Pathophysiology of Cardiovascular System Dr Hemn Hassan Othman




- Slides: 61
Pathophysiology of Cardiovascular System Dr. Hemn Hassan Othman himenho 75@yahoo. com
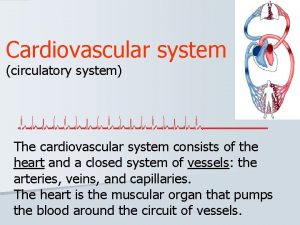
What is the circulatory system? Ø The circulatory system carries blood and dissolved substances to and from different places in the body. Ø The Heart has the job of pumping these things around the body. Ø The Heart pumps blood and substances around the body in tubes called blood vessels. Ø The Heart and blood vessels together make up the Circulatory System.
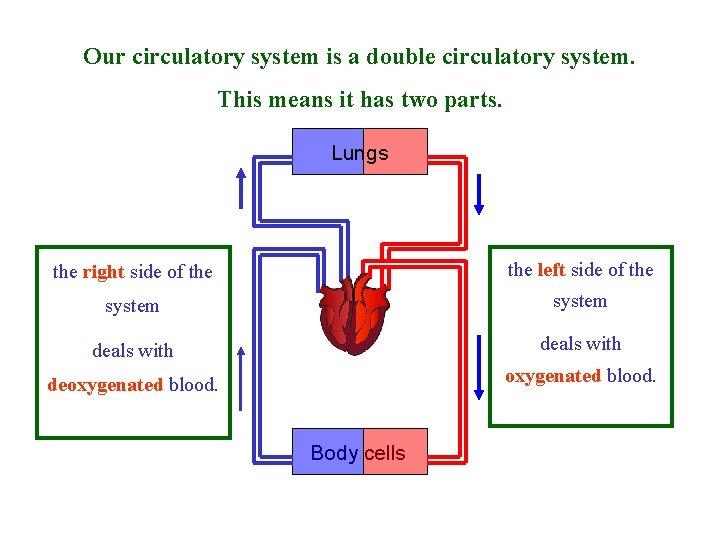
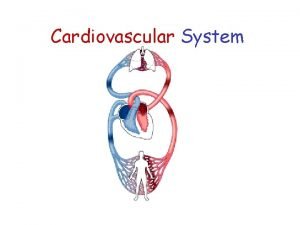
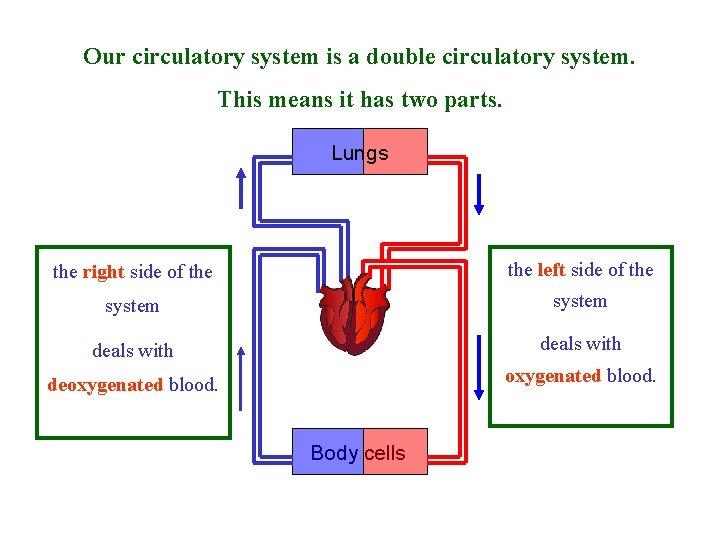
Our circulatory system is a double circulatory system. This means it has two parts. Lungs the right side of the left side of the system deals with deoxygenated blood. Body cells
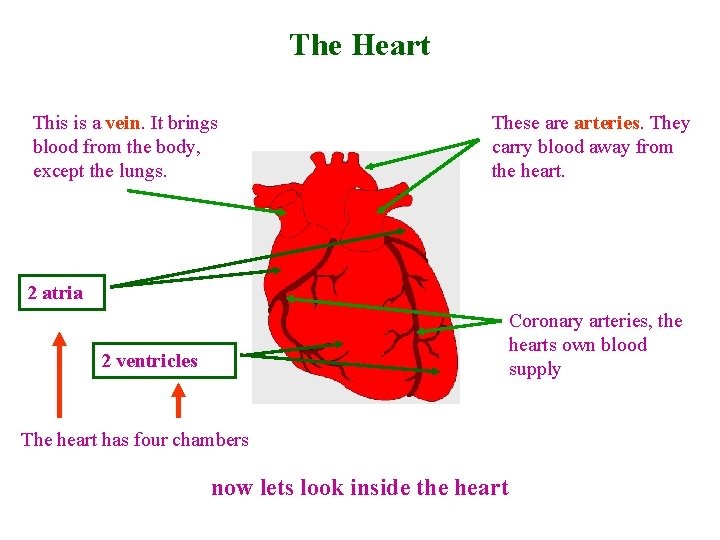
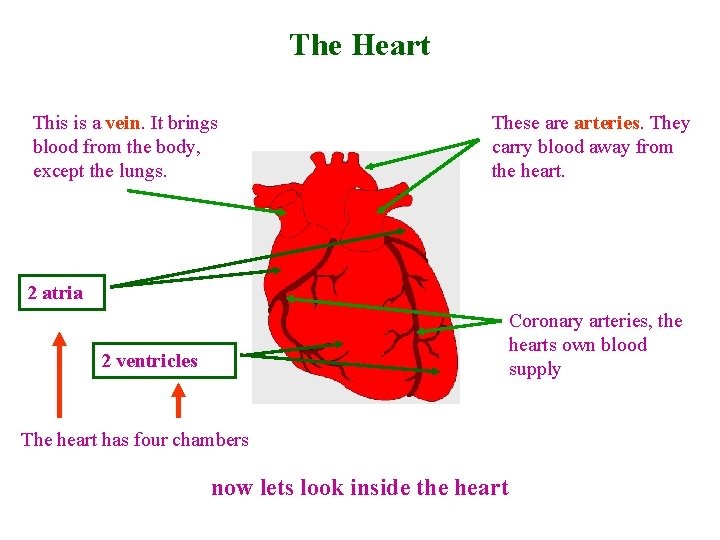
The Heart This is a vein. It brings blood from the body, except the lungs. These arteries. They carry blood away from the heart. 2 atria Coronary arteries, the hearts own blood supply 2 ventricles The heart has four chambers now lets look inside the heart
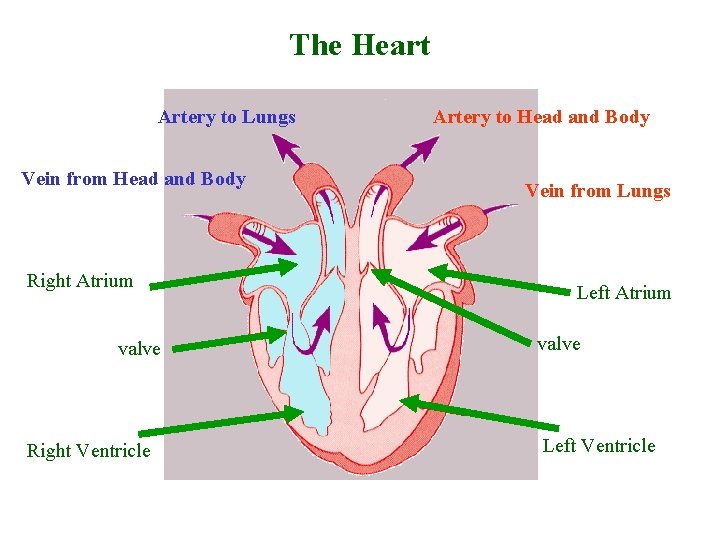
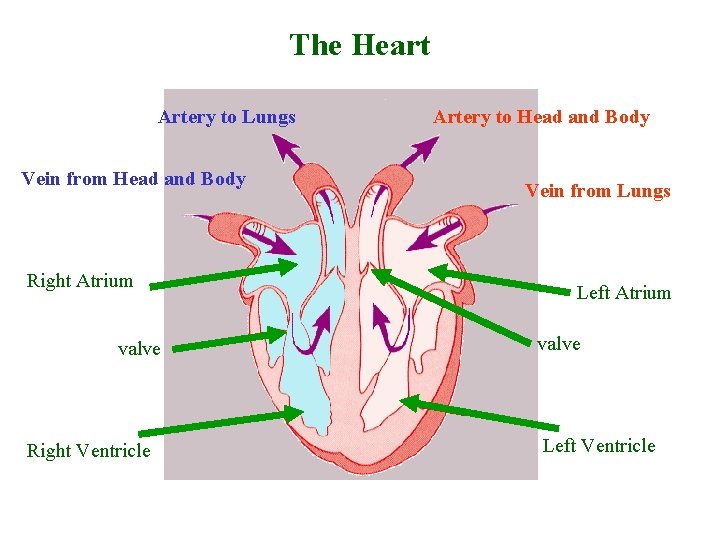
The Heart Artery to Lungs Vein from Head and Body Right Atrium valve Right Ventricle Artery to Head and Body Vein from Lungs Left Atrium valve Left Ventricle
blood from the heart gets around the body through blood vessels There are 3 types of blood vessels a. ARTERY b. VEIN c. CAPILLARY
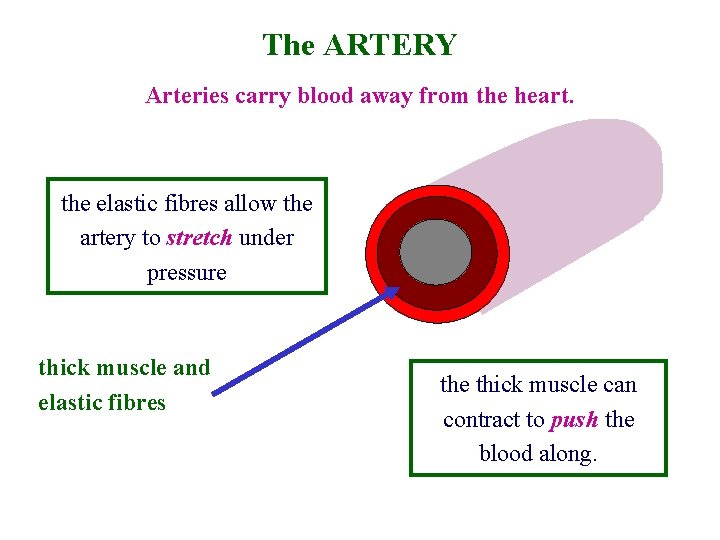
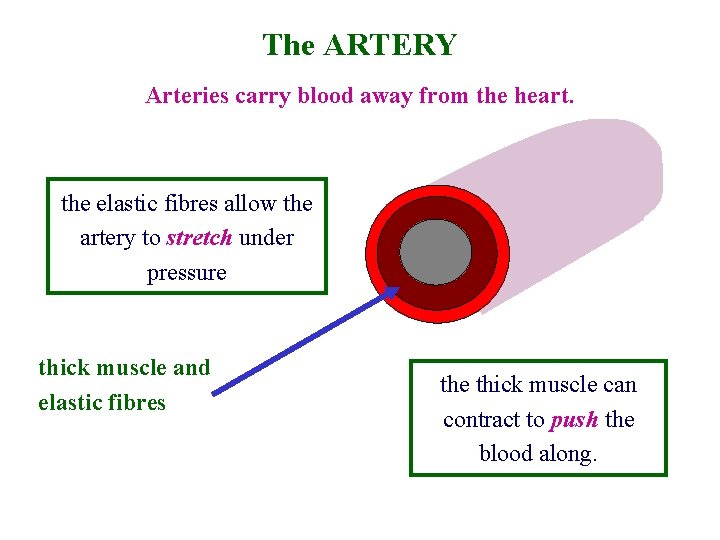
The ARTERY Arteries carry blood away from the heart. the elastic fibres allow the artery to stretch under pressure thick muscle and elastic fibres the thick muscle can contract to push the blood along.
