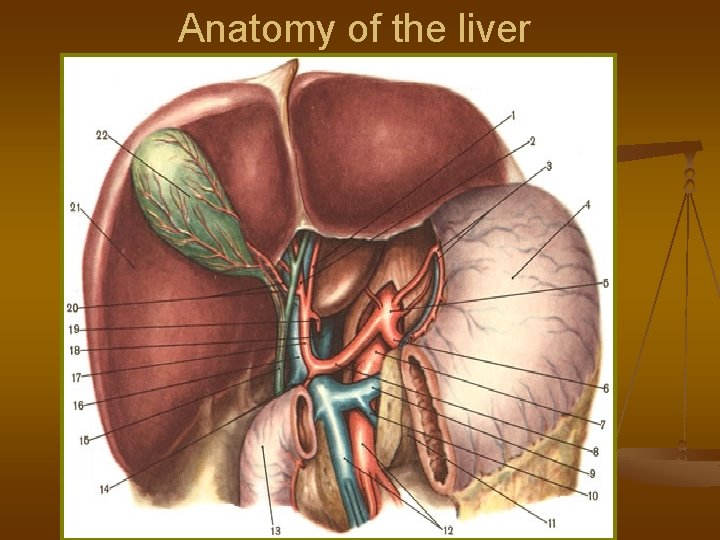
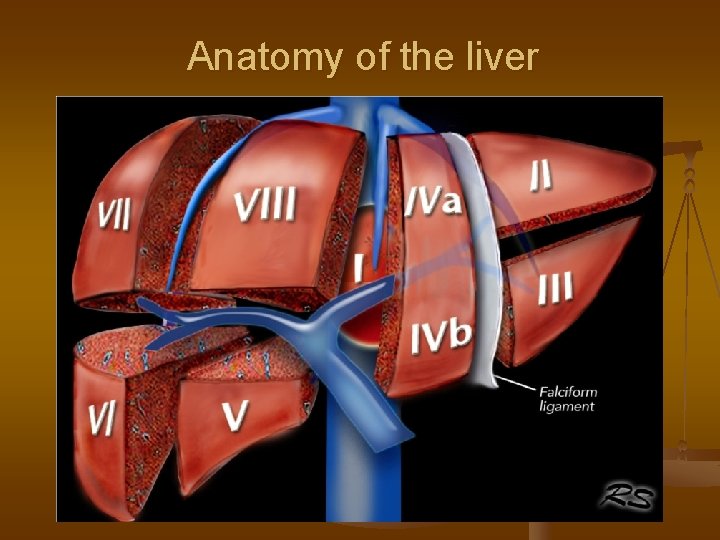
Anatomy of the liver Anatomy of the liver








- Slides: 71
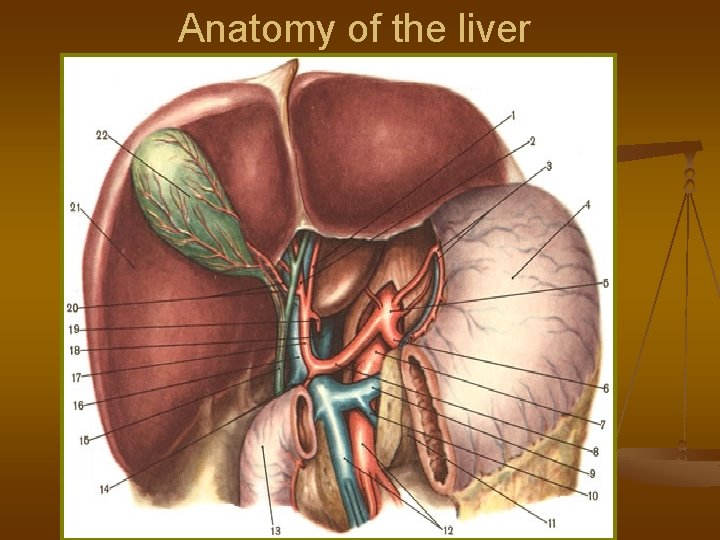
Anatomy of the liver
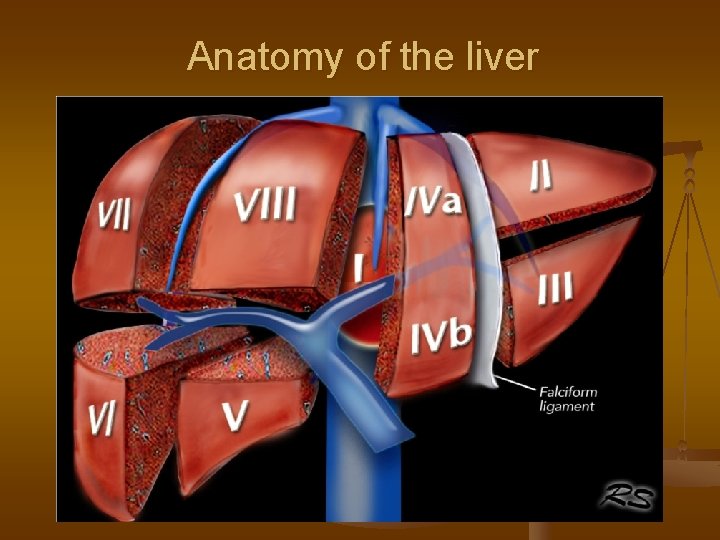
Anatomy of the liver
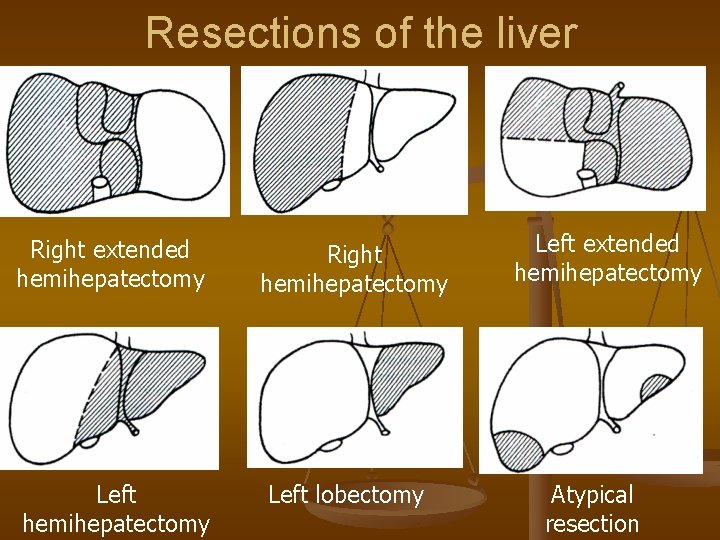
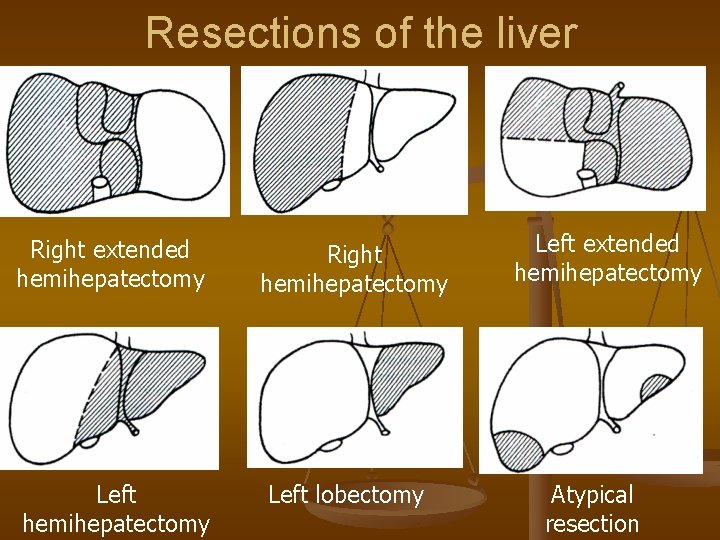
Resections of the liver Right extended hemihepatectomy Left hemihepatectomy Right hemihepatectomy Left lobectomy Left extended hemihepatectomy Atypical resection
SYMPTOMS OF LIVER DISEASES
General symptoms n n n ASYMPTOTIC FORM Discomfort, heaviness in right upper quadrant Right hypochondriac pains Hepatomegaly Elevated transaminase levels (AST, ALT) Liver insufficiency
Hollow structures compression n Biliar hypertension (mechanical jaundice) Yellowish colour of skin and sclerae n Dark urine n High levels of alkaline phosphatase and γ-GTP n Enlargement of biliar ducts n Non-drained segment syndrome n n n Portal hypertension Duodenal stenosis

Instrumental diagnostic of liver lesions n. Ultrasound n. CT scan n. MRI
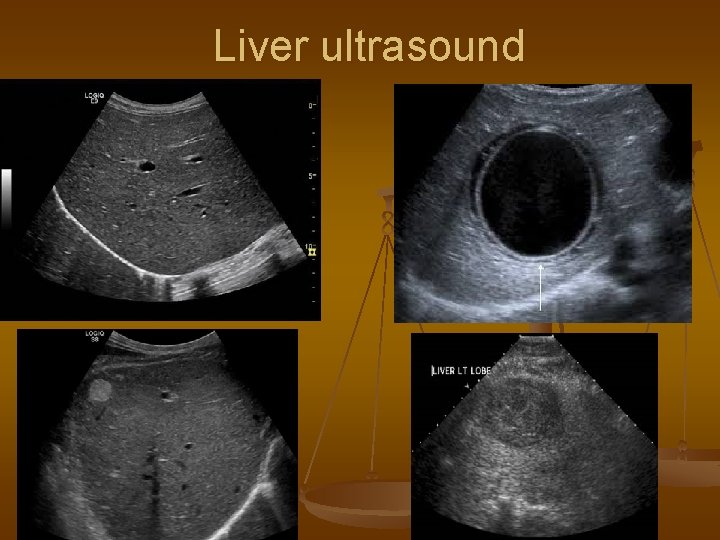
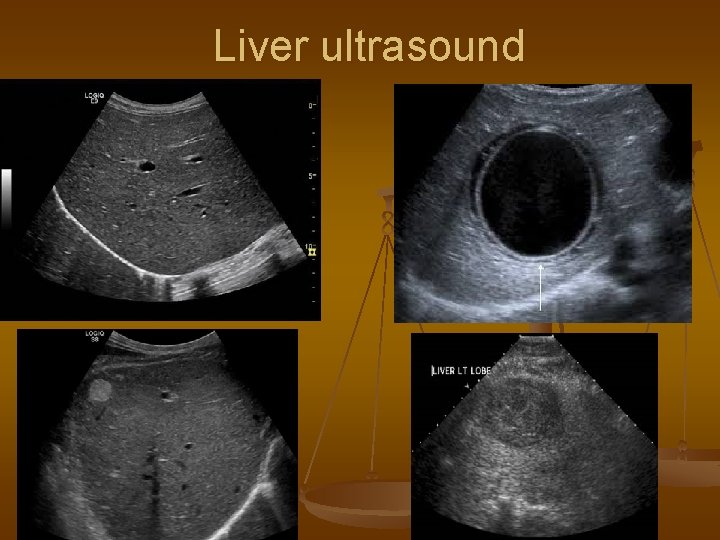
Liver ultrasound
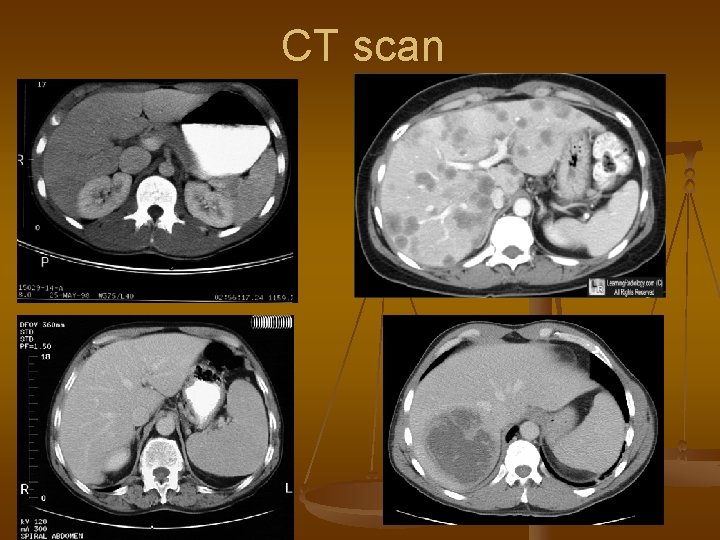
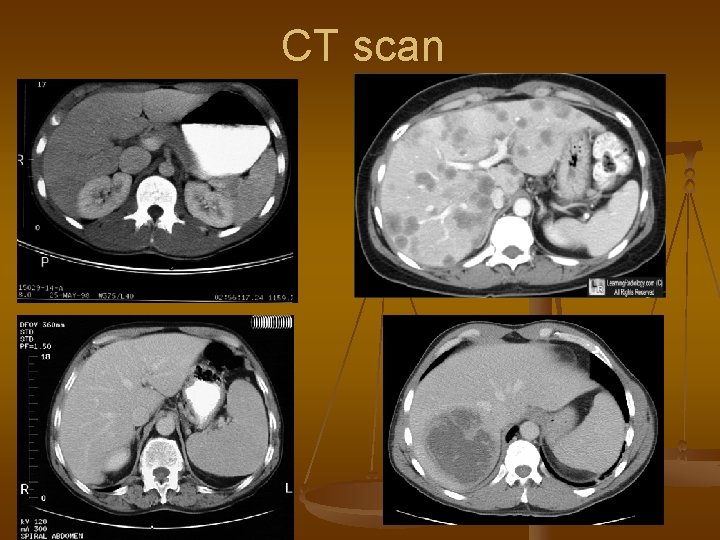
CT scan

SOLID LESIONS OF THE LIVER
What can it be? n Benign diseases: Hemangioma n Focal nodular hyperplasia n Adenoma n n Malignant diseases: Metastases n Hepatocellular carcinoma n Cholagiocellular carcinoma n
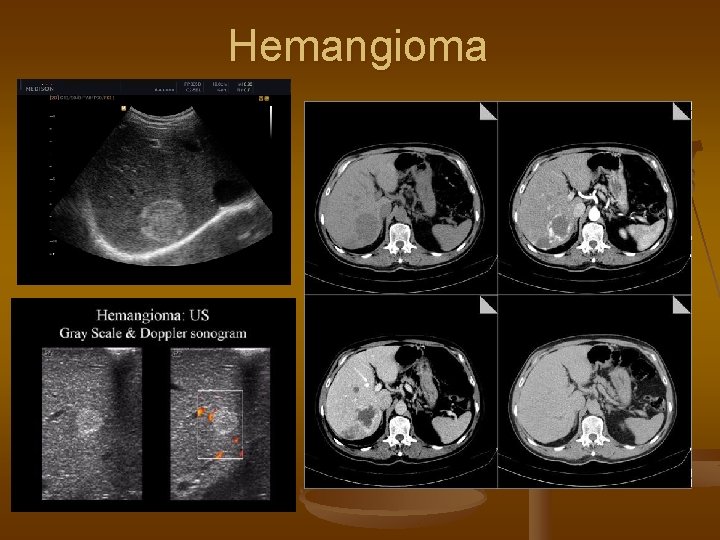
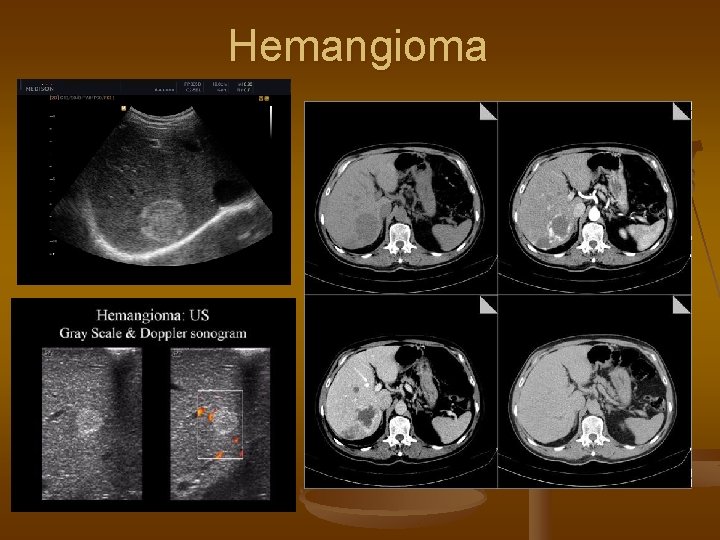
Hemangioma
