Practical Electrocardiography Rate and Rhythm Scott E Ewing




- Slides: 116
Practical Electrocardiography - Rate and Rhythm Scott E. Ewing DO Interventional Cardiology Fellow Lecture #2
Review Electrophysiology n Anatomy n Depolarization n EKG Paper n Lead Placement n Normal EKG n Waves / Intervals / Segments n
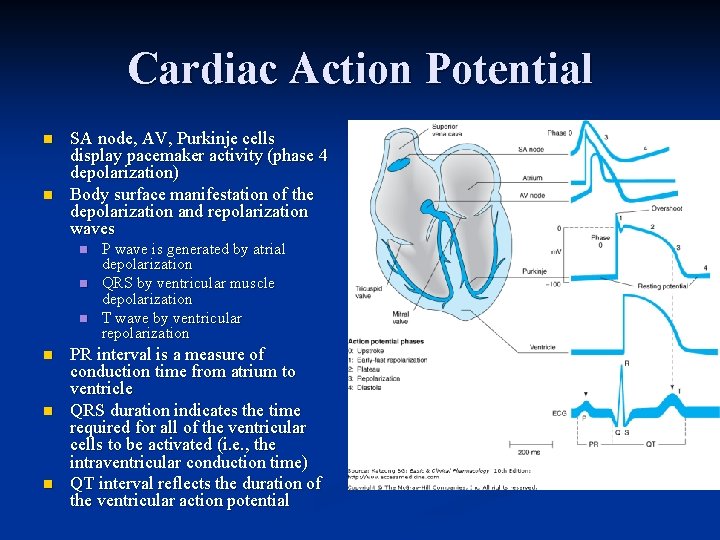
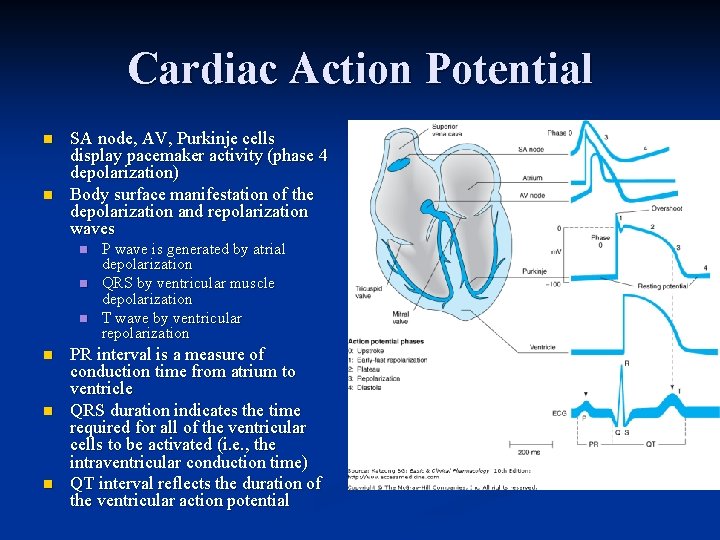
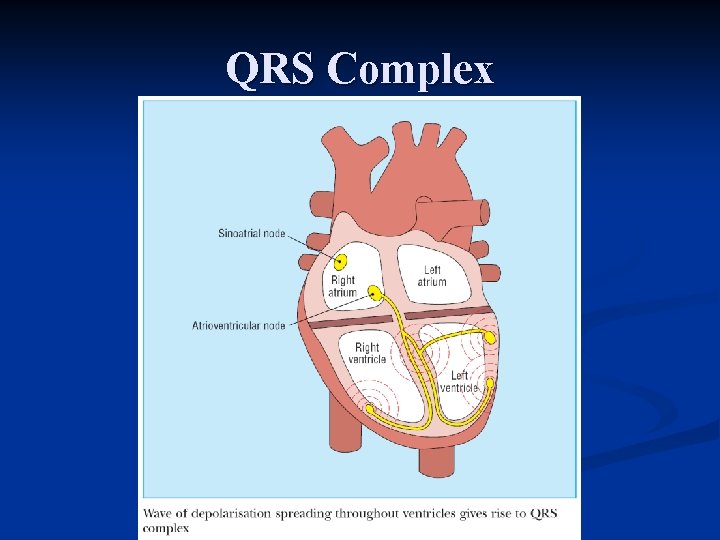
Cardiac Action Potential n n SA node, AV, Purkinje cells display pacemaker activity (phase 4 depolarization) Body surface manifestation of the depolarization and repolarization waves n n n P wave is generated by atrial depolarization QRS by ventricular muscle depolarization T wave by ventricular repolarization PR interval is a measure of conduction time from atrium to ventricle QRS duration indicates the time required for all of the ventricular cells to be activated (i. e. , the intraventricular conduction time) QT interval reflects the duration of the ventricular action potential
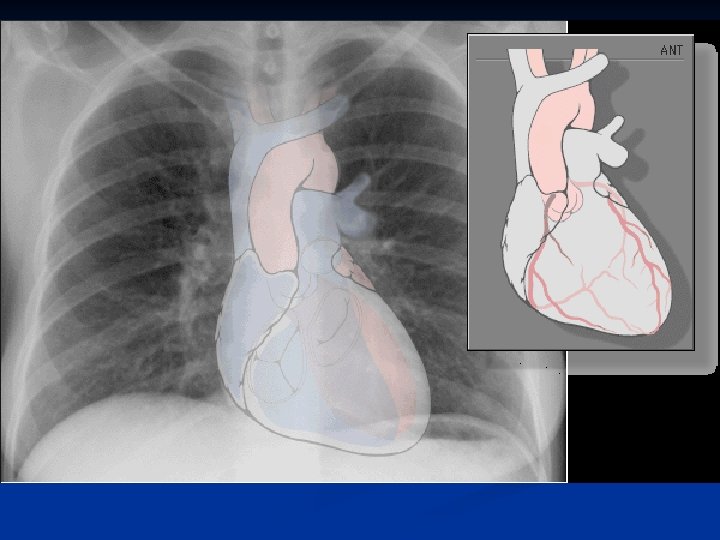
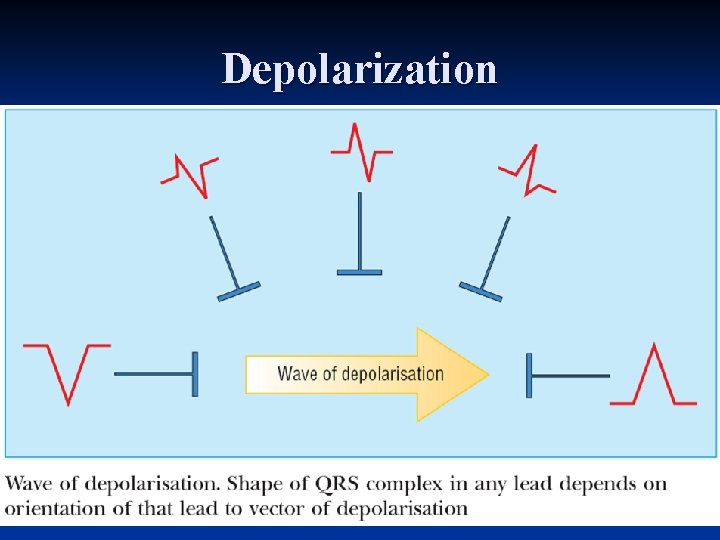
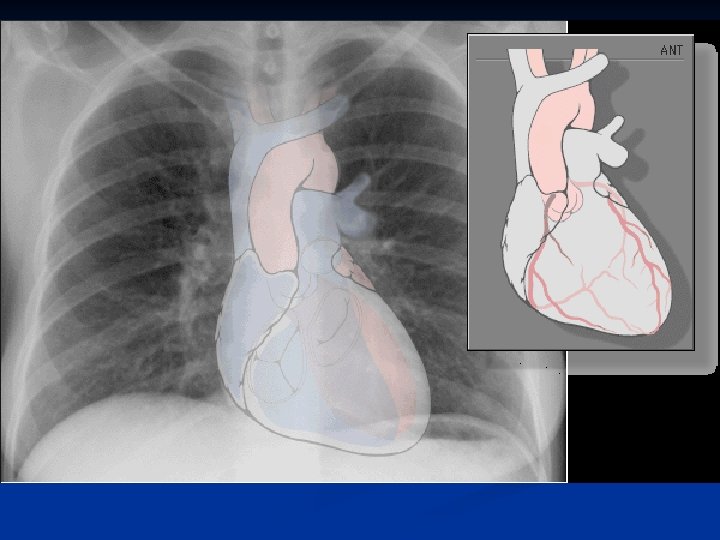
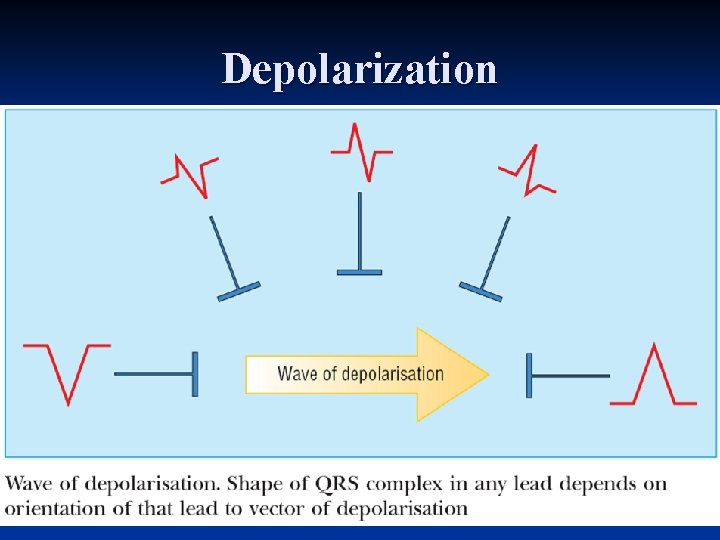
Depolarization
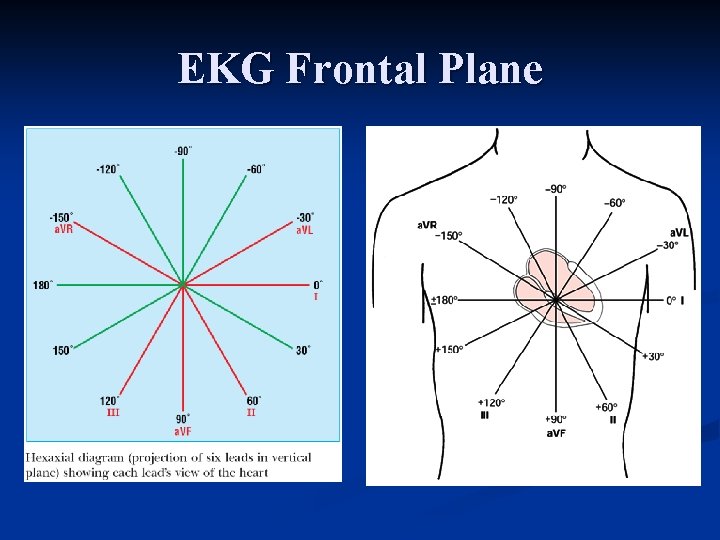
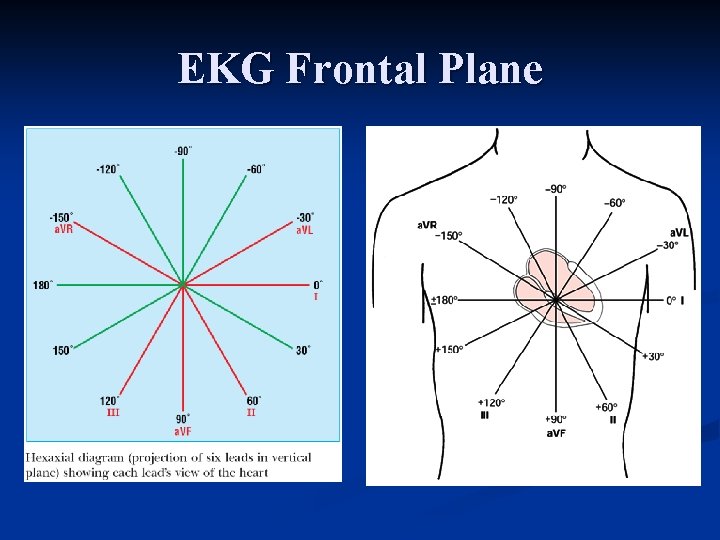
EKG Frontal Plane
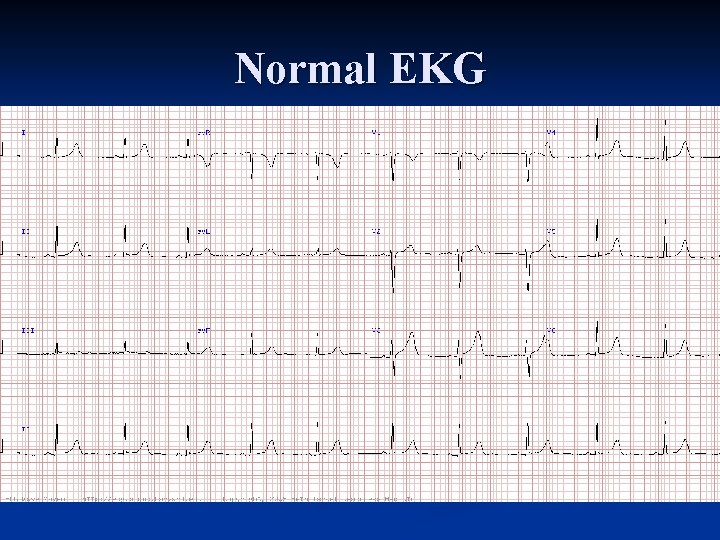
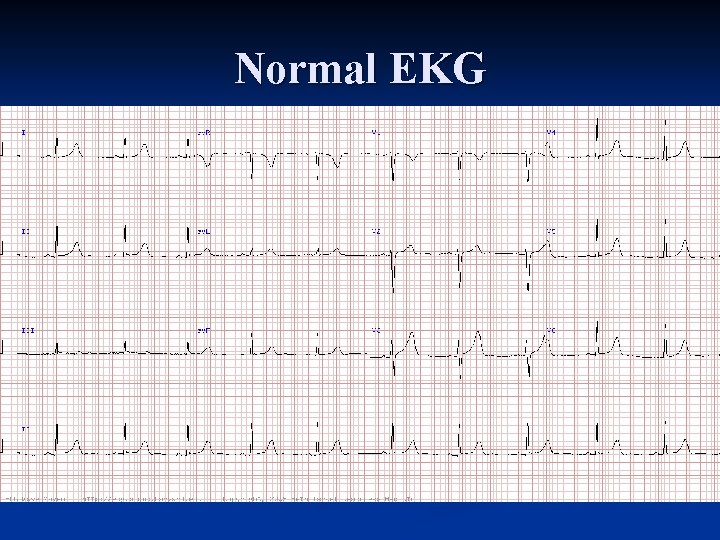
Normal EKG
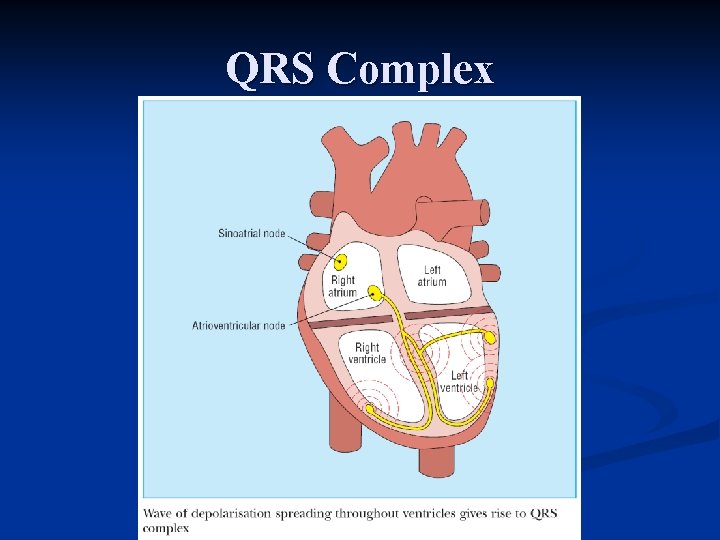
QRS Complex
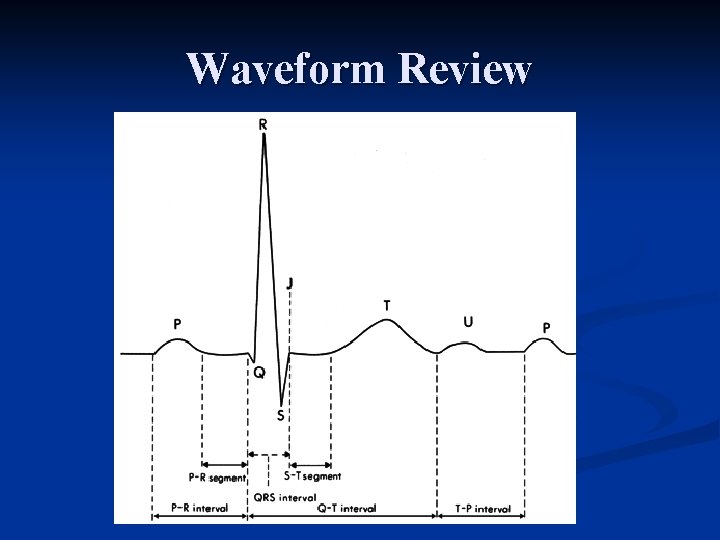
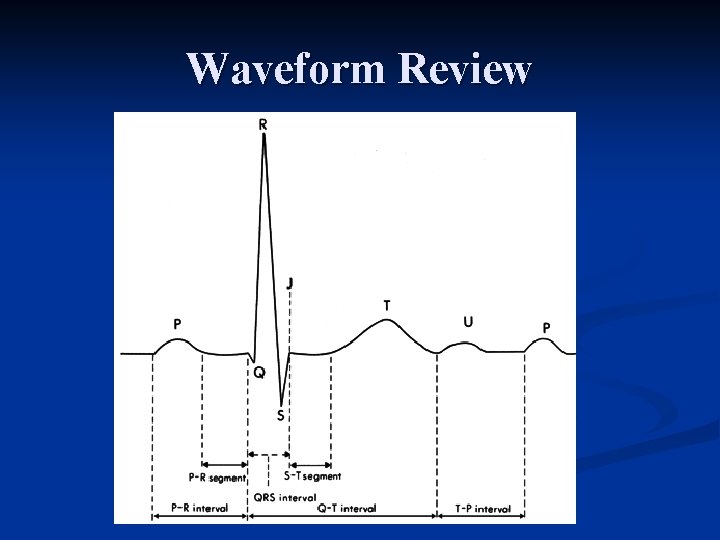
Waveform Review
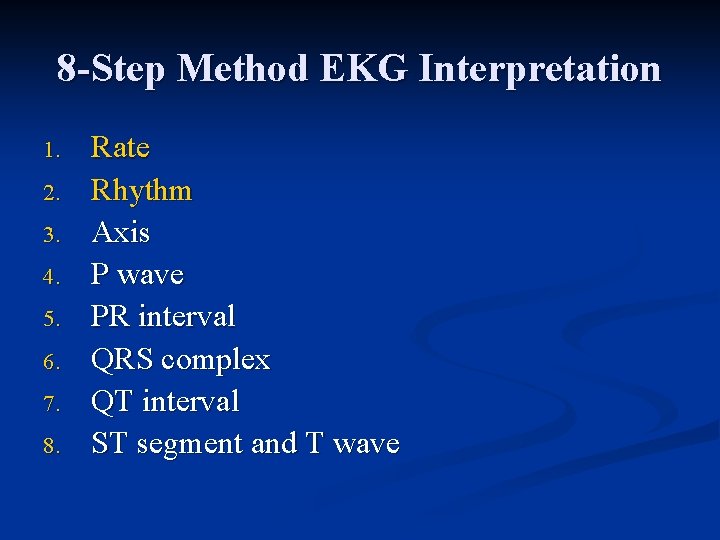
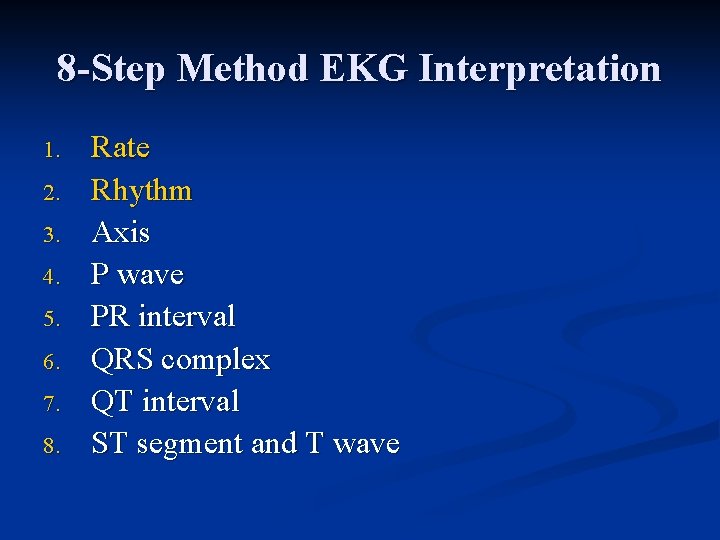
8 -Step Method EKG Interpretation 1. 2. 3. 4. 5. 6. 7. 8. Rate Rhythm Axis P wave PR interval QRS complex QT interval ST segment and T wave
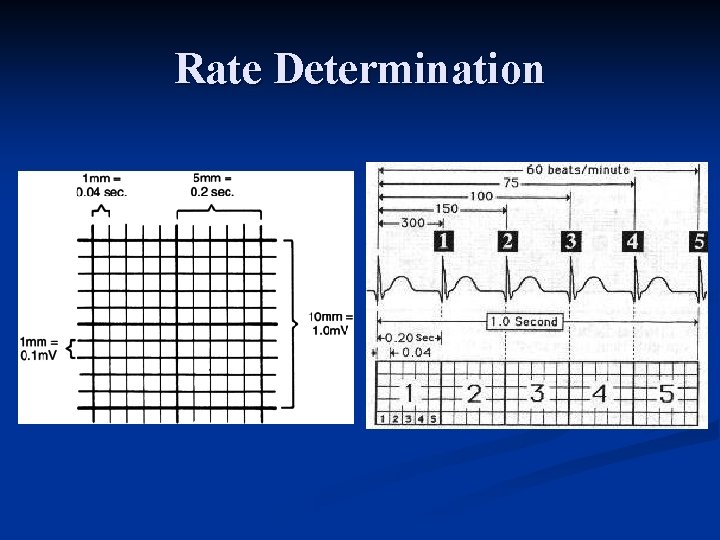
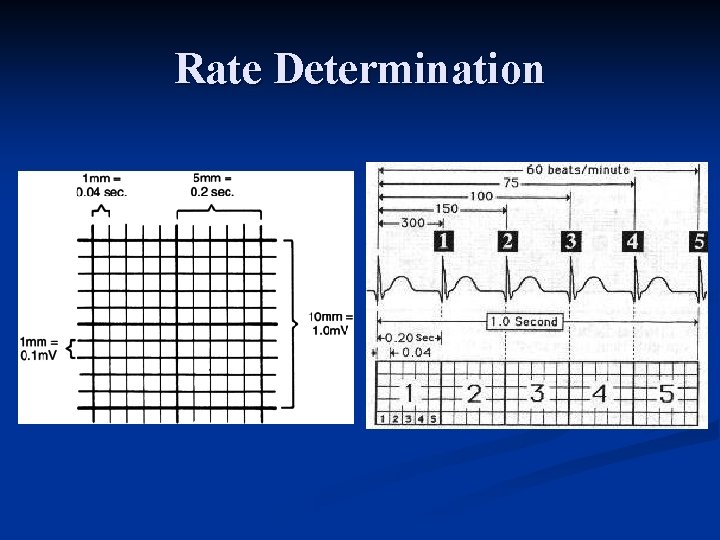
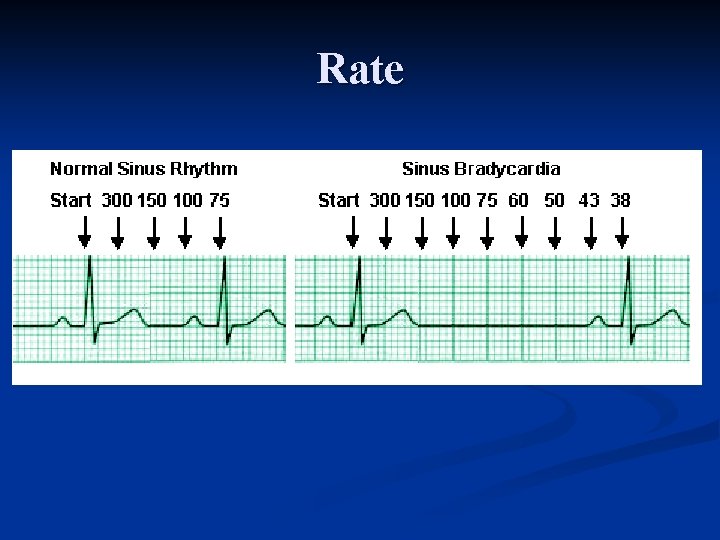
Rate Determination
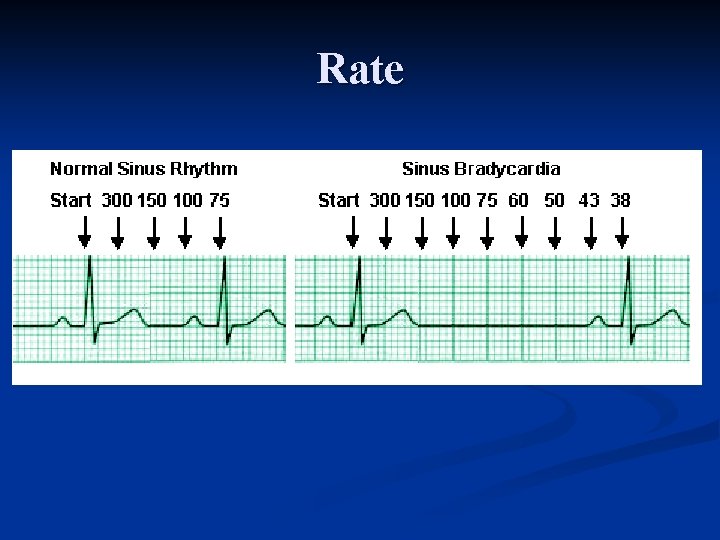
Rate
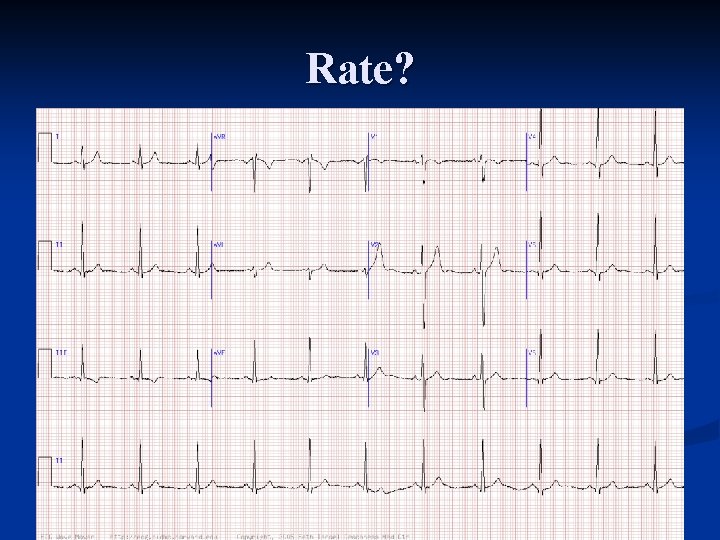
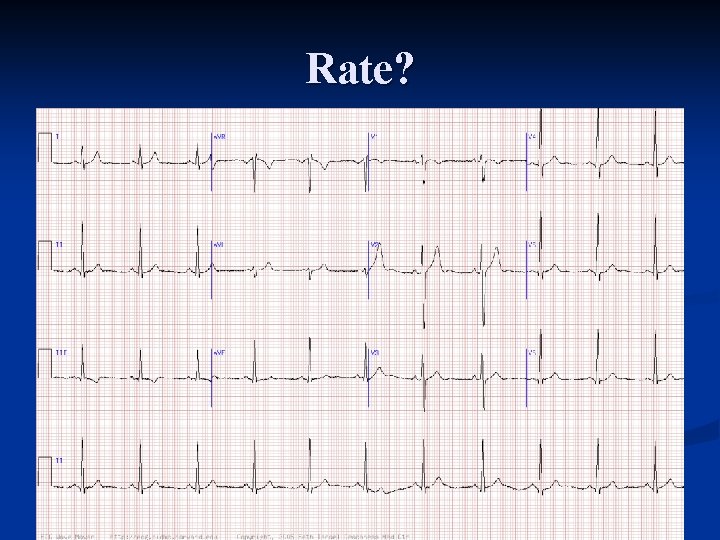
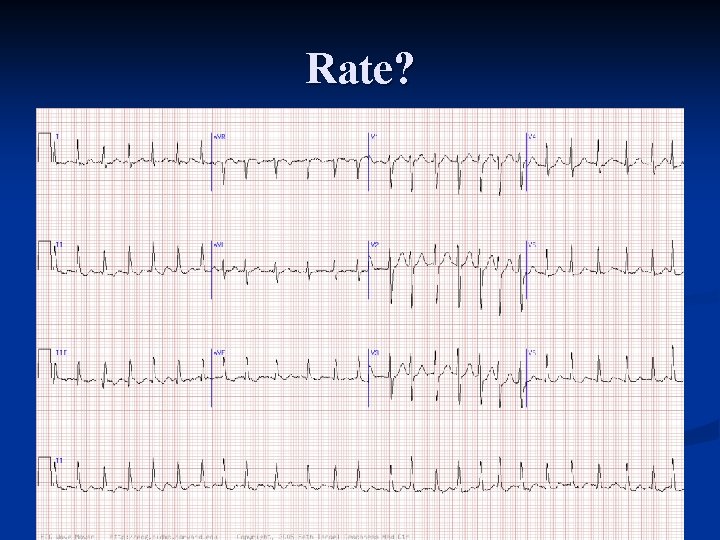
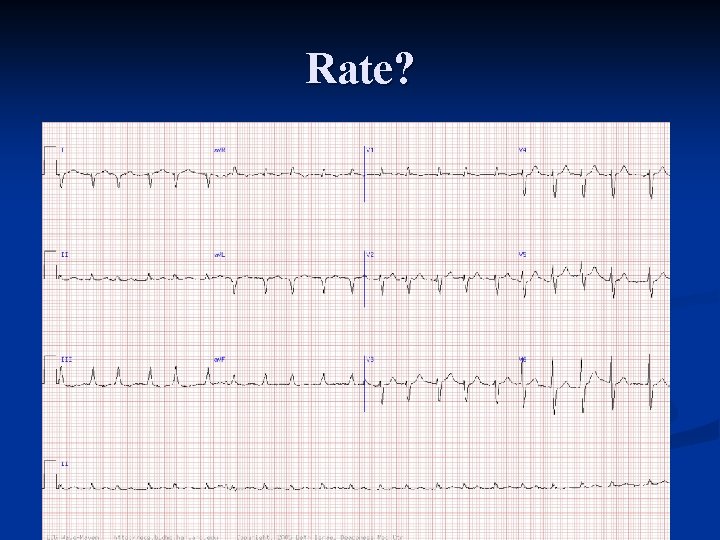
Rate?
