Viral Hepatitis Causes of viral hepatitis Common 1















- Slides: 55

Viral Hepatitis
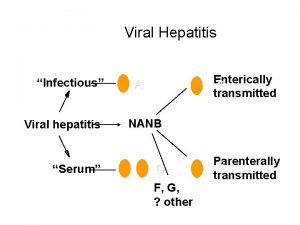
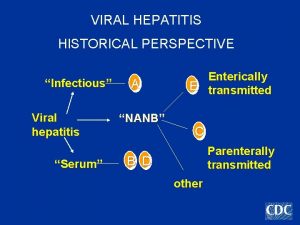
Causes of viral hepatitis Common: 1 -Hepatitis A 2 - Hepatitis B +/- Hepatitis D. 3 - Hepatitis C. 4 -Hepatitis E. Less common: 1 -Cytomegalovrus. 2 -Epstien-Bar virus. Rare: 1 -Herpes simplex. 2 -Yellow fever.
Clinical features of acute infection: Prodromal: few days- 2 weeks before jaundice. GIT symptoms: Vomiting & diarrhea Abdominal pain is common Dark urine & pale stool jaundice: may be mild Symptoms rarely last longer than 3 -6 weeks. Clinical signs: There are few physical signs. Liver is often tender but often minimally enlarged.
Investigations 1 - Hepatitis pattern of LFTs with serum transaminases typically between 200 -2000 U/L. 2 - Plasma bilirubin: reflect the degree of liver damage. 3 - Alkaline phosphetase: rarely > twice the upper limit of normal. 4 - Prothrombin Time prolongation indicates the severity of hepatitis. 5 - WBC count is usually normal with relative lymphocytosis. 6 - Serological tests to confirm the aetiology of infection.
Complications of acute viral hepatitis 1 - Acute liver failure. 2 - Cholestatic hepatitis. 3 - Aplastic anaemia. 4 - Chronic liver disease & cirrhosis (HB & C) 5 - Relapsing hepatitis.
Management Most patients do not need hospital care. Sedative & Narcotics should be avoided. No specific dietary modifications are needed Alcohol should be avoided. Elective surgery should be avoided.
Liver transplantation Rarely indicated for acute viral hepatitis complicated by liver failure. Commonly performed for complications of cirrhosis resulting from chronic hepatitis B and C infection.

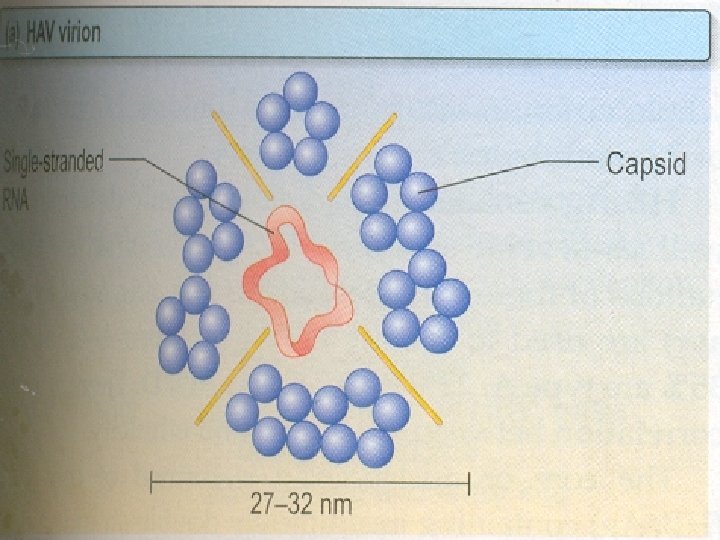
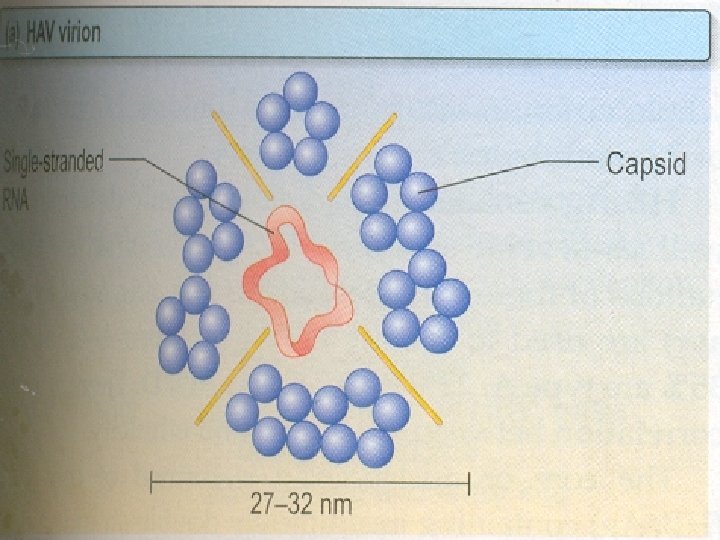
Hepatitis A • Belong to picornavirus group of enteroviruses. • Is highly infectious & spread by feco oral route. • Infected individuals excrete the virus in the faeces for 2 -3 weeks before the appearance of symptoms & then for further 2 weeks. • Infection is common in children , but often asymptomatic. • • Infection is also common in areas of overcrowding & poor sanitation. Water & shellfish are sometimes the vehicles • other ways – blood , sexual are uncommon • no vertical spread & no chronic infection.

