MANAGEMENT OF STROKE Stroke Definition Stroke is clinically

- Slides: 20
MANAGEMENT OF STROKE
Stroke: Definition Stroke is clinically defined as a neurologic syndrome characterized by acute disruption of blood flow to an area of the brain and corresponding onset of neurologic deficits related to the concerned area of the brain Nurs Clin N Am 2002; 37: 35 -57

The Burden of Stroke l l l Most common life-threatening neurologic disease Third most common cause of death globally Incidence in India: 73/1, 000 per year Burden is likely to increase with risk factors like aging, smoking, adverse dietary patterns Most common cause of disability and dependence, with more than 70% of stroke survivors remaining vocationally impaired and more than 30% requiring assistance with daily activities Stroke 1998; 29: 1730 -36 Neurol India 2002; 50: 279 -81
Stroke: Classification Ischemic stroke: Account for 80%. Results from occlusion in the blood vessel supplying the brain u u Thrombotic: Occlusion due to atherothrombosis of small/large vessels supplying the brain Embolic: Occlusion due to embolus arising either from heart (e. g. atrial fibrillation, valvular disease) or blood vessel
Classification (contd. ) Hemorrhagic stroke: Account for 20%. Results from rupture of blood vessels leading to bleeding in brain u u Intracerebral: Bleeding within the brain due to rupture of small blood vessels. Occurs mainly due to high blood pressure Subarachnoid: Bleeding around the brain; commonest cause is rupture of aneurysm. Other causes: Head injury
