LOWER MOTOR NEURON LOWER MOTOR NEURON PARAPLEGIA DR





- Slides: 69

LOWER MOTOR NEURON
LOWER MOTOR NEURON PARAPLEGIA DR RABIA RATHORE ASSISTANT PROFESSOR WEST MEDICAL WARD MAYO HOSPITAL/K. E. M. U

DEFINITION OF PARAPLEGIA • Paraplegia is a word taken from GREEK language para + plessein means STRIKE AT SIDE. • It is defined as impairment of motor function of lower limbs with or without involvement of sensory system.
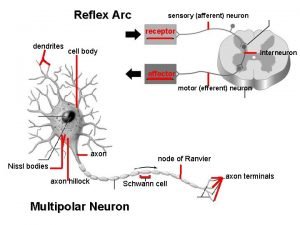
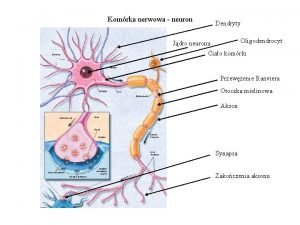
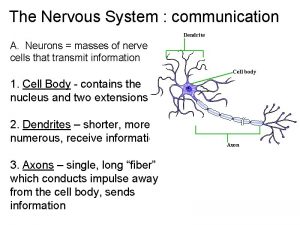
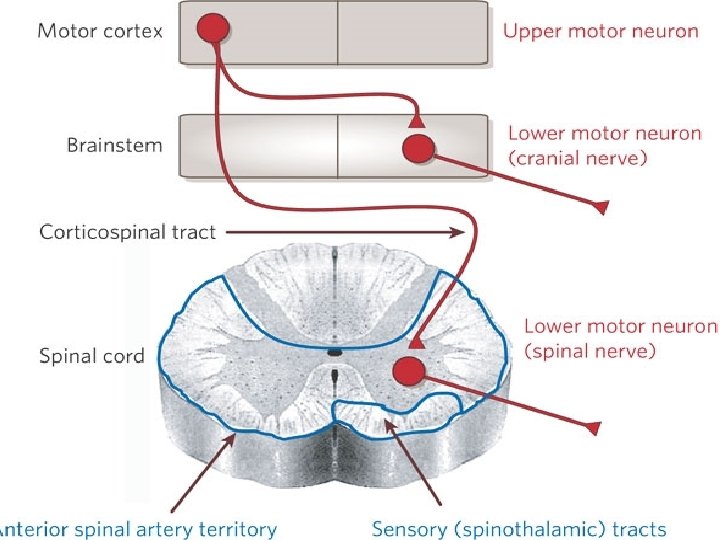
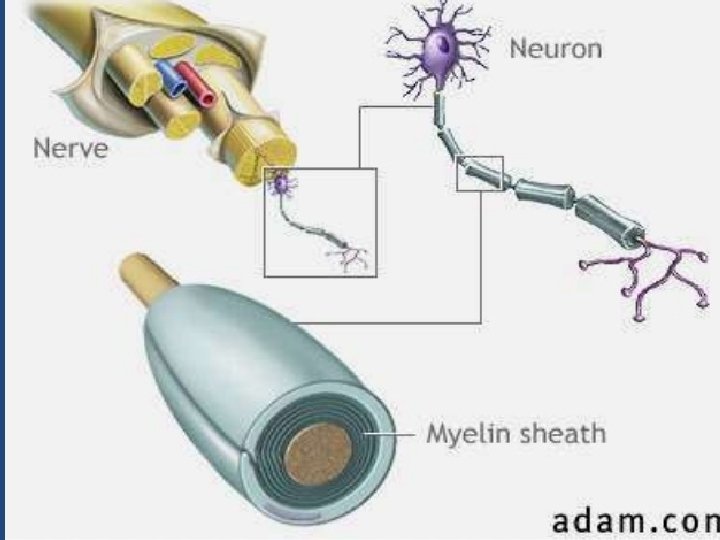
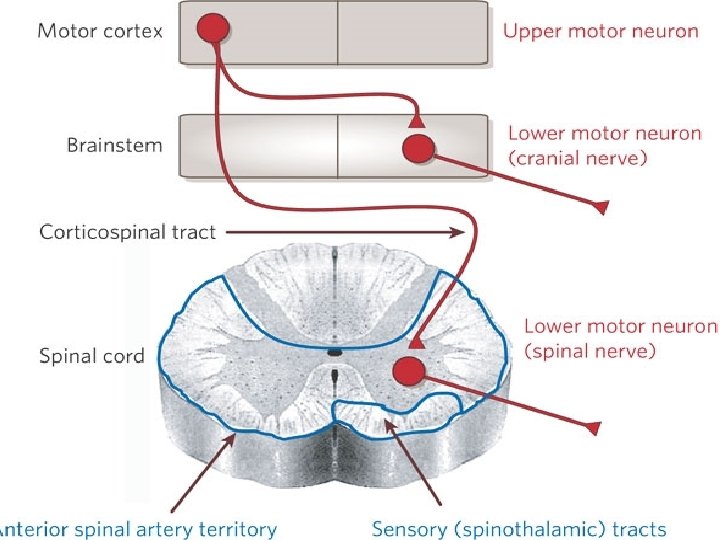
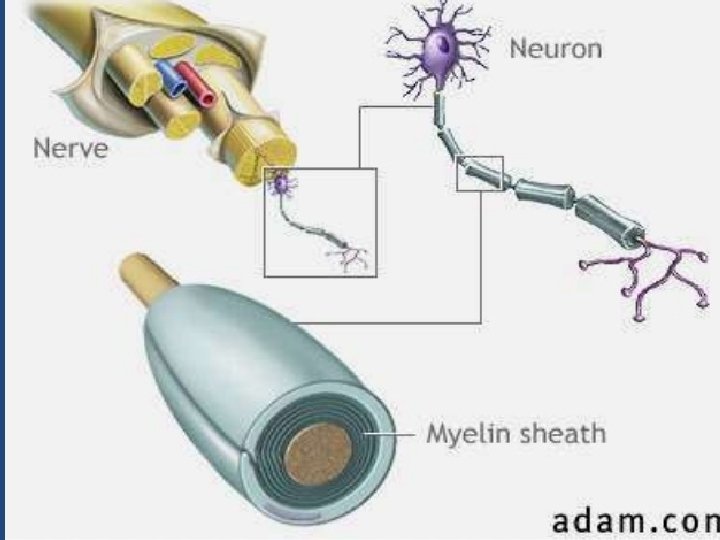
DEFINITION • A lower motor neuron lesion is a lesion which affects nerve fibers traveling from the ventral horn or anterior gray column of the spinal cord to the relevant muscle(s).
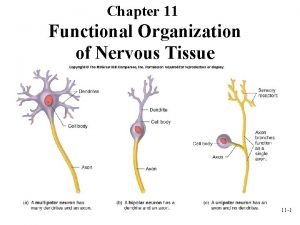
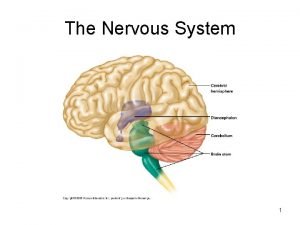
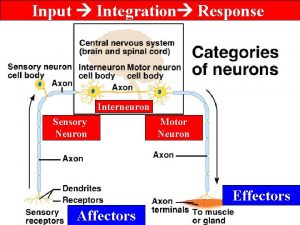
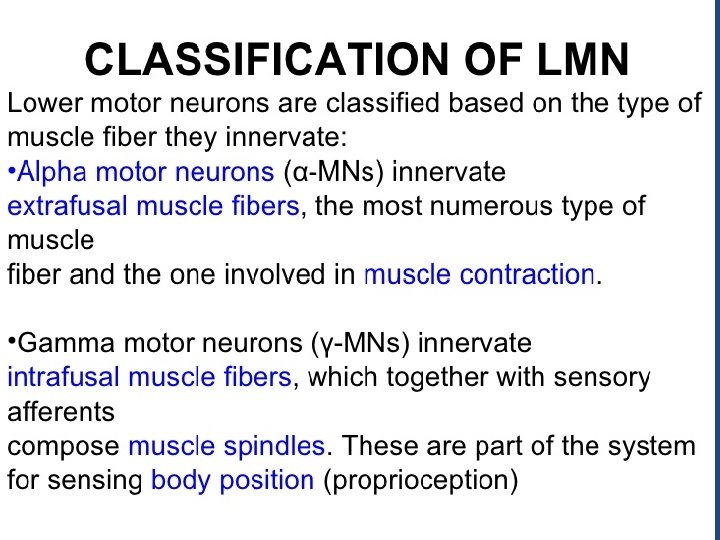
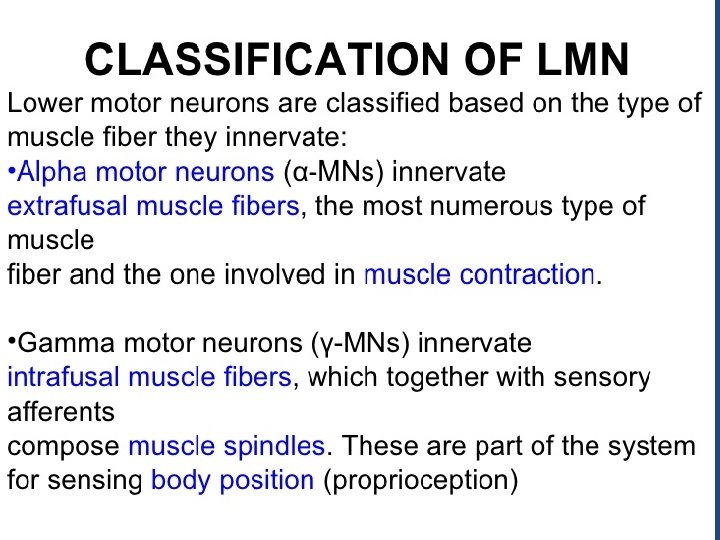
LOWER MOTOR NEURONS • Lower motor neurons are the anterior gray horn cells in the spinal cord and the motor neurons of the cranial nerve nuclei situated in the brain stem, which innervates the muscles directly. • The lower motor neurons are under the influence of upper motor neurons. • The activity of particular muscle depends upon the excitation of the alpha motor neurons in the spinal cord or cranial nerve nuclei(LOWER MOTOR NEURONS)
