Normal structure of liver Normal function of liver














- Slides: 136
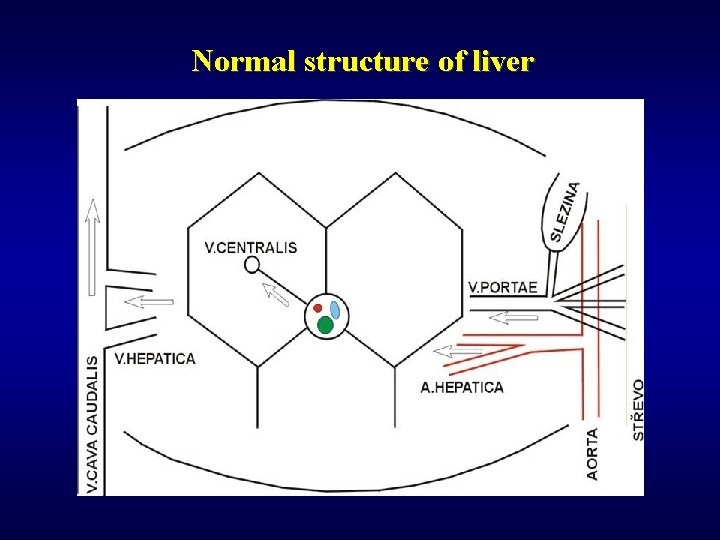
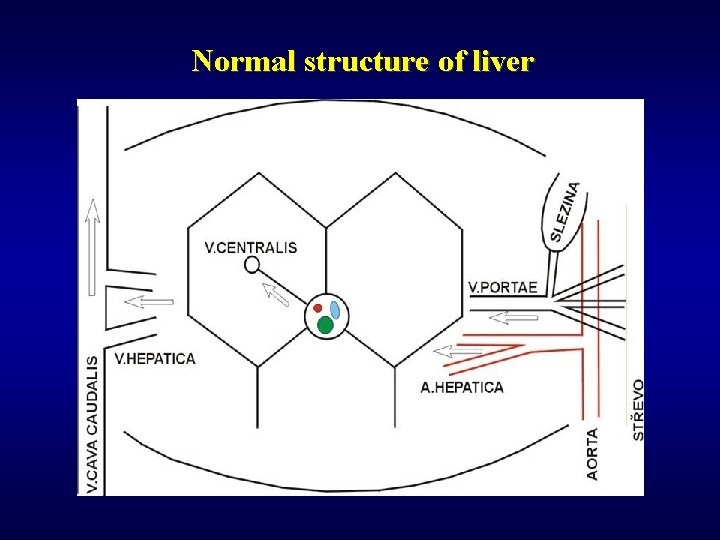
Normal structure of liver
Normal function of liver ü Metabolic (glucose homeostasis…) ü Synthetic (albumin, coagulation factors) ü Storage (glycogen, triglycerides, Fe, Cu, vitamins soluble in fat) ü Catabolic (endogenous substances – hormones…, exogenous substances – drugs, alcohol…) ü Excretoric (bile)
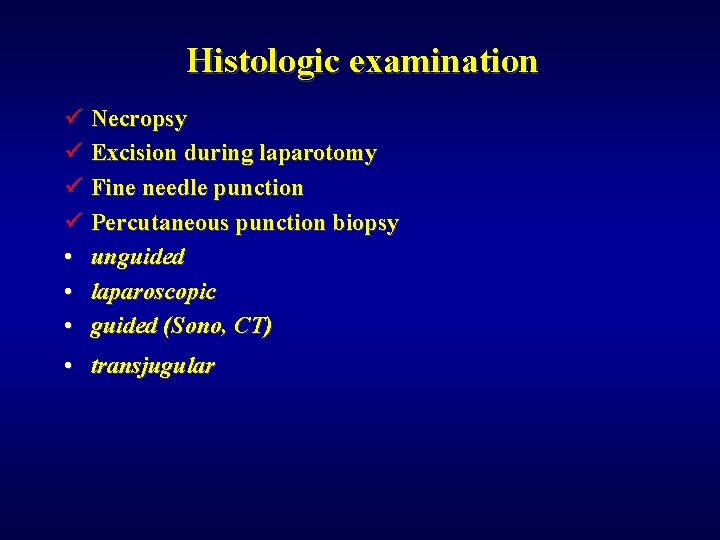
Histologic examination ü Necropsy ü Excision during laparotomy ü Fine needle punction ü Percutaneous punction biopsy • unguided • laparoscopic • guided (Sono, CT) • transjugular
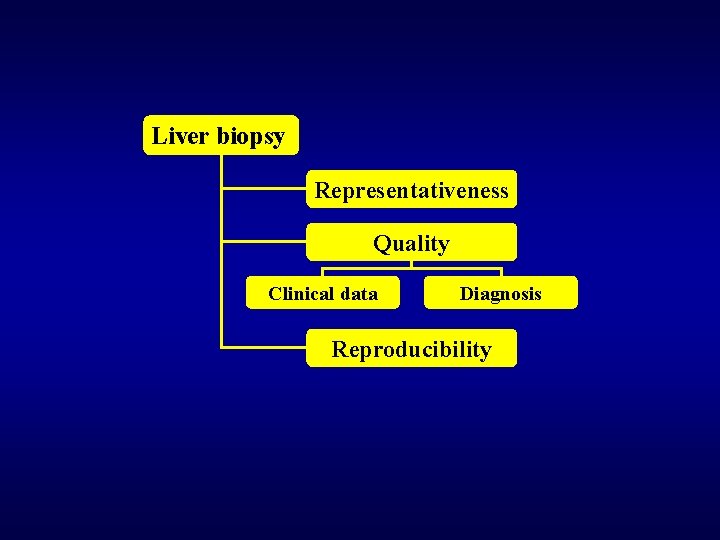
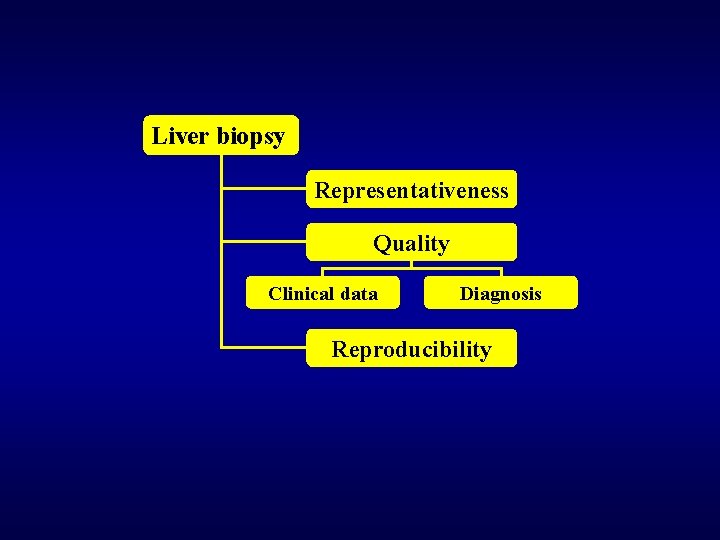
Liver biopsy Representativeness Quality Clinical data Diagnosis Reproducibility
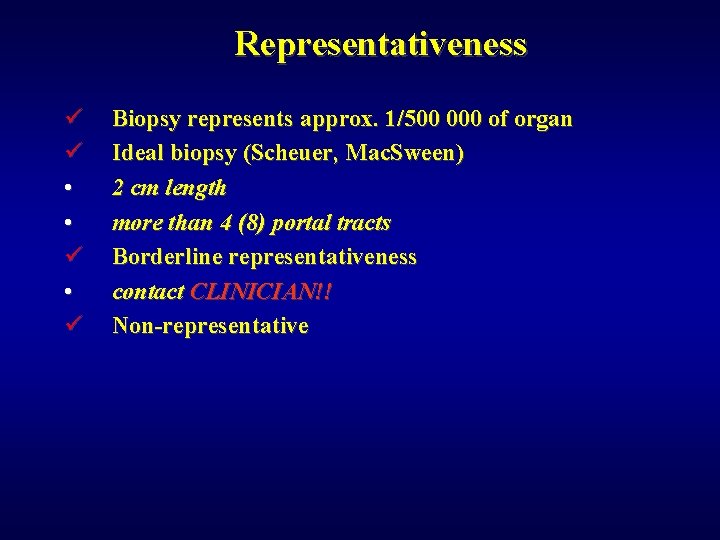
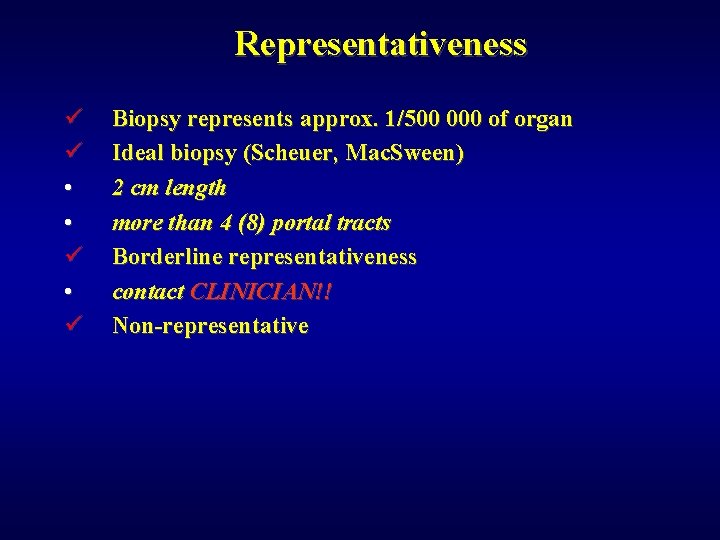
Representativeness ü ü • • ü Biopsy represents approx. 1/500 000 of organ Ideal biopsy (Scheuer, Mac. Sween) 2 cm length more than 4 (8) portal tracts Borderline representativeness contact CLINICIAN!! Non-representative
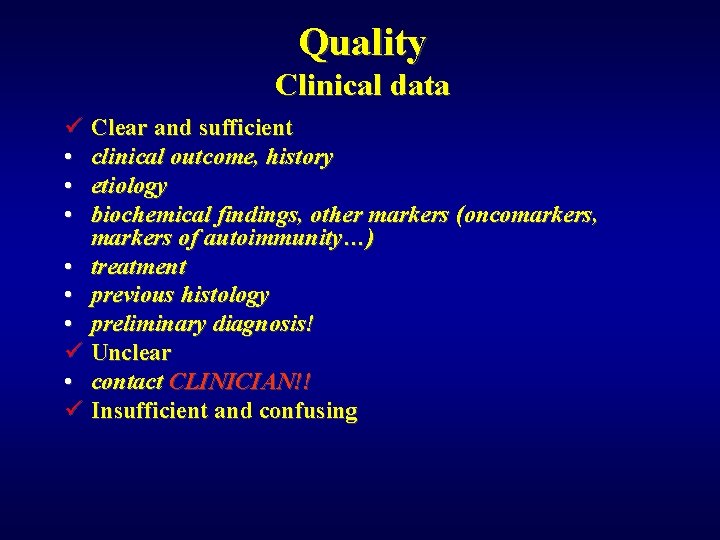
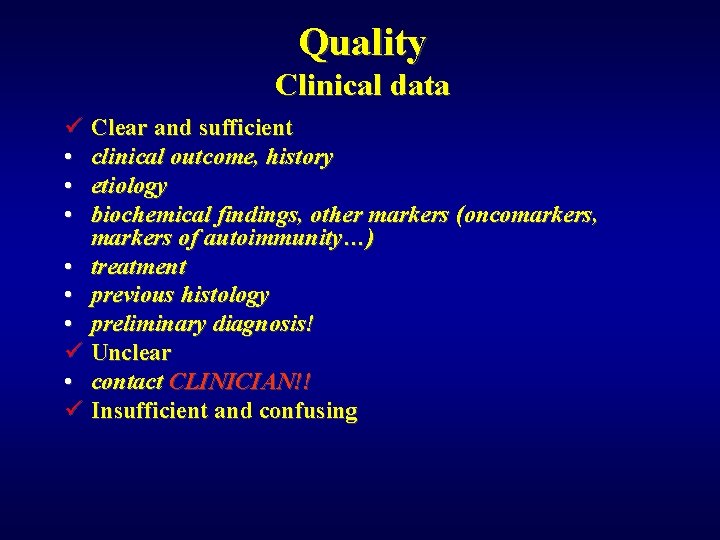
Quality Clinical data ü Clear and sufficient • clinical outcome, history • etiology • biochemical findings, other markers (oncomarkers, markers of autoimmunity…) • treatment • previous histology • preliminary diagnosis! ü Unclear • contact CLINICIAN!! ü Insufficient and confusing
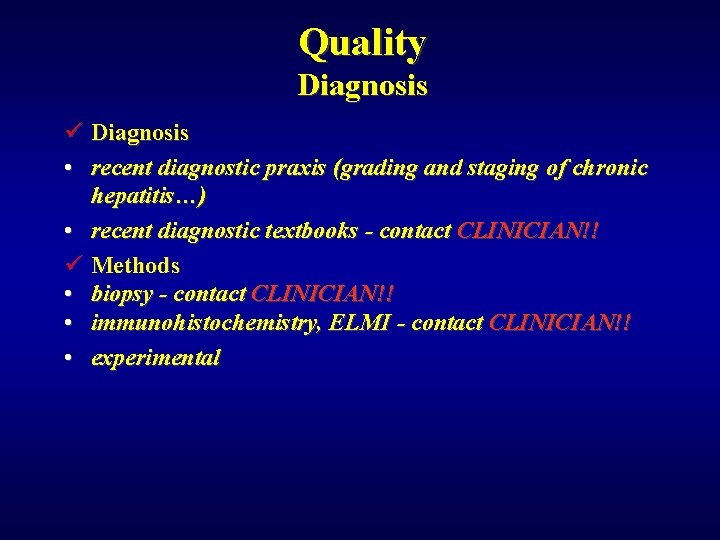
Quality Diagnosis ü Diagnosis • recent diagnostic praxis (grading and staging of chronic hepatitis…) • recent diagnostic textbooks - contact CLINICIAN!! ü Methods • biopsy - contact CLINICIAN!! • immunohistochemistry, ELMI - contact CLINICIAN!! • experimental
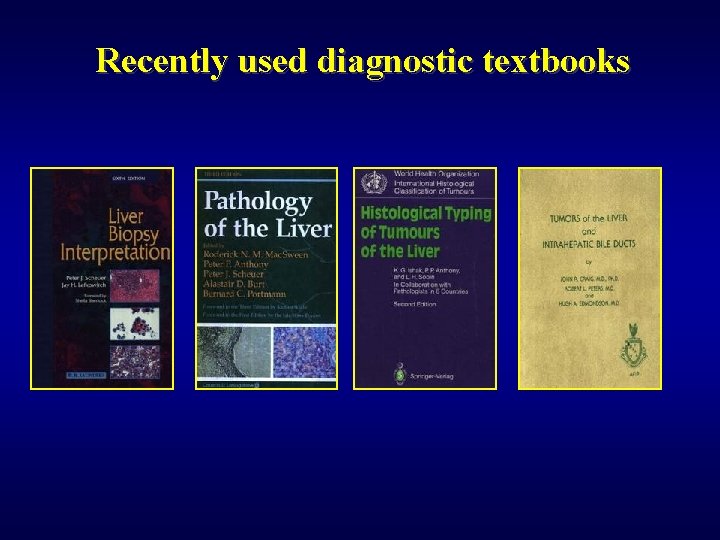
Recently used diagnostic textbooks
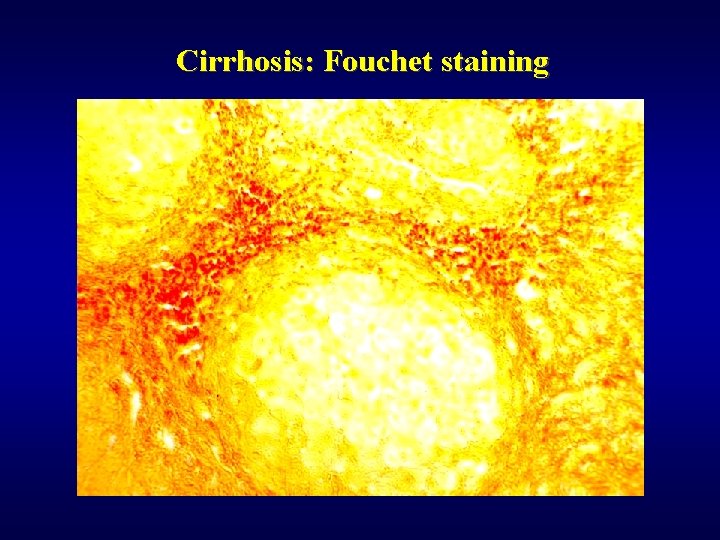
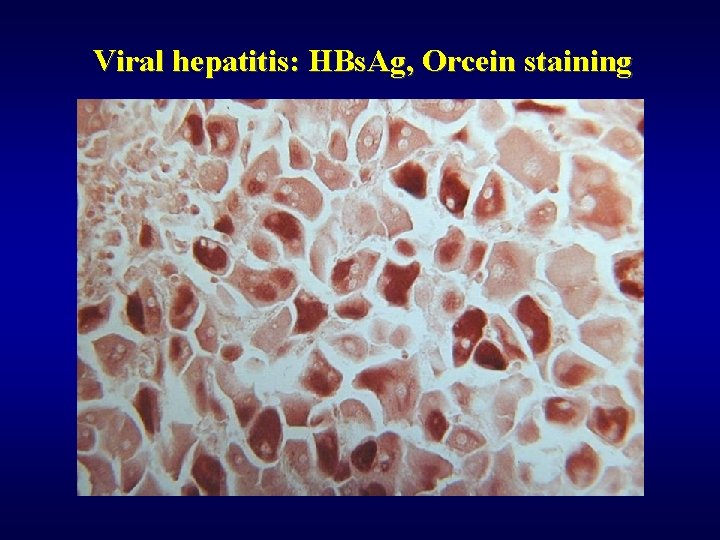
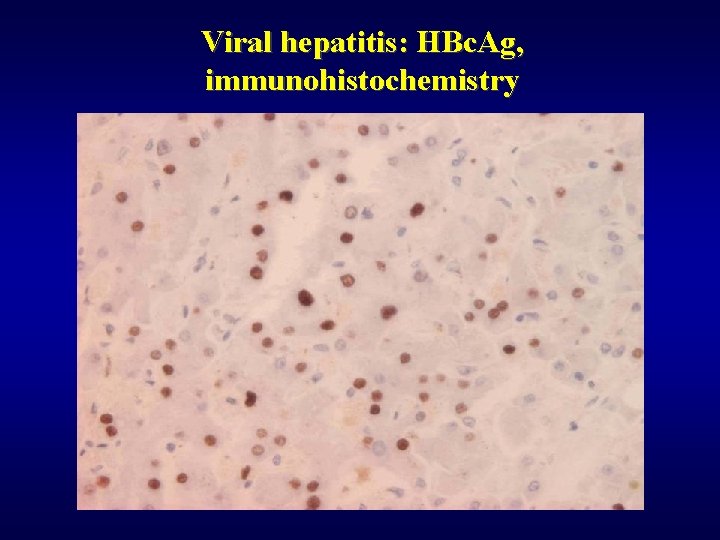
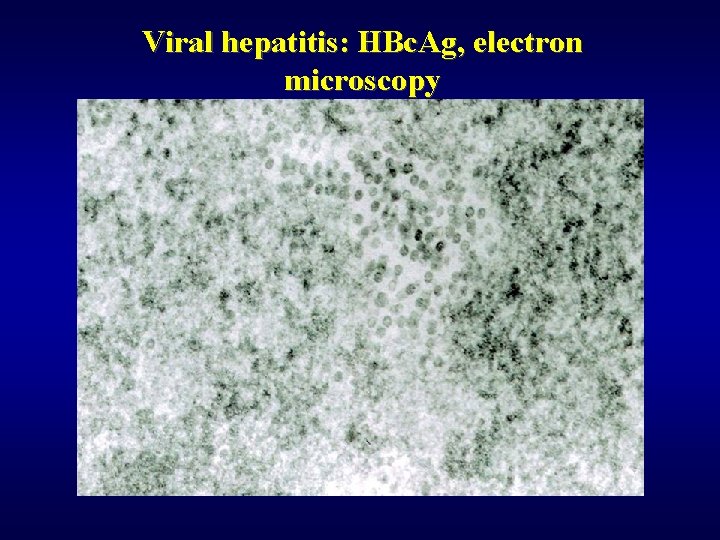
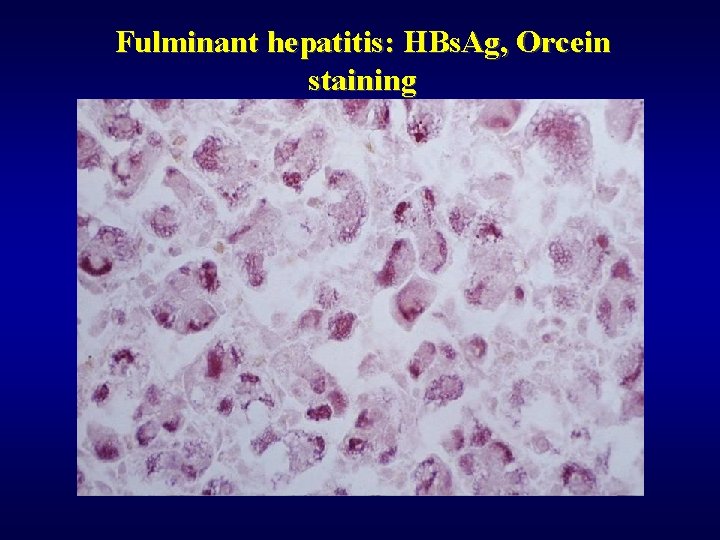
Histologic examination – special stains and methods ü Haematoxylin/eosin ü Fouchet – bile (green), collagen (red) ü Fe, Cu – Fe pigment, Cu pigment ü Gömori – reticulin mesh ü Orcein – HBs. Ag ü PAS, Müller – mucopolysaccharides ü Immunohistochemistry (HBs. Ag, HBc. Ag, a 1 fetoprotein, CEA, hepatocytes – OCH 1 E 5) ü ELMI (metabolic diseases) ü PCR (HBV DNA, HCV RNA, …)
Damage of hepatocytes ü Type (ischemic-coagulation necrosis, piecemal necrosis, apoptosis) ü Extent (monocellular, focal, submassive, bridging: C-C; C-P) ü Localization (centrolobular, periportal, midzonal) ü Course • regeneration, healing ad integrum • regeneration + fibrosis: cirrhosis • acute liver failure: coma and death
Liver failure ü Jaundice ü Hypoalbuminemia ü Coagulopathy ü Hyperamonemia ü Increase of levels of cytosolic enzymes ü Endocrine complications ü Hepatoencephalopathy ü Hepatorenal syndrome ü Coma
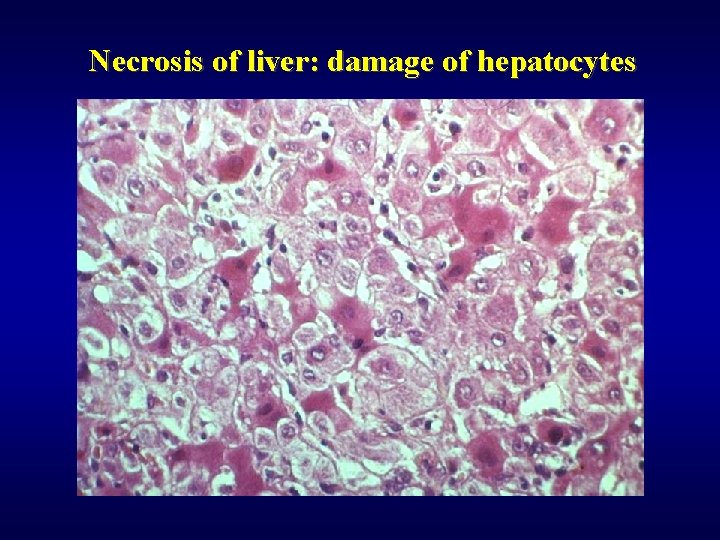
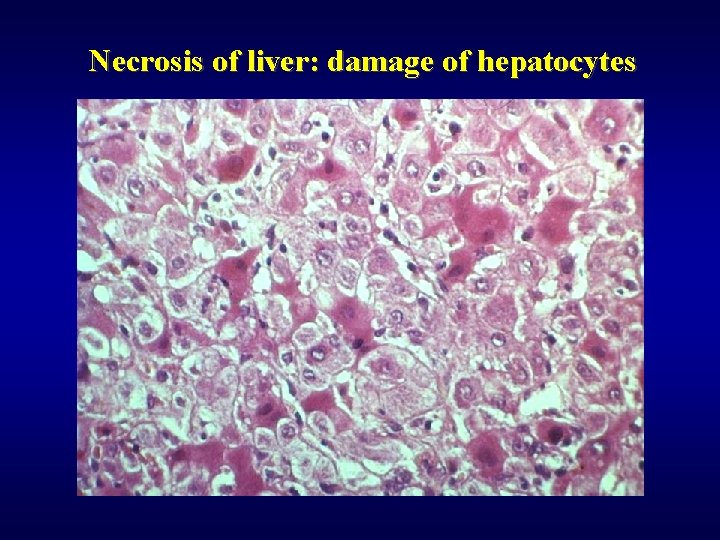
Necrosis of liver: damage of hepatocytes
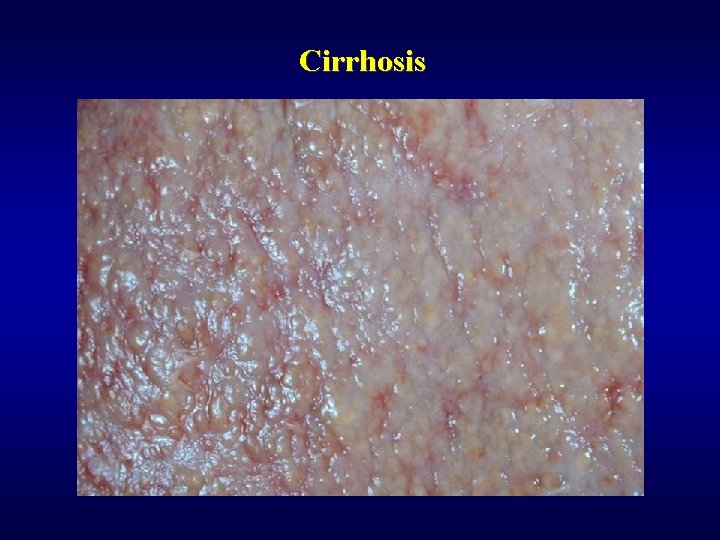
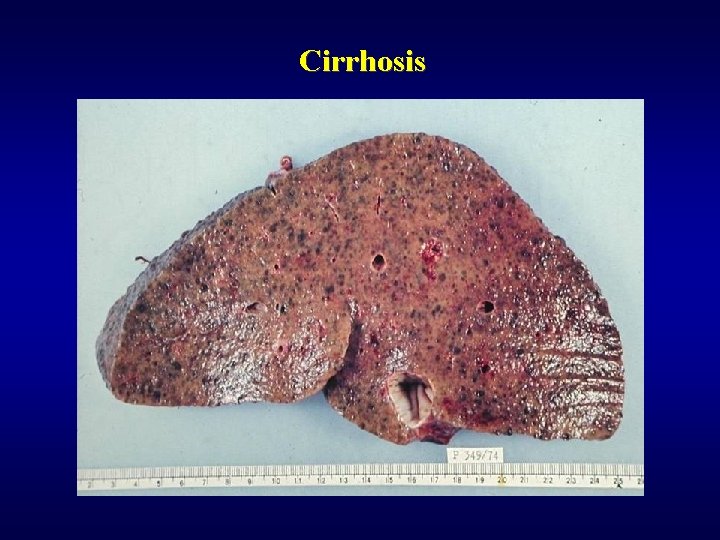
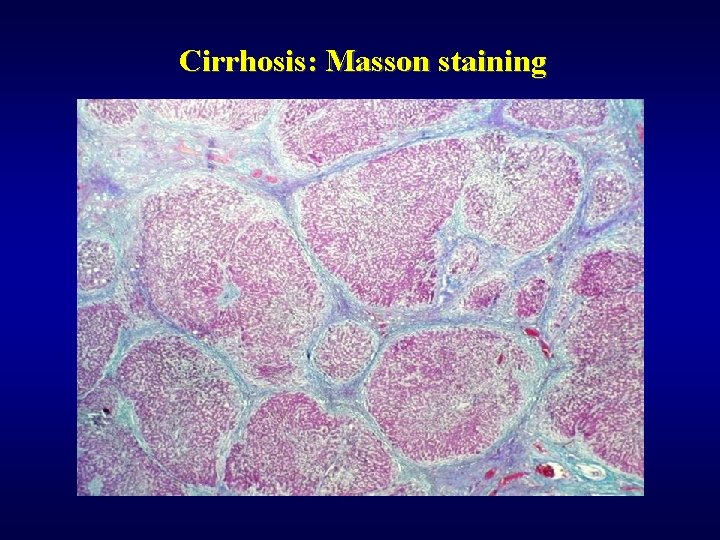
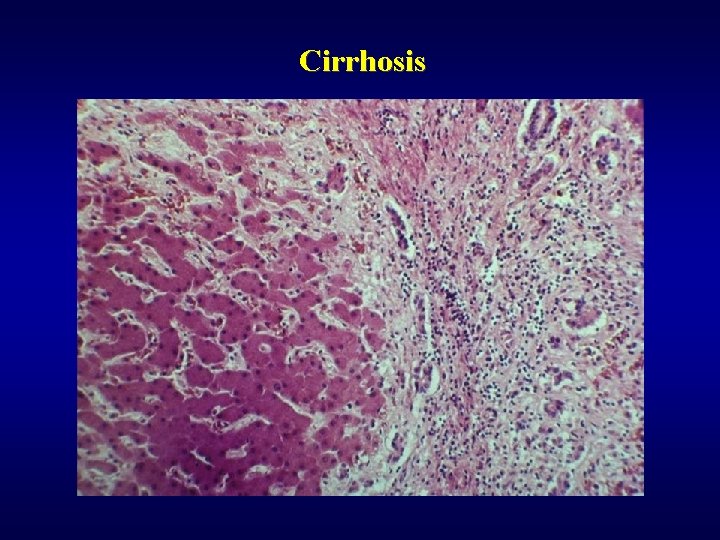
Cirrhosis ü Nodular rearrangement ü Morphology • micronodular • macronodular
Cirrhosis: etiology ü Alcohol (60 -70%) ü Chronic hepatitis (10%) ü Cryptogenic (10 -15%) ü Biliary (primary, secondary) ü Haemochromatosis (primary, secondary) ü Metabolic diseases (tyrosinemia, galactosemia) -very rare
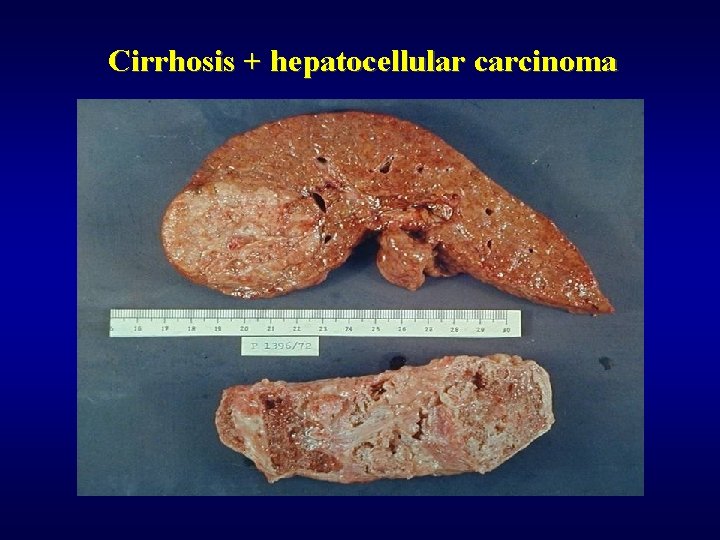
Cirrhosis: complications ü Portal hypertension ü Liver failure ü Hepatocellular carcinoma

