The liver Function Anatomy The liver is a

- Slides: 37
The liver Function
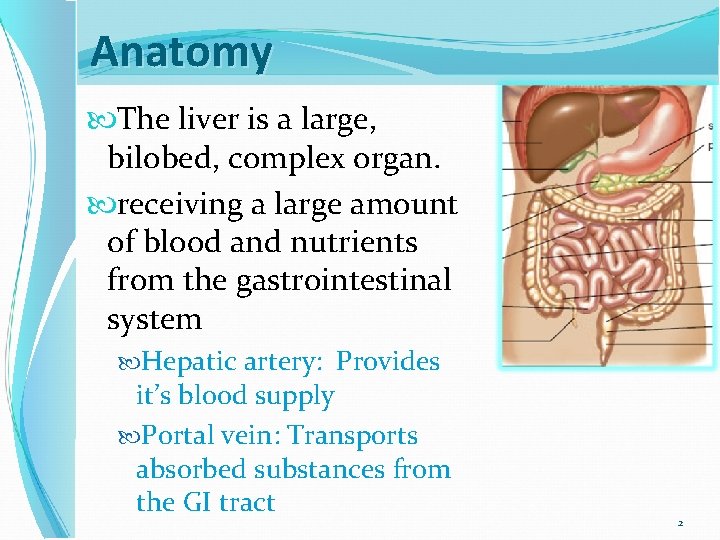
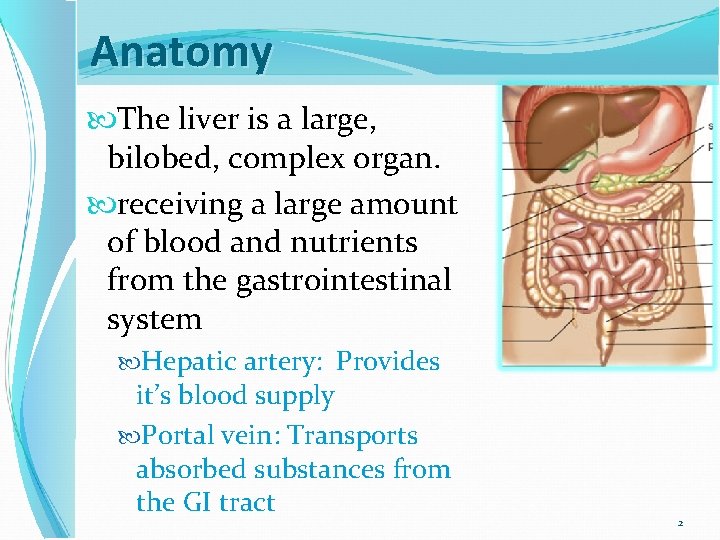
Anatomy The liver is a large, bilobed, complex organ. receiving a large amount of blood and nutrients from the gastrointestinal system Hepatic artery: Provides it’s blood supply Portal vein: Transports absorbed substances from the GI tract 2
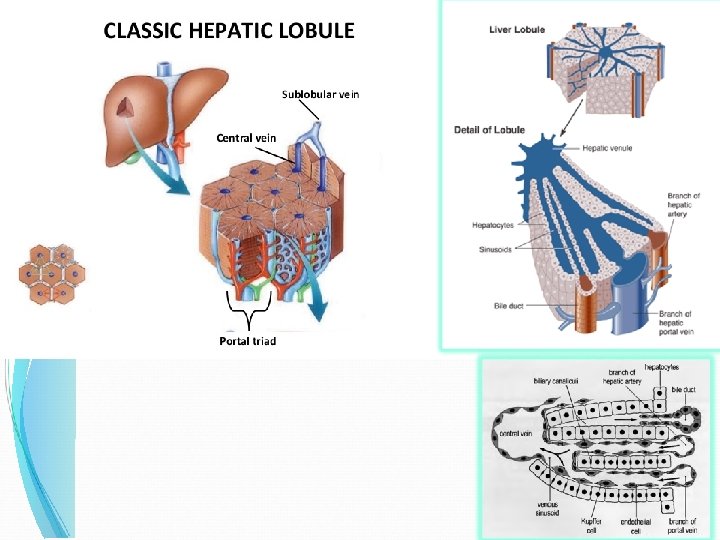
Structural Unit Lobules are the functional units, consisting of clusters of hepatocytes around a central vein Sinusoids, vascular spaces, are lined by Kupffer cells. Blood from these spaces drain into the central veins. 3
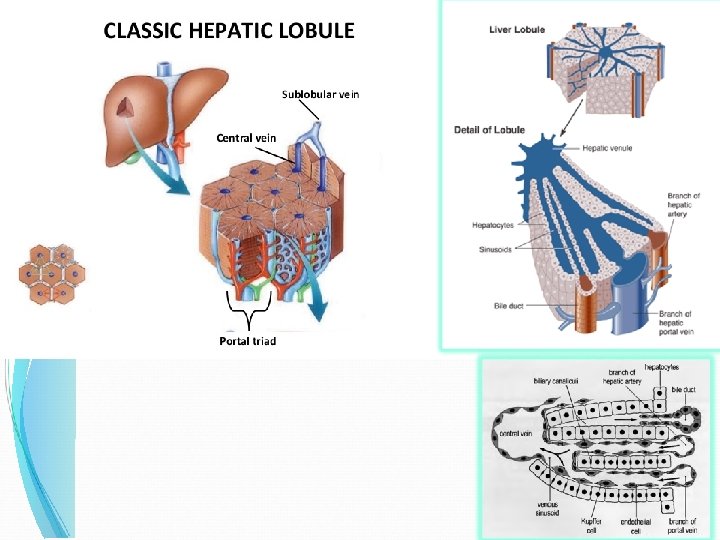
4
Major functions of the liver The liver performs four major functions: excretion, synthesis, detoxification, and storage. The liver is so important that if the liver becomes nonfunctional, death will occur with 24 hours due to hypoglycemia. 5
1 - Excretory Function One of the most important liver functions, and one that is disturbed in a large number of diseases is the excretion of bile Bile comprises: bile acids or salts, bile pigments & others Total bile production averages 3 liters/ day Bilirubin is the principal pigment in bile 6
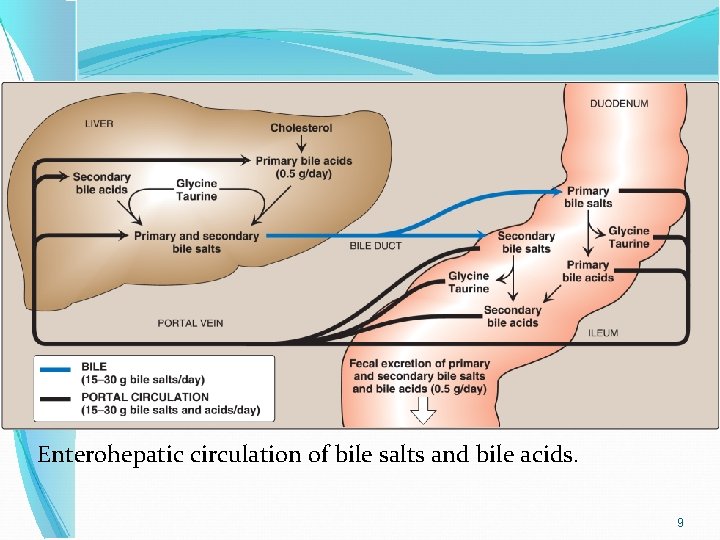
Bile Acids The primary bile acids are: cholic acid and chenodeoxycholic acid Formed in the liver from cholesterol. Bile acids are conjugated with the amino acid glycine or with taurine (derivative of the sulfurcontaining amino acid) forming bile salts. Gall bladder empties bile salts in the small intestine where the bile is involved in digestion and absorption of lipids. 7
