The Cardiovascular System Blood Vessels Physiology Chapter 19
The Cardiovascular System: Blood Vessels Physiology Chapter 19, Cardiovascular System - Blood Vessel 19 1
Capillary Exchange Chapter 19, Cardiovascular System - Blood Vessel 2

Capillary Beds § A microcirculation of interwoven networks of capillaries, consisting of: § Vascular shunts – metarteriole–thoroughfare channel connecting an arteriole directly with a postcapillary venule § True capillaries – 10 to 100 per capillary bed, capillaries branch off the metarteriole and return to the thoroughfare channel at the distal end of the bed Chapter 19, Cardiovascular System - Blood Vessel 3
Blood Flow Through Capillary Beds § Precapillary sphincter § Cuff of smooth muscle that surrounds each true capillary § Regulates blood flow into the capillary § Blood flow is regulated by vasomotor nerves and local chemical conditions, so it can either bypass or flood the capillary bed Chapter 19, Cardiovascular System - Blood Vessel 4
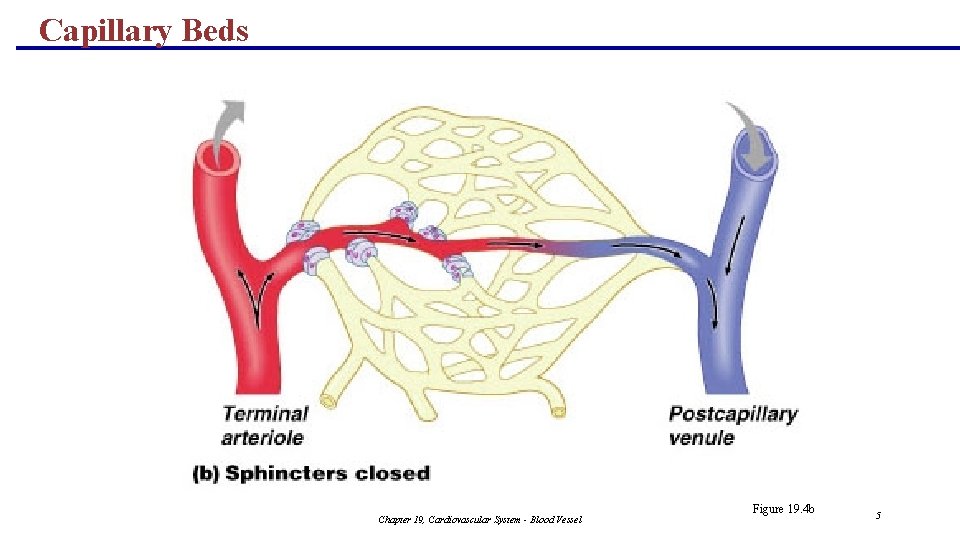
Capillary Beds Chapter 19, Cardiovascular System - Blood Vessel Figure 19. 4 b 5
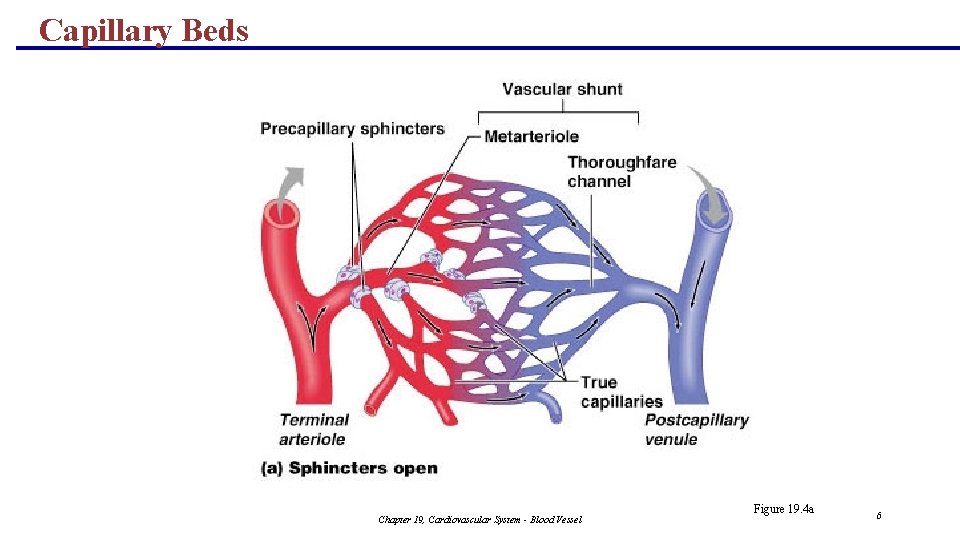
Capillary Beds Chapter 19, Cardiovascular System - Blood Vessel Figure 19. 4 a 6
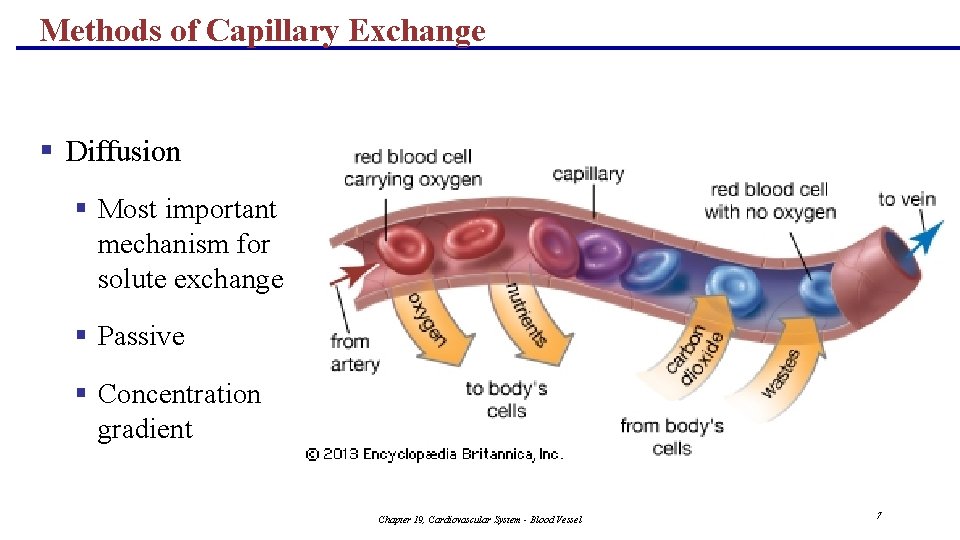
Methods of Capillary Exchange § Diffusion § Most important mechanism for solute exchange § Passive § Concentration gradient Chapter 19, Cardiovascular System - Blood Vessel 7
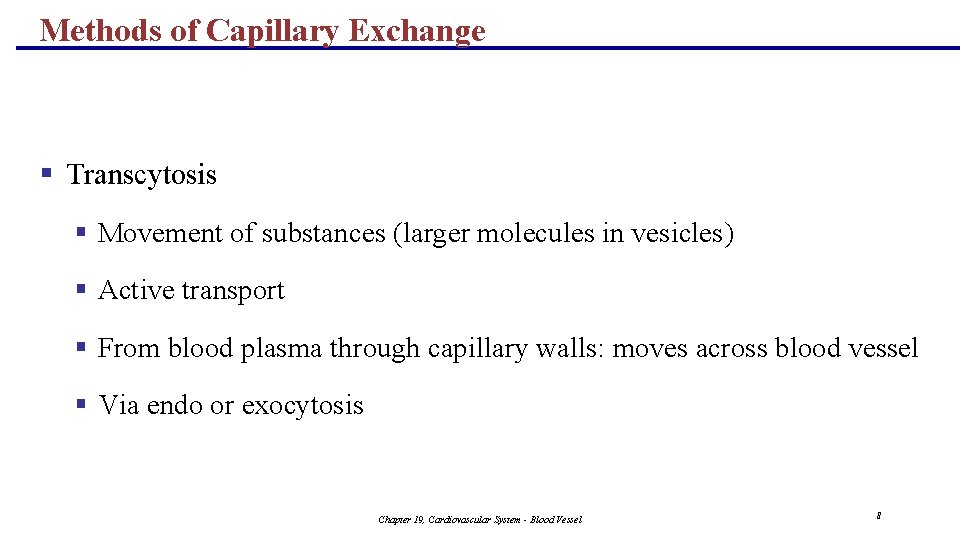
