Medical University of Varna Postgraduate Programme in Internal

- Slides: 44
Medical University of Varna Postgraduate Programme in Internal Medicine “Pathophysiology of Cardiovascular System” PATHOPHYSIOLOGY OF STROKE Apostolos Ι. Hatzitolios Associate Professor of Internal Medicine 1 st Propedeutic Medical Department Aristotle University of Thessaloniki Department of Hypertension AND Vascular Disease AHEPA Hospital
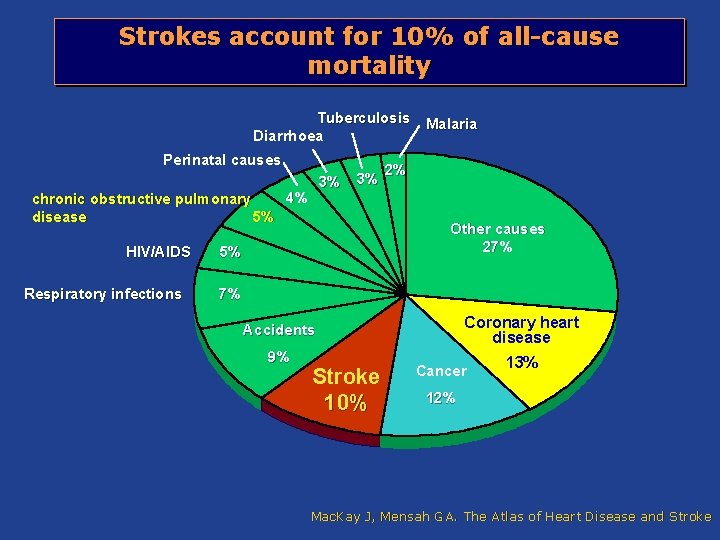
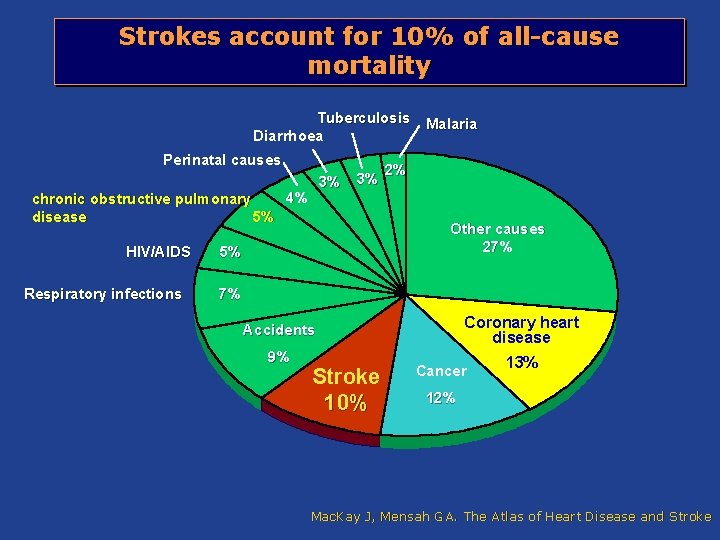
Strokes account for 10% of all-cause mortality Tuberculosis Diarrhoea Perinatal causes 3% 4% chronic obstructive pulmonary disease 5% HIV/AIDS Respiratory infections 3% Malaria 2% Other causes 27% 5% 7% Coronary heart disease Accidents 9% Stroke 10% Cancer 13% 12% Mac. Kay J, Mensah GA. The Atlas of Heart Disease and Stroke
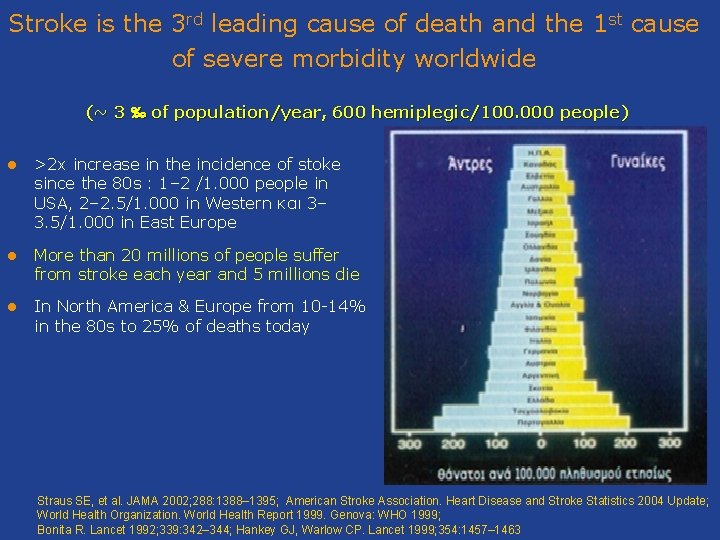
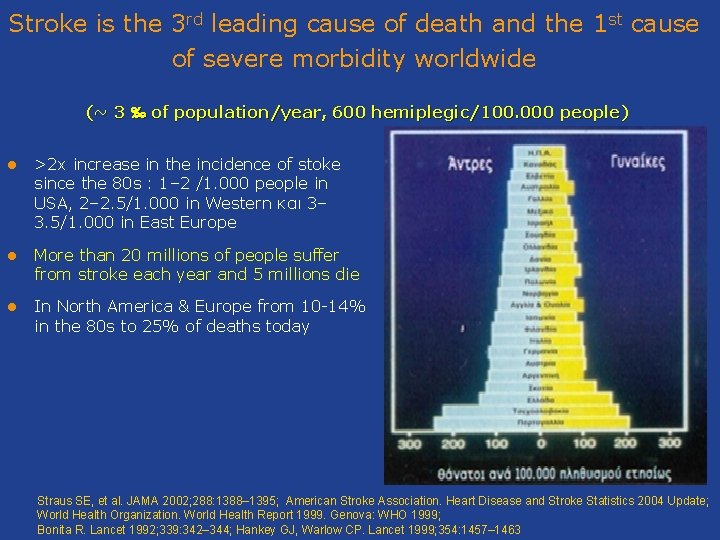
Stroke is the 3 rd leading cause of death and the 1 st cause of severe morbidity worldwide (~ 3 ‰ of population/year, 600 hemiplegic/100. 000 people) l >2 x increase in the incidence of stoke since the 80 s : 1– 2 /1. 000 people in USA, 2– 2. 5/1. 000 in Western και 3– 3. 5/1. 000 in East Europe l More than 20 millions of people suffer from stroke each year and 5 millions die l In North America & Europe from 10 -14% in the 80 s to 25% of deaths today Straus SE, et al. JAMA 2002; 288: 1388– 1395; American Stroke Association. Heart Disease and Stroke Statistics 2004 Update; World Health Organization. World Health Report 1999. Genova: WHO 1999; Bonita R. Lancet 1992; 339: 342– 344; Hankey GJ, Warlow CP. Lancet 1999; 354: 1457– 1463
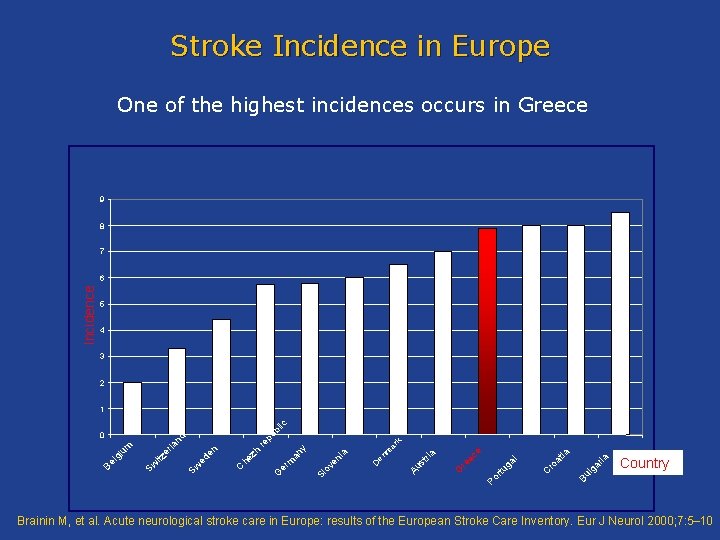
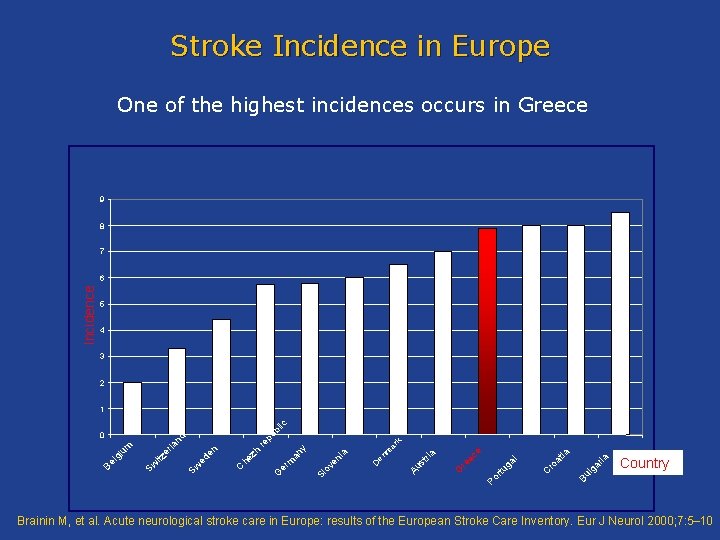
Stroke Incidence in Europe One of the highest incidences occurs in Greece 9 8 7 Incidence 6 5 4 3 2 k ia ar lg Country Bu ro C ga l rtu at ia e Po G re ec ria st Au nm De ov e Sl m er G ni a an y ar re h he z C Sw ed en er la itz Sw Be lg iu m nd 0 pu bl ic 1 Brainin M, et al. Acute neurological stroke care in Europe: results of the European Stroke Care Inventory. Eur J Neurol 2000; 7: 5– 10
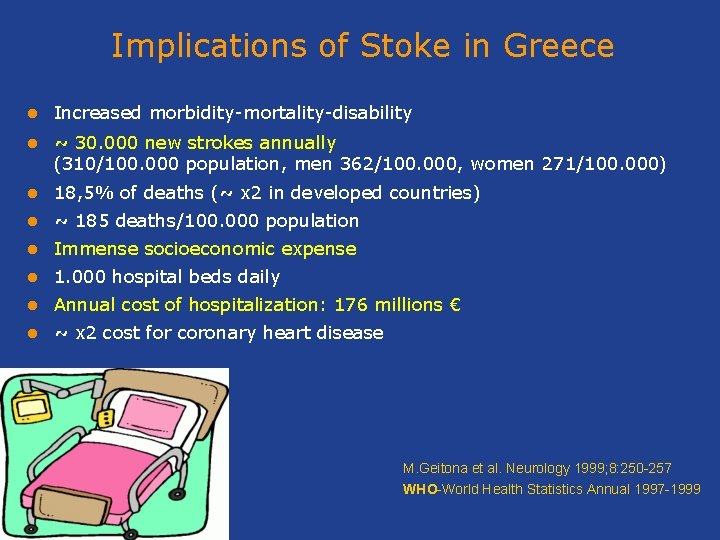
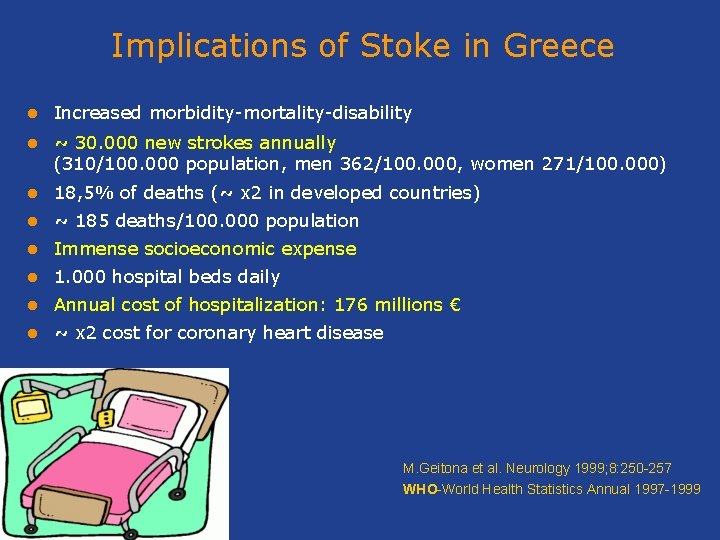
Implications of Stoke in Greece l Increased morbidity-mortality-disability l ~ 30. 000 new strokes annually (310/100. 000 population, men 362/100. 000, women 271/100. 000) l 18, 5% of deaths (~ x 2 in developed countries) l ~ 185 deaths/100. 000 population l Immense socioeconomic expense l 1. 000 hospital beds daily l Annual cost of hospitalization: 176 millions € l ~ x 2 cost for coronary heart disease Μ. Geitona et al. Νeurology 1999; 8: 250 -257 WHO-World Health Statistics Annual 1997 -1999
