Chapter 13 Cardiovascular Alterations Copyright 2017 Elsevier Inc








- Slides: 125
Chapter 13 Cardiovascular Alterations Copyright © 2017 Elsevier Inc. All rights reserved.
Normal Structure Heart Mediastinal space Ø Covered by pericardium Ø Composed of three layers Epicardium Ø Myocardium Ø Endocardium Ø Copyright © 2017 Elsevier Inc. All rights reserved. 2
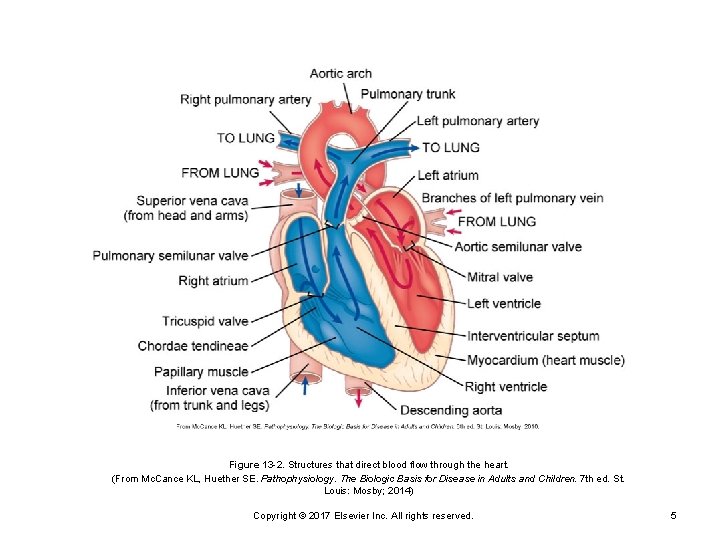
Normal Structure (Cont. ) Right side is low pressure Left side is high pressure Flow of blood Cardiac valves Copyright © 2017 Elsevier Inc. All rights reserved. 3
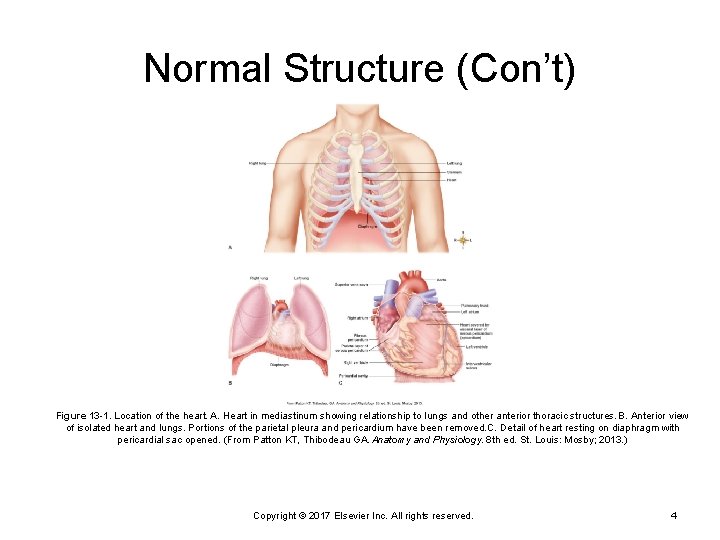
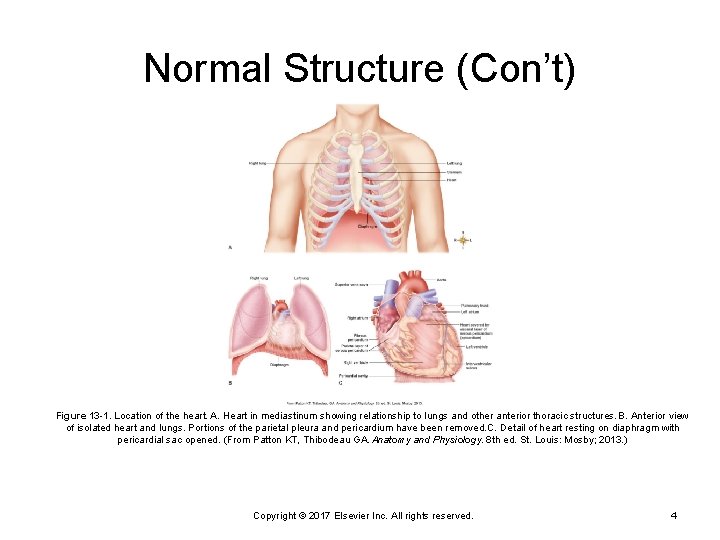
Normal Structure (Con’t) Figure 13 -1. Location of the heart. A. Heart in mediastinum showing relationship to lungs and other anterior thoracic structures. B. Anterior view of isolated heart and lungs. Portions of the parietal pleura and pericardium have been removed. C. Detail of heart resting on diaphragm with pericardial sac opened. (From Patton KT, Thibodeau GA. Anatomy and Physiology. 8 th ed. St. Louis: Mosby; 2013. ) Copyright © 2017 Elsevier Inc. All rights reserved. 4
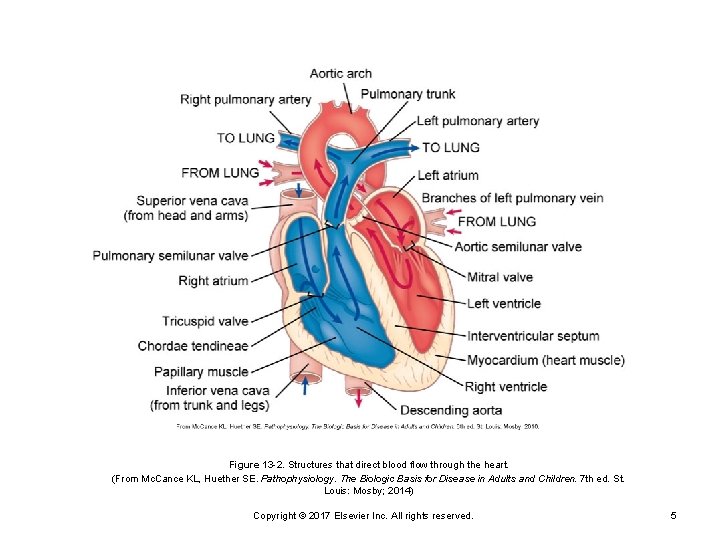
Figure 13 -2. Structures that direct blood flow through the heart. (From Mc. Cance KL, Huether SE. Pathophysiology. The Biologic Basis for Disease in Adults and Children. 7 th ed. St. Louis: Mosby; 2014) Copyright © 2017 Elsevier Inc. All rights reserved. 5
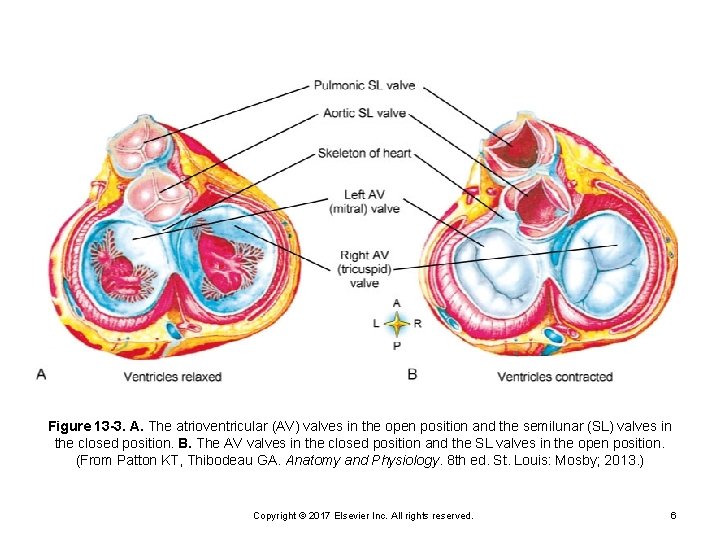
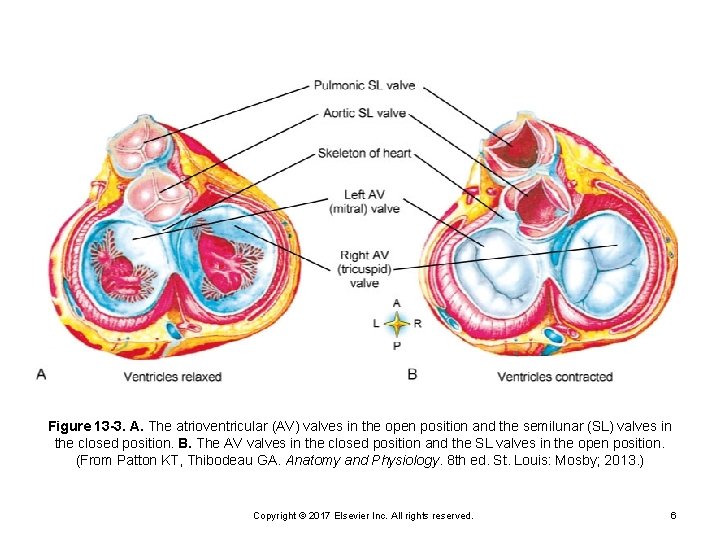
Figure 13 -3. A. The atrioventricular (AV) valves in the open position and the semilunar (SL) valves in the closed position. B. The AV valves in the closed position and the SL valves in the open position. (From Patton KT, Thibodeau GA. Anatomy and Physiology. 8 th ed. St. Louis: Mosby; 2013. ) Copyright © 2017 Elsevier Inc. All rights reserved. 6
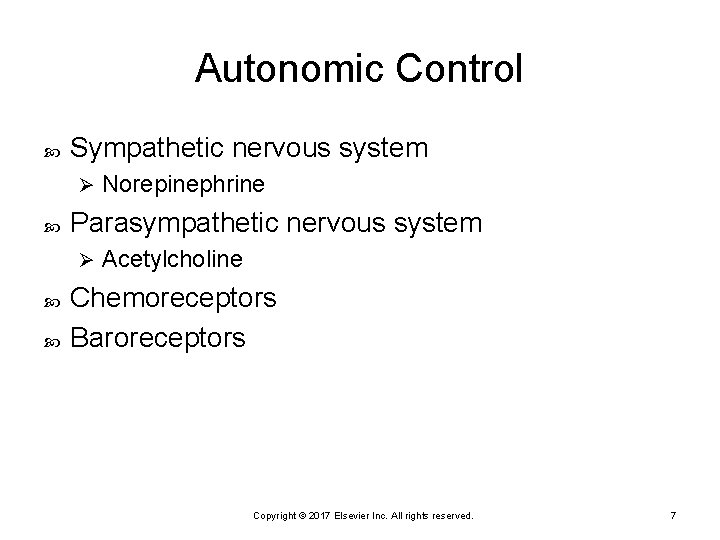
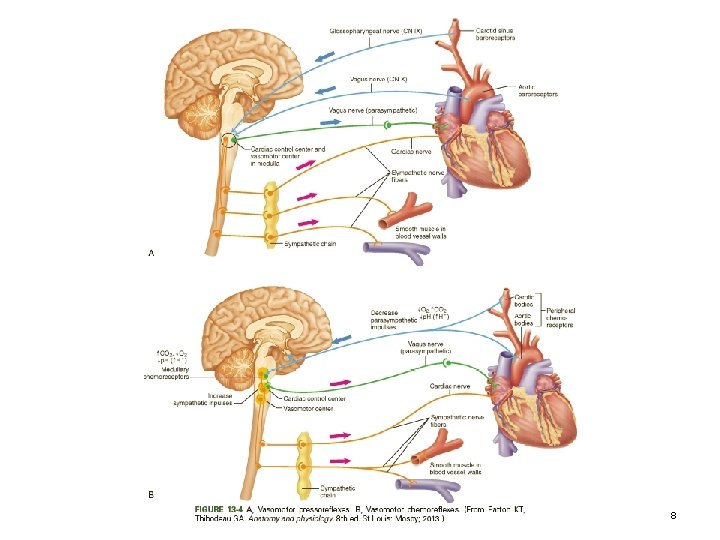
Autonomic Control Sympathetic nervous system Ø Parasympathetic nervous system Ø Norepinephrine Acetylcholine Chemoreceptors Baroreceptors Copyright © 2017 Elsevier Inc. All rights reserved. 7
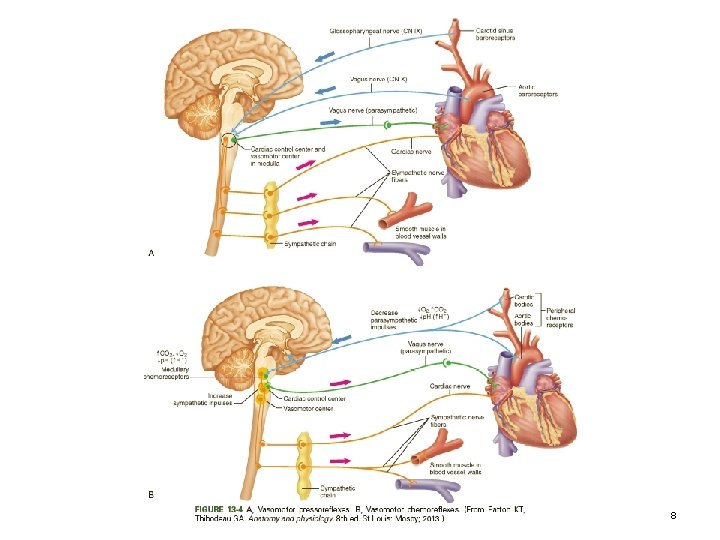
Copyright © 2017 Elsevier Inc. All rights reserved. 8
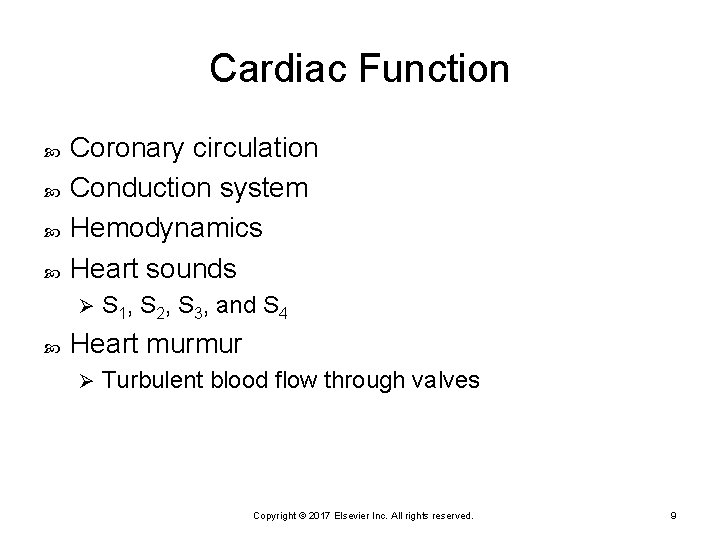
Cardiac Function Coronary circulation Conduction system Hemodynamics Heart sounds Ø S 1, S 2, S 3, and S 4 Heart murmur Ø Turbulent blood flow through valves Copyright © 2017 Elsevier Inc. All rights reserved. 9
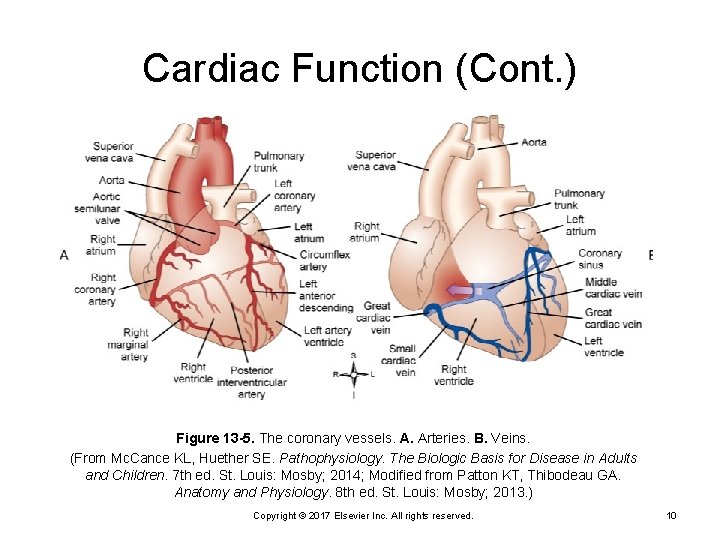
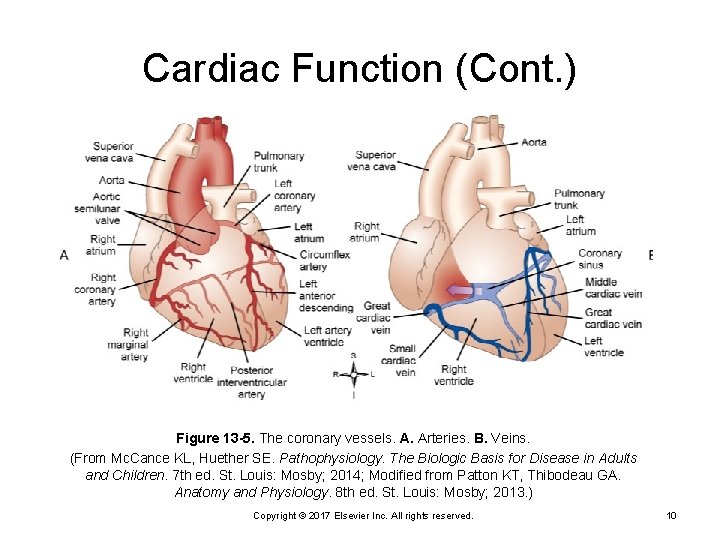
Cardiac Function (Cont. ) Figure 13 -5. The coronary vessels. A. Arteries. B. Veins. (From Mc. Cance KL, Huether SE. Pathophysiology. The Biologic Basis for Disease in Adults and Children. 7 th ed. St. Louis: Mosby; 2014; Modified from Patton KT, Thibodeau GA. Anatomy and Physiology. 8 th ed. St. Louis: Mosby; 2013. ) Copyright © 2017 Elsevier Inc. All rights reserved. 10
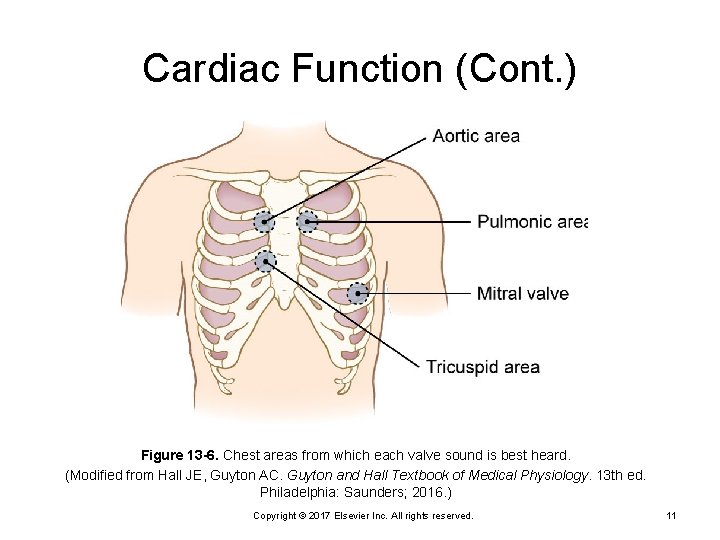
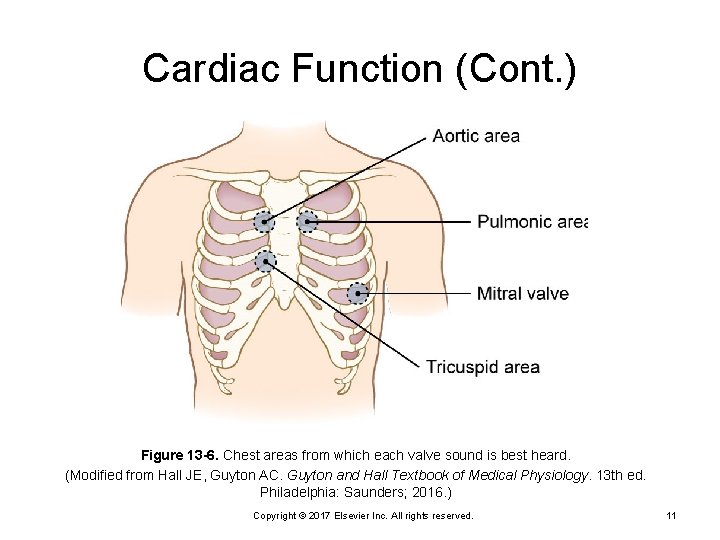
Cardiac Function (Cont. ) Figure 13 -6. Chest areas from which each valve sound is best heard. (Modified from Hall JE, Guyton AC. Guyton and Hall Textbook of Medical Physiology. 13 th ed. Philadelphia: Saunders; 2016. ) Copyright © 2017 Elsevier Inc. All rights reserved. 11
Heart Murmur Caused by a turbulence of blood flow through the valves Rumbling, blowing, harsh, or musical in sound Identify location, sound, loudness, and intensity and whether other heart sounds are heard Copyright © 2017 Elsevier Inc. All rights reserved. 12
Coronary Artery Disease (CAD) Progressive narrowing of coronary arteries by atherosclerosis Coronary heart disease Ø Atherosclerotic heart disease Ø Copyright © 2017 Elsevier Inc. All rights reserved. 13
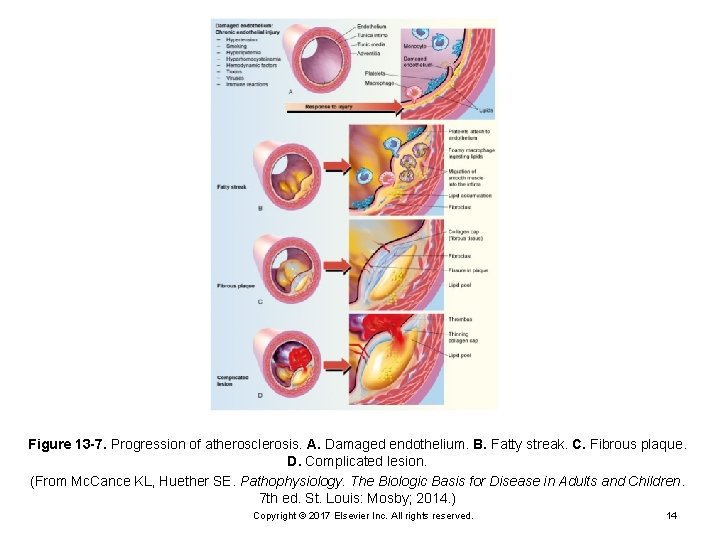
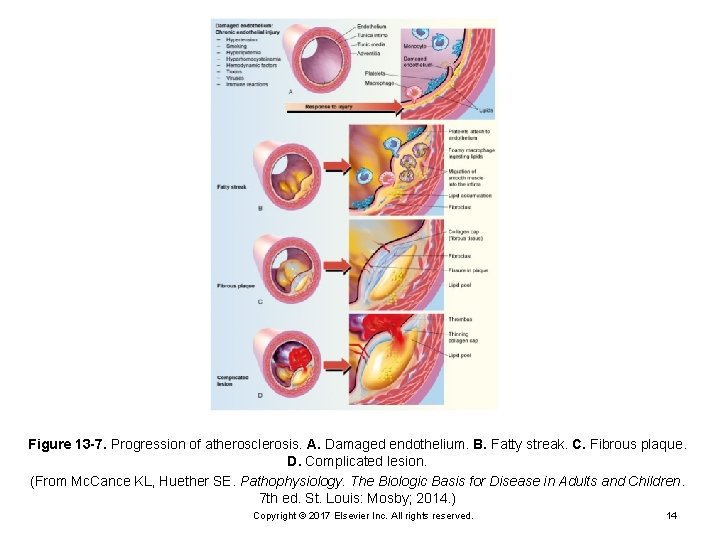
Figure 13 -7. Progression of atherosclerosis. A. Damaged endothelium. B. Fatty streak. C. Fibrous plaque. D. Complicated lesion. (From Mc. Cance KL, Huether SE. Pathophysiology. The Biologic Basis for Disease in Adults and Children. 7 th ed. St. Louis: Mosby; 2014. ) Copyright © 2017 Elsevier Inc. All rights reserved. 14