Portal hypertension ü Prehepatic (tumor, infection, pancreatitis, pregnancy, peroral contraceptives) ü Intrahepatic – most frequent (cirrhosis, fibrosis) ü Posthepatic (congestive cardiac failure, Budd-Chiari syndrome, venoocclusive disease) ü Signs: • portosystemic shunts • splenomegaly • ascites
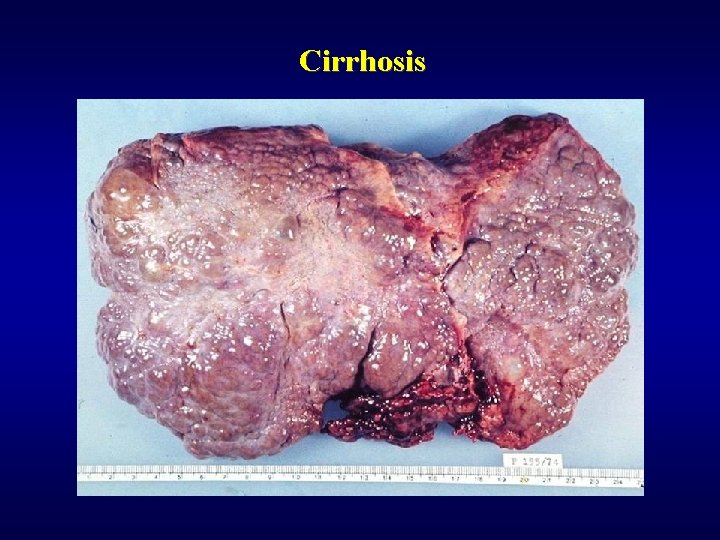
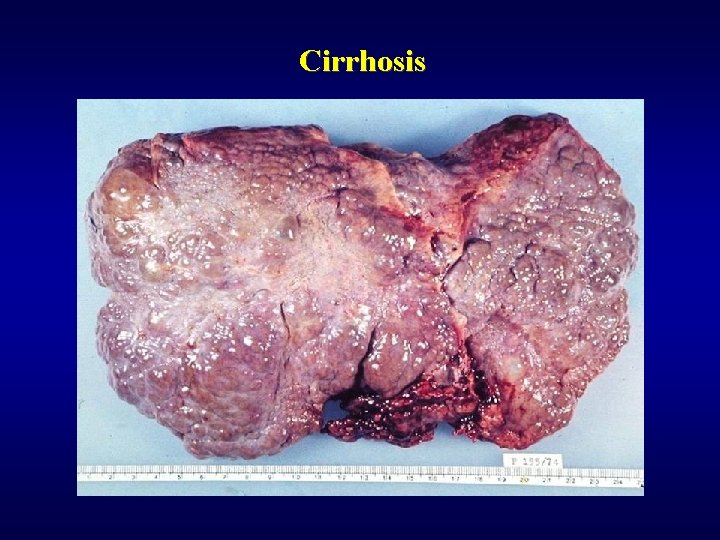
Cirrhosis
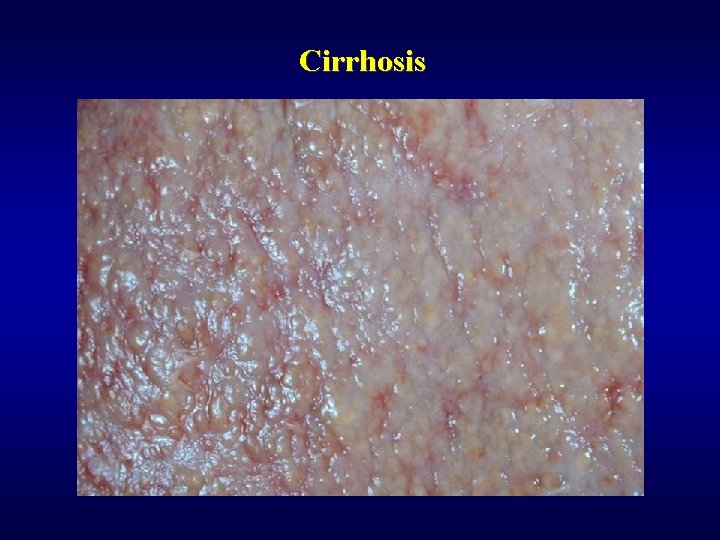
Cirrhosis
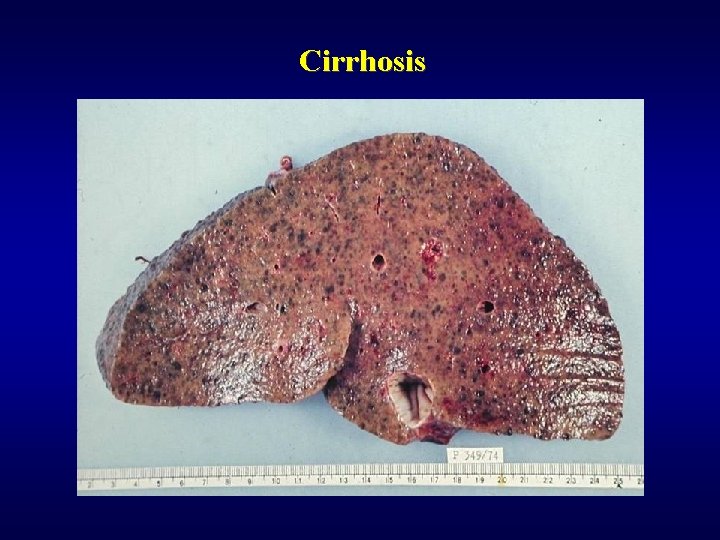
Cirrhosis
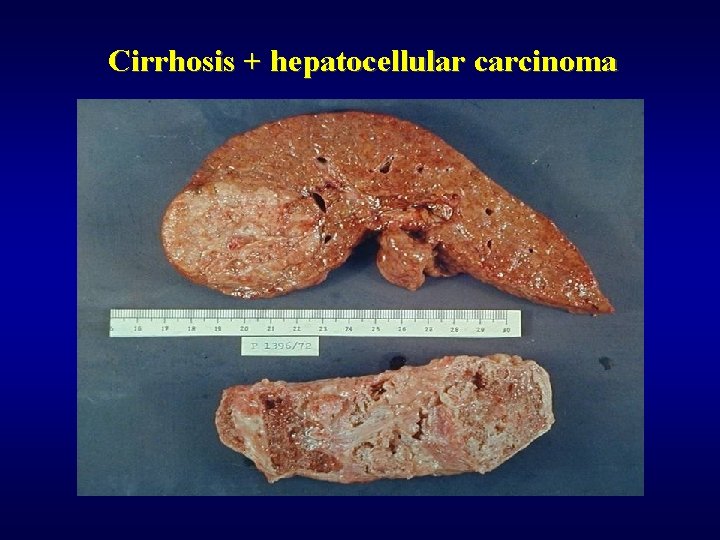
Cirrhosis + hepatocellular carcinoma
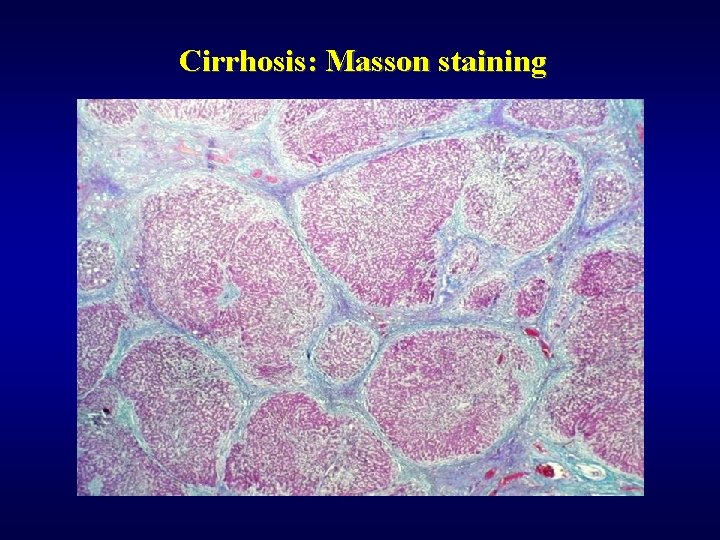
Cirrhosis: Masson staining
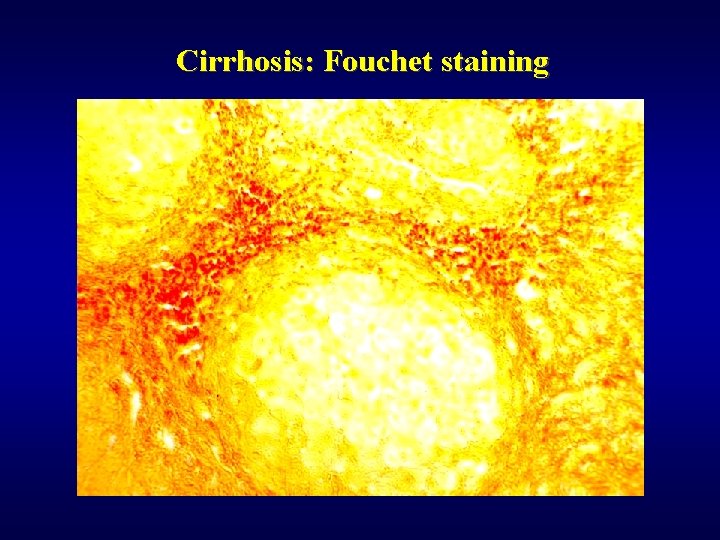
Cirrhosis: Fouchet staining
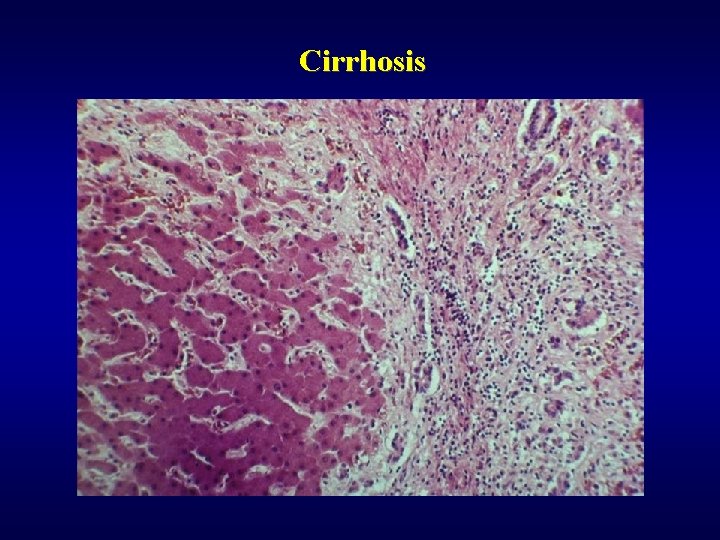
Cirrhosis

Cirrhosis: active
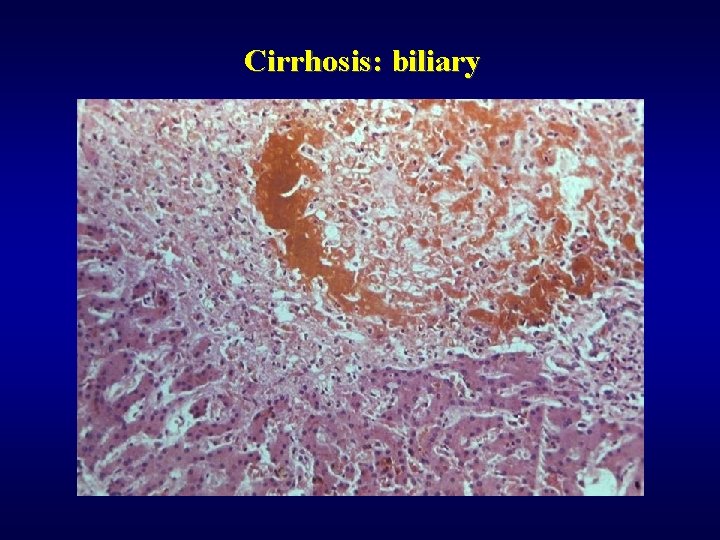
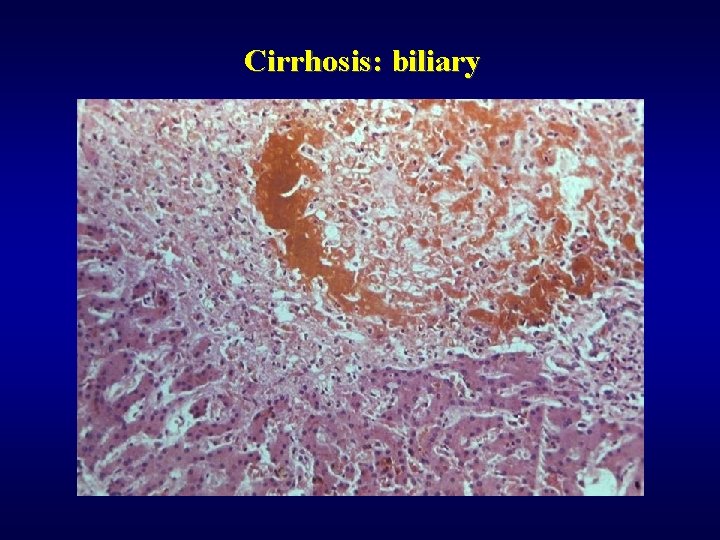
Cirrhosis: biliary
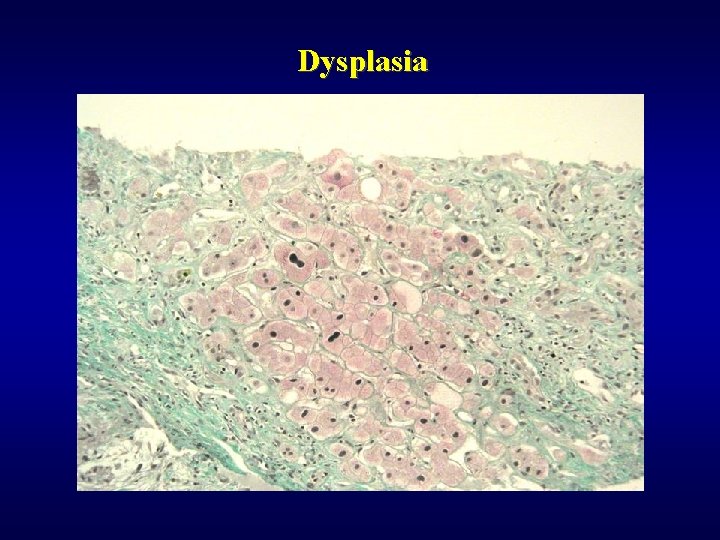
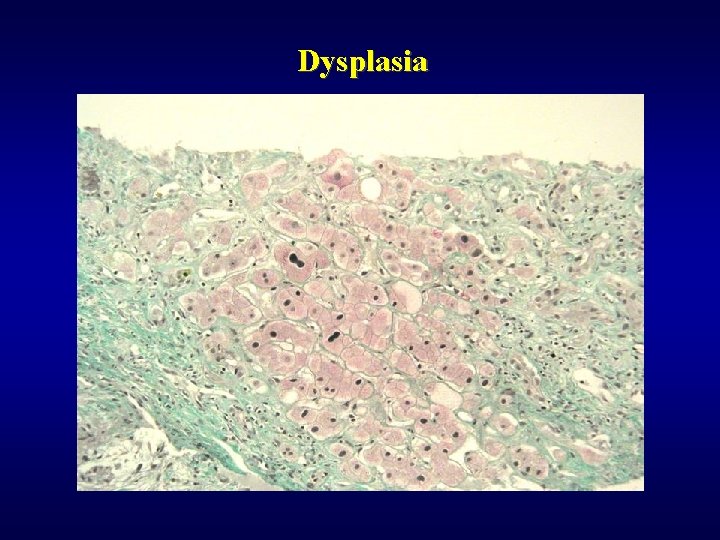
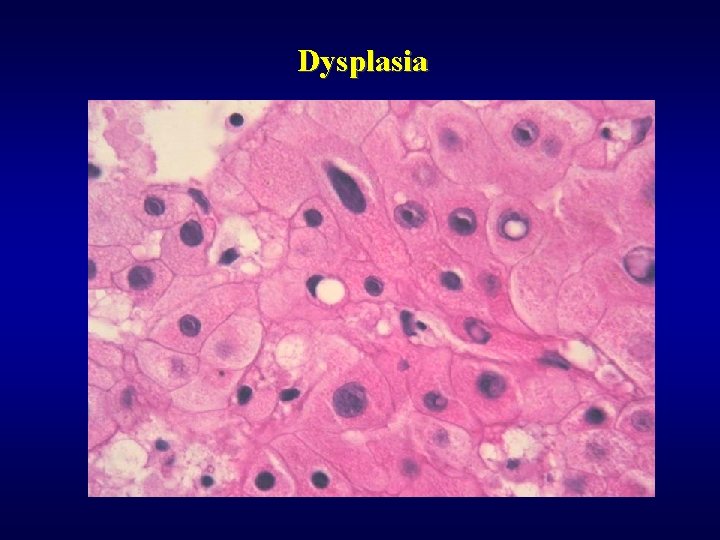
Dysplasia
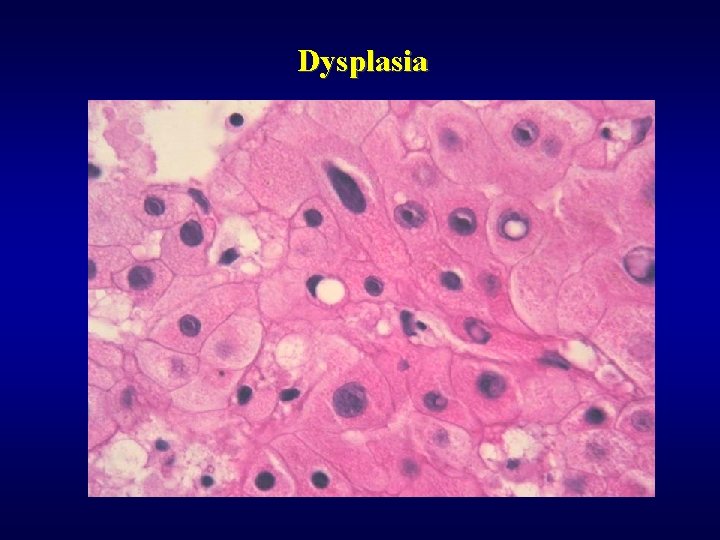
Dysplasia
Hepatitis: etiology ü Infectious (acute, chronic) • viruses (most often) • bacteria (TBC, malaria, salmonelosis, leptospirosis, …) • parazites (ecchinococcus) • protozoal (amebiasis) ü Non-infectious (acute, chronic) • autoimmune • metabolic • drug induced • cryptogenic
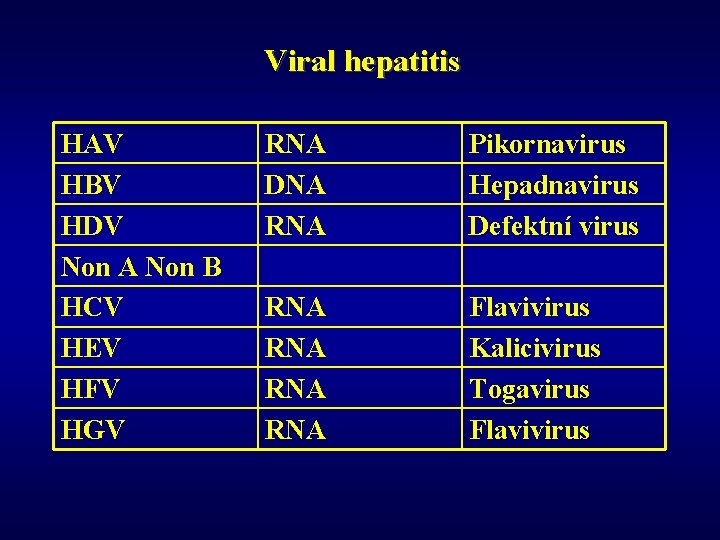
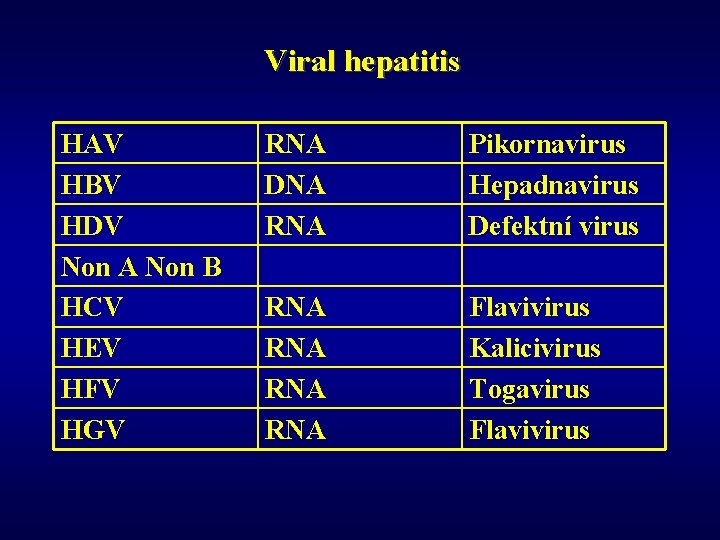
Viral hepatitis HAV HBV HDV Non A Non B HCV HEV HFV HGV RNA DNA RNA Pikornavirus Hepadnavirus Defektní virus RNA RNA Flavivirus Kalicivirus Togavirus Flavivirus
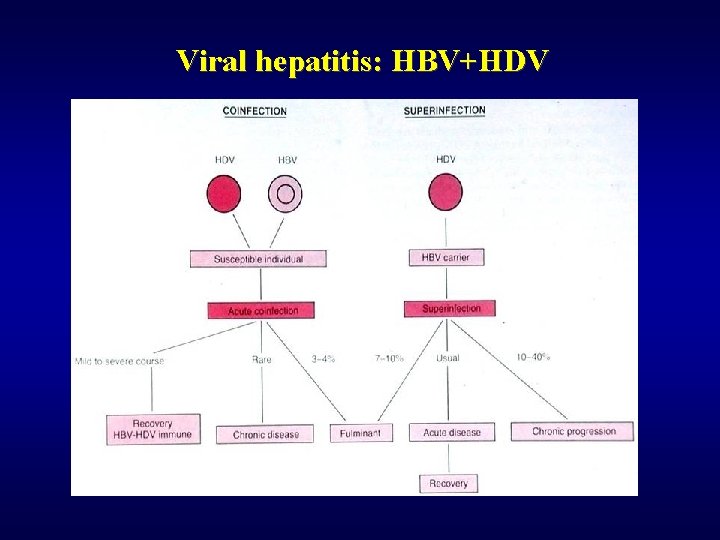
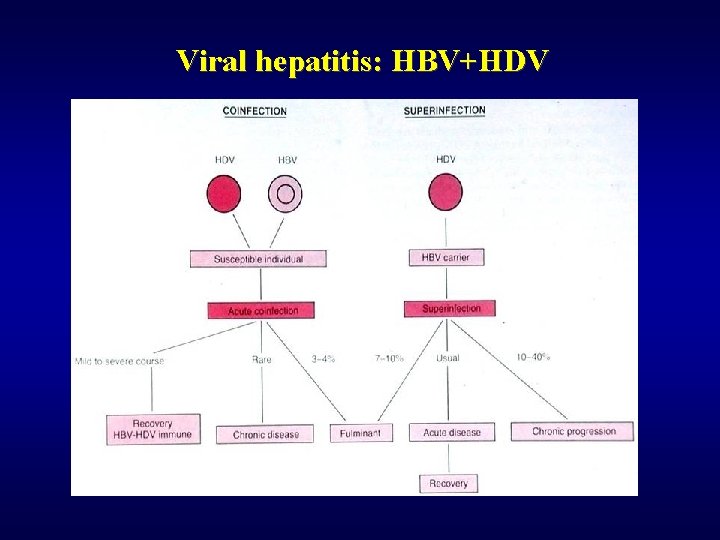
Viral hepatitis: HBV+HDV

