Ischemic optic neuropathy ION Nasr Esfahani MD Ischemic








![Further testing in such patients may include fluorescein angiography. 22]. Contrast-enhanced magnetic re Further testing in such patients may include fluorescein angiography. 22]. Contrast-enhanced magnetic re](https://slidetodoc.com/presentation_image_h/e018fd162ee6123a3fa52175e55ac4a1/image-22.jpg)



















- Slides: 72

Ischemic optic neuropathy (ION) Nasr Esfahani MD

Ischemic optic neuropathy �ION reflecting ischemic damage to different part of optic nerve with different etiologies
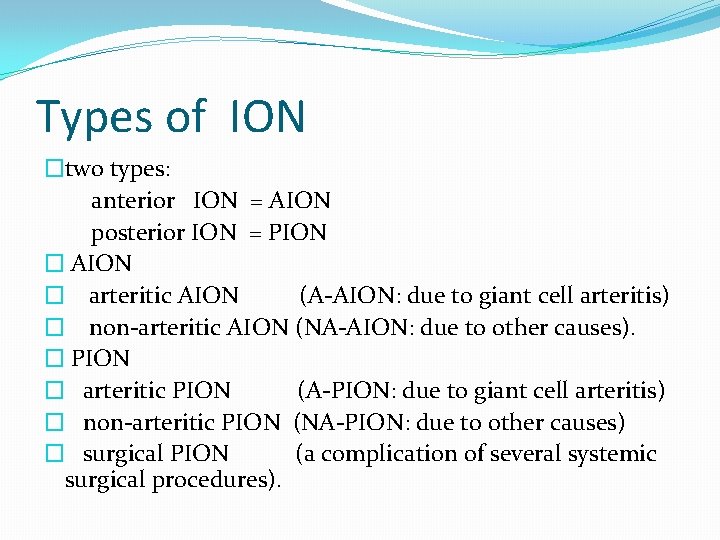
Types of ION �two types: anterior ION = AION posterior ION = PION � AION � arteritic AION (A-AION: due to giant cell arteritis) � non-arteritic AION (NA-AION: due to other causes). � PION � arteritic PION (A-PION: due to giant cell arteritis) � non-arteritic PION (NA-PION: due to other causes) � surgical PION (a complication of several systemic surgical procedures).

VASCULAR ANATOMY � The optic nerve head (ONH) consist of prelaminar and laminar portion supplied by 15 to 20 short posterior ciliary arteries and circle of Zinn-Haller. � circle of Zinn-Haller itself is made by the short posterior ciliary arteries(major part) pial branches , and choroidal vessels.
In summary: PCA is the main source of blood supply to the ONH. the rest of the optic nerve is supplied from other sources and not PCA



Pathogenesis of NA-AION �NA-AION is two types: �the most common is caused by transient nonperfusion or hypoperfusion of the ONH circulation; � the second, and rarer one, is due to embolism to the arteries/arterioles feeding the ONH.
Nonarteritic Anterior ISchemic Optic Neuropathy (NAION) � 90 -95% of AION cases �In younger age groups (mean age 60 yr) �Related to compromise of optic disc microcirculation �↓ VA On awakening, related to noctural systemic Hypotension �Systemic symptoms are absent
DIAGNOSIS � — The diagnosis of NAION in the majority of patients is clinical, based upon age, presence of vasculopathic risk factors, the pattern of visual loss, and the appearance of the swollen disc.
EXAMINATION FINDINGS �Reduced visual acuity �Dyschromatopsia �Afferent pupillary defect �Optic disc edema �Peripapillary splinter hemorrhage �Small optic cup, nerve fiber crowding in the unaffected eye �A relative afferent pupillary defect
�Types of ↓VA(initial V. A > 20/200 in over 60% of cases) � � � static progressive (22 -37 %) episodic stepwise steady decline over weeks to months
VF An altitudinal visual field defect is the classically described field defect seen in NAION, but among reported case series, its prevalence varies from 25 to 79 percent . In one series of perimetry studies in 312 eyes, a variety of visual field defects were observed, with an absolute inferior altitudinal defect observed in only 8 percent. The single most commonly observed defect was an absolute inferior nasal defect, found in 22 percent. Other common defects included central, centrocecal and arcuate scotomas, as well as generalized depression
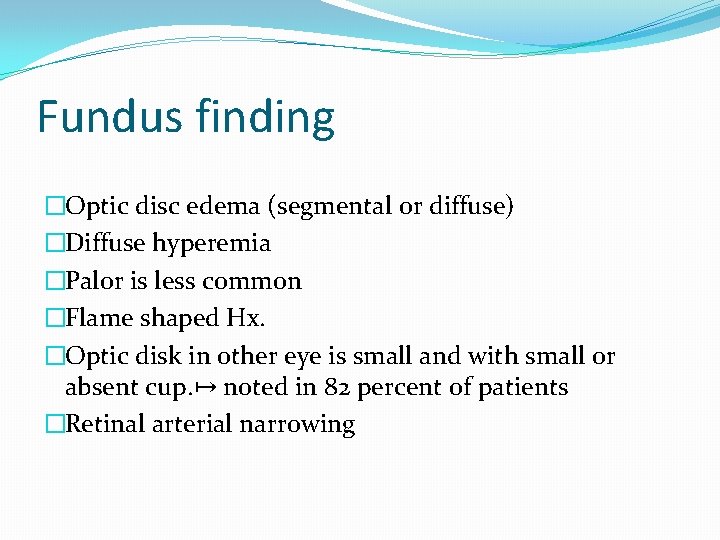
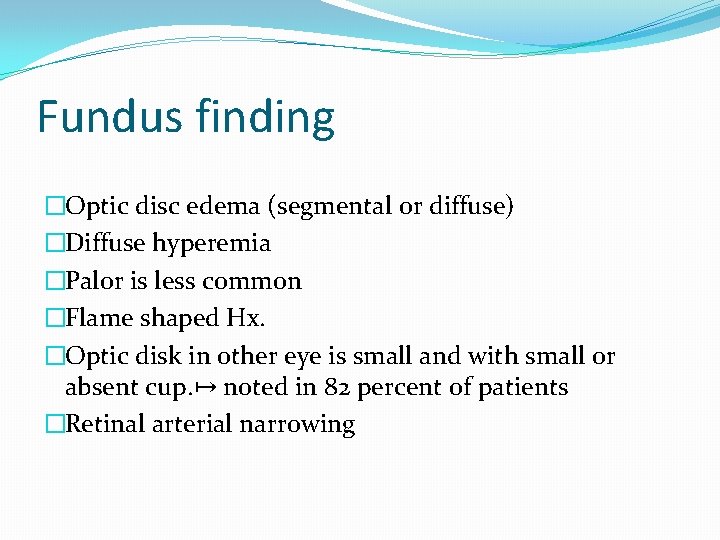
Fundus finding �Optic disc edema (segmental or diffuse) �Diffuse hyperemia �Palor is less common �Flame shaped Hx. �Optic disk in other eye is small and with small or absent cup. ↦ noted in 82 percent of patients �Retinal arterial narrowing
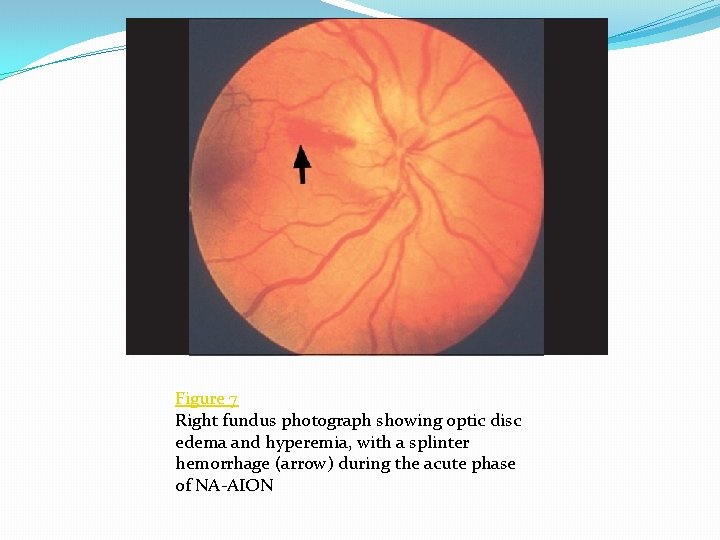
Figure 7 Right fundus photograph showing optic disc edema and hyperemia, with a splinter hemorrhage (arrow) during the acute phase of NA-AION

