Heart Failure Ischemic Heart Disease Aneurysm and Dissection
- Slides: 33
Heart Failure Ischemic Heart Disease Aneurysm and Dissection Maram Abdaljaleel, M. D.
Heart Failure • End point of many heart diseases • Can be called Congestive Heart Failure (CHF) • Common! In USA, 5 millions affected each year • carries an extremely poor prognosis (300, 000 fatalities) • Heart can’t pump blood fast enough to meet needs of body
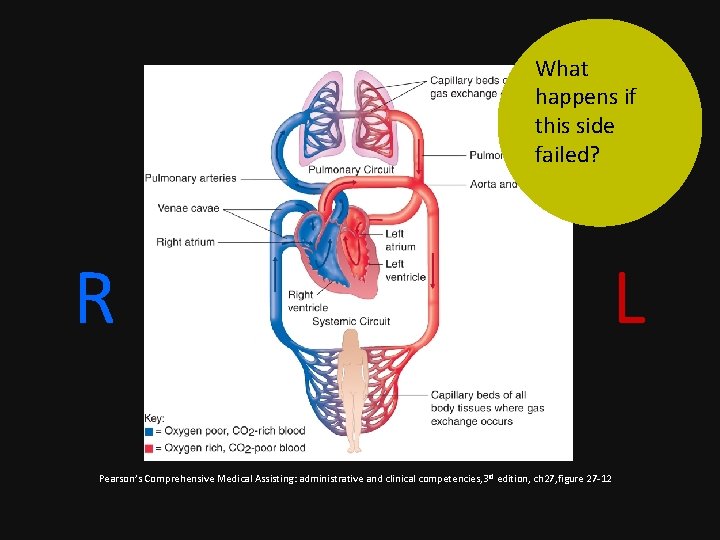
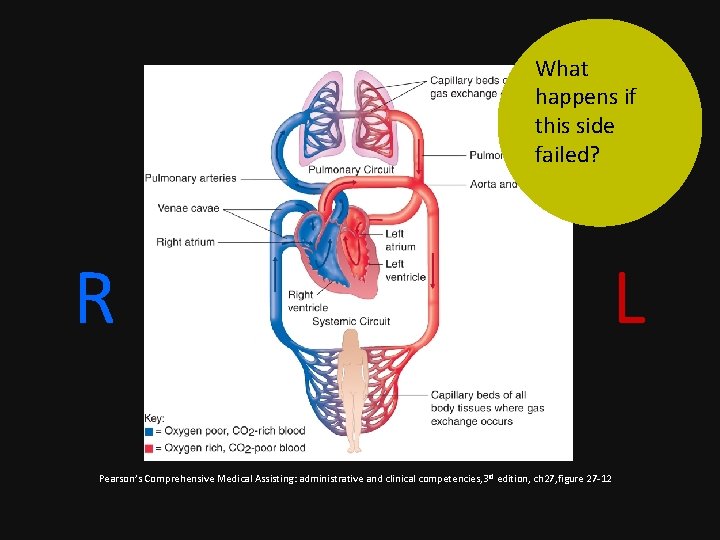
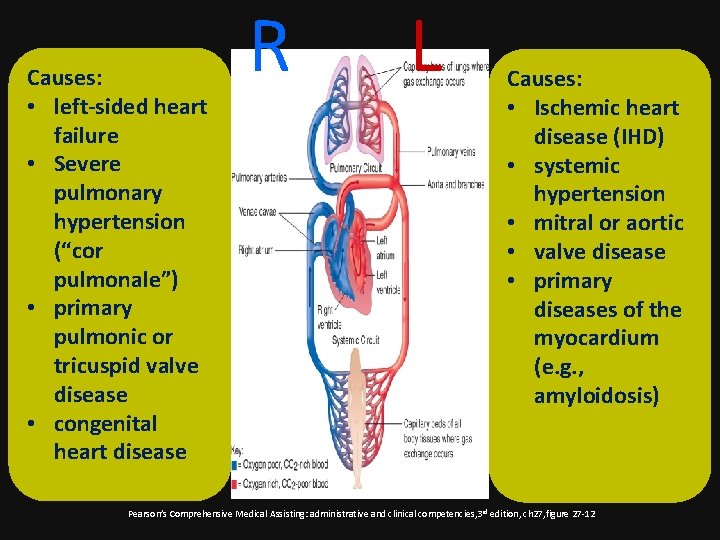
What happens if this side failed? R L Pearson’s Comprehensive Medical Assisting: administrative and clinical competencies, 3 rd edition, ch 27, figure 27 -12
• If the left side of the heart fail blood backs up in the lung! • If the right side of the heart fail blood backs up in the body!