Bile Acids Bacteria in ileum and colon dehydrate bile salts to secondary bile acids "deoxycholic and lithocholic" which are subsequently absorbed. The absorbed bile acids enter the portal circulation to the liver where they are reconjugated and excreted. 8
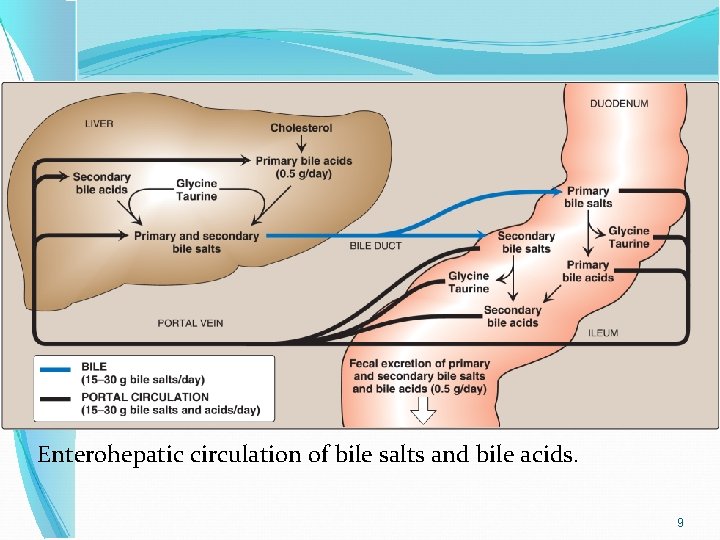
Enterohepatic circulation of bile salts and bile acids. 9
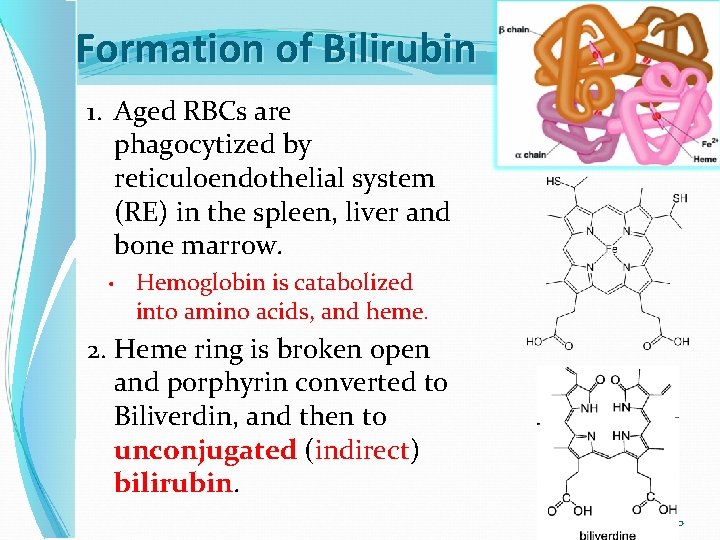
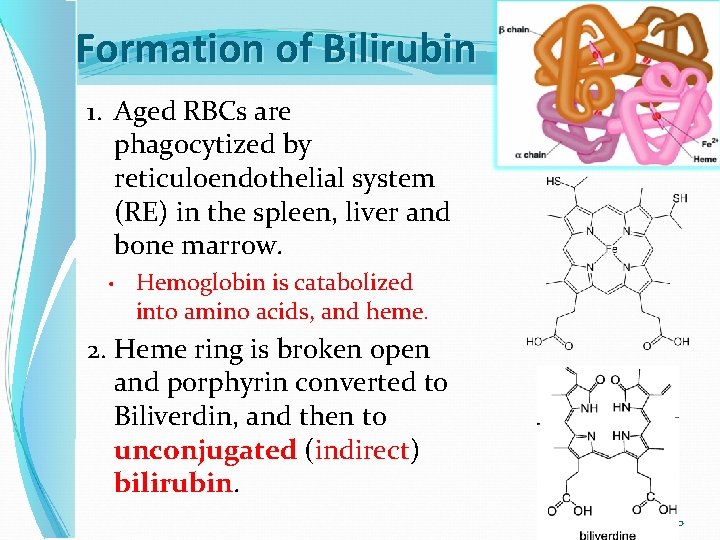
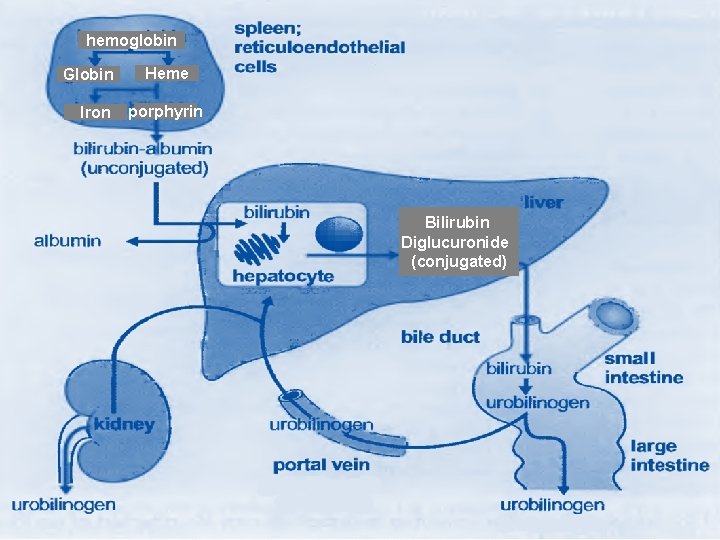
Formation of Bilirubin 1. Aged RBCs are phagocytized by reticuloendothelial system (RE) in the spleen, liver and bone marrow. • Hemoglobin is catabolized into amino acids, and heme. 2. Heme ring is broken open and porphyrin converted to Biliverdin, and then to unconjugated (indirect) bilirubin. 10
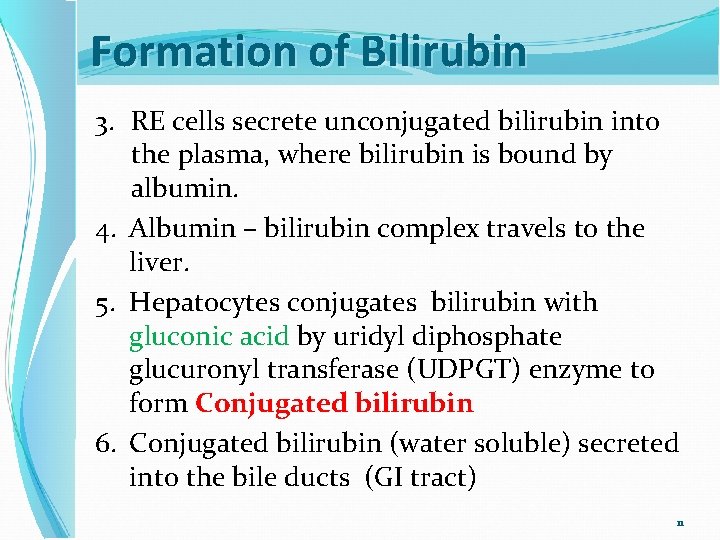
Formation of Bilirubin 3. RE cells secrete unconjugated bilirubin into the plasma, where bilirubin is bound by albumin. 4. Albumin – bilirubin complex travels to the liver. 5. Hepatocytes conjugates bilirubin with gluconic acid by uridyl diphosphate glucuronyl transferase (UDPGT) enzyme to form Conjugated bilirubin 6. Conjugated bilirubin (water soluble) secreted into the bile ducts (GI tract) 11
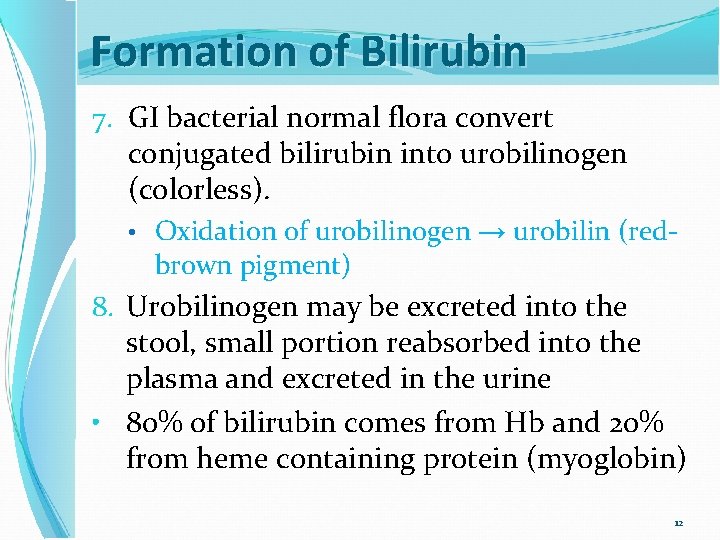