Methods of Capillary Exchange § Transcytosis § Movement of substances (larger molecules in vesicles) § Active transport § From blood plasma through capillary walls: moves across blood vessel § Via endo or exocytosis Chapter 19, Cardiovascular System - Blood Vessel 8
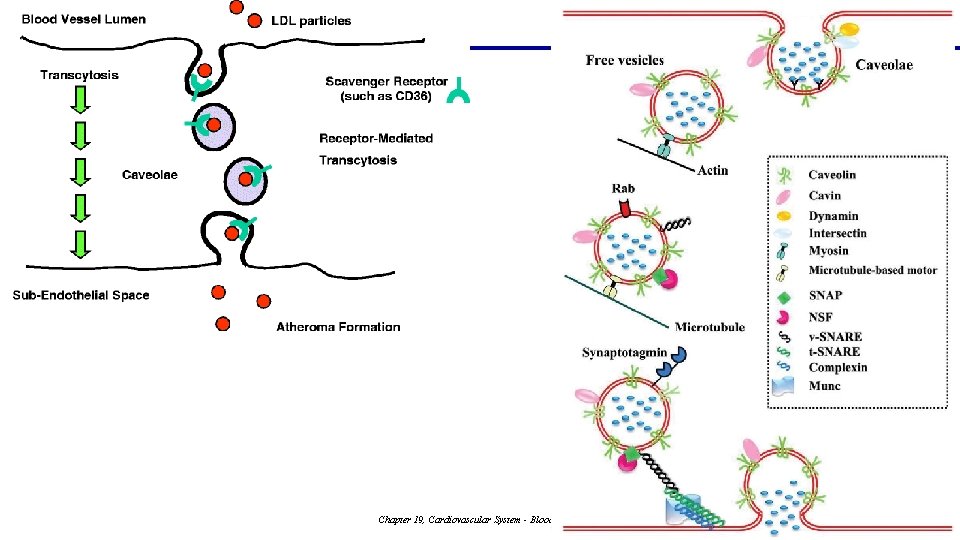
Chapter 19, Cardiovascular System - Blood Vessel 9

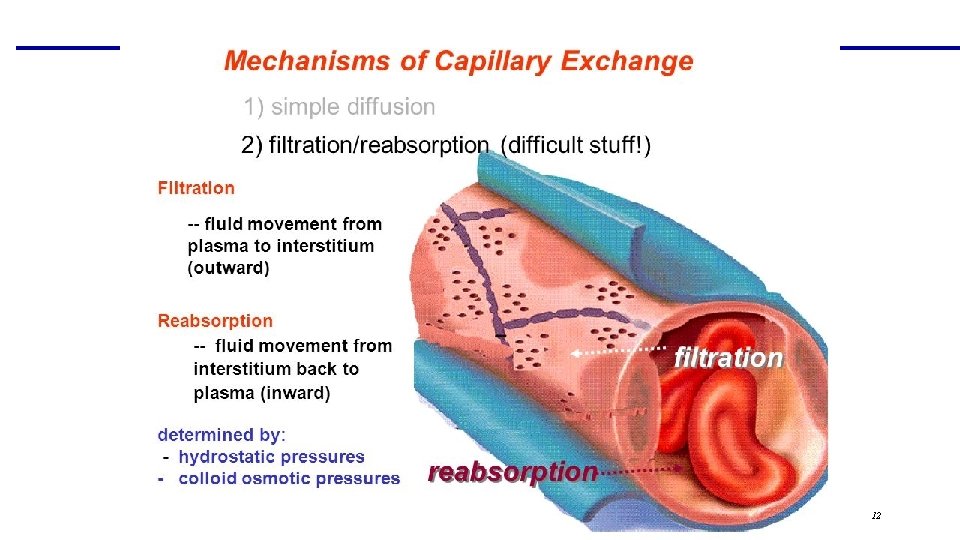
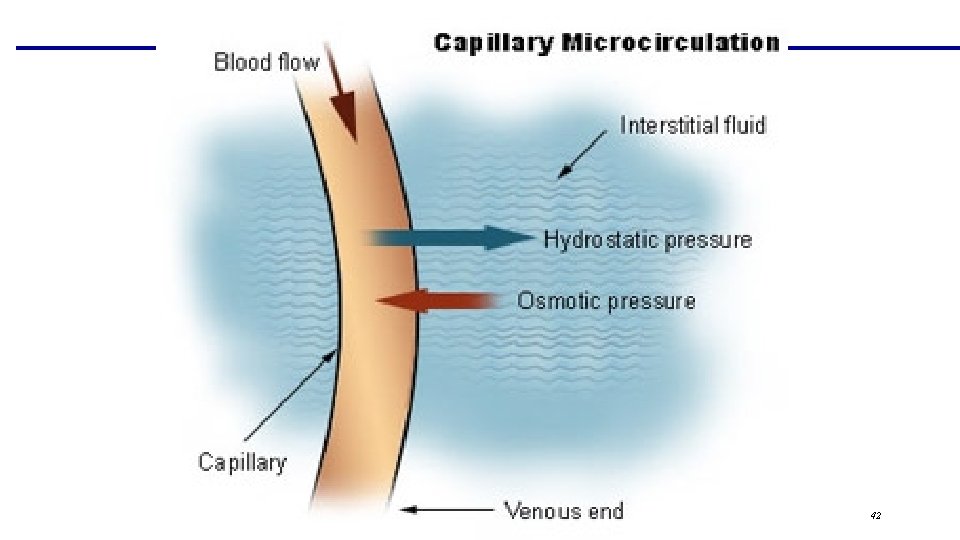
Methods of Capillary Exchange § Bulk flow § Passive transport due to opposing pressures § Faster than diffusion § Function: regulate fluid volume of IVF & ISF § Move large amounts in one direction (at a time) § Hydrostatic pressure § Pressure exerted by IVF & ISF on capillary walls § Colloidal osmotic pressure § Pressure exerted by the non-diffusible solutes on the capillary walls Chapter 19, Cardiovascular System - Blood Vessel 10

Methods of Capillary Exchange § Filtration § Requires positive difference between hydrostatic pressure & colloidal osmotic pressure § Moves fluid from IVF into ISF § Reabsorption § Requires negative difference between hydrostatic pressure & colloidal osmotic pressure § Moves fluid from ISF into IVF Chapter 19, Cardiovascular System - Blood Vessel 11
Chapter 19, Cardiovascular System - Blood Vessel 12
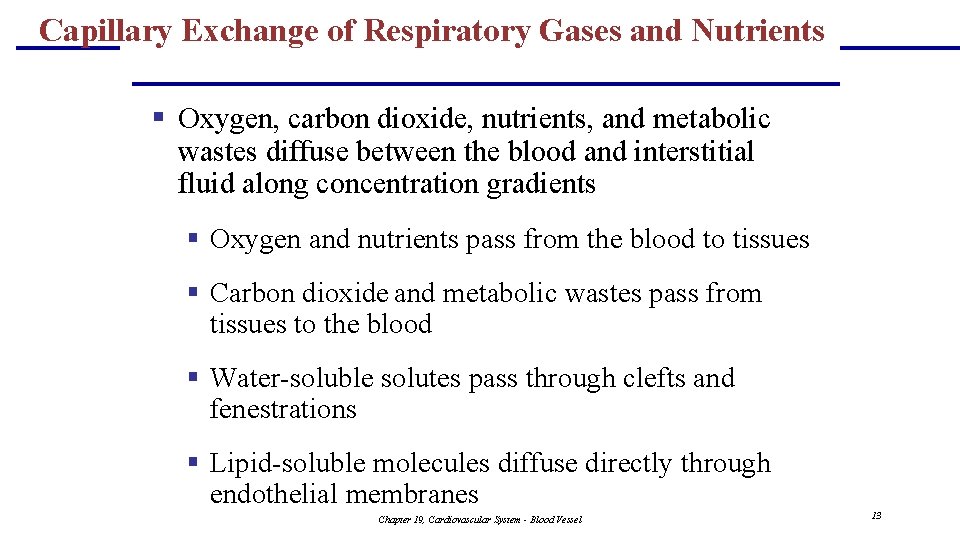
Capillary Exchange of Respiratory Gases and Nutrients § Oxygen, carbon dioxide, nutrients, and metabolic wastes diffuse between the blood and interstitial fluid along concentration gradients § Oxygen and nutrients pass from the blood to tissues § Carbon dioxide and metabolic wastes pass from tissues to the blood § Water-soluble solutes pass through clefts and fenestrations § Lipid-soluble molecules diffuse directly through endothelial membranes Chapter 19, Cardiovascular System - Blood Vessel 13