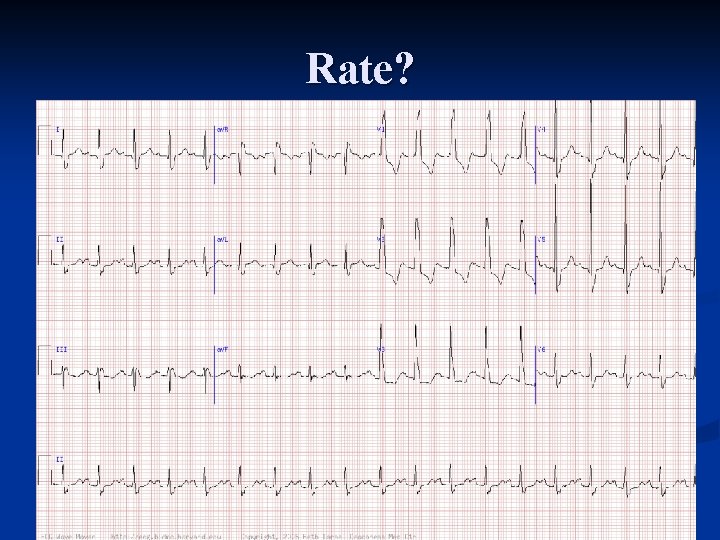
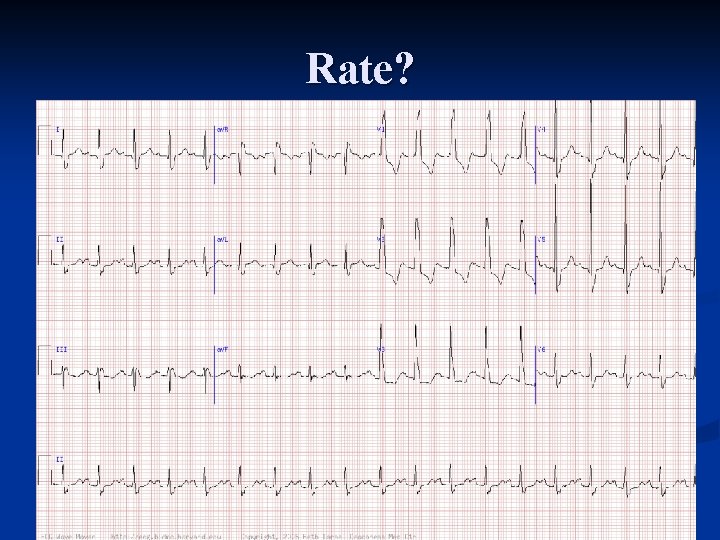
Rate?
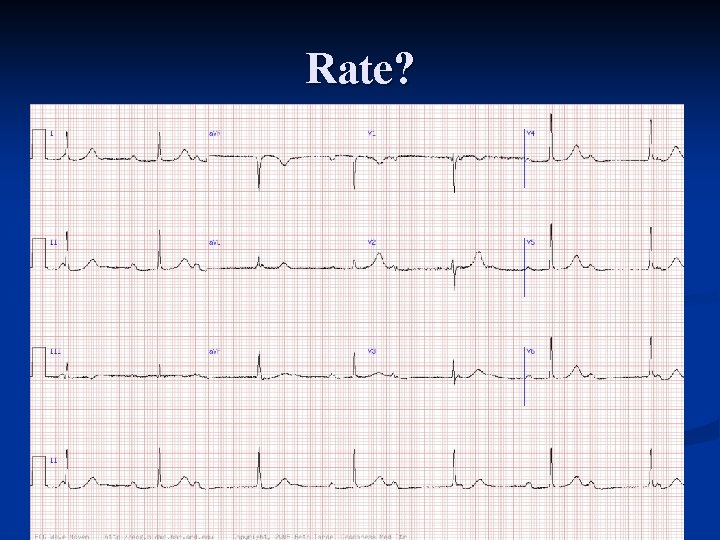
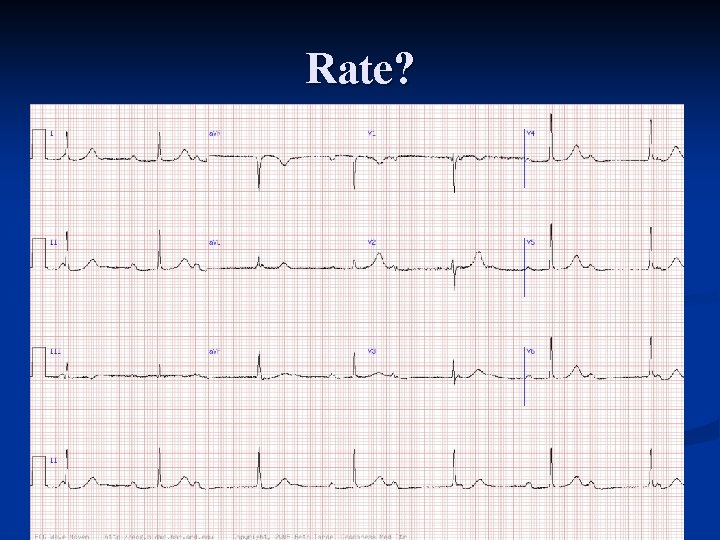
Rate?
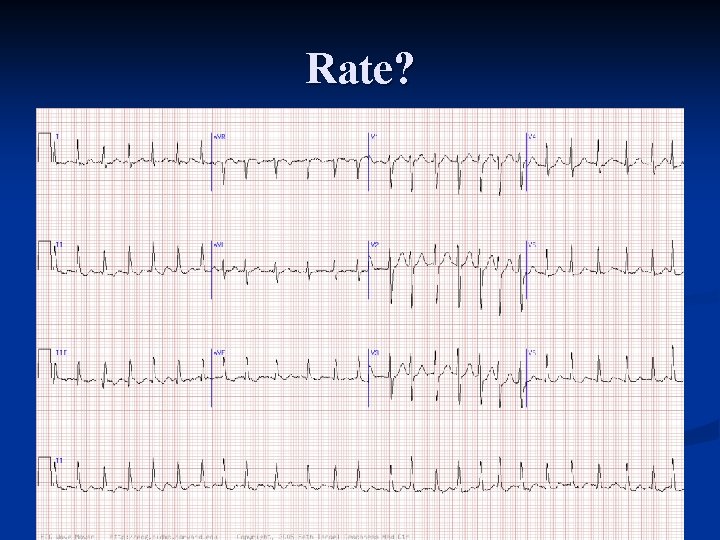
Rate?
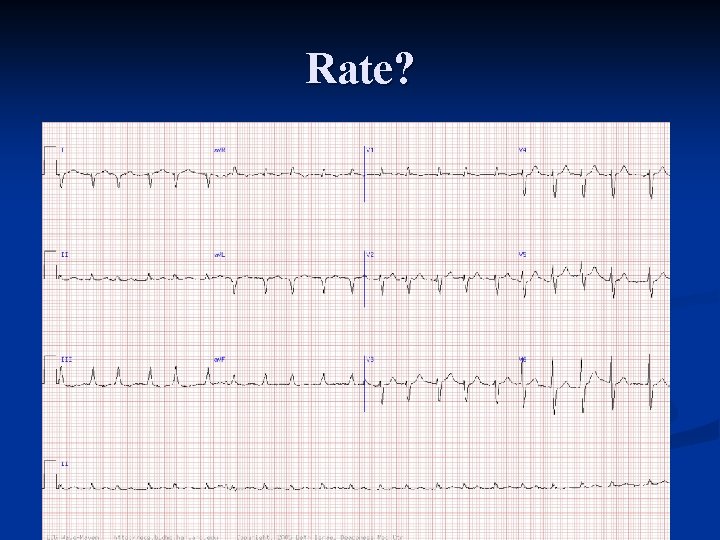
Rate?
Rhythm Atrial n Junctional n Ventricular n Pacemaker n Last but not least n
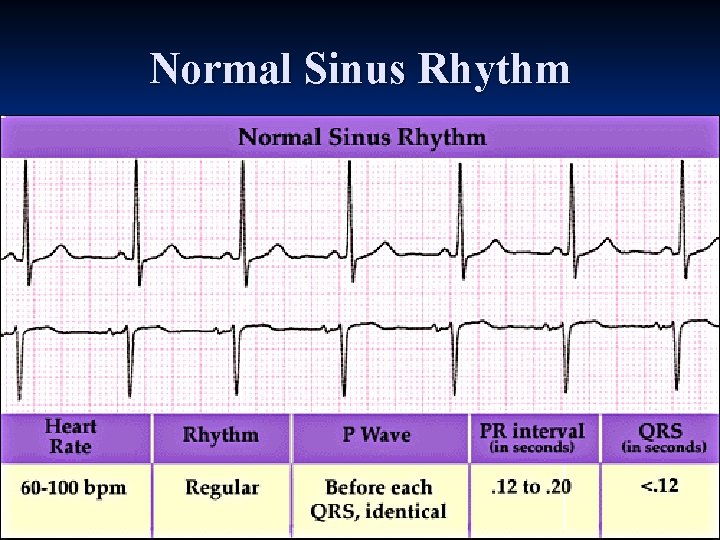
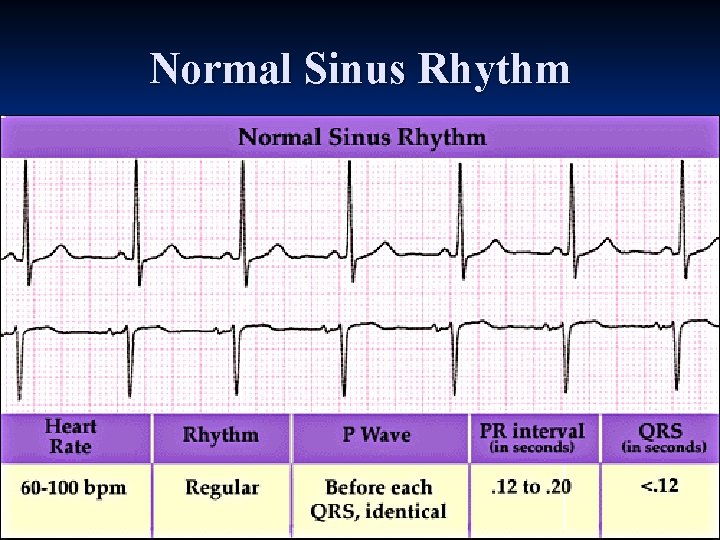
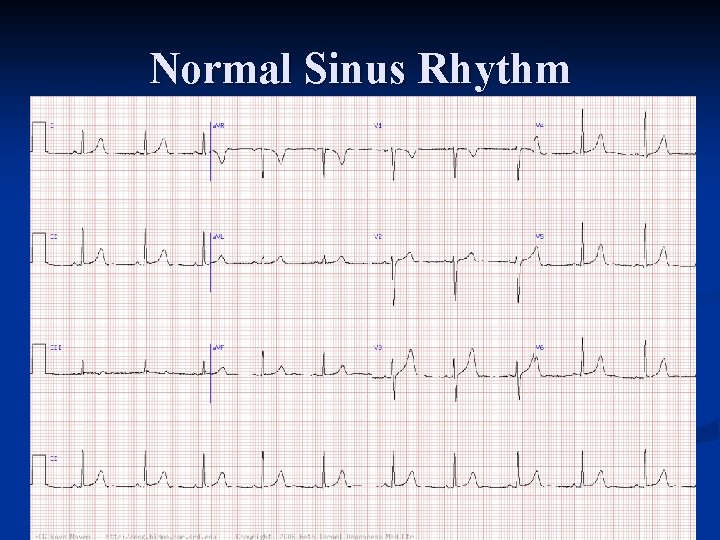
Normal Sinus Rhythm
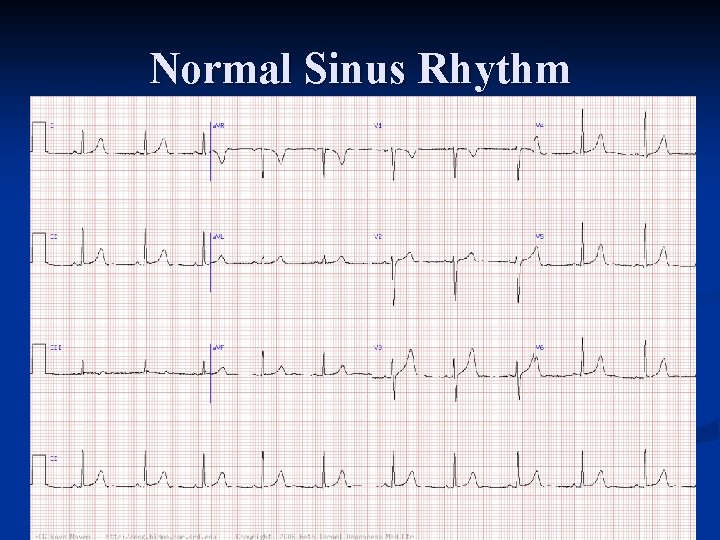
Normal Sinus Rhythm
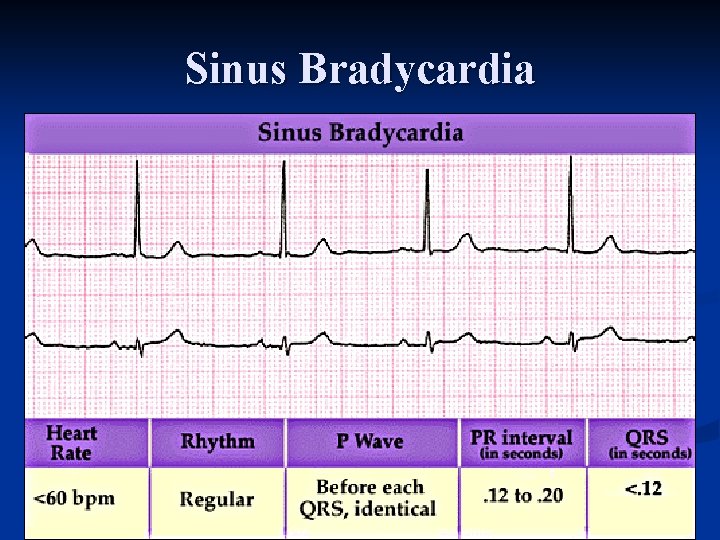
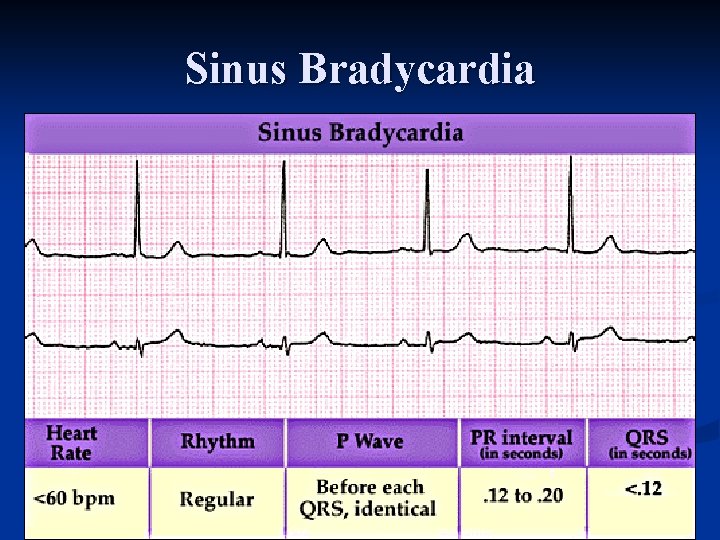
Sinus Bradycardia
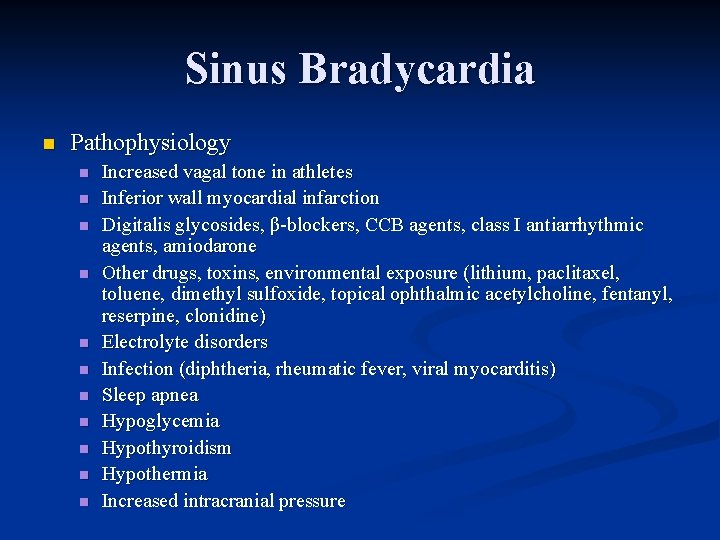
Sinus Bradycardia n Pathophysiology n n n Increased vagal tone in athletes Inferior wall myocardial infarction Digitalis glycosides, β blockers, CCB agents, class I antiarrhythmic agents, amiodarone Other drugs, toxins, environmental exposure (lithium, paclitaxel, toluene, dimethyl sulfoxide, topical ophthalmic acetylcholine, fentanyl, reserpine, clonidine) Electrolyte disorders Infection (diphtheria, rheumatic fever, viral myocarditis) Sleep apnea Hypoglycemia Hypothyroidism Hypothermia Increased intracranial pressure
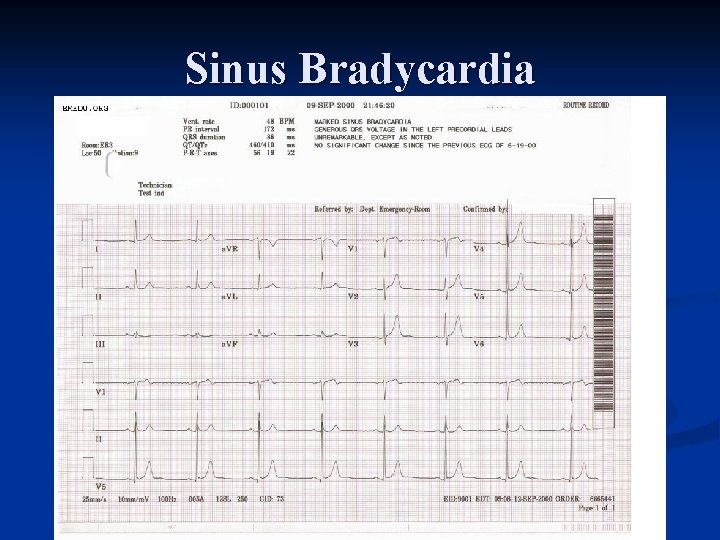
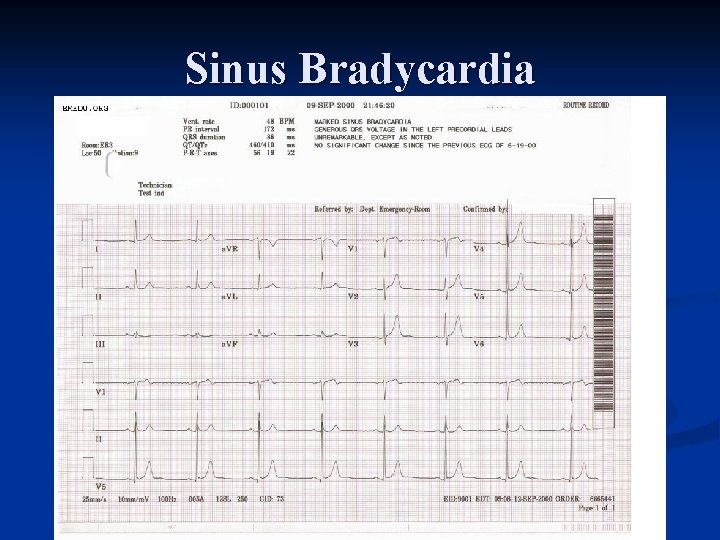
Sinus Bradycardia
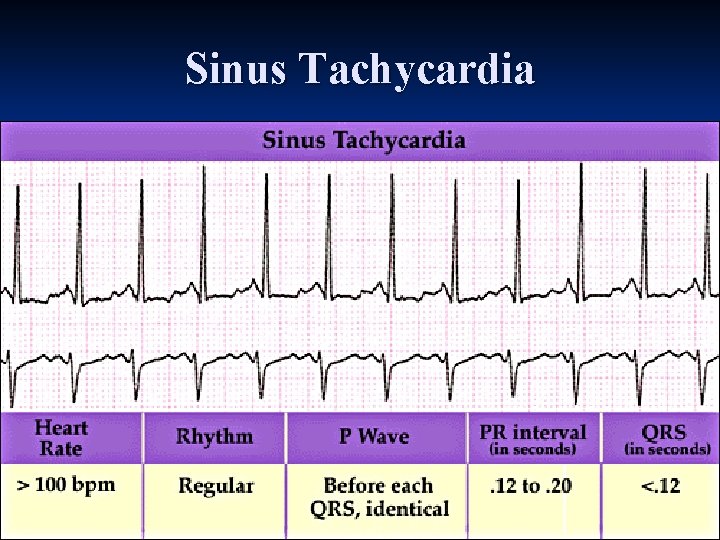
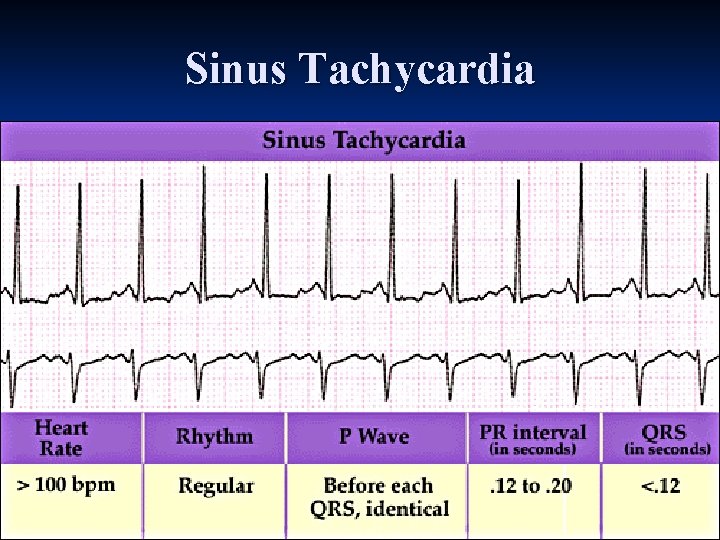
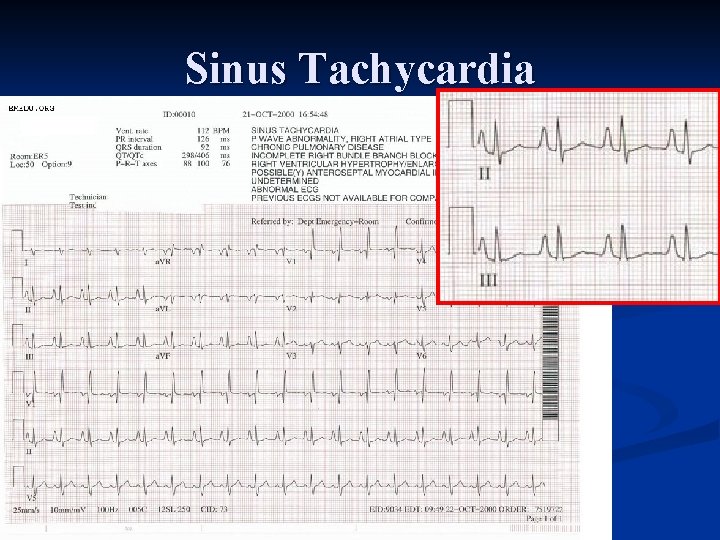
Sinus Tachycardia
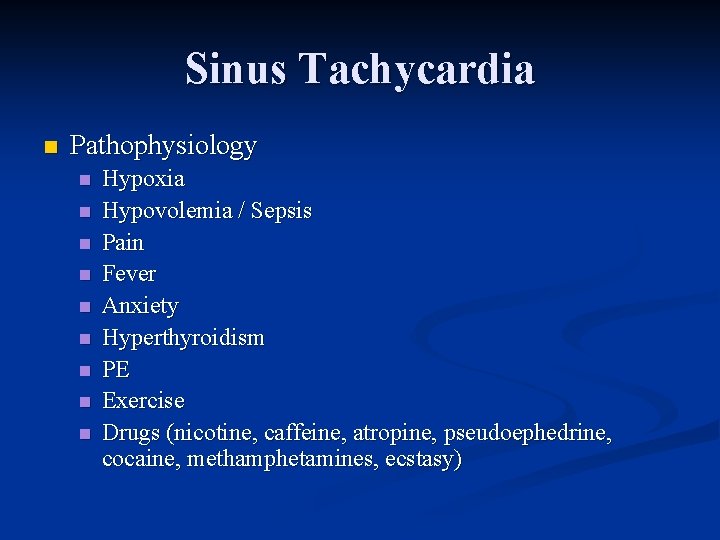
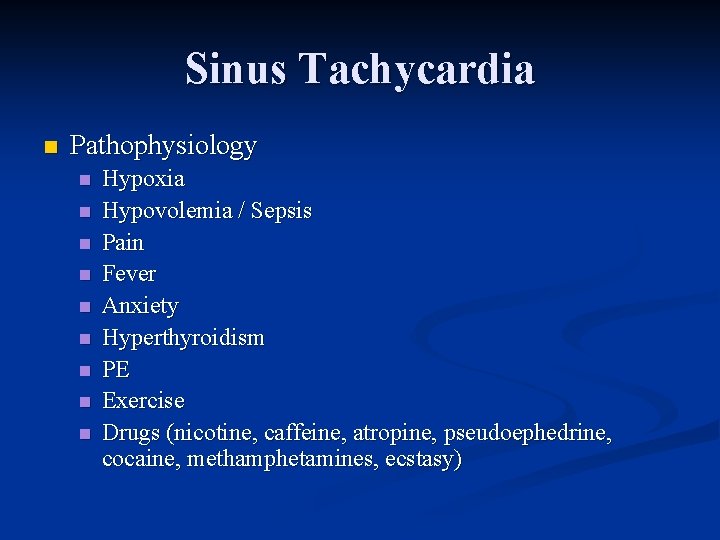
Sinus Tachycardia n Pathophysiology n n n n n Hypoxia Hypovolemia / Sepsis Pain Fever Anxiety Hyperthyroidism PE Exercise Drugs (nicotine, caffeine, atropine, pseudoephedrine, cocaine, methamphetamines, ecstasy)
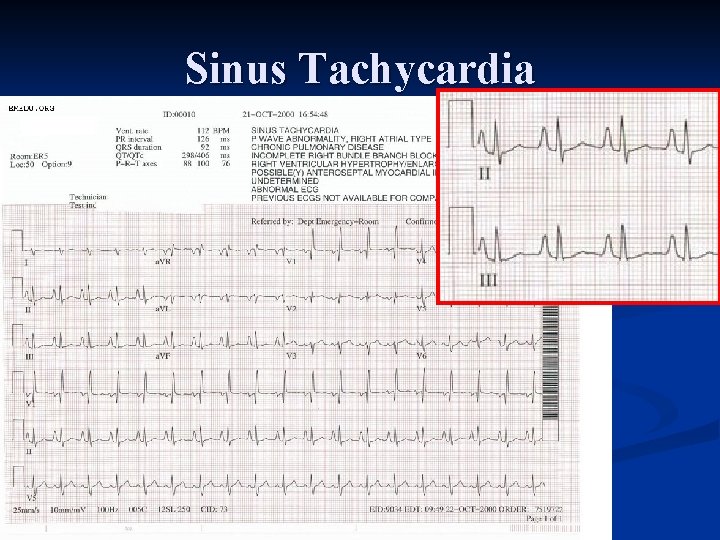
Sinus Tachycardia
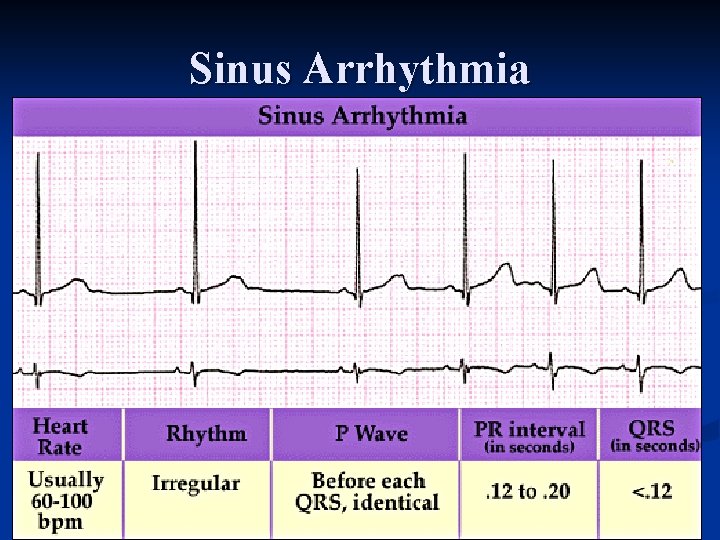
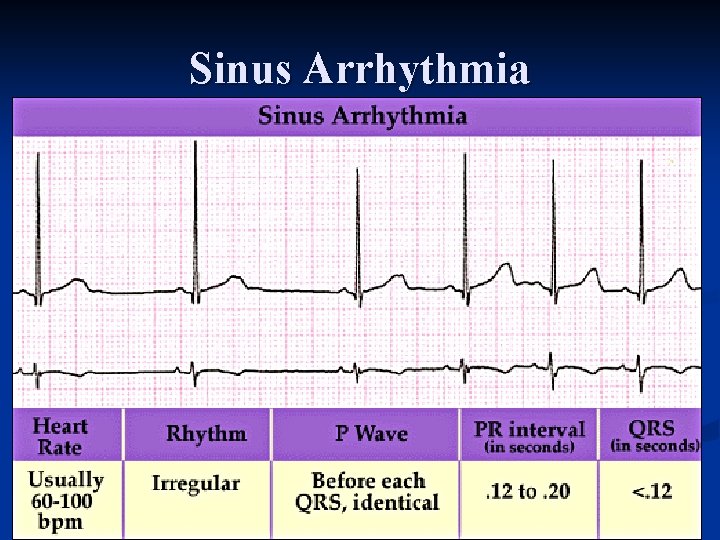
Sinus Arrhythmia
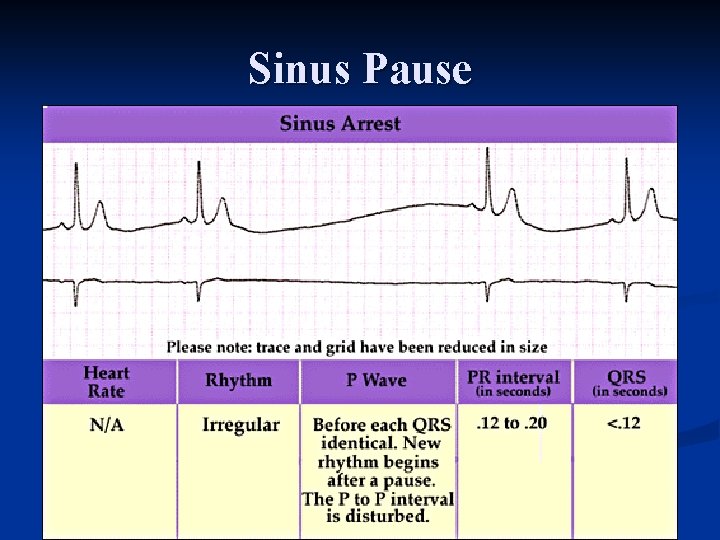
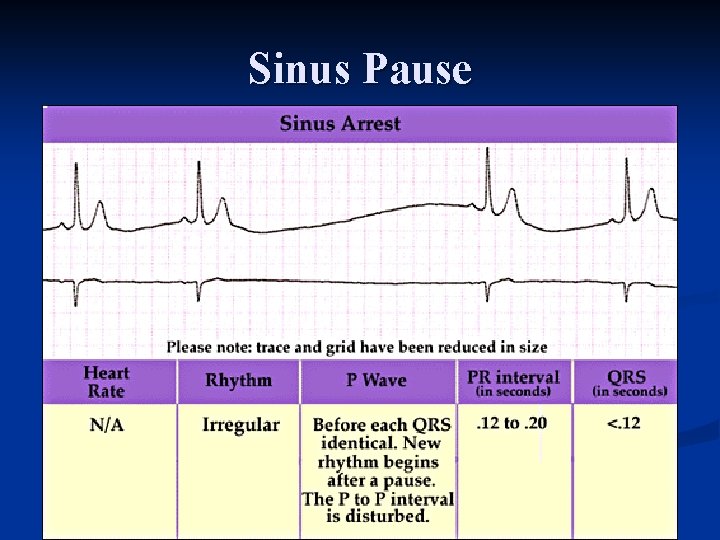
Sinus Pause
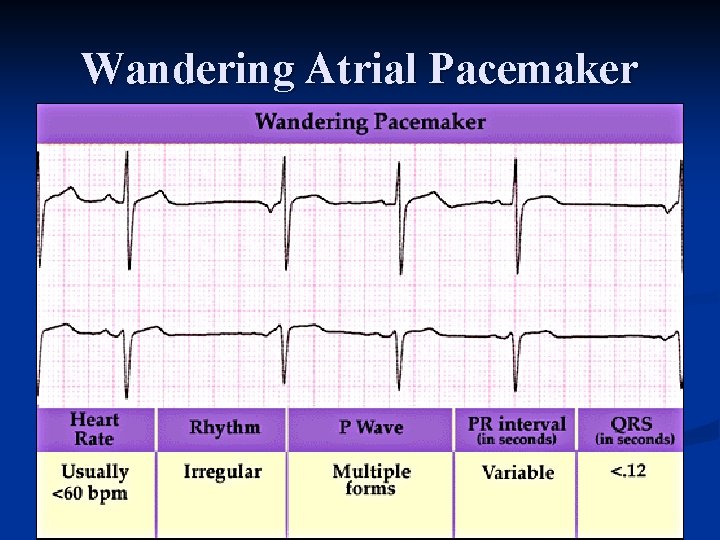
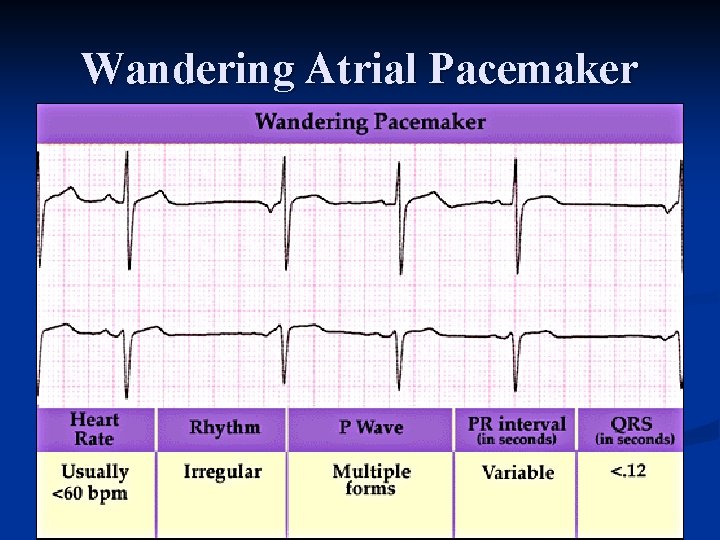
Wandering Atrial Pacemaker
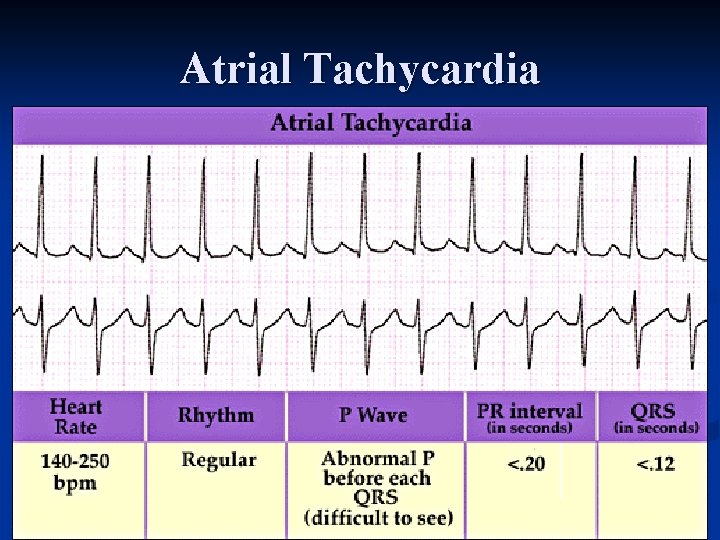
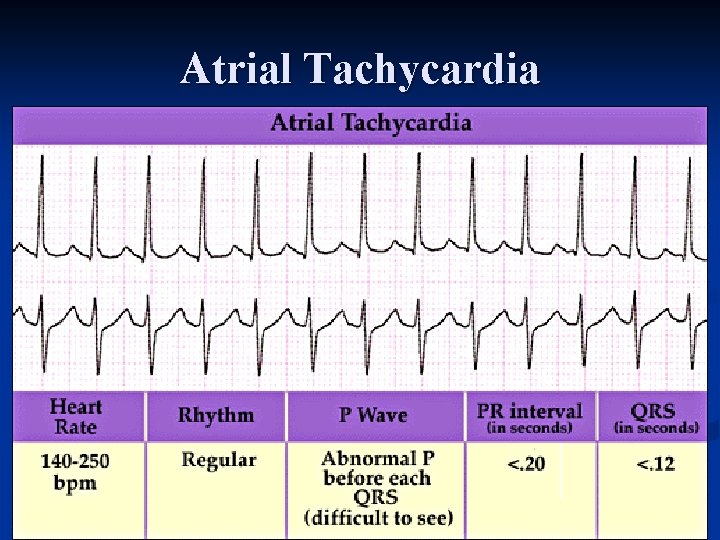
Atrial Tachycardia
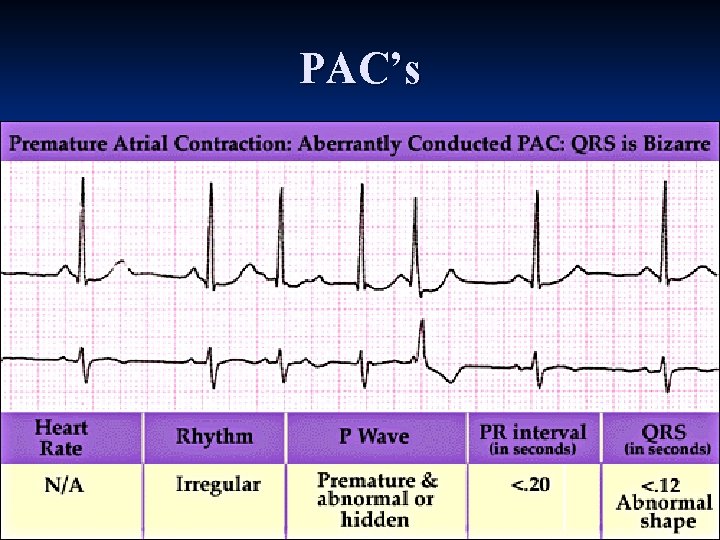
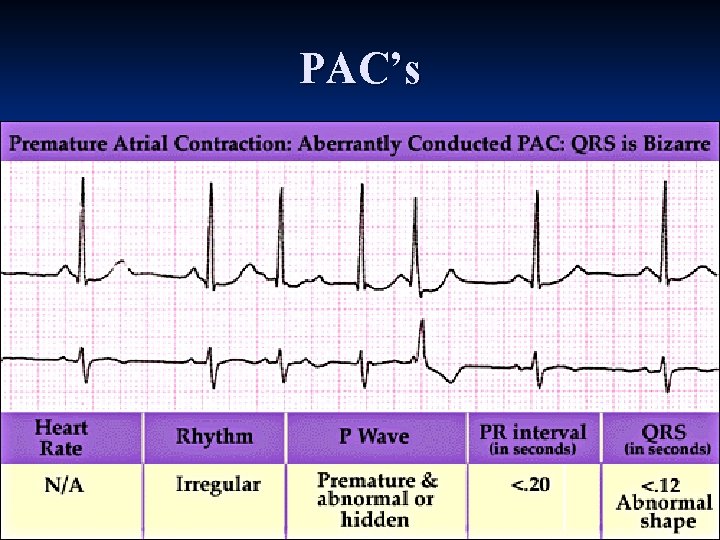
PAC’s
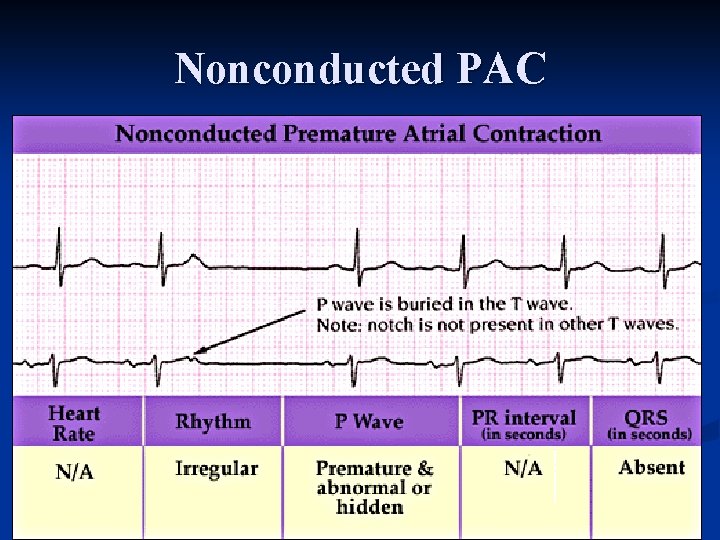
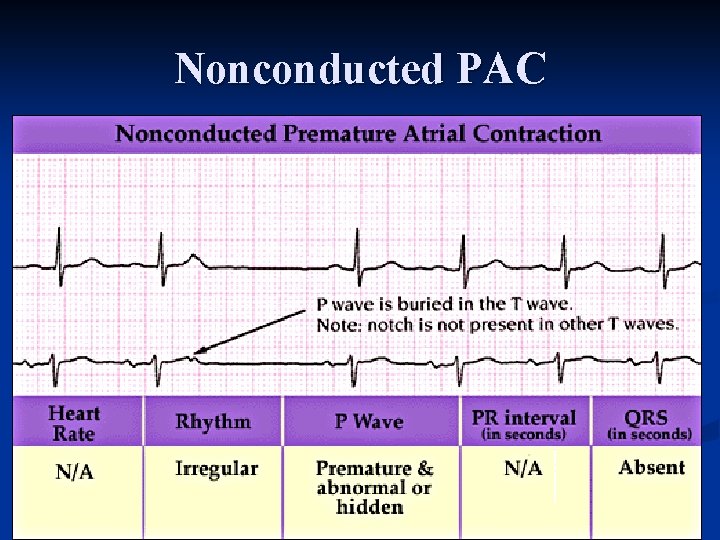
Nonconducted PAC
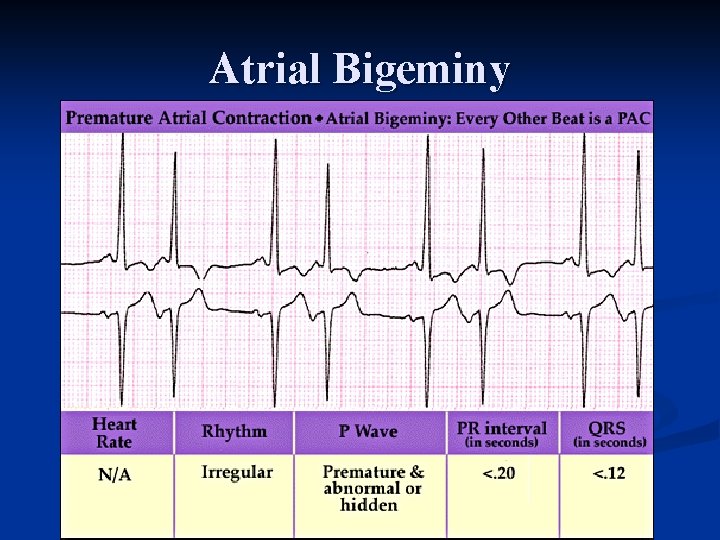
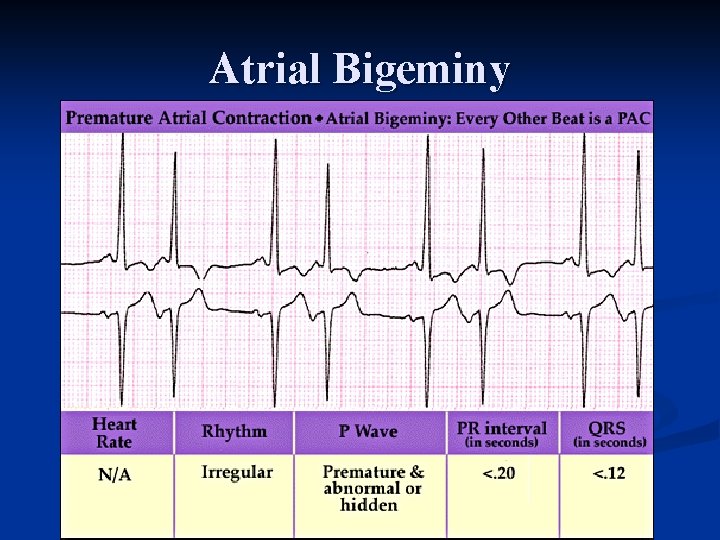
Atrial Bigeminy
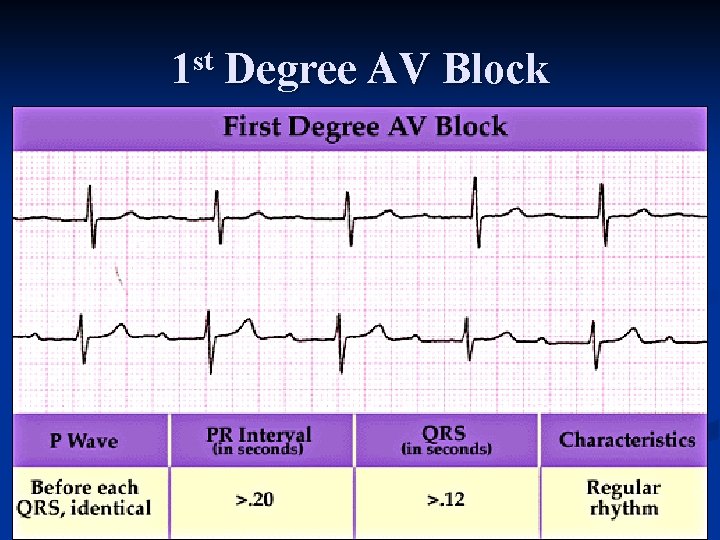
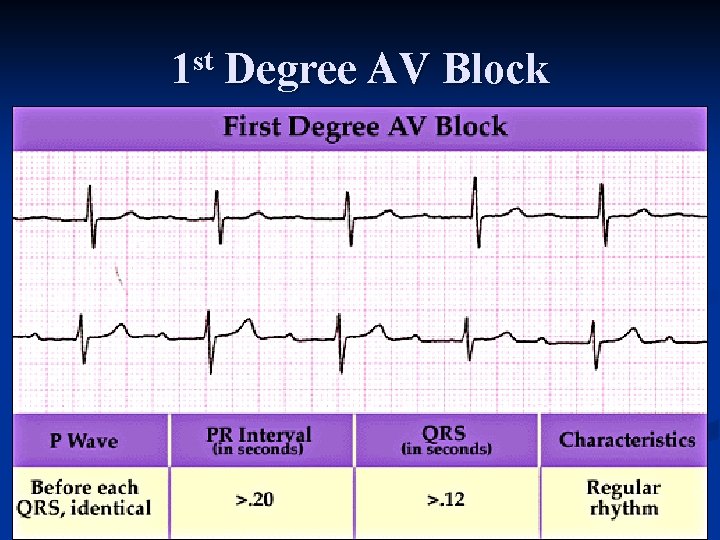
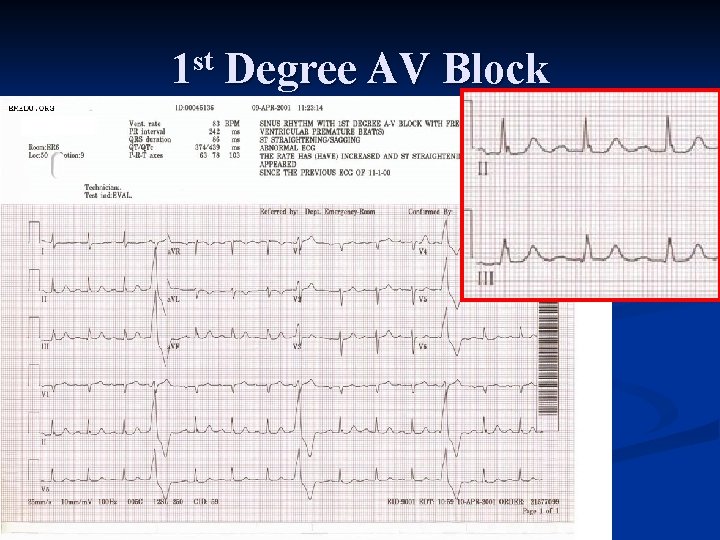
1 st Degree AV Block
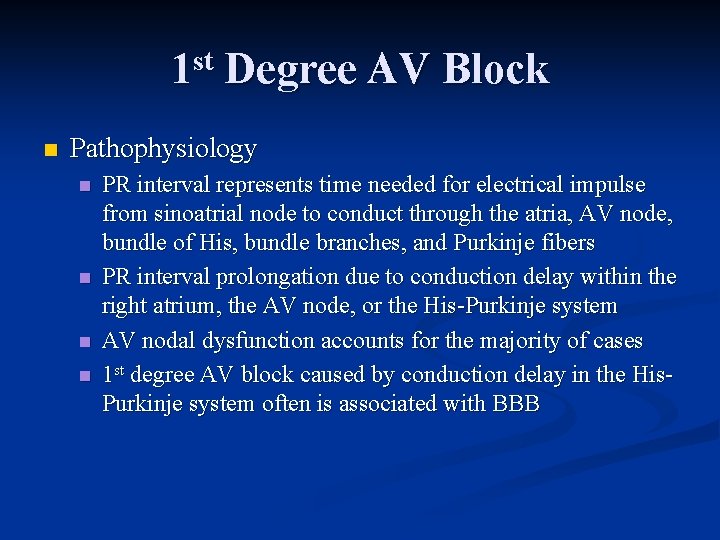
