Heart failure Heart failure In cardiac failure the

- Slides: 17
Heart failure
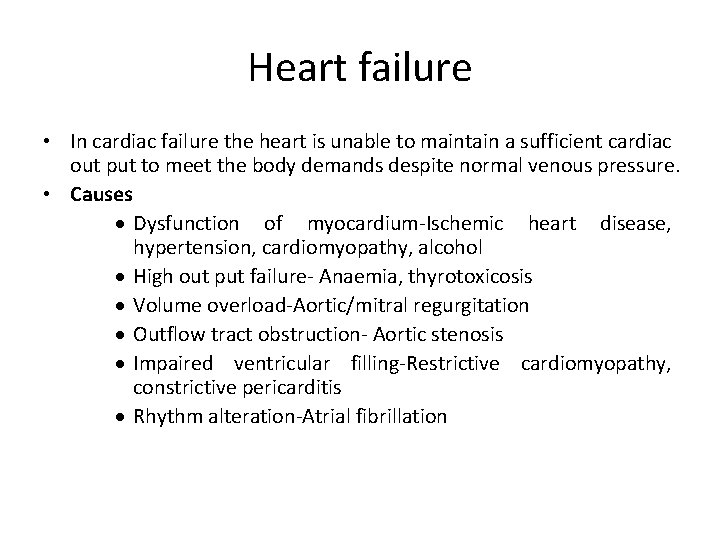
Heart failure • In cardiac failure the heart is unable to maintain a sufficient cardiac out put to meet the body demands despite normal venous pressure. • Causes · Dysfunction of myocardium-Ischemic heart disease, hypertension, cardiomyopathy, alcohol · High out put failure- Anaemia, thyrotoxicosis · Volume overload-Aortic/mitral regurgitation · Outflow tract obstruction- Aortic stenosis · Impaired ventricular filling-Restrictive cardiomyopathy, constrictive pericarditis · Rhythm alteration-Atrial fibrillation
Objectives of treatment • Decrease mortality and morbidity • Decrease symptoms • Decrease disease progression
Methods of treatment • Treat aggravating factors(e, g. arrhythmia, infections, thromboembolism) • Identify and if possible treat causative factors. • Non pharmacolological treatment-Fluid restriction, no added salt, regular aerobic exercise, stop smoking, alcohol in moderation • Pharmacological treatment with, 1. 2. 3. 4. 5. Diuretics ACE inhibitors and angiotensin 11 receptor blockers Beta blockers Digitalis glycosides Vasodilators- Hydralazine, nitrate
Drugs with prognostic benefit • ACEI-Angiotensin converting enzyme inhibitor/Angiotensin 11 receptor blocker • Beta blockers • Spiranolactone • Hydralazine and nitrate
Diuretics • Loop diuretics E. g. Frusemide, bumetanide decrease preload by increasing salt and water excretion and relieve peripheral oedema. • By using I/V frusemide can reduce pulmonary congestion rapidly, by its vasodilator action and is useful in acute left ventricular failure. • A thiazide diuretic when combined with a loop diuretic has a synergistic action and a greater diuretic effect. • Spiranolactone an aldosterone antagonist though a week diuretic has a potassium sparing effect and survival benefits. Other diuretics only have symptomatic benefits
Angiotensin converting enzyme inhibitor (ACEI) • Eg, Captopril, Enalapril • Uses in heart failure: – Symptomatic heart failure – Asymptomatic heart failure. • Actions in heart failure: 1. 2. 3. Inhibition of angiotensin 11 results in vasodilatation. This leads to a reduction in afterload, which improves the cardiac out put. There is also a reduction in aldosterone causing increased excretion of salt and water. This diuretic sparing effect improves symptoms by maintaining peripheral perfusion, and reduces the neurohumoral response to excessive diuresis. This also retards the progression of both symptomatic and asymptomatic heart failure, improves survival, improves quality of life and reduces hospitalization.
Angiotensin converting enzyme inhibitor (Cont. . ) • • ACEI should be initiate in hospital in : – Patients with large doses of diuretics due to risk of hypotension which can lead to renal failure. Omitting the preceding dose of diuretics minimizes the risk. – In patients with hyponatraemia due to risk of hypotension. – In patients with hypotension – In patients with renal impairment for ACEI increases the serum creatinin level. – In patients on high dose vasodilators – In patients over the age of 70 yrs. When starting on ACEI potassium sparing diuretics should be discontinued for ACEI causes potassium retention. ACEI are C/I in patients with known or suspected B/L renovascular disease. In people who develop cough as a side effect: – Angiotensin 11 receptor blockers can be started, which have the same haemodynamic benefits as ACEI.
Beta blockers • Carvedilol, metoprolol and bisoprolol are beneficial in the use of stable heart failure. • They act by reducing the sympathetic activity. Though sympathetic drive is needed for cardiac contractility and blocking it may worsen heart failure, sympathetic over activity can exacerbate heart failure. • So should be initiated with caution for they can cause decompensated heart failure. • These have proven benefits of symptomatic relief, improved exercise tolerance, improved left ventricular function and survival.
Digitalis glycosides • E. g. Digoxin Actions: • Positive inotropic effect (increase force of contraction) on the ventricles shifts the ventricular function curve to normal side increasing the cardiac output. • Reduction in ventricular rate by an action on the vagus, reducing atrioventricular (AV) conduction, for the refractory period in the AV node and the bundle of His is increased, allows for better filling time resulting in an increased cardiac out put. • Promotes diuresis • Decreases elevated end diastolic pressure • Decreases the end systolic volume of the failing heart reducing pulmonary oedema and elevated systemic venous pressure.