Hemangioma - treatment n n Generally requires NO TREATMENT Biopsy is contraindicated Dynamic observation (ultrasound 1 per year) Resection: by compression of nearby structures or rupture
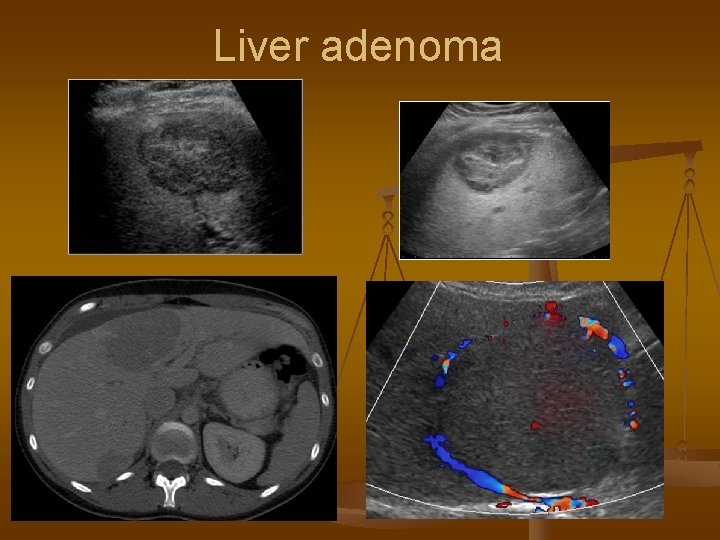
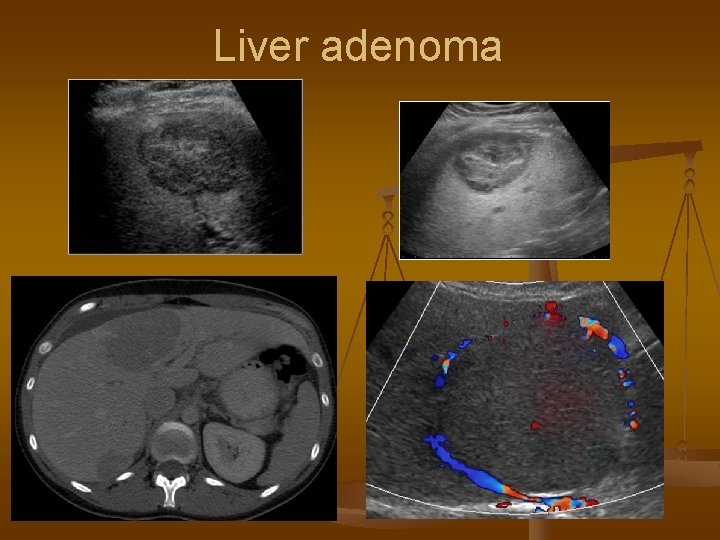
Liver adenoma
Liver adenoma n n Risk factors: peroral contraceptives, steroids If lesser than 5 cm – dynamic observation If larger than 5 cm – can be ruptured or turn malignant Treatment – resection or embolization
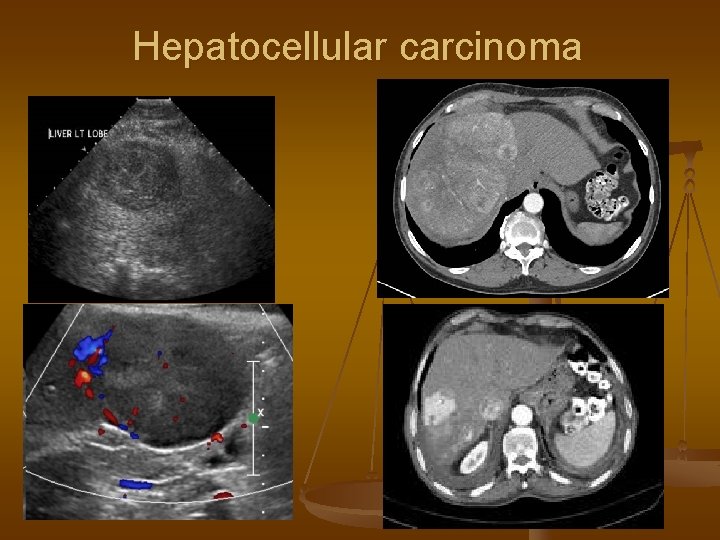
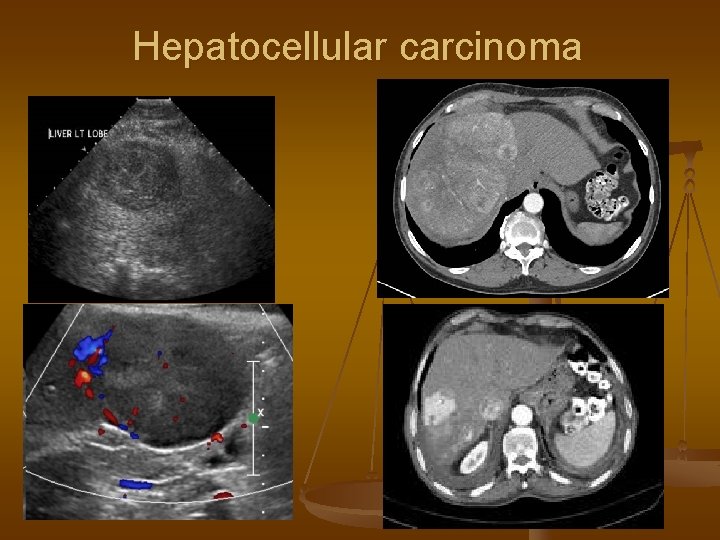
Hepatocellular carcinoma
Hepatocellular carcinoma n n n Elevated levels of CEA and α-fetoprotein Confirmation by biopsy Radical treatment: Resection n Liver transplantation n Radioablation n n Non-radical treatment: Embolization n Chemoembolization n Chemotherapy n
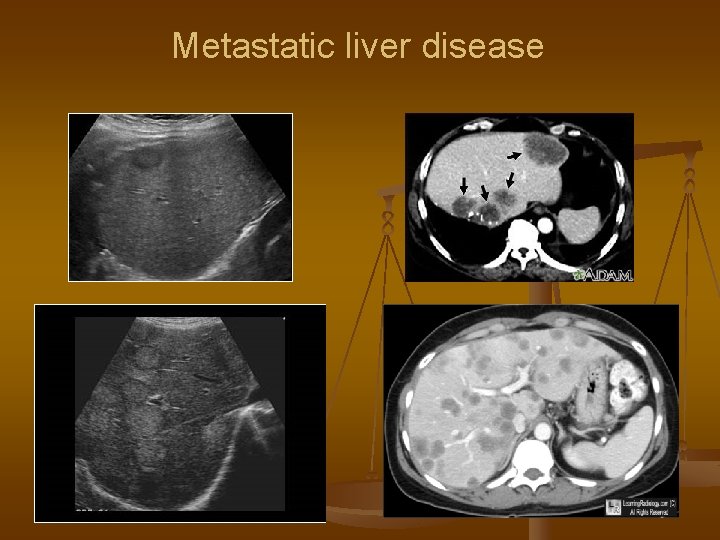
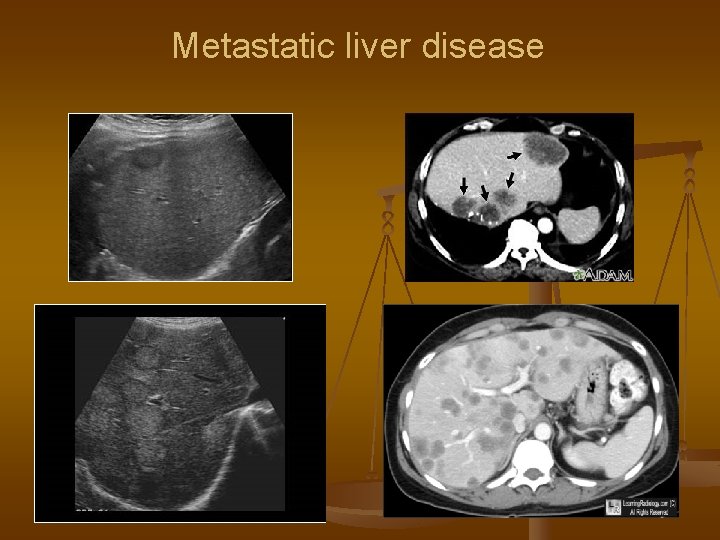
Metastatic liver disease
CYSTIC LESIONS OF THE LIVER
What can it be? n n n n Simple cyst Polycystic liver disease Liver abscess Amebic liver abscess Cystadenocarcinoma Echinococcosis Alveococcosis
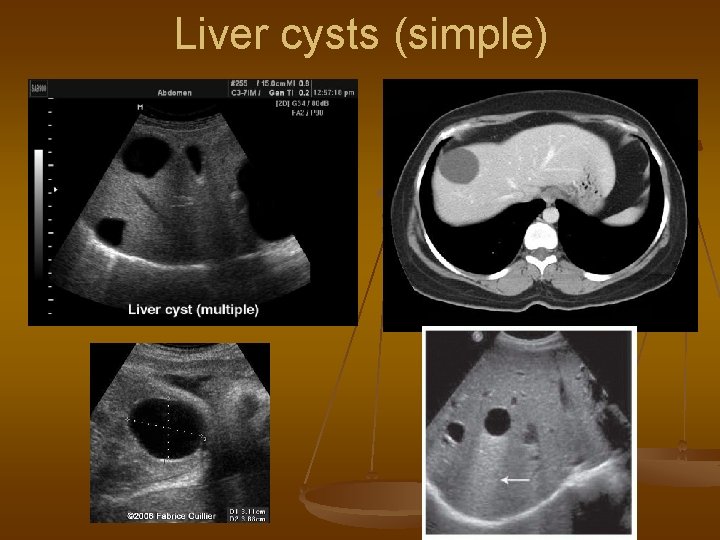
Liver cysts n n Mostly asymptotic Symptoms of compression by large diameter Diagnosed by ultrasound Additional methods: CT, MRI, biopsy – if thick wall, internal septs or calcificates were found
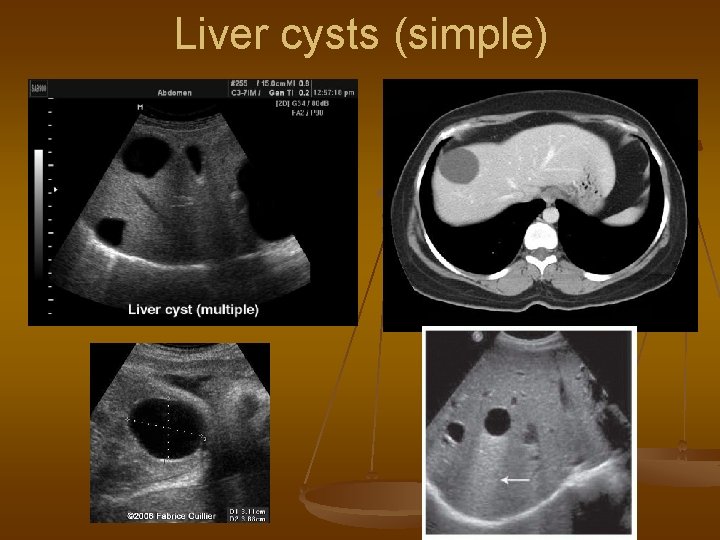
Liver cysts (simple)
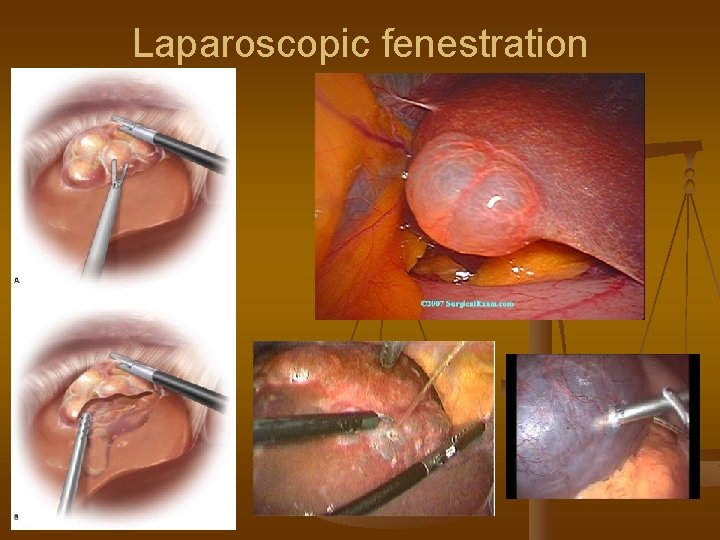
Treatment of simple cysts Asymptotic – dynamic observation n Method of choice for surgery – laparoscopic fenestration n Alternative method – puncture, aspiration and sclerosant injection n
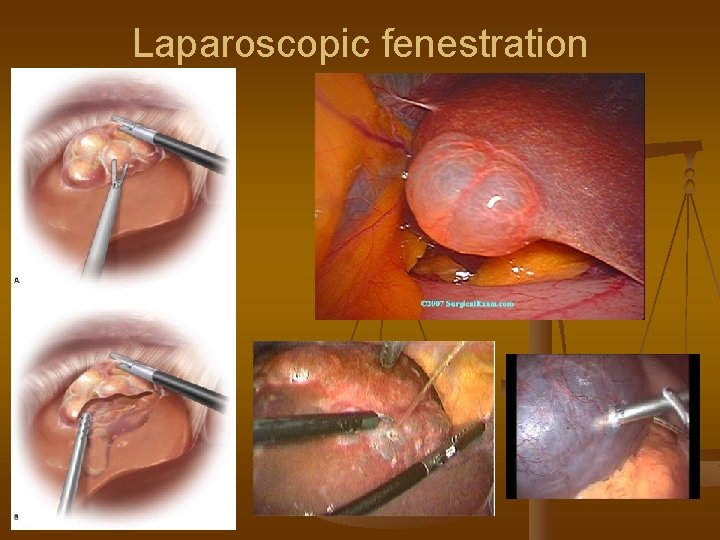