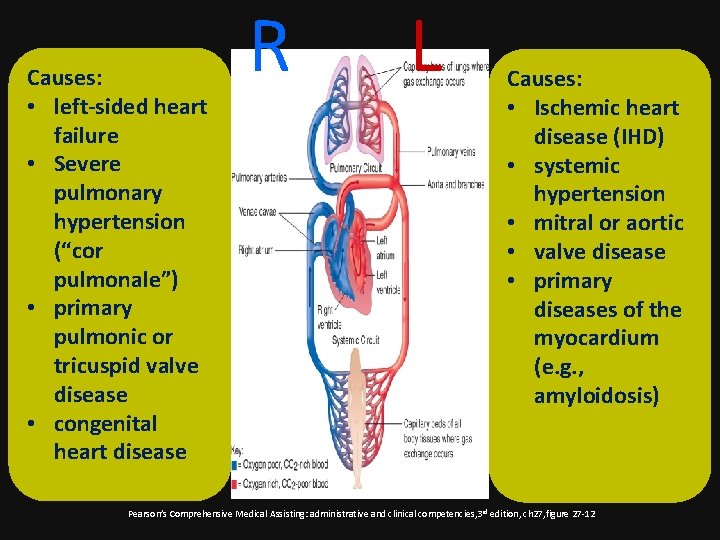
Causes: • left-sided heart failure • Severe pulmonary hypertension (“cor pulmonale”) • primary pulmonic or tricuspid valve disease • congenital heart disease R L Causes: • Ischemic heart disease (IHD) • systemic hypertension • mitral or aortic • valve disease • primary diseases of the myocardium (e. g. , amyloidosis) Pearson’s Comprehensive Medical Assisting: administrative and clinical competencies, 3 rd edition, ch 27, figure 27 -12
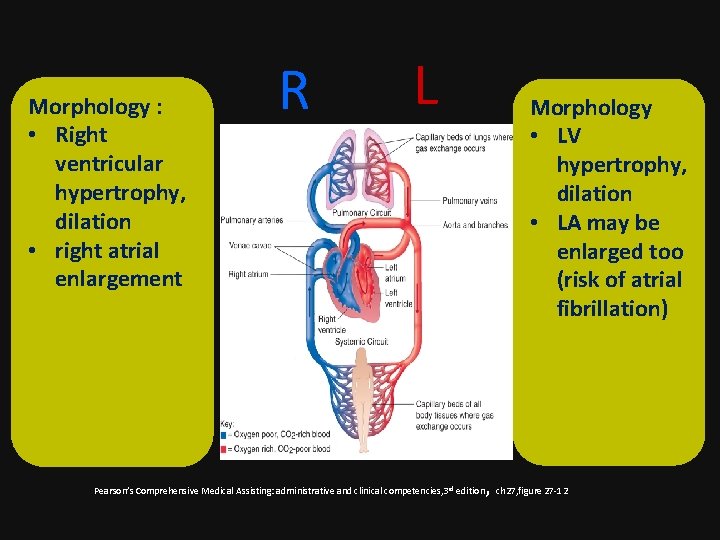
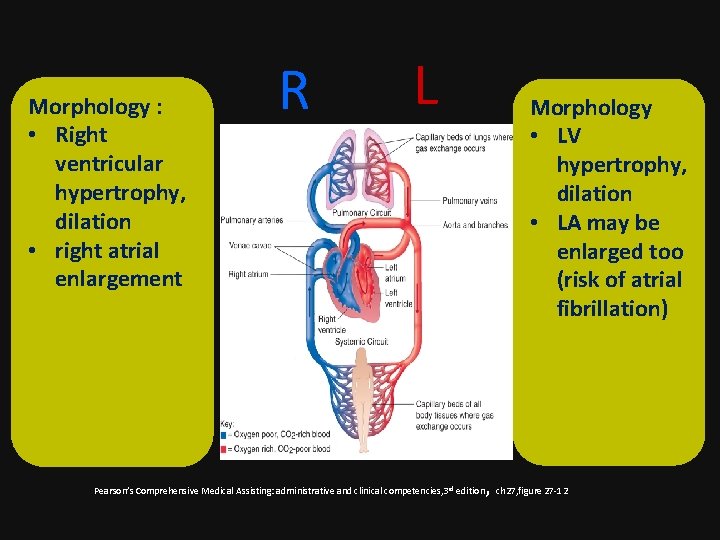
Morphology : • Right ventricular hypertrophy, dilation • right atrial enlargement R L Morphology • LV hypertrophy, dilation • LA may be enlarged too (risk of atrial fibrillation) , ch 27, figure 27 -12 Pearson’s Comprehensive Medical Assisting: administrative and clinical competencies, 3 rd edition
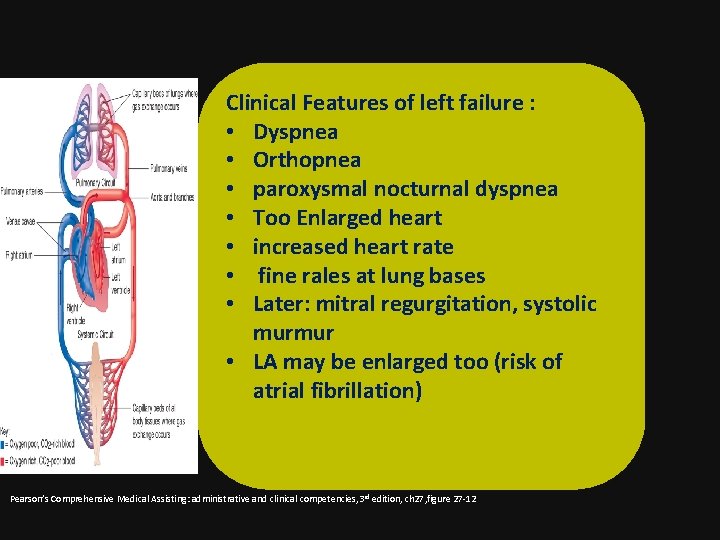
Clinical Features of left failure : • Dyspnea • Orthopnea • paroxysmal nocturnal dyspnea • Too Enlarged heart • increased heart rate • fine rales at lung bases • Later: mitral regurgitation, systolic murmur • LA may be enlarged too (risk of atrial fibrillation) Pearson’s Comprehensive Medical Assisting: administrative and clinical competencies, 3 rd edition, ch 27, figure 27 -12
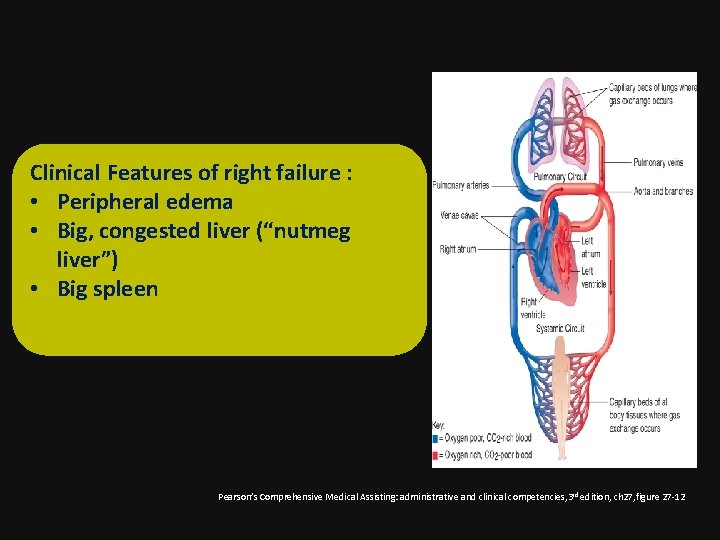
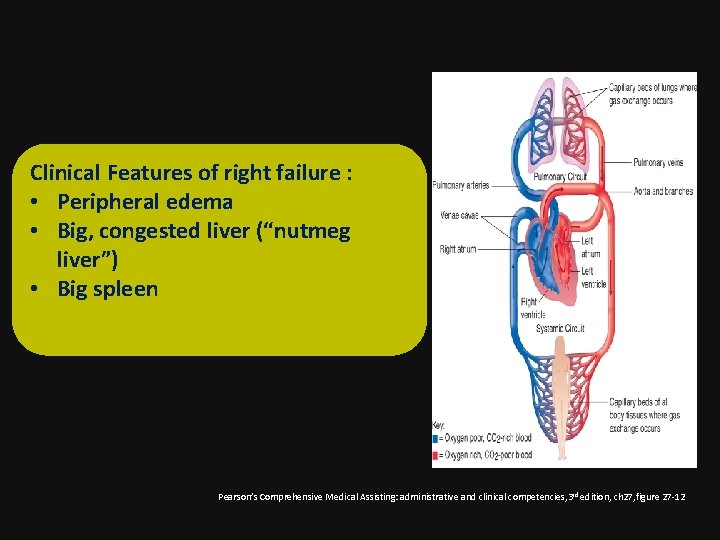
Clinical Features of right failure : • Peripheral edema • Big, congested liver (“nutmeg liver”) • Big spleen Pearson’s Comprehensive Medical Assisting: administrative and clinical competencies, 3 rd edition, ch 27, figure 27 -12
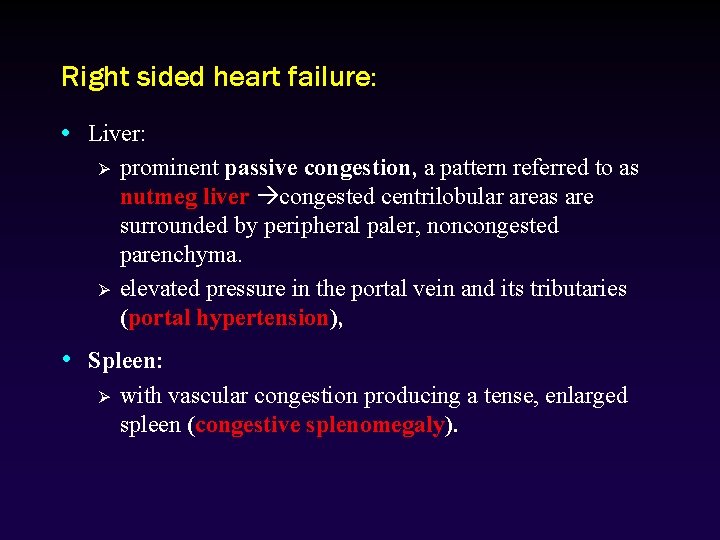
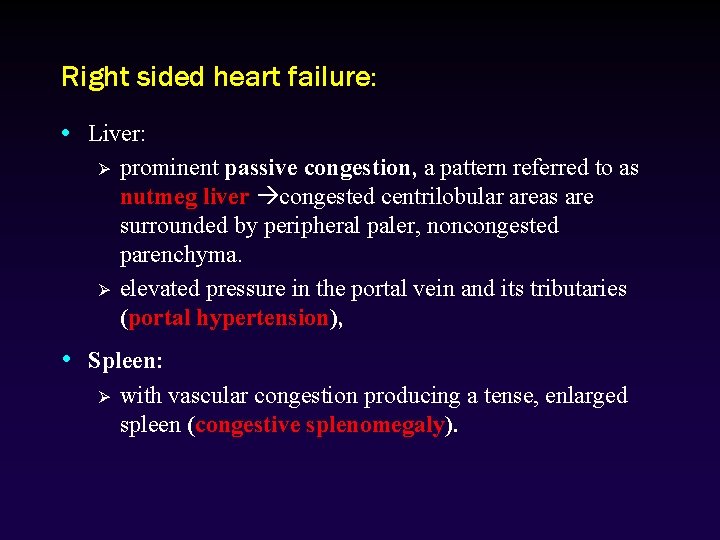
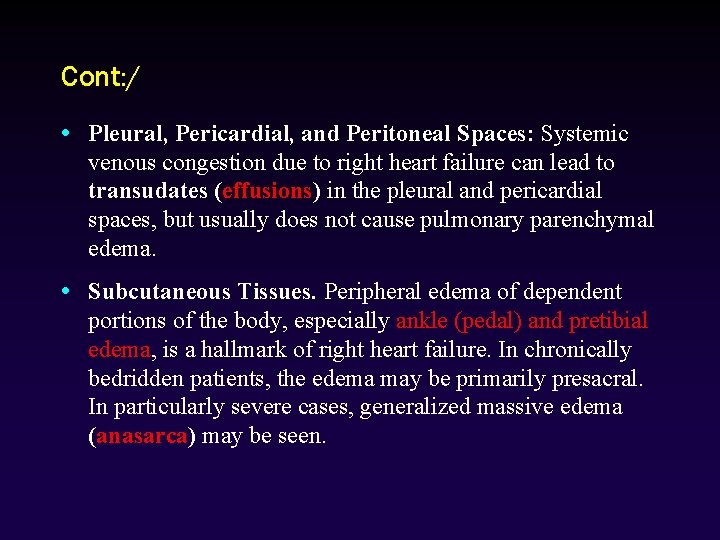
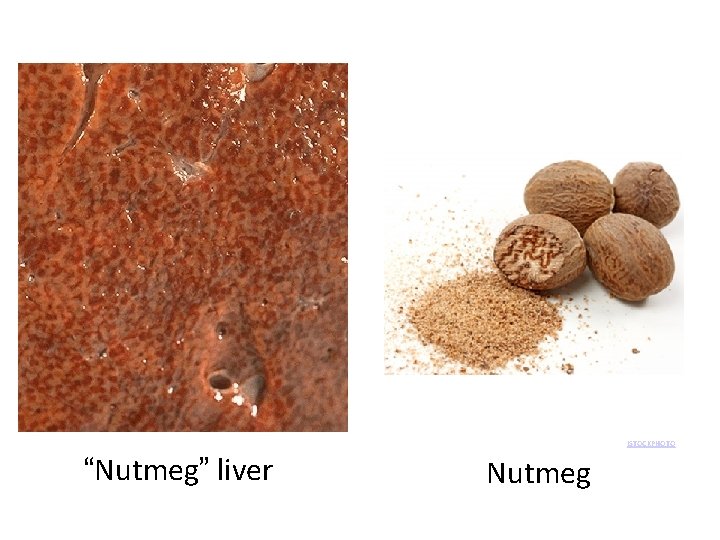
Right sided heart failure: • Liver: Ø Ø prominent passive congestion, a pattern referred to as nutmeg liver congested centrilobular areas are surrounded by peripheral paler, noncongested parenchyma. elevated pressure in the portal vein and its tributaries (portal hypertension), • Spleen: Ø with vascular congestion producing a tense, enlarged spleen (congestive splenomegaly).
