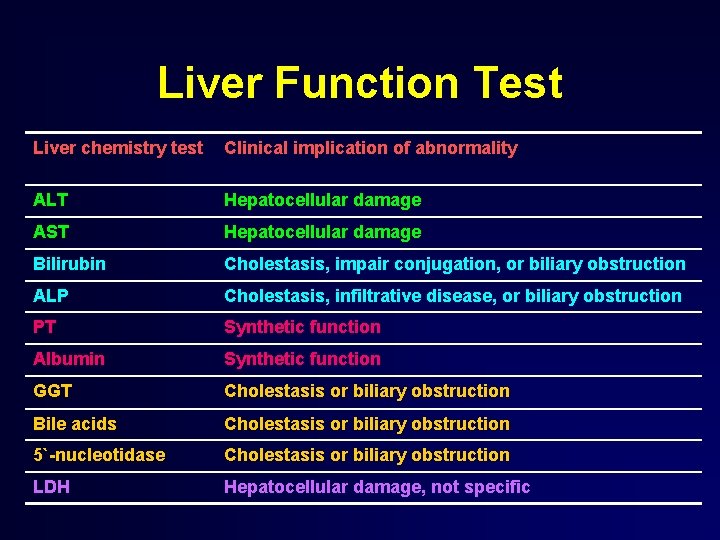
Liver Function Test Liver chemistry test Clinical implication



- Slides: 87

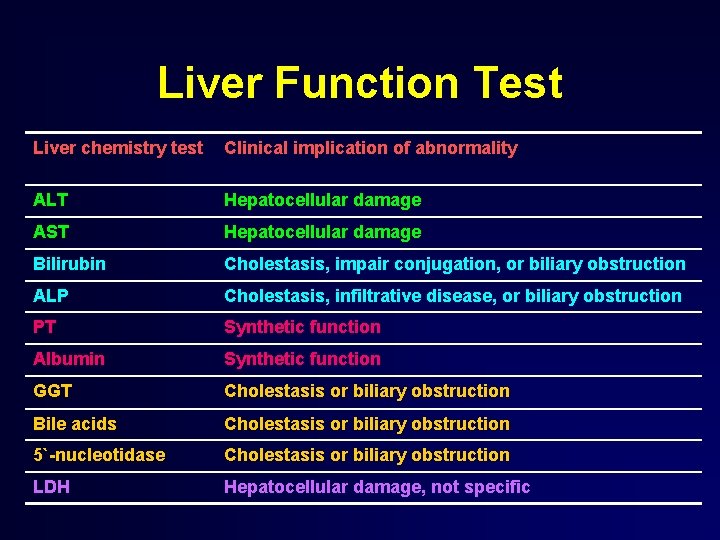
Liver Function Test Liver chemistry test Clinical implication of abnormality ALT Hepatocellular damage AST Hepatocellular damage Bilirubin Cholestasis, impair conjugation, or biliary obstruction ALP Cholestasis, infiltrative disease, or biliary obstruction PT Synthetic function Albumin Synthetic function GGT Cholestasis or biliary obstruction Bile acids Cholestasis or biliary obstruction 5`-nucleotidase Cholestasis or biliary obstruction LDH Hepatocellular damage, not specific
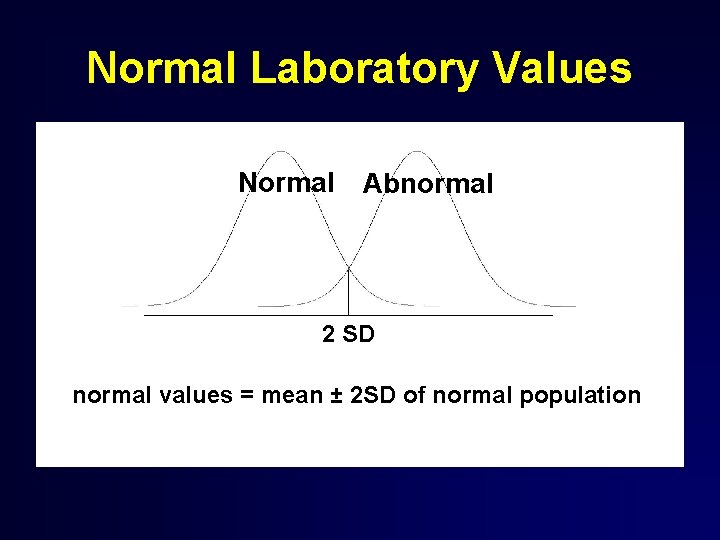
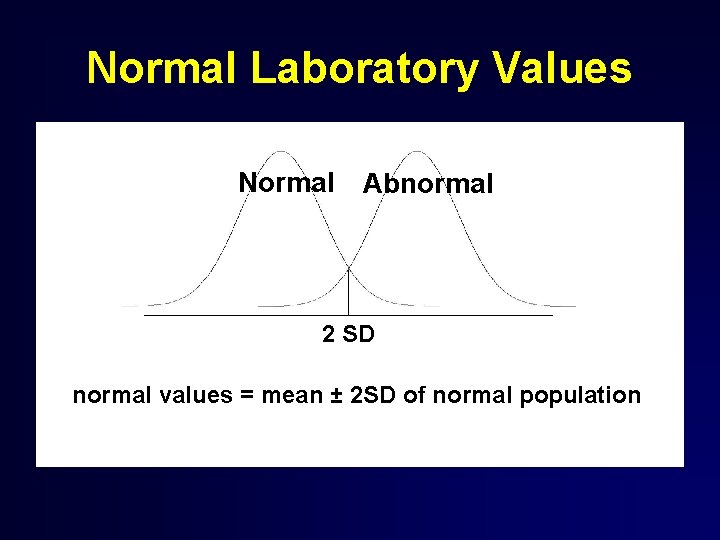
Normal Laboratory Values Normal Abnormal 2 SD normal values = mean ± 2 SD of normal population
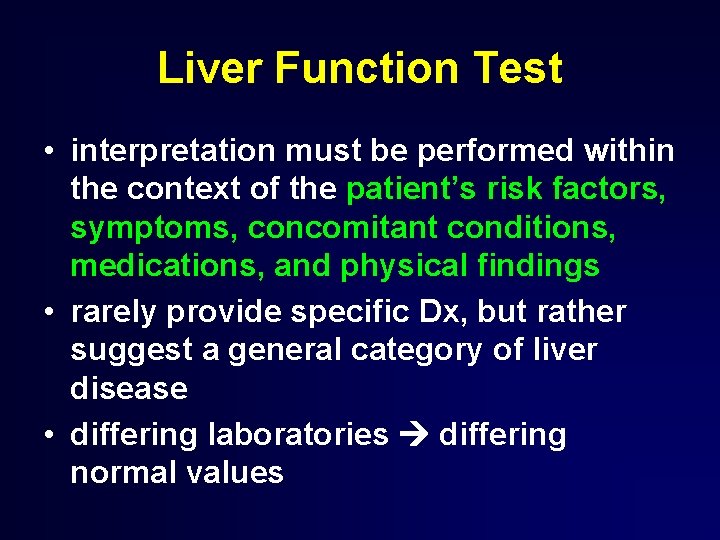
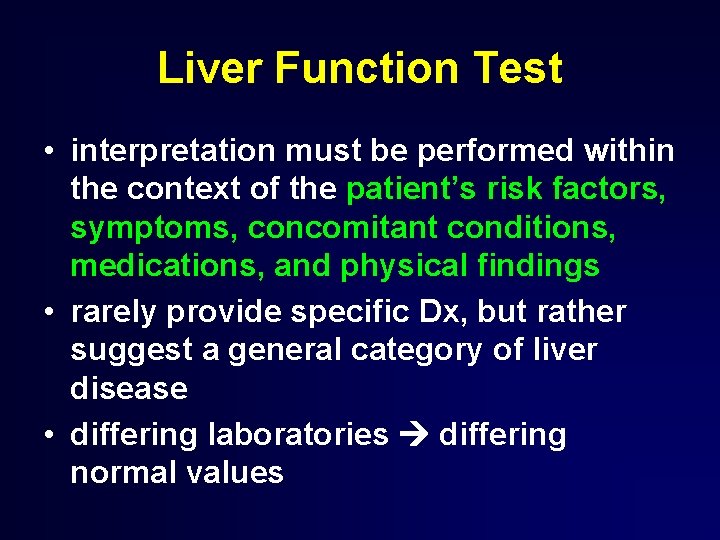
Liver Function Test • interpretation must be performed within the context of the patient’s risk factors, symptoms, concomitant conditions, medications, and physical findings • rarely provide specific Dx, but rather suggest a general category of liver disease • differing laboratories differing normal values
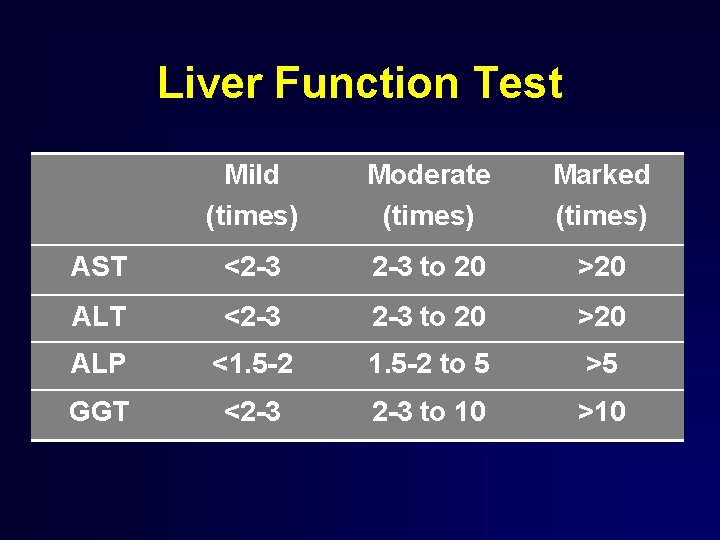
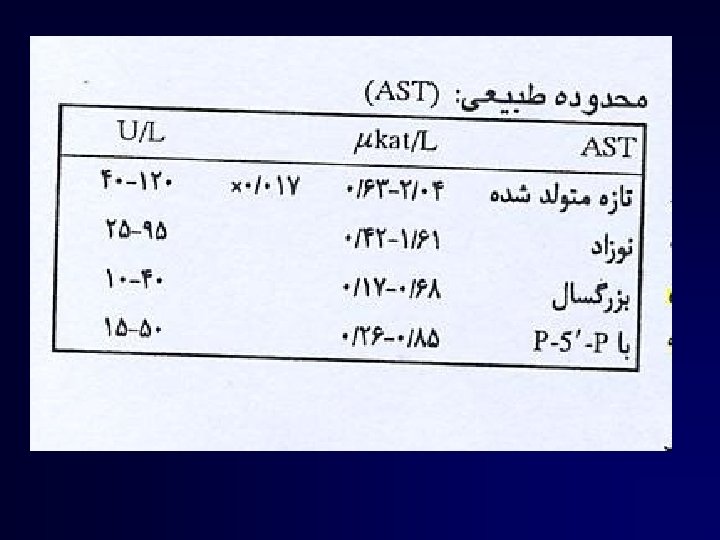
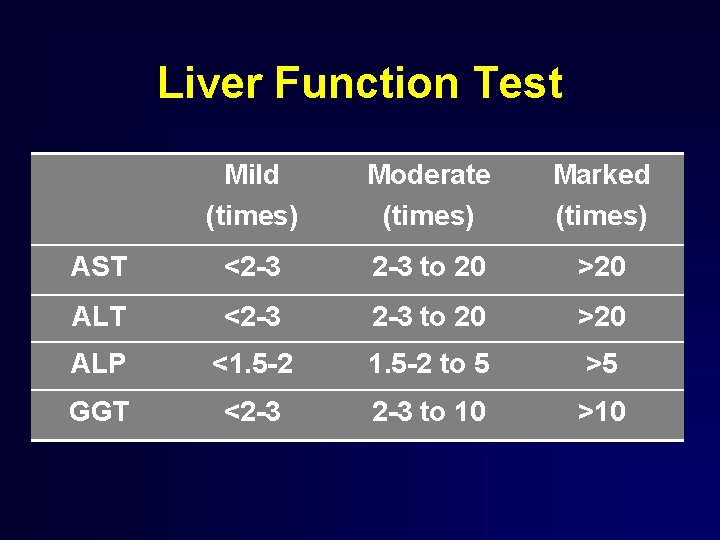
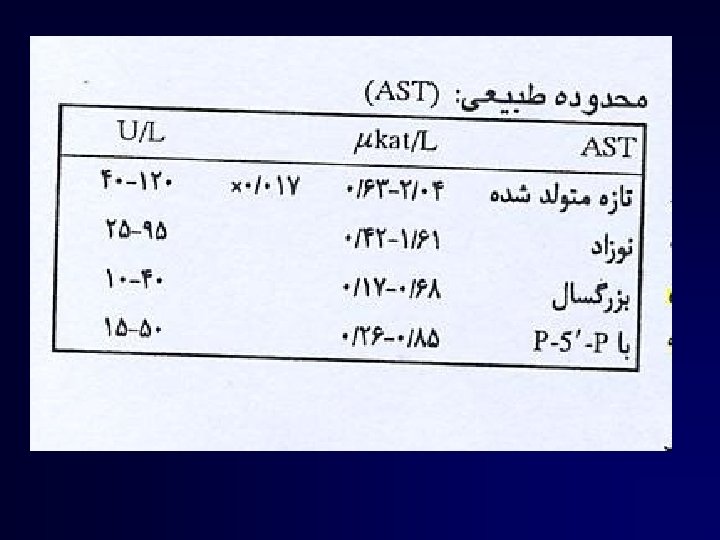
Liver Function Test Mild (times) Moderate (times) Marked (times) AST <2 -3 2 -3 to 20 >20 ALP <1. 5 -2 to 5 >5 GGT <2 -3 to 10 >10
Liver Function Test classified in 3 groups • synthetic function : albumin, PT • hepatocyte injury : AST, ALT • cholestasis : bilirubin, ALP, GGT PT, albumin, bilirubin-most common tests used as prognostic factors
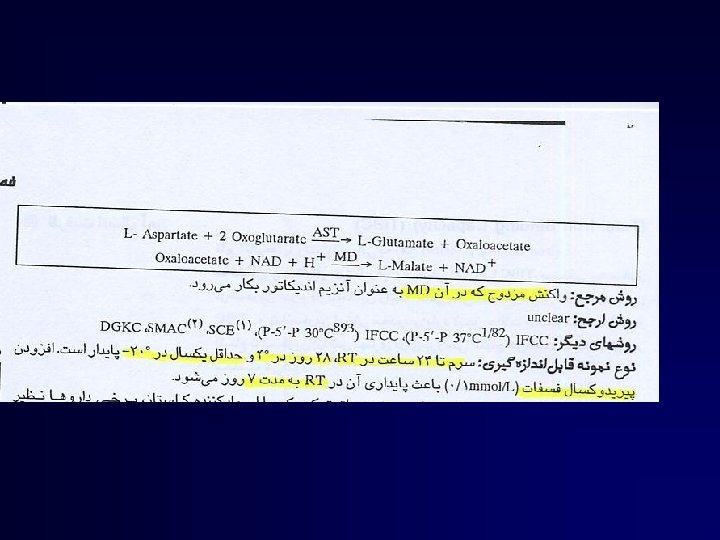
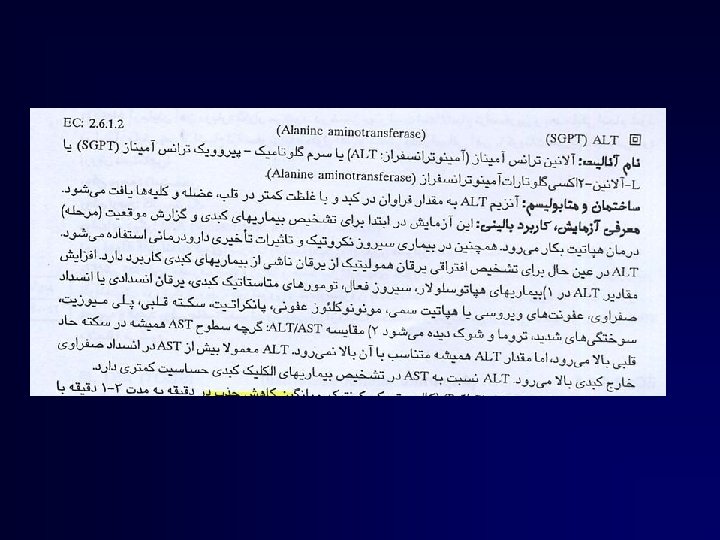
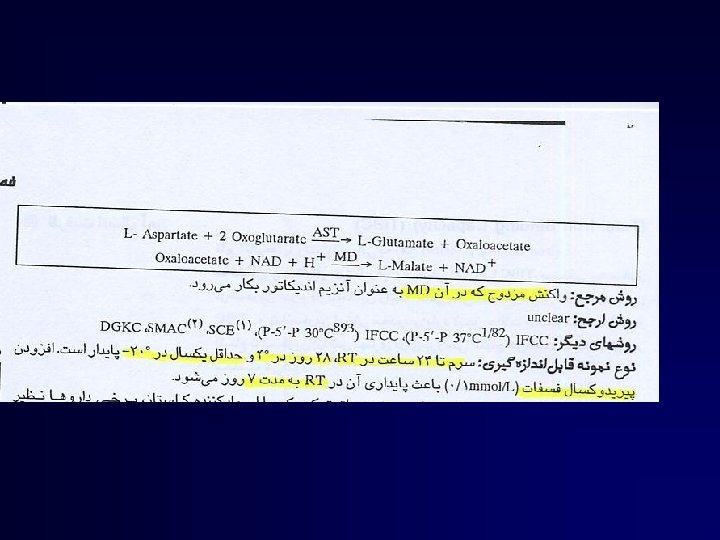
AST and ALT
