Viral Hepatitis Liver Anatomy o o Liver is





- Slides: 60
Viral Hepatitis
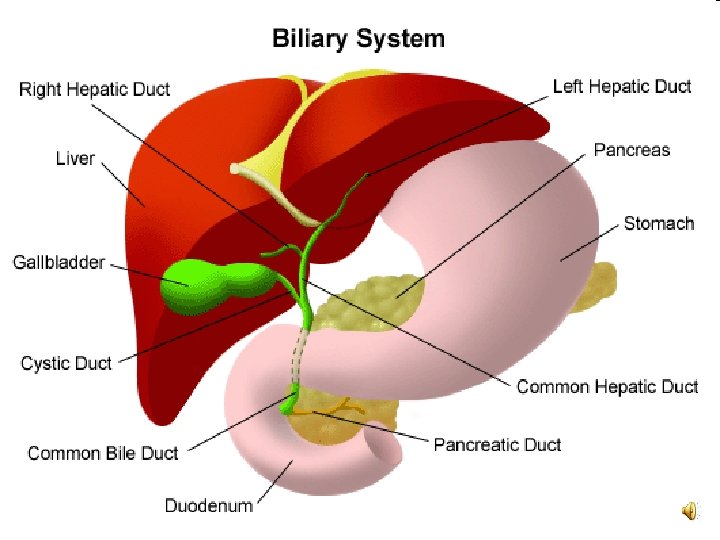
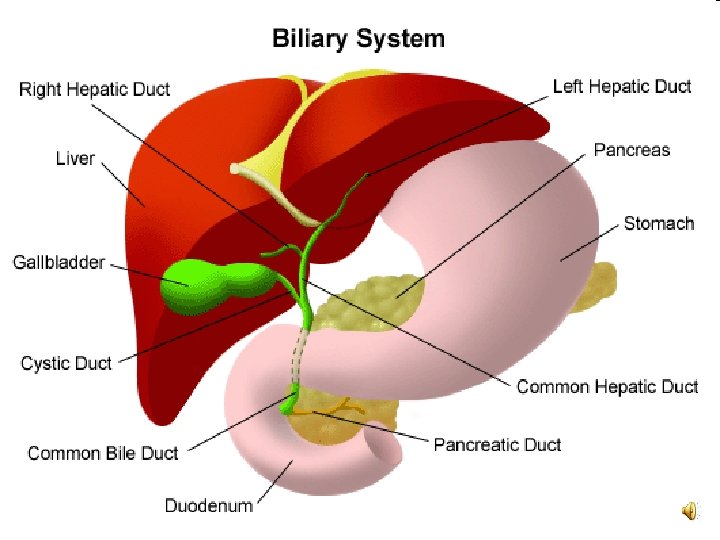
Liver Anatomy… o o Liver is the largest and most versatile organ in the body, The liver is located just below the diaphragm (the muscular membrane separating the chest from the abdomen), in the right upper quadrant of the abdomin.

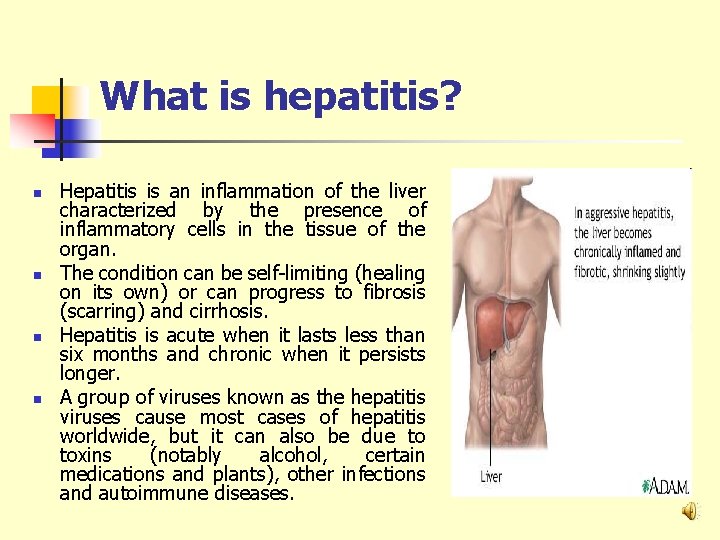
What is hepatitis? n n Hepatitis is an inflammation of the liver characterized by the presence of inflammatory cells in the tissue of the organ. The condition can be self-limiting (healing on its own) or can progress to fibrosis (scarring) and cirrhosis. Hepatitis is acute when it lasts less than six months and chronic when it persists longer. A group of viruses known as the hepatitis viruses cause most cases of hepatitis worldwide, but it can also be due to toxins (notably alcohol, certain medications and plants), other infections and autoimmune diseases.
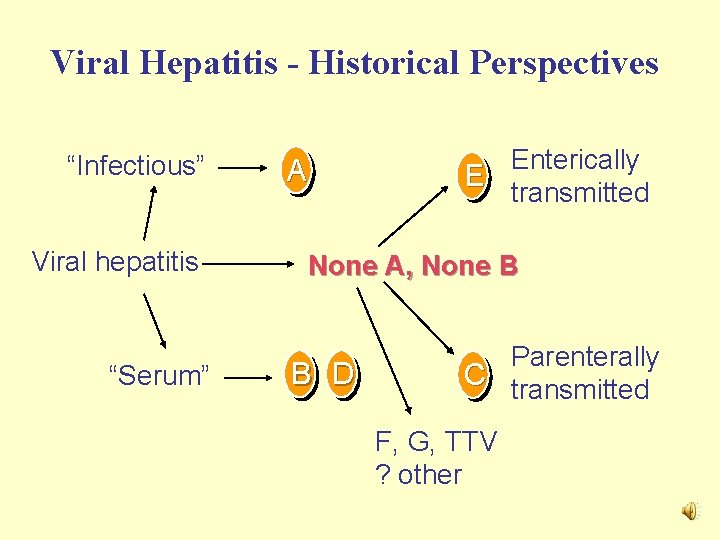
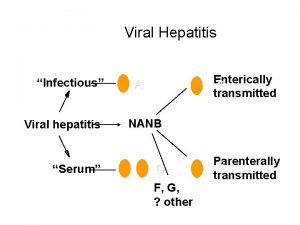
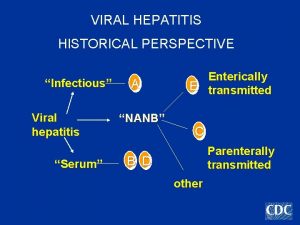
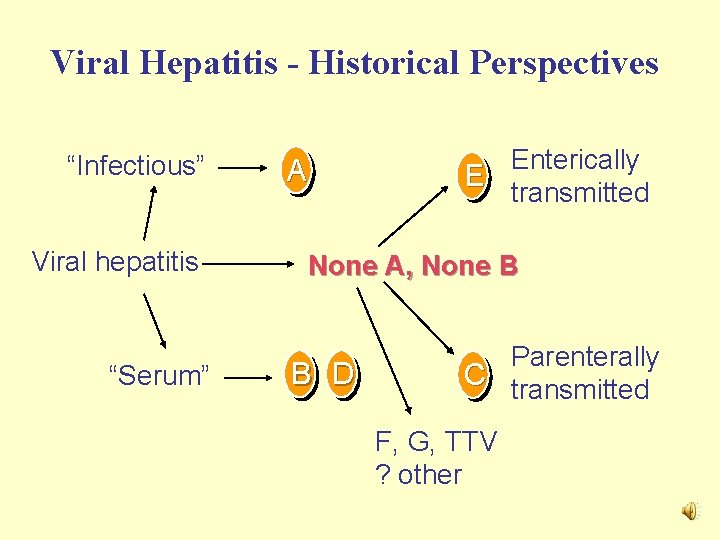
Viral Hepatitis - Historical Perspectives “Infectious” Viral hepatitis “Serum” A Enterically E transmitted None A, None B B D Parenterally C transmitted F, G, TTV ? other
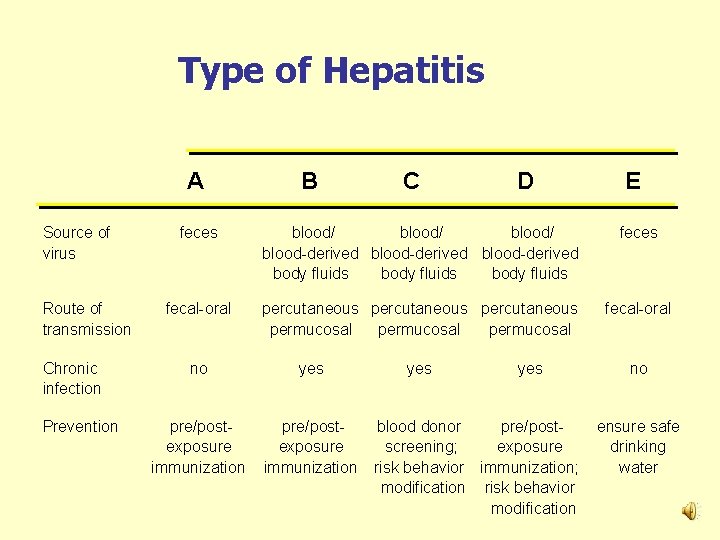
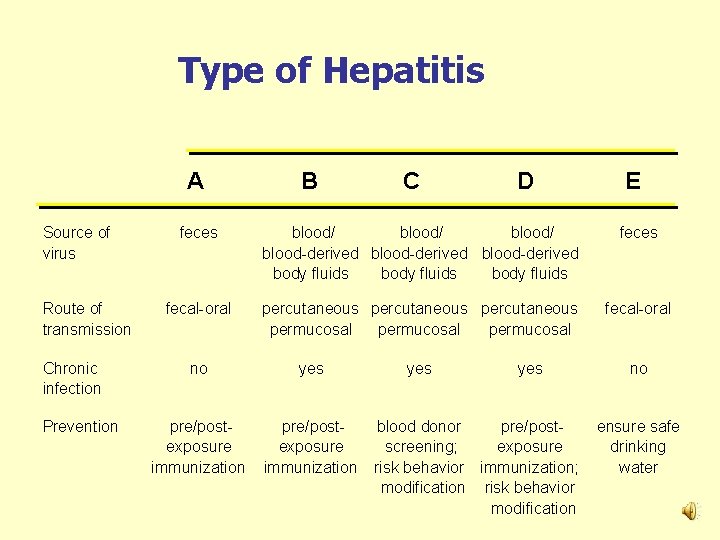
Type of Hepatitis A Source of virus Route of transmission Chronic infection Prevention B C D E feces blood/ blood-derived body fluids feces fecal-oral percutaneous permucosal fecal-oral no yes pre/postexposure immunization yes blood donor pre/postscreening; exposure risk behavior immunization; modification risk behavior modification no ensure safe drinking water
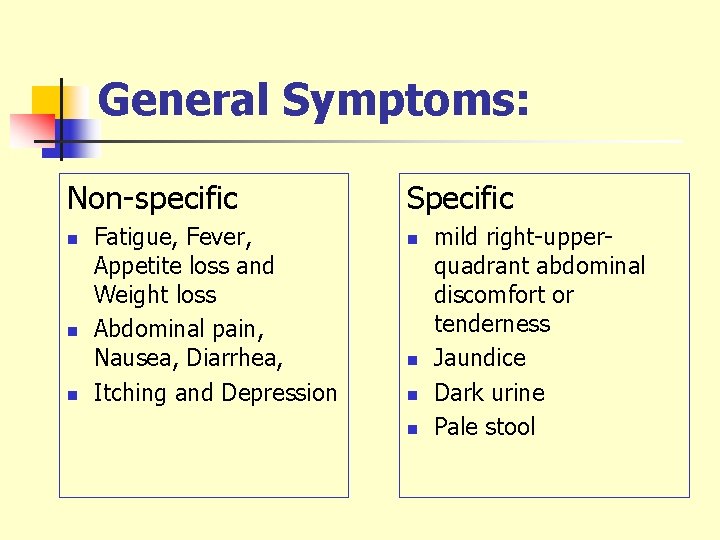
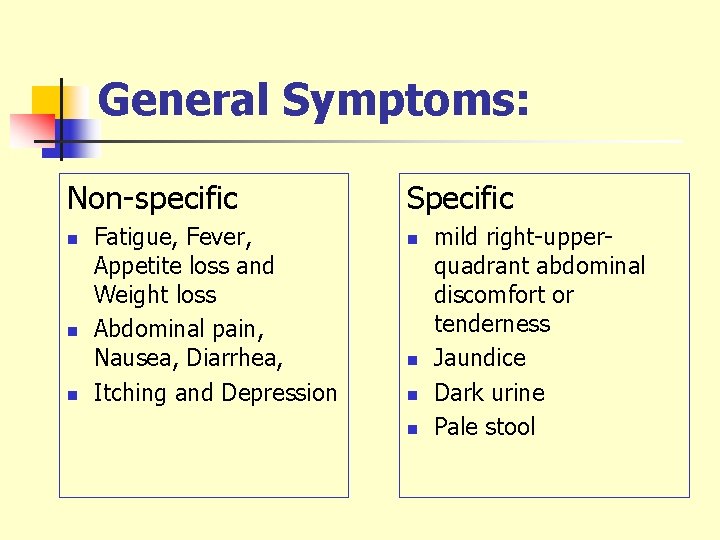
General Symptoms: Non-specific n n n Fatigue, Fever, Appetite loss and Weight loss Abdominal pain, Nausea, Diarrhea, Itching and Depression Specific n n mild right-upperquadrant abdominal discomfort or tenderness Jaundice Dark urine Pale stool