Cont: / • Pleural, Pericardial, and Peritoneal Spaces: Systemic venous congestion due to right heart failure can lead to transudates (effusions) in the pleural and pericardial spaces, but usually does not cause pulmonary parenchymal edema. • Subcutaneous Tissues. Peripheral edema of dependent portions of the body, especially ankle (pedal) and pretibial edema, is a hallmark of right heart failure. In chronically bedridden patients, the edema may be primarily presacral. In particularly severe cases, generalized massive edema (anasarca) may be seen.
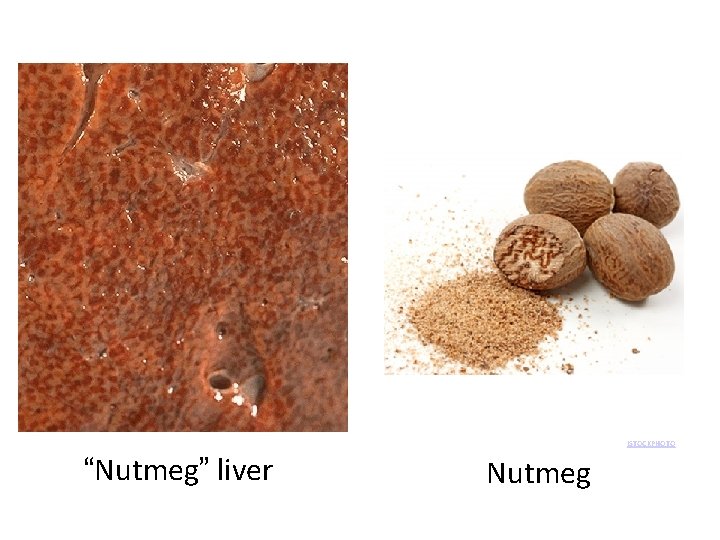
© AL G ISTOCKPHOTO/E “Nutmeg” liver Nutmeg
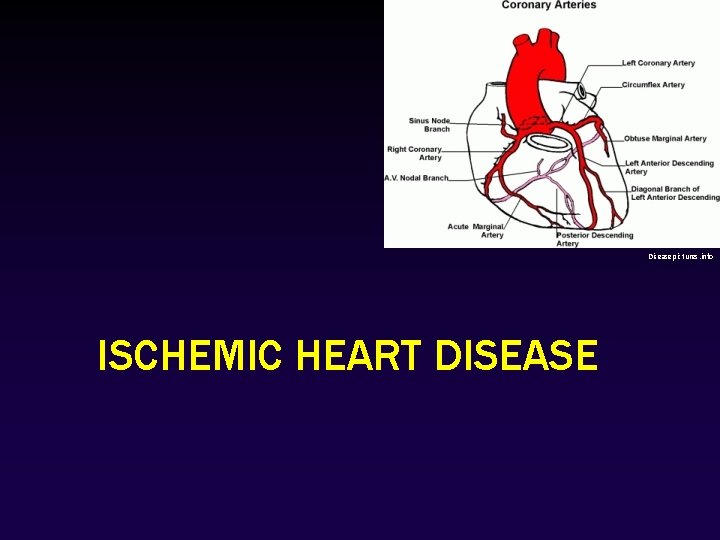
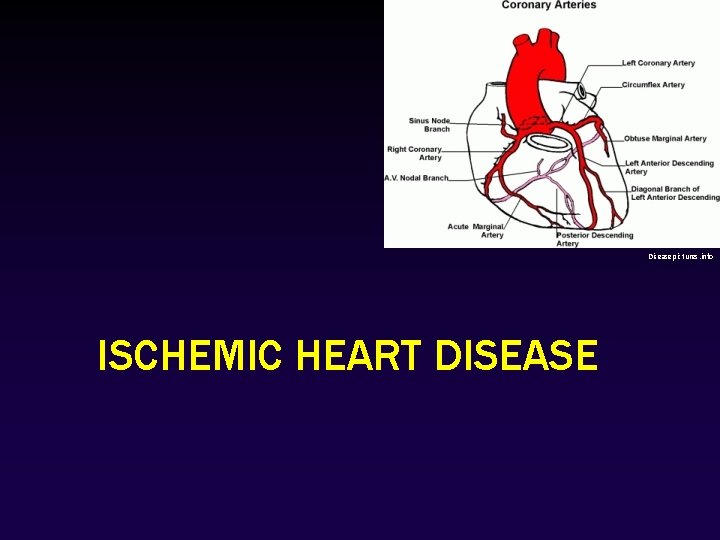
Diseasepictures. info ISCHEMIC HEART DISEASE
Ischemic Heart Disease • It’s a leading cause of mortality in the United States and other developed nations, accounting for 7 million deaths worldwide each year. It happens when Myocardial perfusion can’t meet demand
Ischemic Heart Disease • clinical syndromes: – Angina – Acute myocardial infarction – Chronic IHD with CHF – Sudden cardiac death
Clinical syndromes • Angina pectoris (literally, “chest pain” 0: Ischemia induces pain but is insufficient to cause myocyte death. • Acute myocardial infarction (MI): The severity or duration of ischemia is sufficient to cause myocyte death. • Chronic IHD with CHF: Progressive cardiac decompensation eventually precipitates mechanical pump failure. • Sudden cardiac death (SCD): results mostly from a lethal arrhythmia without myocyte necrosis
Angina can be: ü stable (occurring at certain levels of exertion), ü Prinzmetal angina caused by vessel spasm ü unstable (occurring with less exertion or at rest).
