Community Pharmacy PGDs for Minor Ailments Helen Wilkinson




































- Slides: 102
Community Pharmacy PGDs for Minor Ailments Helen Wilkinson, Principal Medicines Optimisation Pharmacist, BNSSG CCG
Welcome 1. 2. 3. 4. 5. Introductions & Housekeeping (RB) 5 mins Pharmacy’s role in urgent care (HW) 5 mins Shared Decision Making (SN) 10 mins Antimicrobial Stewardship (EJ) 10 min Clinical Session(SN / MJ / HW) UTI 15 mins - LJ Sore Throat – SN 15 mins Skin – 15 mins SN/MJ Conjunctivitis – HW 10 mins Pharm. Outcomes & accreditation process (RB) 10 mins 6. Q&A 15 mins

Community Pharmacy Supporting Urgent Care • Each year the NHS provides around 110 million urgent same-day patient contacts. Around 85 million of these are urgent GP appointments, and the rest are A&E or minor injuries-type visits. Estimates are that 6% of GP appointments are potentially avoidable through better use of self-care and community pharmacy. • BNSSG CCG recognises the important role that community pharmacy has in supporting the urgent care system and how the valuable skills of pharmacy teams can support patients to manage common illnesses. • The new BNSSG Urgent & Emergency Care Model (UEC) model clearly identifies a place for community pharmacy supporting urgent care and self-care.
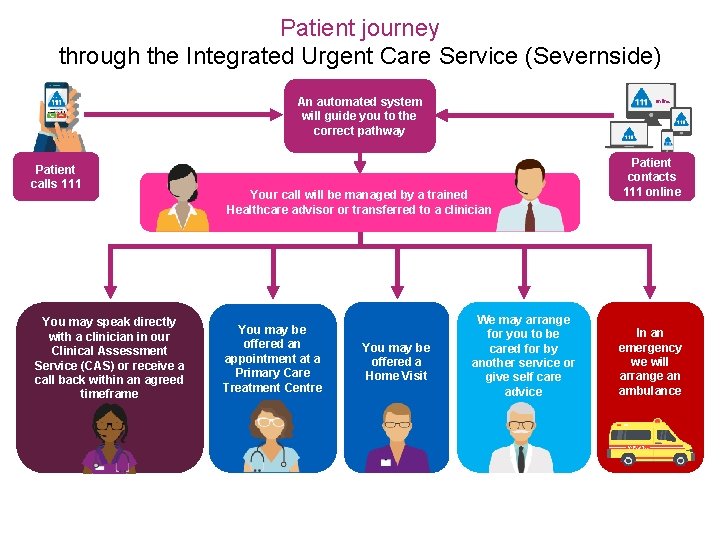
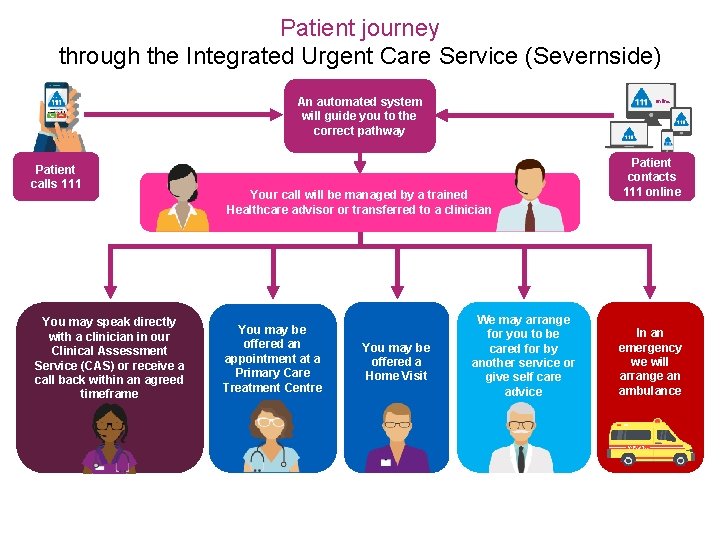
Patient journey through the Integrated Urgent Care Service (Severnside) An automated system will guide you to the correct pathway Patient calls 111 You may speak directly with a clinician in our Clinical Assessment Service (CAS) or receive a call back within an agreed timeframe Online Your call will be managed by a trained Healthcare advisor or transferred to a clinician You may be offered an appointment at a Primary Care Treatment Centre You may be offered a Home Visit We may arrange for you to be cared for by another service or give self care advice Patient contacts 111 online In an emergency we will arrange an ambulance
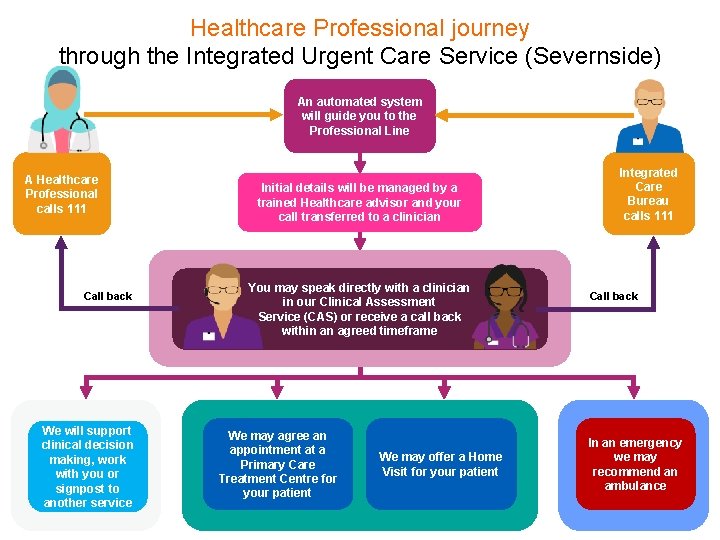
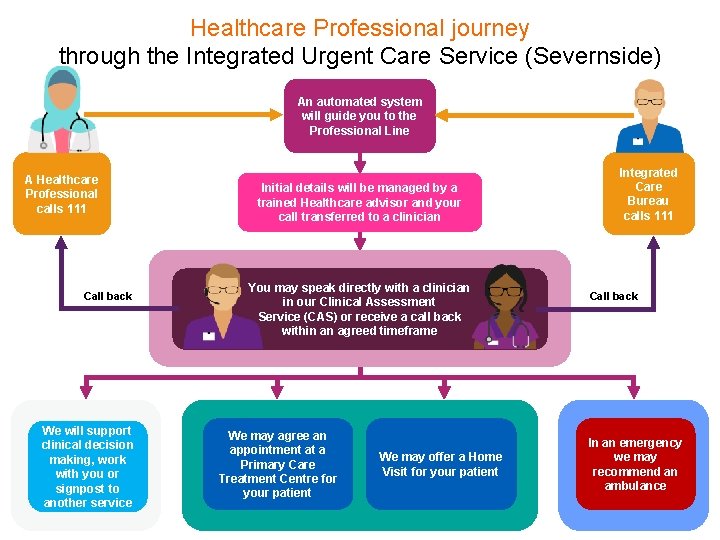
Healthcare Professional journey through the Integrated Urgent Care Service (Severnside) An automated system will guide you to the Professional Line A Healthcare Professional calls 111 Call back We will support clinical decision making, work with you or signpost to another service Initial details will be managed by a trained Healthcare advisor and your call transferred to a clinician You may speak directly with a clinician in our Clinical Assessment Service (CAS) or receive a call back within an agreed timeframe We may agree an appointment at a Primary Care Treatment Centre for your patient We may offer a Home Visit for your patient Integrated Care Bureau calls 111 Call back In an emergency we may recommend an ambulance
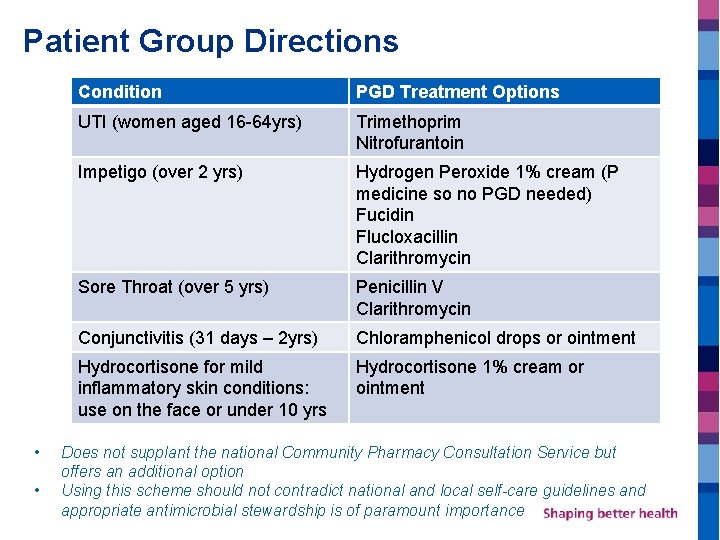
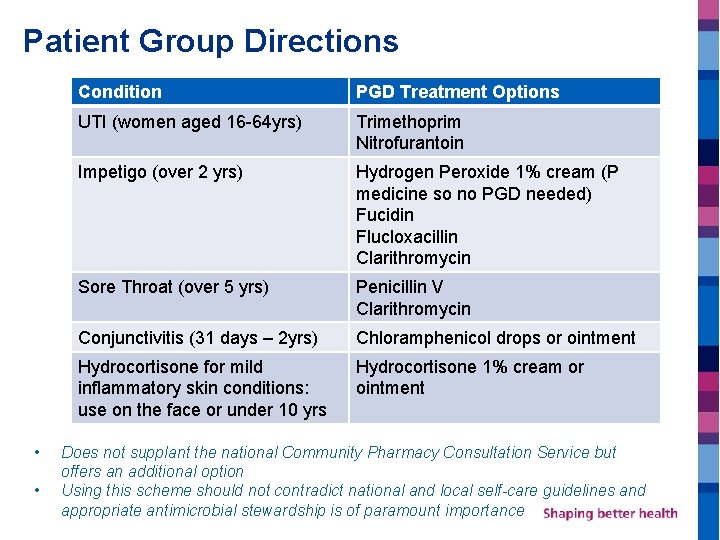
Patient Group Directions • • Condition PGD Treatment Options UTI (women aged 16 -64 yrs) Trimethoprim Nitrofurantoin Impetigo (over 2 yrs) Hydrogen Peroxide 1% cream (P medicine so no PGD needed) Fucidin Flucloxacillin Clarithromycin Sore Throat (over 5 yrs) Penicillin V Clarithromycin Conjunctivitis (31 days – 2 yrs) Chloramphenicol drops or ointment Hydrocortisone for mild inflammatory skin conditions: use on the face or under 10 yrs Hydrocortisone 1% cream or ointment Does not supplant the national Community Pharmacy Consultation Service but offers an additional option Using this scheme should not contradict national and local self-care guidelines and appropriate antimicrobial stewardship is of paramount importance
PGD Training: Consultation Skills Dr Shaba Nabi GP Clinical Lead Prescribing Bristol, North Somerset, South Gloucestershire CCG



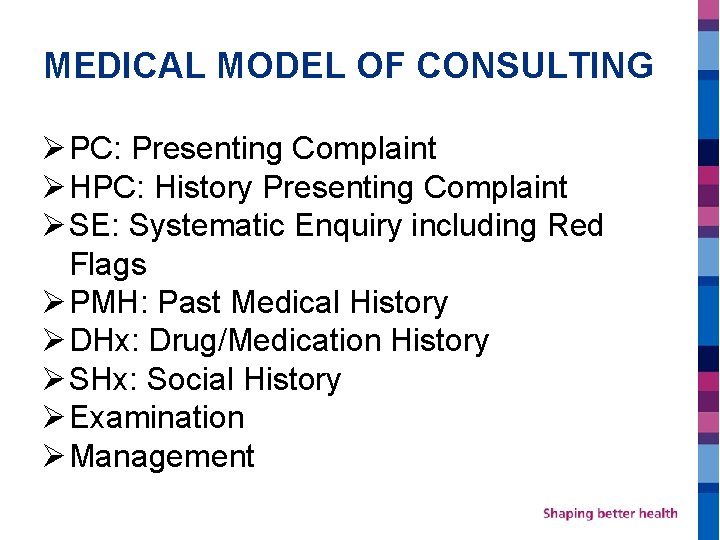
MEDICAL MODEL OF CONSULTING Ø PC: Presenting Complaint Ø HPC: History Presenting Complaint Ø SE: Systematic Enquiry including Red Flags Ø PMH: Past Medical History Ø DHx: Drug/Medication History Ø SHx: Social History Ø Examination Ø Management