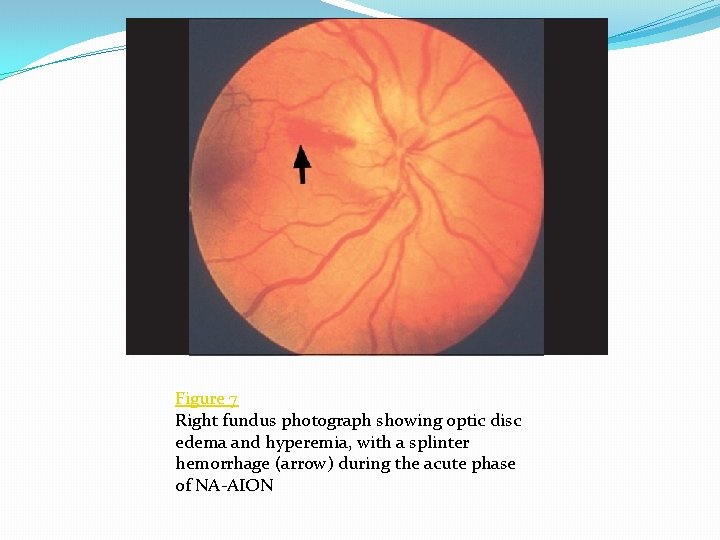
Figure 5 Fundus photographs of left eye of a 53 -year-old man: (a) Normal disc before developing NA-AION, (b) with optic disc edema and hyperemia during the active phase of NA-AION, and (c) after resolution of optic disc edema and development of
sectorial edema

FA �Delayed optic disc filling in 75% of NAION �Normal choroidal filling �In the acute phase of NAION there is delayed filling of the prelaminar layers of the edematous optic disc. Poor or absent filling of the choroid is not typical of NAION and suggests giant cell arteritis [
![Further testing in such patients may include fluorescein angiography 22 Contrastenhanced magnetic re Further testing in such patients may include fluorescein angiography. 22]. Contrast-enhanced magnetic re](https://slidetodoc.com/presentation_image_h/e018fd162ee6123a3fa52175e55ac4a1/image-22.jpg)
Further testing in such patients may include fluorescein angiography. 22]. Contrast-enhanced magnetic re


FA in acute non-arteritic AION Localized hyperfluorescence Increasing localized hyperfluorescence Generalized hyperfluorescence

Risk Factors of NAION �Systemic and ocular �Optic disc drusen �Small optic disc: Crowding of disk (disk at risk)↦ a process similar to that of a compartment syndrome �Systemic hypertension �Diabetes (young) �Smoking, �hyperlipidemia �Hyperhomocysteinemia, platelet polymorphism, �Phosphodiestrase inhibitors (sildenafil or viagra) ? ? �Nocturnal hypotension �Sleep apnea prolonged hypoxia
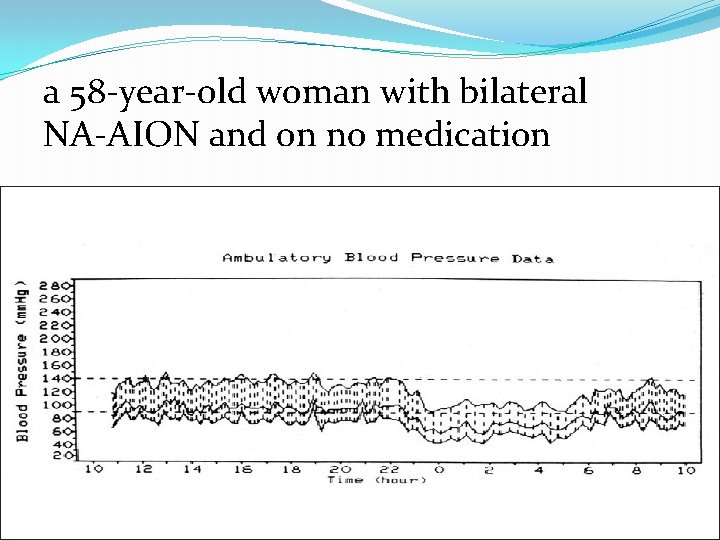
a 58 -year-old woman with bilateral NA-AION and on no medication