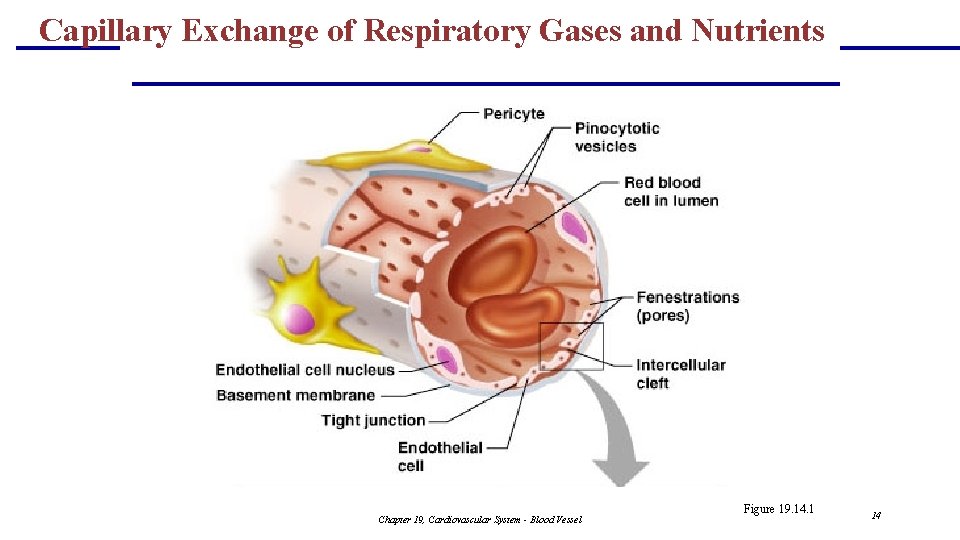
Capillary Exchange of Respiratory Gases and Nutrients Chapter 19, Cardiovascular System - Blood Vessel Figure 19. 14. 1 14
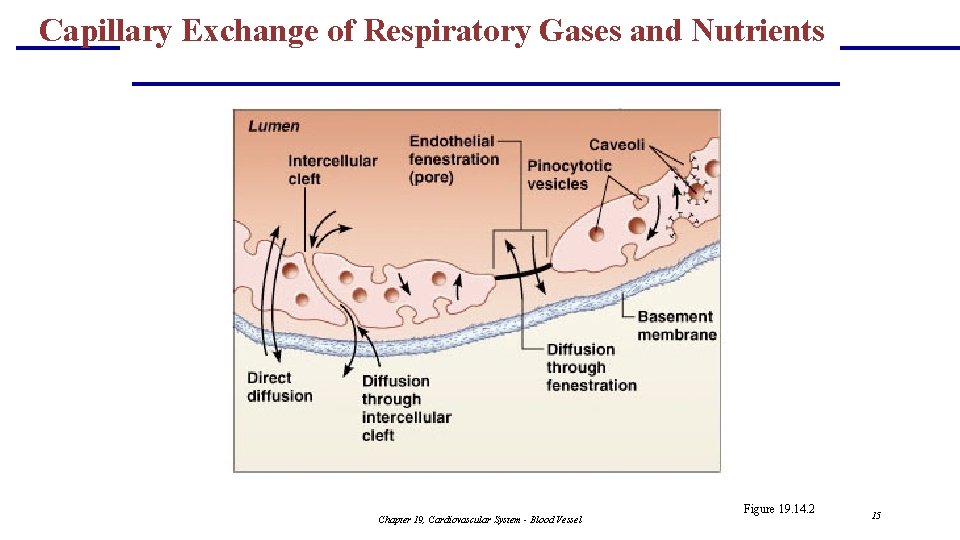
Capillary Exchange of Respiratory Gases and Nutrients Chapter 19, Cardiovascular System - Blood Vessel Figure 19. 14. 2 15
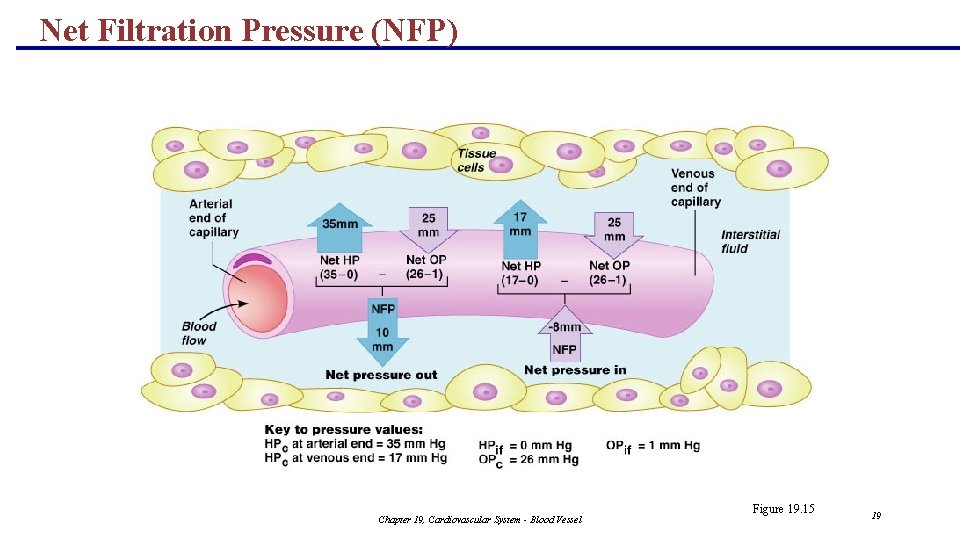
Capillary Exchange: Fluid Movements § Direction and amount of fluid flow depends upon the difference between: § Capillary hydrostatic pressure (HPc) § Capillary colloid osmotic pressure (OPc) § HPc – pressure of blood against the capillary walls: § Tends to force fluids through the capillary walls § Is greater at the arterial end of a bed than at the venule end § OPc– created by nondiffusible plasma proteins, which draw water toward themselves Chapter 19, Cardiovascular System - Blood Vessel 16
Net Filtration Pressure (NFP) § NFP – considers all the forces acting on a capillary bed § NFP = (HPc – HPif) – (OPc – OPif) § At the arterial end of a bed, hydrostatic forces dominate (fluids flow out) Chapter 19, Cardiovascular System - Blood Vessel 17
Net Filtration Pressure (NFP) § At the venous end of a bed, osmotic forces dominate (fluids flow in) § More fluids enter the tissue beds than return blood, and the excess fluid is returned to the blood via the lymphatic system PLAY Inter. Active Physiology®: Cardiovascular System: Autoregulation and Capillary Dynamics Chapter 19, Cardiovascular System - Blood Vessel 18