PERSON-CENTRED APPROACH SPICESS

S P I C E S S Social Impact on Psychological patient Ideas Concerns Expectations Shared Decision Making Safety Netting
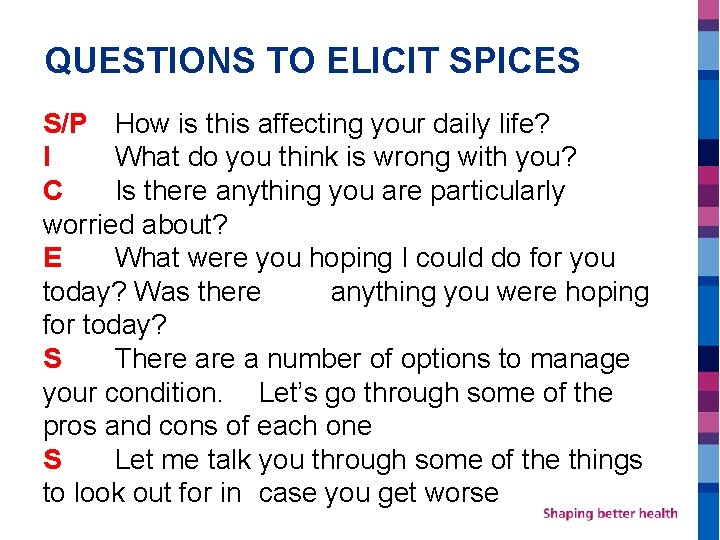
QUESTIONS TO ELICIT SPICES S/P How is this affecting your daily life? I What do you think is wrong with you? C Is there anything you are particularly worried about? E What were you hoping I could do for you today? Was there anything you were hoping for today? S There a number of options to manage your condition. Let’s go through some of the pros and cons of each one S Let me talk you through some of the things to look out for in case you get worse
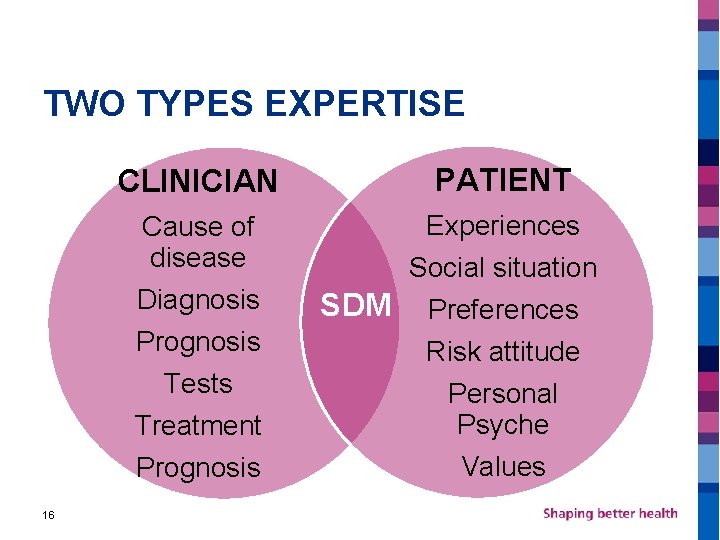
WHAT IS SHARED DECISION MAKING? Shared decision making is a process in which clinicians and patients work together in partnership to clarify treatment, management or self management support goals, sharing information about options and preferred outcomes with the aim of reaching mutual agreement on the best course of action The care people need and no less The care people want and no more 15
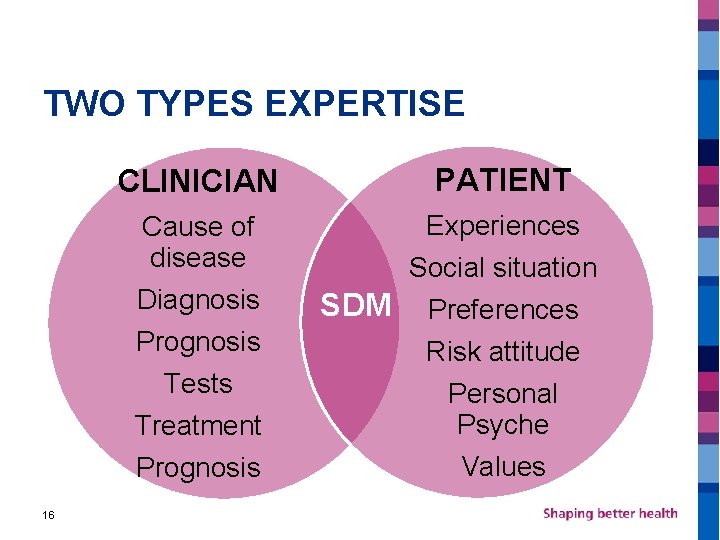
TWO TYPES EXPERTISE 16 CLINICIAN PATIENT Cause of disease Diagnosis Prognosis Tests Treatment Prognosis Experiences Social situation SDM Preferences Risk attitude Personal Psyche Values
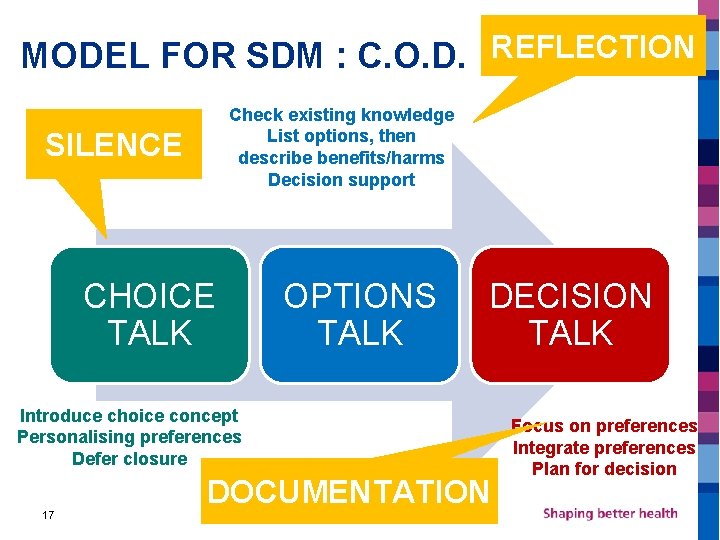
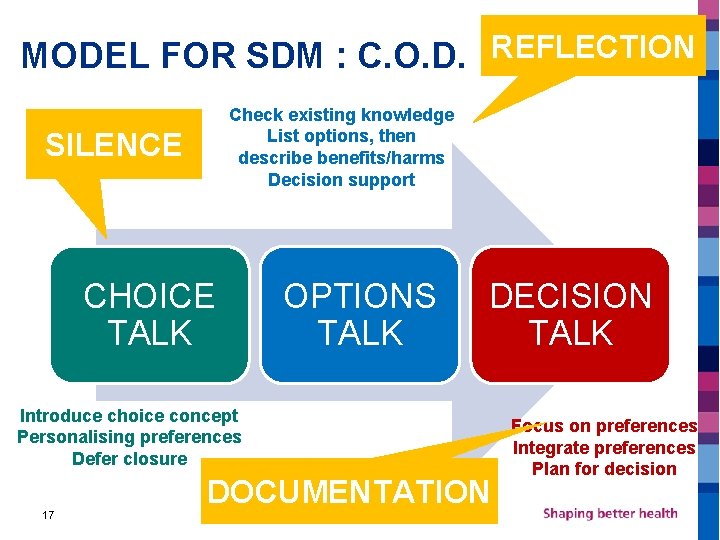
MODEL FOR SDM : C. O. D. REFLECTION Check existing knowledge List options, then describe benefits/harms Decision support SILENCE CHOICE TALK OPTIONS TALK DECISION TALK Introduce choice concept Personalising preferences Defer closure 17 DOCUMENTATION Focus on preferences Integrate preferences Plan for decision

Supplying Antimicrobials Antimicrobial Stewardship

We really are facing, if we don’t take action now, a dreadful post-antibiotic apocalypse, ” Dame Sally Davis AMR is an increasingly serious threat to global public health that requires action across all government sectors and society. Without effective antibiotics, the success of major surgery and cancer chemotherapy would be compromised. WHO

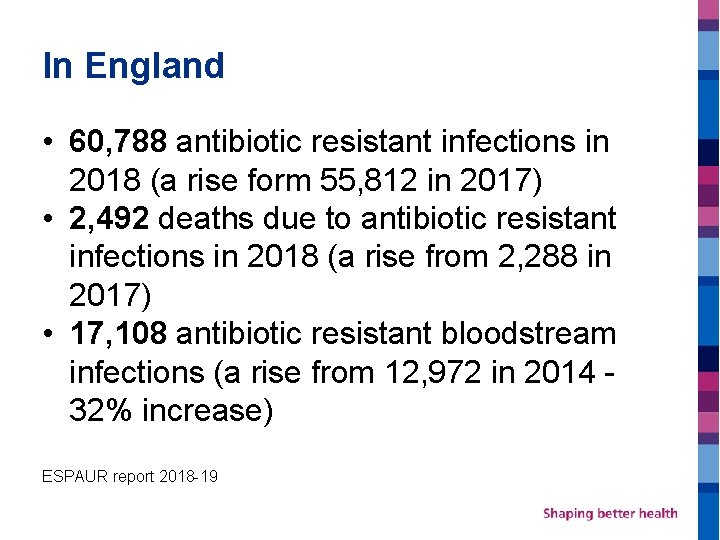
In England • 60, 788 antibiotic resistant infections in 2018 (a rise form 55, 812 in 2017) • 2, 492 deaths due to antibiotic resistant infections in 2018 (a rise from 2, 288 in 2017) • 17, 108 antibiotic resistant bloodstream infections (a rise from 12, 972 in 2014 - 32% increase) ESPAUR report 2018 -19



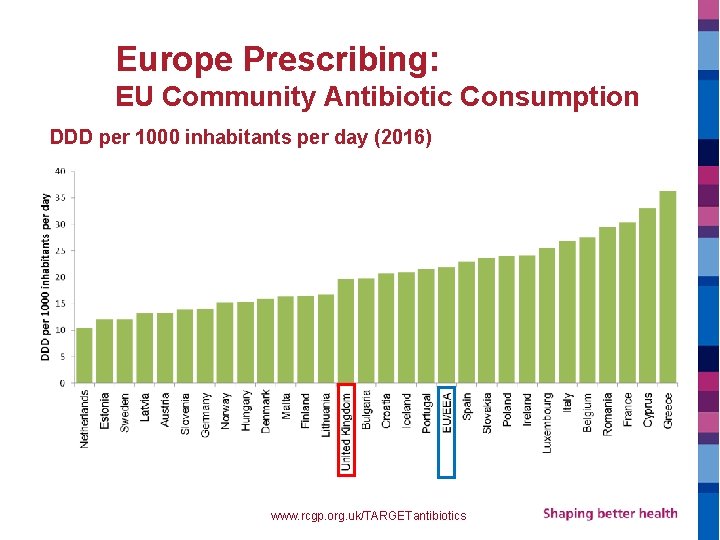
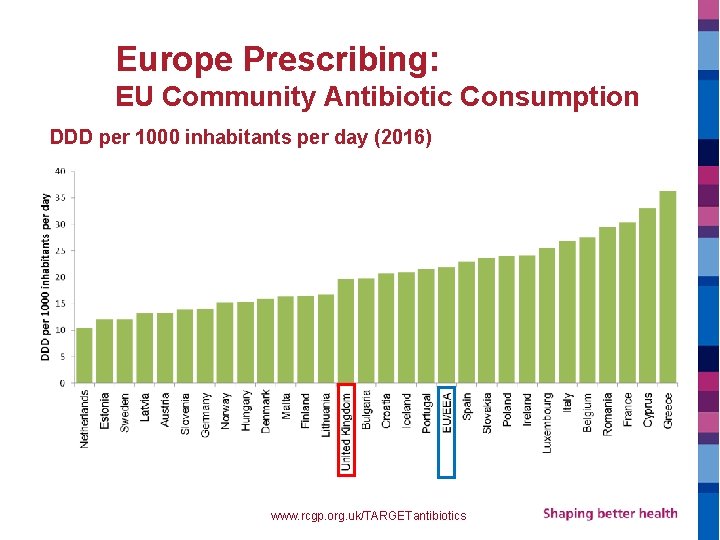
Europe Prescribing: EU Community Antibiotic Consumption DDD per 1000 inhabitants per day (2016) © ECDC www. rcgp. org. uk/TARGETantibiotics
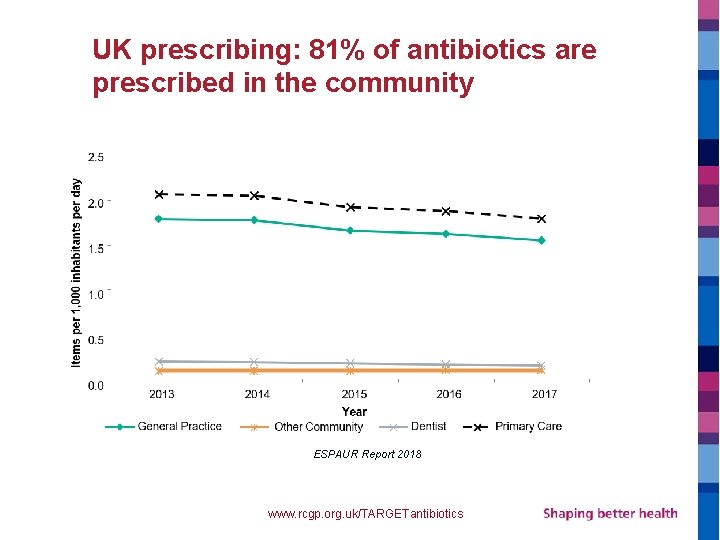
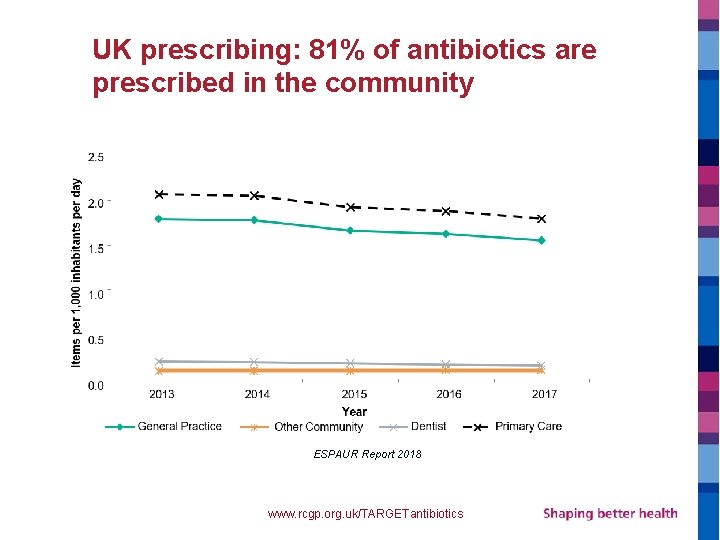
UK prescribing: 81% of antibiotics are prescribed in the community ESPAUR Report 2018 www. rcgp. org. uk/TARGETantibiotics