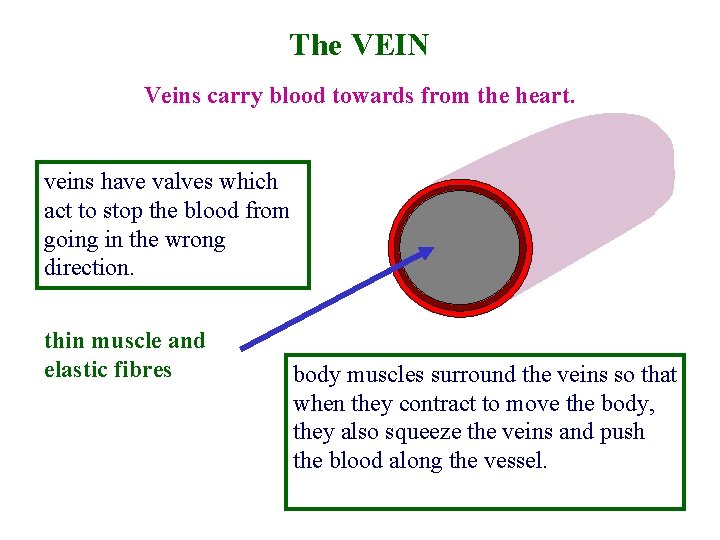
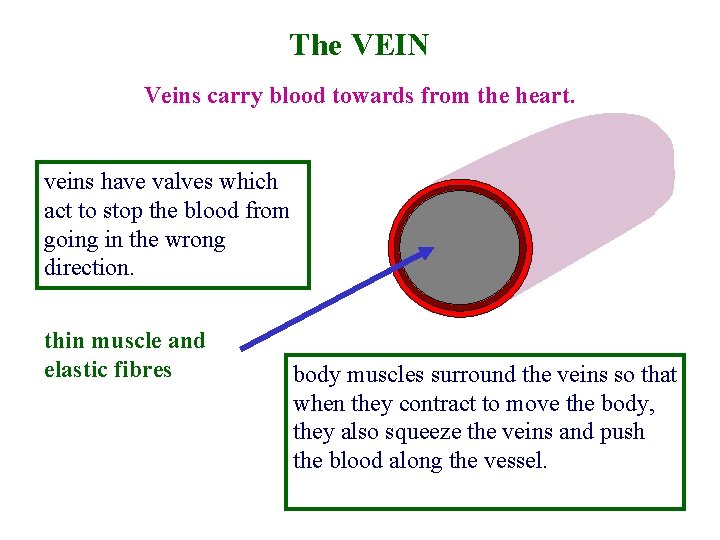
The VEIN Veins carry blood towards from the heart. veins have valves which act to stop the blood from going in the wrong direction. thin muscle and elastic fibres body muscles surround the veins so that when they contract to move the body, they also squeeze the veins and push the blood along the vessel.
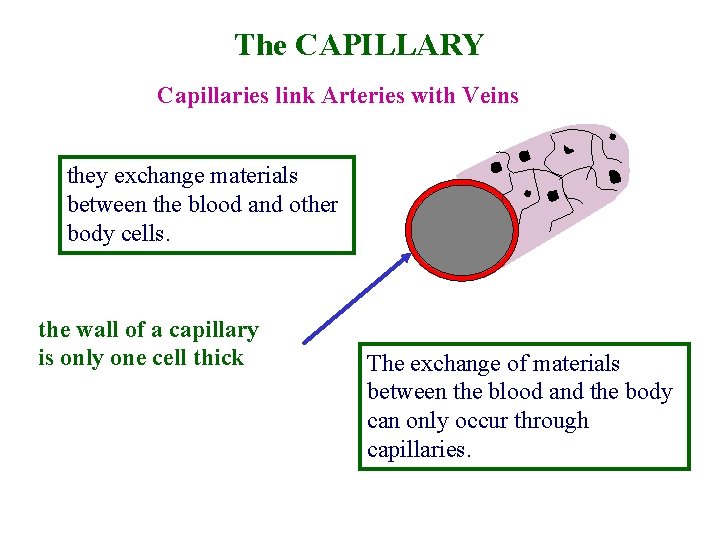
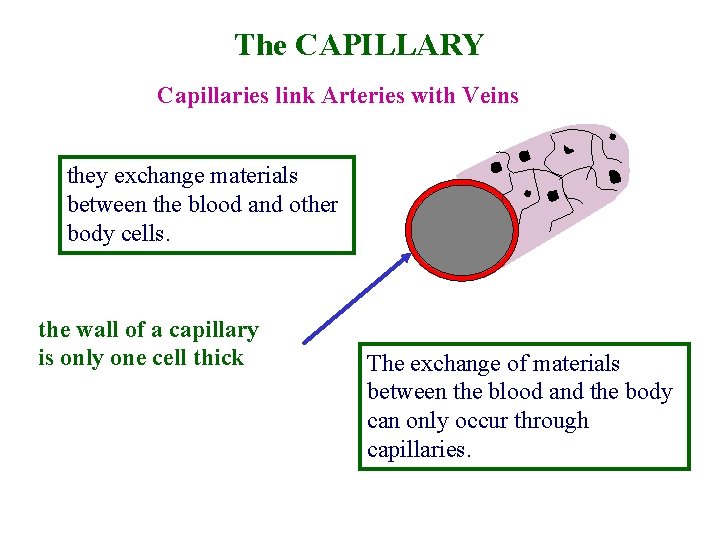
The CAPILLARY Capillaries link Arteries with Veins they exchange materials between the blood and other body cells. the wall of a capillary is only one cell thick The exchange of materials between the blood and the body can only occur through capillaries.
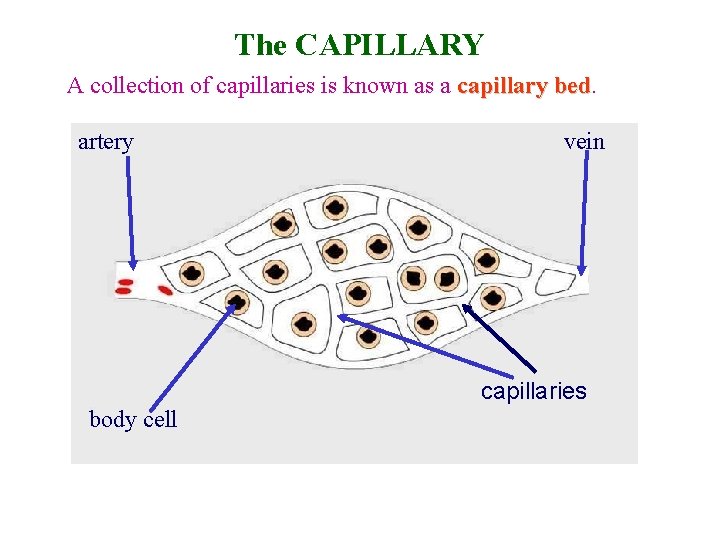
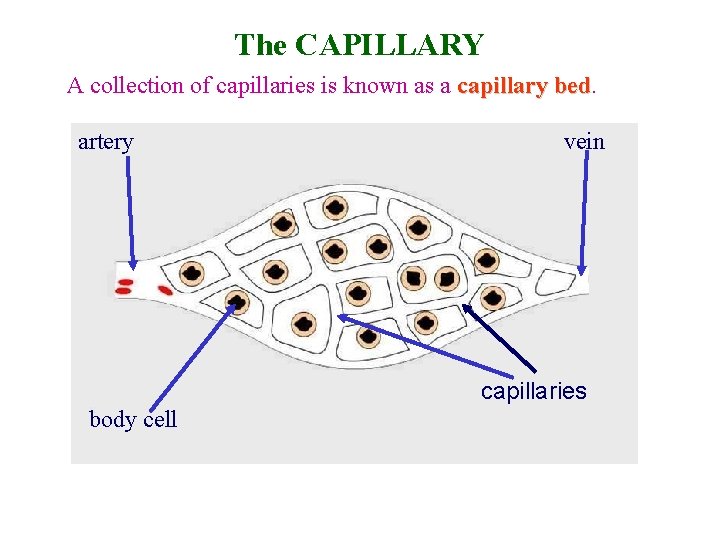
The CAPILLARY A collection of capillaries is known as a capillary bed artery vein capillaries body cell
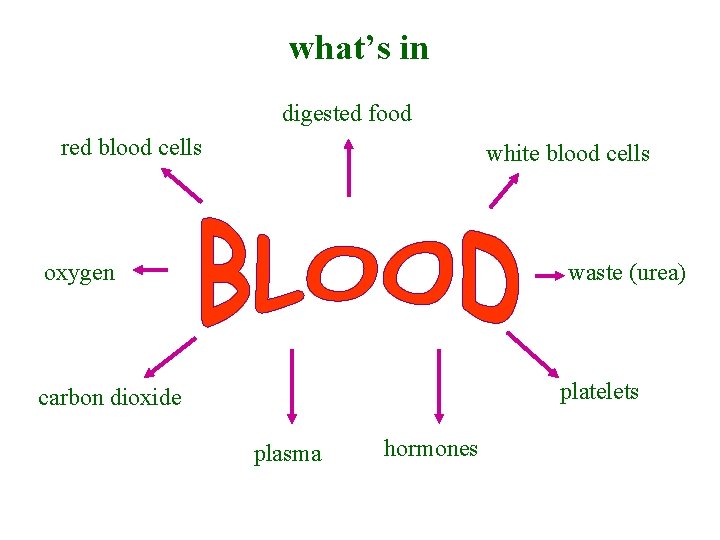
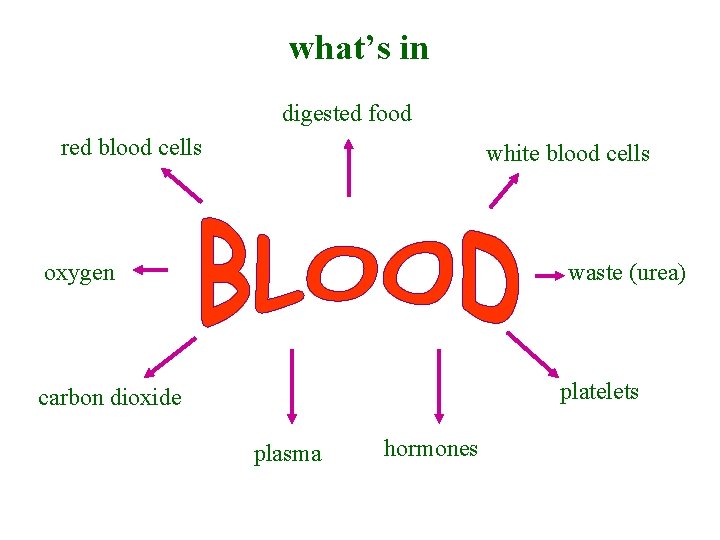
what’s in digested food red blood cells white blood cells oxygen waste (urea) platelets carbon dioxide plasma hormones
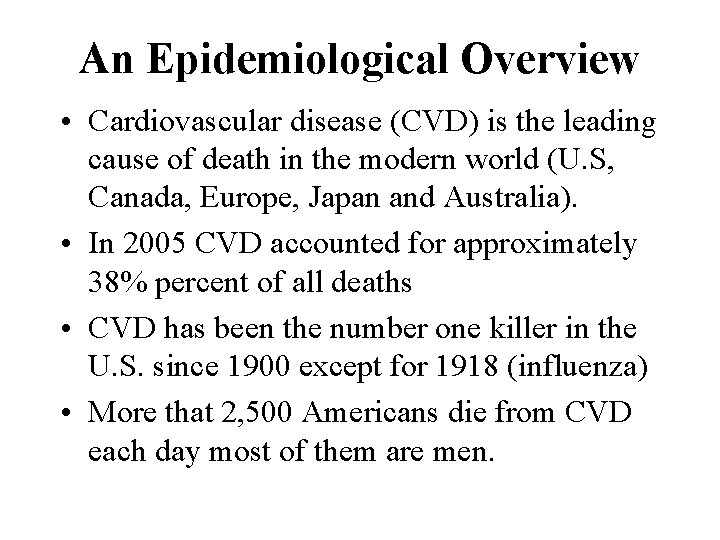
An Epidemiological Overview • Cardiovascular disease (CVD) is the leading cause of death in the modern world (U. S, Canada, Europe, Japan and Australia). • In 2005 CVD accounted for approximately 38% percent of all deaths • CVD has been the number one killer in the U. S. since 1900 except for 1918 (influenza) • More that 2, 500 Americans die from CVD each day most of them are men.