Formation of Bilirubin 7. GI bacterial normal flora convert conjugated bilirubin into urobilinogen (colorless). • Oxidation of urobilinogen → urobilin (redbrown pigment) 8. Urobilinogen may be excreted into the stool, small portion reabsorbed into the plasma and excreted in the urine • 80% of bilirubin comes from Hb and 20% from heme containing protein (myoglobin) 12
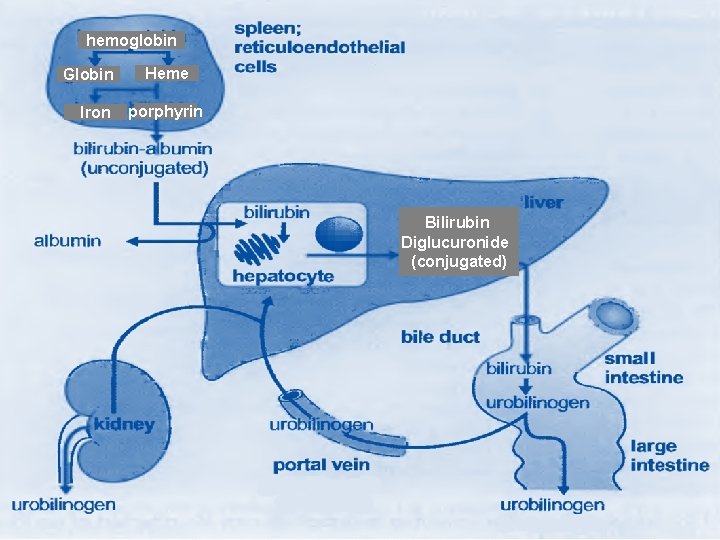
hemoglobin Globin Iron Heme porphyrin Bilirubin Diglucuronide (conjugated) 13

Major functions of the liver 2. Synthetic Carbohydrate metabolism gluconeogenesis, glycogen synthesis and breakdown Fat metabolism fatty acid synthesis, cholesterol synthesis and excretion, lipoprotein synthesis…. . Protein metabolism synthesis of plasma proteins (including some coagulation factors but not immunoglobulins) 14
Major functions of the liver 3. Detoxification and Drug Metabolism Every substance that is absorbed in the GIT must first pass through the liver (first pass). This allows important substances to reach the circulation and prevent toxic or harmful substances from reaching the circulation The body has two mechanisms for detoxification of foreign materials and metabolic products: It may either bind the material reversibly so as to inactivate the compound, or it may chemically modify the compound so it can be excreted � Storage Glycogen, vitamin A , vitamin B 12 15
Disorders of Liver Jaundice Cirrhosis Tumors Hepatitis Drug & Alcohol related disorders 16
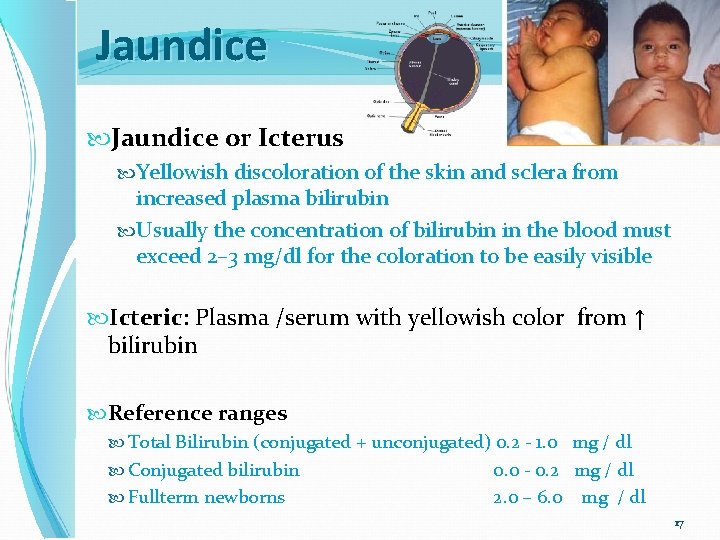
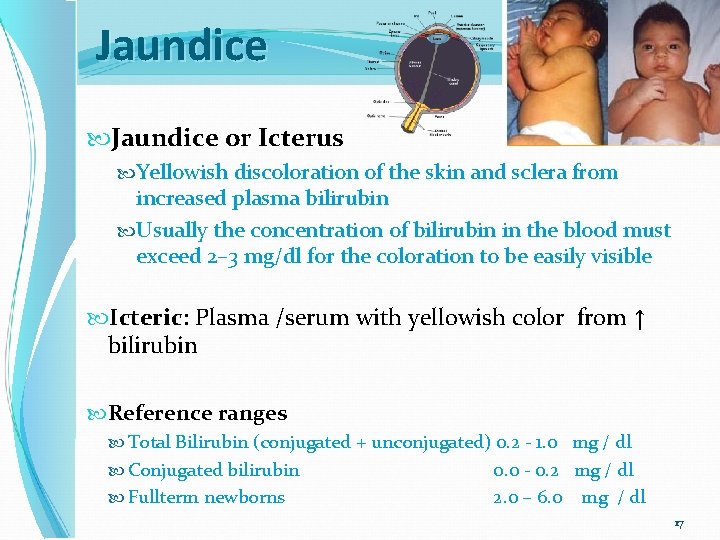