Digitalis glycosides (Cont. . ) • Pharmacokinetics: Half life 36 hrs. Can be given oral or I/V. There is no advantage in oral over I/V route can be used in people who are unable to take orally. Excreted mainly unchanged by the kidney. • This is not essential to treat all cases of heart failure. It is most beneficial in heart failure associated with atrial fibrillation, chronic ischemic heart disease, hypertensive heart disease and valvular heart disease. • These causes symptomatic relief, increase in exercise tolerance, reduction in the risk of clinical deterioration in heart failure patients who are in sinus rhythm. • Side effects: Abnormal cardiac rhythms(ectopics dysrhythmias, heart blocks), nausea and vomiting, disturbances in colour vision, confusion, digoxin toxicity for has a narrow therapeutic range
Digitalis glycosides (Cont. . ) • Effects of toxicity: Nausea, vomiting, hypokalaemia, any kind of arrhythmia, E. C. G. changes(Increased PR interval, sinus bradycardia, depressed ST segment which is the mirror image of mark) • Treatment of toxicity depends on the severity and includes stopping the drug, gastric lavage, ICU care, potassium supplements, antiarrhythmics (phenytoin, lignocaine, cardioversion by DC shocks, digoxin specific Ab fragments in life threatening situations. • Some contraindications: intermittent complete heart block, second degree AV block, supraventricular tachycardia caused by Wolff-Parkinson-White syndrome. • Other uses: Atrial fibrillation treatment
Vasodilators • E. g. Nitrates, Hydralazine • Nitrates reduce both preload and the afterload • Hydralazine is used only when ACEI can’t be used. • The combination of nitrates and hydralazine has shown to have survival benefits.
Anticoagulants • Heart failure is a risk factor for strokes. • Oral anticoagulants are recommended in: – – Patients with atrial fibrillation Past history of thromboembolism Identified thrombus Left ventricular aneurysm, etc.
Antiarrhythmics • Precipitating factors should be treated. • Restoration of sinus rhythm or in presence of structural defects, rate control with digoxin is done.

Drugs used in acute left ventricular failure Oxygen Morphine I/V Frusemide Nitrates-GTN, ISDN I/V Dobutamine infusion ( 1 adrenoceptor agonist) • Antiarrhythmics if needed • • •
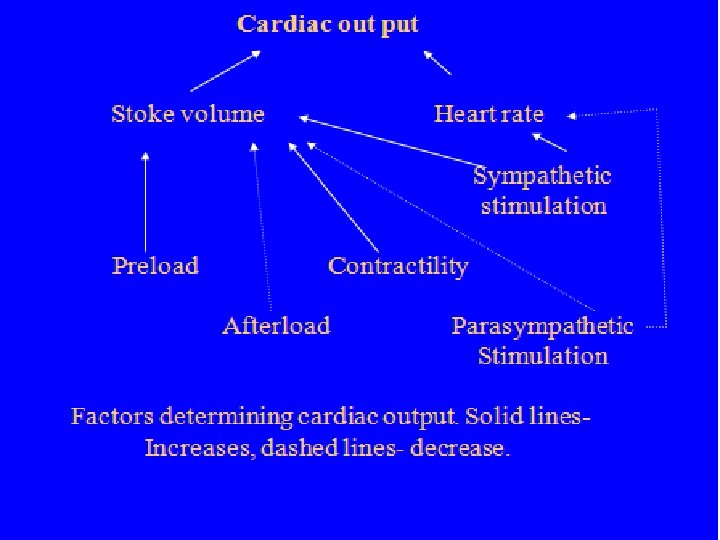
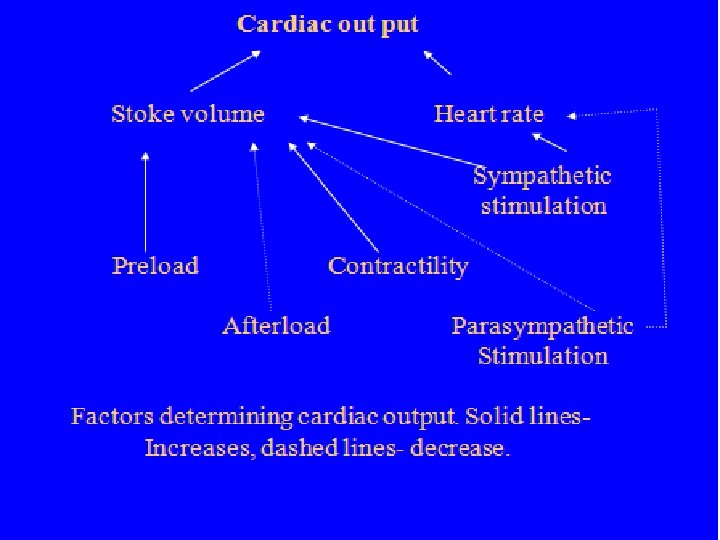
 Cardiac output and heart rate
Cardiac output and heart rate Events of cardiac cycle class 11
Events of cardiac cycle class 11 Ductile break
Ductile break Non conducted pac ecg
Non conducted pac ecg Pacer failure to sense
Pacer failure to sense Acute vs chronic heart failure
Acute vs chronic heart failure Cor pulmonale
Cor pulmonale New york scale heart failure
New york scale heart failure Diabetes and heart failure
Diabetes and heart failure Chapter 24 heart failure drugs
Chapter 24 heart failure drugs Lmnop heart failure
Lmnop heart failure Lvedp normal range
Lvedp normal range Right vs left-sided heart failure chart
Right vs left-sided heart failure chart Acute pulmonary congestion histology
Acute pulmonary congestion histology Edema assessment
Edema assessment Compensatory mechanisms of heart failure
Compensatory mechanisms of heart failure Heart failure
Heart failure Keith rn heart failure case study
Keith rn heart failure case study