Community antibiotic prescribing in BNSSG
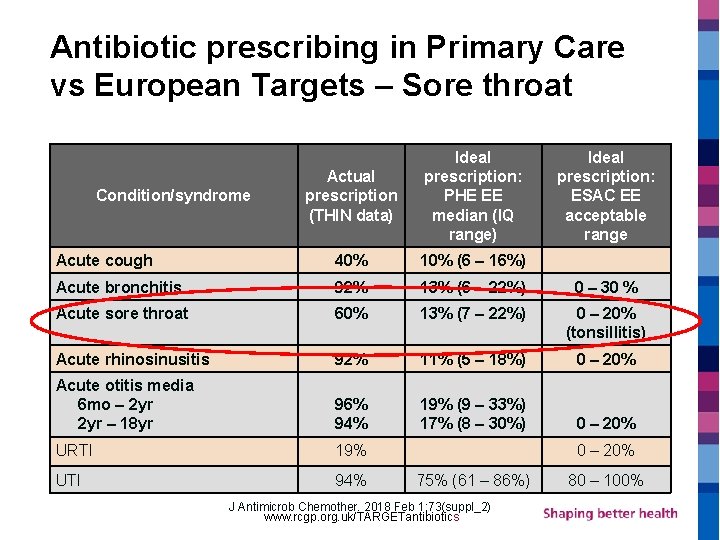
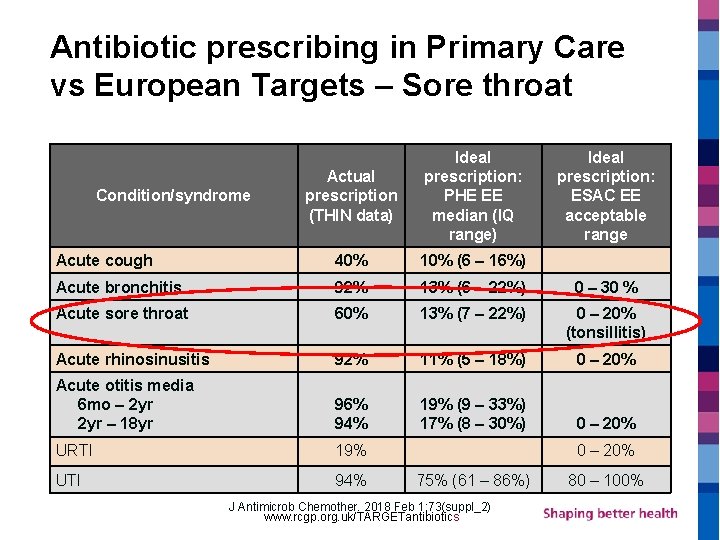
Antibiotic prescribing in Primary Care vs European Targets – Sore throat Actual prescription (THIN data) Ideal prescription: PHE EE median (IQ range) Acute cough 40% 10% (6 – 16%) Acute bronchitis 92% 13% (6 – 22%) 0 – 30 % Acute sore throat 60% 13% (7 – 22%) 0 – 20% (tonsillitis) Acute rhinosinusitis 92% 11% (5 – 18%) 0 – 20% Acute otitis media 6 mo – 2 yr – 18 yr 96% 94% 19% (9 – 33%) 17% (8 – 30%) 0 – 20% URTI 19% UTI 94% Condition/syndrome Ideal prescription: ESAC EE acceptable range 0 – 20% 75% (61 – 86%) J Antimicrob Chemother. 2018 Feb 1; 73(suppl_2) www. rcgp. org. uk/TARGETantibiotics 80 – 100%
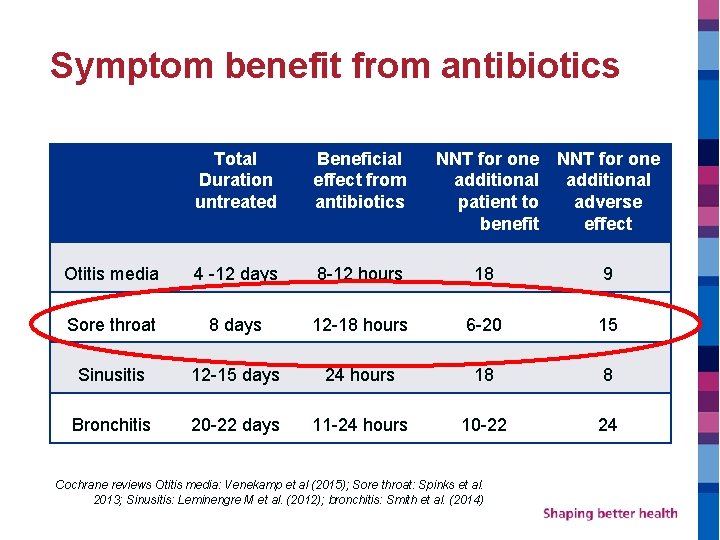
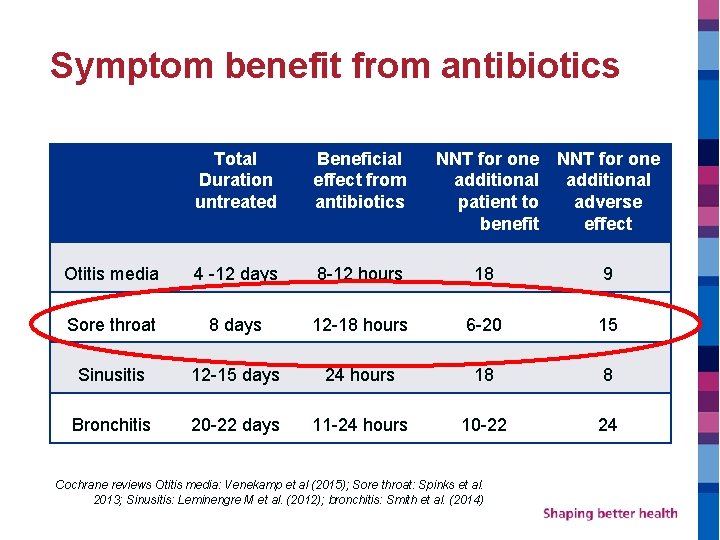
Symptom benefit from antibiotics Total Duration untreated Beneficial effect from antibiotics NNT for one additional patient to adverse benefit effect Otitis media 4 -12 days 8 -12 hours 18 9 Sore throat 8 days 12 -18 hours 6 -20 15 Sinusitis 12 -15 days 24 hours 18 8 Bronchitis 20 -22 days 11 -24 hours 10 -22 24 Cochrane reviews Otitis media: Venekamp et al (2015); Sore throat: Spinks et al. 2013; Sinusitis: Leminengre M et al. (2012); bronchitis: Smith et al. (2014)
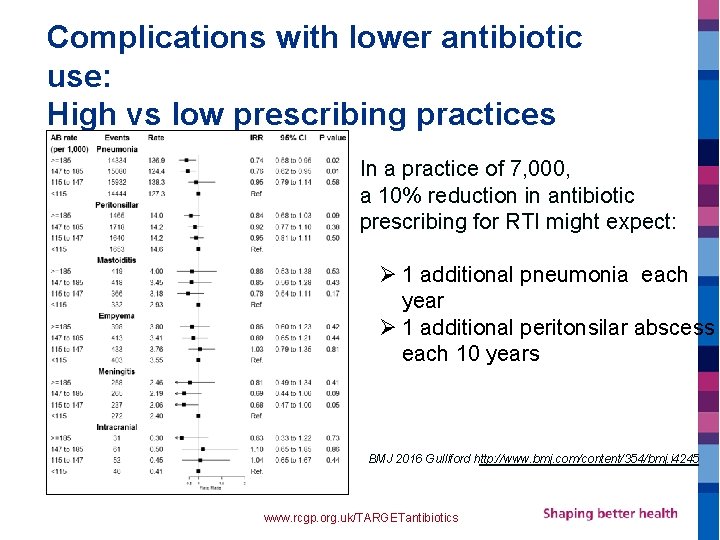
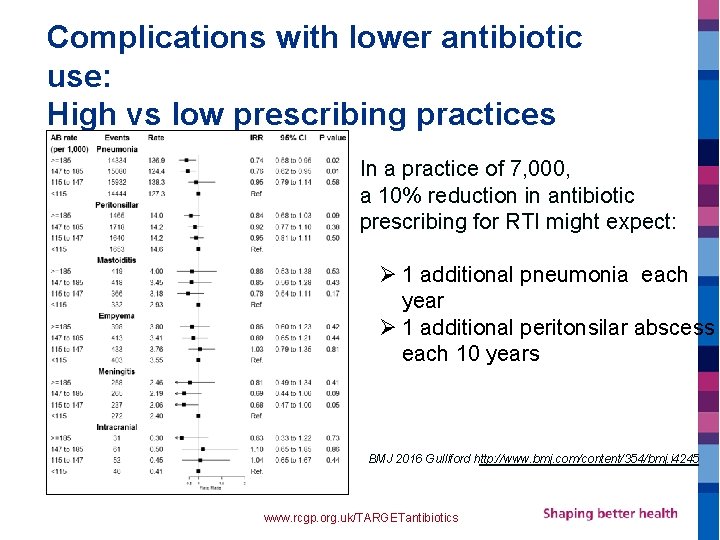
Complications with lower antibiotic use: High vs low prescribing practices In a practice of 7, 000, a 10% reduction in antibiotic prescribing for RTI might expect: Ø 1 additional pneumonia each year Ø 1 additional peritonsilar abscess each 10 years BMJ 2016 Gulliford http: //www. bmj. com/content/354/bmj. i 4245 www. rcgp. org. uk/TARGETantibiotics
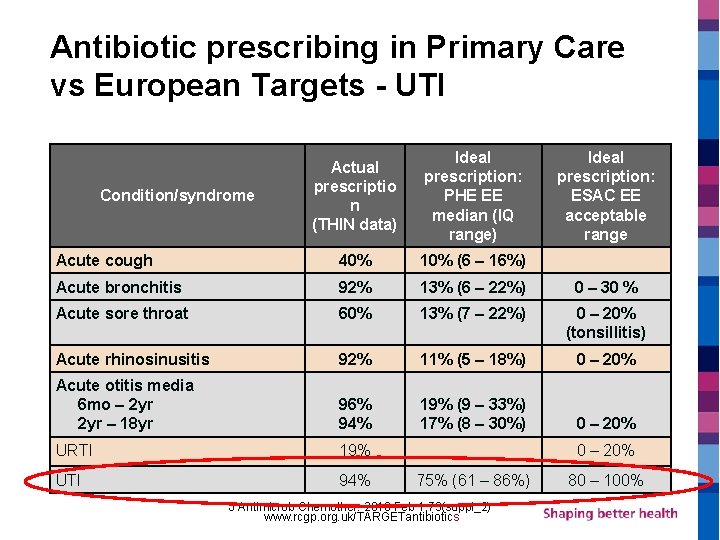
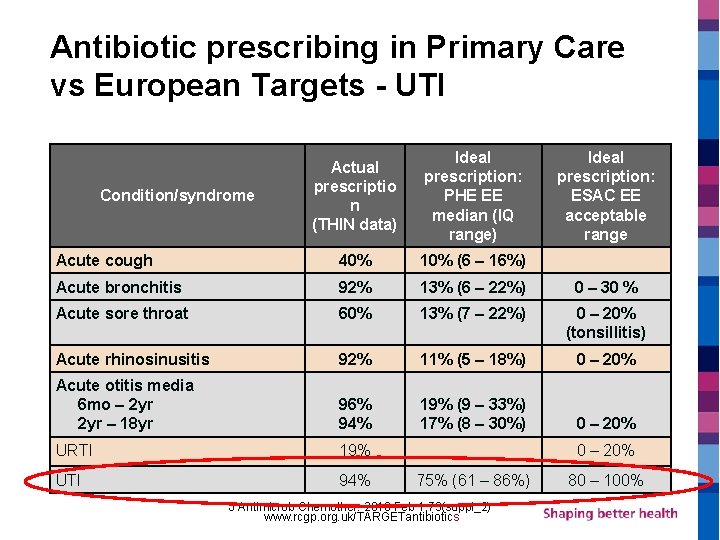
Antibiotic prescribing in Primary Care vs European Targets - UTI Actual prescriptio n (THIN data) Ideal prescription: PHE EE median (IQ range) Acute cough 40% 10% (6 – 16%) Acute bronchitis 92% 13% (6 – 22%) 0 – 30 % Acute sore throat 60% 13% (7 – 22%) 0 – 20% (tonsillitis) Acute rhinosinusitis 92% 11% (5 – 18%) 0 – 20% Acute otitis media 6 mo – 2 yr – 18 yr 96% 94% 19% (9 – 33%) 17% (8 – 30%) 0 – 20% URTI 19% UTI 94% Condition/syndrome Ideal prescription: ESAC EE acceptable range 0 – 20% 75% (61 – 86%) J Antimicrob Chemother. 2018 Feb 1; 73(suppl_2) www. rcgp. org. uk/TARGETantibiotics 80 – 100%
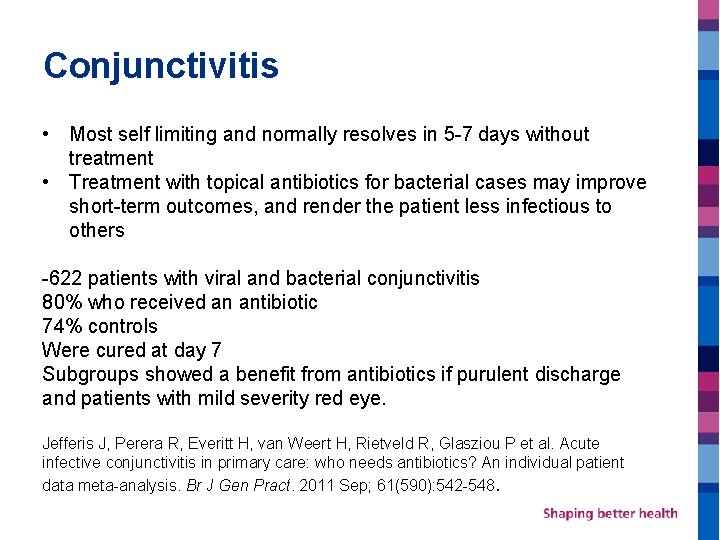
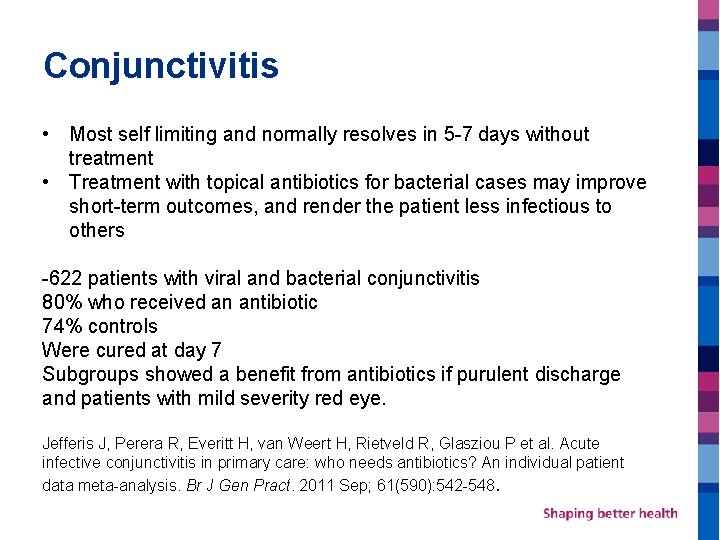
Conjunctivitis • Most self limiting and normally resolves in 5 -7 days without treatment • Treatment with topical antibiotics for bacterial cases may improve short-term outcomes, and render the patient less infectious to others -622 patients with viral and bacterial conjunctivitis 80% who received an antibiotic 74% controls Were cured at day 7 Subgroups showed a benefit from antibiotics if purulent discharge and patients with mild severity red eye. Jefferis J, Perera R, Everitt H, van Weert H, Rietveld R, Glasziou P et al. Acute infective conjunctivitis in primary care: who needs antibiotics? An individual patient data meta-analysis. Br J Gen Pract. 2011 Sep; 61(590): 542 -548.
Impetigo • Some people with impetigo given a placebo achieved cure or improvement • But as highly infectious, treatment should be offered to help limit the spread of infection, to hasten recovery and to limit deterioration.
Urinary Tract Infections Created by Elizabeth Jonas
Why do we need to worry about our antibiotic use in suspected UTI? • Rates of E. coli blood stream infections have increased by 24. 3% from 2012 -2016 • Mandatory surveillance indicates the following risk factors o previous urinary tract infections (UTIs) o urinary catheters o antibiotics in the previous month o older age www. rcgp. org. uk/TARGETantibiotics



