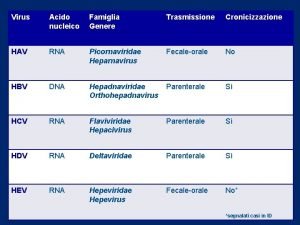
Viral Hepatitis HIV HEPATITIS A VIRUS HAV Hepatitis




- Slides: 33
Viral Hepatitis & HIV
HEPATITIS A VIRUS HAV
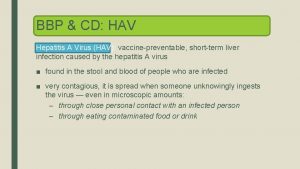
Hepatitis A (infectious hepatitis and epidemical virus) q Is an acute infectious disease of the liver caused by the hepatitis A virus (Hep A), an RNA virus. q Usually spread the fecal-oral route; transmitted person-to- person by ingestion of contaminated food or water or through direct contact with an infectious person q Infection with the hepatitis A virus leads to inflammation of the liver, liver but complications are rarely serious.
HAV transmission: • The hepatitis A virus (HAV) is found in the faeces of infected person with the virus. A tiny amount of the virus will cause the infection. • Personal hygiene, such as careful hand washing, can minimize the risk of the virus transmission to other person.
Characteristics of HAV: q A member of the enteroviruses (picornaviridae family). family q Spherical, single strand RNA- containing particle. q Icosahedral, naked and 27 – 32 nm in diameter q Incubation period: 2 – 6 weeks
Signs and symptoms of HAV virus: • A short, mild, flu-like illness. • Nausea, vomiting and diarrhea. • Loss of appetite. • Weight loss. • Jaundice (yellow skin and whites of eyes, darker yellow urine and pale faeces). • Itchy skin. • Abdominal pain.
Laboratory diagnosis of HAV: • Blood bilirubin. • Liver enzymes (AST and ALT). • Detect virus in faeces by used immune- electron microscopy. • RIA or ELISA for Ig. M.

Treatment for HAV: • No specific treatment. • Affected people fight off the virus naturally, returning to full health within a couple of months. • The doctor will advise avoiding alcohol and fatty foods as these can be hard for the liver to process and may exacerbate the inflammation. • Patients should get plenty of rest and eat a nutritious diet. • They should also ensure they do not spread HAV by washing their hands after using the toilet and before preparing food. • Patients with more severe symptoms may be monitored in hospital for a short period.
HEPATITIS B VIRUS HBV
Characteristics of HBV: • Belongs to the hepadnaviridae family. • Spherical, double- shelled DNA containing particles. • Icosahedral, enveloped and 42 nm in diameter. • Incubation period: 2 – 6 months (50 - 180 days).
HBV transmission: • Sexual Transmission. • Sharing contaminated needles or other drug-injecting equipment. • From an infected mother to her baby, most commonly during delivery. • Immunization of the baby at birth prevents the transmission of hepatitis B. • Through a blood transfusion in a country where blood is not screened for blood-borne viruses such as HBV.
Signs and symptoms of HBV: • A short, mild, flu-like illness. • Nausea, vomiting and diarrhea. • Loss of appetite. • Weight loss. • Jaundice. • Itchy skin. • If a person lives with hepatitis B infection for a number of years then they may develop the following complications: • Chronic hepatitis. • Liver cirrhosis. • Liver cancer.
Laboratory diagnosis of HBV: • Liver function tests, abnormally elevated (ALT and AST), bilirubin, alkaline phosphatase (ALP) and lactate dehydrogenase (LDH). • The presence of HBs Ag confirms diagnosis, tested by ELISA, RIA and real PCR. • Liver biopsy
Treatment for HBV: • Prevent further liver damage. These medications may be injected or given in pill form. Examples are Interferon Alpha, Lamivudine. Treatment usually lasts 6 months, during which time the patient will be carefully monitored. • Regardless of whether the infection is producing symptoms or not, the patient will be advised to avoid alcohol, get plenty of rest and maintain a healthy diet
HBV immunization: • Three immunization injections are given over a period of 3 -6 months. A blood test is taken once the course of injections is completed to check they have worked. Immunity should last for at least 5 years.