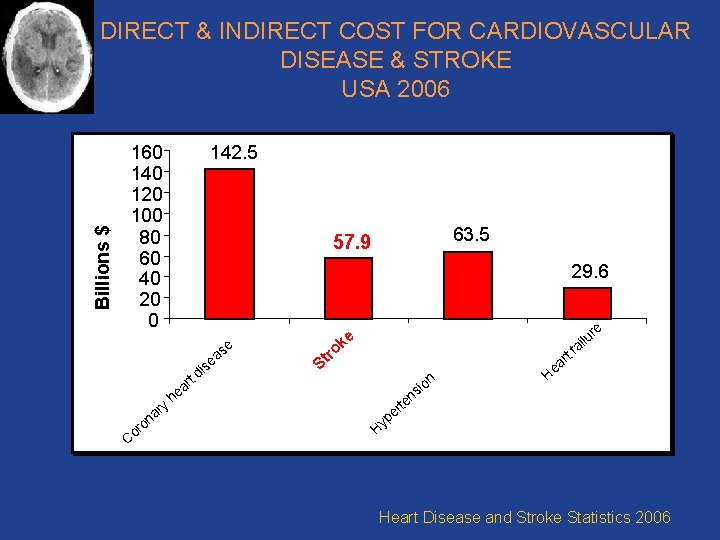
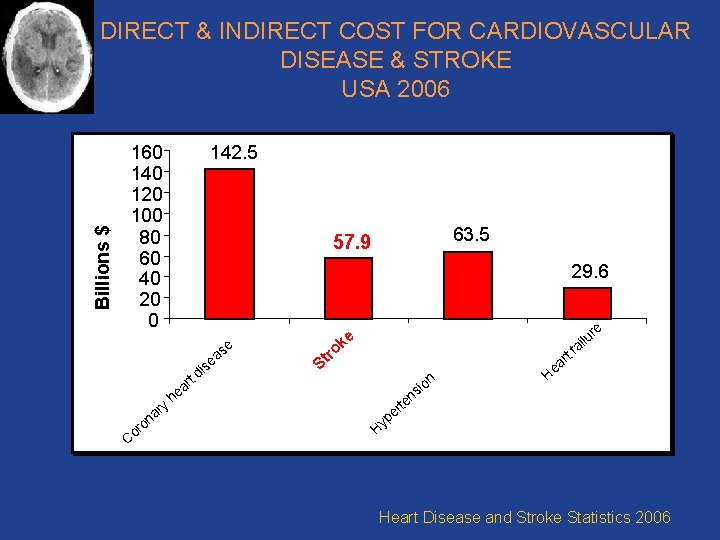
Billions $ DIRECT & INDIRECT COST FOR CARDIOVASCULAR DISEASE & STROKE USA 2006 160 140 120 100 80 60 40 20 0 142. 5 29. 6 e i td y ar n ro Co 63. 5 57. 9 s s ea ke ro t S ar e h i on s en t ar lu ai re f He rt e yp H Heart Disease and Stroke Statistics 2006
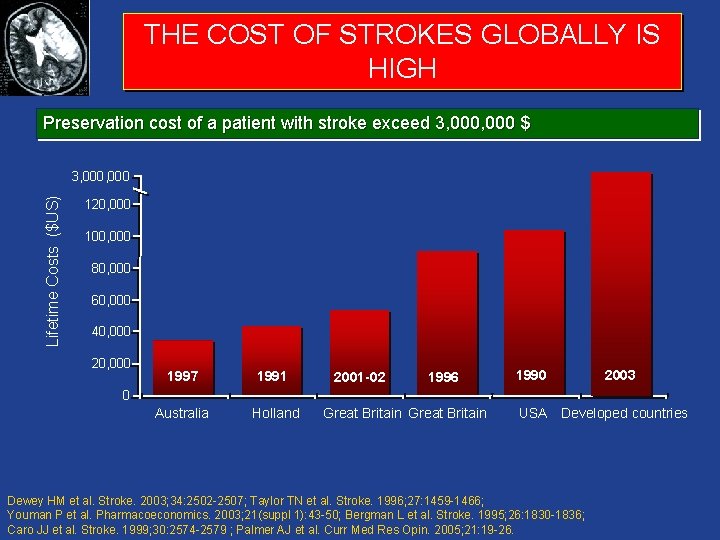
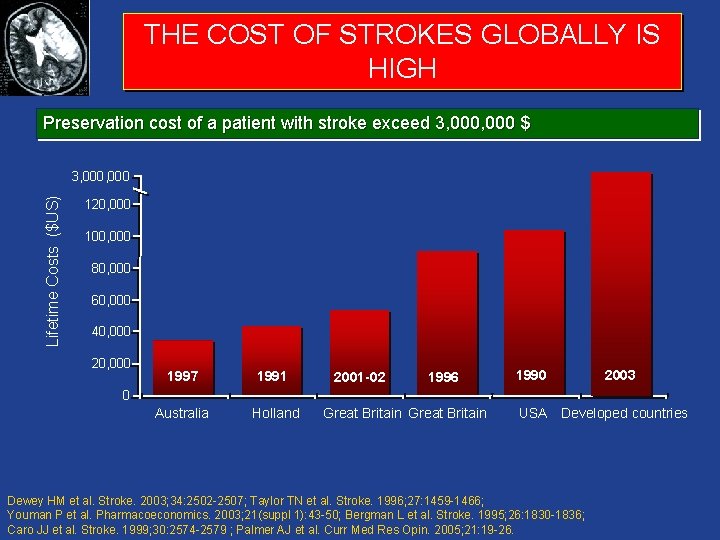
THE COST OF STROKES GLOBALLY IS HIGH Preservation cost of a patient with stroke exceed 3, 000 $ Lifetime Costs ($US) 3, 000 120, 000 100, 000 80, 000 60, 000 40, 000 20, 000 1997 1991 Australia Holland 2001 -02 1996 1990 2003 0 Great Britain USA Developed countries Dewey HM et al. Stroke. 2003; 34: 2502 -2507; Taylor TN et al. Stroke. 1996; 27: 1459 -1466; Youman P et al. Pharmacoeconomics. 2003; 21(suppl 1): 43 -50; Bergman L et al. Stroke. 1995; 26: 1830 -1836; Caro JJ et al. Stroke. 1999; 30: 2574 -2579 ; Palmer AJ et al. Curr Med Res Opin. 2005; 21: 19 -26.
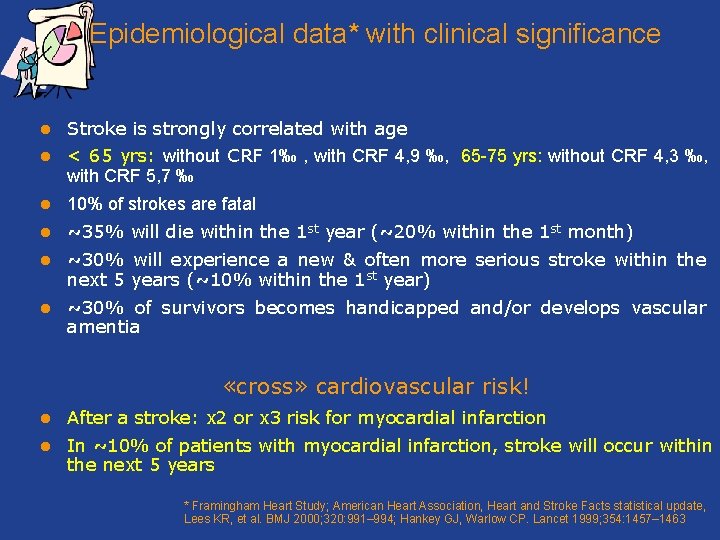
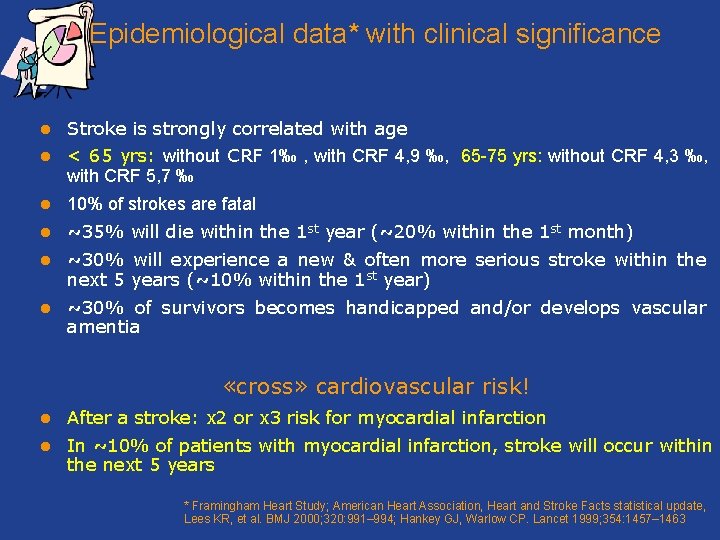
Epidemiological data* with clinical significance l Stroke is strongly correlated with age l < 65 yrs: without CRF 1‰ , with CRF 4, 9 ‰, 65 -75 yrs: without CRF 4, 3 ‰, with CRF 5, 7 ‰ l 10% of strokes are fatal l ~35% will die within the 1 st year (~20% within the 1 st month) l ~30% will experience a new & often more serious stroke within the next 5 years (~10% within the 1 st year) l ~30% of survivors becomes handicapped and/or develops vascular amentia «cross» cardiovascular risk! l After a stroke: x 2 or x 3 risk for myocardial infarction l In ~10% of patients with myocardial infarction, stroke will occur within the next 5 years * Framingham Heart Study; American Heart Association, Heart and Stroke Facts statistical update, Lees KR, et al. BMJ 2000; 320: 991– 994; Hankey GJ, Warlow CP. Lancet 1999; 354: 1457– 1463
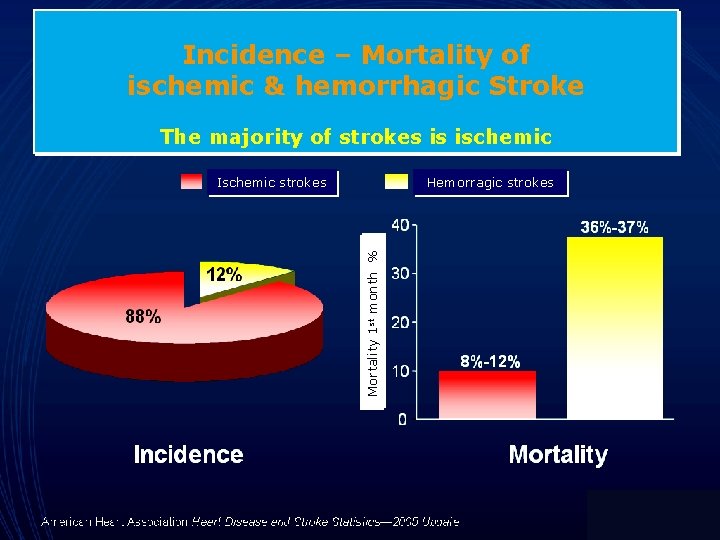
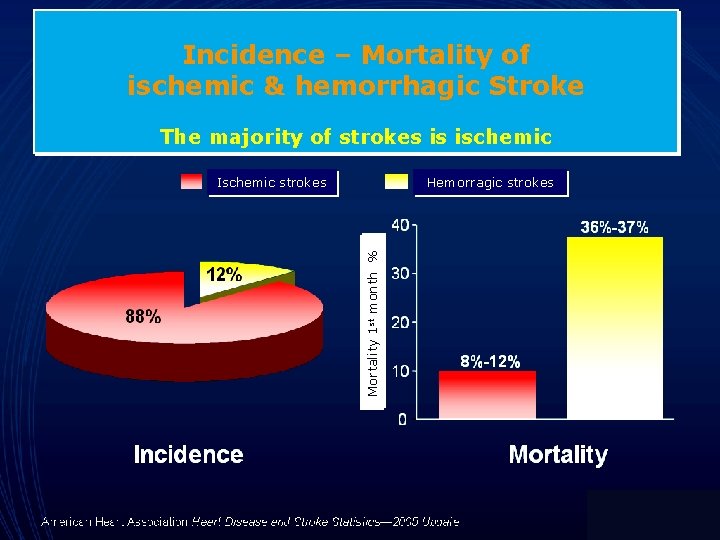
Incidence – Mortality of ischemic & hemorrhagic Stroke The majority of strokes is ischemic Ischemic strokes Mortality 1 st month % Hemorragic strokes

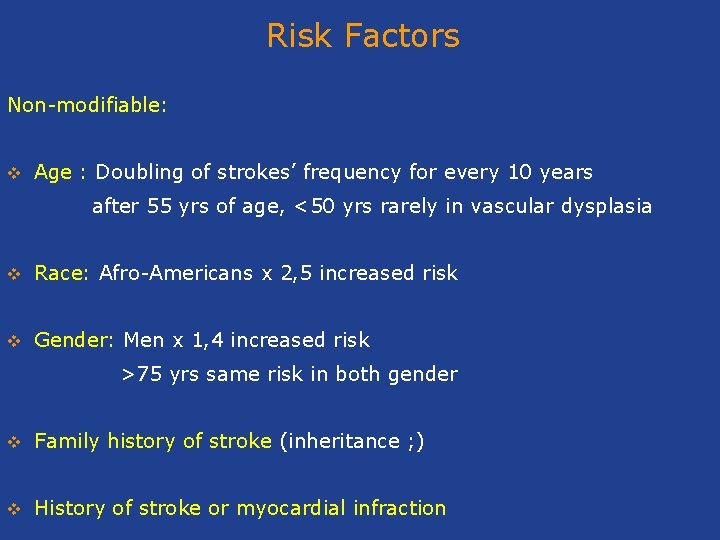
Risk Factors Non-modifiable: v Age : Doubling of strokes’ frequency for every 10 years after 55 yrs of age, <50 yrs rarely in vascular dysplasia v Race: Afro-Americans x 2, 5 increased risk v Gender: Men x 1, 4 increased risk >75 yrs same risk in both gender v Family history of stroke (inheritance ; ) v History of stroke or myocardial infraction
