RESPIRATORY FAILURE Mikls Molnr Semmelweis University Institute of








- Slides: 126
RESPIRATORY FAILURE Miklós Molnár Semmelweis University Institute of Pathophysiology 2005
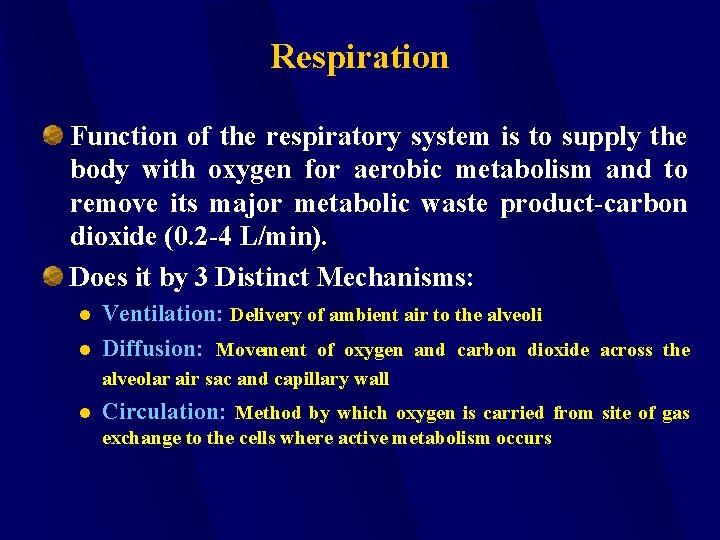
Respiration Function of the respiratory system is to supply the body with oxygen for aerobic metabolism and to remove its major metabolic waste product-carbon dioxide (0. 2 -4 L/min). Does it by 3 Distinct Mechanisms: l l Ventilation: Delivery of ambient air to the alveoli Diffusion: Movement of oxygen and carbon dioxide across the alveolar air sac and capillary wall l Circulation: Method by which oxygen is carried from site of gas exchange to the cells where active metabolism occurs
Respiration Is dependent on vital links of various anatomic subcomponents
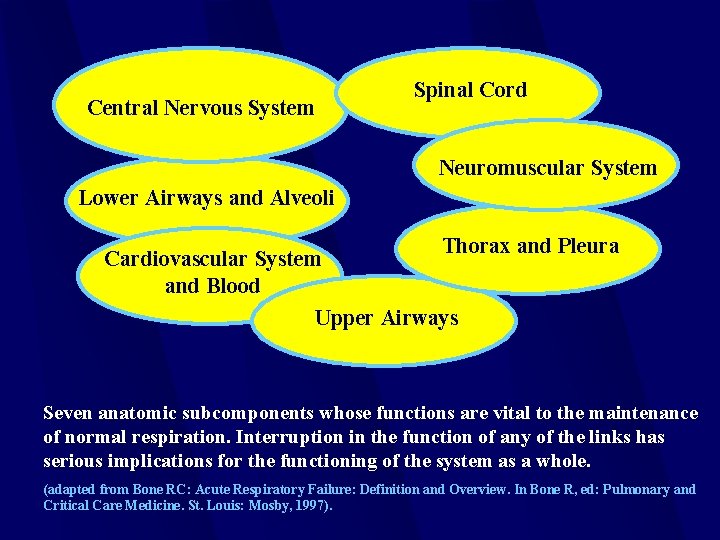
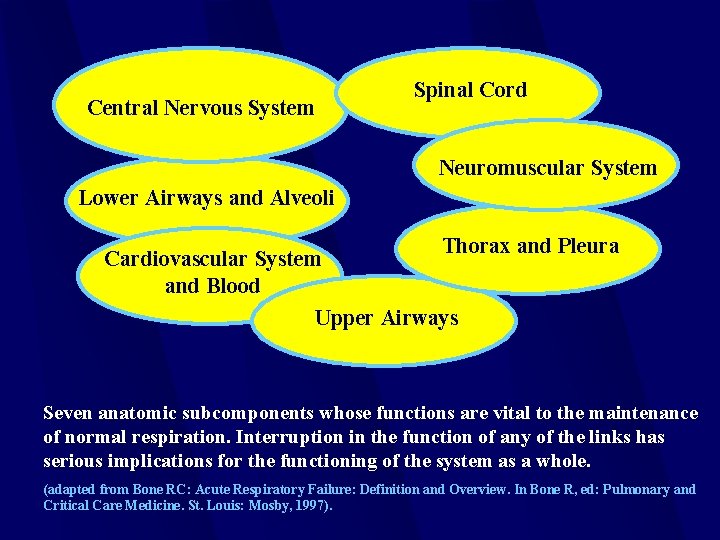
Central Nervous System Spinal Cord Neuromuscular System Lower Airways and Alveoli Thorax and Pleura Cardiovascular System and Blood Upper Airways Seven anatomic subcomponents whose functions are vital to the maintenance of normal respiration. Interruption in the function of any of the links has serious implications for the functioning of the system as a whole. (adapted from Bone RC: Acute Respiratory Failure: Definition and Overview. In Bone R, ed: Pulmonary and Critical Care Medicine. St. Louis: Mosby, 1997).
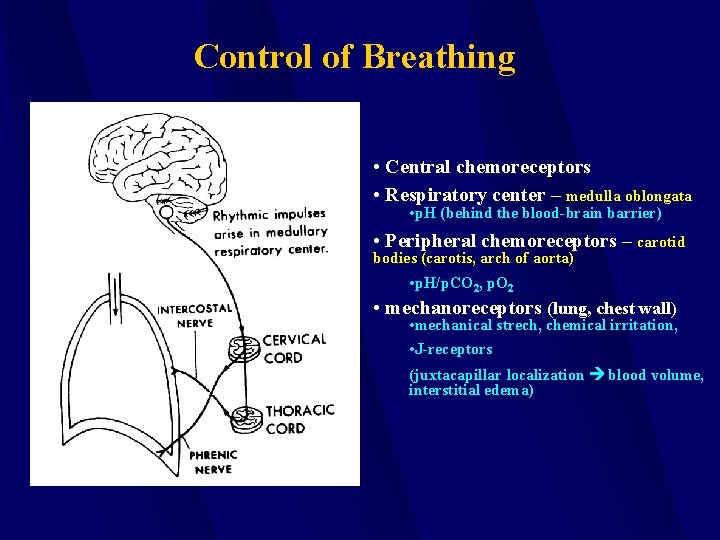
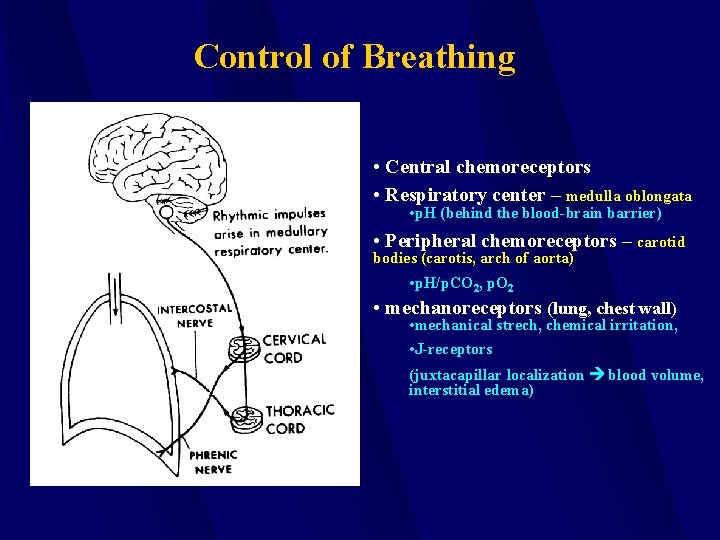
Control of Breathing • Central chemoreceptors • Respiratory center – medulla oblongata • p. H (behind the blood-brain barrier) • Peripheral chemoreceptors – carotid bodies (carotis, arch of aorta) • p. H/p. CO 2, p. O 2 • mechanoreceptors (lung, chest wall) • mechanical strech, chemical irritation, • J-receptors (juxtacapillar localization blood volume, interstitial edema)

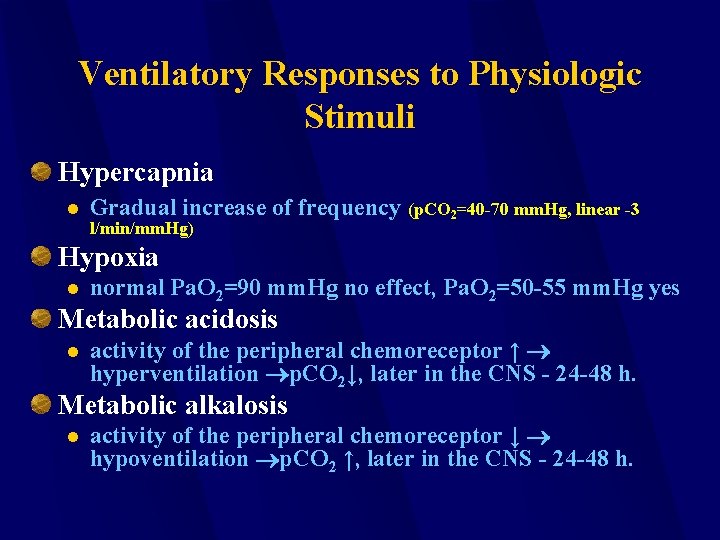
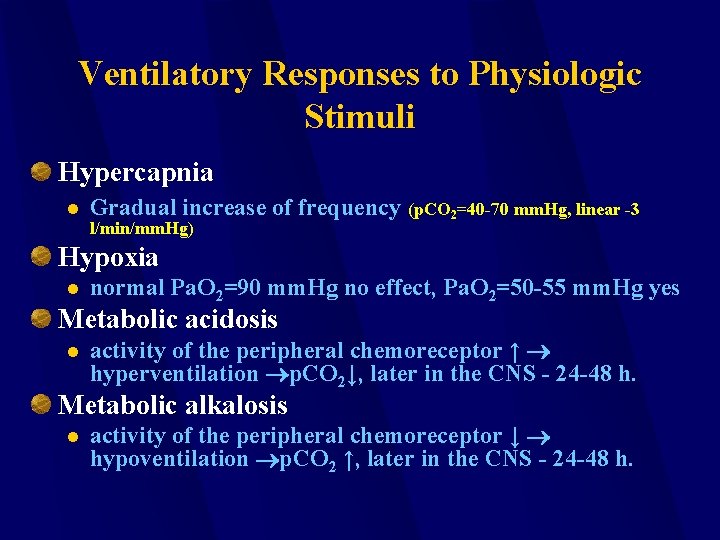
Ventilatory Responses to Physiologic Stimuli Hypercapnia l Gradual increase of frequency (p. CO 2=40 -70 mm. Hg, linear -3 l/min/mm. Hg) Hypoxia l normal Pa. O 2=90 mm. Hg no effect, Pa. O 2=50 -55 mm. Hg yes Metabolic acidosis l activity of the peripheral chemoreceptor ↑ hyperventilation p. CO 2↓, later in the CNS - 24 -48 h. Metabolic alkalosis l activity of the peripheral chemoreceptor ↓ hypoventilation p. CO 2 ↑, later in the CNS - 24 -48 h.
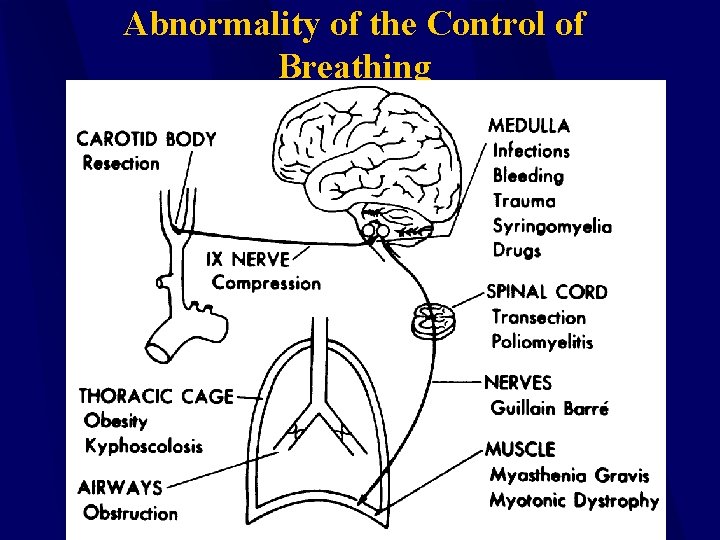
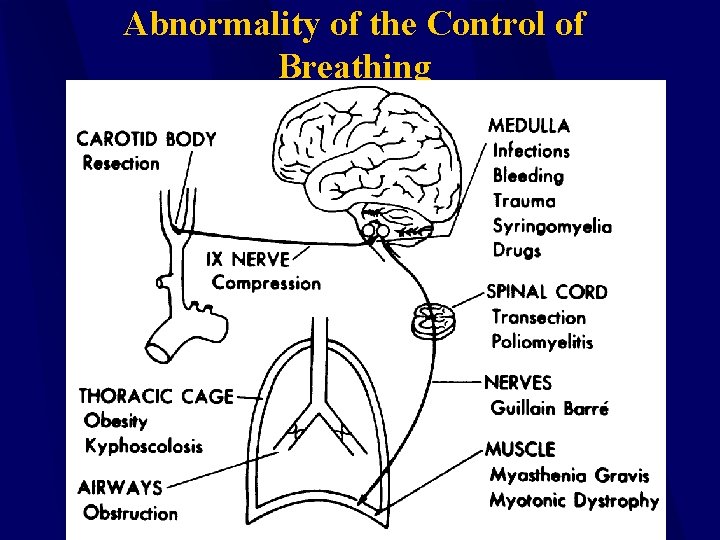
Abnormality of the Control of Breathing
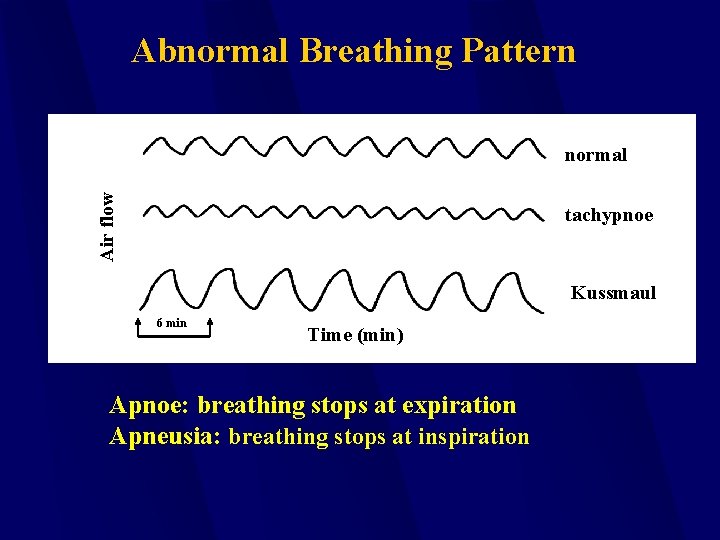
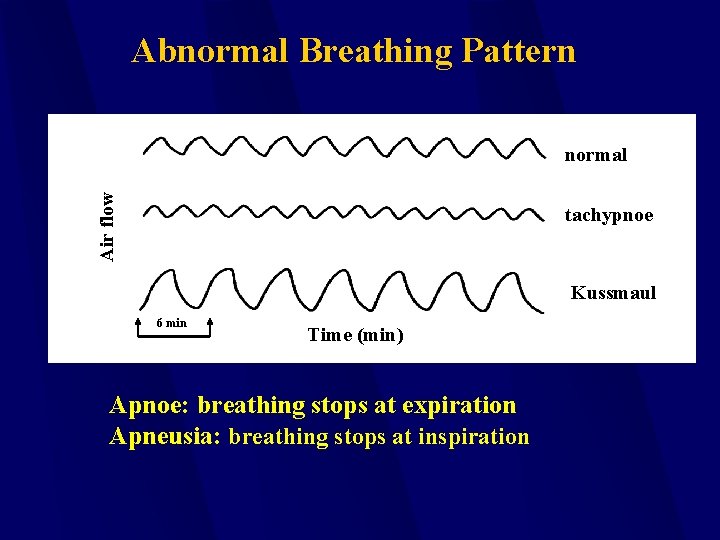