Viral hepatitis: HBs. Ag, ground glass
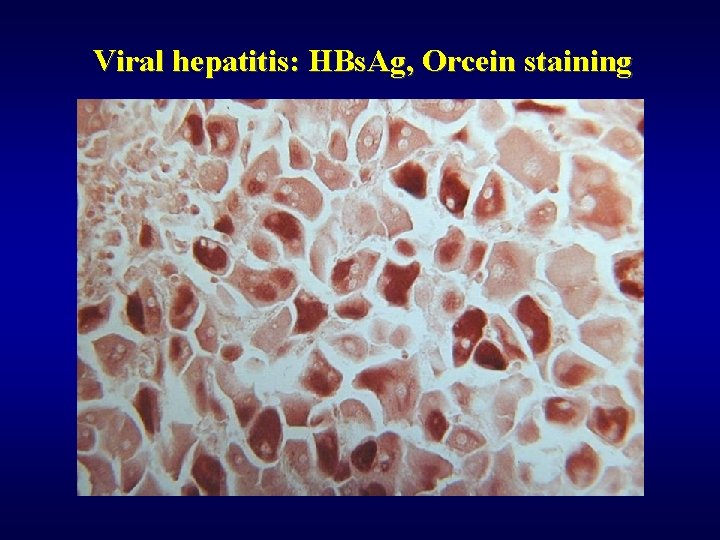
Viral hepatitis: HBs. Ag, Orcein staining
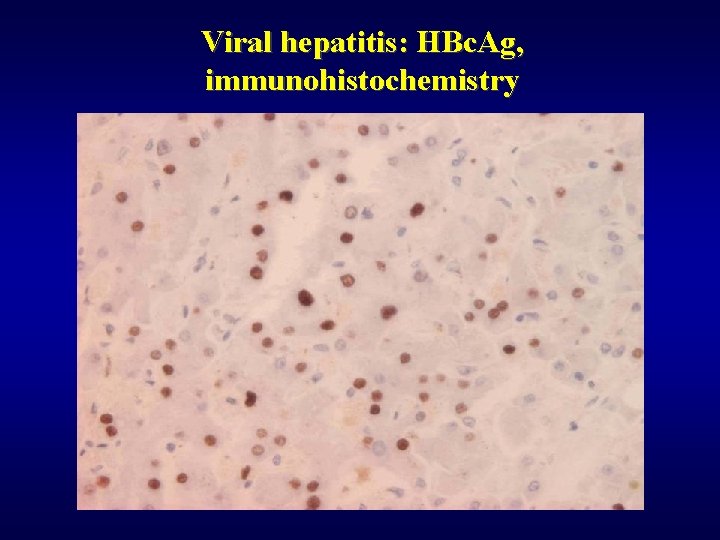
Viral hepatitis: HBc. Ag, immunohistochemistry
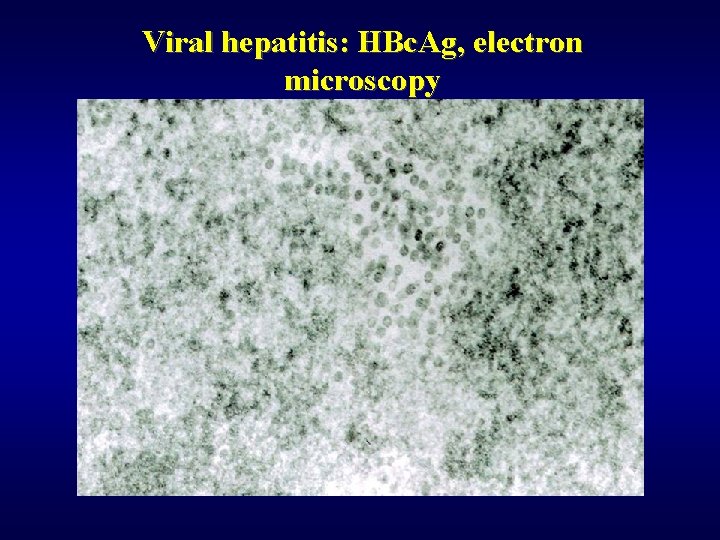
Viral hepatitis: HBc. Ag, electron microscopy
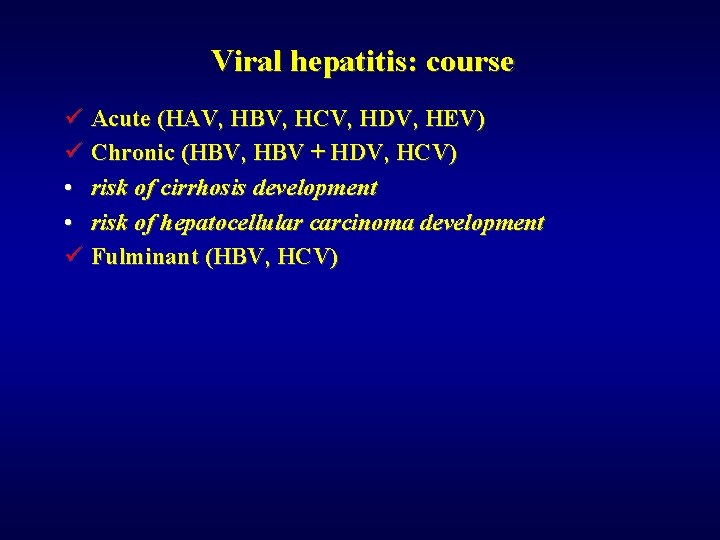
Viral hepatitis: course ü Acute (HAV, HBV, HCV, HDV, HEV) ü Chronic (HBV, HBV + HDV, HCV) • risk of cirrhosis development • risk of hepatocellular carcinoma development ü Fulminant (HBV, HCV)
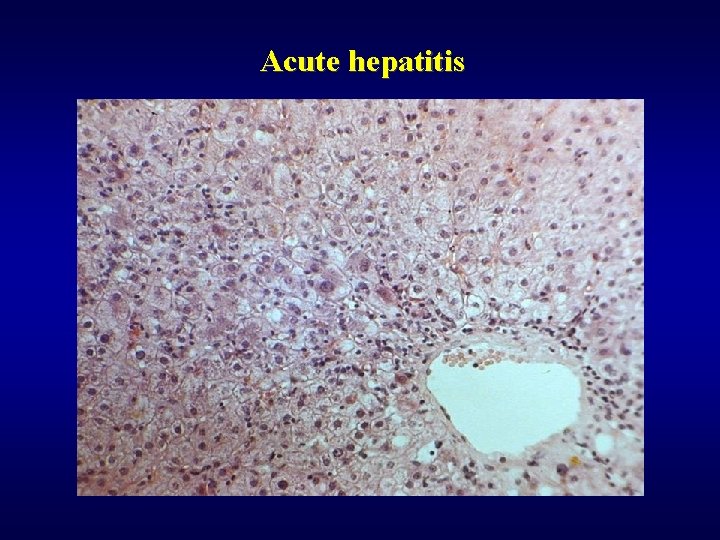
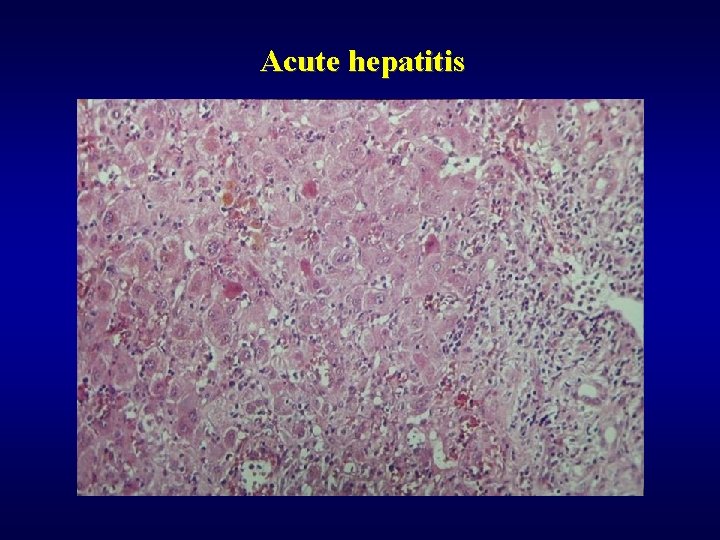
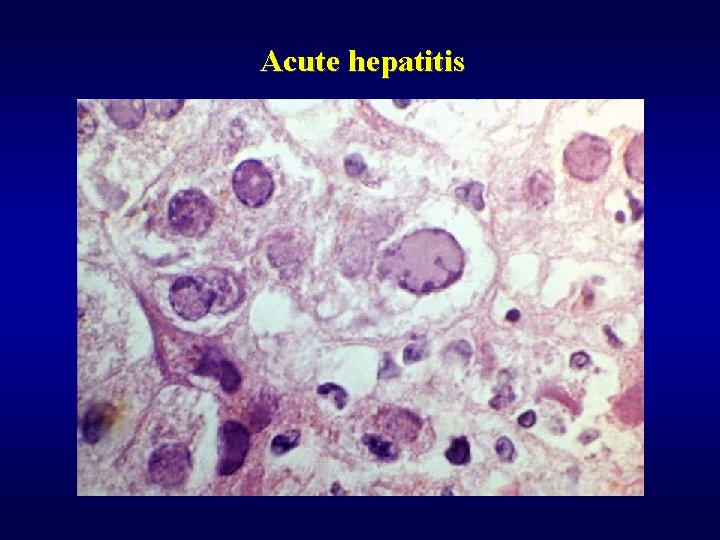
Acute hepatitis ü Gross finding – oedematous, red liver ü Microscopic finding • focal necrosis • bridging necrosis • panacinar/multiacinar necrosis • periportal necrosis ü Hepatocytes • polymorphism • balooning degeneration
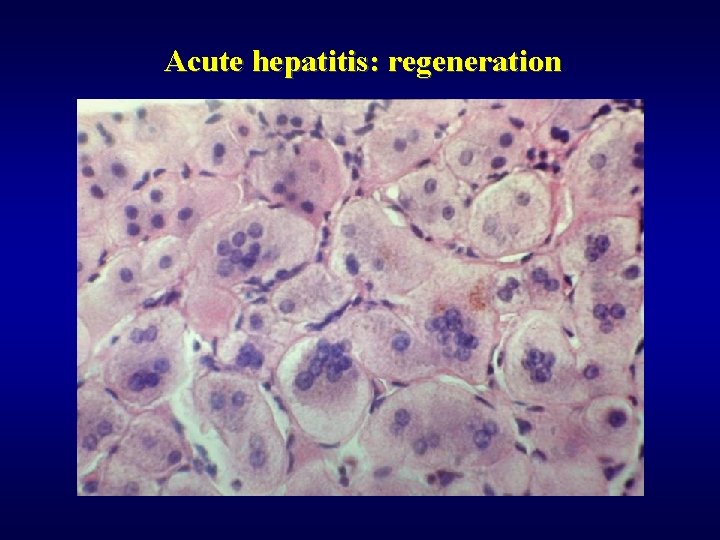
Acute hepatitis ü Inflammation • polynuclear/mononuclear infiltration • activation of Kupfer’s cells ü Other changes • cholestasis • damage of bile ducts ü Regeneration
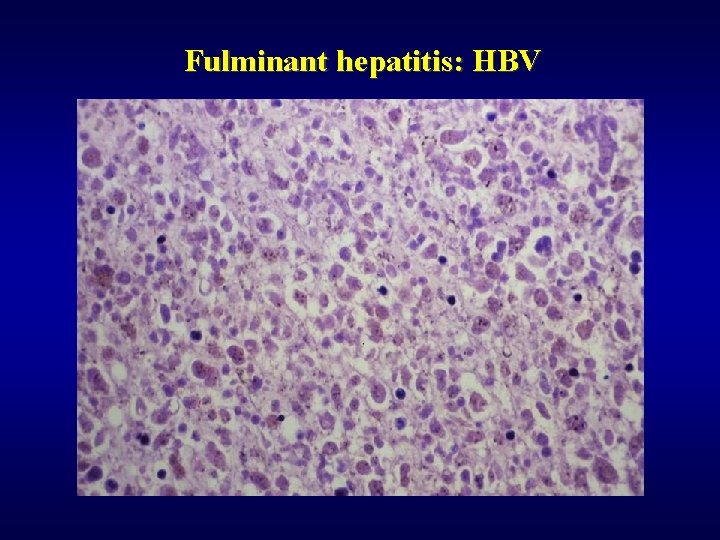
Fulminant hepatitis ü Gross finding - soft consistency ü Microscopic finding – complete necrosis of parenchyma ü Course • liver failure - coma - death • regeneration – postnecrotic cirrhosis
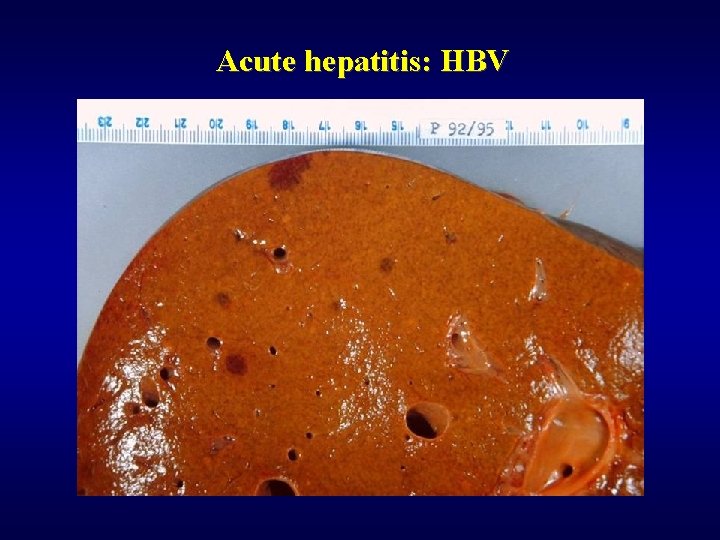
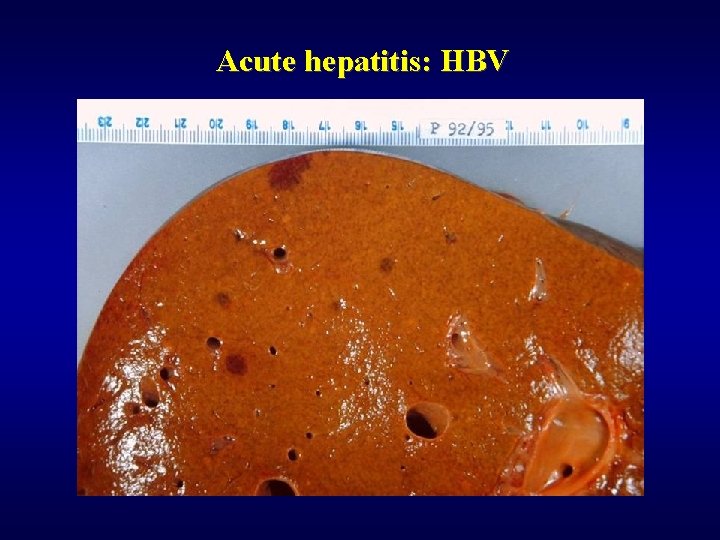
Acute hepatitis: HBV
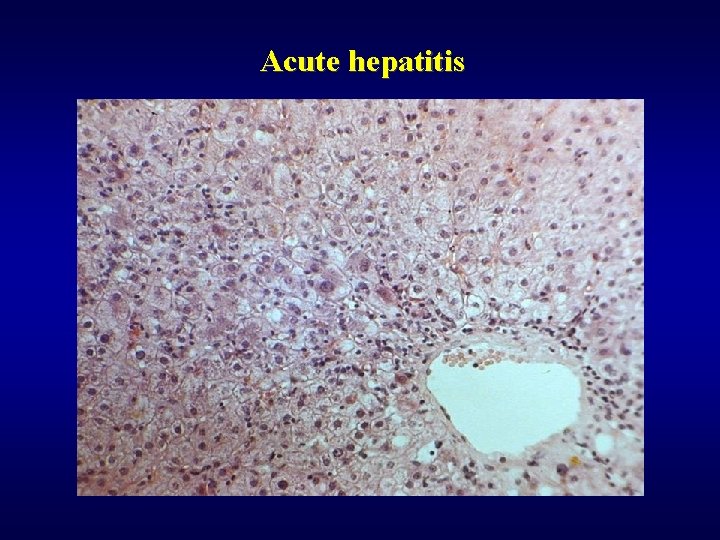
Acute hepatitis
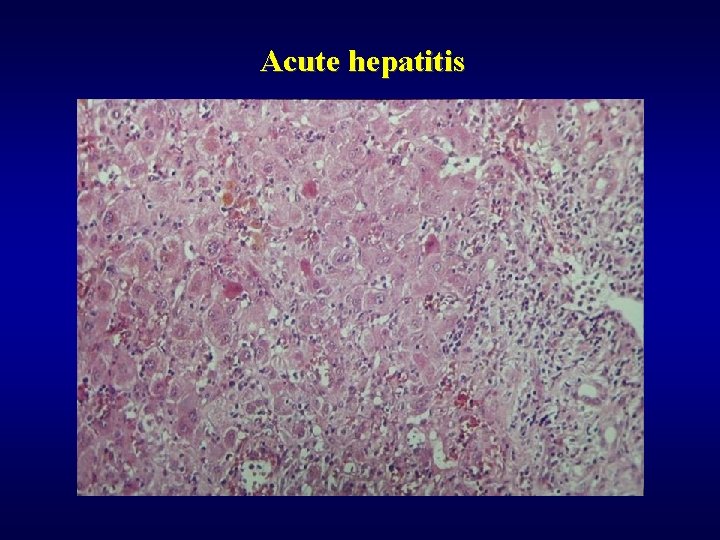
Acute hepatitis
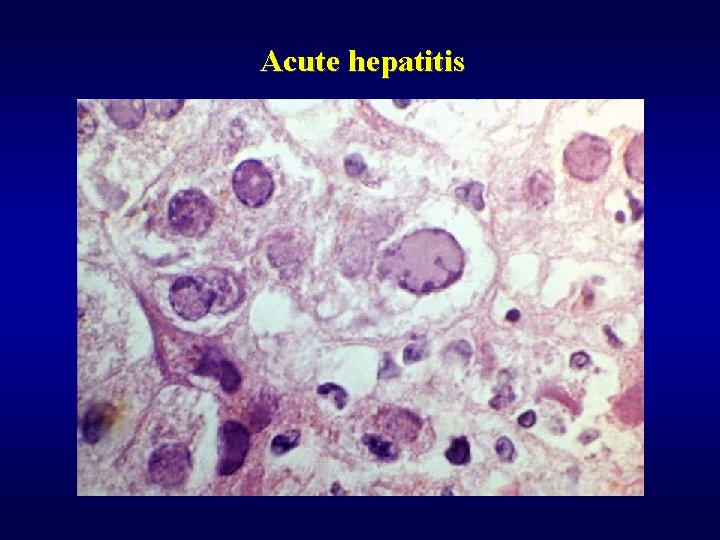
Acute hepatitis
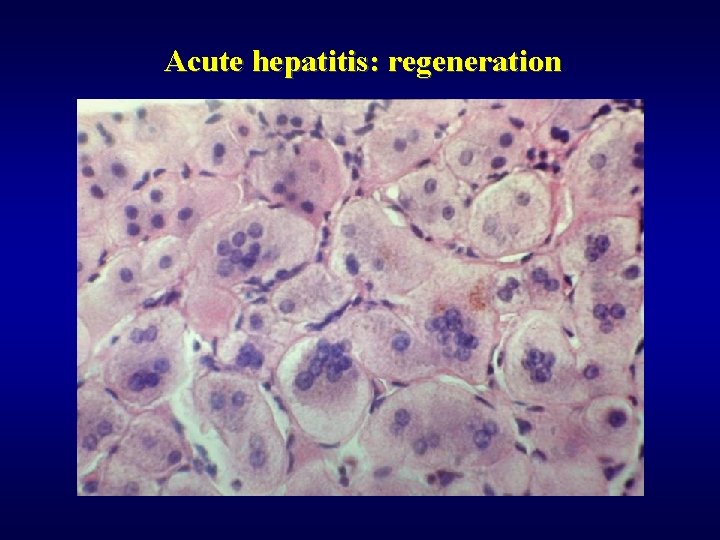
Acute hepatitis: regeneration
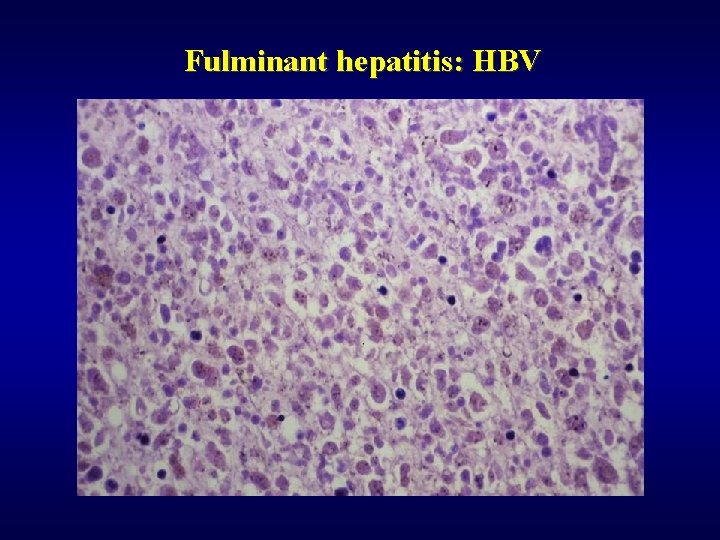
Fulminant hepatitis: HBV
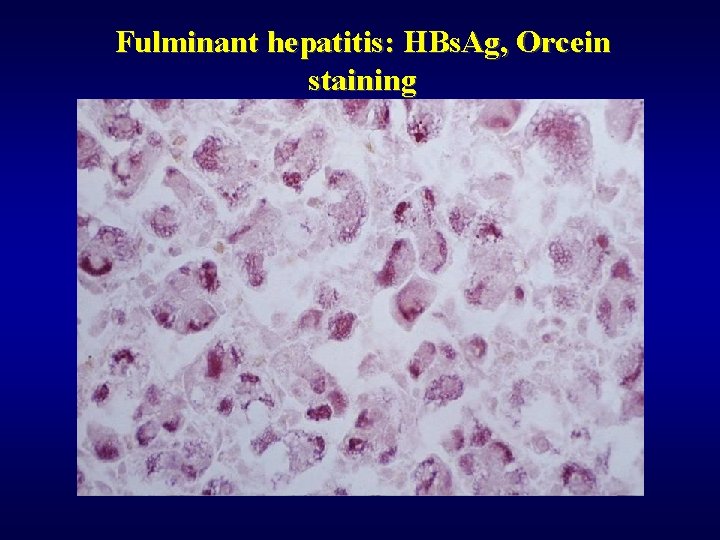
Fulminant hepatitis: HBs. Ag, Orcein staining
Chronic hepatitis: etiology ü HBV, HBV+HDV, HCV ü Autoimmune ü Drug induced ü Wilson’s disease ü a 1 anti-trypsin deficiency ü Cryptogenic
Chronic hepatitis: clinical definition Clinical symptoms of hepatitis more than: ü 6 months ü 12 months in HCV
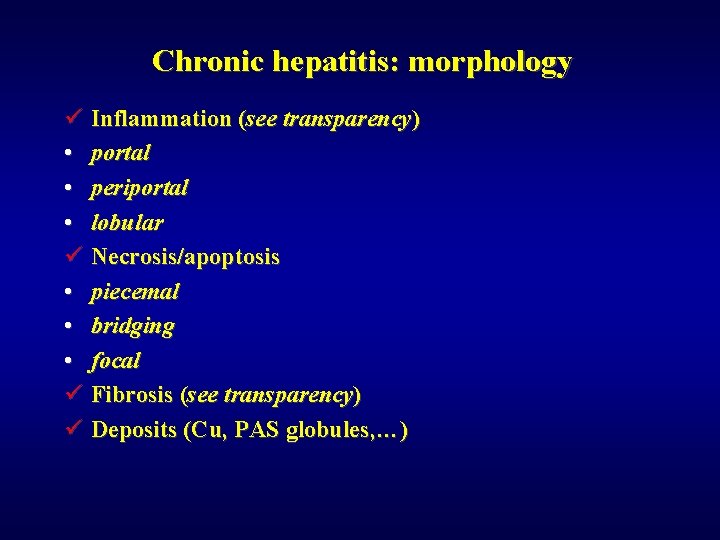
Chronic hepatitis: morphology ü Inflammation (see transparency) • portal • periportal • lobular ü Necrosis/apoptosis • piecemal • bridging • focal ü Fibrosis (see transparency) ü Deposits (Cu, PAS globules, …)