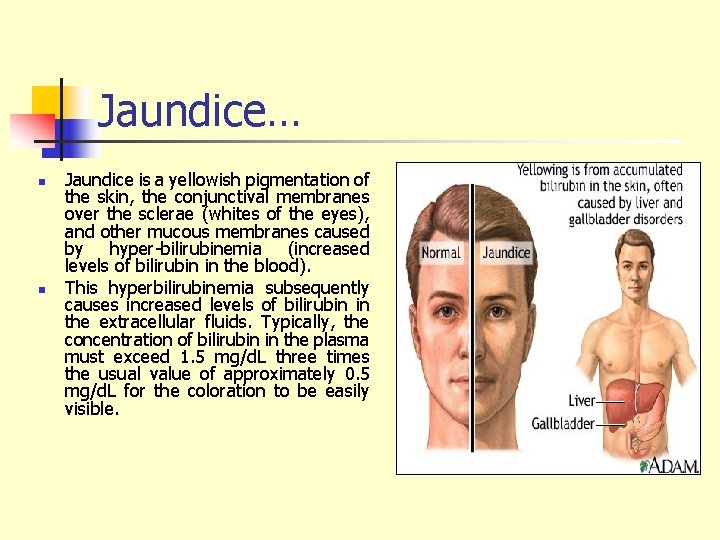
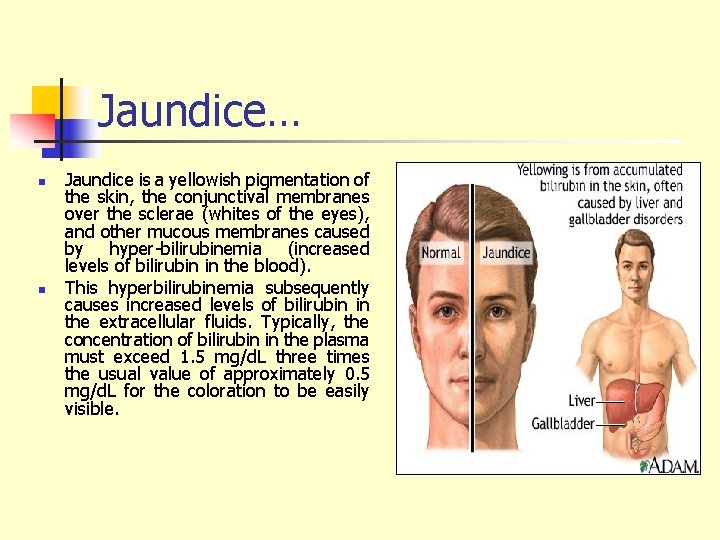
Jaundice… n n Jaundice is a yellowish pigmentation of the skin, the conjunctival membranes over the sclerae (whites of the eyes), and other mucous membranes caused by hyper-bilirubinemia (increased levels of bilirubin in the blood). This hyperbilirubinemia subsequently causes increased levels of bilirubin in the extracellular fluids. Typically, the concentration of bilirubin in the plasma must exceed 1. 5 mg/d. L three times the usual value of approximately 0. 5 mg/d. L for the coloration to be easily visible.

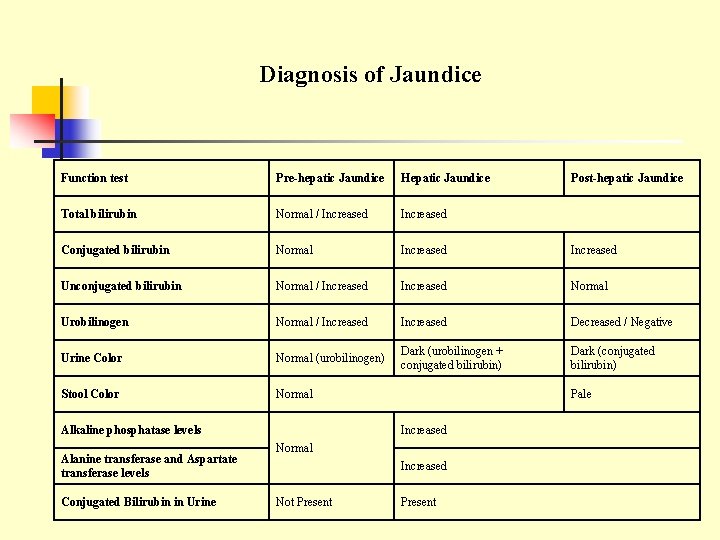
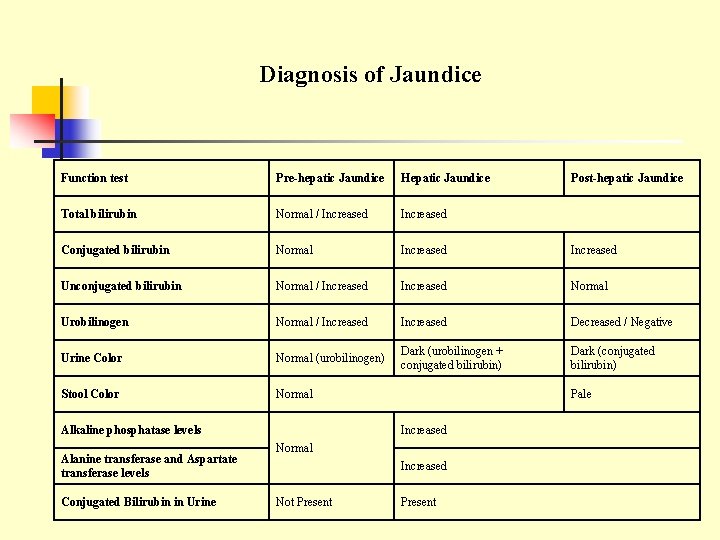
Diagnosis of Jaundice Function test Pre-hepatic Jaundice Hepatic Jaundice Total bilirubin Normal / Increased Conjugated bilirubin Normal Increased Unconjugated bilirubin Normal / Increased Normal Urobilinogen Normal / Increased Decreased / Negative Urine Color Normal (urobilinogen) Dark (urobilinogen + conjugated bilirubin) Dark (conjugated bilirubin) Stool Color Normal Alkaline phosphatase levels Alanine transferase and Aspartate transferase levels Conjugated Bilirubin in Urine Pale Increased Normal Increased Not Present Post-hepatic Jaundice Present
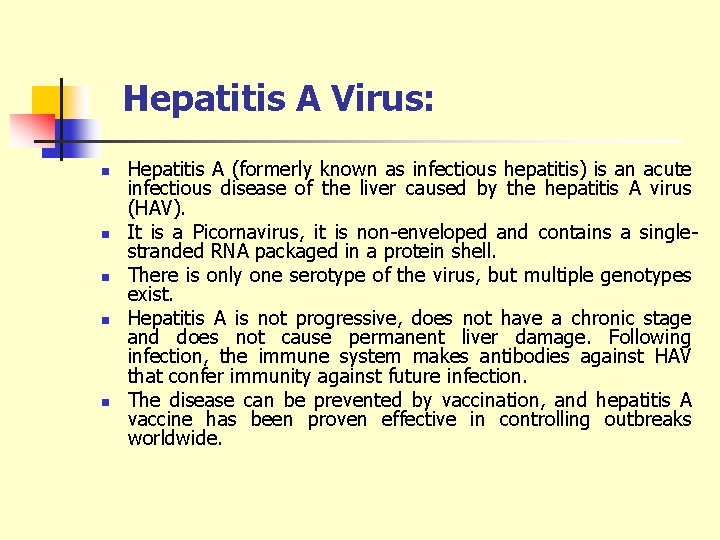
Hepatitis A Virus
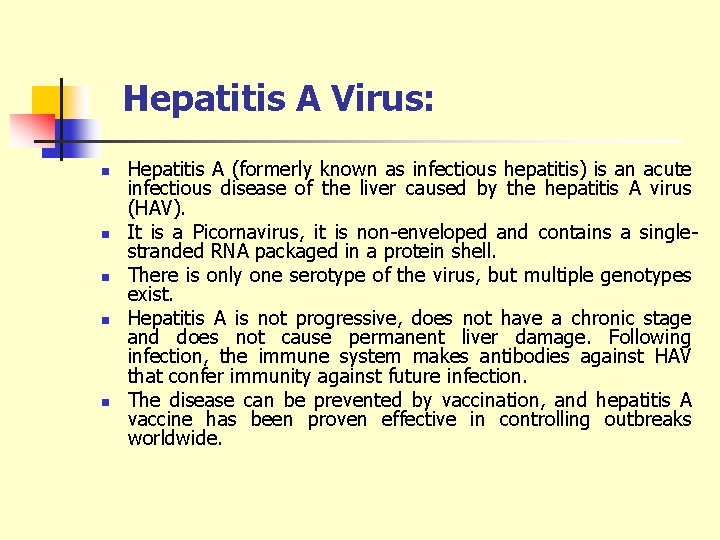
Hepatitis A Virus: n n n Hepatitis A (formerly known as infectious hepatitis) is an acute infectious disease of the liver caused by the hepatitis A virus (HAV). It is a Picornavirus, it is non-enveloped and contains a singlestranded RNA packaged in a protein shell. There is only one serotype of the virus, but multiple genotypes exist. Hepatitis A is not progressive, does not have a chronic stage and does not cause permanent liver damage. Following infection, the immune system makes antibodies against HAV that confer immunity against future infection. The disease can be prevented by vaccination, and hepatitis A vaccine has been proven effective in controlling outbreaks worldwide.