Laparoscopic fenestration
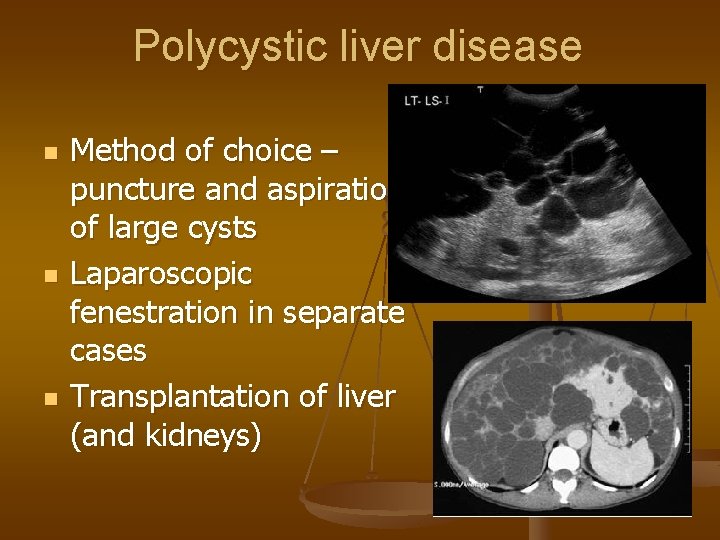
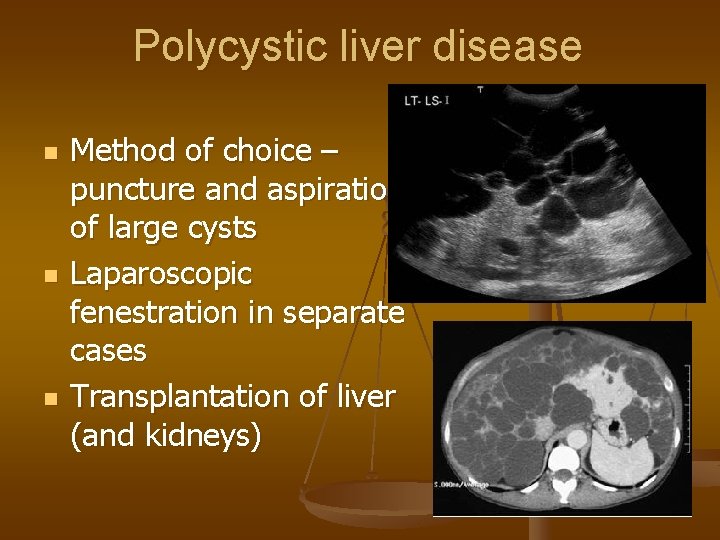
Polycystic liver disease n n n Method of choice – puncture and aspiration of large cysts Laparoscopic fenestration in separate cases Transplantation of liver (and kidneys)
LIVER ABSCESS
Liver abscess etiology n Enterogenic (through v. portae) n Cholangiogenic n Hematogenic n Posttraumatic (also iatrogenic) n Contact
Bacterial abscesses 1. 2. 3. 4. Intoxication Liver affection symptoms Other organs involvement Complications
Intoxication symptoms n Hectic fever n Shivering n Sweating n Left shift, leukocytosis
Local liver symptoms n Pain in right hypochondrium n Hepatomegaly n Jaundice n High levels of AST, ALT n Ascites
Nearby organs reaction n High position of diaphragm n Reactive pleuritis n Cholecystitis n Duodenal compression n Kidney reaction

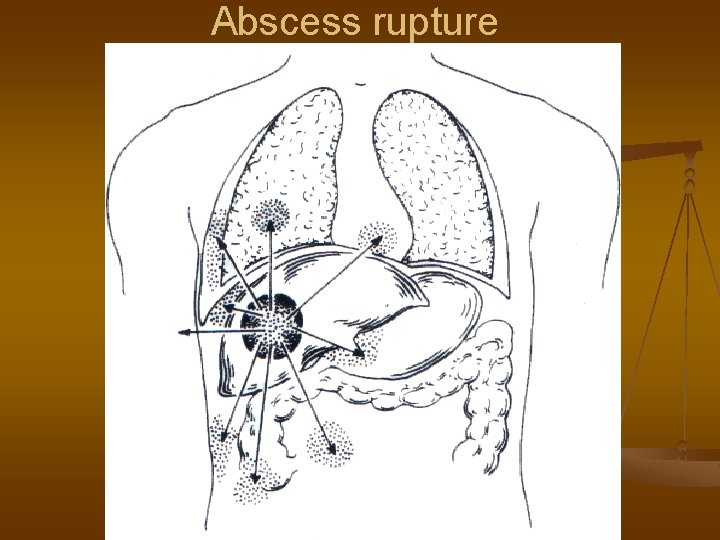
Complications of abscesses n Toxic shock n Septic metastases n Liver insufficiency n Bleeding n Fistula formation n Rupture of abscess
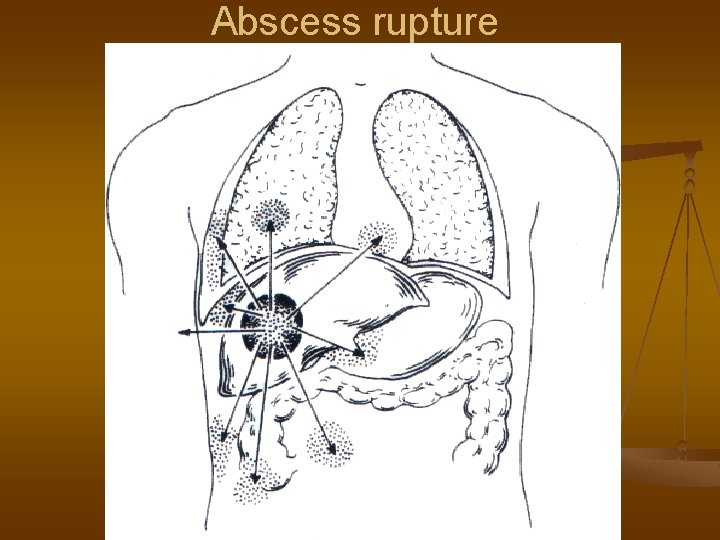
Abscess rupture
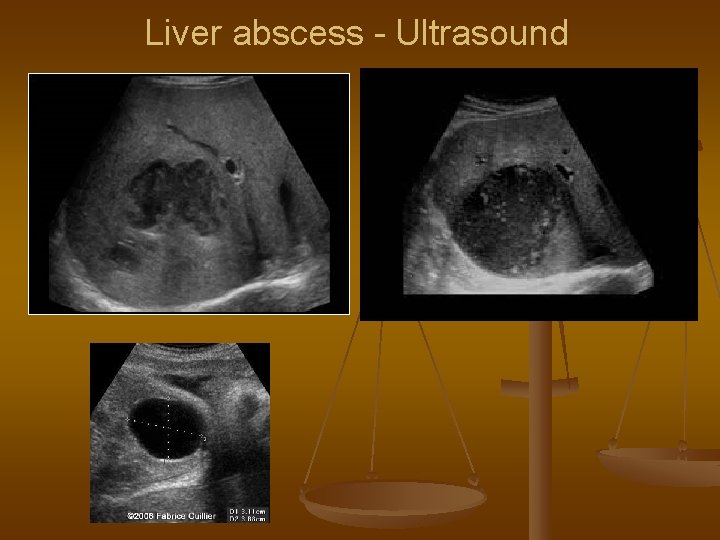
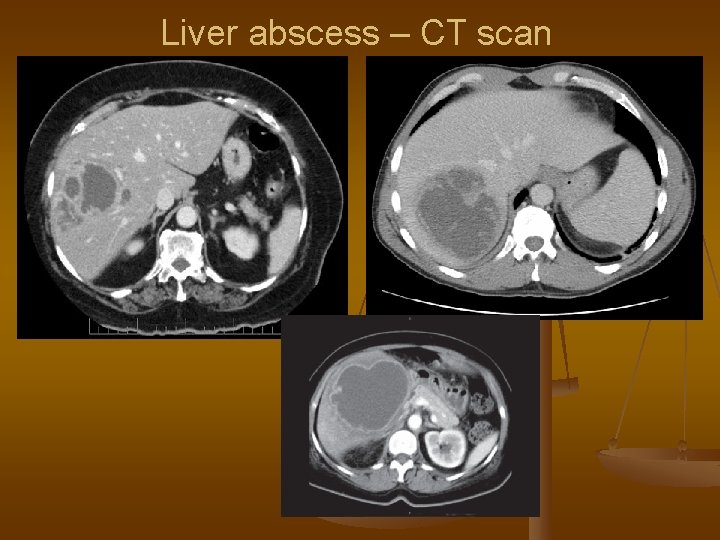
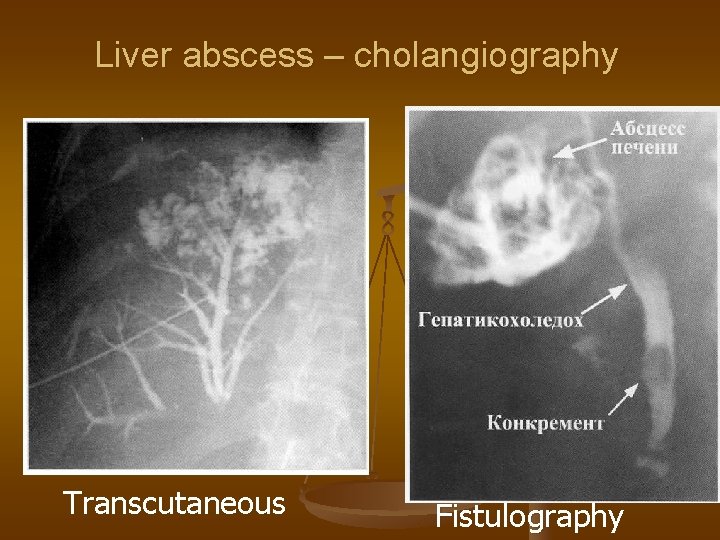
Diagnostic of abscess n Ultrasound n CT scan n Chest X-ray n ERCPG or TTCG by biliar abscess n Serologic test for Entamoeba histolytica
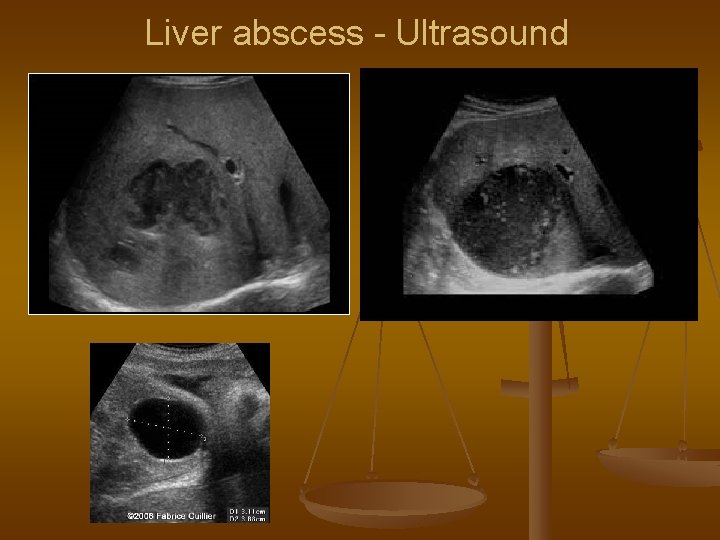
Liver abscess - Ultrasound
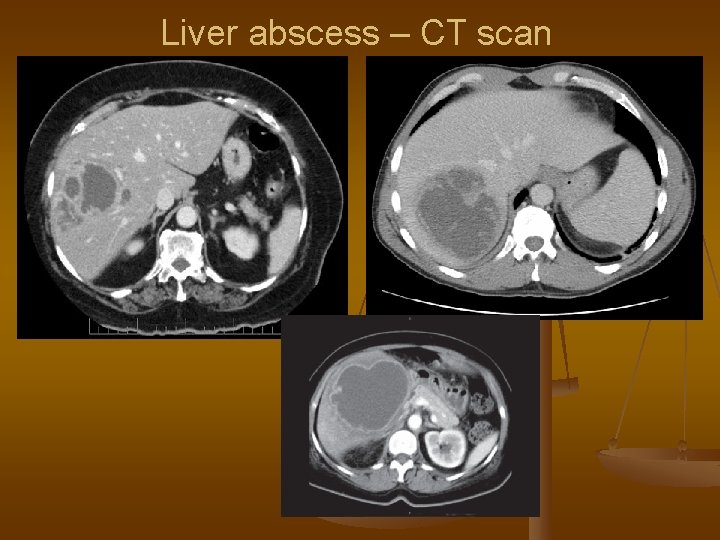
Liver abscess – CT scan
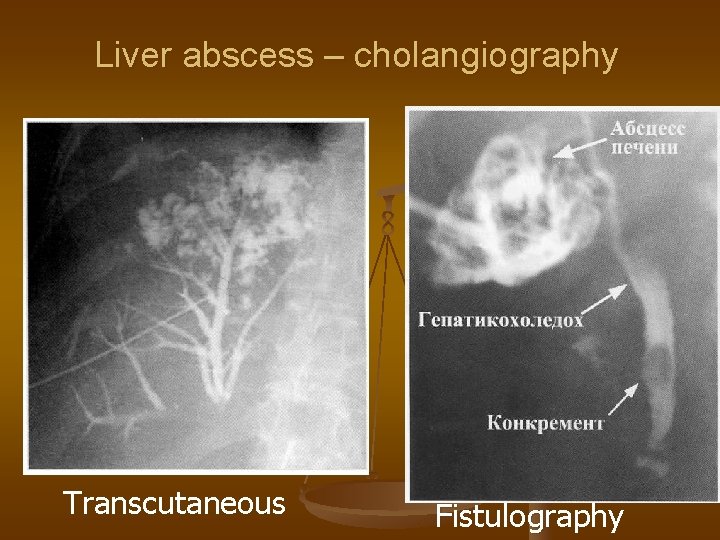
Liver abscess – cholangiography Transcutaneous Fistulography
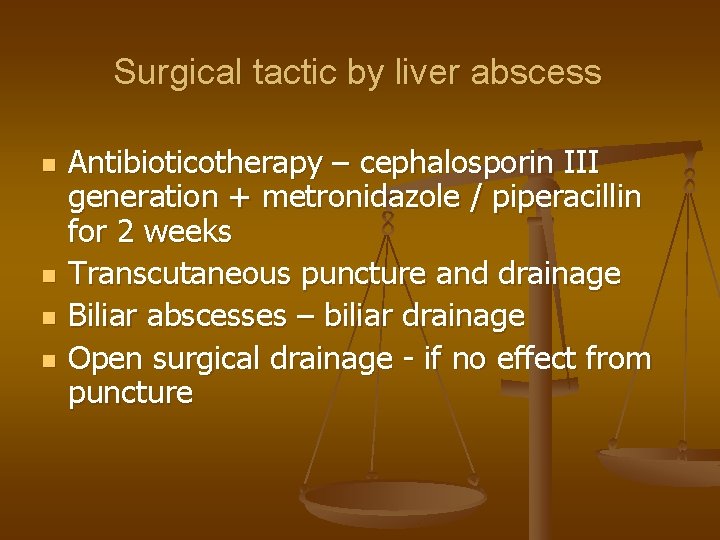