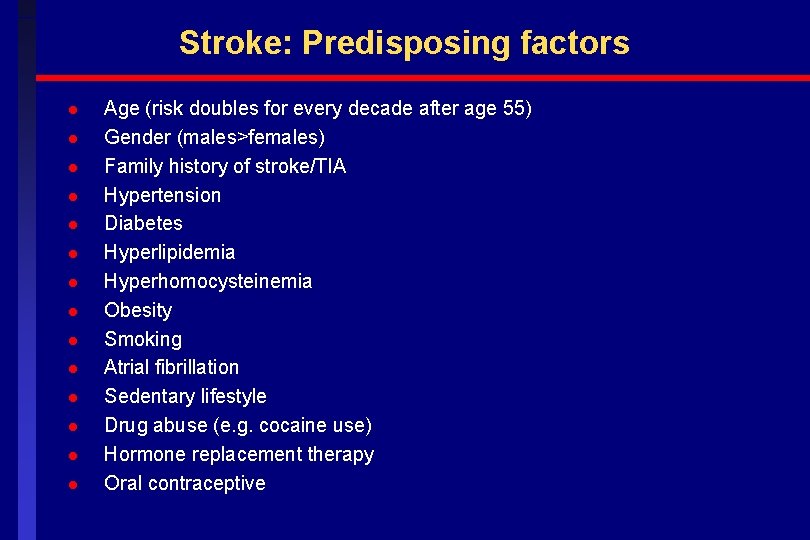
Stroke: Predisposing factors l l l l Age (risk doubles for every decade after age 55) Gender (males>females) Family history of stroke/TIA Hypertension Diabetes Hyperlipidemia Hyperhomocysteinemia Obesity Smoking Atrial fibrillation Sedentary lifestyle Drug abuse (e. g. cocaine use) Hormone replacement therapy Oral contraceptive
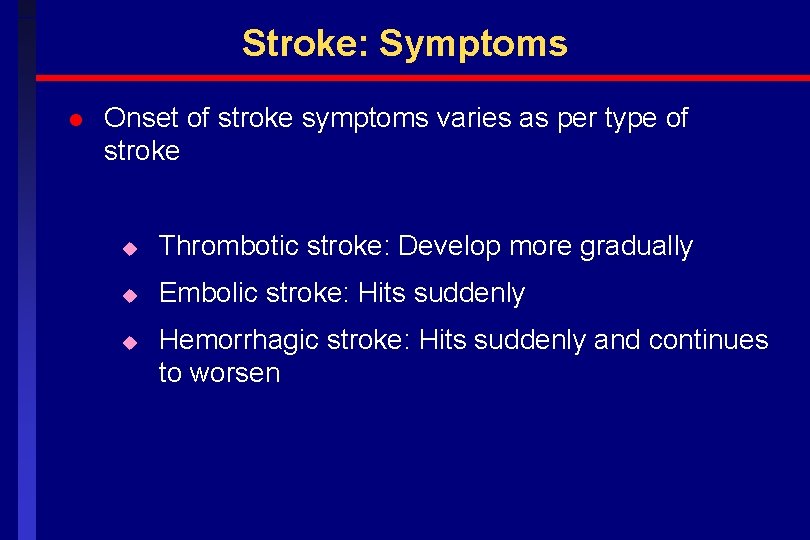
Stroke: Symptoms l Onset of stroke symptoms varies as per type of stroke u Thrombotic stroke: Develop more gradually u Embolic stroke: Hits suddenly u Hemorrhagic stroke: Hits suddenly and continues to worsen
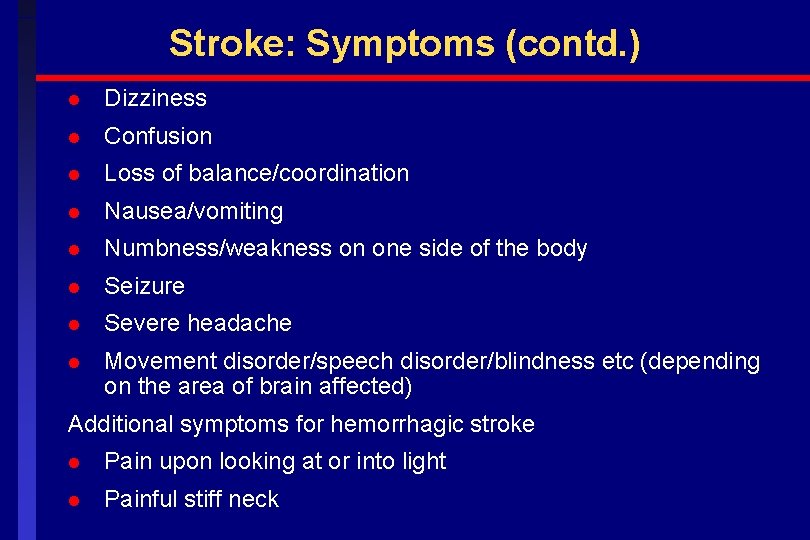
Stroke: Symptoms (contd. ) l Dizziness l Confusion l Loss of balance/coordination l Nausea/vomiting l Numbness/weakness on one side of the body l Seizure l Severe headache l Movement disorder/speech disorder/blindness etc (depending on the area of brain affected) Additional symptoms for hemorrhagic stroke l Pain upon looking at or into light l Painful stiff neck
People may also experience “silent strokes” with no symptoms A silent stroke is a stroke which causes brain damage, but does not exhibit classic symptoms of stroke. They are detected only when a person undergoes a brain scan.