AST and ALT • most frequent used markers of hepatocellular necrosis, but not correlate with eventual outcome • decrease : recovery or poor prognosis – poor prognosis : rapid fall with rising of bilirubin and PT
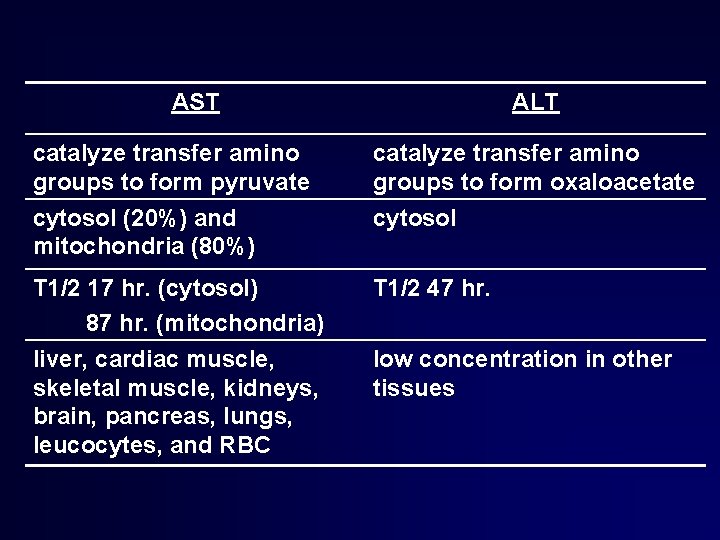
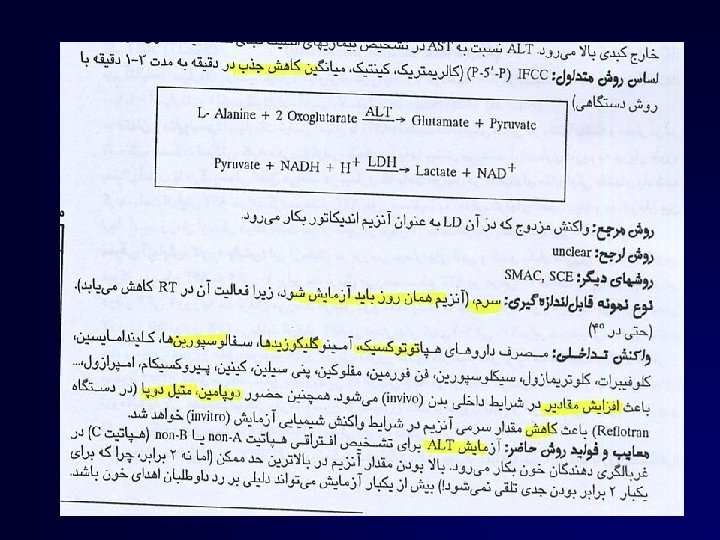
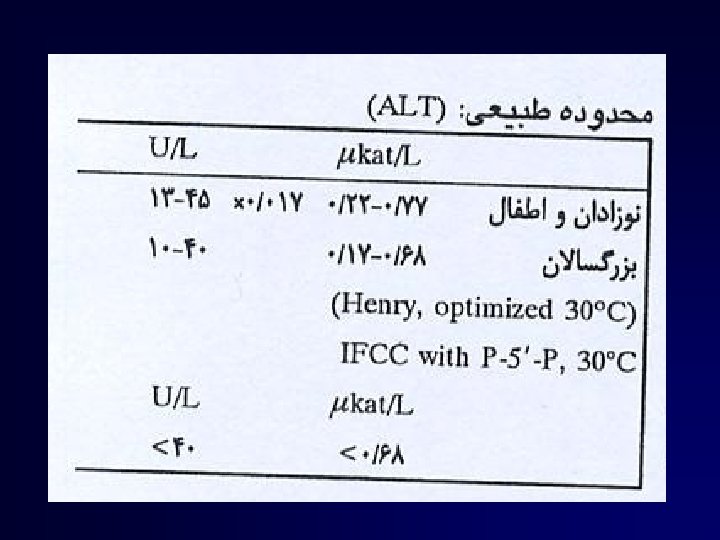
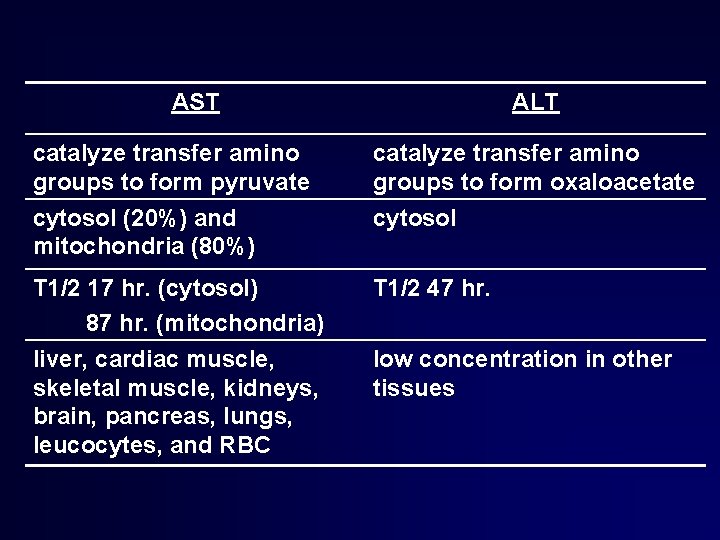
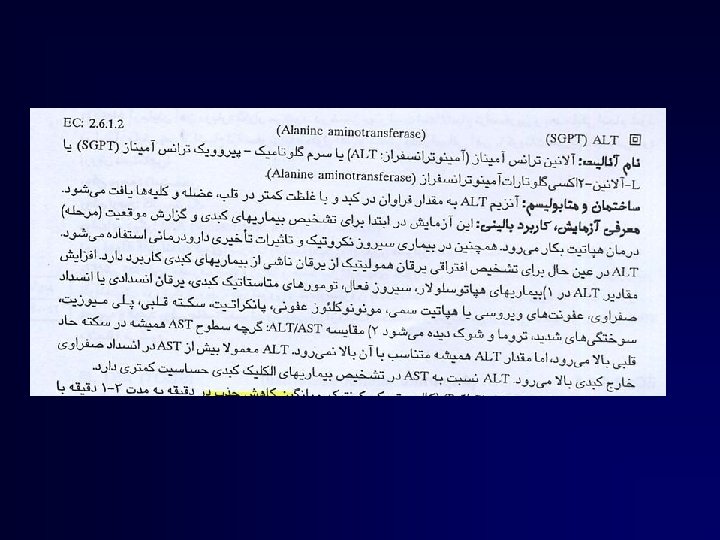
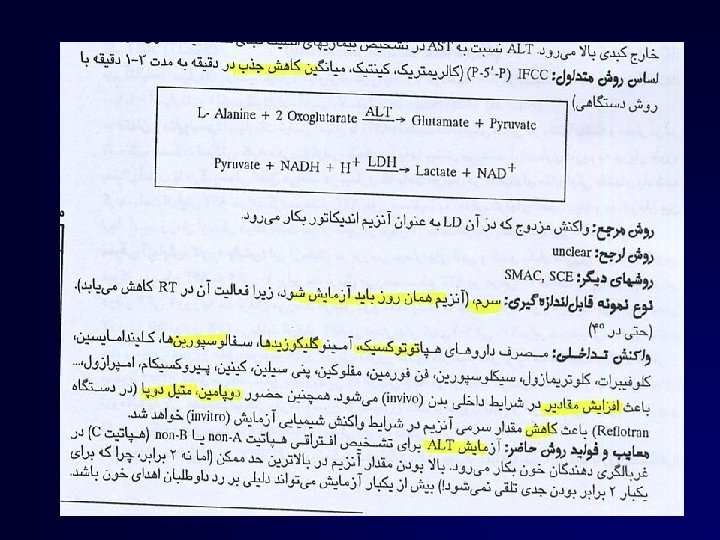
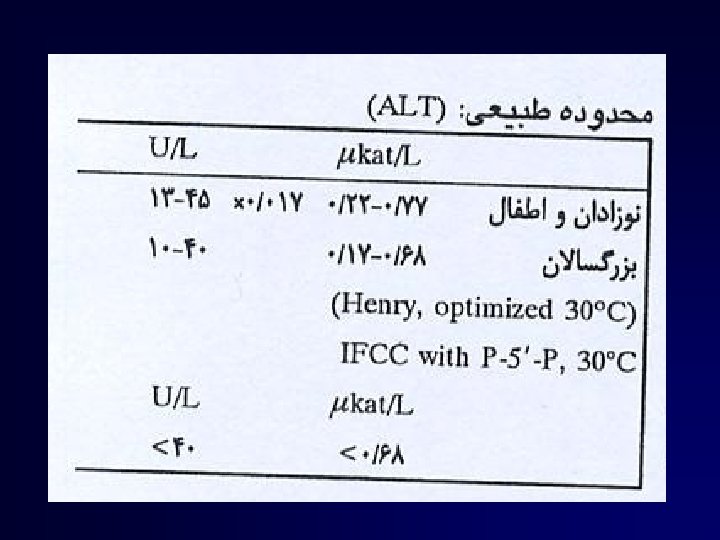
AST ALT catalyze transfer amino groups to form pyruvate catalyze transfer amino groups to form oxaloacetate cytosol (20%) and mitochondria (80%) cytosol T 1/2 17 hr. (cytosol) 87 hr. (mitochondria) liver, cardiac muscle, skeletal muscle, kidneys, brain, pancreas, lungs, leucocytes, and RBC T 1/2 47 hr. low concentration in other tissues
AST, ALT • level of transminase elevation • predominant AST elevation • rate of transaminase declination
• Peak values of transaminase activity occur between the 7 th and l 2 th days; • activities then gradually decreaser, e aching normal levelsb ythe 3 rd to 5 th week if recovery is uneventful • Persistenceo f increased A LT for more than 6 months after an episode of acute hepatitis is used to diagnose chronic hepatitis
• After AMI, increased AST activity appears in serum, as might be expected from the high AST concentration in heart muscle. AST activity also is increased in progressive muscu-
• The ratio seems to clearly identify the livercell "necrotic type" condition (i'e'' slight enzyme increase concomitant with relatively high activities of mitochondrial enzymes), typical of alcoholic hepatitis
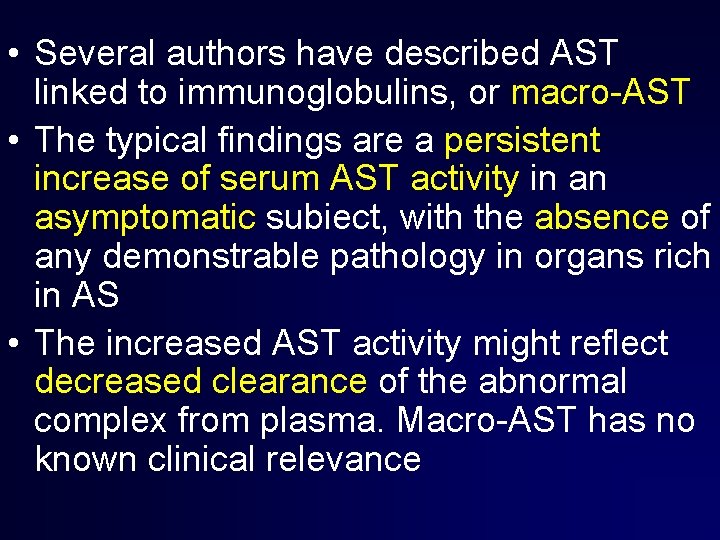
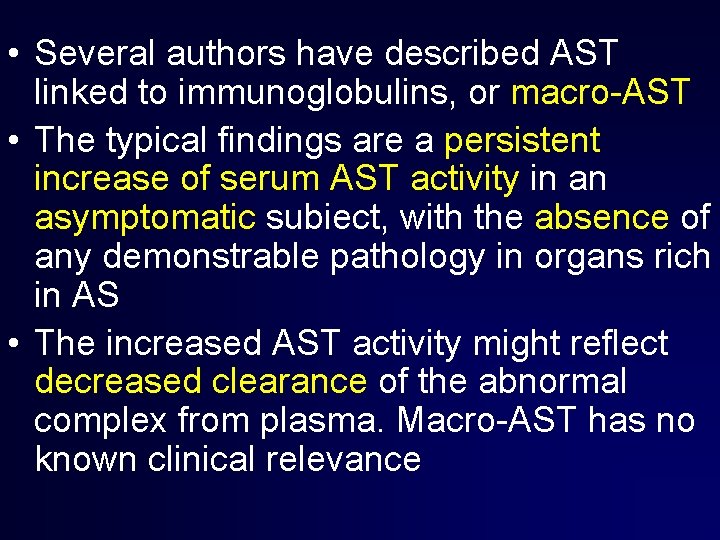
• Several authors have described AST linked to immunoglobulins, or macro-AST • The typical findings are a persistent increase of serum AST activity in an asymptomatic subiect, with the absence of any demonstrable pathology in organs rich in AS • The increased AST activity might reflect decreased clearance of the abnormal complex from plasma. Macro-AST has no known clinical relevance