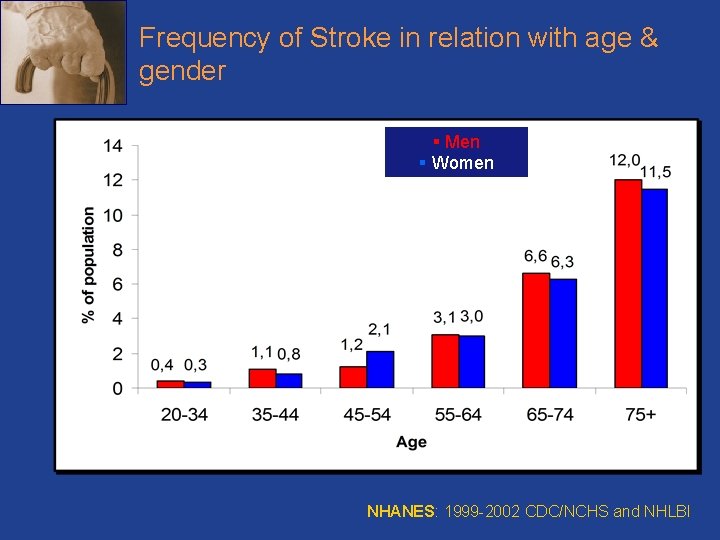
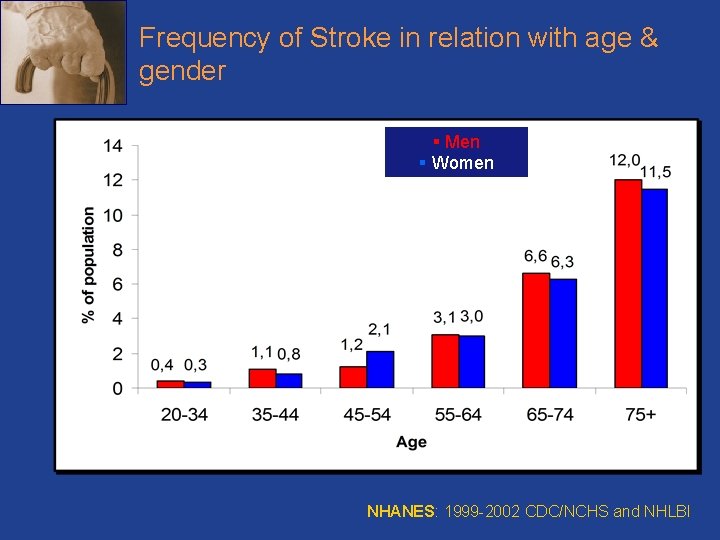
Frequency of Stroke in relation with age & gender § Men § Women NHANES: 1999 -2002 CDC/NCHS and NHLBI
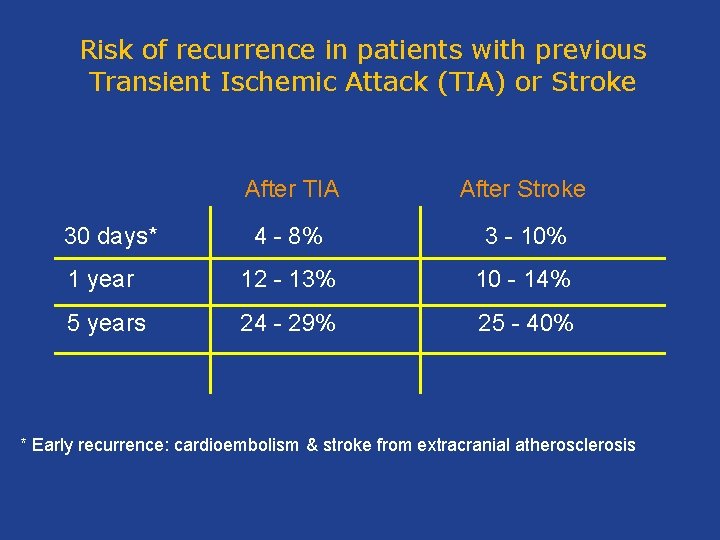
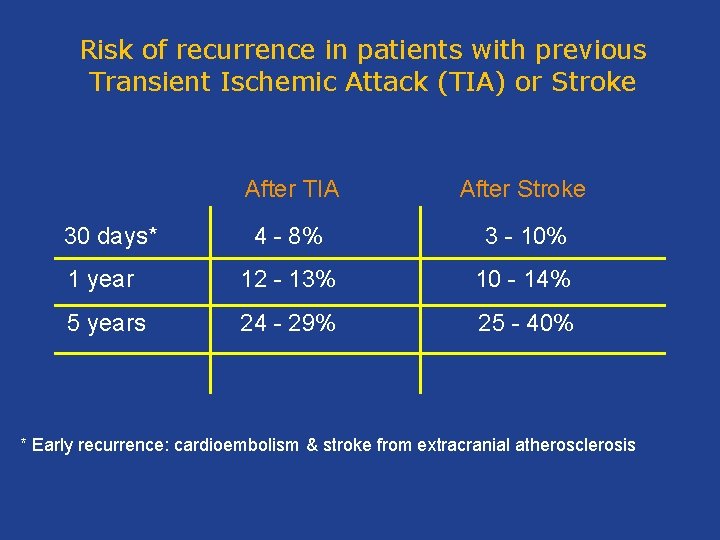
Risk of recurrence in patients with previous Transient Ischemic Attack (TIA) or Stroke After TIA After Stroke 4 - 8% 3 - 10% 1 year 12 - 13% 10 - 14% 5 years 24 - 29% 25 - 40% 30 days* * Early recurrence: cardioembolism & stroke from extracranial atherosclerosis
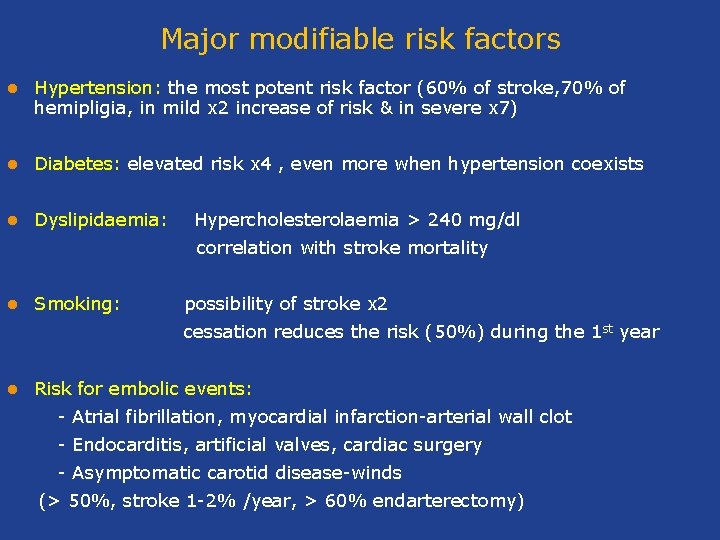
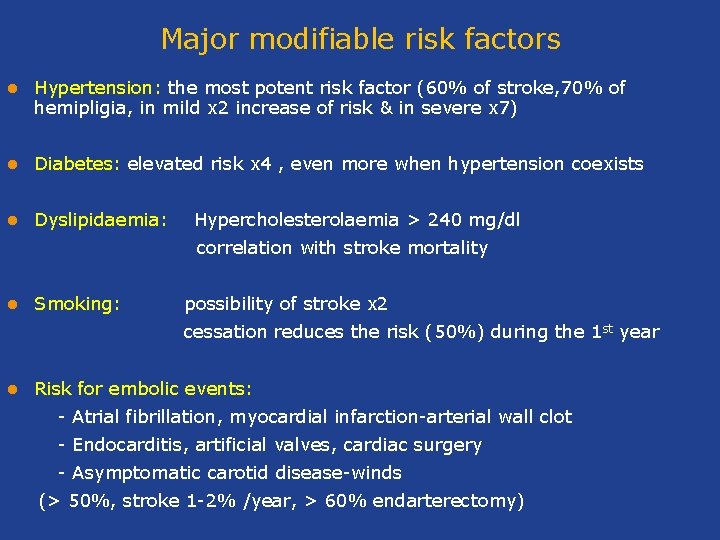
Major modifiable risk factors l Hypertension: the most potent risk factor (60% of stroke, 70% of hemipligia, in mild x 2 increase of risk & in severe x 7) l Diabetes: elevated risk x 4 , even more when hypertension coexists l Dyslipidaemia: Hypercholesterolaemia > 240 mg/dl correlation with stroke mortality l Smoking: possibility of stroke x 2 cessation reduces the risk (50%) during the 1 st year l Risk for embolic events: - Atrial fibrillation, myocardial infarction-arterial wall clot - Εndocarditis, artificial valves, cardiac surgery - Asymptomatic carotid disease-winds (> 50%, stroke 1 -2% /year, > 60% endarterectomy)
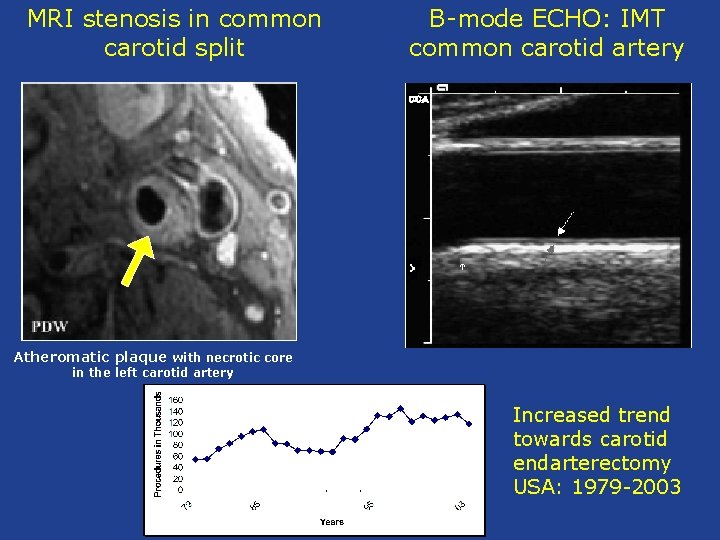
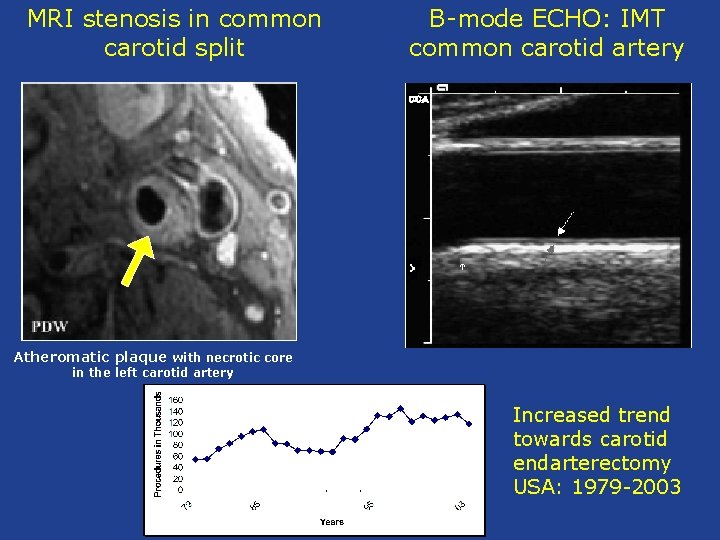
MRI stenosis in common carotid split B-mode ECHO: IMT common carotid artery Atheromatic plaque with necrotic core in the left carotid artery Increased trend towards carotid endarterectomy USA: 1979 -2003
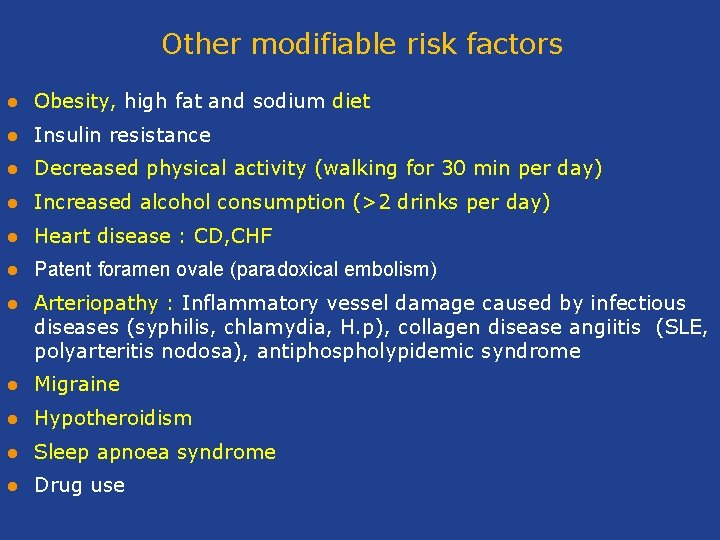
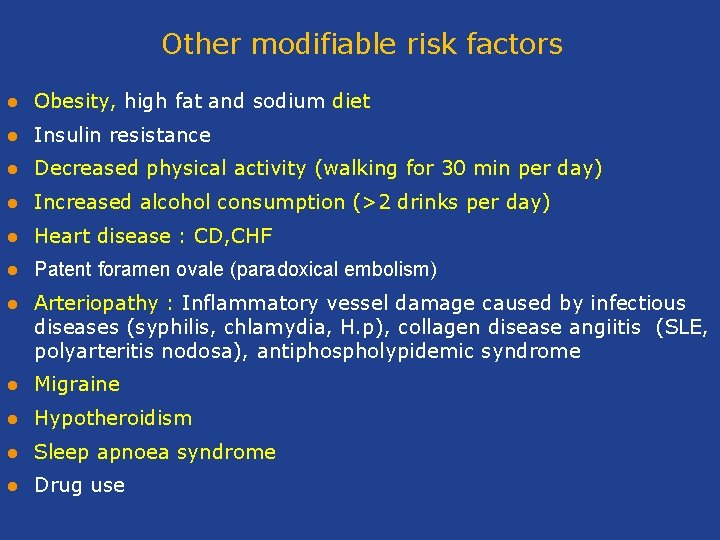
Other modifiable risk factors l Obesity, high fat and sodium diet l Insulin resistance l Decreased physical activity (walking for 30 min per day) l Increased alcohol consumption (>2 drinks per day) l Heart disease : CD, CHF l Patent foramen ovale (paradoxical embolism) l Arteriopathy : Inflammatory vessel damage caused by infectious diseases (syphilis, chlamydia, Η. p), collagen disease angiitis (SLE, polyarteritis nodosa), antiphospholypidemic syndrome l Migraine l Hypotheroidism l Sleep apnoea syndrome l Drug use
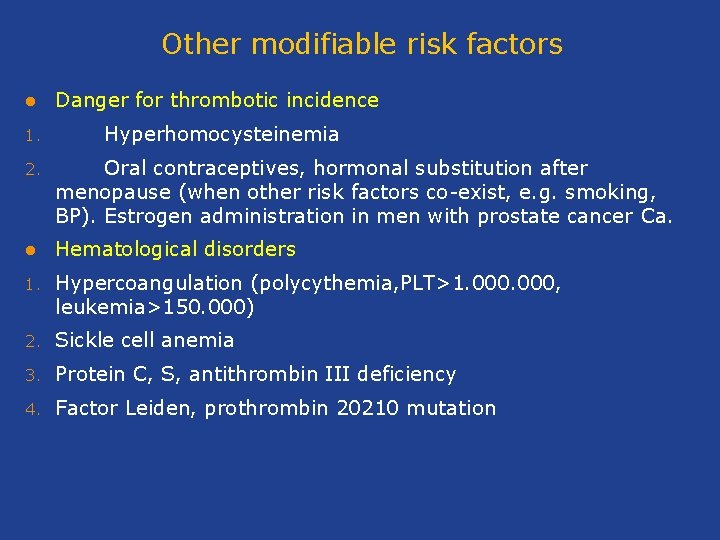
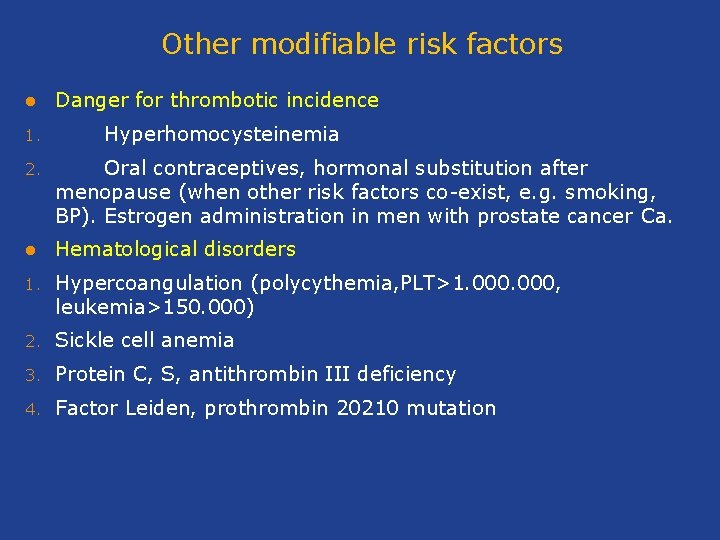