Types of Cardiovascular Disease • • Atherosclerosis Coronary heart disease (CHD) Chest pain (angina pectoris) Irregular heartbeat (arrhythmia) Congestive heart failure (CHF) Congenital and rheumatic heart disease Stroke
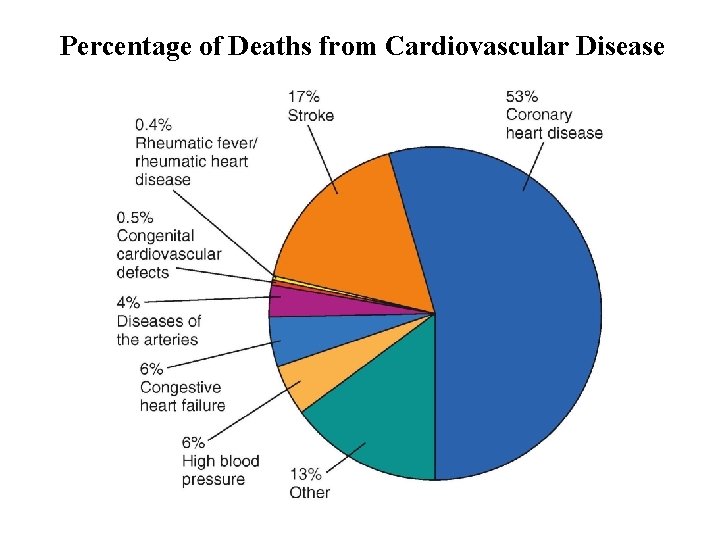
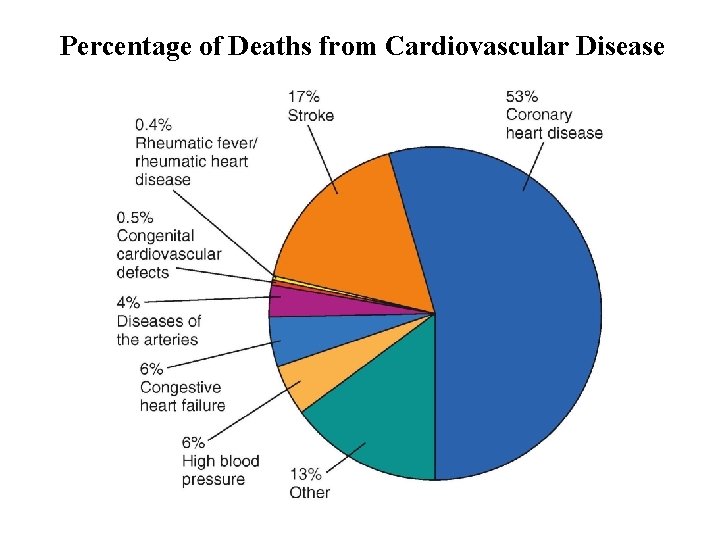
Percentage of Deaths from Cardiovascular Disease
Diseases of the Arteries and Veins
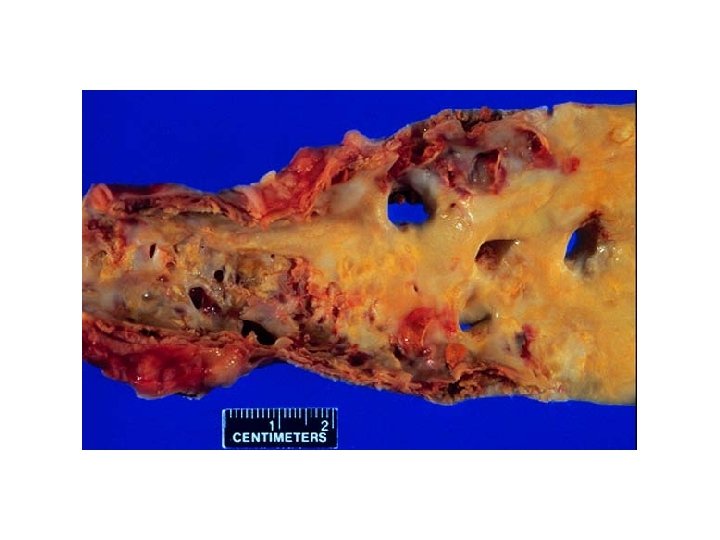
Arteriosclerosis is a general term describing hardening and loss of elasticity of the arteries. Forms of arteriosclerosis 1. Atherosclerosis is the most common form of arteriosclerosis and it refers to hardening and loss of elasticity of large and medium-sized elastic arteries such as the aorta and coronary & cerebral arteries.
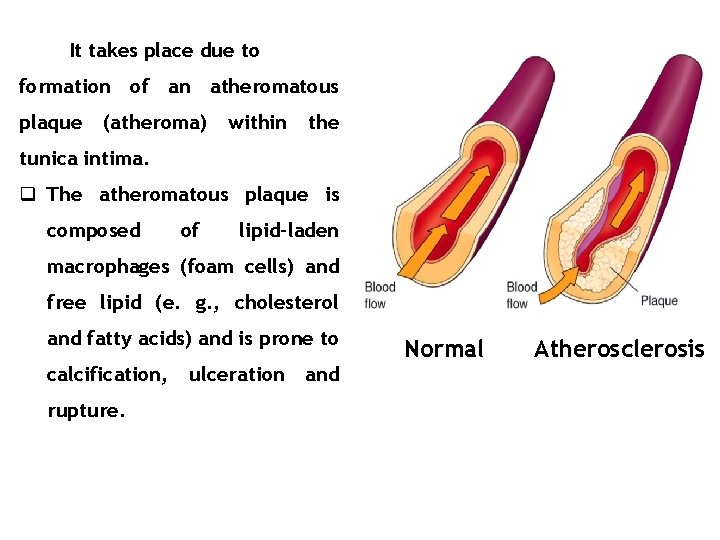
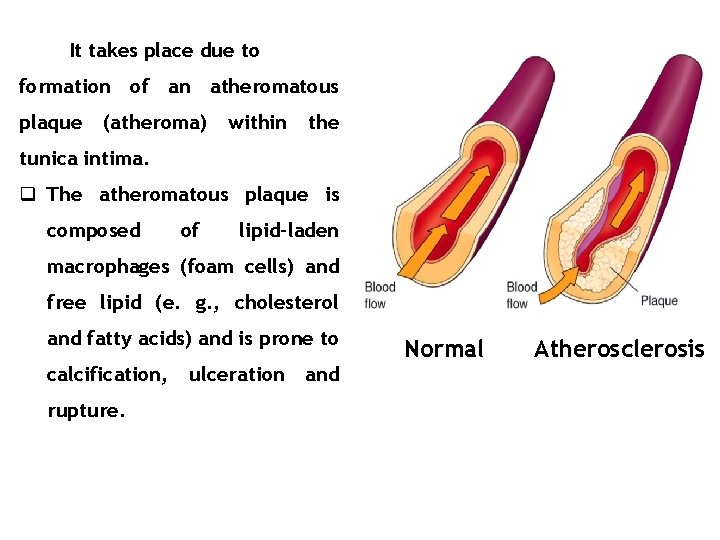
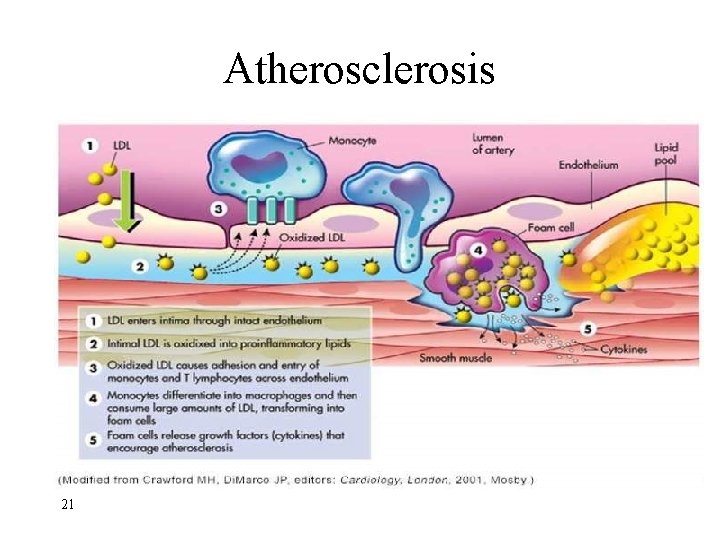
It takes place due to formation of an atheromatous plaque (atheroma) within the tunica intima. q The atheromatous plaque is composed of lipid-laden macrophages (foam cells) and free lipid (e. g. , cholesterol and fatty acids) and is prone to calcification, rupture. ulceration and Normal Atherosclerosis
Atherosclerosis • Characterized by deposits of fatty substances, cholesterol, cellular waste products, calcium, and fibrin in the inner lining of the artery • Hyperlipidemia – abnormally high blood lipid level • Plaque – the buildup of deposits in the arteries