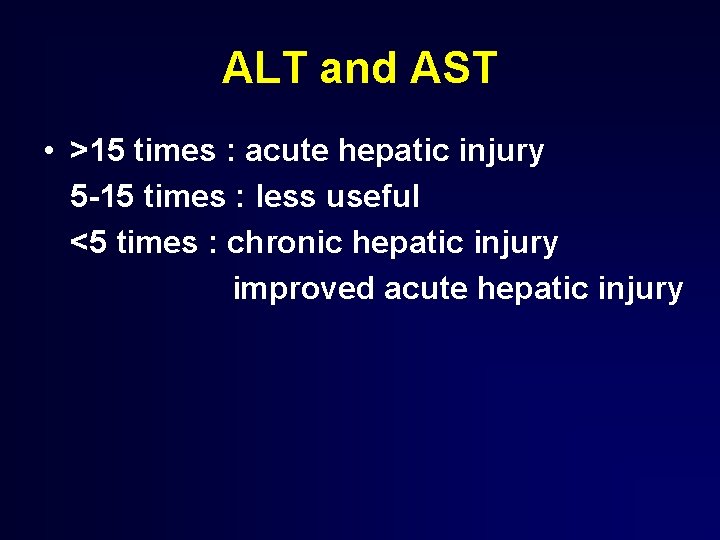
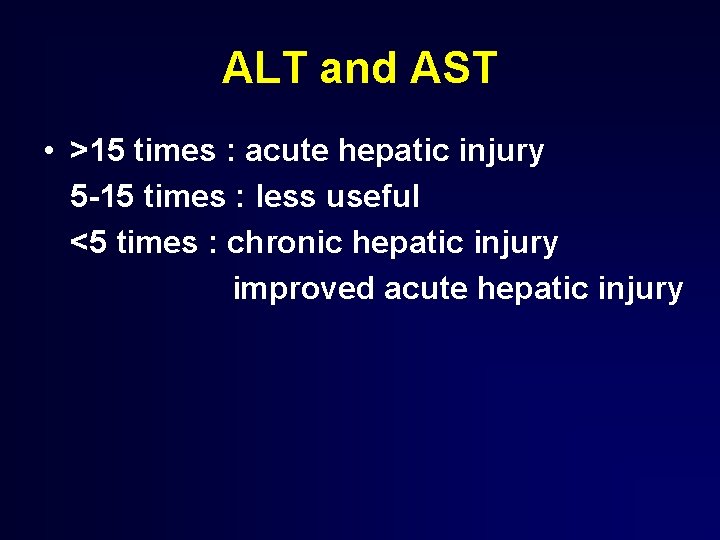
ALT and AST • >15 times : acute hepatic injury 5 -15 times : less useful <5 times : chronic hepatic injury improved acute hepatic injury
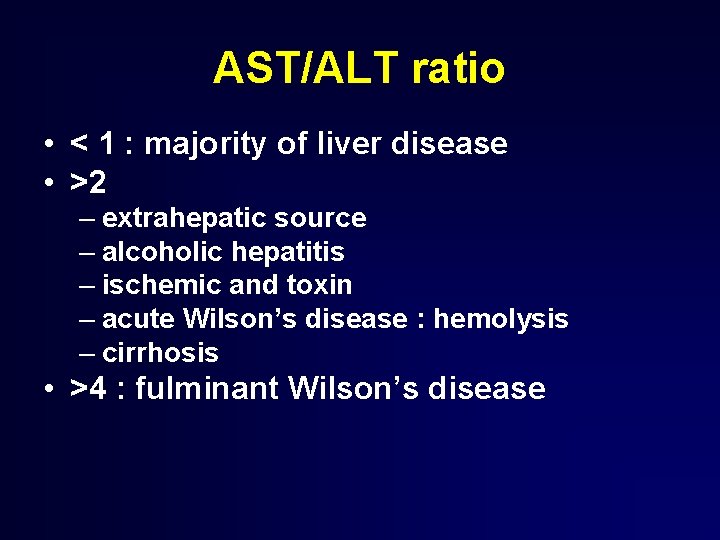
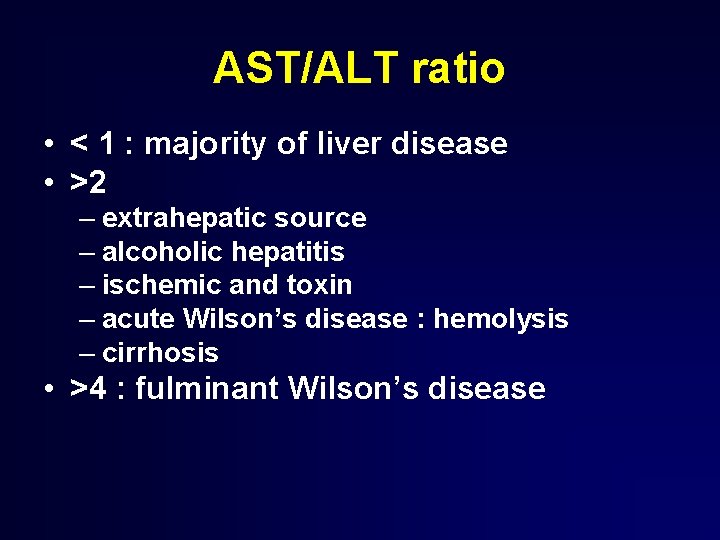
AST/ALT ratio • < 1 : majority of liver disease • >2 – extrahepatic source – alcoholic hepatitis – ischemic and toxin – acute Wilson’s disease : hemolysis – cirrhosis • >4 : fulminant Wilson’s disease
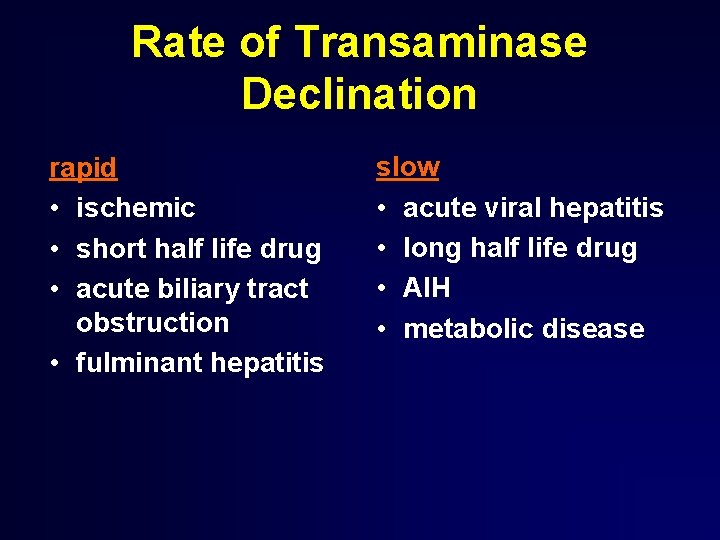
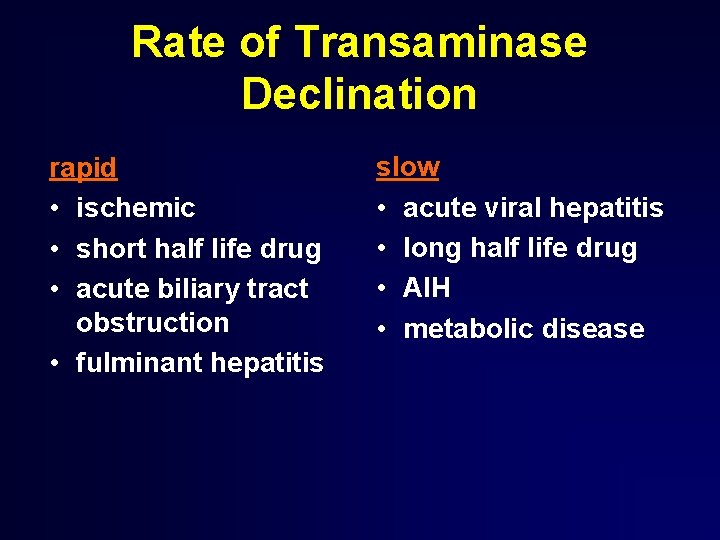
Rate of Transaminase Declination rapid • ischemic • short half life drug • acute biliary tract obstruction • fulminant hepatitis slow • acute viral hepatitis • long half life drug • AIH • metabolic disease
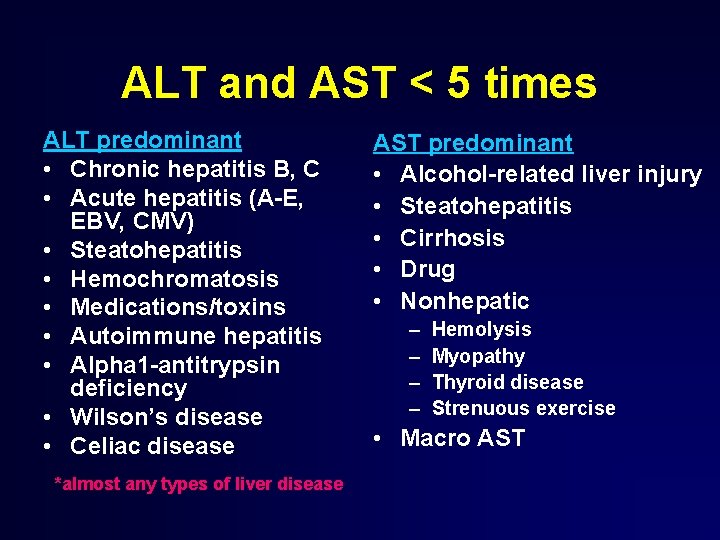
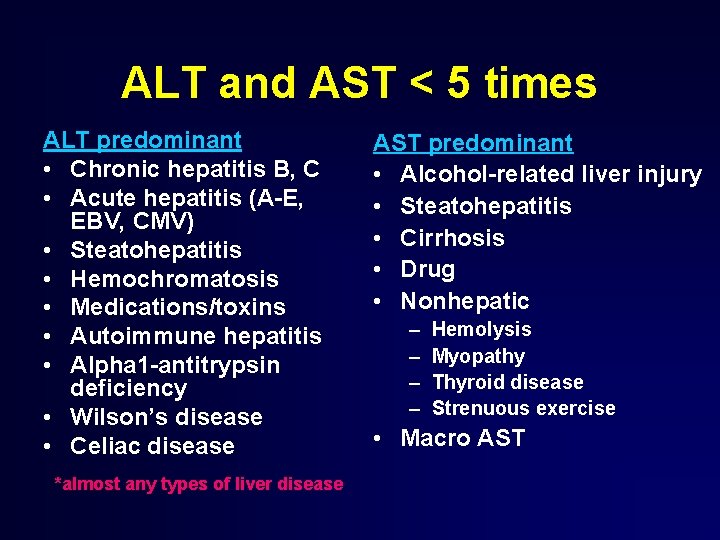
ALT and AST < 5 times ALT predominant • Chronic hepatitis B, C • Acute hepatitis (A-E, EBV, CMV) • Steatohepatitis • Hemochromatosis • Medications/toxins • Autoimmune hepatitis • Alpha 1 -antitrypsin deficiency • Wilson’s disease • Celiac disease *almost any types of liver disease AST predominant • Alcohol-related liver injury • Steatohepatitis • Cirrhosis • Drug • Nonhepatic – – Hemolysis Myopathy Thyroid disease Strenuous exercise • Macro AST

Common medication • • Acetaminophen overdose Statins NSAIDs Antibiotics Antiepileptics Antituberculosis drugs Herbal remedies, alternative medications and substance abuse
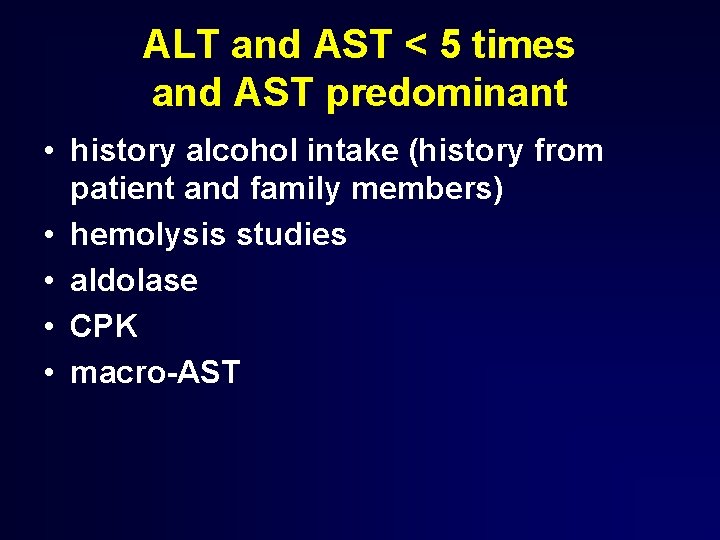
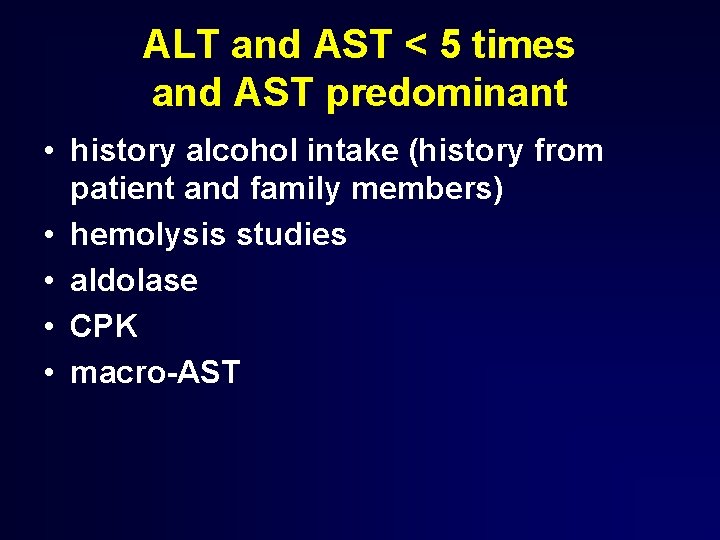
ALT and AST < 5 times and AST predominant • history alcohol intake (history from patient and family members) • hemolysis studies • aldolase • CPK • macro-AST
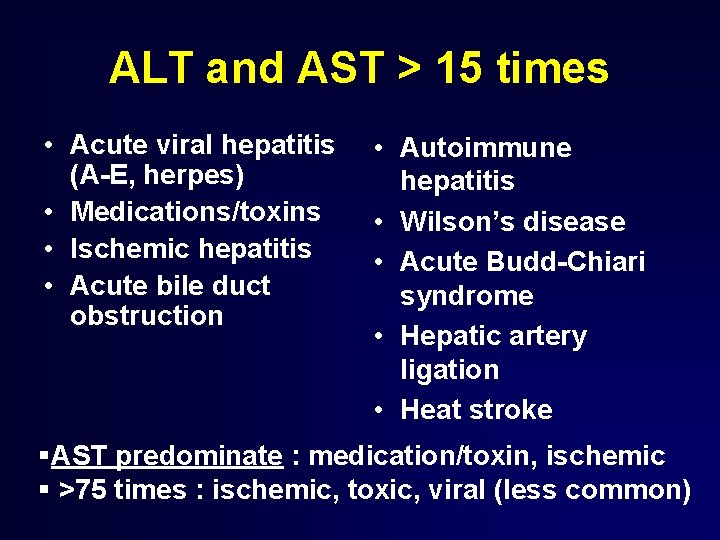