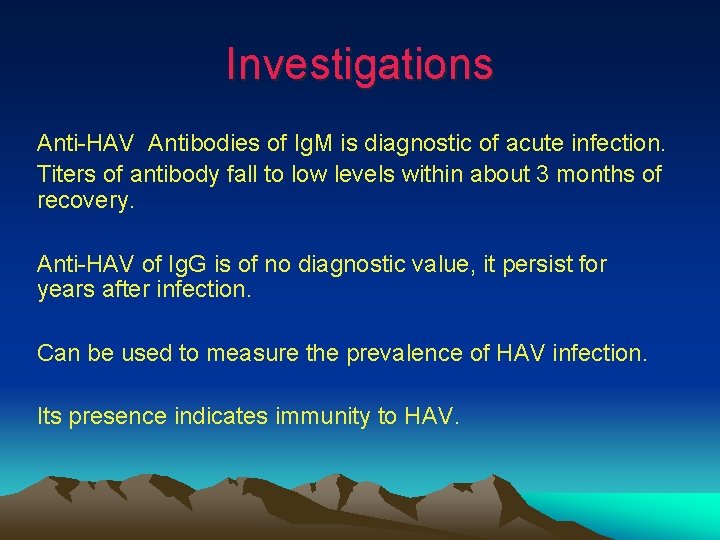
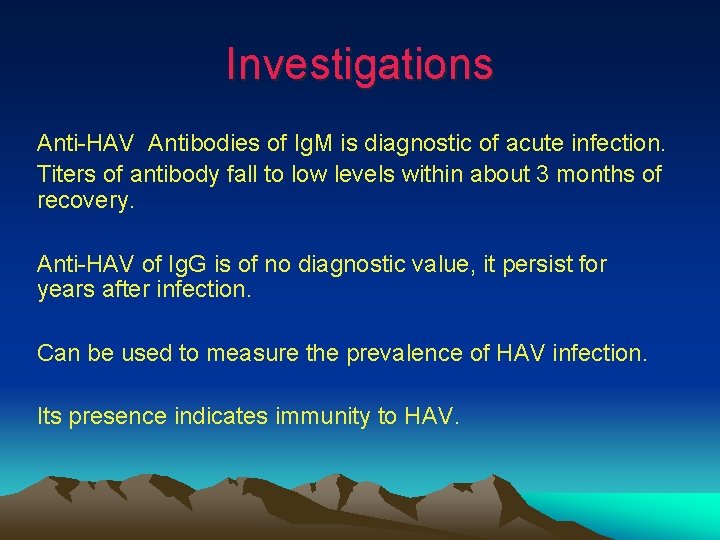
Investigations Anti-HAV Antibodies of Ig. M is diagnostic of acute infection. Titers of antibody fall to low levels within about 3 months of recovery. Anti-HAV of Ig. G is of no diagnostic value, it persist for years after infection. Can be used to measure the prevalence of HAV infection. Its presence indicates immunity to HAV.