Abnormal Breathing Pattern Air flow normal tachypnoe Kussmaul 6 min Time (min) Apnoe: breathing stops at expiration Apneusia: breathing stops at inspiration
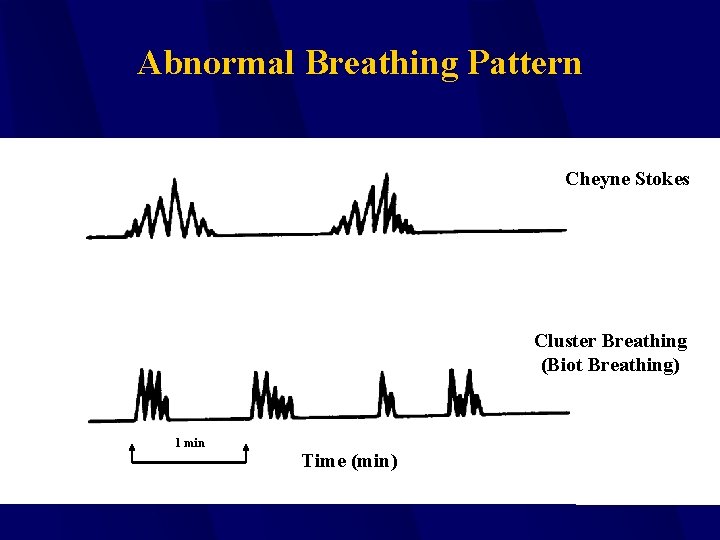
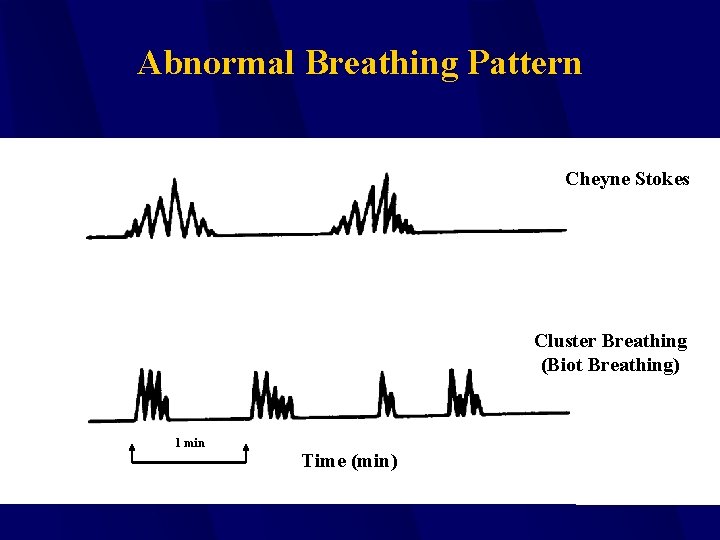
Abnormal Breathing Pattern Cheyne Stokes Cluster Breathing (Biot Breathing) 1 min Time (min)
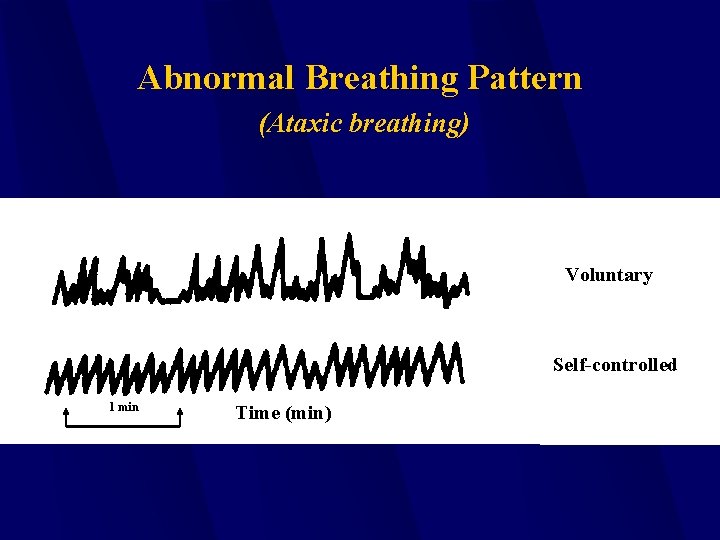
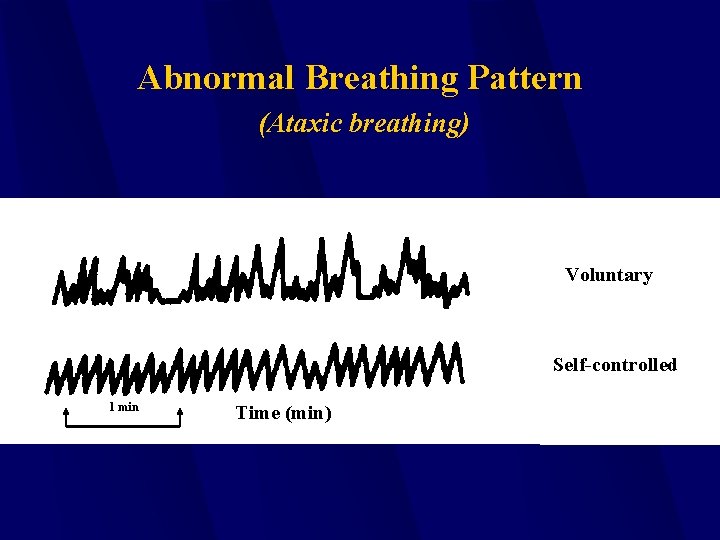
Abnormal Breathing Pattern (Ataxic breathing) Voluntary Self-controlled 1 min Time (min)
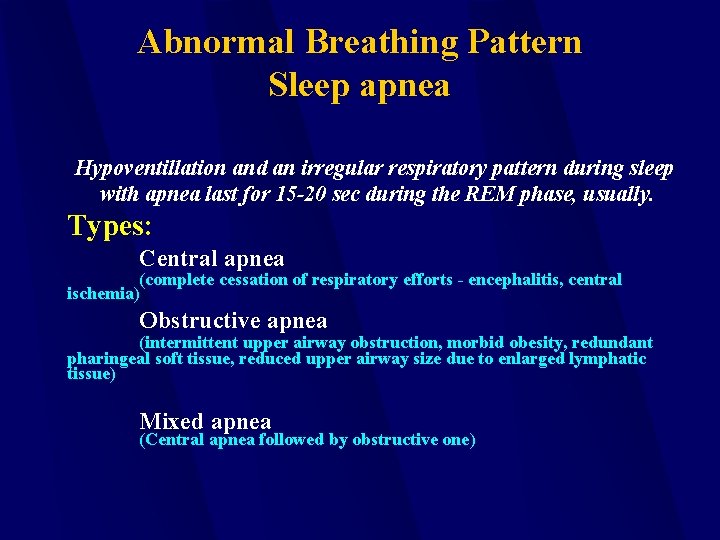
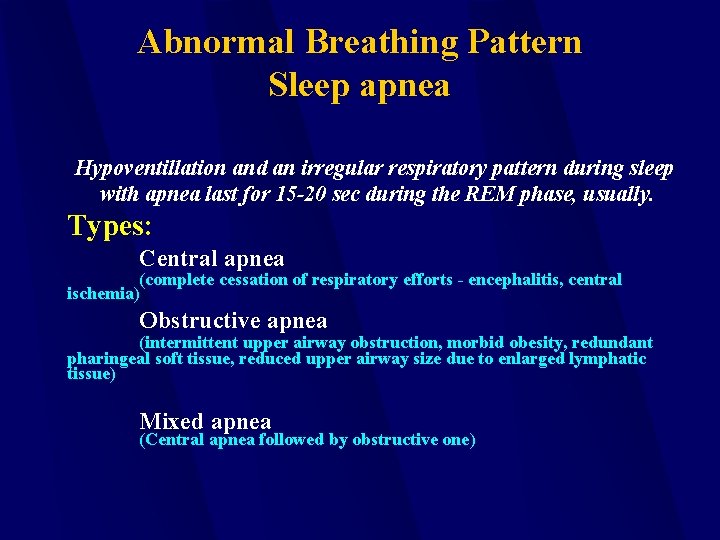
Abnormal Breathing Pattern Sleep apnea Hypoventillation and an irregular respiratory pattern during sleep with apnea last for 15 -20 sec during the REM phase, usually. Types: Central apnea (complete cessation of respiratory efforts - encephalitis, central ischemia) Obstructive apnea (intermittent upper airway obstruction, morbid obesity, redundant pharingeal soft tissue, reduced upper airway size due to enlarged lymphatic tissue) Mixed apnea (Central apnea followed by obstructive one)
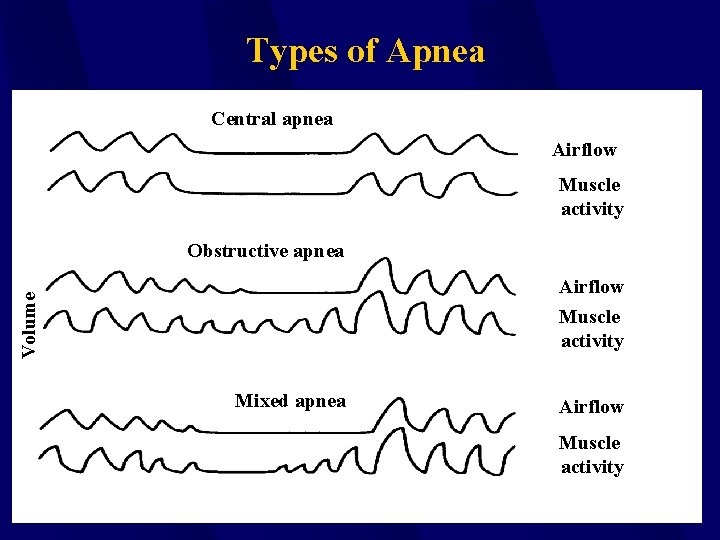
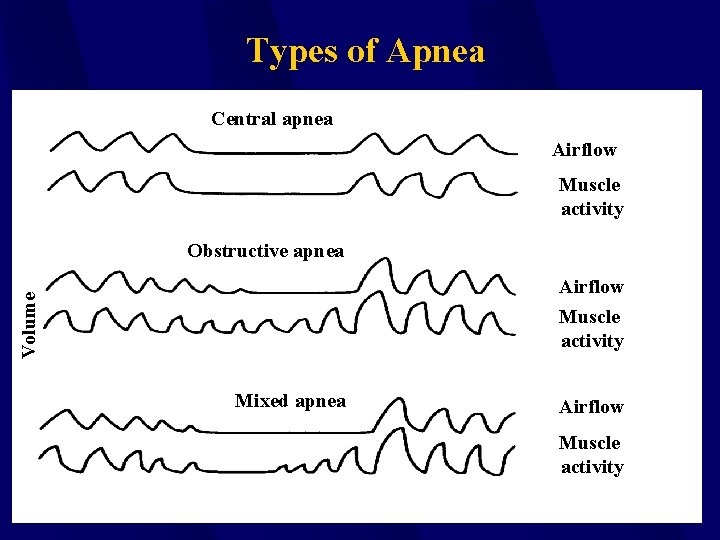
Types of Apnea Central apnea Airflow Muscle activity Obstructive apnea Volume Airflow Muscle activity Mixed apnea Airflow Muscle activity
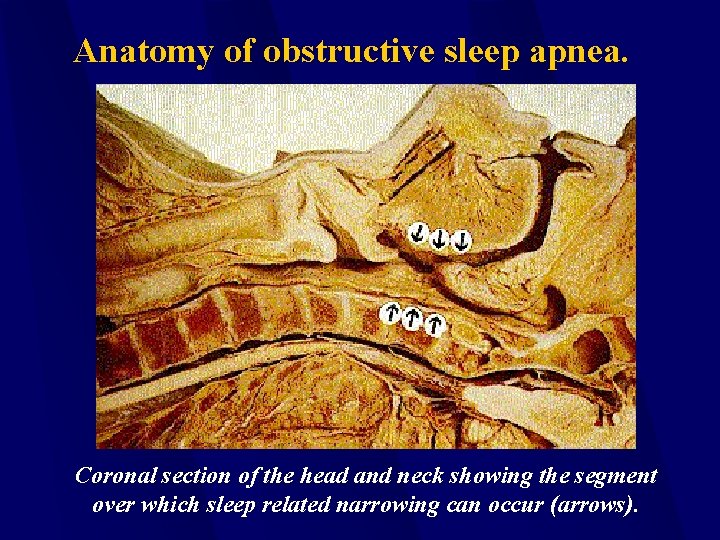
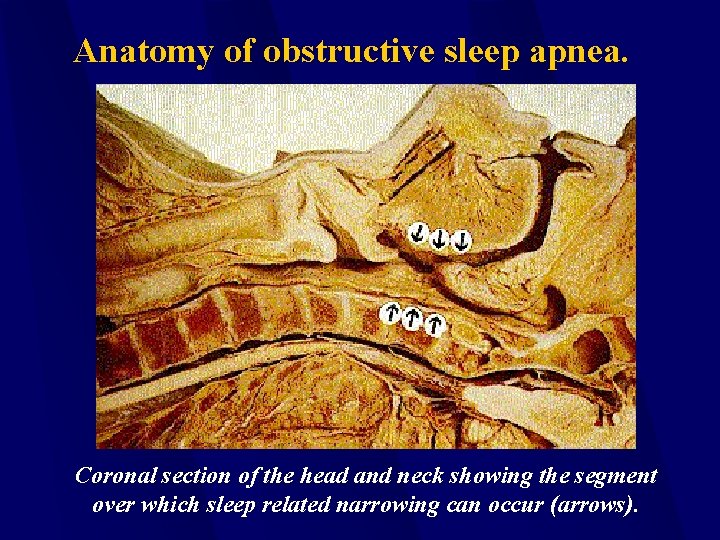
Anatomy of obstructive sleep apnea. Coronal section of the head and neck showing the segment over which sleep related narrowing can occur (arrows).
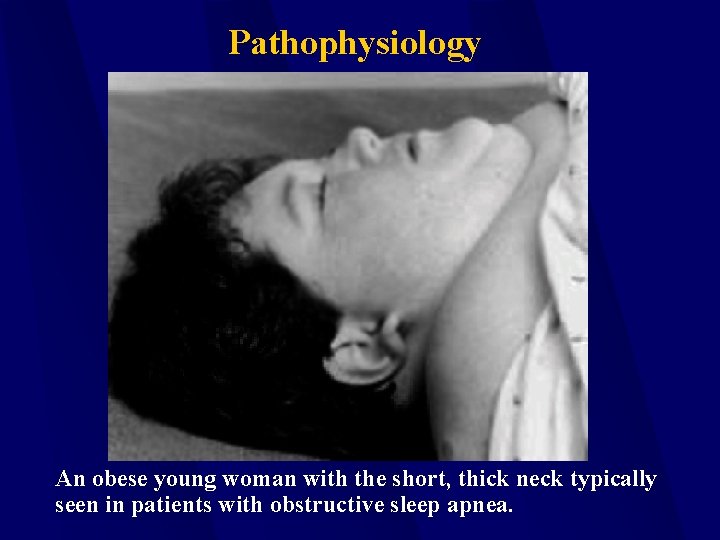
Pathophysiology An obese young woman with the short, thick neck typically seen in patients with obstructive sleep apnea.
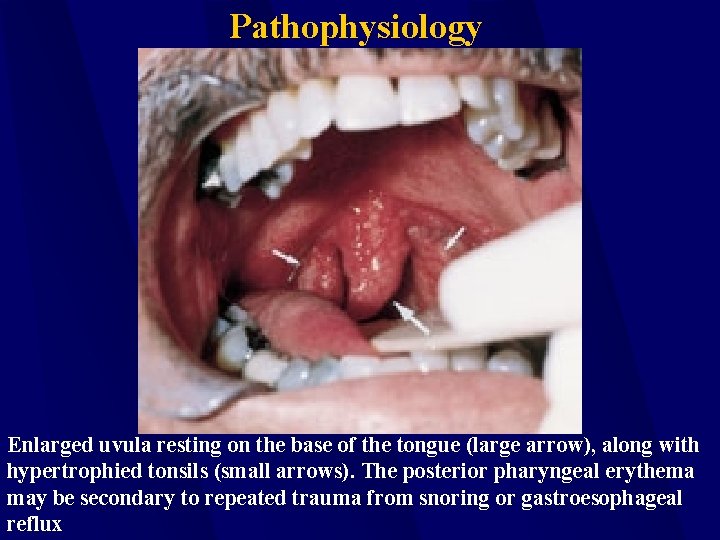
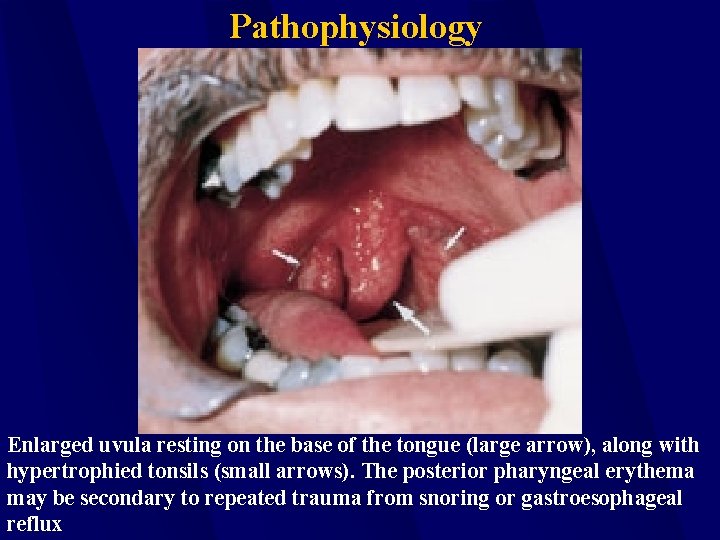
Pathophysiology Enlarged uvula resting on the base of the tongue (large arrow), along with hypertrophied tonsils (small arrows). The posterior pharyngeal erythema may be secondary to repeated trauma from snoring or gastroesophageal reflux
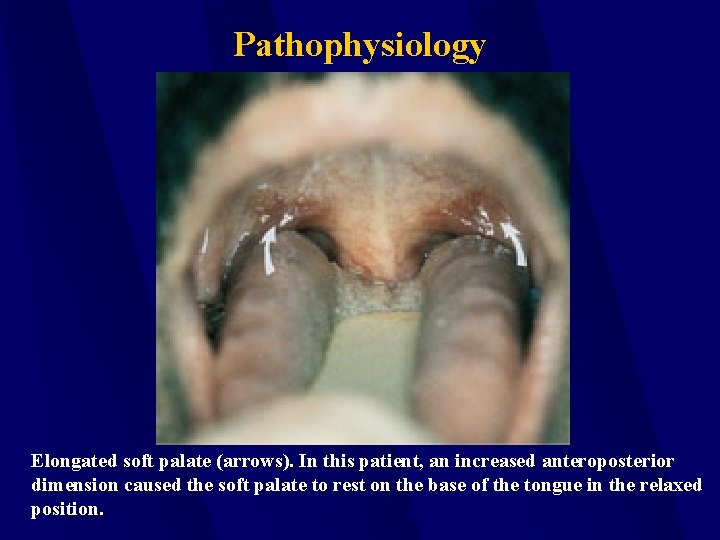
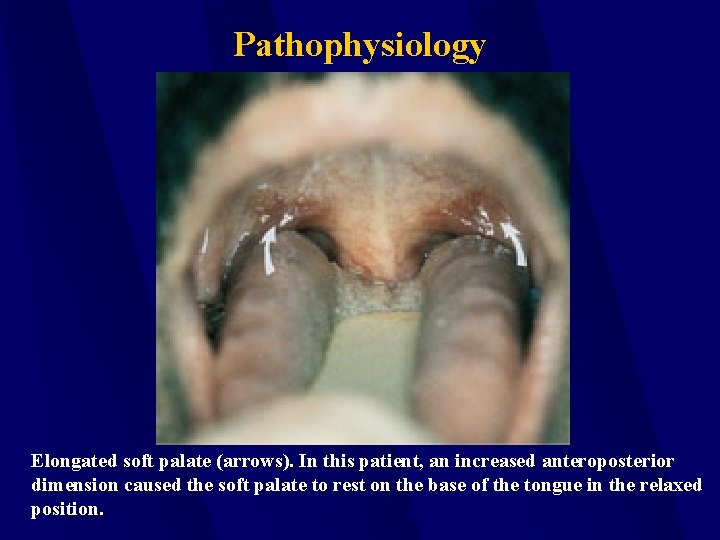
Pathophysiology Elongated soft palate (arrows). In this patient, an increased anteroposterior dimension caused the soft palate to rest on the base of the tongue in the relaxed position.
Clinical Manifestation Family members or partners complaint that the patient has loud snoring, nocturnal gasping or choking.
Pathophysiologic Consequences Sleep Apnea Syndrome is profoundly associated with hypertension independent of all relevant risk factors. Arrhythmias from mild to severe. Motor vehicle accident : Six time increased accident rate compared to the general population.