DEFINITION
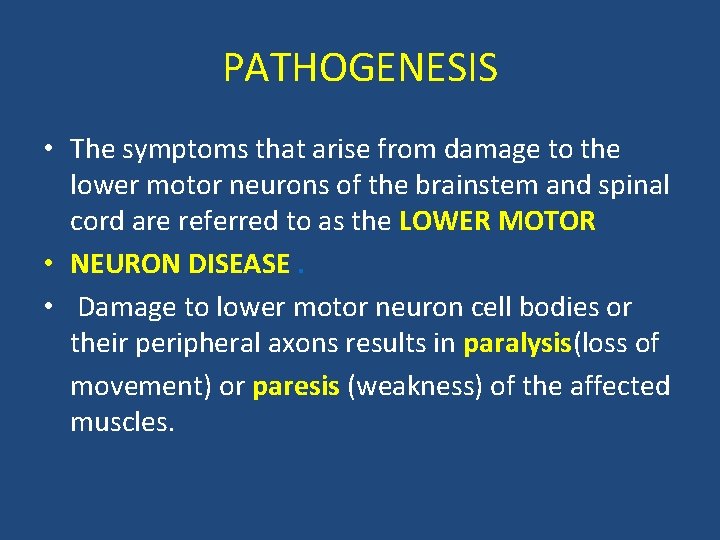
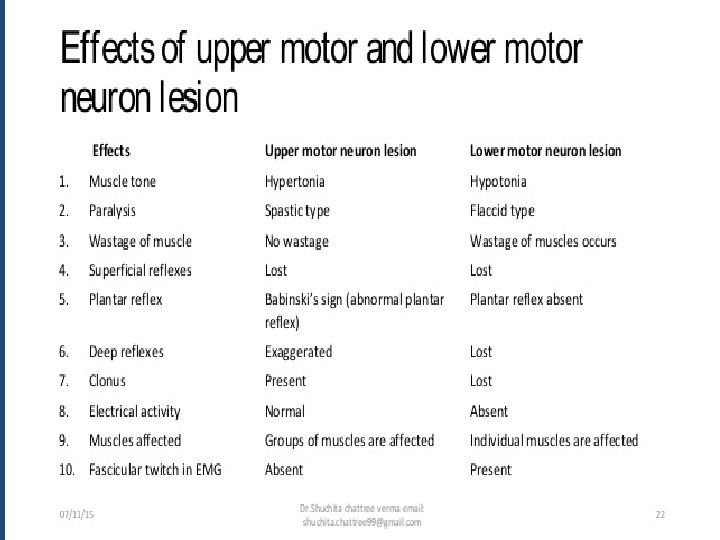
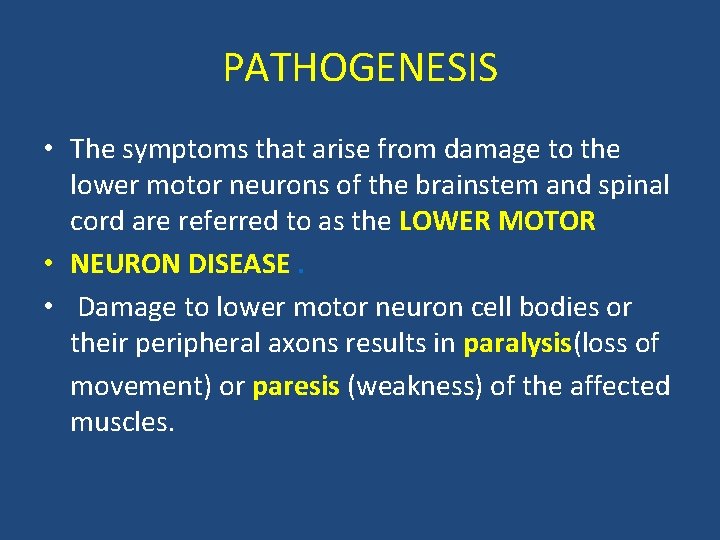
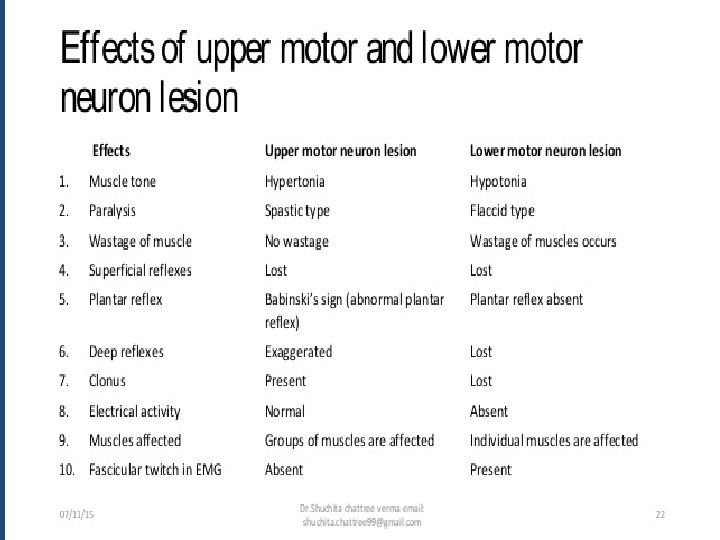
PATHOGENESIS • The symptoms that arise from damage to the lower motor neurons of the brainstem and spinal cord are referred to as the LOWER MOTOR • NEURON DISEASE. • Damage to lower motor neuron cell bodies or their peripheral axons results in paralysis(loss of movement) or paresis (weakness) of the affected muscles.
• In addition to paralysis or paresis , the lower motor neuron includes loss of reflexes (AREFLEXIA) due to interruption of the efferent (motor) limb of the sensory motor reflex arcs. Damage to lower motor neurons also entails a loss of muscle tone, since tone is in part dependent on the mono synaptic reflex arc that links the muscle spindles to the lower motor neurons.
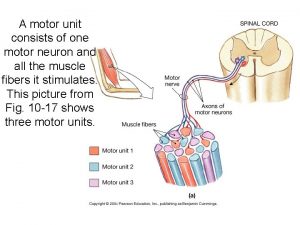
• A somewhat later effect is atrophy of the affected muscles due to denervation and disuse. The muscles involved may also exhibit fibrillations and fasciculations, which are spontaneous twitches characteristic of single denervated muscle fibers or motor units, respectively.
• These phenomena arise from changes in the excitability of denervated muscle fibers in the case of fibrillation, and from abnormal activity of injured α motor neurons in the case of fasciculations. These spontaneous contractions can be readily recognized in an electromyogram , providing an especially helpful clinical tool in diagnosing lower motor neuron disorders.