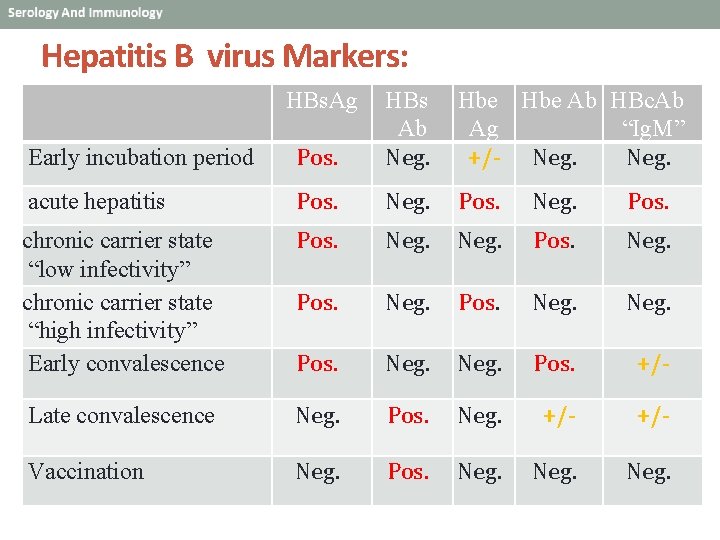
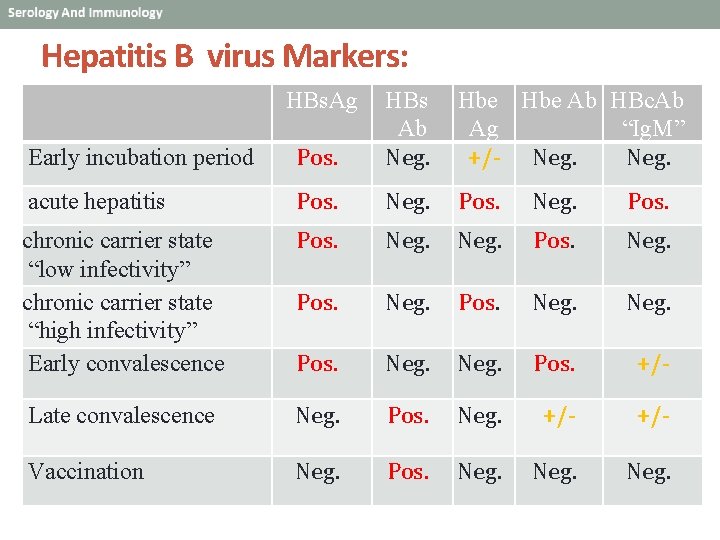
Hepatitis B virus Markers: HBs. Ag Early incubation period Pos. HBs Ab Neg. Hbe Ab HBc. Ab Ag “Ig. M” +/- Neg. acute hepatitis Pos. Neg. Pos. chronic carrier state “low infectivity” chronic carrier state “high infectivity” Early convalescence Pos. Neg. Pos. +/- Late convalescence Neg. Pos. Neg. +/- Vaccination Neg. Pos. Neg.
HEPATITIS C VIRUS HCV
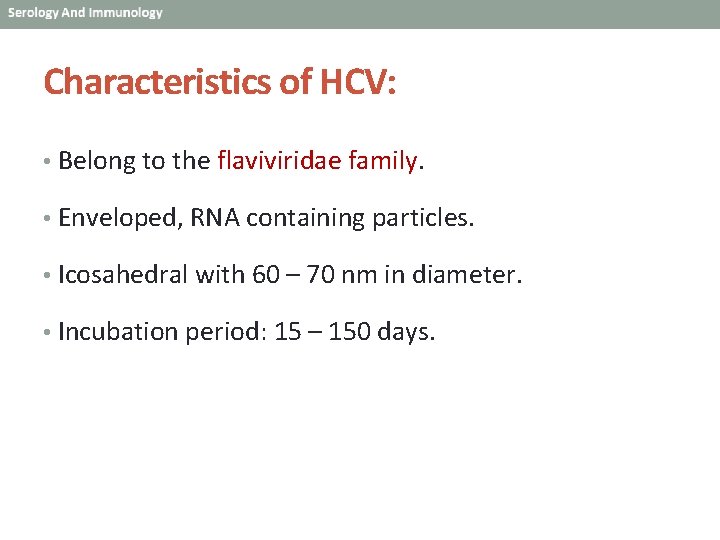
Characteristics of HCV: • Belong to the flaviviridae family. • Enveloped, RNA containing particles. • Icosahedral with 60 – 70 nm in diameter. • Incubation period: 15 – 150 days.