Net Filtration Pressure (NFP) Chapter 19, Cardiovascular System - Blood Vessel Figure 19. 15 19
Circulatory Routes Page 8 of notes Chapter 19, Cardiovascular System - Blood Vessel 20
Circulatory Pathways § The vascular system has two distinct circulations: § Know the pathway of circulation!! § Pulmonary circulation § Right side of heart - short loop that runs from the heart to the lungs and back to the heart § Systemic circulation § Left side of heart - routes blood through a long loop to all parts of the body and returns to the heart Chapter 19, Cardiovascular System - Blood Vessel 21
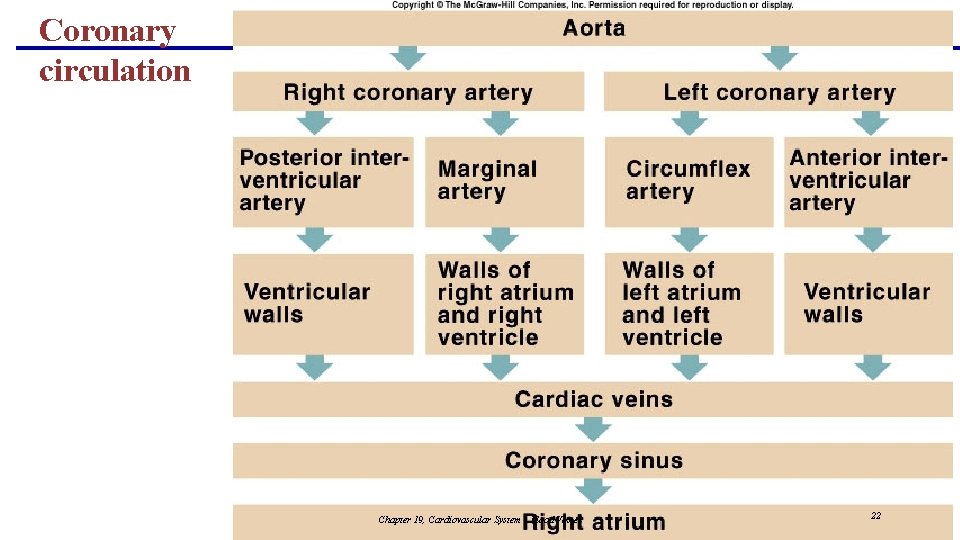
Coronary circulation Chapter 19, Cardiovascular System - Blood Vessel 22
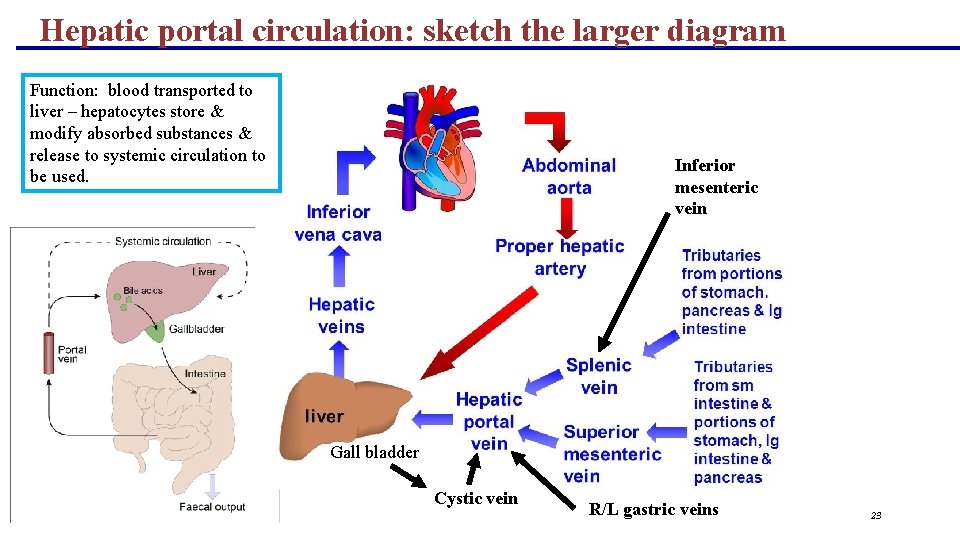
Hepatic portal circulation: sketch the larger diagram Function: blood transported to liver – hepatocytes store & modify absorbed substances & release to systemic circulation to be used. Inferior mesenteric vein Gall bladder Cystic vein R/L gastric veins 23

Hemodynamics Pages 6 -7 of notes Chapter 19, Cardiovascular System - Blood Vessel 24
Blood flow Page 6 top Chapter 19, Cardiovascular System - Blood Vessel 25
Blood Flow: top of page 6 § Actual volume of blood flowing through a vessel, an organ, or the entire circulation in a given period: § Is measured in ml per min. § Is equivalent to cardiac output (CO), considering the entire vascular system § Varies widely through individual organs, according to immediate needs Chapter 19, Cardiovascular System - Blood Vessel 26
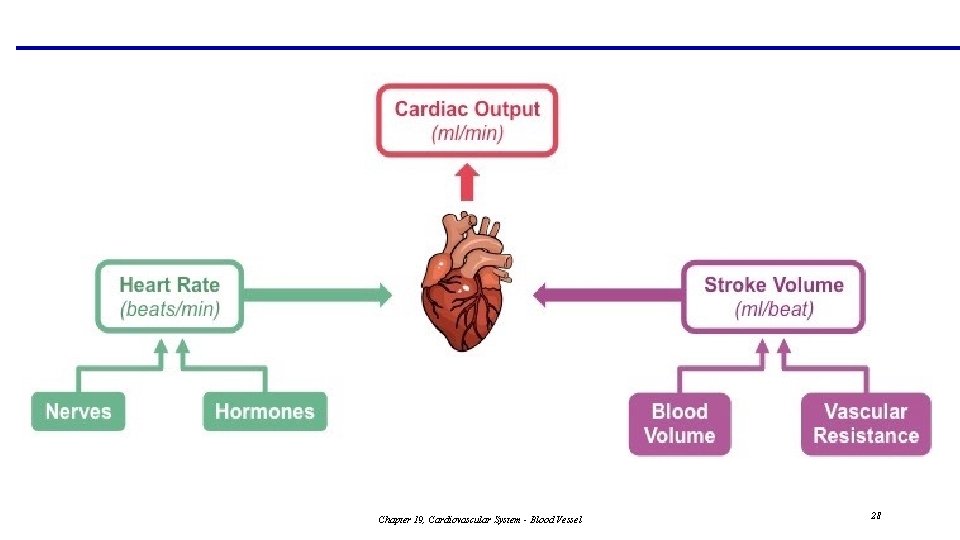