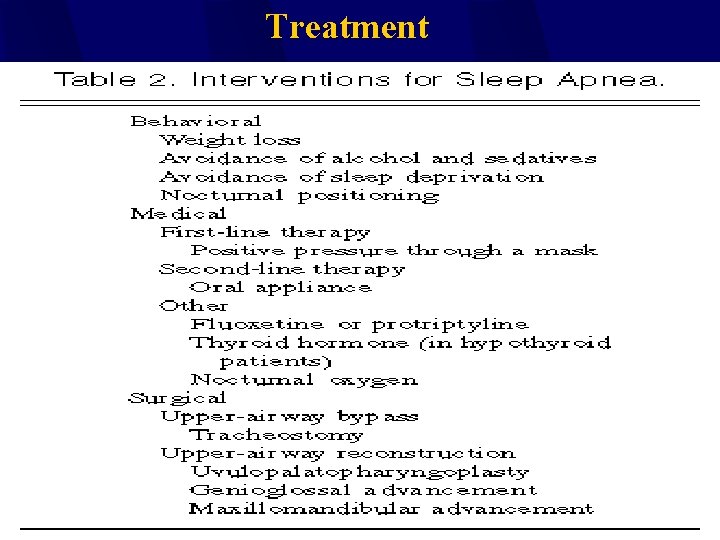
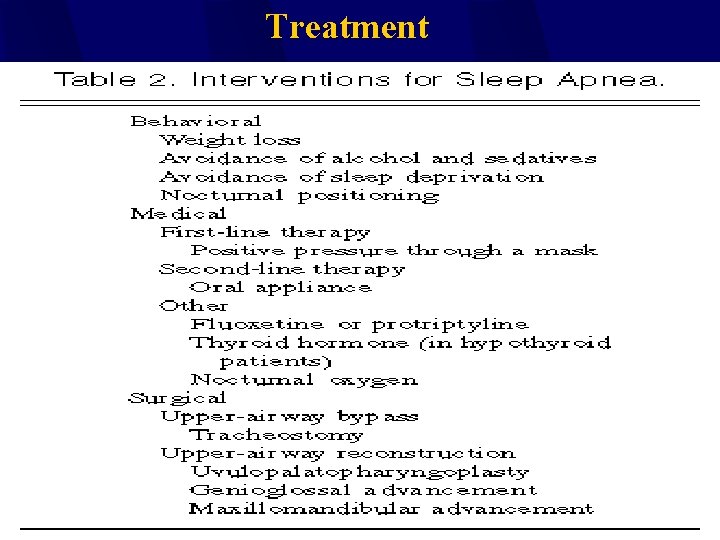
Treatment

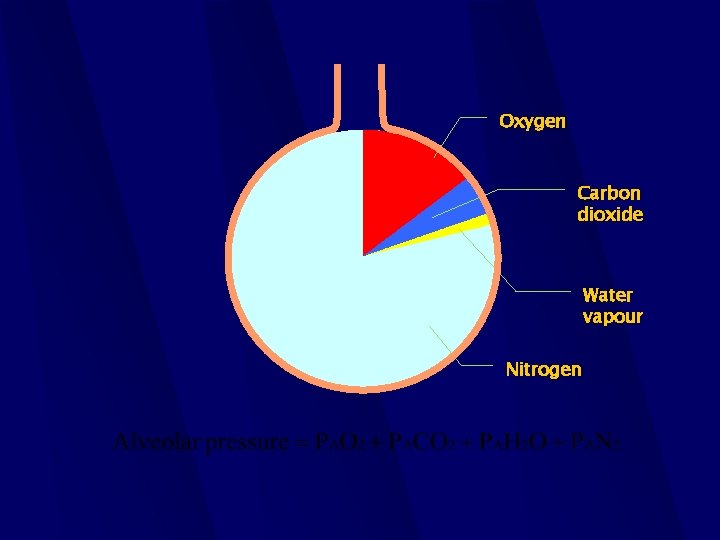
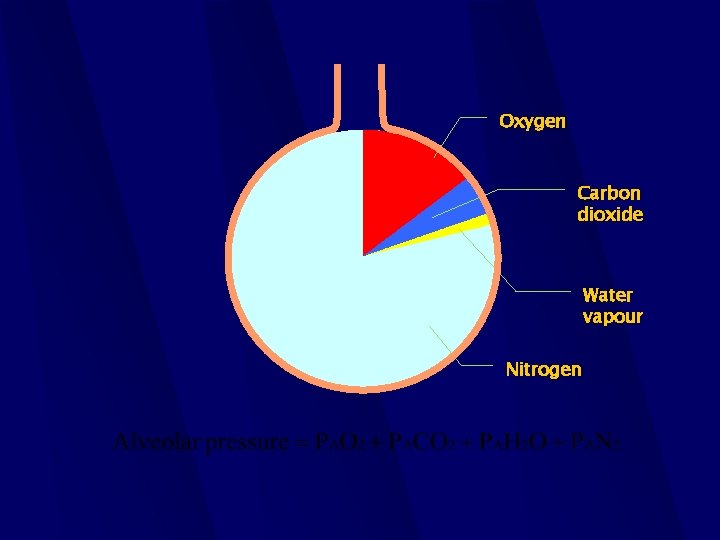
Oxygen Carbon dioxide Water vapour Nitrogen
Someone told me that each equation I included in the book would halve the sales. Stephen Hawking “A Brief History of Time”: 1988.
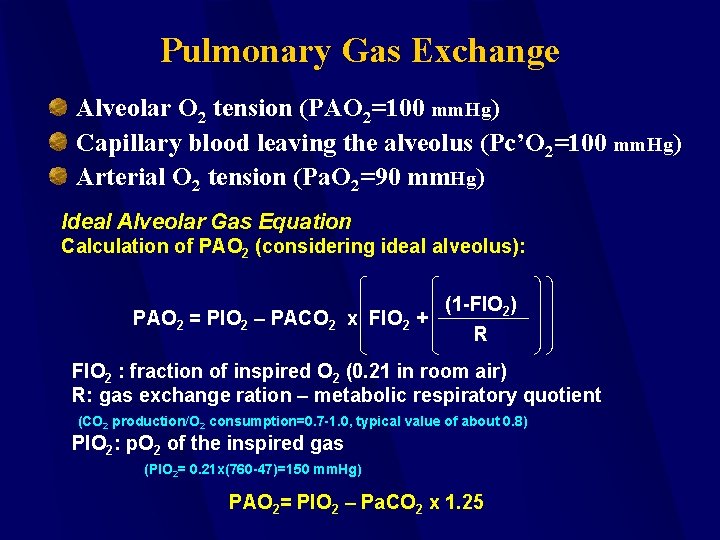
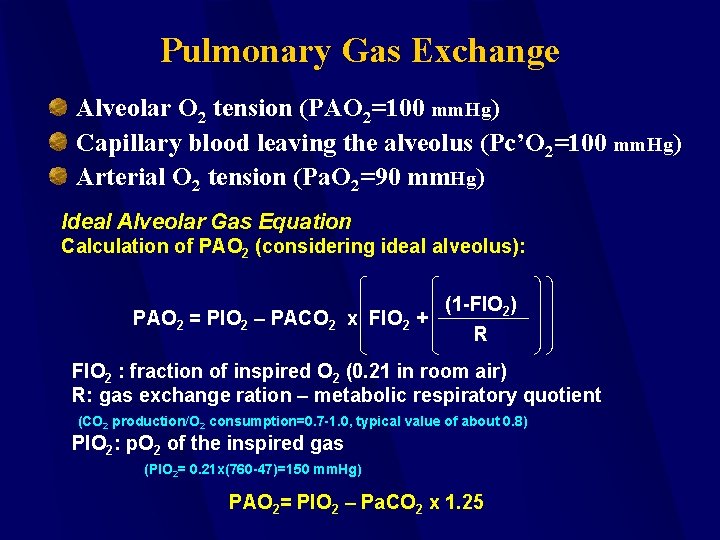
Pulmonary Gas Exchange Alveolar O 2 tension (PAO 2=100 mm. Hg) Capillary blood leaving the alveolus (Pc’O 2=100 mm. Hg) Arterial O 2 tension (Pa. O 2=90 mm. Hg) Ideal Alveolar Gas Equation Calculation of PAO 2 (considering ideal alveolus): (1 -FIO 2) PAO 2 = PIO 2 – PACO 2 x FIO 2 + R FIO 2 : fraction of inspired O 2 (0. 21 in room air) R: gas exchange ration – metabolic respiratory quotient (CO 2 production/O 2 consumption=0. 7 -1. 0, typical value of about 0. 8) PIO 2: p. O 2 of the inspired gas (PIO 2= 0. 21 x(760 -47)=150 mm. Hg) PAO 2= PIO 2 – Pa. CO 2 x 1. 25
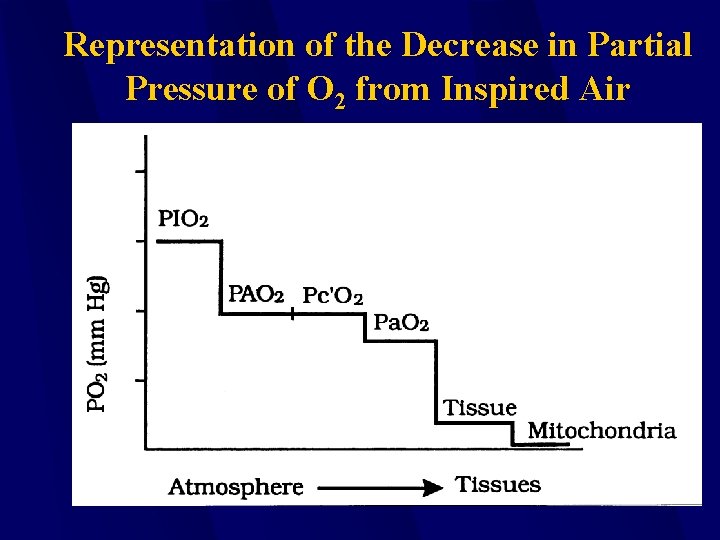
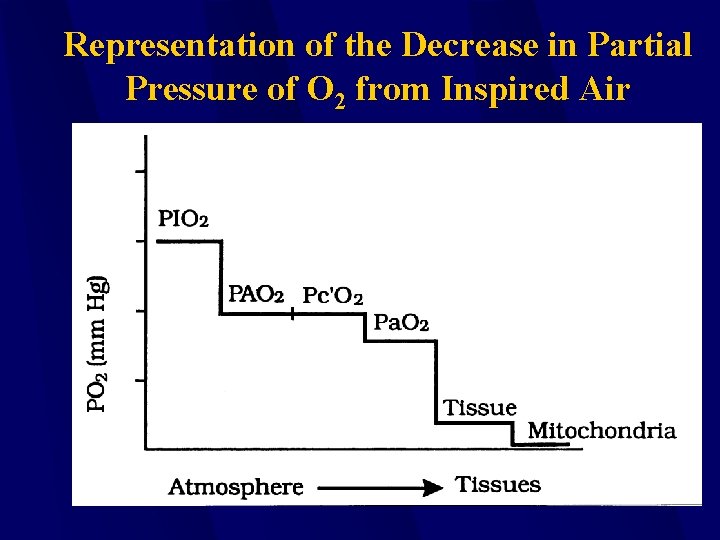
Representation of the Decrease in Partial Pressure of O 2 from Inspired Air
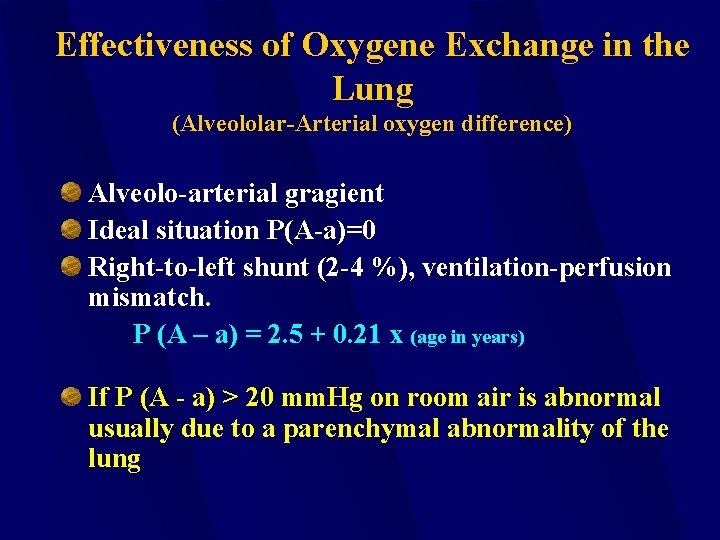
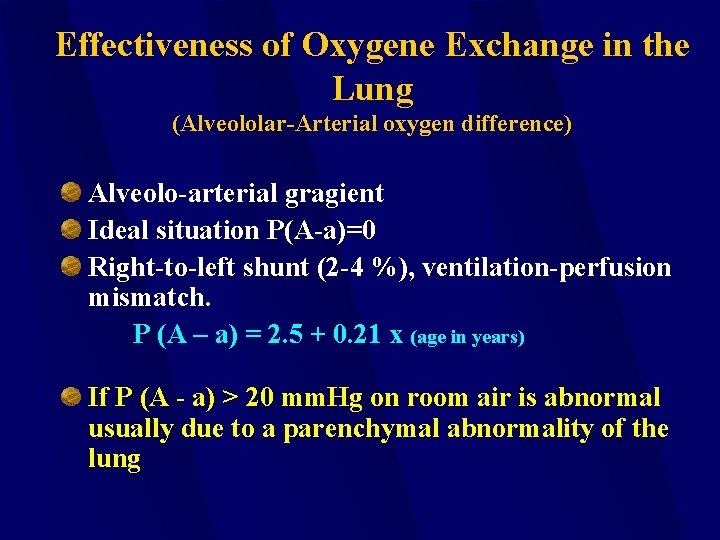
Effectiveness of Oxygene Exchange in the Lung (Alveololar-Arterial oxygen difference) Alveolo-arterial gragient Ideal situation P(A-a)=0 Right-to-left shunt (2 -4 %), ventilation-perfusion mismatch. P (A – a) = 2. 5 + 0. 21 x (age in years) If P (A - a) > 20 mm. Hg on room air is abnormal usually due to a parenchymal abnormality of the lung
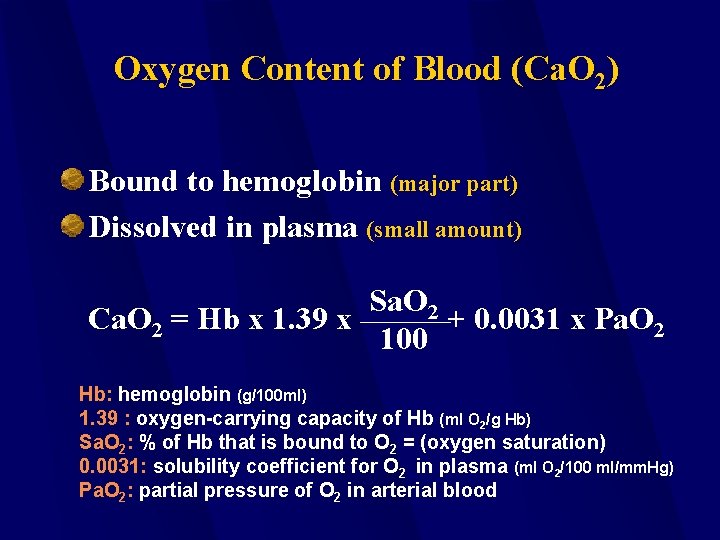
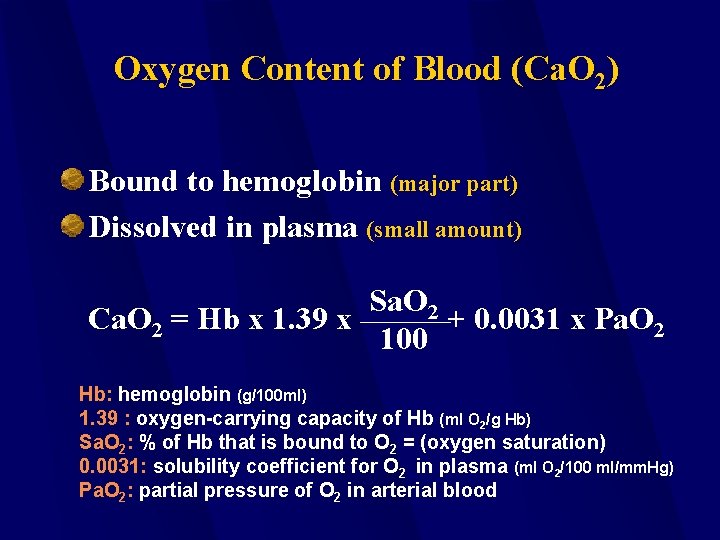
Oxygen Content of Blood (Ca. O 2) Bound to hemoglobin (major part) Dissolved in plasma (small amount) Sa. O 2 Ca. O 2 = Hb x 1. 39 x + 0. 0031 x Pa. O 2 100 Hb: hemoglobin (g/100 ml) 1. 39 : oxygen-carrying capacity of Hb (ml O 2/g Hb) Sa. O 2: % of Hb that is bound to O 2 = (oxygen saturation) 0. 0031: solubility coefficient for O 2 in plasma (ml O 2/100 ml/mm. Hg) Pa. O 2: partial pressure of O 2 in arterial blood
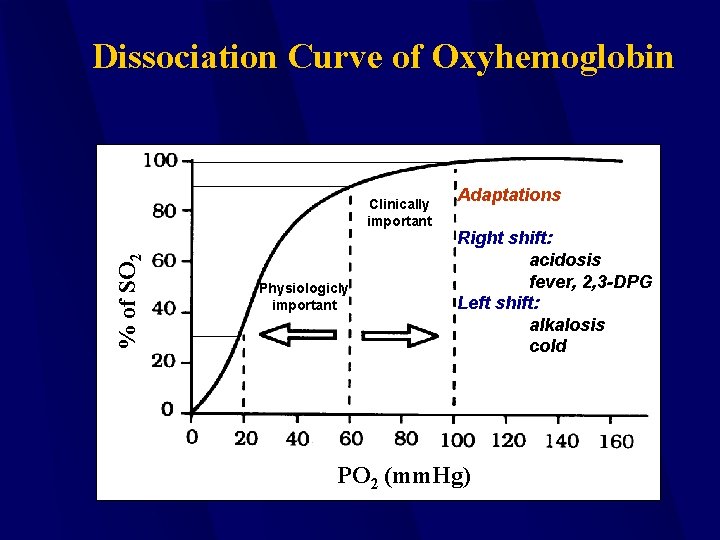
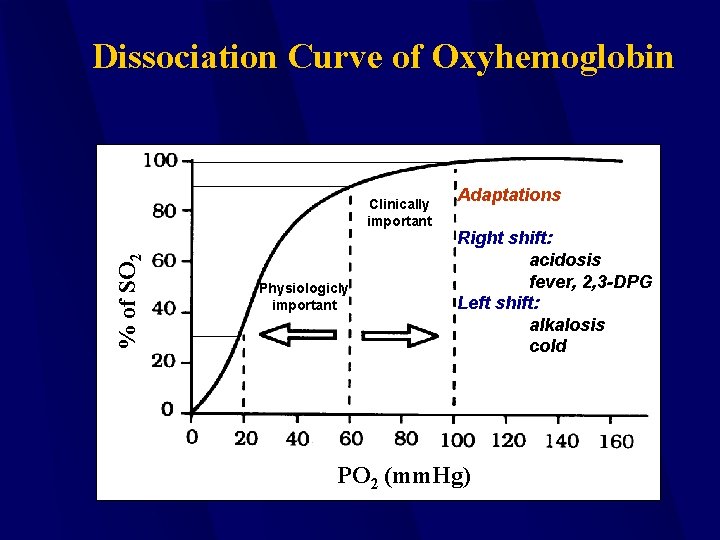
Dissociation Curve of Oxyhemoglobin % of SO 2 Clinically important Physiologicly important Adaptations Right shift: acidosis fever, 2, 3 -DPG Left shift: alkalosis cold PO 2 (mm. Hg)
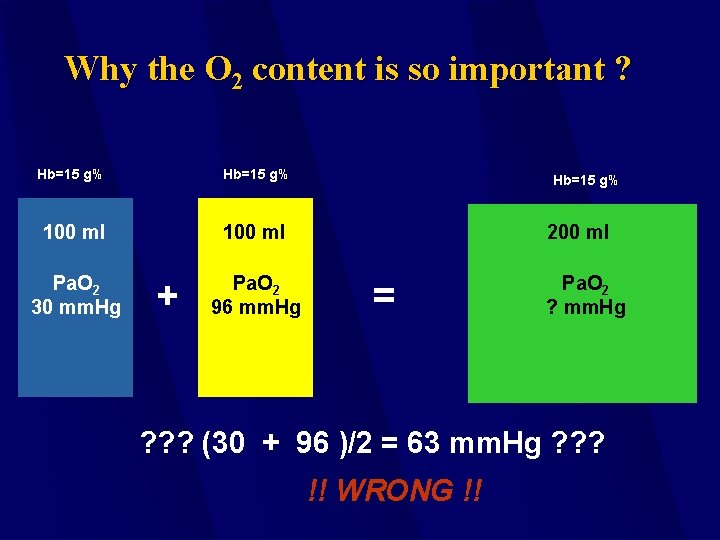
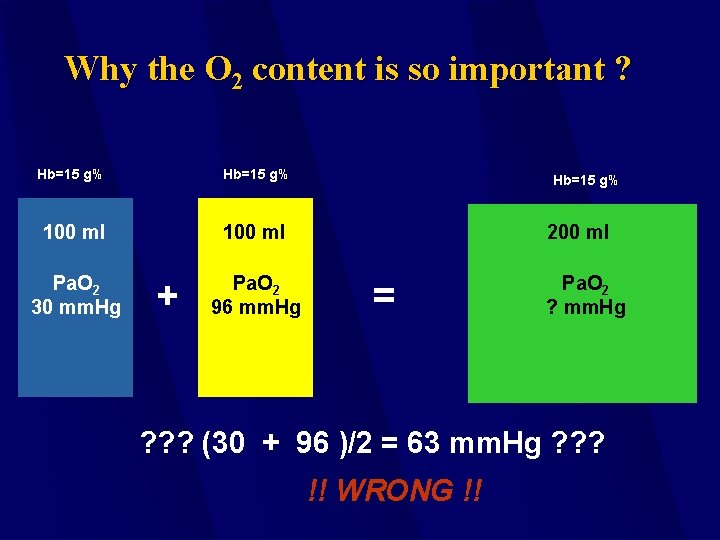
Why the O 2 content is so important ? Hb=15 g% 100 ml Pa. O 2 30 mm. Hg Pa. O 2 96 mm. Hg + Hb=15 g% 200 ml = Pa. O 2 ? mm. Hg ? ? ? (30 + 96 )/2 = 63 mm. Hg ? ? ? !! WRONG !!