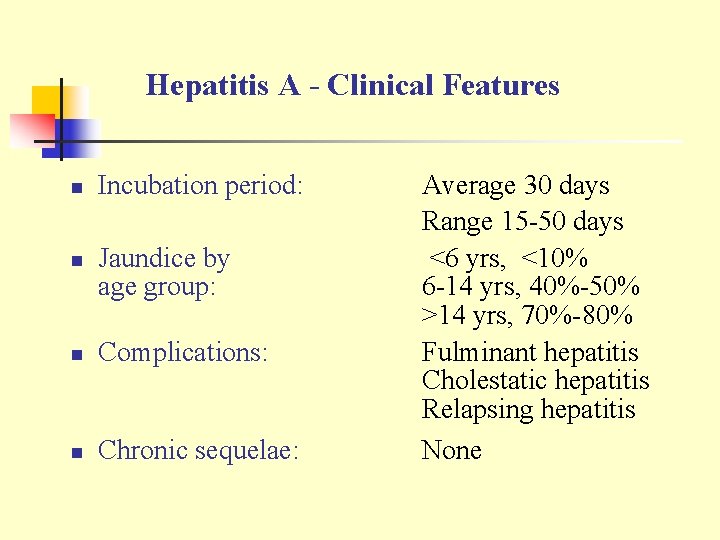
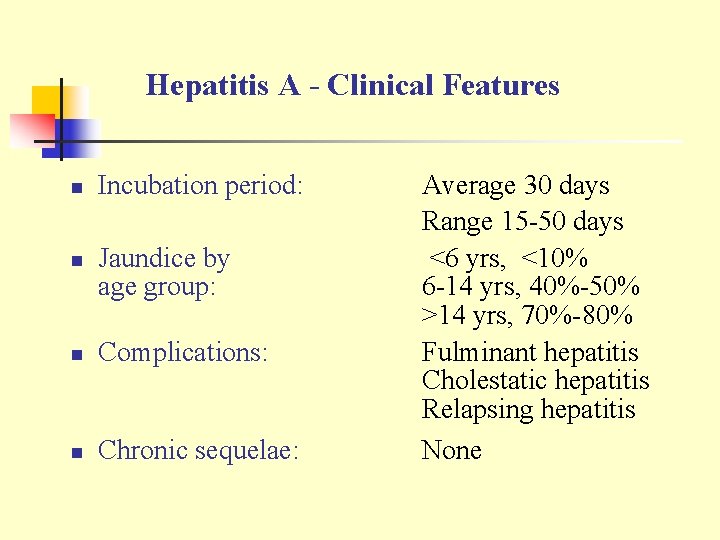
Hepatitis A - Clinical Features n n Incubation period: Jaundice by age group: n Complications: n Chronic sequelae: Average 30 days Range 15 -50 days <6 yrs, <10% 6 -14 yrs, 40%-50% >14 yrs, 70%-80% Fulminant hepatitis Cholestatic hepatitis Relapsing hepatitis None
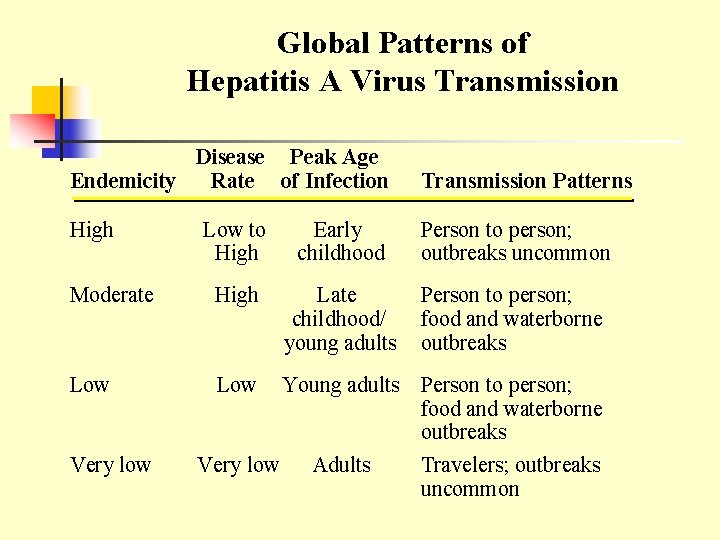
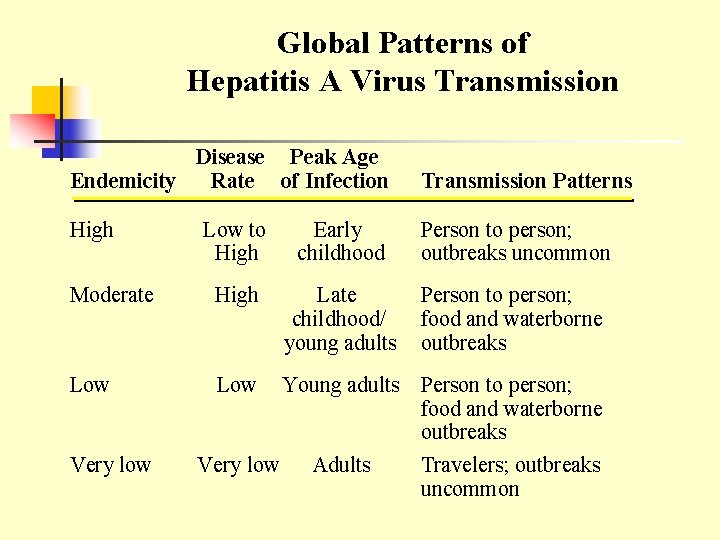
Global Patterns of Hepatitis A Virus Transmission Disease Peak Age Endemicity Rate of Infection High Transmission Patterns Low to High Early childhood Person to person; outbreaks uncommon Moderate High Late childhood/ young adults Person to person; food and waterborne outbreaks Low Very low Young adults Person to person; food and waterborne outbreaks Very low Adults Travelers; outbreaks uncommon

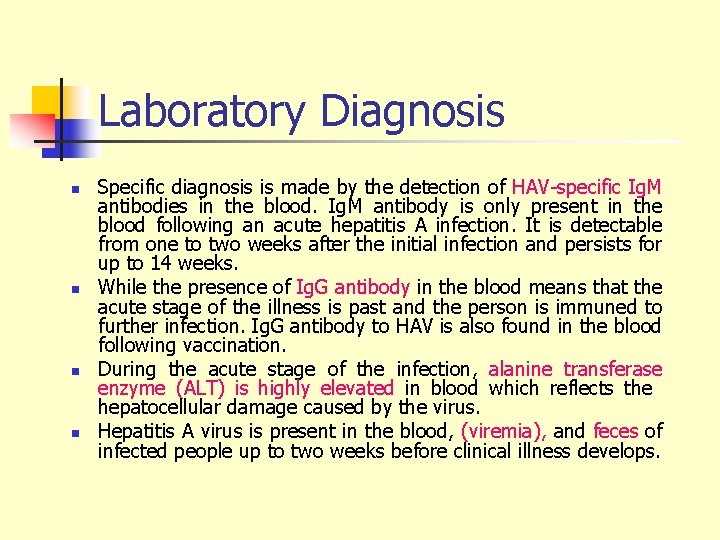
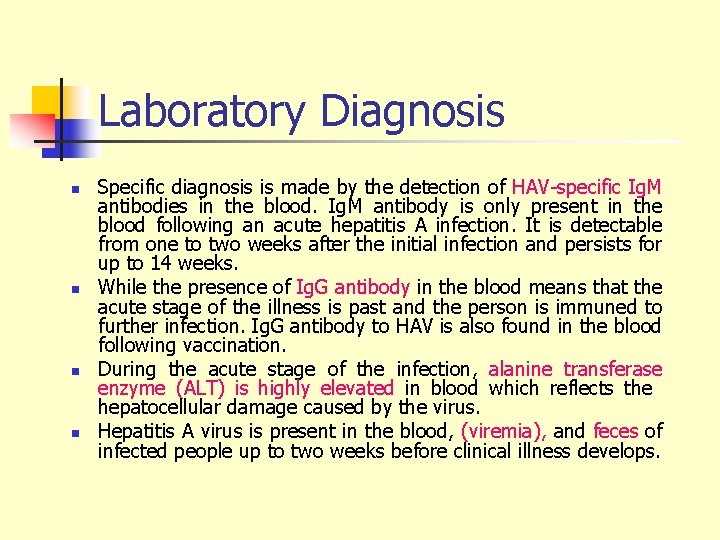
Laboratory Diagnosis n n Specific diagnosis is made by the detection of HAV-specific Ig. M antibodies in the blood. Ig. M antibody is only present in the blood following an acute hepatitis A infection. It is detectable from one to two weeks after the initial infection and persists for up to 14 weeks. While the presence of Ig. G antibody in the blood means that the acute stage of the illness is past and the person is immuned to further infection. Ig. G antibody to HAV is also found in the blood following vaccination. During the acute stage of the infection, alanine transferase enzyme (ALT) is highly elevated in blood which reflects the hepatocellular damage caused by the virus. Hepatitis A virus is present in the blood, (viremia), and feces of infected people up to two weeks before clinical illness develops.
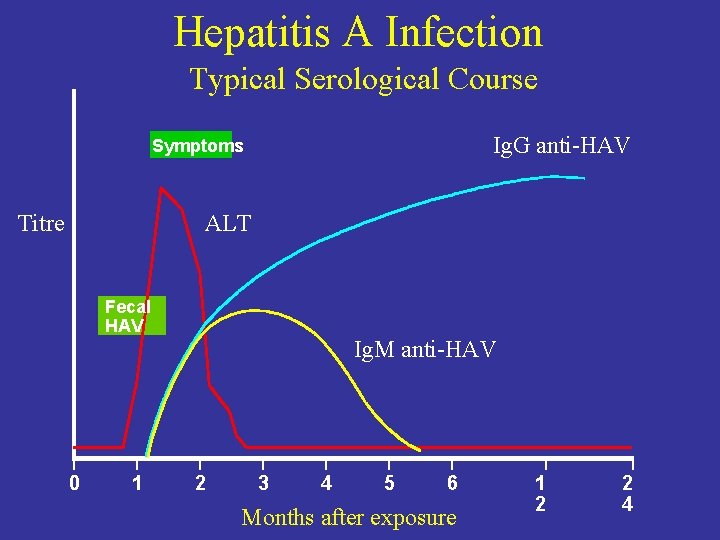
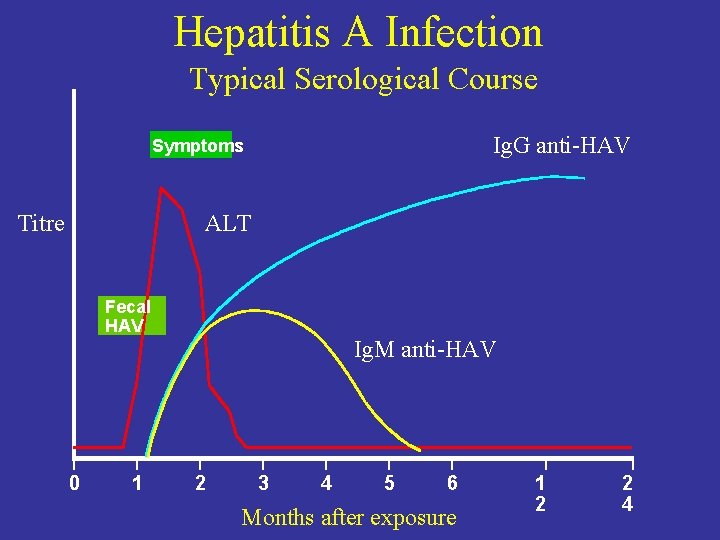
Hepatitis A Infection Typical Serological Course Ig. G anti-HAV Symptoms Titre ALT Fecal HAV 0 1 Ig. M anti-HAV 2 3 4 5 6 Months after exposure 1 2 2 4
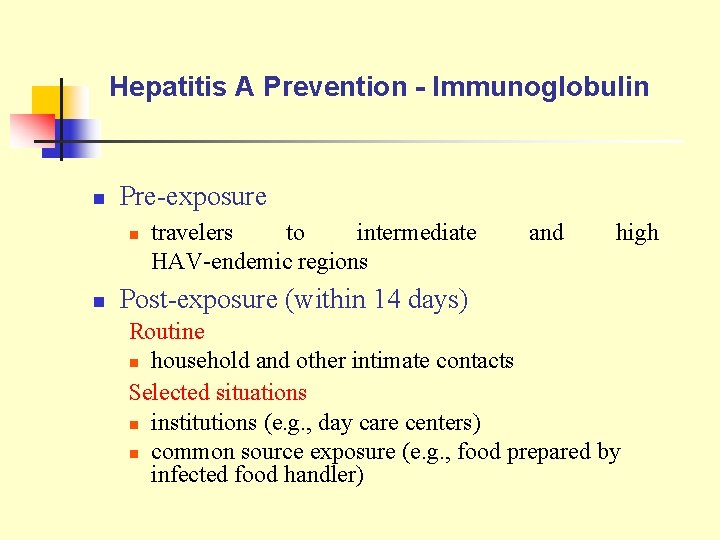
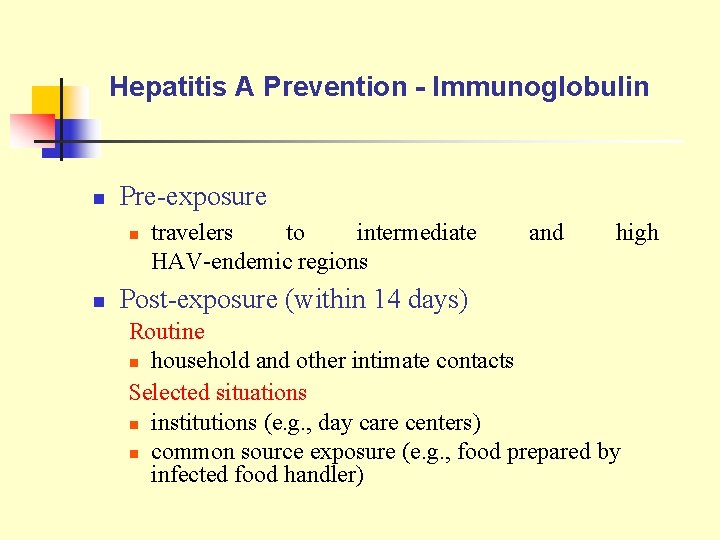
Hepatitis A Prevention - Immunoglobulin n Pre-exposure n n travelers to intermediate HAV-endemic regions and high Post-exposure (within 14 days) Routine n household and other intimate contacts Selected situations n institutions (e. g. , day care centers) n common source exposure (e. g. , food prepared by infected food handler)
Treatment… n n There is no specific treatment for hepatitis A. Patients are advised to rest, avoid fatty foods and alcohol (these may be poorly tolerated for some additional months during the recovery phase and cause minor relapses), eat a well-balanced diet, and stay hydrated.