The Heart: Cardiac Output · Cardiac output (CO) · Amount of blood pumped by each ventricle in one minute · CO = (heart rate [HR]) x (stroke volume [SV]) · Resting values · HR = 75 beats per minute · SV = 70 ml per beat · CO = 5250 ml per minute Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide
Chapter 19, Cardiovascular System - Blood Vessel 28
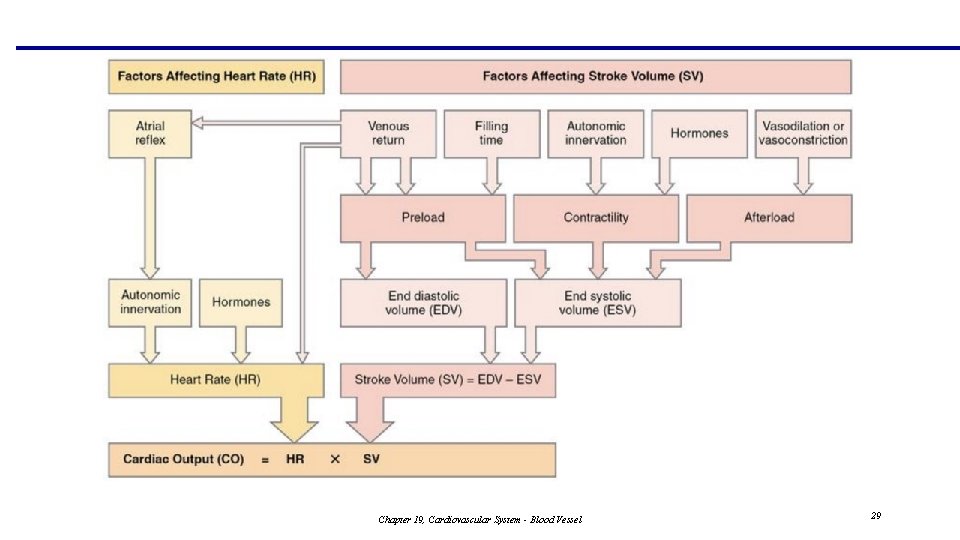
Chapter 19, Cardiovascular System - Blood Vessel 29
Vascular resistance page 7 bottom, page 8 top Chapter 19, Cardiovascular System - Blood Vessel 30
Resistance: bottom of page 7 & top of page 8 § Resistance – opposition to flow § Measure of the amount of friction between blood and the walls of the blood vessels § Most significant in the systemic circuit § Referred to as peripheral resistance (PR) (or vascular resistance) § The three important sources of resistance are blood viscosity, total blood vessel length, and blood vessel lumen diameter Chapter 19, Cardiovascular System - Blood Vessel 31
Resistance Factors: Viscosity and Vessel Length § Resistance factors that remain relatively constant are: § Blood viscosity § Direct relationship § Blood vessel length § Direct relationship Chapter 19, Cardiovascular System - Blood Vessel 32
Resistance Factors: Blood Vessel Diameter § Changes in vessel diameter (esp. arterioles) are frequent and significantly alter peripheral resistance § Resistance varies inversely with the fourth power of vessel radius (onehalf the diameter) § Resistance increases, blood flow decreases: and vice versa. § For example, if the radius is doubled, the resistance is 1/16 as much Chapter 19, Cardiovascular System - Blood Vessel 33