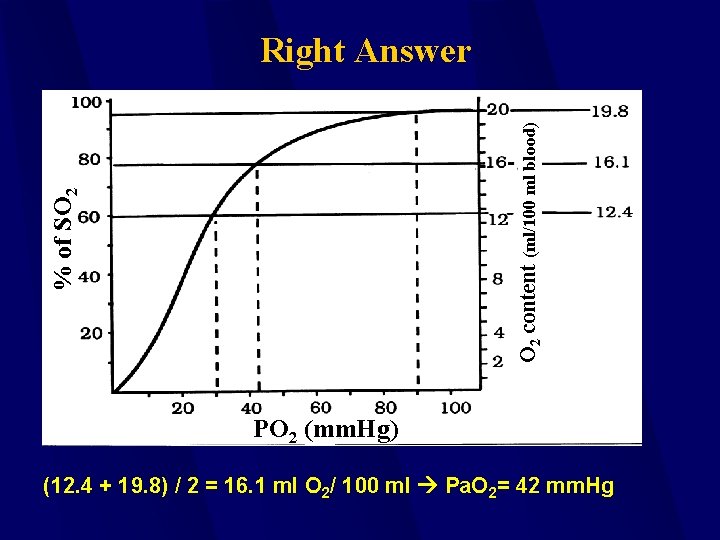
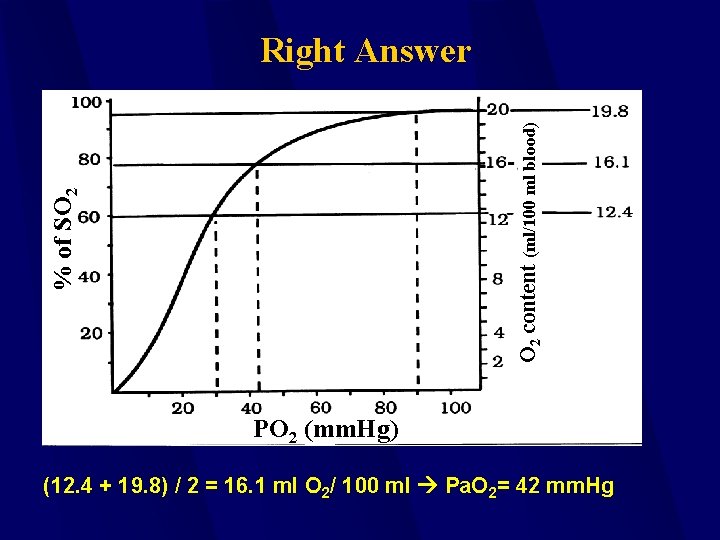
% of SO 2 content (ml/100 ml blood) Right Answer PO 2 (mm. Hg) (12. 4 + 19. 8) / 2 = 16. 1 ml O 2/ 100 ml Pa. O 2= 42 mm. Hg
Respiratory Failure Impaired gas exchange: Hypoxia with or without hypercapnia Can be subclassified into acute and chronic presentations
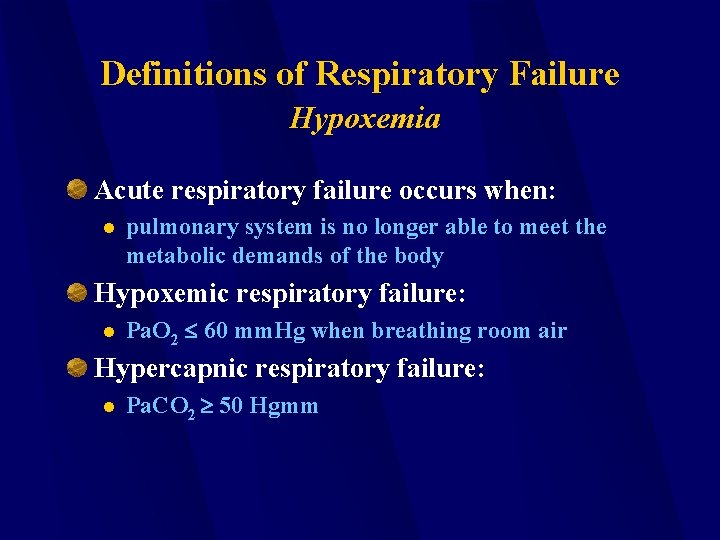
Definitions of Respiratory Failure Hypoxemia Acute respiratory failure occurs when: l pulmonary system is no longer able to meet the metabolic demands of the body Hypoxemic respiratory failure: l Pa. O 2 60 mm. Hg when breathing room air Hypercapnic respiratory failure: l Pa. CO 2 50 Hgmm
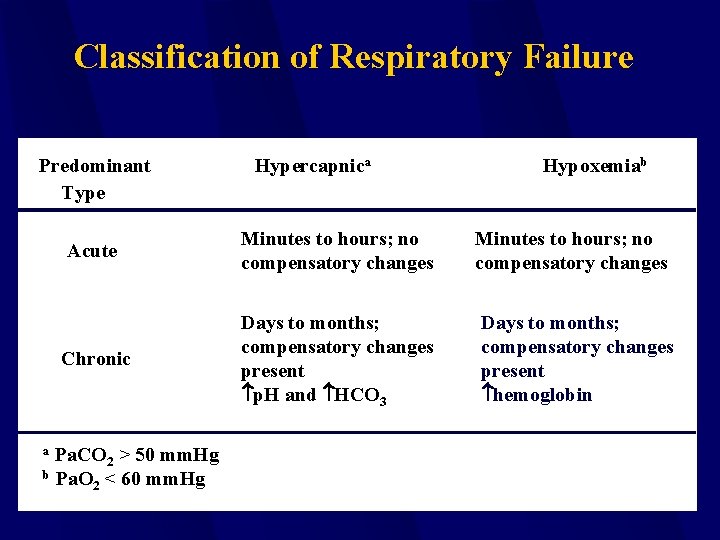
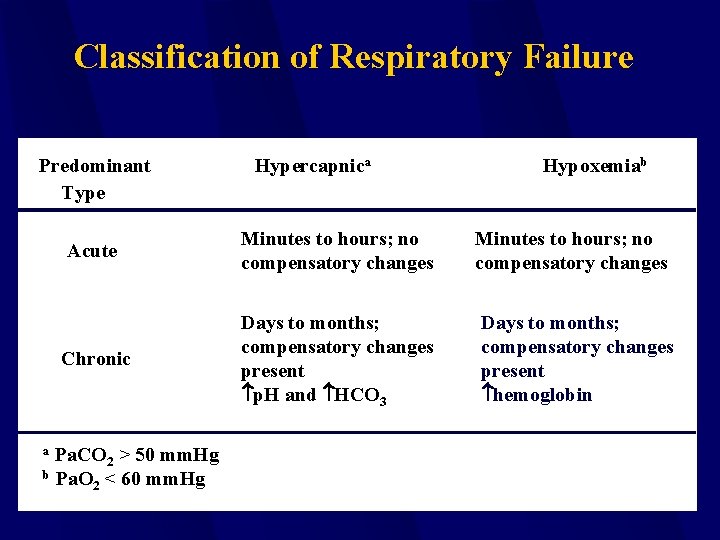
Classification of Respiratory Failure Predominant Type Hypoxemiab Acute Minutes to hours; no compensatory changes Chronic Days to months; compensatory changes present p. H and HCO 3 Days to months; compensatory changes present hemoglobin Pa. CO 2 > 50 mm. Hg b Pa. O < 60 mm. Hg 2 a Hypercapnica
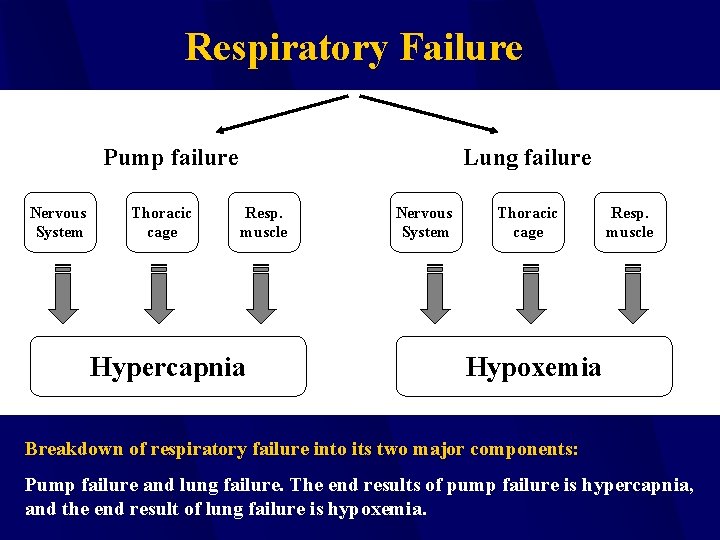
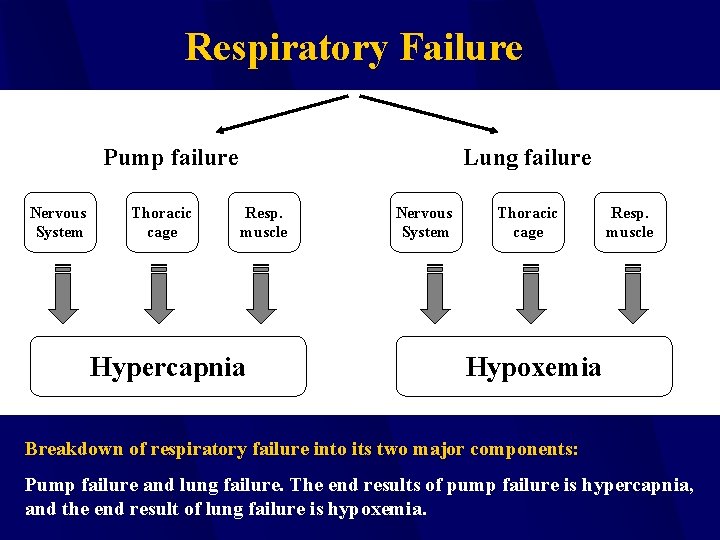
Respiratory Failure Pump failure Nervous System Thoracic cage Lung failure Resp. muscle Hypercapnia Nervous System Thoracic cage Resp. muscle Hypoxemia Breakdown of respiratory failure into its two major components: Pump failure and lung failure. The end results of pump failure is hypercapnia, and the end result of lung failure is hypoxemia.