Jaundice or Icterus Yellowish discoloration of the skin and sclera from increased plasma bilirubin Usually the concentration of bilirubin in the blood must exceed 2– 3 mg/dl for the coloration to be easily visible Icteric: Plasma /serum with yellowish color from ↑ bilirubin Reference ranges Total Bilirubin (conjugated + unconjugated) 0. 2 - 1. 0 mg / dl Conjugated bilirubin Fullterm newborns 0. 0 - 0. 2 mg / dl 2. 0 – 6. 0 mg / dl 17
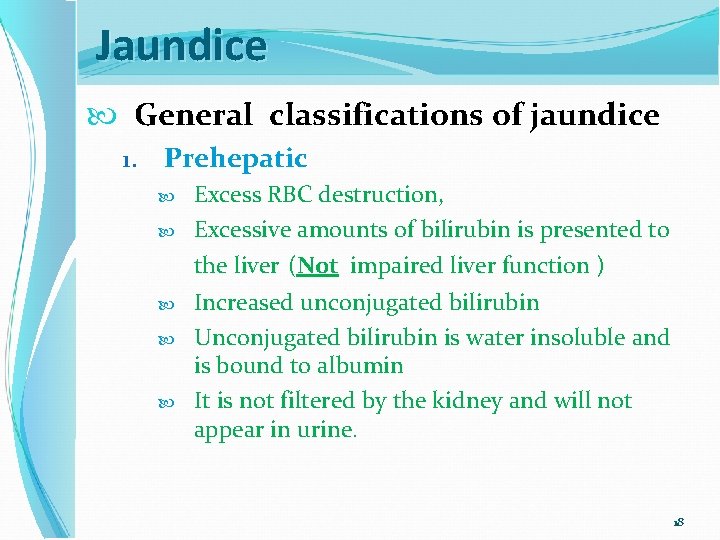
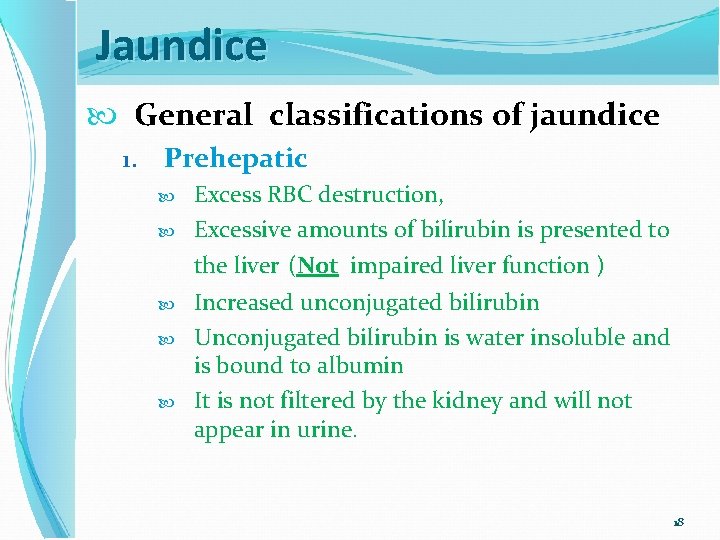
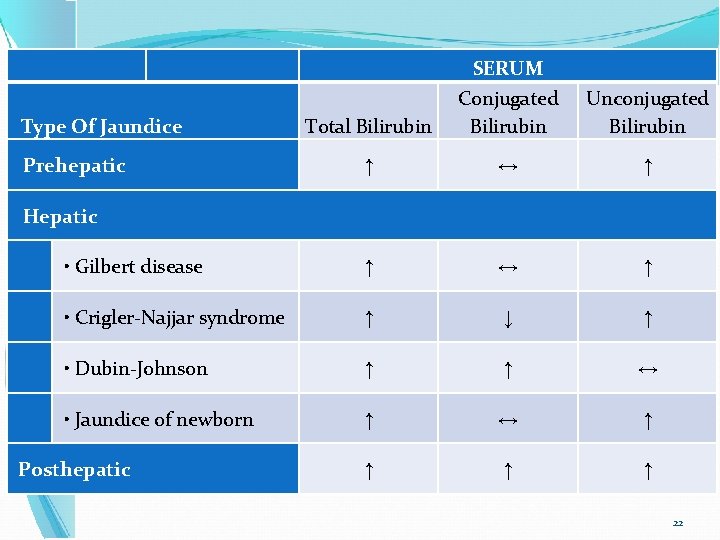
Jaundice General classifications of jaundice 1. Prehepatic Excess RBC destruction, Excessive amounts of bilirubin is presented to the liver (Not impaired liver function ) Increased unconjugated bilirubin Unconjugated bilirubin is water insoluble and is bound to albumin It is not filtered by the kidney and will not appear in urine. 18
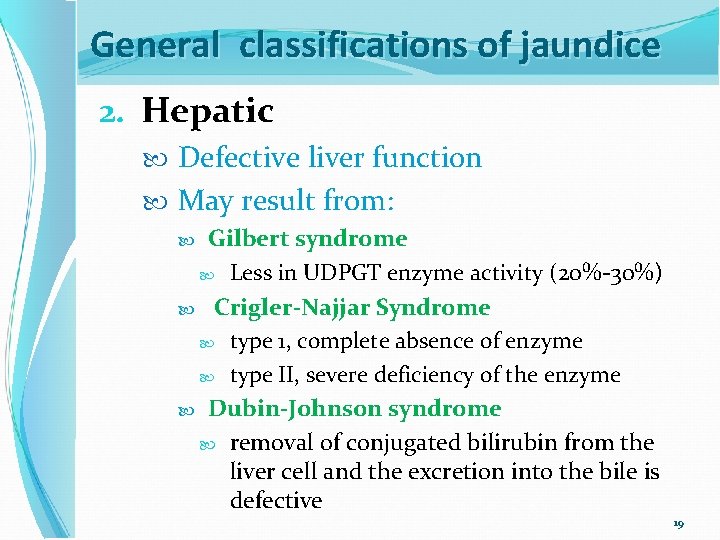
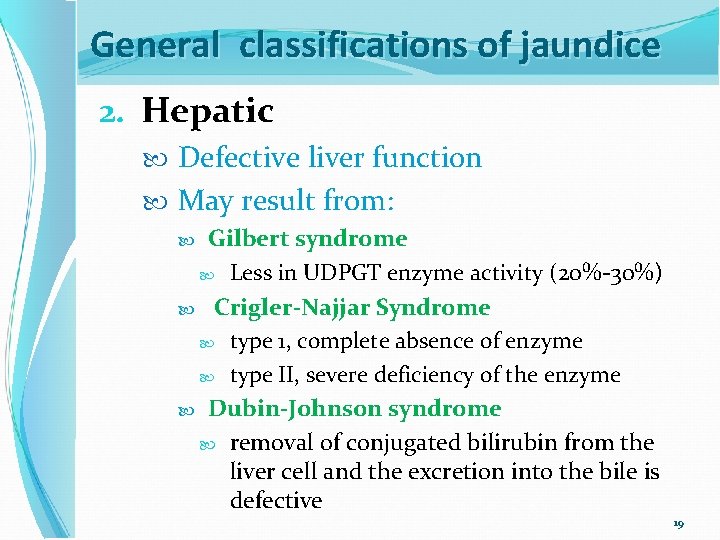
General classifications of jaundice 2. Hepatic Defective liver function May result from: Gilbert syndrome Less in UDPGT enzyme activity (20%-30%) Crigler-Najjar Syndrome type 1, complete absence of enzyme type II, severe deficiency of the enzyme Dubin-Johnson syndrome removal of conjugated bilirubin from the liver cell and the excretion into the bile is defective 19
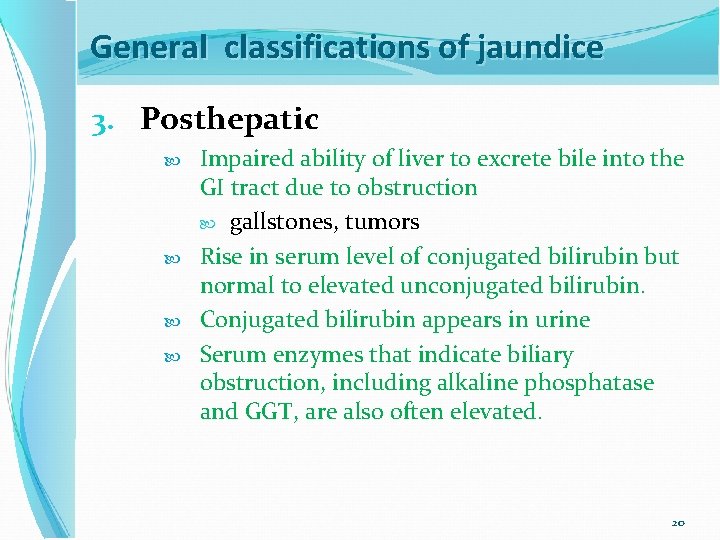
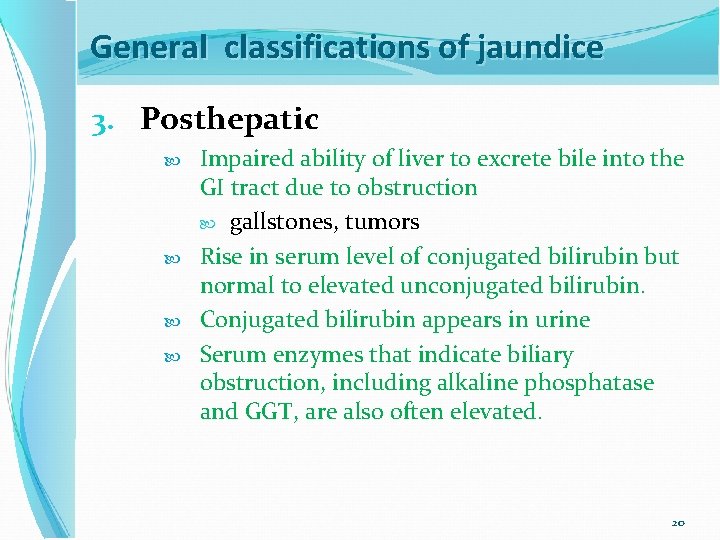
