INTRODUCTION TO COMMUNITY PHARMACY COMMUNITY PHARMACY Community pharmacists
- Slides: 17
INTRODUCTION TO COMMUNITY PHARMACY
COMMUNITY PHARMACY �Community pharmacists are the most accessible healthcare professional. �No appointment is needed to consult a pharmacist and patients can receive free, unbiased advice almost anywhere.
Continued �A community pharmacist is often the first health professional the patient seeks advice from and, as such, provides a filtering mechanism whereby minor self-limiting conditions can be appropriately treated with the correct medication and patients with more sinister pathology referred on to the GP for further investigation. �On a typical day a pharmacist practicing in an 'average‘ community pharmacy can realistically expect to help between 5 and 15 patients a day who present with various
Continued �Current UK health policy, and that of other Western countries, of making more medicines available has promoted patient self-care, and with it a greater role for Community pharmacists. �The UK over-the-counter (OTC) medicines market has seen considerable growth over the last few years, and in 2010 was worth over £ 2. 3 billion. �The upward sales trend for OTC medicines, the UK government's continued promotion of self-care and ever increasing demands on primary healthcare services means that ore medicines have, and will
COMMUNICATION SKILLS �The ability of the community pharmacist to diagnose the patient's presenting signs and symptoms is a significant challenge. �Given that, unlike most other healthcare professionals, community pharmacists do not normally have access to the patient's medical record and thus have no idea about what the person's problem is until a conversation is initiated.
Continued �For the most part, pharmacists will be totally dependent on their ability to question patients in order to arrive at a differential diagnosis. �This is in stark contrast to the GP and to a lesser extent the nurse, who can draw on physical examination and diagnostic tests to help them arrive at a diagnosis.
Continued – limitations!! �Whilst pharmacists could (and some argue should) perform simple physical examinations, most do not, due to the lack of training they receive; diagnostic testing is never employed because of the cost (which would have to be passed on to the patient), the invasive nature of most tests (e. g. blood taking for analysis) and the lack of immediacy in gaining test results.
Continued �Having said this, a number of studies have shown that patient history taking is by far the most important element of arriving at a correct diagnosis. �Although performing physical examinations and conducting laboratory investigations do improve the odds of getting the diagnosis right.
Continued �It is vital, therefore, that pharmacists possess excellent communication skills to ensure the correct information is obtained from the patient. �This will be drawn from a combination of good questioning technique, listening actively to the patient and picking up on non-verbal cues.
CLINICAL REASONING �Whether we are conscious of it or not, most people will - at some level - use clinical reasoning to arrive at a differential diagnosis. �Clinical reasoning relates to the decision-making processes associated with clinical practice. �It is a thinking process directed towards enabling the pharmacist to take appropriate action in a specific context.
Continued �It fundamentally differs from using acronyms in that it is built around clinical knowledge and skills that are applied to the individual patient. �It involves recognition of cues and analysis of data. �Very early in a clinical encounter, and based on limited information, the person
Continued �The pharmacist then sets about testing these hypotheses by asking the patient a series of questions. �The answer to each question allows the pharmacist to narrow down the possible diagnosis by either eliminating particular conditions or confirming his or her suspicions of a particular condition. �Once the questioning is over, the pharmacist should be in a position to differentially diagnose
Continued �In addition, clinical experience (pattern recognition) also plays a part in the process. �Certain conditions have very characteristic presentations and, once seen, it is a relatively straightforward task to diagnose the next case by recalling the appearance of the rash. �Therefore, much of daily practice will consist of seeing new cases that strongly resemble previous encounters and comparing new cases to old.
Key steps in the process 1. Formulating a diagnosis based on the patient and the initial presenting complaint 2. Asking questions 3. Confirm facts
Key Steps In The Process 1. Formulating a diagnosis based on the patient and the initial presenting complaint à Before any questions are asked of the patient you should consider who the patient is and how this may influence your thinking. à General appearance of the patient, age, sex, complaint.
Key Steps In The Process 2. Asking questions àThe questions you ask the patient will be specific to that patient. After establishing who the person is, how poorly he or she is and what the presenting complaint is, a number of targeted questions specific to that patient should be asked. �Finally, even though at this stage you are conf 1 dent of your differential diagnosis you should still ask a couple of questions to rule out any sinister pathology. �Obviously you are expecting the answers from these questions to be negative to support your
Key Steps In The Process 3. Confirm facts � Before making a recommendation to the patient it is always helpful to try and re-cap on the information elicited. This is especially important when you have had to ask a lot of questions. It is well known that short-term working memory is relatively small and that remembering all the pertinent facts is difficult. � Summarising the information at this stage will not only help you formulate your final diagnosis but will also allow the patient to add further information or correct you on facts that you have failed to remember correctly. � Using a clinical reasoning approach to differential diagnosis allows you to build a fuller picture of the patient's presenting complaint. It is both flexible and specific to each individual.
 Colorado pharmacists society
Colorado pharmacists society The apprentice pharmacist
The apprentice pharmacist Introduction to community pharmacy
Introduction to community pharmacy Emergency cart drugs
Emergency cart drugs Community pharmacy forward view
Community pharmacy forward view Objectives of a community pharmacy
Objectives of a community pharmacy Type of community pharmacy
Type of community pharmacy Community pharmacy enhanced services network
Community pharmacy enhanced services network Community pharmacy contractual framework
Community pharmacy contractual framework Nhs community pharmacy contractual framework
Nhs community pharmacy contractual framework Define clinical pharmacy
Define clinical pharmacy Community pharmacy forward view
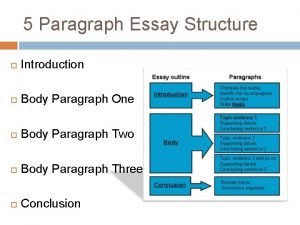
Community pharmacy forward view Introduction paragraph format
Introduction paragraph format Introduction of community policing
Introduction of community policing Introduction to community medicine
Introduction to community medicine Introduction to community medicine
Introduction to community medicine Characteristics of community health nursing
Characteristics of community health nursing An introduction to community asset mapping
An introduction to community asset mapping