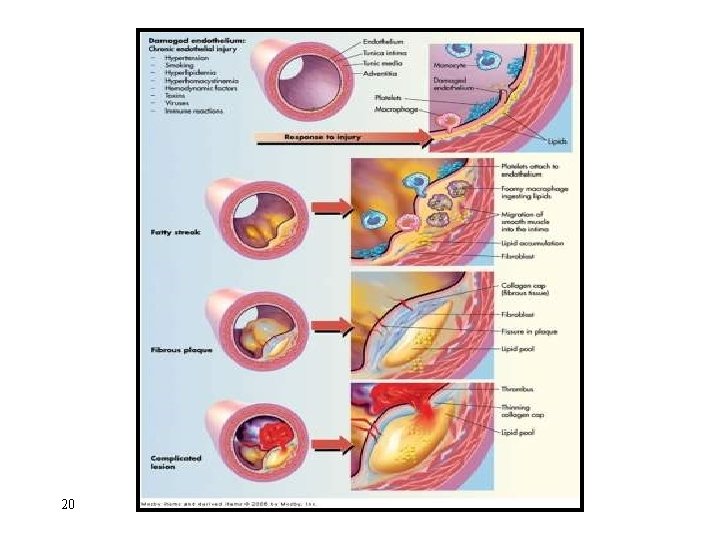
• Atherosclerosis – Pathogenesis and progression: • Inflammation of endothelium • Cellular proliferation • Macrophage migration • LDL oxidation (foam cell formation) • Fatty streak • Fibrous plaque • Complicated plaque
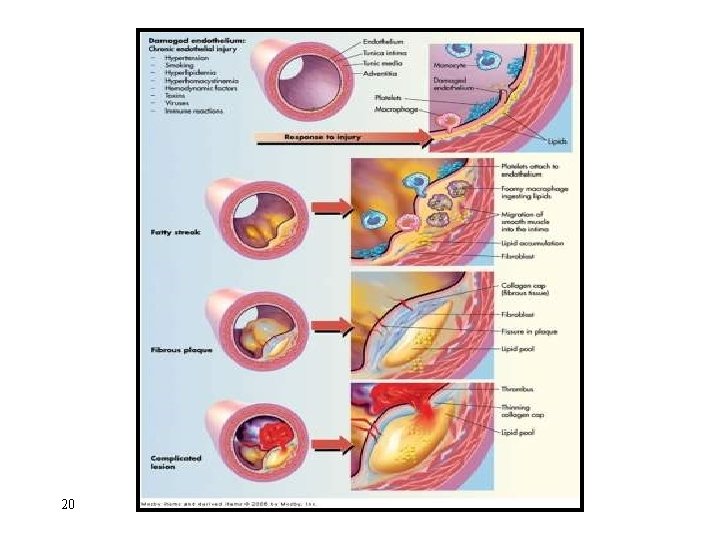
Atherosclerosis 20
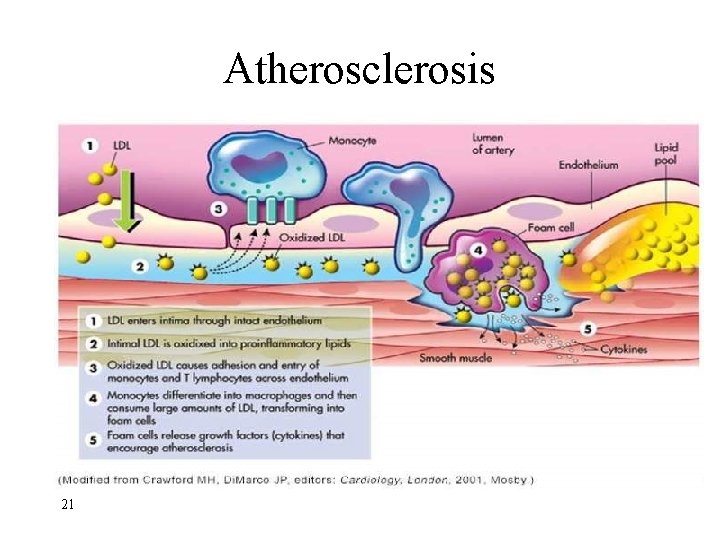
Atherosclerosis 21
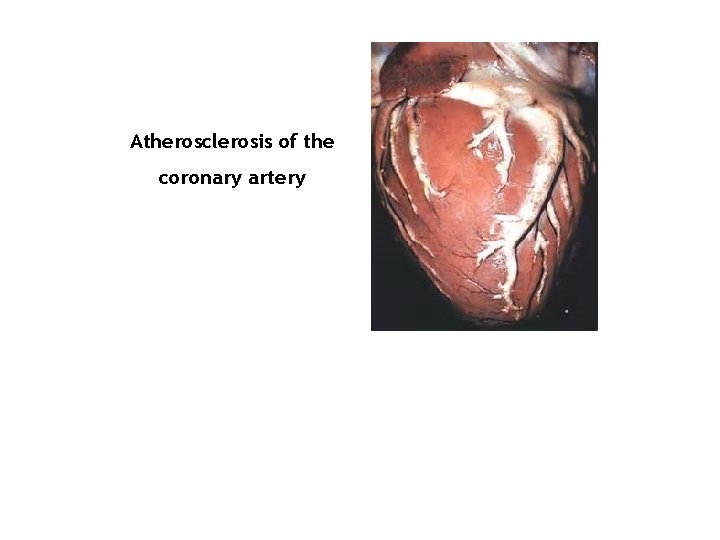
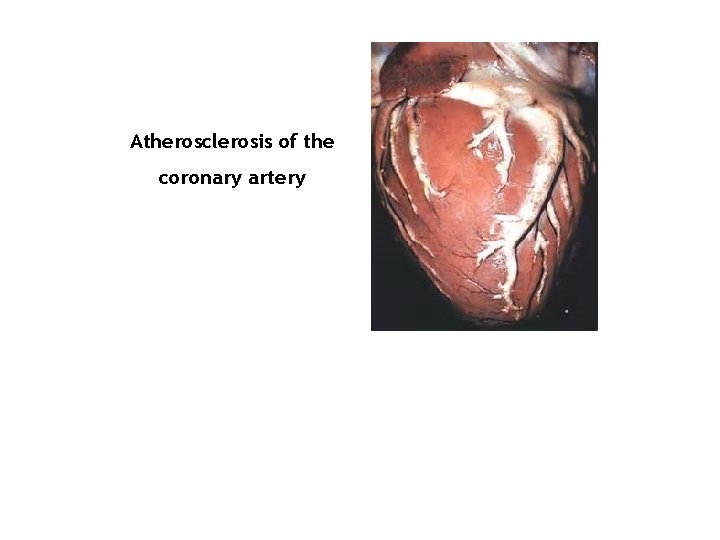
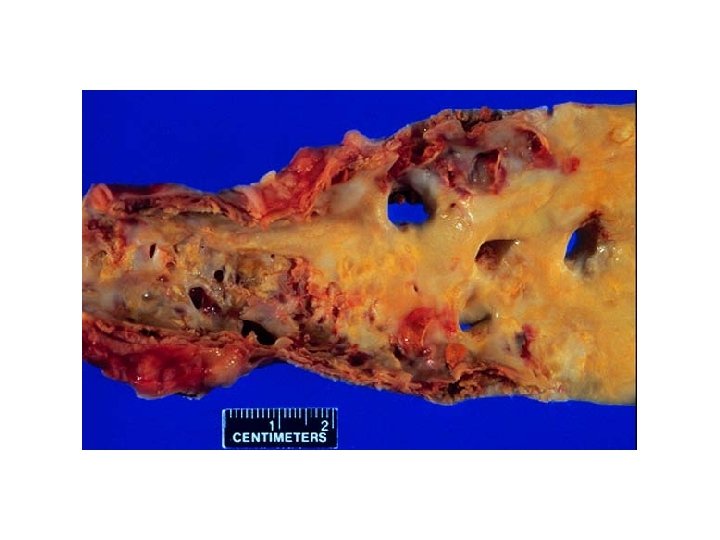
Atherosclerosis of the coronary artery
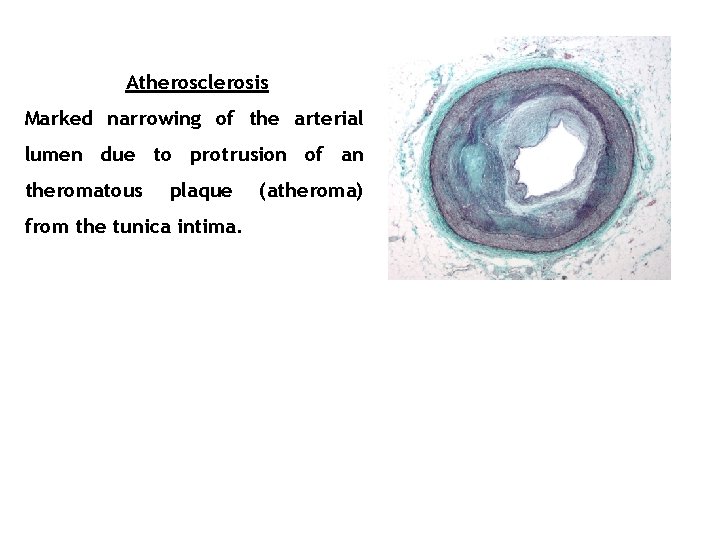
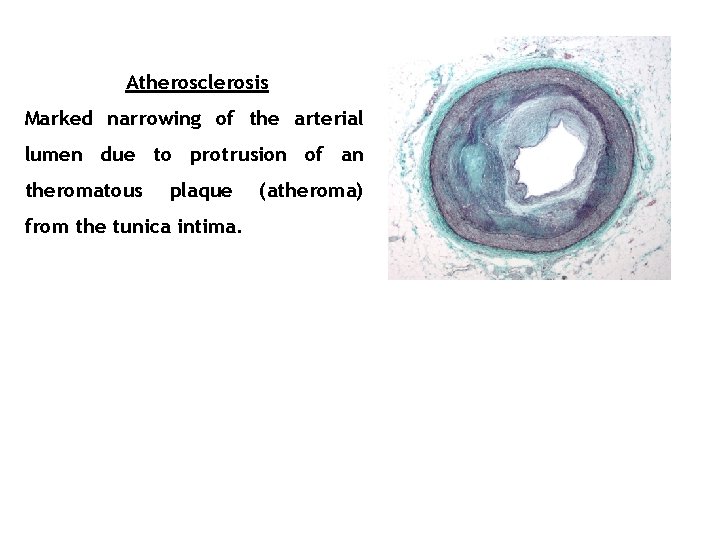
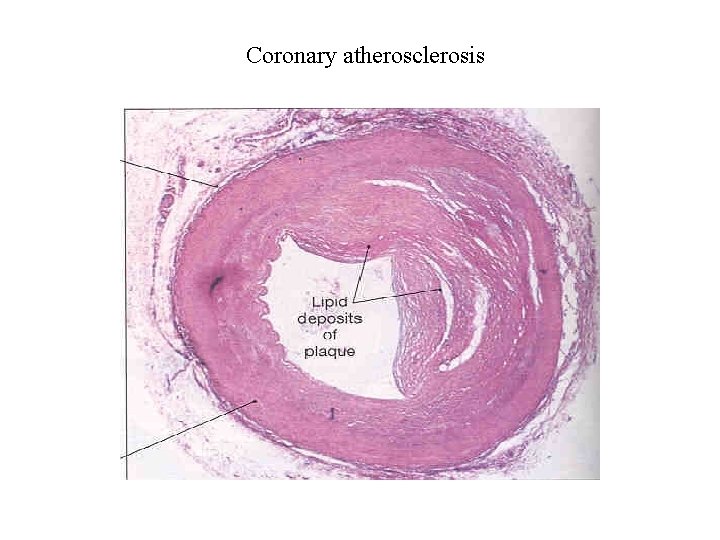
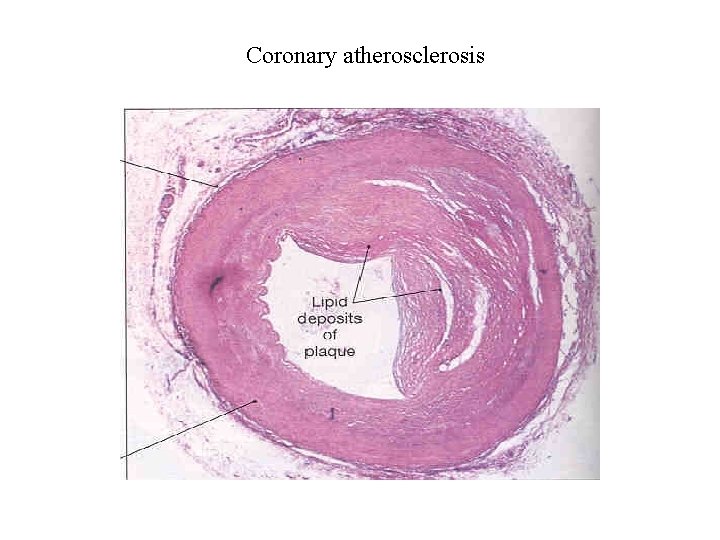
Atherosclerosis Marked narrowing of the arterial lumen due to protrusion of an theromatous plaque from the tunica intima. (atheroma)

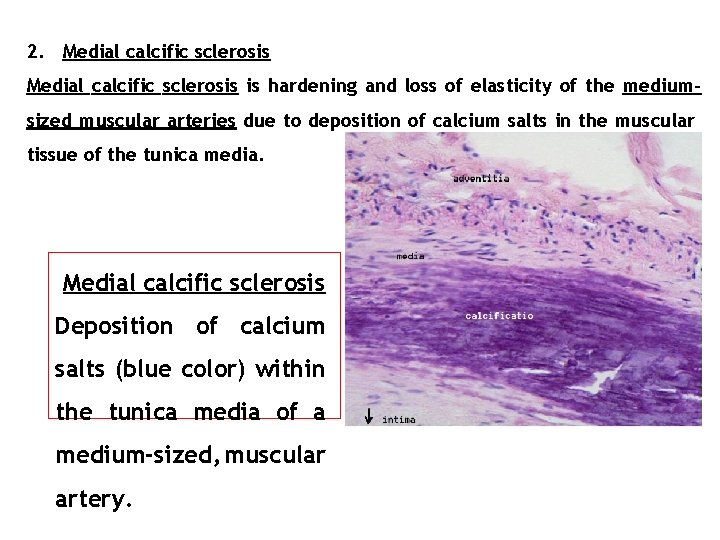
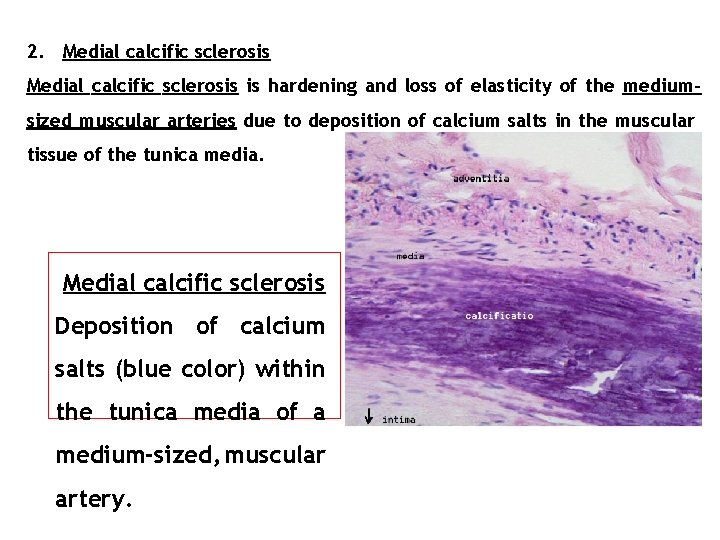
2. Medial calcific sclerosis is hardening and loss of elasticity of the mediumsized muscular arteries due to deposition of calcium salts in the muscular tissue of the tunica media. Medial calcific sclerosis Deposition of calcium salts (blue color) within the tunica media of a medium-sized, muscular artery.
v It is usually more benign than other forms of arteriosclerosis because it does not cause narrowing of the lumen. v It is seen mostly in the elderly.