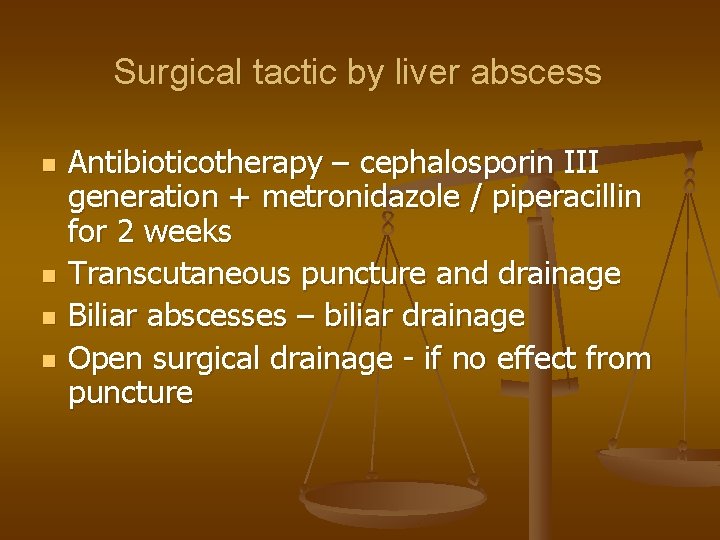
Surgical tactic by liver abscess n n Antibioticotherapy – cephalosporin III generation + metronidazole / piperacillin for 2 weeks Transcutaneous puncture and drainage Biliar abscesses – biliar drainage Open surgical drainage - if no effect from puncture
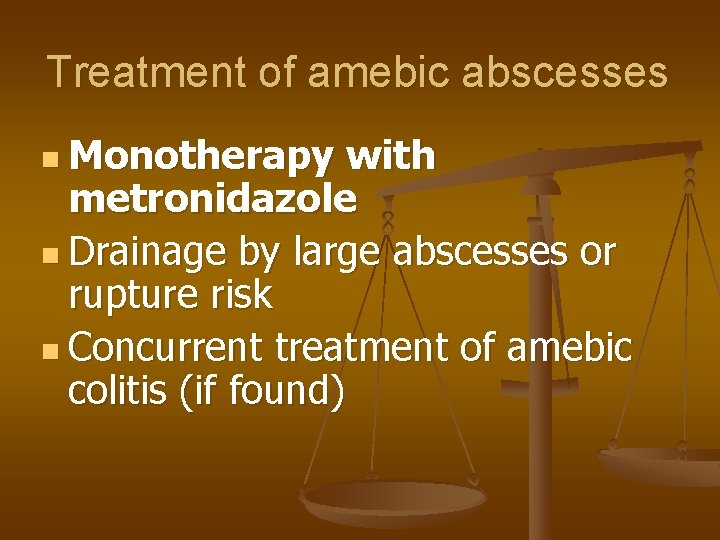
Treatment of amebic abscesses n Monotherapy with metronidazole n Drainage by large abscesses or rupture risk n Concurrent treatment of amebic colitis (if found)
PARASITIC DISEASES OF THE LIVER
Liver parasites Entamoeba hystolitica n Ascaris lumbricoideus n Opisthorchis felineus n Fasciola hepatica n Clonorchis sinensis n Schistosoma haematobium n Echinococcus granulosus n Alveococcus multilocularis n Taenia solium n
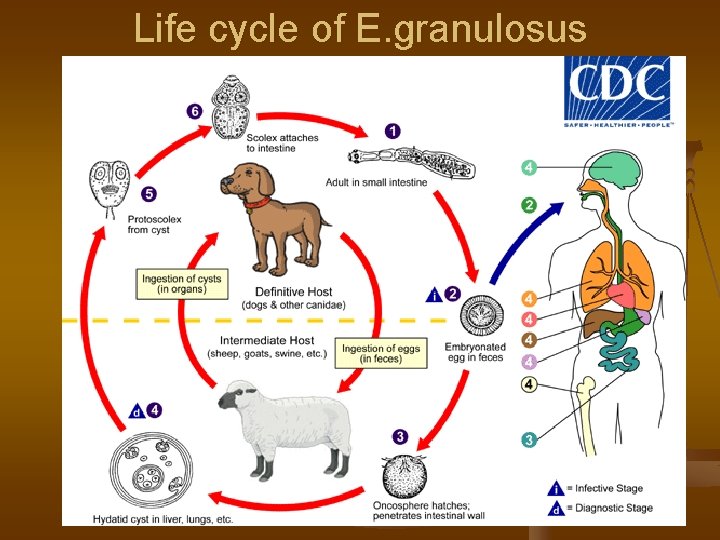
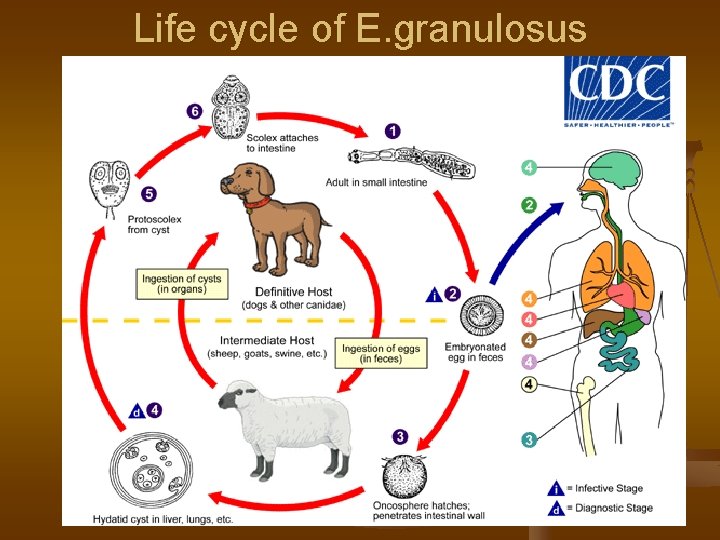
Life cycle of E. granulosus
Echinococcal cyst structure n Fibrous capsule n Chitinous layer n Germinative layer n Secondary cysts (hydatids) n Hydatid liquid
Echinococcosis - symptoms n. I stage - asymptotic n II stage: n Heaviness, discomfort n Pains in right upper quadrant n Weakness n Allergic reactions - urticaria n Nausea
Ecinococcosis - symptoms n III stage – complications: n Suppuration n Perforation n Ascites n Jaundice n Anaphylaxis
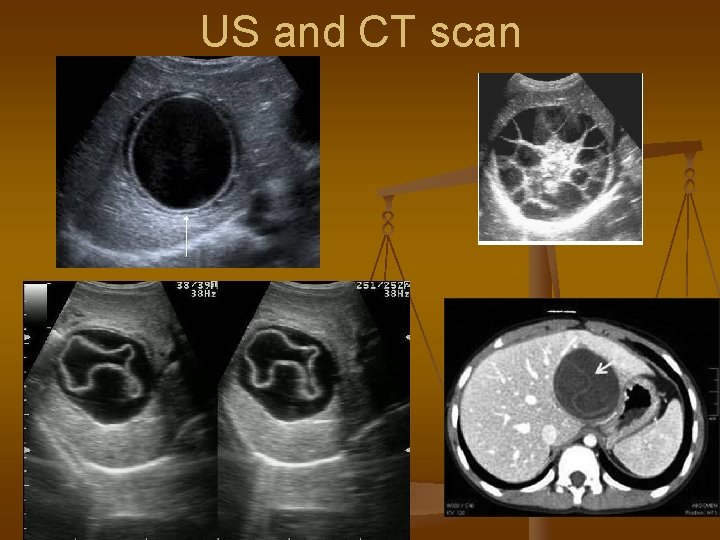
Echinococcosis - diagnostic n Ultrasound n CT scan n Eosinophilia n Serologic reactions n Aspiration of hydatid liquid
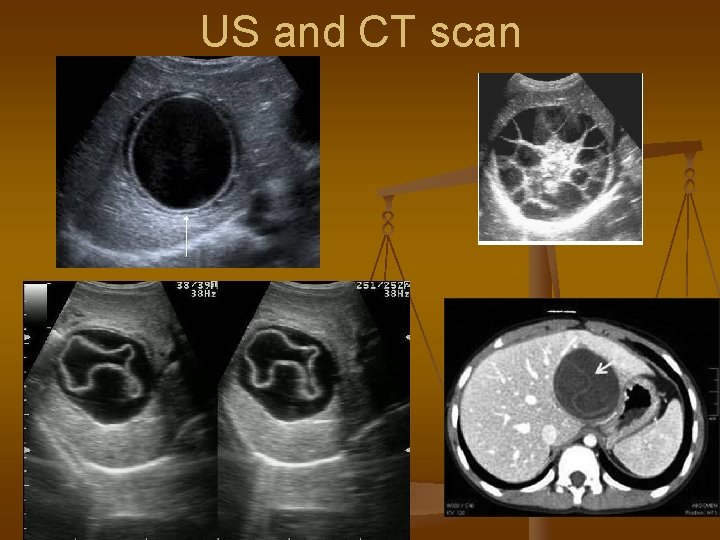
US and CT scan
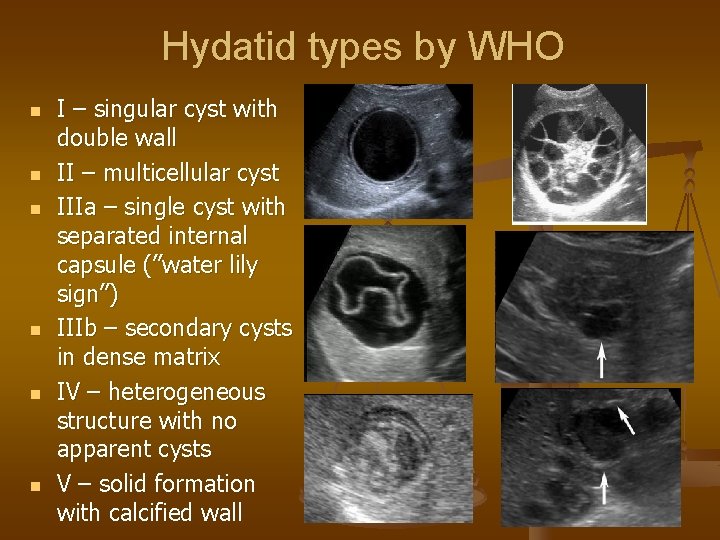
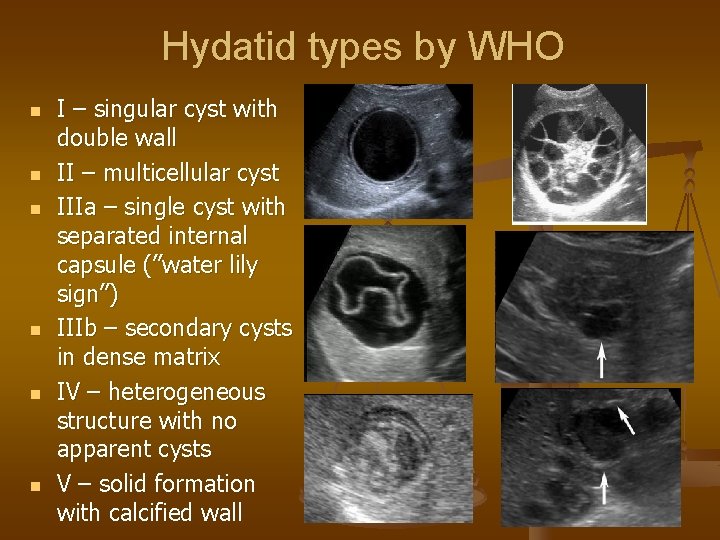