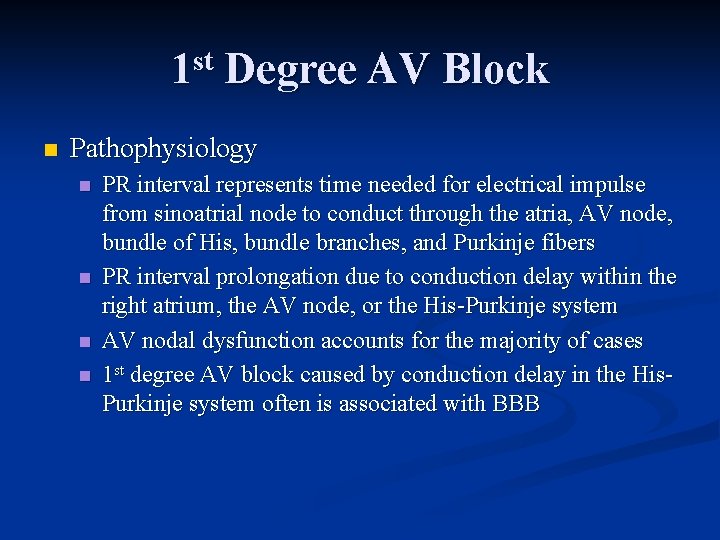
1 st Degree AV Block n Pathophysiology n n PR interval represents time needed for electrical impulse from sinoatrial node to conduct through the atria, AV node, bundle of His, bundle branches, and Purkinje fibers PR interval prolongation due to conduction delay within the right atrium, the AV node, or the His Purkinje system AV nodal dysfunction accounts for the majority of cases 1 st degree AV block caused by conduction delay in the His Purkinje system often is associated with BBB
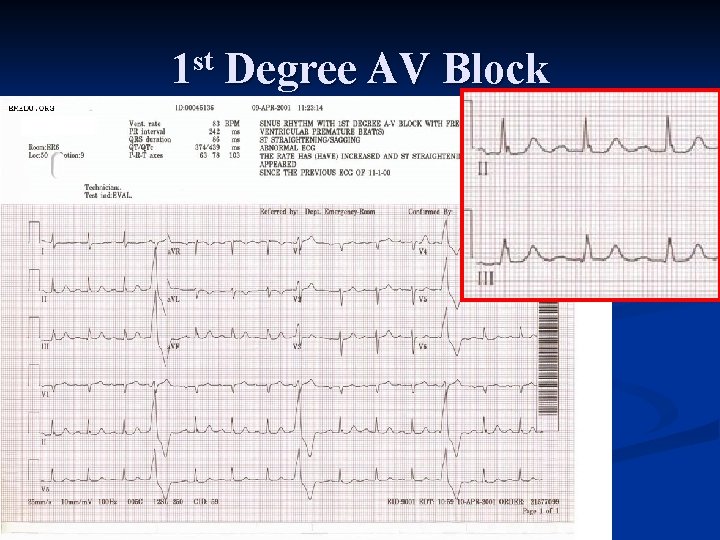
1 st Degree AV Block
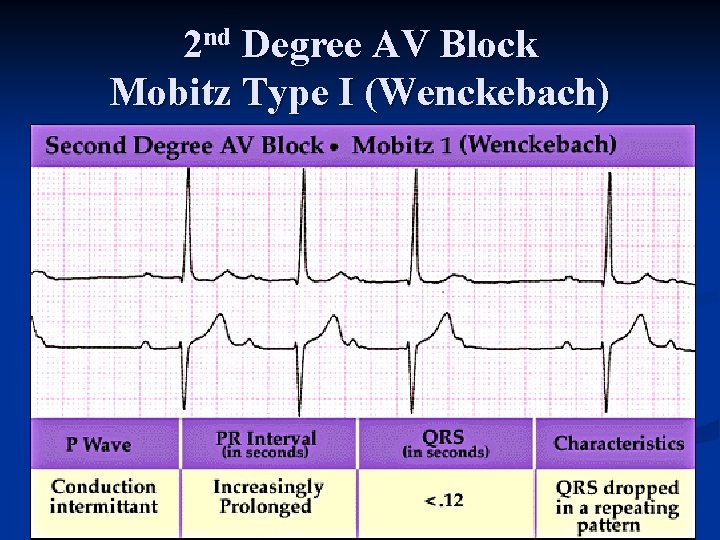
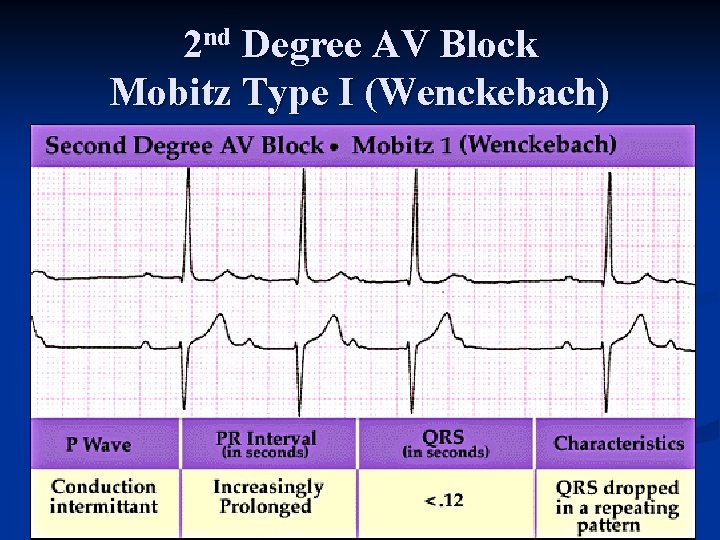
2 nd Degree AV Block Mobitz Type I (Wenckebach)
Karel Frederik Wenckebach (1864 – 1940) n n n n 1988 – Doctorate University of Utrecht, Netherlands 1901 1910 – professor of IM Groningen, Netherlands 1911 1914 – professor of IM Strasbourg , France 1915 1929 – professor of IM Vienna, Austria, retired from his chair 1929 Early work concerned embryology, later pathology of heart and circulatory diseases 1903 1904 – first description of the beneficial effects of quinine alkaloids on arrhythmias and mainly in patients with auricular fibrillation of recent onset 1905 1906 – 2 nd degree AV block independently discovered by English physician John Hay and Wenckebach
2 nd Degree AV Block Mobitz Type I (Wenckebach) n Pathophysiology n n n Conduction disturbance in the AV node Rarely secondary to AV nodal structural abnormalities when the QRS complex is narrow in width and no underlying cardiac disease is present May be vagally mediated (well trained athletes, digoxin excess, neurally mediated syncopal syndromes) Vagally mediated AV block improves with exercise and may occur more commonly during sleep when parasympathetic tone dominates Cardioactive drugs (digoxin, β blockers, CCBs, certain antiarrhythmic drugs) Various inflammatory, infiltrative, metabolic, endocrine, collagen vascular disorders
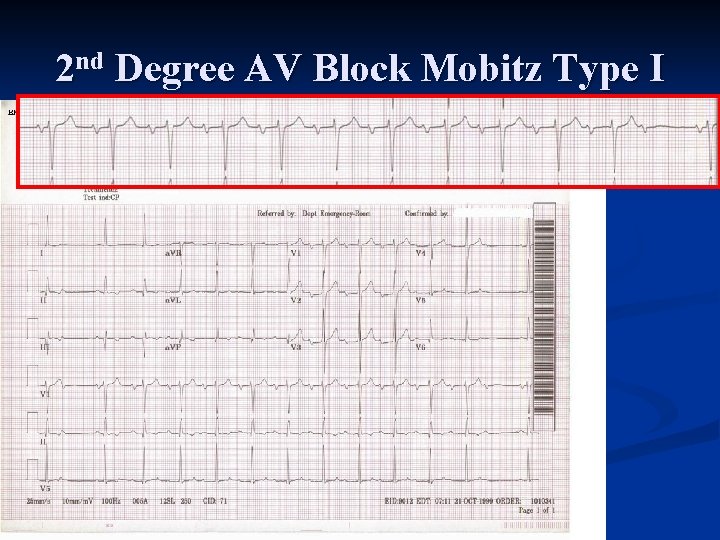
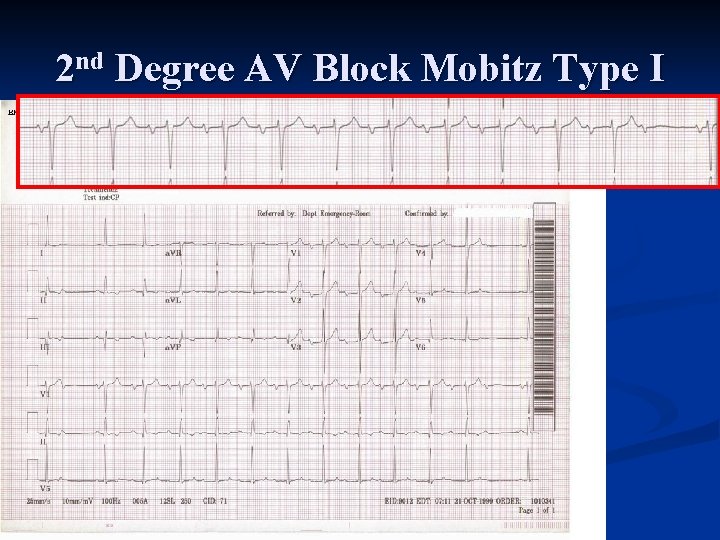
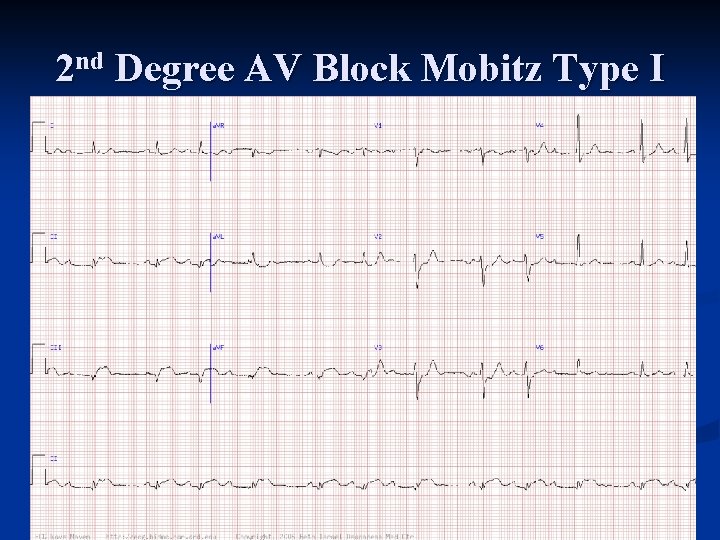
2 nd Degree AV Block Mobitz Type I
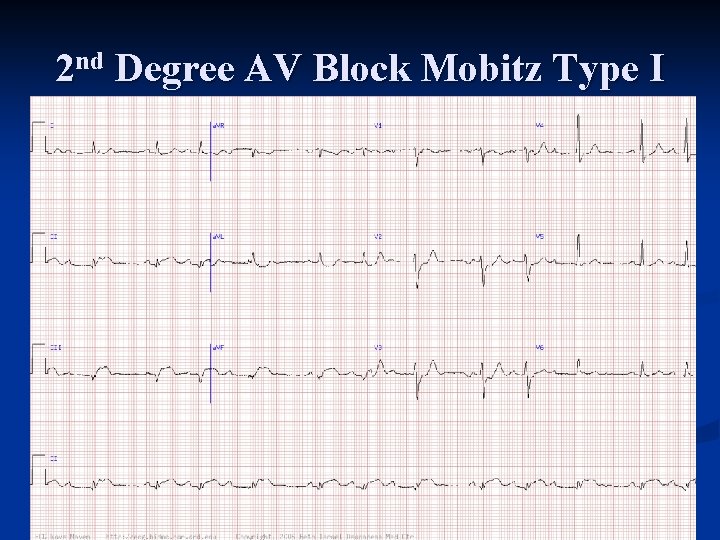
2 nd Degree AV Block Mobitz Type I
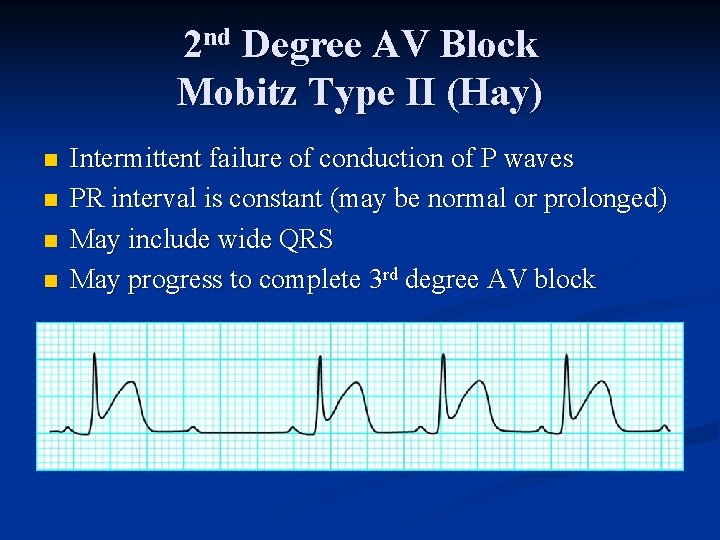
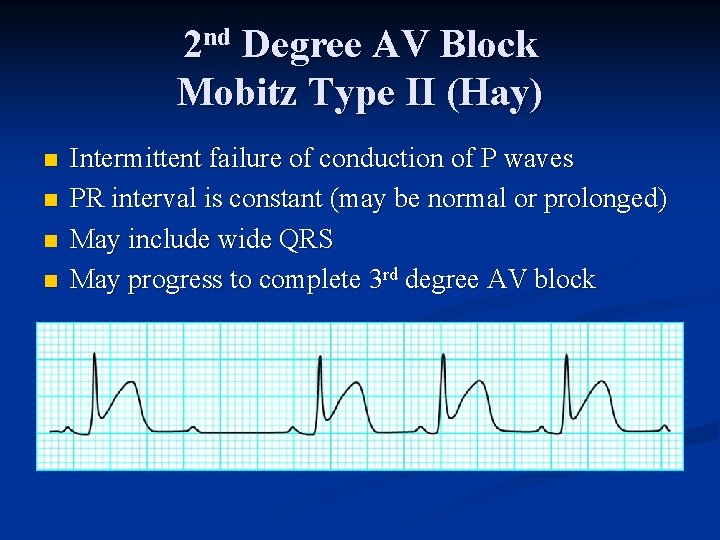
2 nd Degree AV Block Mobitz Type II (Hay) n n Intermittent failure of conduction of P waves PR interval is constant (may be normal or prolonged) May include wide QRS May progress to complete 3 rd degree AV block
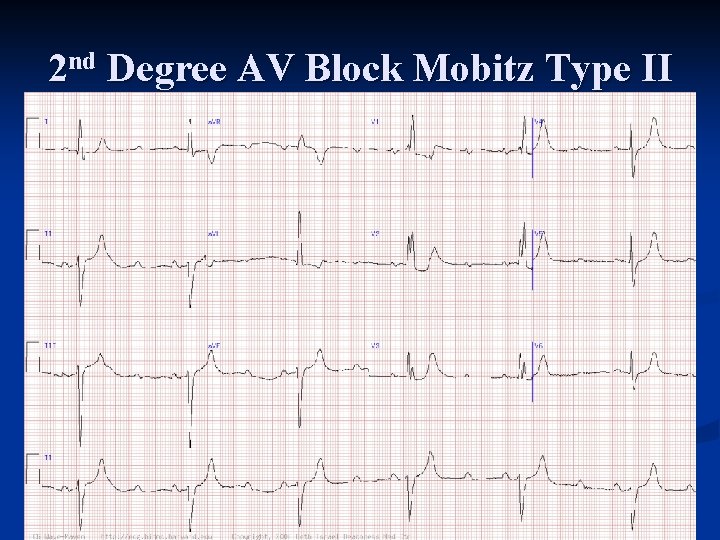
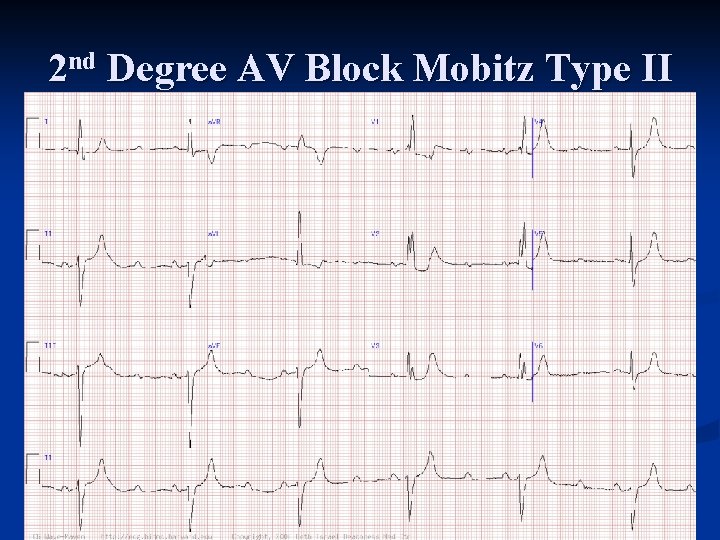
2 nd Degree AV Block Mobitz Type II