3. Arteriolosclerosis is hardening and loss of elasticity of arterioles. It is most often associated with hypertension and/or diabetes mellitus. Types of arteriolosclerosis include hyaline arteriolosclerosis and hyperplastic arteriolosclerosis. Both are associated with vessel wall thickening and luminal narrowing that may cause ischemic injury.
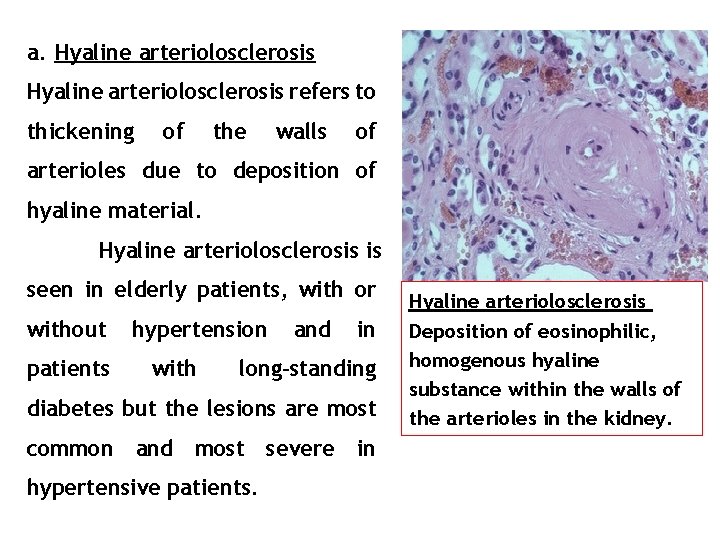
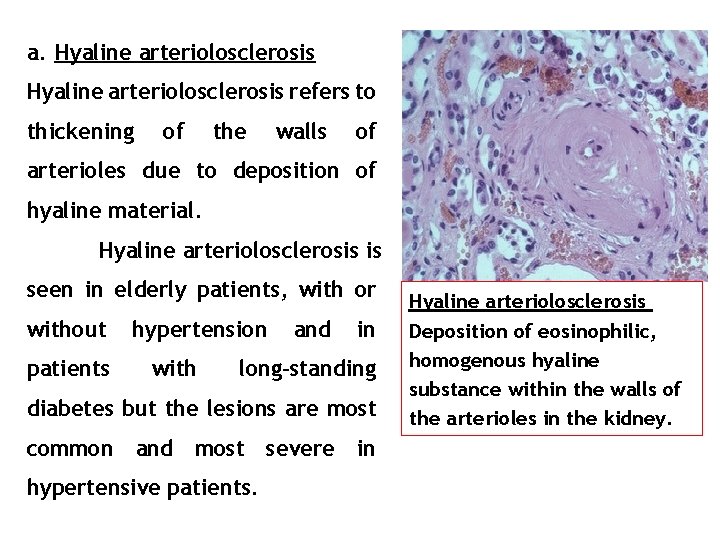
a. Hyaline arteriolosclerosis refers to thickening of the walls of arterioles due to deposition of hyaline material. Hyaline arteriolosclerosis is seen in elderly patients, with or without patients hypertension with and in long-standing diabetes but the lesions are most common and most severe in hypertensive patients. Hyaline arteriolosclerosis Deposition of eosinophilic, homogenous hyaline substance within the walls of the arterioles in the kidney.
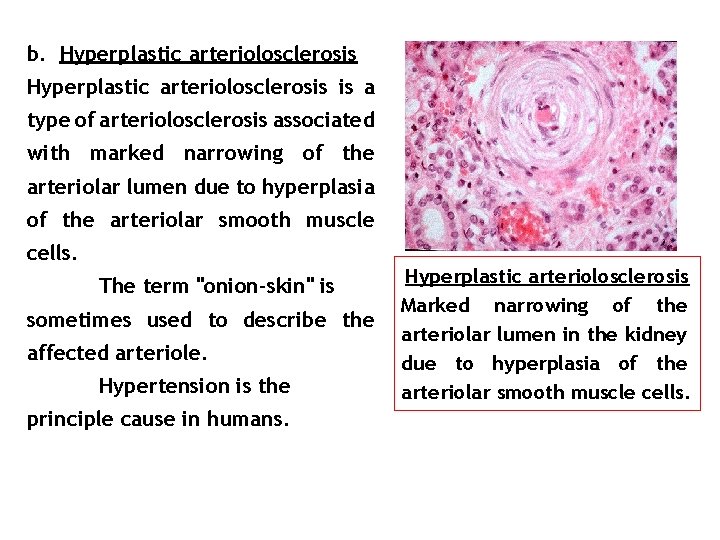
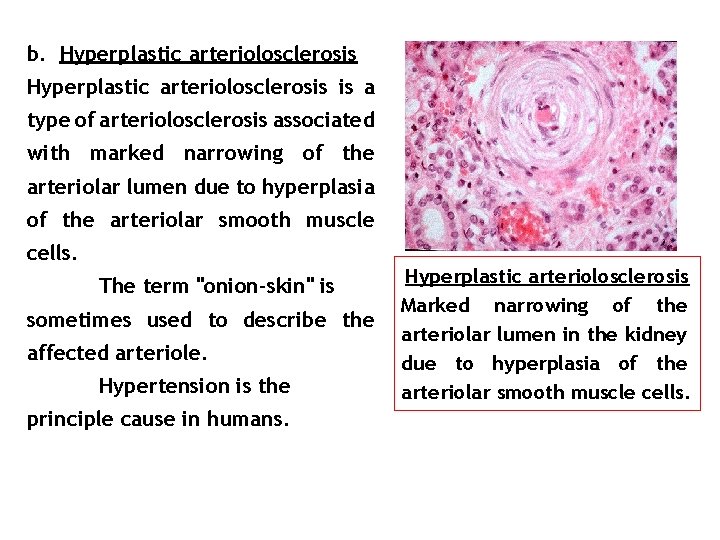
b. Hyperplastic arteriolosclerosis is a type of arteriolosclerosis associated with marked narrowing of the arteriolar lumen due to hyperplasia of the arteriolar smooth muscle cells. The term "onion-skin" is sometimes used to describe the affected arteriole. Hypertension is the principle cause in humans. Hyperplastic arteriolosclerosis Marked narrowing of the arteriolar lumen in the kidney due to hyperplasia of the arteriolar smooth muscle cells.
Ischemic Heart Diseases • This is a generic name for a group of closely related syndromes that result from myocardial ischemia. • In over 90%, this is due to a reduction in coronary blood flow. (Decrease in supply) • Other conditions arise as a result of increases in demand e. g. hypertrophy, shock, increase heart rate, etc.
Coronary Heart Disease • Myocardial infarction (MI) or heart attack – blood supplying the heart is disrupted • Coronary thrombosis – blood clot in the artery • Embolus – when the blood clot is dislodged and moves through the circulatory system
Coronary Artery Disease • Any vascular disorder that narrows or occludes the coronary arteries • Atherosclerosis is the most common cause • Risk factors – – – 33 Dyslipidemia Hypertension Cigarette smoking Diabetes mellitus Obesity/sedentary lifestyle