Cardiac syndromes The term ACUTE CORONARY SYNDROME is applied to any of this three catastrophic manifestations of IHD: unstable angina, acute MI, and SCD
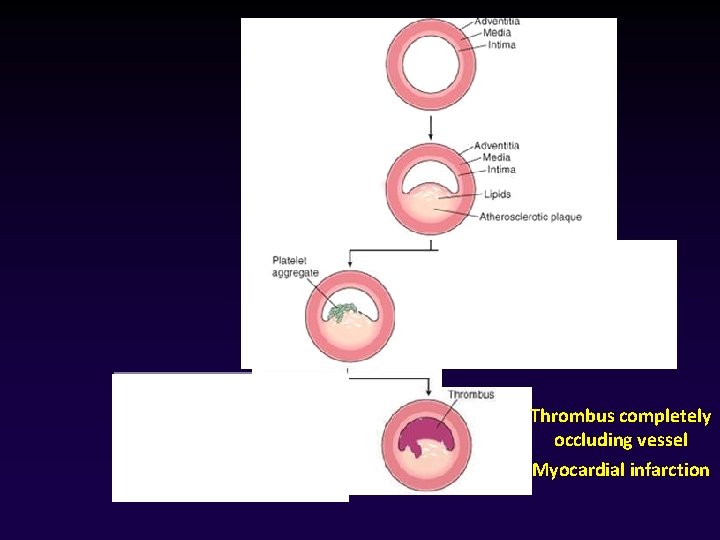
PATHOGENESIS • IHD is a consequence of inadequate coronary perfusion relative to myocardial demand. • It’s a consequence of the combination of preexisting (“fixed”) atherosclerotic occlusion of coronary arteries and new, superimposed thrombosis and/or vasospasm.
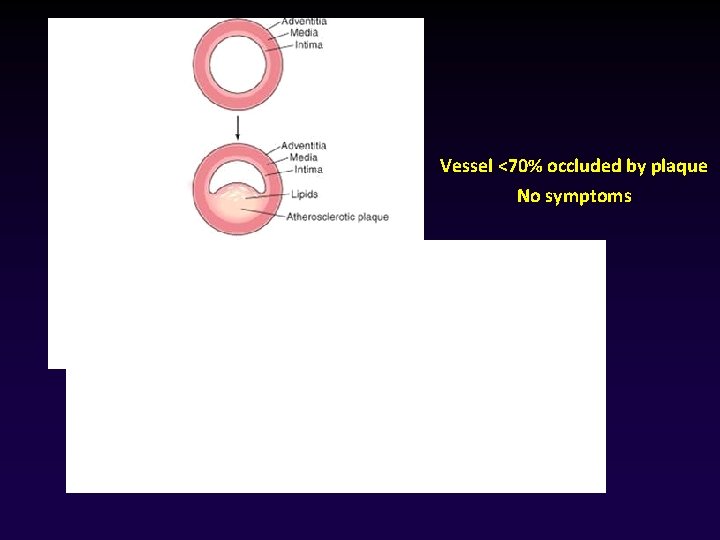
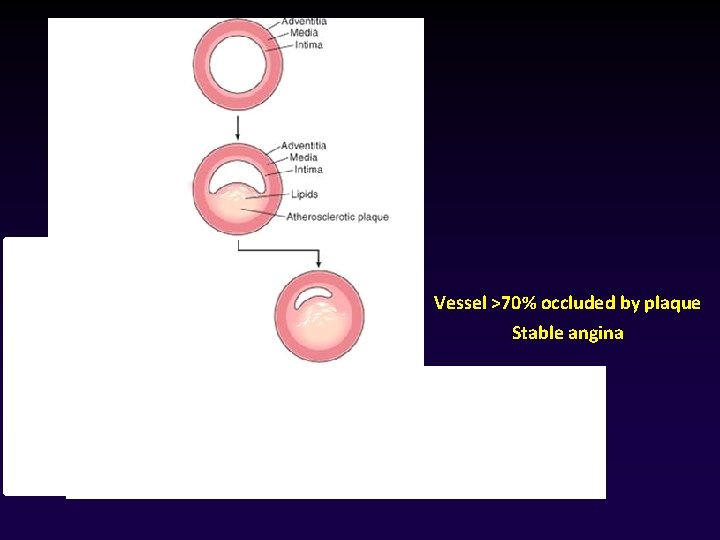
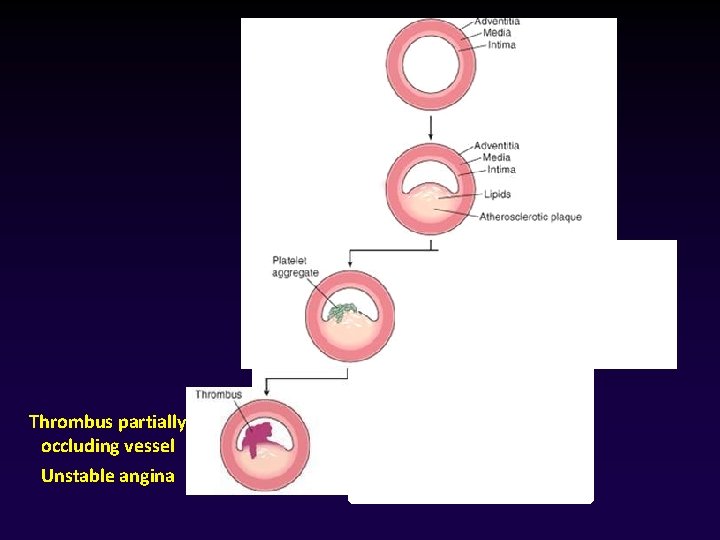
• Fixed obstructions that occlude < 70% of a coronary vessel lumen typically are asymptomatic, even with exertion. • CRITICAL STENOSIS lesions occluding > 70% of a vessel lumen & cause symptoms with increased demand STABLE ANGINA