Other modifiable risk factors l 1. Danger for thrombotic incidence Hyperhomocysteinemia 2. Oral contraceptives, hormonal substitution after menopause (when other risk factors co-exist, e. g. smoking, BP). Estrogen administration in men with prostate cancer Ca. l Hematological disorders 1. Hypercoangulation (polycythemia, PLT>1. 000, leukemia>150. 000) 2. Sickle cell anemia 3. Protein C, S, antithrombin III deficiency 4. Factor Leiden, prothrombin 20210 mutation
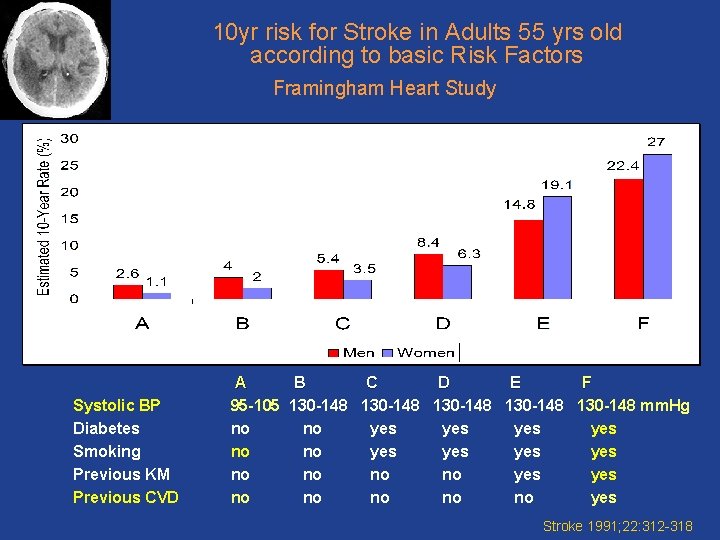
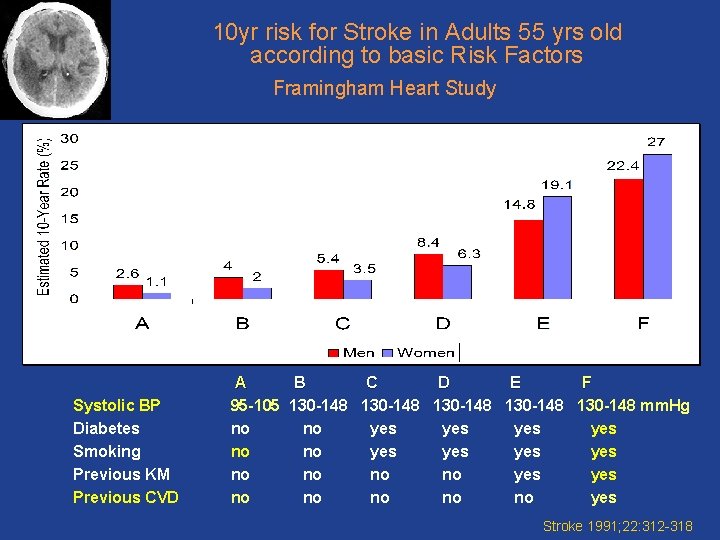
10 yr risk for Stroke in Adults 55 yrs old according to basic Risk Factors Framingham Heart Study Systolic BP Diabetes Smoking Previous ΚΜ Previous CVD A B C D E F 95 -105 130 -148 130 -148 mm. Hg no no yes yes no no yes no no no yes Stroke 1991; 22: 312 -318
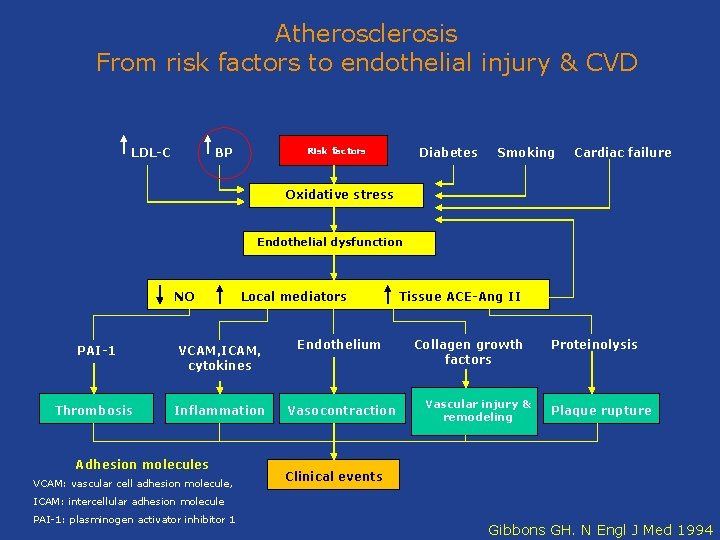
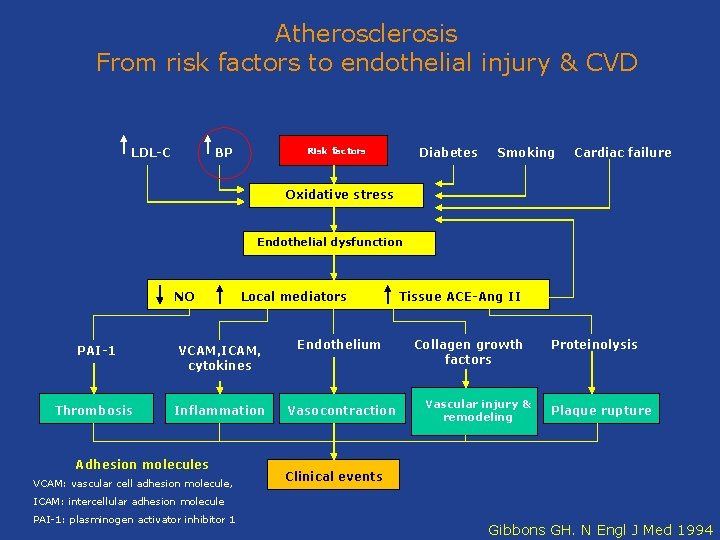
Atherosclerosis From risk factors to endothelial injury & CVD LDL-C BP Diabetes Risk factors Smoking Cardiac failure Oxidative stress Endothelial dysfunction NO Local mediators PAI-1 VCAM, ICAM, cytokines Endothelium Thrombosis Inflammation Vasocontraction Adhesion molecules VCAM: vascular cell adhesion molecule, Tissue ACE-Ang II Collagen growth factors Vascular injury & remodeling Proteinolysis Plaque rupture Clinical events ICAM: intercellular adhesion molecule PAI-1: plasminogen activator inhibitor 1 Gibbons GH. N Engl J Med 1994
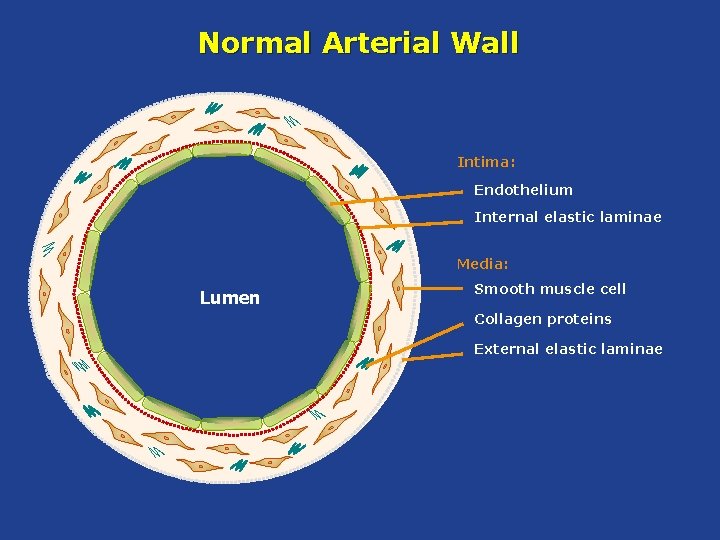
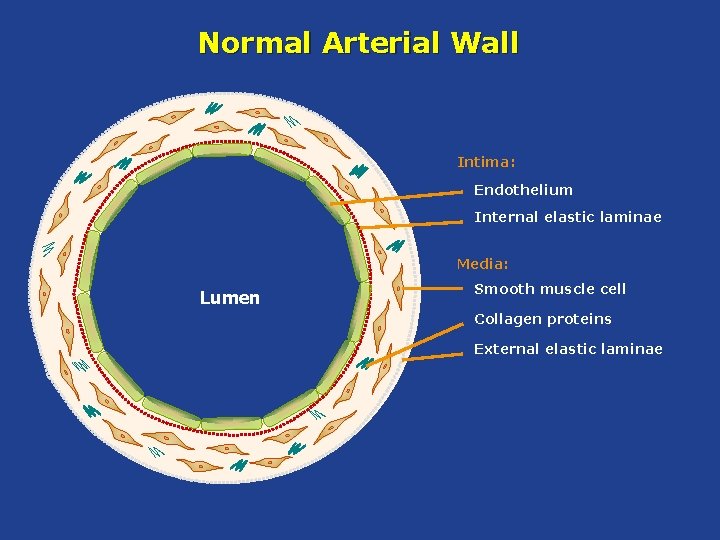
Normal Arterial Wall Intima: Endothelium Internal elastic laminae Media: Lumen Smooth muscle cell Collagen proteins External elastic laminae
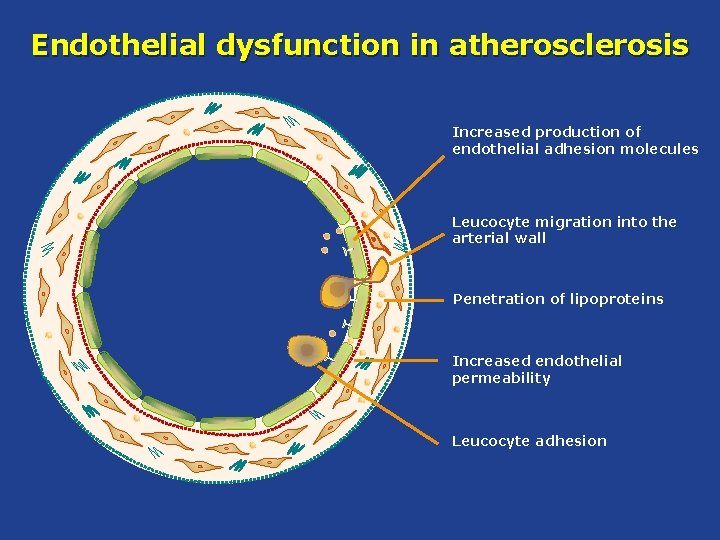
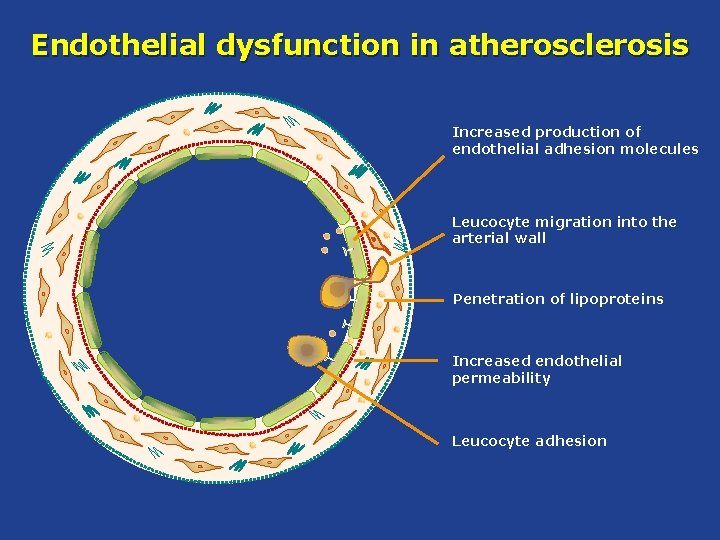
Endothelial dysfunction in atherosclerosis Increased production of endothelial adhesion molecules Leucocyte migration into the arterial wall Penetration of lipoproteins Increased endothelial permeability Leucocyte adhesion
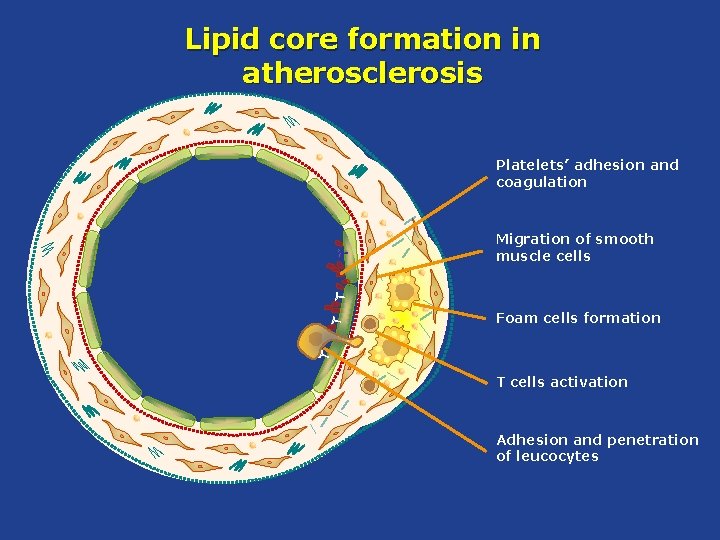
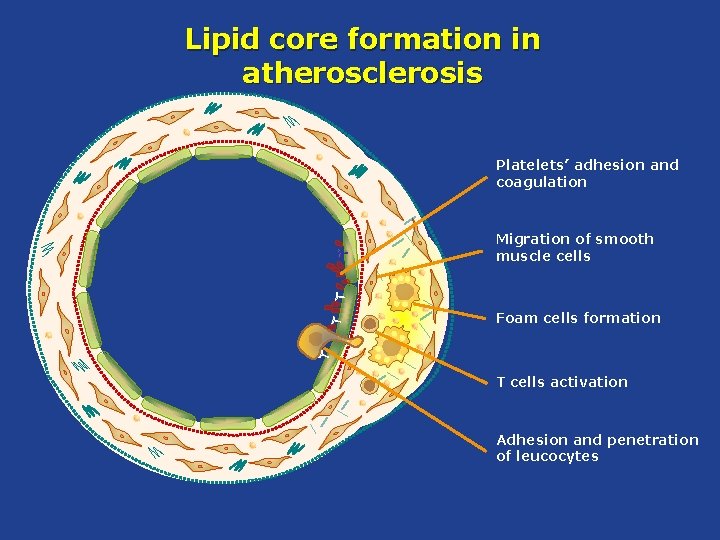
Lipid core formation in atherosclerosis Platelets’ adhesion and coagulation Migration of smooth muscle cells Foam cells formation T cells activation Adhesion and penetration of leucocytes
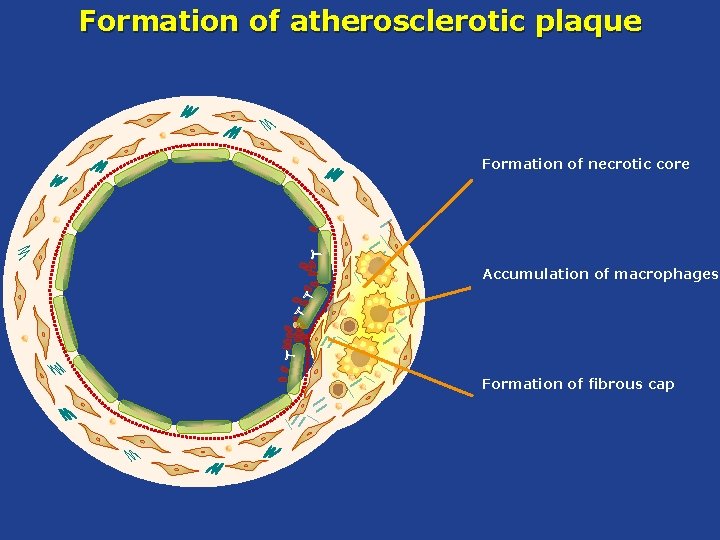
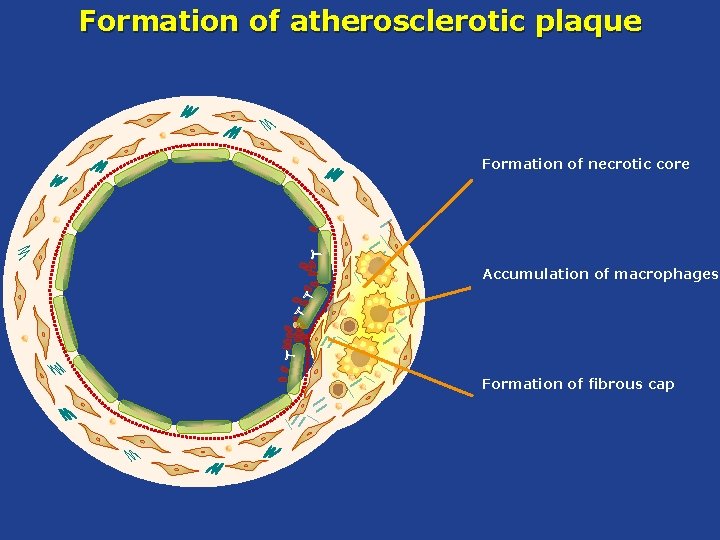
Formation of atherosclerotic plaque Formation of necrotic core Accumulation of macrophages Formation of fibrous cap
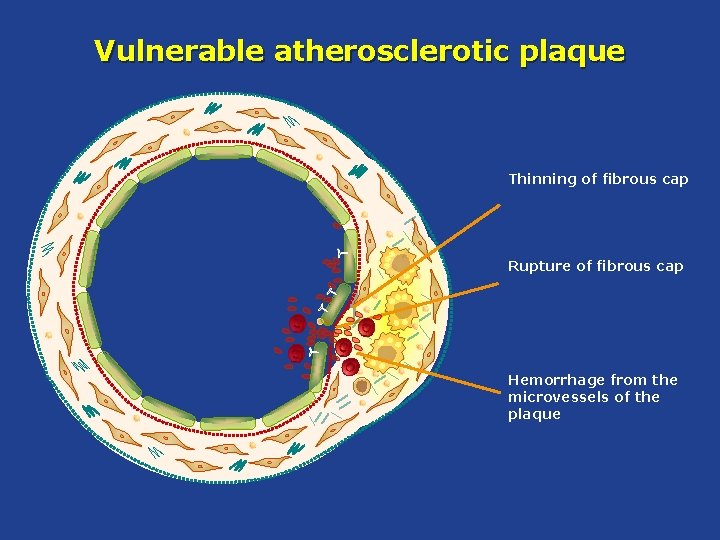
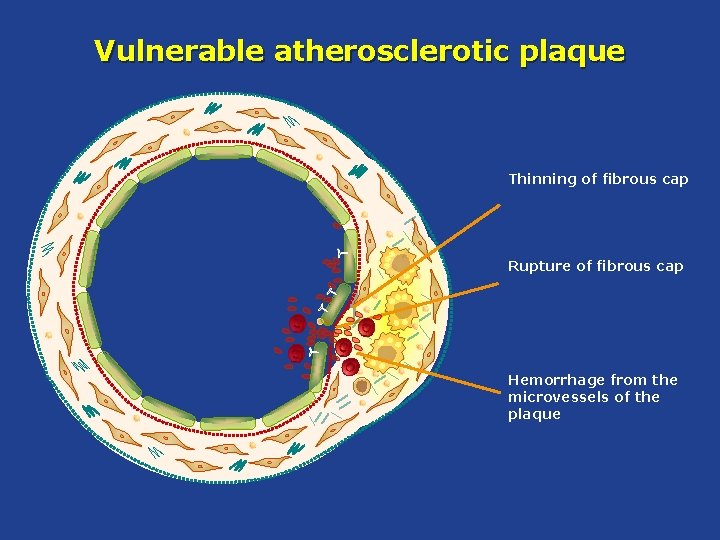
Vulnerable atherosclerotic plaque Thinning of fibrous cap Rupture of fibrous cap Hemorrhage from the microvessels of the plaque
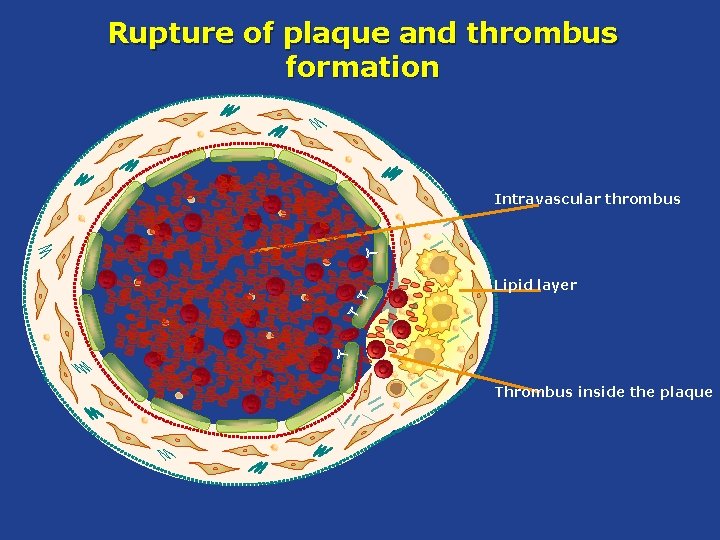