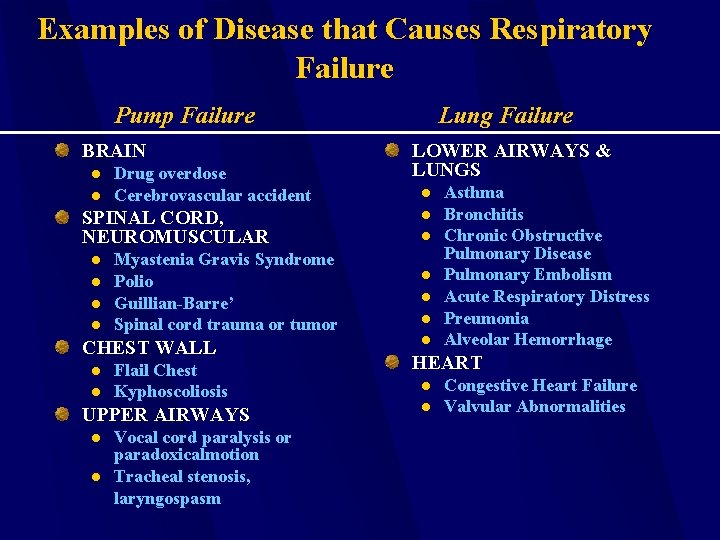
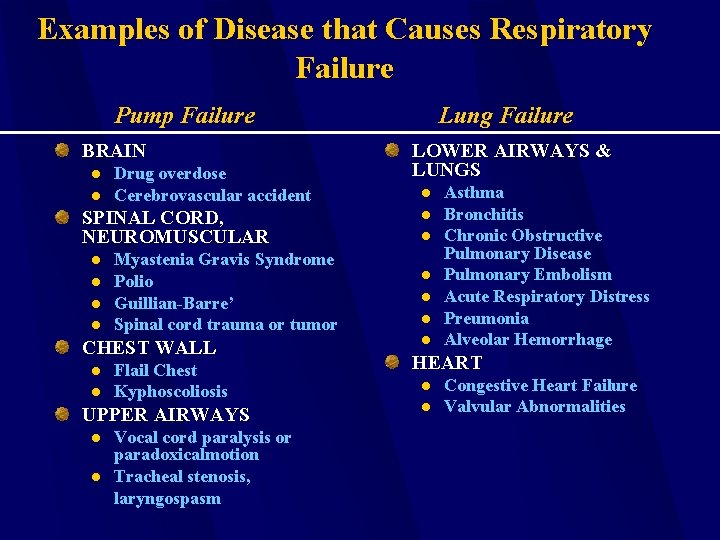
Examples of Disease that Causes Respiratory Failure Pump Failure BRAIN l l Drug overdose Cerebrovascular accident SPINAL CORD, NEUROMUSCULAR l l Myastenia Gravis Syndrome Polio Guillian-Barre’ Spinal cord trauma or tumor CHEST WALL l l Flail Chest Kyphoscoliosis UPPER AIRWAYS l l Vocal cord paralysis or paradoxicalmotion Tracheal stenosis, laryngospasm Lung Failure LOWER AIRWAYS & LUNGS l l l l Asthma Bronchitis Chronic Obstructive Pulmonary Disease Pulmonary Embolism Acute Respiratory Distress Preumonia Alveolar Hemorrhage HEART l l Congestive Heart Failure Valvular Abnormalities
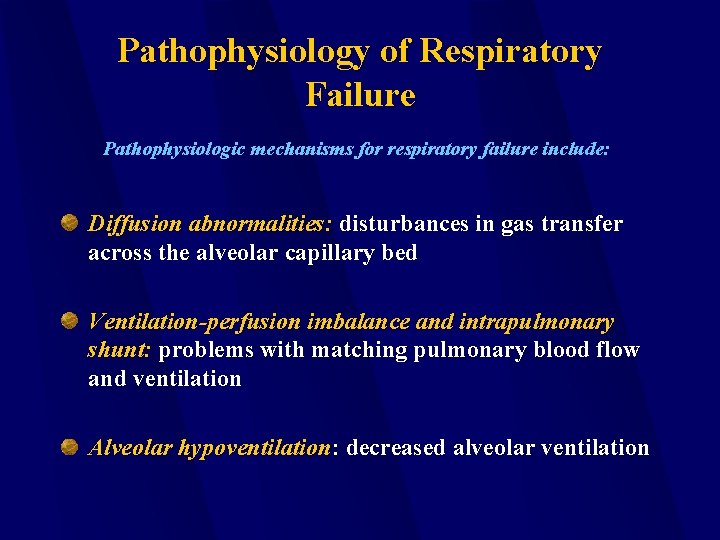
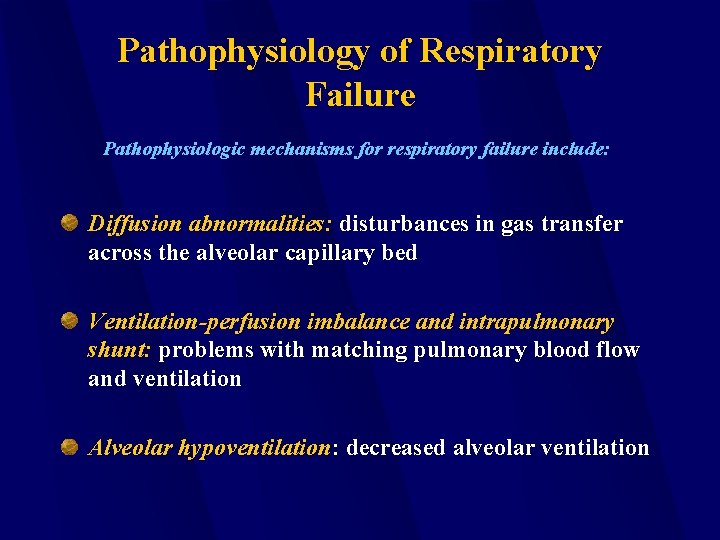
Pathophysiology of Respiratory Failure Pathophysiologic mechanisms for respiratory failure include: Diffusion abnormalities: disturbances in gas transfer across the alveolar capillary bed Ventilation-perfusion imbalance and intrapulmonary shunt: problems with matching pulmonary blood flow and ventilation Alveolar hypoventilation: decreased alveolar ventilation
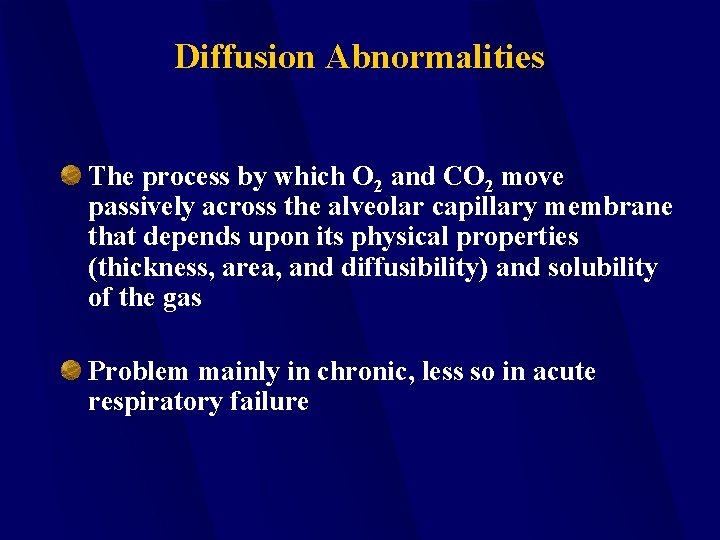
Diffusion Abnormalities The process by which O 2 and CO 2 move passively across the alveolar capillary membrane that depends upon its physical properties (thickness, area, and diffusibility) and solubility of the gas Problem mainly in chronic, less so in acute respiratory failure
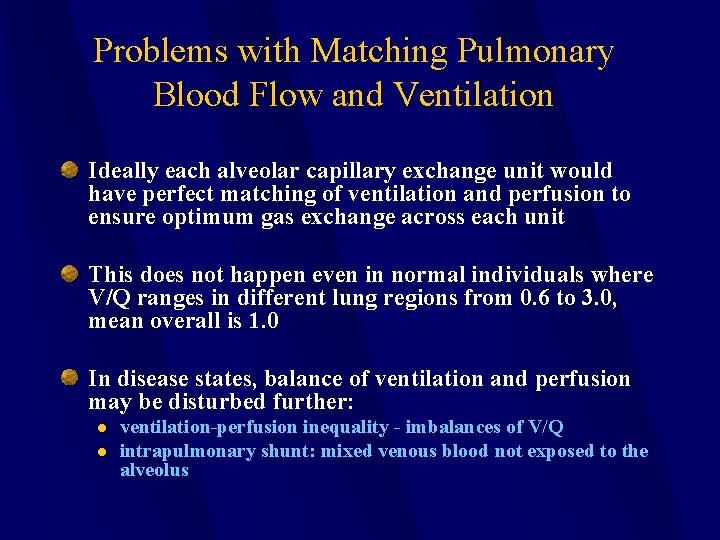
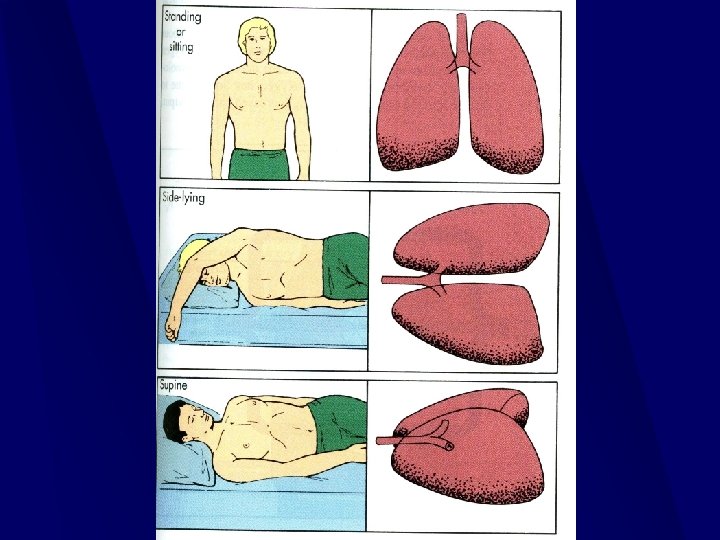
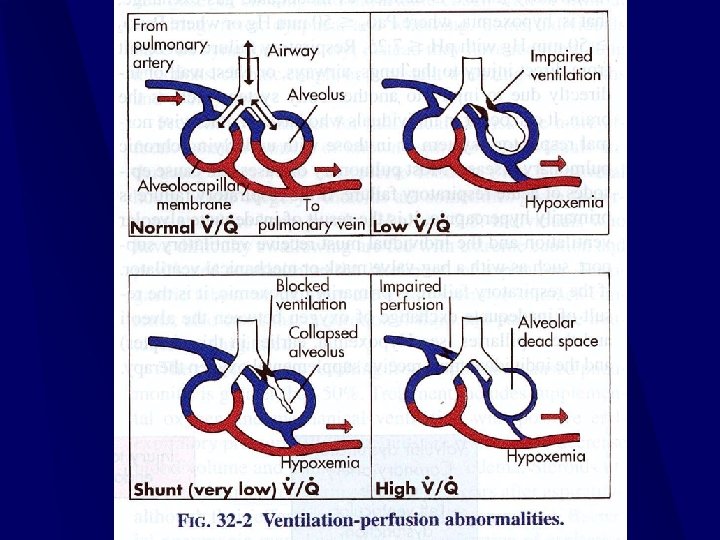
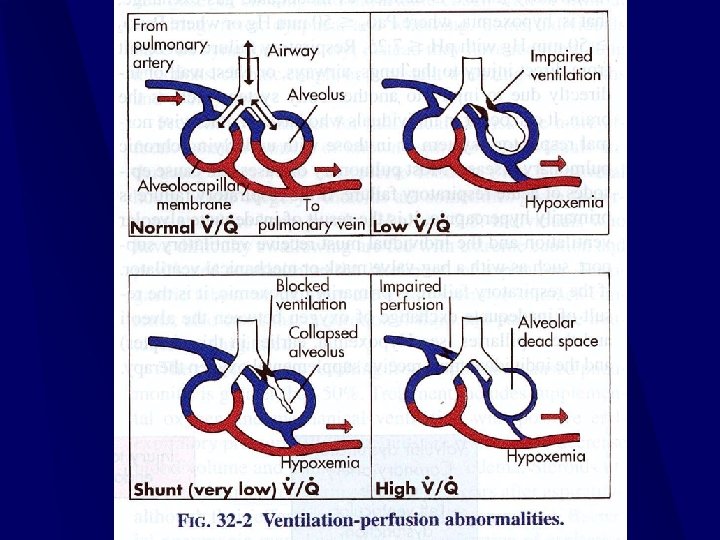
Problems with Matching Pulmonary Blood Flow and Ventilation Ideally each alveolar capillary exchange unit would have perfect matching of ventilation and perfusion to ensure optimum gas exchange across each unit This does not happen even in normal individuals where V/Q ranges in different lung regions from 0. 6 to 3. 0, mean overall is 1. 0 In disease states, balance of ventilation and perfusion may be disturbed further: l l ventilation-perfusion inequality - imbalances of V/Q intrapulmonary shunt: mixed venous blood not exposed to the alveolus

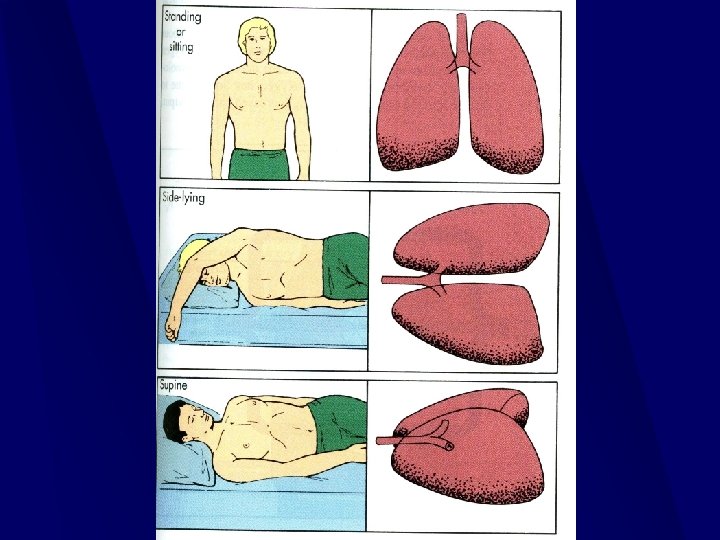
Problems with Matching Pulmonary Blood Flow and Ventilation In disease states, balance of ventilation and perfusion may be disturbed further: l l ventilation-perfusion inequality - imbalances of V/Q intrapulmonary shunt: mixed venous blood not exposed to the alveolus
Hypoventilation To prevent the development of respiratory acidosis, the carbon dioxide produced each day (17, 000 meq acid) must be exhaled by the lungs at the same rate The relationship among alveolar ventilation (VA), carbon dioxide production (VCO 2) and the partial pressure of carbon dioxide in the blood (Pa. CO 2) is expressed using a modification of the Fick principle of mass balance that quantitates VCO 2 as the product of VA and the fractional concentration of CO 2 in the alveolar gas
Diagnosis of Respiratory Failure History and Physical Examination patient symptoms l physical examination l Laboratory Tests
Patient Symptoms in Respiratory Failure Mental function: headache, visual disturbances, confusion, memory loss, hallucinations, loss of consciousness. Dyspnea (resting vs. exertional). Cough, sputum production, chest pain.
Arterial Blood Gas Analysis The most important lab test to subclassify respiratory failure Provides an indication of the duration and severity of respiratory failure Gives 3 Types of Information: l l l presence and degree of hypoxemia (Pa. O 2) presence and degree of hypercapnia (Pa. CO 2) arterial Acid-Base Status (p. H)
Hypoxemia Reduction of partial pressure of oxygen in the blood Resting Pa. O 2 normally 75 -80 mm. Hg, 60 mm. Hg lower limit of safety Oxygenation failure considered if Pa. O 2 < 50 -60 mm. Hg on Fi. O 2 40% or greater Decreases in Pa. O 2 Occur Secondary To: l l l intracardiac or intrapulmonary shunting of blood V/Q mismatch alveolar hypoventilation Alveolar gas equation is helpful in sorting out causes of hypoxemia
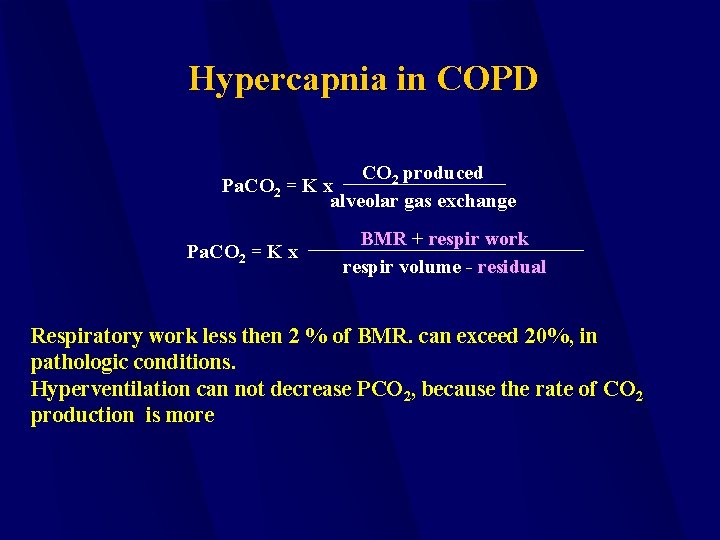
Hypercapnia in an increase Pa. CO 2 > 50 mm. Hg. Pa. CO 2 = KVO 2 * VA VCO 2 (carbon dioxide) is produced by the oxidative metabolism of carbon containing food products. Any increase in VCO 2 or decrease in VA will result in hypercapnia.
Respiratory Failure Examples of Lung vs. Pump Failure Disorders causing respiratory failure can usually be divided into those causing lung failure (impaired oxygenation) vs. pump failure (hypercapnia). Adult Respiratory Distress Syndrome (ARDS) is an example of lung failure, drug overdose is an example of pump failure.