Hydatid types by WHO n n n I – singular cyst with double wall II – multicellular cyst IIIa – single cyst with separated internal capsule (”water lily sign”) IIIb – secondary cysts in dense matrix IV – heterogeneous structure with no apparent cysts V – solid formation with calcified wall

Treatment of echinococcosis n n Type I or 3 a, smaller than 5 cm – monotherapy with albendazole or mebendazole Type I or 3 a, larger than 5 cm – PAIR (puncture-aspiration-irrigation-reaspiration), then albendazole
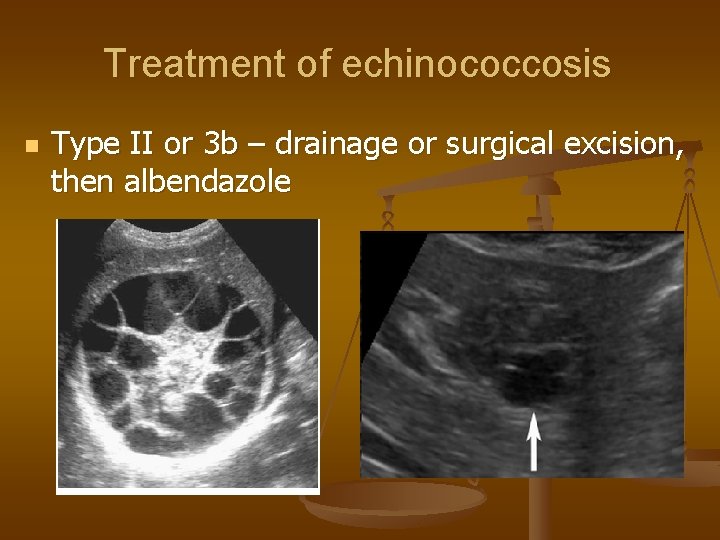
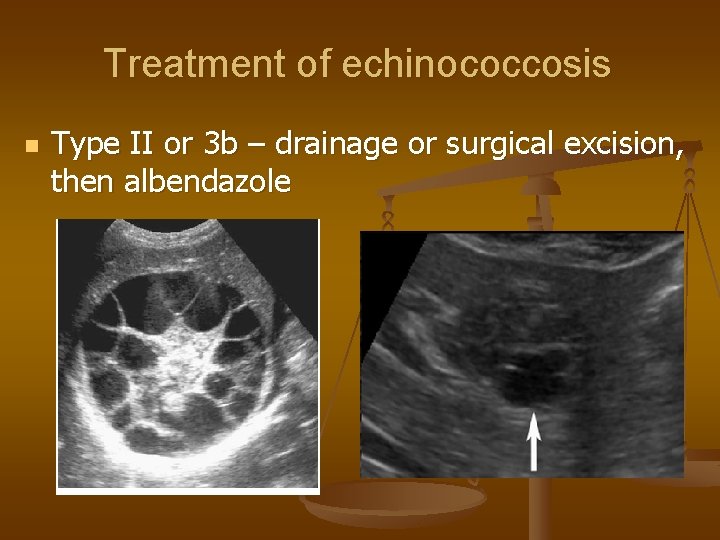
Treatment of echinococcosis n Type II or 3 b – drainage or surgical excision, then albendazole

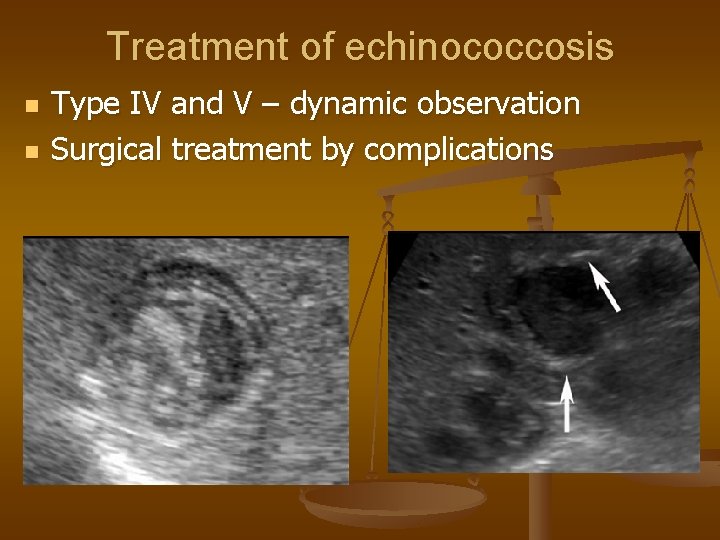
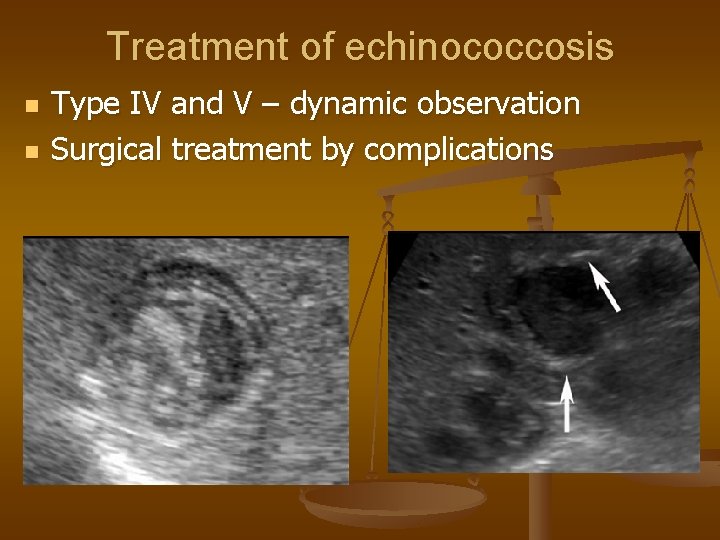
Treatment of echinococcosis n n Type IV and V – dynamic observation Surgical treatment by complications
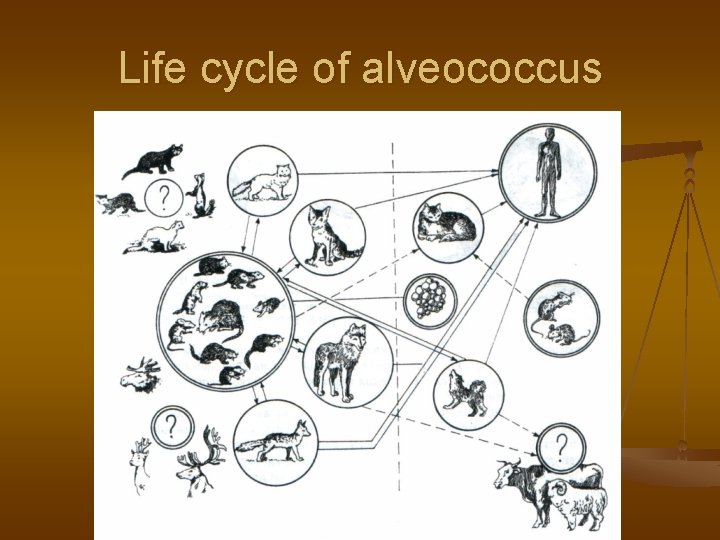
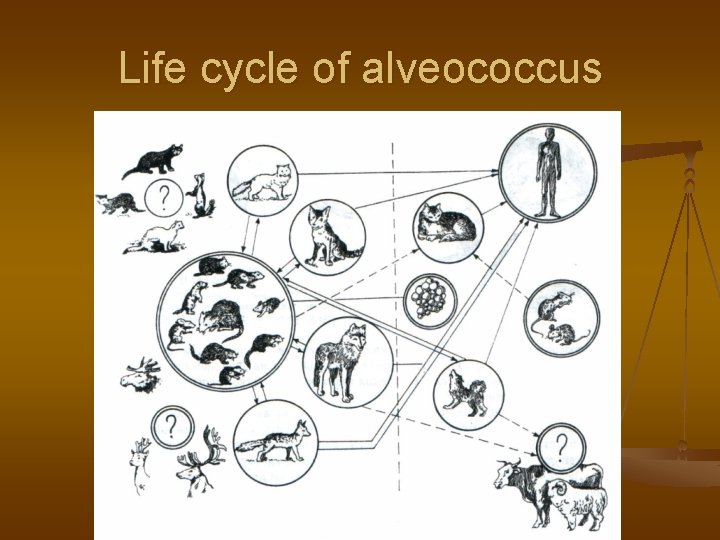
Life cycle of alveococcus

Alveococcus
Treatment of alveococcosis n n n Method of choice – liver resection, parasite excision or liver transplantation After surgery – 2 year course of albendazole Palliative treatment – albendazole, miniinvasive surgery
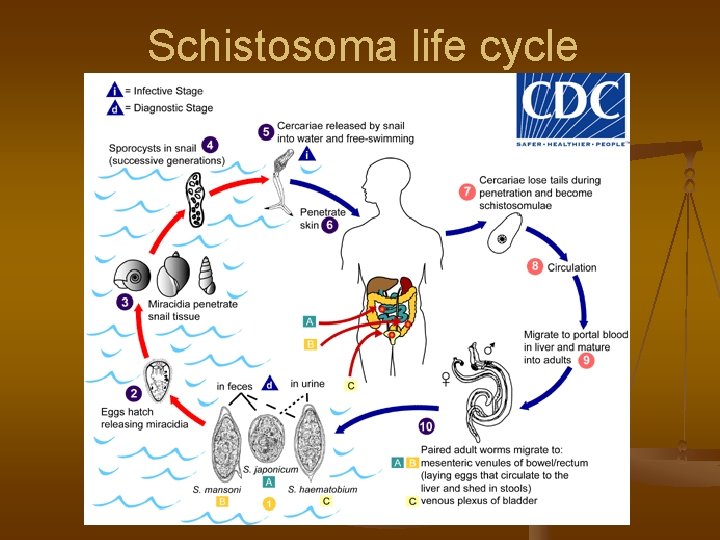
Schistosomiasis n Caused by trematodes of Schistosoma genus: S. haematobium, S. mansoni, S. japonicum, S. guineensis, S. mekongi
Schistosomiasis n n n Occurs in Africa, Brazil, Cambodia, the Caribbean, China, Corsica, Indonesia, Laos, the Middle East, the Philippines, Suriname, and Venezuela Transmitted through water Affects liver, then blood vessels of the intestine, bladder, genitals
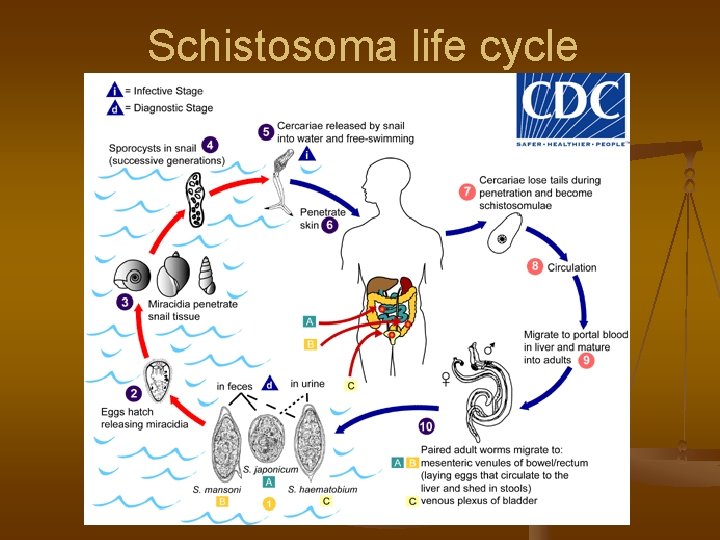