Transient Ischemic Attack (TIA) l “Mini stroke” l Stroke symptoms last for less than 24 hours (usually 10 to 15 mins) l Result as a brief interruption in blood flow to brain l Every TIA is an emergency l TIA may be a warning sign of a larger stroke l Patients with possible TIA should be evaluated by a physician
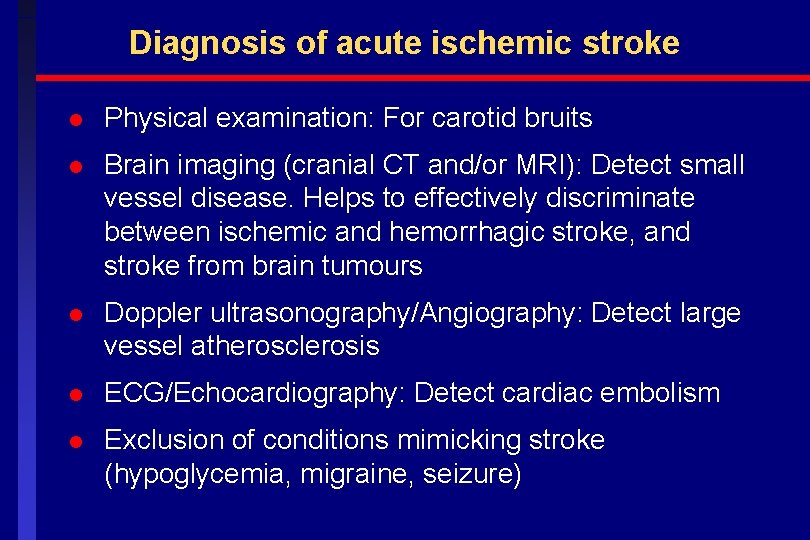
Diagnosis of acute ischemic stroke l Physical examination: For carotid bruits l Brain imaging (cranial CT and/or MRI): Detect small vessel disease. Helps to effectively discriminate between ischemic and hemorrhagic stroke, and stroke from brain tumours l Doppler ultrasonography/Angiography: Detect large vessel atherosclerosis l ECG/Echocardiography: Detect cardiac embolism l Exclusion of conditions mimicking stroke (hypoglycemia, migraine, seizure)
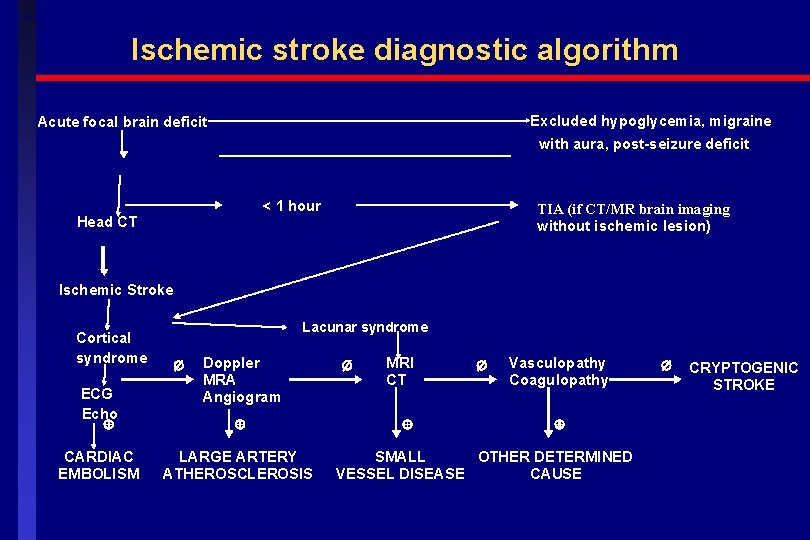
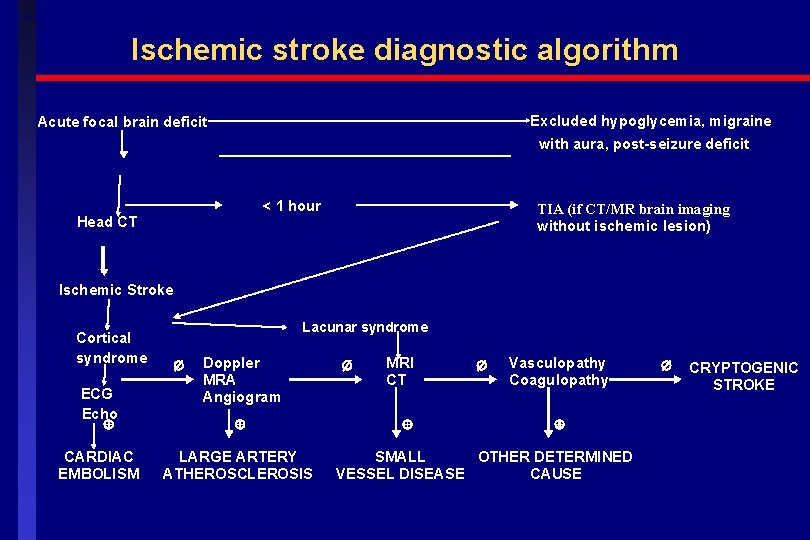
Ischemic stroke diagnostic algorithm Excluded hypoglycemia, migraine Acute focal brain deficit with aura, post-seizure deficit < 1 hour Head CT TIA (if CT/MR brain imaging without ischemic