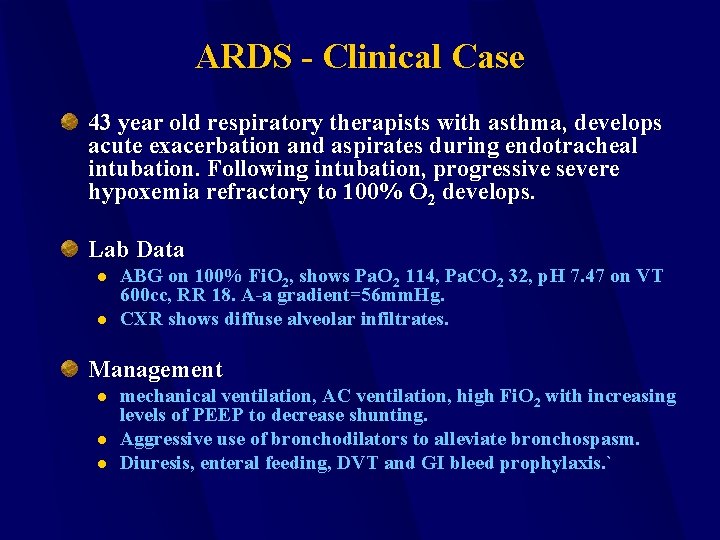
ARDS - Clinical Case 43 year old respiratory therapists with asthma, develops acute exacerbation and aspirates during endotracheal intubation. Following intubation, progressive severe hypoxemia refractory to 100% O 2 develops. Lab Data l l ABG on 100% Fi. O 2, shows Pa. O 2 114, Pa. CO 2 32, p. H 7. 47 on VT 600 cc, RR 18. A-a gradient=56 mm. Hg. CXR shows diffuse alveolar infiltrates. Management l l l mechanical ventilation, AC ventilation, high Fi. O 2 with increasing levels of PEEP to decrease shunting. Aggressive use of bronchodilators to alleviate bronchospasm. Diuresis, enteral feeding, DVT and GI bleed prophylaxis. `
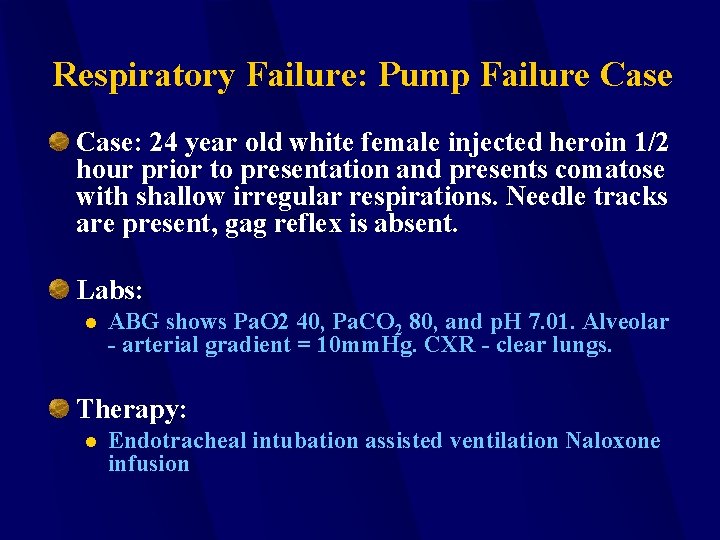
Respiratory Failure: Pump Failure Case: 24 year old white female injected heroin 1/2 hour prior to presentation and presents comatose with shallow irregular respirations. Needle tracks are present, gag reflex is absent. Labs: l ABG shows Pa. O 2 40, Pa. CO 2 80, and p. H 7. 01. Alveolar - arterial gradient = 10 mm. Hg. CXR - clear lungs. Therapy: l Endotracheal intubation assisted ventilation Naloxone infusion
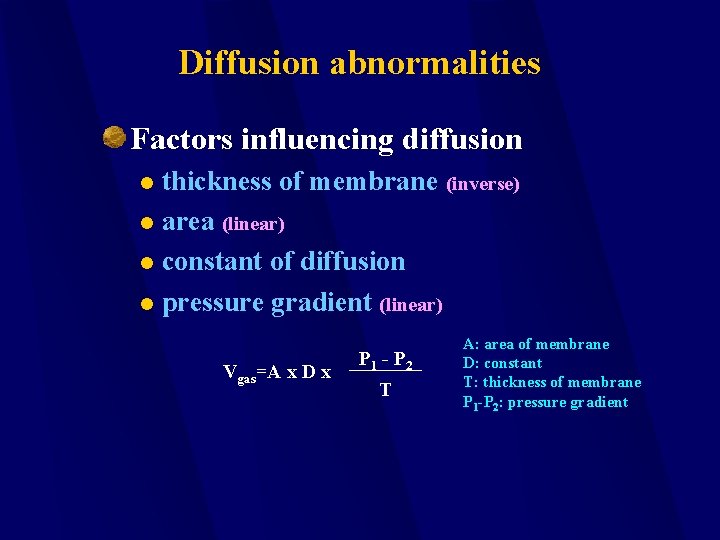
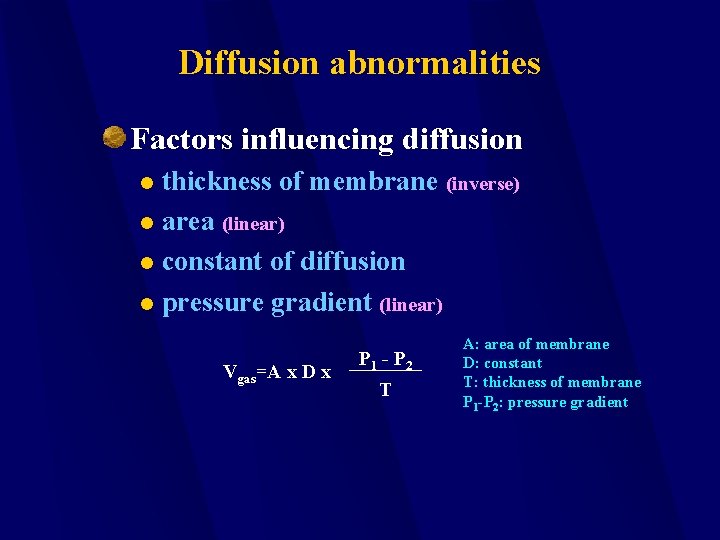
Diffusion abnormalities Factors influencing diffusion thickness of membrane (inverse) l area (linear) l constant of diffusion l pressure gradient (linear) l Vgas=A x D x P 1 - P 2 T A: area of membrane D: constant T: thickness of membrane P 1 -P 2: pressure gradient
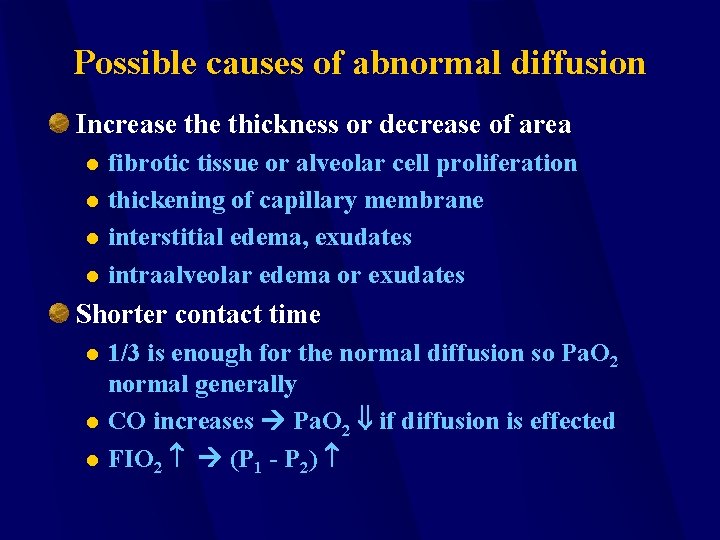
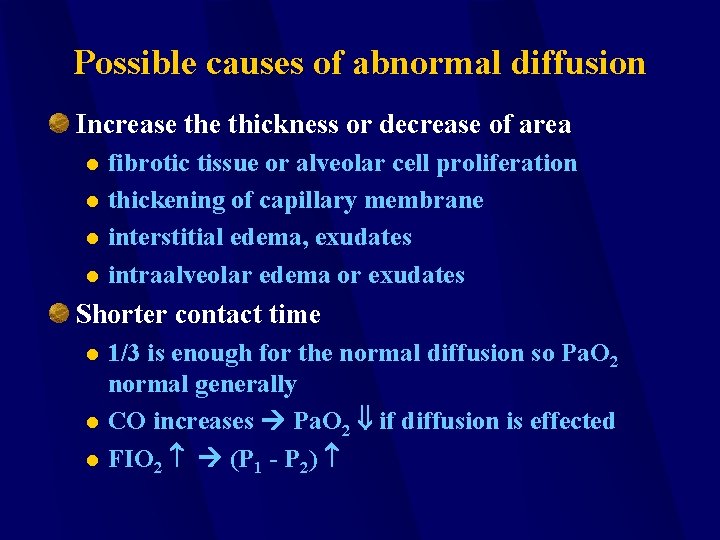
Possible causes of abnormal diffusion Increase thickness or decrease of area l l fibrotic tissue or alveolar cell proliferation thickening of capillary membrane interstitial edema, exudates intraalveolar edema or exudates Shorter contact time l l l 1/3 is enough for the normal diffusion so Pa. O 2 normal generally CO increases Pa. O 2 if diffusion is effected FIO 2 (P 1 - P 2)
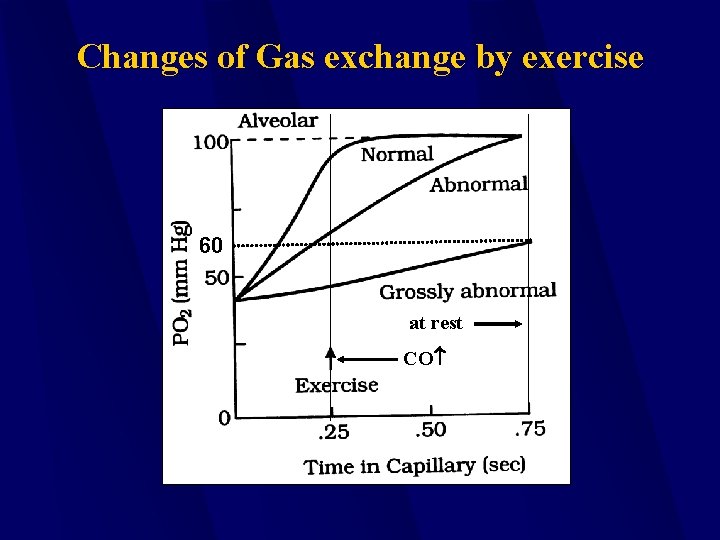
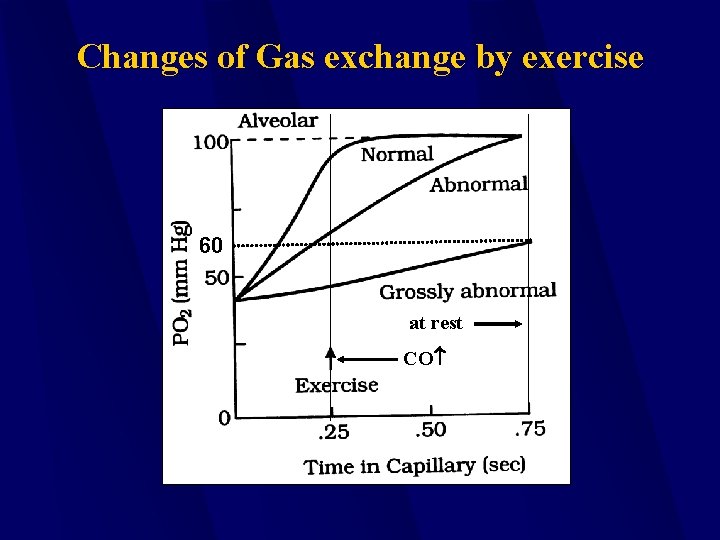
Changes of Gas exchange by exercise 60 at rest CO
Summary Abnormal diffusion: PAO 2 normal but Pa. O 2 decreased P(A - a)O 2 >10 mm. Hg Usually triggered by exercise FIO 2 ↑ improves Rarely the cause of hypoxia

Mechanical component of breathing Mechanisms influencing inspiration and expiration l elasticity Lung parenchyma l Cavity of chest l resistance of airways l other forces against the mechanism of respiration l
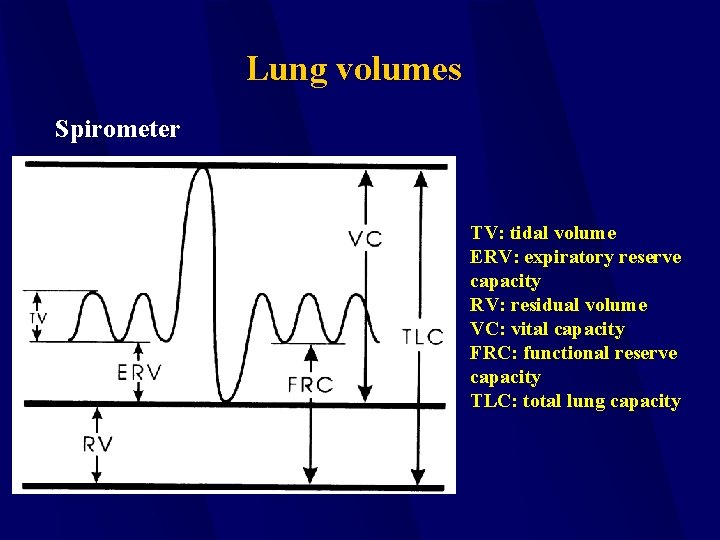
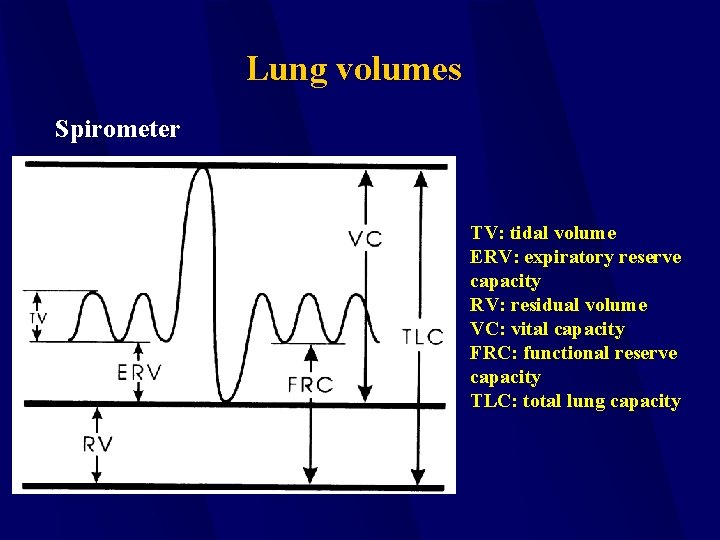
Lung volumes Spirometer TV: tidal volume ERV: expiratory reserve capacity RV: residual volume VC: vital capacity FRC: functional reserve capacity TLC: total lung capacity

Measurement of lung volumes Spirometer – RV can not be determined body plethysmograph Inert gas dilution test FRC can be estimated. RV = FRC-ERV TLC = RV + VC
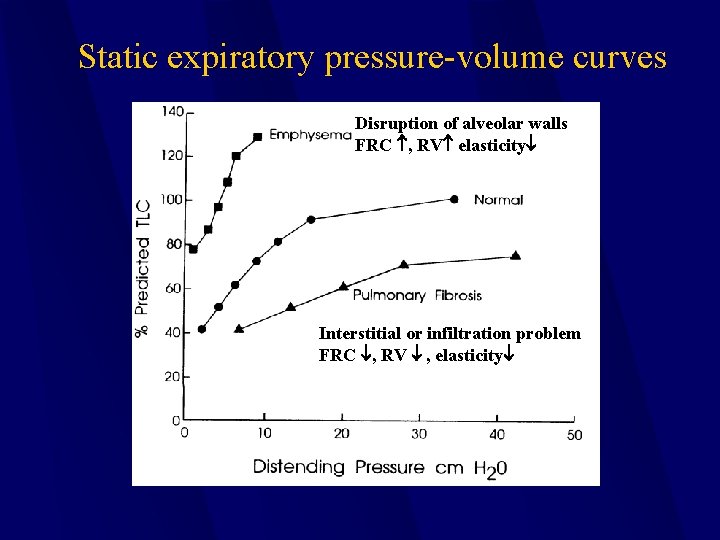
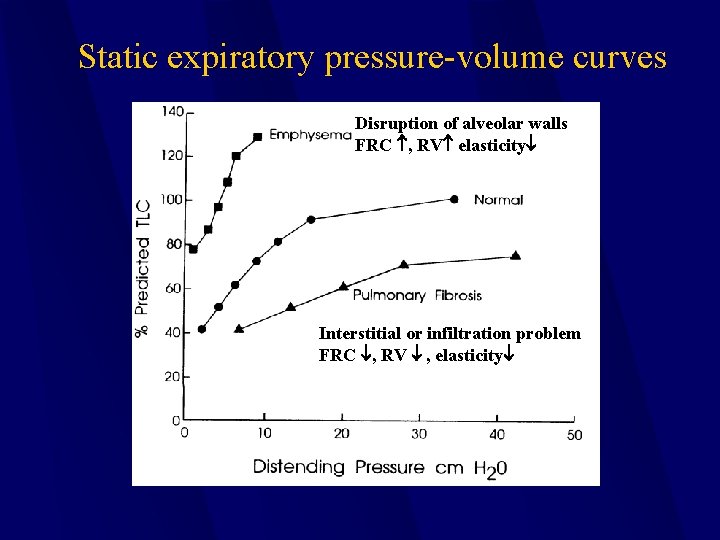
Static expiratory pressure volume curves Disruption of alveolar walls FRC , RV elasticity Interstitial or infiltration problem FRC , RV , elasticity
Factors influencing the elastic recoil Surface tension (surfactant -dipalmitodylphosfatidilcholin, other produced by type II. alveolar cells Tissue elasticity (amount of elastin and collagen) lipids and proteins-
The importance of surface tension. If two connected alveoli have the same surface tension, then the smaller the radius, the greater the pressure tending to collapse the sphere. This could lead to alveolar instability, with smaller units emptying info larger ones. Alveoli typically do not have the same surface tension because surface forces vary according to surface area, due to the presence of surfactant. Since the relative concentration of surfactant in the surface layer of the sphere increases as the radius of the sphere falls, the effect of surfactant is increased at low lung volumes. This tends to counterbal ancethe increase in pressure needed to keep alveoli open at diminished lung volume and adds stability to alveoli which might otherwise tend to collapse info one another. Surfactant thus protects against regional col lapseof lung units, a condition known as atelectasis, in addition to its other functions.