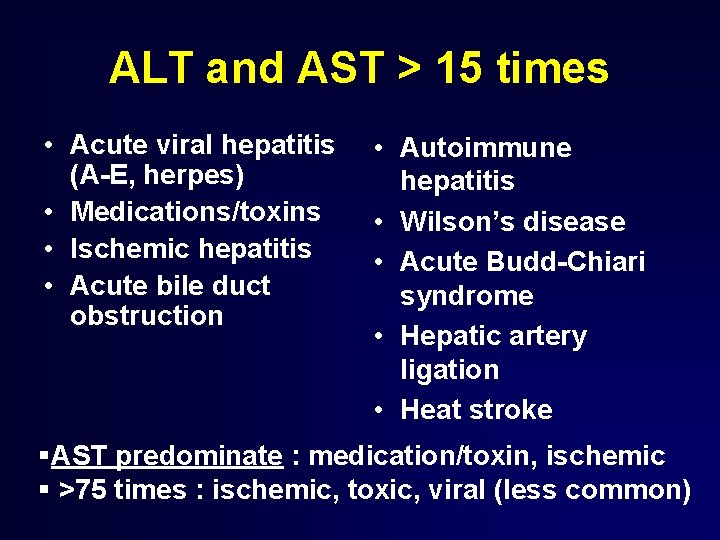
ALT and AST > 15 times • Acute viral hepatitis (A-E, herpes) • Medications/toxins • Ischemic hepatitis • Acute bile duct obstruction • Autoimmune hepatitis • Wilson’s disease • Acute Budd-Chiari syndrome • Hepatic artery ligation • Heat stroke §AST predominate : medication/toxin, ischemic § >75 times : ischemic, toxic, viral (less common)
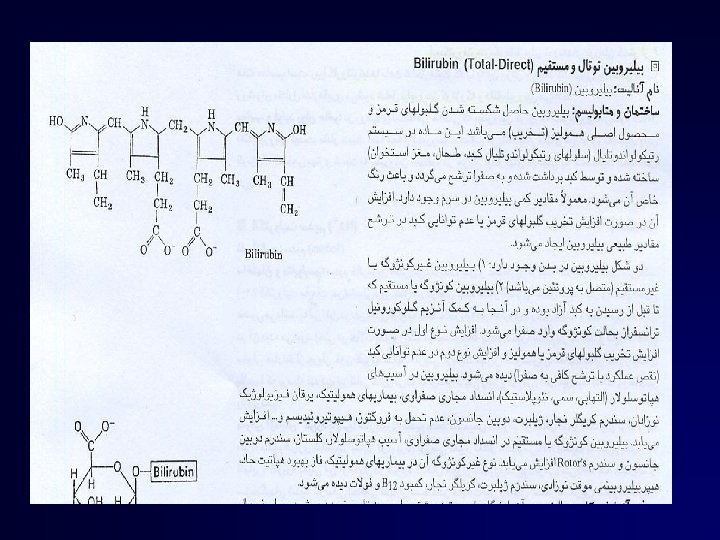
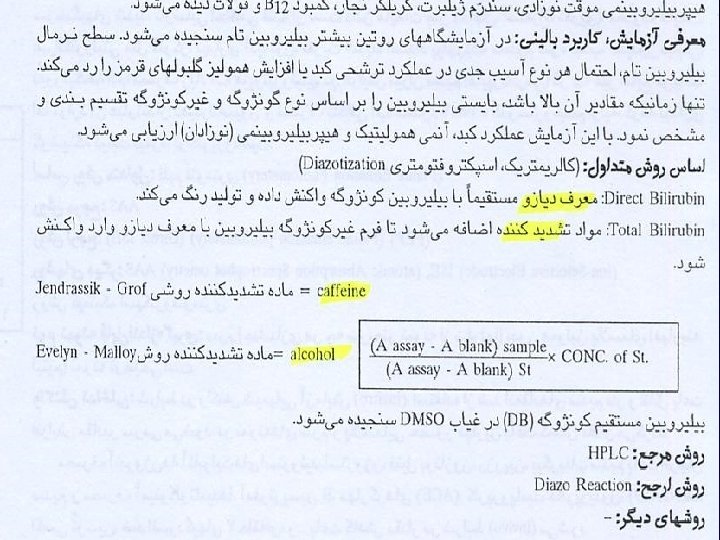
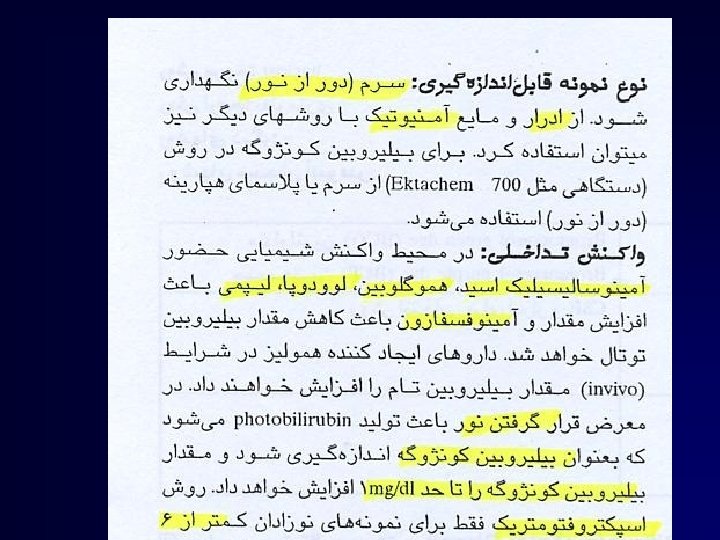
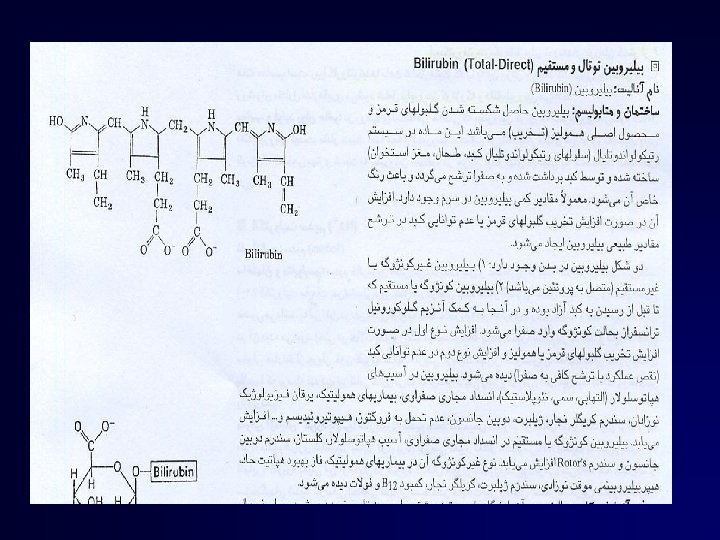
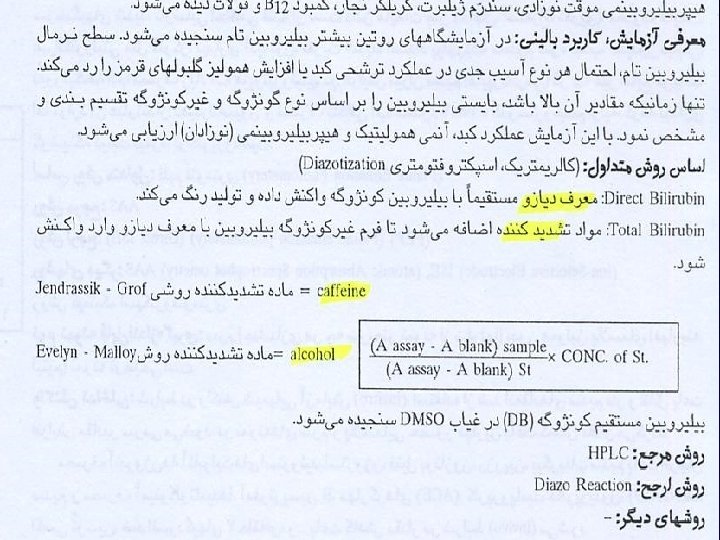
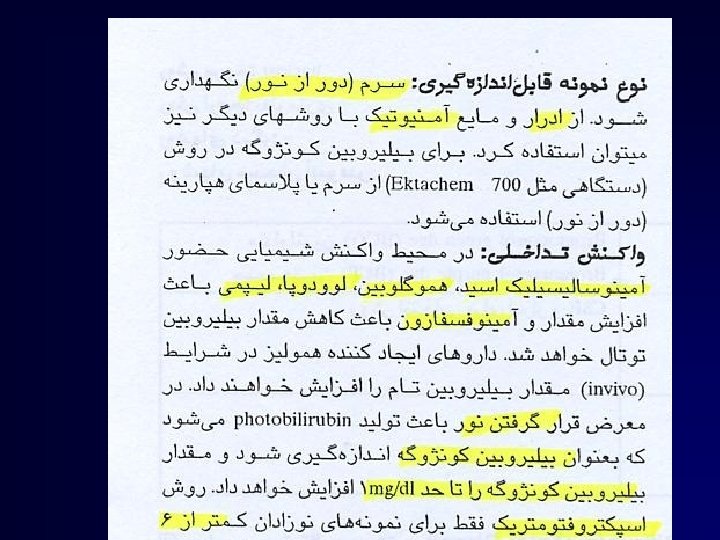
Bilirubin
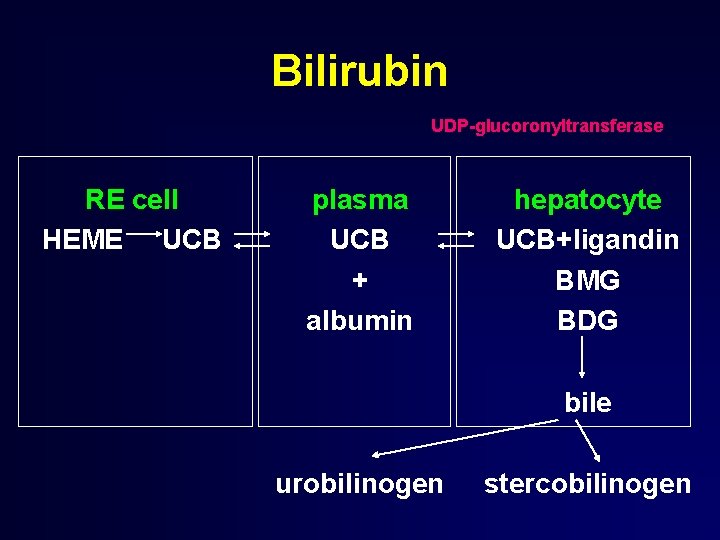
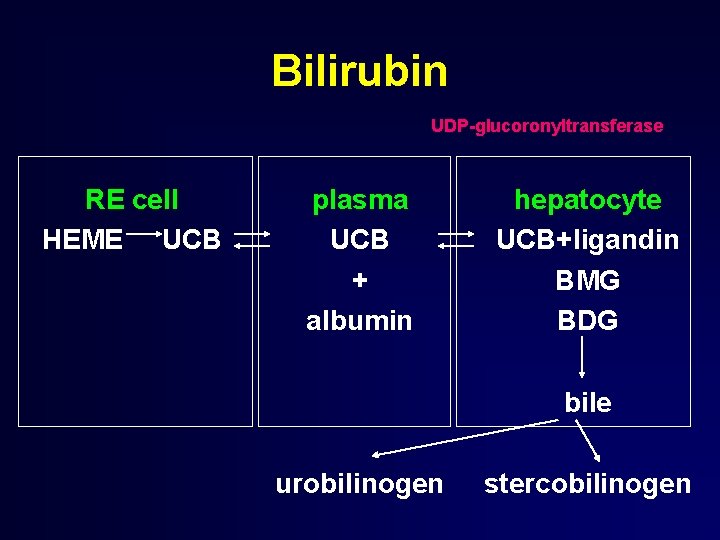
Bilirubin UDP-glucoronyltransferase RE cell HEME UCB plasma UCB + albumin hepatocyte UCB+ligandin BMG BDG bile urobilinogen stercobilinogen
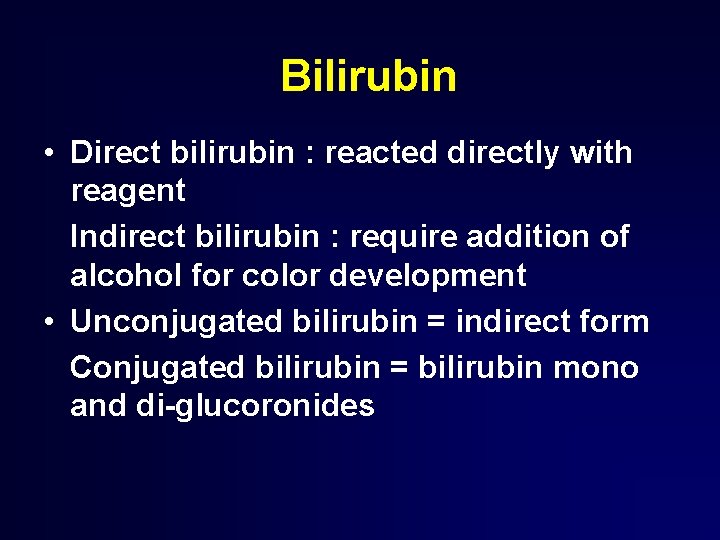
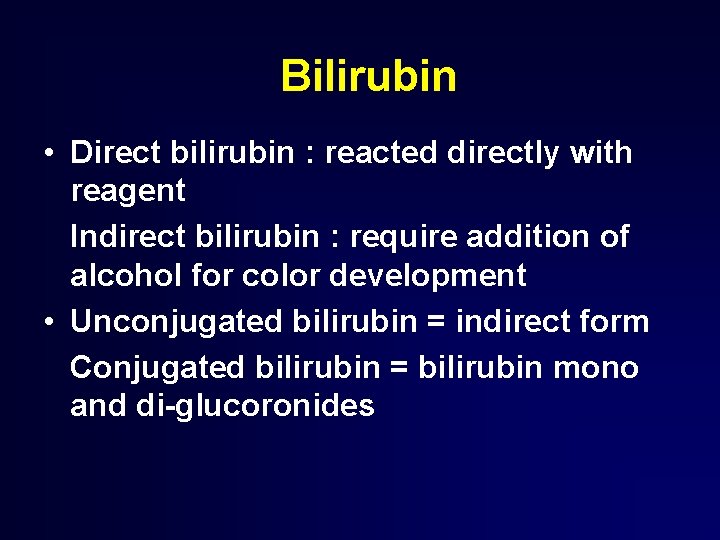
Bilirubin • Direct bilirubin : reacted directly with reagent Indirect bilirubin : require addition of alcohol for color development • Unconjugated bilirubin = indirect form Conjugated bilirubin = bilirubin mono and di-glucoronides
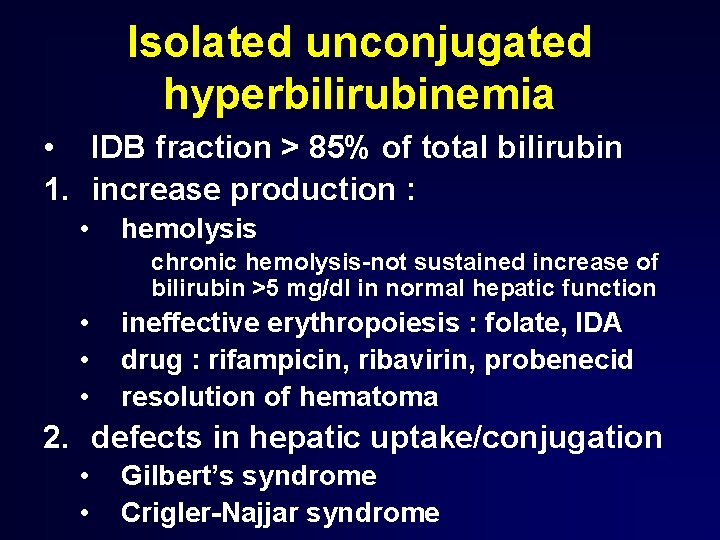
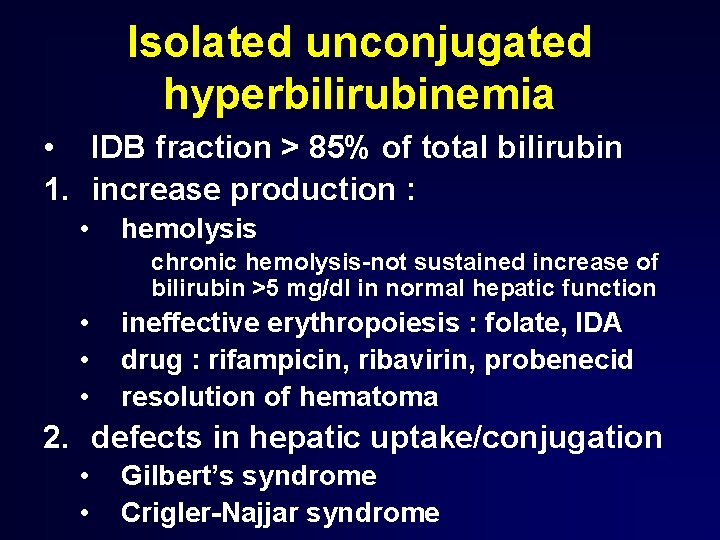
Isolated unconjugated hyperbilirubinemia • IDB fraction > 85% of total bilirubin 1. increase production : • hemolysis chronic hemolysis-not sustained increase of bilirubin >5 mg/dl in normal hepatic function • • • ineffective erythropoiesis : folate, IDA drug : rifampicin, ribavirin, probenecid resolution of hematoma 2. defects in hepatic uptake/conjugation • • Gilbert’s syndrome Crigler-Najjar syndrome
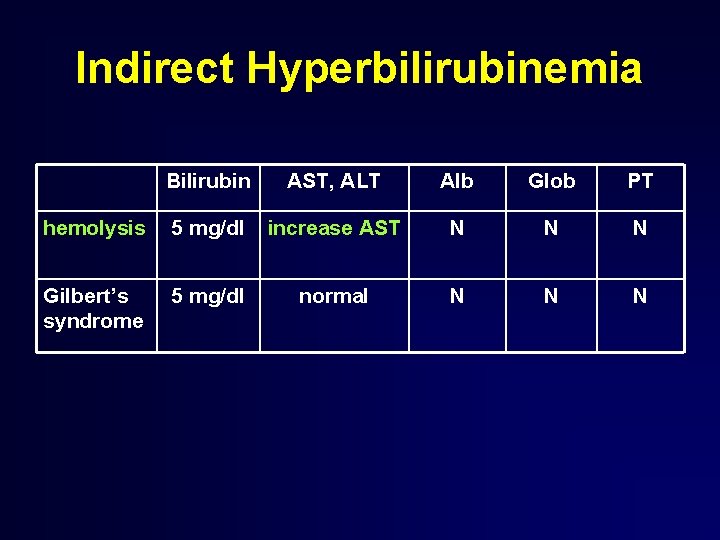
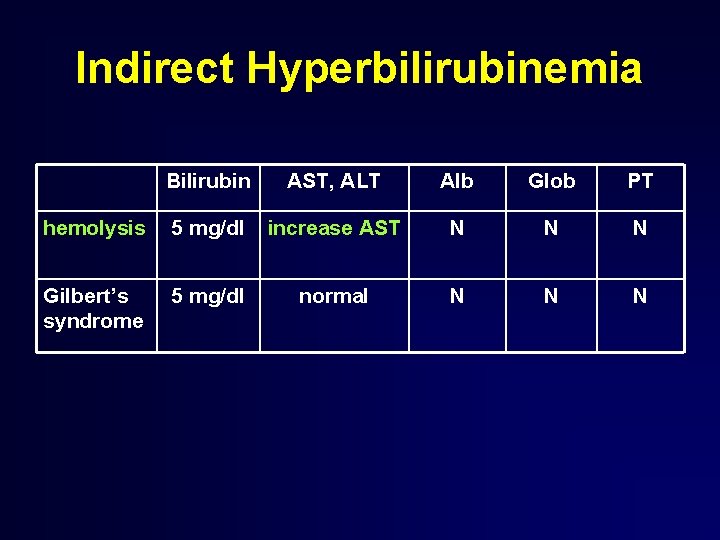
Indirect Hyperbilirubinemia Bilirubin AST, ALT Alb Glob PT hemolysis 5 mg/dl increase AST N N N Gilbert’s syndrome 5 mg/dl normal N N N
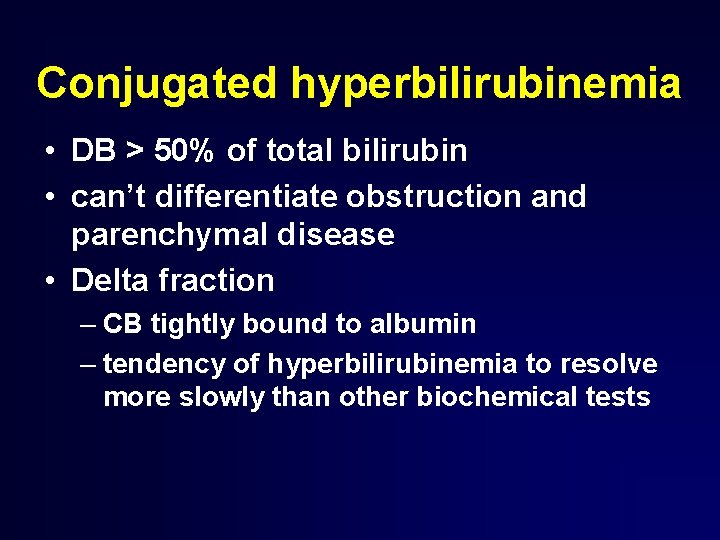