Blood Pressure Back to page 6 Chapter 19, Cardiovascular System - Blood Vessel 34
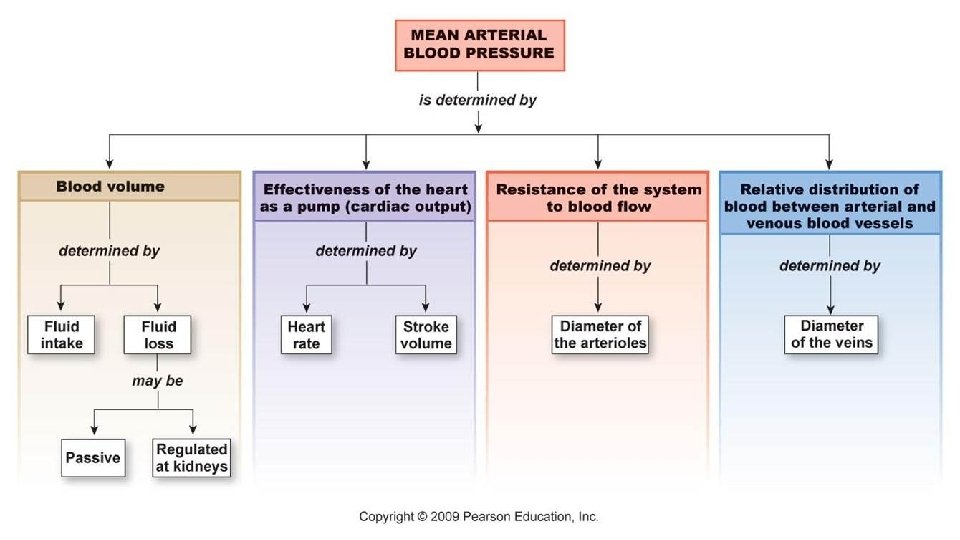
Blood Pressure (BP) § Measured as: Hydrostatic pressure exerted by blood on larger (close to heart) systemic arterial walls during ventricular systole/diastole. § Expressed in millimeters of mercury (mm Hg) § The differences in BP within the vascular system provide the driving force that keeps blood moving from higher to lower pressure areas Chapter 19, Cardiovascular System - Blood Vessel 35
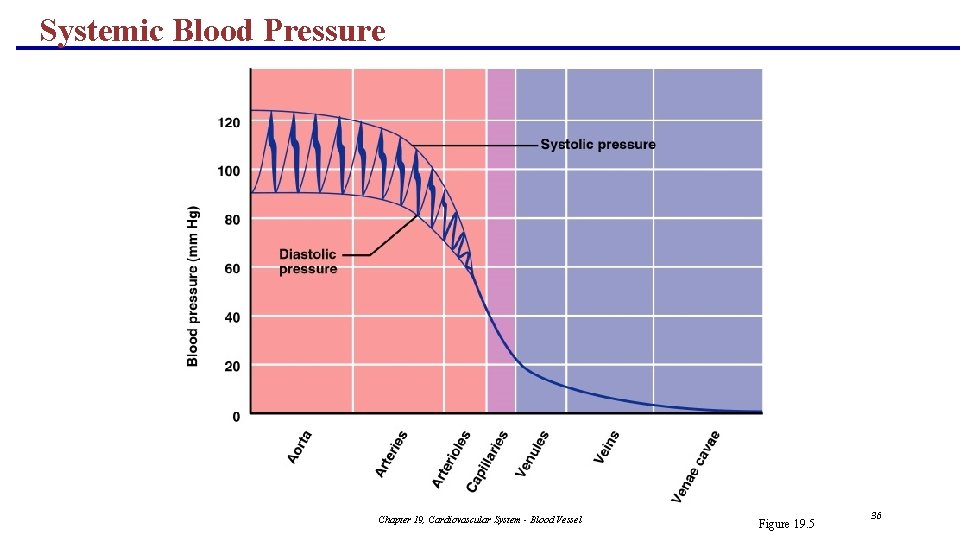
Systemic Blood Pressure Chapter 19, Cardiovascular System - Blood Vessel Figure 19. 5 36

Systemic Blood Pressure § The pumping action of the heart generates blood flow through the vessels along a pressure gradient, always moving from higher- to lower-pressure areas § Pressure results when flow is opposed by resistance § Systemic pressure: § Is highest in the aorta § Declines throughout the length of the pathway § Is 0 mm Hg in the right atrium § The steepest change in blood pressure occurs in the arterioles Chapter 19, Cardiovascular System - Blood Vessel 37
Arterial Blood Pressure § Arterial BP reflects two factors of the arteries close to the heart § Their elasticity (compliance or distensibility) § The amount of blood forced into them at any given time § Blood pressure in elastic arteries near the heart is pulsatile (BP rises and falls) Chapter 19, Cardiovascular System - Blood Vessel 38