UTIs in Community Pharmacy • • Females 16 -65 years old Not pregnant or breastfeeding Two or three of the key diagnostic signs/ symptoms
Red Flags § Signs of sepsis § Pyelonephritis § Visible haematuria
Pyelonephritis Infection of the upper urinary tract – one or both kidneys Higher risk of complications including sepsis • Kidney pain/ tenderness in back under ribs • New/different myalgia • Flu like illness • Shaking chills (rigors) or temperature 37. 9 o. C or above • Nausea or vomiting Refer to GP practice – require different antibiotics and further review
Visible Haematuria - Haematuria (blood in urine) can occur in association with UTIs but can also be caused by non-infective conditions such as malignancy, kidney stones, renal disease or trauma. - Because of this an automatic referral. - GP practice may treat as UTI but will need a urine sample done.
Other initial exclusions • Vaginal and urethral causes of urinary symptoms - vaginal discharge – 80% do not have a UTI treat as appropriate - urethritis – inflammation post sexual intercourse, irritants - sexually transmitted infections - genitourinary syndrome of the menopause Effects about half of postmenopausal women. Symptoms include: - Dryness, burning sensations and irritation in the genital area - Poor vaginal lubrication during sex, discomfort or pain with intercourse and impaired sexual function - An urgent need to urinate, painful urination or recurrent urinary tract infections
Other exclusion criteria cont • Acute porphyria • Known renal impairment • Drug induced cystitis (allopurinol, danazol, cyclophosphamide, tiaprofenic acid and possibly other NSAIDs) • Urological abnormalities or urinary catheter • Recent UTI treated with antibiotics in the last 2 weeks • Immunocompromised Refer to GP practice
Diagnosis - Key Diagnostic Signs • Dysuria – burning pain when passing urine • New nocturia – passing urine more often than usual at night • Urine cloudy to the naked eye

How many symptoms? Two or three - treat with PGD One – Refer to GP practice for a urine dip stick to be performed and actioned None – other urinary symptoms? - Urgency - Frequency - Suprapubic tenderness Yes – refer to GP practice for a urine dipstick No – advise UTI not likely
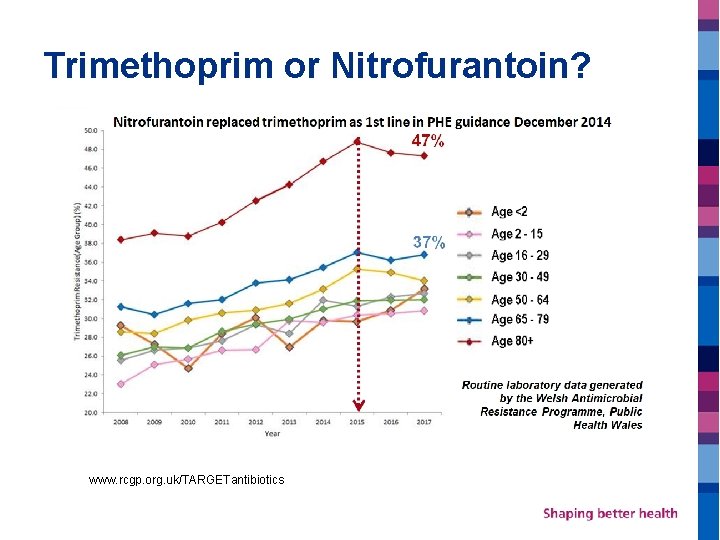
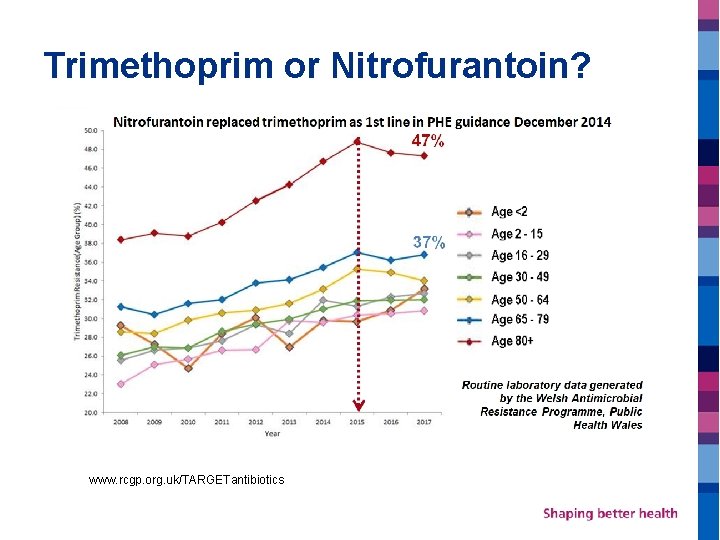
Trimethoprim or Nitrofurantoin? www. rcgp. org. uk/TARGETantibiotics
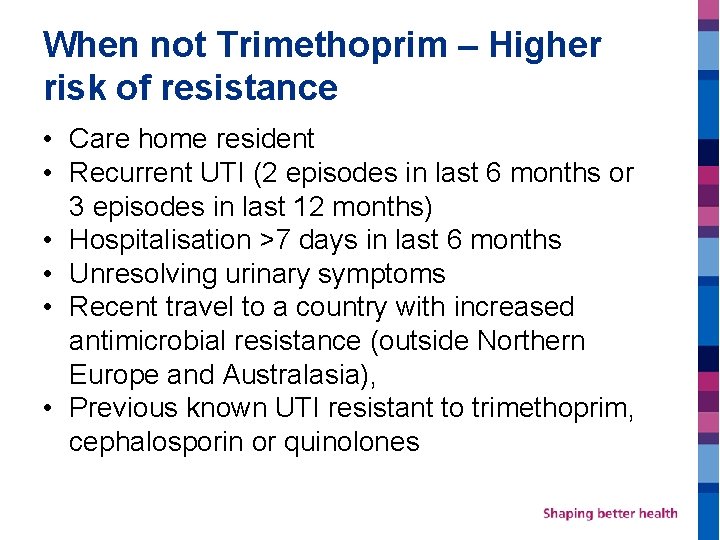
When not Trimethoprim – Higher risk of resistance • Care home resident • Recurrent UTI (2 episodes in last 6 months or 3 episodes in last 12 months) • Hospitalisation >7 days in last 6 months • Unresolving urinary symptoms • Recent travel to a country with increased antimicrobial resistance (outside Northern Europe and Australasia), • Previous known UTI resistant to trimethoprim, cephalosporin or quinolones