General classifications of jaundice 3. Posthepatic Impaired ability of liver to excrete bile into the GI tract due to obstruction gallstones, tumors Rise in serum level of conjugated bilirubin but normal to elevated unconjugated bilirubin. Conjugated bilirubin appears in urine Serum enzymes that indicate biliary obstruction, including alkaline phosphatase and GGT, are also often elevated. 20
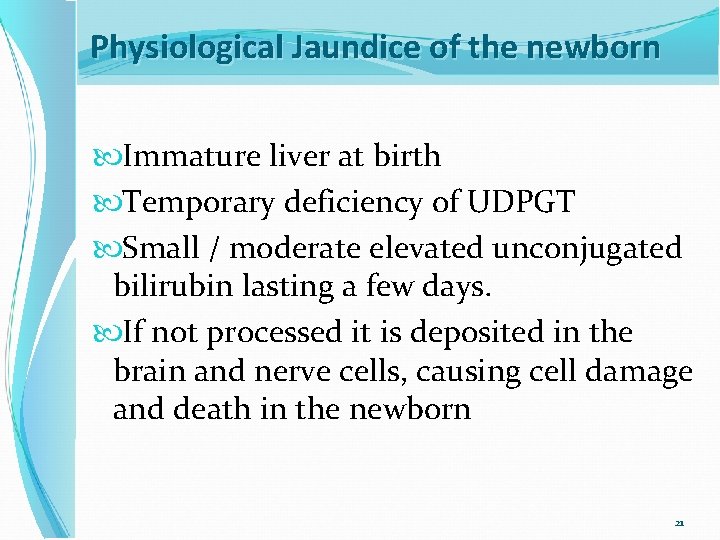
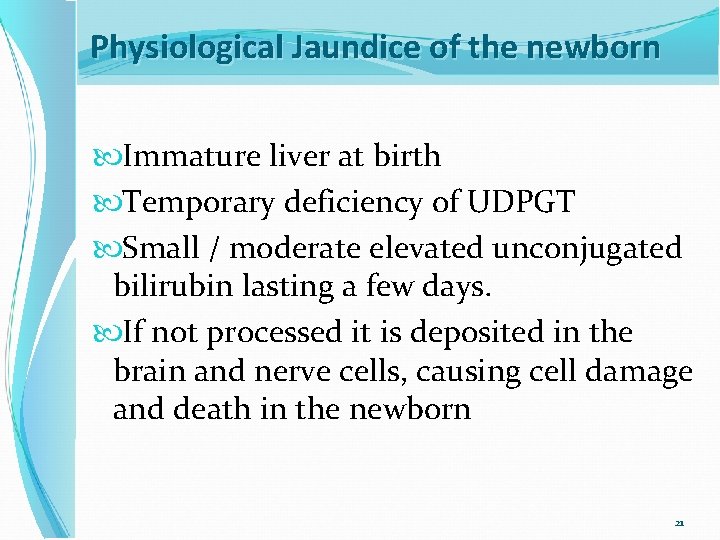
Physiological Jaundice of the newborn Immature liver at birth Temporary deficiency of UDPGT Small / moderate elevated unconjugated bilirubin lasting a few days. If not processed it is deposited in the brain and nerve cells, causing cell damage and death in the newborn 21
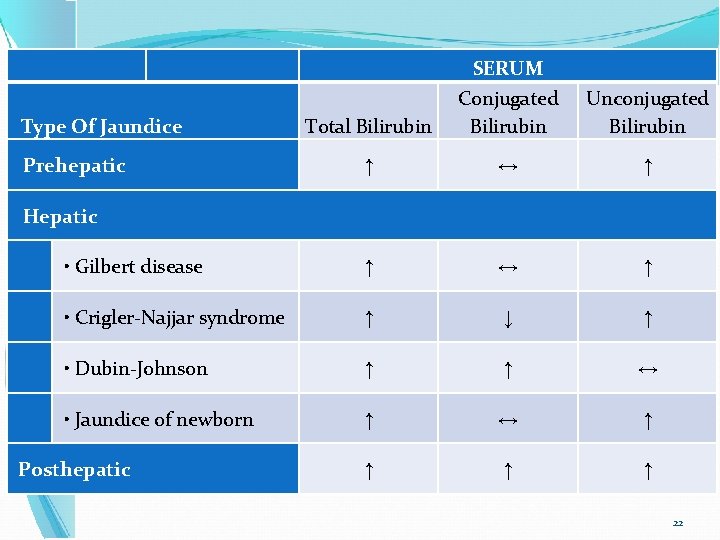
Total Bilirubin SERUM Conjugated Bilirubin Unconjugated Bilirubin ↑ ↔ ↑ • Gilbert disease ↑ ↔ ↑ • Crigler-Najjar syndrome ↑ ↓ ↑ • Dubin-Johnson ↑ ↑ ↔ • Jaundice of newborn ↑ ↔ ↑ ↑ Type Of Jaundice Prehepatic Hepatic Posthepatic 22
Other Disorders of Liver Cirrhosis A consequence of chronic liver disease characterized by replacement of liver tissue by fibrous scar tissue leading to progressive loss of liver function. Cirrhosis is most commonly caused by alcoholism, hepatitis B and C and fatty liver disease but has many other possible causes. 23
Other Disorders of Liver Tumors Cancers of the liver are classified as: Primary (cancer that begins in the liver cells) metastatic when tumors from other parts of the body spread (metastasize) to the liver. Cancers of the liver may also be classified as: benign or malignant Whether primary or metastasic, any malignant tumor in the liver is: a serious finding and carries a poor prognosis, with survival times measured in months. 24