Coronary Artery Disease • Nontraditional risk factors – Markers of inflammation and thrombosis • C-reactive protein, fibrinogen, protein C, and plasminogen activator inhibitor – Hyperhomocysteinemia – Infections 34
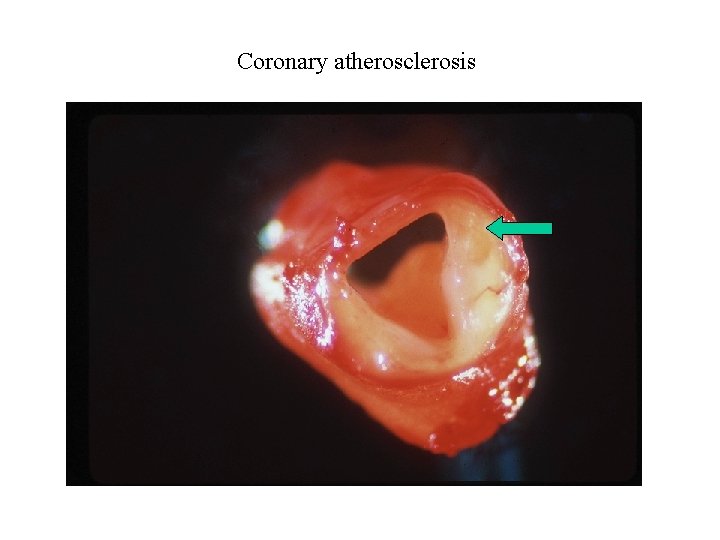
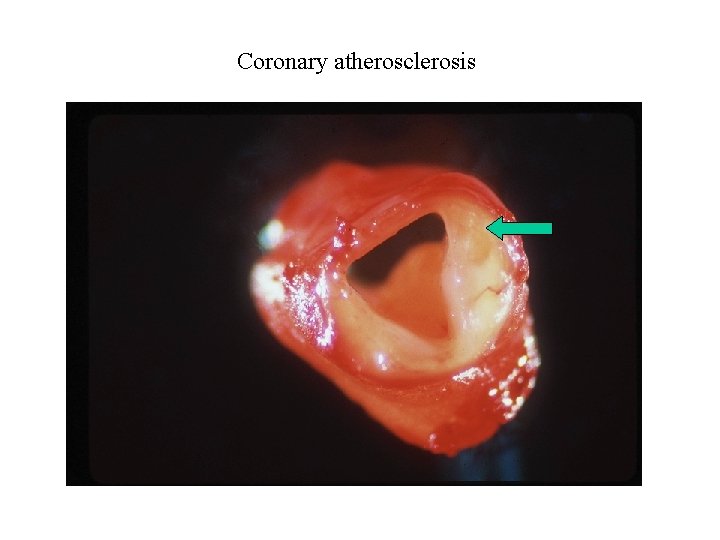
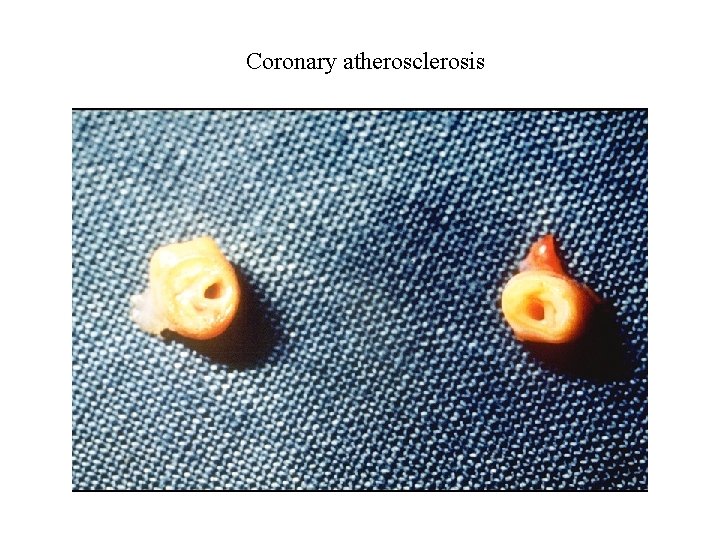
Coronary atherosclerosis
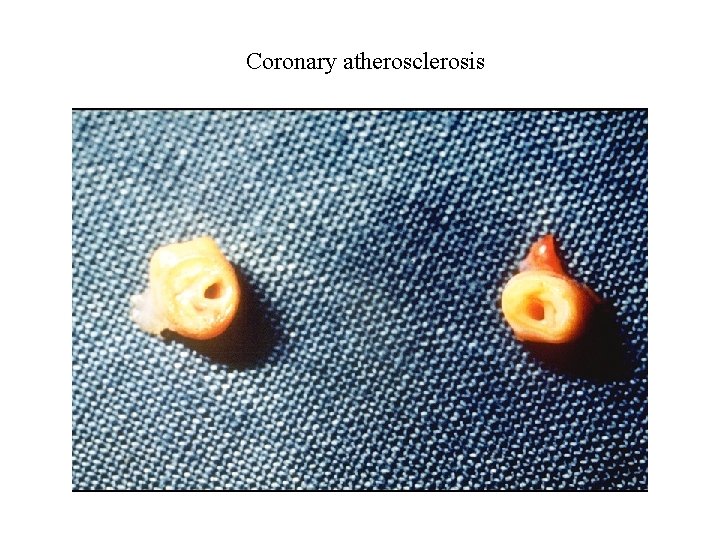
Coronary atherosclerosis
Coronary atherosclerosis
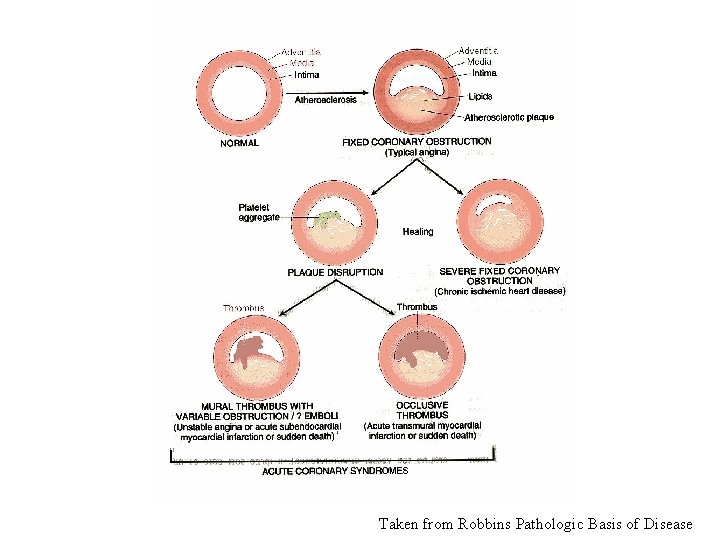
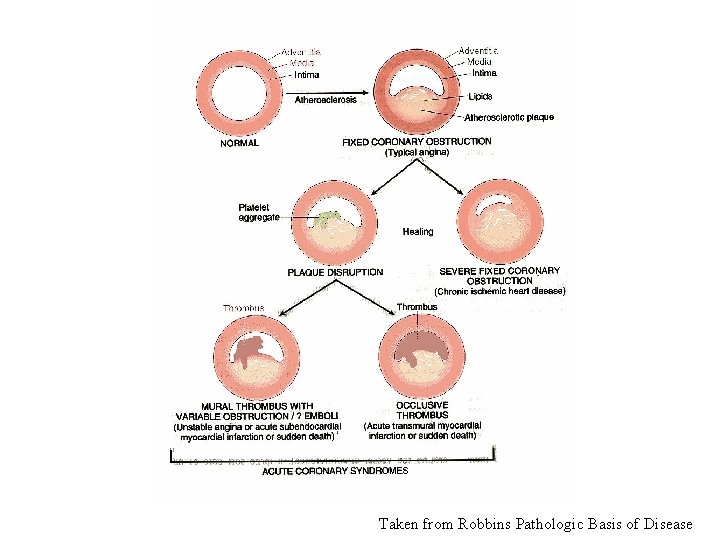
Taken from Robbins Pathologic Basis of Disease
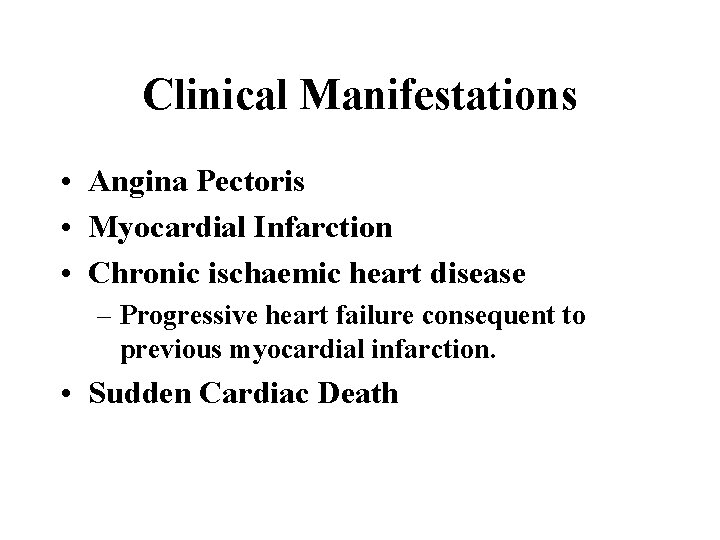
Clinical Manifestations • Angina Pectoris • Myocardial Infarction • Chronic ischaemic heart disease – Progressive heart failure consequent to previous myocardial infarction. • Sudden Cardiac Death
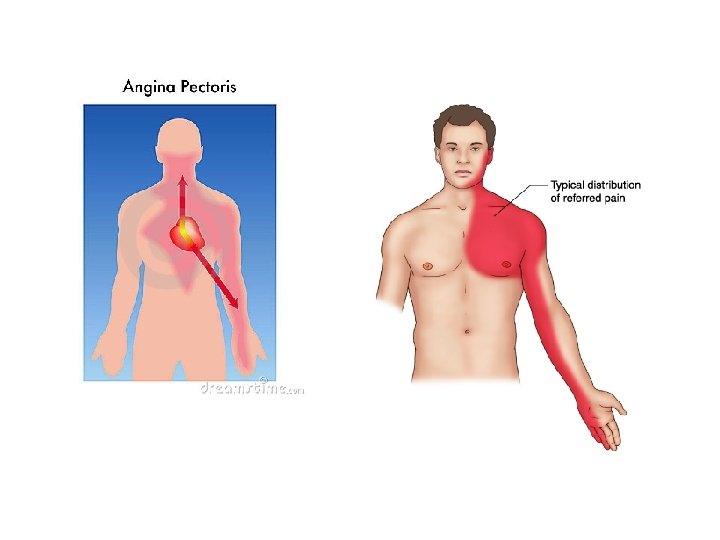
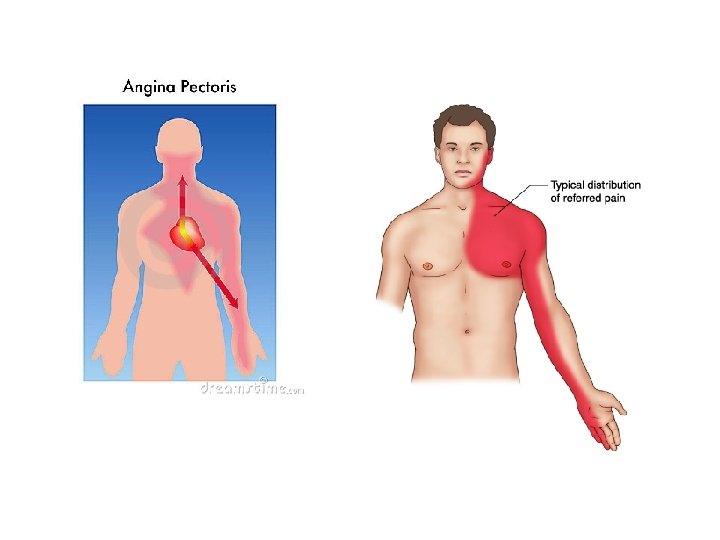
Angina Pectoris • This is a symptom complex. Symptoms caused by transient myocardial ischemia that falls short of inducing the cellular necrosis that defines myocardial infarction. • Three variants: – Stable angina – Prinzmental angina – Unstable angina
• Stable Angina – Most common form. Chronic stenosing coronary atherosclerosis, reaching a critical level, leaving the heart vulnerable to increased demand. • Typically relieved by rest or a vasodilator
Prinzmetal Angina • • Uncommon pattern Occurs at rest Documented to be due to arterial spasm Unrelated to physical activity, heart rate or blood pressure. • Generally responds to vasodilators.
Unstable Angina • Pattern here is the pain occurs with progressively increasing frequency and tends to be more prolonged • Associated with disruption of the atherosclerotic plaque, with superimposed thrombosis, embolisation or spasm. • Predictor of Myocardial Infarction

Myocardial Infarction (MI) Transmural Infarction – The ischaemic necrosis involves the full or nearly the full thickness of the ventricular wall in the distribution of a single coronary artery. – Usually associated with chronic coronary atherosclerosis, acute plaque change and superimposed completely obstructive thrombosis.
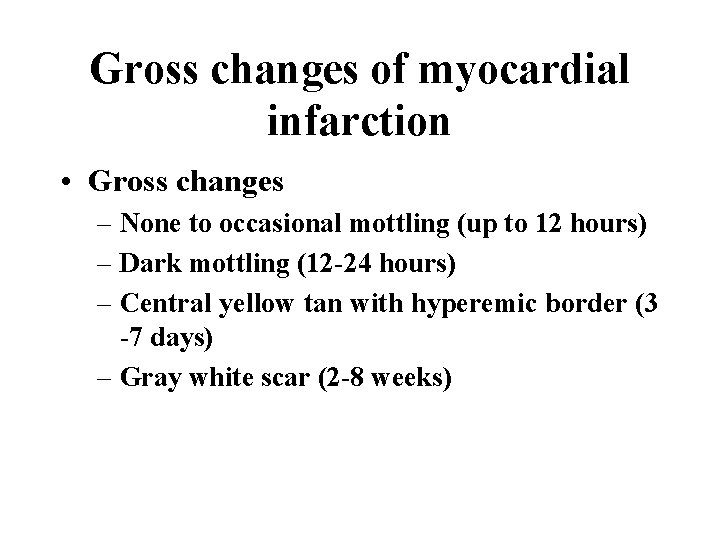
Gross changes of myocardial infarction • Gross changes – None to occasional mottling (up to 12 hours) – Dark mottling (12 -24 hours) – Central yellow tan with hyperemic border (3 -7 days) – Gray white scar (2 -8 weeks)