Other reasons not Trimethoprim • • Taking Trimethoprim prophylaxis Hypersensitivity to Trimethoprim Taking methotrexate Blood dyscrasias including patients with megaloblastic anaemia e. g. vitamin B 12 or folate deficiency • Patients with rare hereditary problem of galactose intolerance, the Lapp lactase deficiency or glucosegalactose malabsorption • If excluded consider if Nitrofurantoin is appropriate
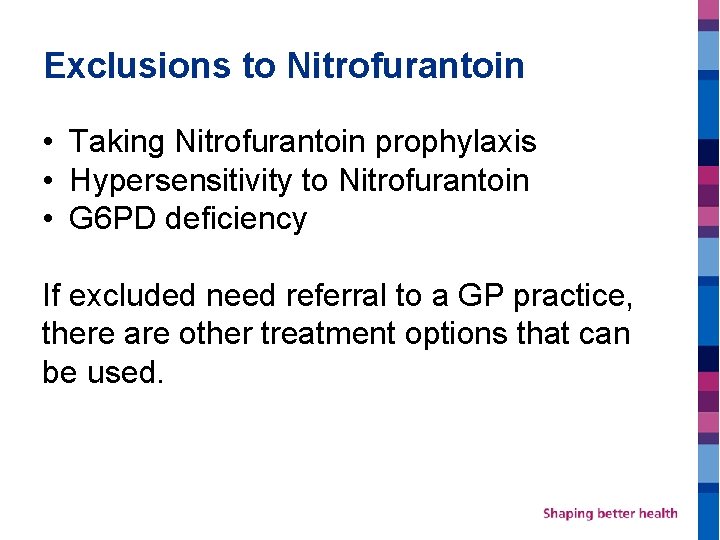
Exclusions to Nitrofurantoin • Taking Nitrofurantoin prophylaxis • Hypersensitivity to Nitrofurantoin • G 6 PD deficiency If excluded need referral to a GP practice, there are other treatment options that can be used.
Repeat Presentations Can be treated But – refer to GP practice / advice to seek advise next UTI if having more than 2 episodes in 6 months or 3 episodes in 12 months as will need a discussion about the prevention of UTIs and may need investigations.
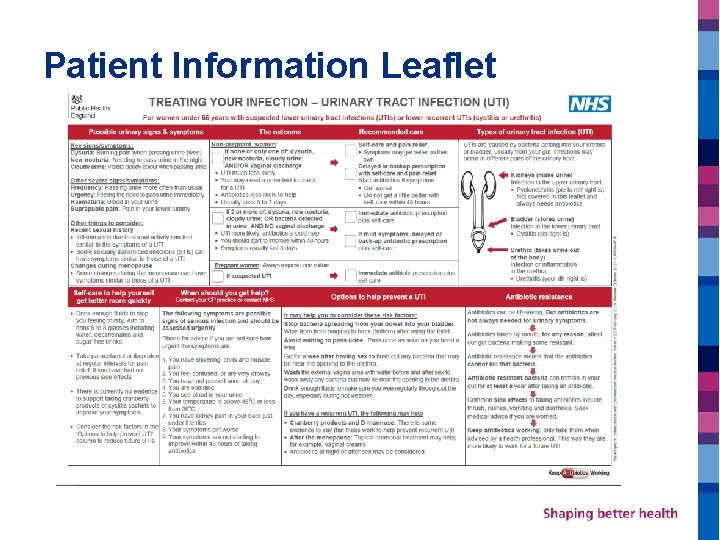
Patient Information Leaflet
PGD Training: Sore Throat Dr Shaba Nabi GP Clinical Lead Prescribing Bristol, North Somerset, South Gloucestershire CCG
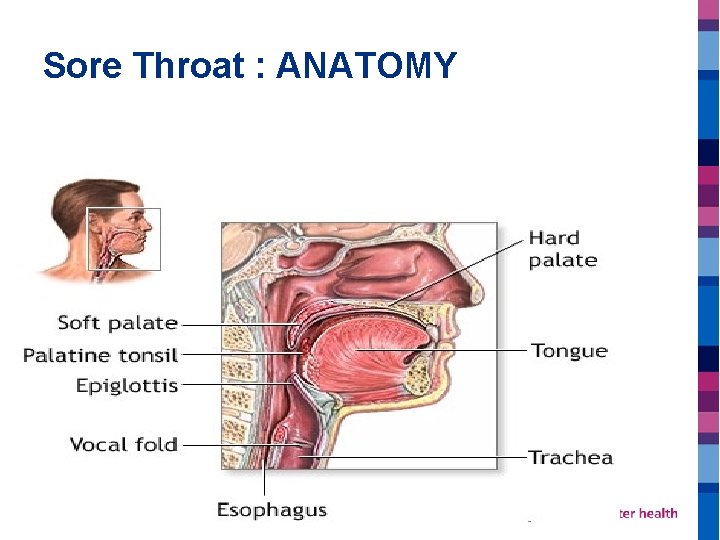
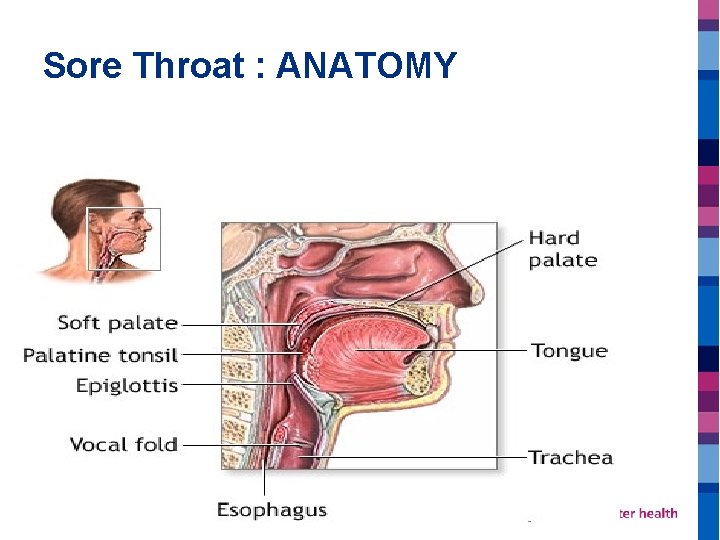
Sore Throat : ANATOMY