Chronic hepatitis: classification (see transparency)
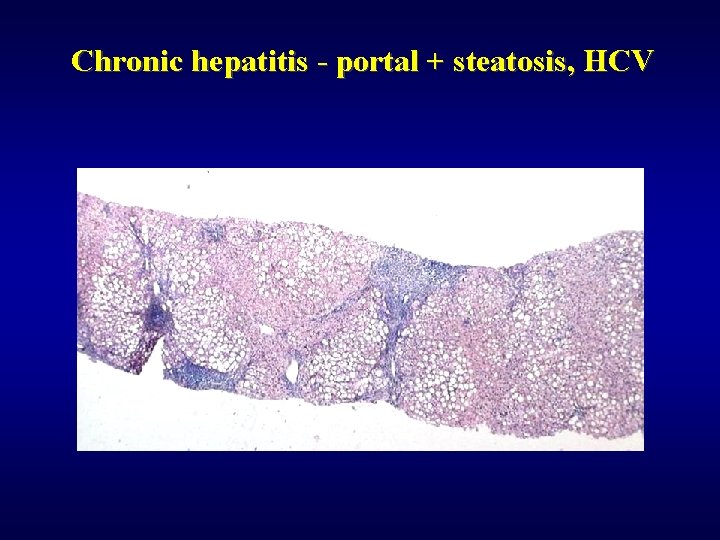
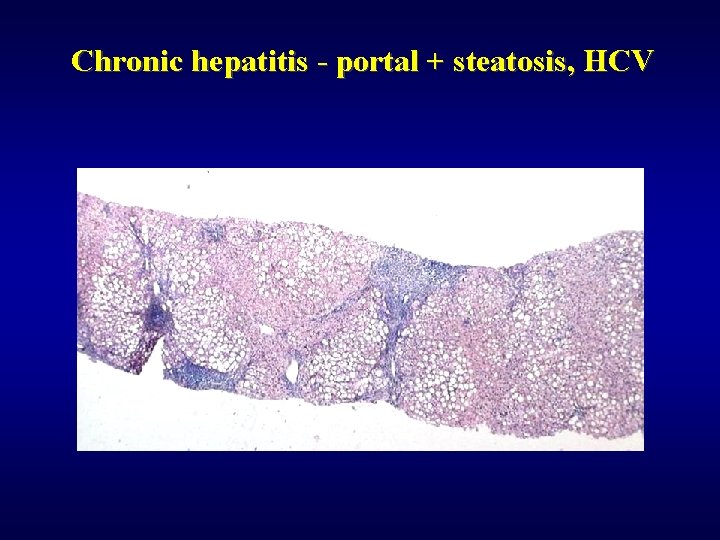
Chronic hepatitis - portal + steatosis, HCV
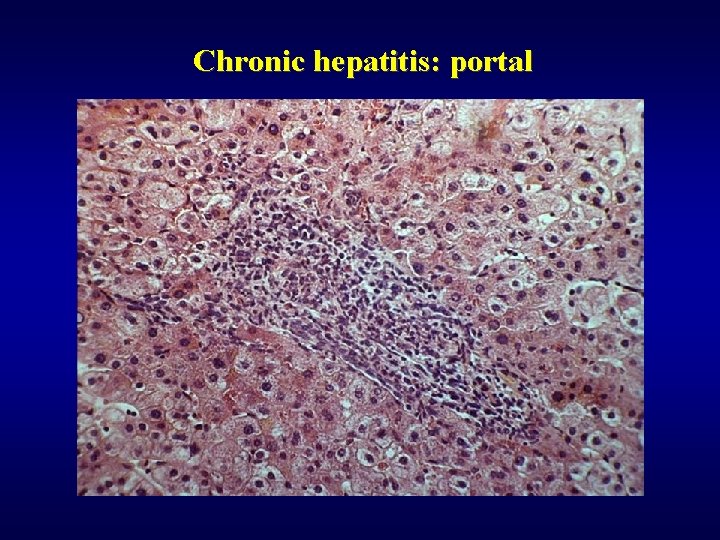
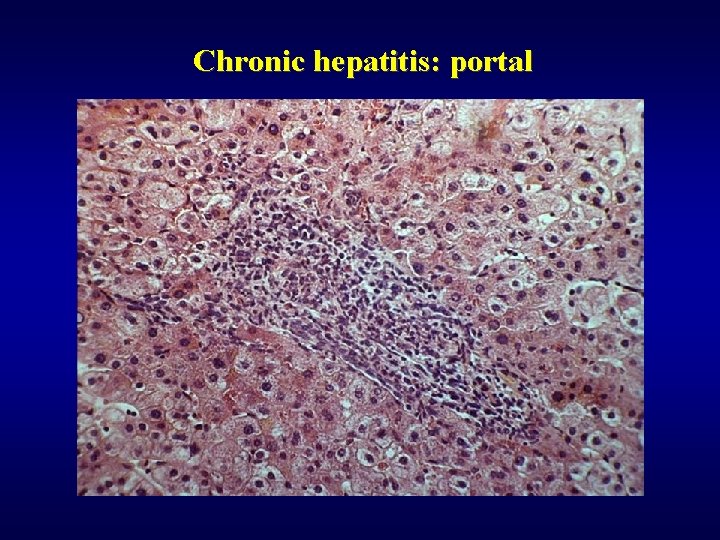
Chronic hepatitis: portal
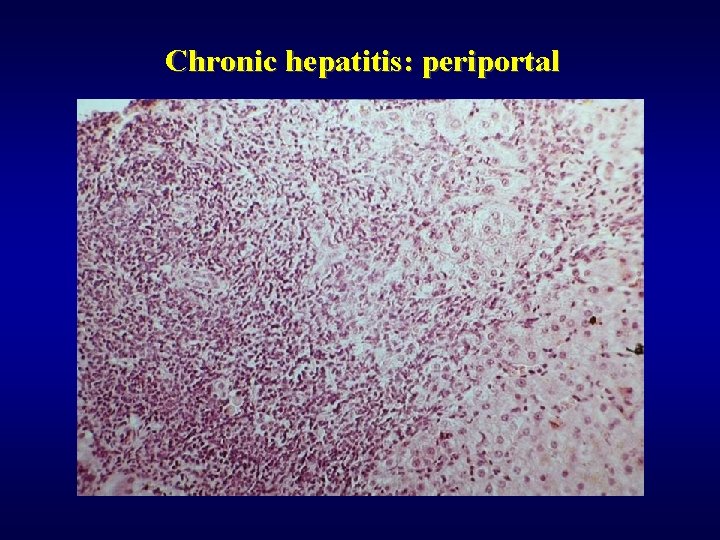
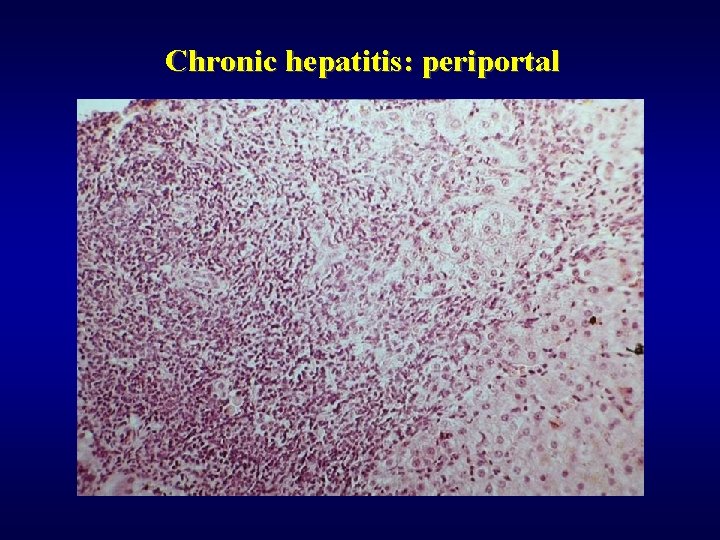
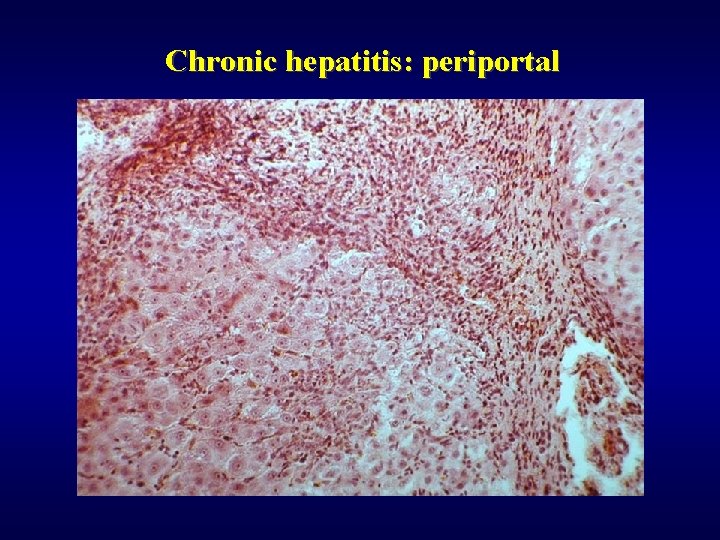
Chronic hepatitis: periportal
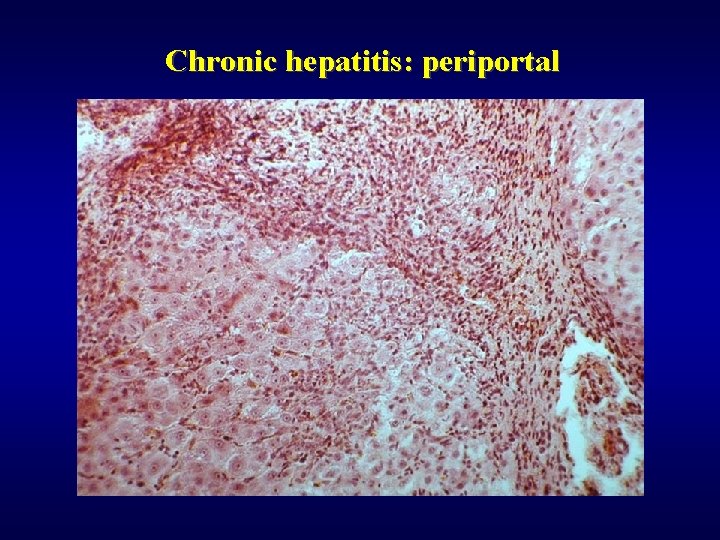
Chronic hepatitis: periportal
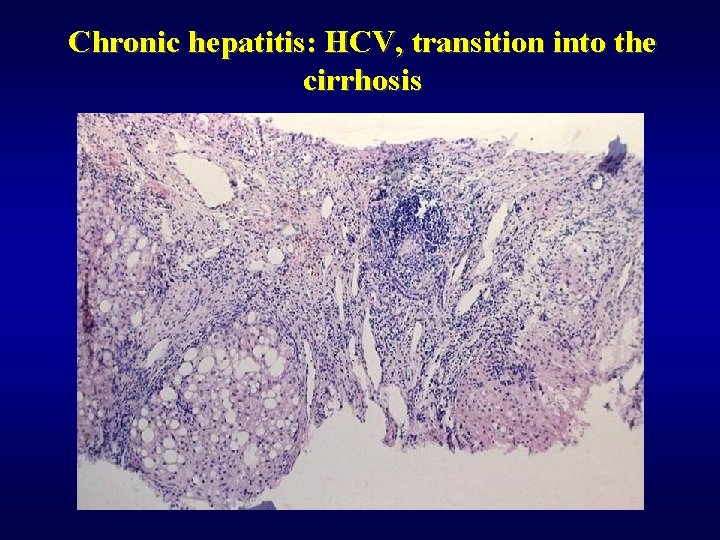
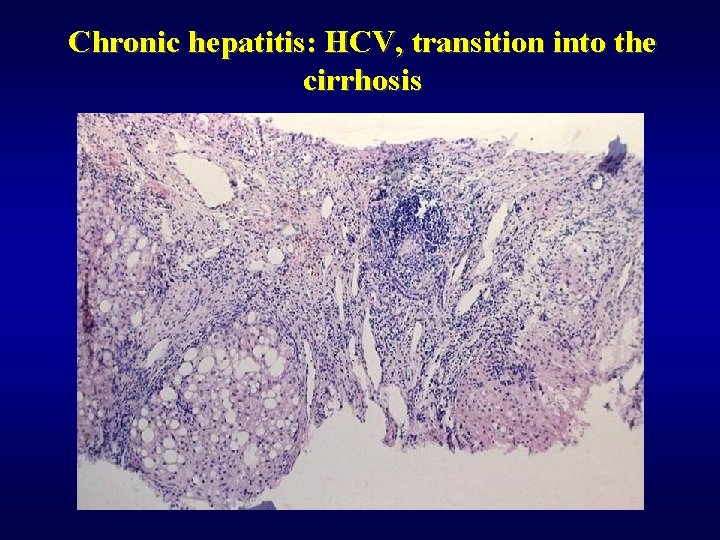
Chronic hepatitis: HCV, transition into the cirrhosis
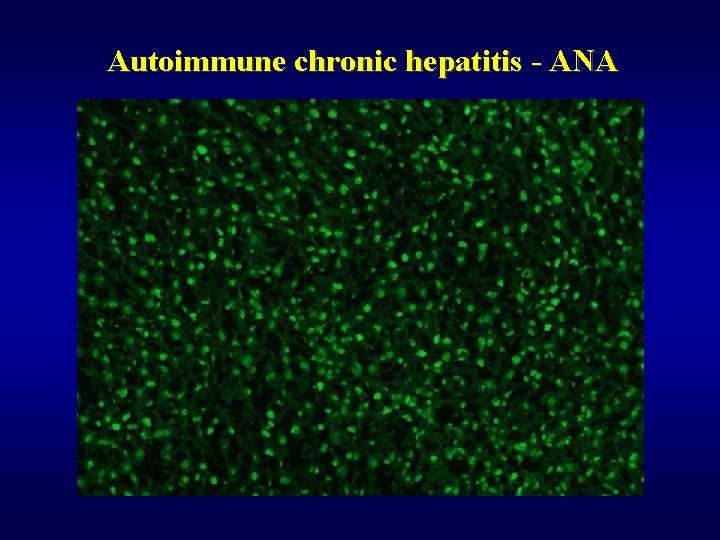
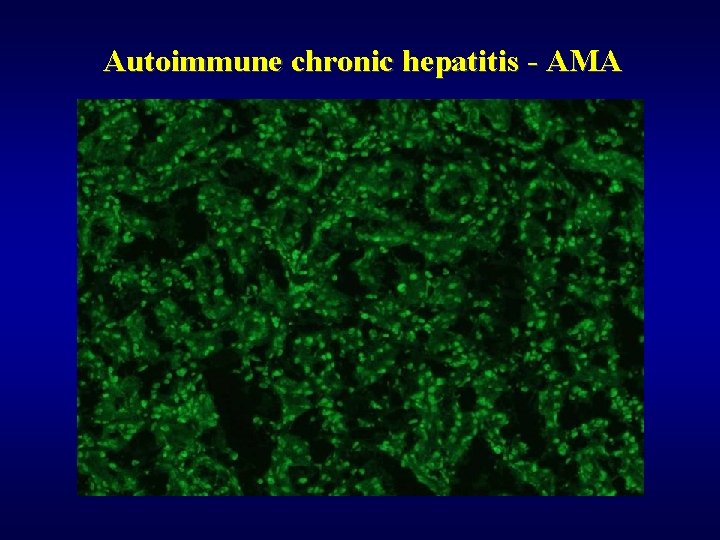
Autoimmune chronic hepatitis ü Females, young/middle age ü Autoantibodies – ANA, AMA ü Autoimmune „overlap“ syndromes • lupus erythematodes • arthritis
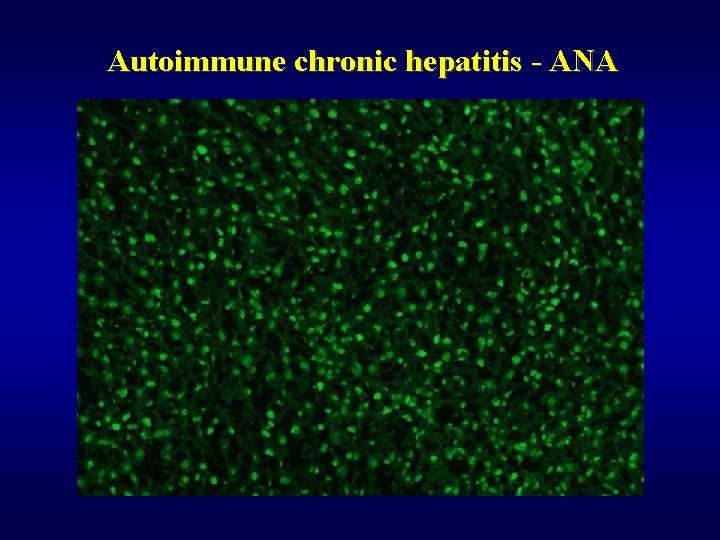
Autoimmune chronic hepatitis - ANA
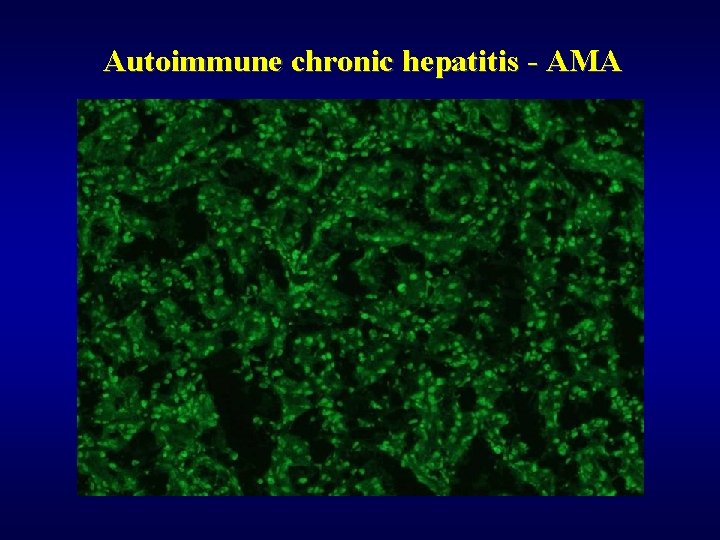
Autoimmune chronic hepatitis - AMA
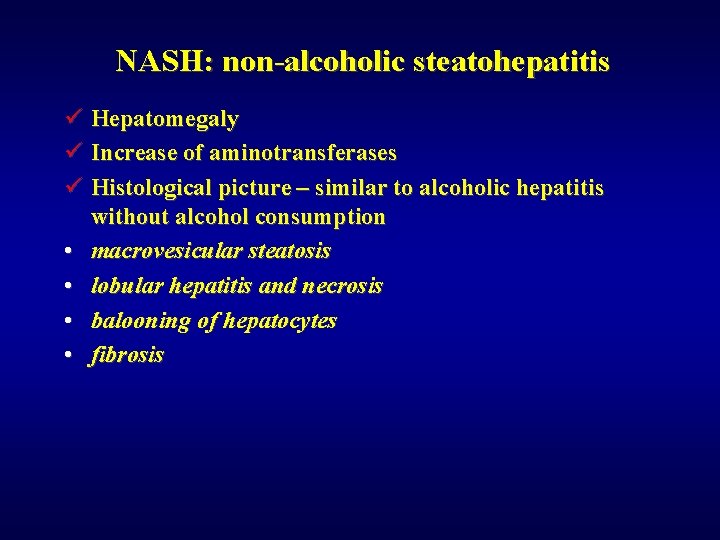
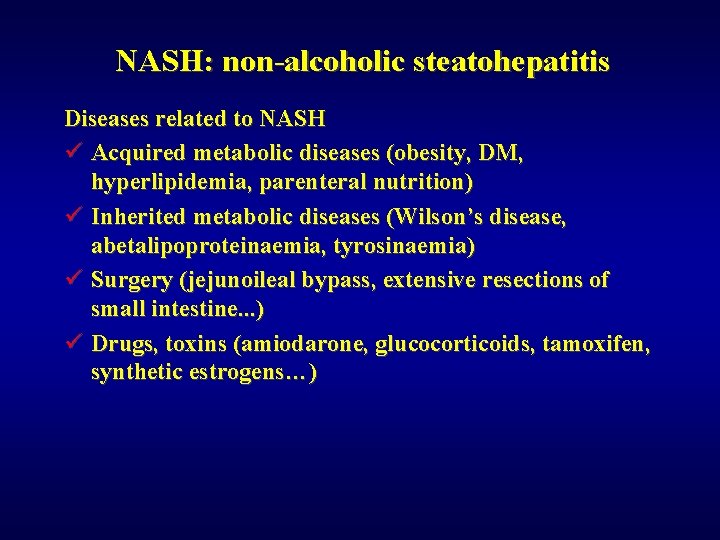
NASH: non-alcoholic steatohepatitis ü Hepatomegaly ü Increase of aminotransferases ü Histological picture – similar to alcoholic hepatitis without alcohol consumption • macrovesicular steatosis • lobular hepatitis and necrosis • balooning of hepatocytes • fibrosis
NASH: non-alcoholic steatohepatitis Epidemiologic signs of NASH ü Females ü Obesity ü DM of II type, hyperglycaemia
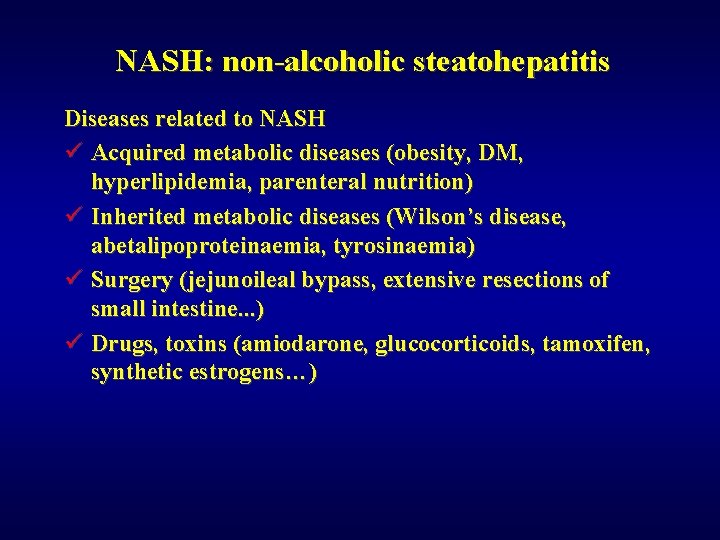
NASH: non-alcoholic steatohepatitis Diseases related to NASH ü Acquired metabolic diseases (obesity, DM, hyperlipidemia, parenteral nutrition) ü Inherited metabolic diseases (Wilson’s disease, abetalipoproteinaemia, tyrosinaemia) ü Surgery (jejunoileal bypass, extensive resections of small intestine. . . ) ü Drugs, toxins (amiodarone, glucocorticoids, tamoxifen, synthetic estrogens…)
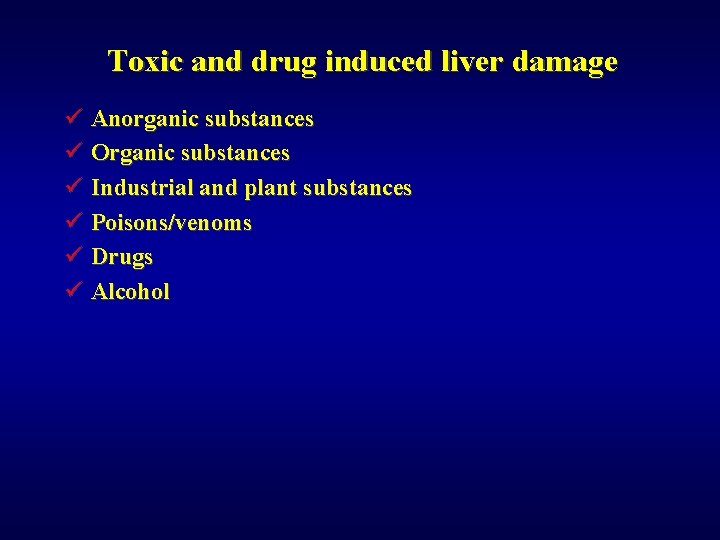
Toxic and drug induced liver damage ü Anorganic substances ü Organic substances ü Industrial and plant substances ü Poisons/venoms ü Drugs ü Alcohol
Toxic and drug induced liver damage: effect ü Expectable ü Non-expectable (idiosyncratic)