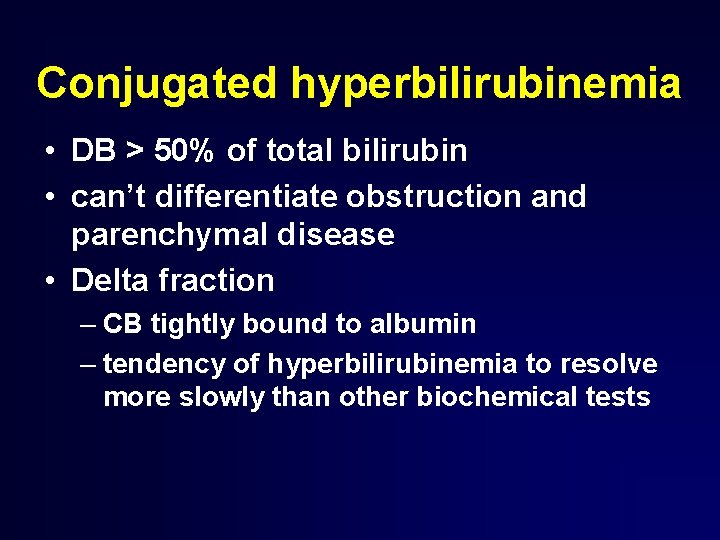
Conjugated hyperbilirubinemia • DB > 50% of total bilirubin • can’t differentiate obstruction and parenchymal disease • Delta fraction – CB tightly bound to albumin – tendency of hyperbilirubinemia to resolve more slowly than other biochemical tests
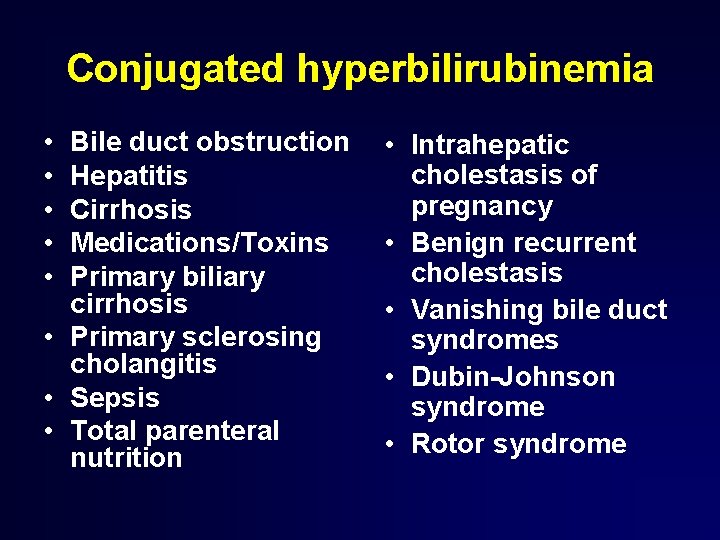
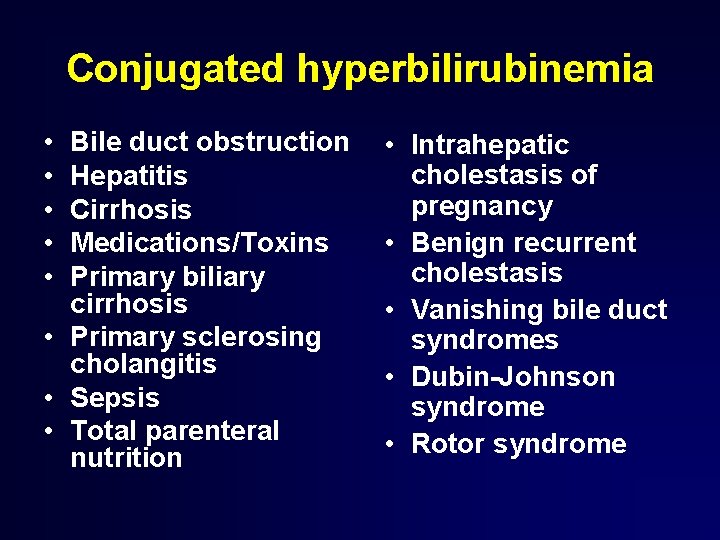
Conjugated hyperbilirubinemia • • • Bile duct obstruction Hepatitis Cirrhosis Medications/Toxins Primary biliary cirrhosis • Primary sclerosing cholangitis • Sepsis • Total parenteral nutrition • Intrahepatic cholestasis of pregnancy • Benign recurrent cholestasis • Vanishing bile duct syndromes • Dubin-Johnson syndrome • Rotor syndrome
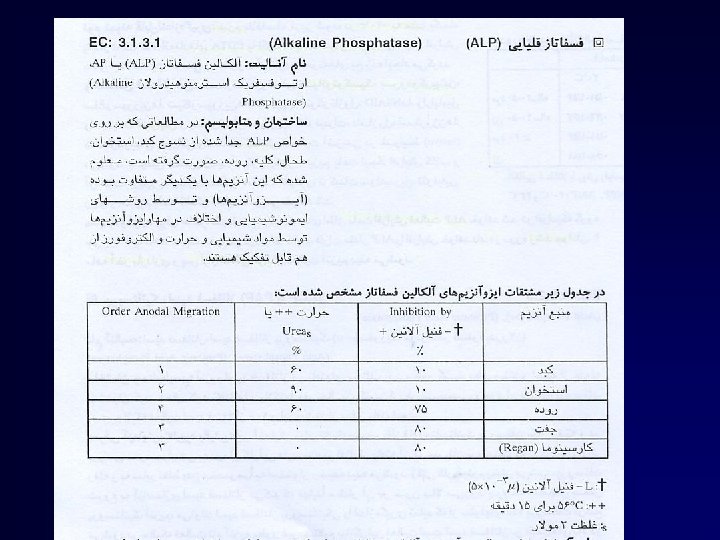
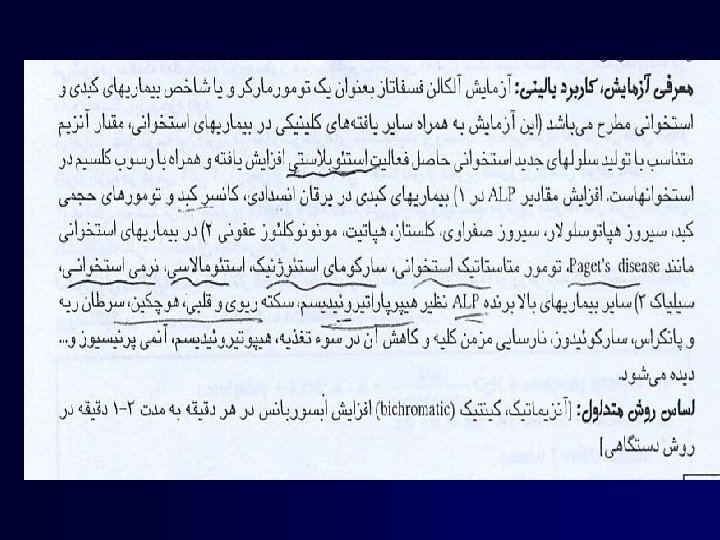
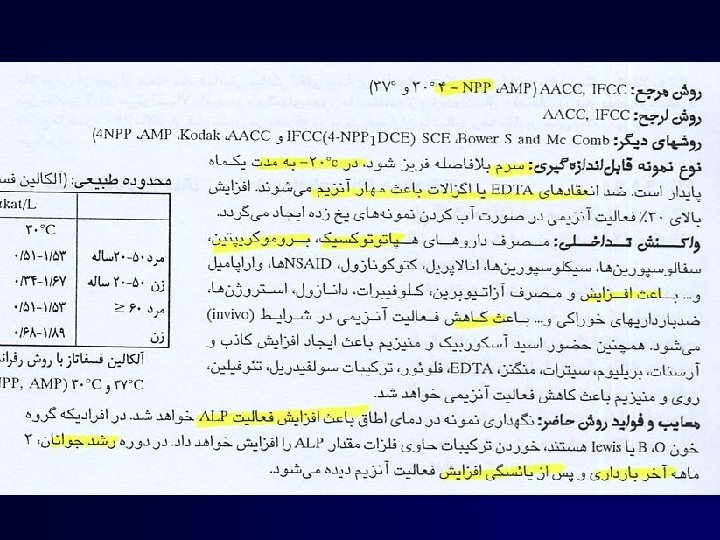
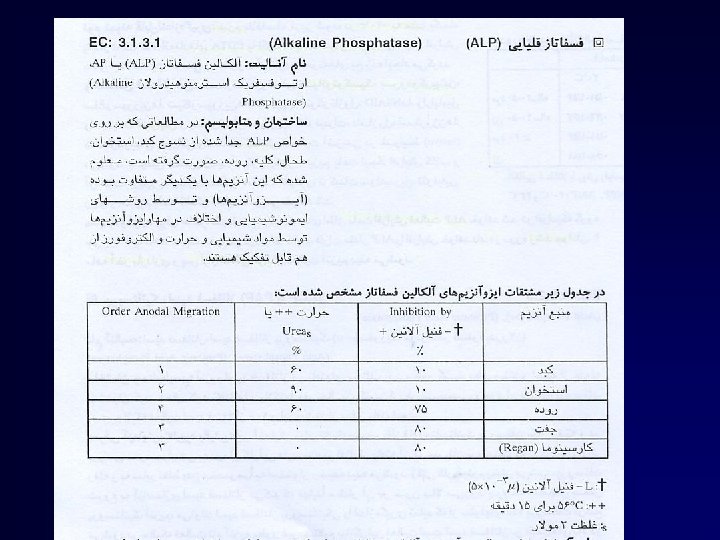
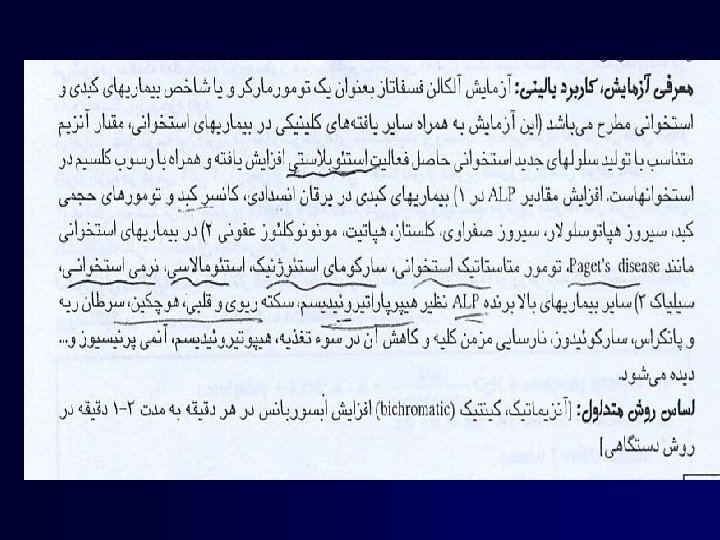
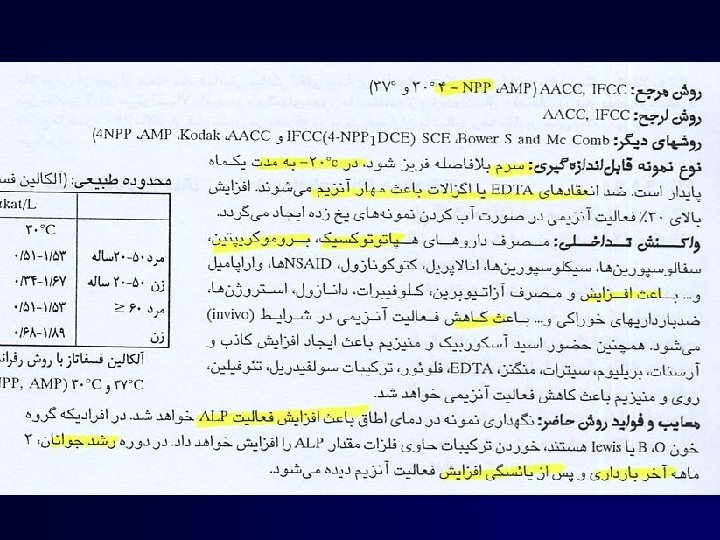
Alkaline phosphatase
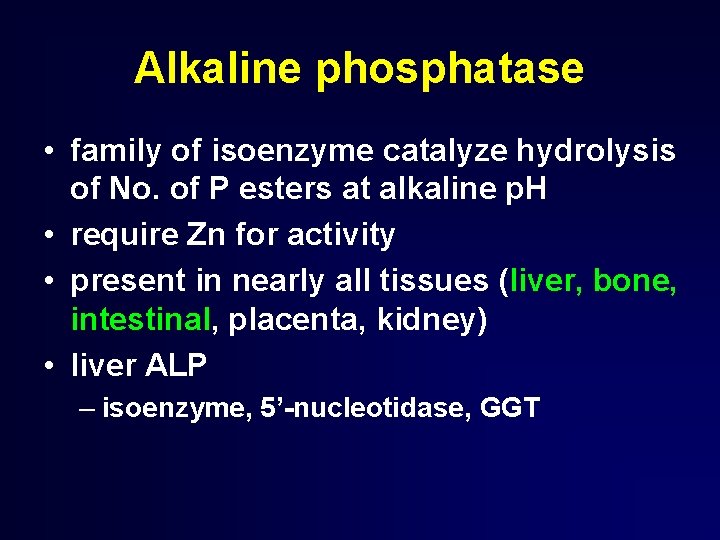
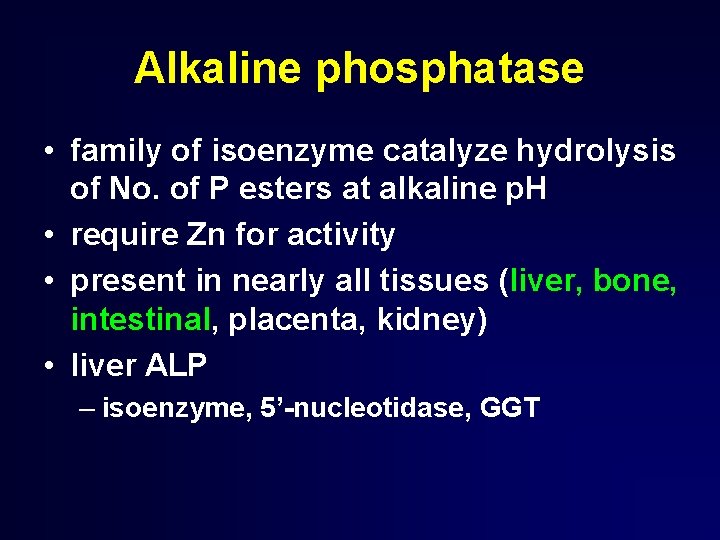
Alkaline phosphatase • family of isoenzyme catalyze hydrolysis of No. of P esters at alkaline p. H • require Zn for activity • present in nearly all tissues (liver, bone, intestinal, placenta, kidney) • liver ALP – isoenzyme, 5’-nucleotidase, GGT
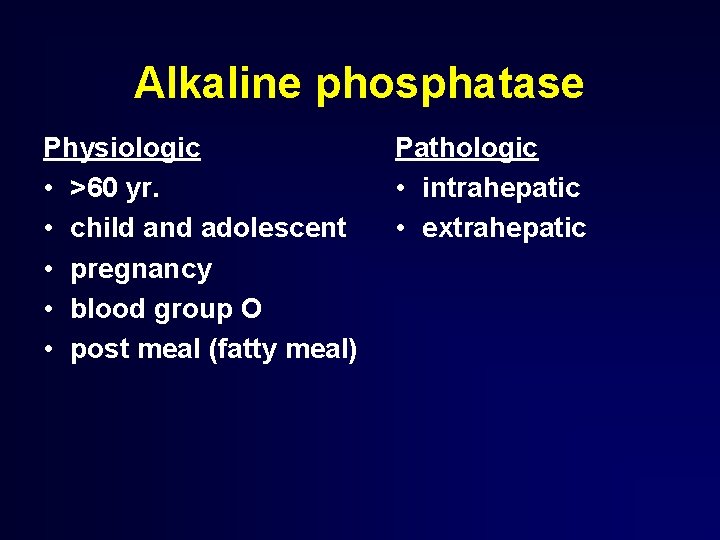
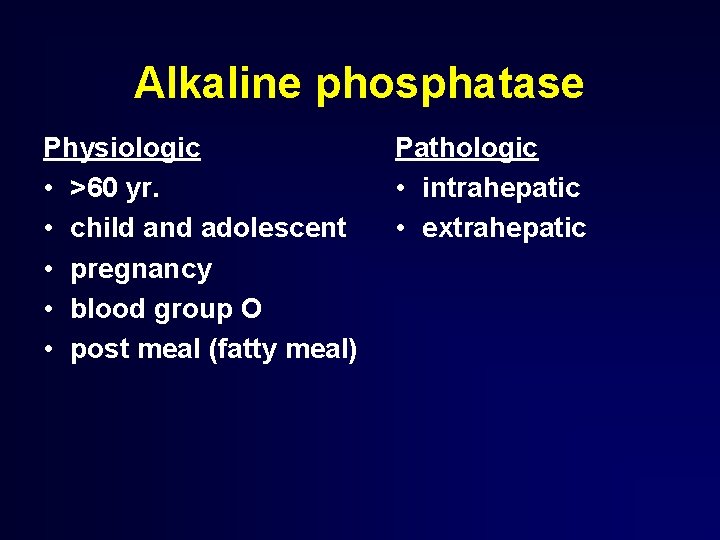
Alkaline phosphatase Physiologic • >60 yr. • child and adolescent • pregnancy • blood group O • post meal (fatty meal) Pathologic • intrahepatic • extrahepatic
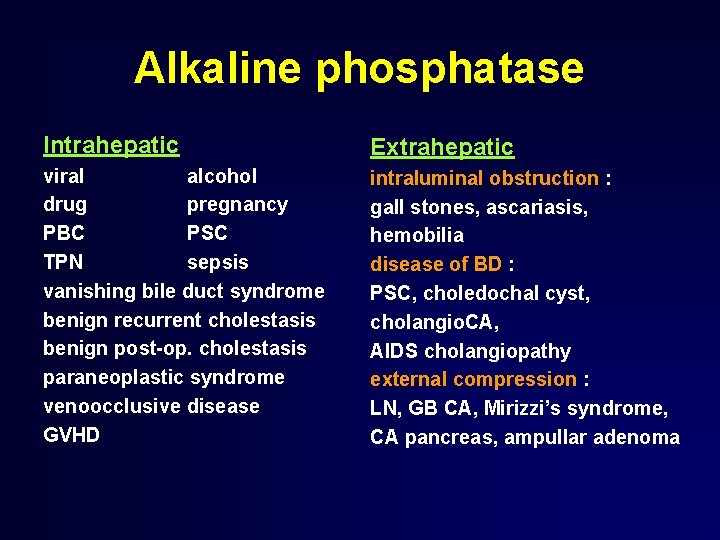
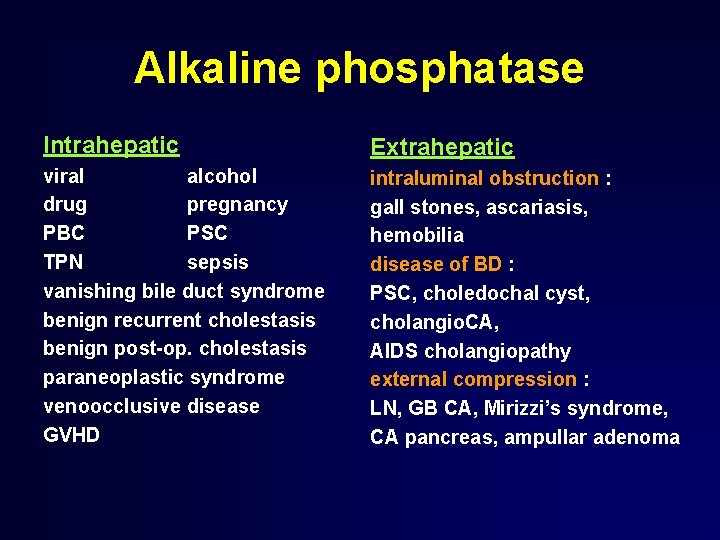
Alkaline phosphatase Intrahepatic Extrahepatic viral alcohol drug pregnancy PBC PSC TPN sepsis vanishing bile duct syndrome benign recurrent cholestasis benign post-op. cholestasis paraneoplastic syndrome venoocclusive disease GVHD intraluminal obstruction : gall stones, ascariasis, hemobilia disease of BD : PSC, choledochal cyst, cholangio. CA, AIDS cholangiopathy external compression : LN, GB CA, Mirizzi’s syndrome, CA pancreas, ampullar adenoma