Sore Throat : EQUIPMENT?
Sore Throat : ENQUIRY v Duration v Severity v Fever v Self-Treatment v Cough/Coryza v Rash v Difficulty swallowing v Difficulty breathing v Trismus v PMH/Pregnancy/Medication
Sore Throat : Fever. PAIN score FEVER In last 24 hrs
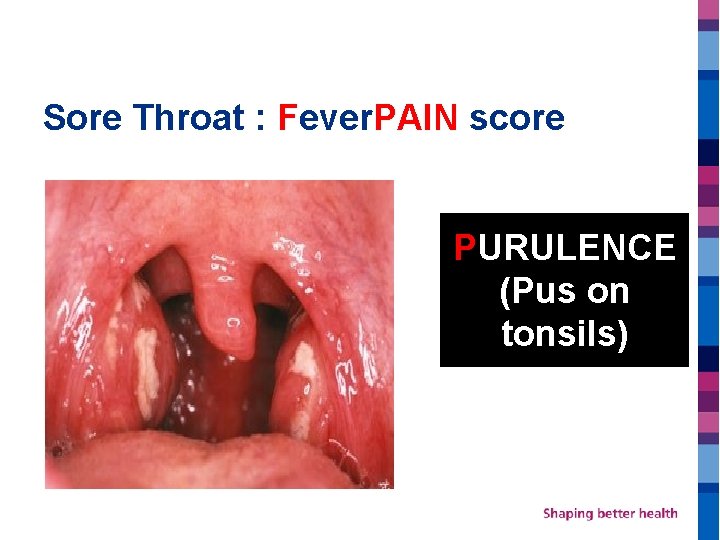
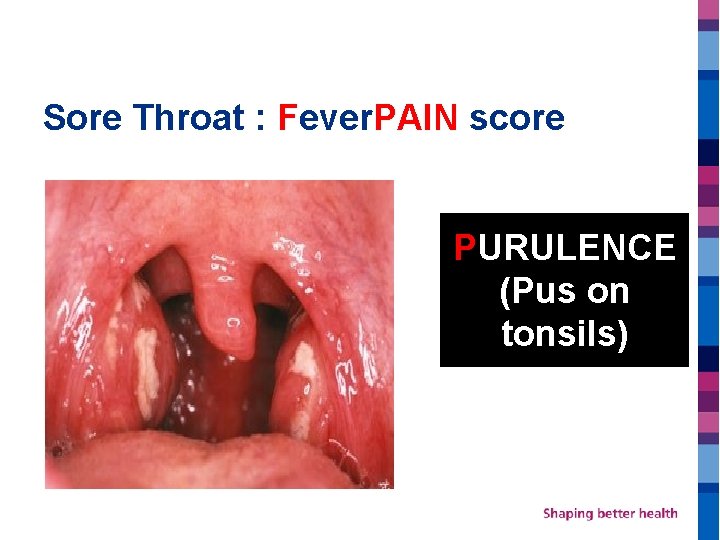
Sore Throat : Fever. PAIN score PURULENCE (Pus on tonsils)
Sore Throat : Fever. PAIN score ATTENDS RAPIDLY (within 3 days)
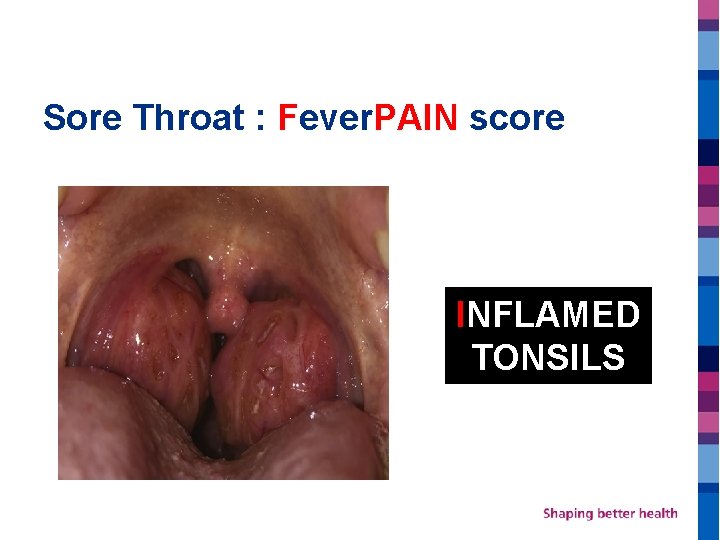
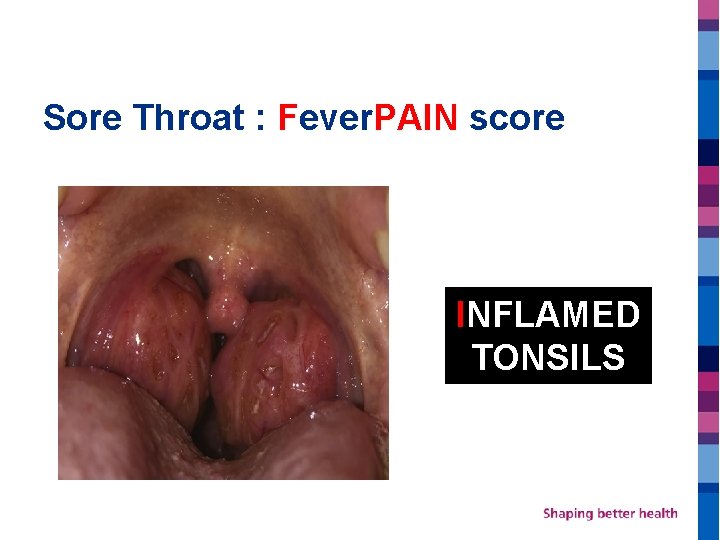
Sore Throat : Fever. PAIN score INFLAMED TONSILS
Sore Throat : Fever. PAIN score NO COUGH/CORYZA
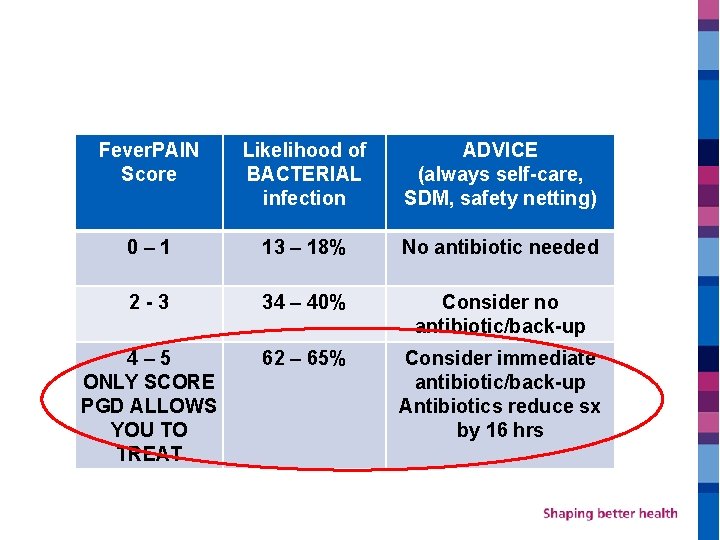
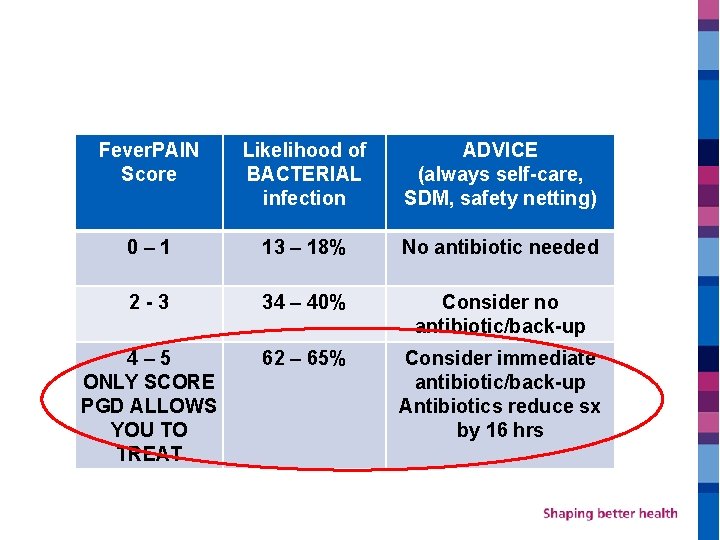
Fever. PAIN Score Likelihood of BACTERIAL infection ADVICE (always self-care, SDM, safety netting) 0– 1 13 – 18% No antibiotic needed 2 -3 34 – 40% Consider no antibiotic/back-up 4– 5 ONLY SCORE PGD ALLOWS YOU TO TREAT 62 – 65% Consider immediate antibiotic/back-up Antibiotics reduce sx by 16 hrs
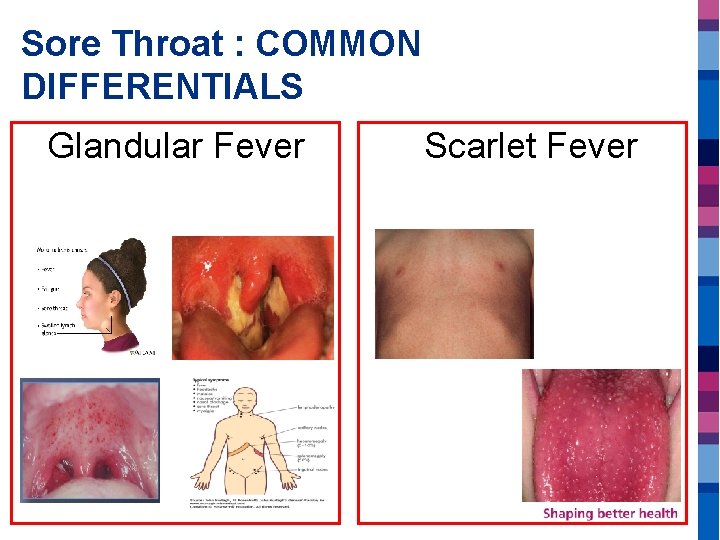
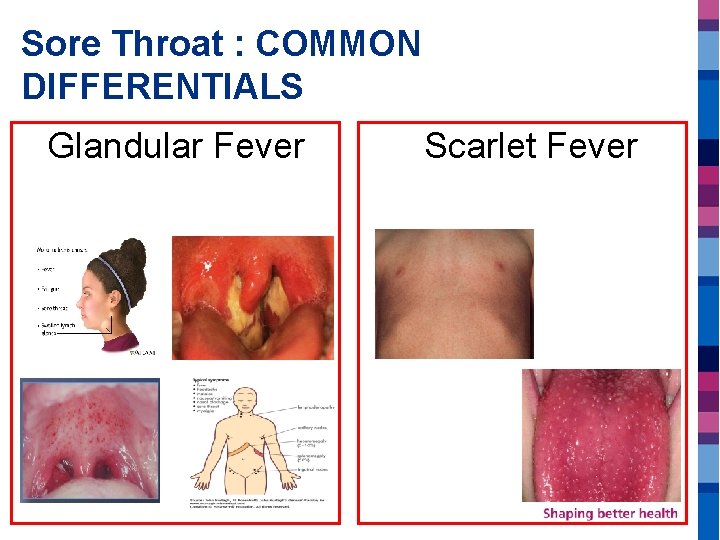
Sore Throat : COMMON DIFFERENTIALS Glandular Fever Scarlet Fever
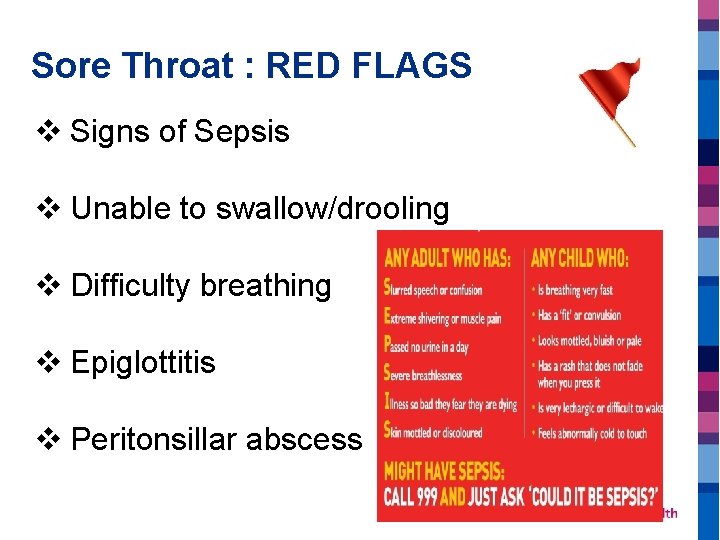
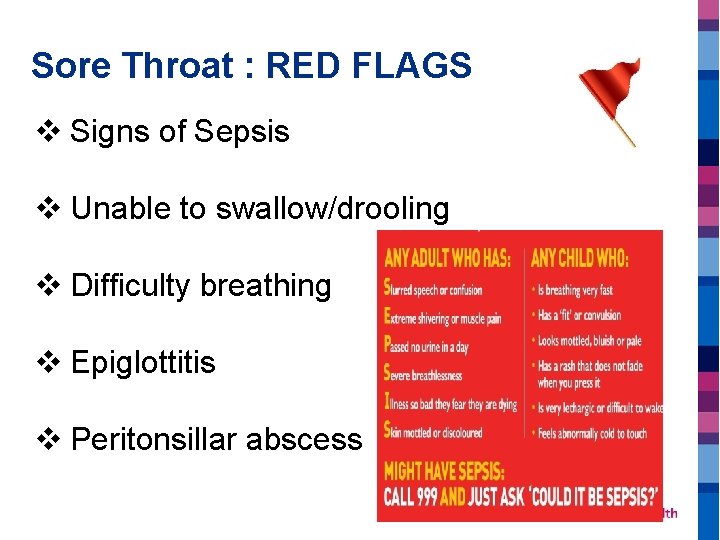
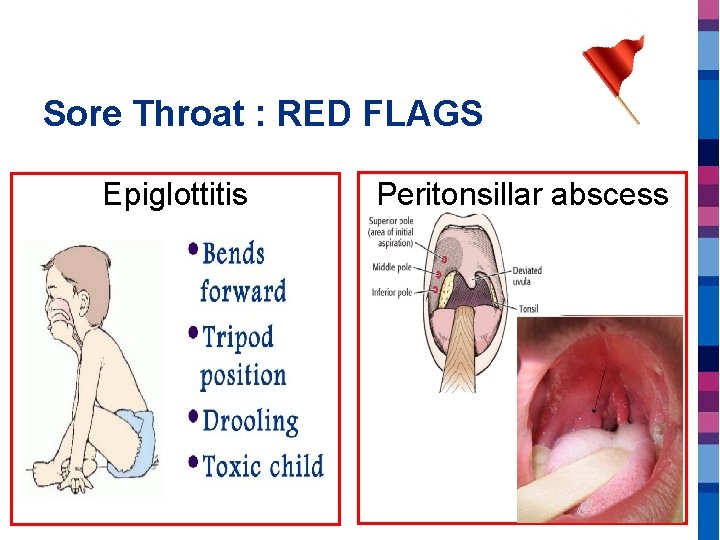
Sore Throat : RED FLAGS v Signs of Sepsis v Unable to swallow/drooling v Difficulty breathing v Epiglottitis v Peritonsillar abscess
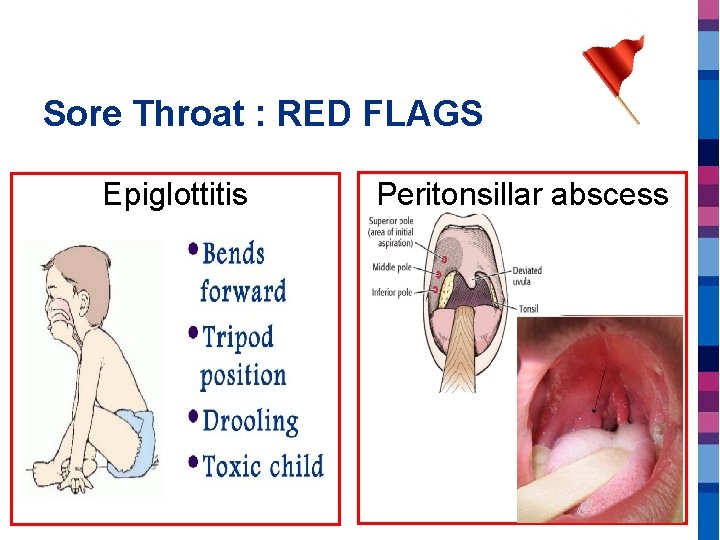
Sore Throat : RED FLAGS Epiglottitis Peritonsillar abscess
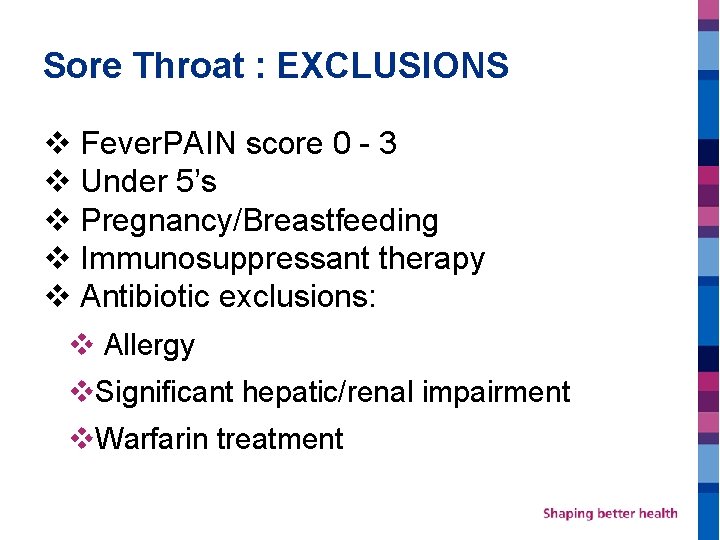
Sore Throat : EXCLUSIONS v Fever. PAIN score 0 - 3 v Under 5’s v Pregnancy/Breastfeeding v Immunosuppressant therapy v Antibiotic exclusions: v Allergy v. Significant hepatic/renal impairment v. Warfarin treatment
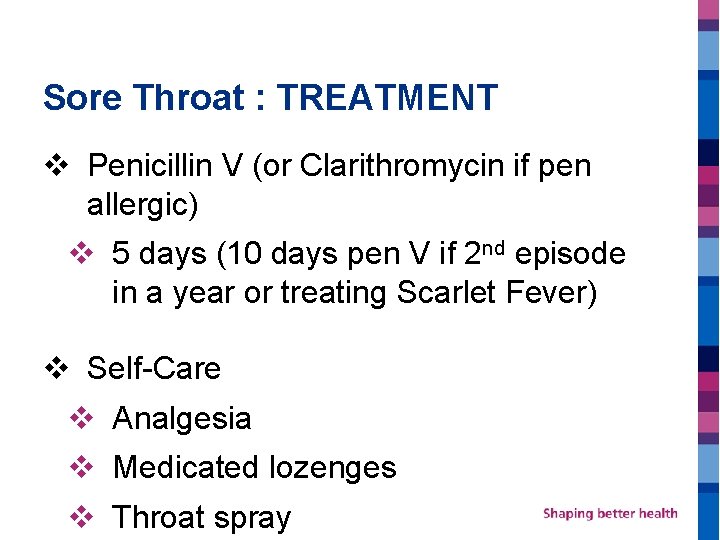
Sore Throat : TREATMENT v Penicillin V (or Clarithromycin if pen allergic) v 5 days (10 days pen V if 2 nd episode in a year or treating Scarlet Fever) v Self-Care v Analgesia v Medicated lozenges v Throat spray
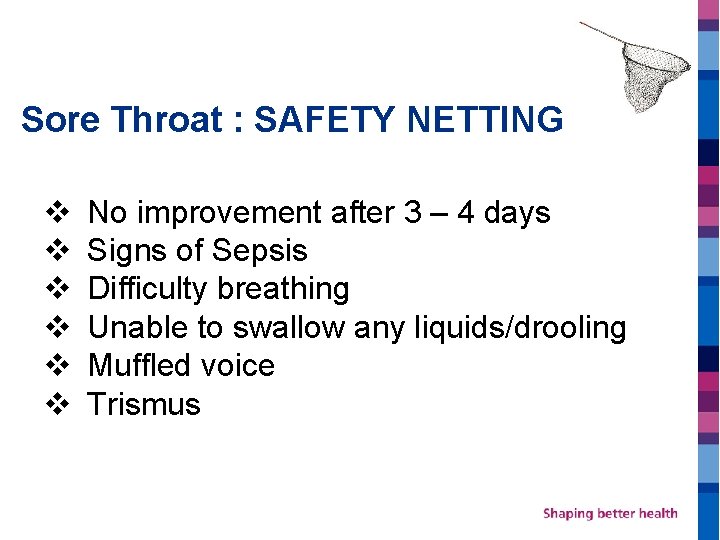
Sore Throat : SAFETY NETTING v No improvement after 3 – 4 days v Signs of Sepsis v Difficulty breathing v Unable to swallow any liquids/drooling v Muffled voice v Trismus
Sore Throat : RESOURCES v https: //www. nice. org. uk/guidance/ng 84/chapter/Re commendations v https: //cks. nice. org. uk/sore-throatacute#!diagnosis v https: //www. rcgp. org. uk/clinical-andresearch/resources/toolkits/amr/target-antibioticstoolkit//media/12992 E 5 D 00 BE 4709 BB 7 A 3112749 B 0279. ashx
PGD Training: Skin Dr Shaba Nabi GP Clinical Lead Prescribing Bristol, North Somerset, South Gloucestershire CCG









Hydrocortisone PGD v On FACE for aged 1 year and over v Anywhere on body aged under 10 years v Exclusions v Ano-genital application v Skin trauma v Pregnancy v Failed steroid treatment
Impetigo v Usually self-limiting v Caused by staph or strep v Stay off school until lesions healed over and dry or 48 hrs after antibiotic use

Impetigo - EXCLUSIONS v Under 2 years v Immunocompromised v Bullous Impetigo (30%)