happens when there is occlusion of > 70% of a vessel lumen at certain level of exertion UNSTABLE ANGINA happens with fixed stenosis occluding > 90% of a vascular lumen
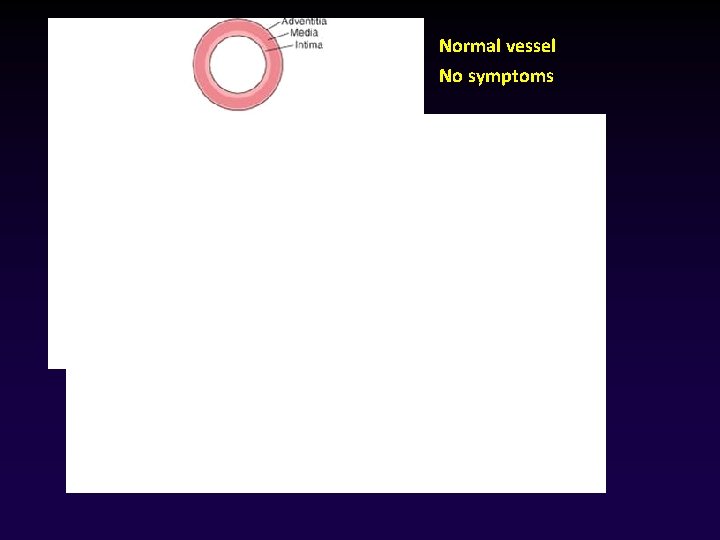
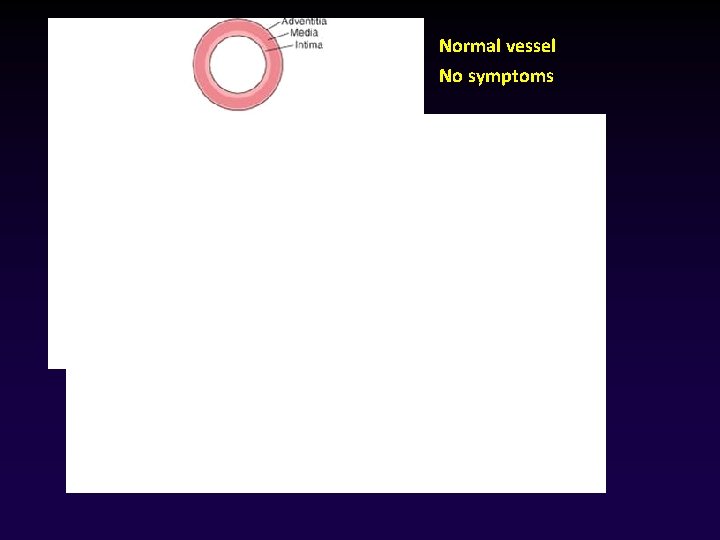
Normal vessel No symptoms
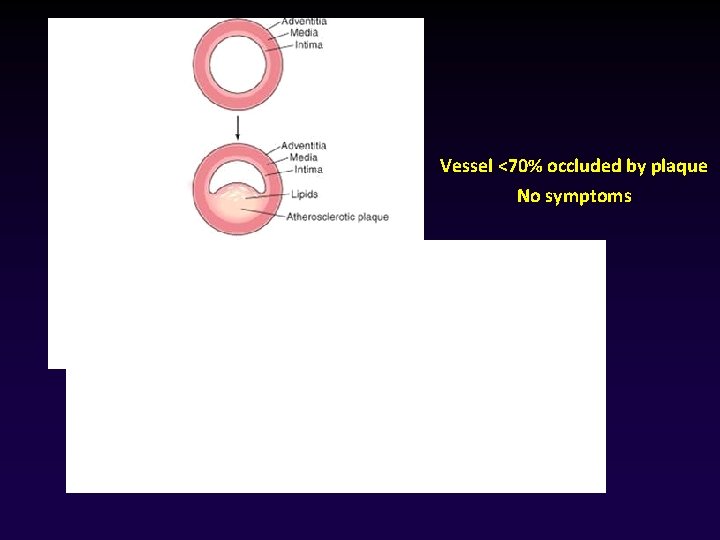
Vessel <70% occluded by plaque No symptoms
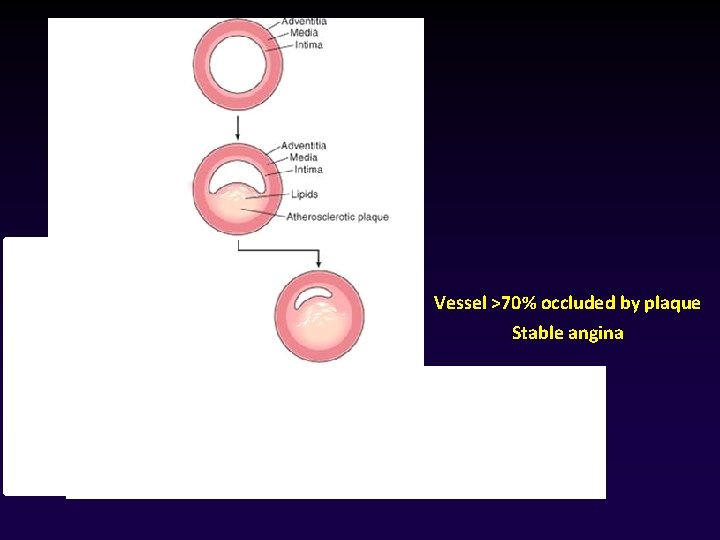
Vessel >70% occluded by plaque Stable angina
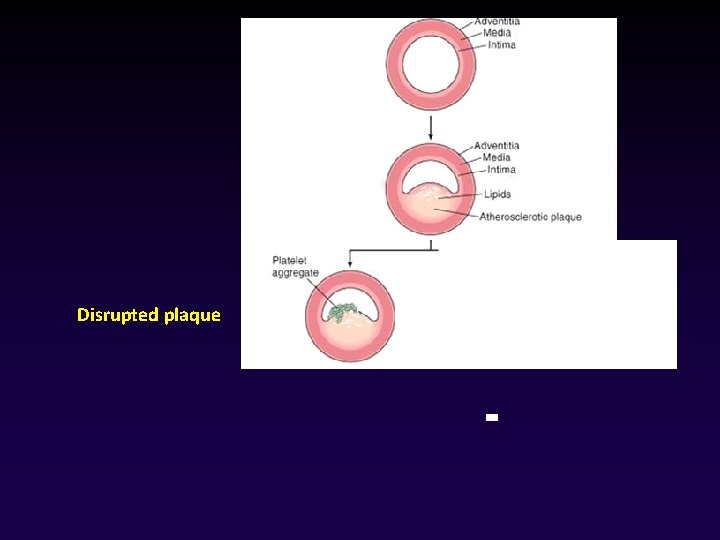
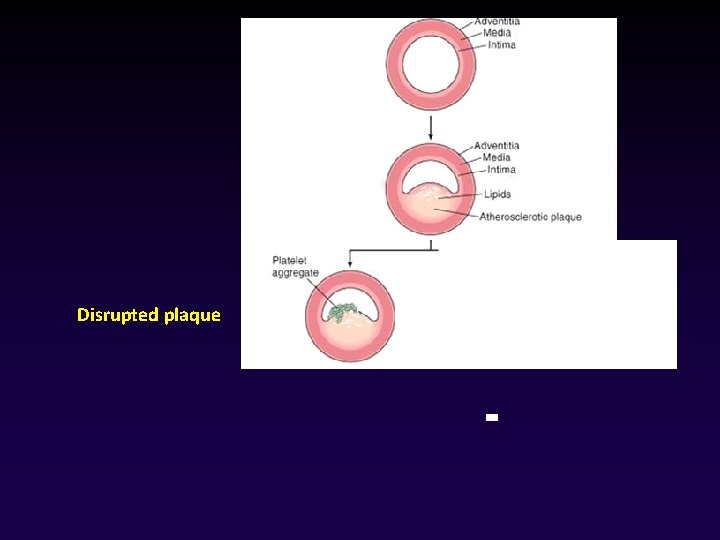
Disrupted plaque
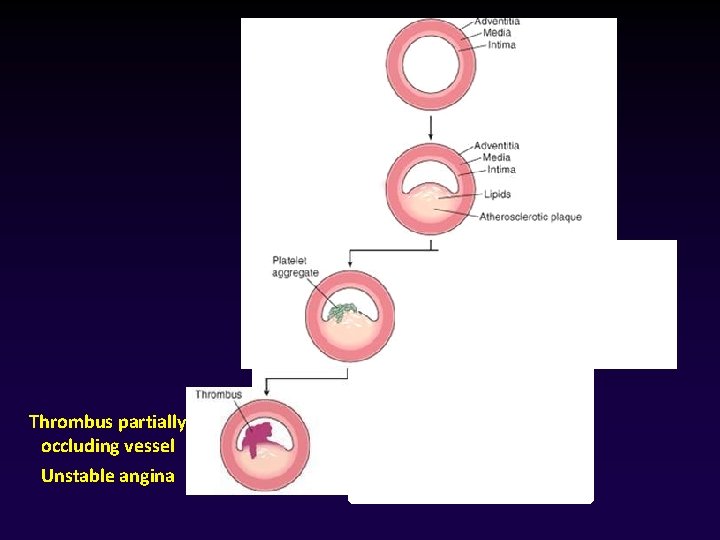
Thrombus partially occluding vessel Unstable angina
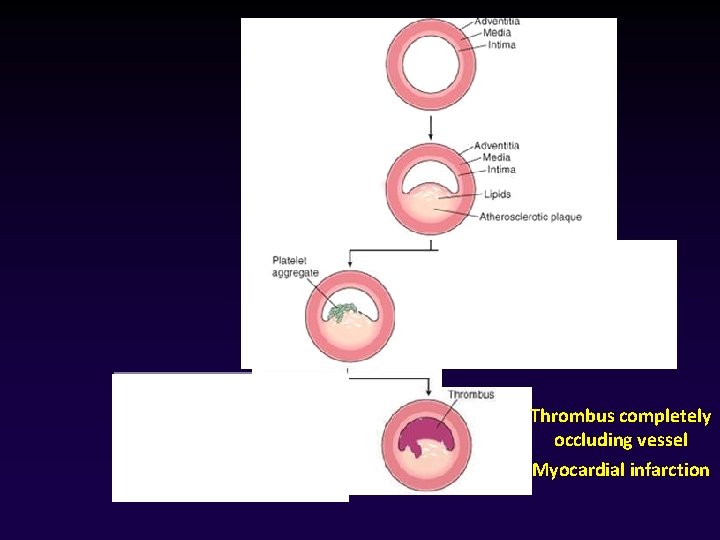
Thrombus completely occluding vessel Myocardial infarction
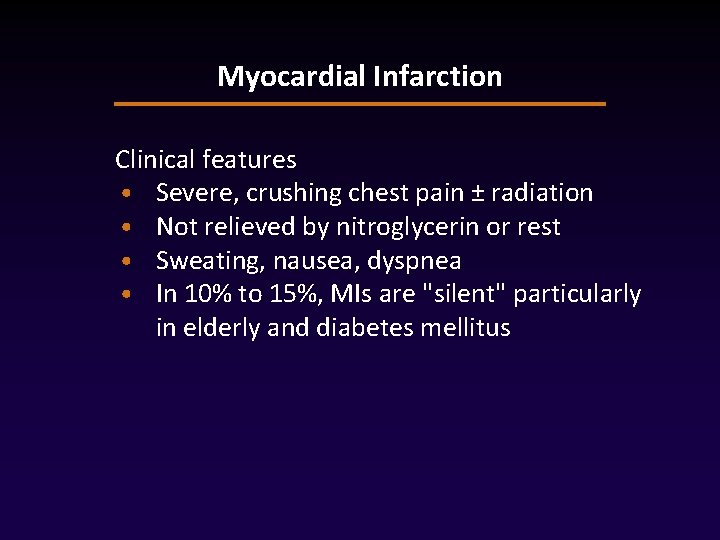
