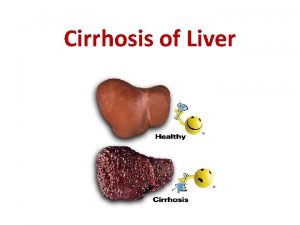
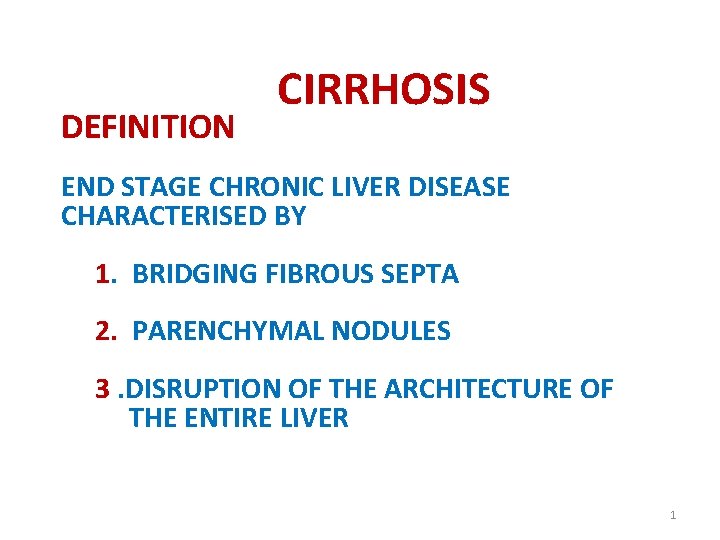
DEFINITION CIRRHOSIS END STAGE CHRONIC LIVER DISEASE CHARACTERISED












- Slides: 50
DEFINITION CIRRHOSIS END STAGE CHRONIC LIVER DISEASE CHARACTERISED BY 1. BRIDGING FIBROUS SEPTA 2. PARENCHYMAL NODULES 3. DISRUPTION OF THE ARCHITECTURE OF THE ENTIRE LIVER 1
CIRRHOSIS 1. DEFINITION 2. MORPHOLOGIC CLASSIFICATION 3. ETIOLOGIC CLASSIFICATION 4. PATHOGENESIS-MAJOR PATHOLOGIC MECHANISM 5. ALCOHOLIC LIVER DISEASES- PATHOGENESIS, ALCOHOLIC STEATOSIS, ALCOHOLIC HEPATITIS, ALCOHOLIC CIRRHOSISMORPHOLOGY, 6. OTHER TYPES OF CIRRHOSIS PATHOGENESIS, MORPHOLOGY, PROGNOSIS 7. CLINICAL FEATURES, PORTAL HYPERTENSION 2
MORPHOLOGIC CLASSIFICATION OF CIRRHOSIS 1. MICRONODULAR- NODULES EQUAL TO OR LESS THAN 3 mm 2. MACRONODULAR – NODULES MORE THAN 3 mm 3. MIXED TYPE 3

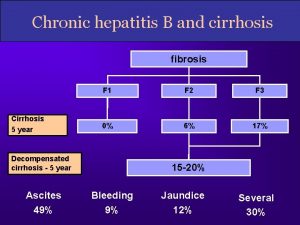
ETIOLOGIC CLASSIFICATION OF CIRRHOSIS ALCOHOLIC LIVER DESEASE 60 – 70 % VIRAL HEPATITIS (POSTNECROTIC CIRRHOSIS) 10% BILIARY DESEASES 5 – 10% HEREDITARY HEMOCHROMATOSIS- 5% 4
ETIOLOGIC CLASSIFICATION OF CIRRHOSIS WILSON DESEASE ALFA –I ANTITRYPSIN DEFICIENCY CRYPTOGENIC CIRRHOSIS -10 – 15% 5
OTHER INFREQUENT CAUSES IN INFANTS & CHILDREN GALACTOSEMIA OR TYROSINOSIS INDIAN CHILDHOOD CIRRHOSIS DRUG INDUSED CIRRHOSIS SYPHILIS CARDIAC CIRRHOSIS CRYPTOGENIC CIRRHOSIS 6