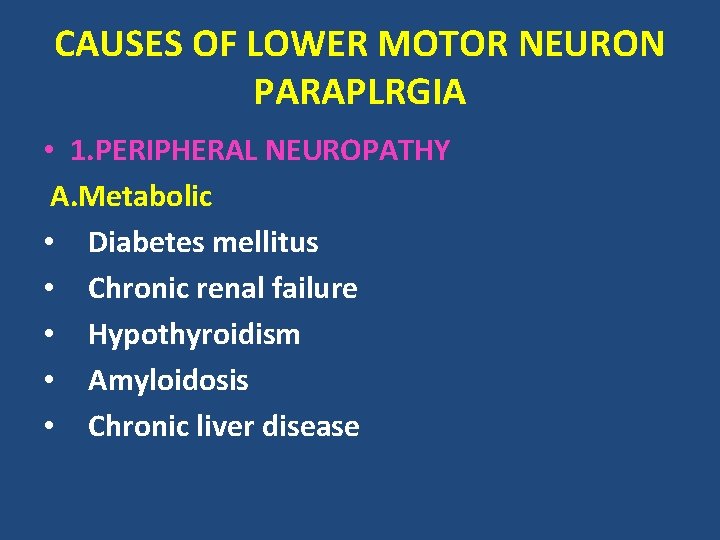
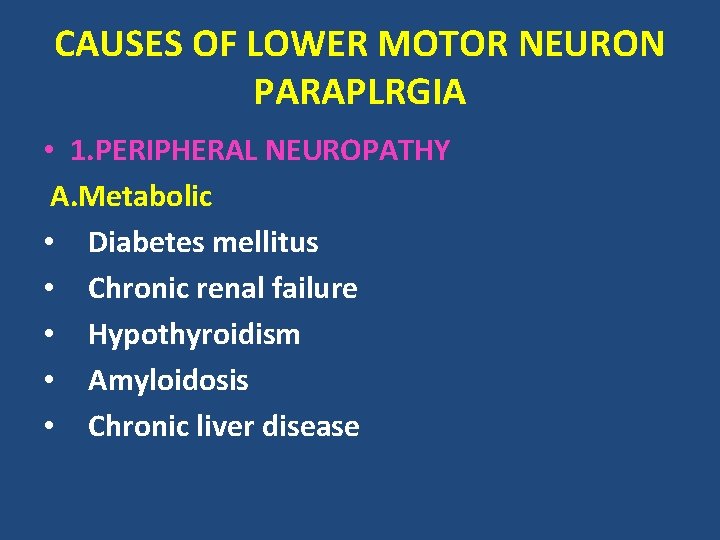
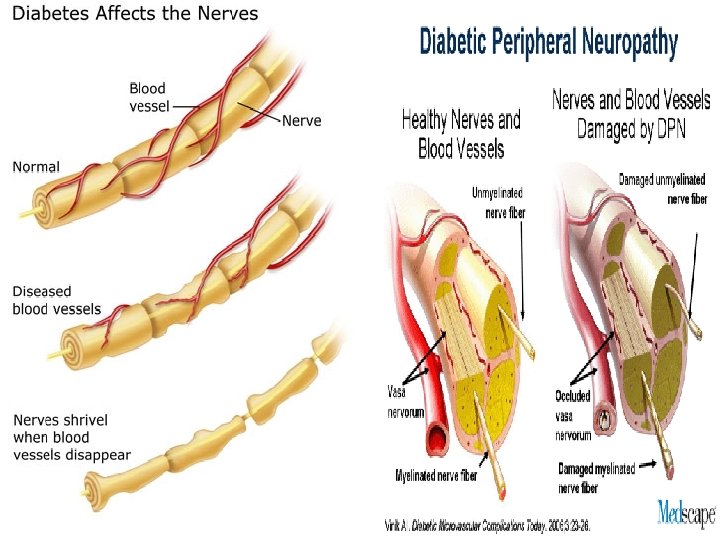
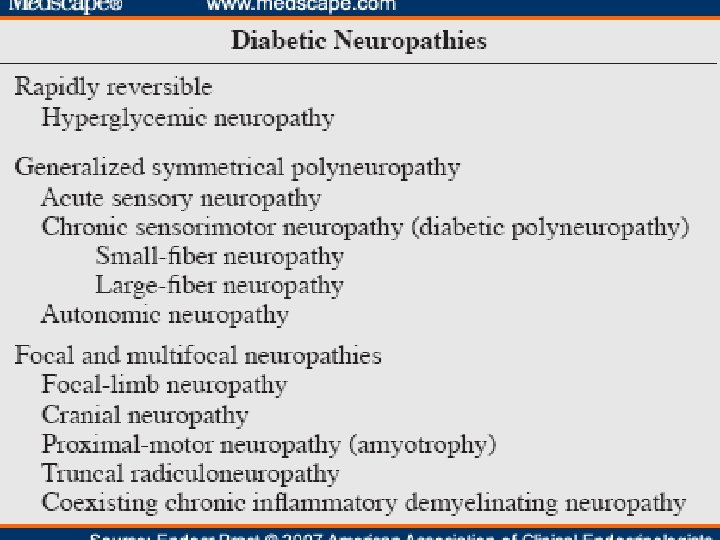
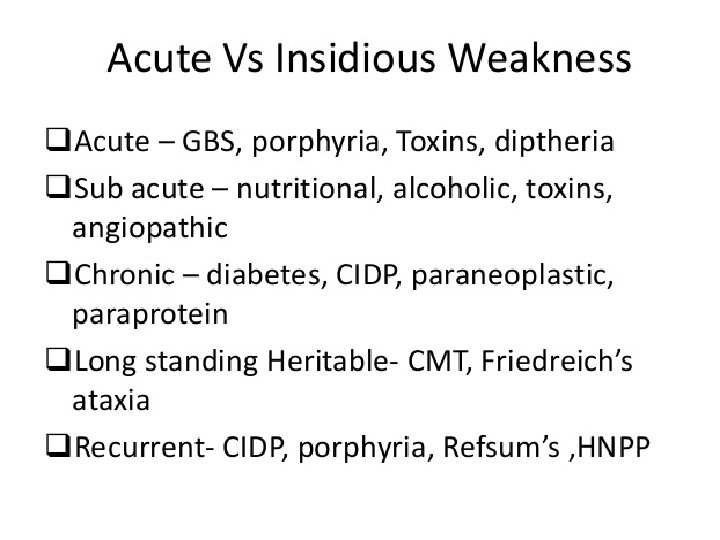
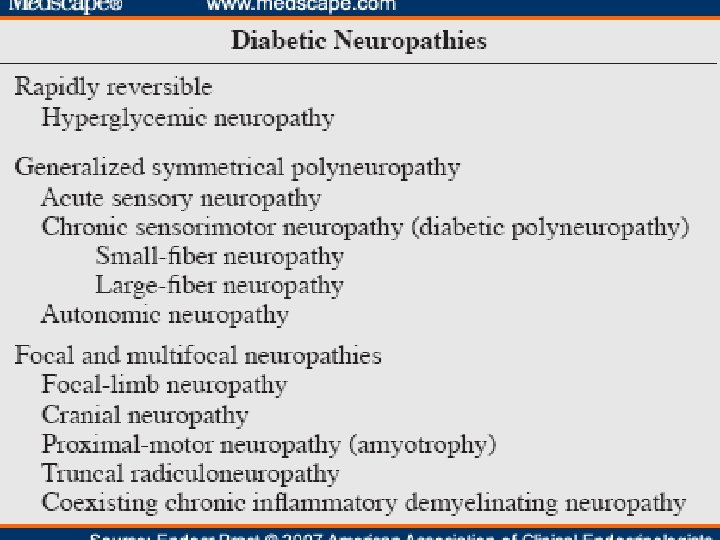
CAUSES OF LOWER MOTOR NEURON PARAPLRGIA • 1. PERIPHERAL NEUROPATHY A. Metabolic • Diabetes mellitus • Chronic renal failure • Hypothyroidism • Amyloidosis • Chronic liver disease
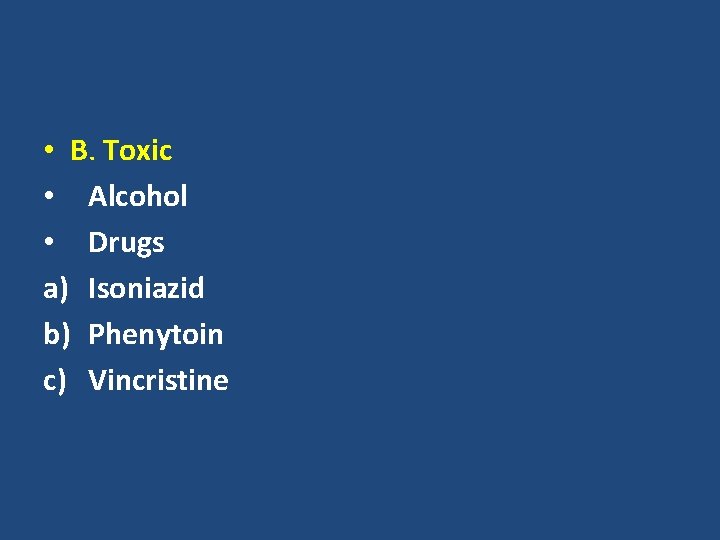
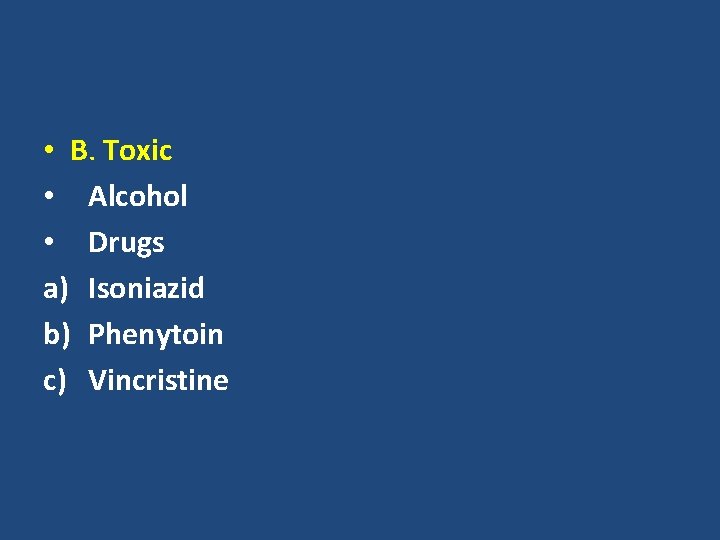
• B. Toxic • Alcohol • Drugs a) Isoniazid b) Phenytoin c) Vincristine
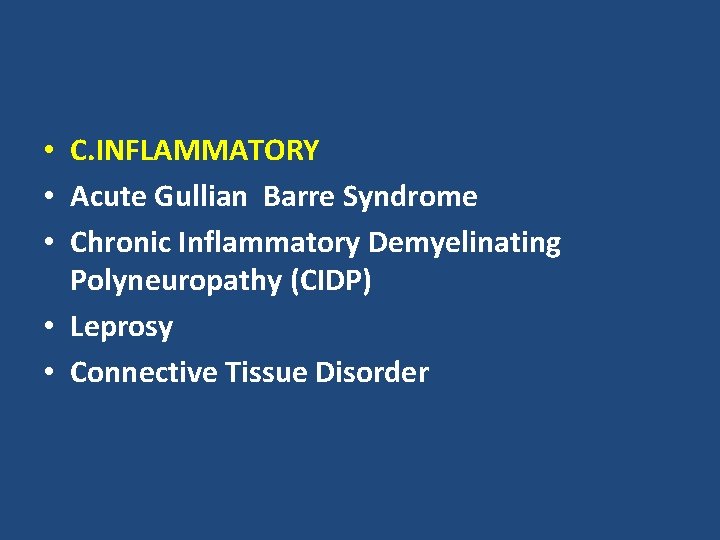
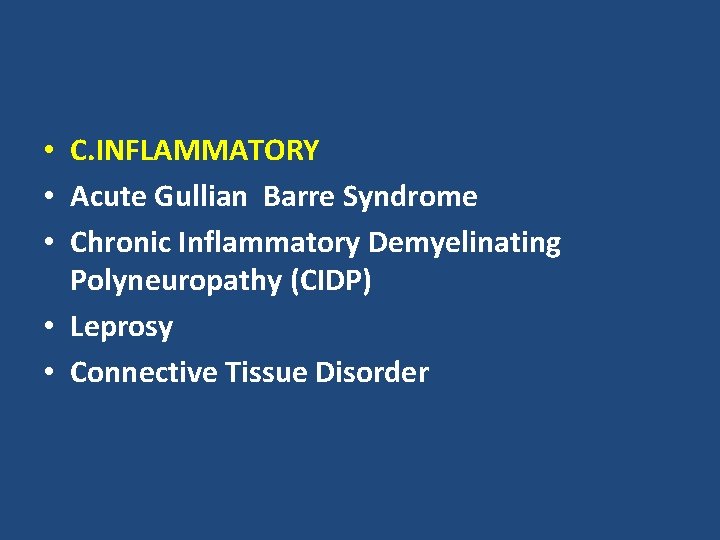
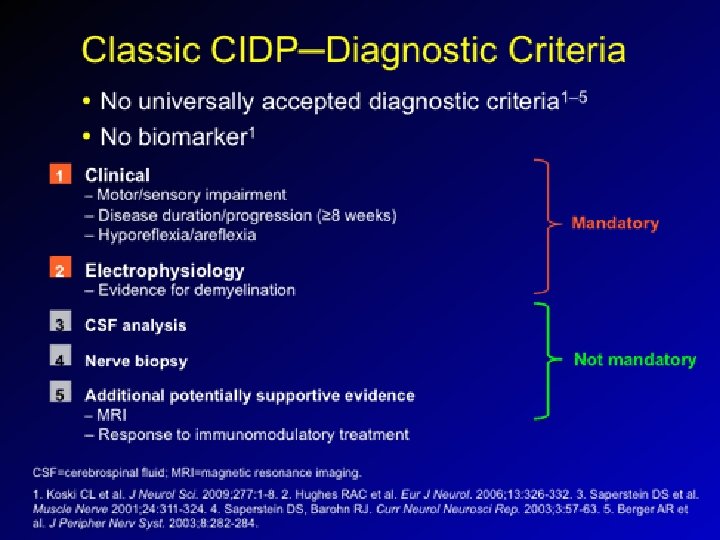
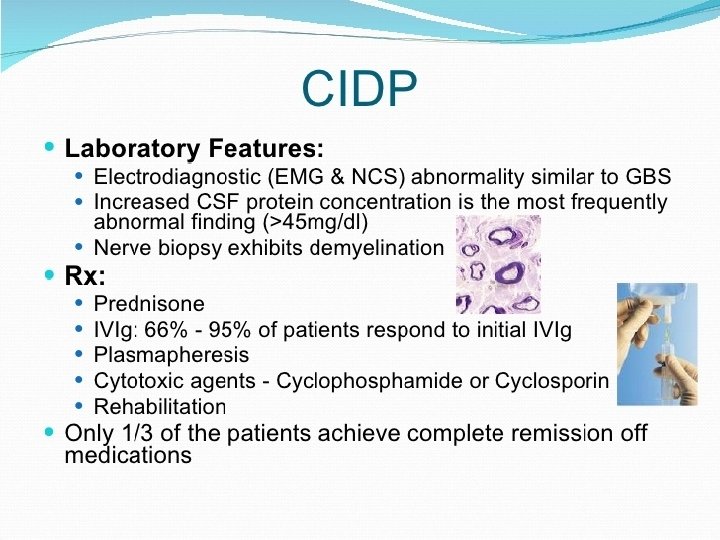
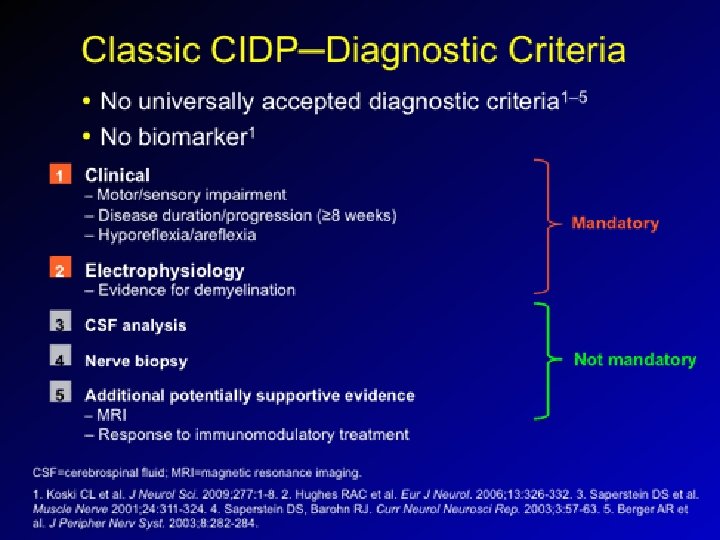
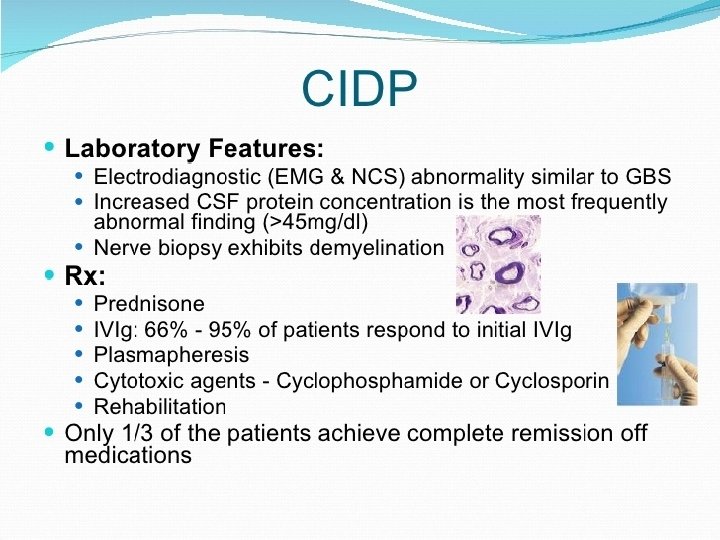
• C. INFLAMMATORY • Acute Gullian Barre Syndrome • Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) • Leprosy • Connective Tissue Disorder

D. GENETIC i. Hereditary Motor And Sensory Neuropthies E. DEFICIENCY DISEASES i. Thiamine Deficiency ii. Vitamin A Deficiency F. MISCELLANEOUS Malignancy
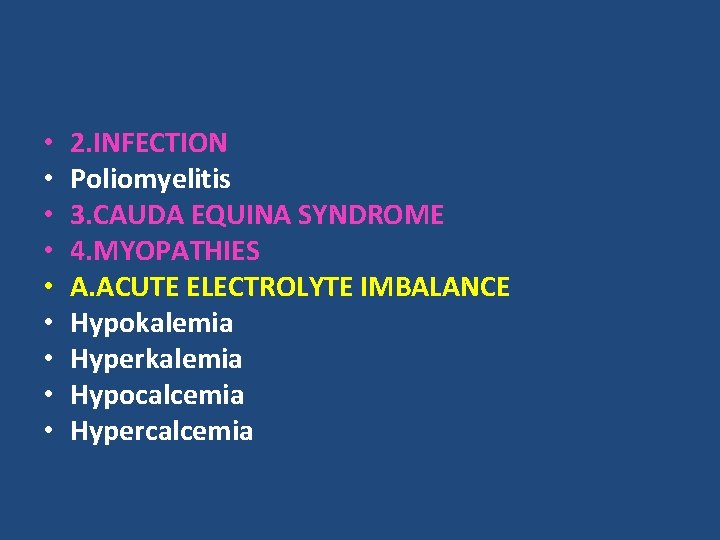
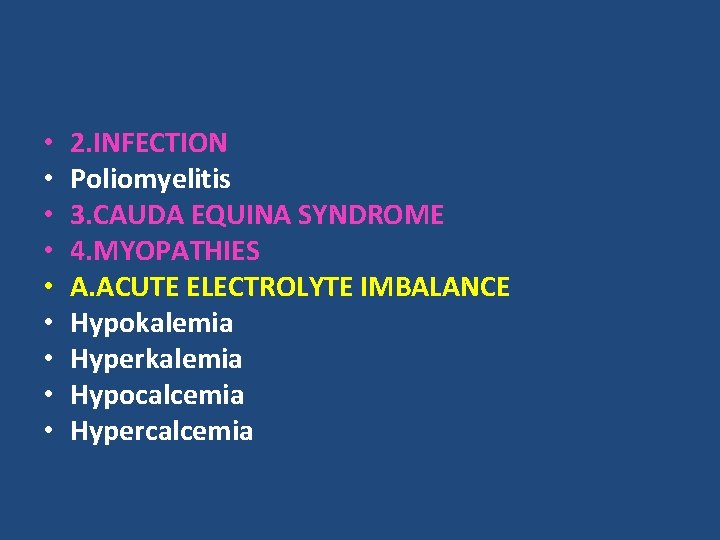
• • • 2. INFECTION Poliomyelitis 3. CAUDA EQUINA SYNDROME 4. MYOPATHIES A. ACUTE ELECTROLYTE IMBALANCE Hypokalemia Hyperkalemia Hypocalcemia Hypercalcemia
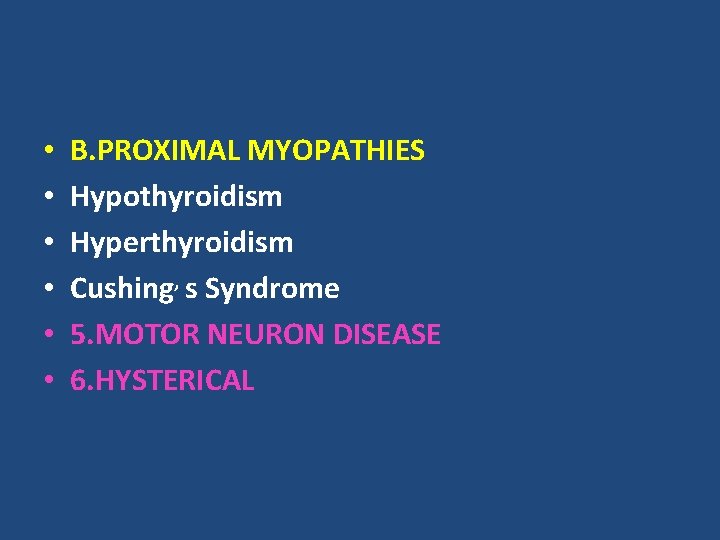
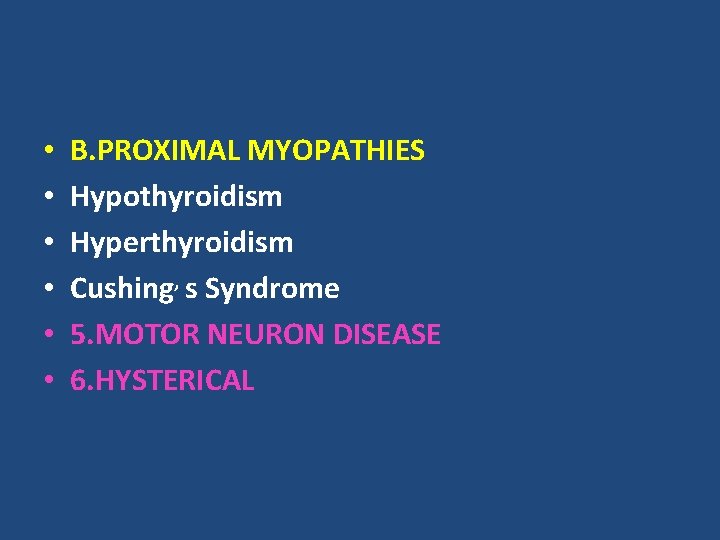
• • • B. PROXIMAL MYOPATHIES Hypothyroidism Hyperthyroidism Cushing, s Syndrome 5. MOTOR NEURON DISEASE 6. HYSTERICAL