Pathophysiology of CAD Injury to epithelial cells in intima Platelet aggregation Ø Migration of monocytes Ø Lipoproteins enter intima Ø Fatty streak Monocytes develop into macrophages Ø Lipid-rich "foam cells” develop Ø Atheroma Copyright © 2017 Elsevier Inc. All rights reserved. 15
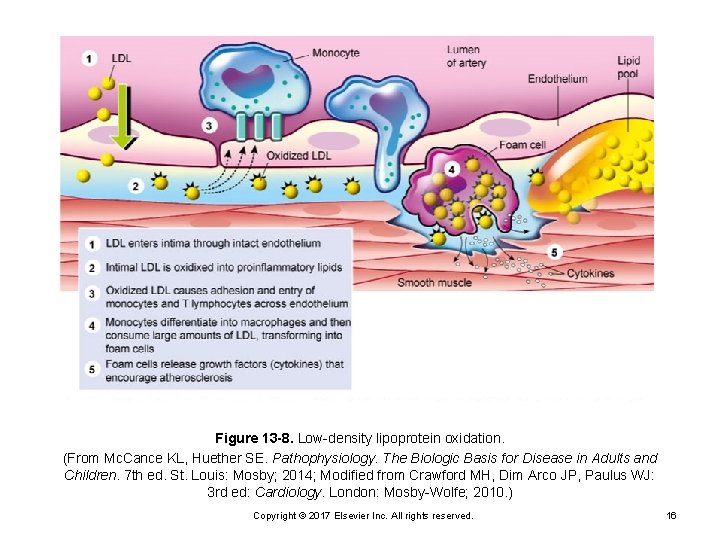
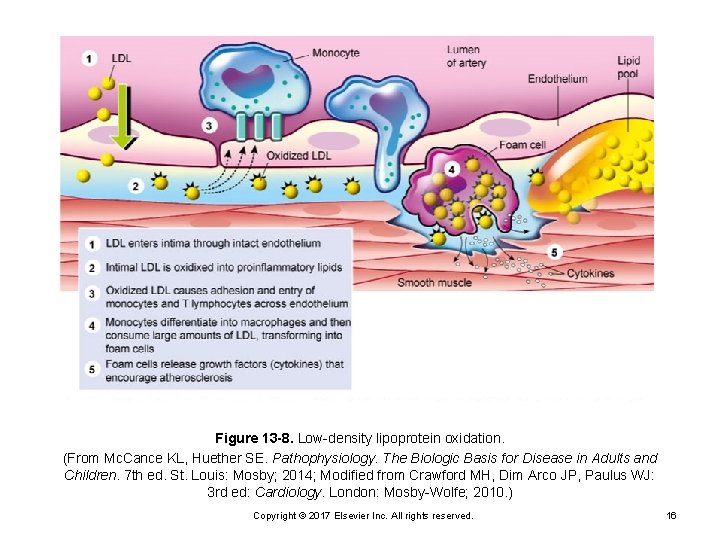
Figure 13 -8. Low-density lipoprotein oxidation. (From Mc. Cance KL, Huether SE. Pathophysiology. The Biologic Basis for Disease in Adults and Children. 7 th ed. St. Louis: Mosby; 2014; Modified from Crawford MH, Dim Arco JP, Paulus WJ: 3 rd ed: Cardiology. London: Mosby-Wolfe; 2010. ) Copyright © 2017 Elsevier Inc. All rights reserved. 16
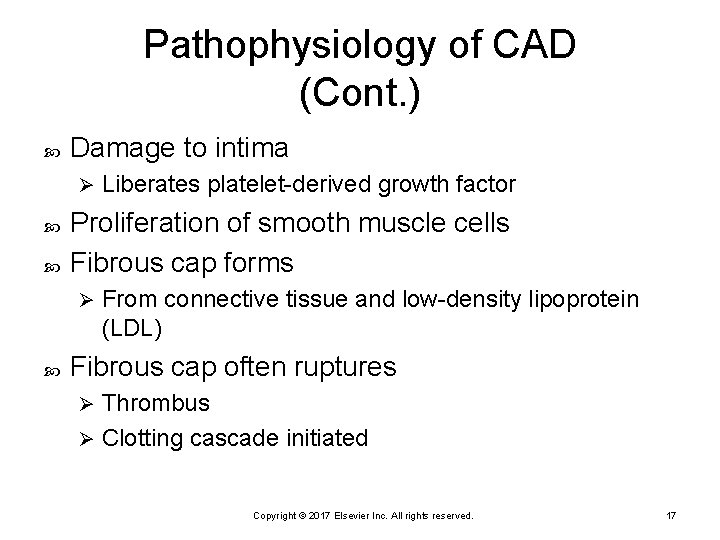
Pathophysiology of CAD (Cont. ) Damage to intima Ø Proliferation of smooth muscle cells Fibrous cap forms Ø Liberates platelet-derived growth factor From connective tissue and low-density lipoprotein (LDL) Fibrous cap often ruptures Thrombus Ø Clotting cascade initiated Ø Copyright © 2017 Elsevier Inc. All rights reserved. 17
Pathophysiology of CAD (Cont. ) Adhesion: platelets bind to receptors Activation: platelets change shape and activate receptors Release: thromboxane A 2 and serotonin Ø Activate glycoprotein IIb/IIIa receptors Ø Aggregation: platelets clump together Drugs administered to stop the process Aspirin Ø Glycoprotein IIb/IIIa inhibitors Ø Copyright © 2017 Elsevier Inc. All rights reserved. 18
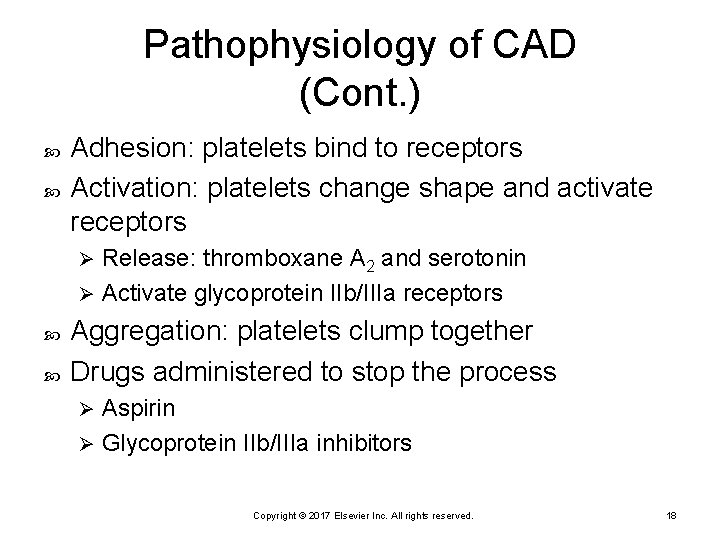
Risk Factors Nonmodifiable factors Age Men > 45 years Ø Women > 55 years Ø Family history Modifiable Smoking Inactivity Overweight Cholesterol High LDL Ø Low levels of HDL Ø Diabetes Hypertension Copyright © 2017 Elsevier Inc. All rights reserved. 19
History Risk factors Prior hospitalizations Shortness of breath, chest pain Medications Ø Erectile dysfunction meds if considering nitroglycerin Psychosocial history Ø Include stressors Copyright © 2017 Elsevier Inc. All rights reserved. 20
Diagnostic Studies 12 -lead electrocardiogram (ECG) Holter monitor Exercise tolerance test (stress test) Exercise to increase demand on heart Ø Stressed via drugs (e. g. , adenosine) if patient cannot tolerate exercise Ø Monitoring vital signs, ECG Ø Pharmacological stress testing Nuclear stress testing Chest x-ray Copyright © 2017 Elsevier Inc. All rights reserved. 21
Diagnostic Studies (Cont. ) Echocardiography Ø Ultrasound to visualize cardiac structures Transesophageal echocardiography Multigated blood pool study (MUGA scan) Copyright © 2017 Elsevier Inc. All rights reserved. 22
Diagnostic Studies (Cont. ) Positron emission tomography (PET scan) Cardiac magnetic resonance imaging Copyright © 2017 Elsevier Inc. All rights reserved. 23
Cardiac Catheterization and Arteriography Electrophysiology study Catheter (right or left) Heart pressures (similar to PA catheter) Ø Cardiac output Ø Arteriography Ø Visualize blood vessels Copyright © 2017 Elsevier Inc. All rights reserved. 24
Post-catheterization Care Bed rest; head of bed no higher than 30 degrees Monitor bleeding; newer collagents for hemostasis may be used Monitor pulses Antiplatelet drugs after the procedure (usually after interventions such as PCI) May be discharged in 6 to 8 hours; depends on diagnosis and procedures done in catheterization laboratory Copyright © 2017 Elsevier Inc. All rights reserved. 25
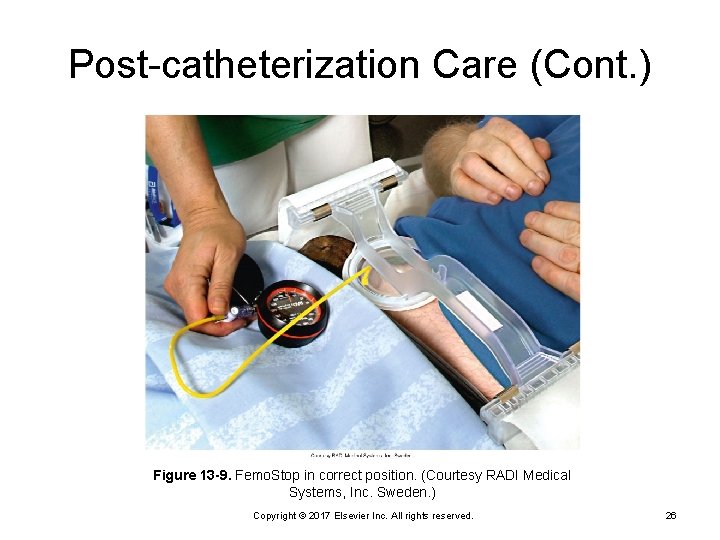
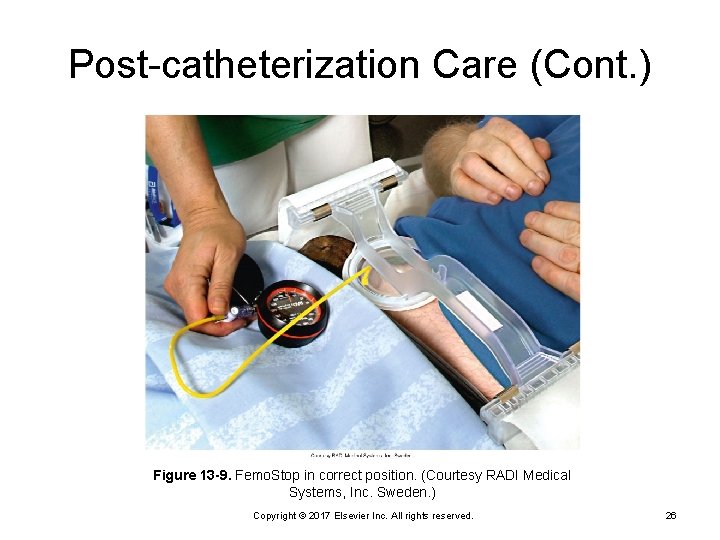
Post-catheterization Care (Cont. ) Figure 13 -9. Femo. Stop in correct position. (Courtesy RADI Medical Systems, Inc. Sweden. ) Copyright © 2017 Elsevier Inc. All rights reserved. 26
Laboratory Tests CBC Hemoglobin Ø Hematocrit Ø Sodium Potassium Calcium Magnesium Copyright © 2017 Elsevier Inc. All rights reserved. 27
Cardiac Enzymes Troponin I and T As early as 1 hour after injury Ø Normal values less than 0. 5 mcg/L for Troponin I Ø Normal values less than 0. 1 mcg/L for Troponin T Ø Copyright © 2017 Elsevier Inc. All rights reserved. 28