Hepatitis B Virus
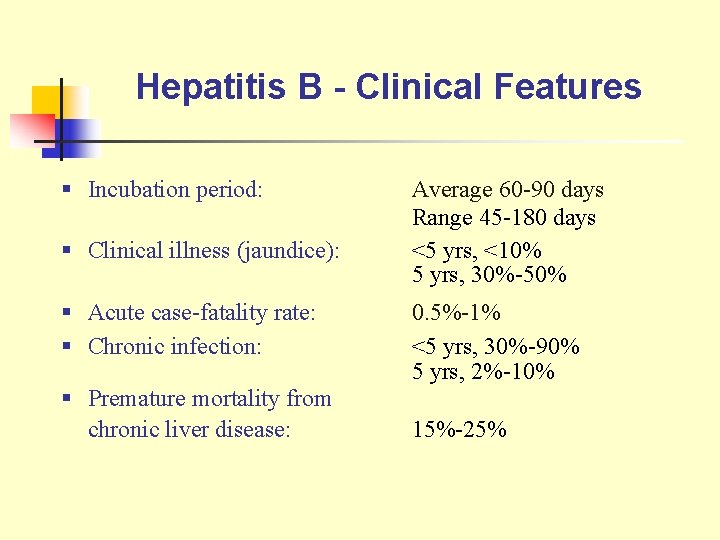
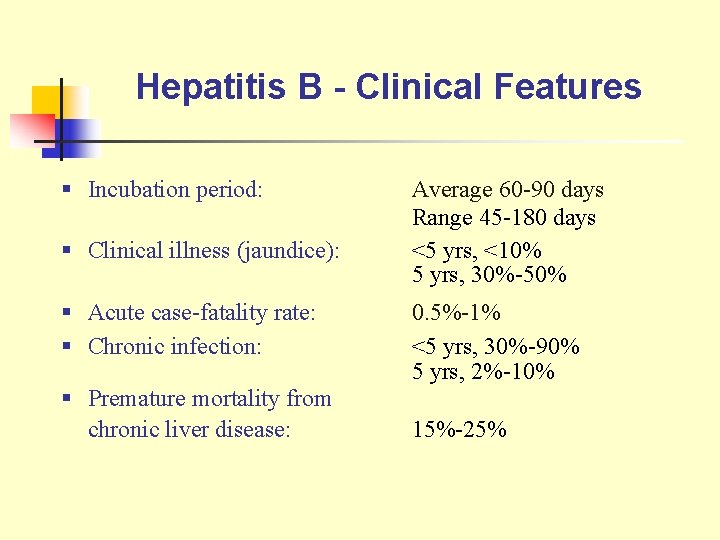
Hepatitis B - Clinical Features § Incubation period: § Clinical illness (jaundice): § Acute case-fatality rate: § Chronic infection: § Premature mortality from chronic liver disease: Average 60 -90 days Range 45 -180 days <5 yrs, <10% 5 yrs, 30%-50% 0. 5%-1% <5 yrs, 30%-90% 5 yrs, 2%-10% 15%-25%

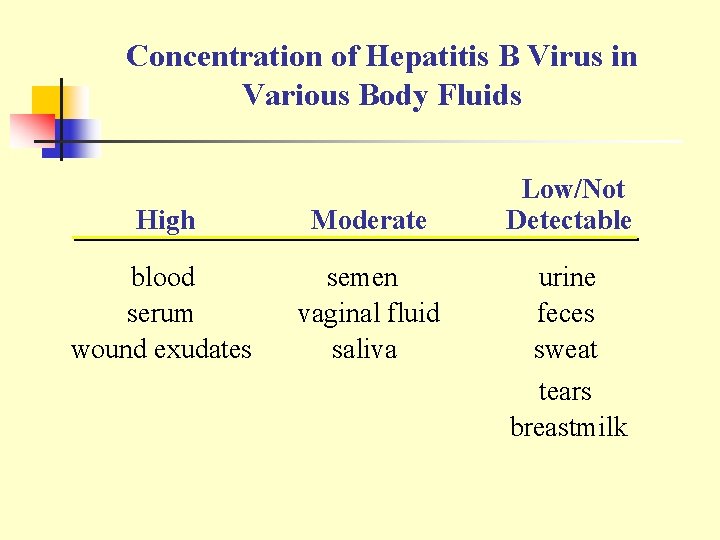
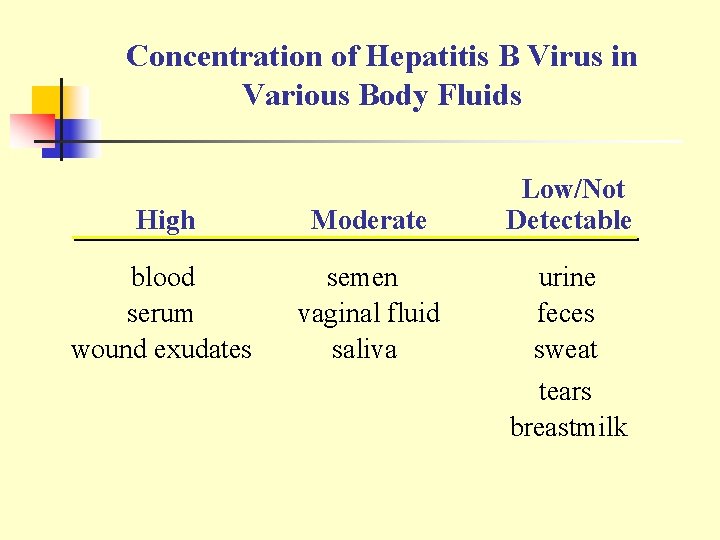
Concentration of Hepatitis B Virus in Various Body Fluids High Moderate blood serum wound exudates semen vaginal fluid saliva Low/Not Detectable urine feces sweat tears breastmilk
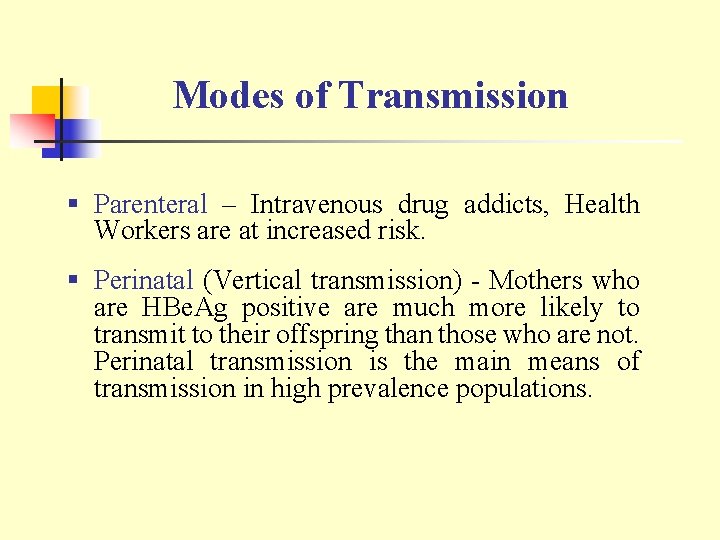
Modes of Transmission § Parenteral – Intravenous drug addicts, Health Workers are at increased risk. § Perinatal (Vertical transmission) - Mothers who are HBe. Ag positive are much more likely to transmit to their offspring than those who are not. Perinatal transmission is the main means of transmission in high prevalence populations.
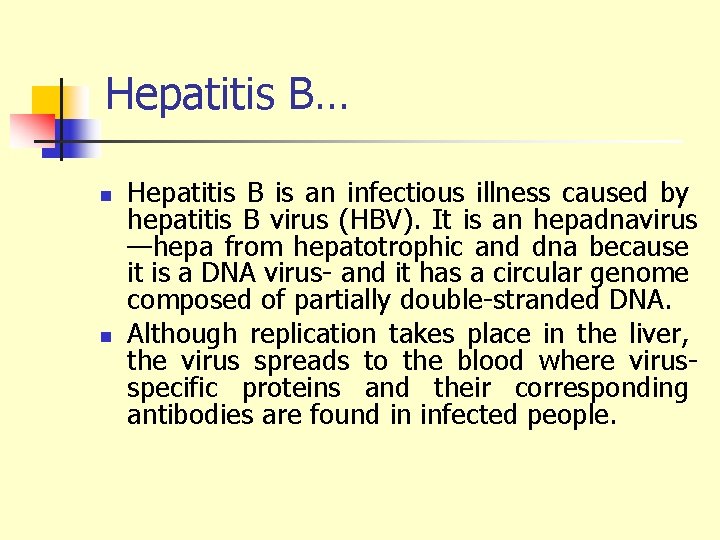
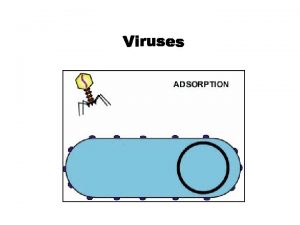
Hepatitis B… n n Hepatitis B is an infectious illness caused by hepatitis B virus (HBV). It is an hepadnavirus —hepa from hepatotrophic and dna because it is a DNA virus- and it has a circular genome composed of partially double-stranded DNA. Although replication takes place in the liver, the virus spreads to the blood where virusspecific proteins and their corresponding antibodies are found in infected people.