Other Disorders of Liver Drug- and Alcohol-Related Disorders most common mechanism of toxicity is via an immune-mediated injury to the hepatocytes Hepatitis Inflammation of the liver Caused by viruses, bacteria, chemicals and others Among viruses causing hepatitis are hepatitis types A, B, C, D & E 25
Assessment of Liver Function A liver function tests (LFT) are group of blood tests that give an indication of whether the liver is functioning properly. The tests are also very useful to see if there is active damage in the liver (hepatitis) or slow bile flow (cholestasis). Because the liver is the site for the conjugation of bilirubin, The liver may be assessed by measurement of total and conjugated bilirubin. 26
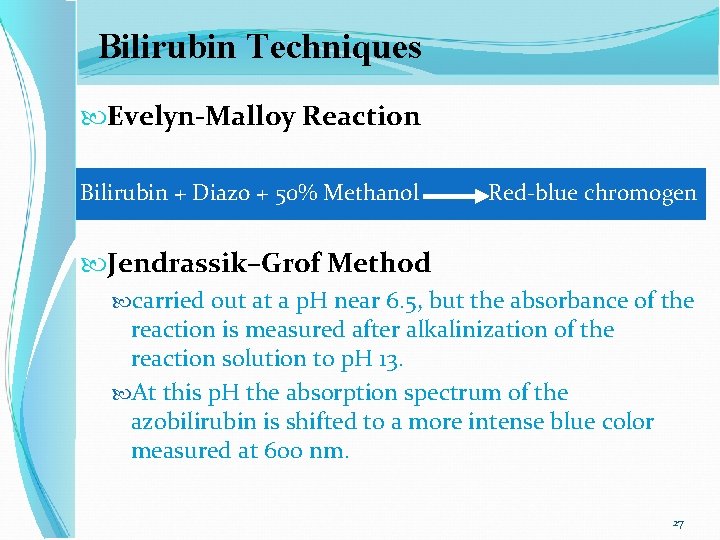
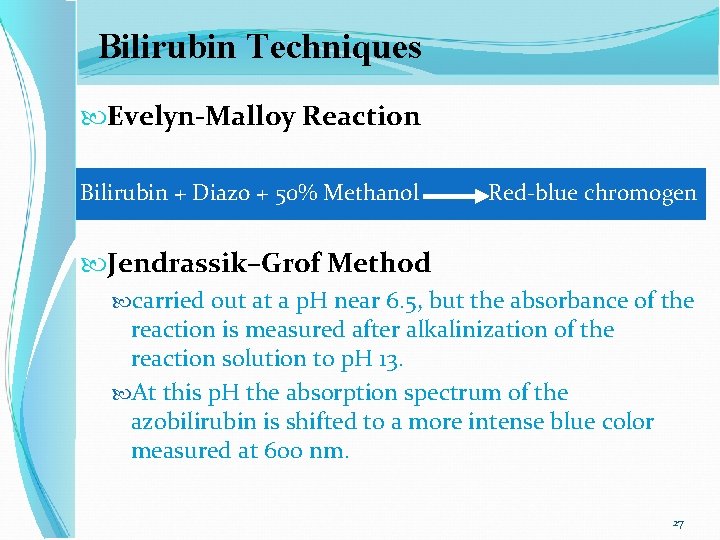
Bilirubin Techniques Evelyn-Malloy Reaction Bilirubin + Diazo + 50% Methanol Red-blue chromogen Jendrassik–Grof Method carried out at a p. H near 6. 5, but the absorbance of the reaction is measured after alkalinization of the reaction solution to p. H 13. At this p. H the absorption spectrum of the azobilirubin is shifted to a more intense blue color measured at 600 nm. 27
Direct measurement of bilirubin Because bilirubin has a distinctive color, it is possible to measure bilirubin directly No chemical reaction is necessary This procedure has limited value because of other colored plasma substances that interfere Only newborns lack these interfering substances. 28