Woldemar Mobitz (1889 – 1951) n n n n n Born May 31, 1889 St. Petersburg, Russia, the son of a prominent surgeon 1908 – gymnasium Meiningen, Saxony 1914 – doctorate University of Munich Internship, hospital service, and assistant years in the surgical clinics in Berlin and Halle, and medical clinics Munich and Freiburg 1924 – first classified 2 nd degree AV block into Type I and II 1928 1943 – professor extraordinary at University of Freiburg in Breisgau Remained in Magdeburg until it was occupied by the Russian army in 1945 Suffered from laryngeal tuberculosis until his death April 11, 1951 Primary interest in cardiovascular circulation and arrhythmias
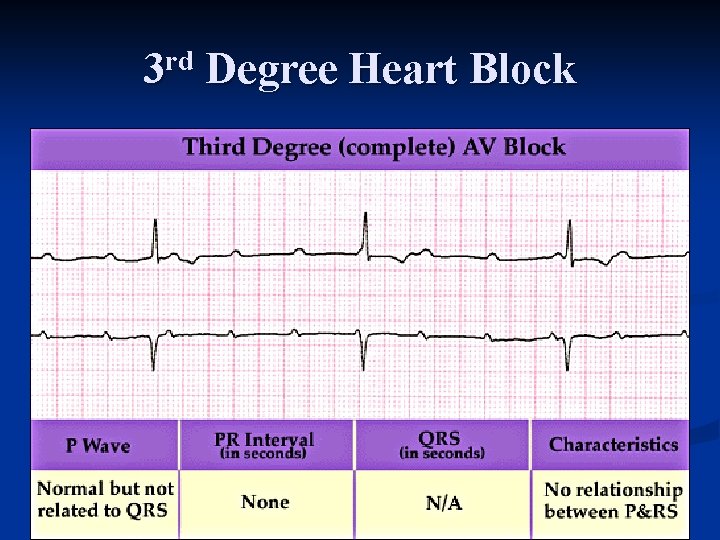
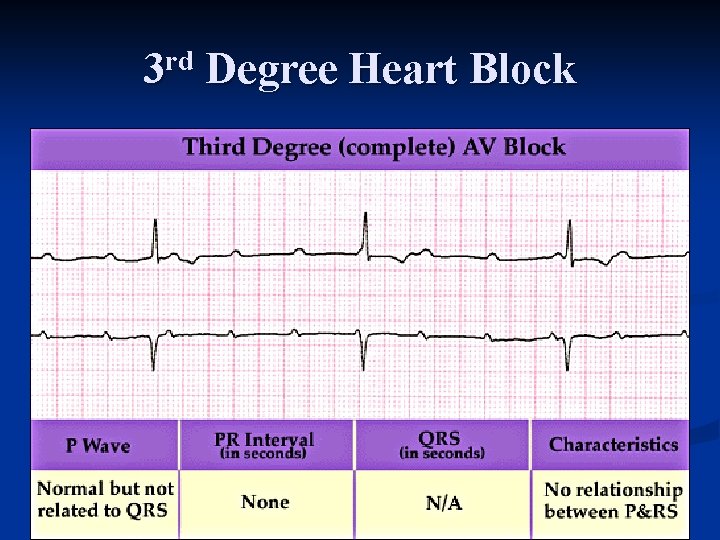
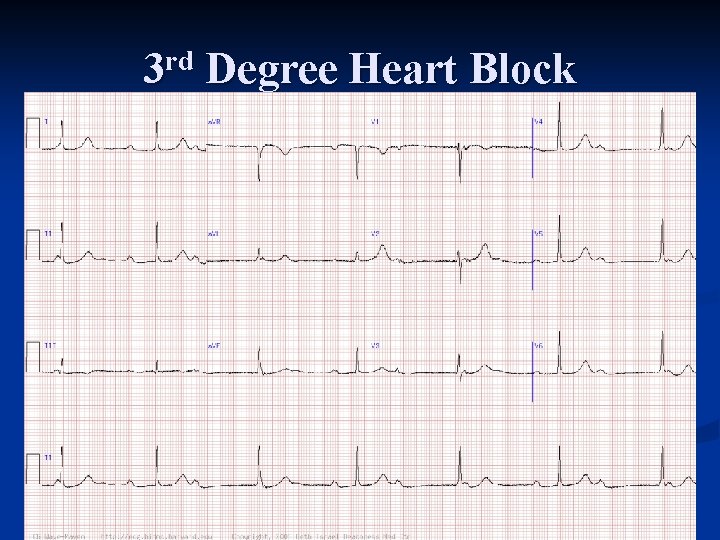
3 rd Degree Heart Block
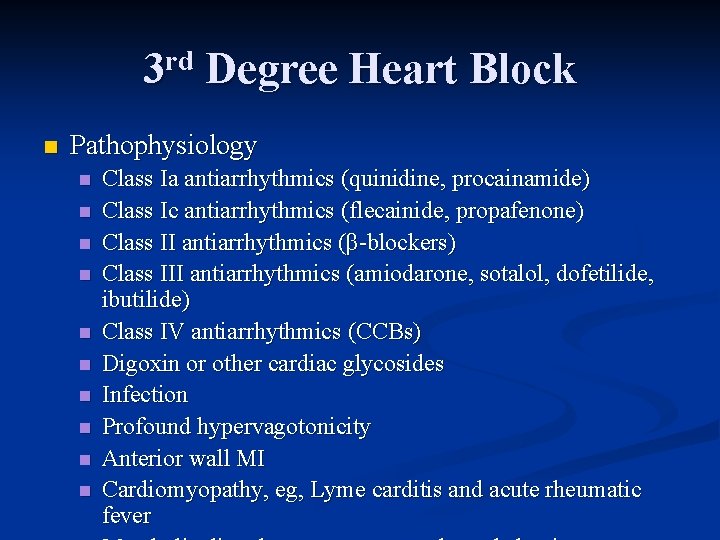
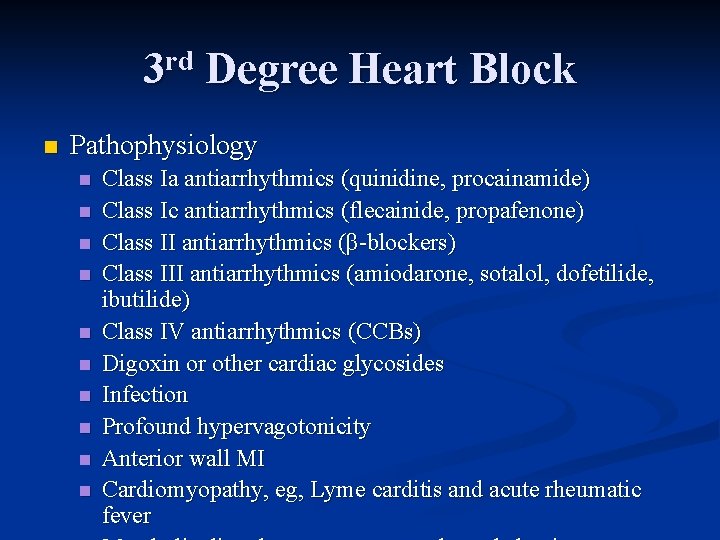
3 rd Degree Heart Block n Pathophysiology n n n n n Class Ia antiarrhythmics (quinidine, procainamide) Class Ic antiarrhythmics (flecainide, propafenone) Class II antiarrhythmics (β blockers) Class III antiarrhythmics (amiodarone, sotalol, dofetilide, ibutilide) Class IV antiarrhythmics (CCBs) Digoxin or other cardiac glycosides Infection Profound hypervagotonicity Anterior wall MI Cardiomyopathy, eg, Lyme carditis and acute rheumatic fever
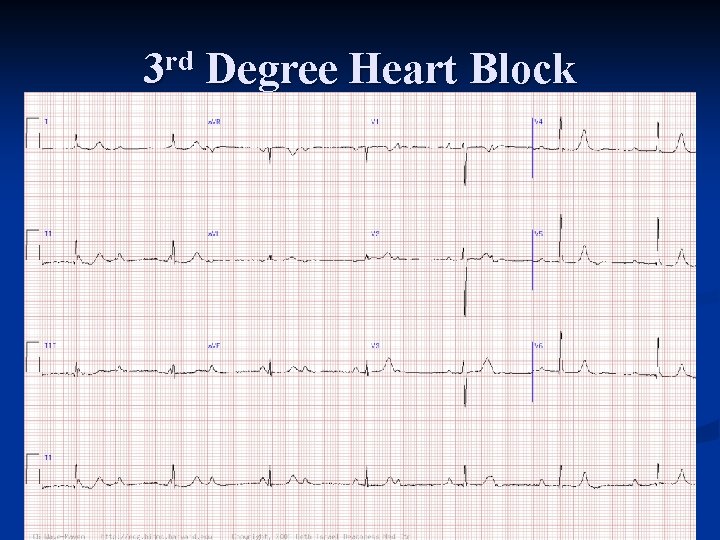
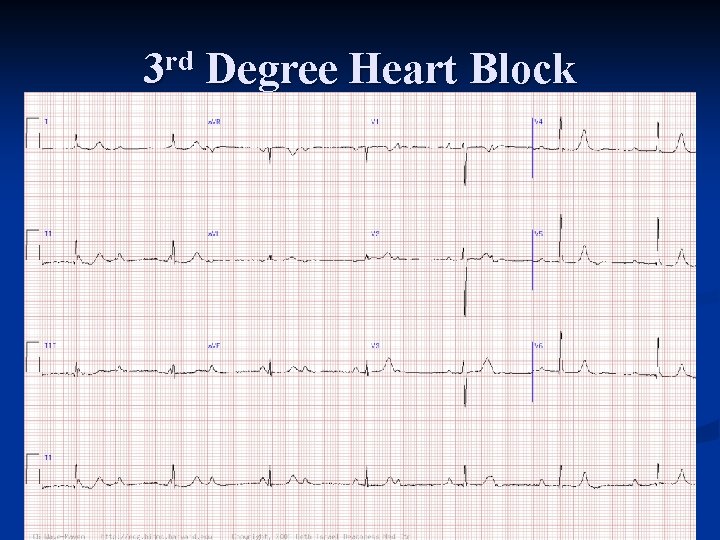
3 rd Degree Heart Block
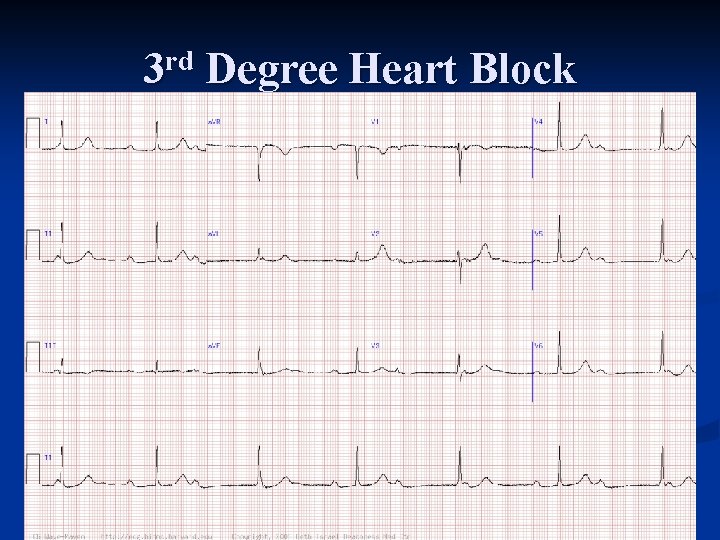
3 rd Degree Heart Block
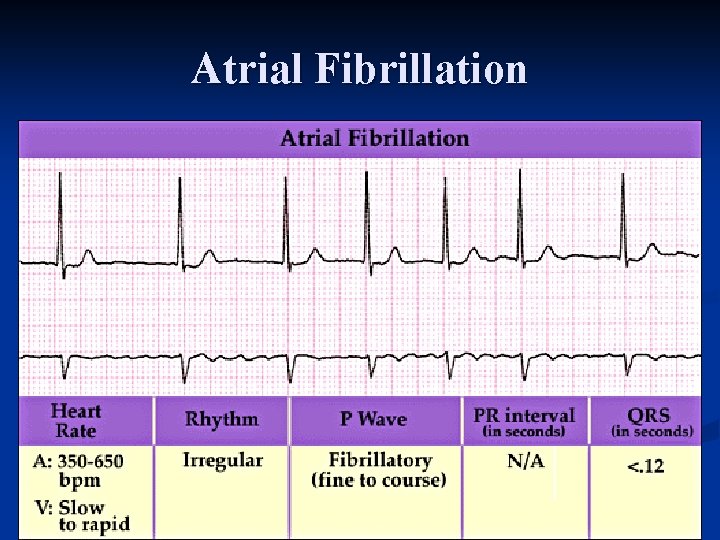
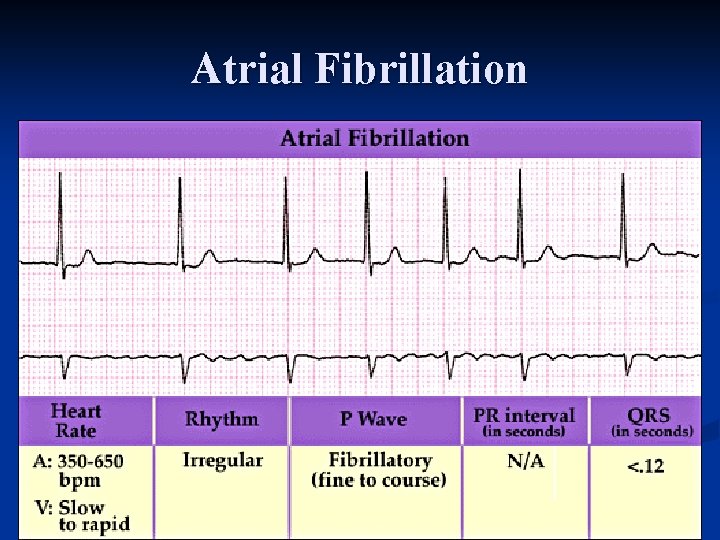
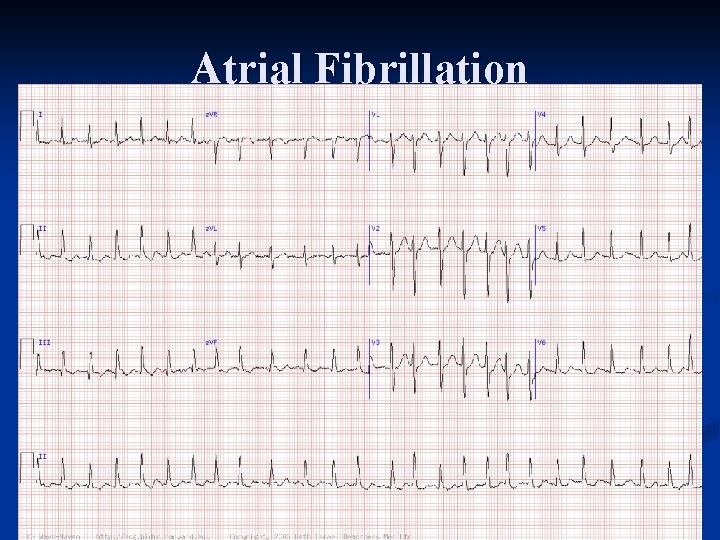
Atrial Fibrillation
Atrial Fibrillation n Pathophysiology n n n n Long standing hypertension Valvular heart disease (rheumatic) LVH CAD DM AMI CHF Pulmonary embolism Cardiomyopathy Pericarditis Hyperthyroidism ETOH (holiday heart) Postoperative revascularization Use of illegal drugs, such as cocaine or amphetamine derivatives Over the counter herbs (ephedra, ginseng) Idiopathic or “Lone” AF
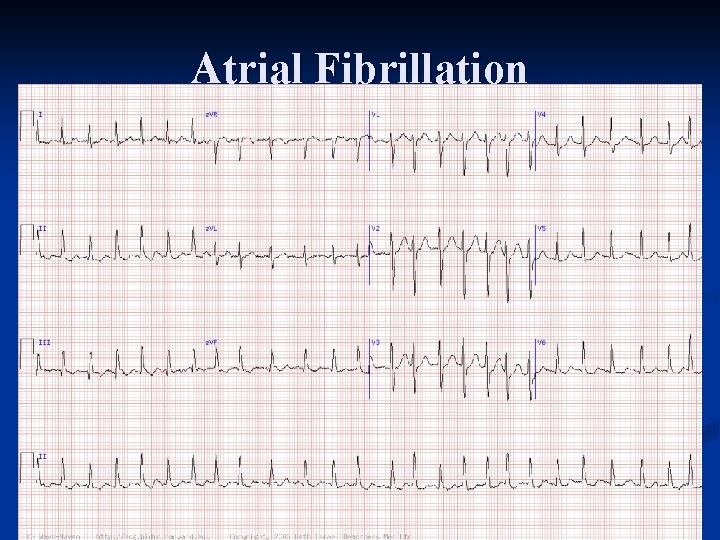
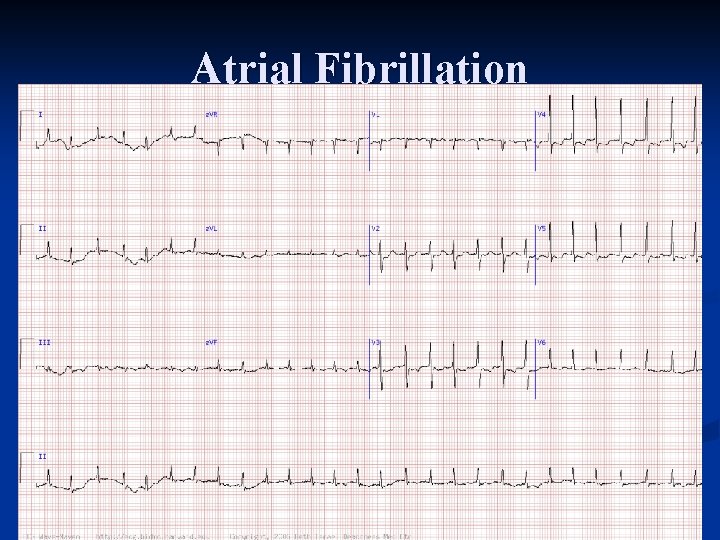
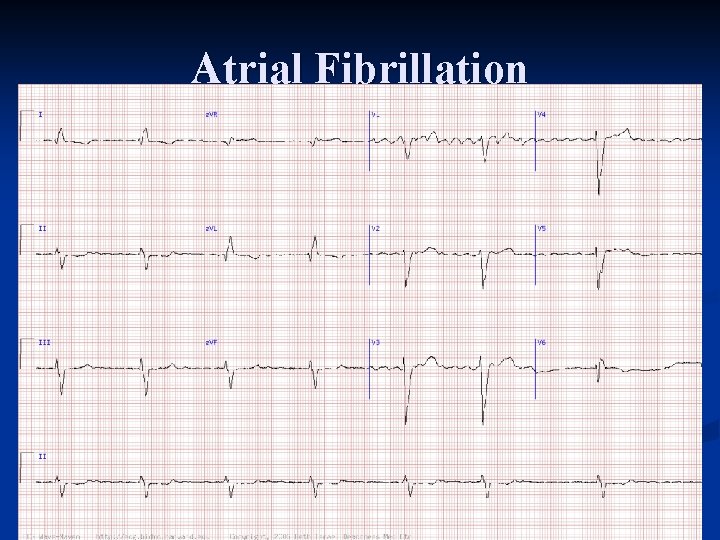
Atrial Fibrillation
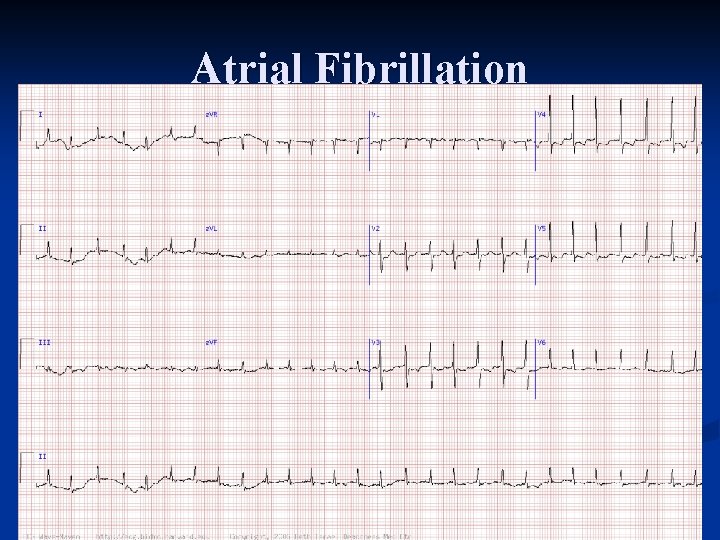
Atrial Fibrillation
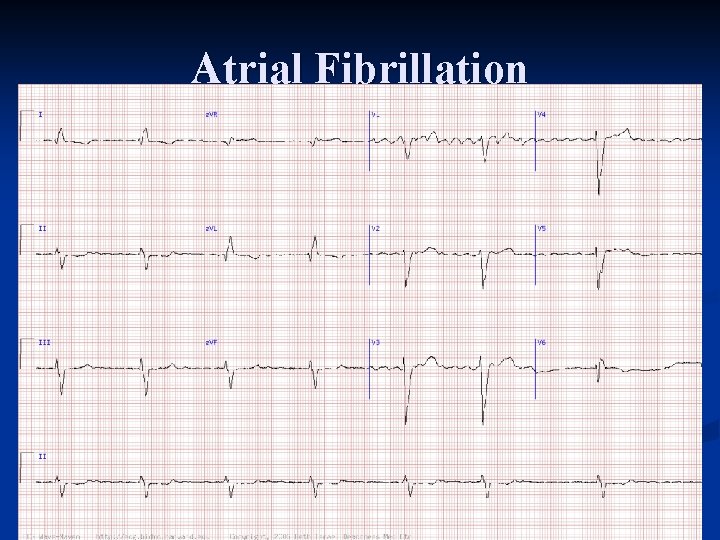
Atrial Fibrillation
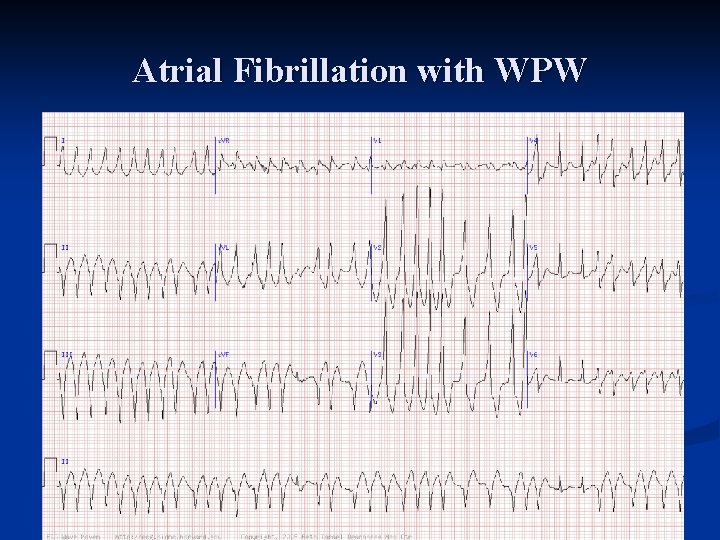
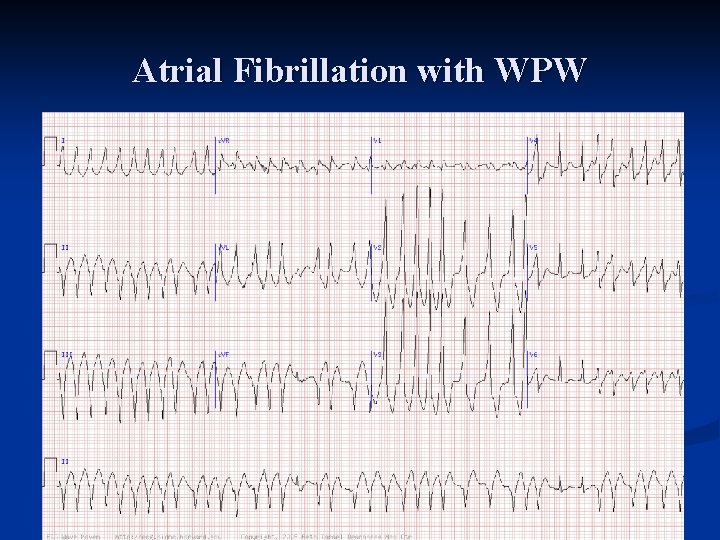
Atrial Fibrillation with WPW
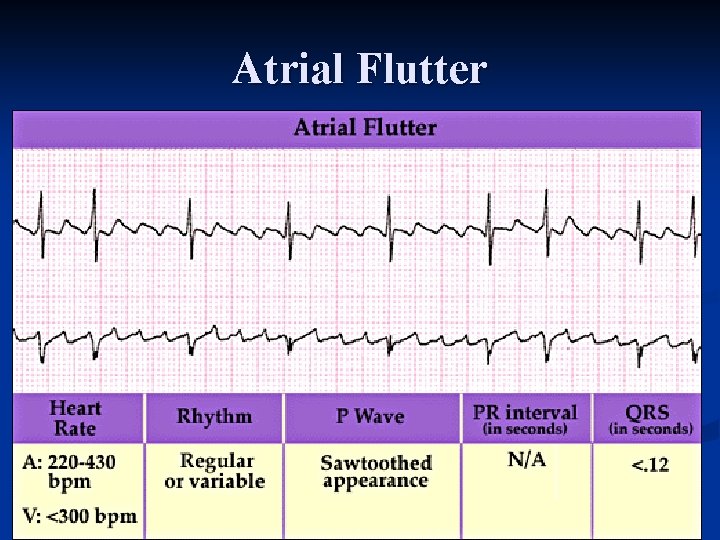
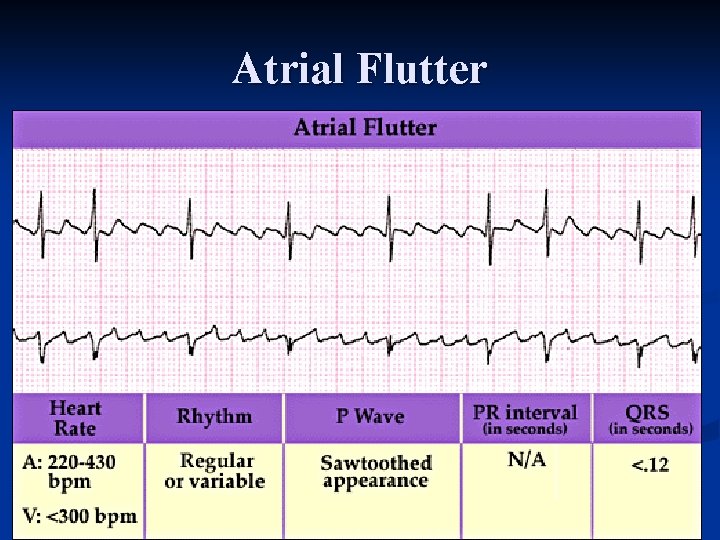
Atrial Flutter
Atrial Flutter n Pathophysiology n n n Long standing hypertension Valvular heart disease (rheumatic) LVH CAD with or without depressed left ventricular function DM CHF Pulmonary embolism Pericarditis Hyperthyroidism Postoperative revascularization Digitalis toxicity
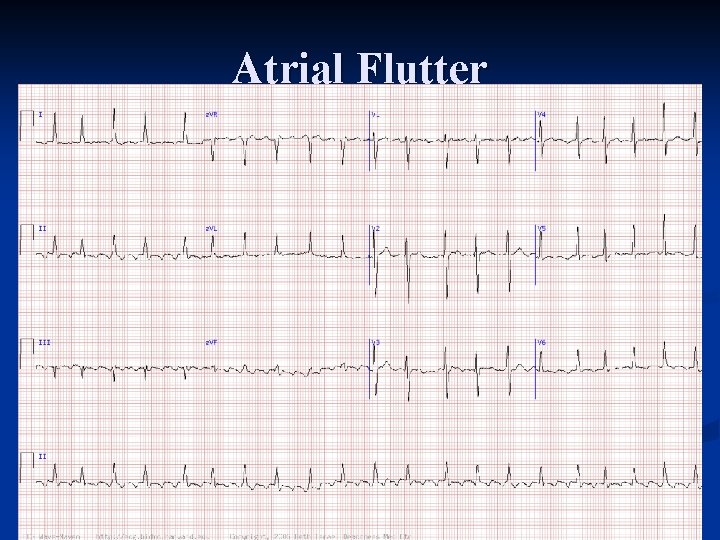