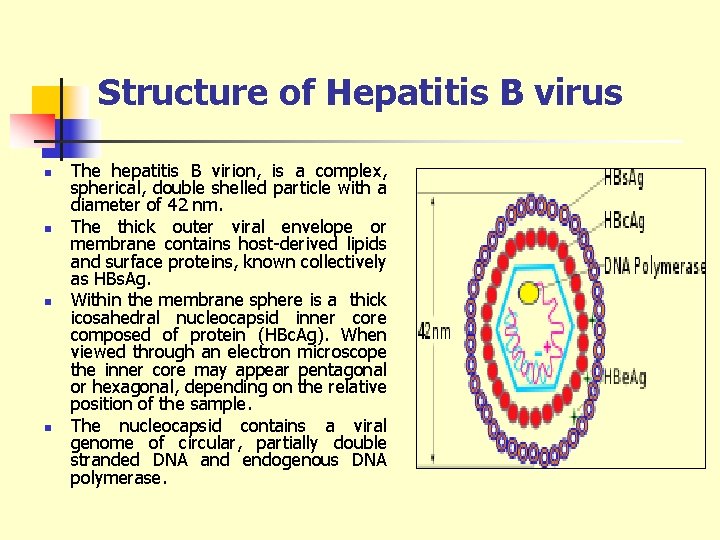
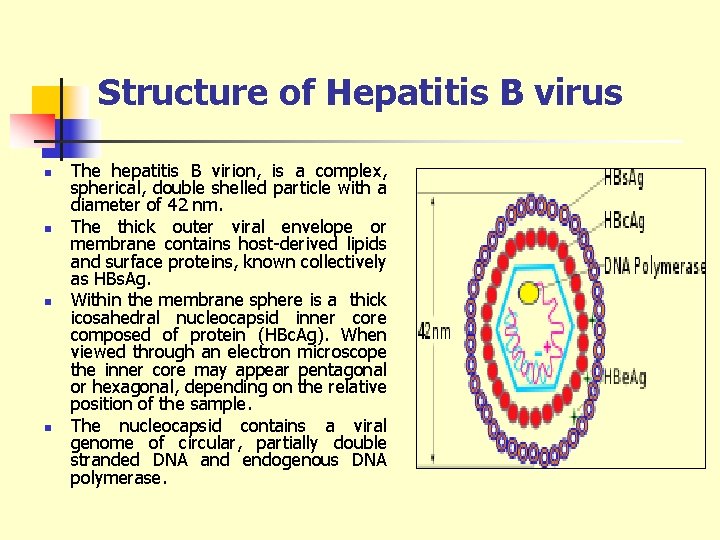
Structure of Hepatitis B virus n n The hepatitis B virion, is a complex, spherical, double shelled particle with a diameter of 42 nm. The thick outer viral envelope or membrane contains host-derived lipids and surface proteins, known collectively as HBs. Ag. Within the membrane sphere is a thick icosahedral nucleocapsid inner core composed of protein (HBc. Ag). When viewed through an electron microscope the inner core may appear pentagonal or hexagonal, depending on the relative position of the sample. The nucleocapsid contains a viral genome of circular, partially double stranded DNA and endogenous DNA polymerase.
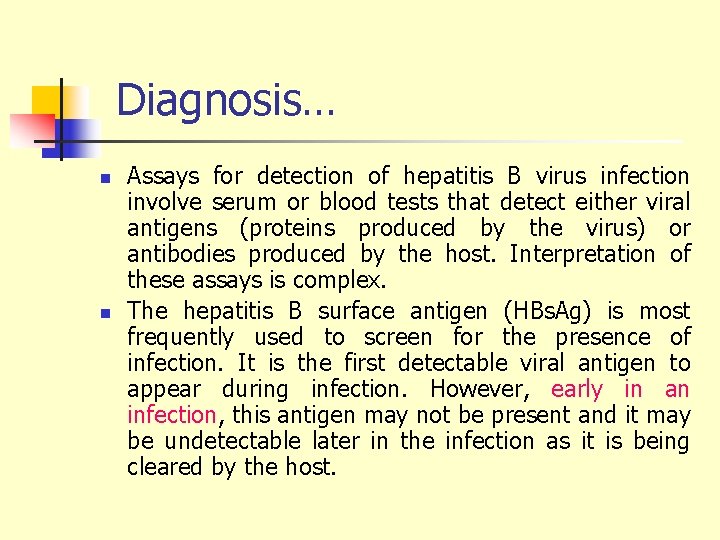
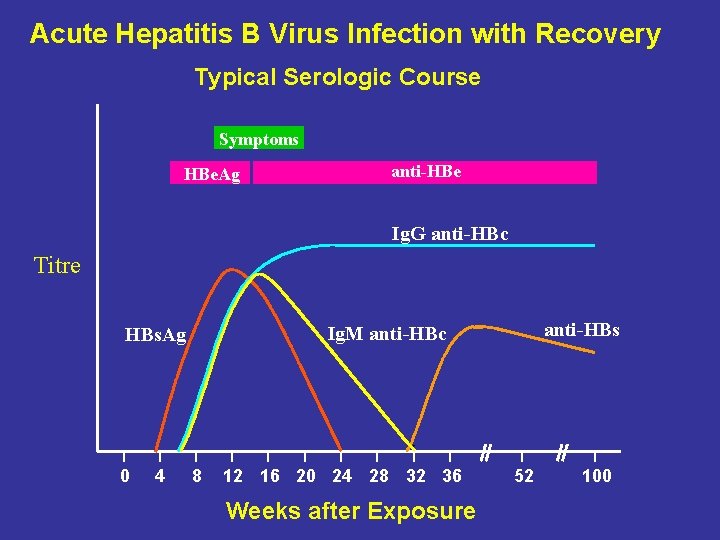
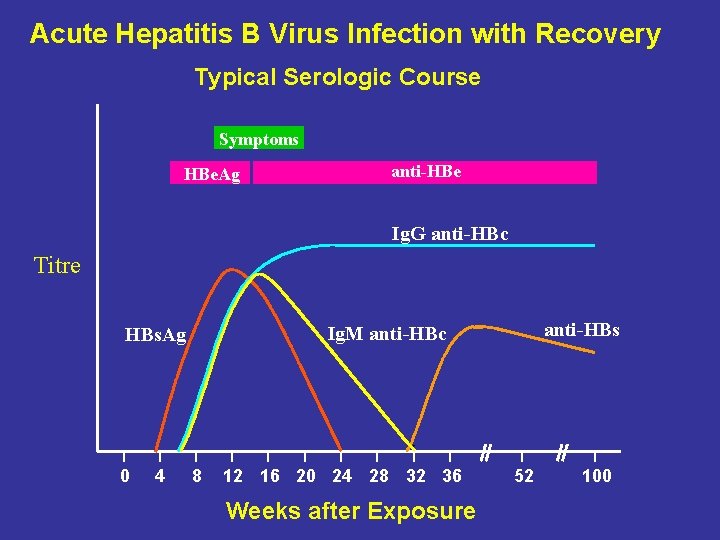
Diagnosis… n n Assays for detection of hepatitis B virus infection involve serum or blood tests that detect either viral antigens (proteins produced by the virus) or antibodies produced by the host. Interpretation of these assays is complex. The hepatitis B surface antigen (HBs. Ag) is most frequently used to screen for the presence of infection. It is the first detectable viral antigen to appear during infection. However, early in an infection, this antigen may not be present and it may be undetectable later in the infection as it is being cleared by the host.
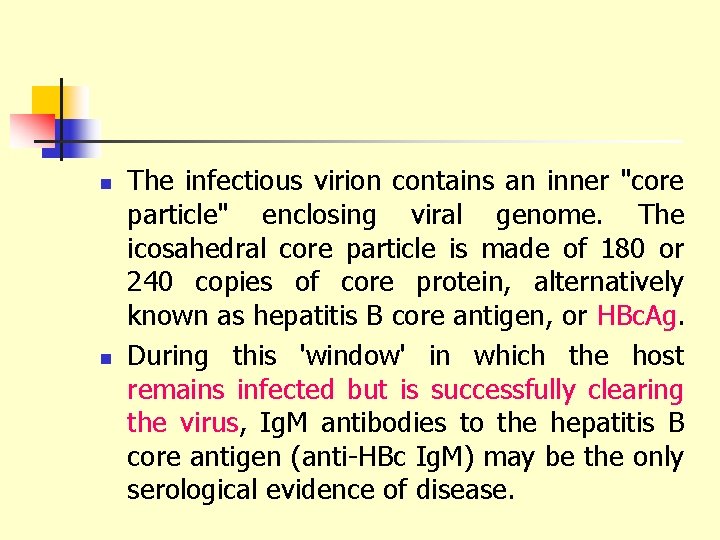
n n The infectious virion contains an inner "core particle" enclosing viral genome. The icosahedral core particle is made of 180 or 240 copies of core protein, alternatively known as hepatitis B core antigen, or HBc. Ag. During this 'window' in which the host remains infected but is successfully clearing the virus, Ig. M antibodies to the hepatitis B core antigen (anti-HBc Ig. M) may be the only serological evidence of disease.
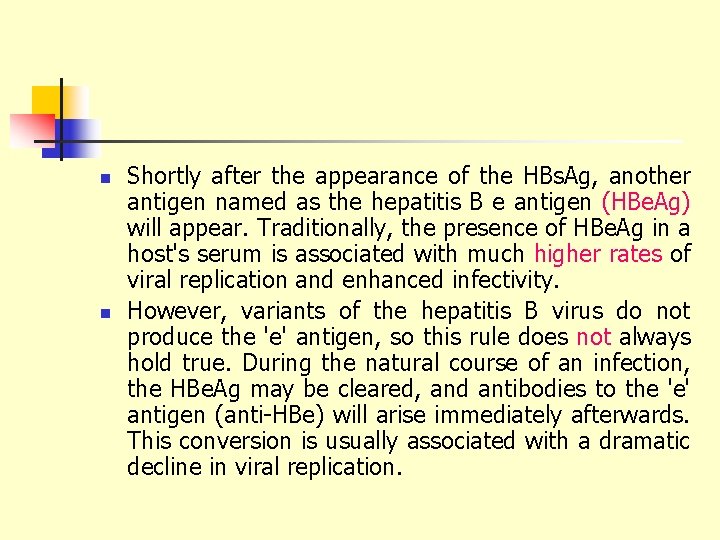
n n Shortly after the appearance of the HBs. Ag, another antigen named as the hepatitis B e antigen (HBe. Ag) will appear. Traditionally, the presence of HBe. Ag in a host's serum is associated with much higher rates of viral replication and enhanced infectivity. However, variants of the hepatitis B virus do not produce the 'e' antigen, so this rule does not always hold true. During the natural course of an infection, the HBe. Ag may be cleared, and antibodies to the 'e' antigen (anti-HBe) will arise immediately afterwards. This conversion is usually associated with a dramatic decline in viral replication.
n n If the host is able to clear the infection, eventually the HBs. Ag will become undetectable and will be followed by Ig. G antibodies to the hepatitis B surface antigen and core antigen, (anti-HBs and anti HBc Ig. G). The time between the removal of the HBs. Ag and the appearance of anti-HBs is called the window period. A person negative for HBs. Ag but positive for anti-HBs has either cleared an infection or has been vaccinated previously.