Impetigo: RED FLAGS CELLULITIS

Impetigo: RED FLAGS LYMPHAN GITIS

Imetigo: RED FLAGS SCARLET FEVER

Imetigo: RED FLAGS ERYTHEMA MULTIFORME

Imetigo: RED FLAGS v Cellulitis v Lymphangitis v Scarlet Fever v Erythema Multiformae v Sepsis v Scalded Skin Syndrome v Osteomyelitis/Septic Arthritis v Acute Glomerulonephritis
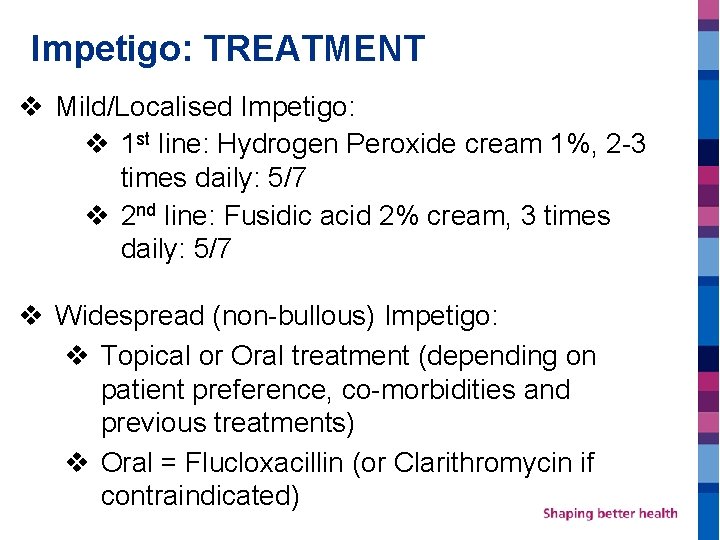
Impetigo: TREATMENT v Mild/Localised Impetigo: v 1 st line: Hydrogen Peroxide cream 1%, 2 -3 times daily: 5/7 v 2 nd line: Fusidic acid 2% cream, 3 times daily: 5/7 v Widespread (non-bullous) Impetigo: v Topical or Oral treatment (depending on patient preference, co-morbidities and previous treatments) v Oral = Flucloxacillin (or Clarithromycin if contraindicated)
RESOURCES https: //www. nice. org. uk/guidance/NG 153
Conjunctivitis Chloramphenicol PGD: Children aged 31 days or older, up to 2 years OTC sale: 2 years + Created by Helen Wilkinson
Symptoms • • Eyelid Oedema Watery Eye Gunky Mucus Red Eye Irritation Blurred Vision which clears with blinking Conjunctival Chemosis (swollen inner lining of eyelids) Subtarsal Erythema (red inner lid surface) • Classic presentation would be a sudden onset red eye, which causes a lot of watering, eye lid oedema and a sticky, gunky eye in the mornings • Within the first 48 hours it often transfers to the other eye and the second eye is always less affected as the patient’s immune system would have started mounting a defence
Bacterial or Viral Conjunctivitis? • Viral Conjunctivitis tends to cause more watering, more eyelid oedema and less mucus • May be associated with cough, cold, bilateral red eyes • Bacterial Conjunctivitis is generally more associated with less watering and more mucus production than viral conjunctivitis (purulent sticky discharge with red eye) • More likely to be unilateral but may spread to both eyes • Chlamydia/gonorrhoeal conjunctivitis tend to be unilateral and cause persistent symptoms. They can present as an emergency with significant eyelid swelling, hyper-purulence and reduced vision. Bristol Eye Hospital Ophthalmology Primary Care Advice 2020 https: //remedy. bnssgccg. nhs. uk/media/3861/ophthalmology-primary-care-advicefinal-12. pdf

Conjunctivitis Reference : Bristol Eye Hospital Ophthalmology Primary Care Advice 2020 https: //remedy. bnssgccg. nhs. uk/medi a/3861/ophthalmology-primary-careadvice-final-12. pdf
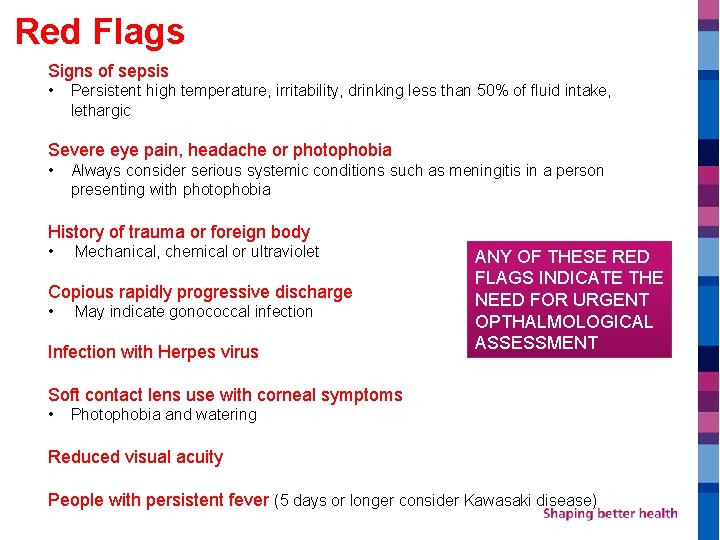
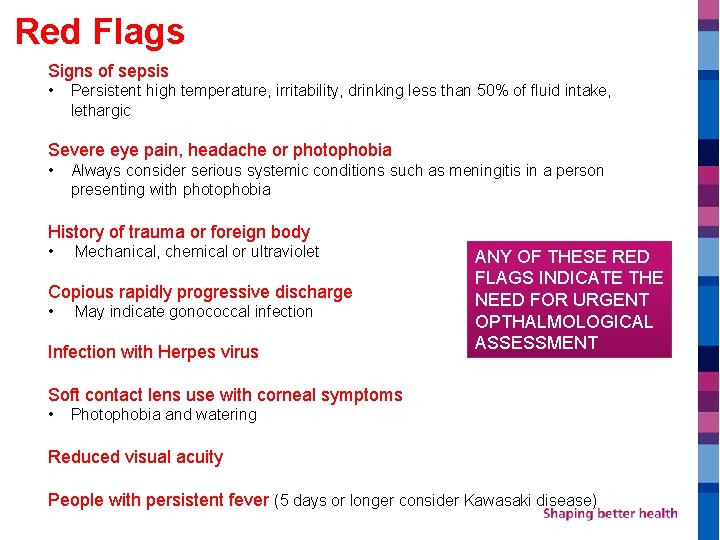
Red Flags Signs of sepsis • Persistent high temperature, irritability, drinking less than 50% of fluid intake, lethargic Severe eye pain, headache or photophobia • Always consider serious systemic conditions such as meningitis in a person presenting with photophobia History of trauma or foreign body • Mechanical, chemical or ultraviolet Copious rapidly progressive discharge • May indicate gonococcal infection Infection with Herpes virus ANY OF THESE RED FLAGS INDICATE THE NEED FOR URGENT OPTHALMOLOGICAL ASSESSMENT Soft contact lens use with corneal symptoms • Photophobia and watering Reduced visual acuity People with persistent fever (5 days or longer consider Kawasaki disease)
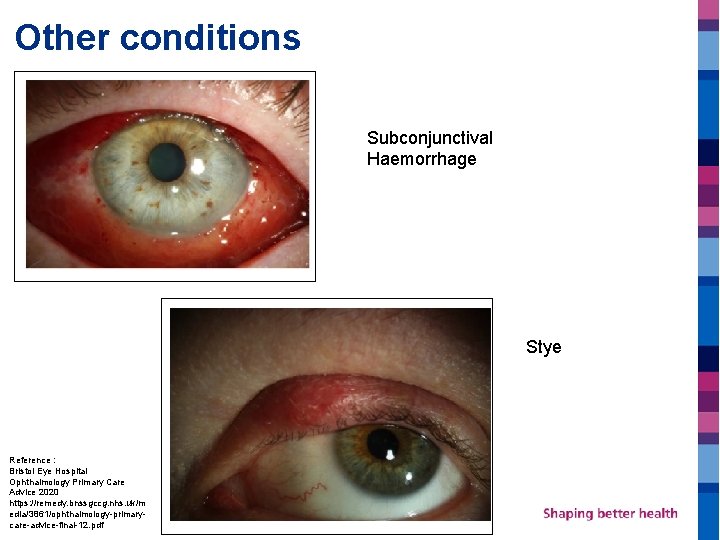
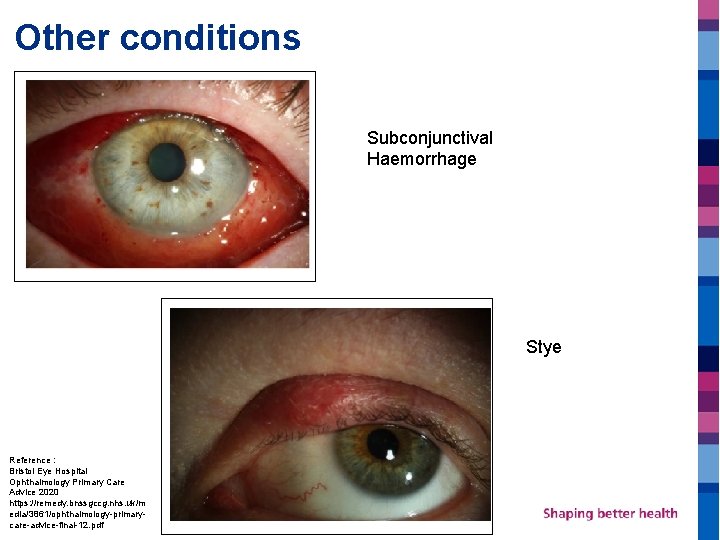
Other conditions Subconjunctival Haemorrhage Stye Reference : Bristol Eye Hospital Ophthalmology Primary Care Advice 2020 https: //remedy. bnssgccg. nhs. uk/m edia/3861/ophthalmology-primarycare-advice-final-12. pdf