Arterial Blood Pressure § Systolic pressure – pressure exerted on arterial walls during ventricular contraction: average = 120 mm. Hg § Diastolic pressure – pressure exerted on arterial walls during ventricular relaxation: average = 80 mm. Hg § Pulse pressure – the difference between systolic and diastolic pressure § SBP-DBP = PP § Mean arterial pressure (MAP) – pressure that propels the blood to the tissues § MAP = DBP + (PP/3) Chapter 19, Cardiovascular System - Blood Vessel 39
Chapter 19, Cardiovascular System - Blood Vessel 40
Capillary Blood Pressure § Capillary BP ranges from 20 to 40 mm Hg § Low capillary pressure is desirable because high BP would rupture fragile, thin-walled capillaries § Low BP is sufficient to force filtrate out into interstitial space and distribute nutrients, gases, and hormones between blood and tissues Chapter 19, Cardiovascular System - Blood Vessel 41
Chapter 19, Cardiovascular System - Blood Vessel 42
Venous Blood Pressure § Venous BP is steady and changes little during the cardiac cycle § The pressure gradient in the venous system is only about 20 mm Hg § A cut vein has even blood flow; a lacerated artery flows in spurts Chapter 19, Cardiovascular System - Blood Vessel 43
Factors Aiding Venous Return § Venous BP alone is too low to promote adequate blood return and is aided by the: § Respiratory “pump” – pressure changes created during breathing suck blood toward the heart by squeezing local veins § Muscular “pump” – contraction of skeletal muscles “milk” blood toward the heart § Valves prevent backflow during venous return § SNS control – contraction of smooth muscle in tunica media causing vasocontriction PLAY Inter. Active Physiology®: Cardiovascular System: Anatomy Review: Blood Vessel Structure and Function Chapter 19, Cardiovascular System - Blood Vessel 44