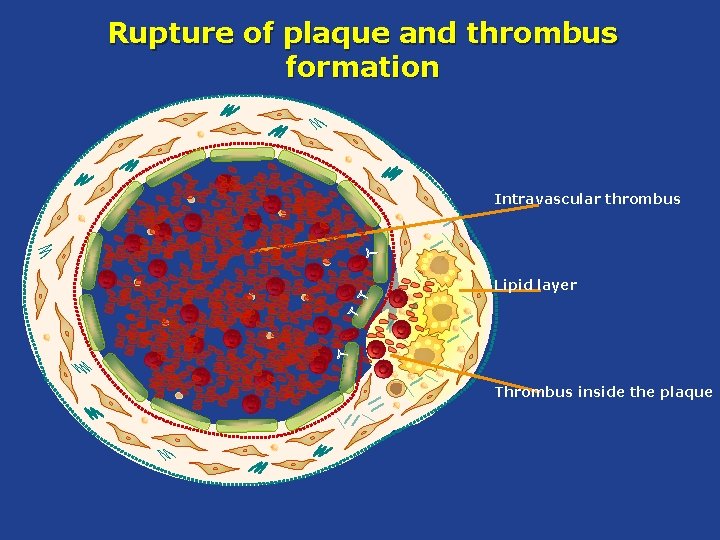
Rupture of plaque and thrombus formation Intravascular thrombus Lipid layer Thrombus inside the plaque
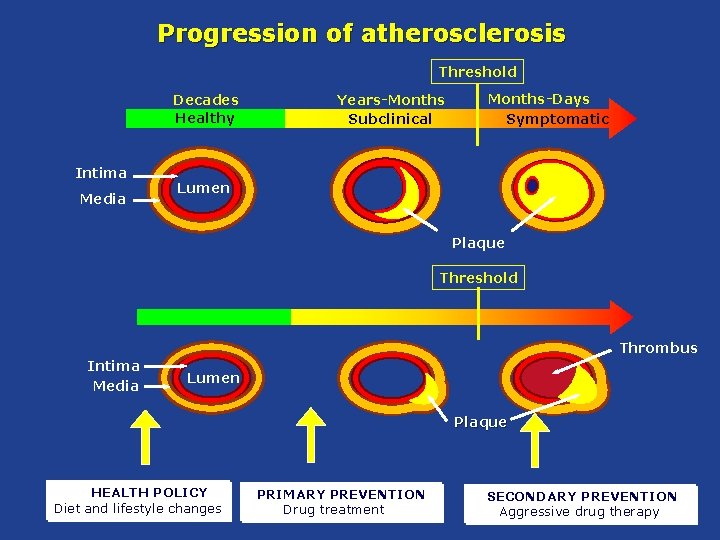
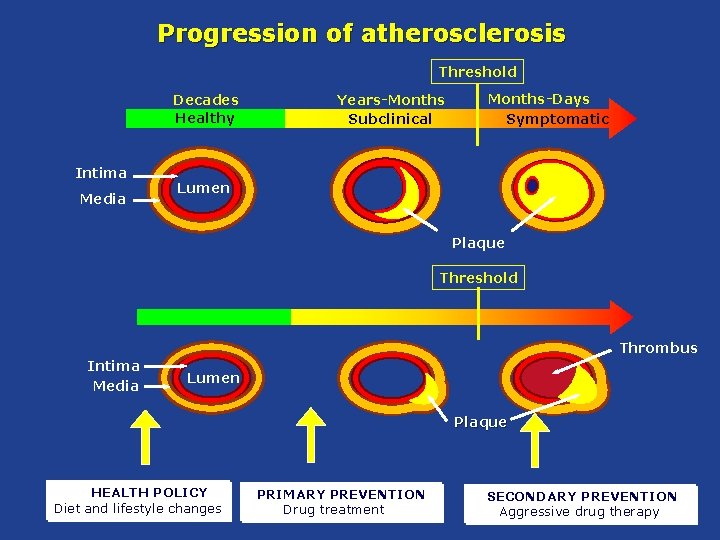
Progression of atherosclerosis Threshold Decades Healthy Intima Media Years-Months Subclinical Months-Days Symptomatic Lumen Plaque Threshold Thrombus Intima Media Lumen Plaque HEALTH POLICY Diet and lifestyle changes PRIMARY PREVENTION Drug treatment SECONDARY PREVENTION Aggressive drug therapy
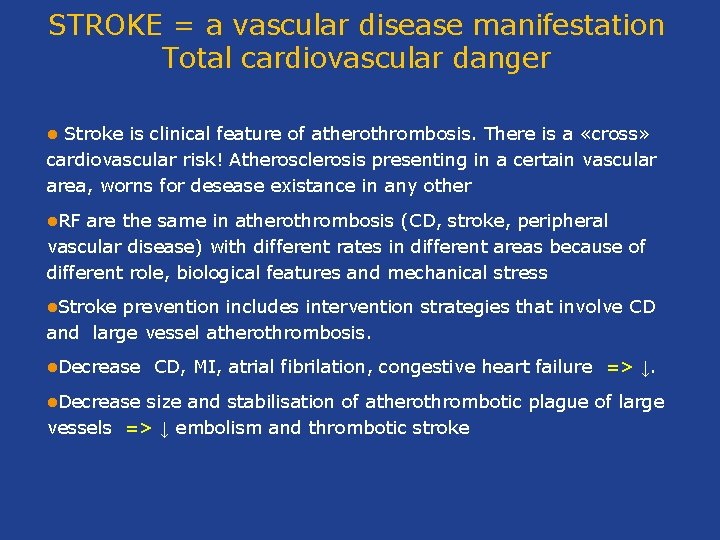
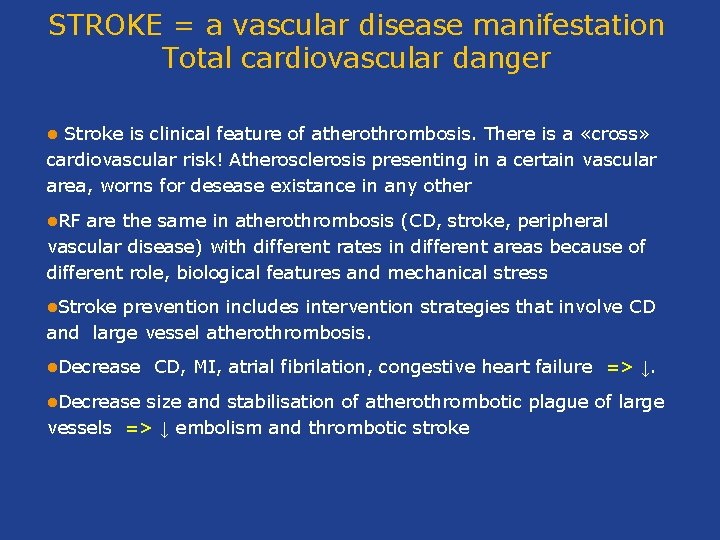
STROKE = a vascular disease manifestation Total cardiovascular danger Stroke is clinical feature of atherothrombosis. There is a «cross» cardiovascular risk! Atherosclerosis presenting in a certain vascular area, worns for desease existance in any other l l. RF are the same in atherothrombosis (CD, stroke, peripheral vascular disease) with different rates in different areas because of different role, biological features and mechanical stress l. Stroke prevention includes intervention strategies that involve CD and large vessel atherothrombosis. l. Decrease CD, MI, atrial fibrilation, congestive heart failure => ↓. size and stabilisation of atherothrombotic plague of large vessels => ↓ embolism and thrombotic stroke
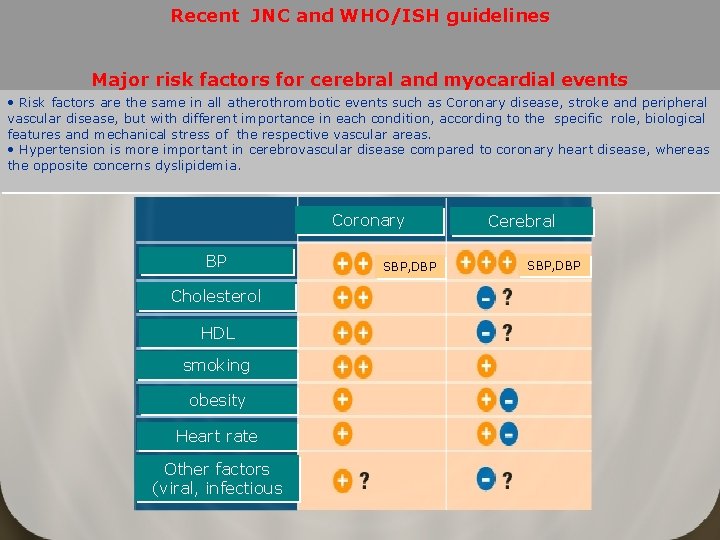
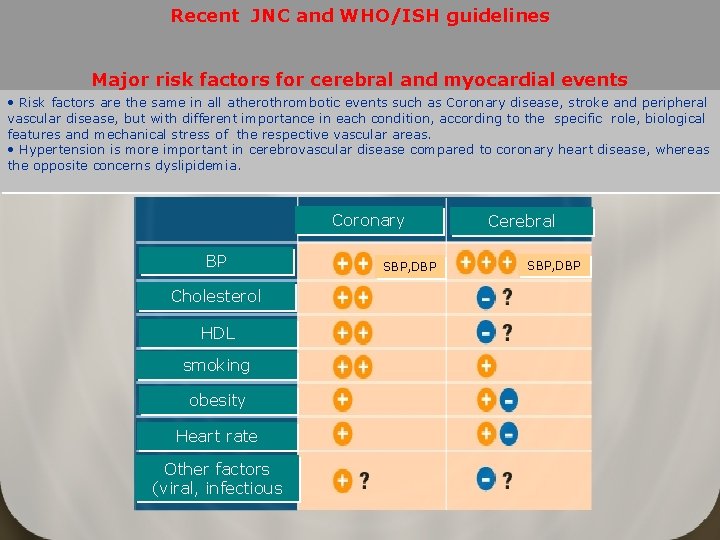
Recent JNC and WHO/ISH guidelines Major risk factors for cerebral and myocardial events • Risk factors are the same in all atherothrombotic events such as Coronary disease, stroke and peripheral vascular disease, but with different importance in each condition, according to the specific role, biological features and mechanical stress of the respective vascular areas. • Hypertension is more important in cerebrovascular disease compared to coronary heart disease, whereas the opposite concerns dyslipidemia. Coronary BP Cholesterol HDL smoking obesity Heart rate Other factors (viral, infectious SBP, DBP Cerebral SBP, DBP
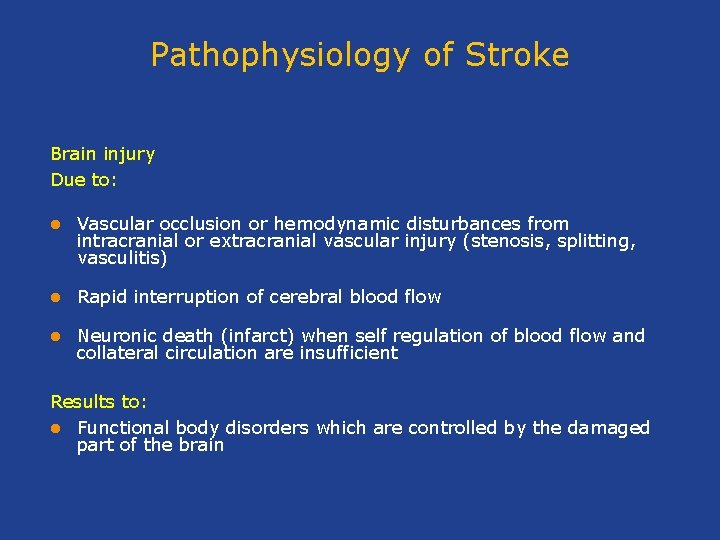
Pathophysiology of Stroke Brain injury Due to: l Vascular occlusion or hemodynamic disturbances from intracranial or extracranial vascular injury (stenosis, splitting, vasculitis) l Rapid interruption of cerebral blood flow l Neuronic death (infarct) when self regulation of blood flow and collateral circulation are insufficient Results to: l Functional body disorders which are controlled by the damaged part of the brain
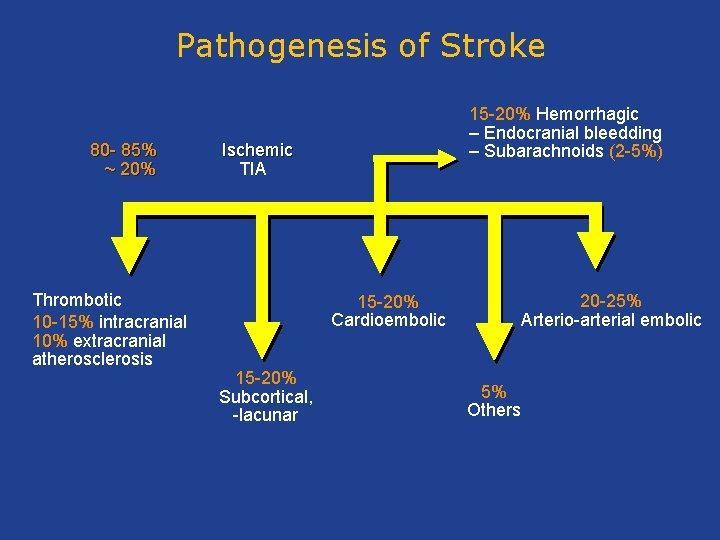