Myocardial Infarction Clinical features • Severe, crushing chest pain ± radiation • Not relieved by nitroglycerin or rest • Sweating, nausea, dyspnea • In 10% to 15%, MIs are "silent" particularly in elderly and diabetes mellitus
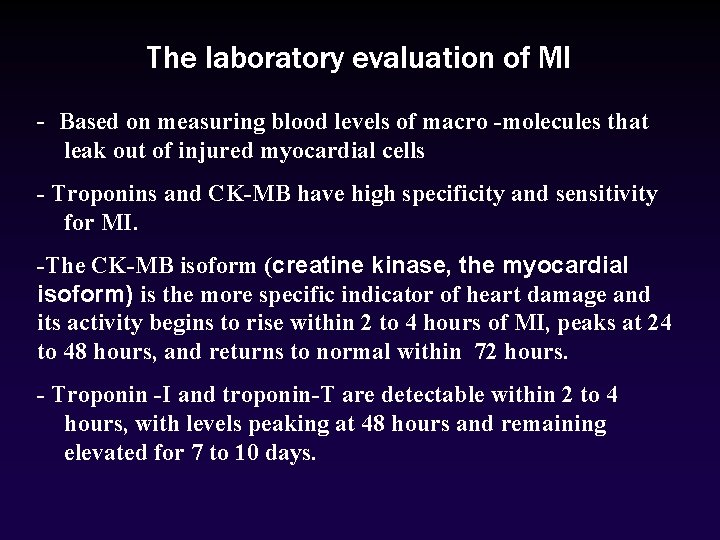
The laboratory evaluation of MI - Based on measuring blood levels of macro -molecules that leak out of injured myocardial cells - Troponins and CK-MB have high specificity and sensitivity for MI. -The CK-MB isoform (creatine kinase, the myocardial isoform) is the more specific indicator of heart damage and its activity begins to rise within 2 to 4 hours of MI, peaks at 24 to 48 hours, and returns to normal within 72 hours. - Troponin -I and troponin-T are detectable within 2 to 4 hours, with levels peaking at 48 hours and remaining elevated for 7 to 10 days.