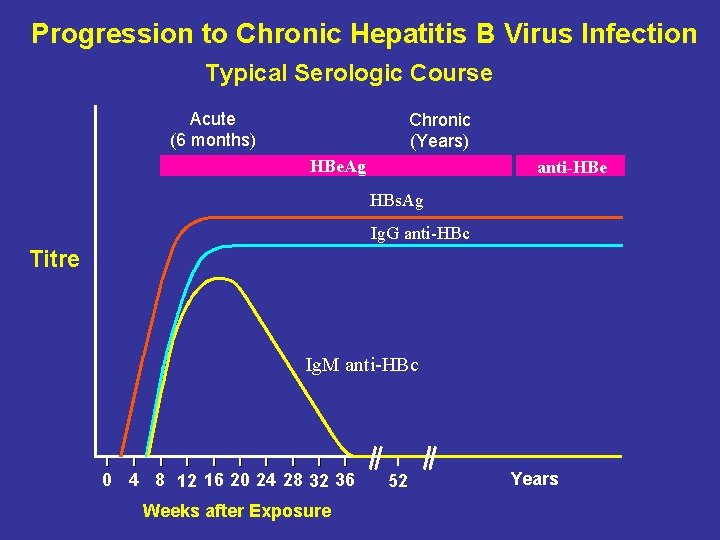
n n Individuals who remain HBs. Ag positive for at least six months are considered to be hepatitis B carriers. Carriers of the virus may have chronic hepatitis B, which would be reflected by elevated serum alanine aminotransferase levels and inflammation of the liver, as revealed by biopsy. Carriers who have seroconverted to HBe. Ag negative status, particularly those who acquired the infection as adults, have very little viral multiplication and hence may be at little risk of long-term complications or of transmitting infection to others.
n PCR tests have been developed to detect and measure the amount of HBV DNA, called the viral load, in clinical specimens. These tests are used to assess a person's infection status and to monitor treatment.
Acute Hepatitis B Virus Infection with Recovery Typical Serologic Course Symptoms HBe. Ag anti-HBe Ig. G anti-HBc Titre 0 4 anti-HBs Ig. M anti-HBc HBs. Ag 8 12 16 20 24 28 32 36 Weeks after Exposure 52 100
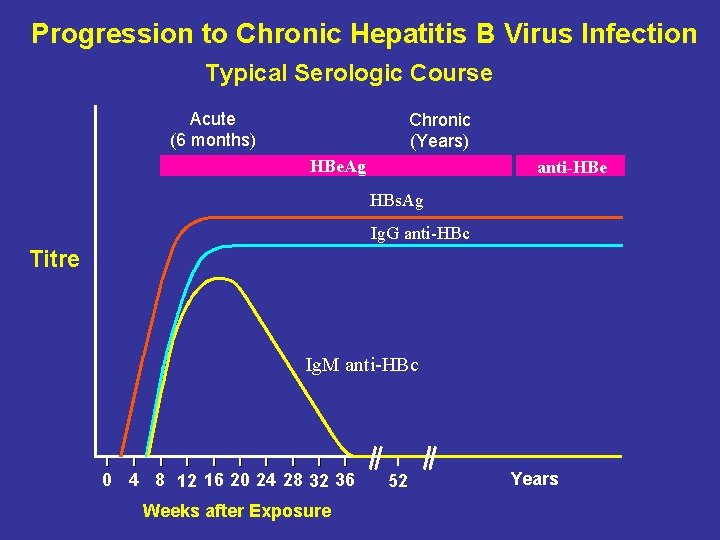
Progression to Chronic Hepatitis B Virus Infection Typical Serologic Course Acute (6 months) Chronic (Years) HBe. Ag anti-HBe HBs. Ag Ig. G anti-HBc Titre Ig. M anti-HBc 0 4 8 12 16 20 24 28 32 36 Weeks after Exposure 52 Years
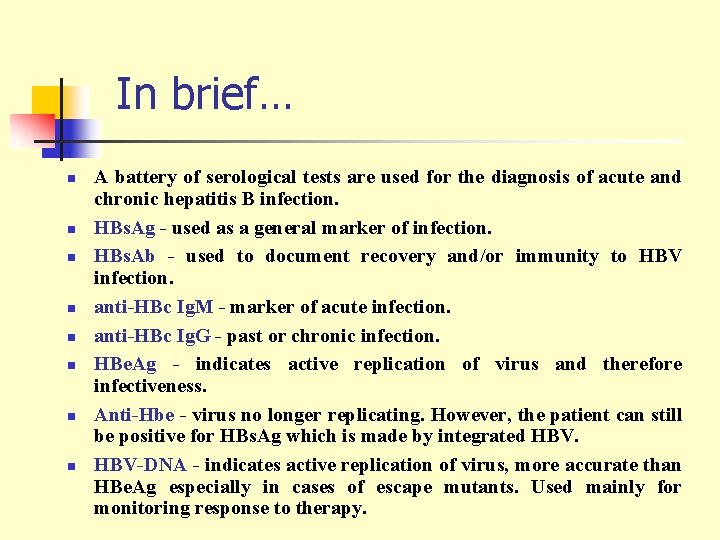
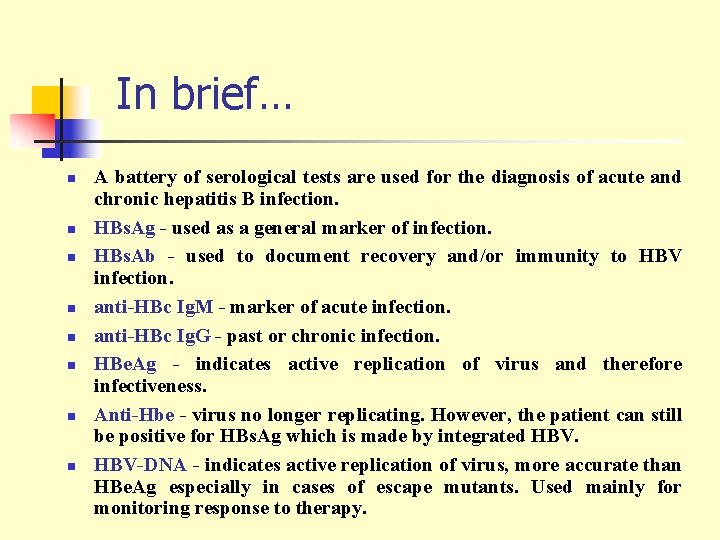
In brief… n n n n A battery of serological tests are used for the diagnosis of acute and chronic hepatitis B infection. HBs. Ag - used as a general marker of infection. HBs. Ab - used to document recovery and/or immunity to HBV infection. anti-HBc Ig. M - marker of acute infection. anti-HBc Ig. G - past or chronic infection. HBe. Ag - indicates active replication of virus and therefore infectiveness. Anti-Hbe - virus no longer replicating. However, the patient can still be positive for HBs. Ag which is made by integrated HBV-DNA - indicates active replication of virus, more accurate than HBe. Ag especially in cases of escape mutants. Used mainly for monitoring response to therapy.
Spectrum of Chronic Hepatitis B Diseases 1. Chronic Persistent Hepatitis - asymptomatic 2. Chronic Active Hepatitis - symptomatic exacerbations of hepatitis 3. Cirrhosis of Liver 4. Hepatocellular Carcinoma
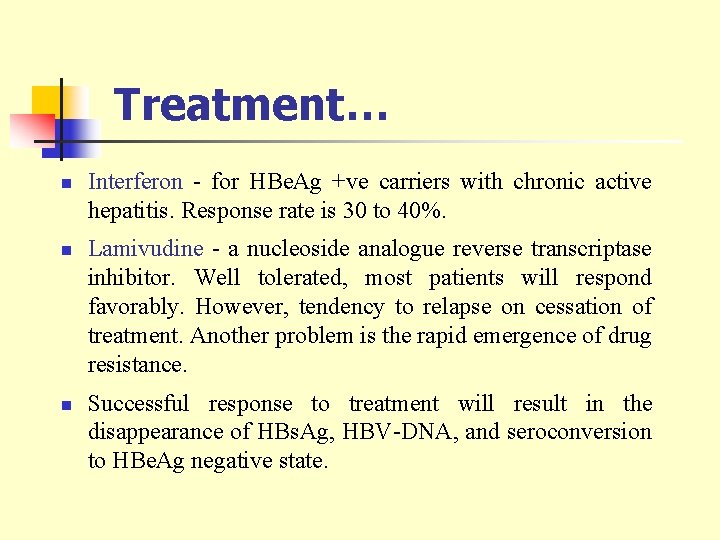
Treatment… n n n Interferon - for HBe. Ag +ve carriers with chronic active hepatitis. Response rate is 30 to 40%. Lamivudine - a nucleoside analogue reverse transcriptase inhibitor. Well tolerated, most patients will respond favorably. However, tendency to relapse on cessation of treatment. Another problem is the rapid emergence of drug resistance. Successful response to treatment will result in the disappearance of HBs. Ag, HBV-DNA, and seroconversion to HBe. Ag negative state.
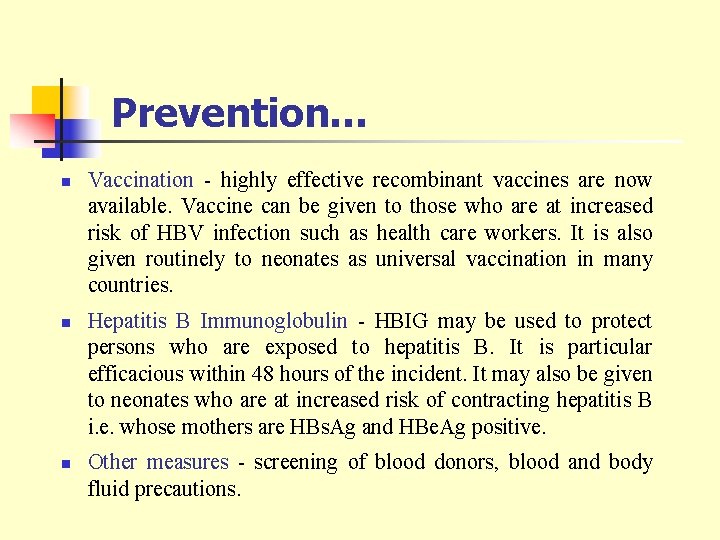
Prevention… n n n Vaccination - highly effective recombinant vaccines are now available. Vaccine can be given to those who are at increased risk of HBV infection such as health care workers. It is also given routinely to neonates as universal vaccination in many countries. Hepatitis B Immunoglobulin - HBIG may be used to protect persons who are exposed to hepatitis B. It is particular efficacious within 48 hours of the incident. It may also be given to neonates who are at increased risk of contracting hepatitis B i. e. whose mothers are HBs. Ag and HBe. Ag positive. Other measures - screening of blood donors, blood and body fluid precautions.