lesion) Ischemic Stroke Cortical syndrome ECG Echo CARDIAC EMBOLISM Lacunar syndrome Doppler MRA Angiogram LARGE ARTERY ATHEROSCLEROSIS MRI CT Vasculopathy Coagulopathy SMALL OTHER DETERMINED VESSEL DISEASE CAUSE CRYPTOGENIC STROKE
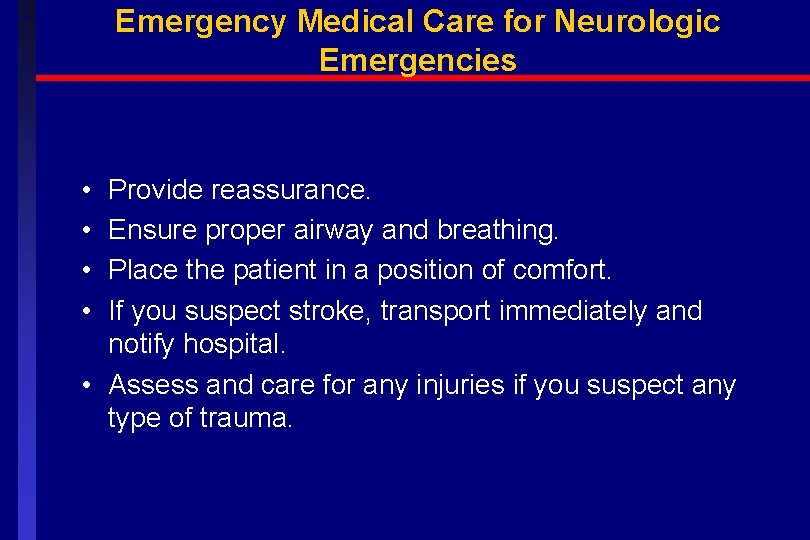
Emergency Medical Care for Neurologic Emergencies • • Provide reassurance. Ensure proper airway and breathing. Place the patient in a position of comfort. If you suspect stroke, transport immediately and notify hospital. • Assess and care for any injuries if you suspect any type of trauma.
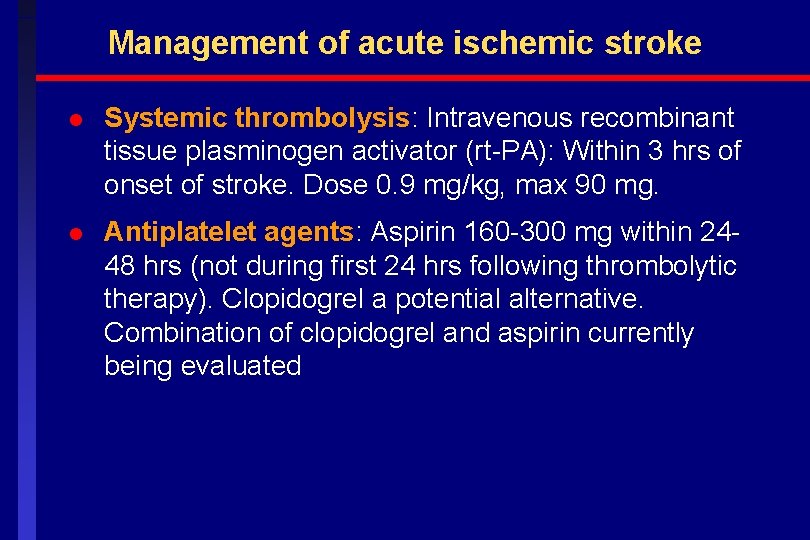
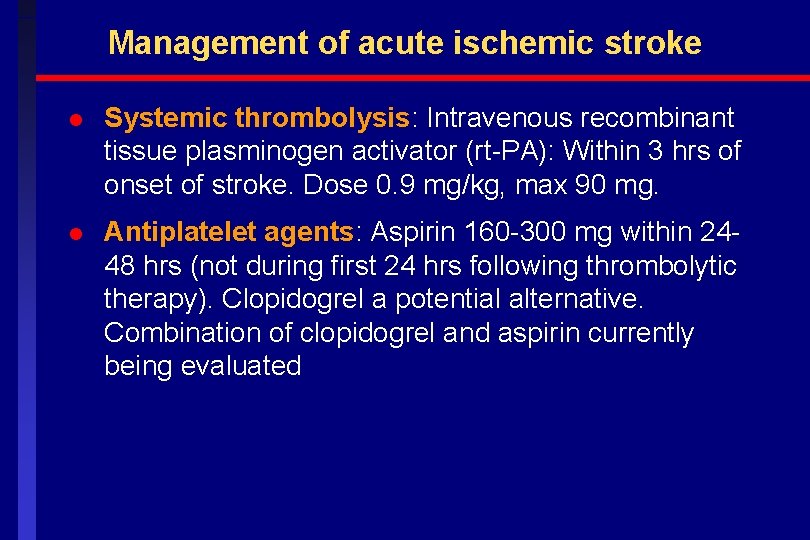
Management of acute ischemic stroke l Systemic thrombolysis: Intravenous recombinant tissue plasminogen activator (rt-PA): Within 3 hrs of onset of stroke. Dose 0. 9 mg/kg, max 90 mg. l Antiplatelet agents: Aspirin 160 -300 mg within 2448 hrs (not during first 24 hrs following thrombolytic therapy). Clopidogrel a potential alternative. Combination of clopidogrel and aspirin currently being evaluated
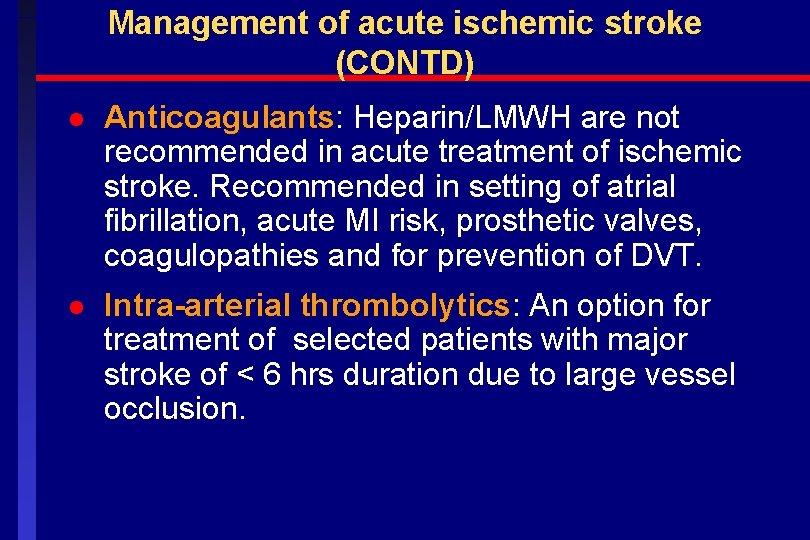