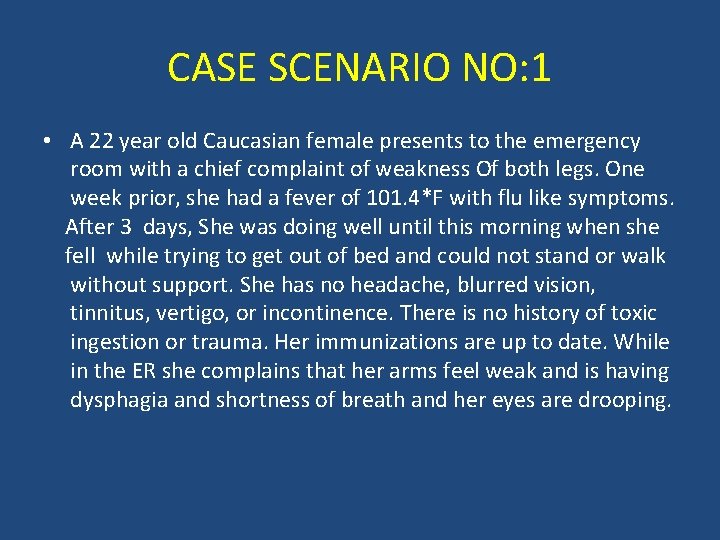
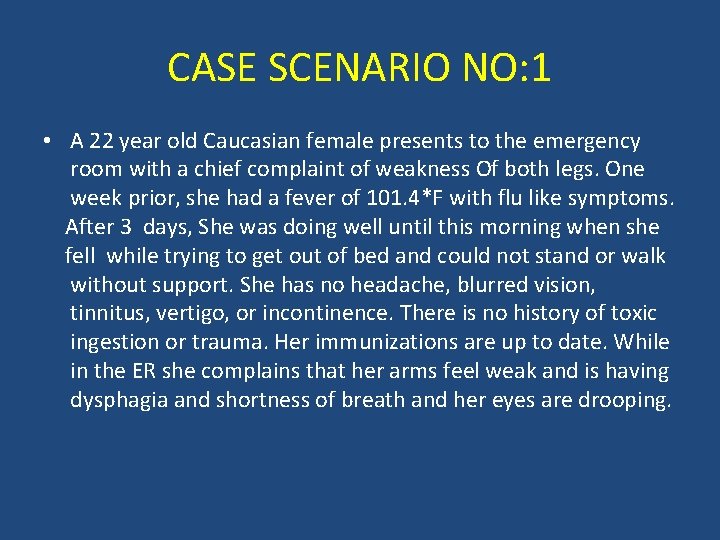
CASE SCENARIO NO: 1 • A 22 year old Caucasian female presents to the emergency room with a chief complaint of weakness Of both legs. One week prior, she had a fever of 101. 4*F with flu like symptoms. After 3 days, She was doing well until this morning when she fell while trying to get out of bed and could not stand or walk without support. She has no headache, blurred vision, tinnitus, vertigo, or incontinence. There is no history of toxic ingestion or trauma. Her immunizations are up to date. While in the ER she complains that her arms feel weak and is having dysphagia and shortness of breath and her eyes are drooping.
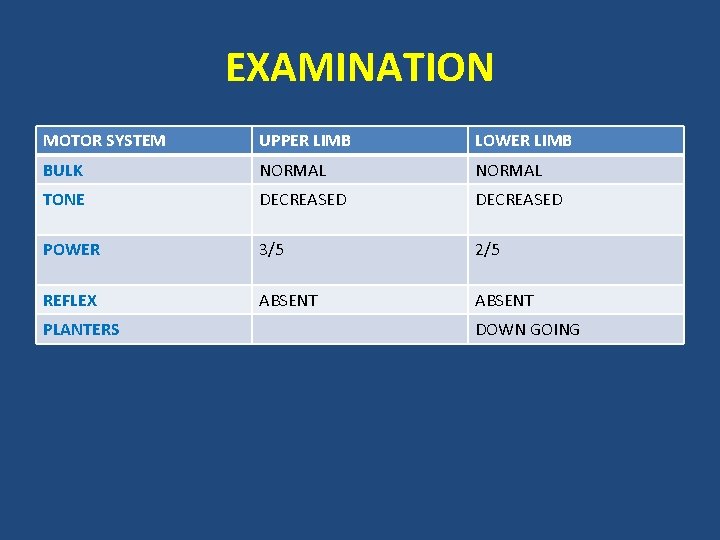
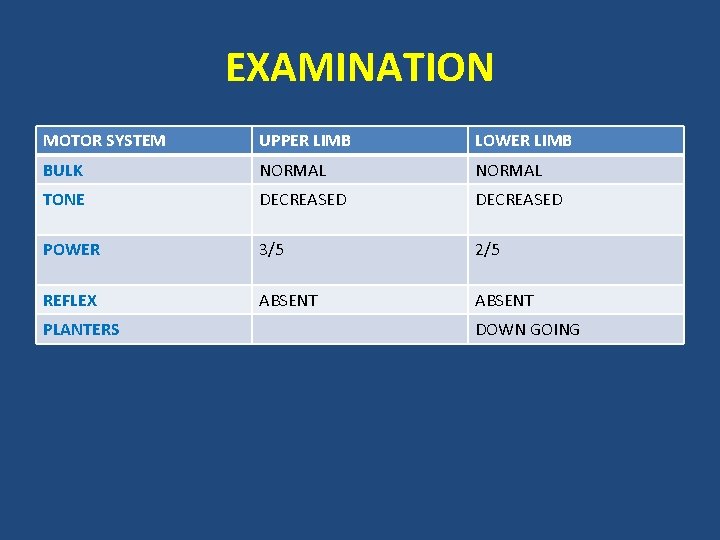
EXAMINATION MOTOR SYSTEM UPPER LIMB LOWER LIMB BULK NORMAL TONE DECREASED POWER 3/5 2/5 REFLEX ABSENT PLANTERS DOWN GOING
• SENSORY SYSTEM : Intact • CEREBELLAR SYSTEM : Intact • CRANIAL NERVES : Bilateral 7 th Nerve Palsy
• WHAT IS THE DIAGNOSIS ?
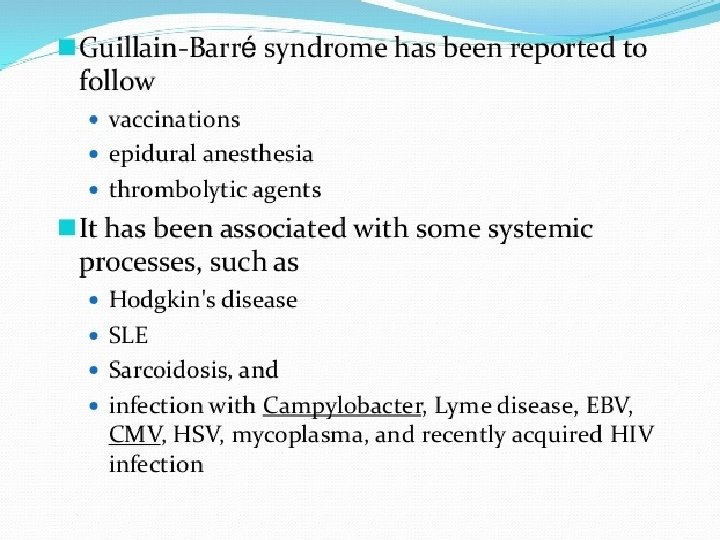
WHAT IS GULLAIN BARRE SYNDROME • Guillain- Barre syndrome (GBS) is an acute demyelinating polyneuropathy of the peripheral nervous system characterized by progressive flaccid paralysis. It is an acquired disorder that affects people of all ages, although only rarely in children under one year of age. It has a slight male predominance of 1. 5 to 1 and has an estimated annual incidence rate of 1/100, 000.