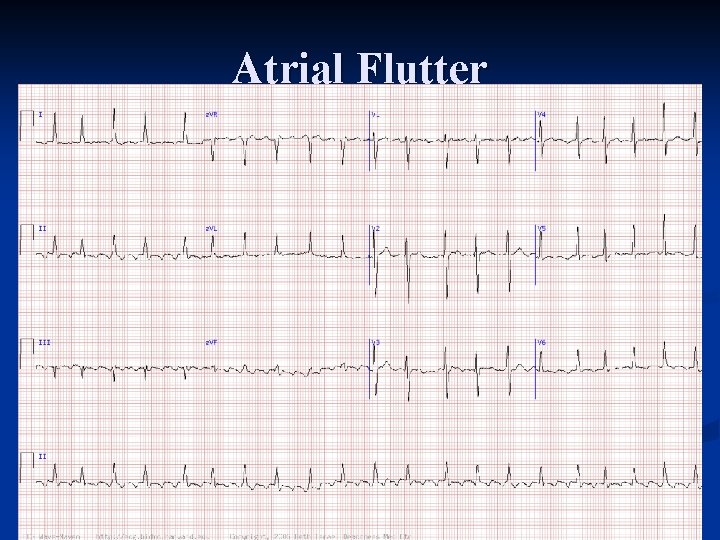
Atrial Flutter
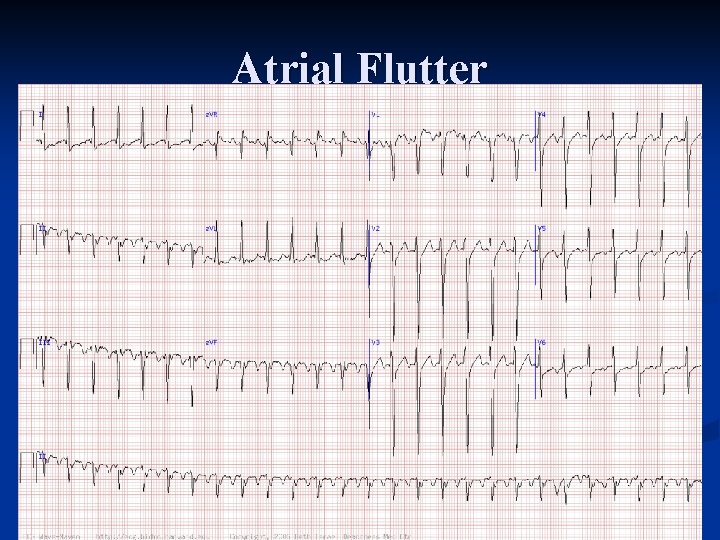
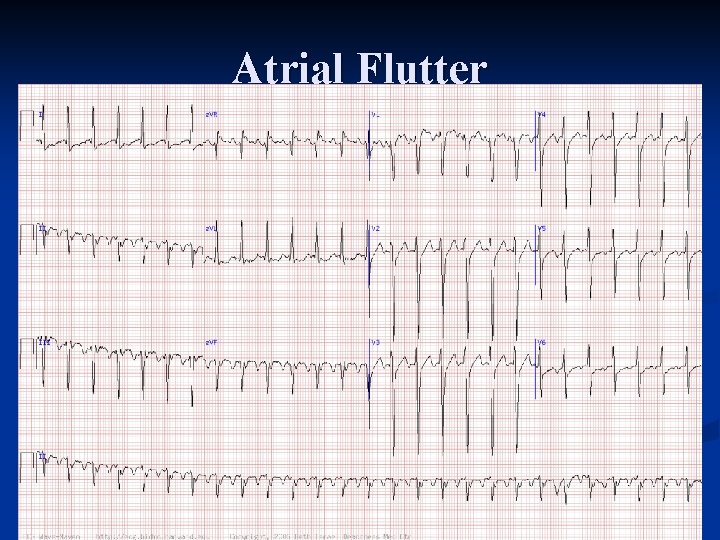
Atrial Flutter
AV Node (Junctional) Origin
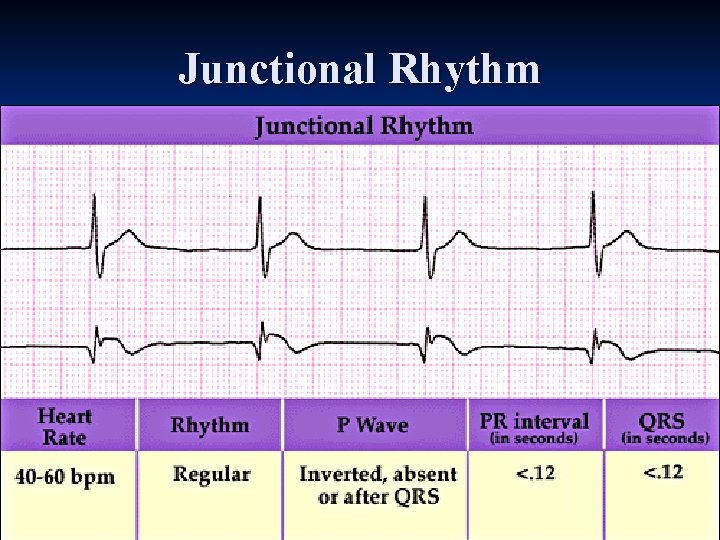
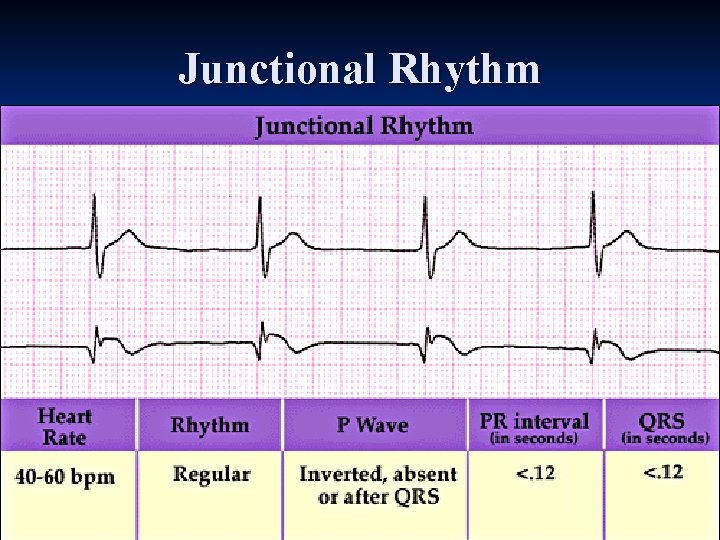
Junctional Rhythm
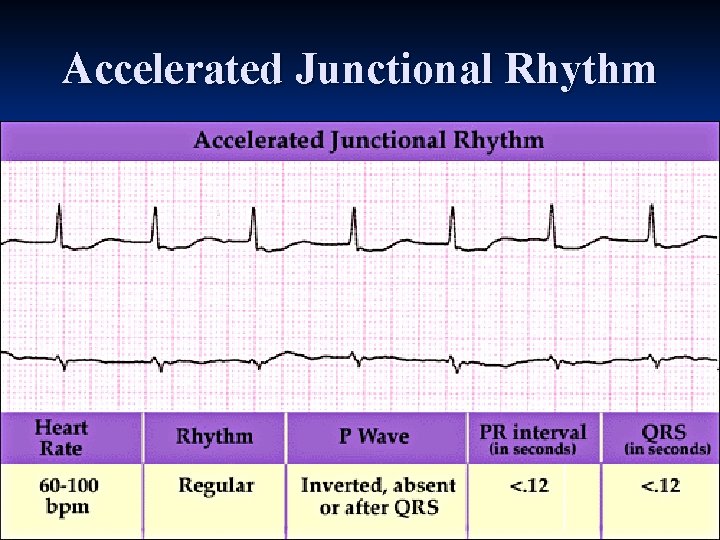
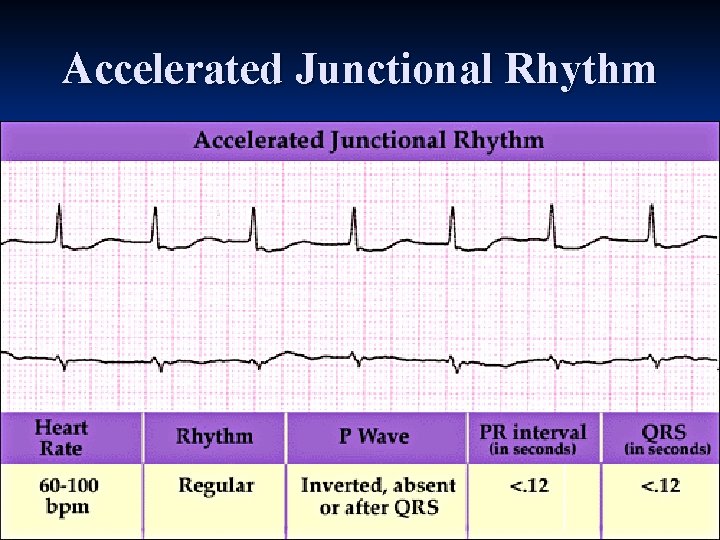
Accelerated Junctional Rhythm
Ventricular Origins
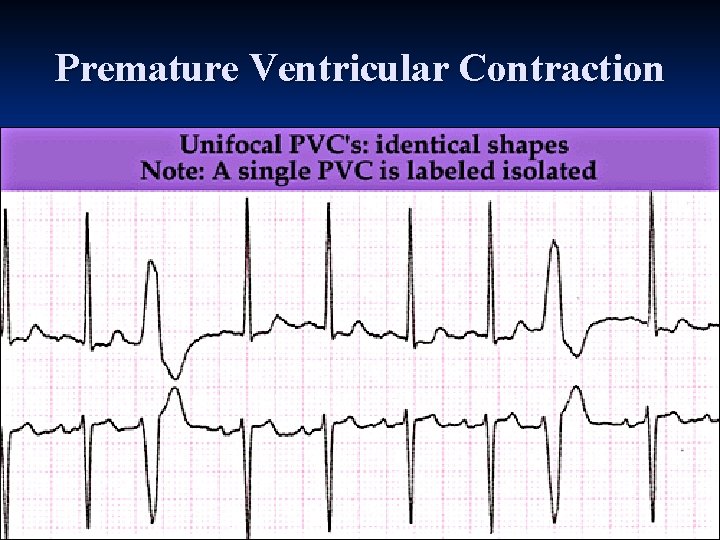
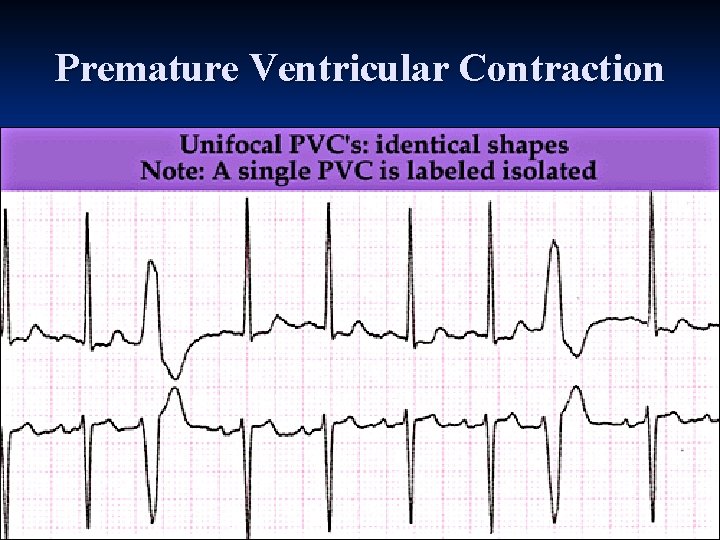
Premature Ventricular Contraction
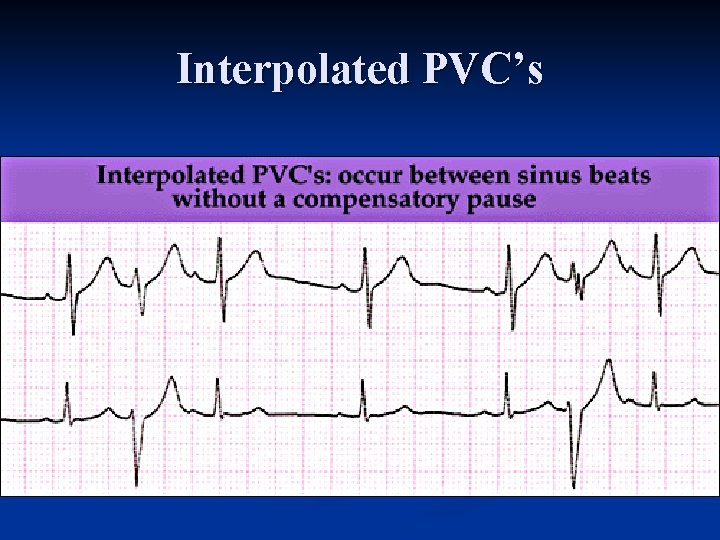
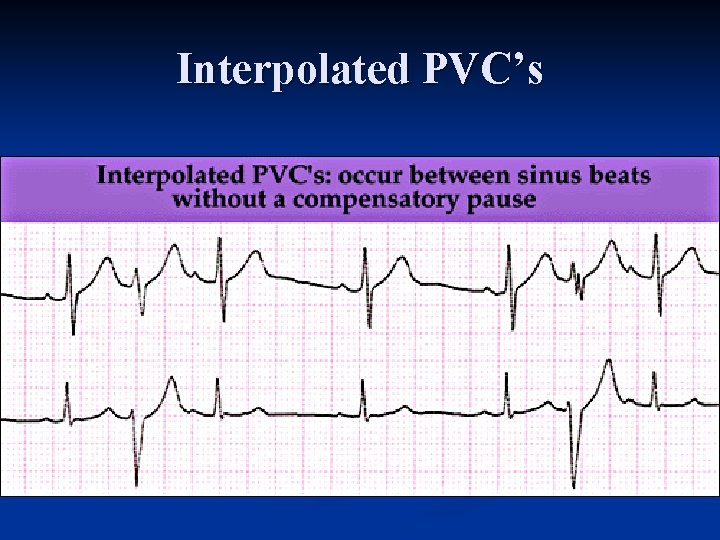
Interpolated PVC’s
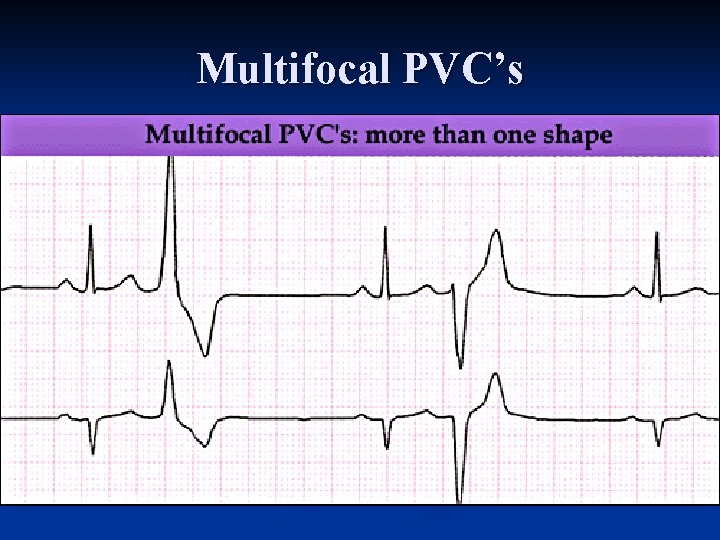
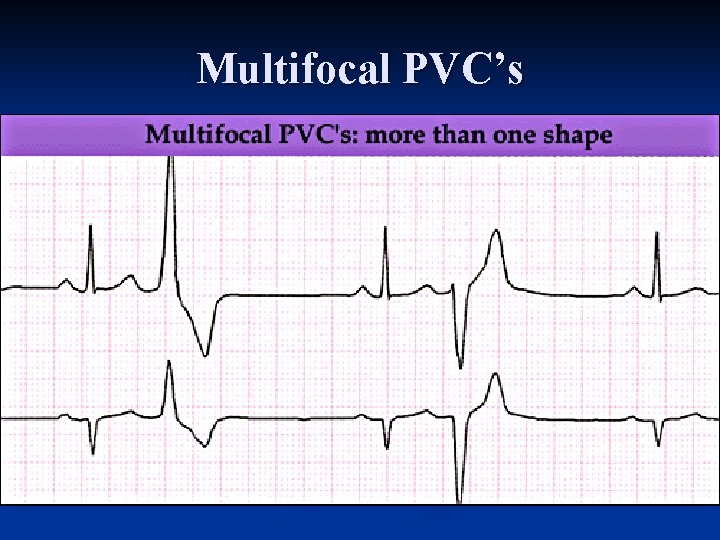
Multifocal PVC’s
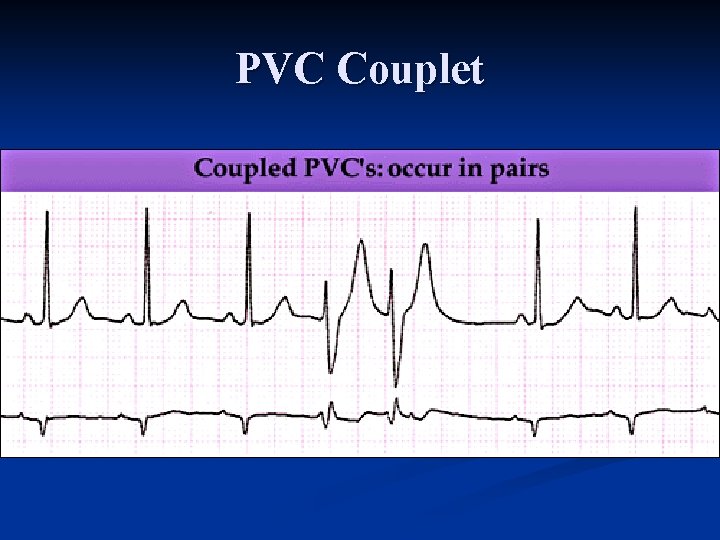
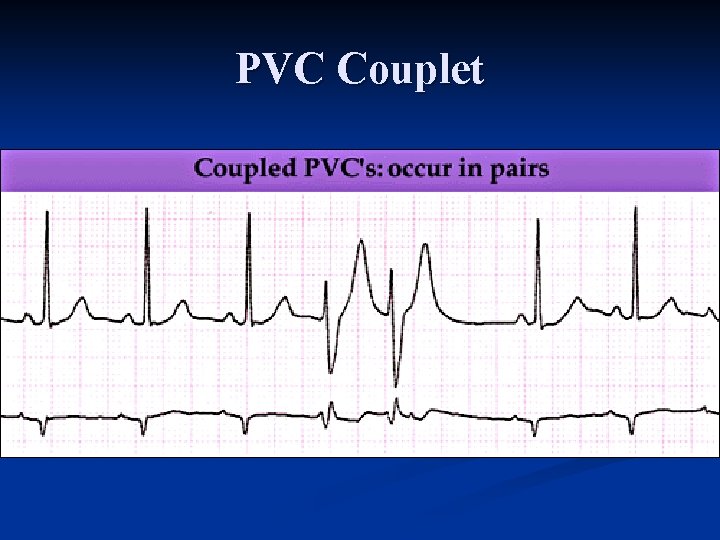
PVC Couplet
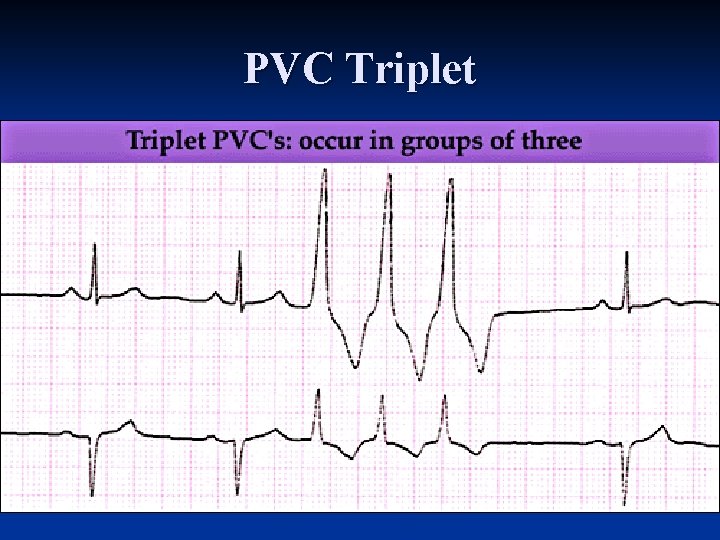
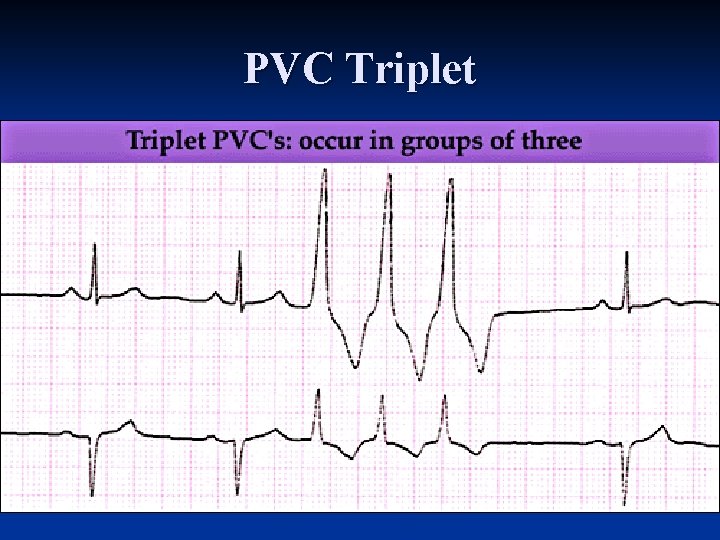
PVC Triplet
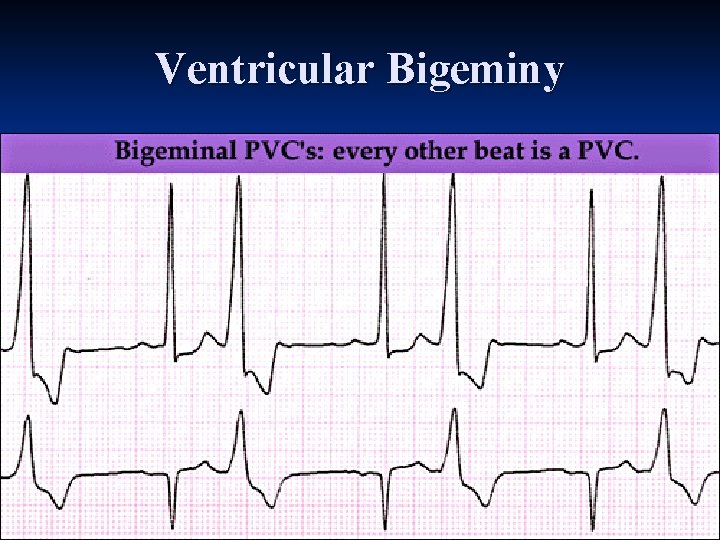
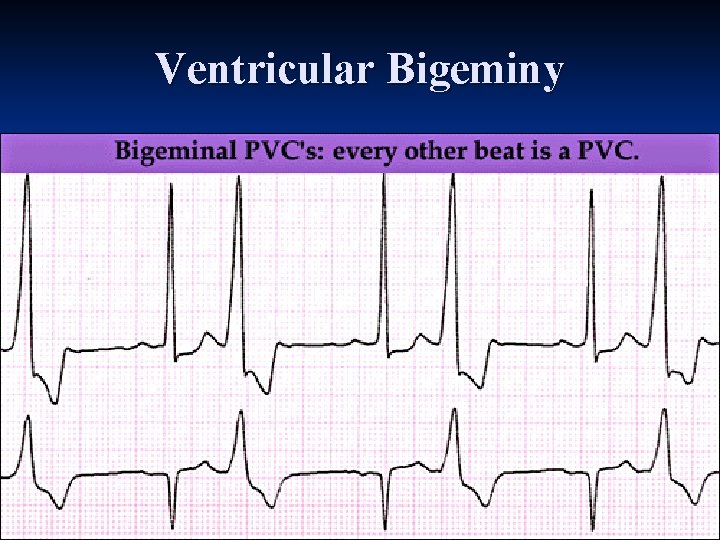
Ventricular Bigeminy
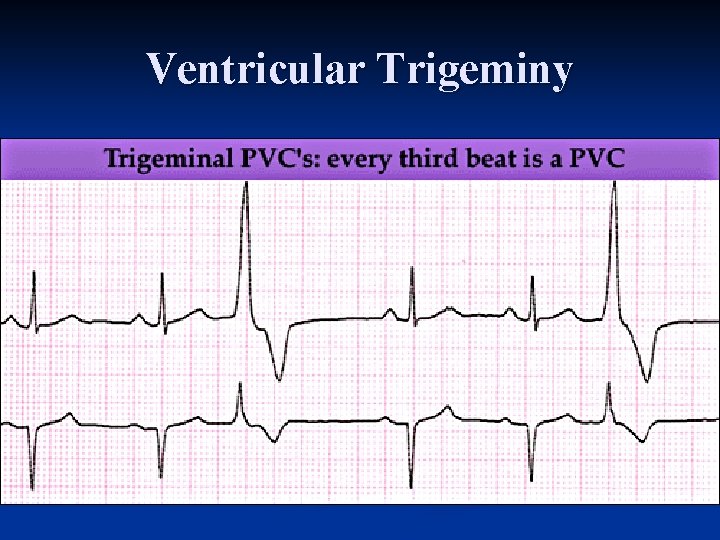
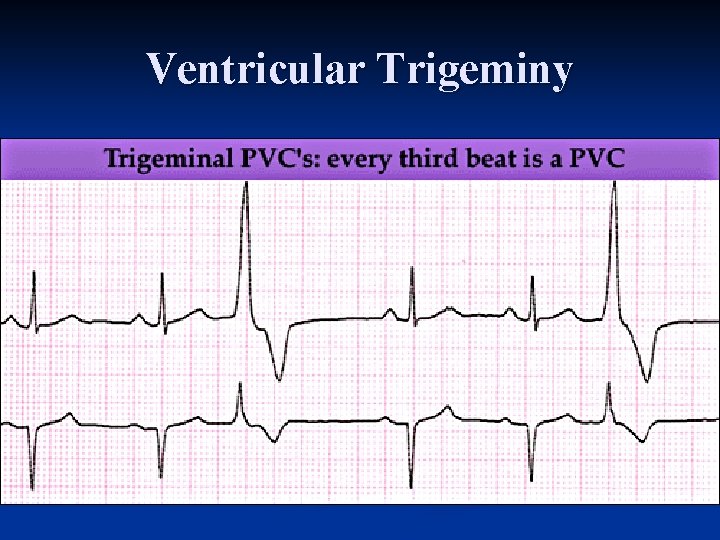
Ventricular Trigeminy
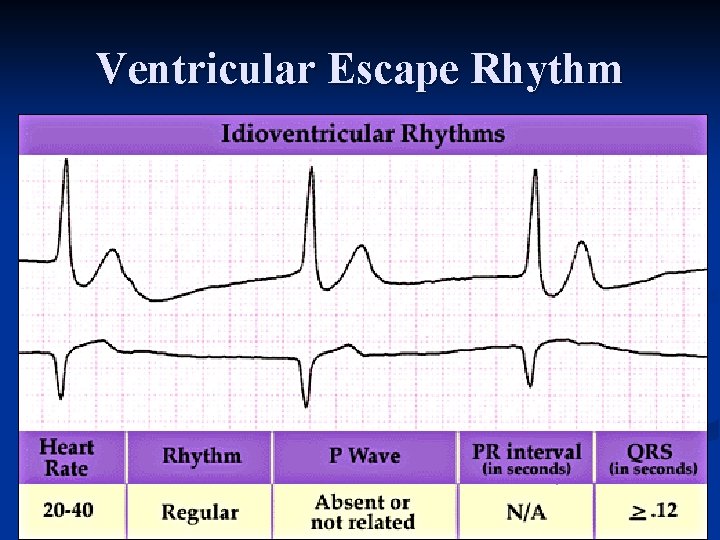
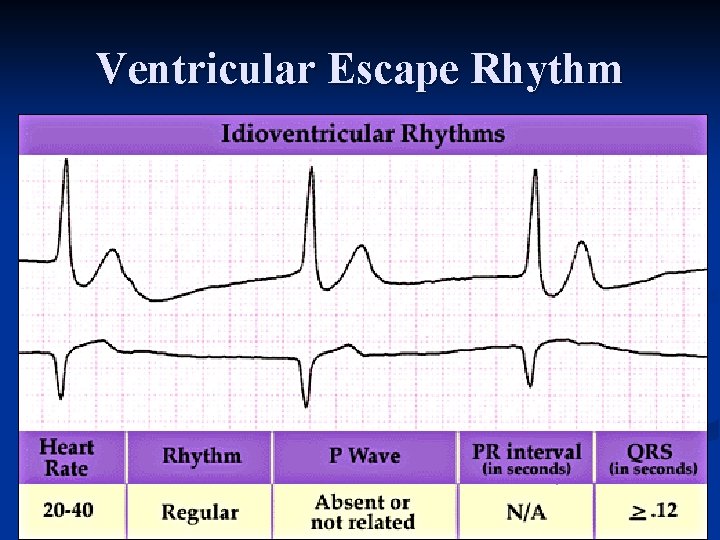
Ventricular Escape Rhythm
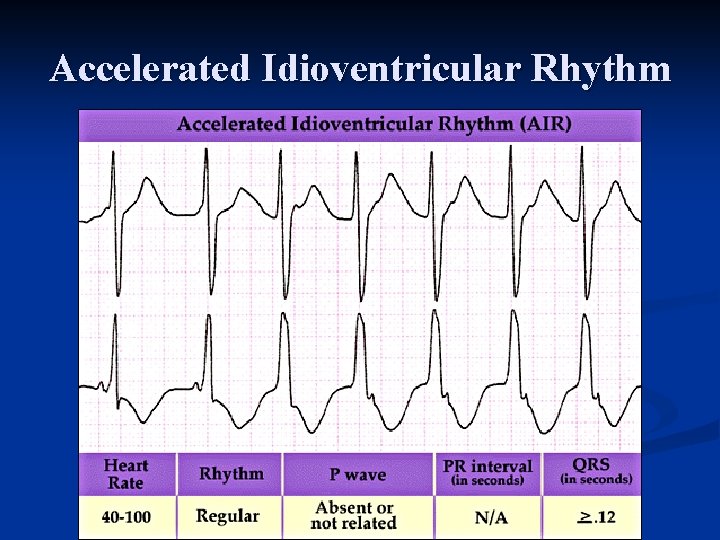
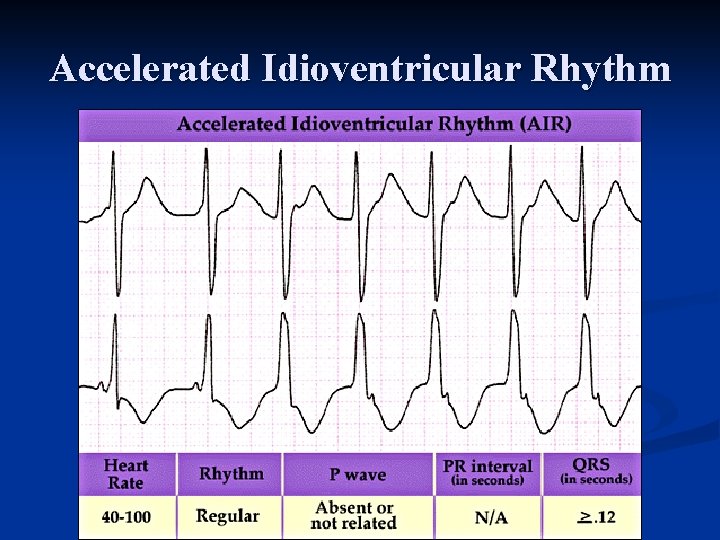
Accelerated Idioventricular Rhythm
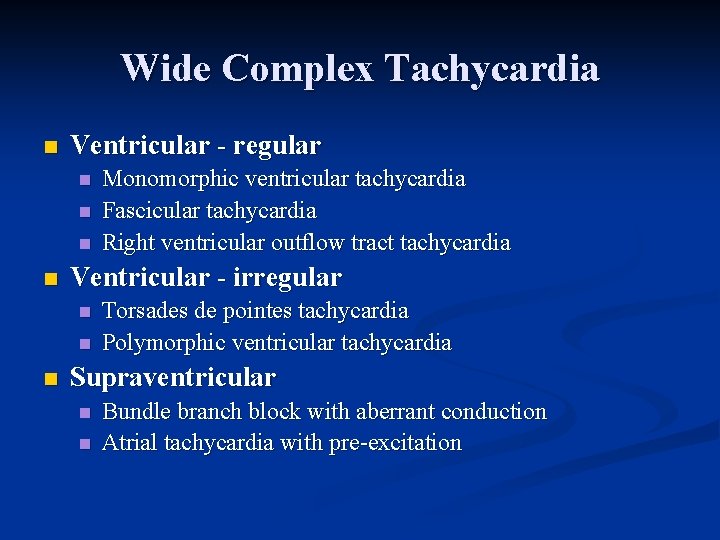
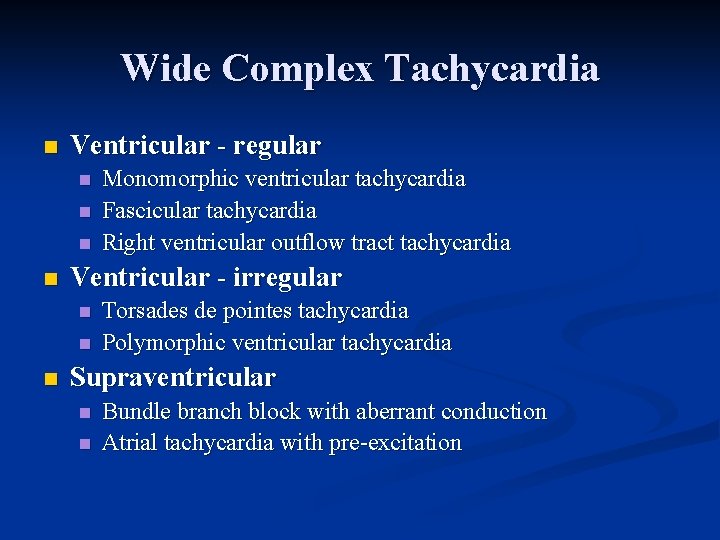
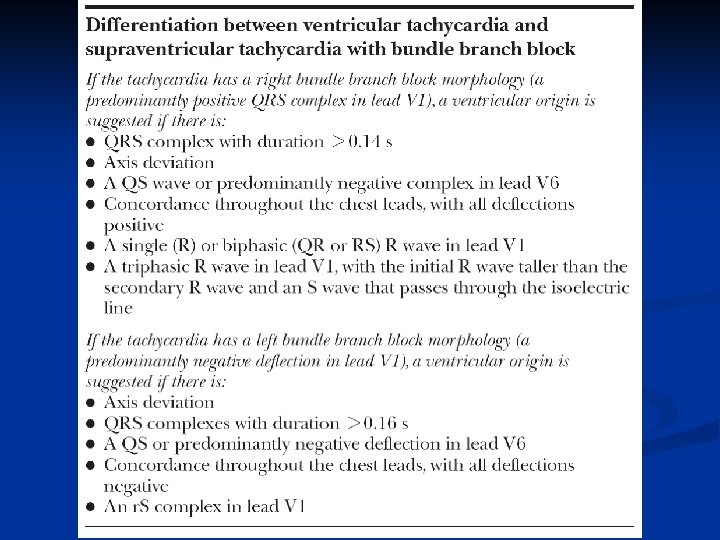
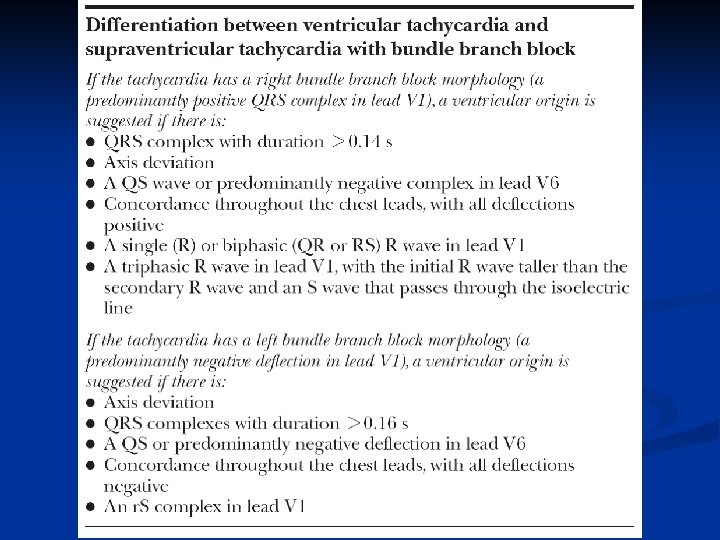
Wide Complex Tachycardia n Ventricular - regular n n Ventricular - irregular n n n Monomorphic ventricular tachycardia Fascicular tachycardia Right ventricular outflow tract tachycardia Torsades de pointes tachycardia Polymorphic ventricular tachycardia Supraventricular n n Bundle branch block with aberrant conduction Atrial tachycardia with pre excitation
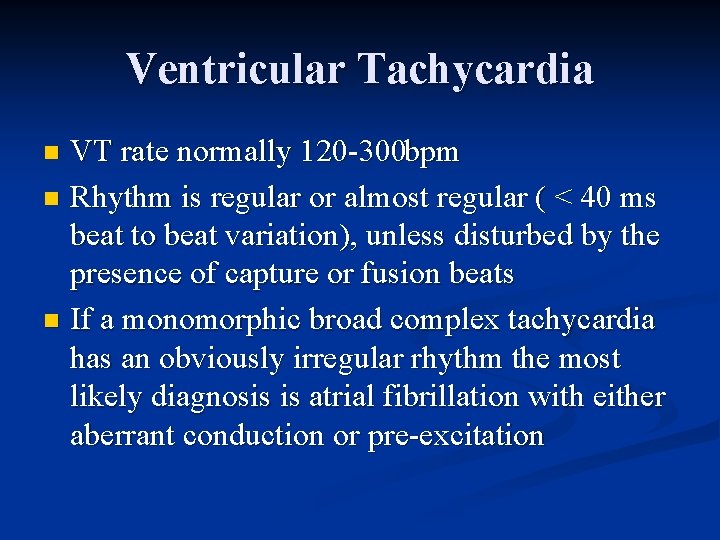
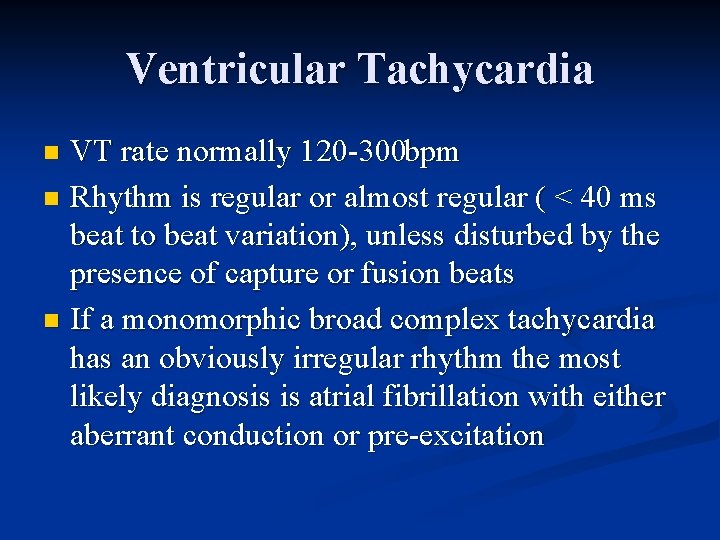
Ventricular Tachycardia VT rate normally 120 300 bpm n Rhythm is regular or almost regular ( < 40 ms beat to beat variation), unless disturbed by the presence of capture or fusion beats n If a monomorphic broad complex tachycardia has an obviously irregular rhythm the most likely diagnosis is atrial fibrillation with either aberrant conduction or pre excitation n
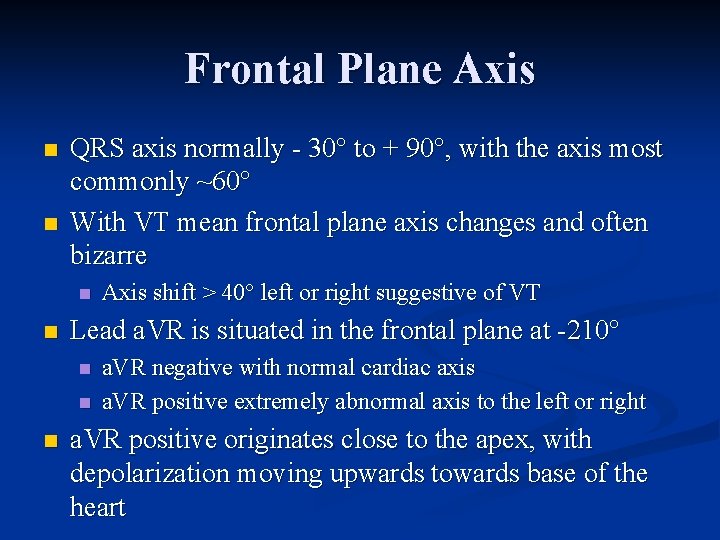
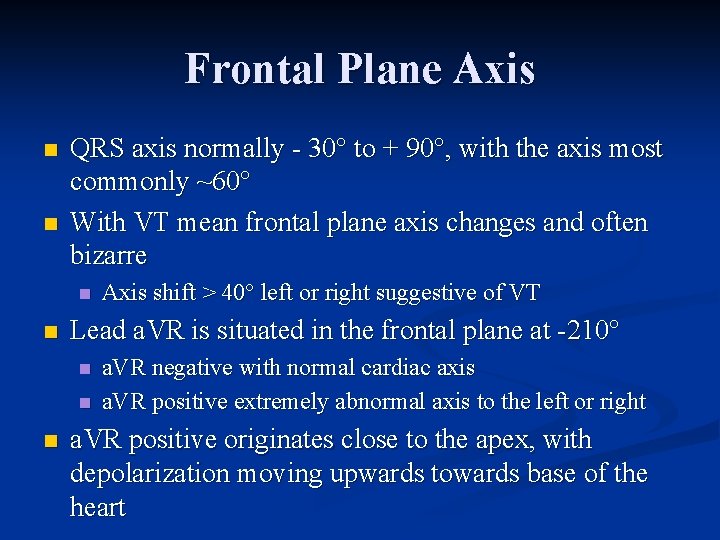
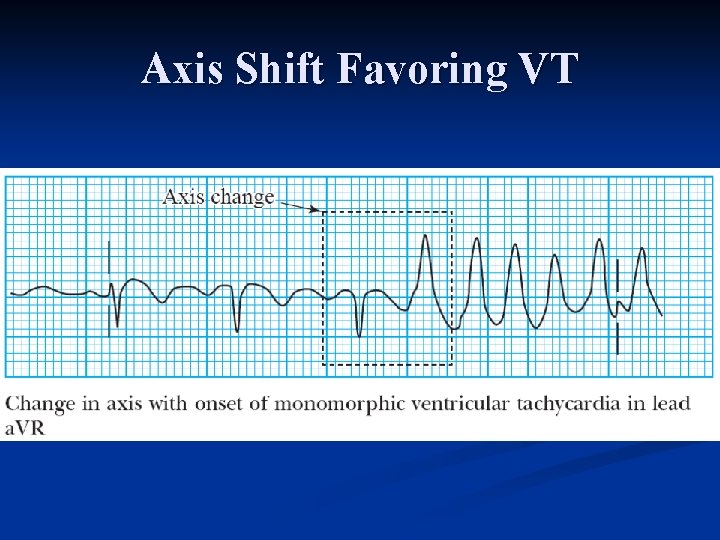
Frontal Plane Axis n n QRS axis normally 30° to + 90°, with the axis most commonly ~60° With VT mean frontal plane axis changes and often bizarre n n Lead a. VR is situated in the frontal plane at 210° n n n Axis shift > 40° left or right suggestive of VT a. VR negative with normal cardiac axis a. VR positive extremely abnormal axis to the left or right a. VR positive originates close to the apex, with depolarization moving upwards towards base of the heart