Quick Quiz! Which value, when elevated, places the patient at lowest risk for CAD? Triglycerides B. Low-density lipoproteins (LDLs) C. High-density lipoproteins (HDLs) D. Very-low-density lipoproteins (VLDLs) A. Copyright © 2017 Elsevier Inc. All rights reserved. 29
Cholesterol in CAD Categories HDL is considered good Ø LDL is considered bad Ø Copyright © 2017 Elsevier Inc. All rights reserved. 30
LDL Target Levels (NIH) No CHD and fewer than two risk factors o No CHD and two or more risk factors o 160 mg/d. L 130 mg/d. L CAD o <100 mg/d. L Copyright © 2017 Elsevier Inc. All rights reserved. 31
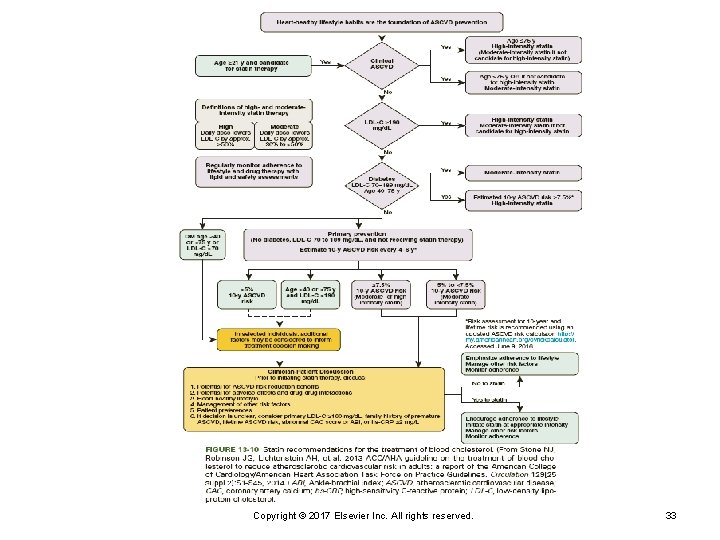
Treatment Diet: low cholesterol, low salt Exercise: aerobic Weight loss Smoking cessation Management of hypertension and diabetes if present Medications: lipid-lowering agents Ø Various types: weigh advantages and disadvantages of each Copyright © 2017 Elsevier Inc. All rights reserved. 32
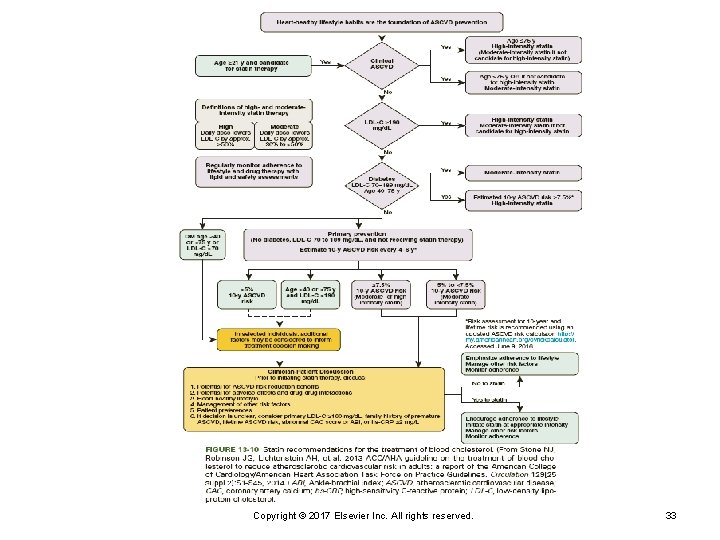
Copyright © 2017 Elsevier Inc. All rights reserved. 33
Medications for Hyperlipidemia HMG-Co. A reductase inhibitors; slow production: most effective Ø Statins Bile acid resins bind are excreted via bowel. Cholestyramine Ø Colestipol Ø Ezetimibe (Zetia) blocks the absorption of cholesterol in the digestive tract. Copyright © 2017 Elsevier Inc. All rights reserved. 34
Medications for Hyperlipidemia (Cont. ) Nicotinic acid; inhibits LDL synthesis and increases HDL; many side effects Fibric acid derivatives; increase VLDL clearance Ø Gemfibrozil Copyright © 2017 Elsevier Inc. All rights reserved. 35
Medications for Hyperlipidemia (Cont. ) Patients carefully monitored Combination therapy may be needed to reach target goals Copyright © 2017 Elsevier Inc. All rights reserved. 36
Medications Affecting Platelets ASA (inhibits thromboxane A 2) Others: dipyridamole, ticlopidine, and clopidogrel Copyright © 2017 Elsevier Inc. All rights reserved. 37
Types of Angina Stable (chronic, exertional) = effort, classic T-wave inversion on ECG Ø Treatment: rest and nitroglycerin Ø Unstable (crescendo) = more often and more severe, less relief May see ST elevation on ECG Ø Treatment: rest and nitroglycerin; drugs affecting platelets; revascularization Ø Variant = Prinzmetal’s (vasospasms) ST elevation during pain episodes Ø Treatment: calcium channel blockers Ø Copyright © 2017 Elsevier Inc. All rights reserved. 38
Angina Myocardial ischemia: the heart’s demand for oxygen is higher than the supply Copyright © 2017 Elsevier Inc. All rights reserved. 39
Angina/Chest Pain Classic symptom Often midsternal May radiate to arms, jaw, or back ECG changes to the ST segment/T wave Copyright © 2017 Elsevier Inc. All rights reserved. 40
Case Study Mr. and Mrs. T. are naturalized Americans. They were born and raised in Japan and moved to the United States 20 years ago. Mrs. T. is 45 and teaches kindergarten. Mr. T. is 54 and runs an import store. Their son, Rutchie, 16 years old, was born in the United States. He is a sophomore in high school, where he plays baseball. Mr. T. started having some chest pains 2 years ago and was diagnosed at the clinic with mild angina. He takes nitroglycerin (NTG) 0. 3 mg SL when he feels any discomfort. His chest pain is usually exertion related. Lately, he has had to take the NTG more often. He has an appointment with the cardiologist next week. Copyright © 2017 Elsevier Inc. All rights reserved. 41
Questions Why is Mr. T. experiencing more pain? What could be done at this point to prevent an MI? Copyright © 2017 Elsevier Inc. All rights reserved. 42
Nursing Diagnoses Acute chest pain related to myocardial ischemia Knowledge deficit related to unfamiliarity with disease processes and treatment Activity intolerance related to ischemic changes Copyright © 2017 Elsevier Inc. All rights reserved. 43
Nursing Management: Angina Maintain cardiac output Pain relief Self-care; risk-factor modification Medications Postprocedure observation and care following cardiac catheterization, angioplasty, bypass surgery. Copyright © 2017 Elsevier Inc. All rights reserved. 44