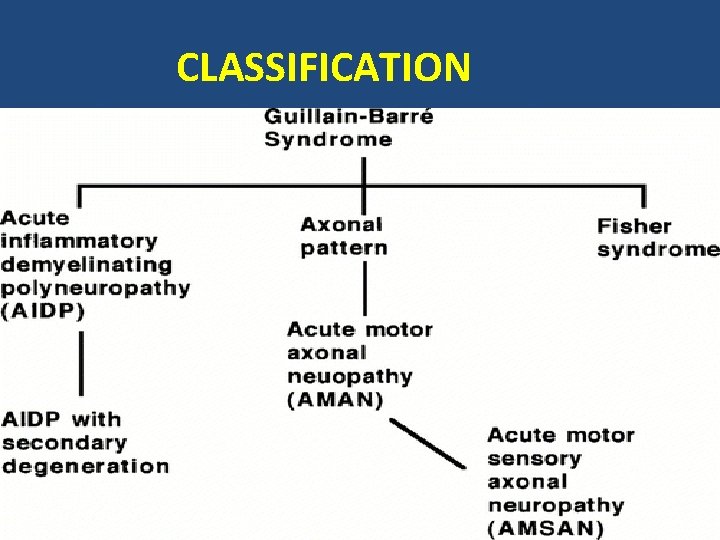
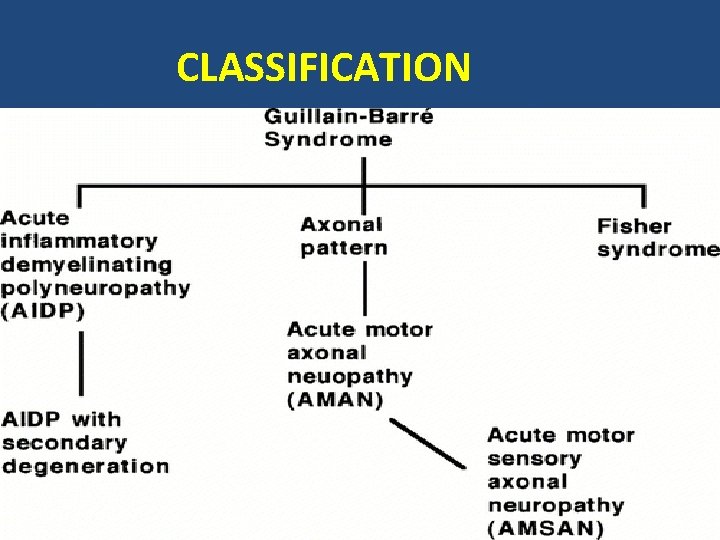
CLASSIFICATION
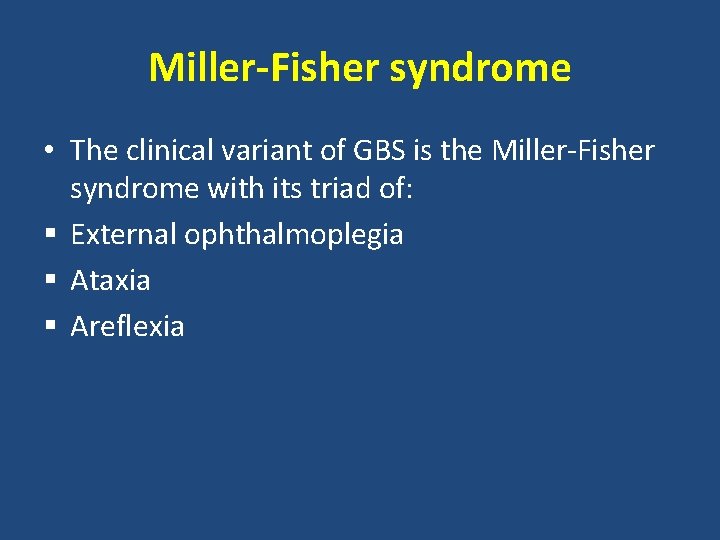
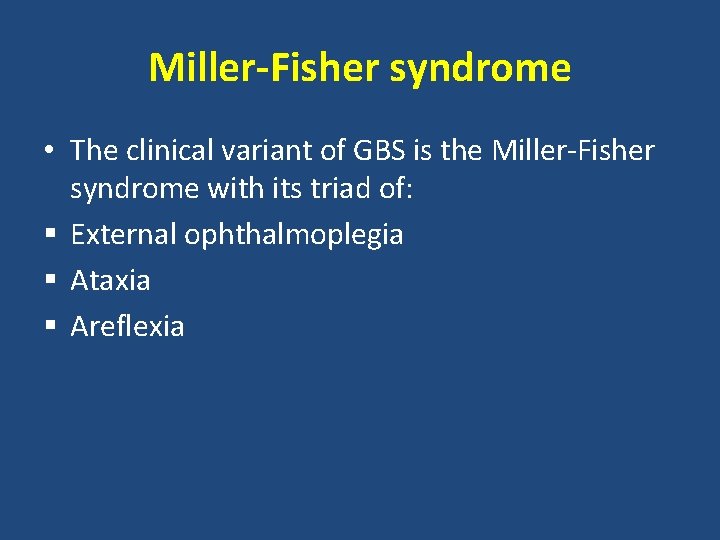
Miller-Fisher syndrome • The clinical variant of GBS is the Miller-Fisher syndrome with its triad of: § External ophthalmoplegia § Ataxia § Areflexia
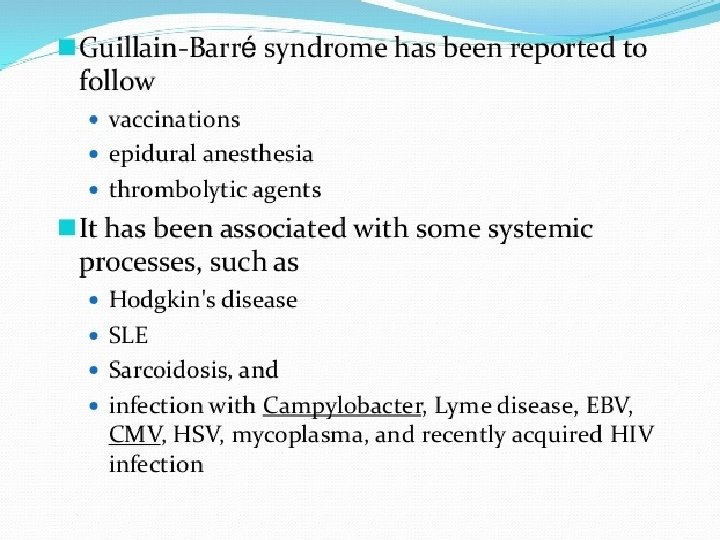
PATHOGENESIS • Current research suggests that ANTI GANGIOSIDE ANTIBODIES play an important role in the pathogenesis of GBS. Gangliosides are glycolipids containing sialic acid residues and are the surface components of many cells, including nerve cells. Many patients with GBS have antibodies to various gangliosides such as GM 1, GD 1 a, GD 1 b, and GQ 1 b.
INVESTIGATIONS 1. BLOOD COMPLETE EXAMINATION & ESR 2. BLOOD CULTURE 3. LUMBAR PUNCTURE § Elevated protein level § Normal cell counts § Glucose level normal § Culture negative
4. ELECTRODIAGNOSTIC STUDIES: Nerve conduction: studies reveal slowing in both motor and sensory nerves.
• Electromyography (EMG) • May show acute denervation of muscle.
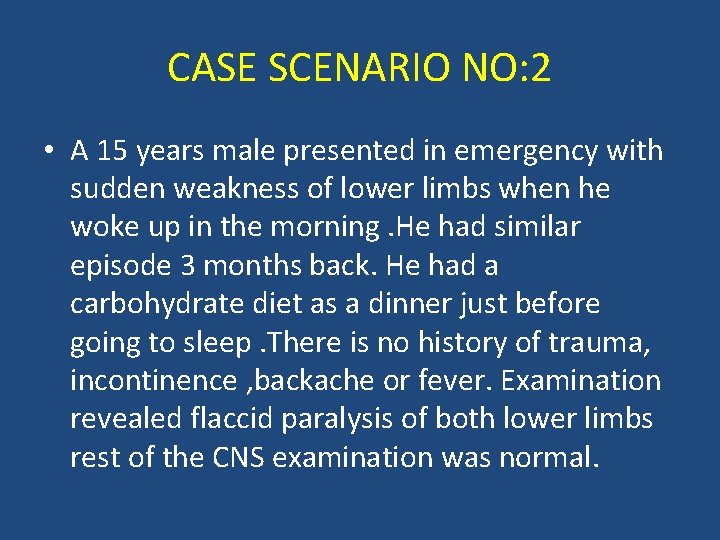
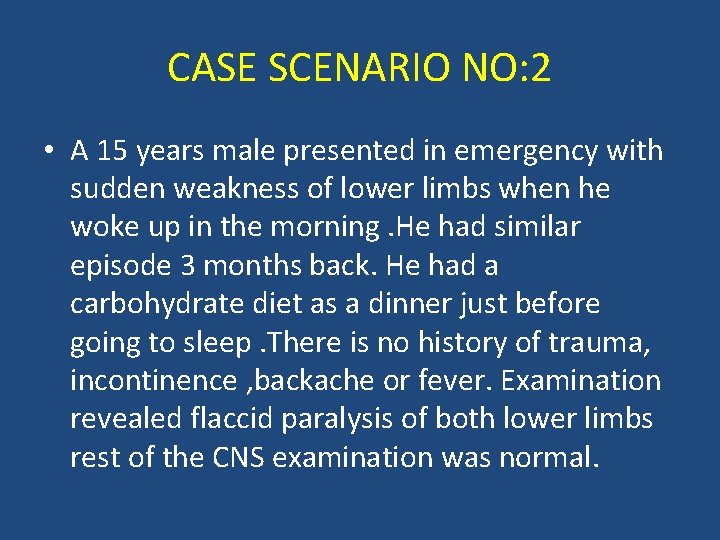
CASE SCENARIO NO: 2 • A 15 years male presented in emergency with sudden weakness of lower limbs when he woke up in the morning. He had similar episode 3 months back. He had a carbohydrate diet as a dinner just before going to sleep. There is no history of trauma, incontinence , backache or fever. Examination revealed flaccid paralysis of both lower limbs rest of the CNS examination was normal.
• What is the likely diagnosis?