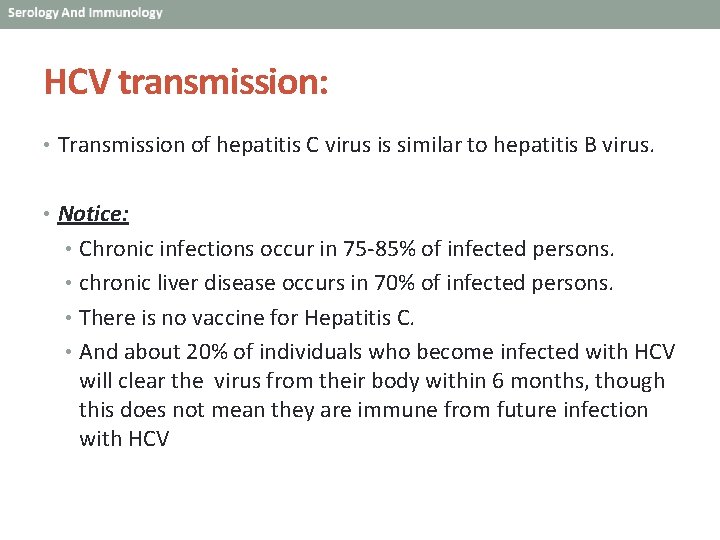
HCV transmission: • Transmission of hepatitis C virus is similar to hepatitis B virus. • Notice: • Chronic infections occur in 75 -85% of infected persons. • chronic liver disease occurs in 70% of infected persons. • There is no vaccine for Hepatitis C. • And about 20% of individuals who become infected with HCV will clear the virus from their body within 6 months, though this does not mean they are immune from future infection with HCV
Laboratory diagnosis of HCV: • Serological blood tests used to detect antibodies to HCV. • Anti-HCV antibodies can be detected in 80% of patients within 15 weeks after exposure, • >90% within 5 months after exposure, and • >97% by 6 months after exposure. • PCR to detect The presence of the viruses, also transcription mediated amplification (TMA), or branched DNA (b-DNA). • HCV viral load , to measure the amount of virus present in the blood. The HCV viral load is an important factor in determining the probability of response to interferon-based therapy, but does not indicate disease severity nor the likelihood of disease progression. • Liver function tests. • Liver biopsy.
Treatment for HCV: • Treatment combines the antiviral drugs interferon and ribavirin. Although treatment has improved in recent years, the success rates vary depending on which genotype the patient has and how long they have had HCV. • Notice: There is no vaccine for Hepatitis C virus.

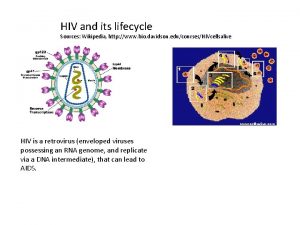
Characteristics of HIV: • The causative agent of acquired immunodeficiency syndrome (AIDS). • Belong to the lentivirus subfamily of the retrovidridae family. • Enveloped, icosahedral, RNA containing particles. • Have envelope glycoproteins: gp 120 and gp 41. • Infect immune system (T helper lymphocyte; CD 4). • Incubation period: 3 – 5 years.
Mode of transmission of HIV: • Sexual contact (homosexual and heterosexual). • Sharing contaminated intravenous needles. • Breastfeeding (mother to baby). • Infected mother to fetus during pregnancy or birth. • Blood transfusions and tissue transplantation.