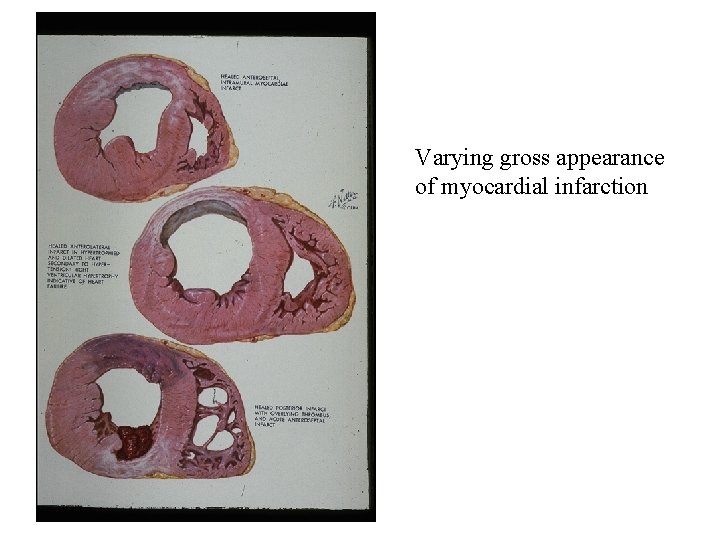
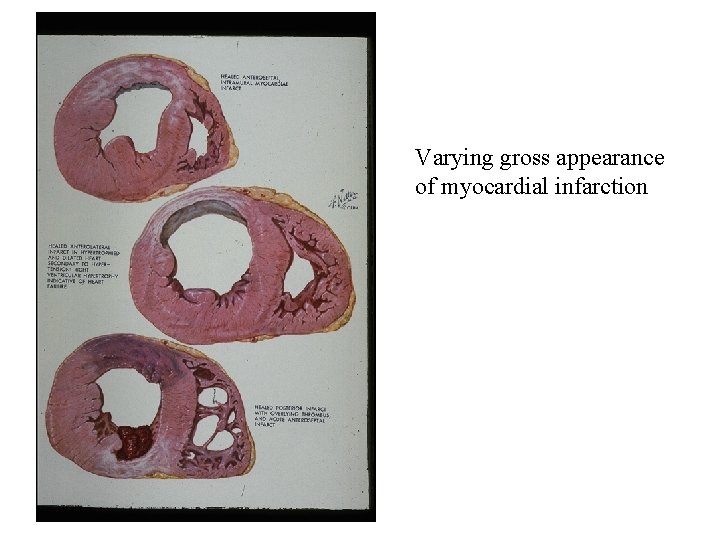
Varying gross appearance of myocardial infarction


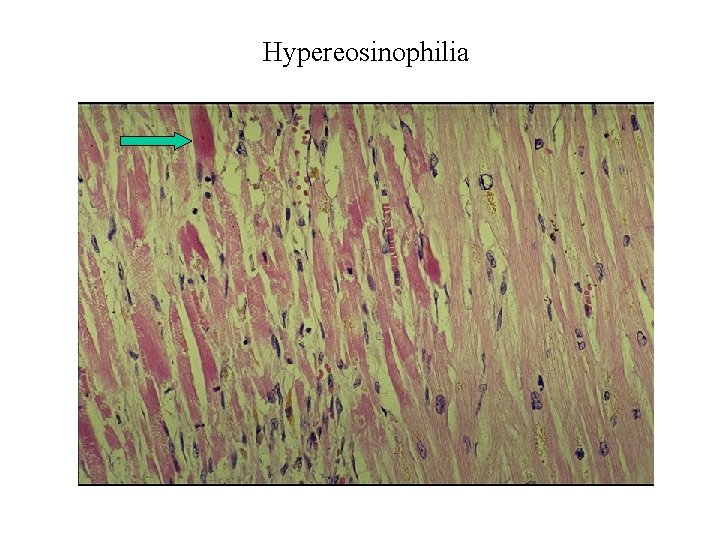
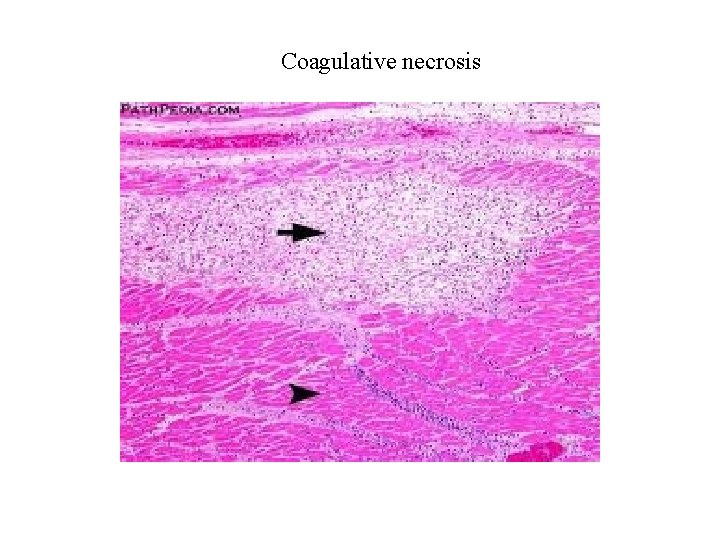
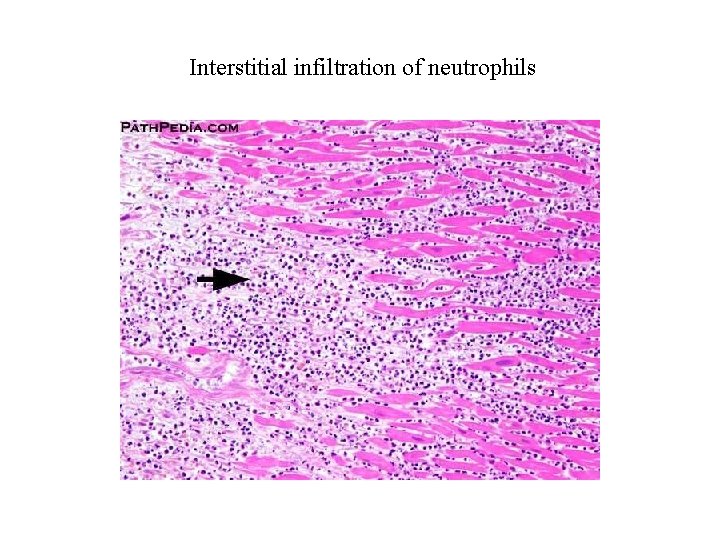
Microscopic changes of myocardial infarct • Early coagulation necrosis and oedema; haemorrhage (4 -12 hours) • Pyknosis of nucleic, hypereosinophilia, early neutrophilic infiltrate (12 -24 hours) • Coagulation necrosis, interstitial infiltrate of neutrophils (1 -3 days) • Dense collagenous scar (> 2 months)
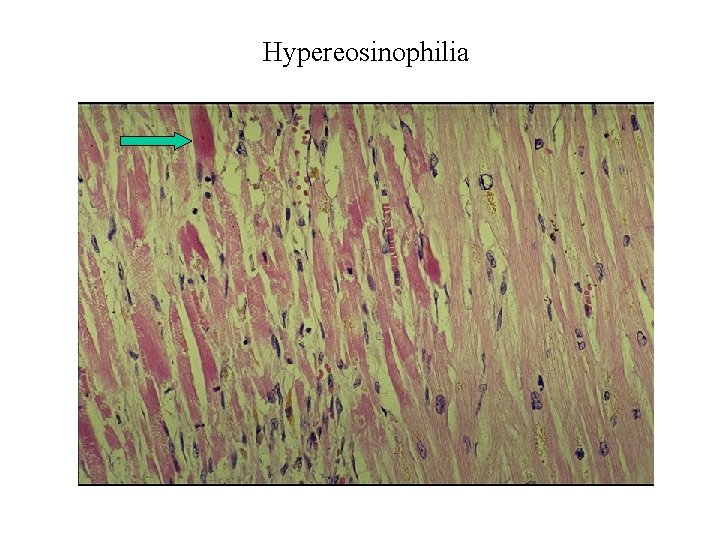
Hypereosinophilia
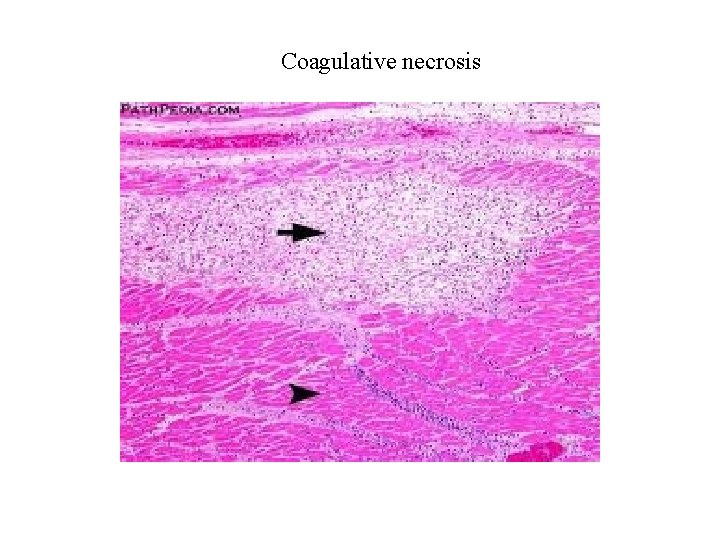
Coagulative necrosis
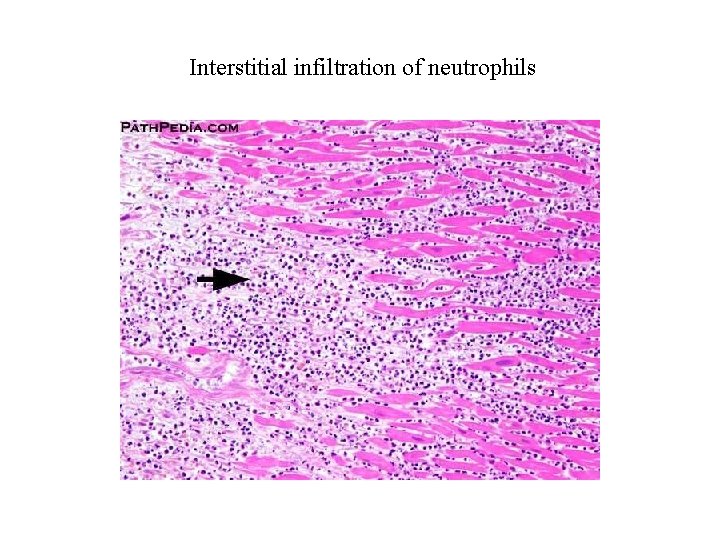
Interstitial infiltration of neutrophils
Acute effects of myocardial infarction • • • Contractile dysfunction Arrhythmias Cardiac rupture Pericarditis Sudden death – Invariably this would be due to a lethal arrhythmia (asystole or ventricular fibrillation)
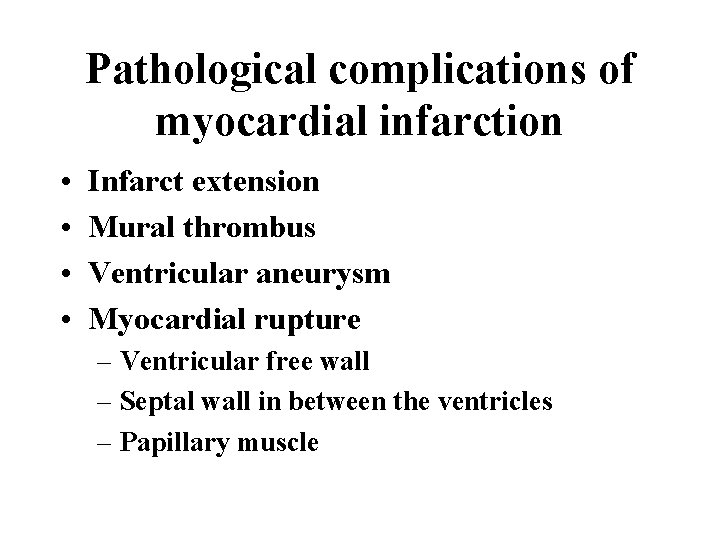
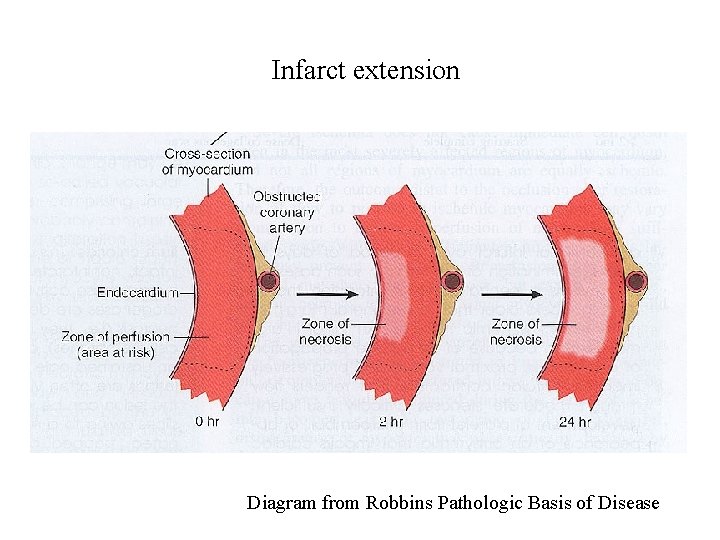
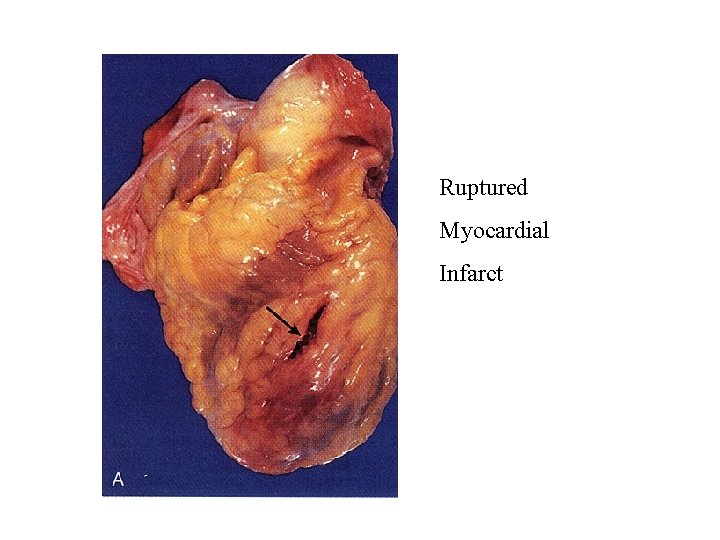
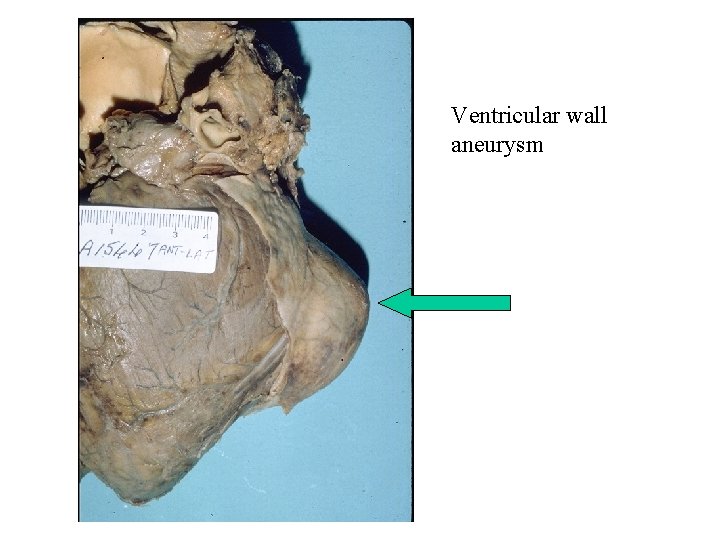
Pathological complications of myocardial infarction • • Infarct extension Mural thrombus Ventricular aneurysm Myocardial rupture – Ventricular free wall – Septal wall in between the ventricles – Papillary muscle
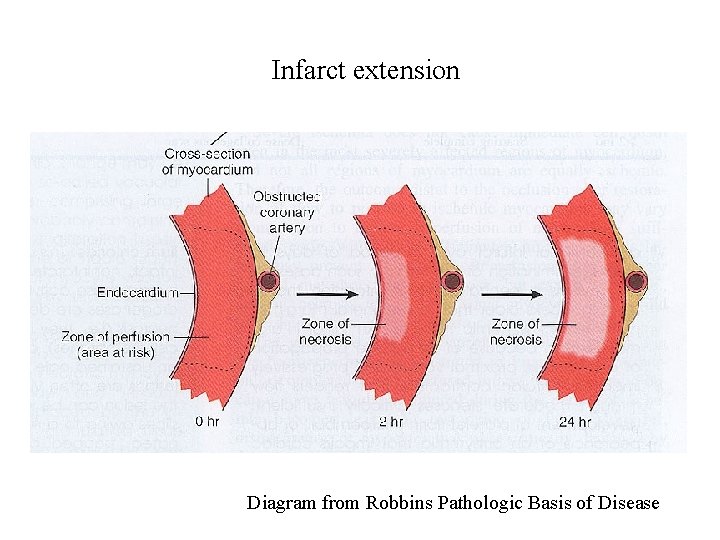
Infarct extension Diagram from Robbins Pathologic Basis of Disease
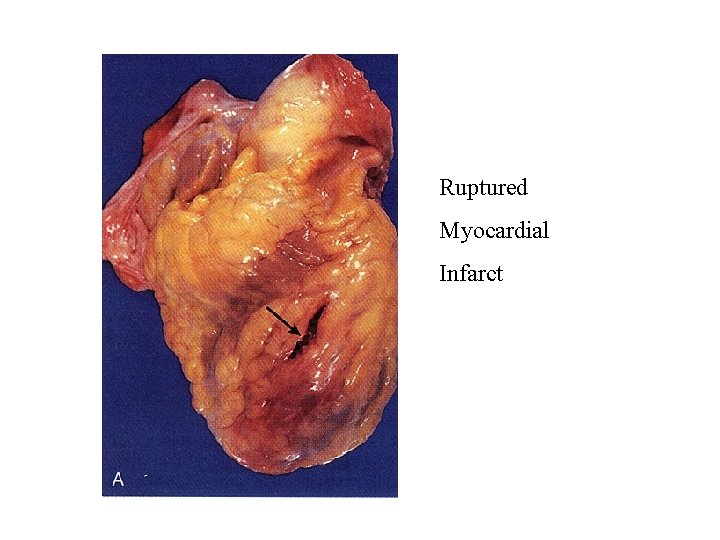
Ruptured Myocardial Infarct
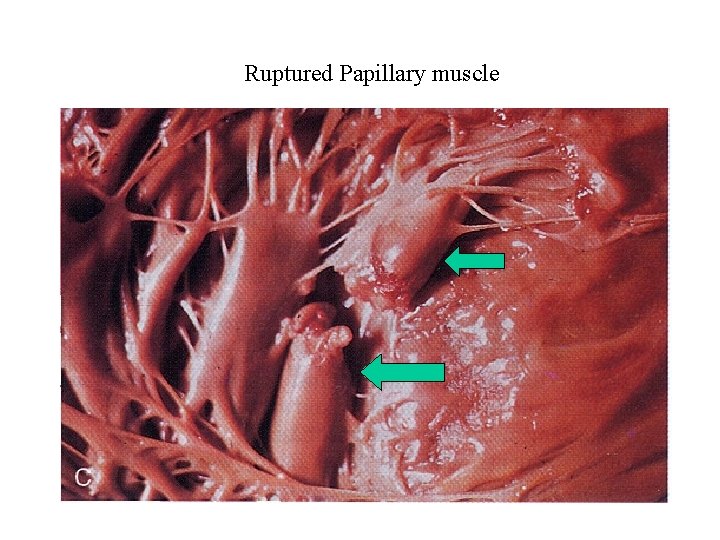
Ruptured Papillary muscle
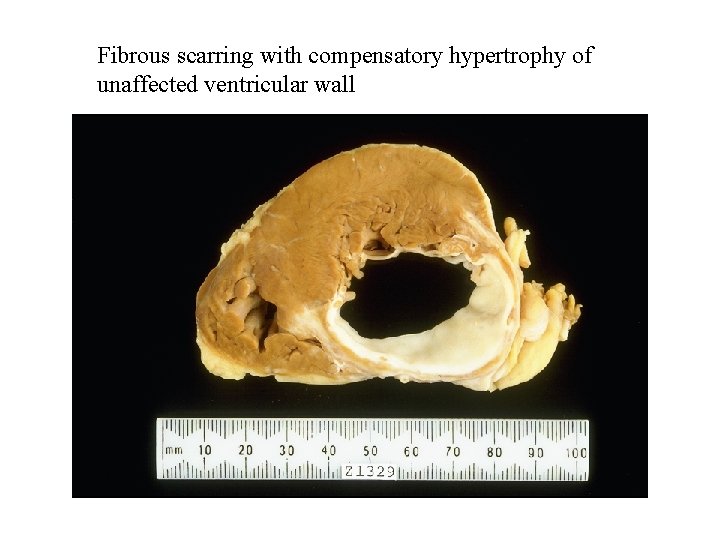
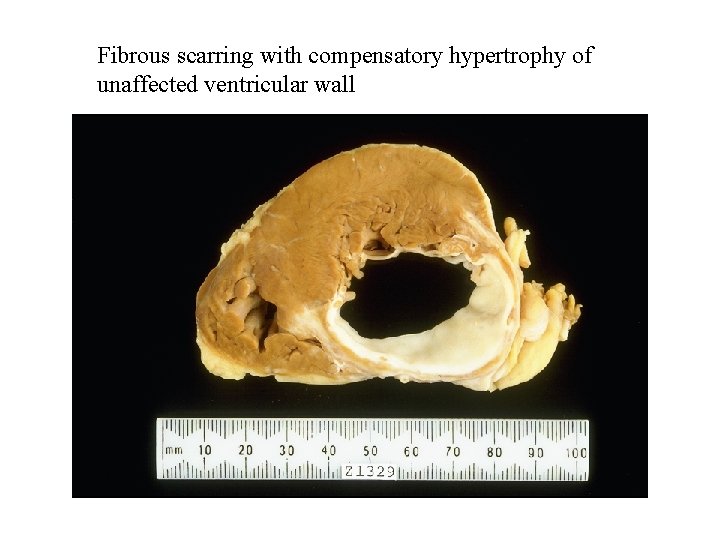
Fibrous scarring with compensatory hypertrophy of unaffected ventricular wall
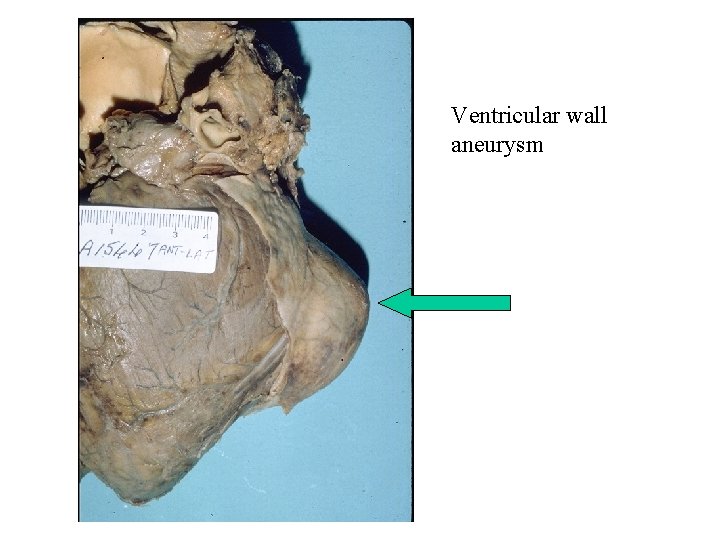
Ventricular wall aneurysm
 Othman najmi
Othman najmi Othman line 2
Othman line 2 Othman line 2
Othman line 2 Fauziah othman
Fauziah othman Breakdown due to treeing and tracking
Breakdown due to treeing and tracking Blood vesel
Blood vesel What makes up the circulatory system
What makes up the circulatory system Pithed rat model
Pithed rat model Its tubular dude