PATHOGENESIS 3 MAJOR PATHOLOGIC MECHANISMS 1. HEPATOCELLULAR DEATH 2. REGENERATION 3. PROGRESSIVE FIBROSIS 7
ALCOHOLIC LIVER DISEASE 1. HEPATIC STEATOSIS(FATTY CHANGE) 2. ALCOHOLIC HEPATITIS 3. ALCOHOLIC CIRRHOSIS 8
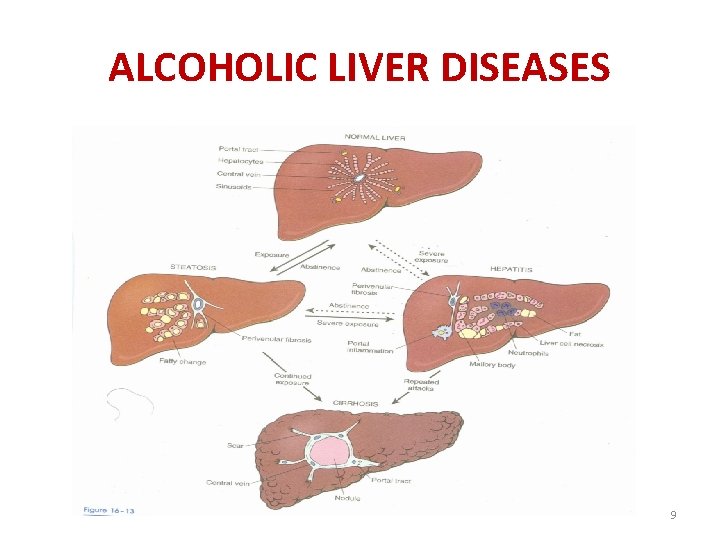
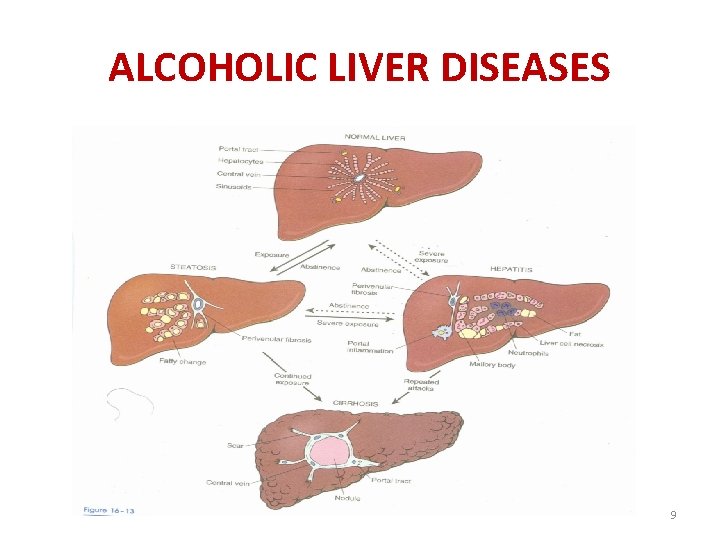
ALCOHOLIC LIVER DISEASES 9

PATHOGENESIS OF ALCOHOLIC LIVER DISEASE DETRIMENTAL EFFECTS OF ALCOHOL & ITS PRODUCTS. HEPATOCELLULAR STEATOSIS. RESULTS FROM SHUNTING OF NORMAL SUBSTRATE AWAY FROM CATABOLISM TOWARDS- LIPID BIOSYNTHESIS 10
PATHOGENESIS OF ALCOHOLIC LIVER DISEASE DETRIMENTAL EFFECTS OF ALCOHOL & ITS PRODUCTS. HEPATOCELLULAR STEATOSIS. RESULTS FROM SHUNTING OF NORMAL SUBSTRATE AWAY FROM CATABOLISM TOWARDS- LIPID BIOSYNTHESIS 11
PATHOGENESIS OF ALCOHOLIC LIVER DISEASE 1. INCREASED PERIPHERAL CATABOLISM OF FAT. 2. LIPID BIOSYNTHESIS BY THE ACTION OF ALCOHOL DEHYDROGENASE & ACETALDEHYDE DEHYDROGENASE. 3. DECREASED LIPOPROTEIN SECRETION 12

PATHOGENESIS CONTINEUD 4. FREE RADICAL GENERATED DURING OXIDATION OF ETHANOL BY MICROSOMAL ENZYMES INJURE THE HEPATOCYTE. 5. ALCOHOL DIRECTLY AFFECTS MICROTUBULAR & MITOCHONDRIAL FUNCTION - CAUSE INJURY TO HEPATOCYTE 13
PATHOGENESIS CONTINEUD 6. ACETALDEHYDE – LIPID PEROXIDATION – DISRUPTS CYTOSKELETAL & MEMBRANE FUNCTION. 7. OTHER FACTORS CAUSING INJURY TO HEPATOCYTES ARE-TOXIC OXYGEN METABOLITES FROM ACTIVATED NEUTROPHILS 14
