HEART FAILURE pump failure DEFINITION Heart failure is














- Slides: 40
HEART FAILURE “pump failure”
DEFINITION Heart failure is the inability of the heart to supply adequate blood flow and therefore oxygen delivery to the peripheral tissues and organs
v. Cardiac output is about 5 l /min at rest v. Increases to upto 25 l/ min v. Heart failure occurs when the heart is unable to meet the demand
EPIDEMIOLOGY § Only cardiovascular disease with increasing incidence and prevalance due to § Aging population § Increased survival after MI--thrombolysis § Improvement of medical and surgical treatment

v Important cause of morbidity and mortality § 1 yr mortality – 10 – 20 % § NYHA class 1 V -- > 50 % § 4 yr mortality – 50 % v Debilitating disease § Significant decrease in quality of life • Due to symptoms • Decrease functional capabilities • Frequent hospitalizations

CLASSIFICATION OF HEART FAILURE This is based on: § How rapid symptoms develop---acute HF ---chronic HF § Which ventricle is involved---right side HF ---left side HF § Over all cardiac output---systolic HF ---diastolic HF
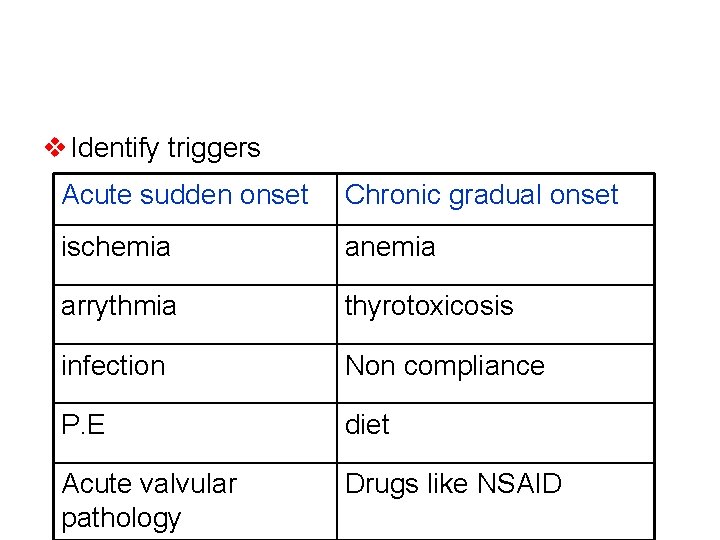
CLASSIFICATION ACCORDING TO ONSET OF SYMPTOMS: Acute heart failure --characterized by a rapid onset of heart failure that may occur following 1 - MI 2 -myocarditis 3 -arrythmias 4 - infection 5 - PE If it is not fatal may progress to chronic heart failure
Chronic heart failure This results from the heart undergoing adaptive responses to precipitating cause and this cardiac response leads to impaired function. 1 - anemia 2 -thyrotoxicosis 3 -non compliance to medications 4 - diet—high salt
ETIOLOGY § Myocardial infarction § Coronary artery disease § Valvular heart disease § Idiopathic cardiomyopathy § Viral or bacterial cardiomyopathy § myocarditis
ETIOLOGY cont. § Pericarditis § Arryhthmias § Hypertension § Thyroid disease § Pregnancy § Septic shock
ETIOLOGY cont. § Toxins—anthracyclines amphetamine cocaine § Metabolic---haemachromatosis wilson, s disease pheochromocytoma

SYMPTOMS cont. { FACES} § Fatigue § Activity decrease § Cough { specially supine, frothy red sputum § Edema § Shortness of breath { NYHA }
SYMPTOMS NYHA classification of dyspnoe § Class 1—no shortness of breath {SOB} § Class 11—SOB on severe exertion § Class 111—SOB on mild exertion § Class 1 v---SOB at rest

Heart failure management issues § High mortality § High readmission rates § Poor Rx adherance § On going symptoms § Reduced quality of life § Dose adjustment in the elderly
Heart failure therapeutic goals § 1 ry goal = reduce symptoms § Improve quality of life § Reduce hospitalization § Prevent sudden death

DIET approach to the pt. with heart failure Ø D—diagnose---eteiology ---severity of LV dysfunction Ø I –initiate---diuretics { thiazide , frusemide } ---beta blockers ---ACEI ---digoxin ---spironolactone