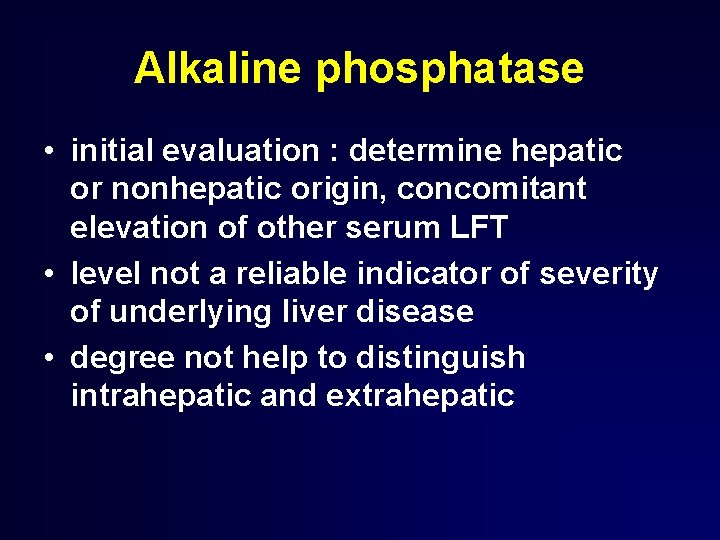
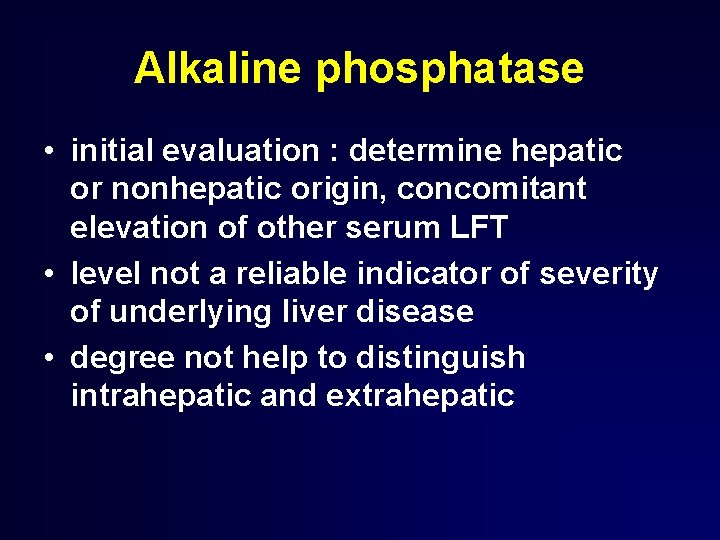
Alkaline phosphatase • initial evaluation : determine hepatic or nonhepatic origin, concomitant elevation of other serum LFT • level not a reliable indicator of severity of underlying liver disease • degree not help to distinguish intrahepatic and extrahepatic
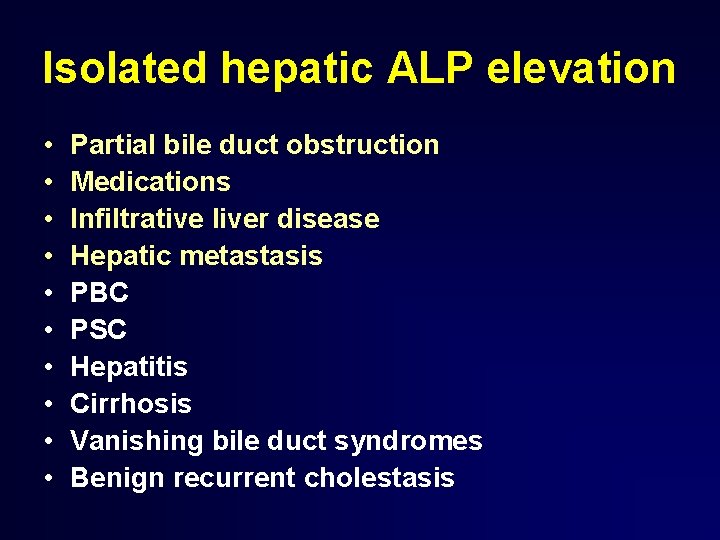
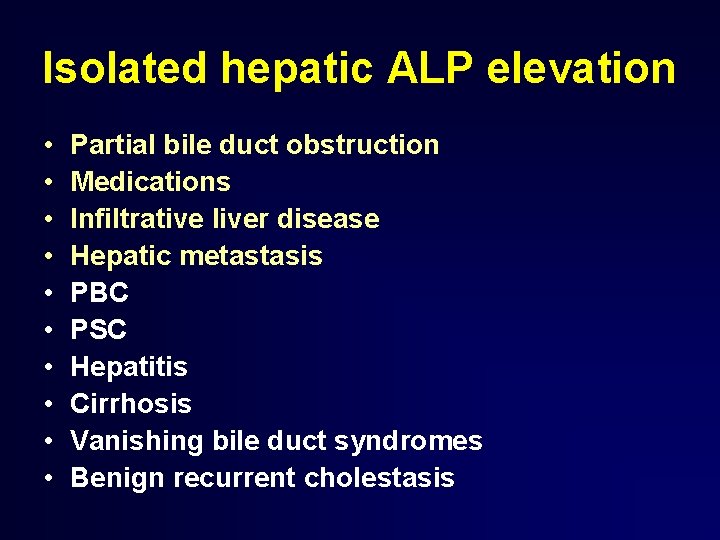
Isolated hepatic ALP elevation • • • Partial bile duct obstruction Medications Infiltrative liver disease Hepatic metastasis PBC PSC Hepatitis Cirrhosis Vanishing bile duct syndromes Benign recurrent cholestasis
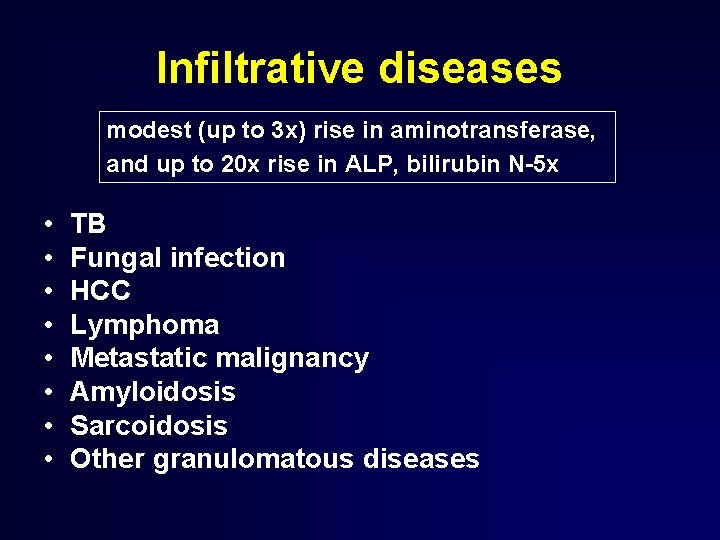
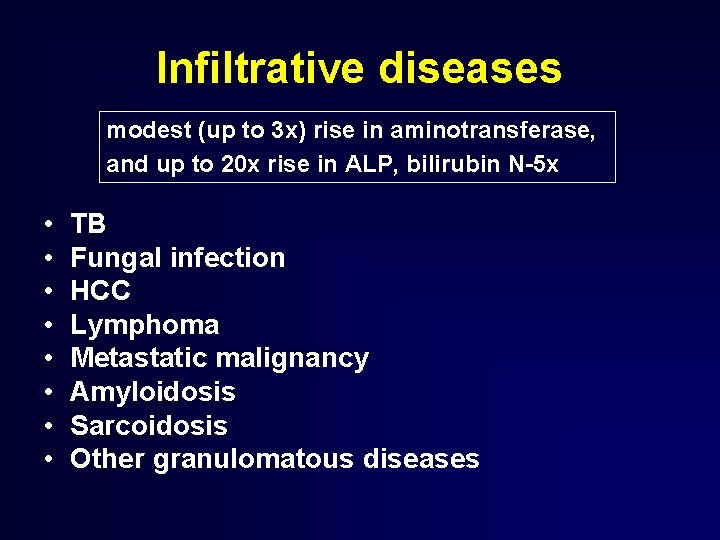
Infiltrative diseases modest (up to 3 x) rise in aminotransferase, and up to 20 x rise in ALP, bilirubin N-5 x • • TB Fungal infection HCC Lymphoma Metastatic malignancy Amyloidosis Sarcoidosis Other granulomatous diseases
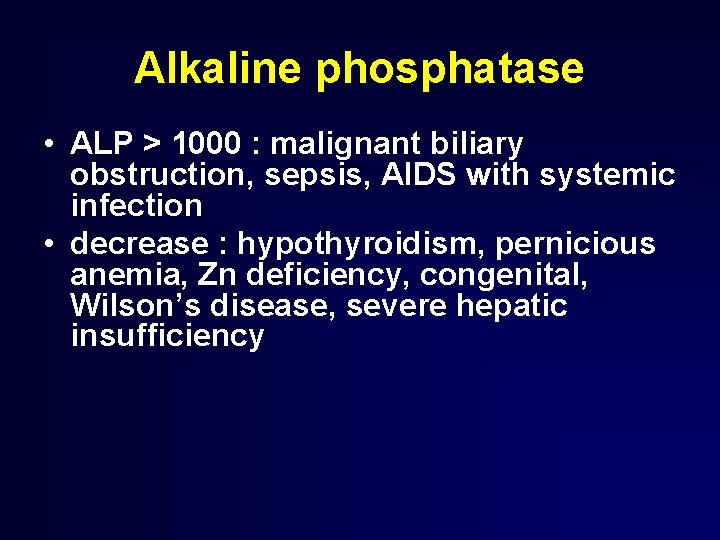
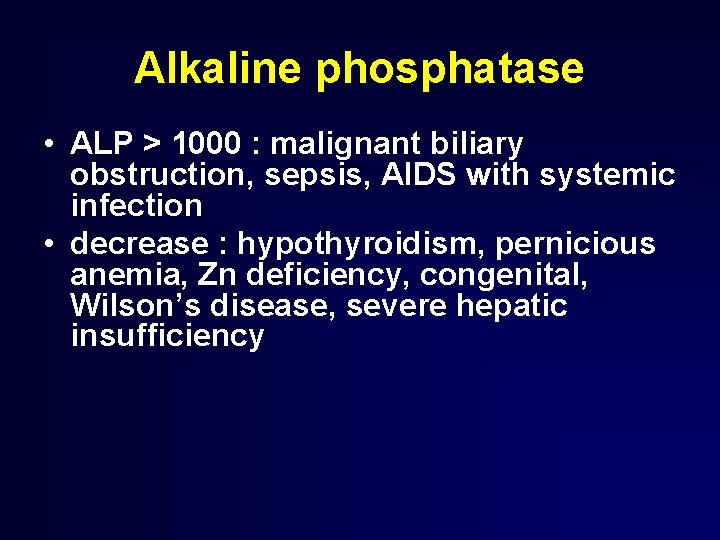
Alkaline phosphatase • ALP > 1000 : malignant biliary obstruction, sepsis, AIDS with systemic infection • decrease : hypothyroidism, pernicious anemia, Zn deficiency, congenital, Wilson’s disease, severe hepatic insufficiency
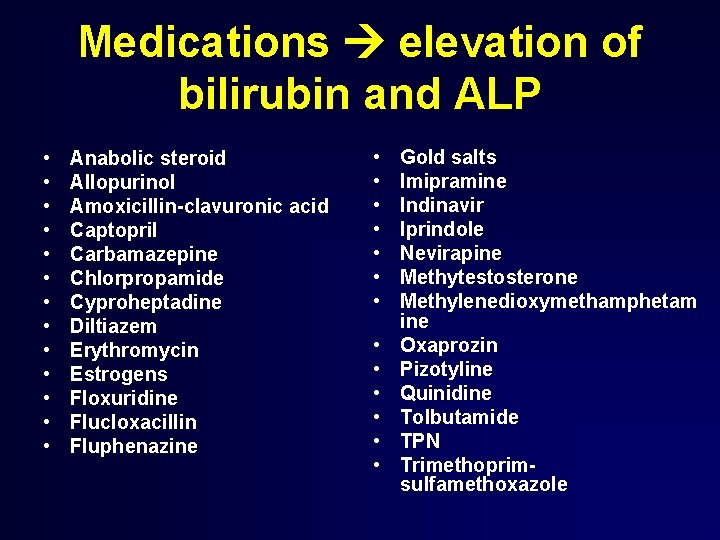
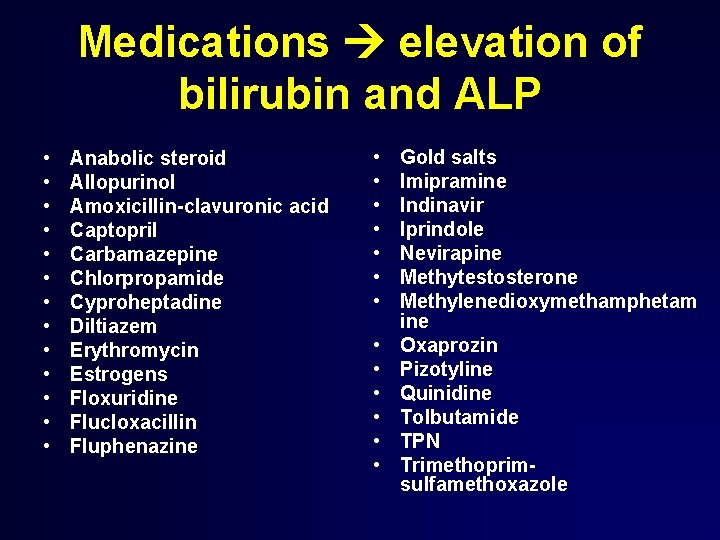
Medications elevation of bilirubin and ALP • • • • Anabolic steroid Allopurinol Amoxicillin-clavuronic acid Captopril Carbamazepine Chlorpropamide Cyproheptadine Diltiazem Erythromycin Estrogens Floxuridine Flucloxacillin Fluphenazine • • • • Gold salts Imipramine Indinavir Iprindole Nevirapine Methytestosterone Methylenedioxymethamphetam ine Oxaprozin Pizotyline Quinidine Tolbutamide TPN Trimethoprimsulfamethoxazole