Toxic and drug induced liver damage : forms ü Necrosis ü Steatosis • macrovesicular (alcohol, corticoids) • microvesicular (tetracyklin, aspirine) ü Cholestasis (steroids-anabolic, contraceptives) ü Hepatitis mild (aspirin, synthetic penicilines) ü Hepatitis serious (halotan) ü Chronic periportal hepatitis (sulphonamides)

Toxic and drug induced liver damage : forms ü Granulomatous hepatitis (phenylbutazone) ü Vascular lesions (contraceptives, cytostatics) ü Hyperplasia, neoplasia (contraceptives)
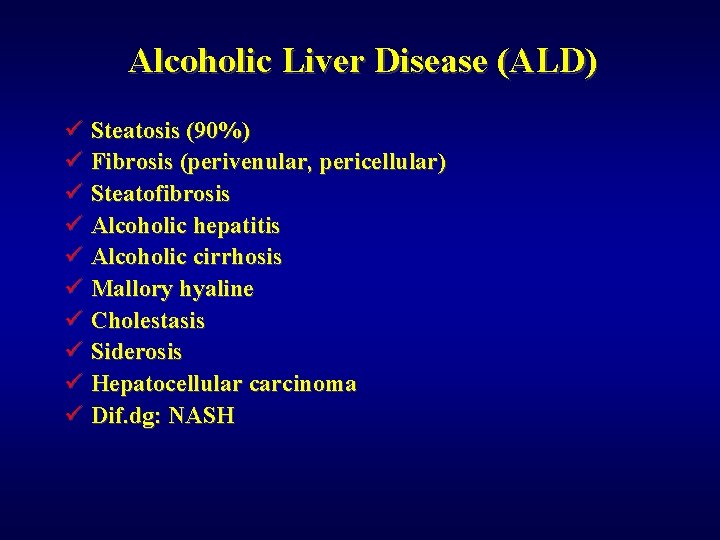
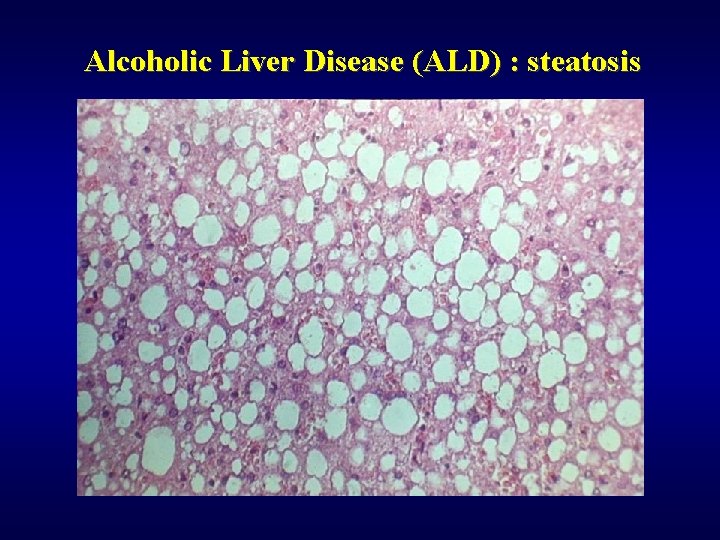
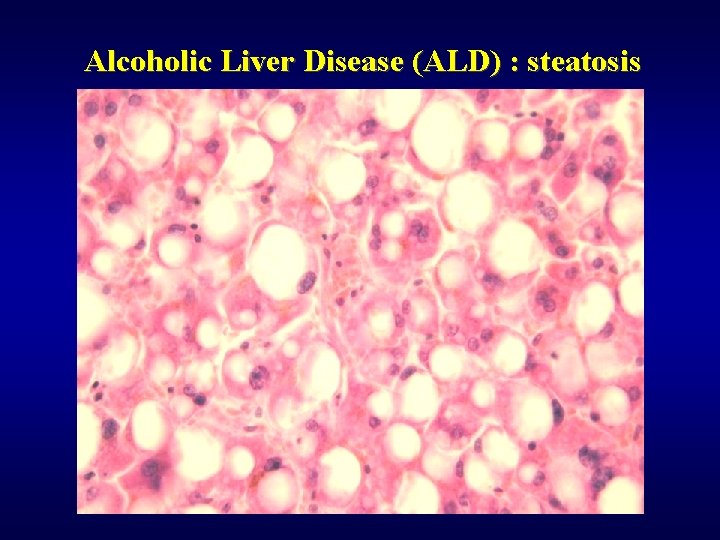
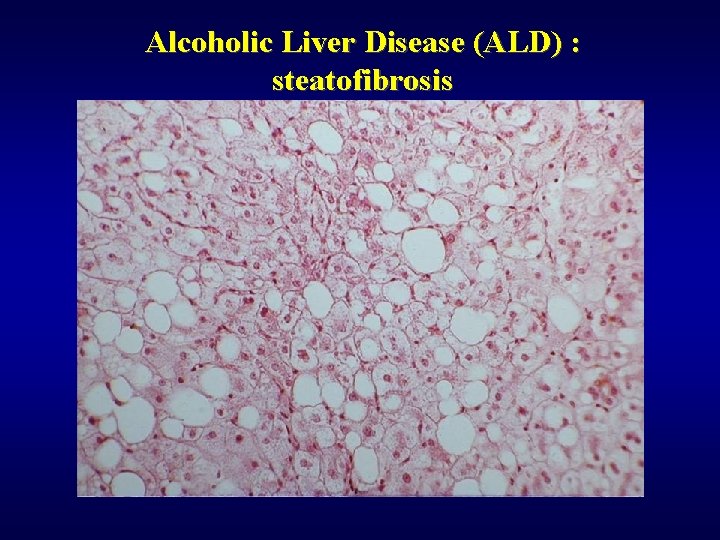
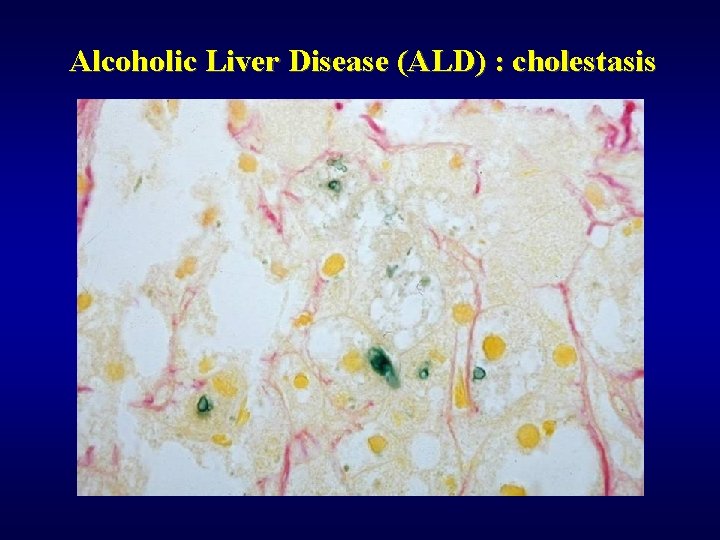
Alcoholic Liver Disease (ALD) ü Steatosis (90%) ü Fibrosis (perivenular, pericellular) ü Steatofibrosis ü Alcoholic hepatitis ü Alcoholic cirrhosis ü Mallory hyaline ü Cholestasis ü Siderosis ü Hepatocellular carcinoma ü Dif. dg: NASH
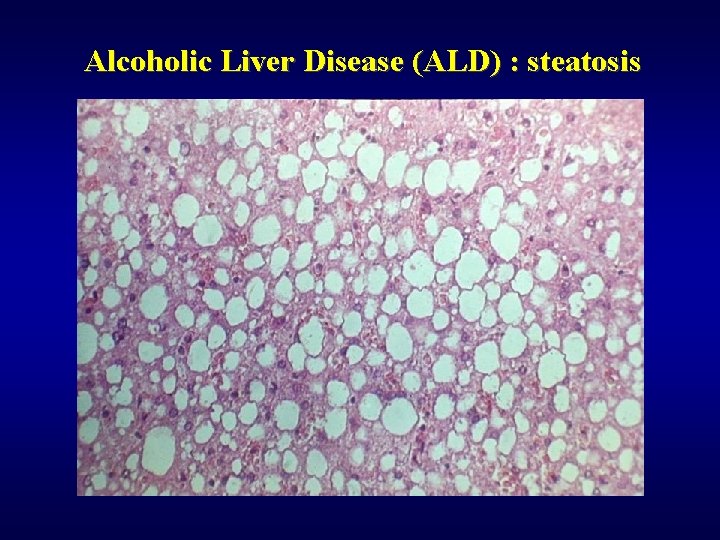
Alcoholic Liver Disease (ALD) : steatosis
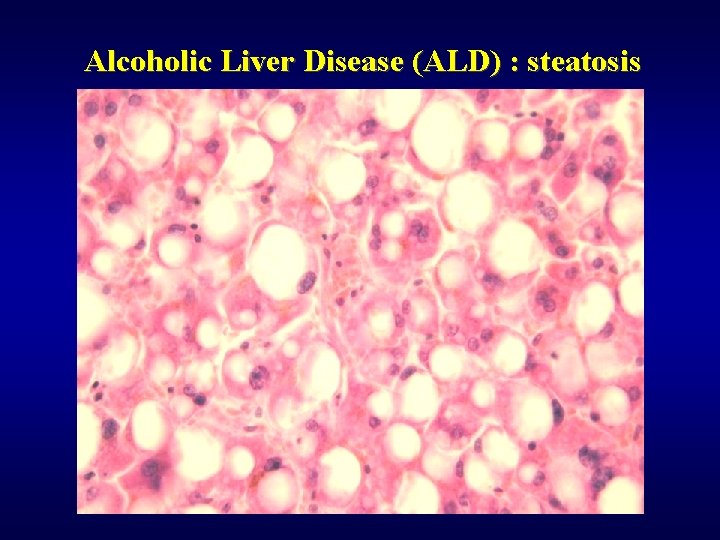
Alcoholic Liver Disease (ALD) : steatosis
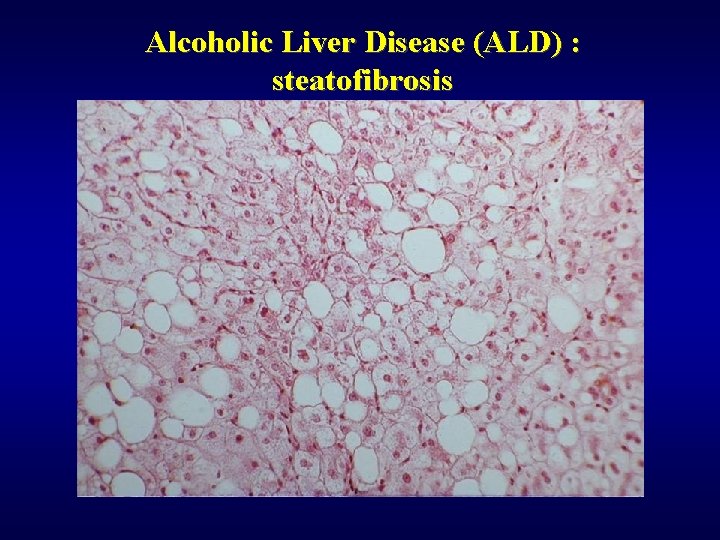
Alcoholic Liver Disease (ALD) : steatofibrosis
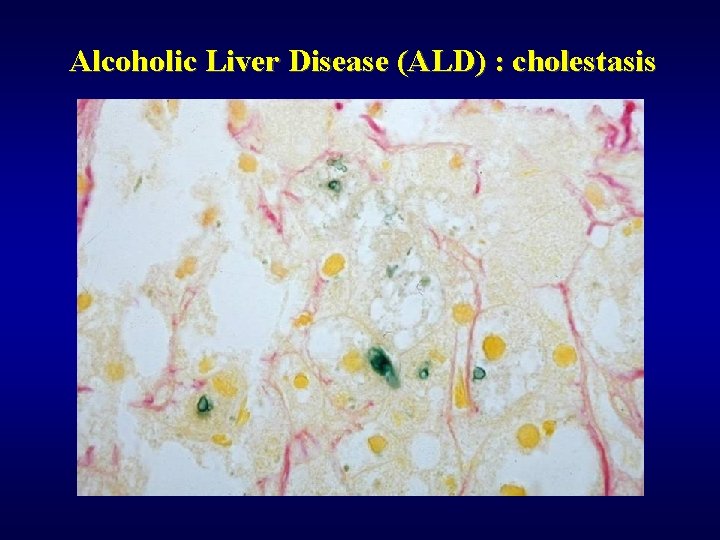
Alcoholic Liver Disease (ALD) : cholestasis
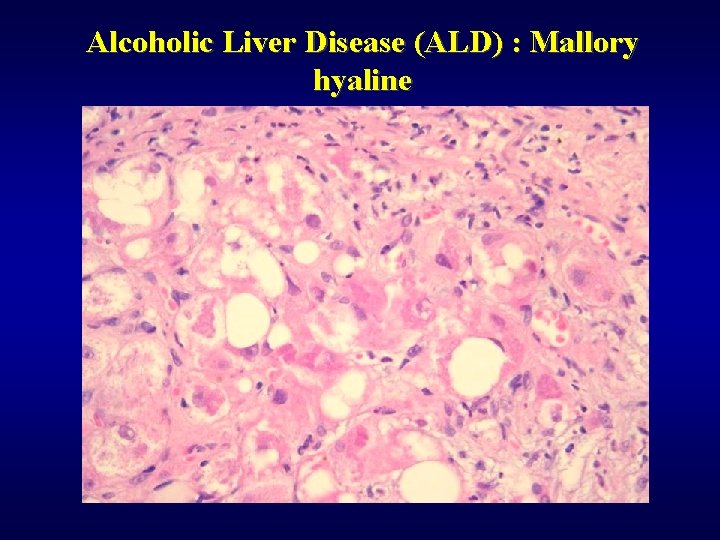
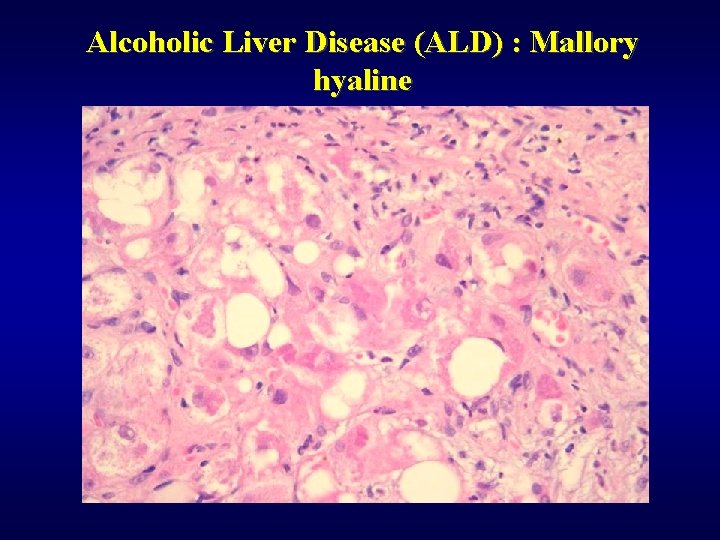
Alcoholic Liver Disease (ALD) : Mallory hyaline

Alcoholic Liver Disease (ALD) : Mallory hyaline
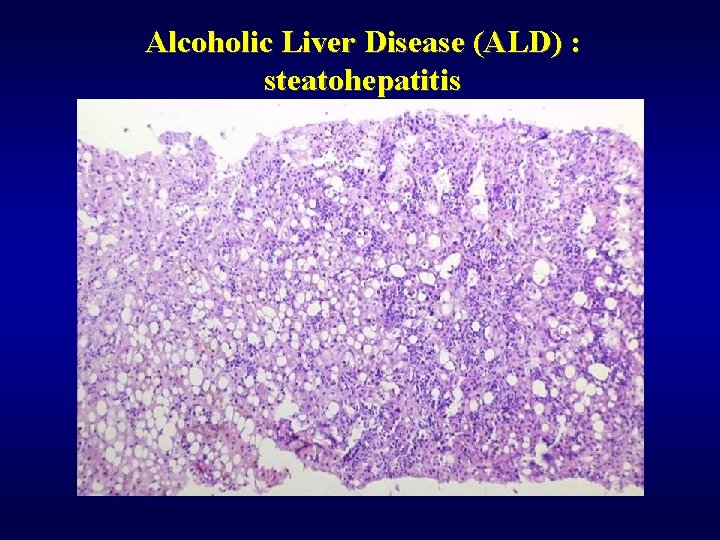
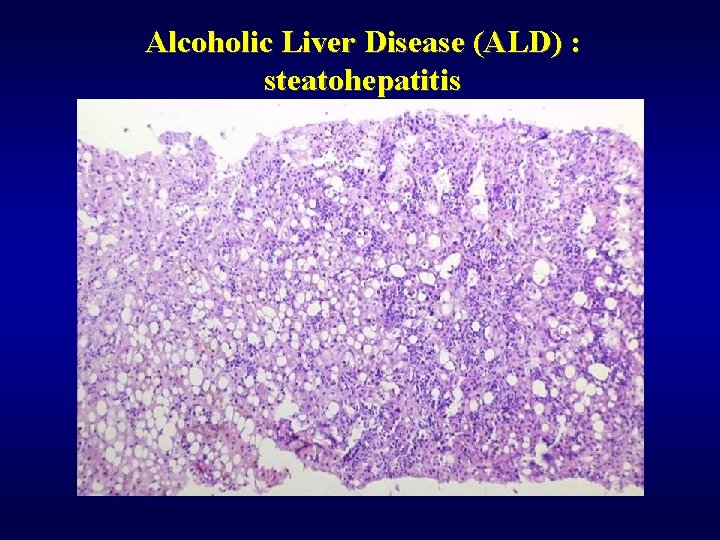
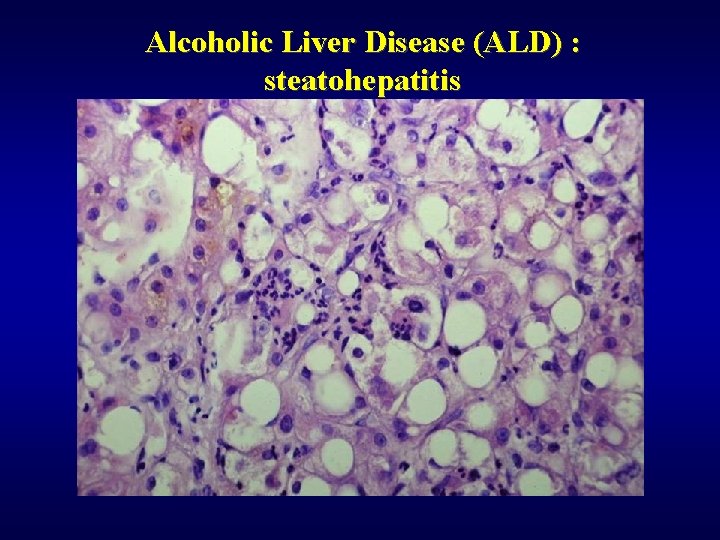
Alcoholic Liver Disease (ALD) : steatohepatitis
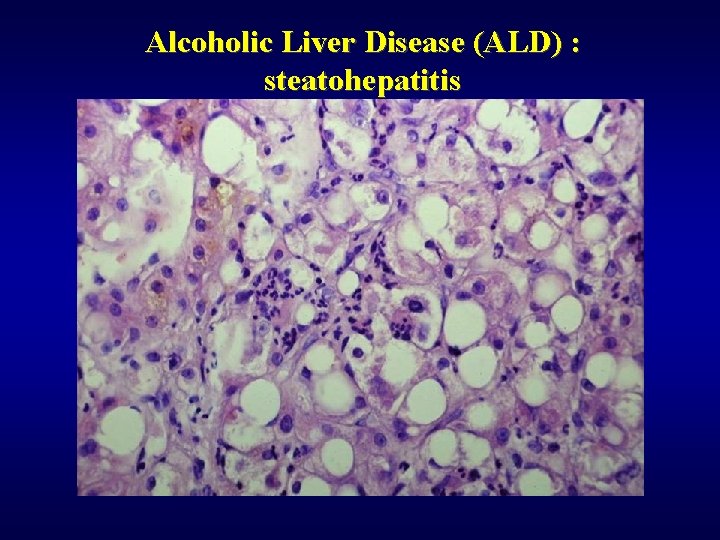
Alcoholic Liver Disease (ALD) : steatohepatitis
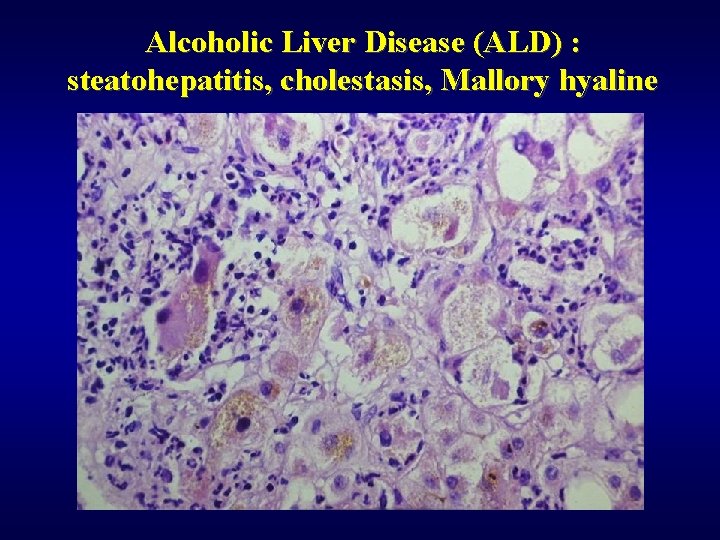
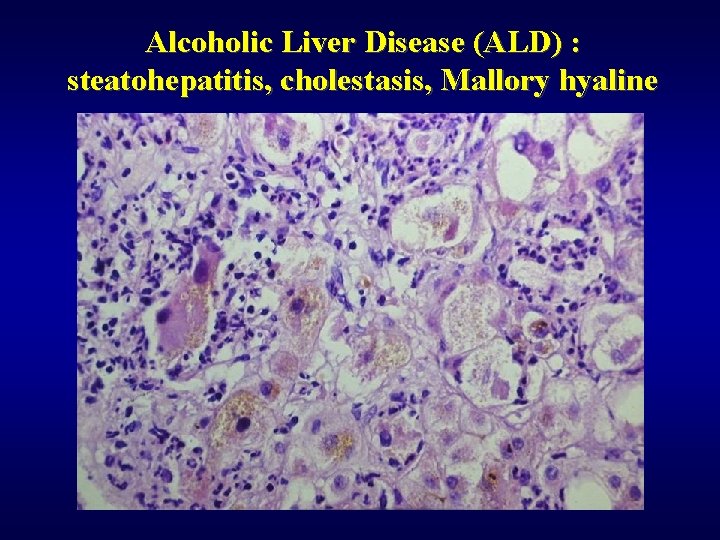
Alcoholic Liver Disease (ALD) : steatohepatitis, cholestasis, Mallory hyaline
Metabolic liver disease ü Haemochromatosis ü Wilson’s disease ü a 1 anti-trypsin deficiency ü Glycogenoses
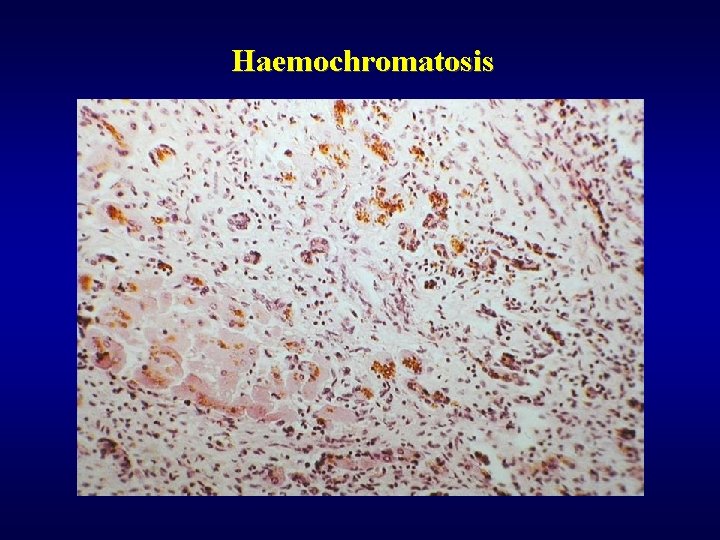
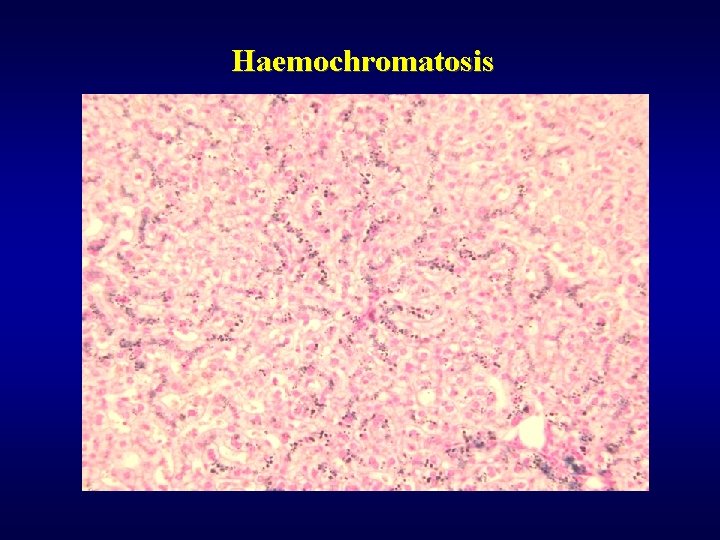
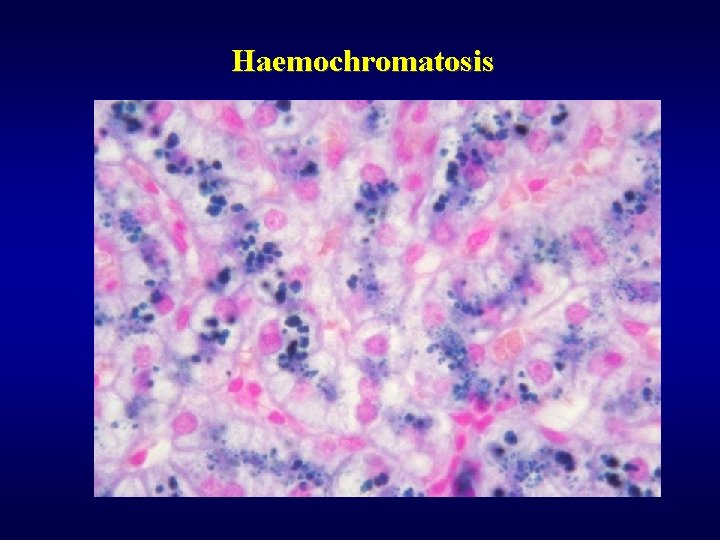
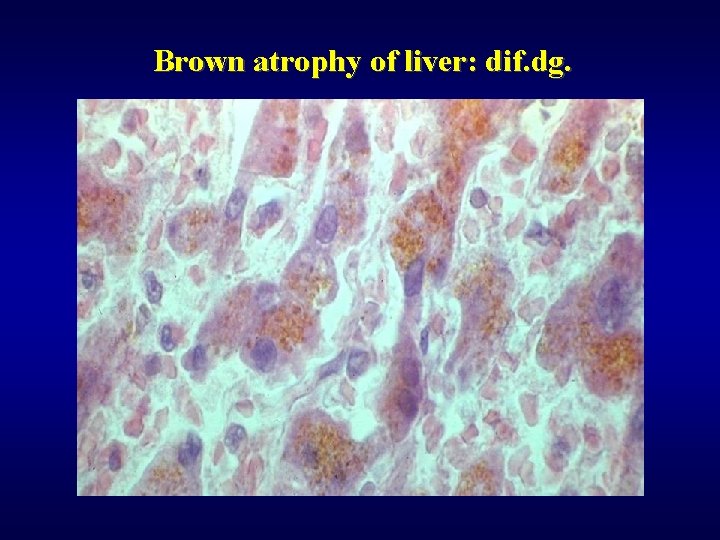
Haemochromatosis ü Excessive accumulation of iron in parenchymatous organs ü Primary (idiopatic), secondary ü Cirrhosis, diabetes mellitus, pigmentation of skin ü Dif. dg. of brown pigment within the liver • Fe (haemochromatosis) • Cu (Wilson’s disease) • lipopigment (brown atrophy of liver, lipopigment dystrophy)
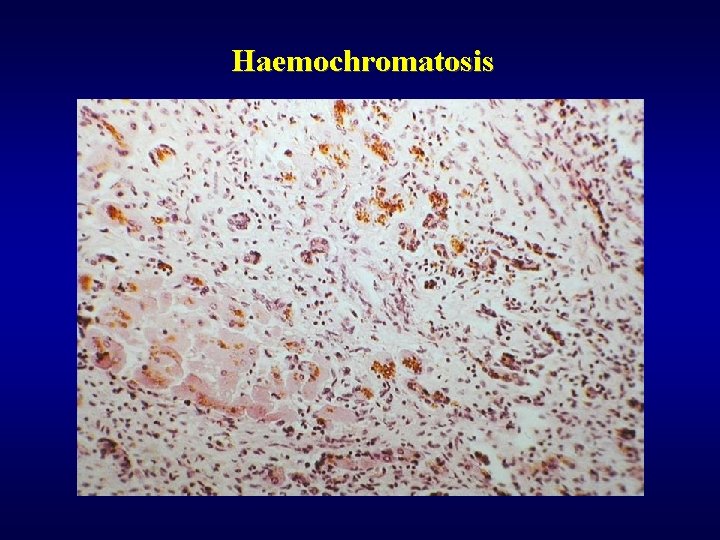
Haemochromatosis
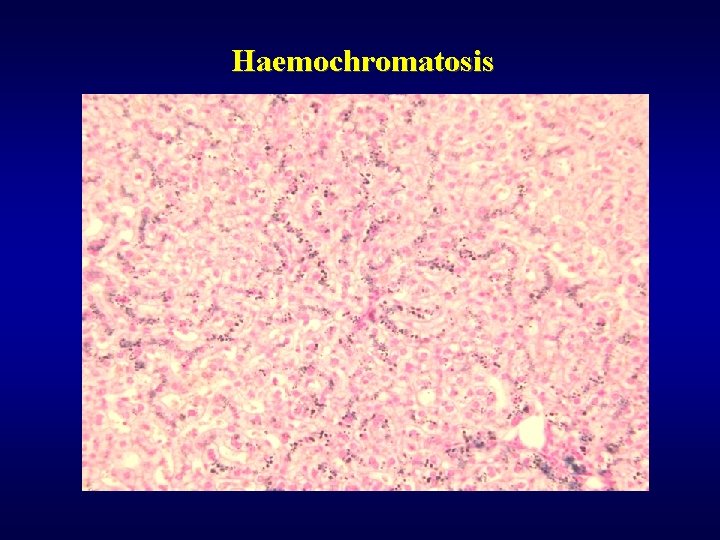
Haemochromatosis
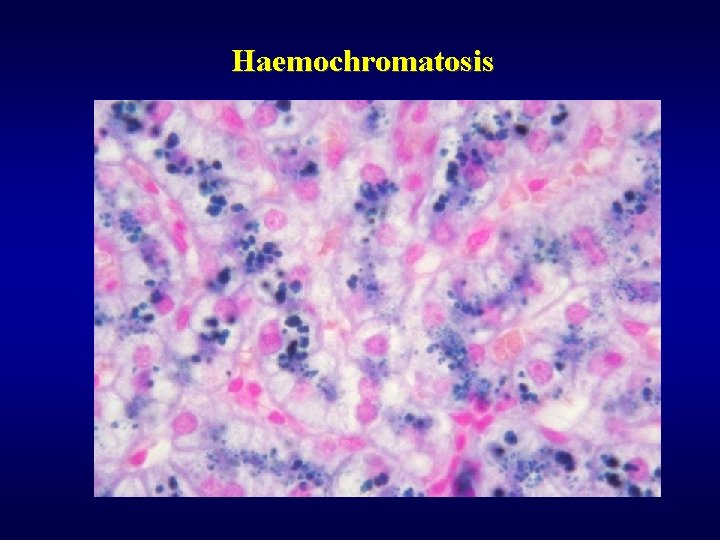
Haemochromatosis
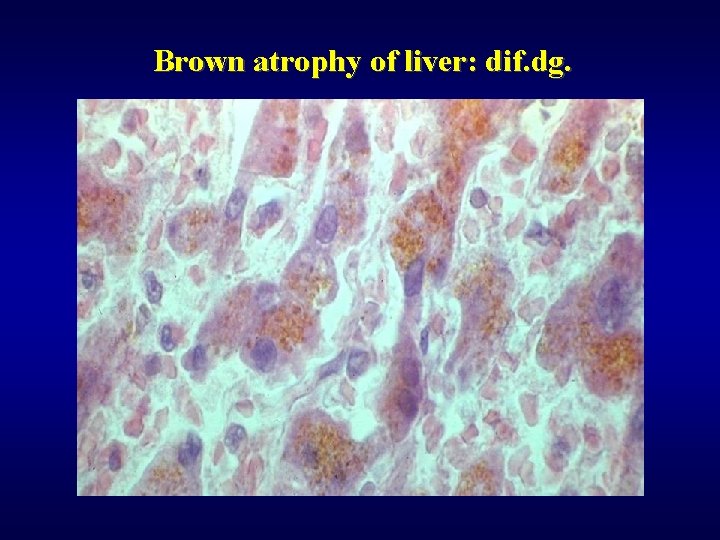
Brown atrophy of liver: dif. dg.
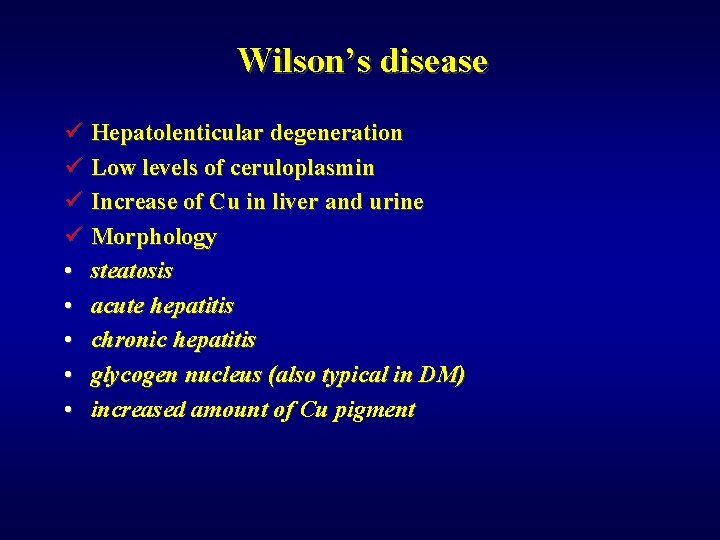
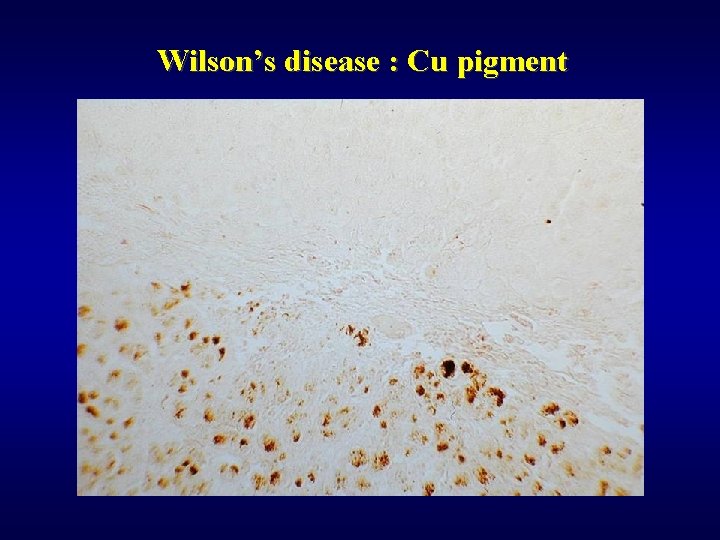
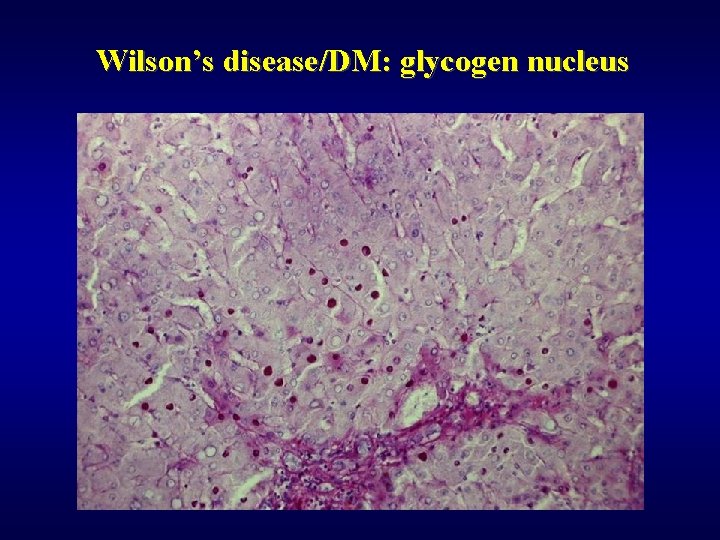
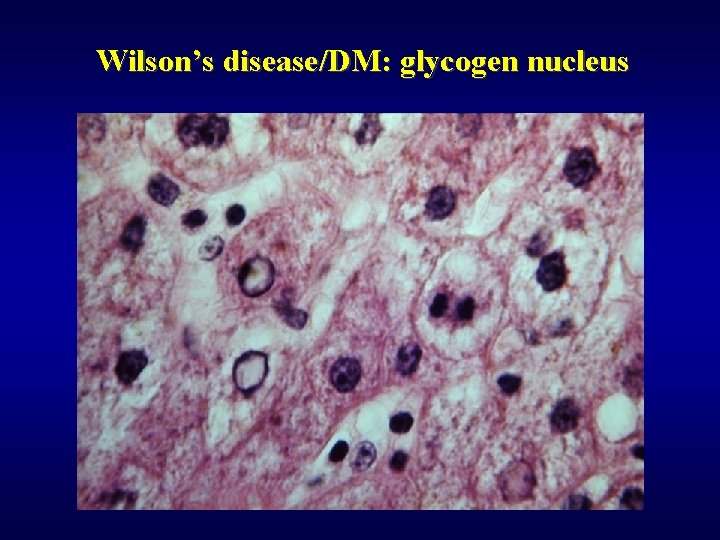
Wilson’s disease ü Hepatolenticular degeneration ü Low levels of ceruloplasmin ü Increase of Cu in liver and urine ü Morphology • steatosis • acute hepatitis • chronic hepatitis • glycogen nucleus (also typical in DM) • increased amount of Cu pigment
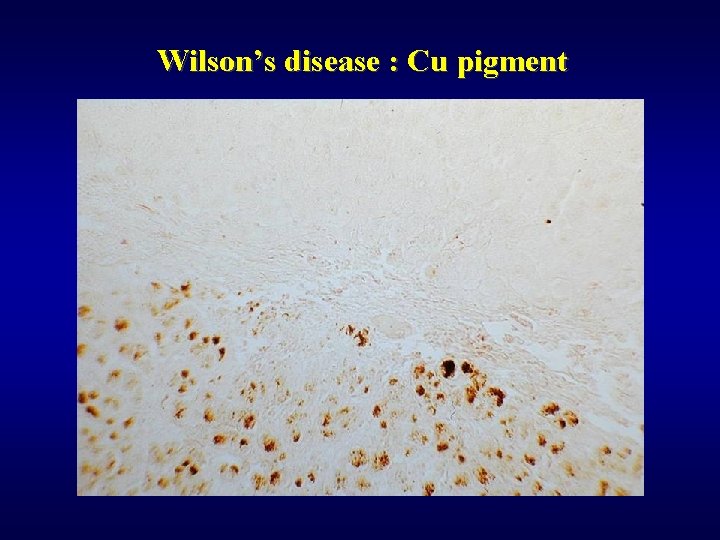
Wilson’s disease : Cu pigment
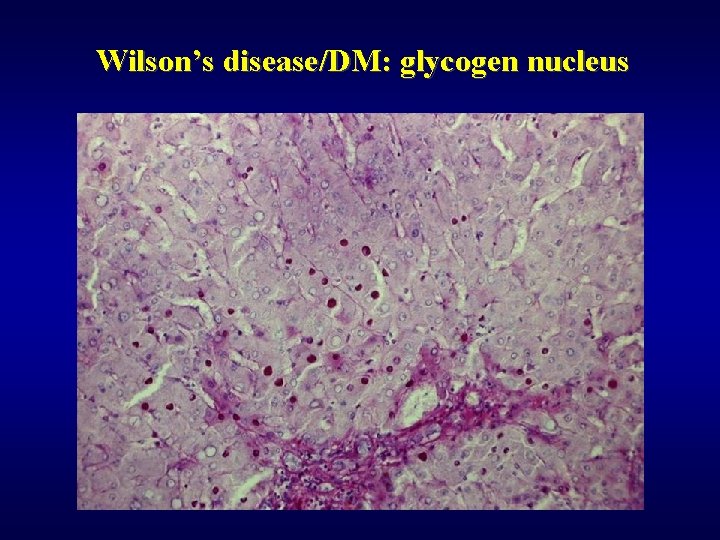
Wilson’s disease/DM: glycogen nucleus
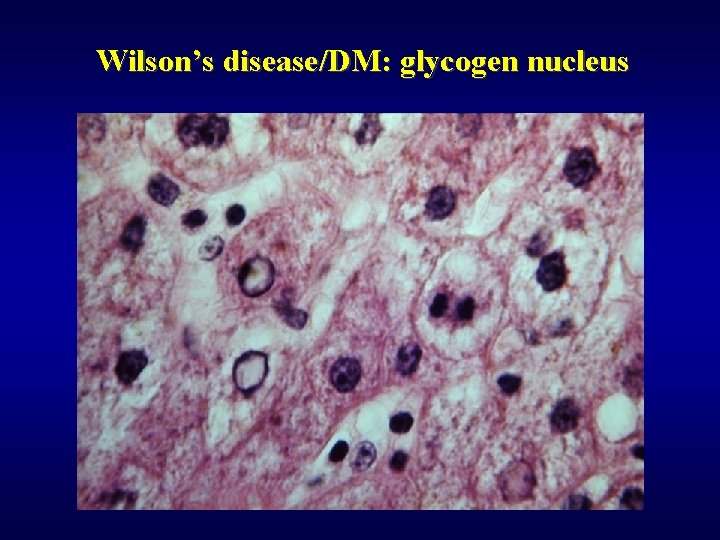
Wilson’s disease/DM: glycogen nucleus
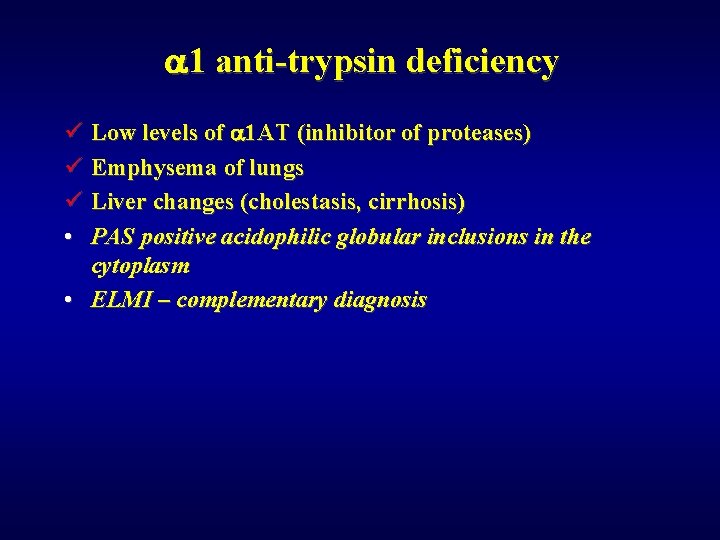
a 1 anti-trypsin deficiency ü Low levels of a 1 AT (inhibitor of proteases) ü Emphysema of lungs ü Liver changes (cholestasis, cirrhosis) • PAS positive acidophilic globular inclusions in the cytoplasm • ELMI – complementary diagnosis
Circulatory disorders of the liver ü Disorders of arterial system ü Disorders of portal system ü Disorders of venous system ü Disorders of lobular system
Disorders of arterial system Infarct of the liver ü Rare ü Thrombosis, compression, obliteration of a. hepatis branch (polyarteritis nodosa, …) ü Pale ü Dif. dg. : • Zahn infarct (occlusion of intrahepatic branch of v. portae): no necrosis, local congestion of sinusoids and secondary atrophy