OTHER FACTORS ACCELERATING ALCOHOLIC LIVER DISEASE MALNUTRITION & VITAMIN DEFICIENCY - SPECIALLY THIAMINE & VITAMINE B 12 DUE TO IMPAIRED DIGESTIVE FUNCTION DUE TO DAMAGE TO GASTRIC & INTESTINAL MUCOSA & PANCREATITIS. 15

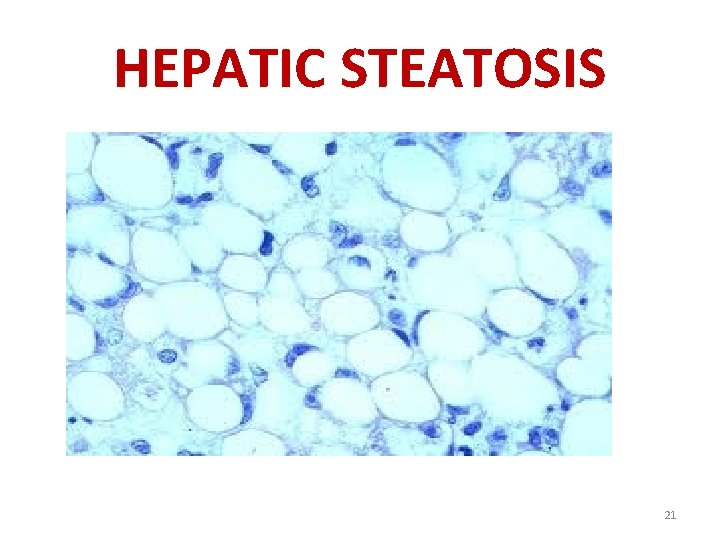
GROSS APPEARANCE OF LIVER IN HEPATIC STEATOSIS FATTY LIVER OF CHRONIC ALCOHOLISMLARGE UP TO 4 - 6 Kg SOFT , YELLOW , GREASY 16

HEPATIC STEATOSIS 17
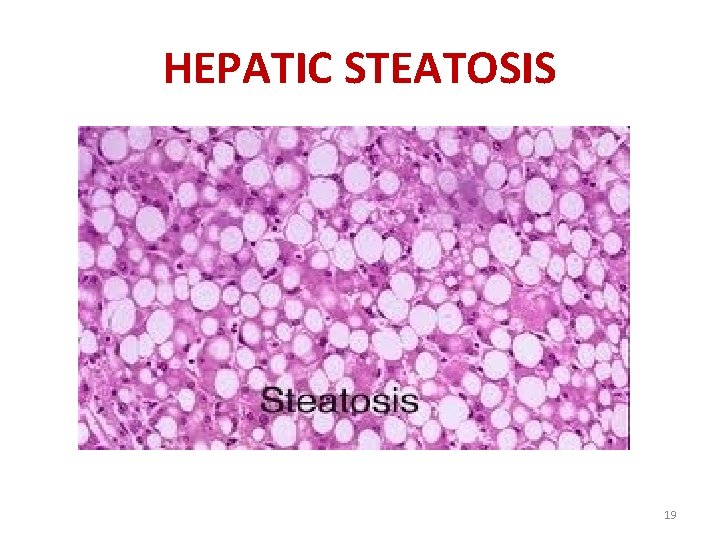
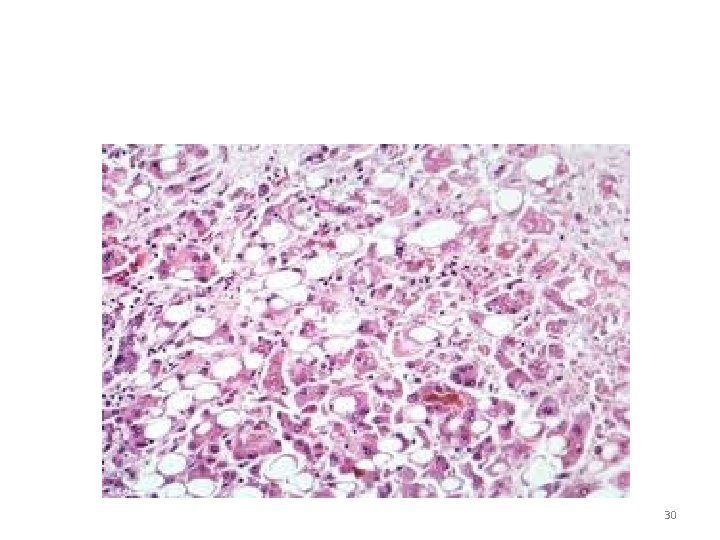
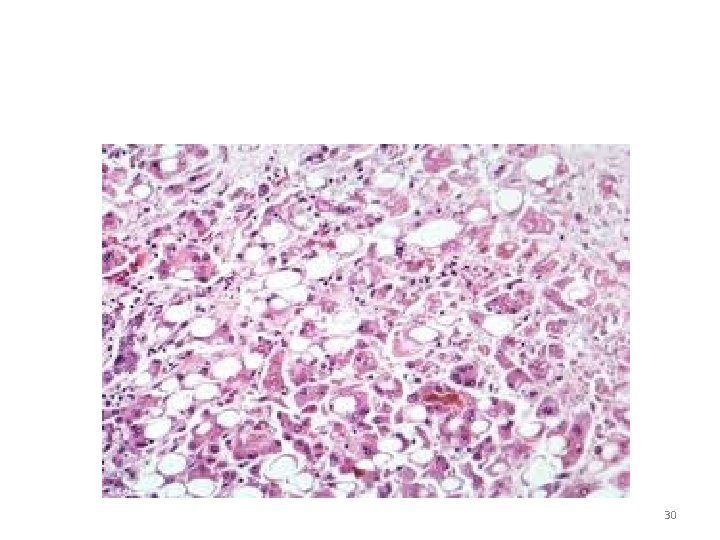
HEPATIC STEATOSIS REVERSIBLE- MICROSCOPIC FEATURES MICROVASICULAR MACROVASICULARCENTRILOBULAR INITIALLY CONTINUED INTAKE OF ALCOHOLFIBROSIS AROUND THE CENTRAL VEIN EXTENDING IN TO SINUSOIDS. 18
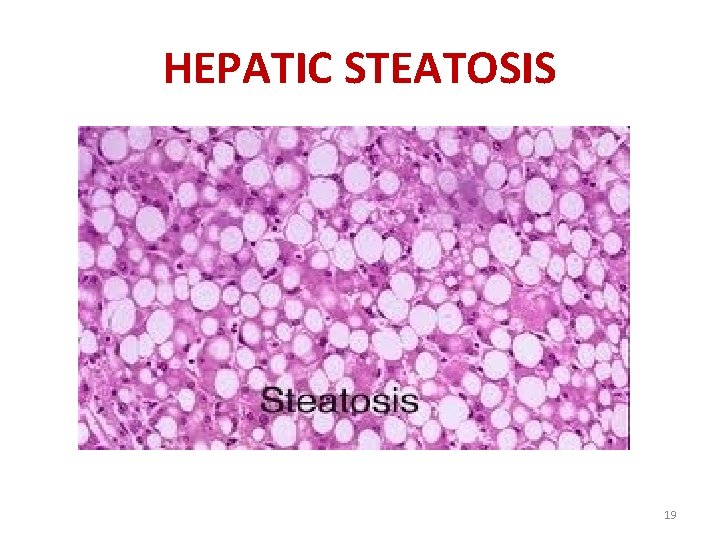
HEPATIC STEATOSIS 19

HEPATIC STEATOSIS 20
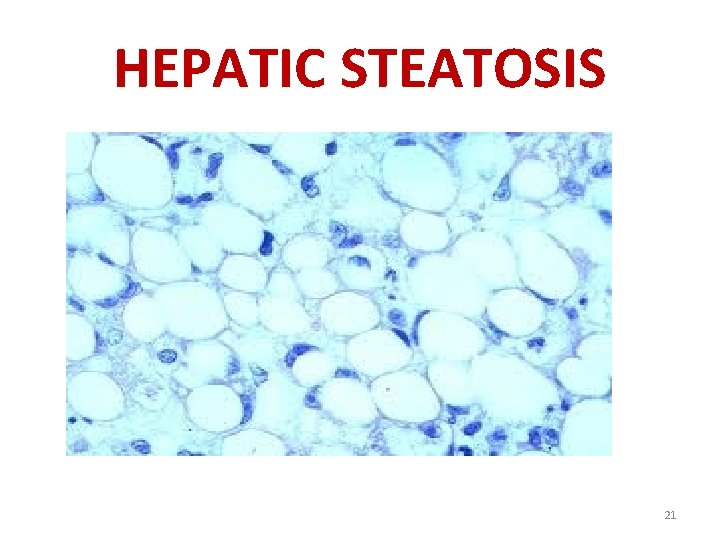
HEPATIC STEATOSIS 21
ALCOHOLIC HEPATITIS-GROSS LIVER – NORMAL OR INCREASED IN SIZE. MOTTLED RED GREENISH BILE STAINED AREAS. OFTEN – VISIBLE NODULES & FIBROSIS - INDICATIVE OF EVOLUTION OF CIRRHOSIS. 22
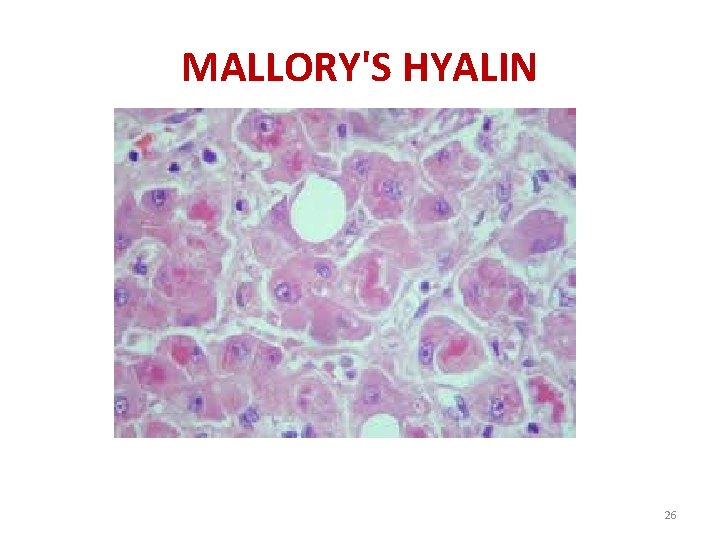
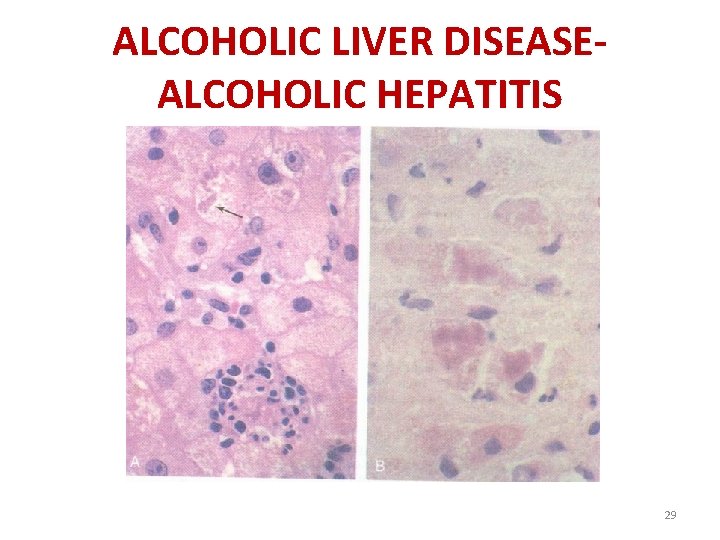
ALCOHOLIC HEPATITIS MICROSCOPY HEPATOCYTE SWELLING (BALLOONING –FAT & WATER ACCUMULATION) & SCATTERED FOCI OF NECROSIS. MALLORY BODIES(ACCUMULATION OF CYTOKERATIN INTERMEDIATE FILAMENTS)- EOSINOPHILIC INCLUSIONS IN THE CYTOPLASM OF DEGENERATING CELLS. 23