Differential Diagnosis of NAION �Optic neuritis �Infiltrative optic neuropathies �Anterior orbital lesion �Diabetic papillopathy
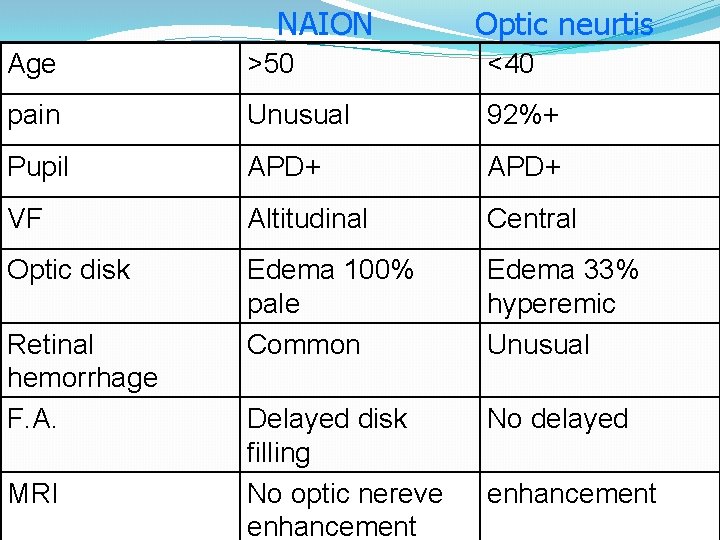
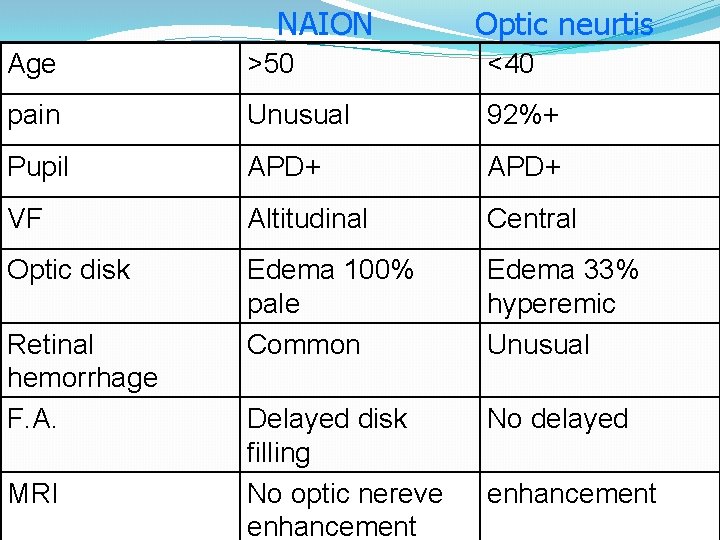
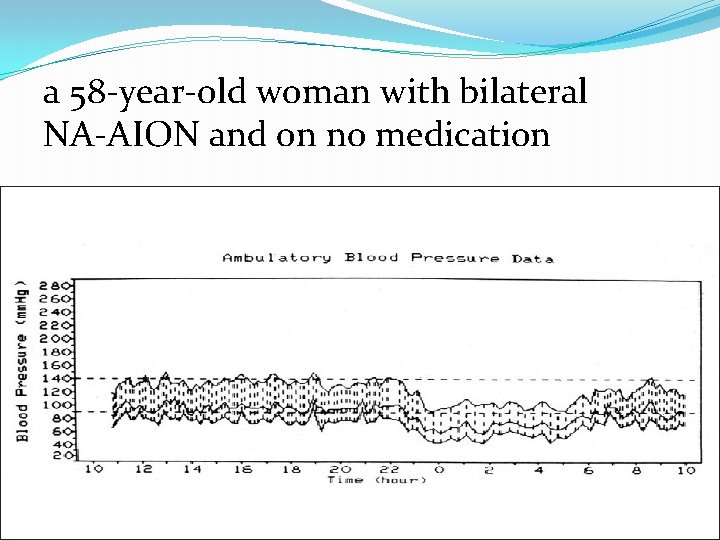
NAION Optic neurtis Age >50 <40 pain Unusual 92%+ Pupil APD+ VF Altitudinal Central Optic disk Edema 100% pale Common Edema 33% hyperemic Unusual Delayed disk filling No optic nereve enhancement No delayed Retinal hemorrhage F. A. MRI enhancement
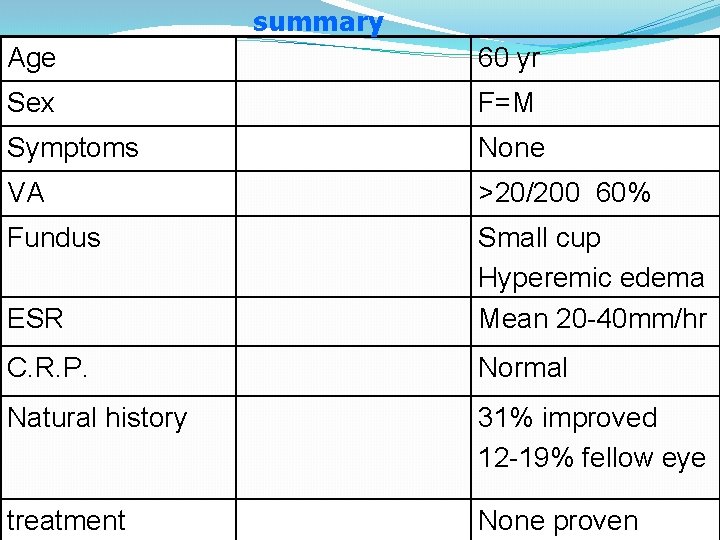
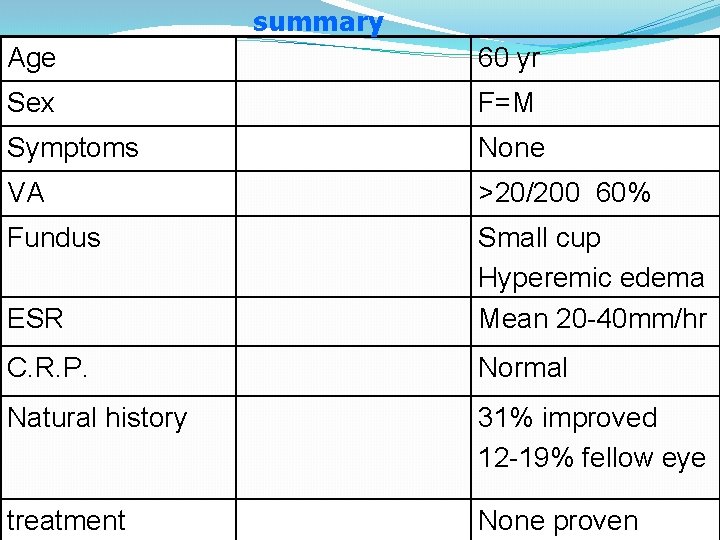
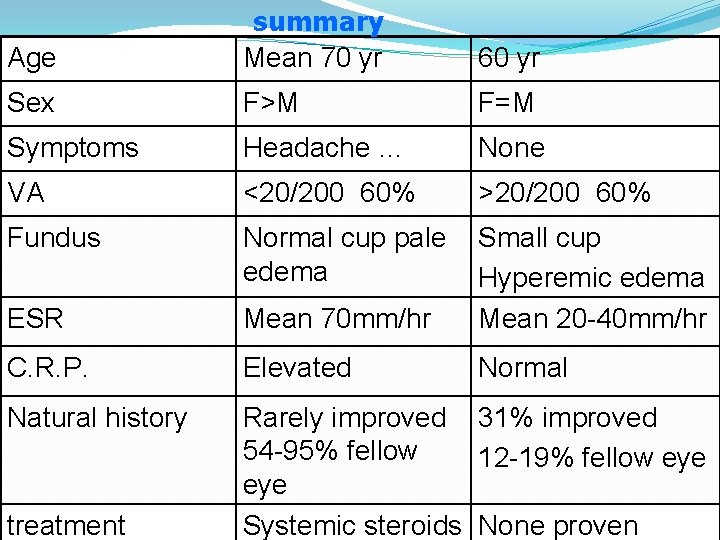
summary Age 60 yr Sex F=M Symptoms None VA >20/200 60% Fundus ESR Small cup Hyperemic edema Mean 20 -40 mm/hr C. R. P. Normal Natural history 31% improved 12 -19% fellow eye treatment None proven
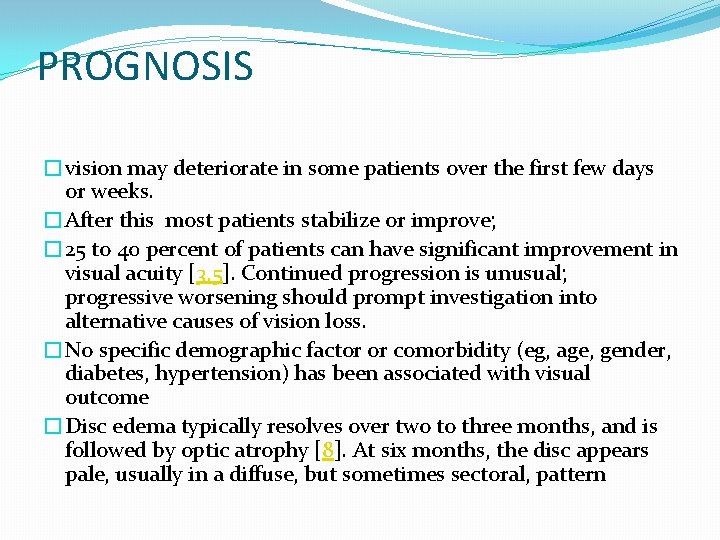
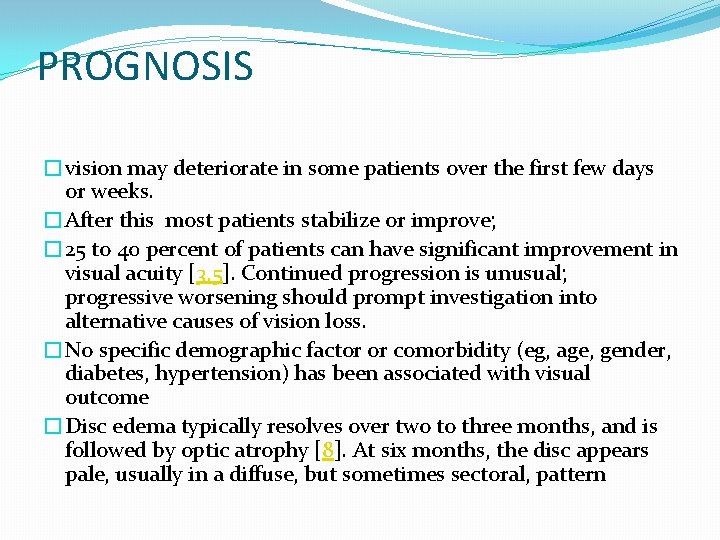
PROGNOSIS �vision may deteriorate in some patients over the first few days or weeks. �After this most patients stabilize or improve; � 25 to 40 percent of patients can have significant improvement in visual acuity [3, 5]. Continued progression is unusual; progressive worsening should prompt investigation into alternative causes of vision loss. �No specific demographic factor or comorbidity (eg, age, gender, diabetes, hypertension) has been associated with visual outcome �Disc edema typically resolves over two to three months, and is followed by optic atrophy [8]. At six months, the disc appears pale, usually in a diffuse, but sometimes sectoral, pattern