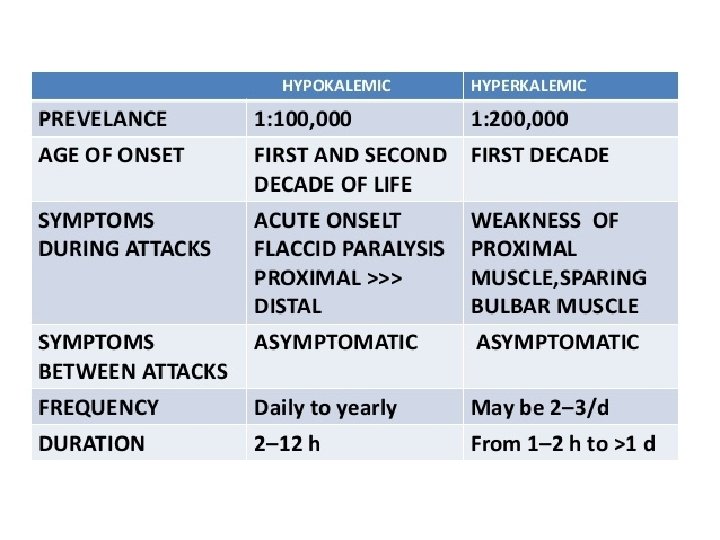
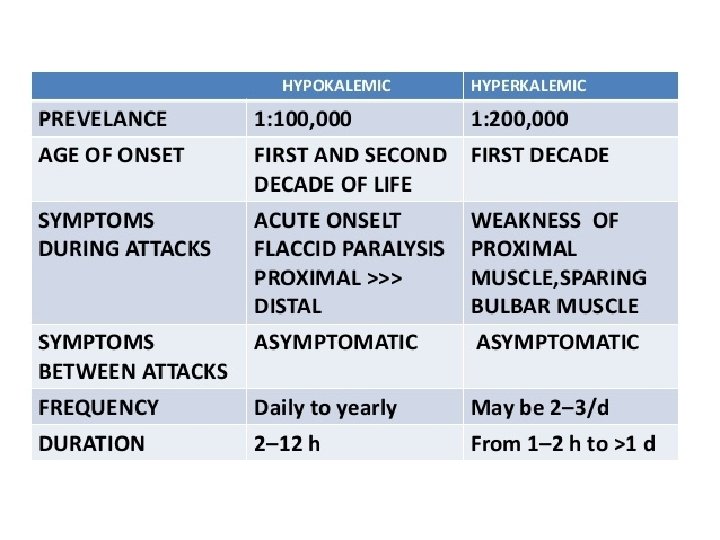
• HYPOKALEMIC PERIODIC PARALYSIS • HYPERKALEMIC PERIODIC PARALYSIS • NORMOKALEMIC PERIODIC PARALYSIS
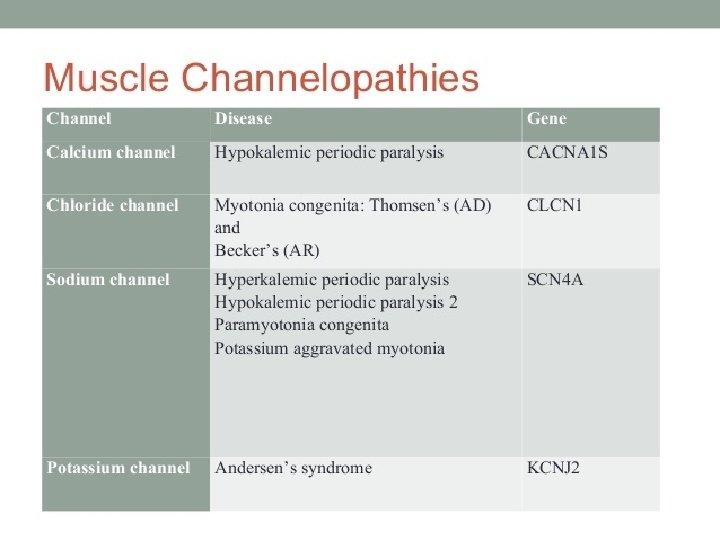
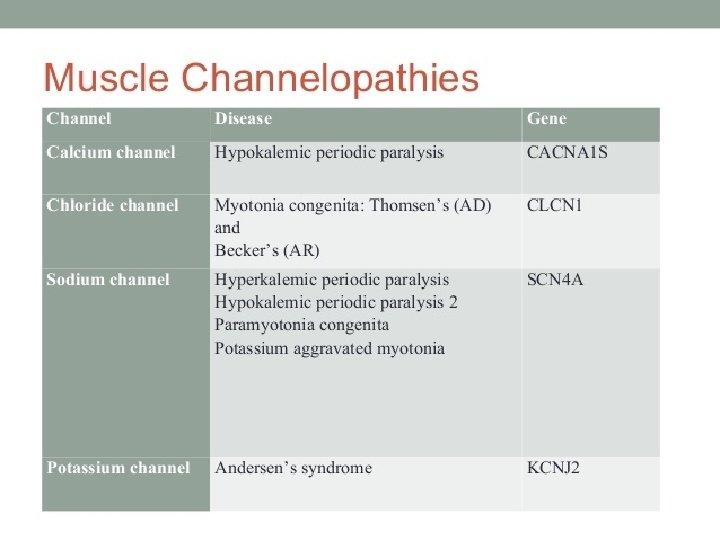
• HYPOKALEMIC PERIODIC PARALYSIS: • Periodic paralysis may have a familial (dominant inheritance)basis. The syndromes to be described are channelopathies that manifest as abnormal, often potassium-sensitive, muscle-membrane excitability and lead clinically to episodes of flaccid weakness or paralysis, sometimes in association with abnormalities of the plasma potassium level.
PATHOGENESIS • Hypokalemic periodic paralysis has been • related to mutations in the CACNL 1 A 3, SCN 4 A, or KCNE 3(11 q 13 -q 14) gene.
CLINICAL FEATURES • It is characterized by attacks that tend to occur on awakening, after exercise, or after a heavy meal and may last for several days. It may be associated with thyroid disorders.
INVESTIGATIONS Serum potassium level Thyroid function test. Electro diagnostic studies : Nerve Conduction Studies There is reduced motor amplitude during the attack and normal in between the attacks. • Electromyography (EMG) • Often demonstrate myotonic discharges during the attack. • • •
• MUSCLE BIOPSY : • It shows vacuoles that are smaller, less numerous and more peripherally placed.
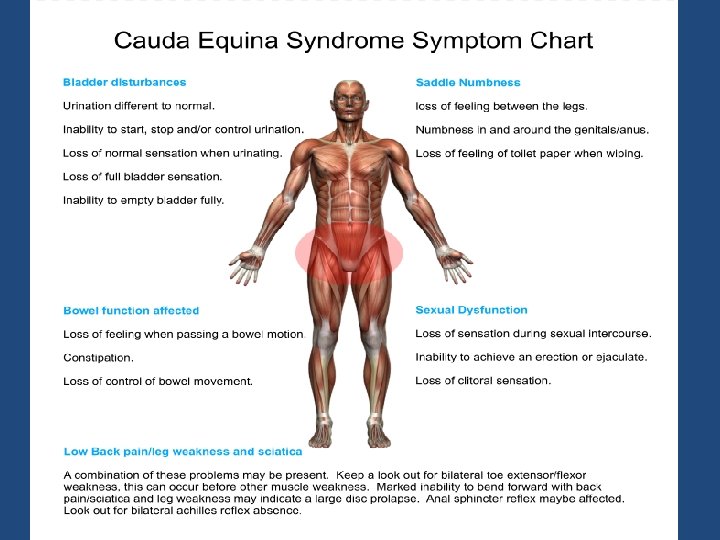
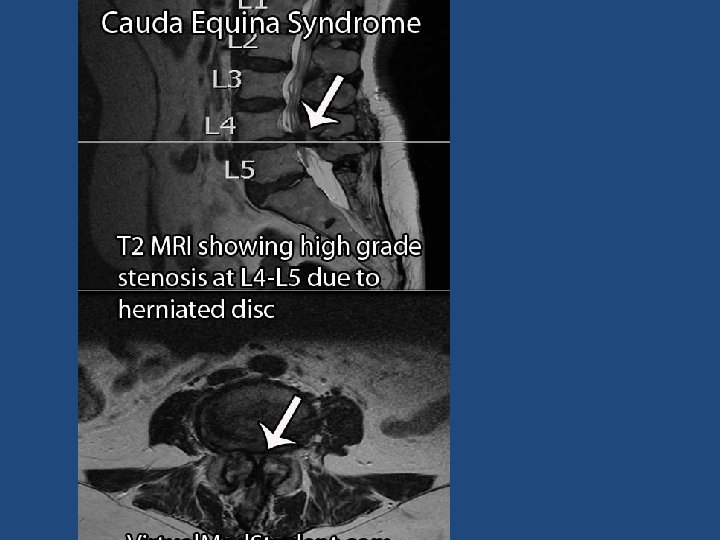
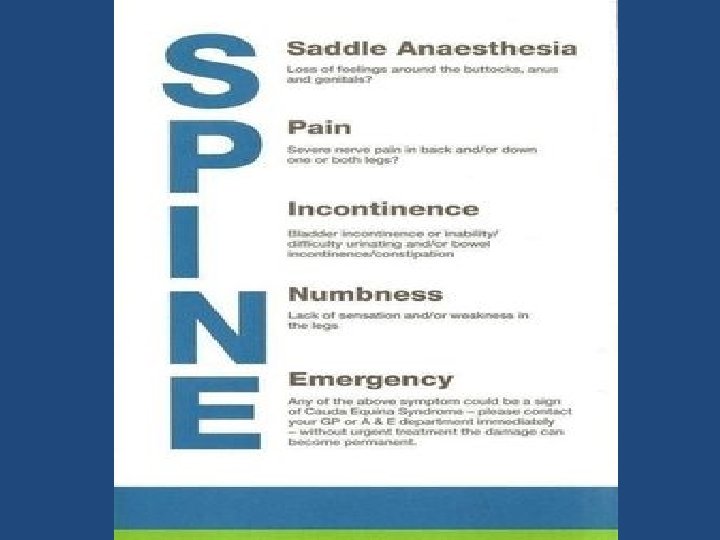
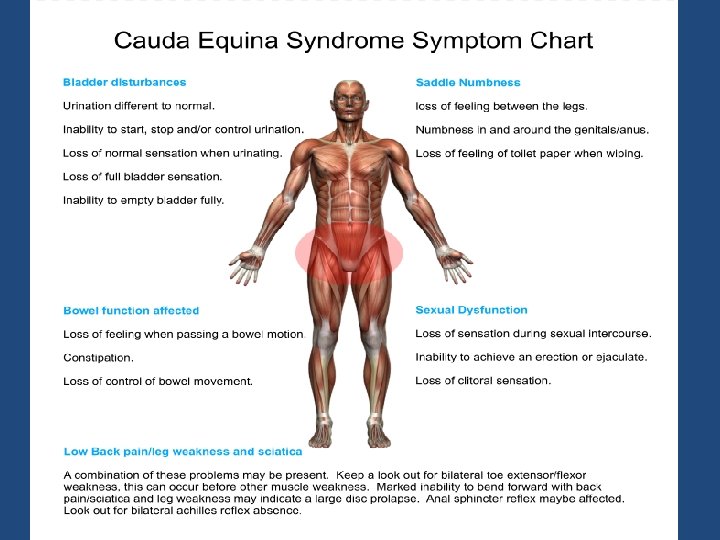
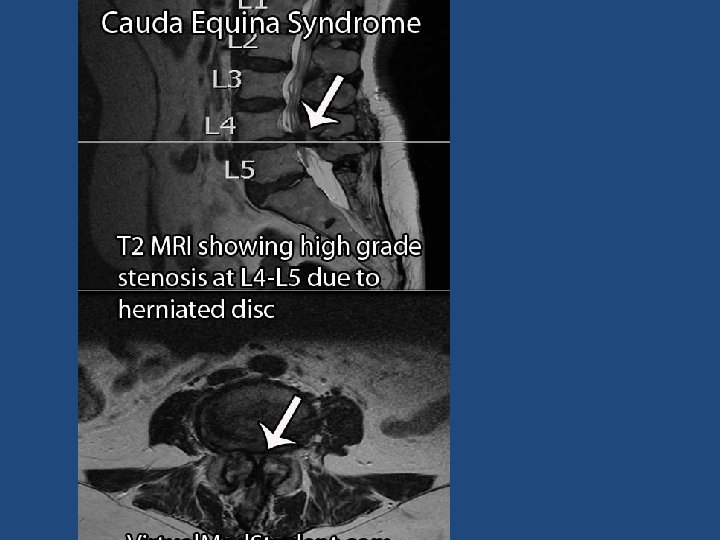
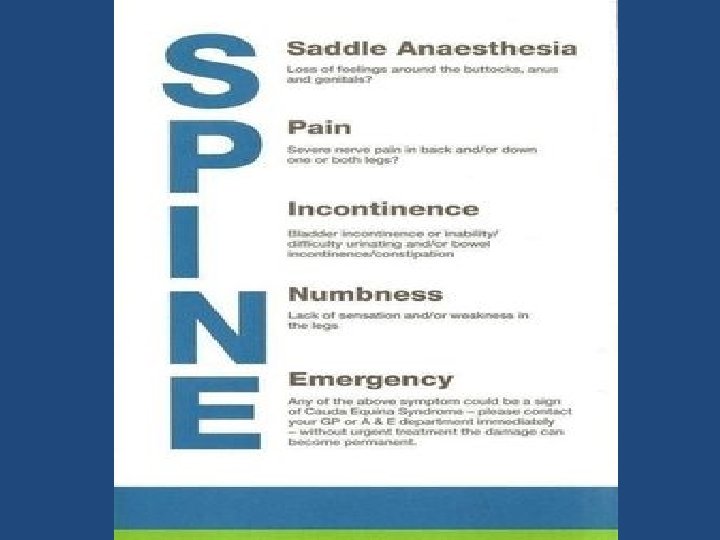
CASE SCENARIO NO: 3 • A 60 Years school teacher had complaints of pain in both thighs radiating to the perineum while walking for few months. This pain is relieved by resting or bending forward. Now presented with weakness of both lower limbs , perianal numbness with bowel and bladder incontinence. Examination revealed wasting of quadriceps, weakness of foot inverters, absent ankle and knee jerk with down going planters and saddle anesthesia. • WHAT IS THE LIKELY DIAGNOSIS?