Hepatitis C Virus
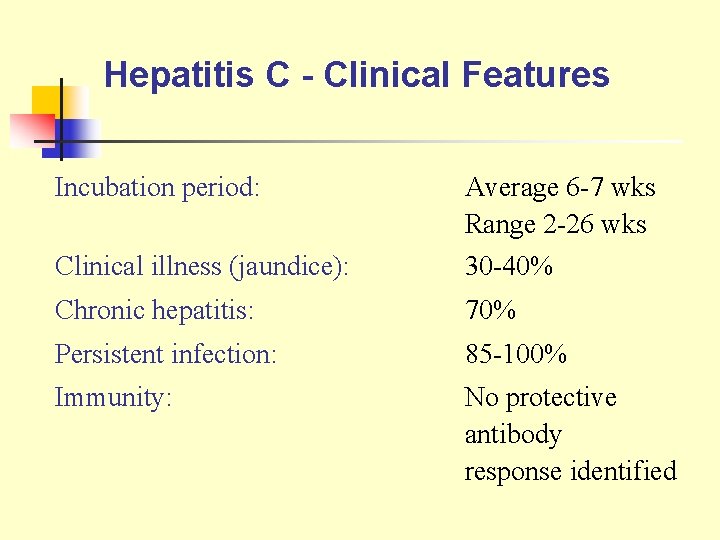
Hepatitis C - Clinical Features Incubation period: Average 6 -7 wks Range 2 -26 wks Clinical illness (jaundice): 30 -40% Chronic hepatitis: 70% Persistent infection: 85 -100% Immunity: No protective antibody response identified
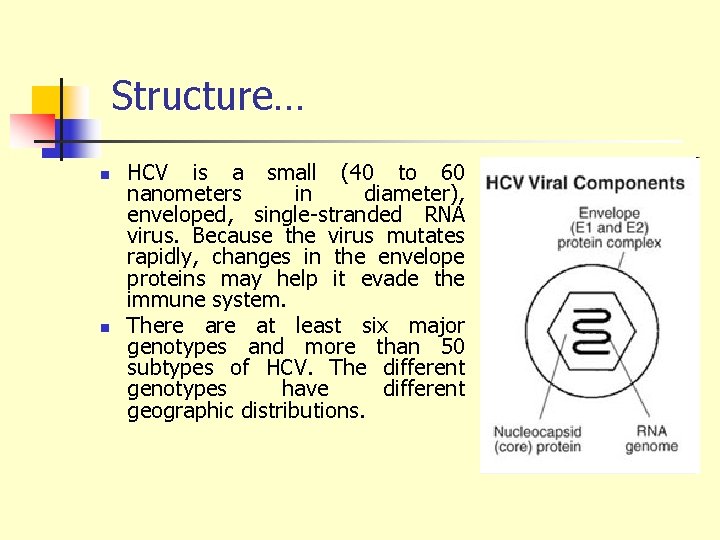
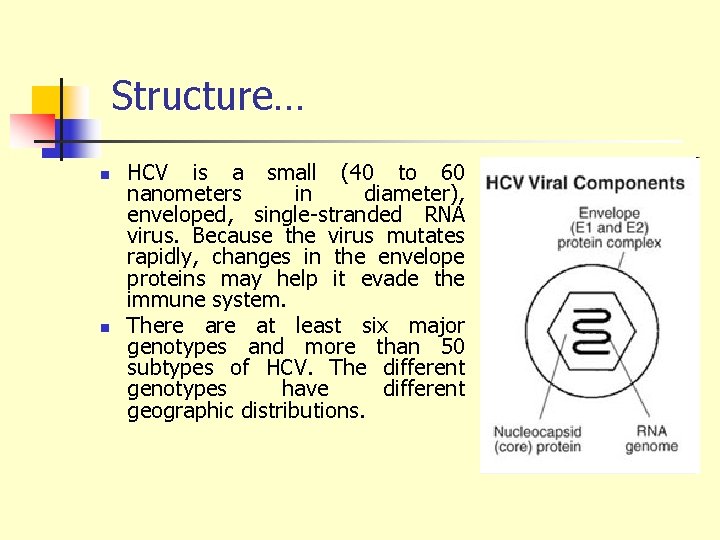
Structure… n n HCV is a small (40 to 60 nanometers in diameter), enveloped, single-stranded RNA virus. Because the virus mutates rapidly, changes in the envelope proteins may help it evade the immune system. There at least six major genotypes and more than 50 subtypes of HCV. The different genotypes have different geographic distributions.
Risk Factors Associated with Transmission of HCV § Transfusion or transplant from infected donor § Injecting drug use § Hemodialysis § Accidental injuries with needles/sharps
n Maternal-infant Transmission: Maternal-infant transmission is not common. In most studies, less than 5 percent (one in 20) of infants born to HCVinfected mothers become infected. The disease in newborns is usually mild and free of symptoms. The risk of maternal-infant spread rises with the amount of virus in the mother’s blood, if the mother also has human immunodeficiency virus (HIV) infection, or if there are complications of delivery that require fetal monitoring, such as early rupture of membranes. Breastfeeding has not been linked to the spread of HCV.
n n Sporadic transmission— when the source of infection is unknown—is the basis for about 10 percent of acute hepatitis C cases and for 30 percent of chronic hepatitis C cases. These cases are usually referred to as sporadic or community-acquired infections. These infections may have come from exposure to the virus from cuts, wounds, or medical injections or procedures. Spread of hepatitis C in the workplace and the household contacts is extremely rare. For this reason, precautions about limitations on casual contact, food preparation, and sharing food and utensils are unnecessary.

Symptoms… n n n Many people with chronic hepatitis C have no symptoms of liver disease. If symptoms are present, they are usually mild, nonspecific, and intermittent. They may include fatigue mild right-upper-quadrant abdominal discomfort or tenderness (“liver pain”) nausea poor appetite muscle and joint pains
Once a patient develops cirrhosis—or if the patient has severe disease—symptoms and signs are more prominent. In addition to fatigue, the patient may complain of muscle weakness, poor appetite, nausea, weight loss, itching, dark urine, fluid retention, and abdominal swelling. Physical findings of cirrhosis may include: n enlarged liver n enlarged spleen n jaundice n muscle wasting n excoriations (scratches or abrasions on the skin) n ascites (fluid-filled belly) n ankle swelling
Extrahepatic Manifestations: Complications that do not involve the liver develop in 1 to 2 percent of people with hepatitis C; the most common is cryoglobulinemia, which is marked by n skin rashes, such as purpura, vasculitis, or urticaria n joint and muscle aches n kidney disease n neuropathy n cryoglobulins, rheumatoid factor,
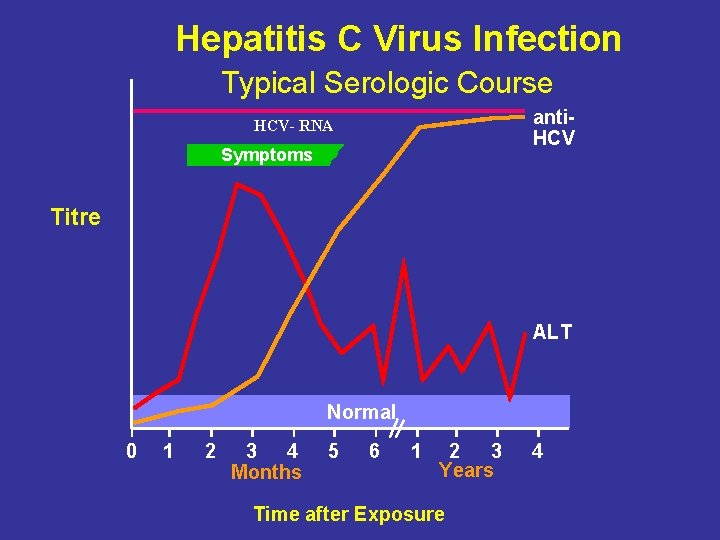
Laboratory Diagnosis n Hepatitis C is most readily diagnosed when serum aminotransferases are elevated anti-HCV is present in serum. The diagnosis is confirmed by the finding of HCV RNA in serum.
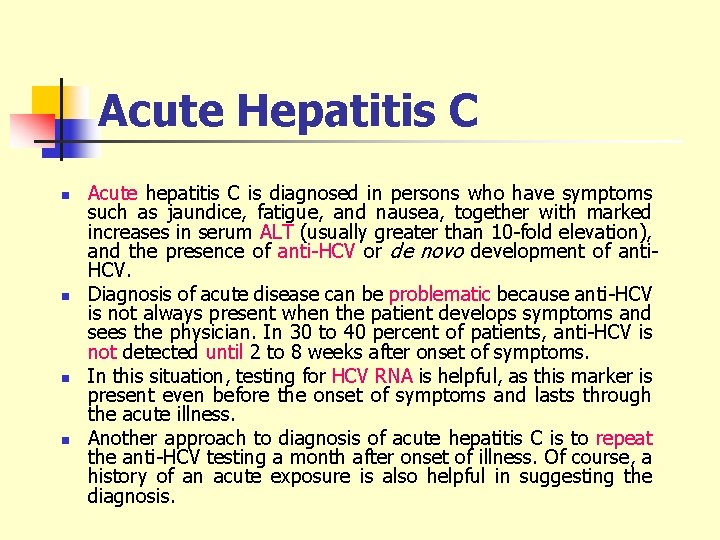
Acute Hepatitis C n n Acute hepatitis C is diagnosed in persons who have symptoms such as jaundice, fatigue, and nausea, together with marked increases in serum ALT (usually greater than 10 -fold elevation), and the presence of anti-HCV or de novo development of anti. HCV. Diagnosis of acute disease can be problematic because anti-HCV is not always present when the patient develops symptoms and sees the physician. In 30 to 40 percent of patients, anti-HCV is not detected until 2 to 8 weeks after onset of symptoms. In this situation, testing for HCV RNA is helpful, as this marker is present even before the onset of symptoms and lasts through the acute illness. Another approach to diagnosis of acute hepatitis C is to repeat the anti-HCV testing a month after onset of illness. Of course, a history of an acute exposure is also helpful in suggesting the diagnosis.
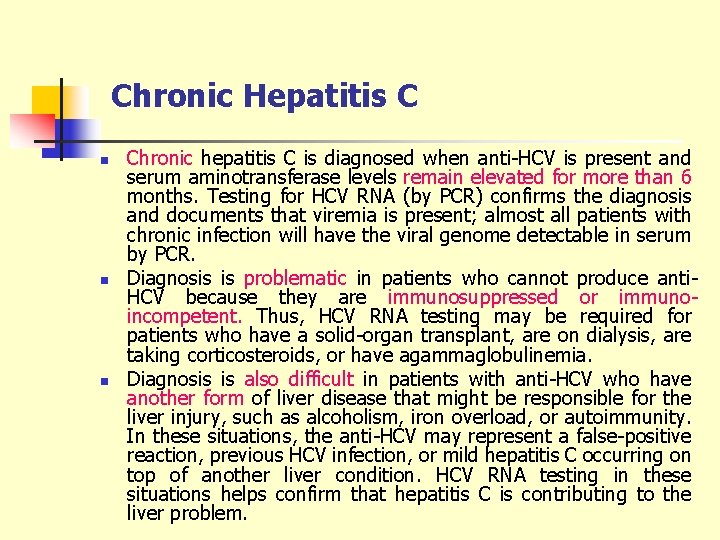
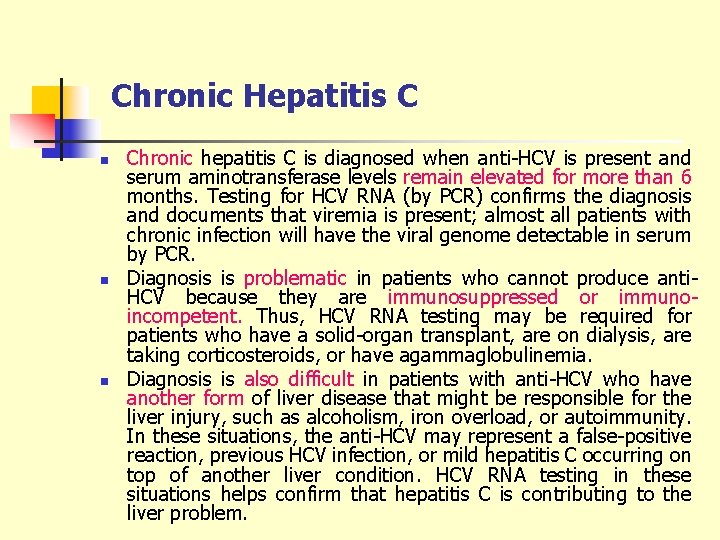
Chronic Hepatitis C n n n Chronic hepatitis C is diagnosed when anti-HCV is present and serum aminotransferase levels remain elevated for more than 6 months. Testing for HCV RNA (by PCR) confirms the diagnosis and documents that viremia is present; almost all patients with chronic infection will have the viral genome detectable in serum by PCR. Diagnosis is problematic in patients who cannot produce anti. HCV because they are immunosuppressed or immunoincompetent. Thus, HCV RNA testing may be required for patients who have a solid-organ transplant, are on dialysis, are taking corticosteroids, or have agammaglobulinemia. Diagnosis is also difficult in patients with anti-HCV who have another form of liver disease that might be responsible for the liver injury, such as alcoholism, iron overload, or autoimmunity. In these situations, the anti-HCV may represent a false-positive reaction, previous HCV infection, or mild hepatitis C occurring on top of another liver condition. HCV RNA testing in these situations helps confirm that hepatitis C is contributing to the liver problem.