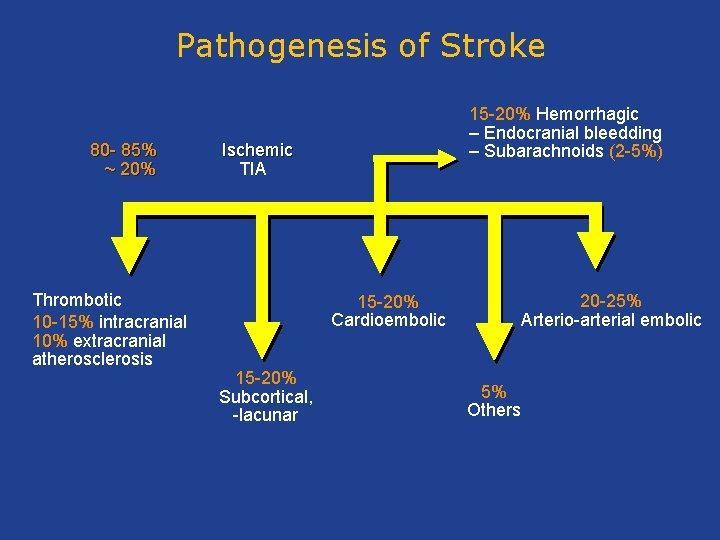
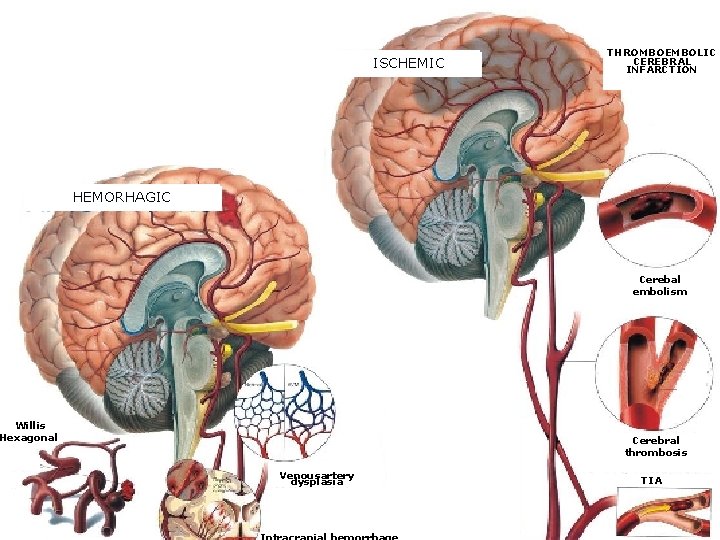
Pathogenesis of Stroke 80 - 85% ~ 20% Thrombotic 10 -15% intracranial 10% extracranial atherosclerosis 15 -20% Hemorrhagic – Endocranial bleedding – Subarachnoids (2 -5%) Ischemic TIA 15 -20% Cardioembolic 15 -20% Subcortical, -lacunar 20 -25% Arterio-arterial embolic 5% Others
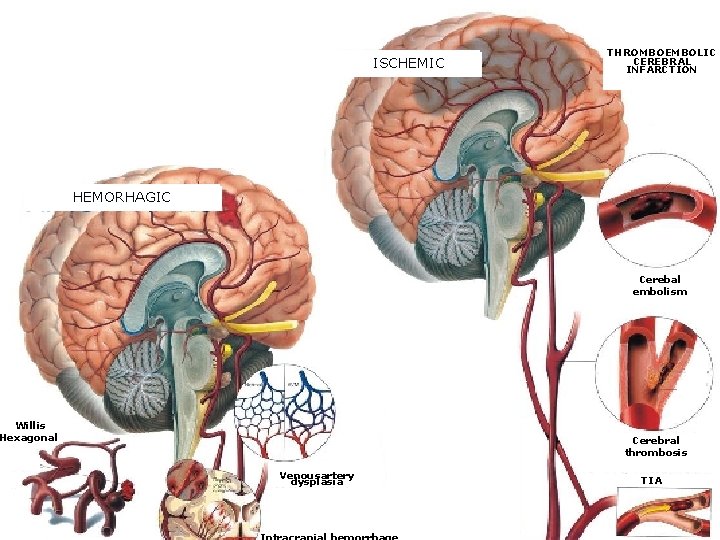
ISCHEMIC THROMBOEMBOLIC CEREBRAL INFARCTION HEMORHAGIC Cerebal embolism Willis Hexagonal Cerebral thrombosis Venousartery dysplasia TIA
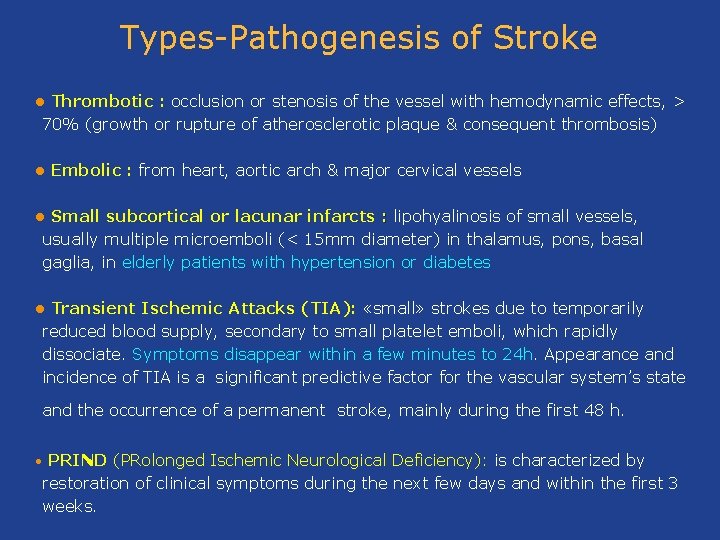
Types-Pathogenesis of Stroke Thrombotic : occlusion or stenosis of the vessel with hemodynamic effects, > 70% (growth or rupture of atherosclerotic plaque & consequent thrombosis) l l Embolic : from heart, aortic arch & major cervical vessels Small subcortical or lacunar infarcts : lipohyalinosis of small vessels, usually multiple microemboli (< 15 mm diameter) in thalamus, pons, basal gaglia, in elderly patients with hypertension or diabetes l Transient Ischemic Attacks (ΤΙΑ): «small» strokes due to temporarily reduced blood supply, secondary to small platelet emboli, which rapidly dissociate. Symptoms disappear within a few minutes to 24 h. Appearance and incidence of TIA is a significant predictive factor for the vascular system’s state l and the occurrence of a permanent stroke, mainly during the first 48 h. PRIND (PRolonged Ischemic Neurological Deficiency): is characterized by restoration of clinical symptoms during the next few days and within the first 3 weeks. •
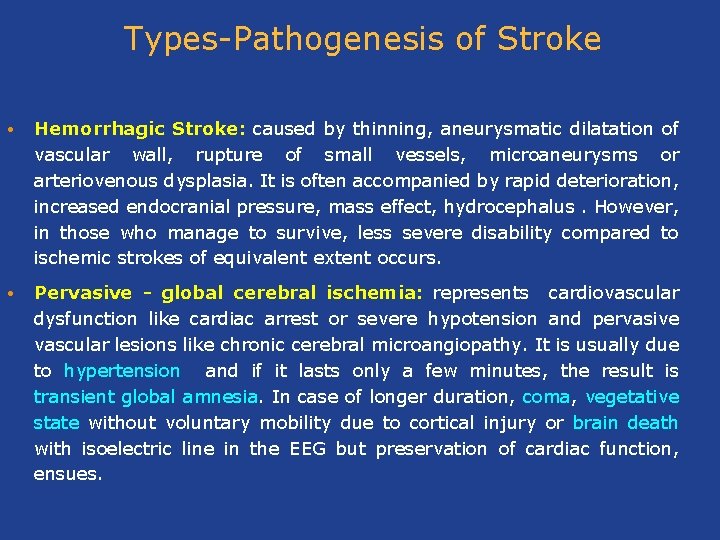
Types-Pathogenesis of Stroke • Hemorrhagic Stroke: caused by thinning, aneurysmatic dilatation of vascular wall, rupture of small vessels, microaneurysms or arteriovenous dysplasia. It is often accompanied by rapid deterioration, increased endocranial pressure, mass effect, hydrocephalus. However, in those who manage to survive, less severe disability compared to ischemic strokes of equivalent extent occurs. • Pervasive - global cerebral ischemia: represents cardiovascular dysfunction like cardiac arrest or severe hypotension and pervasive vascular lesions like chronic cerebral microangiopathy. It is usually due to hypertension and if it lasts only a few minutes, the result is transient global amnesia. In case of longer duration, coma, vegetative state without voluntary mobility due to cortical injury or brain death with isoelectric line in the EEG but preservation of cardiac function, ensues.