Liver infarct
Disorders of portal system Thrombosis and occlusion of v. portae ü Extrahepatal (phlebitis, pancreatitis, surgery, trauma) ü Intrahepatal (invasion of tumor)
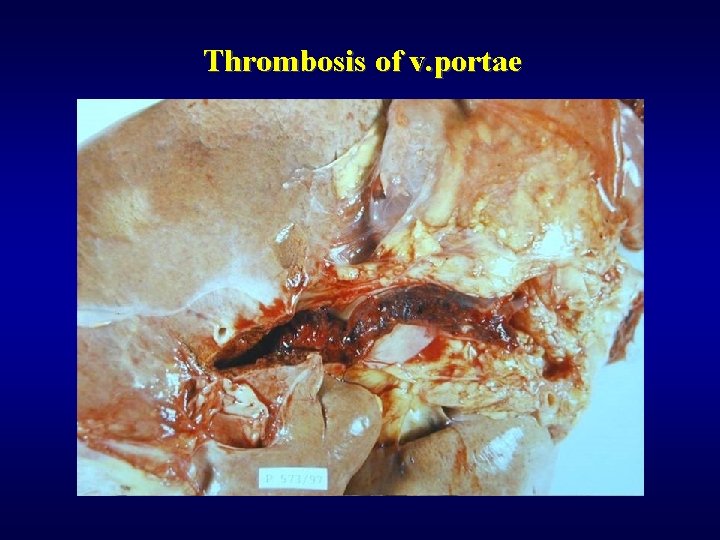
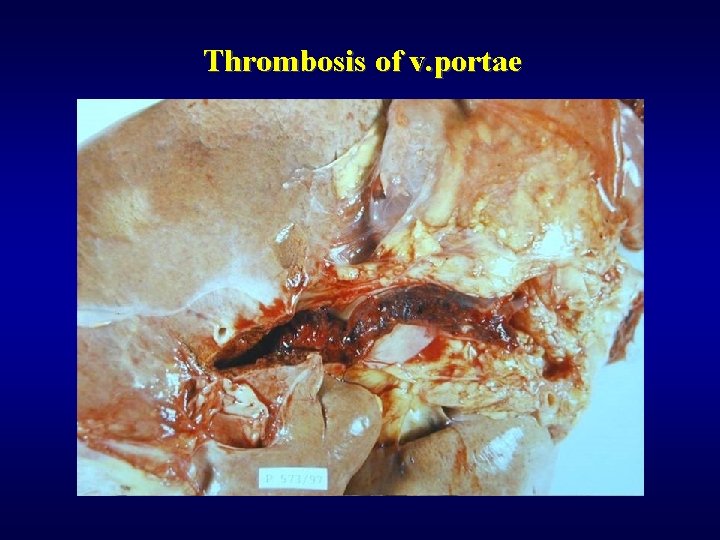
Thrombosis of v. portae
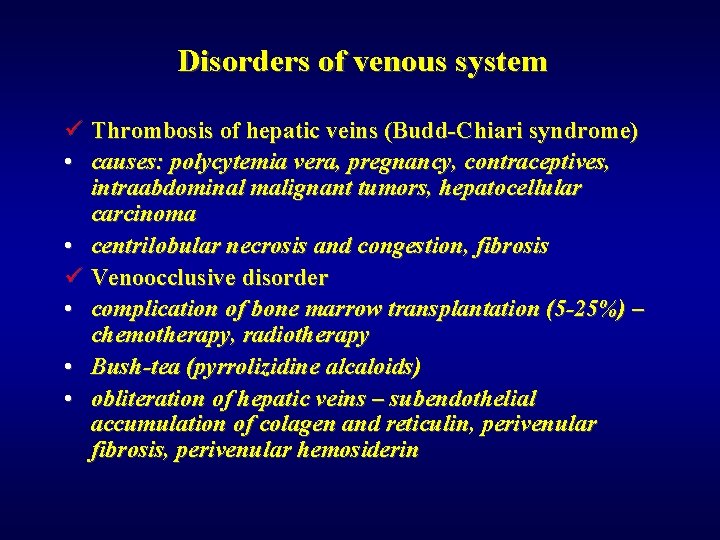
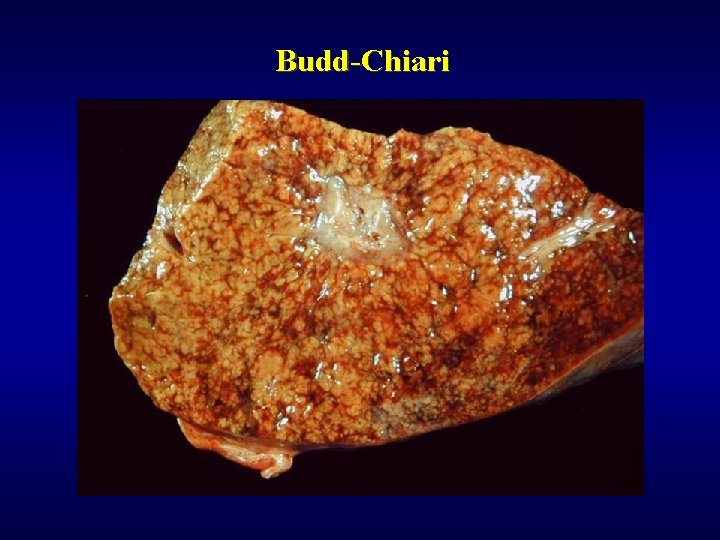
Disorders of venous system ü Thrombosis of hepatic veins (Budd-Chiari syndrome) • causes: polycytemia vera, pregnancy, contraceptives, intraabdominal malignant tumors, hepatocellular carcinoma • centrilobular necrosis and congestion, fibrosis ü Venoocclusive disorder • complication of bone marrow transplantation (5 -25%) – chemotherapy, radiotherapy • Bush-tea (pyrrolizidine alcaloids) • obliteration of hepatic veins – subendothelial accumulation of colagen and reticulin, perivenular fibrosis, perivenular hemosiderin
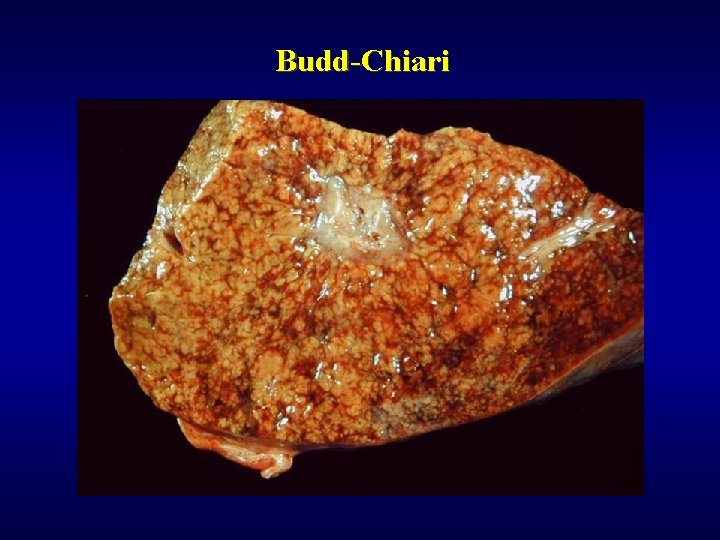
Budd-Chiari
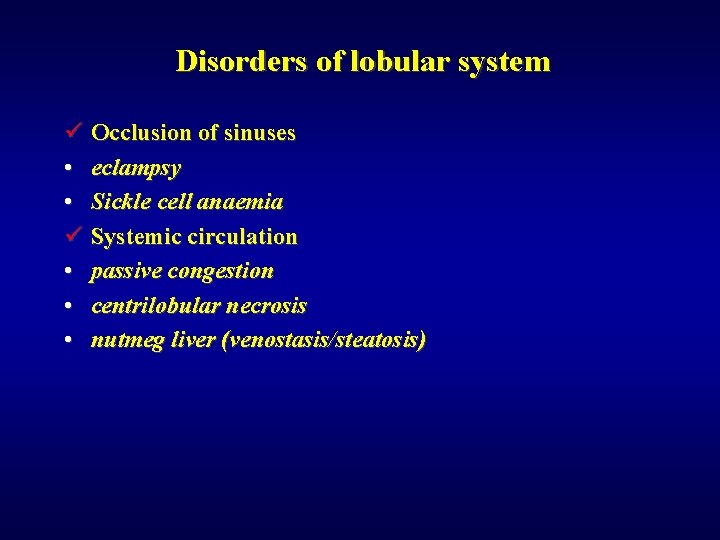
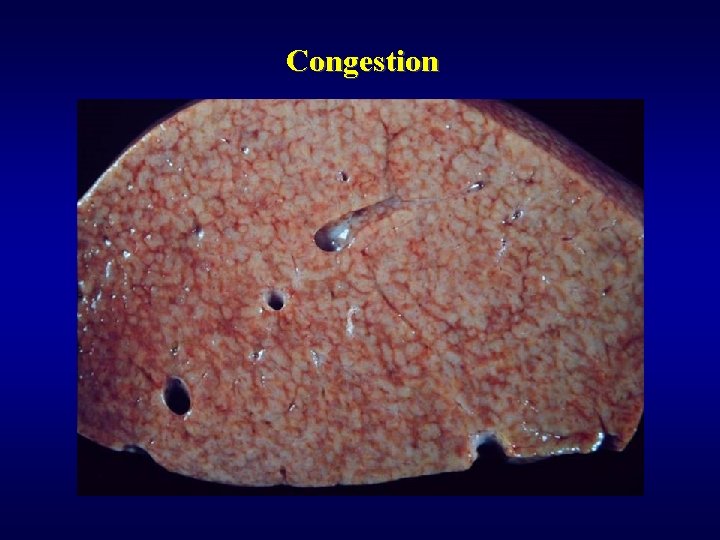
Disorders of lobular system ü Occlusion of sinuses • eclampsy • Sickle cell anaemia ü Systemic circulation • passive congestion • centrilobular necrosis • nutmeg liver (venostasis/steatosis)
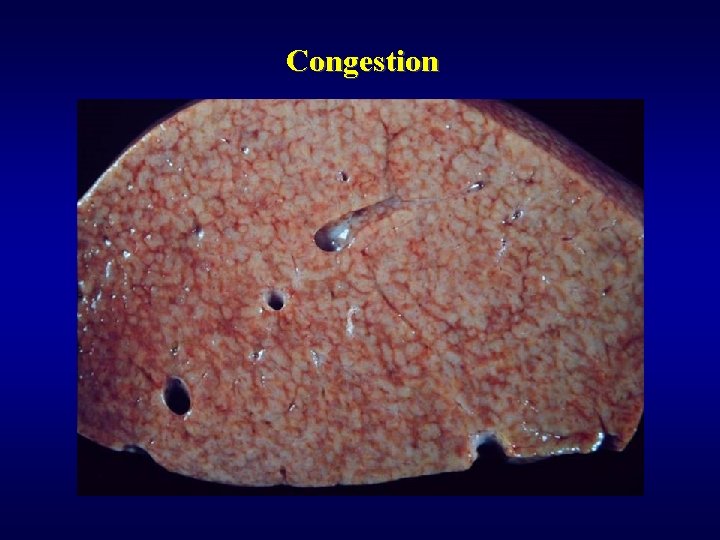
Congestion
Pathology of intrahepatal bile ducts ü Secondary biliary cirrhosis (SBC) ü Primary biliary cirrhosis (PBC) ü Primary sclerosing cholangitis (PSC)
SBC ü Obstruction of extrahepatal bile ducts: atresia, lithiasis, tumor, iatrogenic ü Striking cholestasis
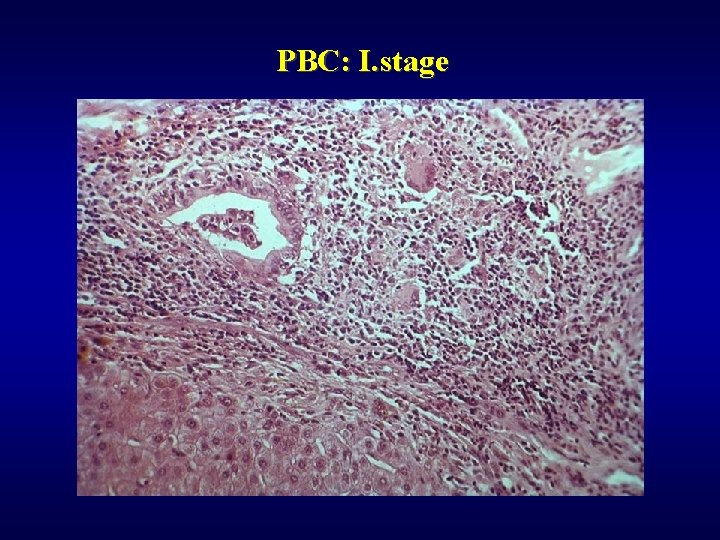
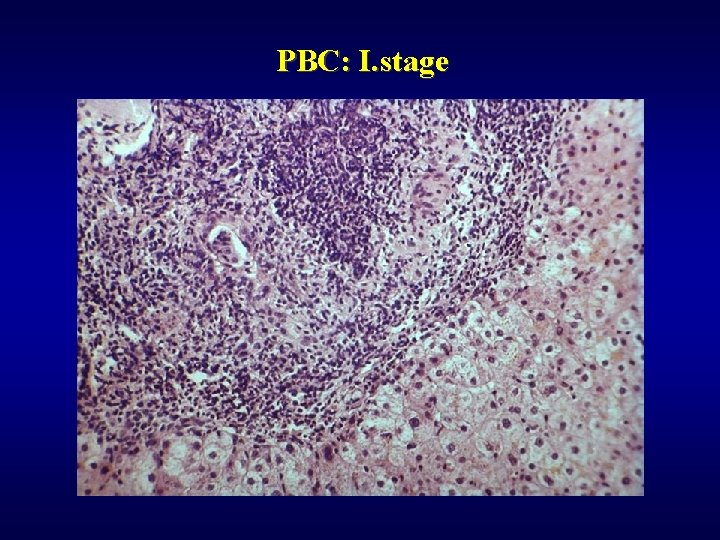
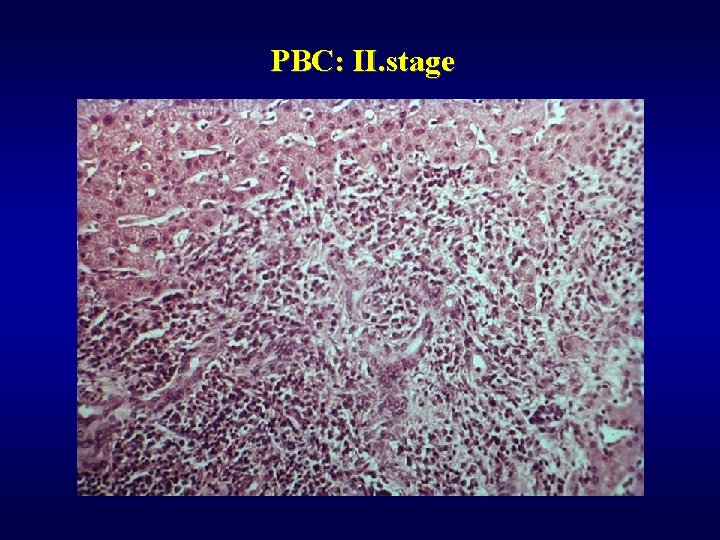
PBC ü Autoimmune (AMA), ü Majority of females ü Coincidency: Sjögren sy. , arthritis, thyreoiditis, vasculitis, . . ü Hepatomegaly, ü 4 stages • I - granulomatous destruction of ducts • II - ductular proliferation and periportal hepatitis • III - scarring, necrosis, septal fibrosis • IV - cirrhosis
PSC ü Autoimmune (ANA) ü Inflammation and obliterative fibrosis of bile ducts ü Coincidency: IBD (Inflammatory Bowel Disease – ulcerative colitis, m. Crohn)
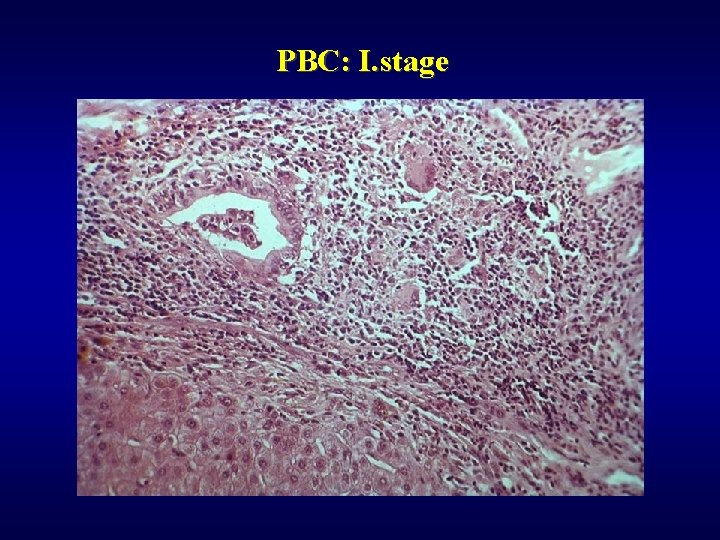
PBC: I. stage
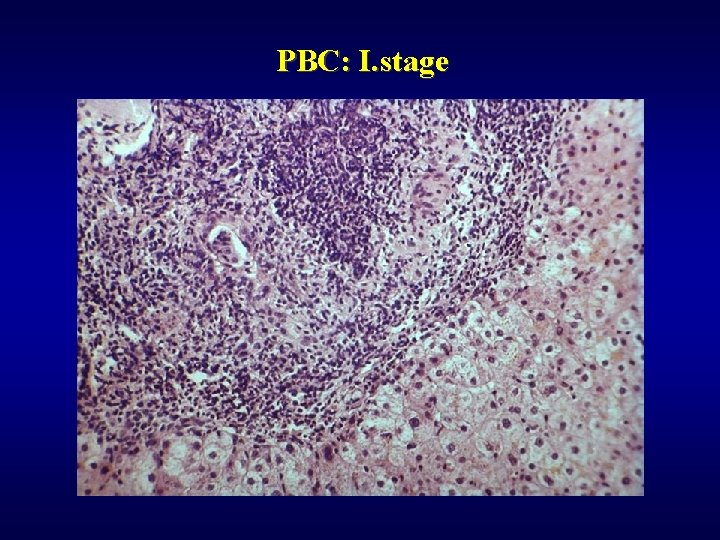
PBC: I. stage
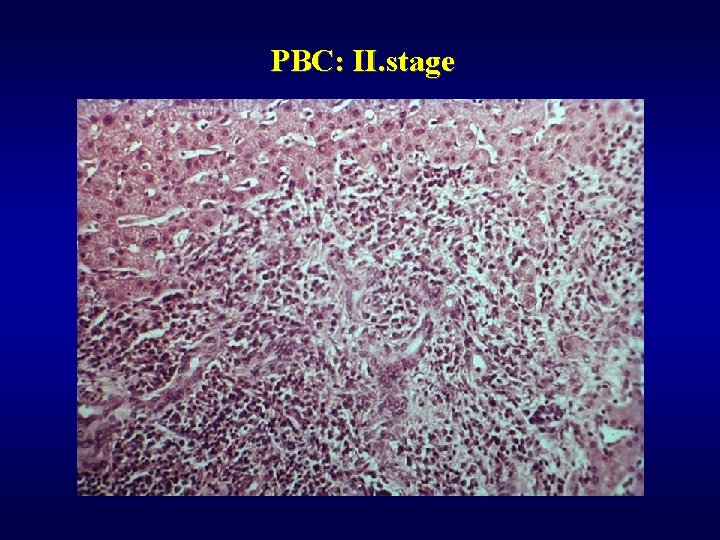
PBC: II. stage