Patient Care Outcomes The patient will verbalize relief of chest discomfort, appear relaxed and comfortable, verbalize an understanding of angina pectoris and its management, describe cardiac risk factors and strategies to reduce them, and perform activities within limits of the disease, as evidenced by absence of chest pain or discomfort and no ECG changes reflecting ischemia. Copyright © 2017 Elsevier Inc. All rights reserved. 45
Quick Quiz! Nursing management of the patient with angina is directed toward A. immediate administration of nitrates. B. assessment of history of previous anginal episodes. C. assessment and documentation of chest pain episodes. D. administration of prophylactic lidocaine for ventricular ectopy. Copyright © 2017 Elsevier Inc. All rights reserved. 46
Acute Coronary Syndrome (ACS) Ischemia with myocardial cell death Imbalance of oxygen supply and demand Includes stable angina, unstable angina or acute myocardial infarction Causes Atherosclerosis Ø Emboli Ø Blunt trauma Ø Spasm Ø Copyright © 2017 Elsevier Inc. All rights reserved. 47
Acute Myocardial Infarction (AMI) Types Non-ST segment elevation (NSTEMI) Ø ST segment elevation (STEMI) Ø Collateral circulation Copyright © 2017 Elsevier Inc. All rights reserved. 48
Assessment of AMI Midsternal chest pain Ø Severe, crushing, and squeezing pressure Ø May radiate Ø Unrelieved with nitrates Pale and diaphoretic Dyspnea, tachypnea, and/or hypotension Syncope Feeling of impending doom Nausea and vomiting Dysrhythmias Copyright © 2017 Elsevier Inc. All rights reserved. 49
Diagnosis of AMI Signs and symptoms Ø Often atypical symptoms in women 12 -lead: ST elevation followed by Q wave (Q-wave myocardial infarction) Ø ST depression (non–Q-wave myocardial infarction) Ø Elevated serum troponin Troponin I Ø Troponin T Ø Copyright © 2017 Elsevier Inc. All rights reserved. 50
Case Study The paramedics put an oxygen cannula on Mr. T. and start an IV in his left arm. They give him a baby aspirin to chew, contact the local hospital, and prepare Mr. T. for transport. Upon arrival in the ED, Mr. T. ’s heart rate is 110 beats/min, and he is diaphoretic. What is the danger of the tachycardia? Copyright © 2017 Elsevier Inc. All rights reserved. 51
Question A 12 -lead ECG is done by the paramedic in the field. What changes would you expect to see if Mr. T. is having an MI? Copyright © 2017 Elsevier Inc. All rights reserved. 52
Question (Cont. ) The paramedics note ST-segment elevation in Leads II, III, and a. VF. What therapies will be administered in the field? In what area of the heart do changes in these leads indicate damage? Copyright © 2017 Elsevier Inc. All rights reserved. 53
Quick Quiz! Which finding on the ECG is most conclusive for infarction? Q waves B. Inverted T waves C. Tall, peaked T waves D. ST-segment depression A. Copyright © 2017 Elsevier Inc. All rights reserved. 54
Nursing Diagnoses Acute Chest Pain Poor Tissue Perfusion Copyright © 2017 Elsevier Inc. All rights reserved. 55
Nursing Goals: AMI Maintain cardiac output Treat pain Assess for complications Increase activity tolerance Relieve anxiety Ongoing and discharge teaching Copyright © 2017 Elsevier Inc. All rights reserved. 56
Medical Management: AMI Pain relief: morphine, nitroglycerin Oxygen Prevention of platelet aggregation Percutaneous Coronary Intervention (PCI) Fibrinolytic therapy Medications (nitrates, beta blockers, angiotensinconverting enzyme inhibitors Autologous bone marrow stem cell treatment to the damaged myocardium. Copyright © 2017 Elsevier Inc. All rights reserved. 57
Complications of AMI Dysrhythmias Sudden death Heart failure Cardiogenic shock Ventricular aneurysm or rupture Papillary muscle dysfunction Pericarditis Infarct extension Copyright © 2017 Elsevier Inc. All rights reserved. 58
Quick Quiz! After giving the first dose of morphine to relieve the chest pain of a critical care patient, the next priority action is to A. change the intravenous tubing to maintain a patent infusion line and reduce risk of infection. B. bathe patient while the analgesic is still in effect. C. assess the patient for pain relief and signs of any adverse effects of the medication. D. initiate administration of oxygen by nasal cannula. Copyright © 2017 Elsevier Inc. All rights reserved. 59