Its tubular dude Com
Com Chapter 5 the cardiovascular system labeling exercises
Chapter 5 the cardiovascular system labeling exercises Figure 11-7 veins labeled
Figure 11-7 veins labeled Figure 11-2 is an anterior view of the heart
Figure 11-2 is an anterior view of the heart Chapter 11 the cardiovascular system
Chapter 11 the cardiovascular system Lesson 11 cardiovascular system
Lesson 11 cardiovascular system The circulatory system includes
The circulatory system includes Anatomy blood vessels
Anatomy blood vessels Introduction of heart
Introduction of heart Ptca
Ptca Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 Chapter 13 cardiovascular system
Chapter 13 cardiovascular system Chapter 11 the cardiovascular system figure 11-2
Chapter 11 the cardiovascular system figure 11-2 The cardiovascular system includes the
The cardiovascular system includes the Chapter 19 cardiovascular system blood
Chapter 19 cardiovascular system blood True capillaries
True capillaries Ent université hassan 2
Ent université hassan 2 Khaled hosseini hassan
Khaled hosseini hassan Hassan hadith
Hassan hadith Amanda hassan
Amanda hassan Hassan chafi
Hassan chafi Mahmood ul hassan islamic aid
Mahmood ul hassan islamic aid Marwan hassan mustafa
Marwan hassan mustafa Affine cipher
Affine cipher Comparati baladele pasa hassan
Comparati baladele pasa hassan Anil hassan
Anil hassan Hassan amjahad
Hassan amjahad Hassan akbari
Hassan akbari Hassan tout
Hassan tout Dr sheref hassan
Dr sheref hassan Crao
Crao Hassan takabi
Hassan takabi Yasir drabu
Yasir drabu Dr mona idris
Dr mona idris Hassan mokhlis
Hassan mokhlis Junaid hassan
Junaid hassan Spermatic cord
Spermatic cord Literary analysis of the kite runner
Literary analysis of the kite runner Dr uzma hassan
Dr uzma hassan Dr hassan abdalla
Dr hassan abdalla Bassidi hassan
Bassidi hassan Muhammad hasmi abu hassan asaari
Muhammad hasmi abu hassan asaari Saad mohsen ٨- احذر احذر
Saad mohsen ٨- احذر احذر Hassan makki
Hassan makki Mohamed akel
Mohamed akel Bad writing examples
Bad writing examples Ayaz ul hassan
Ayaz ul hassan Syed afaq hassan solicitor
Syed afaq hassan solicitor Junaid hassan
Junaid hassan Theme of sacrifice
Theme of sacrifice Hassan peerhossaini
Hassan peerhossaini Hassan sayyadi
Hassan sayyadi