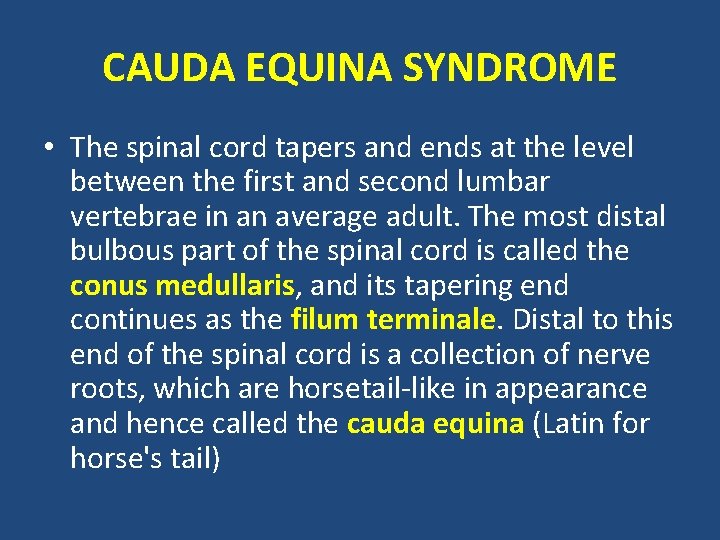
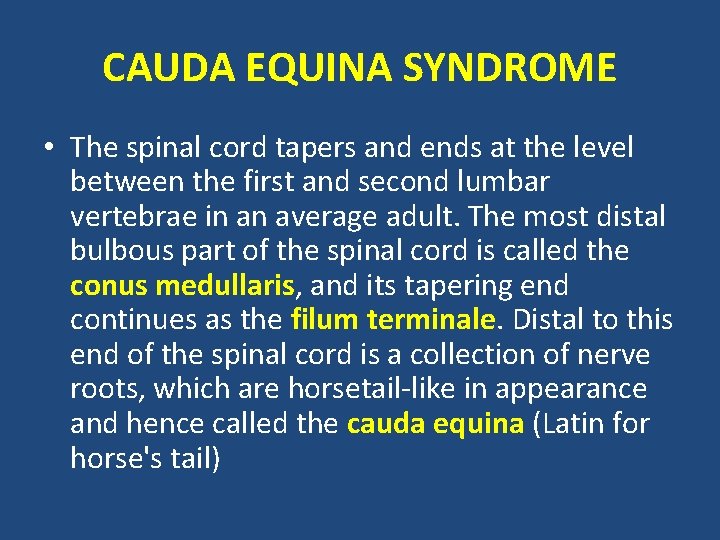
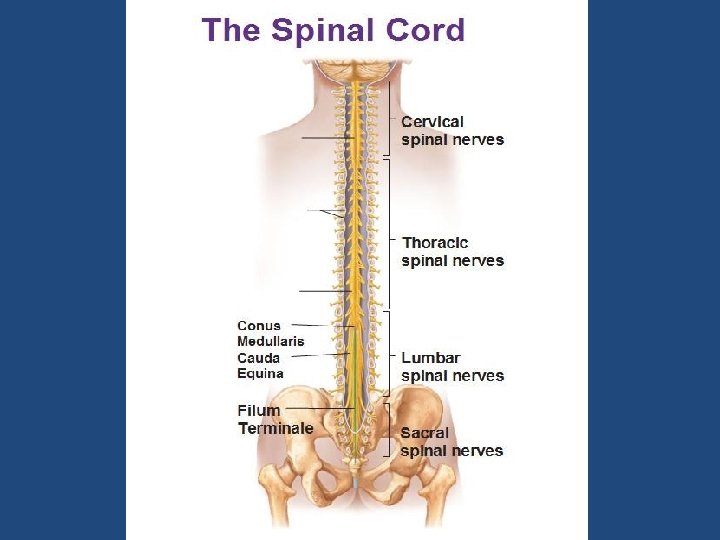
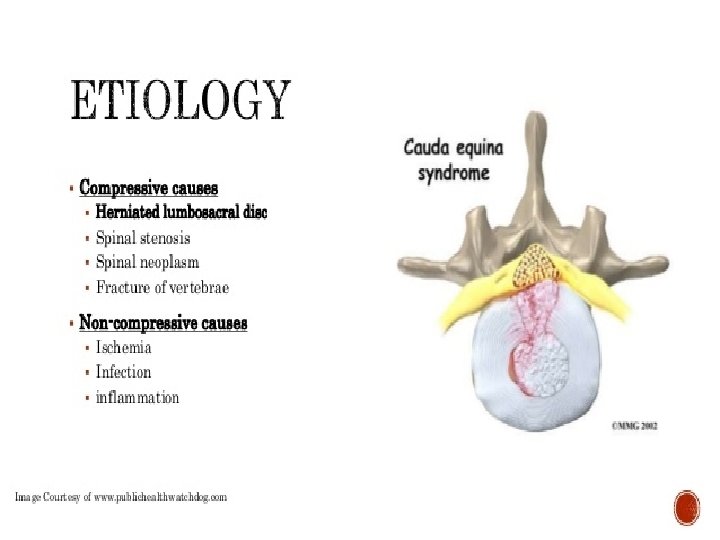
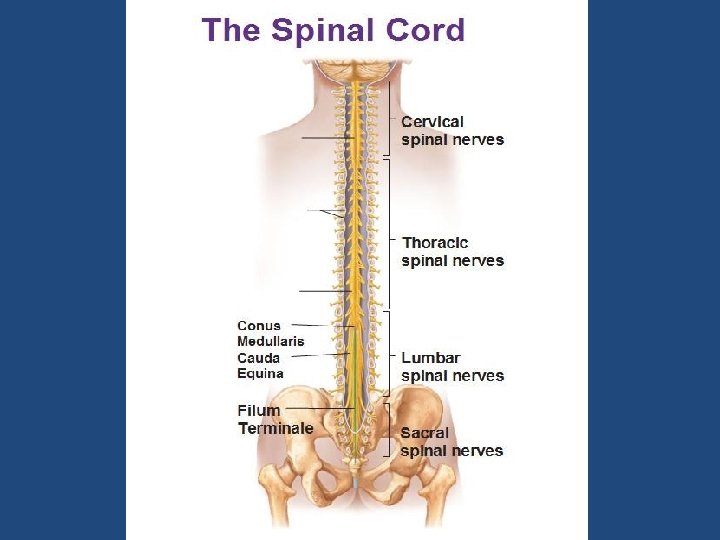
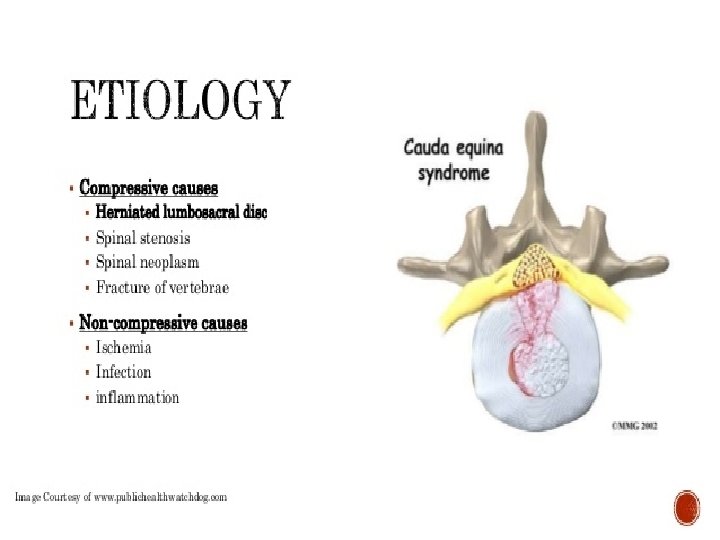
CAUDA EQUINA SYNDROME • The spinal cord tapers and ends at the level between the first and second lumbar vertebrae in an average adult. The most distal bulbous part of the spinal cord is called the conus medullaris, and its tapering end continues as the filum terminale. Distal to this end of the spinal cord is a collection of nerve roots, which are horsetail-like in appearance and hence called the cauda equina (Latin for horse's tail)
INVESTIGATIONS • • Plain Radiographs Lumbo sacral spine Myelography Computed tomography MRI
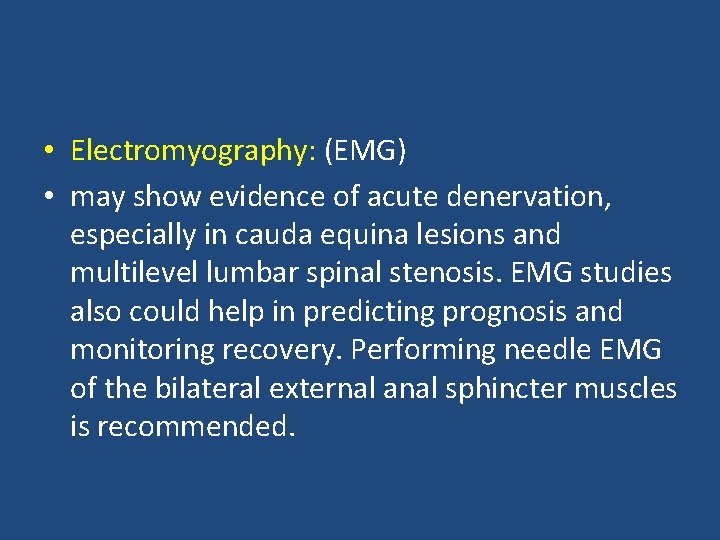
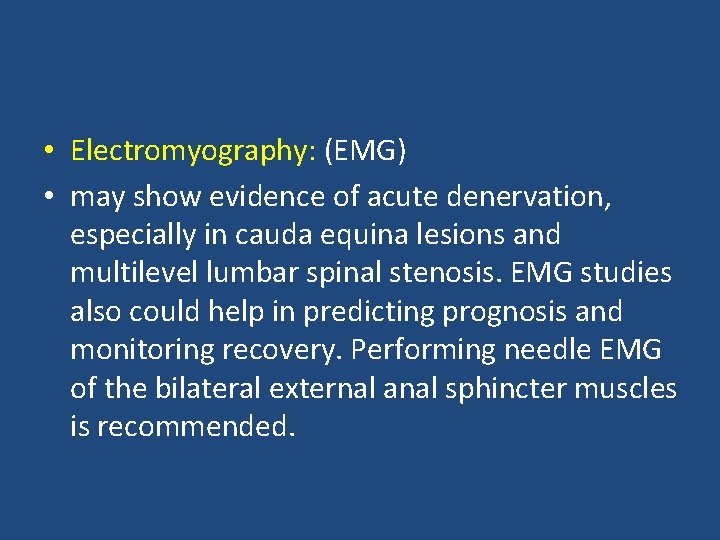
• Electromyography: (EMG) • may show evidence of acute denervation, especially in cauda equina lesions and multilevel lumbar spinal stenosis. EMG studies also could help in predicting prognosis and monitoring recovery. Performing needle EMG of the bilateral external anal sphincter muscles is recommended.