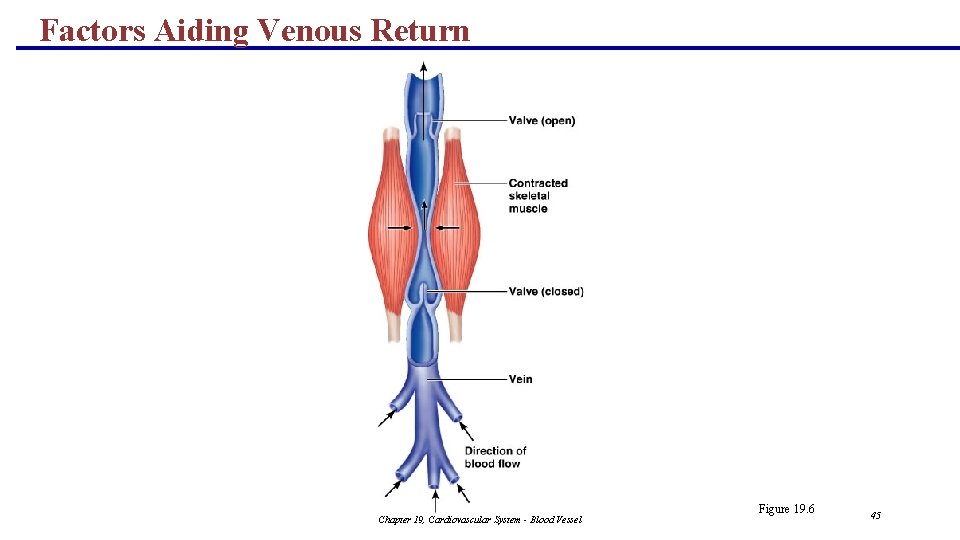
Factors Aiding Venous Return Chapter 19, Cardiovascular System - Blood Vessel Figure 19. 6 45
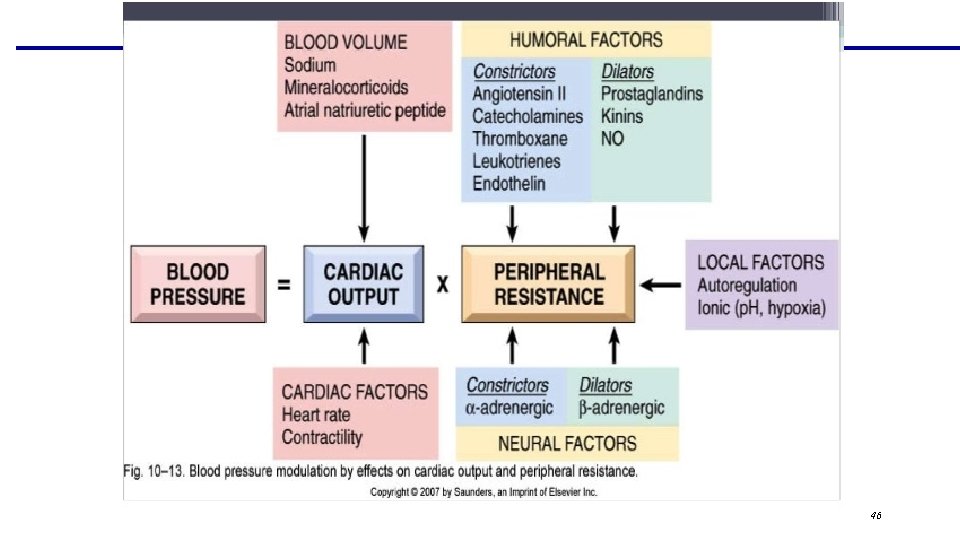
Chapter 19, Cardiovascular System - Blood Vessel 46
SUMMARY: Blood Flow, Blood Pressure, and Resistance § Blood flow (F) is directly proportional to the difference in blood pressure ( P) between two points in the circulation § If P increases, blood flow speeds up; if P decreases, blood flow declines § Blood flow is inversely proportional to resistance (R) § If R increases, blood flow decreases § R is more important than P in influencing local blood pressure Chapter 19, Cardiovascular System - Blood Vessel 47
Examples of factors that affect Cardiovascular system Do not need to memorize Chapter 19, Cardiovascular System - Blood Vessel 48
Heart Regulation § Ions § Calcium § Hypocalcemia – depresses heart – stops beating § Hypercalcemia – excites heart – prolonged contraction with force heart rigor (cramp) § Sodium § Hypernatremia – blocks calcium causing hypocalcemia
Heart Regulation § Potassium § Hyperkalemia – prevents depolarization – heart becomes less active then stops (heart block/cardiac arrest) § Hypokalemia – feeble heart rate and arrhythmias – affects SA node directly
Physical Factors § Age § Fetal rate vs adult § 150 vs. 75 § Due to difference in metabolic rate § Gender § Men have slightly lower due to hormones § Exercise § Fit have lower than nonfit due to efficiency of heart muscle contractions § Body Temperature § Hotter has faster rate due to increase in metabolic rate
- Slides: 51