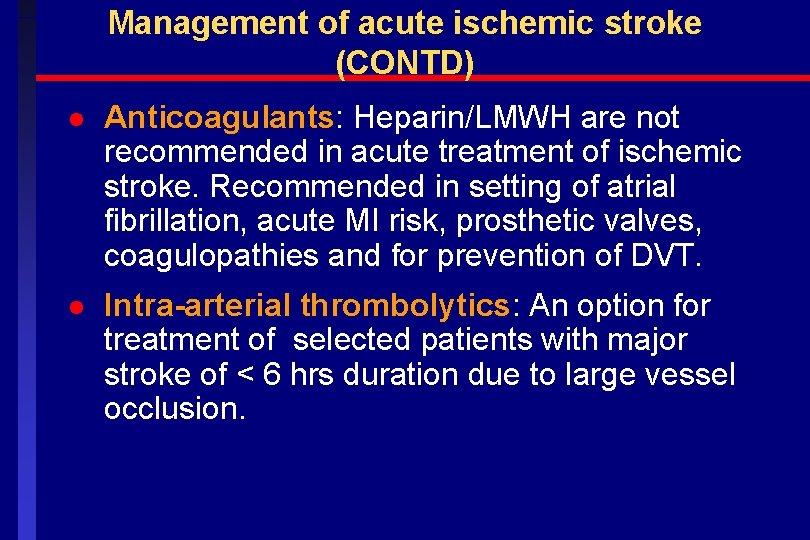
Management of acute ischemic stroke (CONTD) l Anticoagulants: Heparin/LMWH are not recommended in acute treatment of ischemic stroke. Recommended in setting of atrial fibrillation, acute MI risk, prosthetic valves, coagulopathies and for prevention of DVT. l Intra-arterial thrombolytics: An option for treatment of selected patients with major stroke of < 6 hrs duration due to large vessel occlusion.
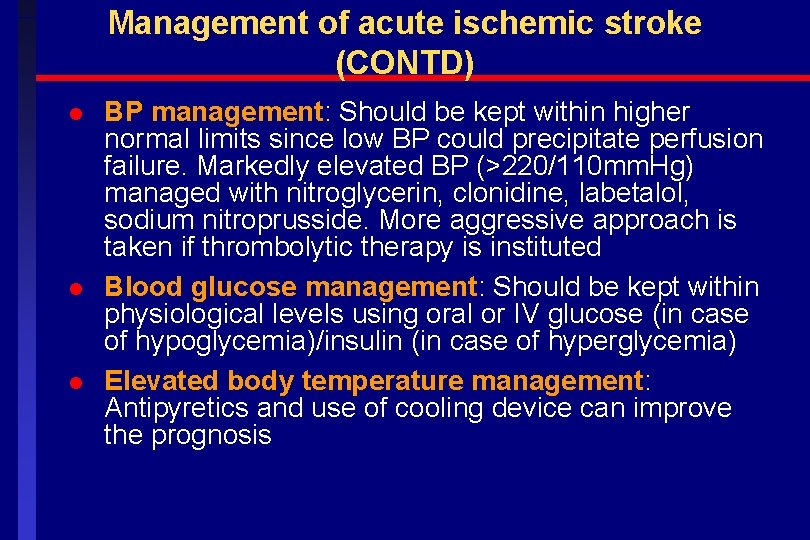
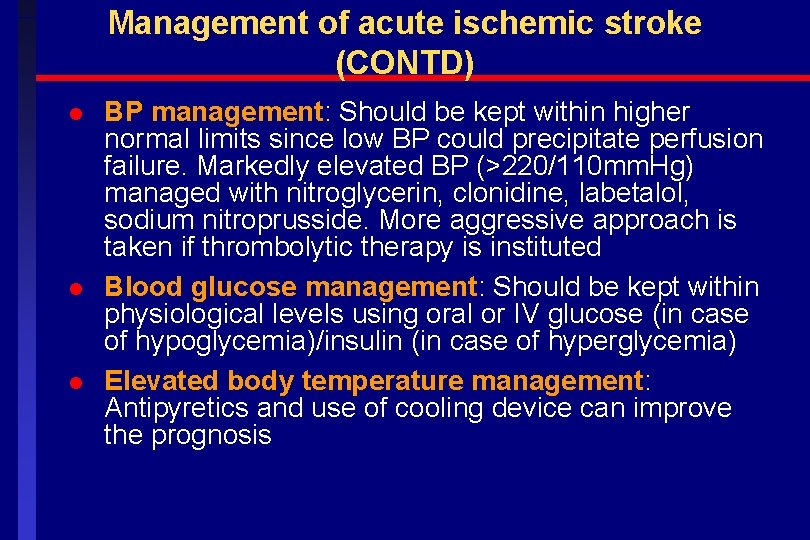
Management of acute ischemic stroke (CONTD) l l l BP management: Should be kept within higher normal limits since low BP could precipitate perfusion failure. Markedly elevated BP (>220/110 mm. Hg) managed with nitroglycerin, clonidine, labetalol, sodium nitroprusside. More aggressive approach is taken if thrombolytic therapy is instituted Blood glucose management: Should be kept within physiological levels using oral or IV glucose (in case of hypoglycemia)/insulin (in case of hyperglycemia) Elevated body temperature management: Antipyretics and use of cooling device can improve the prognosis