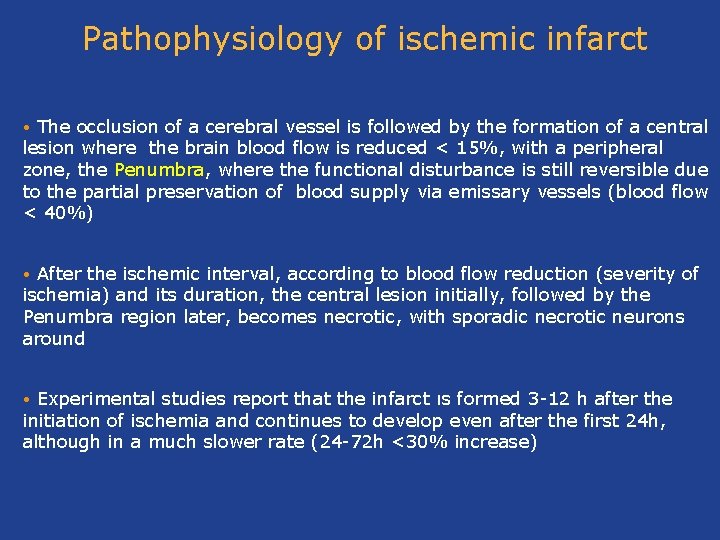
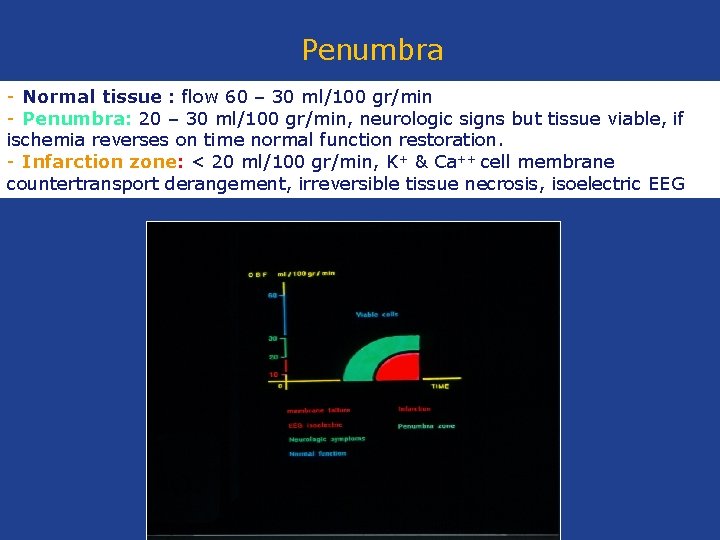
Pathophysiology of ischemic infarct The occlusion of a cerebral vessel is followed by the formation of a central lesion where the brain blood flow is reduced < 15%, with a peripheral zone, the Penumbra, where the functional disturbance is still reversible due to the partial preservation of blood supply via emissary vessels (blood flow < 40%) • After the ischemic interval, according to blood flow reduction (severity of ischemia) and its duration, the central lesion initially, followed by the Penumbra region later, becomes necrotic, with sporadic necrotic neurons around • Experimental studies report that the infarct ιs formed 3 -12 h after the initiation of ischemia and continues to develop even after the first 24 h, although in a much slower rate (24 -72 h <30% increase) •
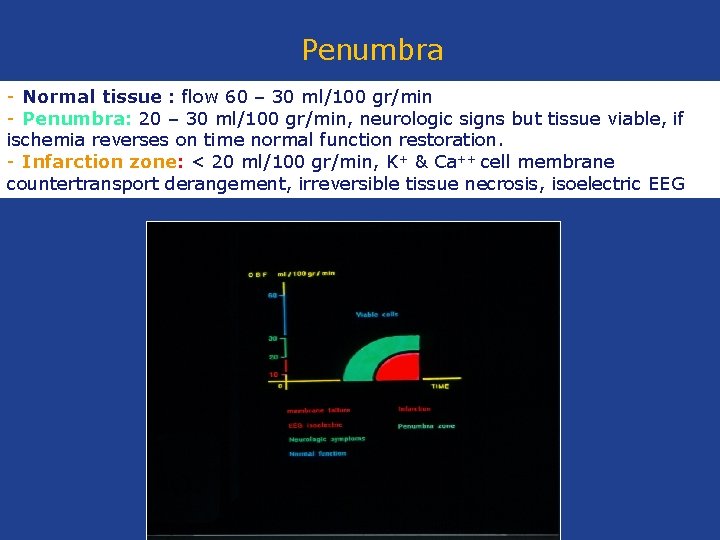
Penumbra - Normal tissue : flow 60 – 30 ml/100 gr/min - Penumbra: 20 – 30 ml/100 gr/min, neurologic signs but tissue viable, if ischemia reverses on time normal function restoration. - Infarction zone: < 20 ml/100 gr/min, K+ & Ca++ cell membrane countertransport derangement, irreversible tissue necrosis, isoelectric EEG
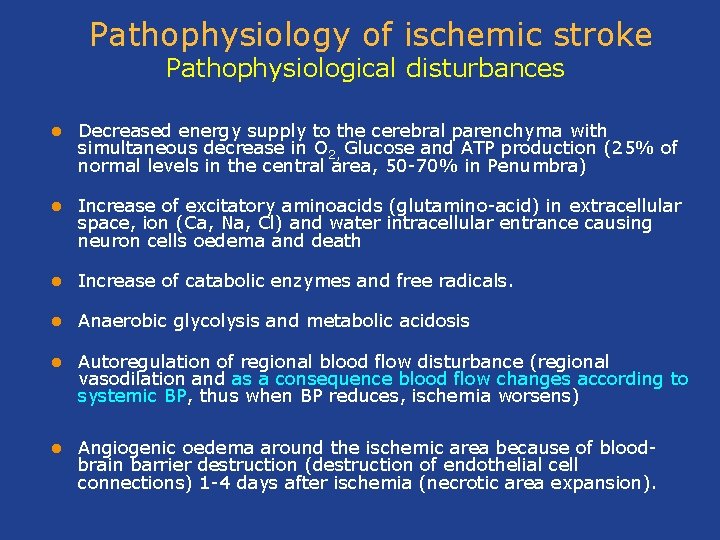
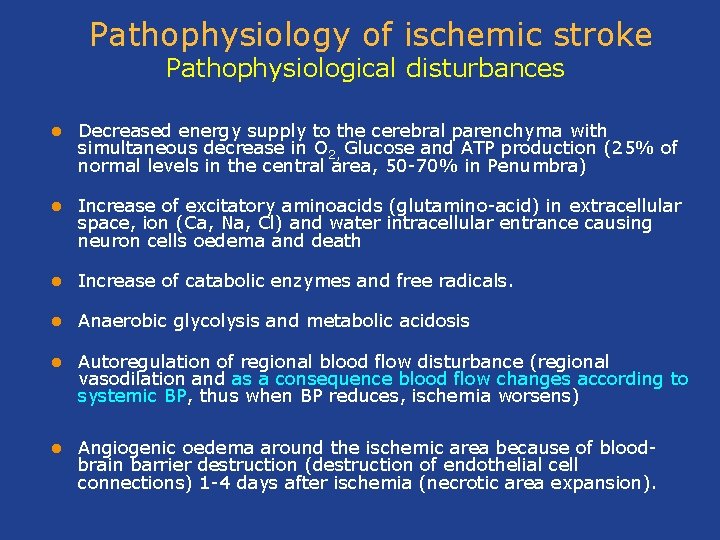
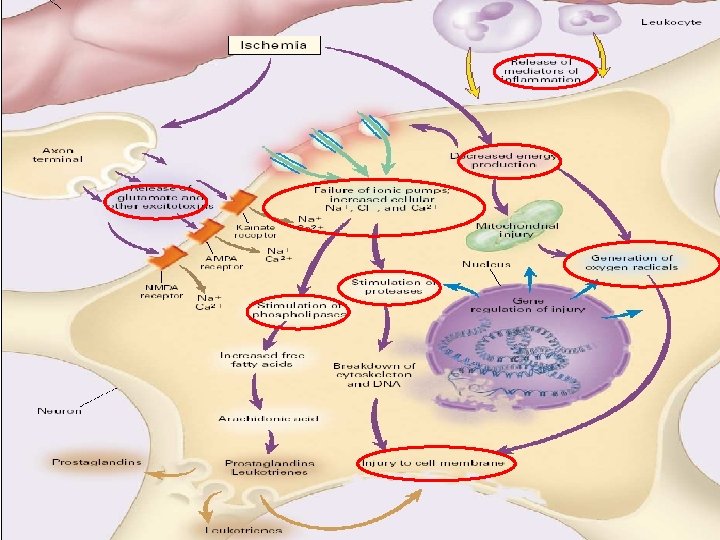
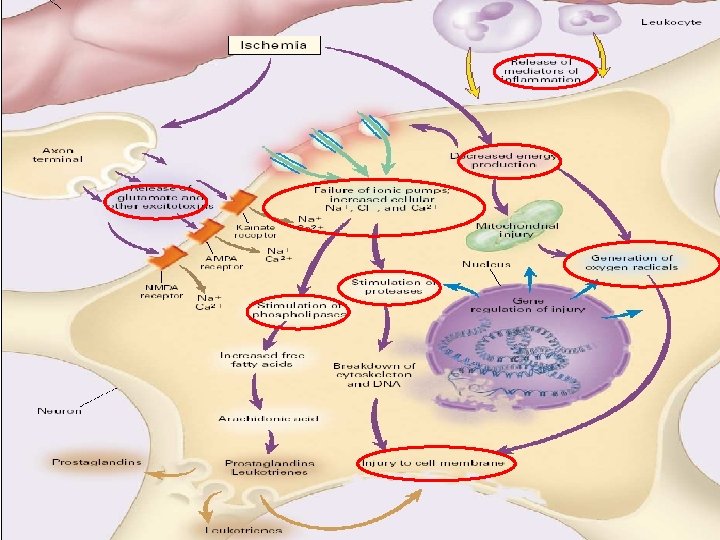
Pathophysiology of ischemic stroke Pathophysiological disturbances l Decreased energy supply to the cerebral parenchyma with simultaneous decrease in Ο 2, Glucose and ATP production (25% of normal levels in the central area, 50 -70% in Penumbra) l Increase of excitatory aminoacids (glutamino-acid) in extracellular space, ion (Ca, Na, Cl) and water intracellular entrance causing neuron cells oedema and death l Increase of catabolic enzymes and free radicals. l Anaerobic glycolysis and metabolic acidosis l Autoregulation of regional blood flow disturbance (regional vasodilation and as a consequence blood flow changes according to systemic BP, thus when BP reduces, ischemia worsens) l Angiogenic oedema around the ischemic area because of bloodbrain barrier destruction (destruction of endothelial cell connections) 1 -4 days after ischemia (necrotic area expansion).