Prevention HAV: 1. 2 - Active immunization for. People traveling to endemic area. Patients with chronic hepatitis B & C infection. Immune S. globulin for immediate protection after exposure indicated for. Close contacts. Elderly. Those with major diseases. Pregnant. Outbreak of hepatitis in school , nursery to prevent secondary spread to families. 3 - Improving social conditions especially. Over crowding Poor sanitation
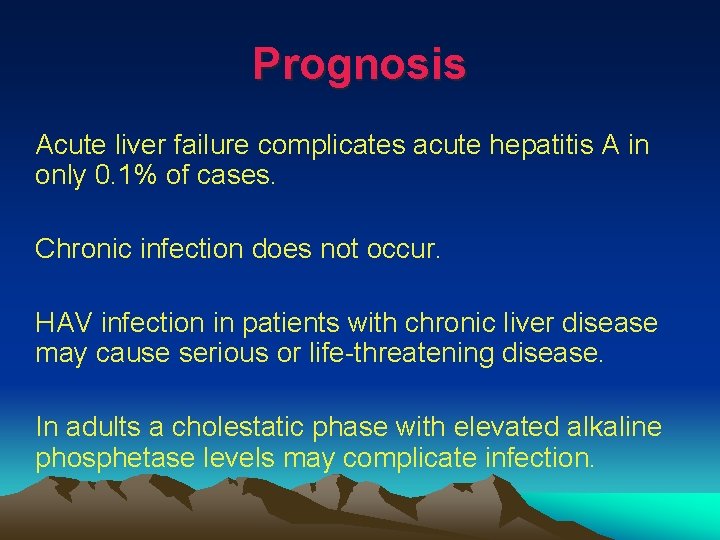
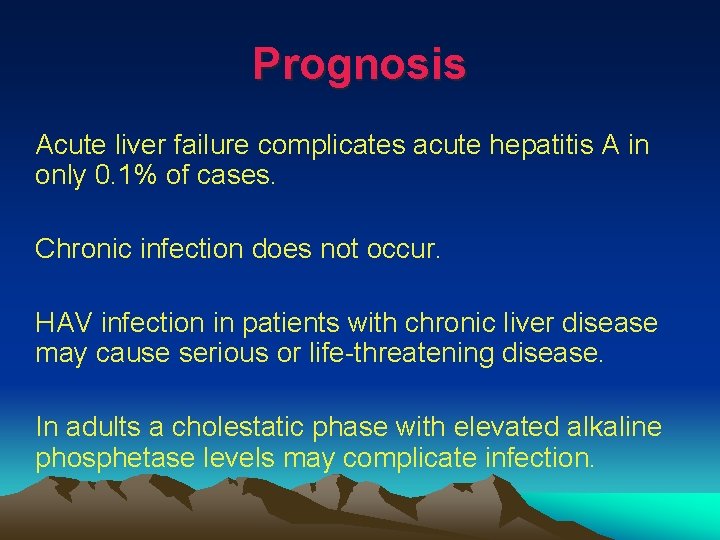
Prognosis Acute liver failure complicates acute hepatitis A in only 0. 1% of cases. Chronic infection does not occur. HAV infection in patients with chronic liver disease may cause serious or life-threatening disease. In adults a cholestatic phase with elevated alkaline phosphetase levels may complicate infection.
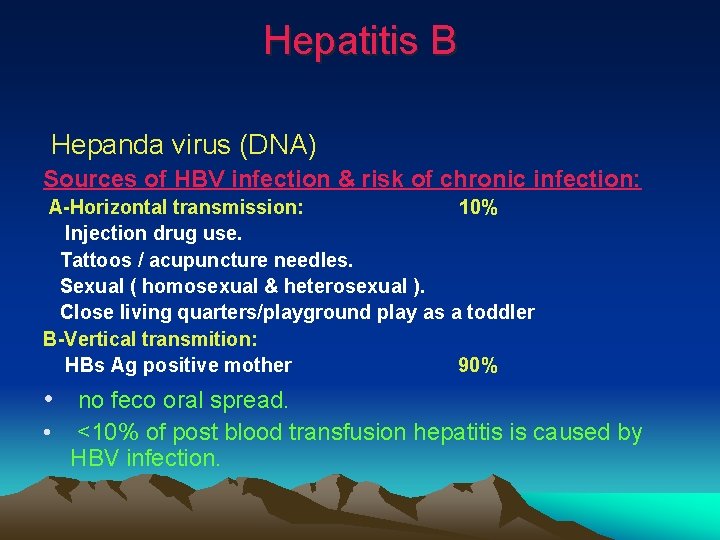
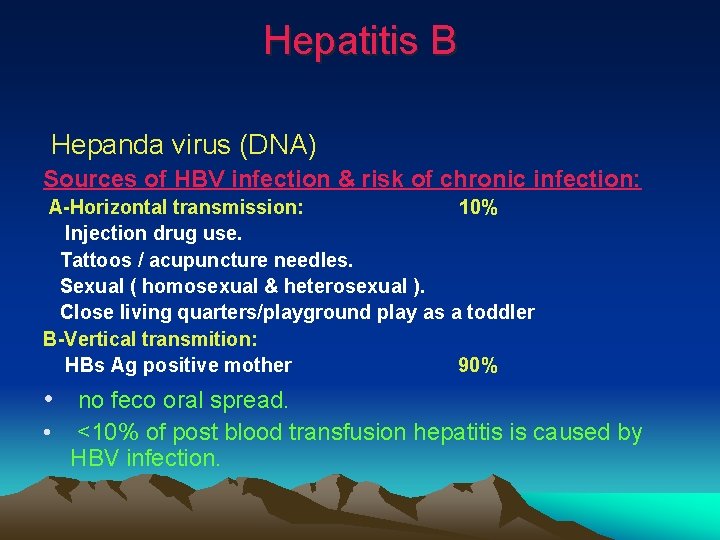
Hepatitis B Hepanda virus (DNA) Sources of HBV infection & risk of chronic infection: A-Horizontal transmission: 10% Injection drug use. Tattoos / acupuncture needles. Sexual ( homosexual & heterosexual ). Close living quarters/playground play as a toddler B-Vertical transmition: HBs Ag positive mother 90% • no feco oral spread. • <10% of post blood transfusion hepatitis is caused by HBV infection.