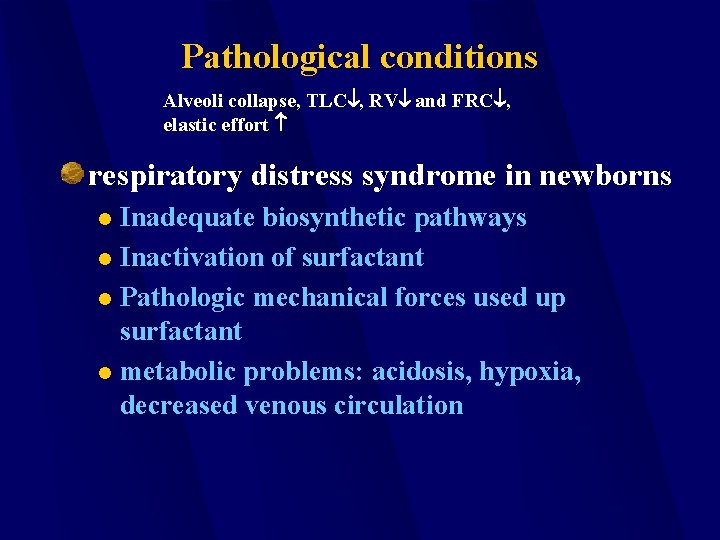
Pathological conditions Alveoli collapse, TLC , RV and FRC , elastic effort respiratory distress syndrome in newborns Inadequate biosynthetic pathways l Inactivation of surfactant l Pathologic mechanical forces used up surfactant l metabolic problems: acidosis, hypoxia, decreased venous circulation l
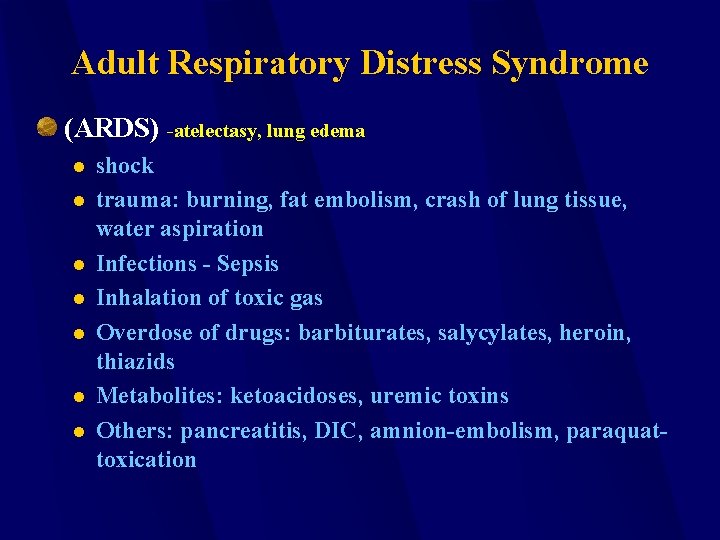
Adult Respiratory Distress Syndrome (ARDS) -atelectasy, lung edema l l l l shock trauma: burning, fat embolism, crash of lung tissue, water aspiration Infections - Sepsis Inhalation of toxic gas Overdose of drugs: barbiturates, salycylates, heroin, thiazids Metabolites: ketoacidoses, uremic toxins Others: pancreatitis, DIC, amnion-embolism, paraquattoxication
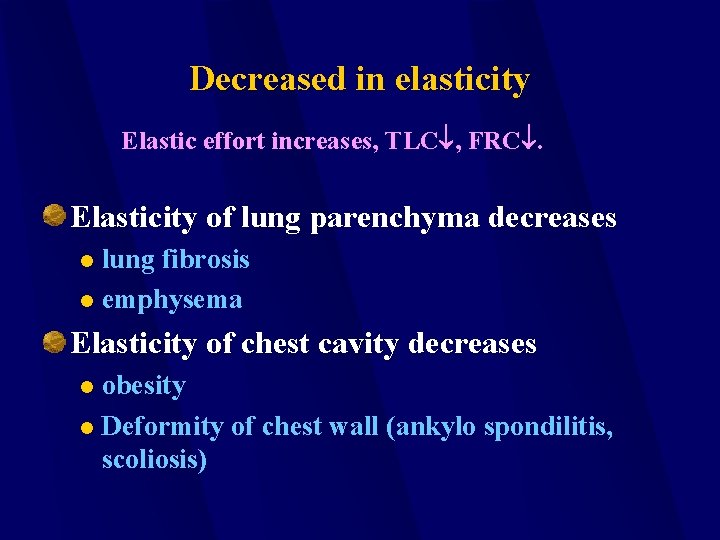
Decreased in elasticity Elastic effort increases, TLC , FRC. Elasticity of lung parenchyma decreases lung fibrosis l emphysema l Elasticity of chest cavity decreases obesity l Deformity of chest wall (ankylo spondilitis, scoliosis) l
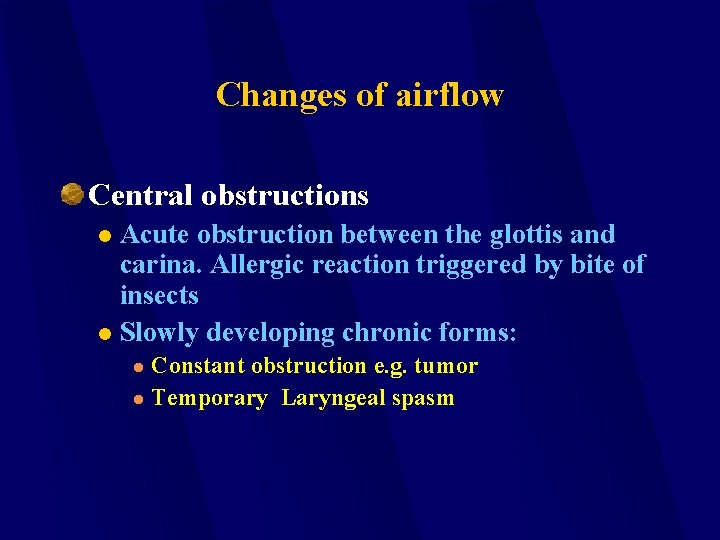
Changes of airflow Central obstructions Acute obstruction between the glottis and carina. Allergic reaction triggered by bite of insects l Slowly developing chronic forms: l Constant obstruction e. g. tumor l Temporary Laryngeal spasm l
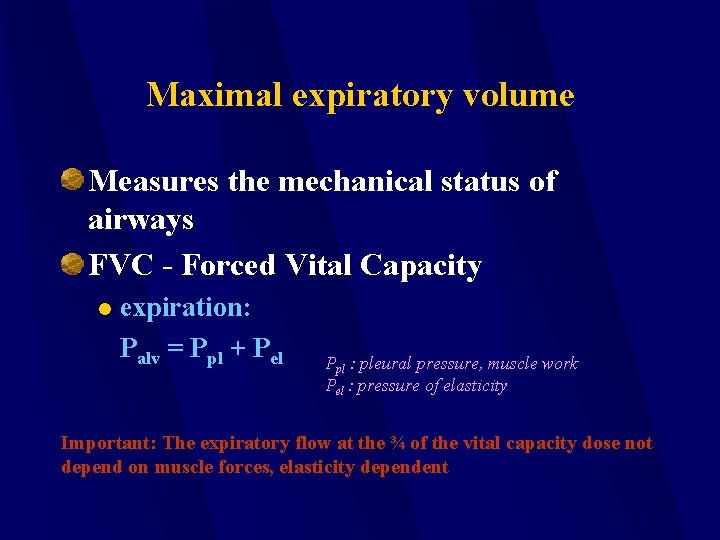
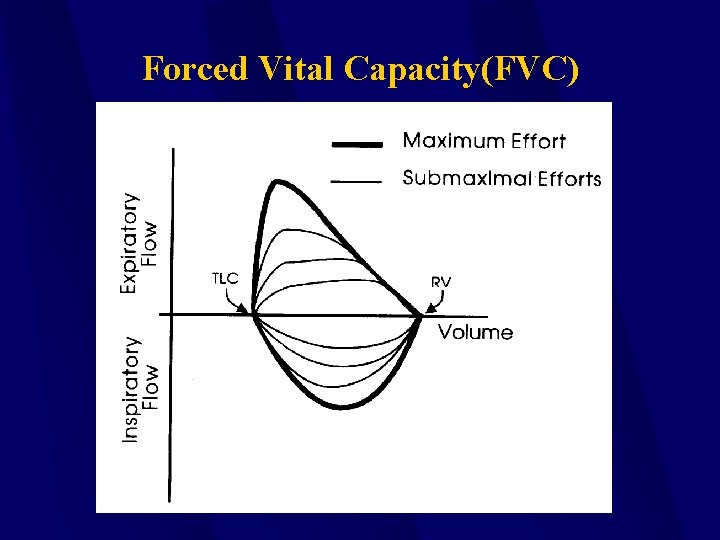
Maximal expiratory volume Measures the mechanical status of airways FVC - Forced Vital Capacity l expiration: Palv = Ppl + Pel Ppl : pleural pressure, muscle work Pel : pressure of elasticity Important: The expiratory flow at the ¾ of the vital capacity dose not depend on muscle forces, elasticity dependent
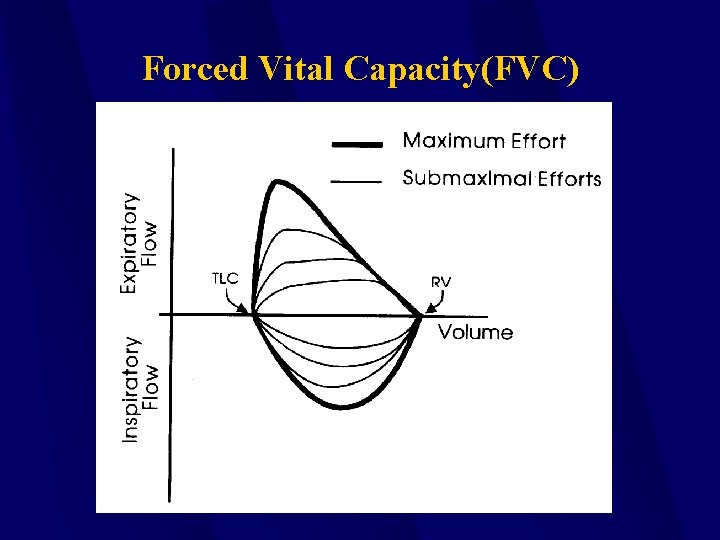
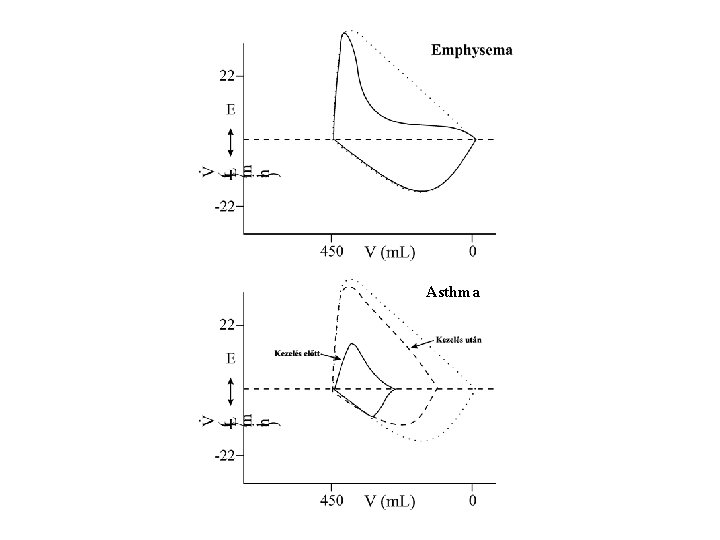
Forced Vital Capacity(FVC)

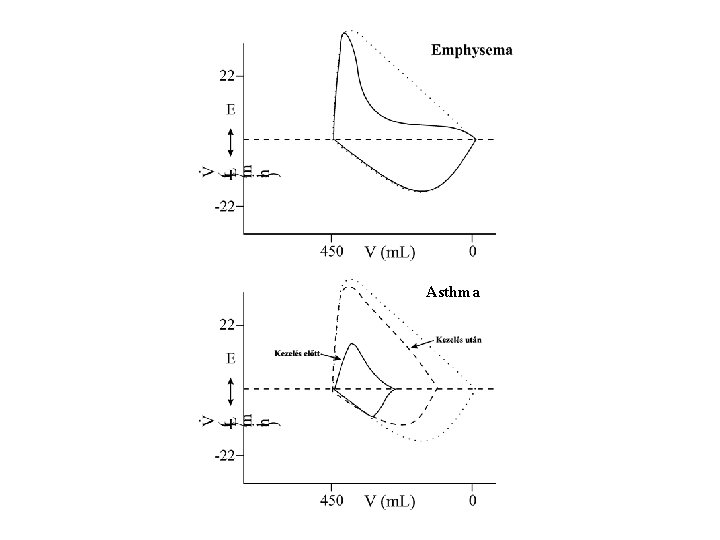
Asthma
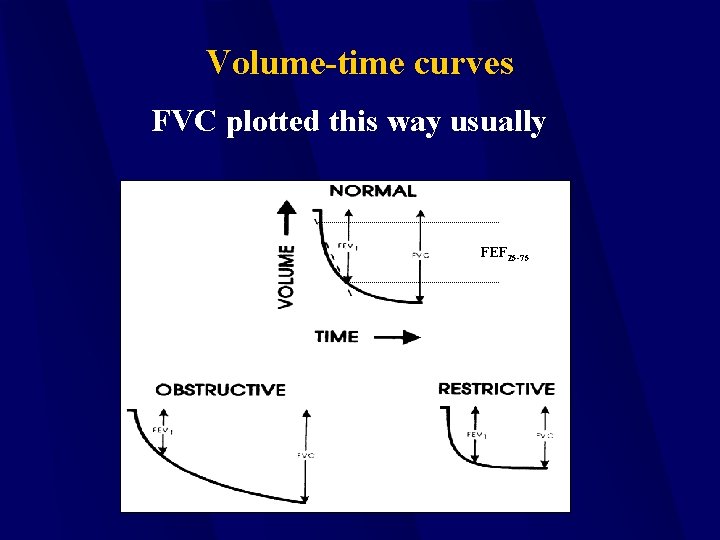
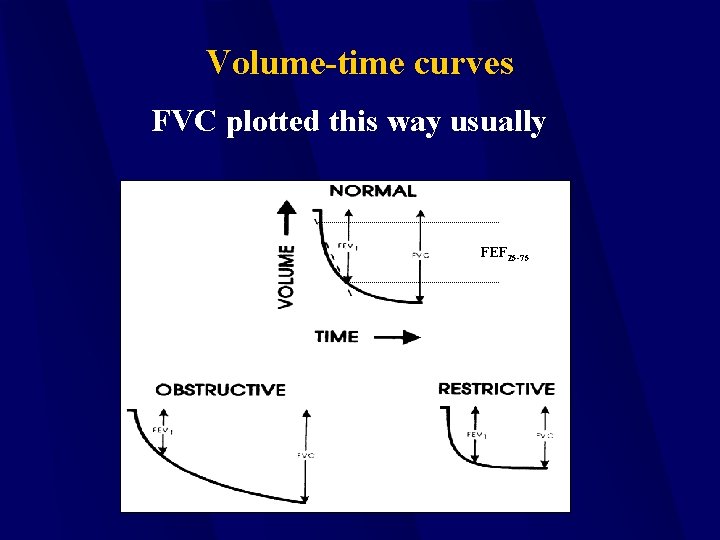
Volume-time curves FVC plotted this way usually FEF 25 -75
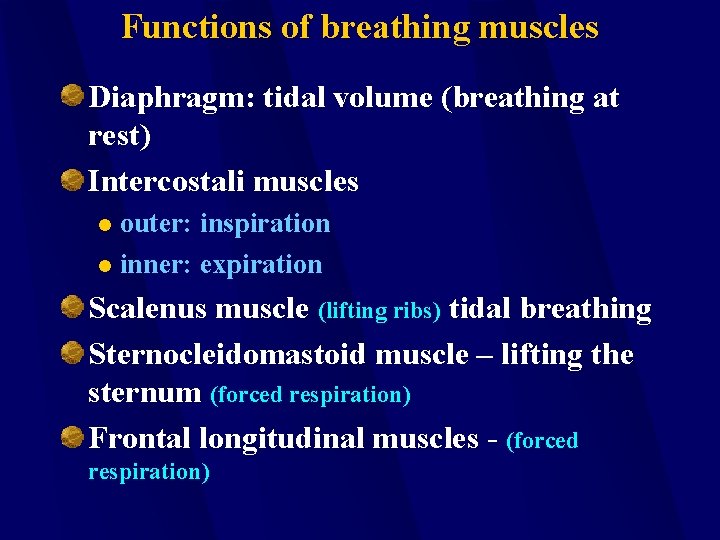
Functions of breathing muscles Diaphragm: tidal volume (breathing at rest) Intercostali muscles outer: inspiration l inner: expiration l Scalenus muscle (lifting ribs) tidal breathing Sternocleidomastoid muscle – lifting the sternum (forced respiration) Frontal longitudinal muscles - (forced respiration)
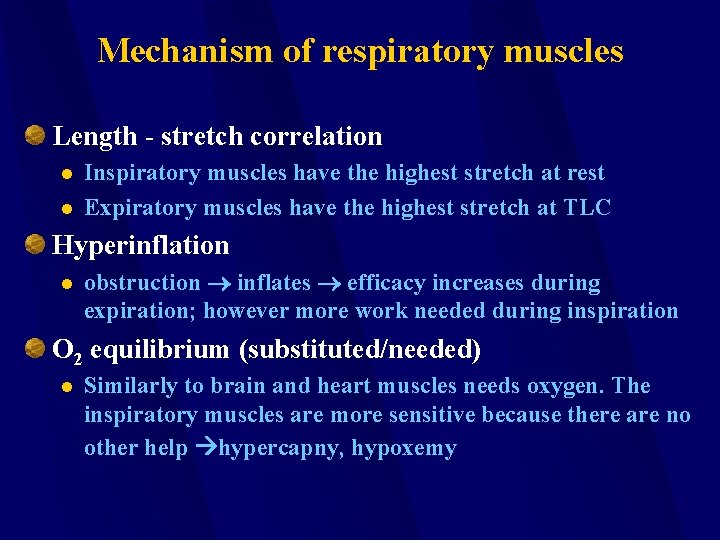
Mechanism of respiratory muscles Length - stretch correlation l l Inspiratory muscles have the highest stretch at rest Expiratory muscles have the highest stretch at TLC Hyperinflation l obstruction inflates efficacy increases during expiration; however more work needed during inspiration O 2 equilibrium (substituted/needed) l Similarly to brain and heart muscles needs oxygen. The inspiratory muscles are more sensitive because there are no other help hypercapny, hypoxemy
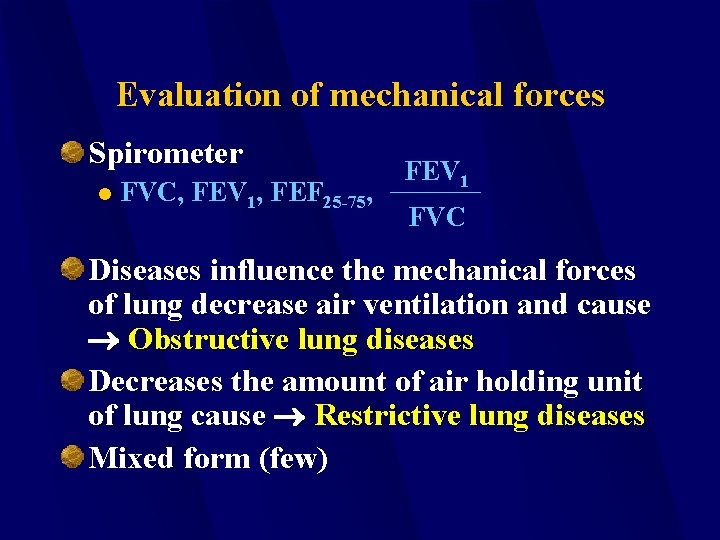
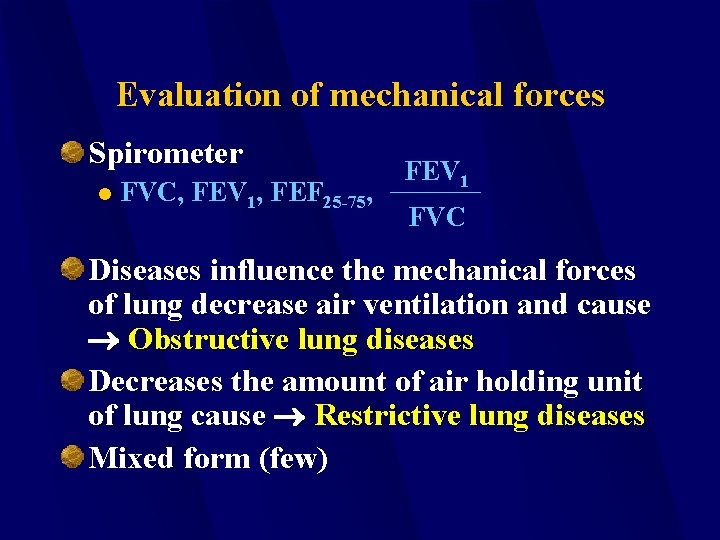
Evaluation of mechanical forces Spirometer l FVC, FEV 1, FEF 25 -75, FEV 1 FVC Diseases influence the mechanical forces of lung decrease air ventilation and cause Obstructive lung diseases Decreases the amount of air holding unit of lung cause Restrictive lung diseases Mixed form (few)
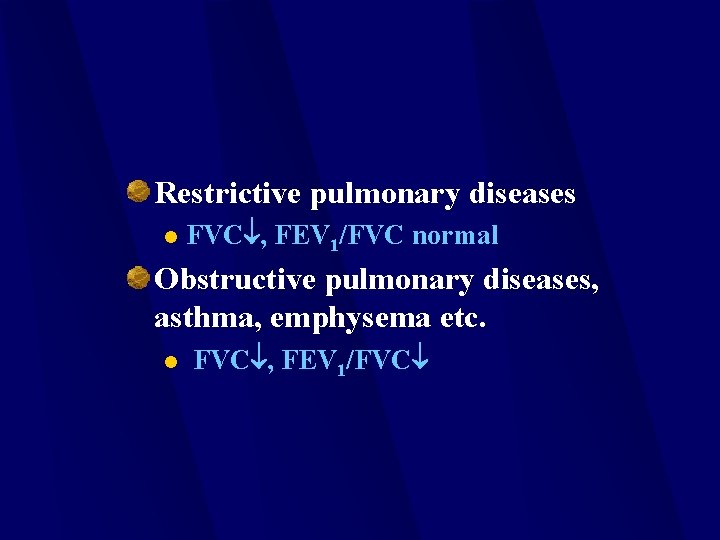
Restrictive pulmonary diseases l FVC , FEV 1/FVC normal Obstructive pulmonary diseases, asthma, emphysema etc. l FVC , FEV 1/FVC

Obstructive Pulmonary Diseases “COPD” Emphysema Chronic Bronchitis Asthma Cystic Fibrosis Interstitial Lung Disease (ILD).