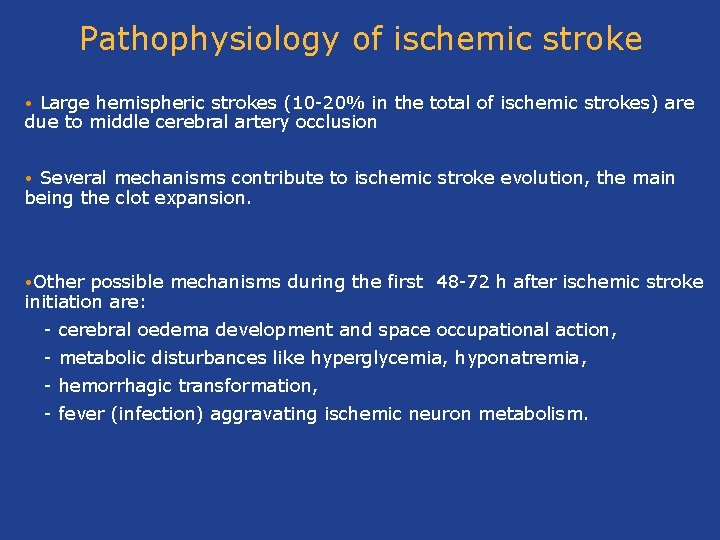
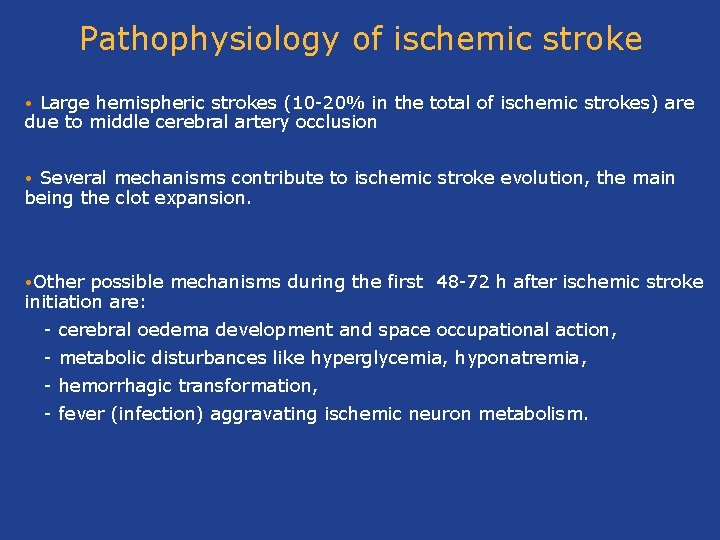
Pathophysiology of ischemic stroke Large hemispheric strokes (10 -20% in the total of ischemic strokes) are due to middle cerebral artery occlusion • Several mechanisms contribute to ischemic stroke evolution, the main being the clot expansion. • • Other possible mechanisms during the first 48 -72 h after ischemic stroke initiation are: - cerebral oedema development and space occupational action, - metabolic disturbances like hyperglycemia, hyponatremia, - hemorrhagic transformation, - fever (infection) aggravating ischemic neuron metabolism.
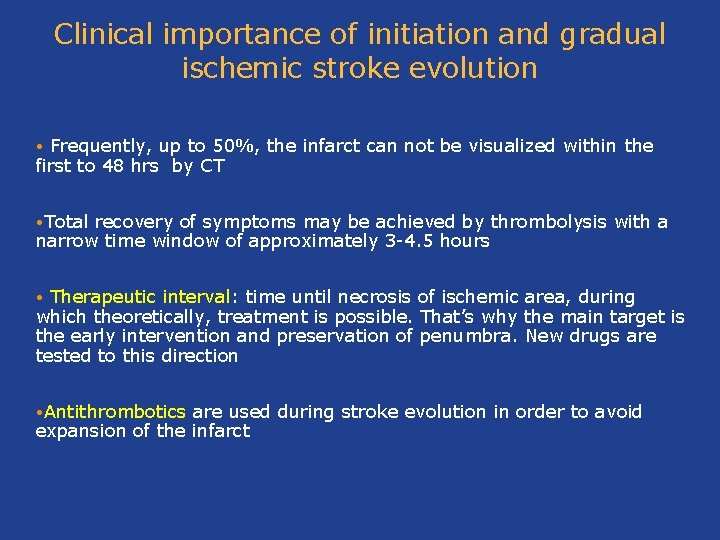
Clinical importance of initiation and gradual ischemic stroke evolution Frequently, up to 50%, the infarct can not be visualized within the first to 48 hrs by CT • • Total recovery of symptoms may be achieved by thrombolysis with a narrow time window of approximately 3 -4. 5 hours Therapeutic interval: time until necrosis of ischemic area, during which theoretically, treatment is possible. That’s why the main target is the early intervention and preservation of penumbra. New drugs are tested to this direction • • Antithrombotics are used during stroke evolution in order to avoid expansion of the infarct
Interesti ng issue The importance of treatment of metabolichemodynamic factors to the evolution of stroke Hyperglycemia but also hypoglycemia should be treated because they might worsen the ischemic damage (anaerobic glycolysis, lactic acidosis, intracellular oedema), neuron metabolism and restoration l Atherosclerosis progression as well as oxidative stress induction should be inhibited by use of agents exerting endothelium protection, inflammation decrease, stabilization of atherosclerotic plaque and possibly neuroprotection from ischemia (drugs acting on RAAS, statins, vitamin E) l
Hypertension treatment according to stroke development In hypertension, cerebral vessels adjust to elevated BP by wall thickening, increased resistance and shift of blood flow autoregulation at higher BP level. The problem is greater in older patients because of increased vascular resistance and decreased cerebral blood flow. Great and abrupt BP decrease results in blood flow disturbance, cerebral ischemia and cognitive function deterioration.
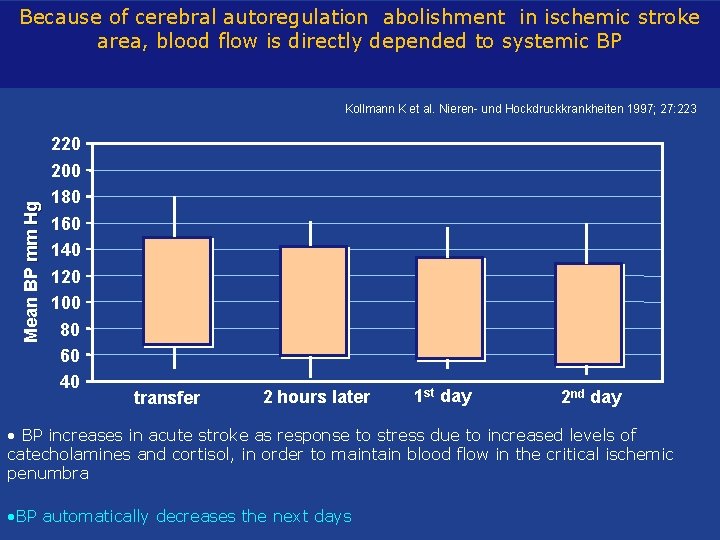
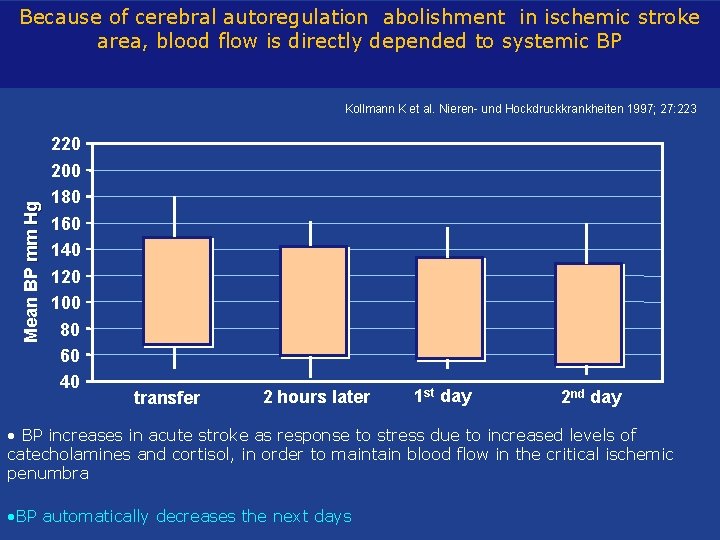
Because of cerebral autoregulation abolishment in ischemic stroke area, blood flow is directly depended to systemic BP Mean BP mm Hg Kollmann K et al. Nieren- und Hockdruckkrankheiten 1997; 27: 223 220 200 180 160 140 120 100 80 60 40 transfer 2 hours later 1 st day 2 nd day • BP increases in acute stroke as response to stress due to increased levels of catecholamines and cortisol, in order to maintain blood flow in the critical ischemic penumbra • BP automatically decreases the next days
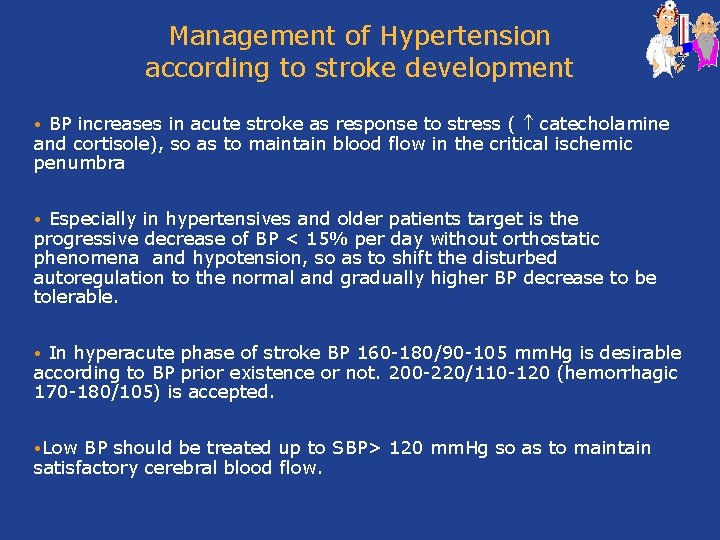
Management of Hypertension according to stroke development BP increases in acute stroke as response to stress ( catecholamine and cortisole), so as to maintain blood flow in the critical ischemic penumbra • Especially in hypertensives and older patients target is the progressive decrease of BP < 15% per day without orthostatic phenomena and hypotension, so as to shift the disturbed autoregulation to the normal and gradually higher BP decrease to be tolerable. • In hyperacute phase of stroke BP 160 -180/90 -105 mm. Hg is desirable according to BP prior existence or not. 200 -220/110 -120 (hemorrhagic 170 -180/105) is accepted. • • Low BP should be treated up to SBP> 120 mm. Hg so as to maintain satisfactory cerebral blood flow.
Thank you for your attention!
 Belarusian medical academy of postgraduate education
Belarusian medical academy of postgraduate education Kramer's postgraduate resocialization model stages
Kramer's postgraduate resocialization model stages Undergraduate graduate postgraduate
Undergraduate graduate postgraduate Postgraduate training authorization letter
Postgraduate training authorization letter Difference between postgraduate and undergraduate
Difference between postgraduate and undergraduate Difference between postgraduate and undergraduate
Difference between postgraduate and undergraduate Susi grant rates
Susi grant rates Clinical governance postgraduate
Clinical governance postgraduate What is postgraduate
What is postgraduate Alexmed postgraduate
Alexmed postgraduate Varna spa
Varna spa Varnas definition
Varnas definition Dolphinarium varna
Dolphinarium varna Varna system
Varna system Emona durmati
Emona durmati Gupta empire social classes
Gupta empire social classes Caste indian
Caste indian Casta systme
Casta systme Varna rna
Varna rna Medical education reform programme
Medical education reform programme Www.hrdc.amu.ac.in
Www.hrdc.amu.ac.in Internal control introduction
Internal control introduction Vouching in auditing
Vouching in auditing Internal quality control laboratory
Internal quality control laboratory Doctors license number
Doctors license number Gbmc infoweb
Gbmc infoweb Hepburn osteometric board
Hepburn osteometric board Torrance memorial outpatient lab
Torrance memorial outpatient lab Cartersville medical center medical records
Cartersville medical center medical records Unm im residency
Unm im residency University medical centre maribor
University medical centre maribor Liaoning medical university
Liaoning medical university Vietnam military medical university
Vietnam military medical university M.gorky donetsk national medical university
M.gorky donetsk national medical university Masaryk university medical faculty
Masaryk university medical faculty Ibn sina university of medical and pharmaceutical sciences
Ibn sina university of medical and pharmaceutical sciences Seoul national university college of medicine
Seoul national university college of medicine Kirovohrad medical university
Kirovohrad medical university University of maryland capital region health medical group
University of maryland capital region health medical group Stavropol state medical university
Stavropol state medical university Empp university medical center
Empp university medical center David tvildiani medical university
David tvildiani medical university Slowenien university medical center
Slowenien university medical center Columbia university medical center
Columbia university medical center Columbia university medical center
Columbia university medical center