Ø Affect 300 million people & one of the most common cause of chronic liver disease & hepatocellular carcinoma world-wide. Ø The most common cause of infection worldwide is vertical transmission. Ø HBV may cause an acute hepatitis which often asymptomatic especially when infection acquired at birth. Ø The risk of progression to chronic liver disease depend on the source of infection.



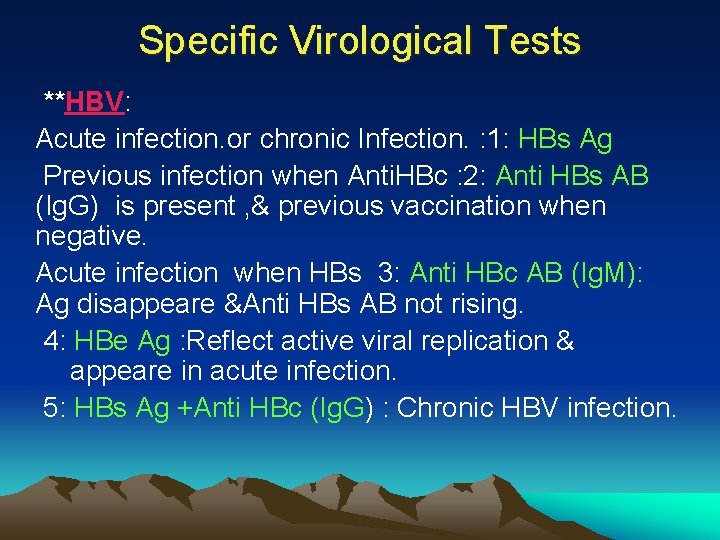
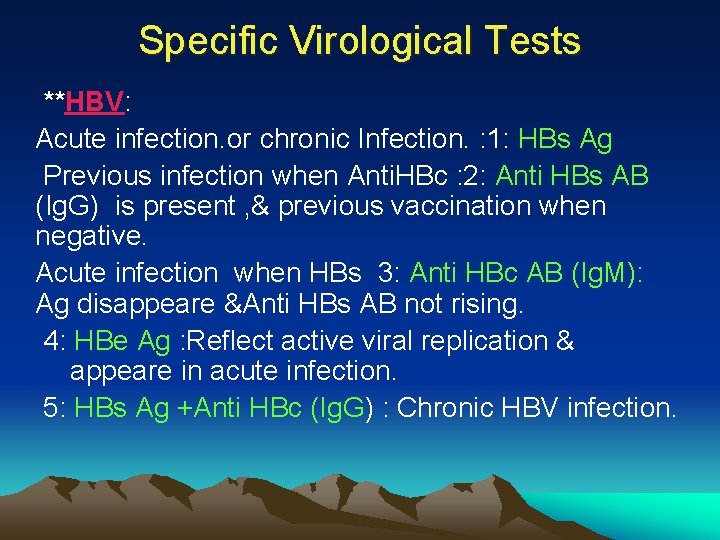
Specific Virological Tests **HBV: Acute infection. or chronic Infection. : 1: HBs Ag Previous infection when Anti. HBc : 2: Anti HBs AB (Ig. G) is present , & previous vaccination when negative. Acute infection when HBs 3: Anti HBc AB (Ig. M): Ag disappeare &Anti HBs AB not rising. 4: HBe Ag : Reflect active viral replication & appeare in acute infection. 5: HBs Ag +Anti HBc (Ig. G) : Chronic HBV infection.

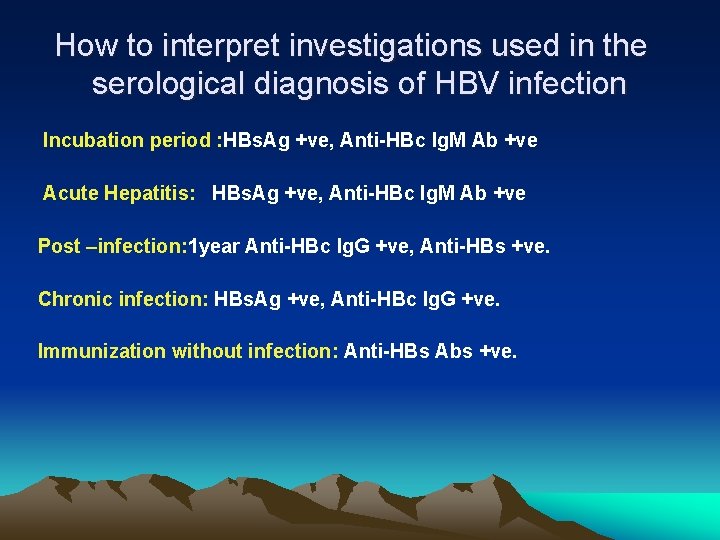
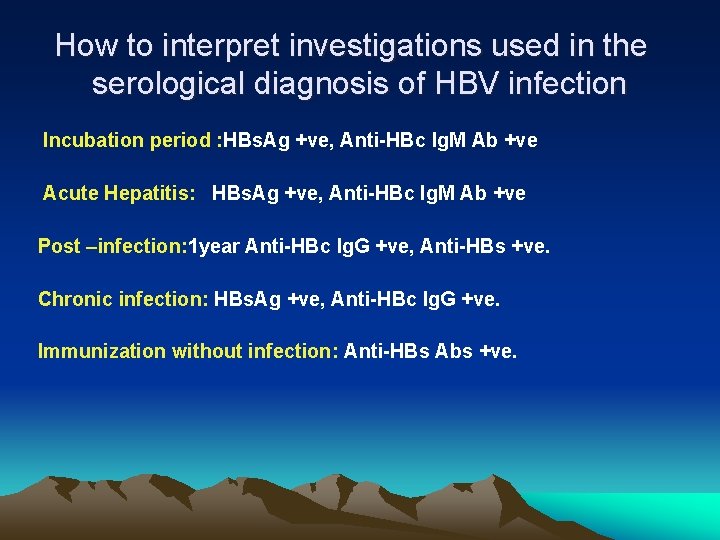