Ø E—educate----diet ---exercise ---life style Ø T---titrate---optimize ACEI ---optimize beta blockers
General measures v. Correct precipitating causes § Treat ischemia § Control hypertension § D/C smoking § Treat lipid abnormality § Treat and control hypertension
v. Low salt diet v. Fluid restriction v. Regular exercise v. Upright position to reduce pulmonary congestion v. Prophylactic anticoaggulation v. Avoid –ve inatropic drugs
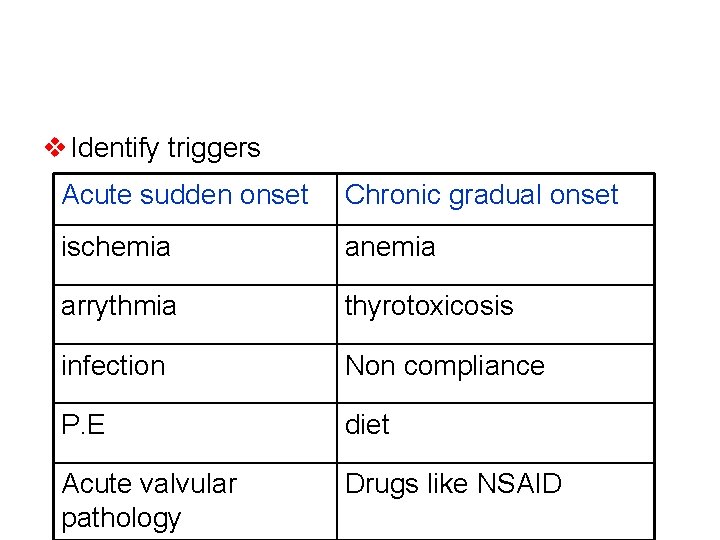
v Identify triggers Acute sudden onset Chronic gradual onset ischemia anemia arrythmia thyrotoxicosis infection Non compliance P. E diet Acute valvular pathology Drugs like NSAID

INVESTIGATION § CBC § U+E § LFT § Cardiac enzymes § CXR § ECG § Echocardiogram

TREATMENT § Diuretics § Digoxin § ACE inhibitors § Vasodilators § Beta blockers

DRUGS v. Diuretics ---thiazide diuretic ---frusemide {loop diuretic} ----spironolactone { K sparing} § Titrate to euvolumic state § Maintain ideal body wt ={ dry wt= normal JVP / trace or no pedal edema}
v. ACEI § Cornerstone in the Rx of heart failure § Continue indefinitely if EF < 40 % § Rx for all asymptomatic pts with EF < 35% § Rx for all symptomatic pts with EF =35% § Use max. tolerated dose
ACEI cont. . § Captopril---capoten § Enalapril----renetic § Lisinopril----zestril § Fosinopril---staril
Angiotensin receptor blockers § Same action and benefits as ACEI § Used in pts who cannot tolerate ACEI due to side effects § Candesartan § Irbesartan § Losartan § Valsartan § Telemisartan

Beta blockers § Titrate to max. tolerated dose § Continue indefinitely § Bisoprolol § Carvidelol § metaprolol
patient selection for successful beta blocker initiation § Stable symptoms § Stable background heart failure medication § No hypotension § No bradycardia § Euvolumic status § Start low and titrate slowly
Patients with heart failure who should NOT be started on beta blockers § Bronchospastic pulmonary disease § Severe bradycardia § High degree A / V block § Sick sinus syndrome § NYHA class 1 V § Pts. Who require IV therapy for HF § Hospitalized pts specially for worsening HF § Unstable symptoms

Digoxin § For persisting symptoms in systolic dysfunction § For symptomatic and rate control of AF § To decrease the dose in elderly and pts with renal failure
Aldosterone antagonist v. Spironolactone § Add to ACEI , diuretics , beta blockers , +/digoxin § Used in NYHA class 111 and 1 V CHF § EF < 35% § It leads to 30 % ↓ in death from progressive HF
Cardiac resynchronization therapy {CRT}

ACC / AHA guidline summary– management of pts with current or prior symptoms of heart failure and a reduced left ventricular EF v. Diuretics and salt restrictions for fluid retention v. ACE I in all pts unless CI v. Beta blockers in all stable pts , unless CI
Three beta blockers proven to reduce mortality should be used… § Metaprolol § Bisoprolol § Carvidelol v Drugs that adversely affect the pts should be avoided or withdrawn if possible… • NSAID • Most antiarrythmic drugs • Most calcium channel blockers

v Angiotensin 11 receptor blockers are used in pts who cannot tolerate ACEI. Two drugs which are approved are • Candesartan • larsartan v. An implantable cardioverter-defibrillator ICD for 2 ry prevention to prolong survival in pts with h/o cardiac arrest , vent. Fib.
Drugs that should be avoided or used with caution § NSAID § Thiozolidindione group § PDE-5 inhibitors—sildenafil § Antiarryhtmics