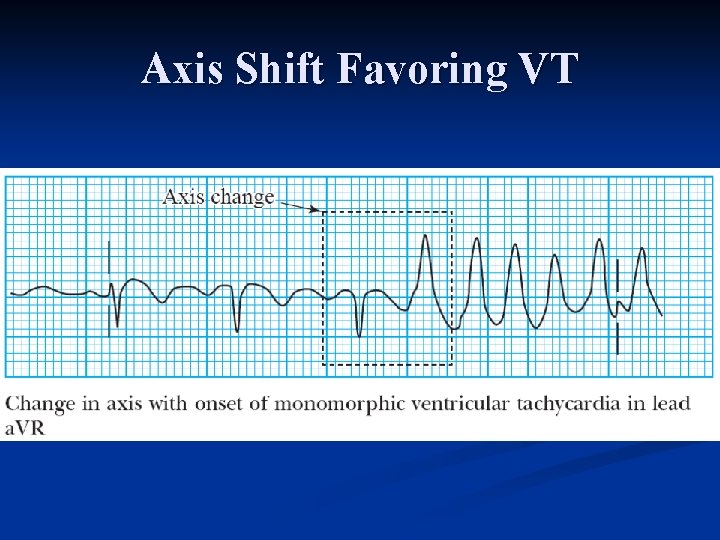
Axis Shift Favoring VT
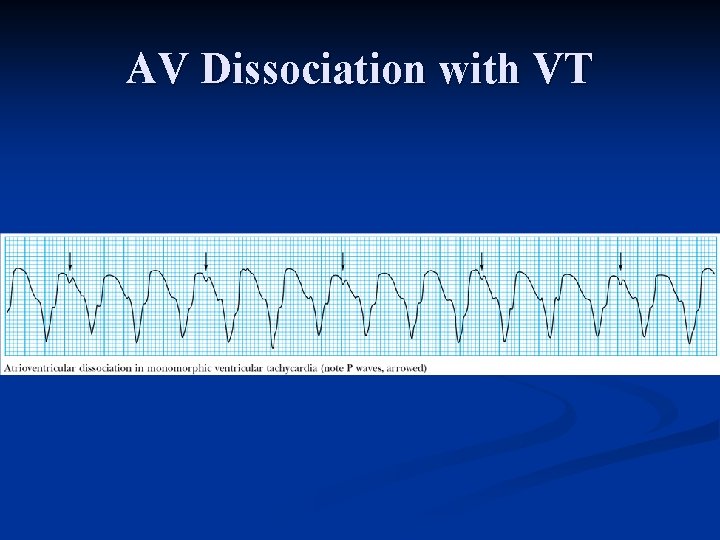
Direct Evidence of Independent Atrial Activity With VT, sinus node continues to initiate atrial contraction n P waves are dissociated from the QRS complexes and are positive in leads I and II n Atrial rate usually slower than the ventricular rate n AV dissociation usually diagnostic for VT, lack of direct evidence of independent P wave activity does not exclude the diagnosis n
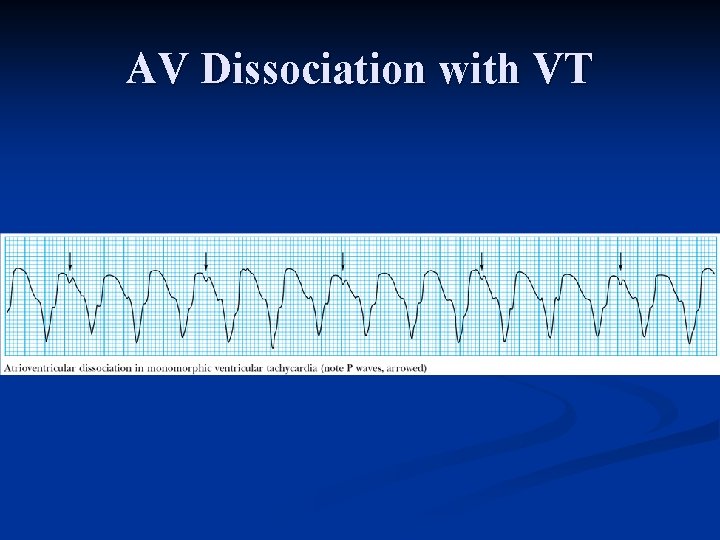
AV Dissociation with VT
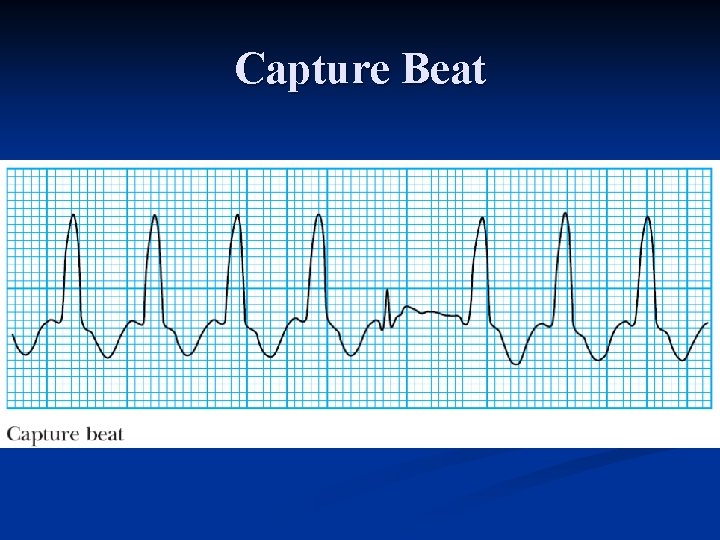
Indirect Evidence of Independent Atrial Activity n Capture beat Occasionally an atrial impulse may cause ventricular depolarization via the normal conduction system n Resulting QRS complex occurs earlier than expected and is narrow n Shows that even at rapid rates the conduction system is able to conduct normally, thus making a diagnosis of SVT with aberrancy unlikely n Capture beats are uncommon and their absence does not exclude the diagnosis n
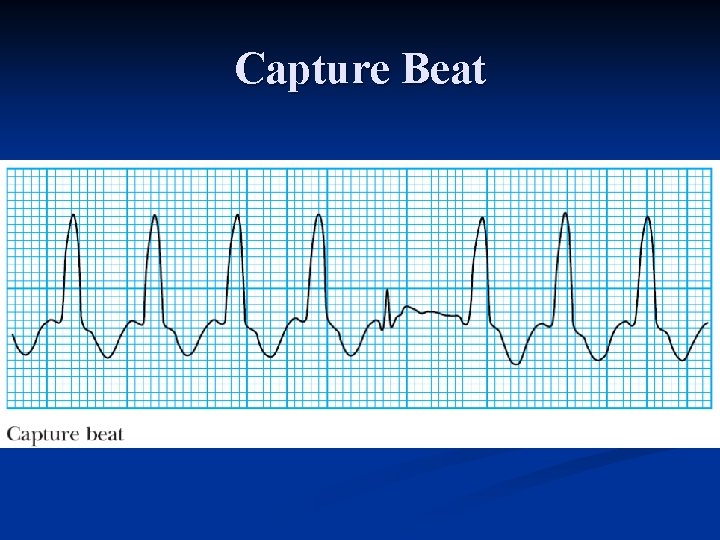
Capture Beat
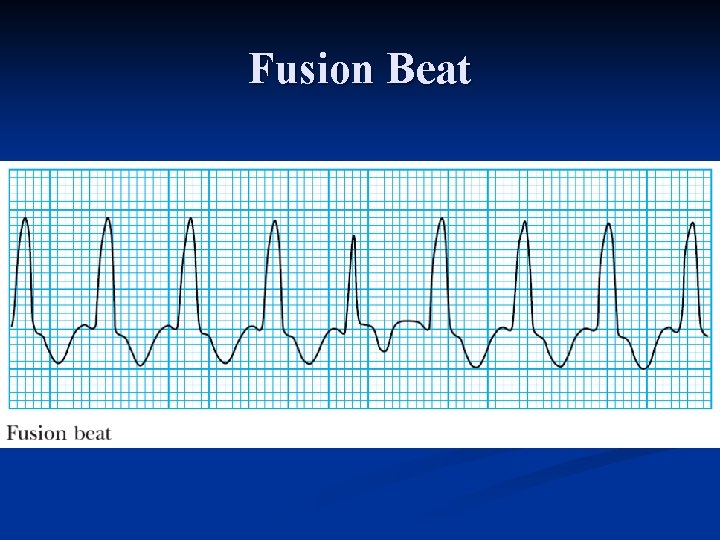
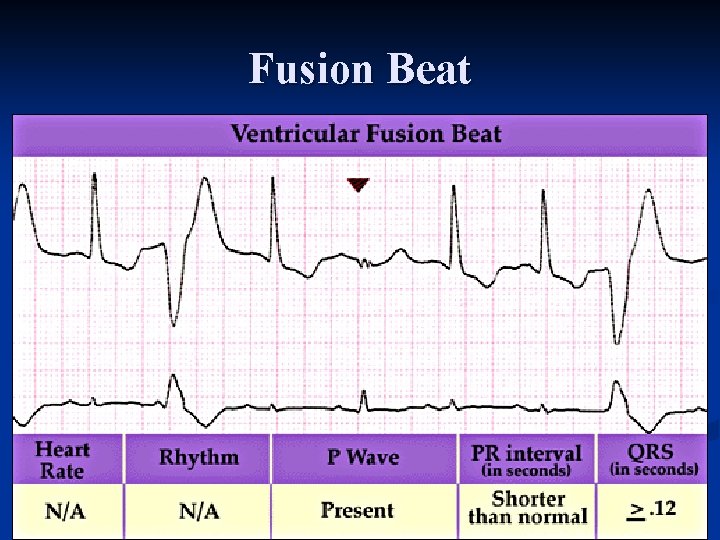
Indirect Evidence of Independent Atrial Activity n Fusion beats Occurs when a sinus beat conducts to the ventricles via the AV node and fuses with a beat arising in the ventricles n Resulting QRS complex has an appearance intermediate between a normal beat and a tachycardia beat n Fusion beats are uncommon and their absence does not exclude the diagnosis n
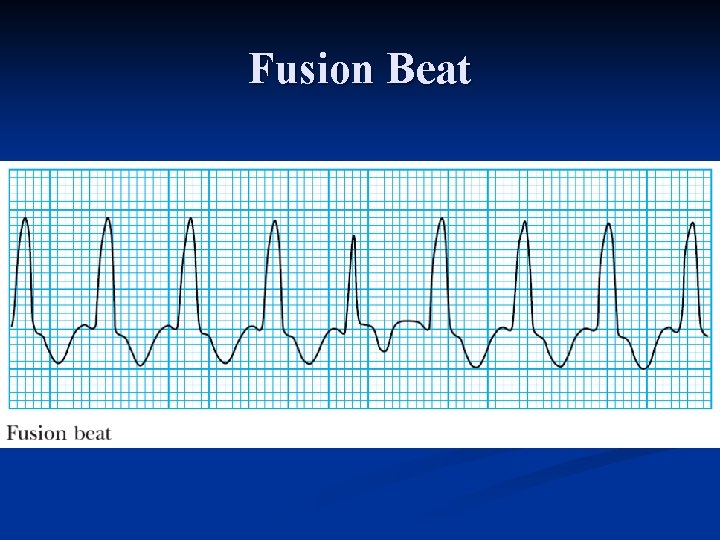
Fusion Beat
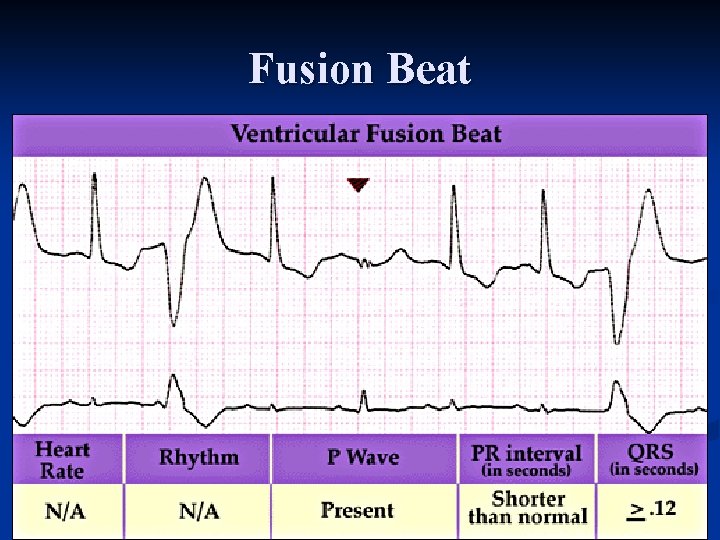
Fusion Beat
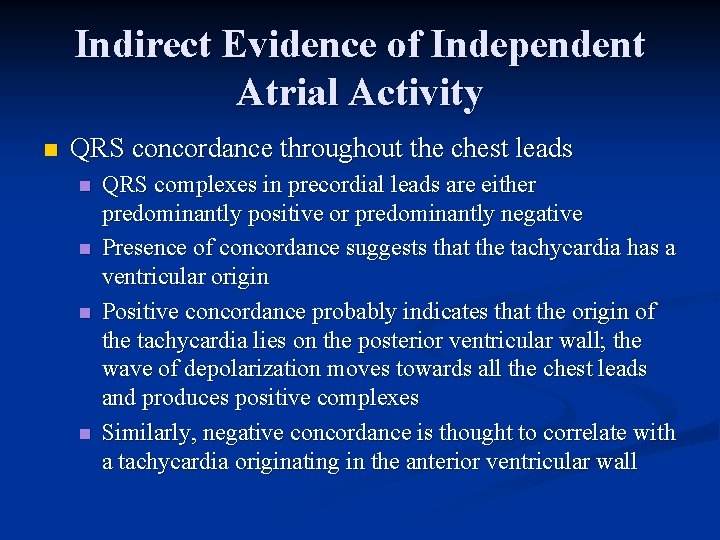
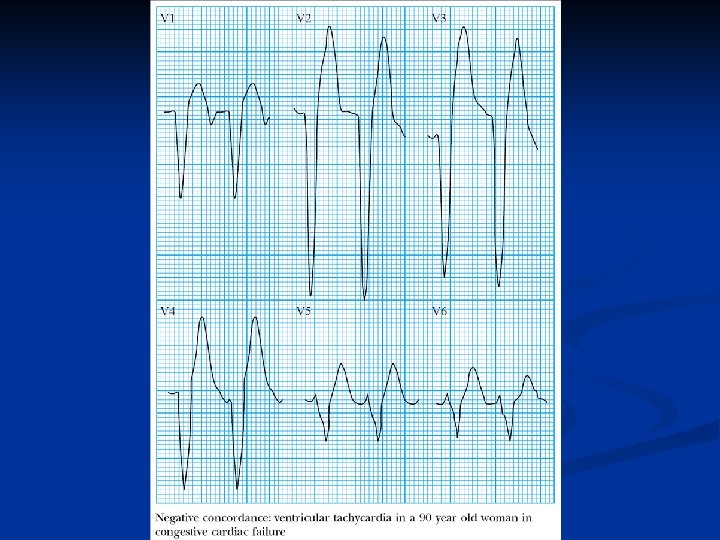
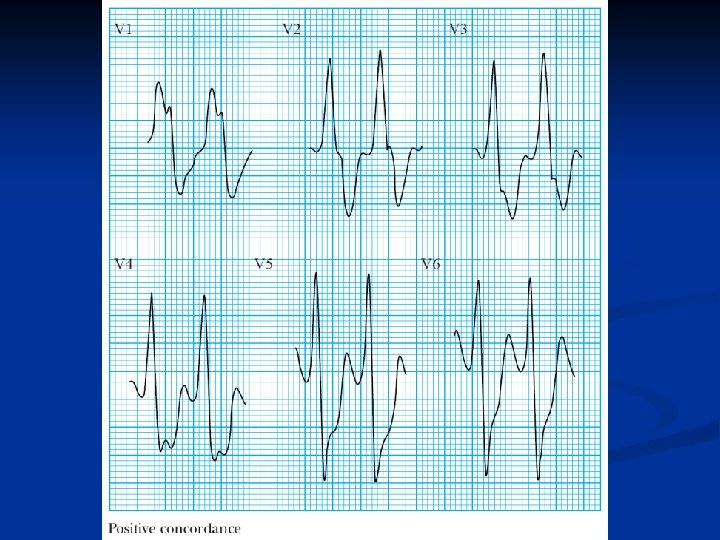
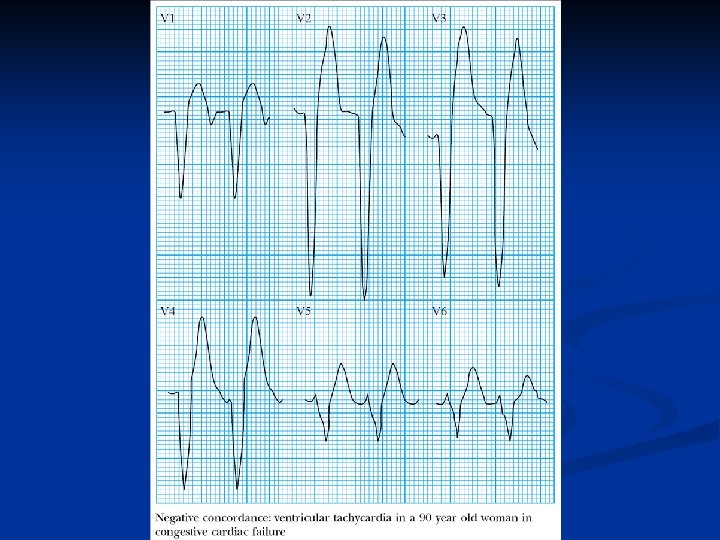
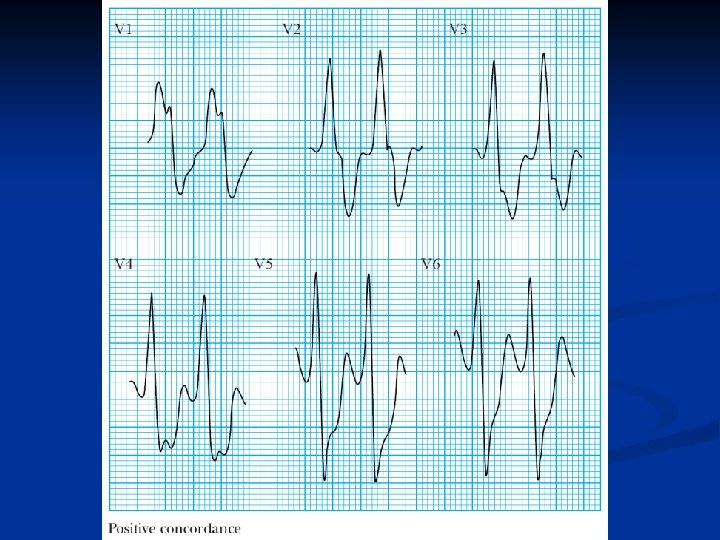
Indirect Evidence of Independent Atrial Activity n QRS concordance throughout the chest leads n n QRS complexes in precordial leads are either predominantly positive or predominantly negative Presence of concordance suggests that the tachycardia has a ventricular origin Positive concordance probably indicates that the origin of the tachycardia lies on the posterior ventricular wall; the wave of depolarization moves towards all the chest leads and produces positive complexes Similarly, negative concordance is thought to correlate with a tachycardia originating in the anterior ventricular wall
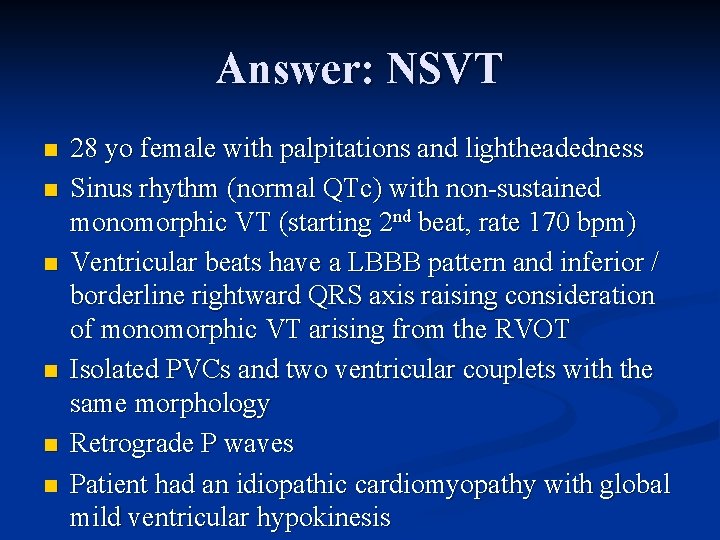