How to interpret investigations used in the serological diagnosis of HBV infection Incubation period : HBs. Ag +ve, Anti-HBc Ig. M Ab +ve Acute Hepatitis: HBs. Ag +ve, Anti-HBc Ig. M Ab +ve Post –infection: 1 year Anti-HBc Ig. G +ve, Anti-HBs +ve. Chronic infection: HBs. Ag +ve, Anti-HBc Ig. G +ve. Immunization without infection: Anti-HBs Abs +ve.
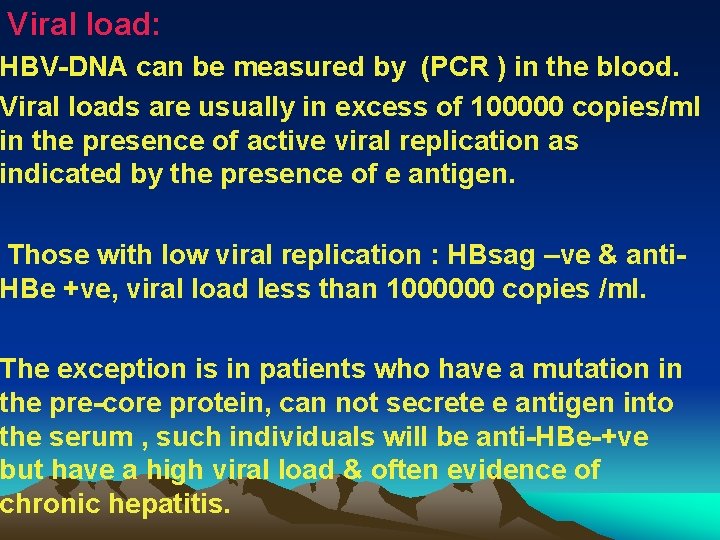
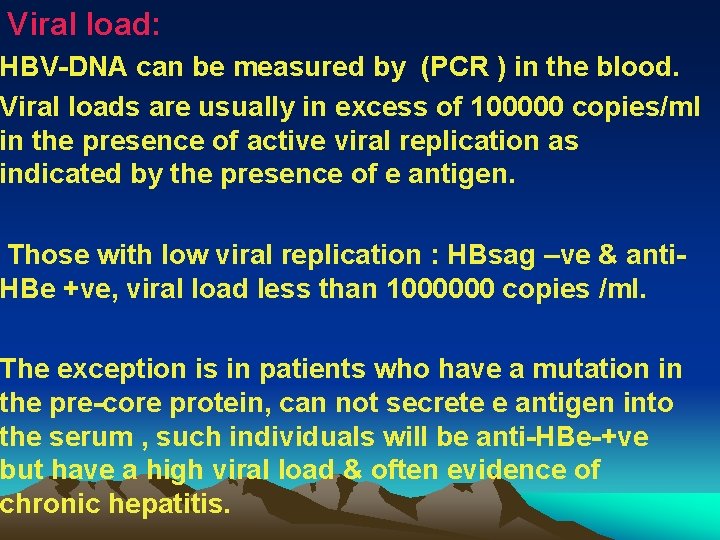
Viral load: HBV-DNA can be measured by (PCR ) in the blood. Viral loads are usually in excess of 100000 copies/ml in the presence of active viral replication as indicated by the presence of e antigen. Those with low viral replication : HBsag –ve & anti. HBe +ve, viral load less than 1000000 copies /ml. The exception is in patients who have a mutation in the pre-core protein, can not secrete e antigen into the serum , such individuals will be anti-HBe-+ve but have a high viral load & often evidence of chronic hepatitis.
e antigen –ve chronic hepatitis respond differently to antiviral drugs. Measurement of viral load is important in monitoring antiviral therapy & identifying patients with pre-core mutants. Specific HBV genotypes can also be identified using PCR. Genotypes B & C appear to have more aggressive disease that responds less well to antiviral therapy.