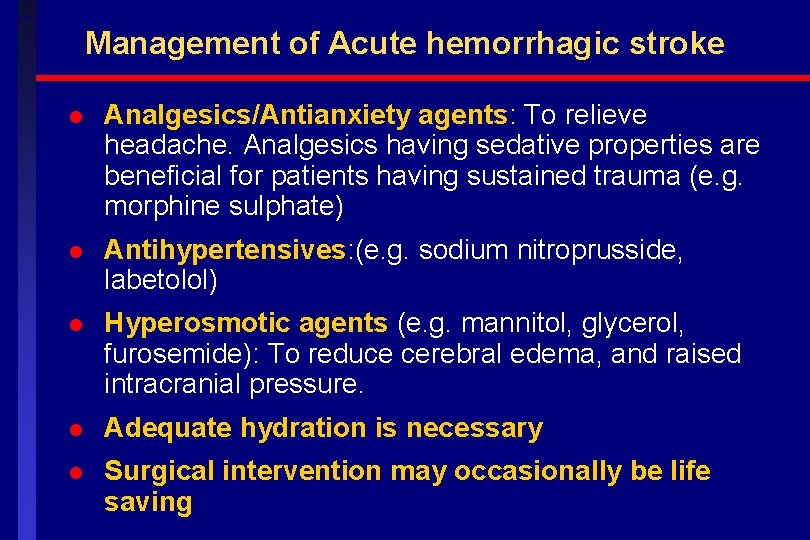
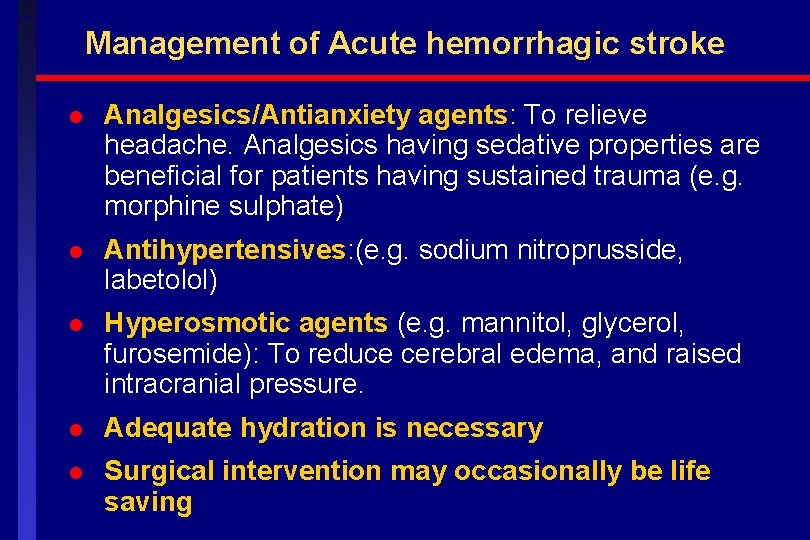
Management of Acute hemorrhagic stroke l Analgesics/Antianxiety agents: To relieve headache. Analgesics having sedative properties are beneficial for patients having sustained trauma (e. g. morphine sulphate) l Antihypertensives: (e. g. sodium nitroprusside, labetolol) l Hyperosmotic agents (e. g. mannitol, glycerol, furosemide): To reduce cerebral edema, and raised intracranial pressure. l Adequate hydration is necessary l Surgical intervention may occasionally be life saving
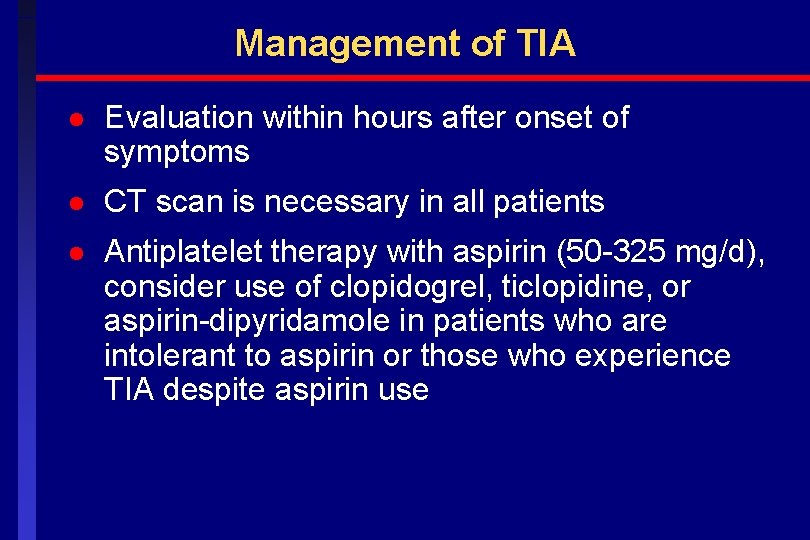
Management of TIA l Evaluation within hours after onset of symptoms l CT scan is necessary in all patients l Antiplatelet therapy with aspirin (50 -325 mg/d), consider use of clopidogrel, ticlopidine, or aspirin-dipyridamole in patients who are intolerant to aspirin or those who experience TIA despite aspirin use