MALLORY'S HYALIN AN EOSINOPHILIC CYTOPLASMIC INCLUSION, ALCOHOLIC HYALIN, FOUND IN THE LIVER CELLS. IT IS TYPICALLY, BUT NOT ALWAYS, ASSOCIATED WITH ACUTE ALCOHOLIC LIVER INJURY. 24
MALLORY'S HYALIN THE GLOBULES ARE AGGREGATES OF INTERMEDIATE FILAMENTS IN THE CYTOPLASM RESULTING FROM HEPATOCYTE INJURY. 25
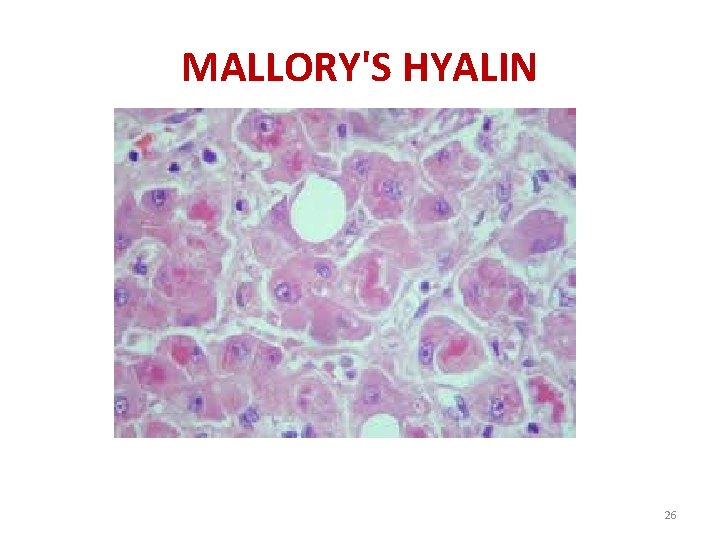
MALLORY'S HYALIN 26
MALLORY'S HYALIN • THEY ARE MOST COMMON IN ALCOHOLIC HEPATITIS (PREVALENCE OF 65%) AND ALCOHOLIC CIRRHOSIS (PREVALENCE OF 51%) • THEY ARE A RECOGNIZED FEATURE OF WILSON'S DISEASE (25%), PRIMARY BILIARY CIRRHOSIS (24%), HEPATOCELLULAR CARCINOMA (23%) AND MORBID OBESITY (8%) 27
ALCOHOLIC HEPATITIS MORPHOLOGY CONTINEUD NEUTROPHILIC REACTION , LYMPHOCYTES MACROPHAGES FIBROSIS – SINUSOIDAL PERIVENULAR FIBROSIS. CHOLESTASIS MILD HEMOSIDERIN DEPOSITION IN HEPATOCYTES & KUPFFER CELLS 28
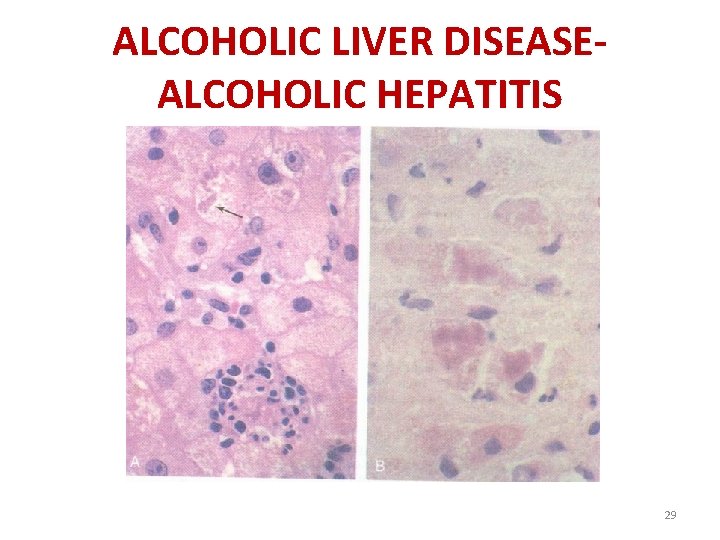
ALCOHOLIC LIVER DISEASEALCOHOLIC HEPATITIS 29
30
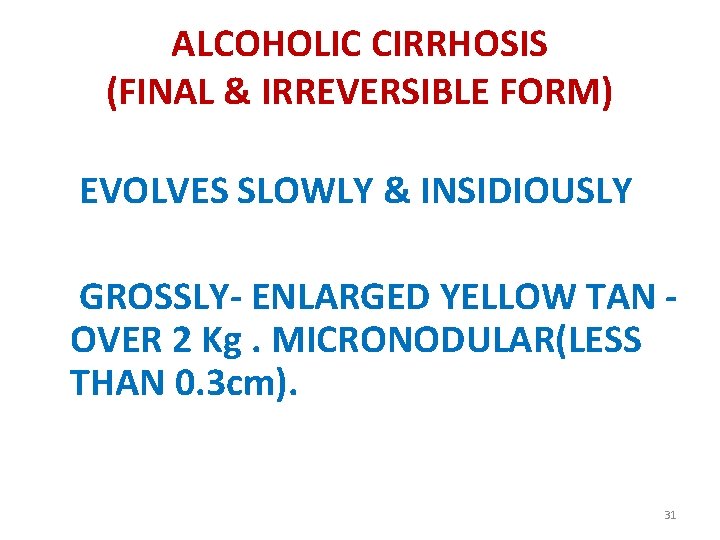
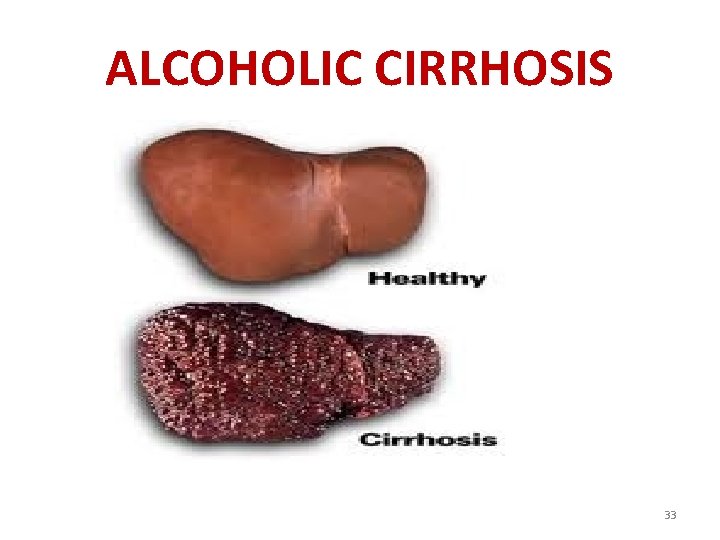
ALCOHOLIC CIRRHOSIS (FINAL & IRREVERSIBLE FORM) EVOLVES SLOWLY & INSIDIOUSLY GROSSLY- ENLARGED YELLOW TAN OVER 2 Kg. MICRONODULAR(LESS THAN 0. 3 cm). 31

ALCOHOLIC CIRRHOSIS (FINAL & IRREVERSIBLE FORM) WITH TIME LARGER NODULES - HOBNAIL APPEARANCE ON THE SURFACE. OVER THE SPAN OF YEARS –BROWN SHRUNKEN NONFATTY ORGAN LESS THAN 1 Kg (NORMAL -1. 5 Kg) – ENDSTAGE ALCOHOLIC CIRRHOSIS 32