Other tests related to hepatic disease Elevated Enzyme activity The enzymes ALP, ALT, AST, GGT, and 5′- nucleotidase are helpful in the assessment of the proper functioning and inflammatory status of the liver. Protein Synthesis Because the liver is the site for the synthesis of many proteins, the liver may be assessed by measurement total protein and albumin Decreased levels of albumin usually develop only in severe hepatic dysfunction, Plasma proteins ↑ Prothrombin time ( PT ) 29
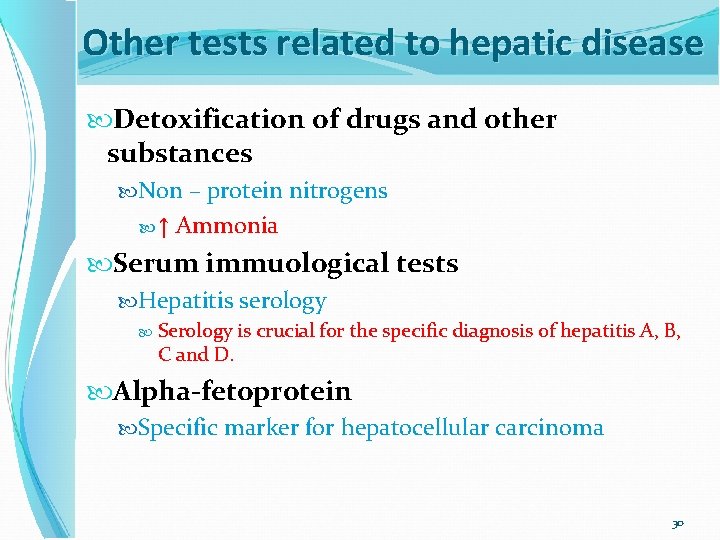
Other tests related to hepatic disease Detoxification of drugs and other substances Non – protein nitrogens ↑ Ammonia Serum immuological tests Hepatitis serology Serology is crucial for the specific diagnosis of hepatitis A, B, C and D. Alpha-fetoprotein Specific marker for hepatocellular carcinoma 30
Correlation of laboratory results is an indication of accuracy and appropriateness of results. In this case, increased levels of enzymes and bilirubin and lowered protein correlate with liver disease. The extent of the increased alkaline phosphatase and the presence of increases in both total and direct bilirubin help to specify this liver disorder as obstructive jaundice 31
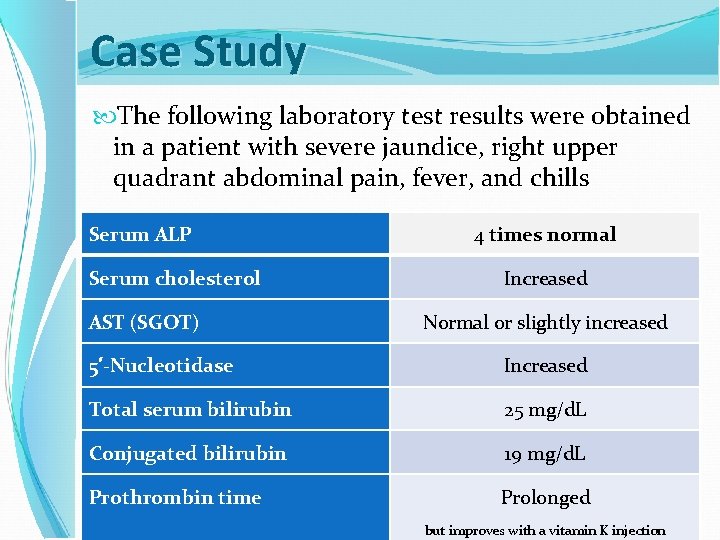
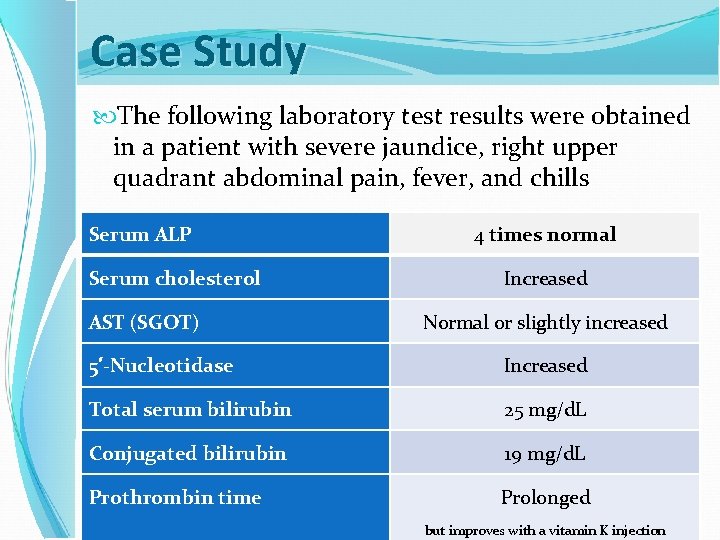
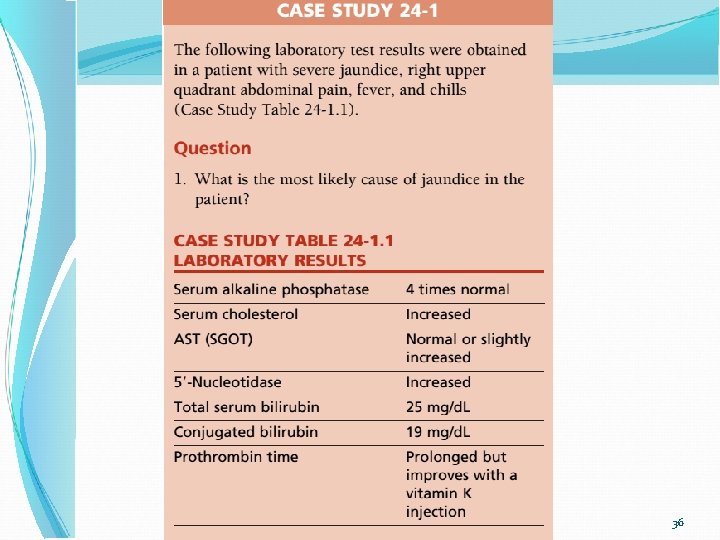
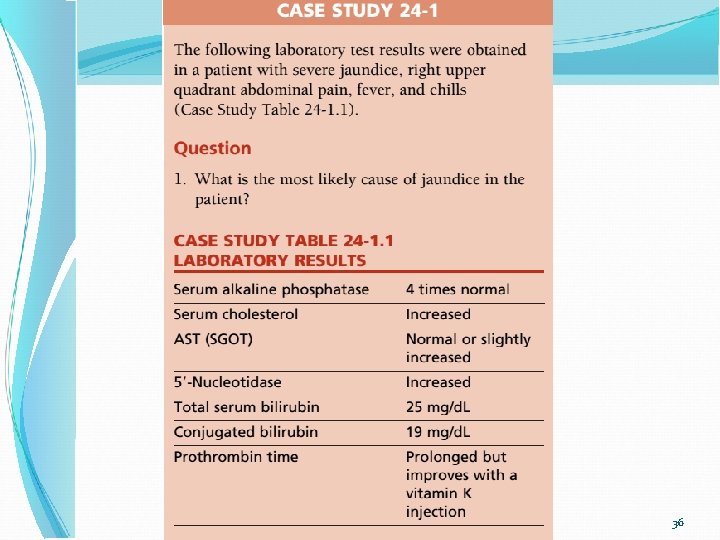