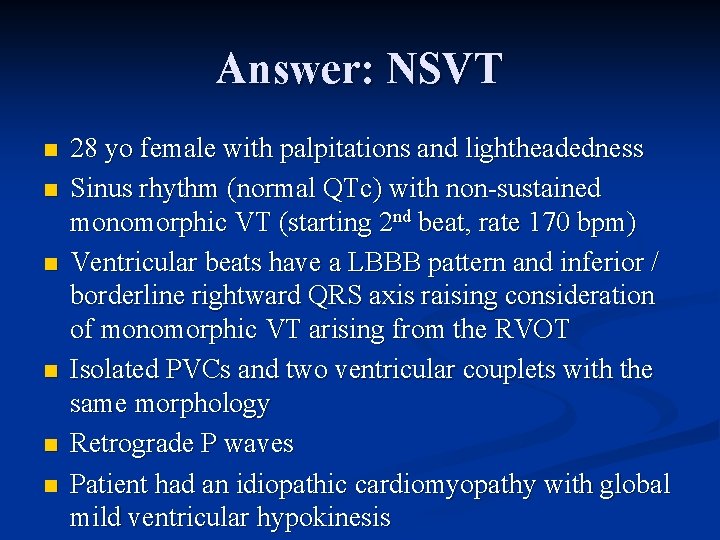
Answer: NSVT n n n 28 yo female with palpitations and lightheadedness Sinus rhythm (normal QTc) with non sustained monomorphic VT (starting 2 nd beat, rate 170 bpm) Ventricular beats have a LBBB pattern and inferior / borderline rightward QRS axis raising consideration of monomorphic VT arising from the RVOT Isolated PVCs and two ventricular couplets with the same morphology Retrograde P waves Patient had an idiopathic cardiomyopathy with global mild ventricular hypokinesis
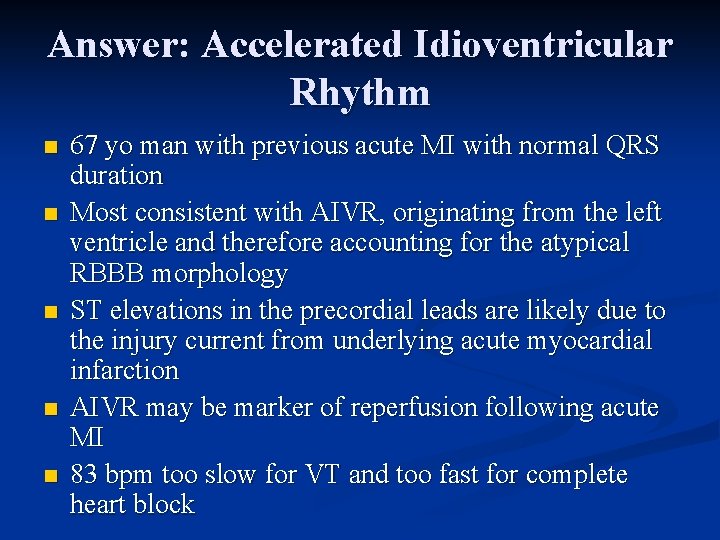
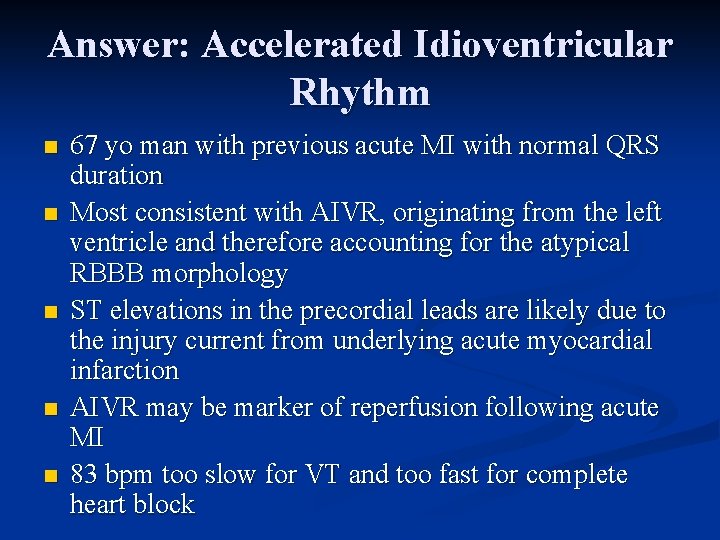
Answer: Accelerated Idioventricular Rhythm n n n 67 yo man with previous acute MI with normal QRS duration Most consistent with AIVR, originating from the left ventricle and therefore accounting for the atypical RBBB morphology ST elevations in the precordial leads are likely due to the injury current from underlying acute myocardial infarction AIVR may be marker of reperfusion following acute MI 83 bpm too slow for VT and too fast for complete heart block

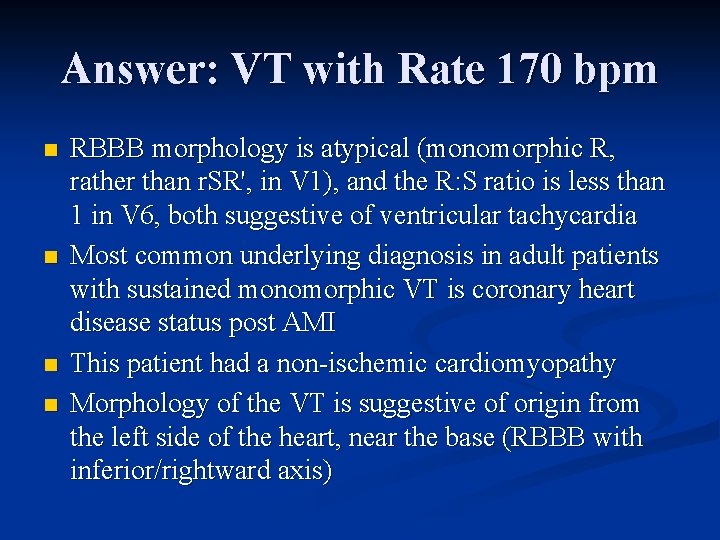
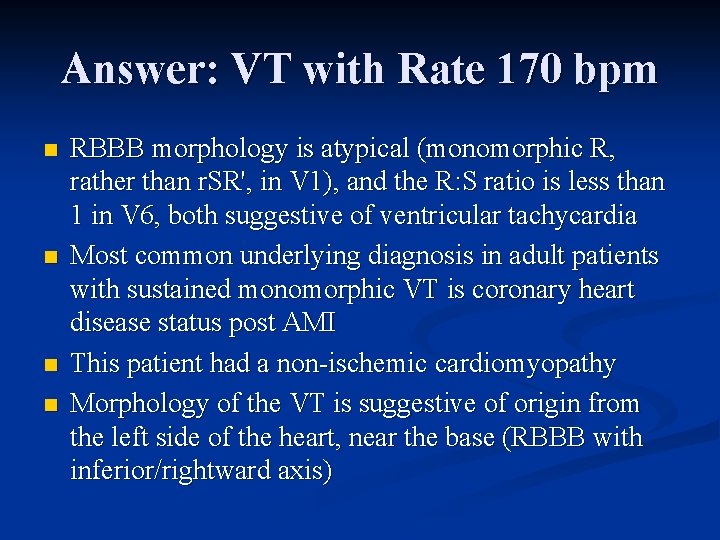
Answer: VT with Rate 170 bpm n n RBBB morphology is atypical (monomorphic R, rather than r. SR', in V 1), and the R: S ratio is less than 1 in V 6, both suggestive of ventricular tachycardia Most common underlying diagnosis in adult patients with sustained monomorphic VT is coronary heart disease status post AMI This patient had a non ischemic cardiomyopathy Morphology of the VT is suggestive of origin from the left side of the heart, near the base (RBBB with inferior/rightward axis)
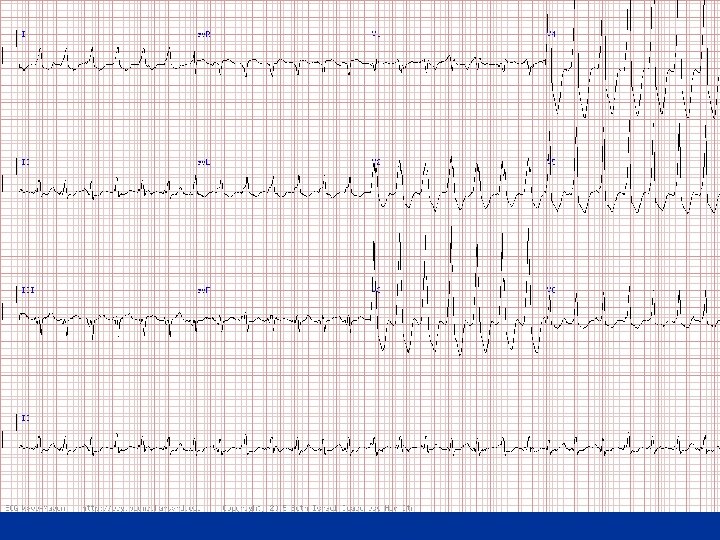
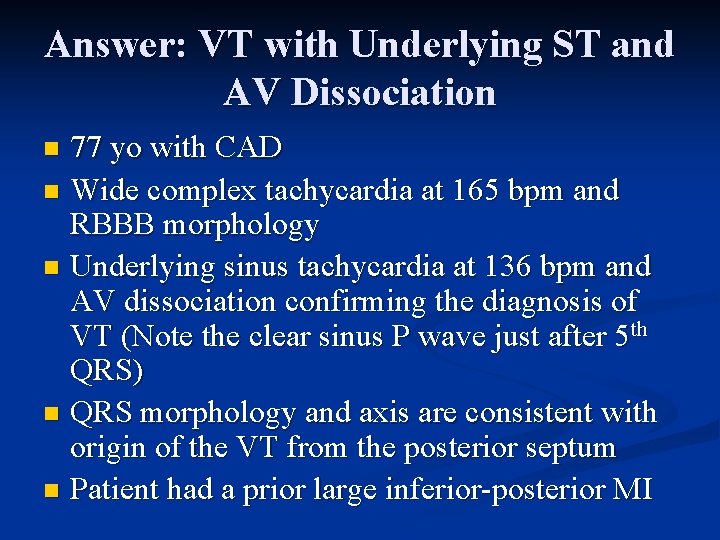
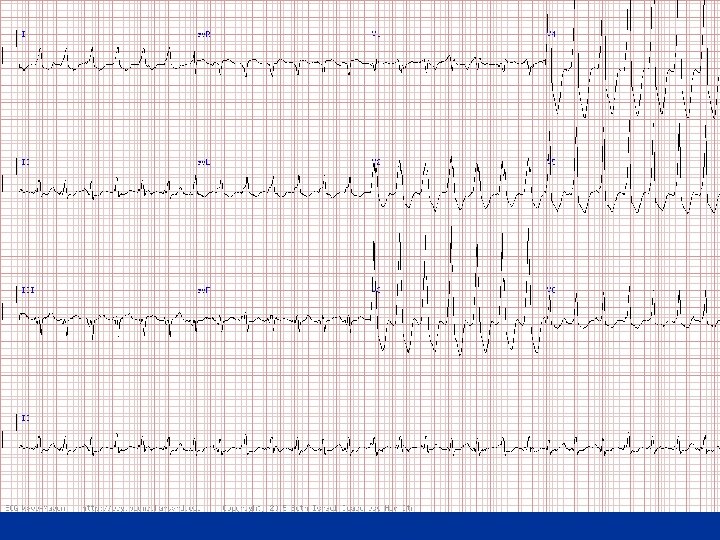
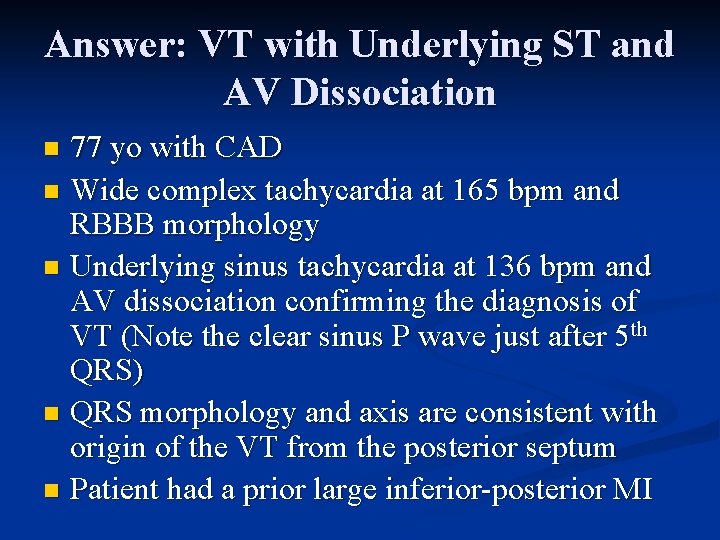
Answer: VT with Underlying ST and AV Dissociation 77 yo with CAD n Wide complex tachycardia at 165 bpm and RBBB morphology n Underlying sinus tachycardia at 136 bpm and AV dissociation confirming the diagnosis of VT (Note the clear sinus P wave just after 5 th QRS) n QRS morphology and axis are consistent with origin of the VT from the posterior septum n Patient had a prior large inferior posterior MI n
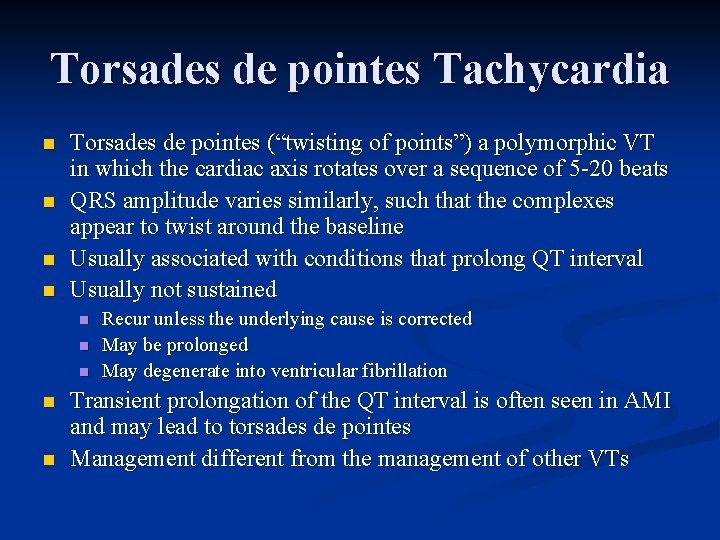
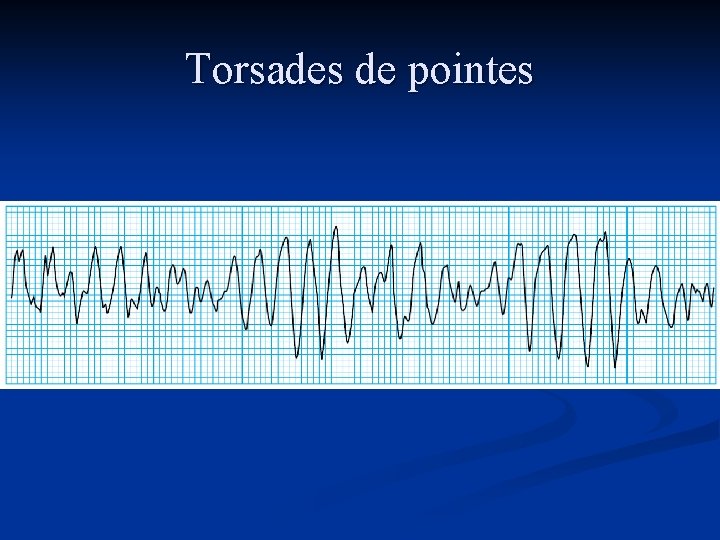
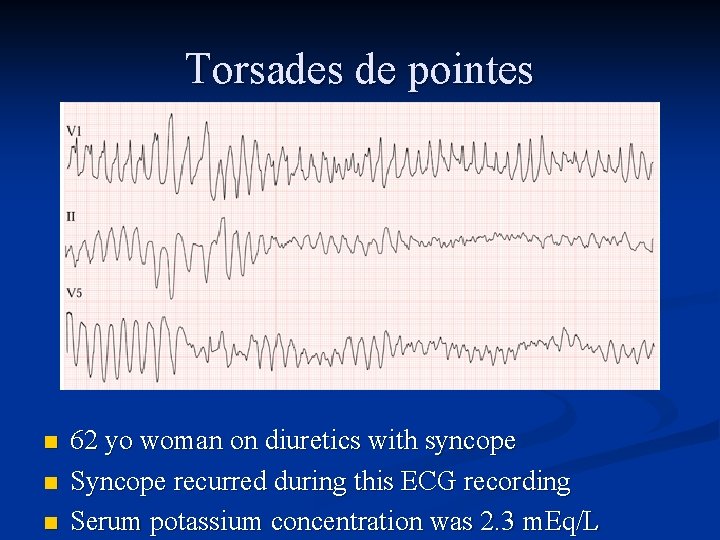
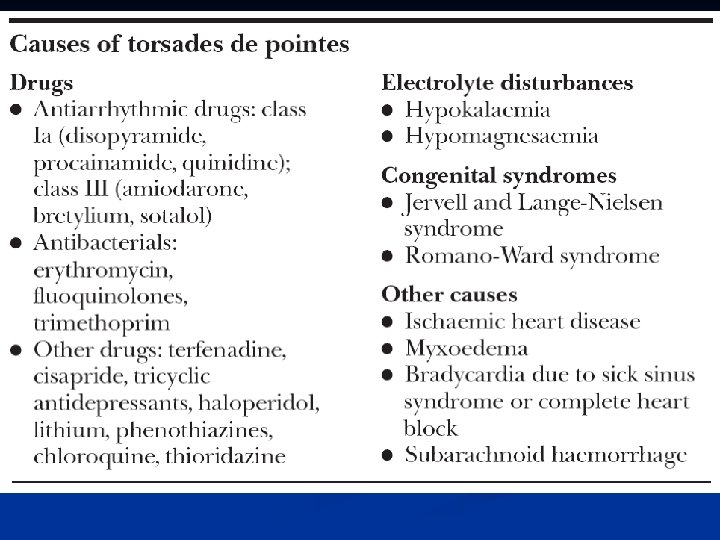
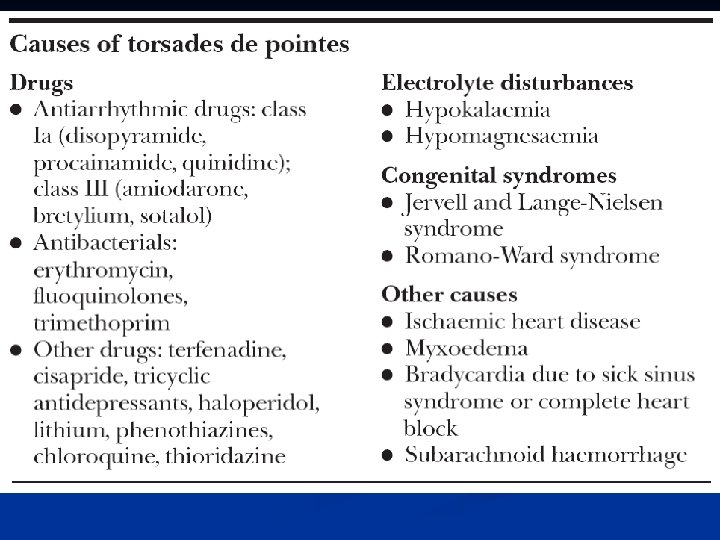
Torsades de pointes Tachycardia n n Torsades de pointes (“twisting of points”) a polymorphic VT in which the cardiac axis rotates over a sequence of 5 20 beats QRS amplitude varies similarly, such that the complexes appear to twist around the baseline Usually associated with conditions that prolong QT interval Usually not sustained n n n Recur unless the underlying cause is corrected May be prolonged May degenerate into ventricular fibrillation Transient prolongation of the QT interval is often seen in AMI and may lead to torsades de pointes Management different from the management of other VTs