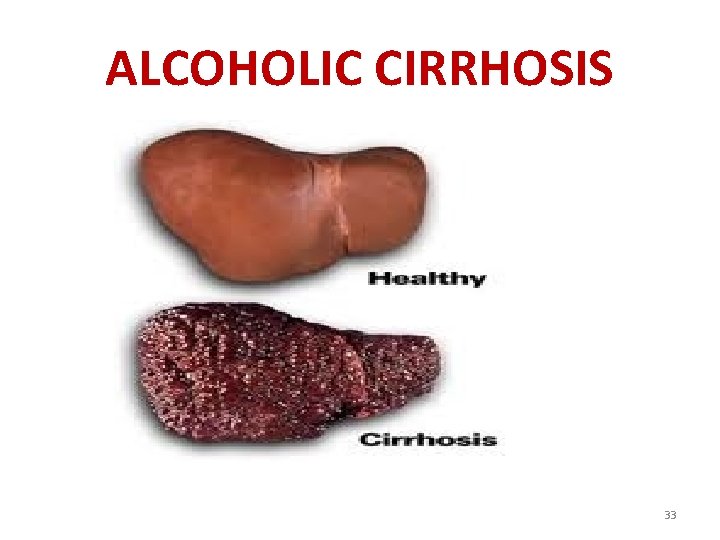
ALCOHOLIC CIRRHOSIS 33
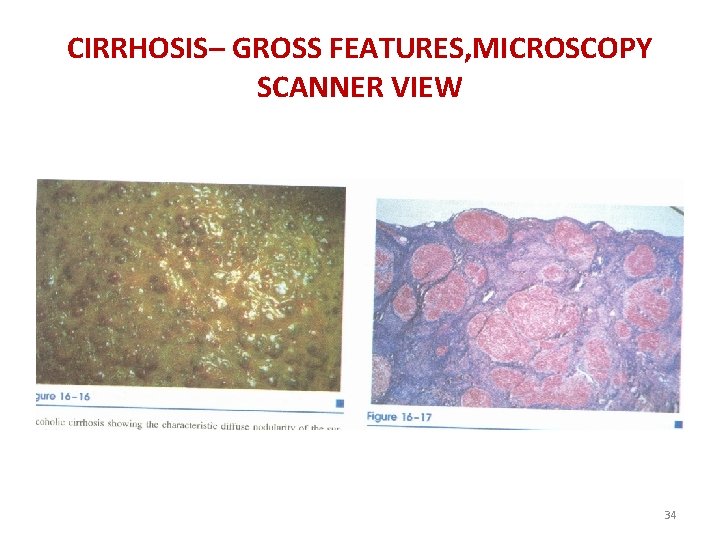
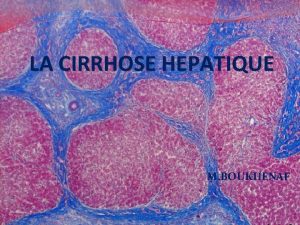
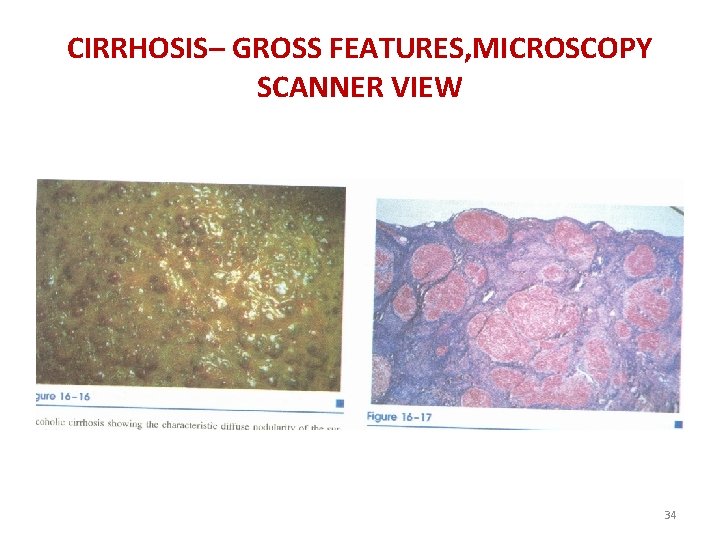
CIRRHOSIS– GROSS FEATURES, MICROSCOPY SCANNER VIEW 34
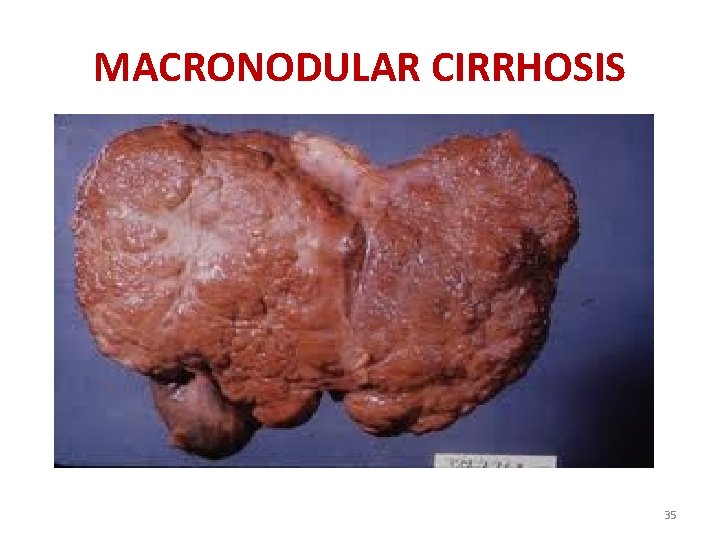
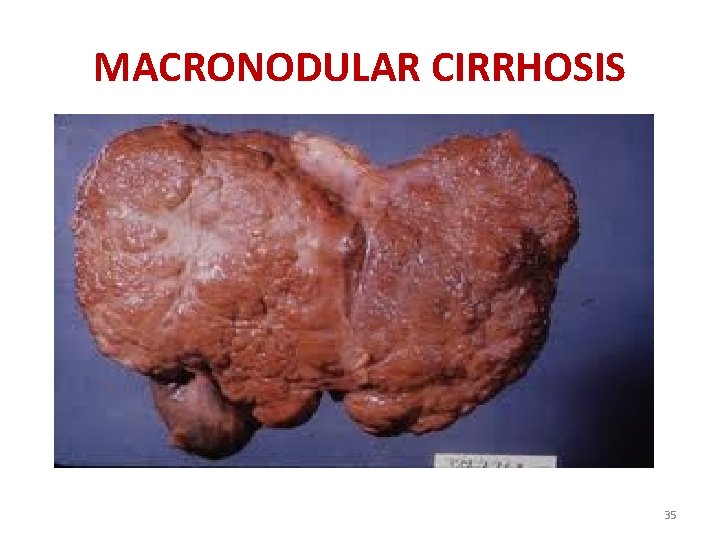
MACRONODULAR CIRRHOSIS 35

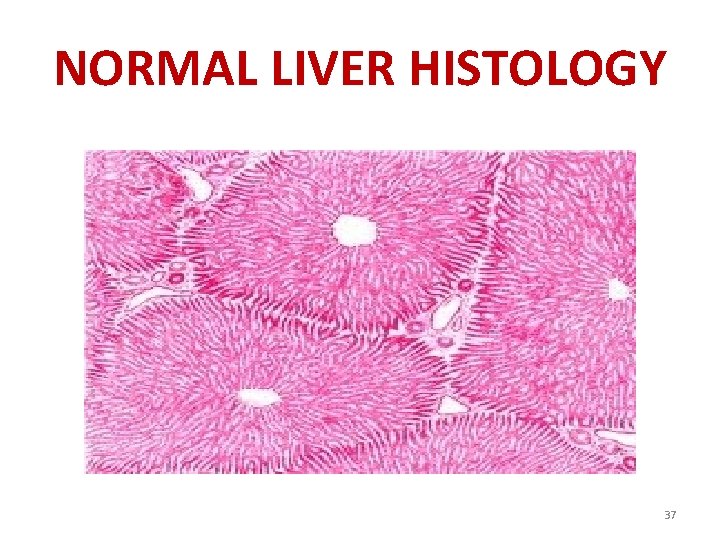
NORMAL LIVER HISTOLOGY 36
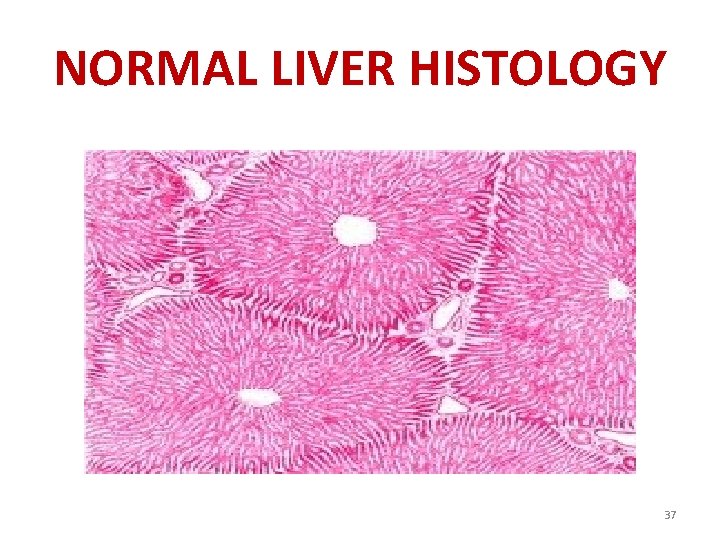
NORMAL LIVER HISTOLOGY 37
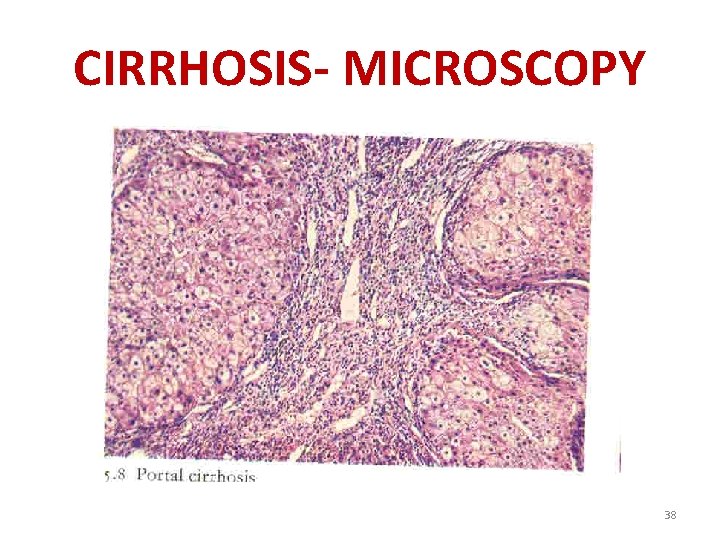
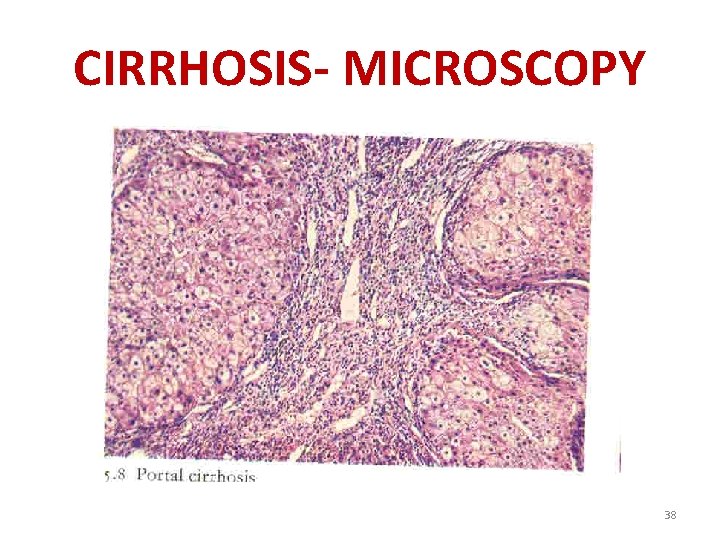
CIRRHOSIS- MICROSCOPY 38
CLINICAL FEATURES HEPATIC STEATOSIS – MILD INCREASED BILIRUBIN & ALKALINE PHOSPHATASE 39

ALCOHOLIC HEPATITIS ACUTE ONSET AFTER A BOUT OF HEAVY DRINKING, MAY BE SEVERE-FULMINANT HEPATIC FAILURE. 40
ALCOHOLIC HEPATITIS LABORATORY INVESTIGATIONS 1. HYPERBILIRUBINEMIA 2. ELEVATED ALKALINE PHOSPHATASE 3. NEUTROPHILIC LEUKOCYTOSIS. 41
ALCOHOLIC HEPATITIS 4. ELEVATED ALENINE AMINOTRANSFERASE (ALT, ALSO KNOWN AS SGPT) & ASPERTATATE AMINOTRANSFERASE(AST , ALSO KNOWN AS SGOT) 42
CLINICAL FEATURES MALAISE , ANOREXIA , WEIGHT LOSS UPPER ABDOMINAL DISCOMFORT, TENDERNESS HEPATOMEGALY - FEVER 43
PROGNOSIS OF ALCOHOLIC HEPATITIS UNPREDICTABLE EACH BOUT CARRIES-10% -20 % RISK OF DEATH CAN SUPERIMPOSED ON CIRRHOSIS PROPER NUTRITION & CESSATION OF ALCOHOL CONSUMPTION ALCOHOLIC HEPATITIS MAY CLEAR SLOWLY 44