Mortality and other vascular events � — Patients with NAION do not appear to have a higher mortality or risk for stroke or cardiovascular disease than would otherwise be expected on the basis of their underlying comorbidities
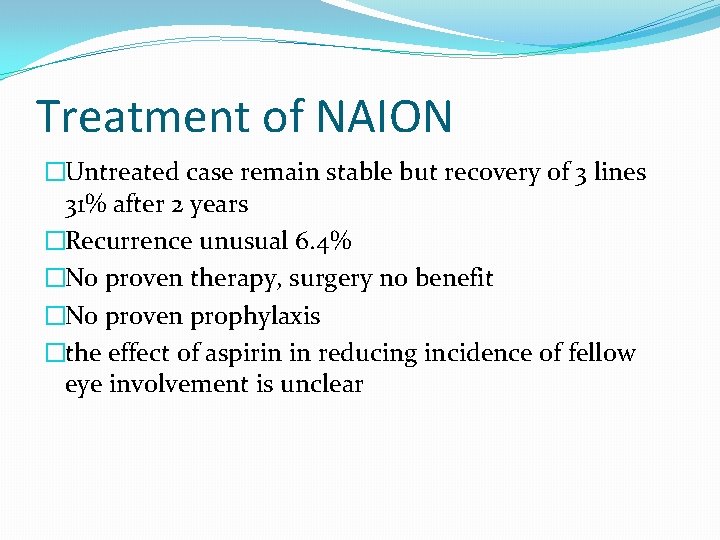
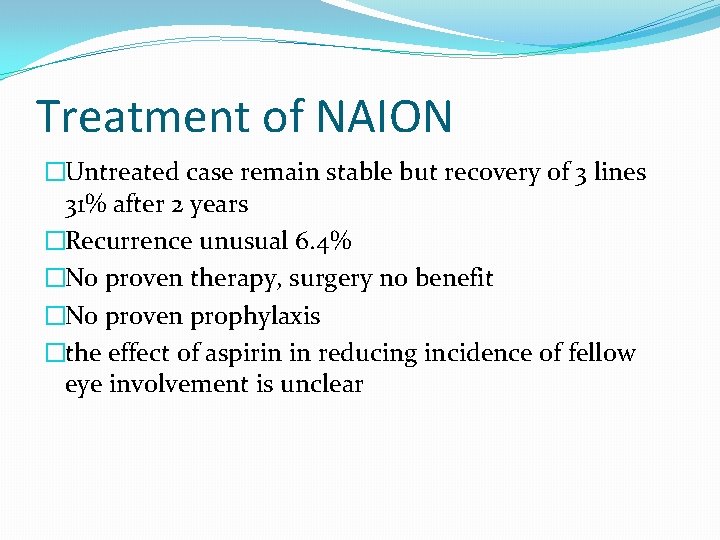
Treatment of NAION �Untreated case remain stable but recovery of 3 lines 31% after 2 years �Recurrence unusual 6. 4% �No proven therapy, surgery no benefit �No proven prophylaxis �the effect of aspirin in reducing incidence of fellow eye involvement is unclear
TREATMENT �— There is no known effective therapy for NAION to ameliorate the degree of visual impairment

Aspirin � Aspirin therapy does not appear to influence visual outcomes of acute NAION. � In a retrospective case-control study, 23 patients treated with aspirin before and during the course of NAION were compared to 55 patients with NAION who did not use aspirin [25]. �Visual outcomes (visual acuity and mean deviation on automated perimetry) were similar in the two groups

Blood pressure � NAION in the setting of severe hypotension ↦ prompt efforts to reverse hypotension, �Patients with acute HTN should have their blood pressure lowered incrementally rather than abruptly, as this has been described as precipitating NAION in at least one case report