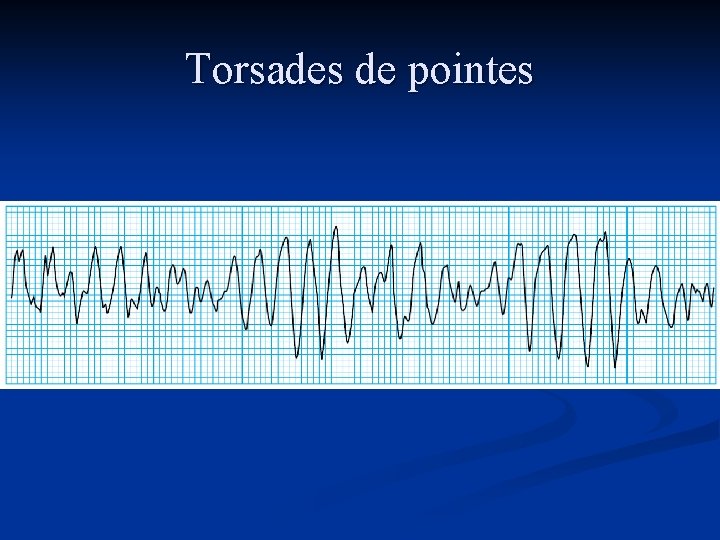
Torsades de pointes
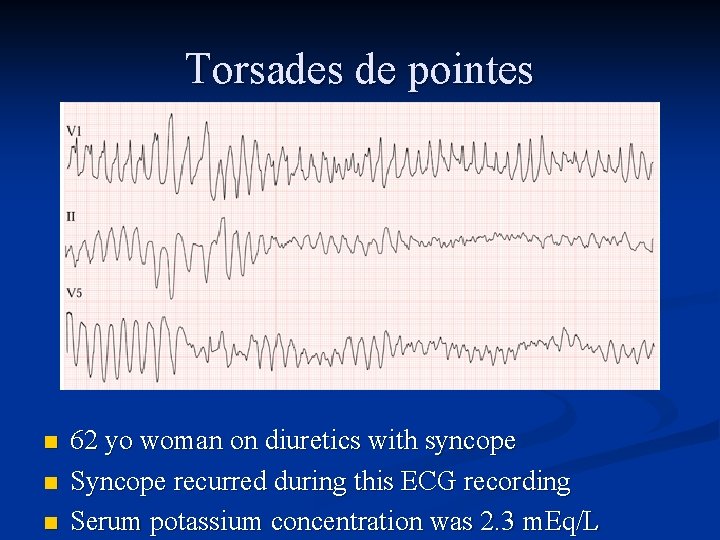
Torsades de pointes n n n 62 yo woman on diuretics with syncope Syncope recurred during this ECG recording Serum potassium concentration was 2. 3 m. Eq/L
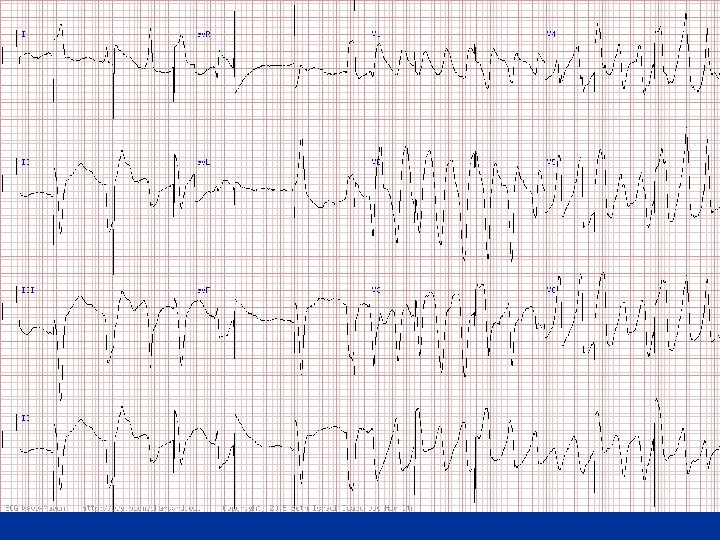
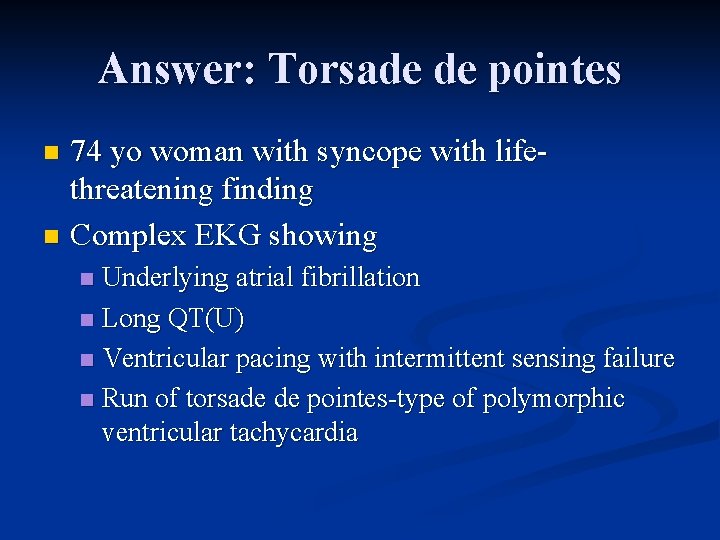
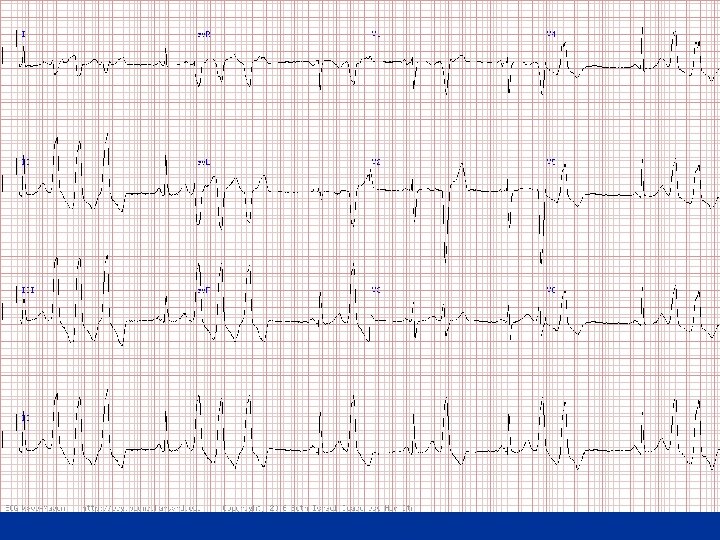
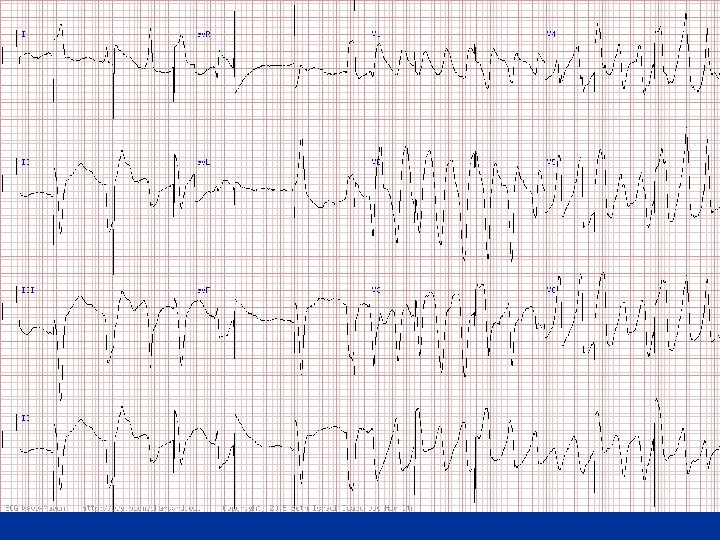
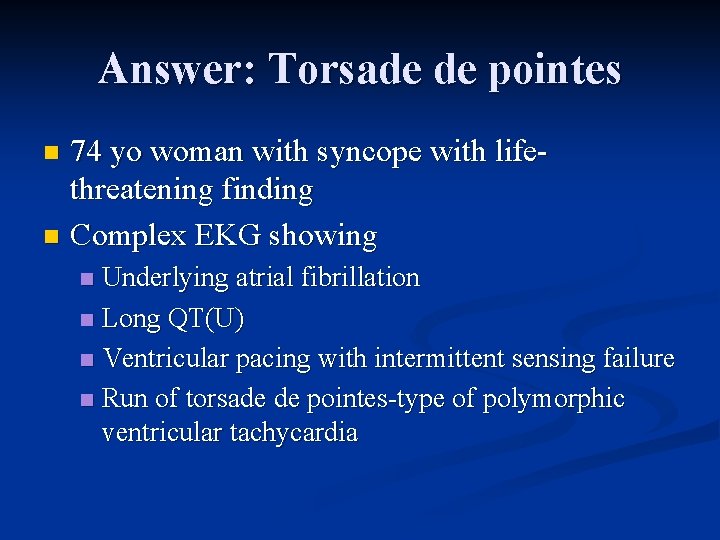
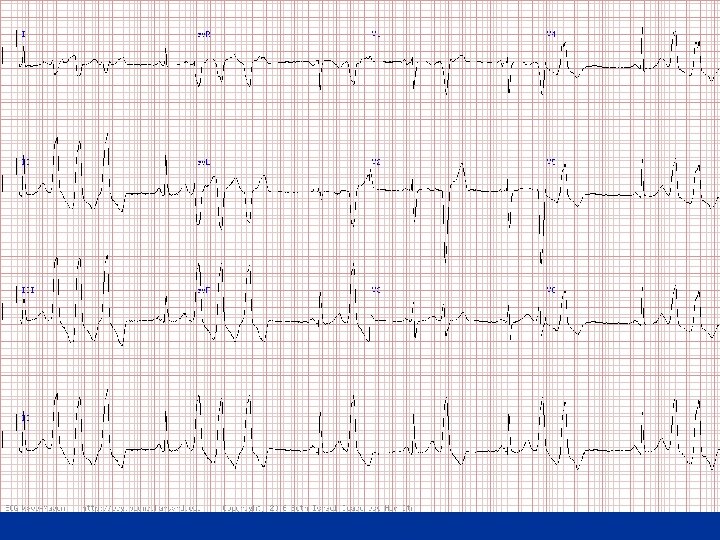
Answer: Torsade de pointes 74 yo woman with syncope with life threatening finding n Complex EKG showing n Underlying atrial fibrillation n Long QT(U) n Ventricular pacing with intermittent sensing failure n Run of torsade de pointes type of polymorphic ventricular tachycardia n
Pacemakers
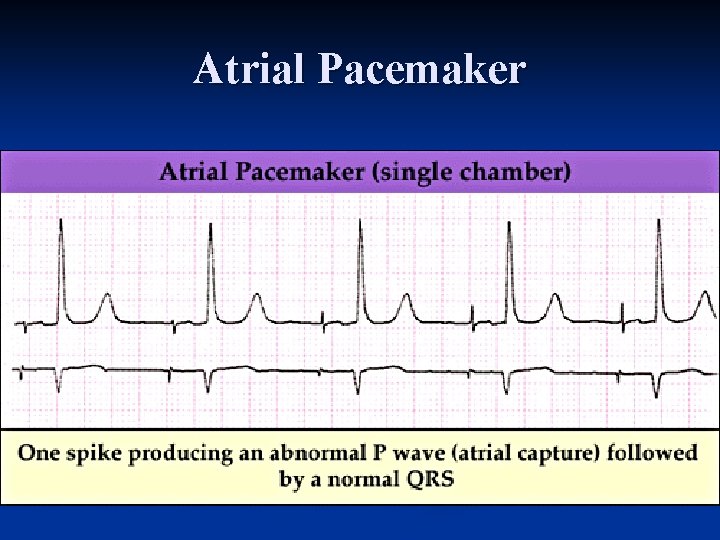
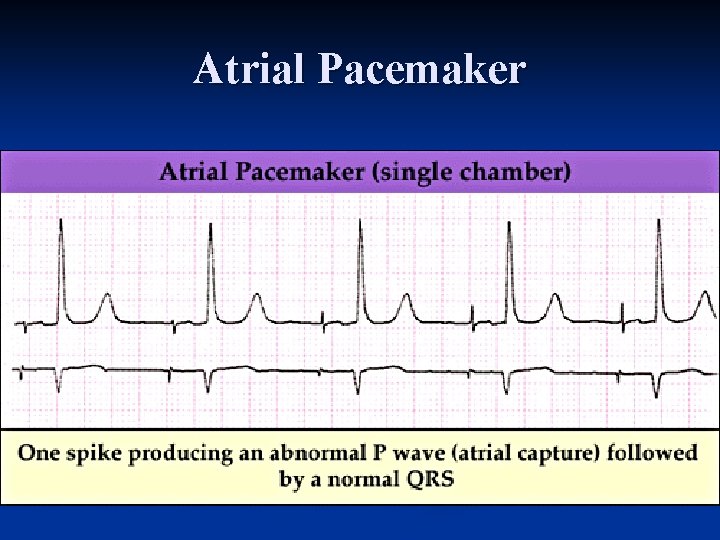
Atrial Pacemaker
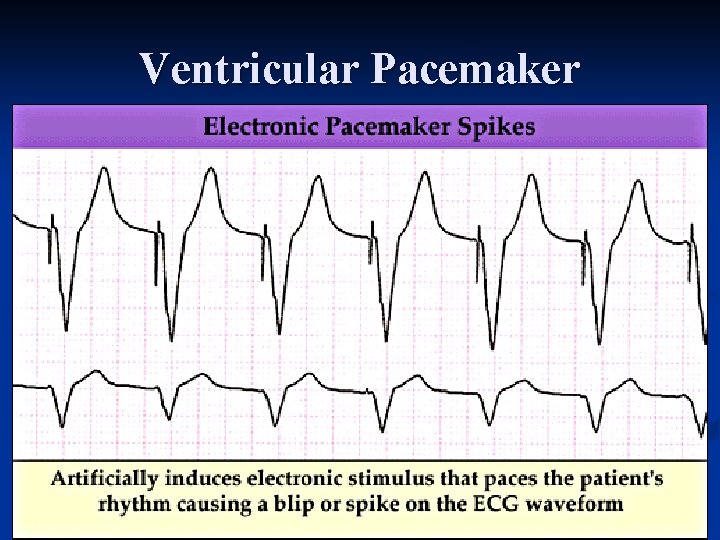
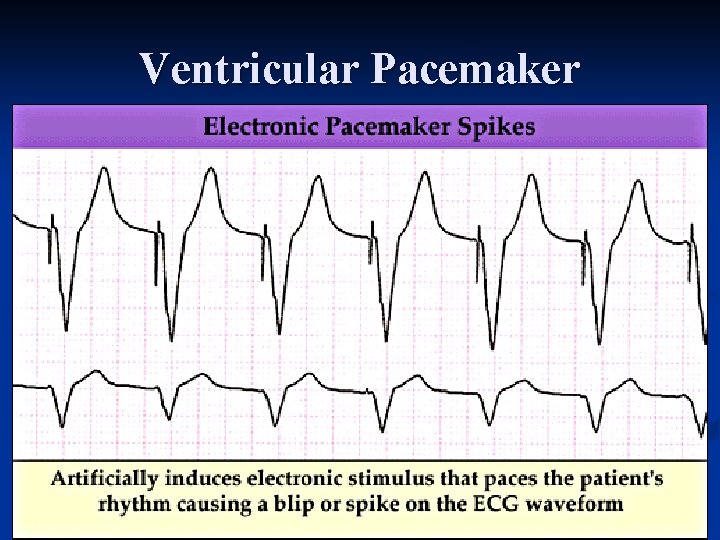
Ventricular Pacemaker
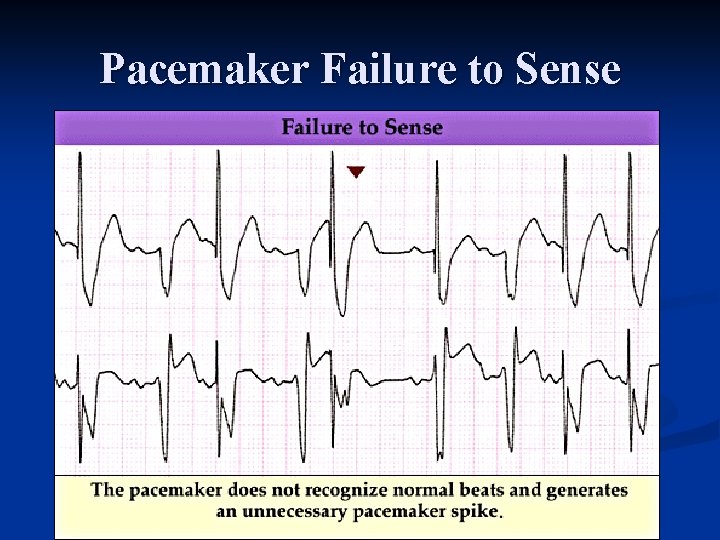
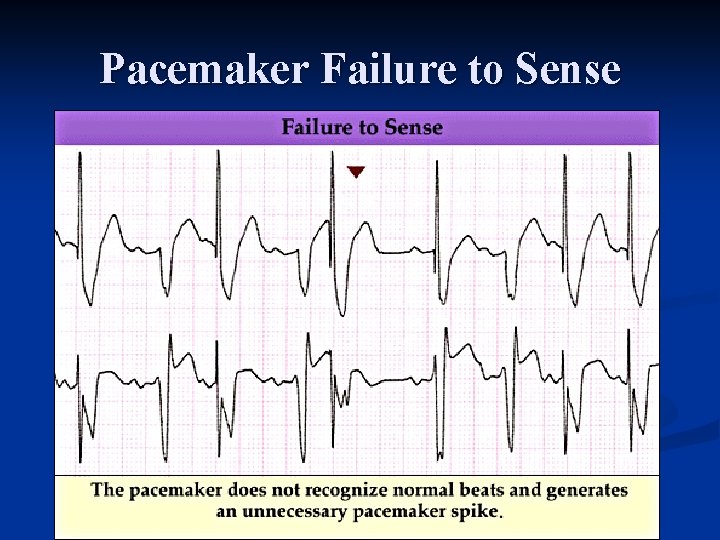
Pacemaker Failure to Sense
Pacemaker Failure to Capture
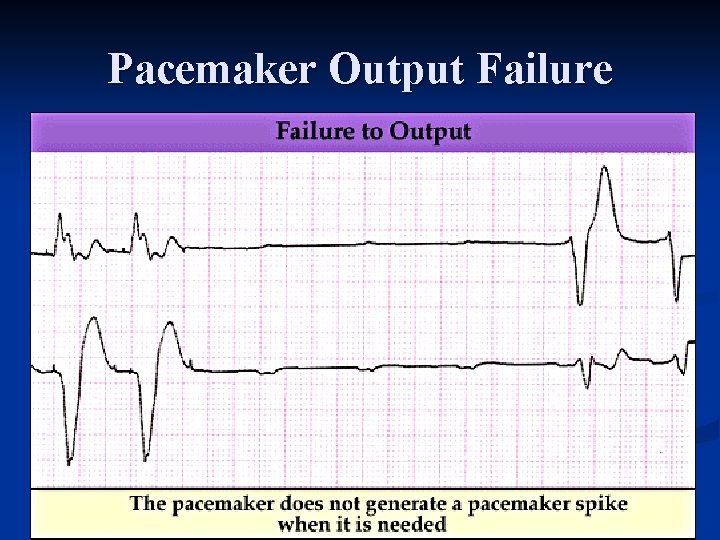
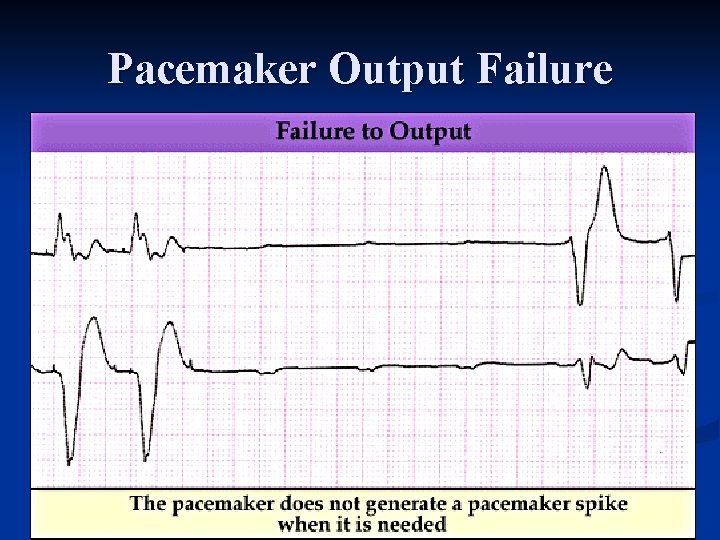
Pacemaker Output Failure
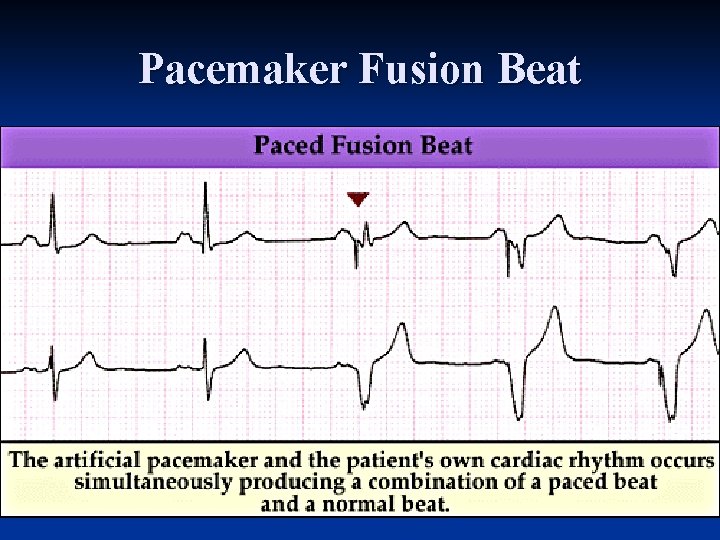
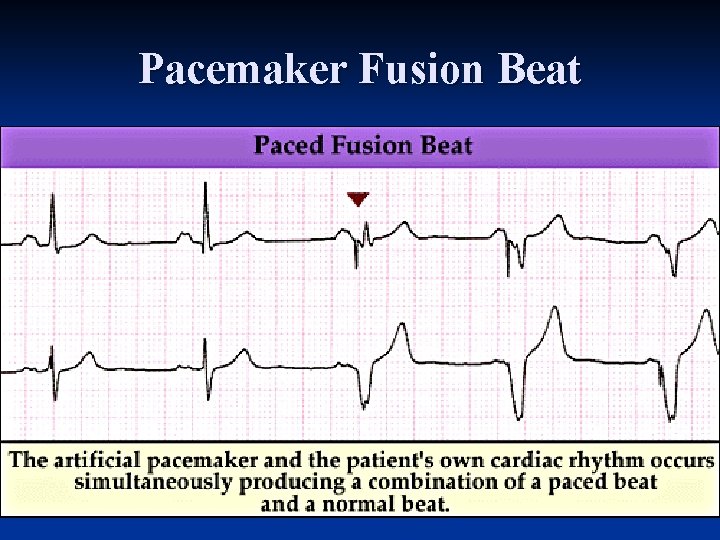
Pacemaker Fusion Beat
Last But Not Least

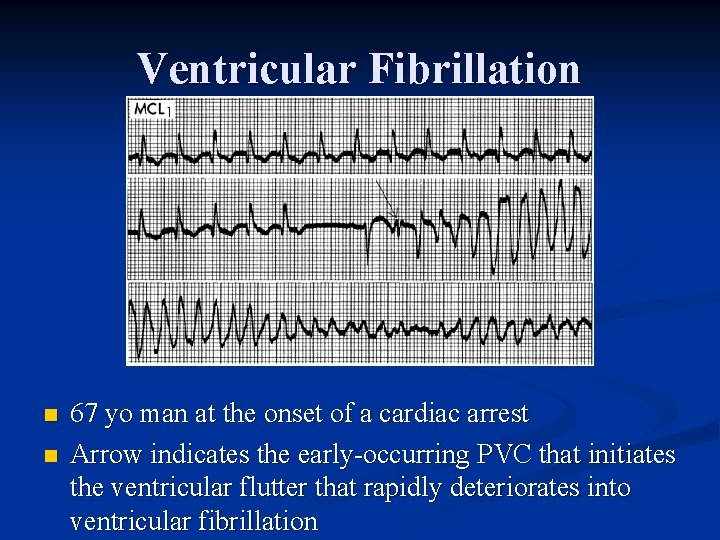
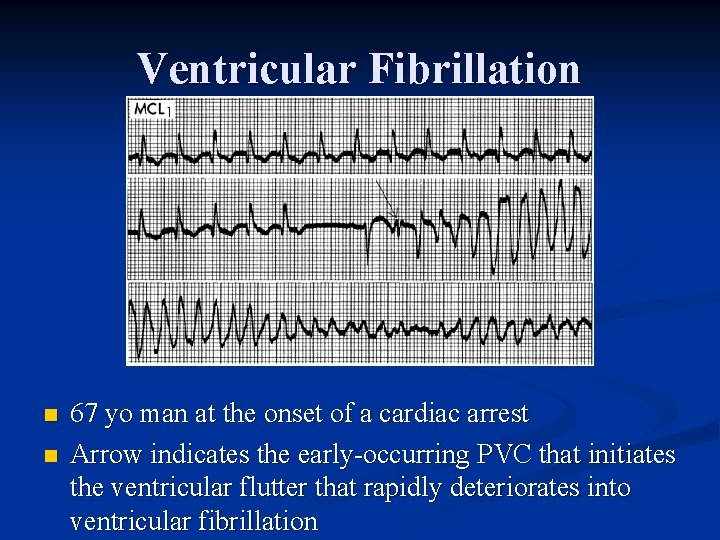
Ventricular Fibrillation n n 67 yo man at the onset of a cardiac arrest Arrow indicates the early occurring PVC that initiates the ventricular flutter that rapidly deteriorates into ventricular fibrillation
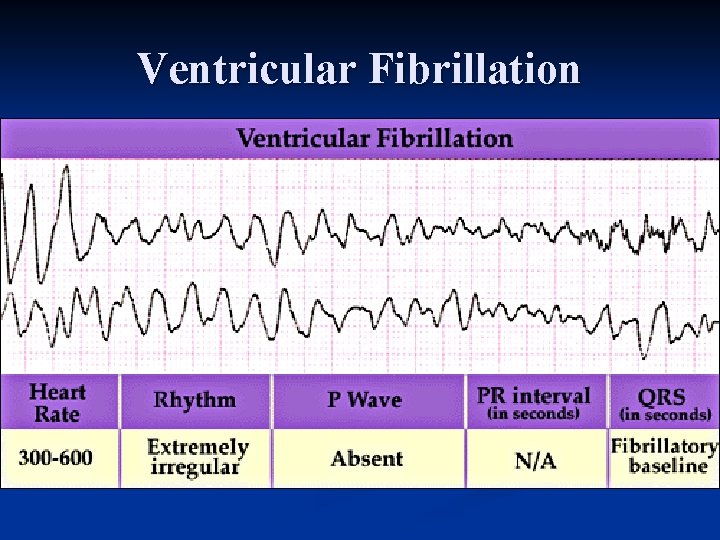
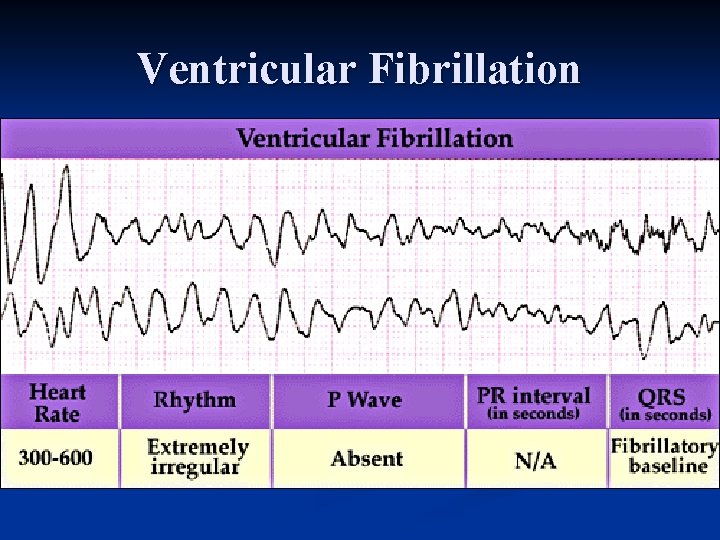
Ventricular Fibrillation

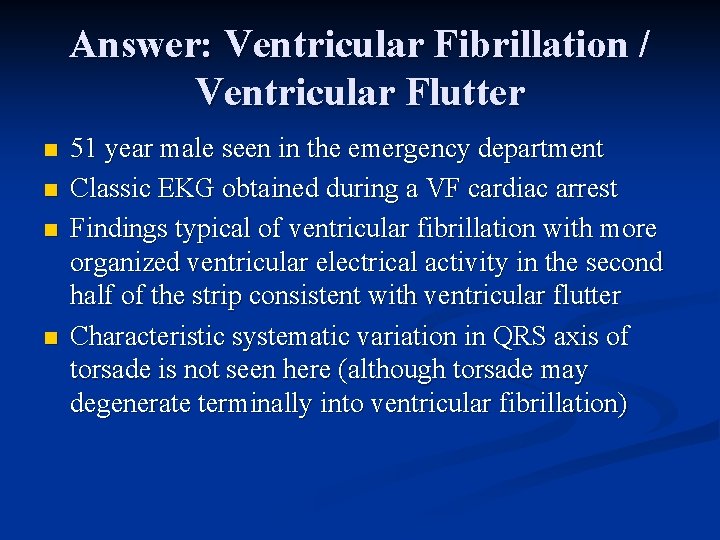
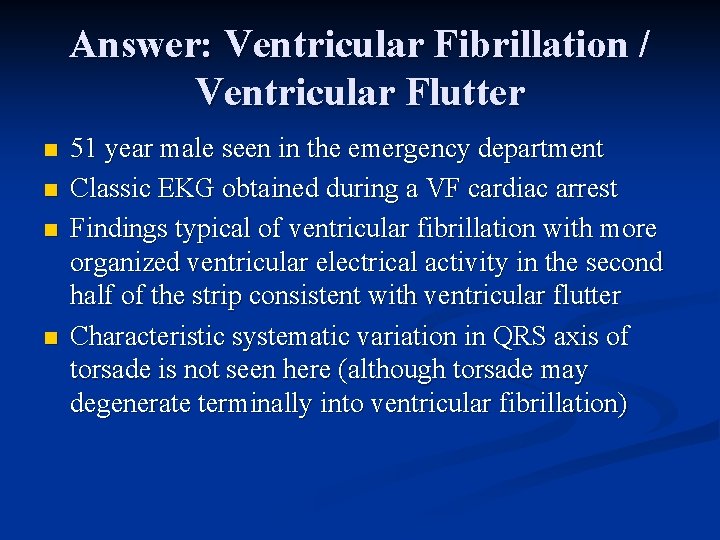
Answer: Ventricular Fibrillation / Ventricular Flutter n n 51 year male seen in the emergency department Classic EKG obtained during a VF cardiac arrest Findings typical of ventricular fibrillation with more organized ventricular electrical activity in the second half of the strip consistent with ventricular flutter Characteristic systematic variation in QRS axis of torsade is not seen here (although torsade may degenerate terminally into ventricular fibrillation)
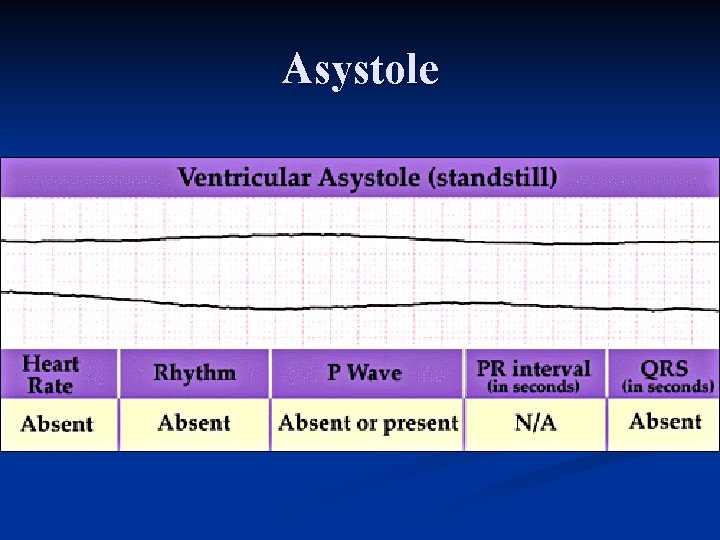
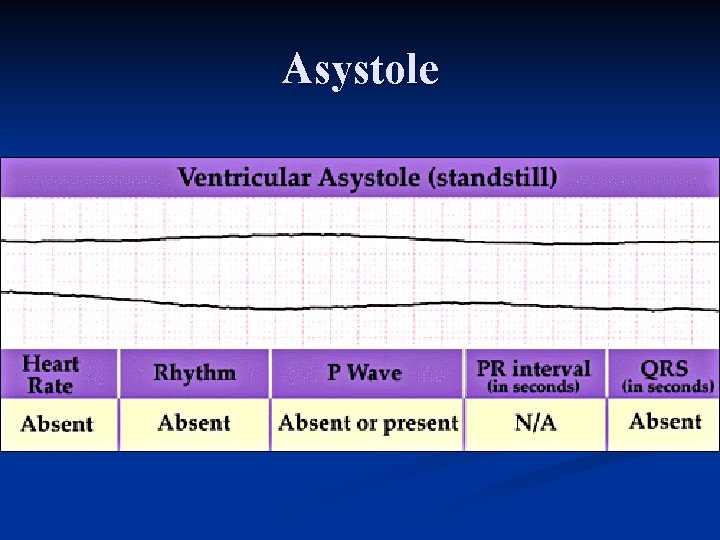
Asystole