CLINICAL FEATURES OF ALCOHOLIC CIRRHOSIS FIRST SIGN IS RELATED TO PORTAL HYPERTENTION – ASCITIS, WASTED EXTREMITIES, CAPUT MEDOSE OR FIRST PRESENTATION MAY BE LIFE THREATENING VARICEAL HEMORRHAGE DEATH 45
HEPATIC ENCEPHALOPATHY IS A DISORDER OF MENTAL ACTIVITY, NEUROMUSCULAR FUNCTION AND CONSCIOUSNESS THAT OCCURS AS A RESULT OF EITHER CHRONIC OR ACUTE LIVER FAILUR EVENTUALLY LEAD TO COMA DUE TO FAILURE OF DETOXICATING FUNCTION OF LIVER(MAINLY INCREASE IN BLOOD AMMONIA) 46
CAPUT MEDUSAE IS THE APPEARANCE OF DISTENDED AND ENGORGED PARAUMBILICAL VEINS, WHICH ARE SEEN RADIATING FROM THE UMBILICUS ACROSS THE ABDOMEN TO JOIN SYSTEMIC VEINS. THE NAME CAPUT MEDUSAE ORIGINATES FROM THE APPARENT SIMILARITY TO MEDUSA'S HAIR(GREEK MYTHOLOGY FIGURE) 47
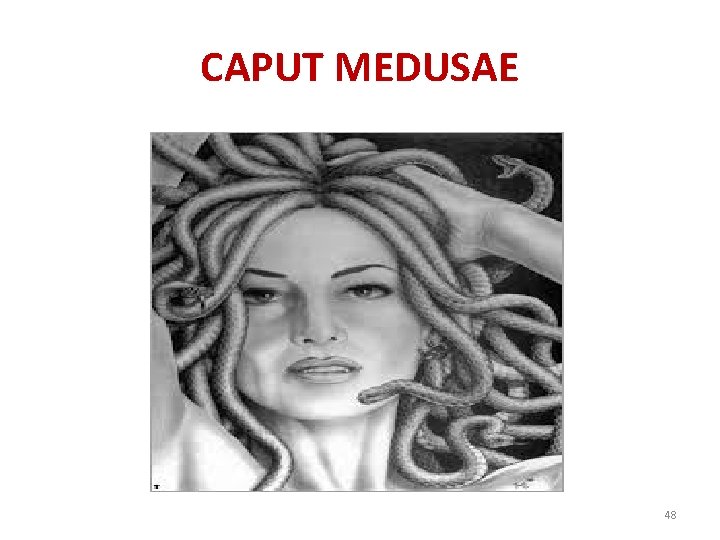
CAPUT MEDUSAE 48

LABORATORY FINDINGS IN ALCOHOLIC CIRRHOSIS 1. ELEVATED AMINOTRANSFERASE 2. HYPERBILIRUBINEMIA 3. VARIABLE ELEVATION OF ALKALINE PHOSPHATASE 4. HYPOPROTEINEMIA 5. ANEMIA 49

CAUSES OF DEATH 1. MASSIVE GIT HEMORRHAGE –FROM ESOPHAGEAL VARICES 2. HEPATIC FAILURE 3. INTERCURRENT INFECTION 4. HEPATORENAL SYNDROME AFTER A BOUT OF ALCOHOLIC HEPATITIS 5. HEPATOCELLULAR CARCINOMA – 3%-6% OF CASES 50
 Defination of liver
Defination of liver Stigmata of chronic liver disease
Stigmata of chronic liver disease Stigmata of portal hypertension