Corticosteroids � — The evidence supporting the use of corticosteroid therapy in NAION is limited �. Corticosteroids are sometimes used in NAION, particularly when there is concern that giant cell arteritis has not been excluded, but also in cases of severe bilateral vision loss as can occur in the perioperative or dialysis setting � Some anecdotal reports suggest that corticosteroids may have some benefit in NAION [30 -32]. � One retrospective study examined outcomes in 613 patients with NAION, 312 of whom were treated with corticosteroids [33]. Treated patients were somewhat younger and less likely to have hypertension or diabetes. After a median followup of 3. 8 years, a benefit for treatment was observed in the subgroup of 70 eyes with initial acuity of 20/70 or worse, who were treated within two weeks of onset; 70 percent improved two or more lines compared with 41 percent in the untreated group. In this subgroup, visual field defects were also more likely to improve in the treated compared with the untreated group (40 versus 25 percent). the author concluded that early (within two weeks) treatment with corticosteroids leads to improvement in both visual acuity and visual fields,
Surgical therapies �Optic Nerve Sheath Decompression — �two or more slits or a window in the optic nerve sheath are created reducing the pressure surrounding the optic nerve. Compression of the optic nerve sheath is possibly pathogenic in NAION �. �The conclusions of IONDT were that Optic Nerve Sheath Decompression appears to be of no value to most patients with NAION and could potentially cause further visual deterioration.
Optic neurotomy �— This investigational surgical procedure relaxes the scleral ring surrounding the prelaminar and laminar regions of the optic nerve head, with the goal of reducing constriction and preventing necrosis of underperfused nerve fibers. �surgical manipulation of the optic nerve head has the potential to further damage nerve fibers and blood vessels, potentially causing devastating loss of vision [37].
Vitrectomy �— A case series of 16 patients with NAION had findings on optical coherence tomography and ultrasound that were consistent with partial posterior vitreous detachment �elevation of the optic nerve head from traction of the posterior vitreous may have disrupted the microcirculation and axoplasmic flow leading to optic nerve edema and visual dysfunction. �Surgical release of epipapillary vitreous traction �this study raises the possibility of a role of vitreous traction in the pathogenesis of NAION
Other investigational medications �medications that may have � neuroprotective effects, � meliorate disc edema and pressure surrounding the optic nerve head, and � improve blood flow to areas of ischemia.

Levodopa �— A potential role for dopamine in the treatment of NAION is based on its putative neuroprotective and neuromodulatory effects in the retina, optic nerve, and/or brain, or its activity as a neurotransmitter in the retina. �The benefit of levodopa in NAION is not established.
Brimonidine �— Brimonidine is an alpha-2 agonist that lowers intraocular pressure and is used in the treatment of glaucoma. �There have been promising reports from animal studies suggesting that topical brimonidine may have a neuroprotective effect on retinal ganglion cells and reduce optic nerve injury after ischemia �However, a randomized placebo controlled trial found no therapeutic effect of brimonidine 0. 2 percent in 36 patients with acute NAION
Citicoline � — Citicoline is a putative neuroprotective agent that has been evaluated �in the treatment of acute cerebral infarction. � In a randomized pilot study, 14 patients with NAION were treated with citicoline 1600 mg per day for 60 days. �After 60 and 180 days, these treated patients demonstrated overall improvement in visual acuity compared to baseline, while untreated patients did not
Intravitreal agents � — Intravitreal administration of medications offers the promise of delivering targeted medications directly to the source of pathology. However, this route of administration is not without risks, including a small risk of infectious endophthalmitis, retinal detachment, and traumatic cataract estimated at about 0. 15 percent [54]. None of the agents discussed below is currently recommended in the treatment of NAION.
Triamcinolone �— Intravitreal triamcinolone acetonide (IVTA), a corticosteroid, has been administered to patients with NAION. In one case series of four patients, treatment was associated with marked, early resolution of optic disc swelling, disappearing by week three in all eyes, in contrast to persistence of disc edema in a control group of six patients [55]. Mean improvements in visual acuity also appeared better with treatment compared with controls; however, treatment was not clearly associated with visual field improvement. In two other small case series of three and four patients, respectively, IVTA was administered with some observed gains in visual acuity, but these case series were not controlled [56, 57]. In one case, treatment was complicated by increase in intraocular pressure requiring anti-glaucoma treatment, a complication that occurs in up to 25 percent of patients when IVTA is administered for other indications [58, 59].
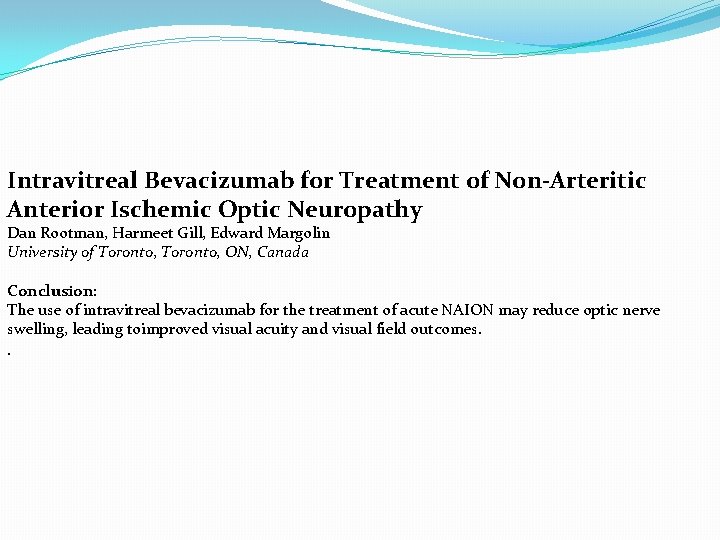
Anti-vascular endothelial growth factor (VEGF) agents �decreasing optic nerve head edema and secondary tissue injury. �A recent report described visual improvement in four eyes of four patients after single intravitreal injection of ranibizumab [60]. � Another case report describes rapid resolution of vision loss and disc edema in a patient with NAION treated with intravitreal bevacizumab [61]. �However, there have been two reports of NAION occurring after intravitreal injection of bevacizumab (for non-NAION indications) at one week and two weeks postinjection [

Erythropoietin �— In one case series, 31 patients with NAION received unilateral intravitreal erythropoietin injection (2000 units), within one month of onset of NAION [64]. Visual acuity improvement occurred in 61 percent of patients within the first month. Vision continued to improve up to three months and then deteriorated, but remained significantly better than baseline at the last, six month, follow-up examination
Fibrinogen/LDL apheresis �— Fibrinogen/LDL apheresis, also known as heparininduced extracorporeal LDL/fibrinogen precipitation (HELP) removes fibrinogen, total cholesterol, low density lipoproteins and triglycerides from plasma and has shown promise in the treatment of microvascular disorders, including peripheral artery disease and sudden hearing loss of vascular origin [65, 66]. In a small, randomized, controlled study, 40 patients with recent-onset NAION, were assigned to treatment with HELP or to hemodilution therapy [67]. There was no significant difference in visual outcomes between the two groups.
Hyperbaric oxygen � — While case reports have suggested a possible benefit for hyperbaric oxygen in the treatment of NAION, these findings have not been confirmed in well-designed studies [68]. � A nonrandomized study compared hyperbaric oxygen treatment in 20 patients with acute NAION with 27 untreated patients and found �no significant difference in visual acuity or visual field outcomes in the groups
SECONDARY PREVENTION �— There is no known effective therapy proven to prevent NAION in the fellow eye [1, 23]. Most patients with NAION are treated with daily aspirin and risk factor management. �Patients taking medications implicated in the pathogenesis of NAION (eg, phosphodiesterase inhibitors, amiodarone, interferon alpha, sympathomimetics) should be counseled about a possible association and consider alternative medications if available.
Aspirin � — Four retrospective studies have evaluated the role of aspirin in the prevention of NAION in the fellow eye with somewhat mixed results: �The largest study compared outcomes in 153 patients who had received aspirin following the development of unilateral NAION and 278 who had not [14]. After five years. the cumulative probability of NAION in the fellow eye was similar in the aspirin and no-aspirin groups (17 and 20 percent respectively
Vascular risk factor management � — Medical control of underlying vasculopathic risk factors (eg, hypertension, diabetes, and smoking) is indicated in the primary prevention of cardiovascular disease and stroke; it is not known whether such interventions decrease the risk of NAION recurrence. �Over-aggressive control of systemic arterial hypertension may produce nocturnal hypotension, which is believed to be a risk factor for NAION [76]. Morning administration of blood pressure medications should be considered. Patients with acutely elevated blood pressure should have their blood pressure lowered incrementally rather than abruptly.