Primary Angioplasty Get patient to catheterization lab for emergent percutaneous intervention or stenting if facilities are available Better outcomes than thrombolytics Copyright © 2017 Elsevier Inc. All rights reserved. 60
Thrombolytic Therapy Time is muscle; 6 -hour window Several thrombolytic agents available, such as: Tissue plasminogen activator (t-PA) Ø Streptokinase Ø Reteplase Ø Heparin and glycoprotein IIb/IIIa inhibitors Copyright © 2017 Elsevier Inc. All rights reserved. 61
Case Study Mr. T. was quickly triaged in the ED with a preliminary diagnosis of acute inferior wall MI. The hospital is in a rural area, and the weather is severe. Ground transport to the nearest hospital able to do PCI is 2 hours. Therefore, a decision is made to administer thrombolytics. Within 1 hour, Mr. T. was started on reteplase. Copyright © 2017 Elsevier Inc. All rights reserved. 62
Question Why was Mr. T. treated with thrombolytics rather than transported to the center for a PCI? Copyright © 2017 Elsevier Inc. All rights reserved. 63
Question (Cont. ) Because Mr. T. is having an inferior wall MI, what complications should be anticipated while getting him ready for the thrombolytic therapy? Copyright © 2017 Elsevier Inc. All rights reserved. 64
Questions What nursing care was done prior to starting reteplase? What is the nursing care associated with a patient receiving reteplase? What complications must be assessed during and after administration of the medication? Copyright © 2017 Elsevier Inc. All rights reserved. 65
Interventional Cardiology Variety of procedures Percutaneous transluminal coronary angioplasty (PTCA) Ø Intracoronary stenting • Drug-eluting stents Ø Copyright © 2017 Elsevier Inc. All rights reserved. 66
PTCA Goal to increase blood flow to myocardium Criteria Uncompromised collateral flow Ø Noncalcified lesions Ø Lesions not on bifurcations of vessels Ø Balloon catheter is inflated Copyright © 2017 Elsevier Inc. All rights reserved. 67
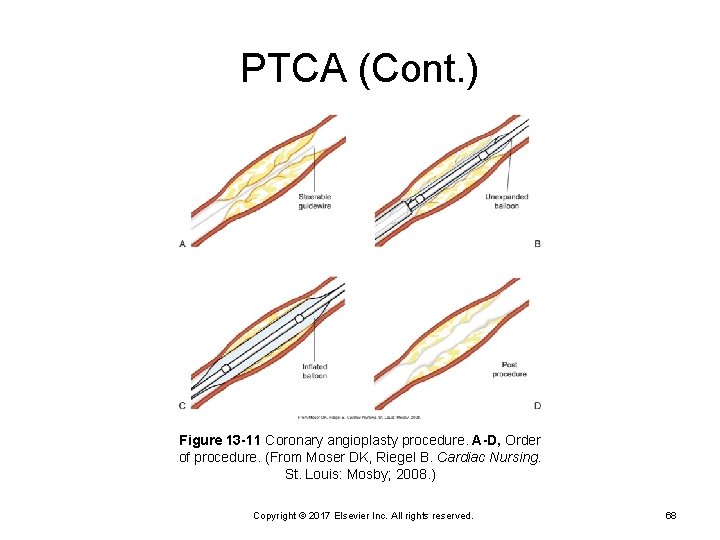
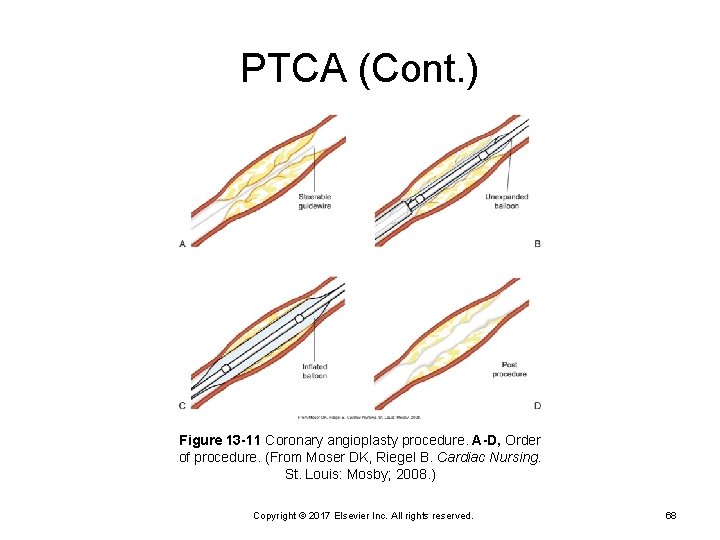
PTCA (Cont. ) Figure 13 -11 Coronary angioplasty procedure. A-D, Order of procedure. (From Moser DK, Riegel B. Cardiac Nursing. St. Louis: Mosby; 2008. ) Copyright © 2017 Elsevier Inc. All rights reserved. 68
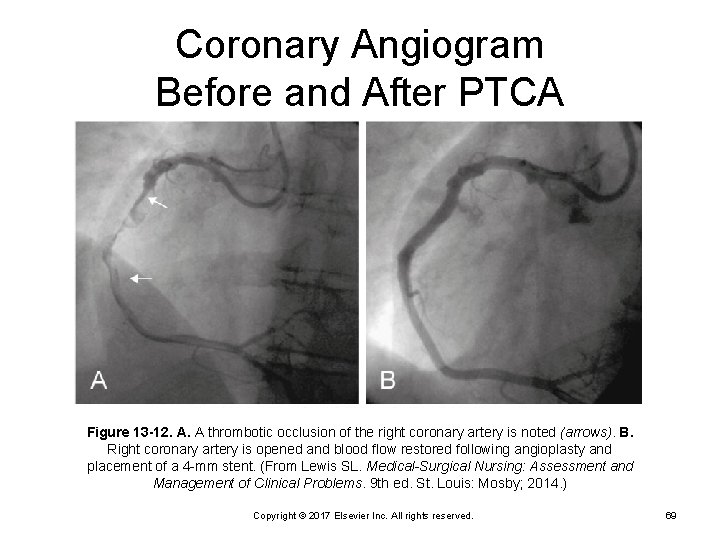
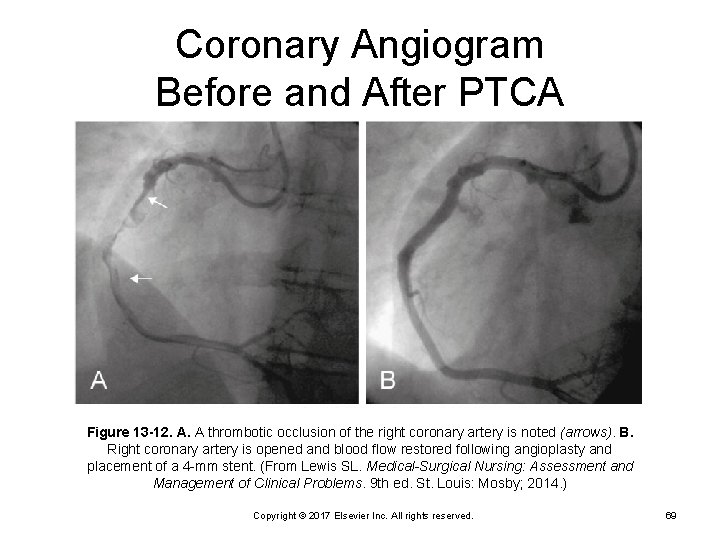
Coronary Angiogram Before and After PTCA Figure 13 -12. A. A thrombotic occlusion of the right coronary artery is noted (arrows). B. Right coronary artery is opened and blood flow restored following angioplasty and placement of a 4 -mm stent. (From Lewis SL. Medical-Surgical Nursing: Assessment and Management of Clinical Problems. 9 th ed. St. Louis: Mosby; 2014. ) Copyright © 2017 Elsevier Inc. All rights reserved. 69
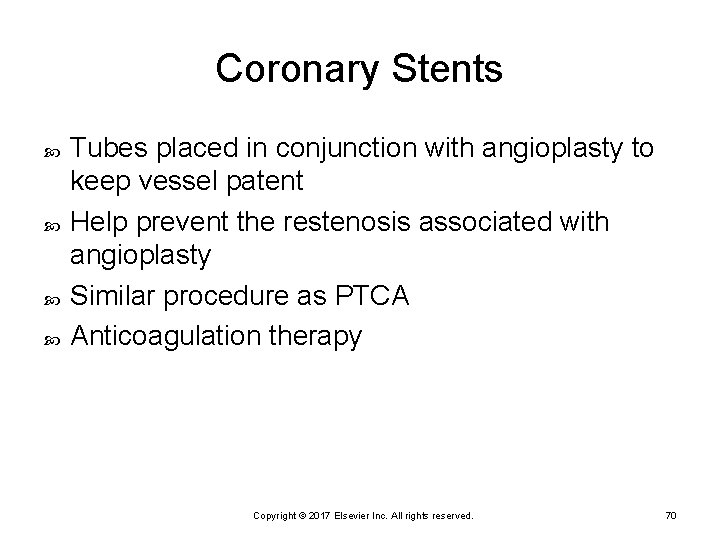
Coronary Stents Tubes placed in conjunction with angioplasty to keep vessel patent Help prevent the restenosis associated with angioplasty Similar procedure as PTCA Anticoagulation therapy Copyright © 2017 Elsevier Inc. All rights reserved. 70
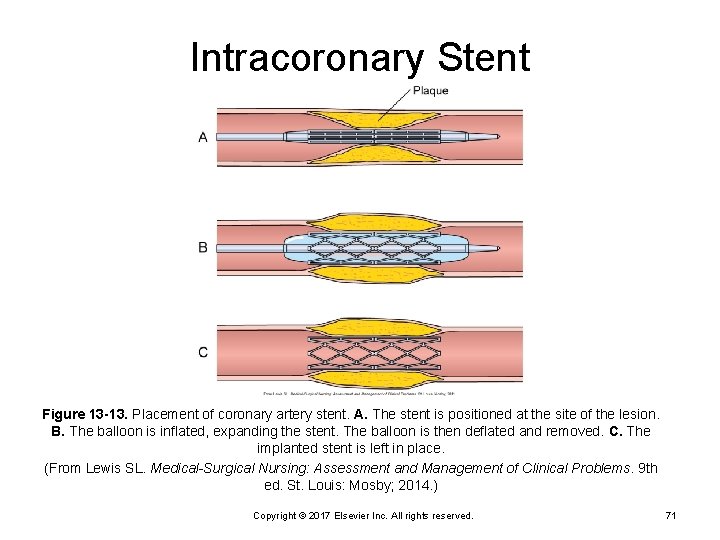
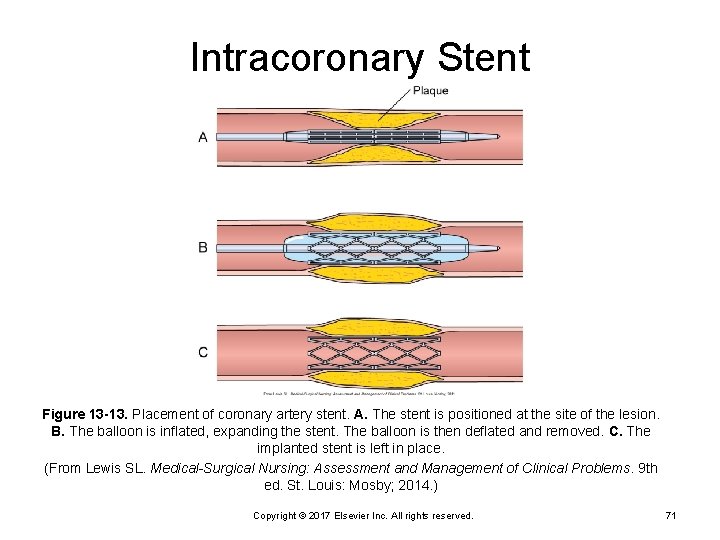
Intracoronary Stent Figure 13 -13. Placement of coronary artery stent. A. The stent is positioned at the site of the lesion. B. The balloon is inflated, expanding the stent. The balloon is then deflated and removed. C. The implanted stent is left in place. (From Lewis SL. Medical-Surgical Nursing: Assessment and Management of Clinical Problems. 9 th ed. St. Louis: Mosby; 2014. ) Copyright © 2017 Elsevier Inc. All rights reserved. 71
Case Study One day after the thrombolytic therapy, Mr. T. ’s cardiac rhythm suddenly dropped to 40 beats/min, and he became very dizzy and breathless. Copyright © 2017 Elsevier Inc. All rights reserved. 72
Questions What action should the nurse take? What drugs could be used? Copyright © 2017 Elsevier Inc. All rights reserved. 73
Case Study/Questions Mr. T. is discharged from the hospital 2 days after the MI. What discharge instructions are needed? What medications will be ordered? What psychosocial support may need to be provided to Mrs. T. and their son, Rutchie? Copyright © 2017 Elsevier Inc. All rights reserved. 74