Management Acute hepatitis B: Treatment is supportive. Monitoring for acute liver failure which occur in less than 1% of cases.

Chronic hepatitis B Treatment are still limited , with no drug able to eradicate hepatitis B infection completely. The indication for treatment: High viral load in presence of active hepatitis as demonstrated by elevated serum transaminases and/or histological evidence of inflammation.

Alfa-interferon: Interferon 5 MU /d or 10 MU three times /w for 16 weeks. Side effects: Influenza like symptoms Depression. Thrombocytopenia. Thyroid abnormalities Most effective in selected patients with a low viral load& serum transaminases > twice the upper limit of normal In HBe Ag +ve chronic hepatitis 33% loss e antigen after 4 -6 months of treatment. Response rates are lower in HBe Ag –ve chronic hepatitis. Interferon is contraindicated in presence of cirrhosis as it precipitate liver failure.
Pegylated interferon in chronic hepatitis B infection: Long acting interferon can be given once weekly. In Hbe. Ag-positive chronic hepatitis treated with pegylated interferon for 6 months eliminates HBe. Agin 35% & normalizes liver biochemistry in 25%of patients. In HBe. Ag-negetive chronic hepatitis treatment with pegylated interferon for 12 months leads to normal liver biochemistry in 60% & sustained suppression of hepatitis B virus load below 400 copies /ml in 20% of patients

Lamivudine: Nucleoside analogue which inhibits DNA polymerase & suppresses HBV-DNA levels. 48 weeks of treatment with Lamivudine induces Anti. HBe seroconversion in 27% patients with HBe. Ag +ve chronic hepatitis It is effective in improving liver function in patients with decompensated cirrhosis & may prevent the need for transplantation. Long term therapy is complicated by the development of HBV -DNA polymerase mutants which may occur after 9 months of treatment & is characterized by arise in viral load during treatment.
Adefovir: Nucleotide analogue that is phosphorelated to yield a drug which inhibits HBV-DNA polymerase. It reduces HBV-DNA by 3 -4 logs. Enhances the frequency of HBe. Ag seroconversion. Leads to histological improvement. Contraindicated in renal failure. HBV-DNA mutant develop at lower rate than with Lamivudine. 2% being identified after 2 years of treatment.
In HBe. Ag positive chronic hepatitis treatment with 10 mg of Adefovir for 48 weeks produces normal liver biochemistry in 48%. Suppresses serum HBV-DNA in 39%. Leads to e antigen seroconversion in 14%. In HBe. Ag negative chronic hepatitis treatment with adefovir for 48 weeks reduces ALT to normal in 72% & renders serum HBV-DNA undetectable in 55% of patients. Relapse occurs on stopping treatment. The optimum length of treatment remains unknown
Other drugs : Entecavir & Telbivudine: These are more effective than Lamivudine & adefovir in reducing viral load in HBe Ag +ve & HBe Ag –ve chronic hepatitis. Tenofovir & Emcitabine which has anti-HIV efficacy. Tenofovir is superior to Adefovir in the treatment of chronic hepatitis. The use of combination antiviral therapy is still unclear.
Liver transplantation was contraindicated in presence of hepatitis B because infection often recurred in the graft. The use of post liver transplant prophylaxis with Lamivudine & hepatitis B immunoglobulin has reduced the reinfection rate to 10% & increased 5 year survival to 80% making transplantation an acceptable treatment option in selected cases.
Prevention The virus is about 10 times more infectious than hepatitis C , which in turn is about 10 times more infectious than HIV. A recombinant hepatitis B vaccin containing HBs. Ag ( Engerix ) & is capable of producing active immunization in 95% of normal individuals.
Recombinant HBV containing HBs Ag vaccin is available& is indicated for: • Parantral drug abuse. • Homosexual. • Close contacts of infected individuals. Newborn of infected mother Regular sexual partners. • Patients on chronic hemodialysis. Patients with chronic liver disease. • Medical &Nursing personnel. • Lab. Staff handling blood. IM injection of Hyper immune S. globulin should be given In <24 H or <1 W of exposure.
Prognosis Acute Hepatitis: 90 - 95% = full recovery. 5 -10% = chronic Infection , which occur in infants infected from mother, Immunedef. Patients like Downs Syndrome, HIV infection. Recovery from acute HBV infection occurs within 6 months by appearance of antibodies to viral antigens.
Chronic infection: Most patients with chronic HBV are asymptomatic & develop complications such as cirrhosis & Hepatocellular carcinoma. Cirrhosis develops in 15 -20% of patients with chronic HBV over 5 -20 years. The risk is higher in those who are e antigen positive.
Hepatitis D RNA defective virus, it requires hepatitis B virus for replication. & has same sources of spread as HBV. 1: Simultaneous infection : acute& severe infection with recovery from HBV infection. 2: Infection in patients with chronic carrier : acute Infection. 3: Chronic infection with both HBV& HDV: more rapid progression to chronic hepatitis & cirrhosis.