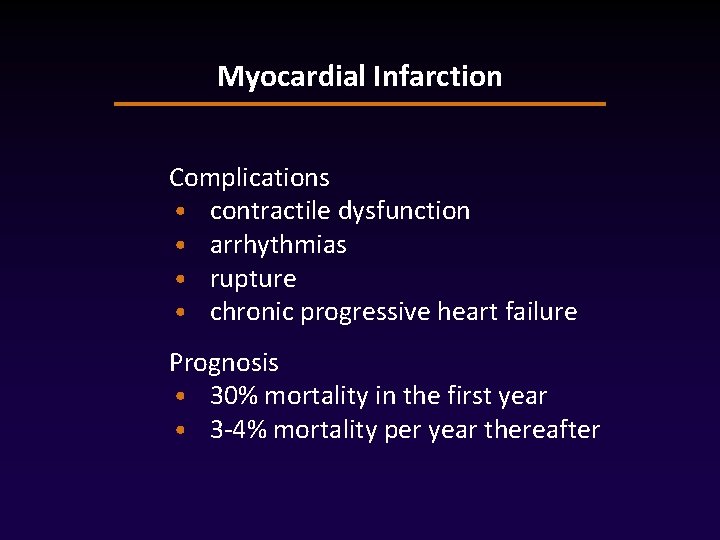
Myocardial Infarction Complications • contractile dysfunction • arrhythmias • rupture • chronic progressive heart failure Prognosis • 30% mortality in the first year • 3 -4% mortality per year thereafter
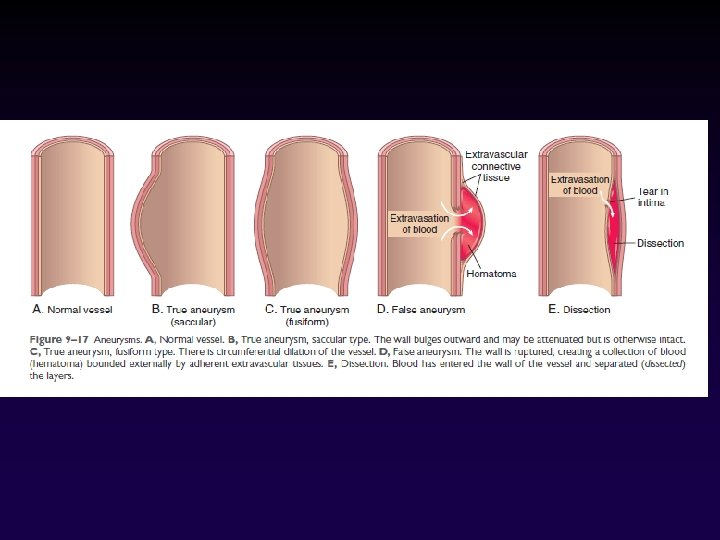
Aneurysms • Aneurysms are congenital or acquired dilations of blood vessels or the heart. • “True” aneurysms involve all three layers of the artery or the attenuated wall of the heart (intima, media, and adventitia) • True aneurysm include atherosclerotic, congenital and ventricular aneurysms • False aneurysm (pseudoaneurysm): a wall defect leads to the formation of an extravascular hematoma that communicates with the intravascular space (“pulsating hematoma”).
• Aneurysms can be classified by shape: Ø Saccular aneurysms: are discrete outpouchings (5 to 20 cm) often with a contained thrombus. Ø Fusiform aneurysms: are circumferential dilations (up to 20 cm) in diameter. most commonly involve: aortic arch, abdominal aorta, or iliac arteries.
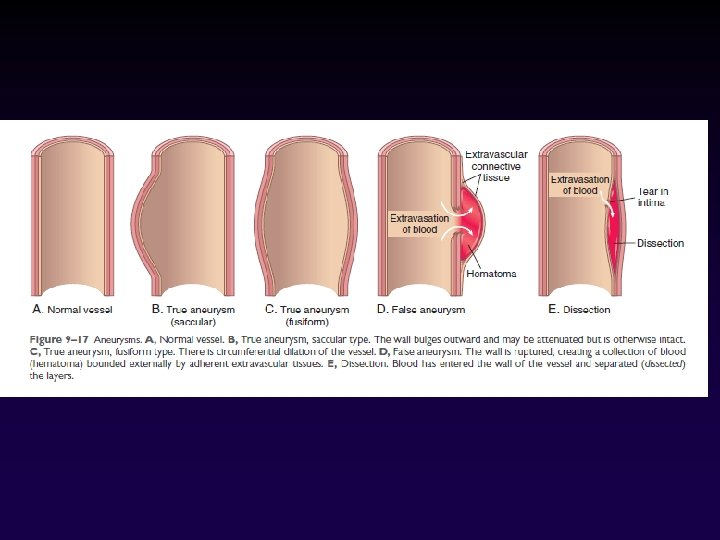
arterial dissections • It happens when pressurized blood gains entry to the arterial wall through a surface defect and then pushes apart the underlying layers. • Aneurysms and dissections are important causes of stasis thrombosis
THANK YOU