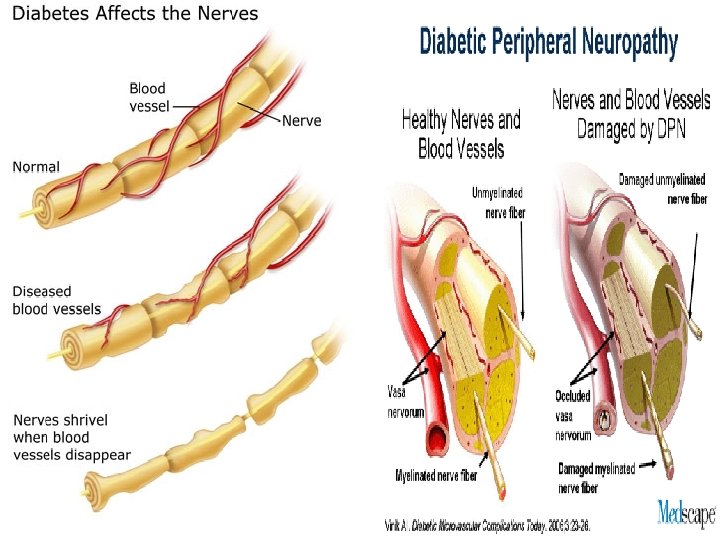
CASE SCENARIO NO. 4 • A 65 years female known diabetic for the last 25 years with poor control of diabetes had complaints of numbness of both hands and feet for many months now for the last few days is unable to walk. On examination there is flaccid paraparesis with glove and stocking pattern of sensory impairment. • WHAT IS THE DIAGNOSIS?
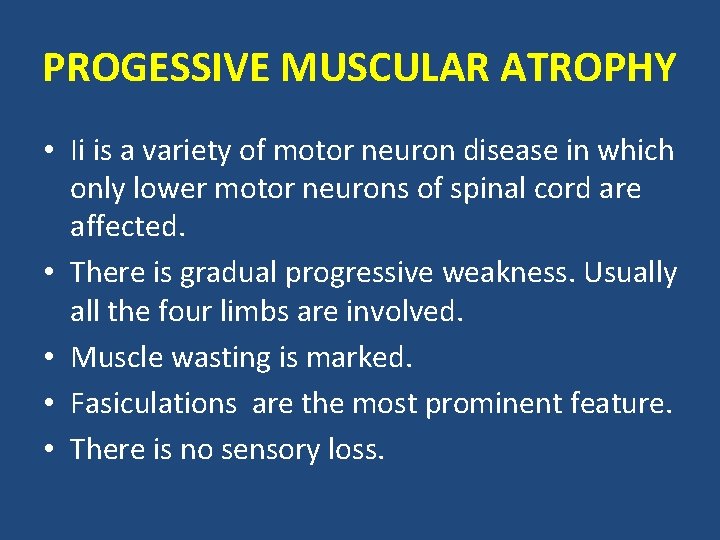
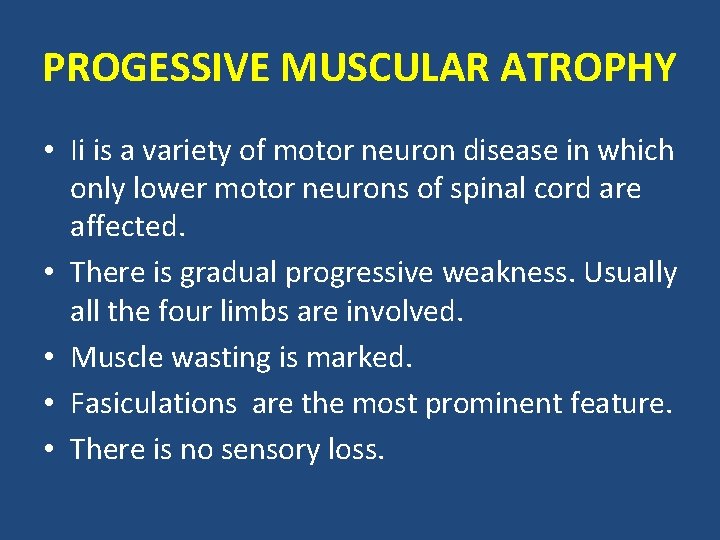
PROGESSIVE MUSCULAR ATROPHY • Ii is a variety of motor neuron disease in which only lower motor neurons of spinal cord are affected. • There is gradual progressive weakness. Usually all the four limbs are involved. • Muscle wasting is marked. • Fasiculations are the most prominent feature. • There is no sensory loss.
ACUTE INTERMITTENT PORPYRIA • The sequence of events in attacks of acute intermittent porphyria (AIP) usually is as follows: • Abdominal pain • Psychiatric symptoms • Peripheral neuropathies, mainly motor neuropathies.

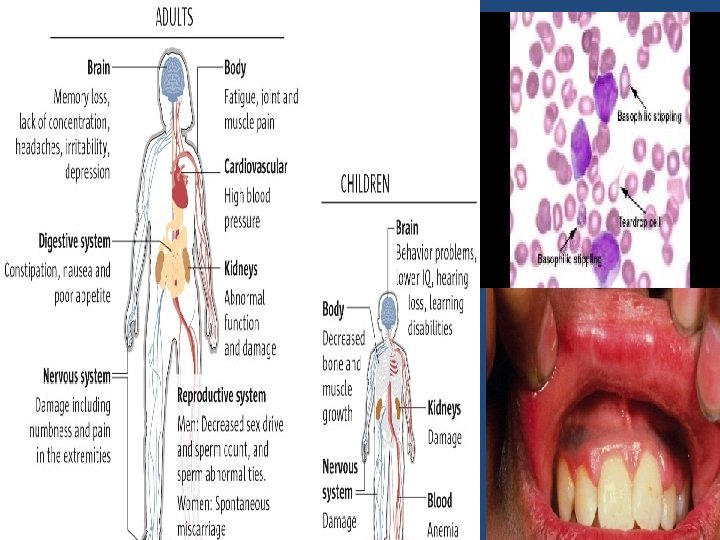
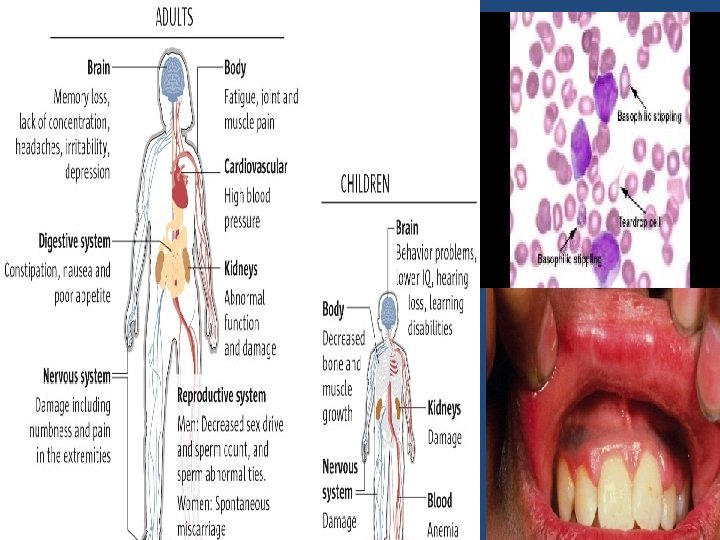
LEAD POISONING • Central nervous system and neuromuscular symptoms usually result from intense exposure, over longer periods. Signs of chronic exposure include • loss of short term memory or concentration, • nausea & abdominal pain • loss of coordination • numbness, tingling in the extremities • lower motor neuron paraparesis • problems with sleep • headaches • stupor • slurred speech • Anemia • A blue line along the gum with bluish black edging to the teeth, known as BURTON LINE is another indication of chronic lead poisoning.
HYSTERICAL • Weakness is variable. • Social history is suggestive of underlying psychiatric problem. • There is anesthesia in a distribution which is not possible due to organic lesion. • Reflexes are normal.

 Lower motor neuron
Lower motor neuron Zapojenie alternatora
Zapojenie alternatora Paraplrgia
Paraplrgia Central causes of paraplegia
Central causes of paraplegia Somministrazione intratecale
Somministrazione intratecale Pott's paraplegia
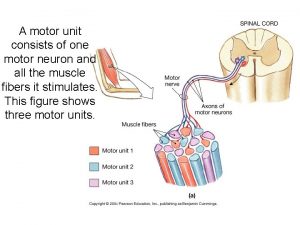
Pott's paraplegia A motor unit consits of
A motor unit consits of Site of somatic motor neuron cell bodies
Site of somatic motor neuron cell bodies Motor neuron
Motor neuron Motor (efferent) division
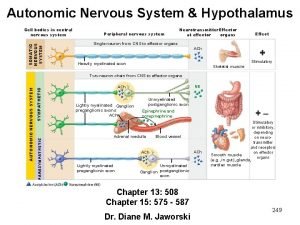
Motor (efferent) division Postasthmatic
Postasthmatic Internal capsule homunculus
Internal capsule homunculus Equine motor neuron disease
Equine motor neuron disease Saliva parasympathetic nervous system
Saliva parasympathetic nervous system Motor neuron adalah
Motor neuron adalah Somatic motor neuron
Somatic motor neuron Somatic vs autonomic nervous system
Somatic vs autonomic nervous system Somatic motor pathway
Somatic motor pathway Site of somatic motor neuron cell bodies
Site of somatic motor neuron cell bodies Motor neuron adalah
Motor neuron adalah Lhermitte sign
Lhermitte sign Chart
Chart Motor parts name
Motor parts name Ee 216
Ee 216 Pony motor starting method
Pony motor starting method Synchronous motor hunting
Synchronous motor hunting Fauziah othman
Fauziah othman Relative refractory period
Relative refractory period Neuron definition
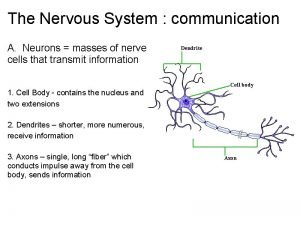
Neuron definition Merkel cells
Merkel cells A neuron without terminal buttons would be unable to
A neuron without terminal buttons would be unable to Vanat
Vanat Postsynaptic neuron
Postsynaptic neuron Cerebeluum
Cerebeluum Neuron sterilizer
Neuron sterilizer Neuron anatomy
Neuron anatomy Neuron n
Neuron n Postsynaptic potential
Postsynaptic potential All or none principle of action potential
All or none principle of action potential Bipolar neuron function
Bipolar neuron function Parts of a neuron
Parts of a neuron Objectives of nervous system
Objectives of nervous system Neuronal pool
Neuronal pool First second and third order neurons
First second and third order neurons Mirror neuron
Mirror neuron Halle berry neuron
Halle berry neuron Figure 12-1 the neuron
Figure 12-1 the neuron Impulsgeleiding neuron
Impulsgeleiding neuron What is multipolar neuron
What is multipolar neuron Neuron diagram
Neuron diagram Anatomy of a synapse
Anatomy of a synapse A neuron without terminal buttons would be unable to
A neuron without terminal buttons would be unable to Reflex
Reflex Quizlet
Quizlet Neuron cell body
Neuron cell body Mirror neuron
Mirror neuron Saraf kranium
Saraf kranium Structure of a typical synapse
Structure of a typical synapse Neuron
Neuron Bipolar neuron function
Bipolar neuron function Oligodendrocyt
Oligodendrocyt Neuron synapse
Neuron synapse Neuronal pools
Neuronal pools Neuron and neuroglial cells
Neuron and neuroglial cells Jaringan
Jaringan Histology of cns ppt
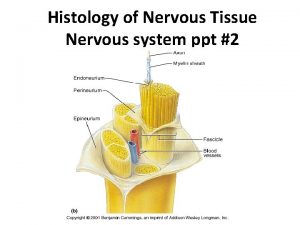
Histology of cns ppt Multipolární neuron
Multipolární neuron Neuron anatomy
Neuron anatomy Unipolar neuron
Unipolar neuron Saraf sensorik
Saraf sensorik