Case Study The following laboratory test results were obtained in a patient with severe jaundice, right upper quadrant abdominal pain, fever, and chills Serum ALP Serum cholesterol AST (SGOT) 4 times normal Increased Normal or slightly increased 5′-Nucleotidase Increased Total serum bilirubin 25 mg/d. L Conjugated bilirubin 19 mg/d. L Prothrombin time Prolonged but improves with a vitamin K injection 32
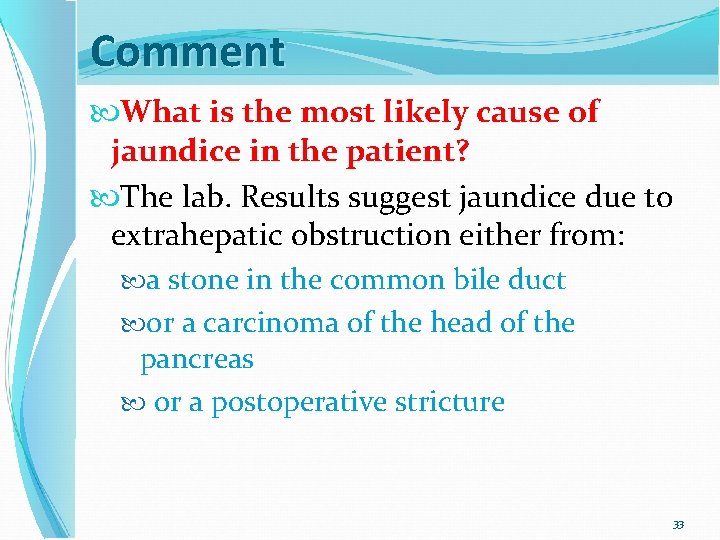
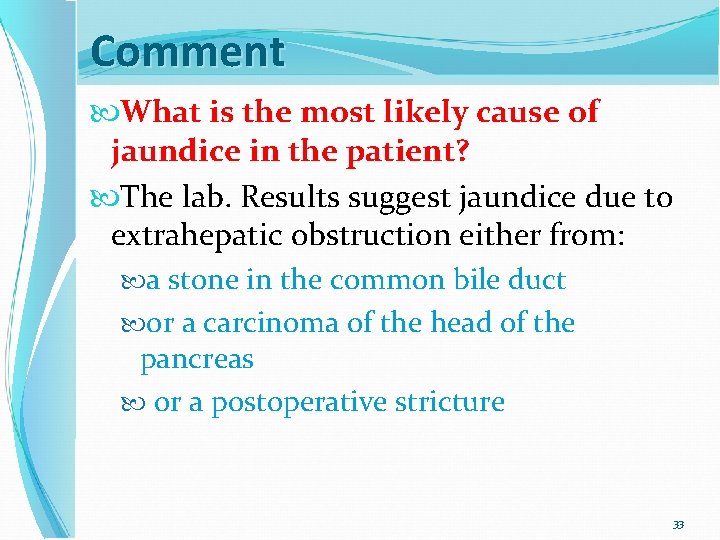
Comment What is the most likely cause of jaundice in the patient? The lab. Results suggest jaundice due to extrahepatic obstruction either from: a stone in the common bile duct or a carcinoma of the head of the pancreas or a postoperative stricture 33
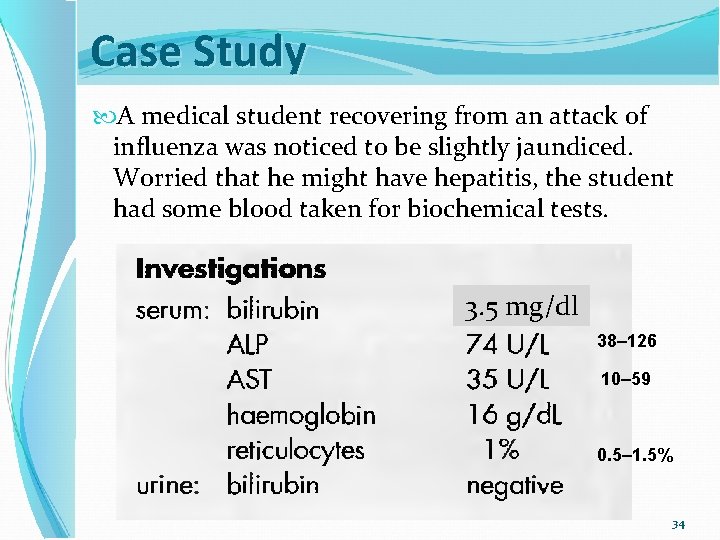
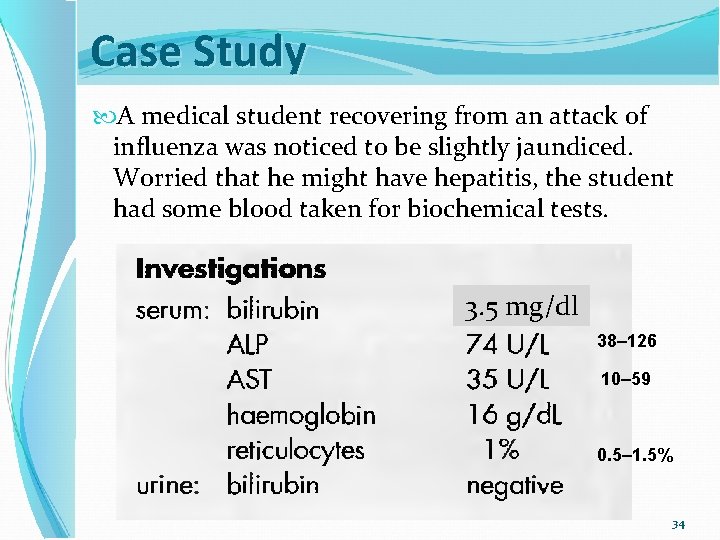
Case Study A medical student recovering from an attack of influenza was noticed to be slightly jaundiced. Worried that he might have hepatitis, the student had some blood taken for biochemical tests. 3. 5 mg/dl 38– 126 10– 59 0. 5– 1. 5% 34
Comment The negative urine bilirubin indicates that the excess bilirubin in the serum is unconjugated. There is no evidence of hepatocellular damage and the normal haemoglobin and reticulocyte count indicate that haemolysis cannot be the cause of the raised bilirubin. By elimination, the diagnosis is Gilbert's syndrome. 35
36
The laboratory test results suggest jaundice as a result of extrahepatic obstruction: Causes A stone in the common bile duct, carcinoma of the head of the pancreas, or, possibly, a postoperative stricture. 37