Schistosoma life cycle
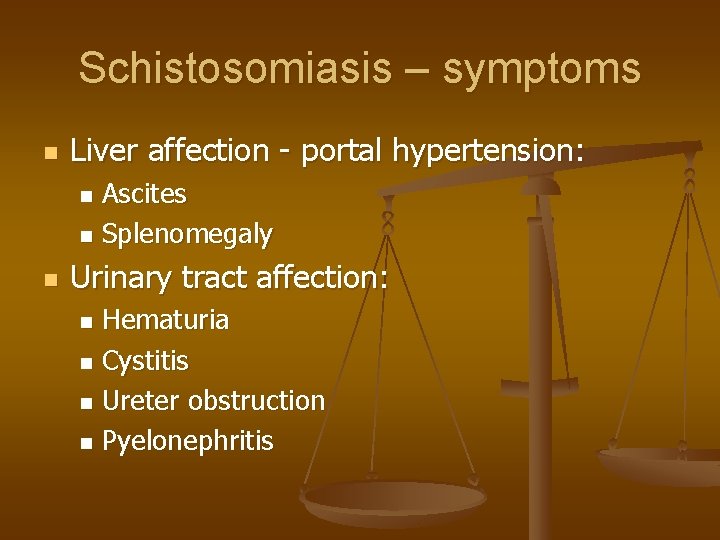
Schistosomiasis – symptoms n Liver affection - portal hypertension: Ascites n Splenomegaly n n Urinary tract affection: Hematuria n Cystitis n Ureter obstruction n Pyelonephritis n
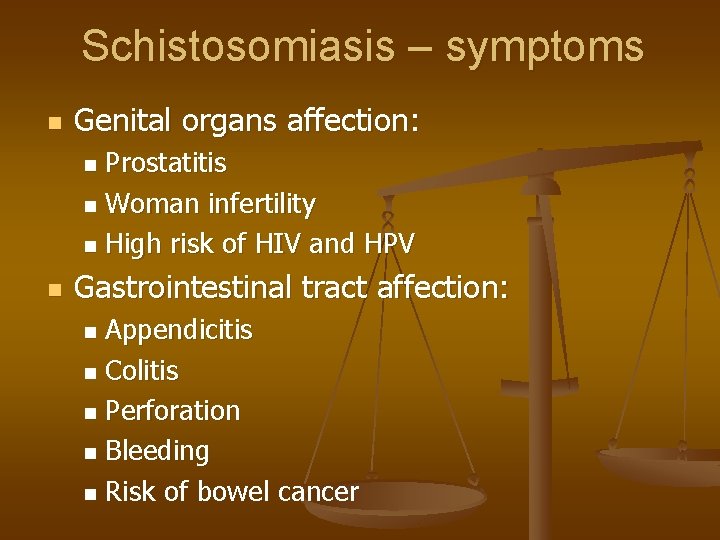
Schistosomiasis – symptoms n Genital organs affection: Prostatitis n Woman infertility n High risk of HIV and HPV n n Gastrointestinal tract affection: Appendicitis n Colitis n Perforation n Bleeding n Risk of bowel cancer n
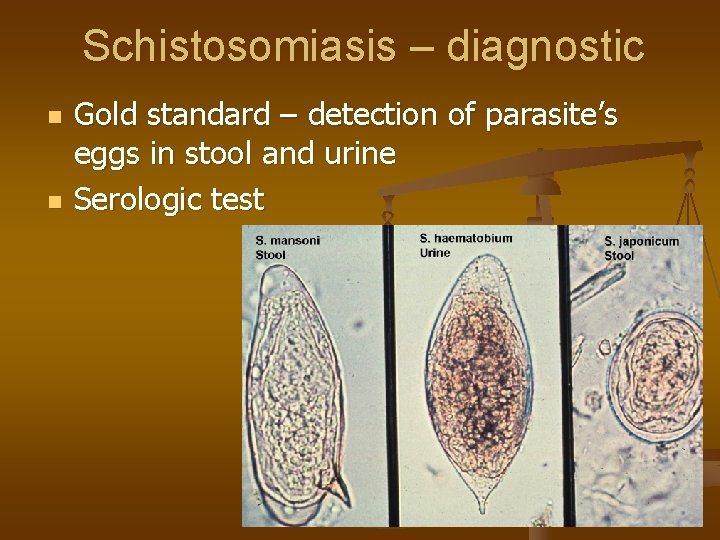
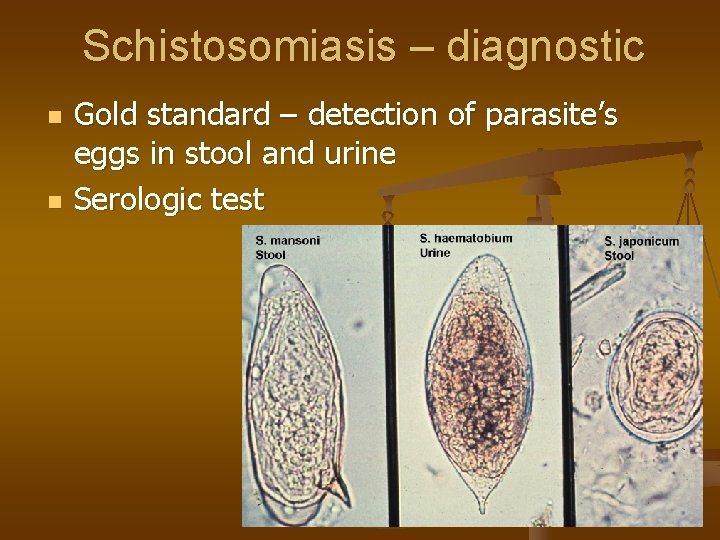
Schistosomiasis – diagnostic n n Gold standard – detection of parasite’s eggs in stool and urine Serologic test
Schistosomiasis – treatment n n n Praziquantel 60 mg/kg per day Prophylaxis with single dose of praziquantel Surgery by complications: Treatment of bleedings n Treatment of portal hypertension n Resection of the intestines n
Liver trematodes n n Fasciola hepatica Opisthorchis felineus Clonorchis sinensis Dicrocoelium lanceatum
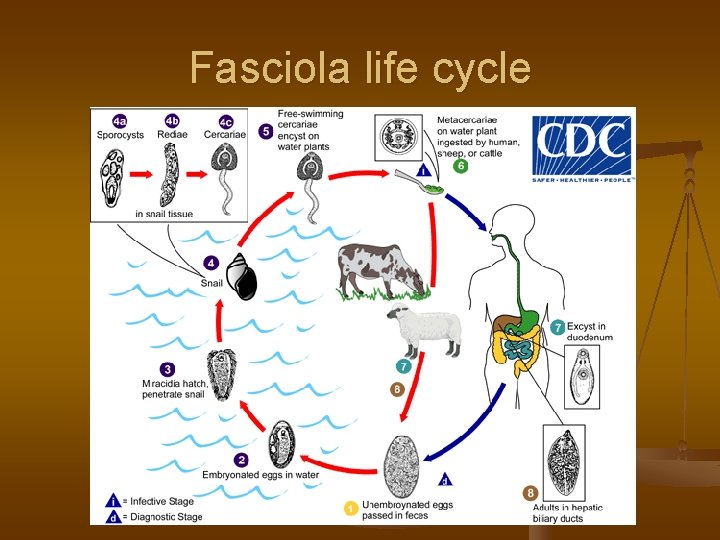
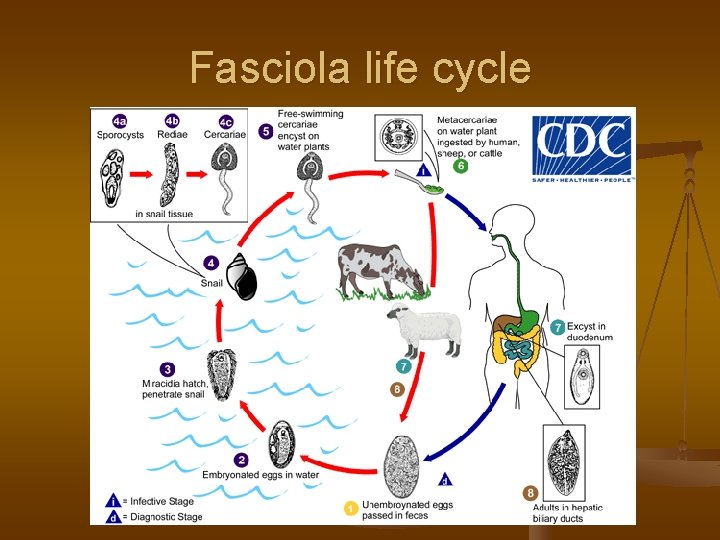
Fasciola life cycle
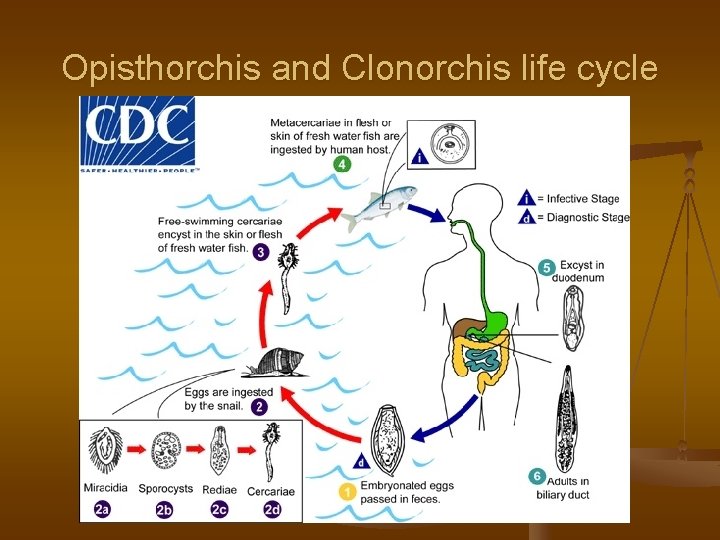
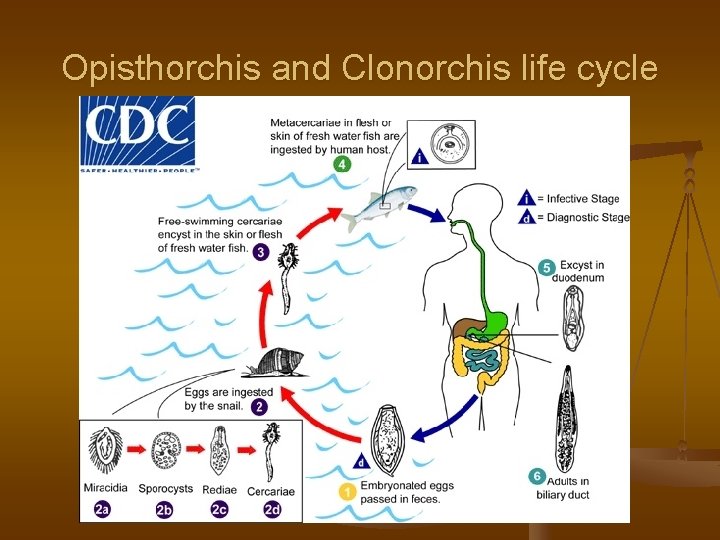
Opisthorchis and Clonorchis life cycle
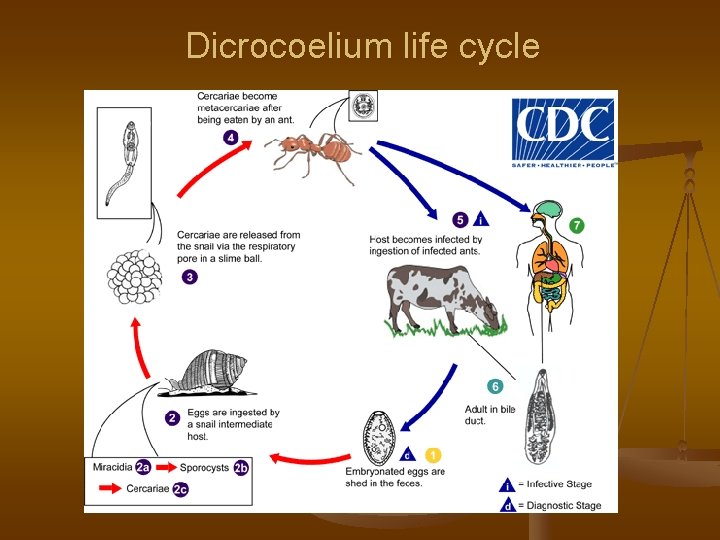
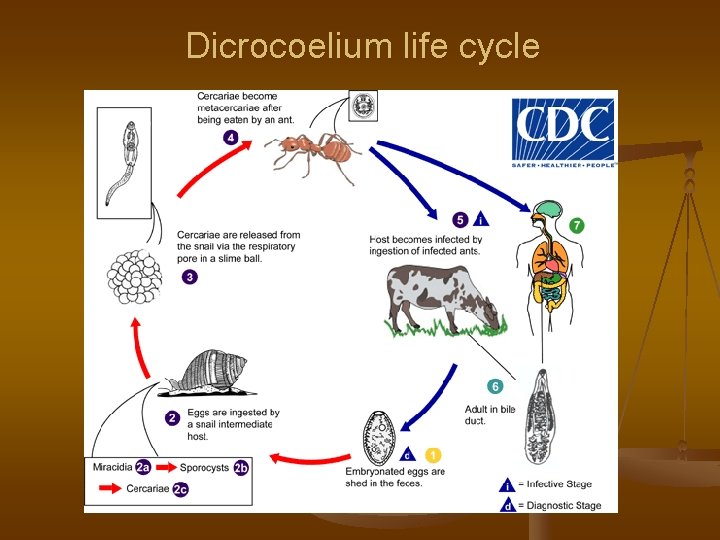
Dicrocoelium life cycle

Symptoms of liver flukes n n n n Abdominal pain Fever Nausea, vomiting Diarrhea Urticaria Malaise, weakness Decreased appetite and weight loss
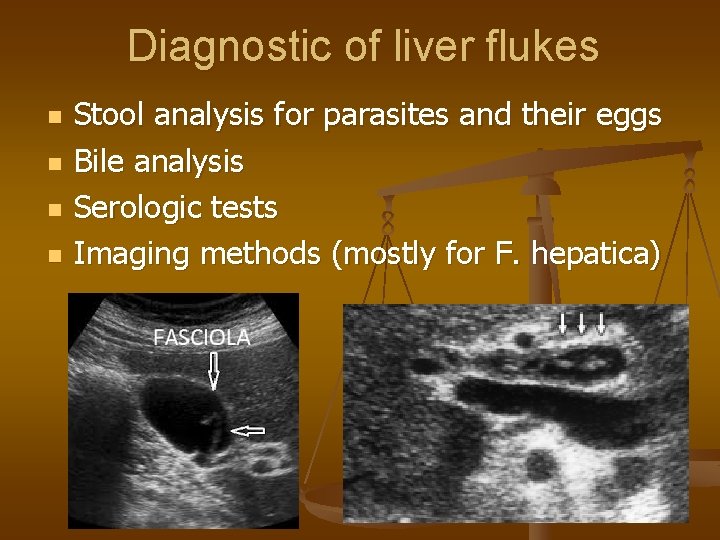
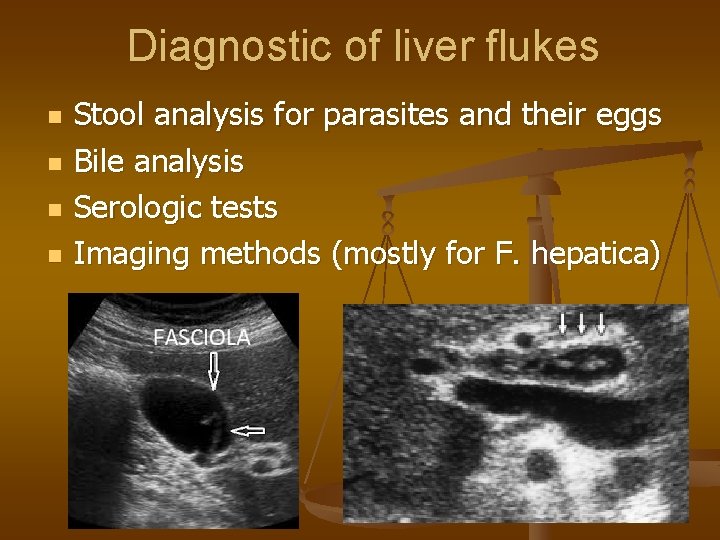