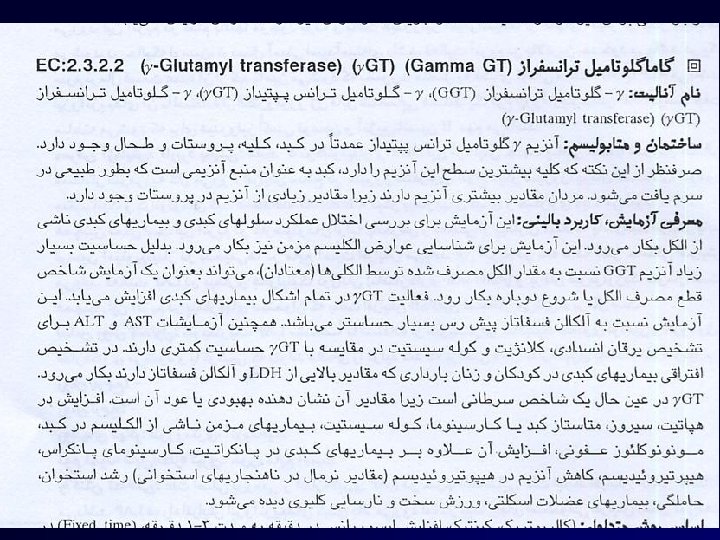
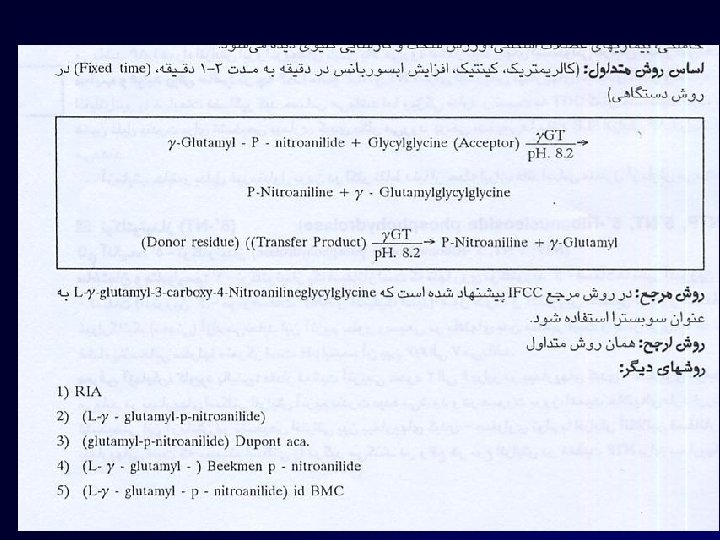
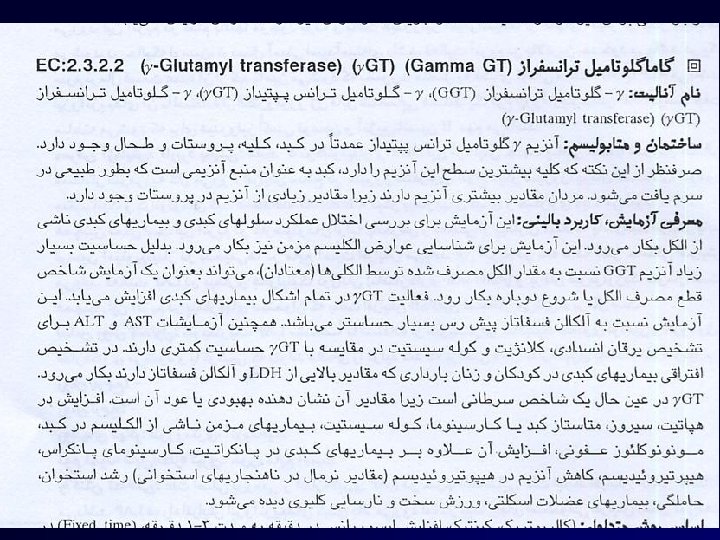
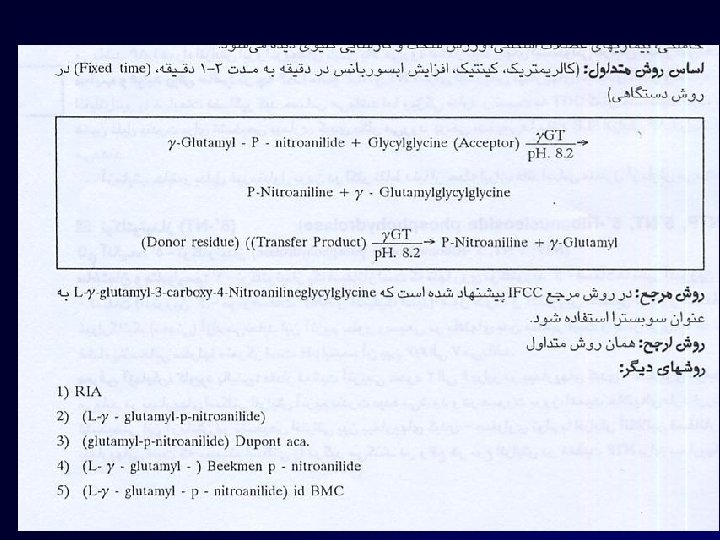
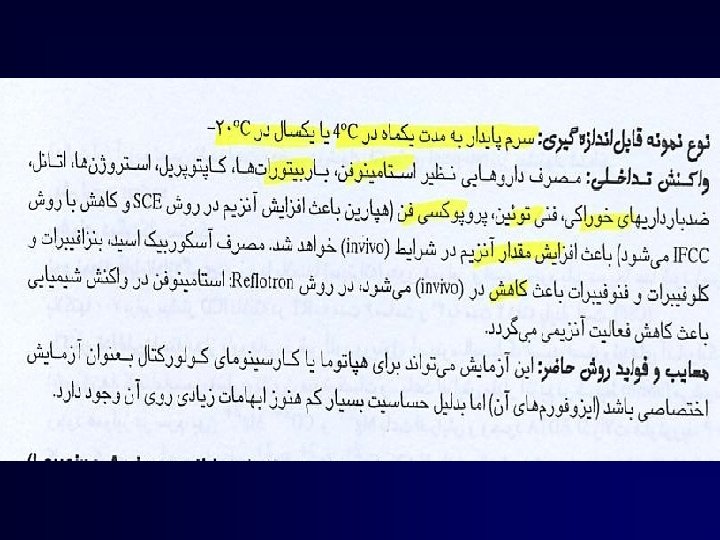
γ-glutamyltransferase (GGT)
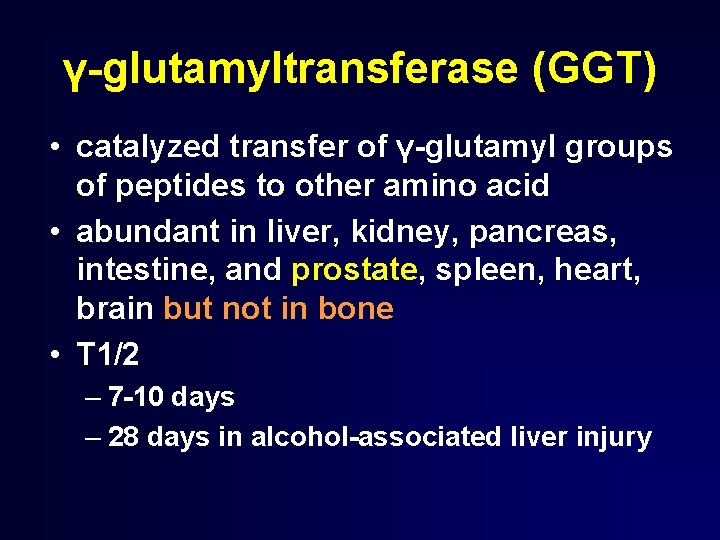
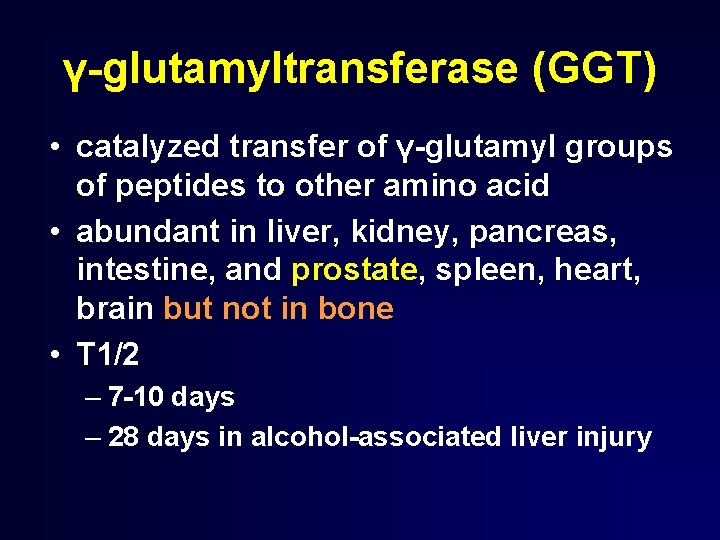
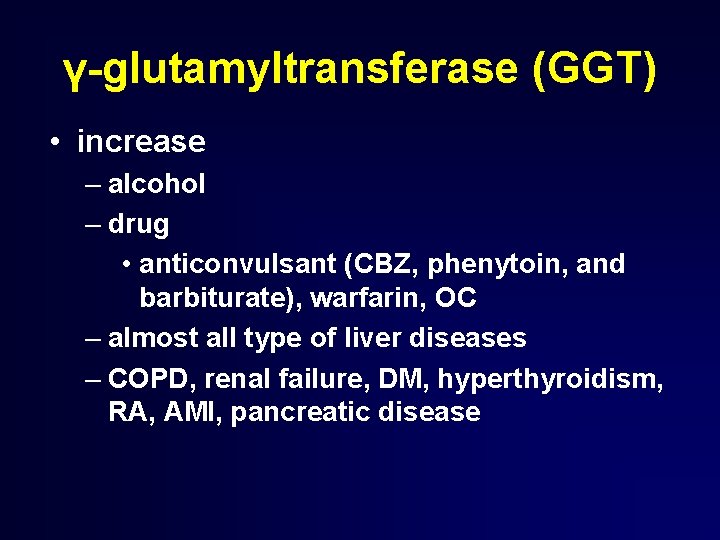
γ-glutamyltransferase (GGT) • catalyzed transfer of γ-glutamyl groups of peptides to other amino acid • abundant in liver, kidney, pancreas, intestine, and prostate, spleen, heart, brain but not in bone • T 1/2 – 7 -10 days – 28 days in alcohol-associated liver injury
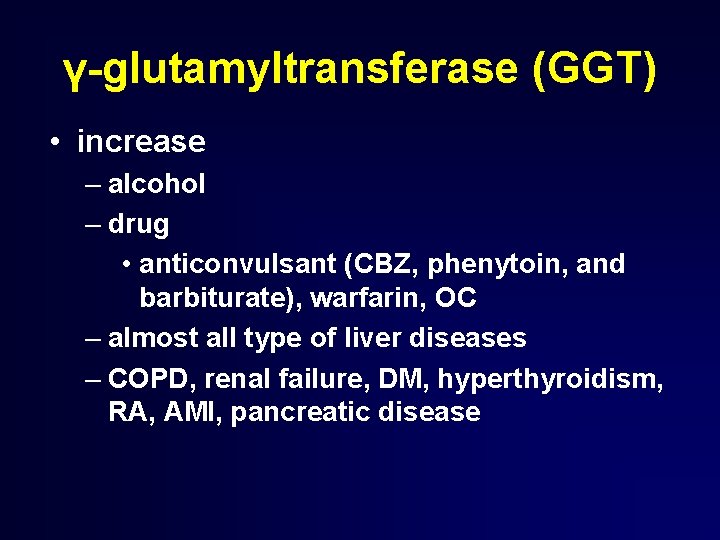
γ-glutamyltransferase (GGT) • increase – alcohol – drug • anticonvulsant (CBZ, phenytoin, and barbiturate), warfarin, OC – almost all type of liver diseases – COPD, renal failure, DM, hyperthyroidism, RA, AMI, pancreatic disease
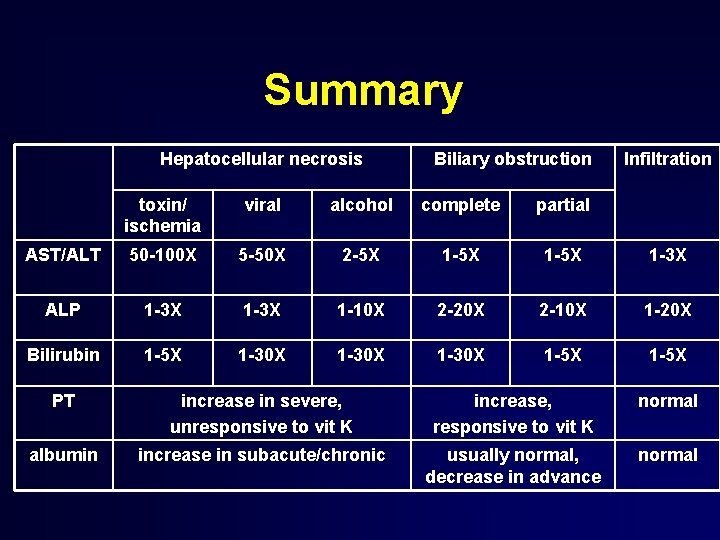
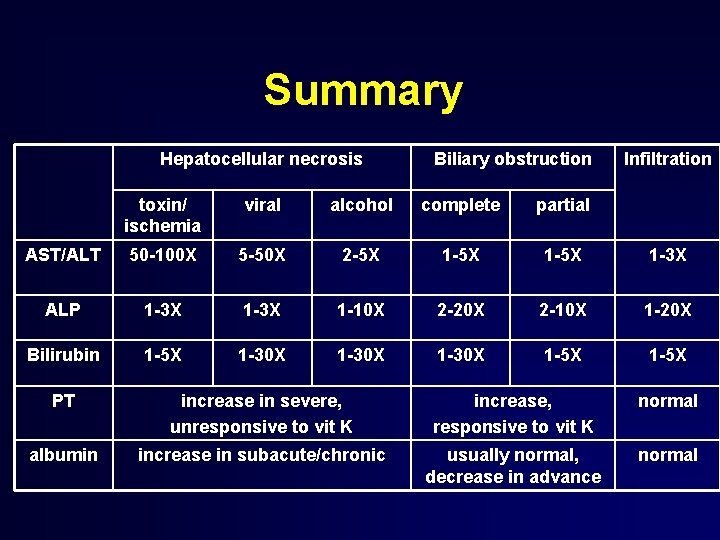
Summary Hepatocellular necrosis Biliary obstruction Infiltration toxin/ ischemia viral alcohol complete partial AST/ALT 50 -100 X 5 -50 X 2 -5 X 1 -5 X 1 -3 X ALP 1 -3 X 1 -10 X 2 -20 X 2 -10 X 1 -20 X Bilirubin 1 -5 X 1 -30 X 1 -5 X PT increase in severe, unresponsive to vit K increase, responsive to vit K normal albumin increase in subacute/chronic usually normal, decrease in advance normal
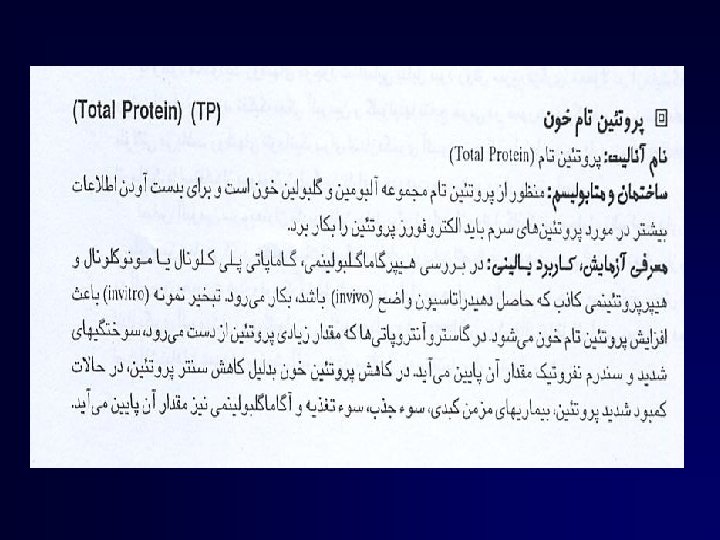
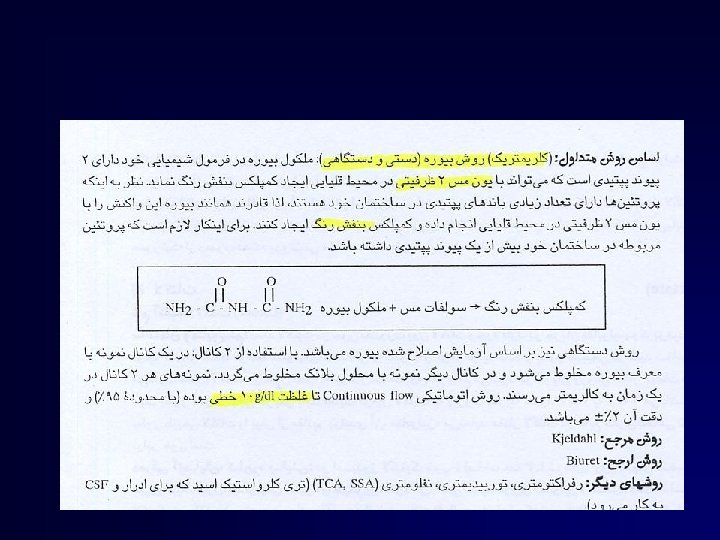
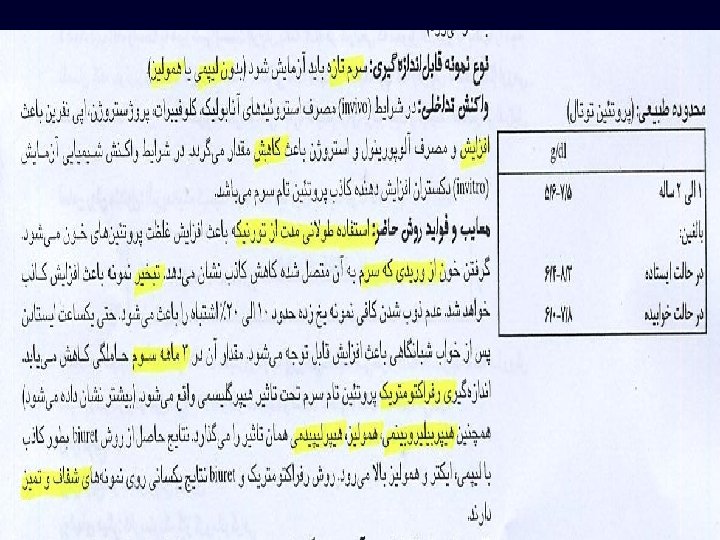
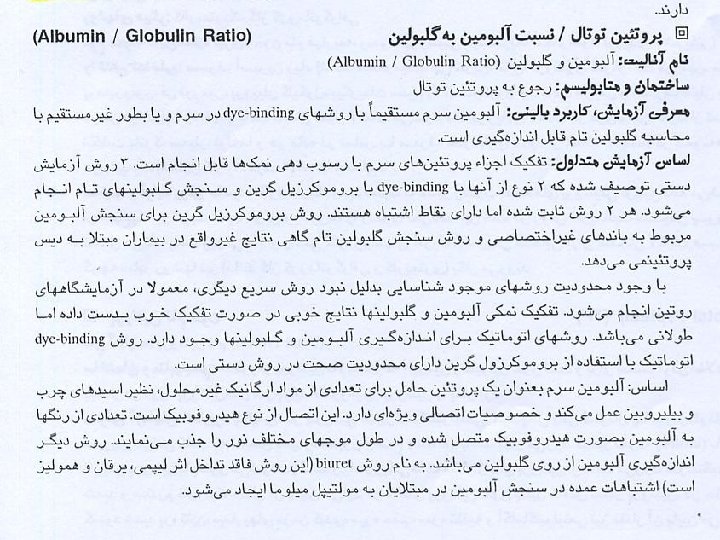
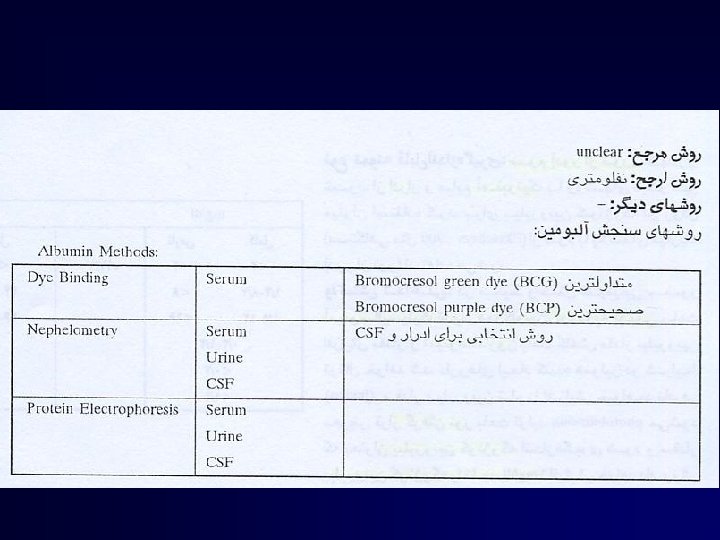
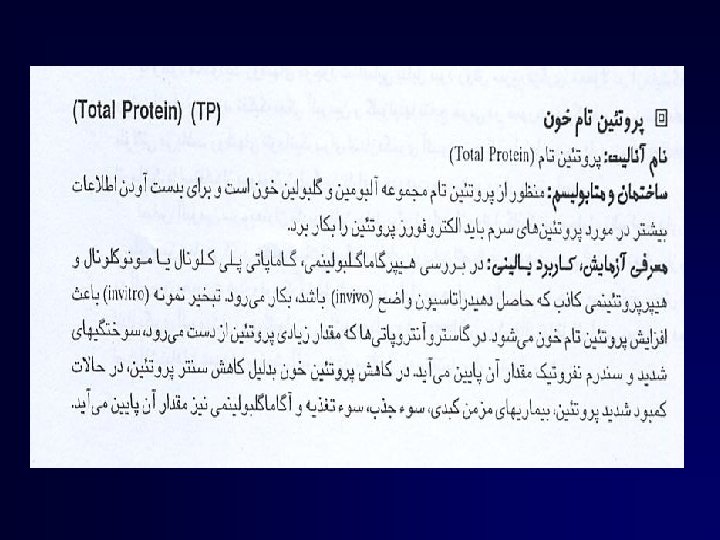
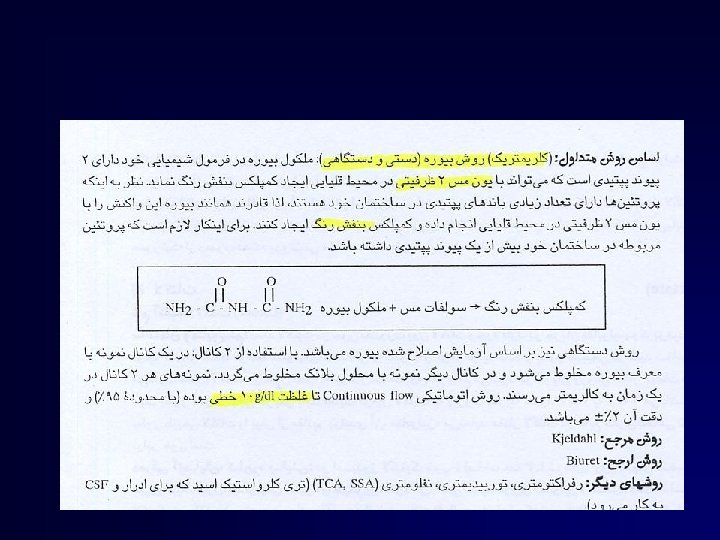
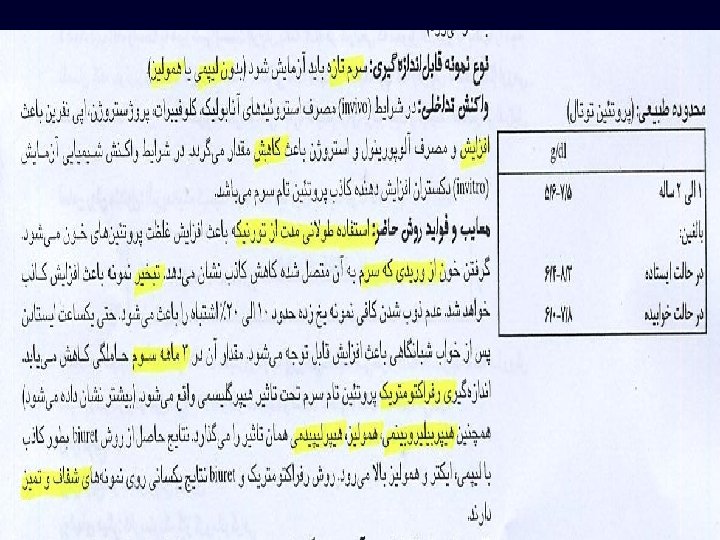
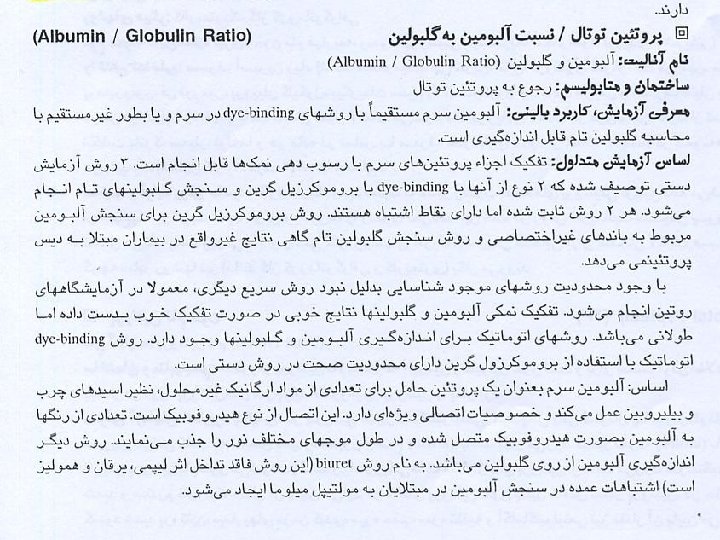
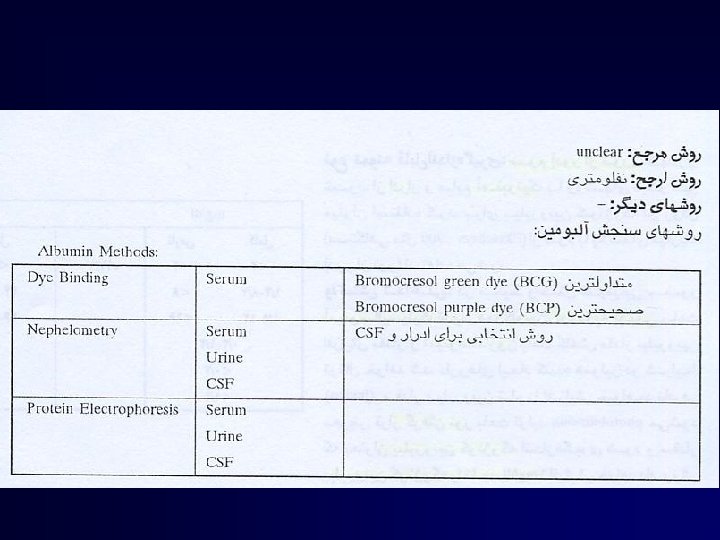
Albumin
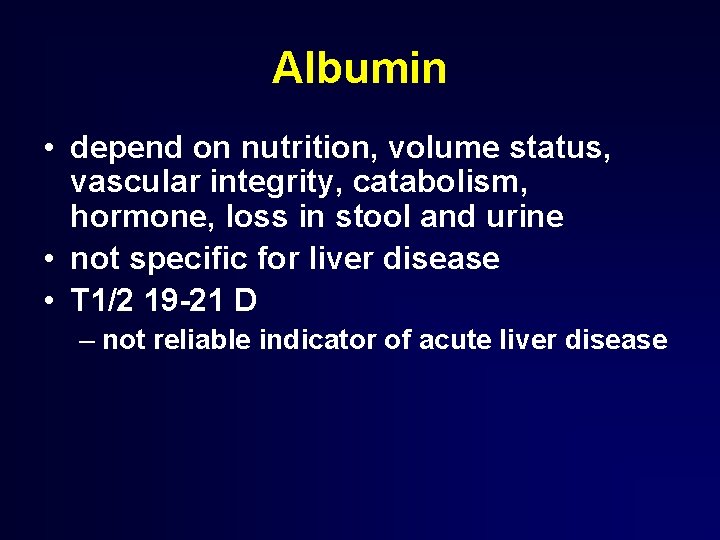
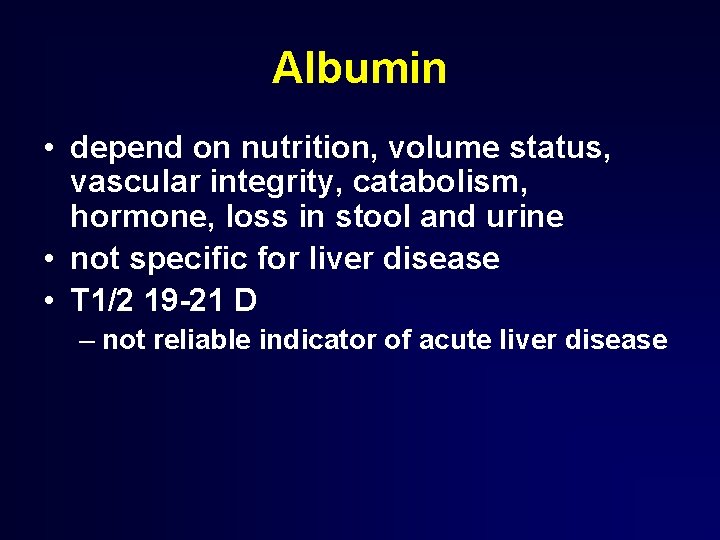