Reference : Bristol Eye Hospital Ophthalmology Primary Care Advice 2020 https: //remedy. bnssgccg. nhs. uk/media/3861/ophthalmology-primary-care-advice-final-12. pdf
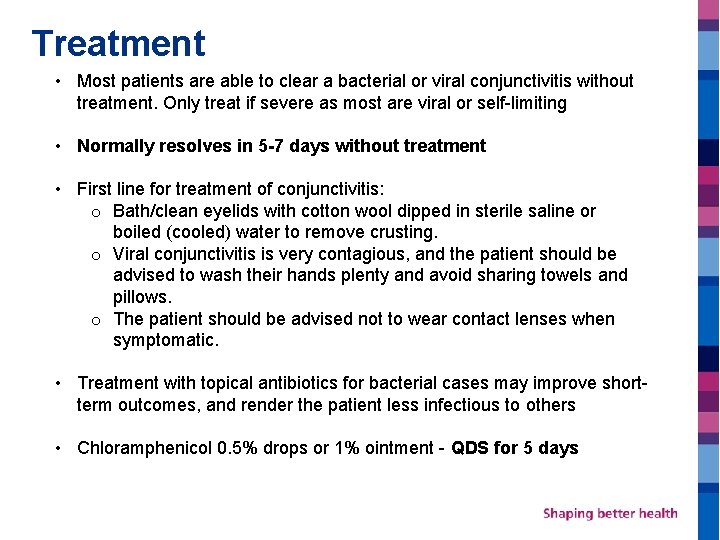
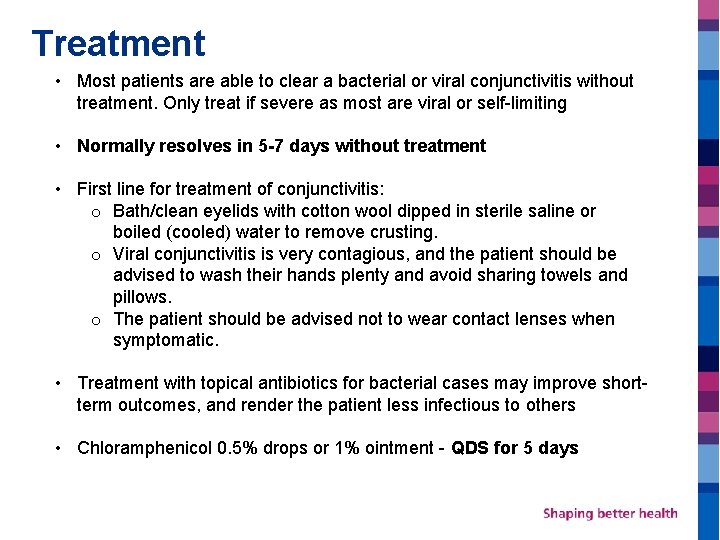
Treatment • Most patients are able to clear a bacterial or viral conjunctivitis without treatment. Only treat if severe as most are viral or self-limiting • Normally resolves in 5 -7 days without treatment • First line for treatment of conjunctivitis: o Bath/clean eyelids with cotton wool dipped in sterile saline or boiled (cooled) water to remove crusting. o Viral conjunctivitis is very contagious, and the patient should be advised to wash their hands plenty and avoid sharing towels and pillows. o The patient should be advised not to wear contact lenses when symptomatic. • Treatment with topical antibiotics for bacterial cases may improve shortterm outcomes, and render the patient less infectious to others • Chloramphenicol 0. 5% drops or 1% ointment - QDS for 5 days
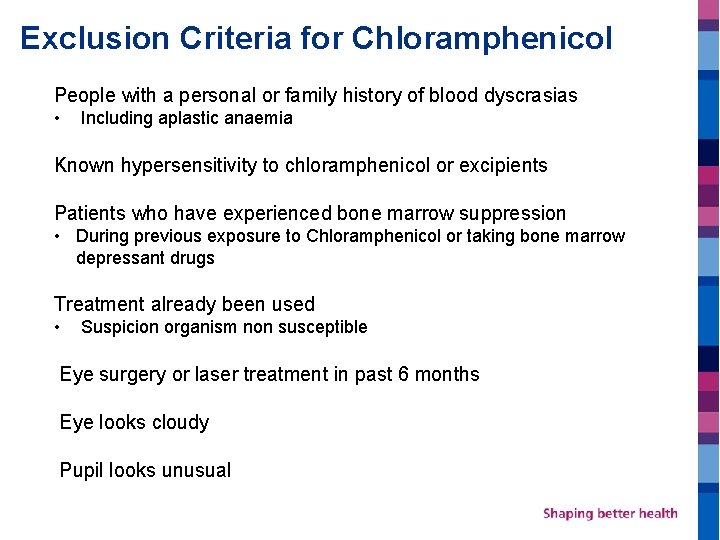
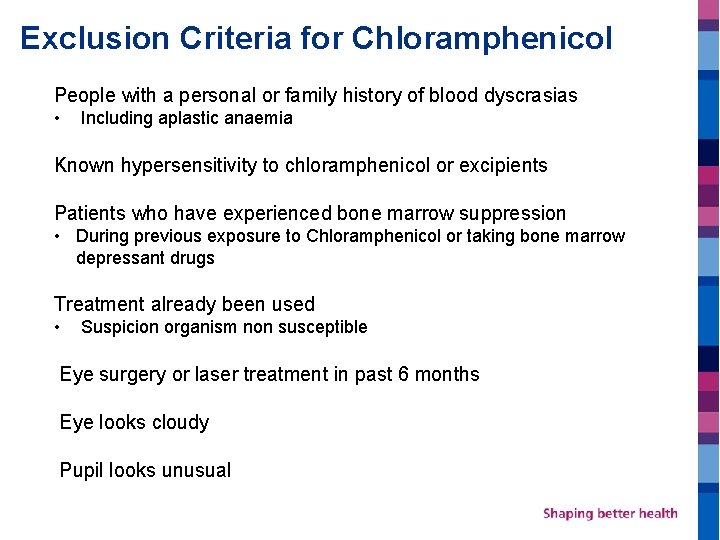
Exclusion Criteria for Chloramphenicol People with a personal or family history of blood dyscrasias • Including aplastic anaemia Known hypersensitivity to chloramphenicol or excipients Patients who have experienced bone marrow suppression • During previous exposure to Chloramphenicol or taking bone marrow depressant drugs Treatment already been used • Suspicion organism non susceptible Eye surgery or laser treatment in past 6 months Eye looks cloudy Pupil looks unusual
Information & Safety Netting • Identification and management of adverse reactions • Supply of PIL • Self care advice • Safety netting - Failure of treatment after 5 days • Also consider exclusion criteria & red flags School/Nursery Public Health England does not recommend school exclusion for children with conjunctivitis (please see https: //www. publichealth. hscni. net/sites/default/files/Guidance_on_inf ection_control_in%20 schools_poster. pdf).
Any questions?
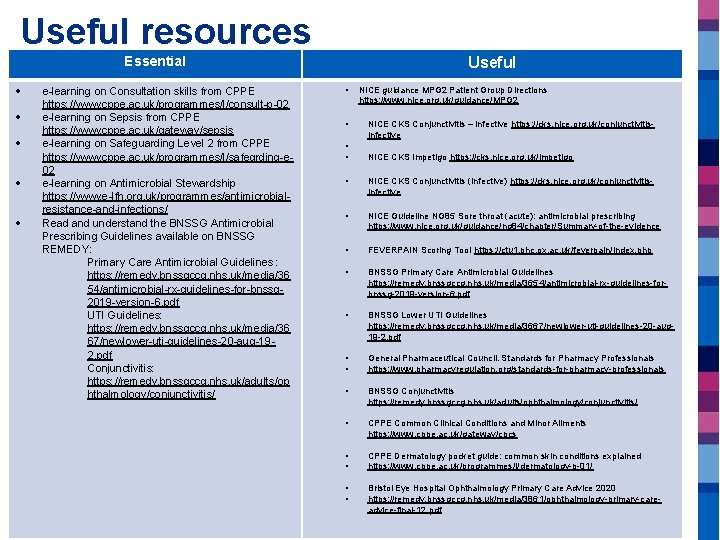
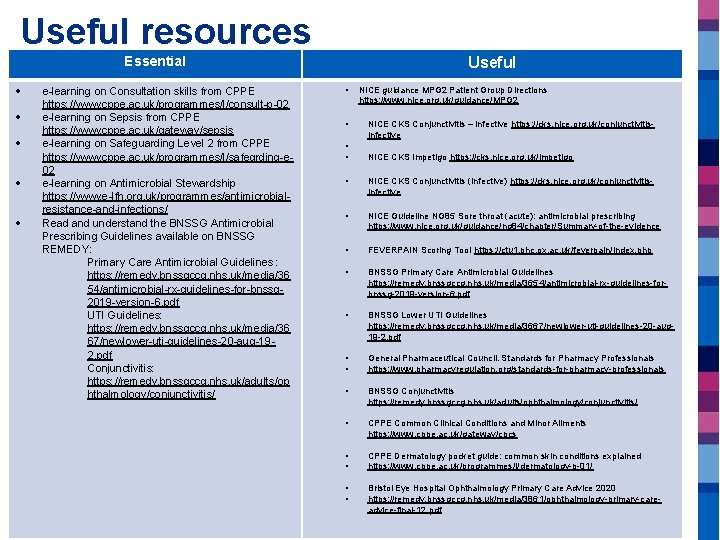
Useful resources Essential e-learning on Consultation skills from CPPE https: //www. cppe. ac. uk/programmes/l/consult-p-02 e-learning on Sepsis from CPPE https: //www. cppe. ac. uk/gateway/sepsis e-learning on Safeguarding Level 2 from CPPE https: //www. cppe. ac. uk/programmes/l/safegrding-e 02 e-learning on Antimicrobial Stewardship https: //www. e-lfh. org. uk/programmes/antimicrobialresistance-and-infections/ Read and understand the BNSSG Antimicrobial Prescribing Guidelines available on BNSSG REMEDY: Primary Care Antimicrobial Guidelines : https: //remedy. bnssgccg. nhs. uk/media/36 54/antimicrobial-rx-guidelines-for-bnssg 2019 -version-6. pdf UTI Guidelines: https: //remedy. bnssgccg. nhs. uk/media/36 67/newlower-uti-guidelines-20 -aug-192. pdf Conjunctivitis: https: //remedy. bnssgccg. nhs. uk/adults/op hthalmology/conjunctivitis/ Useful • • NICE guidance MPG 2 Patient Group Directions https: //www. nice. org. uk/guidance/MPG 2 NICE CKS Conjunctivitis – infective https: //cks. nice. org. uk/conjunctivitisinfective NICE CKS Impetigo https: //cks. nice. org. uk/impetigo • NICE CKS Conjunctivitis (Infective) https: //cks. nice. org. uk/conjunctivitisinfective • NICE Guideline NG 85 Sore throat (acute): antimicrobial prescribing https: //www. nice. org. uk/guidance/ng 84/chapter/Summary-of-the-evidence • FEVERPAIN Scoring Tool https: //ctu 1. phc. ox. ac. uk/feverpain/index. php • BNSSG Primary Care Antimicrobial Guidelines https: //remedy. bnssgccg. nhs. uk/media/3654/antimicrobial-rx-guidelines-forbnssg-2019 -version-6. pdf • BNSSG Lower UTI Guidelines https: //remedy. bnssgccg. nhs. uk/media/3667/newlower-uti-guidelines-20 -aug 19 -2. pdf • • General Pharmaceutical Council. Standards for Pharmacy Professionals https: //www. pharmacyregulation. org/standards-for-pharmacy-professionals • BNSSG Conjunctivitis https: //remedy. bnssgccg. nhs. uk/adults/ophthalmology/conjunctivitis/ • CPPE Common Clinical Conditions and Minor Ailments https: //www. cppe. ac. uk/gateway/cpcs • • CPPE Dermatology pocket guide: common skin conditions explained https: //www. cppe. ac. uk/programmes/l/dermatology-p-01/ • • Bristol Eye Hospital Ophthalmology Primary Care Advice 2020 https: //remedy. bnssgccg. nhs. uk/media/3861/ophthalmology-primary-careadvice-final-12. pdf
 Difference between minor arc and major arc
Difference between minor arc and major arc Helen midtown computer solutions helen speaking
Helen midtown computer solutions helen speaking Helen midtown computer solutions helen speaking
Helen midtown computer solutions helen speaking Gaji pgds
Gaji pgds Pgds kemenkes
Pgds kemenkes Pgds dokter spesialis
Pgds dokter spesialis Compatibil determinat
Compatibil determinat Sheldon wilkinson
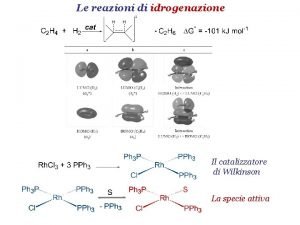
Sheldon wilkinson Catalizzatore di wilkinson
Catalizzatore di wilkinson Dave wilkinson model
Dave wilkinson model Adc
Adc Wilkinson exo
Wilkinson exo Divisor de potencia wilkinson
Divisor de potencia wilkinson Fabio wilkinson
Fabio wilkinson Daryl wilkinson
Daryl wilkinson Esther wilkinson
Esther wilkinson Wilkinson genderquake sociology
Wilkinson genderquake sociology Charlene wilkinson
Charlene wilkinson Characters billy elliot
Characters billy elliot Wilkinson adc converter
Wilkinson adc converter Murray wilkinson
Murray wilkinson Hydrognation
Hydrognation Wilkinson polynomial matlab
Wilkinson polynomial matlab Introduction to community pharmacy
Introduction to community pharmacy Pharmacy contractual framework
Pharmacy contractual framework Community pharmacy topics
Community pharmacy topics Community pharmacy forward view
Community pharmacy forward view Nhs community pharmacy contractual framework
Nhs community pharmacy contractual framework Types of community pharmacies include
Types of community pharmacies include Community pharmacy forward view
Community pharmacy forward view Community pharmacy enhanced services network
Community pharmacy enhanced services network Definition and scope of pharmacy
Definition and scope of pharmacy Objectives of a community pharmacy
Objectives of a community pharmacy Läkarutlåtande för livränta
Läkarutlåtande för livränta Treserva lathund
Treserva lathund Påbyggnader för flakfordon
Påbyggnader för flakfordon Tack för att ni lyssnade
Tack för att ni lyssnade En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Egg för emanuel
Egg för emanuel Atmosfr
Atmosfr Rutin för avvikelsehantering
Rutin för avvikelsehantering Mitos steg
Mitos steg Lågenergihus nyproduktion
Lågenergihus nyproduktion Presentera för publik crossboss
Presentera för publik crossboss Myndigheten för delaktighet
Myndigheten för delaktighet Debatt artikel mall
Debatt artikel mall Kung dog 1611
Kung dog 1611 Vad är densitet
Vad är densitet Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Tack för att ni har lyssnat
Tack för att ni har lyssnat Vad är referatmarkeringar
Vad är referatmarkeringar Frger
Frger Epiteltyper
Epiteltyper Rbk mätning
Rbk mätning Formel för lufttryck
Formel för lufttryck Vilket tal pekar pilen på
Vilket tal pekar pilen på Adressändring ideell förening
Adressändring ideell förening Elektronik för barn
Elektronik för barn Borra hål för knoppar
Borra hål för knoppar Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Bris för vuxna
Bris för vuxna Vad är ett minoritetsspråk
Vad är ett minoritetsspråk Frgar
Frgar För och nackdelar med firo
För och nackdelar med firo Ellika andolf
Ellika andolf Datorkunskap för nybörjare
Datorkunskap för nybörjare Steg för steg rita
Steg för steg rita Blomman för dagen drog
Blomman för dagen drog Ekologiskt fotavtryck
Ekologiskt fotavtryck Redogör för vad psykologi är
Redogör för vad psykologi är Bra mat för unga idrottare
Bra mat för unga idrottare Geometriska former i förskolan
Geometriska former i förskolan Bästa kameran för astrofoto
Bästa kameran för astrofoto Lyrik dikt
Lyrik dikt Ledarskapsteorier
Ledarskapsteorier Svenskt ramverk för digital samverkan
Svenskt ramverk för digital samverkan Vad kallas den mantel som bars av kvinnor i antikens rom
Vad kallas den mantel som bars av kvinnor i antikens rom Vilotidsbok
Vilotidsbok Formuö
Formuö Vilken grundregel finns det för tronföljden i sverige?
Vilken grundregel finns det för tronföljden i sverige? Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Jätte råtta
Jätte råtta Plats för toran ark
Plats för toran ark Sju principer för tillitsbaserad styrning
Sju principer för tillitsbaserad styrning Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Romarriket tidslinje
Romarriket tidslinje Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Mästar lärling modellen
Mästar lärling modellen Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? Stål för stötfångarsystem
Stål för stötfångarsystem Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Shivaismen
Shivaismen Centrum för kunskap och säkerhet
Centrum för kunskap och säkerhet Inköpsprocessen steg för steg
Inköpsprocessen steg för steg Aktiv expektans
Aktiv expektans Jag har nigit för nymånens skära text
Jag har nigit för nymånens skära text Strategi för svensk viltförvaltning
Strategi för svensk viltförvaltning Sura för anatom
Sura för anatom Vad är verksamhetsanalys
Vad är verksamhetsanalys Typiska drag för en novell
Typiska drag för en novell Stickprovsvarians
Stickprovsvarians Tack för att ni har lyssnat
Tack för att ni har lyssnat