Diagnostic of liver flukes n n Stool analysis for parasites and their eggs Bile analysis Serologic tests Imaging methods (mostly for F. hepatica)

Treatment of liver flukes n n Fasciola hepatica – triclabendazole Praziquantel Albendazole Surgery for complications: Cholecystectomy n Biliar drainage n Liver resection n
 Liver anatomy and physiology
Liver anatomy and physiology Gastric emptying ppt
Gastric emptying ppt Brisbane 2000 terminology liver anatomy
Brisbane 2000 terminology liver anatomy Liver anatomy
Liver anatomy Bile juices
Bile juices Surface anatomy of liver
Surface anatomy of liver Art labeling activity figure 23.5
Art labeling activity figure 23.5 Anatomy and histology of liver
Anatomy and histology of liver Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là giọng cùng tên
Thế nào là giọng cùng tên Phép trừ bù
Phép trừ bù Lời thề hippocrates
Lời thề hippocrates Hươu thường đẻ mỗi lứa mấy con
Hươu thường đẻ mỗi lứa mấy con Tư thế worms-breton
Tư thế worms-breton đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Công thức tính thế năng
Công thức tính thế năng Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Dot
Dot Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 Bổ thể
Bổ thể Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phản ứng thế ankan
Phản ứng thế ankan Các môn thể thao bắt đầu bằng tiếng đua
Các môn thể thao bắt đầu bằng tiếng đua Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Hát lên người ơi alleluia
Hát lên người ơi alleluia điện thế nghỉ
điện thế nghỉ Một số thể thơ truyền thống
Một số thể thơ truyền thống Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Số.nguyên tố