Surgical Revascularization Coronary artery bypass graft (CABG) surgery Minimally invasive direct coronary artery bypass (MIDCAB) surgery Transmyocardial revascularization (TMR) Copyright © 2017 Elsevier Inc. All rights reserved. 75
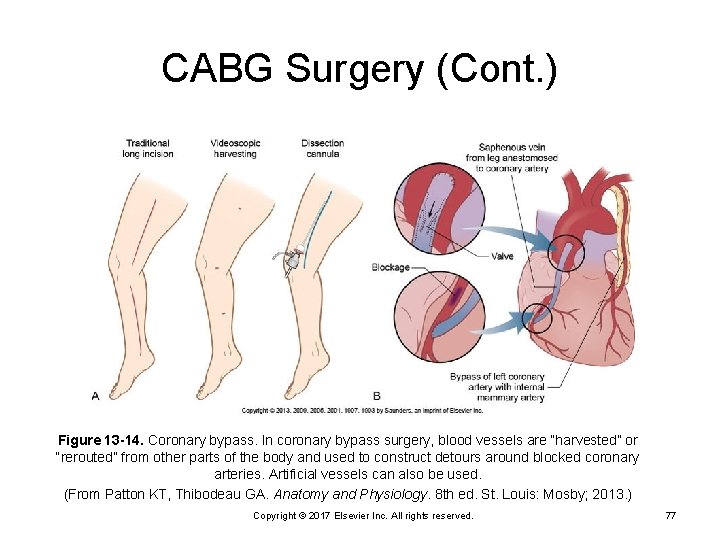
CABG Surgery Provides additional conduits for blood flow Saphenous vein Ø Internal mammary artery Ø Radial artery Ø Arteries longer patency Copyright © 2017 Elsevier Inc. All rights reserved. 76
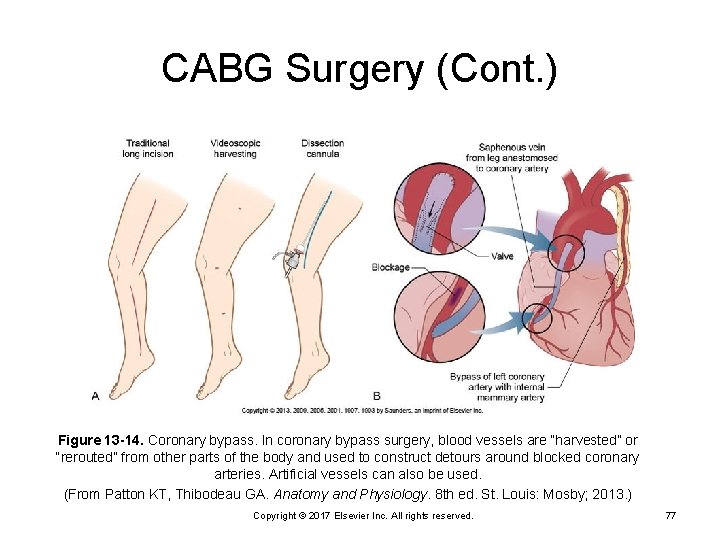
CABG Surgery (Cont. ) Figure 13 -14. Coronary bypass. In coronary bypass surgery, blood vessels are “harvested” or “rerouted” from other parts of the body and used to construct detours around blocked coronary arteries. Artificial vessels can also be used. (From Patton KT, Thibodeau GA. Anatomy and Physiology. 8 th ed. St. Louis: Mosby; 2013. ) Copyright © 2017 Elsevier Inc. All rights reserved. 77
Indications for CABG Unstable angina AMI Failure of percutaneous interventions Copyright © 2017 Elsevier Inc. All rights reserved. 78
Risks Associated with CABG Increased mortality associated with: Left ventricle dysfunction Ø Emergency surgery Ø Age Ø Sex (female) Ø Number of diseased vessels Ø Decreased ejection fraction with congestive heart failure Ø Copyright © 2017 Elsevier Inc. All rights reserved. 79
Traditional CABG Median sternotomy or sternum split Excision of pericardium Cardiopulmonary bypass Myocardial preservation or cardioplegia Copyright © 2017 Elsevier Inc. All rights reserved. 80

Traditional CABG (Cont. ) Grafts Wean bypass; defibrillate if needed Mediastinal and chest tubes Epicardial pacing wires Wire sternum Copyright © 2017 Elsevier Inc. All rights reserved. 81
Goals of CABG Surgery Increase blood flow to myocardium Relieve symptoms Prolong survival Improve quality of life Copyright © 2017 Elsevier Inc. All rights reserved. 82
Minimally Invasive Direct Coronary Artery Bypass Surgery Port-access coronary artery bypass Cardiopulmonary bypass Ø Incisions (ports) Ø Minimally invasive direct coronary artery bypass surgery No cardiopulmonary bypass Ø Heart still beating Ø One or two bypasses Ø Copyright © 2017 Elsevier Inc. All rights reserved. 83
Cardiac Surgery Complications Low cardiac output Renal impairment Ø Gastrointestinal dysfunction Ø Impaired peripheral circulation Ø Mediastinal bleeding Ø Infection: very serious if sternal Atrial dysrhythmias Hypovolemia Copyright © 2017 Elsevier Inc. All rights reserved. 84
Complications of CABG Dysrhythmias Impaired contractility; low cardiac output Intraoperative myocardial infarction Pericardial tamponade Respiratory insufficiency Pain Emboli; stroke AMI Shock Death Copyright © 2017 Elsevier Inc. All rights reserved. 85
Case Study One month after Mr. T. ’s revascularization, he develops chest pain and visits the cardiologist. He is having T-wave changes in the anterior leads. He is referred to the tertiary care center for additional testing. He undergoes cardiac catheterization and angiography, and a lesion of the left main coronary artery is found. He is scheduled for a CABG. Copyright © 2017 Elsevier Inc. All rights reserved. 86
Questions Why is CABG scheduled and not PCI? What are the psychosocial implications of having surgery at a tertiary care center? Copyright © 2017 Elsevier Inc. All rights reserved. 87
Case Study Mr. T. undergoes CABG, and the left internal mammary artery (LIMA) is implanted to the left main coronary artery. Why is the LIMA used? What are the postoperative priorities? Copyright © 2017 Elsevier Inc. All rights reserved. 88
Transmyocardial Revascularization Laser channels into ventricle Goal is to increase perfusion of heart muscle Relief of symptoms occurs over time Poor candidates for CABG Mixed results from clinical trials Copyright © 2017 Elsevier Inc. All rights reserved. 89