Sign and symptom of HIV: • A flu-like illness, develop a rash, or get swollen glands for a brief period soon after they become infected with HIV. • Often people who are infected with HIV don't have any symptoms at all. It is important to remember that a person who has HIV can pass on the virus immediately after becoming infected, even if they feel healthy. It's not possible to tell just by looking if someone has been infected with HIV
Laboratory diagnosis of HIV: 1 - Serological screening: • Antibody detection: • ELISAs are the most frequently used method for screening of blood samples for HIV antibody. The sensitivity and specificity of the presently available commercial systems approaches 100% but false positive and false negative reactions occur. • Other test systems available include passive particle agglutination, immunofluorescence, Western blots. • Western blots are regarded as the gold standard and seropositivity is diagnosed when antibodies against both the envelope and the gag proteins are detected. The sensitivity of the test systems are currently being improved by the use of recombinant antigens.
• Antigen screening: • HIV antigen can be detected early in the course of HIV infection before the appearance of antibody. It is undetectable during the latent period (antigen-antibody complexes are present) but become detectable during the final stages of the infection. It was argued that the routine use of antigen screening tests in the blood transfusion service may result in earlier cases of HIV infection being identified.
2 -Virus isolation: • Virus isolation is accomplished by the cultivation of the patient's lymphocytes with fresh peripheral blood cells of healthy donors or with suitable culture lines such as T-lymphomas. The presence of the virus can be confirmed by reverse transcriptase assays, serological tests, or by changes in growth pattern of the indicator cells. However virus isolation is tedious and time consuming (weeks) and is successful in only 70 to 90% of cases. Therefore virus isolation is mainly used for the characterization of the virus.
3 -Demonstration viral nucleic acid: • This can be accomplished by probes or by PCR techniques. The latter may be useful because of its extremely high sensitivity. 4 -HIV viral load • It appears that HIV viral load has the greatest prognostic value. HIV viral load in serum may be measured by assays which detect HIVRNA e. g. RT-PCR. HIV viral load has now been established as having good prognostic value, and in monitoring response to antiviral chemotherapy. Patients with a low viral load during the incubation period had a better prognosis than those with a high viral load. Patients whose viral load decreased significantly following the commencement of antiviral therapy had a better prognosis than those who did not respond. Among patients who responded to antiviral therapy, those who had a low pretreatment viral load had a better prognosis than those who had a high pre-treatment viral load.
5 - CD 4 count • Despite the increasing use of HIV-RNA assays, measurement of CD 4 still has important value in monitoring disease progression and response to antiviral chemotherapy. Whereas CD 4 count gives an indication of the stage of disease. “The measurement of HIV viral load tells us where the disease is going, whereas CD 4 count tells us where the disease is at this moment”


THANK YOU
 Hgado
Hgado Virus hiv
Virus hiv Hiv virus
Hiv virus Heparnavirus
Heparnavirus Retro yr hav og kyst
Retro yr hav og kyst Home access center crsd
Home access center crsd Hav trasmissione
Hav trasmissione Hav hf
Hav hf Eline's viral
Eline's viral Cultivation of viruses
Cultivation of viruses Virus dna
Virus dna The dynamics of viral marketing
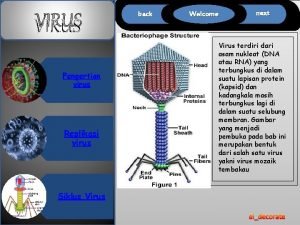
The dynamics of viral marketing Capsid capsomere
Capsid capsomere Spasmodic croup
Spasmodic croup Viral life cycle
Viral life cycle Viral receptors
Viral receptors Viral replikasyon basamakları
Viral replikasyon basamakları Meningitis viral antibiótico
Meningitis viral antibiótico Viral communications
Viral communications Csf findings in meningitis table
Csf findings in meningitis table Viral induced wheeze vs asthma
Viral induced wheeze vs asthma Viral
Viral Dea anggraini viral
Dea anggraini viral Infinitive viral infection
Infinitive viral infection Procalcitonin
Procalcitonin Dha mcq
Dha mcq Egg inoculation diagram
Egg inoculation diagram Causes of viral hemorrhagic fever
Causes of viral hemorrhagic fever Hiv wikipedia
Hiv wikipedia Viral arthritis
Viral arthritis Vrus
Vrus Viral recombination
Viral recombination Decapsidação
Decapsidação Viral shedding
Viral shedding