Investigations Simultaneous infection of HDV + HBV : Generally followed by full recovery. Showed low titers of anti HDV Ig. M within few days of onset of the illness. Antibodies usually disappear within 2 months. Superinfection of HDV+ HBV: High titers of anti-HDV , initially of Ig. M & later Ig. G , such patients develop chronic infection with persistent high AB level.
Prevention Preventing hepatitis B effectively prevent hepatitis D
Hepatitis C v RNA containing flavi virus. v Acute symptomatic infection is rare. Ø Is the cause of what used to be known (non-A , non-B hepatitis) which is a syndrome of acute hepatitis often with jaundice seen after transfusion of blood or blood products q. Chronic infection occur in 80% of individuals exposed to the virus. q Chronic infection is usually asymptomatic until progression to cirrhosis. q Fatigue can complicate chronic infection & unrelated to the degree of liver damage.
. Risk factors for acquisition : 1 -IV drug misuse. 2 -Unscreened blood products. 3 - Vertical transmission ( 3% ). 4 -Needle stick injury ( 3%). 5 -Iatrogenic Parantral transmission unclean vaccination needles. 6 -Sharing tooth brushes/ razors

Investigations Serology & virology: HCV protein contains several antigen that give rise to antibodies which may take 6 -12 weeks to appear following acute infection. Hepatitis C PCR can be identified as early as 2 -4 weeks. Active infection is confirmed by the presence of serum C RNA in anyone with antibody positive.
Genotype: There are 6 common viral genotypes whose distribution varies world-wide. Genotype has no effect on progression of liver disease but does affect response to treatment. Genotype 1 is most common in northern Europe & is less easy to eradicate with current treatment.
Liver function tests May be normal or show fluctuating serum transaminases with ALT between 50200 U/L. Jaundice is rare & only usually appears in end-stage cirrhosis.
Liver histology Serum transaminases in hepatitis C are poor predictor of the degree of liver fibrosis which has developed as a result of chronic viral hepatitis. Liver biopsy is often required to stage the degree of liver damage. The most common scoring system used in hepatitis C is the Metavir system , which scores fibrosis from 1 to 4.
Management The aim of treatment is to eradicate infection. Pegylated alpha-interferon given weekly subcutaneously + oral ribavirin ( a synthetic nucleotide analogue ) 24 - 48 weeks with sustained virological response of 55%. Cure is defined as loss of virus from serum 6 months after completing therapy (SVR). The length of treatment & efficacy depend on viral genotype.
Side effect : Ribavirin : hemolytic anaemia. Interferon : Flu-like illness. Irritability & depression. Liver transplantation is considered: Complications of cirrhosis. Diuretic-resistant ascites. HCV is almost always recurs in the transplanted liver & up to 15% will develop cirrhosis in the liver graft within one year of transplantation.

Prevention & Prognosis There is no passive or active protection against HCV. 20% of chronic HCV develop cirrhosis within 20 years. Risk factors for progression: Male gender. Immsuppression ( such as co-infection with HIV) Heavy alcohol misuse.
Once cirrhosis is present : 2 -5% per year will develop primary Hepatocellular carcinoma. The 5 and 10 year survival rates are 95% & 81% respectively. One quarter of cirrhosis will develop complications within 10 years. Once ascites develop the 5 -survival is around 50%.
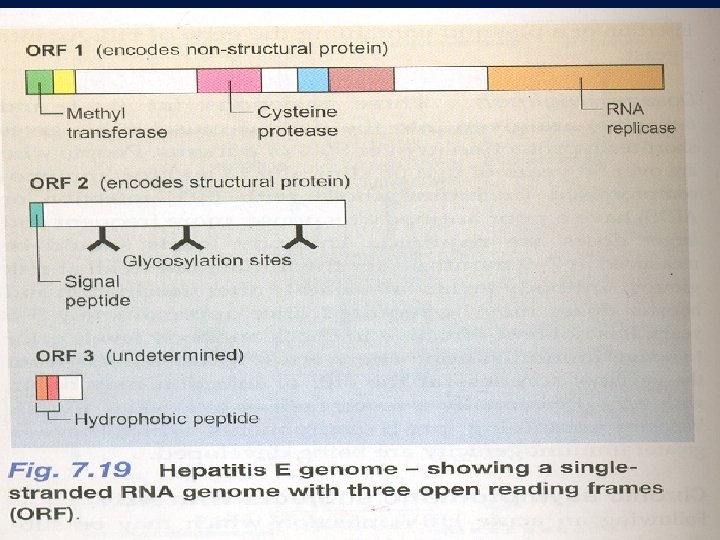
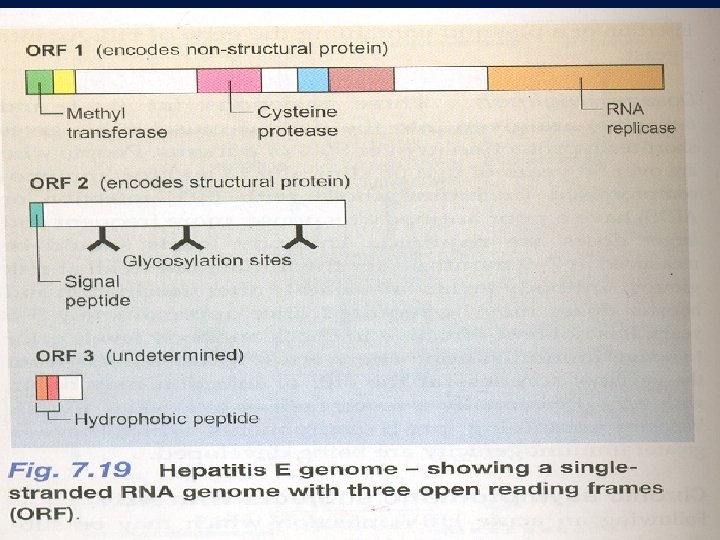
Hepatitis E RNA virus. spread by feco oral route. Clinical illness resemble HAV infection. In most cases is presented with self-limiting acute hepatitis. In pregnant female has high risk of acute hepatic failure which has high mortality. Chronic infection doesn't occur.
