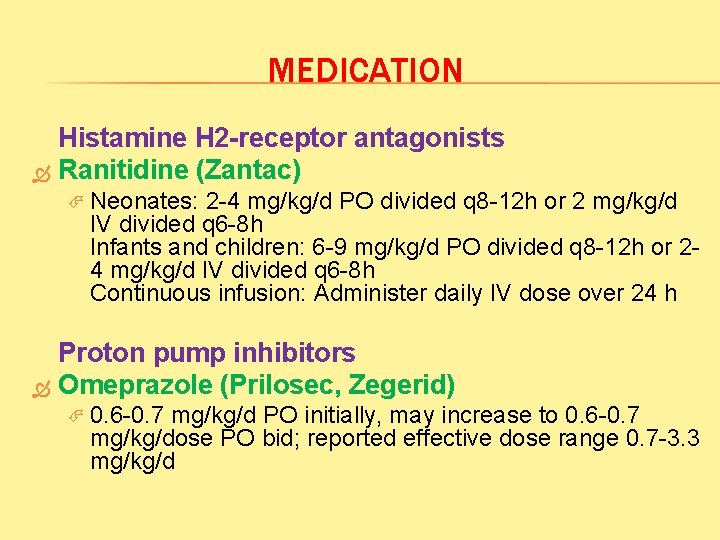
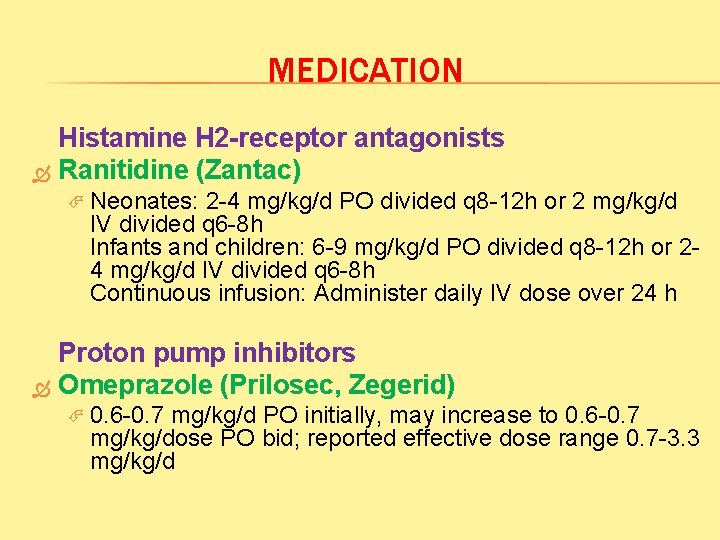
MEDICATION Histamine H 2 -receptor antagonists Ranitidine (Zantac) Neonates: 2 -4 mg/kg/d PO divided q 8 -12 h or 2 mg/kg/d IV divided q 6 -8 h Infants and children: 6 -9 mg/kg/d PO divided q 8 -12 h or 24 mg/kg/d IV divided q 6 -8 h Continuous infusion: Administer daily IV dose over 24 h Proton pump inhibitors Omeprazole (Prilosec, Zegerid) 0. 6 -0. 7 mg/kg/d PO initially, may increase to 0. 6 -0. 7 mg/kg/dose PO bid; reported effective dose range 0. 7 -3. 3 mg/kg/d

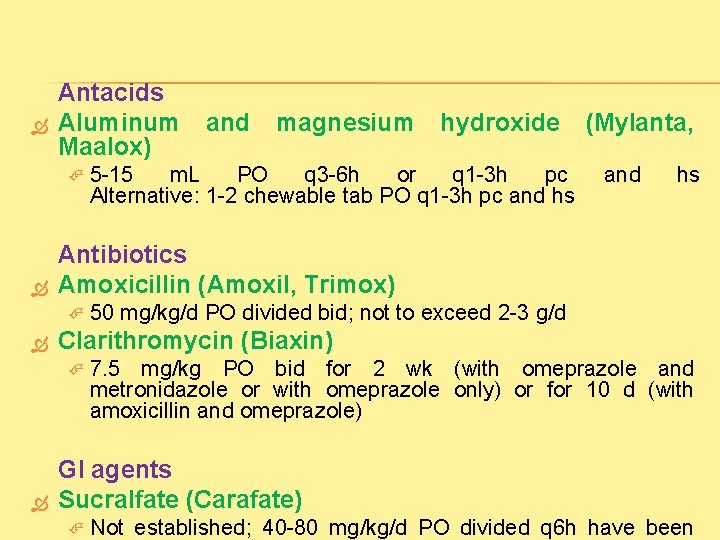
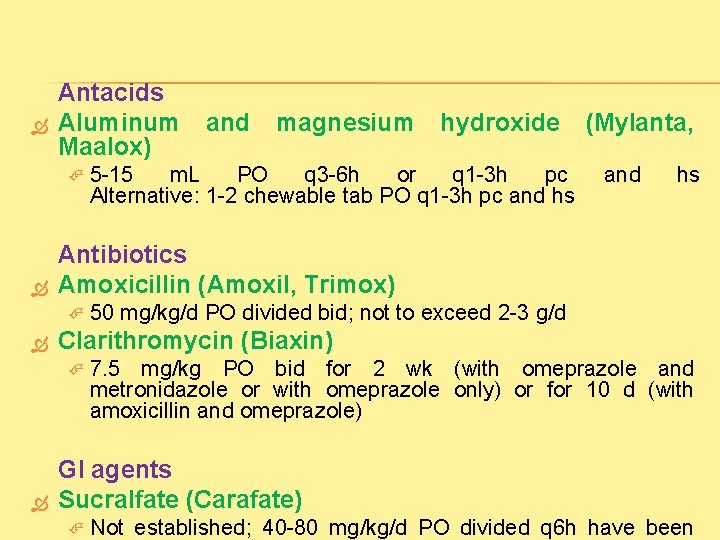
Antacids Aluminum Maalox) hydroxide 5 -15 m. L PO q 3 -6 h or q 1 -3 h pc Alternative: 1 -2 chewable tab PO q 1 -3 h pc and hs (Mylanta, and hs 50 mg/kg/d PO divided bid; not to exceed 2 -3 g/d Clarithromycin (Biaxin) magnesium Antibiotics Amoxicillin (Amoxil, Trimox) and 7. 5 mg/kg PO bid for 2 wk (with omeprazole and metronidazole or with omeprazole only) or for 10 d (with amoxicillin and omeprazole) GI agents Sucralfate (Carafate) Not established; 40 -80 mg/kg/d PO divided q 6 h have been

 Triple therapy for peptic ulcer disease
Triple therapy for peptic ulcer disease Emetic example
Emetic example Triple therapy for peptic ulcer disease
Triple therapy for peptic ulcer disease Ajeerna symptoms
Ajeerna symptoms Patient counselling for peptic ulcer disease
Patient counselling for peptic ulcer disease Triple therapy for peptic ulcer disease
Triple therapy for peptic ulcer disease Peptic ulcer disease