Số.nguyên tố Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Tia chieu sa te
Tia chieu sa te Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Sơ đồ cơ thể người
Sơ đồ cơ thể người ưu thế lai là gì
ưu thế lai là gì Tư thế ngồi viết
Tư thế ngồi viết Cái miệng xinh xinh thế chỉ nói điều hay thôi
Cái miệng xinh xinh thế chỉ nói điều hay thôi Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Tư thế ngồi viết
Tư thế ngồi viết Chó sói
Chó sói Thẻ vin
Thẻ vin Thể thơ truyền thống
Thể thơ truyền thống Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Liver defenition
Liver defenition Mild hepatic steatosis
Mild hepatic steatosis Glisson's capsule
Glisson's capsule Keva liver care
Keva liver care Immediate changes after death
Immediate changes after death Spleen liver gallbladder
Spleen liver gallbladder What is the primary function of the liver
What is the primary function of the liver Types of cirrhosis
Types of cirrhosis Tresia medical term
Tresia medical term Www.brainpopcom
Www.brainpopcom Liver injury grading
Liver injury grading Function of kidney
Function of kidney Renal bruit auscultation
Renal bruit auscultation Stages of cirrhosis
Stages of cirrhosis Nutmeg liver
Nutmeg liver Nursing management of liver abscess
Nursing management of liver abscess Difference between cld and dcld
Difference between cld and dcld Effects of alcohol on the liver
Effects of alcohol on the liver Vascolarizzazione pancreas
Vascolarizzazione pancreas Pes statement for liver cirrhosis
Pes statement for liver cirrhosis Rifaximin in liver failure
Rifaximin in liver failure Porosis of the liver
Porosis of the liver