Stigmata of portal hypertension Stigmata of chronic liver disease
Stigmata of chronic liver disease Nonalcoholic fatty liver disease
Nonalcoholic fatty liver disease Complication of liver cirrhosis
Complication of liver cirrhosis Why does liver disease cause splenomegaly
Why does liver disease cause splenomegaly Complication of liver cirrhosis
Complication of liver cirrhosis Liver cirrhosis stages
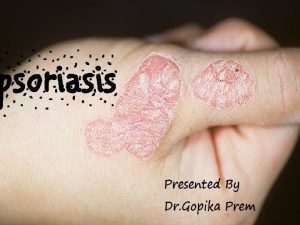
Liver cirrhosis stages Primary biliary cholangitis skin
Primary biliary cholangitis skin Hepatocirhosis
Hepatocirhosis Liver cirrhosis
Liver cirrhosis Pes statement for liver cirrhosis
Pes statement for liver cirrhosis Pes statement for liver cirrhosis
Pes statement for liver cirrhosis Types of cirrhosis
Types of cirrhosis Shifting dullness ascites
Shifting dullness ascites Hobnail fibrotic liver
Hobnail fibrotic liver Circulatory disturbances pathology
Circulatory disturbances pathology Chronic granulomatous disease
Chronic granulomatous disease Jewish chronic disease hospital
Jewish chronic disease hospital Chronic kidney disease near atwater
Chronic kidney disease near atwater Chronic kidney disease near oakley
Chronic kidney disease near oakley Kate lorig chronic disease self-management
Kate lorig chronic disease self-management Wagner's chronic care model
Wagner's chronic care model Chronic disease