Peptic ulcer disease Gastric ulcer vs duodenal ulcer
Gastric ulcer vs duodenal ulcer Peptic ulcer case study
Peptic ulcer case study Peptic ulcer definition
Peptic ulcer definition Peptic ulcer diseas
Peptic ulcer diseas Peptic ulcer morphology
Peptic ulcer morphology Nursing management of peptic ulcer
Nursing management of peptic ulcer Peptic ulcer symptoms
Peptic ulcer symptoms Stages of peptic ulcer perforation
Stages of peptic ulcer perforation Typhoid ulcer gross
Typhoid ulcer gross Classification of ulcer
Classification of ulcer Disease definition
Disease definition Csendes procedure
Csendes procedure Communicable disease and non communicable disease
Communicable disease and non communicable disease Homonynous
Homonynous Lesion of glossopharyngeal nerve
Lesion of glossopharyngeal nerve Lateral geniculate nucleus lesion
Lateral geniculate nucleus lesion Glumerolo
Glumerolo Heterogeneous hypoechoic lesion in liver
Heterogeneous hypoechoic lesion in liver Sugralfate
Sugralfate Quiste meniscal interno
Quiste meniscal interno Lésion
Lésion Subendocardico y subepicardico
Subendocardico y subepicardico Hpv us
Hpv us Patron colestasico
Patron colestasico Tug lesion proximal tibia
Tug lesion proximal tibia Pretectal area
Pretectal area Parakeratin vs orthokeratin
Parakeratin vs orthokeratin Lésion en verre dépoli
Lésion en verre dépoli Accion terapeutica del paracetamol
Accion terapeutica del paracetamol Apergaminamiento medicina legal
Apergaminamiento medicina legal Molusco contagioso lesion elemental
Molusco contagioso lesion elemental