Enhanced External Counterpulsation Enhanced external counterpulsation (EECP) is a treatment for angina when the patient is not a candidate for bypass surgery or PCI. EECP uses cuffs wrapped around the patient’s legs to increase arterial blood pressure and retrograde aortic blood flow during diastole. Sequential pressure, using compressed air, is applied from the lower legs to the upper thighs. There are no definite data that EECP reduces ischemia; however, treatment reduces angina and improves quality of life. Copyright © 2017 Elsevier Inc. All rights reserved. 90
Dysrhythmias Radiofrequency catheter ablation Permanent pacemakers Implantable cardioverter-defibrillator Copyright © 2017 Elsevier Inc. All rights reserved. 91
Radiofrequency Catheter Ablation Supraventricular tachycardia Interrupt electrical conduction or activity Radiofrequency used Electrophysiology Copyright © 2017 Elsevier Inc. All rights reserved. 92
Temporary and Permanent Pacemakers Multiprogrammable for: Rate Ø Voltage Ø Sensitivity Ø Stimulus duration Ø Refractory period Ø Intersociety Commission for Heart Disease (ICHD) Copyright © 2017 Elsevier Inc. All rights reserved. 93
Permanent Pacemakers (Cont. ) Can pace atria, ventricles, or dual chamber Inserted transvenously Copyright © 2017 Elsevier Inc. All rights reserved. 94
Implantable Cardioverter. Defibrillator (ICD) Used to treat survivors of sudden cardiac arrest Some have built-in pacemakers Delivers high-energy shock Patient education Emergency procedures Copyright © 2017 Elsevier Inc. All rights reserved. 95

Heart Failure Inability of the heart to generate adequate flow and to meet the metabolic demands of the body Systolic (impaired contractility) Diastolic (impaired filling) Copyright © 2017 Elsevier Inc. All rights reserved. 96
Etiology AMI Hypertension Idiopathic; cardiomyopathy Valvular disease Copyright © 2017 Elsevier Inc. All rights reserved. 97
Pathophysiology Left heart failure Decreased pumping action Ø Failure to meet metabolic demands Ø Backup of blood from left ventricle Ø Fluid buildup in lungs Ø Backflow leads to right heart failure Ø Copyright © 2017 Elsevier Inc. All rights reserved. 98
Pathophysiology (Cont. ) Compensatory mechanisms Renin-angiotensin-aldosterone system Ø Sympathetic nervous system Ø Right heart failure Ø Leads to systemic symptoms Copyright © 2017 Elsevier Inc. All rights reserved. 99

Copyright © 2017 Elsevier Inc. All rights reserved. 100

Copyright © 2017 Elsevier Inc. All rights reserved. 101

Copyright © 2017 Elsevier Inc. All rights reserved. 102
Pathophysiology (Cont. ) Brain natriuretic peptide (BNP) Cardiac hormone • Secreted by ventricular myocytes in response to wall stretch • Normal 100 pg/m. L Ø Plasma concentrations reflect severity of heart failure • In decompensated heart failure, BNP rises • As heart failure is treated, BNP will lower Ø Good marker for differentiating between pulmonary and cardiac causes of dyspnea Ø Copyright © 2017 Elsevier Inc. All rights reserved. 103
Assessment of Heart Failure Left-sided failure signs and symptoms Right-sided failure signs and symptoms Examination of neck veins Presence or absence of edema Perfusion status Lung sounds Diagnostic findings Chest x-ray Ø Hemodynamic monitoring (pulmonary artery catheter) Ø Copyright © 2017 Elsevier Inc. All rights reserved. 104
Assessment Diagnostics Testing Echocardiogram Arterial blood gases Serum electrolytes BUN/Creatinine Complete blood count B-type natriuretic peptide (BNP) Hepatic function ECG Copyright © 2017 Elsevier Inc. All rights reserved. 105
Heart Failure Nursing Interventions Improve pump function Diuretics Ø ACE inhibitors Ø Angiotensin receptor blockers Ø Beta blockers (carvedilol [Coreg]) Ø Digoxin Ø Copyright © 2017 Elsevier Inc. All rights reserved. 106
Heart Failure Treatment Nesiritide citrate (Natrecor) intravenous for acute decompensation of heart failure Copyright © 2017 Elsevier Inc. All rights reserved. 107
Heart Failure Treatment (Cont. ) Reduce cardiac workload Intraaortic balloon pump Ø Mechanical circulatory support devices (MCSDs) Ø Biventricular pacing Ø Nursing interventions, rest, and activity as tolerated. Ø Cardiac rehabilitation Ø Copyright © 2017 Elsevier Inc. All rights reserved. 108