Pathogenesis of A-AION �When a patient is diagnosed as having AION, the first crucial step in patients aged 50 and over is to identify immediately whether it is arteritic or non-arteritic �In the eye, GCA has a special predilection to involve the PCA, resulting in its thrombotic occlusion
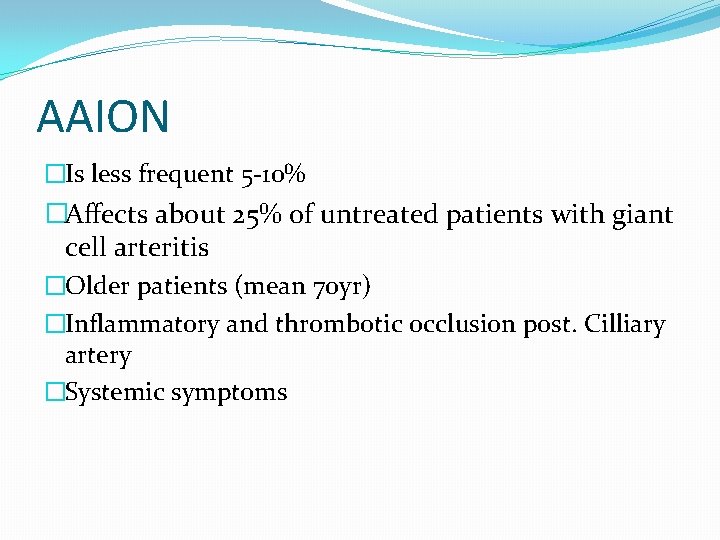
AAION �Is less frequent 5 -10% �Affects about 25% of untreated patients with giant cell arteritis �Older patients (mean 70 yr) �Inflammatory and thrombotic occlusion post. Cilliary artery �Systemic symptoms
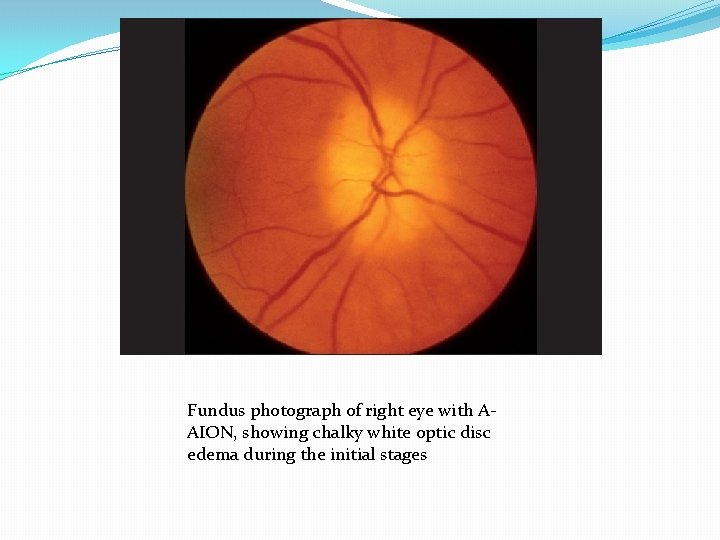
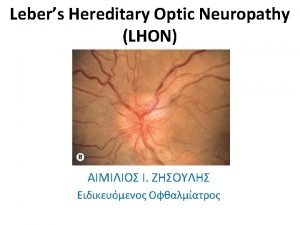
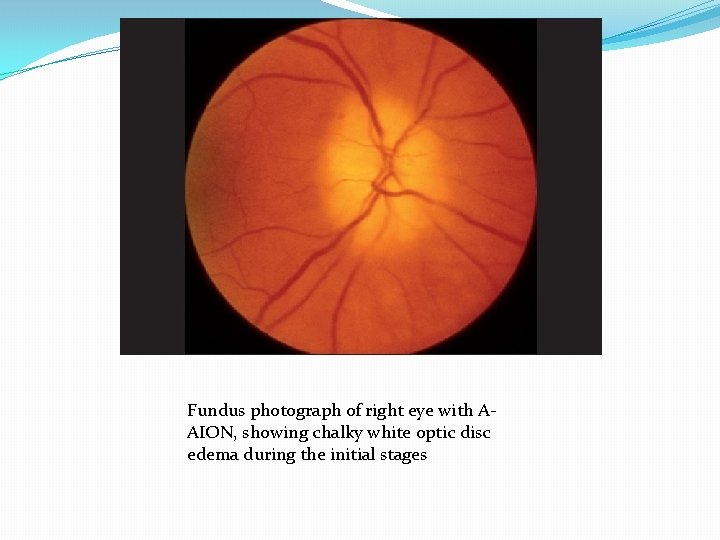
Fundus photograph of right eye with AAION, showing chalky white optic disc edema during the initial stages
AAION �Sever visual loss �Pale edema �Cotton wool spot �F. A. delayed choroidal filling �Normal cup.
Systemic Findings of GCA �Are usually present �Headache, temporal and scalp tenderness �Jaw claudication �Malaise, anorexia, weight loss, fever, joint & muscle pain �Ear pain