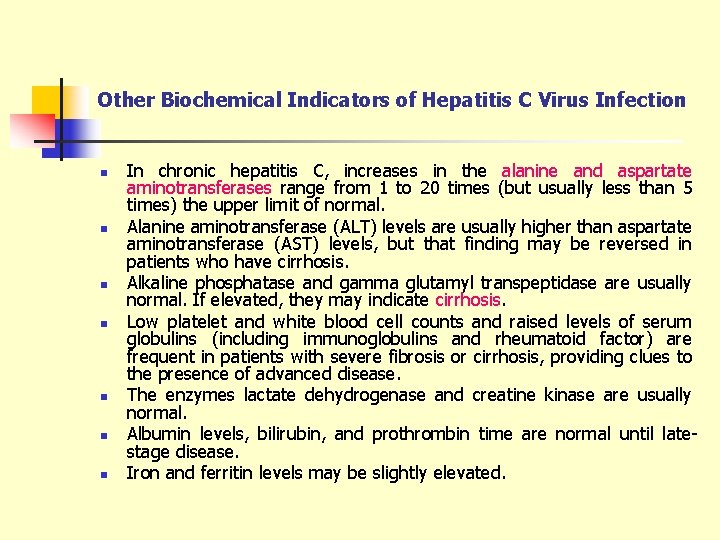
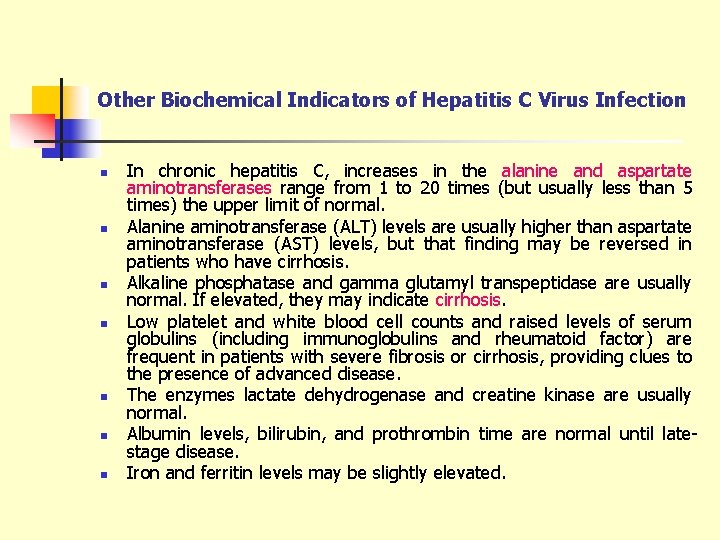
Other Biochemical Indicators of Hepatitis C Virus Infection n n n In chronic hepatitis C, increases in the alanine and aspartate aminotransferases range from 1 to 20 times (but usually less than 5 times) the upper limit of normal. Alanine aminotransferase (ALT) levels are usually higher than aspartate aminotransferase (AST) levels, but that finding may be reversed in patients who have cirrhosis. Alkaline phosphatase and gamma glutamyl transpeptidase are usually normal. If elevated, they may indicate cirrhosis. Low platelet and white blood cell counts and raised levels of serum globulins (including immunoglobulins and rheumatoid factor) are frequent in patients with severe fibrosis or cirrhosis, providing clues to the presence of advanced disease. The enzymes lactate dehydrogenase and creatine kinase are usually normal. Albumin levels, bilirubin, and prothrombin time are normal until latestage disease. Iron and ferritin levels may be slightly elevated.
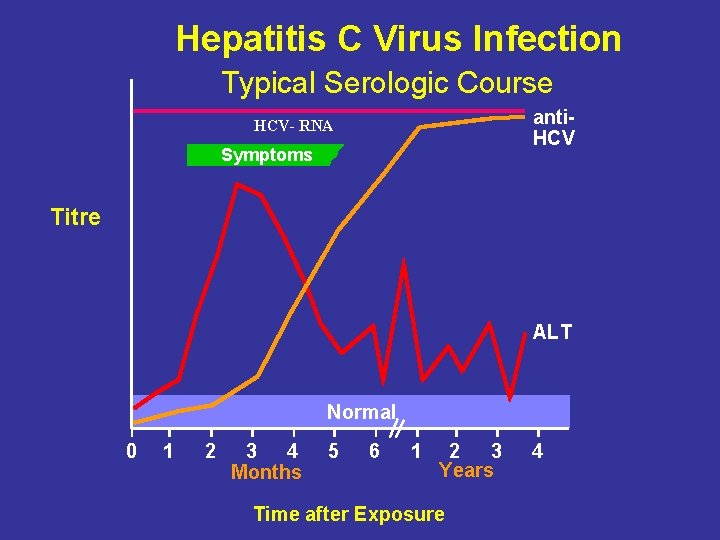
Hepatitis C Virus Infection Typical Serologic Course anti. HCV- RNA Symptoms Titre ALT Normal 0 1 2 3 4 Months 5 6 1 2 3 Years Time after Exposure 4
Differential Diagnosis The major conditions that can be confused clinically with chronic hepatitis C include n autoimmune hepatitis n chronic hepatitis B and D n alcoholic hepatitis n nonalcoholic steatohepatitis (fatty liver) n sclerosing cholangitis n Wilson disease n alpha-1 -antitrypsin-deficiency-related liver disease n drug-induced liver disease
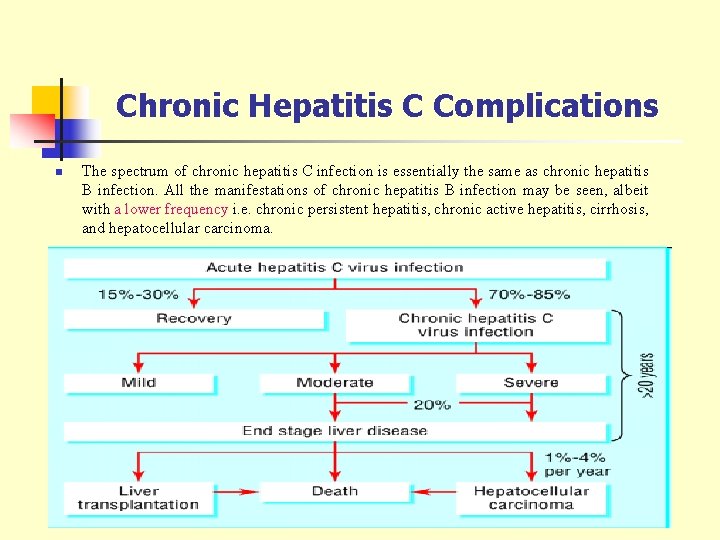
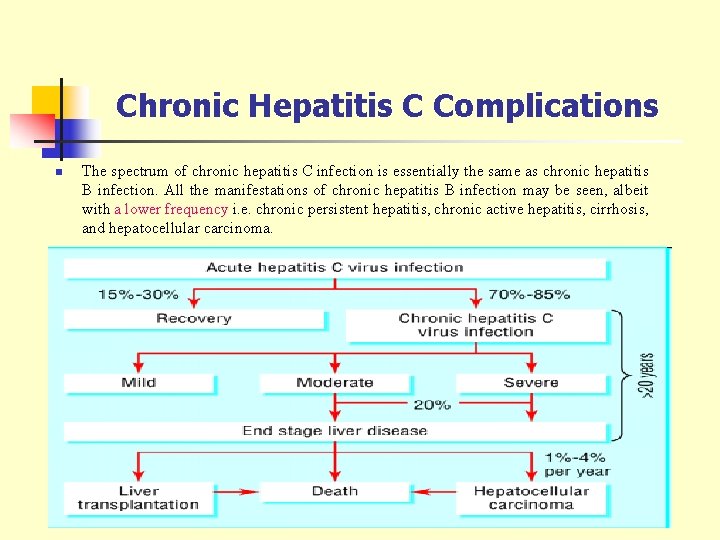
Chronic Hepatitis C Complications n The spectrum of chronic hepatitis C infection is essentially the same as chronic hepatitis B infection. All the manifestations of chronic hepatitis B infection may be seen, albeit with a lower frequency i. e. chronic persistent hepatitis, chronic active hepatitis, cirrhosis, and hepatocellular carcinoma.
Prevention of Hepatitis C § Screening of blood, organ, tissue donors § High-risk behavior modification § Blood and body fluid precautions
EVALUATION… n During the acute stage of hepatitis A infection, all the following can be observed except: A. Eleveted HAV- Ig. M antibody B. Elevated HAV- Ig. G antibody C. Eleveted ALT enzyme D. Viremia E. None of the above.
n Unconjugated bilirubin only is increased in the following condition(s): A. Hepatocellular carcinoma B. Cholelithiasis C. Hemolytic anemia D. All of the above E. None of the above
n Mothers who are ………………positive are much more likely to transmit to their offspring than those who are not. A. HBs. Ag B. HBc. Ag C. anti-HBc D. HBe. Ag E. anti-HBe
n Hepatitis C is most readily diagnosed ALT when serum ……………. are elevated and ……………… is present in serum. The Anti-HCV diagnosis is confirmed by the finding of ………… HCV-RNA in serum.
 Hepatitis viral
Hepatitis viral Art labeling activity figure 23.5
Art labeling activity figure 23.5 Liver histology
Liver histology Liver physiology and anatomy
Liver physiology and anatomy Degluttination
Degluttination Hemiliver 뜻
Hemiliver 뜻 Liver anatomy
Liver anatomy Microscopic anatomy of liver
Microscopic anatomy of liver Liver
Liver Causes of viral hemorrhagic fever
Causes of viral hemorrhagic fever Viral integration
Viral integration Viral inoculation in embryonated egg
Viral inoculation in embryonated egg Viral arthritis
Viral arthritis Viral recombination
Viral recombination Morfologia viral
Morfologia viral Viral shedding
Viral shedding Equine rhinopneumonitis
Equine rhinopneumonitis Replicação viral ciclo lítico e lisogênico
Replicação viral ciclo lítico e lisogênico Viral entry
Viral entry Ciclo viral
Ciclo viral Egg inoculation technique
Egg inoculation technique Trplice
Trplice An acute highly contagious viral disease
An acute highly contagious viral disease Viral inoculation in embryonated egg
Viral inoculation in embryonated egg Vaccins à vecteur viral
Vaccins à vecteur viral Viral load sample collection
Viral load sample collection Eline's viral
Eline's viral Section 24-1 viral structure and replication
Section 24-1 viral structure and replication The dynamics of viral marketing
The dynamics of viral marketing Viral infection
Viral infection Spasmodic croup vs viral croup
Spasmodic croup vs viral croup Viral life cycle
Viral life cycle Viral dna
Viral dna Viral receptors
Viral receptors Meningitis viral antibiótico
Meningitis viral antibiótico Viral communications
Viral communications Viral replikasyon basamakları
Viral replikasyon basamakları Csf findings in meningitis table
Csf findings in meningitis table Viral
Viral Variola varicela
Variola varicela Mobilivirus
Mobilivirus Viral induced wheeze vs asthma
Viral induced wheeze vs asthma Dha mcq
Dha mcq Procalcitonin
Procalcitonin Vena portal hepar
Vena portal hepar Chronic hepatitis
Chronic hepatitis Hepatitis b vaccine series adults
Hepatitis b vaccine series adults Hepatitis e
Hepatitis e Pbc vs psc
Pbc vs psc Hepatitis
Hepatitis Chronic pancreatitis nursing care plan
Chronic pancreatitis nursing care plan Hepatitis b
Hepatitis b Esquema de vacaciones en mexico
Esquema de vacaciones en mexico Ggh providencia
Ggh providencia Hepatitis types chart
Hepatitis types chart Hep b mode of transmission
Hep b mode of transmission Hepatitis d
Hepatitis d Window period of hepatitis b
Window period of hepatitis b Gail lupica
Gail lupica Hepatitis a treatment
Hepatitis a treatment Score simplificado hepatitis autoinmune
Score simplificado hepatitis autoinmune