Heart Failure Treatment (Cont. ) Optimization of gas exchange Airway assessment and degree of respiratory distress Ø Semi-Fowler positioning Ø Supplemental oxygen Ø Continuous positive airway pressure (CPAP) Ø Diuresis Ø Control sodium and fluid retention Ø Daily weights Ø VTE prophylaxis Ø Copyright © 2017 Elsevier Inc. All rights reserved. 109
Case Study Mr. T. had the CABG. It was difficult to get Mr. T. weaned from the cardiopulmonary bypass machine. A decision was made to insert an intraaortic balloon pump (IABP). Why was the IABP inserted? What are some related nursing interventions? Copyright © 2017 Elsevier Inc. All rights reserved. 110
Case Study (Cont. ) Mr. T. required the IABP for 24 hours, at which time it was weaned and removed. The remainder of his postoperative course was uneventful, and he was discharged home 6 days after surgery. Discuss discharge teaching needs. Copyright © 2017 Elsevier Inc. All rights reserved. 111
Heart Failure Complications Pulmonary edema Dyspnea Ø Cyanosis Ø Gurgles Ø Pink, frothy sputum Ø Hypoxemia Ø Cardiogenic shock Copyright © 2017 Elsevier Inc. All rights reserved. 112
Inflammatory Heart Disease Pericarditis—inflammation of the pericardium Endocarditis—inflammation of the endocardium Copyright © 2017 Elsevier Inc. All rights reserved. 113
Pericarditis Etiology After a myocardial infarction Ø Uremia Ø Cancers Ø Can lead to infusion, tamponade, and scarring Copyright © 2017 Elsevier Inc. All rights reserved. 114
Hallmarks of Pericarditis Friction rub Pulsus paradoxus Initial ST elevation Copyright © 2017 Elsevier Inc. All rights reserved. 115
Pericarditis Assessment Relieve pain Procedures: pericardiocentesis Ø pericardial window Ø Copyright © 2017 Elsevier Inc. All rights reserved. 116

Endocarditis Endocardium continuous with valves Vegetation Embolization Valvular dysfunction Copyright © 2017 Elsevier Inc. All rights reserved. 117
Assessment of Endocarditis The clinical presentation High fever and shaking chills Night sweats, cough, weight loss General malaise, weakness, fatigue, headache, musculoskeletal complaints New murmurs Symptoms of HF Skin abnormalities Janeway lesions Ø Osler nodes Ø Copyright © 2017 Elsevier Inc. All rights reserved. 118
Endocarditis (Cont. ) Diagnosis: echocardiogram, transesophageal echocardiography Treatment: antibiotics, rest Prevention: antibiotic prescription before treatments (e. g. , dentist) Heart valve Ø History of endocarditis Ø Microvascular pressure with regurgitation Ø Copyright © 2017 Elsevier Inc. All rights reserved. 119
Vascular Alterations Aortic aneurysms Dilation or thinning of wall Ø Thoracic aortic Ø Thoracoabdominal aortic Ø Abdominal aortic Ø Treat based on size and symptoms Ø False versus true Ø Copyright © 2017 Elsevier Inc. All rights reserved. 120

Anatomy of the Aorta Figure 13 -18. Anatomy of the aorta and its major branches. (From Patton KT, Thibodeau GA. Anatomy and Physiology. 8 th ed. St. Louis: Mosby; 2013. ) Copyright © 2017 Elsevier Inc. All rights reserved. 121
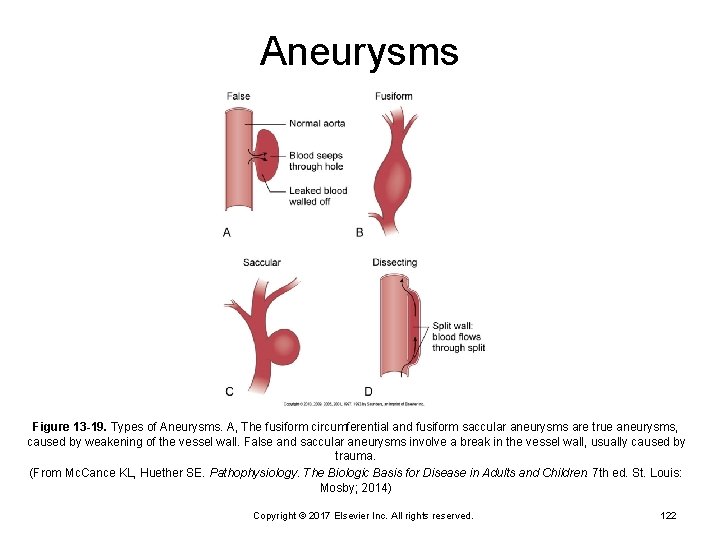
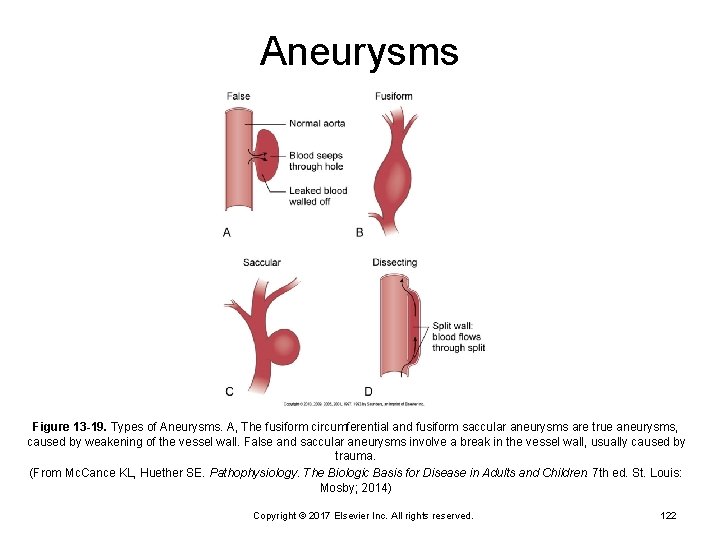
Aneurysms Figure 13 -19. Types of Aneurysms. A, The fusiform circumferential and fusiform saccular aneurysms are true aneurysms, caused by weakening of the vessel wall. False and saccular aneurysms involve a break in the vessel wall, usually caused by trauma. (From Mc. Cance KL, Huether SE. Pathophysiology. The Biologic Basis for Disease in Adults and Children. 7 th ed. St. Louis: Mosby; 2014) Copyright © 2017 Elsevier Inc. All rights reserved. 122
Vascular Alterations (Cont. ) Aortic dissection Tear of intimal layer of the vessel Ø Sudden Ø Sharp Ø Shifting pain Ø Marfan syndrome Ø Copyright © 2017 Elsevier Inc. All rights reserved. 123
Vascular Alterations (Cont. ) Surgical Treatment Open approach Ø Endovascular approach Ø Copyright © 2017 Elsevier Inc. All rights reserved. 124

Endoaneurysmal Repair Figure 13 -20 Surgical repair of an abdominal aortic aneurysm. A. The aneurysmal sac is incised. B. The synthetic graft is inserted. C. The native aortic wall is sutured over the synthetic graft. (From Lewis SL, et al. Medical-Surgical Nursing: Assessment and Management of Clinical Problems. 9 th ed. St. Louis: Mosby; 2014. ) Copyright © 2017 Elsevier Inc. All rights reserved. 125