Superficial temporal arteritis Presentation Age - 65 -80 years • Scalp tenderness • Headache • Jaw claudication • Polymyalgia rheumatica • Superficial temporal arteritis • Acute visual loss • Special investigations ESR - often > 60, but normal in 20% • C-reactive protein - always raised • Temporal artery biopsy •
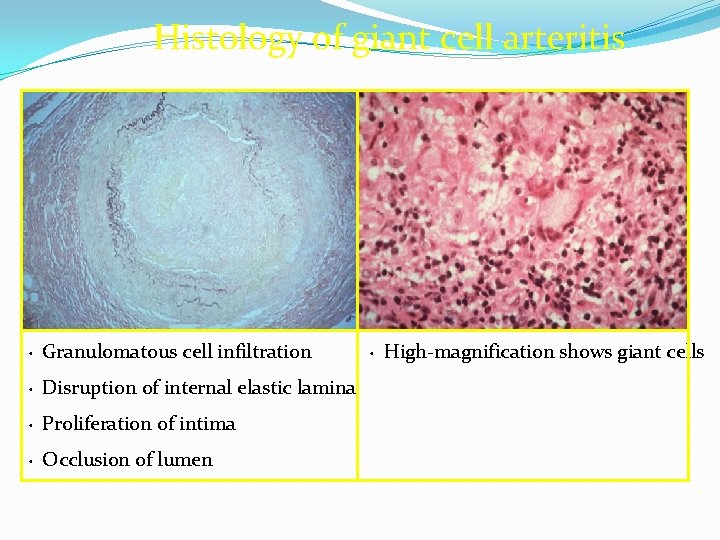
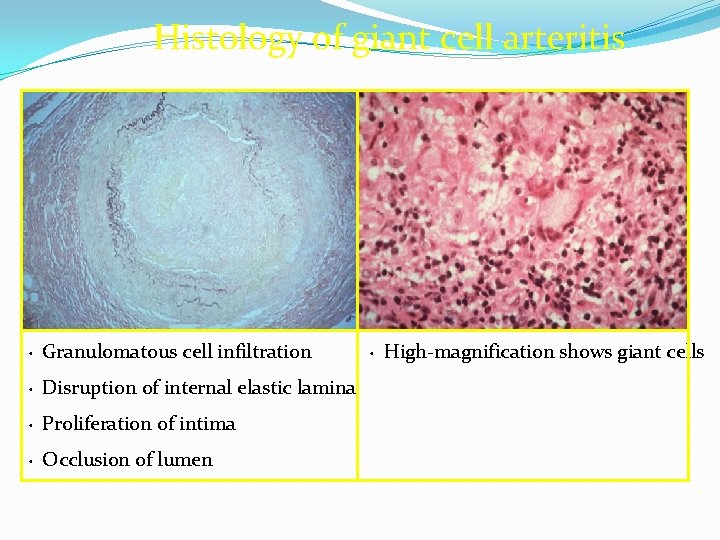
Histology of giant cell arteritis Granulomatous cell infiltration • Disruption of internal elastic lamina • Proliferation of intima • Occlusion of lumen • High-magnification shows giant cells •
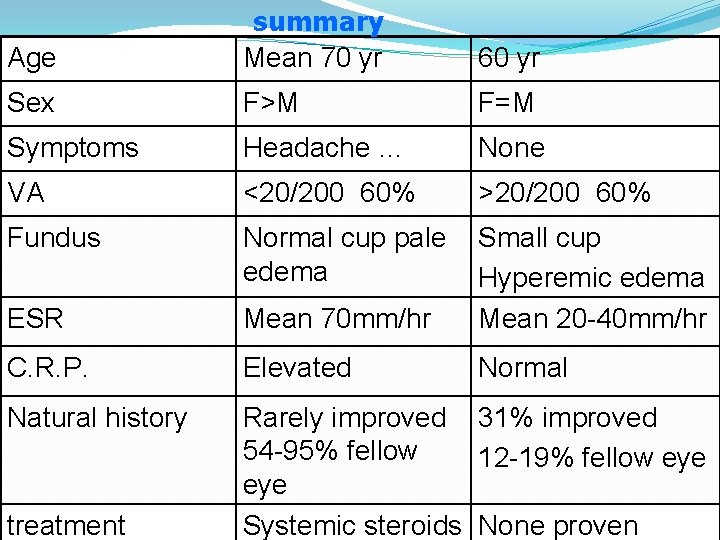
Age summary Mean 70 yr 60 yr Sex F>M F=M Symptoms Headache … None VA <20/200 60% >20/200 60% Fundus Normal cup pale edema ESR Mean 70 mm/hr Small cup Hyperemic edema Mean 20 -40 mm/hr C. R. P. Elevated Normal Natural history Rarely improved 31% improved 54 -95% fellow 12 -19% fellow eye Systemic steroids None proven treatment

Major Goals of Therapy �Prevent contralateral visual loss �Fellow eye involved 95% days or weeks �Affected eye improve somewhat �Avoid systemic vascular complication �Risk of recurrence is 7% so tapering must be slow and careful
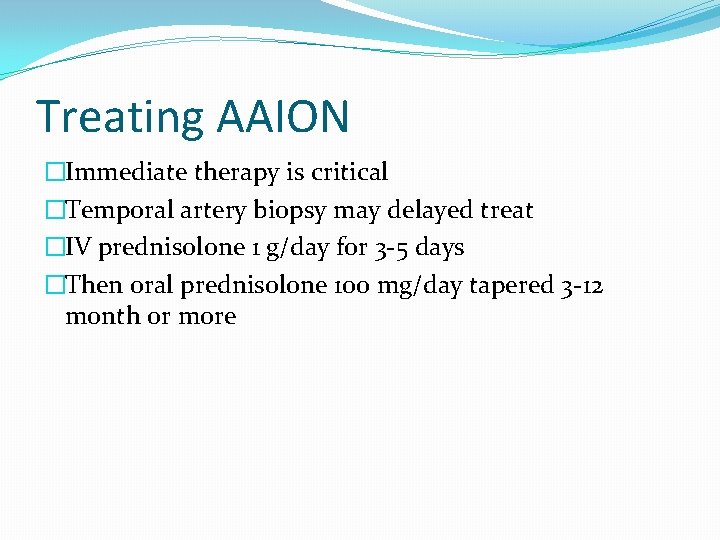
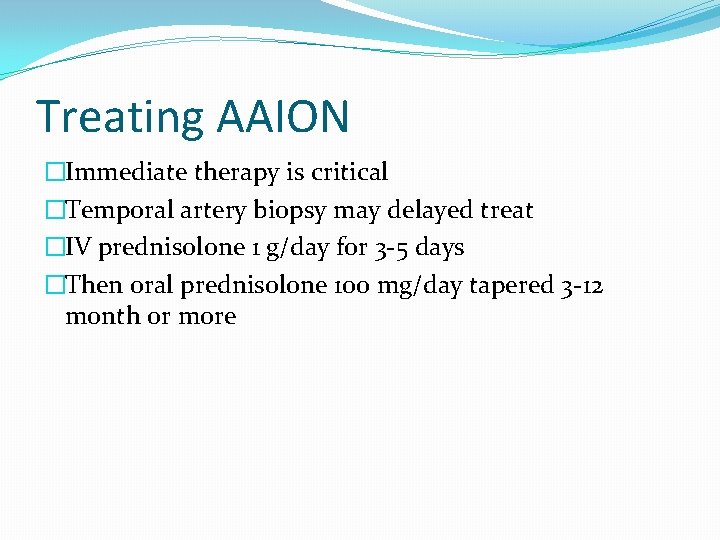
Treating AAION �Immediate therapy is critical �Temporal artery biopsy may delayed treat �IV prednisolone 1 g/day for 3 -5 days �Then oral prednisolone 100 mg/day tapered 3 -12 month or more
Intravitreal Bevacizumab for Treatment of Non-Arteritic Anterior Ischemic Optic Neuropathy Dan Rootman, Harmeet Gill, Edward Margolin University of Toronto, ON, Canada Conclusion: The use of intravitreal bevacizumab for the treatment of acute NAION may reduce optic nerve swelling, leading toimproved visual acuity and visual field outcomes. .
Patients with NA-AION, when treated with systemic corticosteroid therapy within first 2 weeks of onset, had significantly better visual outcome than untreated ones.