PBC: III. stage
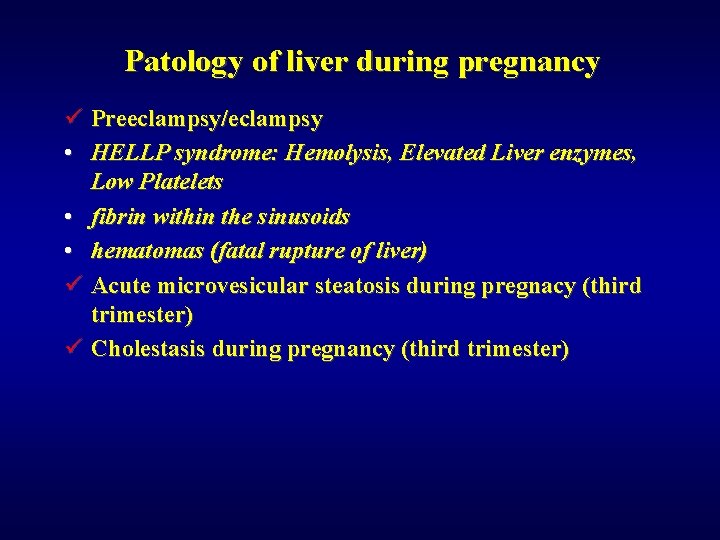
Patology of liver during pregnancy ü Preeclampsy/eclampsy • HELLP syndrome: Hemolysis, Elevated Liver enzymes, Low Platelets • fibrin within the sinusoids • hematomas (fatal rupture of liver) ü Acute microvesicular steatosis during pregnacy (third trimester) ü Cholestasis during pregnancy (third trimester)
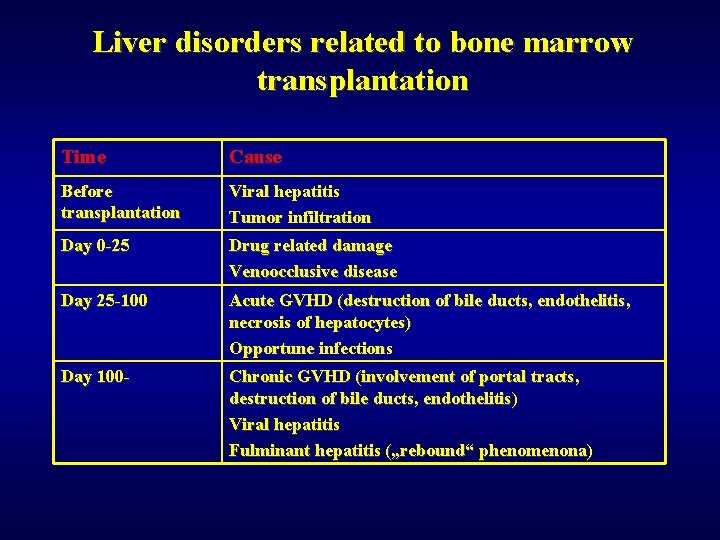
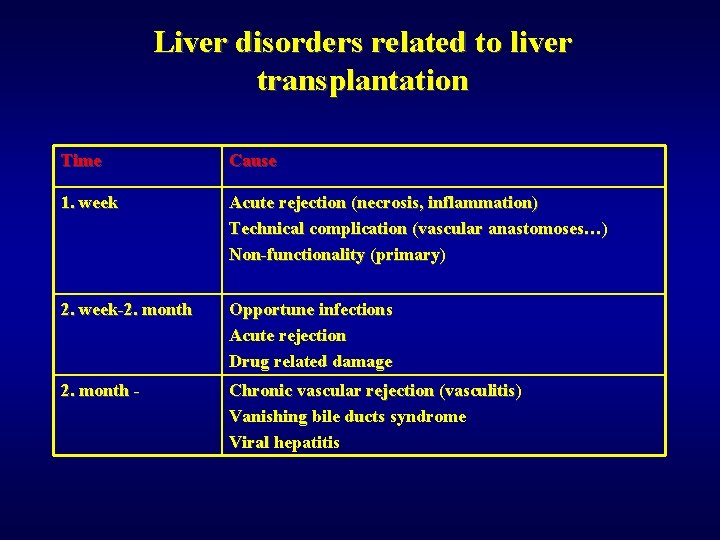
Transplantation ü Liver disorders related to bone marrow transplantation ü Liver disorders related to liver transplantation
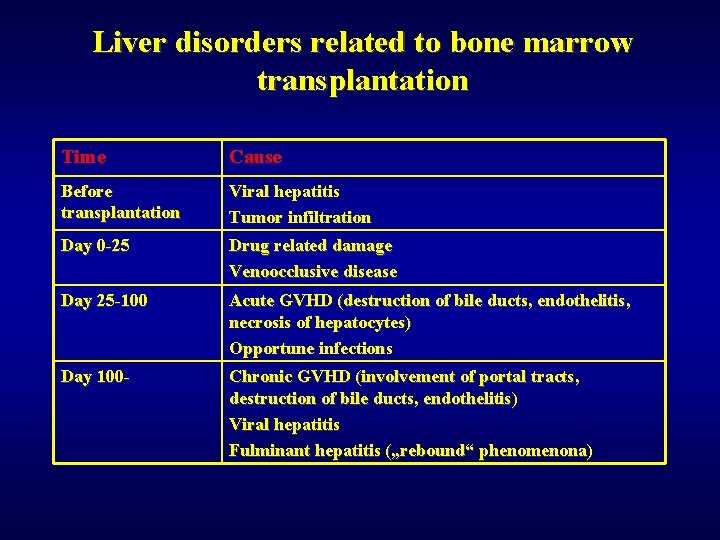
Liver disorders related to bone marrow transplantation Time Cause Before transplantation Viral hepatitis Tumor infiltration Day 0 -25 Drug related damage Venoocclusive disease Day 25 -100 Acute GVHD (destruction of bile ducts, endothelitis, necrosis of hepatocytes) Opportune infections Day 100 - Chronic GVHD (involvement of portal tracts, destruction of bile ducts, endothelitis) Viral hepatitis Fulminant hepatitis („rebound“ phenomenona)
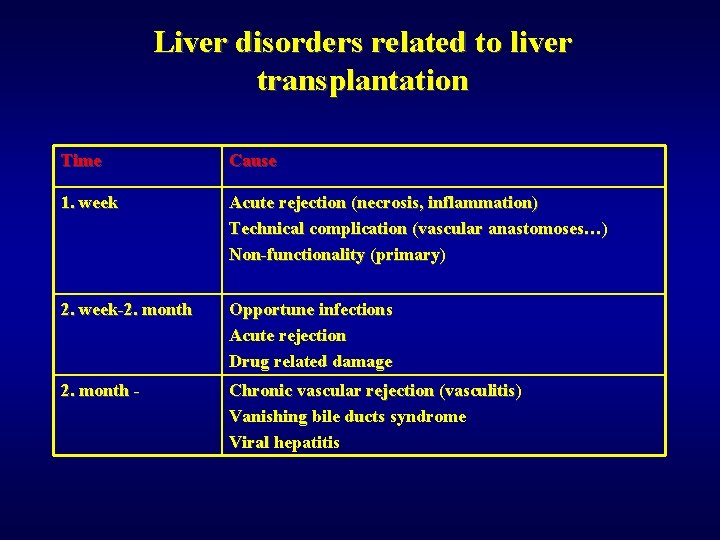
Liver disorders related to liver transplantation Time Cause 1. week Acute rejection (necrosis, inflammation) Technical complication (vascular anastomoses…) Non-functionality (primary) 2. week-2. month Opportune infections Acute rejection Drug related damage 2. month - Chronic vascular rejection (vasculitis) Vanishing bile ducts syndrome Viral hepatitis
Tumors of liver ü Tumor-like lesion ü Benign tumors ü Malignant tumor
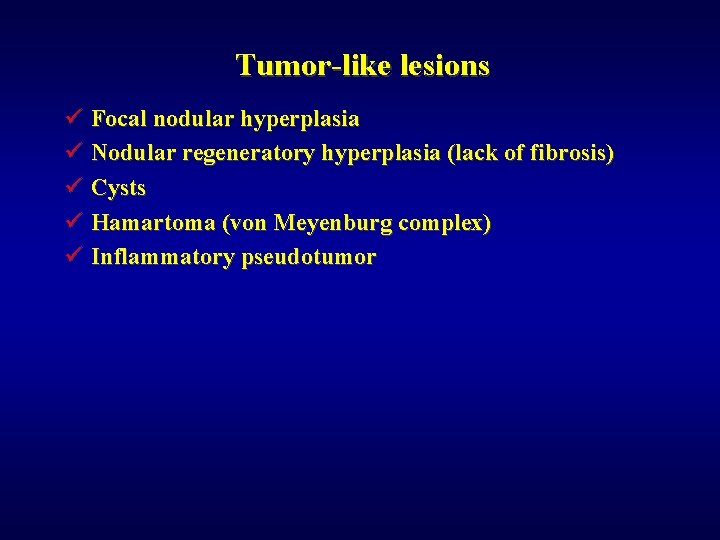
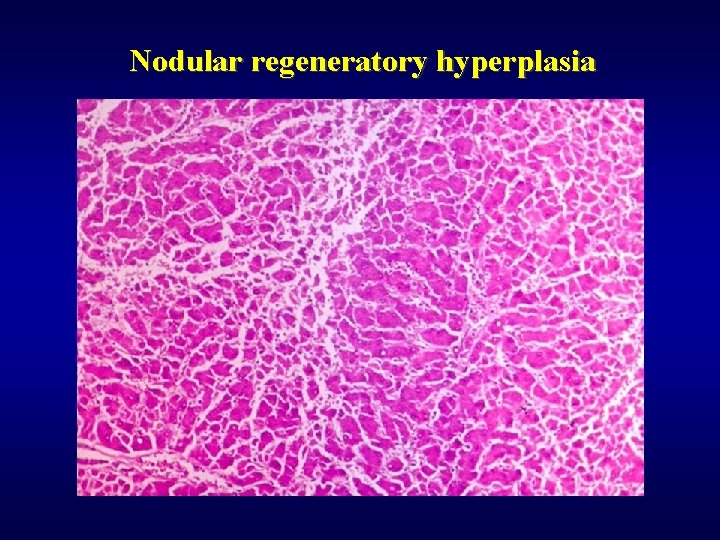
Tumor-like lesions ü Focal nodular hyperplasia ü Nodular regeneratory hyperplasia (lack of fibrosis) ü Cysts ü Hamartoma (von Meyenburg complex) ü Inflammatory pseudotumor
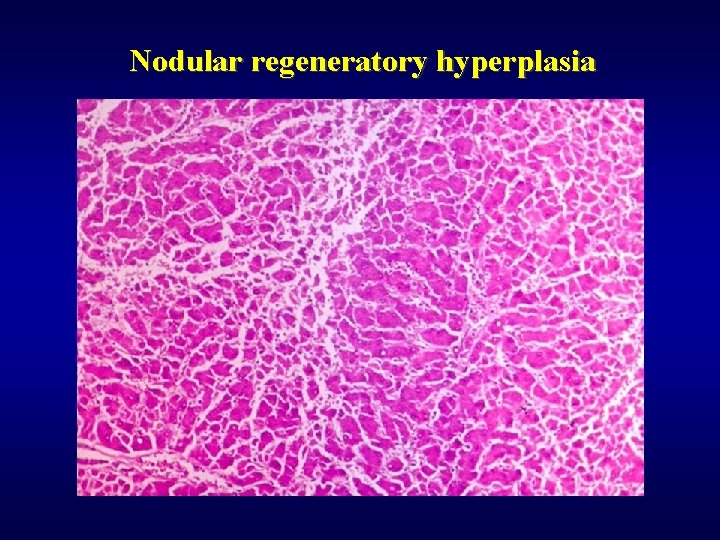
Nodular regeneratory hyperplasia
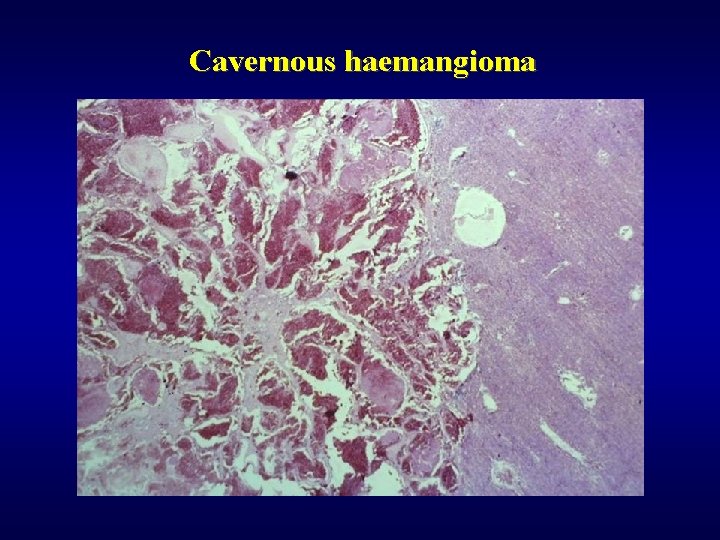
Benign tumors ü Adenoma • hepatocellular (lack of portal tracts!) • cholangiogenic (lack of bile production, less than 1 cm, subcapsular) ü Haemangioma • subcapsular • cavernous • bleeding risk during punction!
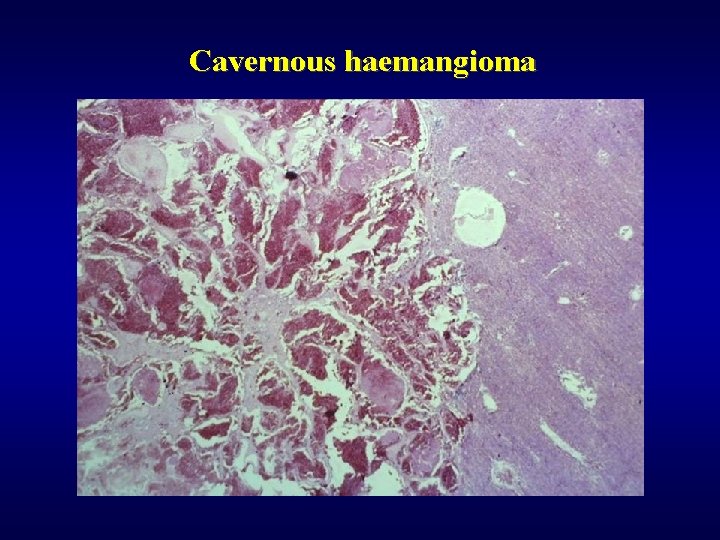
Cavernous haemangioma
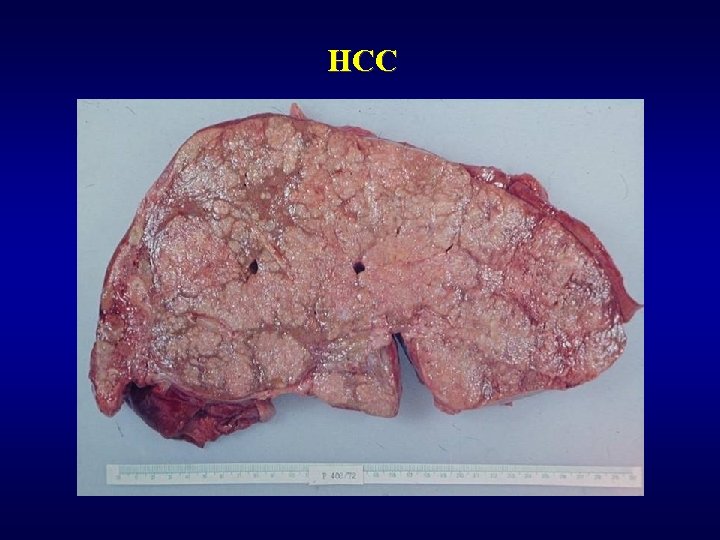
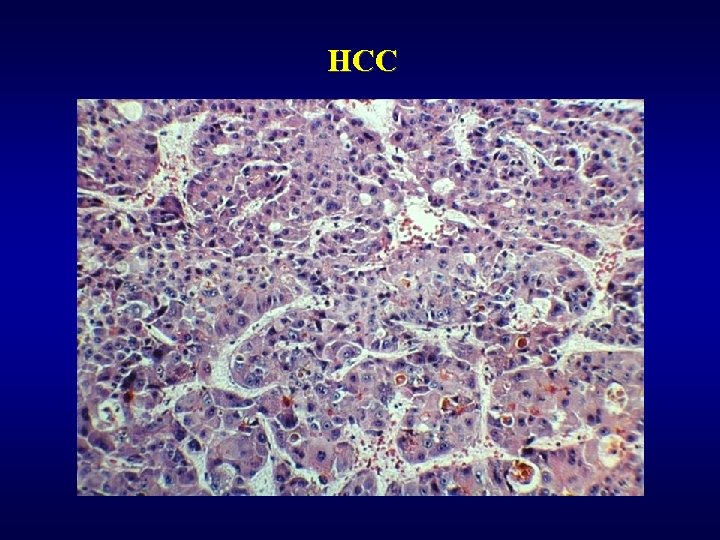
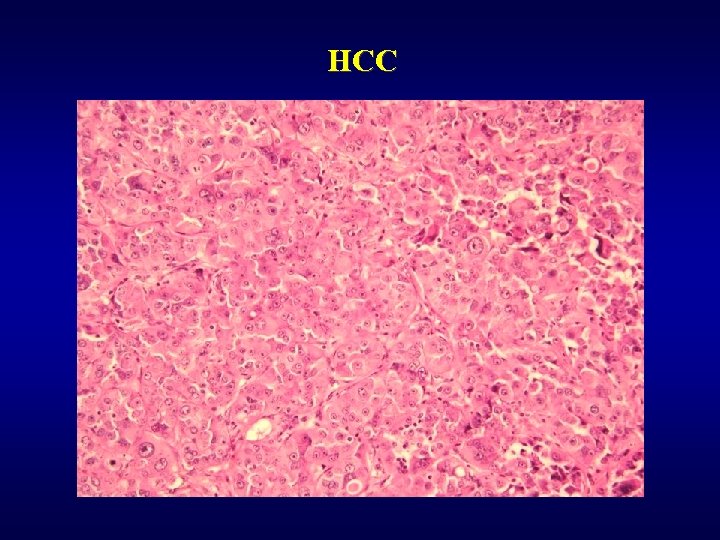
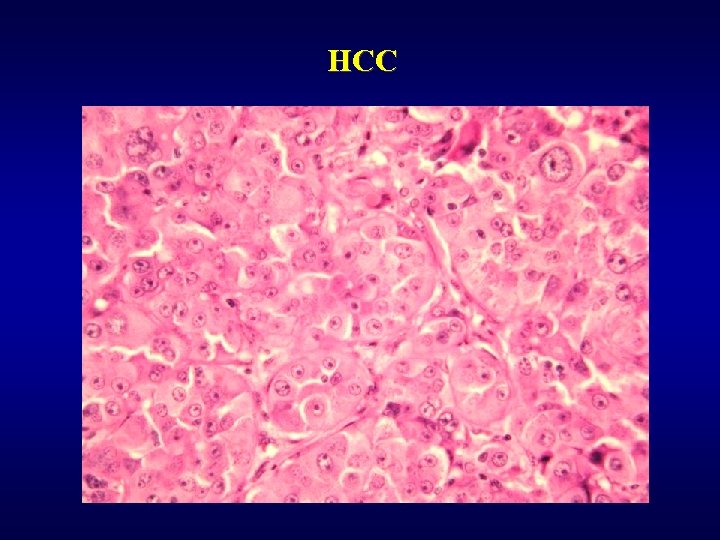
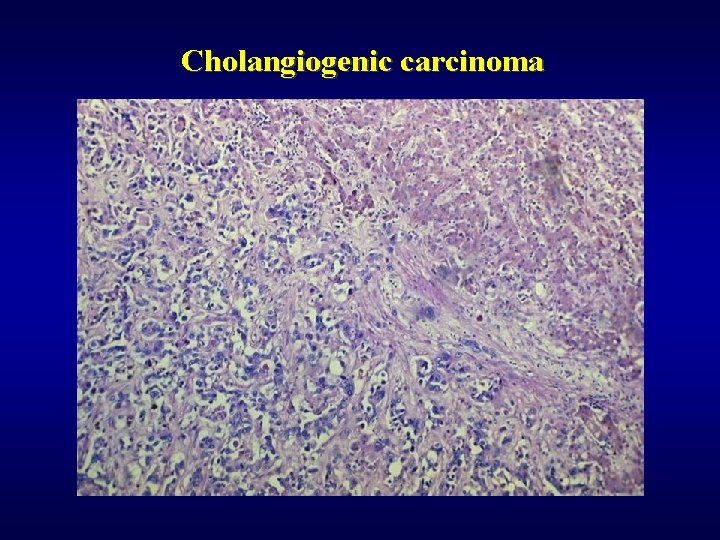
Malignant tumors ü Hepatocellular carcinoma (HCC) • subvariant – fibrolamelar carcinoma ü Cholangiogenic carcinoma (lack of bile production) • peripherial • extrahepatal -Klatskin tumor ü Hepatoblastoma (embryonal, teratoid, …) ü Angiosarcoma, malignant haemangioendothelioma ü Metastases (most often) • GIT, lung, kidney
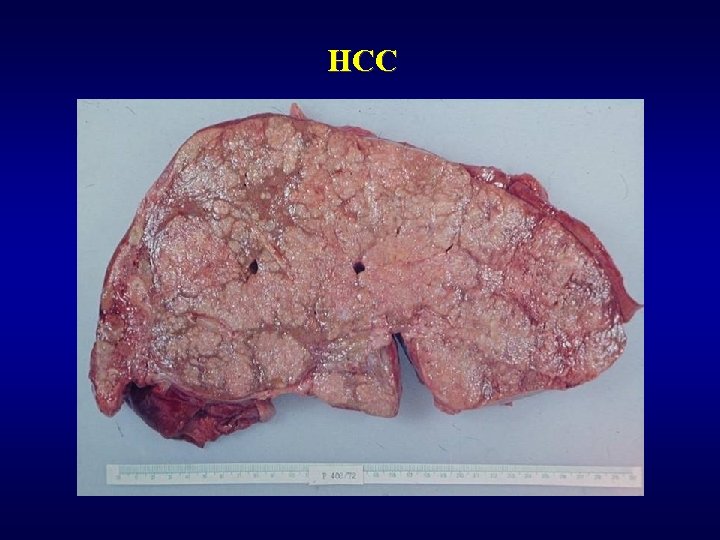
HCC
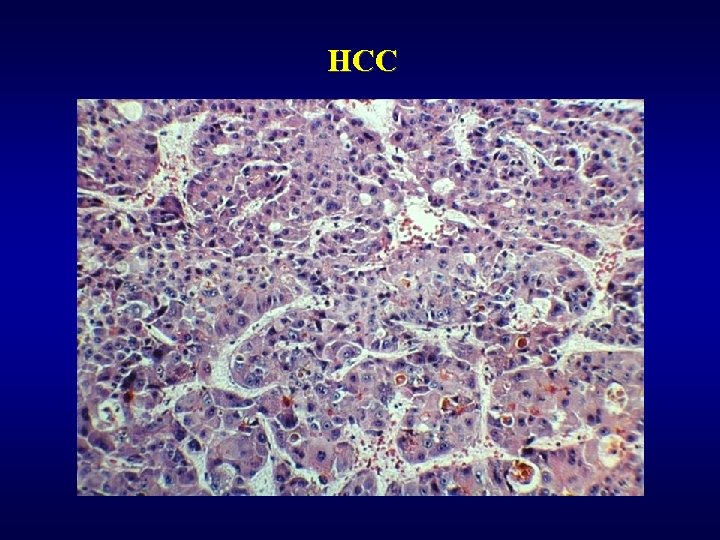
HCC
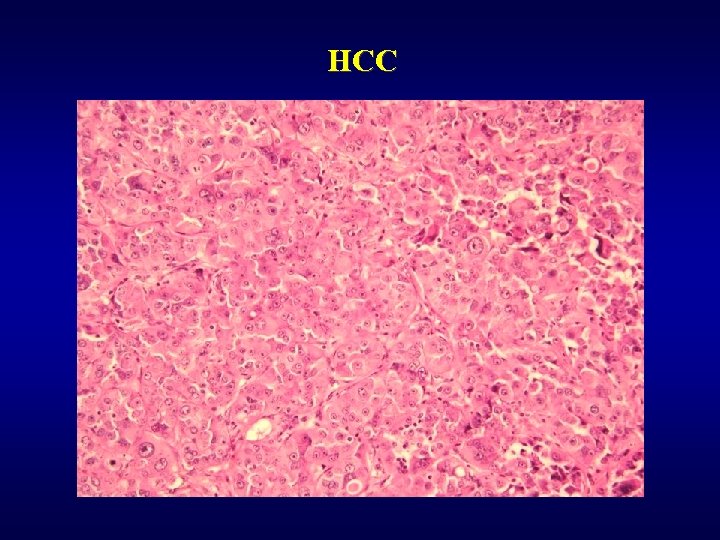
HCC
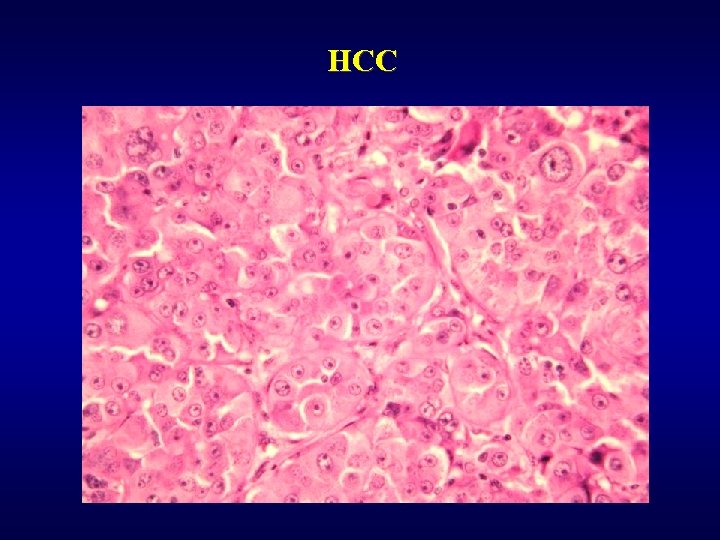
HCC
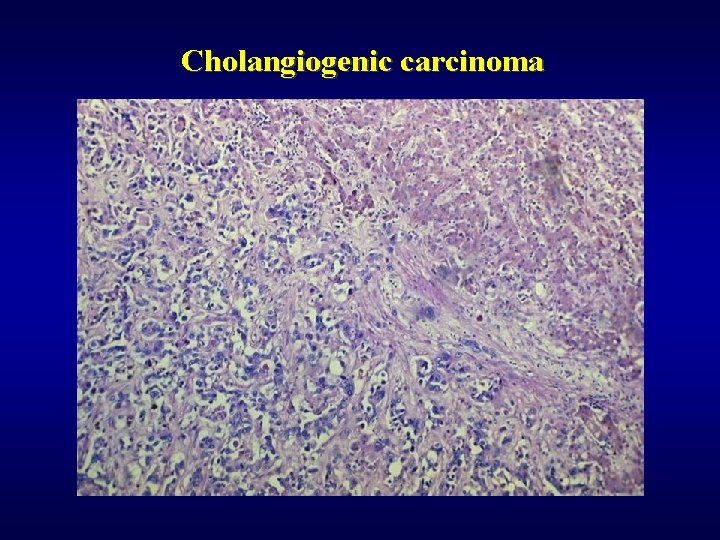
Cholangiogenic carcinoma
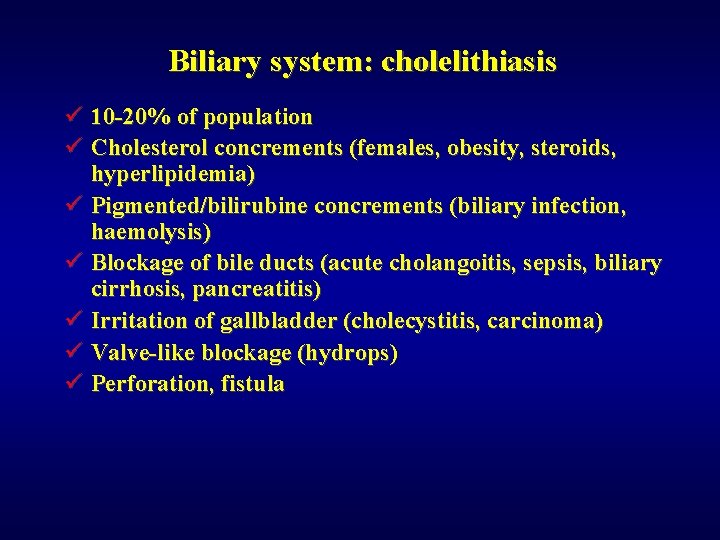
Biliary system: cholelithiasis ü 10 -20% of population ü Cholesterol concrements (females, obesity, steroids, hyperlipidemia) ü Pigmented/bilirubine concrements (biliary infection, haemolysis) ü Blockage of bile ducts (acute cholangoitis, sepsis, biliary cirrhosis, pancreatitis) ü Irritation of gallbladder (cholecystitis, carcinoma) ü Valve-like blockage (hydrops) ü Perforation, fistula
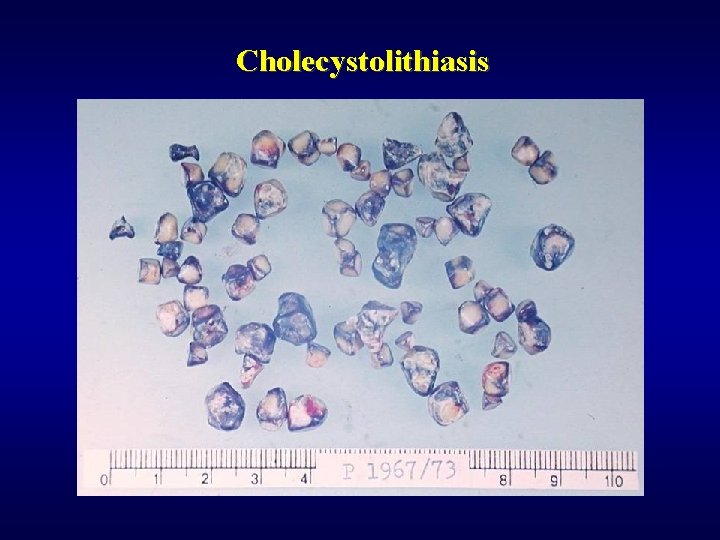
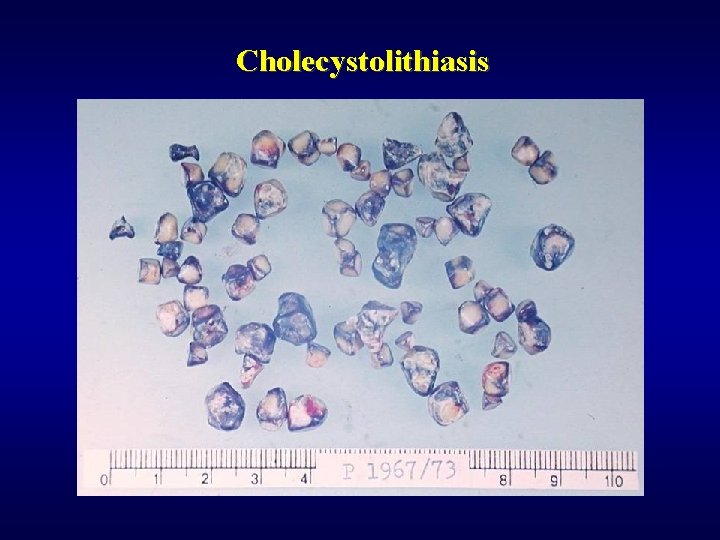
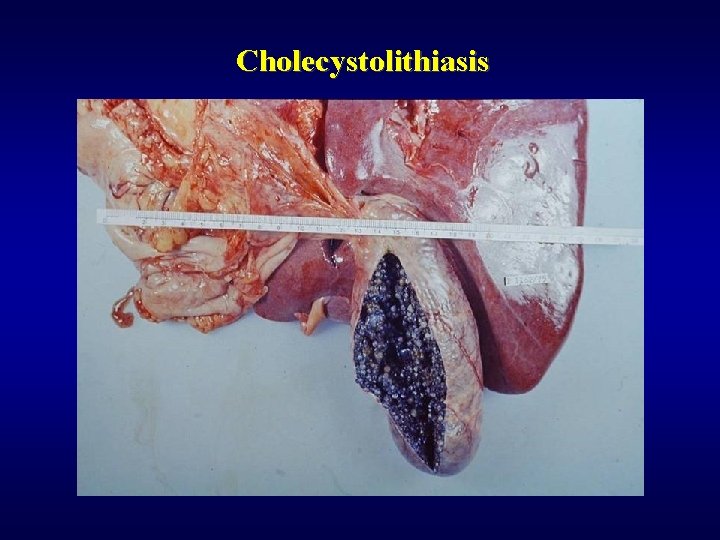
Cholecystolithiasis
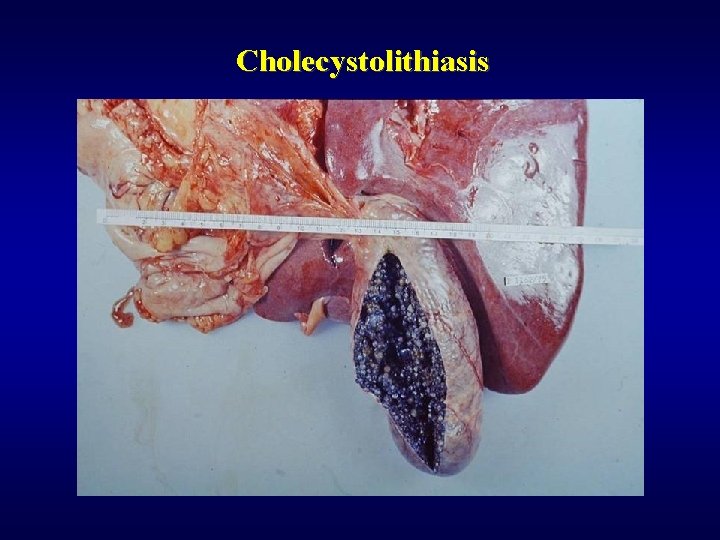
Cholecystolithiasis
Cholecystitis ü Acute • empyema of gallbladder • gangrenous cholecystitis • acalculous cholecystitis (postoperative, trauma, burns, sepsis, …) ü Chronic • fibroproduction (thickening of the wall, adhesion) • chronic inflammmation • dystrophic calcification (risk of carcinoma development) • hydrops
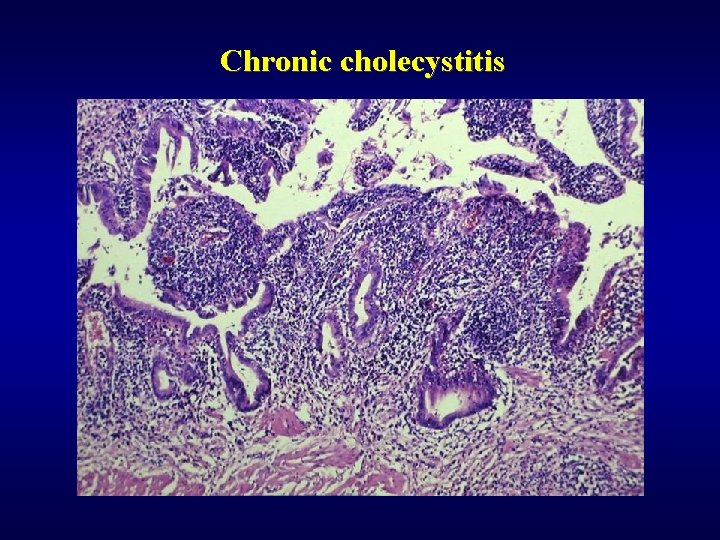
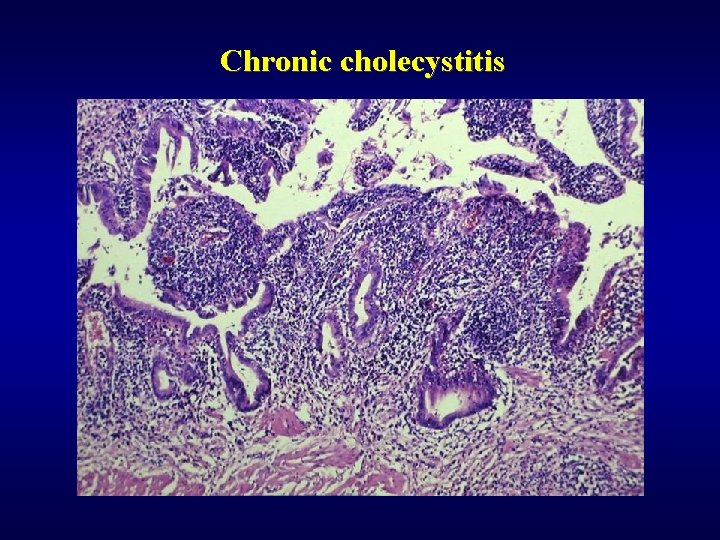
Chronic cholecystitis
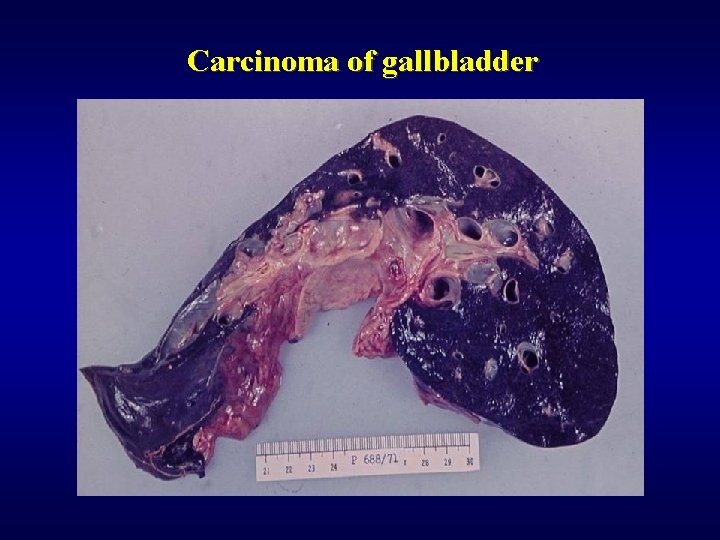
Carcinoma of gallbladder Adenocarcinoma ü Infiltrating ü Exophytic ü Early invasion into the liver – poor prognosis!
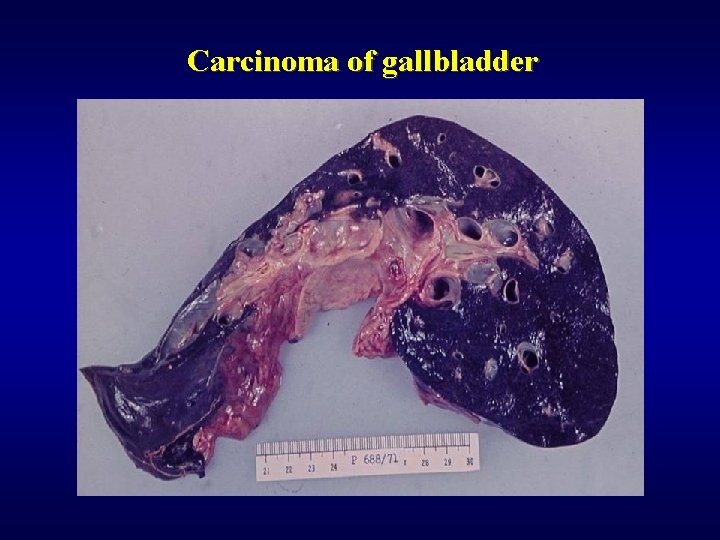
Carcinoma of gallbladder
Other disorders of biliary system ü Atresia of bile ducts (rapid progression, uncelar etiopathogenesis, cirrhosis) ü Cholesterolosis (strawberry gallbladder) ü Choledocholithiasis (risk of ascendent cholangoitis, intrahepatic abscess and sepsis, risk of biliary cirrhosis) ü Tumors of papilla Vateri (ampuloma, periampular carcinoma – difficult diagnosis)
Exocrine pancreas: acute pancreatitis ü • • • ü • • Causes cholelithiasis, alcohol, surgery, trauma, idiopathic Most serious form acute haemorrhagic necrotizing pancreatitis Morphology nekrosis of pancreas nekrosis of fat tissue (steatocytonecrosis, Balzer’s necrosis) haemorrhagy Complication, healing abscesses pseudocysts duodenal obstruction multiorgan failure
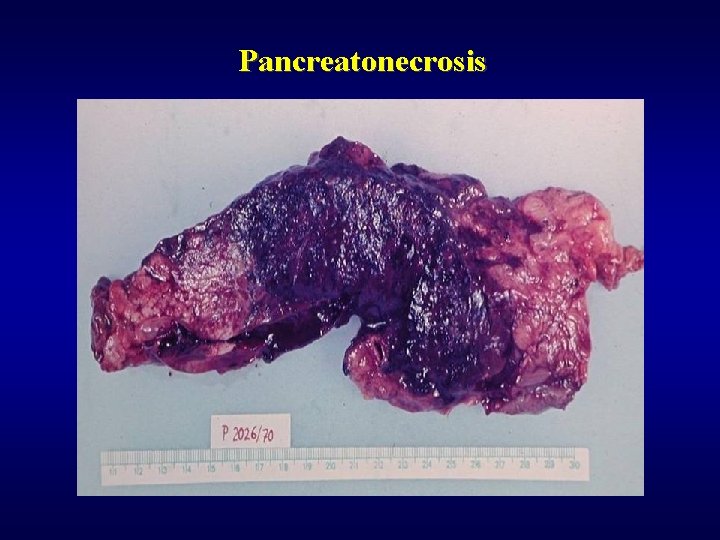
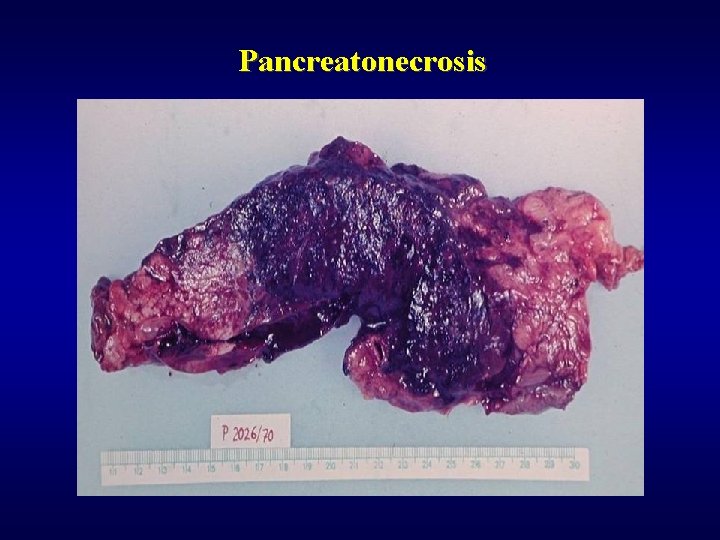
Pancreatonecrosis