Albumin • depend on nutrition, volume status, vascular integrity, catabolism, hormone, loss in stool and urine • not specific for liver disease • T 1/2 19 -21 D – not reliable indicator of acute liver disease
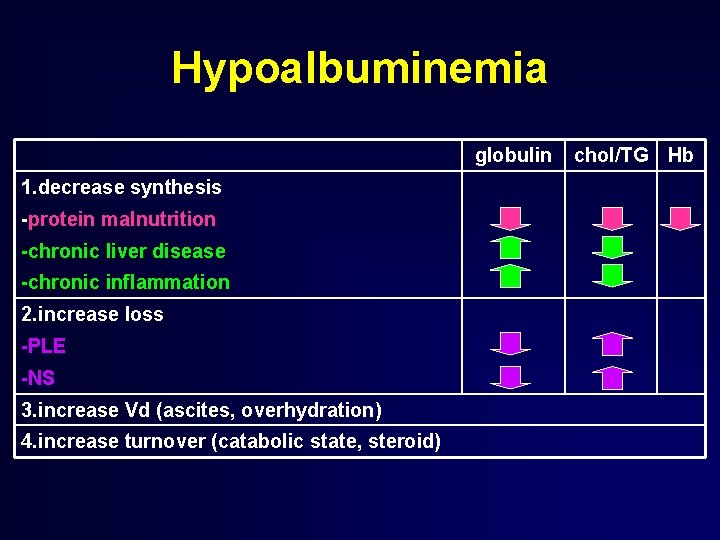
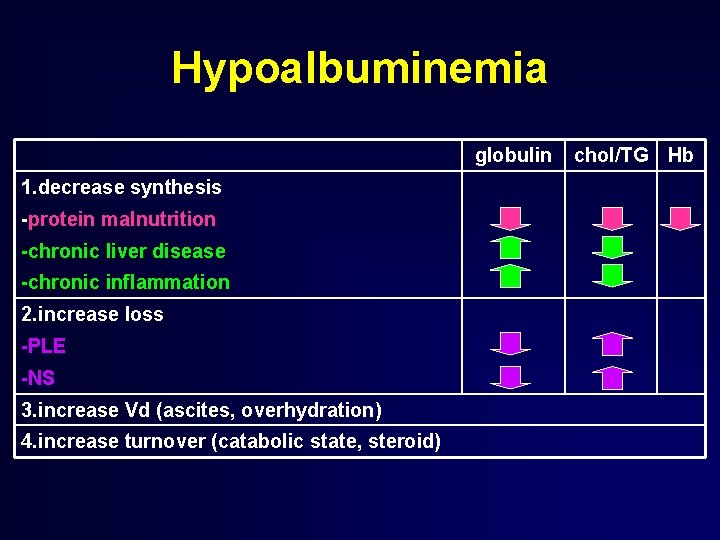
Hypoalbuminemia globulin 1. decrease synthesis -protein malnutrition -chronic liver disease -chronic inflammation 2. increase loss -PLE -NS 3. increase Vd (ascites, overhydration) 4. increase turnover (catabolic state, steroid) chol/TG Hb
Globulin • produced by stimulated B lymphocyte • elevation in • chronic liver disease • chronic inflammation and malignant disease
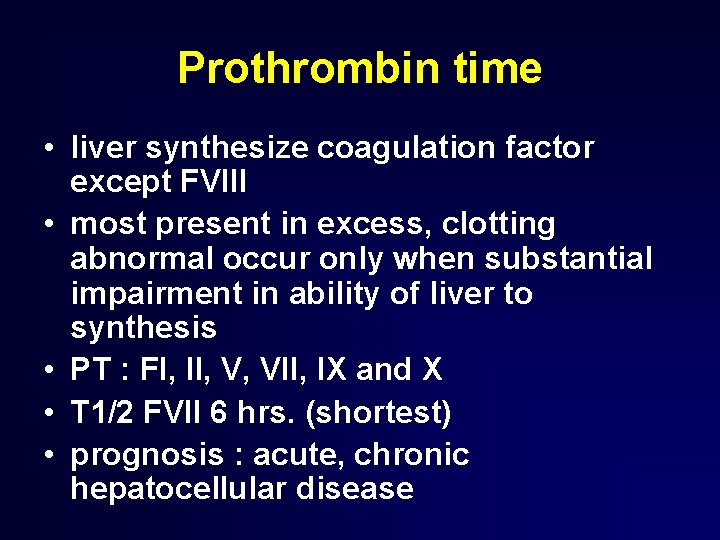
Prothrombin time • liver synthesize coagulation factor except FVIII • most present in excess, clotting abnormal occur only when substantial impairment in ability of liver to synthesis • PT : FI, II, V, VII, IX and X • T 1/2 FVII 6 hrs. (shortest) • prognosis : acute, chronic hepatocellular disease
Prothrombin time prolonged : • vitamin K deficiency (malnutrition, malabsorption, antibiotics) • massive transfusion • congenital disease • liver disease • warfarin • DIC
Prothrombin time • in vit K deficiency, vit K 10 mg SC decrease prolong PT >30% within 24 hrs. • INR : no advantage over PT
Take home message • initial evaluation : assess in clinical context • classified in 3 groups § synthetic function : albumin, clotting time § cholestasis : bilirubin, ALP, GGT § hepatocyte injury : AST, ALT
Liver Function Test misnomer – not effectively assess actual function – not always specific for the liver – limited information regarding presence or severity of complication Liver Chemistry Test
Liver Function Test • normal may have abnormal test • normal value not ensure that patient is free of liver disease • level of abnormality does not reflect severity but may help in DDx • decrease in the value does not mean improvement • limitation in sensitivity and specificity