Secondary prevention of stroke l Recurrence: Annual risk is 4. 5 to 6%. Five year recurrence rates range from 24 to 42%; one-third occur within first 30 days, hence high priority should be given to secondary prevention. l Patients with TIA or stroke have an increased risk of MI or vascular event. l Management of hypertension (goal <140/85 mm Hg) l Diabetes control (goal<126 mg/d. L) l Lipid management: Statins (goal cholesterol<200 mg/d. L, LDL<100 mg/d. L) l Antiplatelet agents: Aspirin (50 -325 mg), clopidogrel (75 mg). A fixed dose combination of the two drug may also be used l Anticoagulants: Warfarin (target INR 2 to 3); esp. recommended in patients with cardioembolic stroke l Appropriate life style modification (cessation of smoking, exercise, diet etc)
Surgical interventions l Balloon angioplasty/stenting l Carotid endarterectomy/Bypass l Decompressive surgery
 Kussmaul sign
Kussmaul sign Latchumanadhas
Latchumanadhas Kussmaul's sign
Kussmaul's sign Anterior stroke vs posterior stroke
Anterior stroke vs posterior stroke Nursing management of stroke
Nursing management of stroke Nursing management of stroke
Nursing management of stroke Stroke precautions nursing
Stroke precautions nursing Wake up stroke definition
Wake up stroke definition What is stroke volume
What is stroke volume Cva complications
Cva complications Top management and middle management
Top management and middle management Top management middle management first line management
Top management middle management first line management Top management middle management first line management
Top management middle management first line management Stroke and turn clinic
Stroke and turn clinic Participle brush stroke
Participle brush stroke Brushstrokes in writing
Brushstrokes in writing The little decoration at the end of a letter stroke is a
The little decoration at the end of a letter stroke is a Back orifice, bifrost, onapsis bizploit are examples of:
Back orifice, bifrost, onapsis bizploit are examples of: Stoke's theorem gives the relation between
Stoke's theorem gives the relation between National stroke audit rehabilitation services
National stroke audit rehabilitation services What decreases stroke volume
What decreases stroke volume