Chronic disease Chronic disease
Chronic disease Copd medical abbreviation
Copd medical abbreviation Chronic rheumatic heart disease
Chronic rheumatic heart disease Decompensated liver disease
Decompensated liver disease Non-alcoholic fatty liver disease (nafld)
Non-alcoholic fatty liver disease (nafld) Portal hypertension signs
Portal hypertension signs Gennifer shafer liver disease
Gennifer shafer liver disease Alcoholic liver disease
Alcoholic liver disease Infiltrative liver disease
Infiltrative liver disease Bharathi viswanathan
Bharathi viswanathan Hepatic coma diet
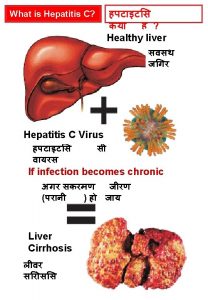
Hepatic coma diet What is cirrhosis
What is cirrhosis Micronodular cirrhosis vs macronodular
Micronodular cirrhosis vs macronodular Hyperestrinism cirrhosis
Hyperestrinism cirrhosis Gastrointestinalis
Gastrointestinalis Cirrhosis care near woodland
Cirrhosis care near woodland Nor-ursodeoxycholsäure
Nor-ursodeoxycholsäure Can ct scan miss cirrhosis
Can ct scan miss cirrhosis Cirrhosis
Cirrhosis Easl 2018 guidelines
Easl 2018 guidelines Definition of chronic toxicity
Definition of chronic toxicity Chronic care model definition
Chronic care model definition Definition of chronic toxicity
Definition of chronic toxicity Chronic pain definition
Chronic pain definition Esv and edv
Esv and edv Preload stroke volume
Preload stroke volume