PION �There are three distinct etiologic categories that account for the majority of patients with PION: perioperative, � arteritic, �and nonarteritic (idiopathic) PION. (See 'Etiologies and pathogenesis' above. )

Perioperative PION �is most often described in the setting of spinal surgeries and radical neck dissection, although a wide range of operative procedures have been implicated. Hypotension and blood loss are the most universal risk factors for this complication. Localized venous hypertension resulting from prolonged use of the prone position in spine surgery and from internal jugular venous ligation in neck dissections are believed to contribute to PION in these cases. (See 'Perioperative PION' above

�PION is an infrequent complication of giant cell arteritis, a condition occurring exclusively in older adults (>50 years) and associated with a prodrome of polymyalgia rheumatica. (See 'Arteritic PION' above. ) �More than half of PION cases are classified as nonarteritic, idiopathic. Associated comorbidities in these patients suggest that nonarteritic PION is a manifestation of systemic vascular disease. (See 'Nonarteritic (idiopathic) PION' above. )

�Most patients with PION present with abrupt, painless, monocular vision loss. About half of patients with perioperative PION will have bilateral vision loss, while patients with arteritic PION are at risk for rapidly sequential vision loss affecting first one eye then the next. Vision loss is usually severe in patients with perioperative and arteritic PION, but is more variable in patients with nonarteritic PION.

PION is a diagnosis of exclusion. � The most urgent diagnostic imperative is to diagnose or exclude GCA with ESR and CRP and/or a temporal artery biopsy. Patients also require ophthalmologic examination and a contrast-enhanced magnetic resonance imaging study that focuses on the optic nerves. (See 'Diagnosis' above. ) � Patients with PION and GCA are treated with corticosteroids. While significant visual recovery is unlikely, treatment is aimed at preventing vision loss in the other eye. (See 'Prognosis and treatment' above. ) � Patients with perioperative PION do not usually experience significant visual recovery, while up to one-third of patients with nonarteritic (idiopathic) PION may improve. There is no treatment for perioperative or nonarteritic PION. Patients with nonarteritic PION may experience a subsequent episode in the other eye over the next months and years, but interventions (such as atherosclerosis risk factor management and aspirin) are not known to prevent this. (See 'Prognosis and treatment' above. )

PION �SUMMARY AND RECOMMENDATIONS — PION is believed to result from an infarction of the retrobulbar optic nerve. While there is much overlap, the vascular anatomy, etiologies, and clinical presentation of PION are distinct from those of anterior ischemic optic neuropathy, which is more common and affects the optic nerve head
THANK YOU
 Optic ischemic neuropathy
Optic ischemic neuropathy Dipolo dipolo inducido
Dipolo dipolo inducido Uniones intramoleculares
Uniones intramoleculares Intermolecular forces on vapor pressure
Intermolecular forces on vapor pressure C6h12 fuerza intermolecular
C6h12 fuerza intermolecular Diabetic peripheral neuropathy icd 9
Diabetic peripheral neuropathy icd 9 Chiropractic marketing flyers
Chiropractic marketing flyers Albuminocytologic dissociation
Albuminocytologic dissociation Diabetic neuropathy schaumburg
Diabetic neuropathy schaumburg Diabetic neuropathy
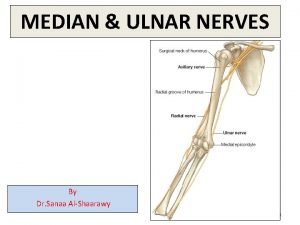
Diabetic neuropathy Ulnar neuropathy
Ulnar neuropathy Neuropathic pain
Neuropathic pain Neuropathy
Neuropathy Large fibre neuropathy
Large fibre neuropathy Neuropathy test
Neuropathy test Diabetic autonomic neuropathy
Diabetic autonomic neuropathy Idiopathic peripheral neuropathy
Idiopathic peripheral neuropathy Types of respiratory failure
Types of respiratory failure Wake up 24 hrs
Wake up 24 hrs Hemorrhagic vs ischemic stroke symptoms
Hemorrhagic vs ischemic stroke symptoms Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Mechanism of ischemic stroke
Mechanism of ischemic stroke Ischemic bile duct injury
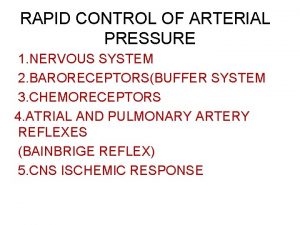
Ischemic bile duct injury Cns ischemic response
Cns ischemic response Chronic coronary syndrome
Chronic coronary syndrome Haemorrhage
Haemorrhage Mean arterial pressure
Mean arterial pressure Heart disease
Heart disease Stroke algorithm
Stroke algorithm Bainbridge reflex
Bainbridge reflex Axim geospatial
Axim geospatial Verilen bilgilerden hangisi asr suresi ile ilgilidir
Verilen bilgilerden hangisi asr suresi ile ilgilidir Dr mohamed nasr
Dr mohamed nasr Circinate impetigo
Circinate impetigo Dr reza nasr
Dr reza nasr Dr reza nasr gynecologist
Dr reza nasr gynecologist Kamal nasr
Kamal nasr Dr samer nasr
Dr samer nasr Ramzi nasr
Ramzi nasr Dr reza nasr gynecologist
Dr reza nasr gynecologist Sam nasr
Sam nasr Nars suresi
Nars suresi Abu nasr farobiy pedagogik g'oyalari
Abu nasr farobiy pedagogik g'oyalari Apakah pokok-pokok isi surat an-nasr
Apakah pokok-pokok isi surat an-nasr Dr reza nasr
Dr reza nasr Ons 15200 dwdm
Ons 15200 dwdm Flourescent optic yellow signs
Flourescent optic yellow signs Joint fiber optic cable
Joint fiber optic cable Optic ataxia
Optic ataxia Trochlear nerve decussation
Trochlear nerve decussation Optic placode
Optic placode Fiber optic cable advantages
Fiber optic cable advantages Disadvantages of fiber optic cable
Disadvantages of fiber optic cable Ear development
Ear development Disadvantages of current transformer
Disadvantages of current transformer Cutandclimb
Cutandclimb Julie greenlee
Julie greenlee Fiber optic hub
Fiber optic hub Afferent cranial nerves
Afferent cranial nerves Hypophyseal fossa
Hypophyseal fossa Eye muscles actions
Eye muscles actions Outer plexiform layer
Outer plexiform layer What makes up the diencephalon
What makes up the diencephalon Hybrid fiber coaxial vs fiber optic
Hybrid fiber coaxial vs fiber optic Optic tract
Optic tract Visual investigative analysis
Visual investigative analysis Fiber optic hardware
Fiber optic hardware Optic disc cube 200x200
Optic disc cube 200x200 Fiber optic disadvantages
Fiber optic disadvantages Clasificarea instrumentelor optice
Clasificarea instrumentelor optice Optic ap world history
Optic ap world history Fiber optic switch hub
Fiber optic switch hub Fluorescent optic yellow sign meaning
Fluorescent optic yellow sign meaning