Pancreatonecrosis

Steatocytonecrosis: omentum

Steatocytonecrosis: omentum
Exocrine pancreas: chronic pancreatitis ü • • ü • • Causes alcohol, hyperlipidemia, hypercalcemia, hereditary Morphology fibrosis reduction of acines obstruction of ducts chronic inflammatory infiltration (lymphocytes, plasmocytes) Complications calcifications, pseudocysts, thrombosis v. lienalis diabetes steatorrhea jaundice

Chronic pancreatitis
Exocrine pancreas: tumors ü Cystic tumors (5%) • mucinous cystadenoma • mucinous cystadenocarcinoma ü Carcinoma of pancreas • Adenocarcinoma, various degree of differentiation • Head (early diagnosis - jaundice), body, tail (difficult diagnosis, late detection) • Often - fibroproduction (dif. dg. chron. pancreatitis) • Trosseau syndrome – migratory thrombophlebitis in 10%

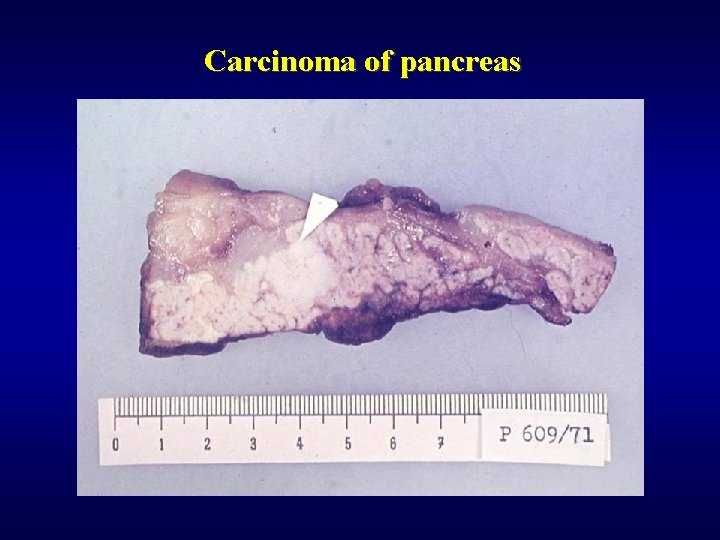
Carcinoma of pancreas
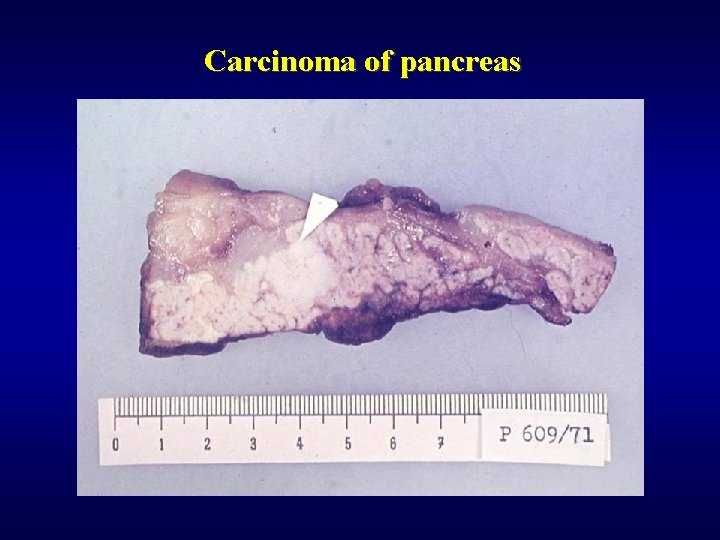
Carcinoma of pancreas

http: //ustavpatologie. upol. cz