Investigations In acute infection Ig. M antibodies to HEV is positive. Prevention There is no active or passive immunity to hepatitis E.

Other forms of viral hepatitis Non A , Non B, Non C (NANBNC) Or non-A-E hepatitis: CMV& EBV , Yellow fever, Chicken pox, Measles, Rubella & HIV infection.
 Hepatitis viral
Hepatitis viral Causes of viral hemorrhagic fever
Causes of viral hemorrhagic fever Hepatitis c symptoms in men
Hepatitis c symptoms in men What is hepatitis b
What is hepatitis b Proximate behaviour in animals
Proximate behaviour in animals Proximate causation biology example
Proximate causation biology example Common causes of faulty radiographs
Common causes of faulty radiographs Viral inoculation in embryonated egg
Viral inoculation in embryonated egg Viral life cycle
Viral life cycle Viral receptors
Viral receptors When blood sample hemolyzed
When blood sample hemolyzed Andrew lippman mit
Andrew lippman mit Csf findings in meningitis table
Csf findings in meningitis table Dha mcq
Dha mcq Section 24-1 viral structure and replication
Section 24-1 viral structure and replication Viral
Viral Viral inoculation in embryonated egg
Viral inoculation in embryonated egg Infinitive viral infection
Infinitive viral infection Procalcitonin
Procalcitonin Meningitis
Meningitis Itil wikipedia fr
Itil wikipedia fr Pantropizm
Pantropizm Viral arthritis
Viral arthritis Viral entry
Viral entry Viral recombination
Viral recombination Varicela variola
Varicela variola Spasmodic croup
Spasmodic croup Viral shedding
Viral shedding Trivalent vaccin herpes
Trivalent vaccin herpes Aerochamber definition
Aerochamber definition Ciclo viral
Ciclo viral Vacina trplice viral
Vacina trplice viral Egg inoculation diagram
Egg inoculation diagram An acute highly contagious viral disease
An acute highly contagious viral disease Vaccins à vecteur viral
Vaccins à vecteur viral Exocitose
Exocitose Eline's viral
Eline's viral Viral dna
Viral dna Replicação viral ciclo lítico e lisogênico
Replicação viral ciclo lítico e lisogênico The dynamics of viral marketing
The dynamics of viral marketing Viral infection
Viral infection Factors of 12 and 42
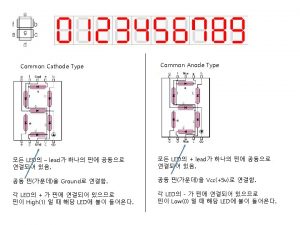
Factors of 12 and 42 Common anode and common cathode
Common anode and common cathode Multiples of 9 and 21
Multiples of 9 and 21 Common factors and common multiples
Common factors and common multiples How to find lowest common factor
How to find lowest common factor Least common multiple of 12 and 42
Least common multiple of 12 and 42 Gail lupica
Gail lupica Hepatitis types chart
Hepatitis types chart Hep b mode of transmission
Hep b mode of transmission Hepatitis c symtoms
Hepatitis c symtoms Hepatitis e
Hepatitis e Alcoholic hepatitis
Alcoholic hepatitis Score simplificado hepatitis autoinmune
Score simplificado hepatitis autoinmune Infectious canine hepatitis in dogs
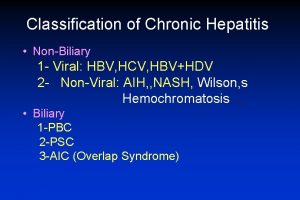
Infectious canine hepatitis in dogs Classification of chronic hepatitis
Classification of chronic hepatitis