Chronic Obstructive Pulmonary Disease (COPD) COPD is an accumulation of symptoms produced by respiratory diseases that result in a diagnosis if COPD. Chronic bronchitis and emphysema. COPD is a respiratory disorder or syndrome rather than a disease state.
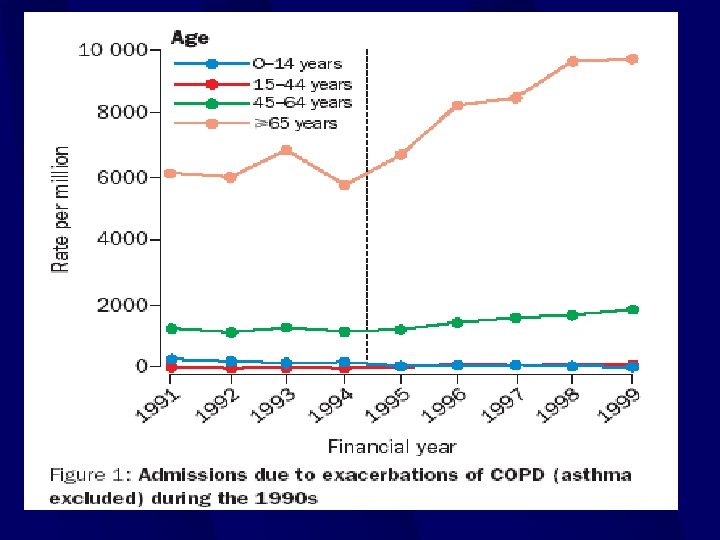
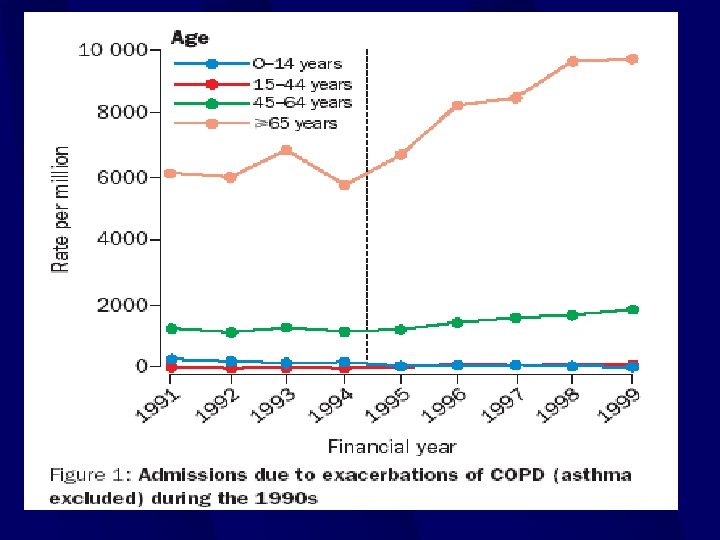
COPD Fourth leading cause of death in US. Approximately 18 million individuals. Results in $440 billion in health care costs annually. Surge of COPD in recent years.
COPD Symptoms COPD is characterized by two concepts: l l Decreased expiratory air flow pressure, and Increased resistance to expiratory air flow. These problems are caused by airway obstruction, determined by specific respiratory disease.
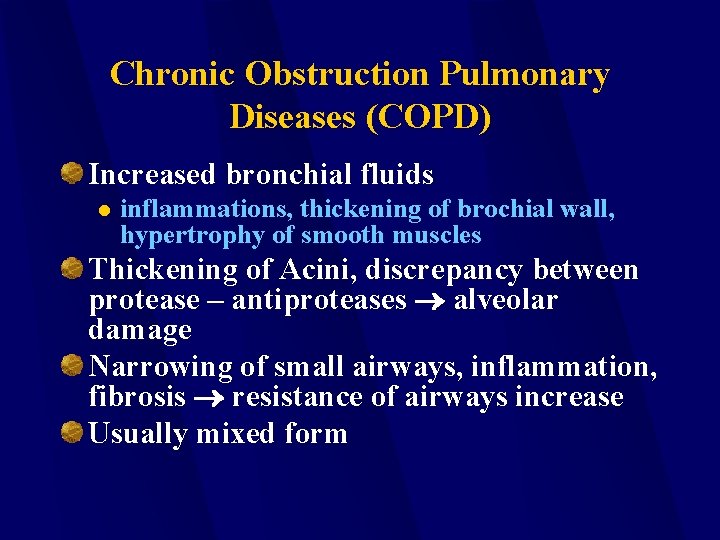
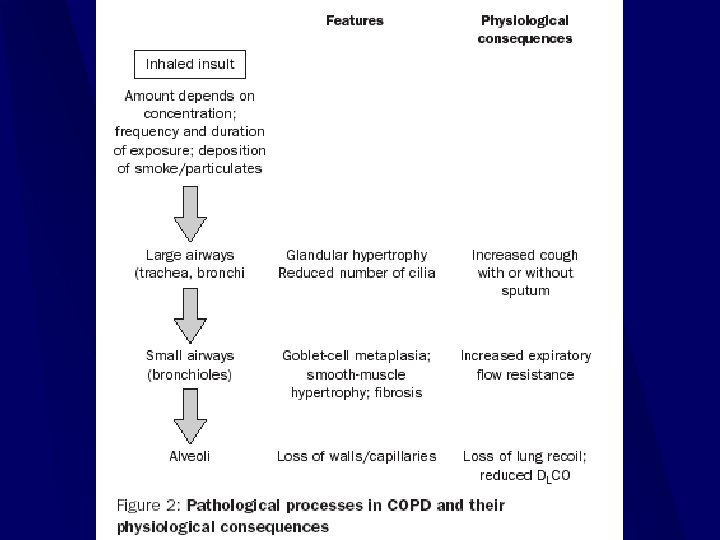
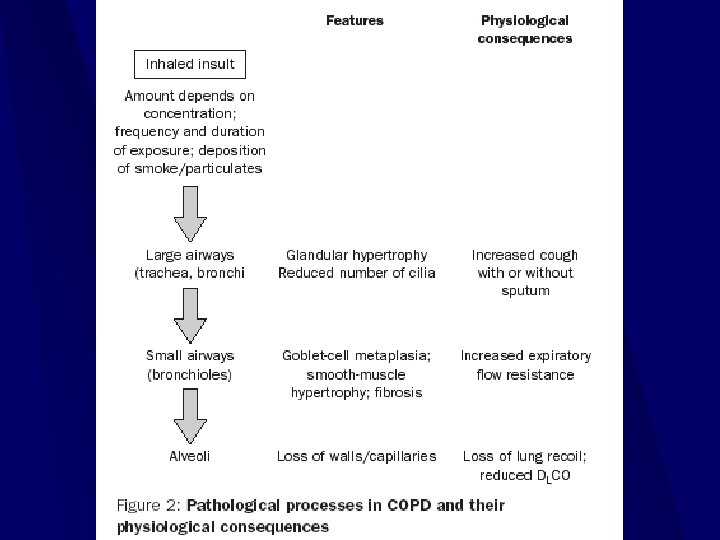
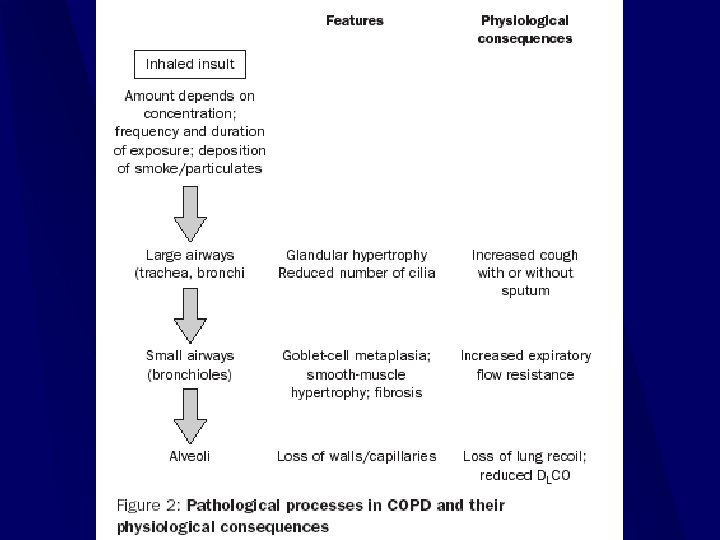
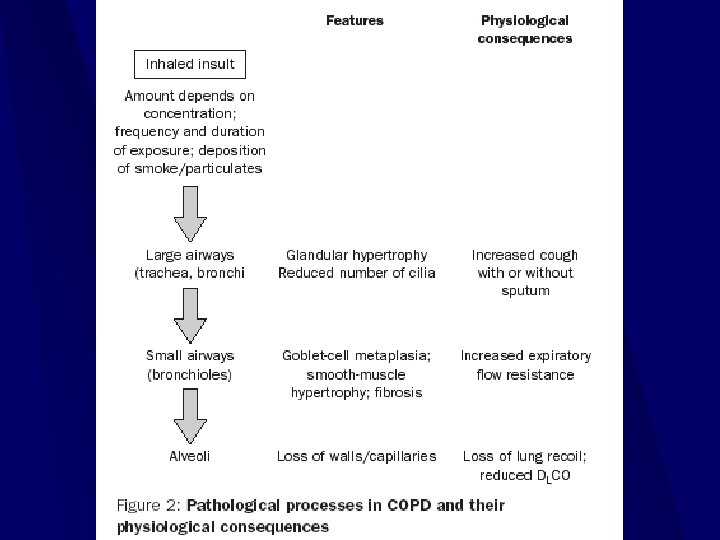
Chronic Obstruction Pulmonary Diseases (COPD) Increased bronchial fluids l inflammations, thickening of brochial wall, hypertrophy of smooth muscles Thickening of Acini, discrepancy between protease – antiproteases alveolar damage Narrowing of small airways, inflammation, fibrosis resistance of airways increase Usually mixed form
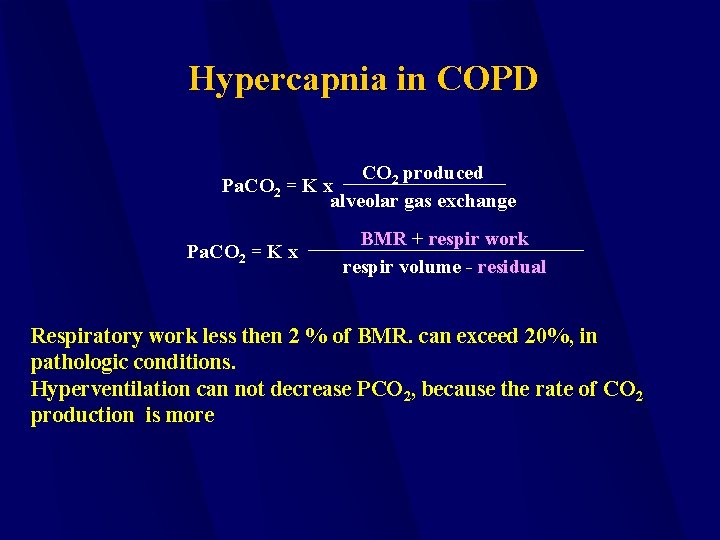
Hypercapnia in COPD CO 2 produced Pa. CO 2 = K x alveolar gas exchange Pa. CO 2 = K x BMR + respir work respir volume - residual Respiratory work less then 2 % of BMR. can exceed 20%, in pathologic conditions. Hyperventilation can not decrease PCO 2, because the rate of CO 2 production is more
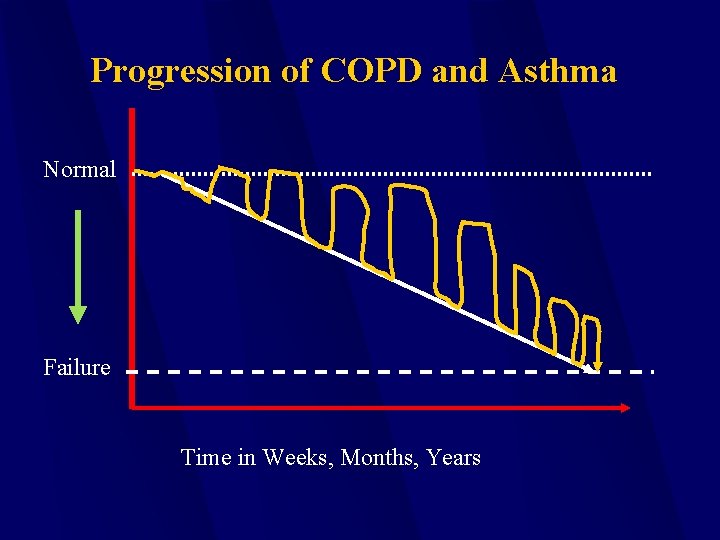
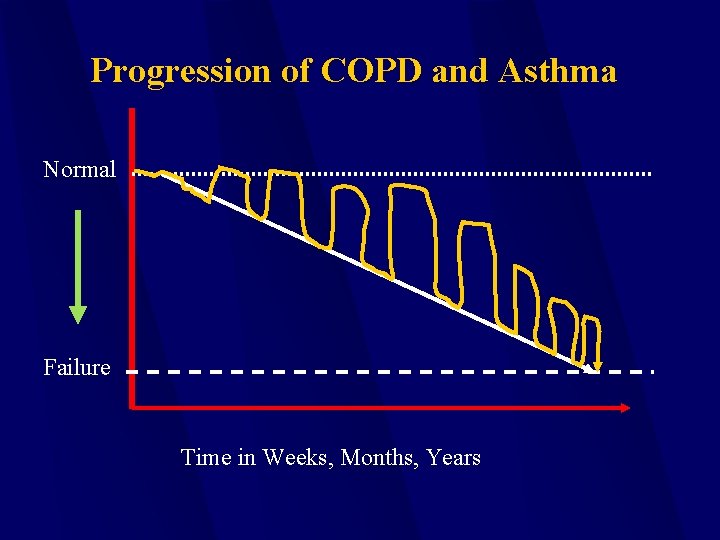
Progression of COPD and Asthma Normal Failure Time in Weeks, Months, Years
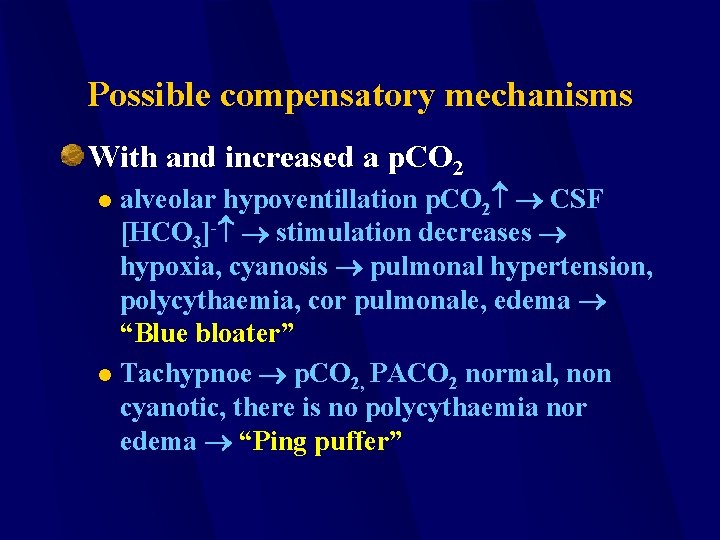
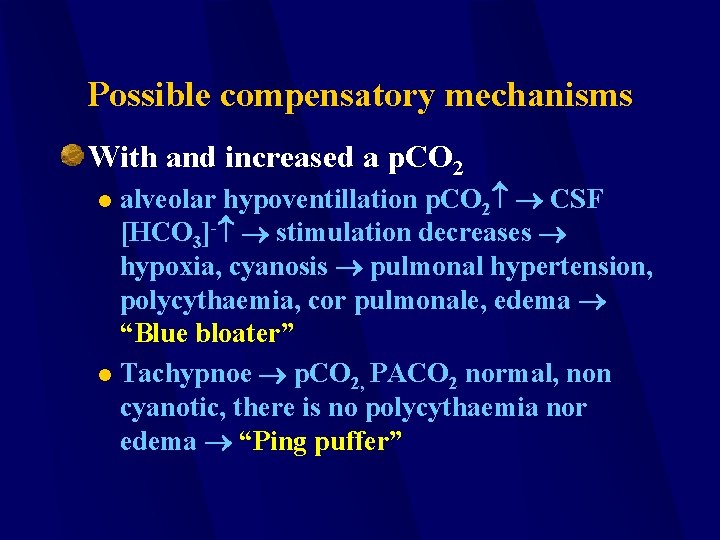
Possible compensatory mechanisms With and increased a p. CO 2 alveolar hypoventillation p. CO 2 CSF [HCO 3]- stimulation decreases hypoxia, cyanosis pulmonal hypertension, polycythaemia, cor pulmonale, edema “Blue bloater” l Tachypnoe p. CO 2, PACO 2 normal, non cyanotic, there is no polycythaemia nor edema “Ping puffer” l

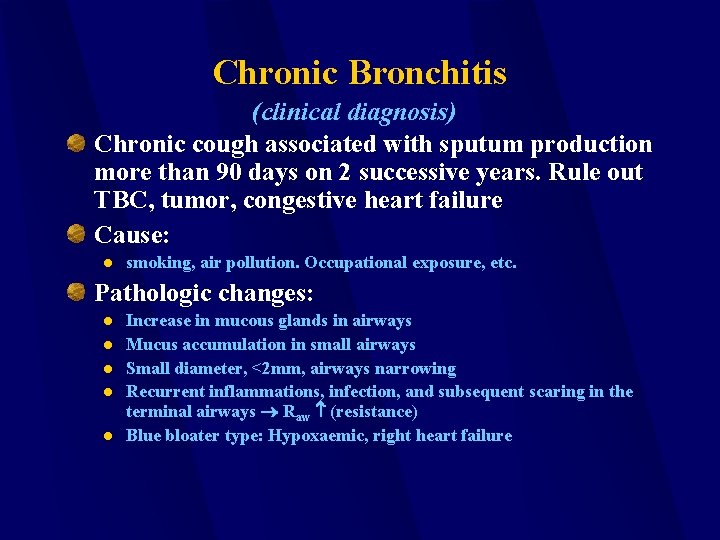
Chronic Bronchitis (clinical diagnosis) Chronic cough associated with sputum production more than 90 days on 2 successive years. Rule out TBC, tumor, congestive heart failure Cause: l smoking, air pollution. Occupational exposure, etc. Pathologic changes: l l l Increase in mucous glands in airways Mucus accumulation in small airways Small diameter, <2 mm, airways narrowing Recurrent inflammations, infection, and subsequent scaring in the terminal airways Raw (resistance) Blue bloater type: Hypoxaemic, right heart failure
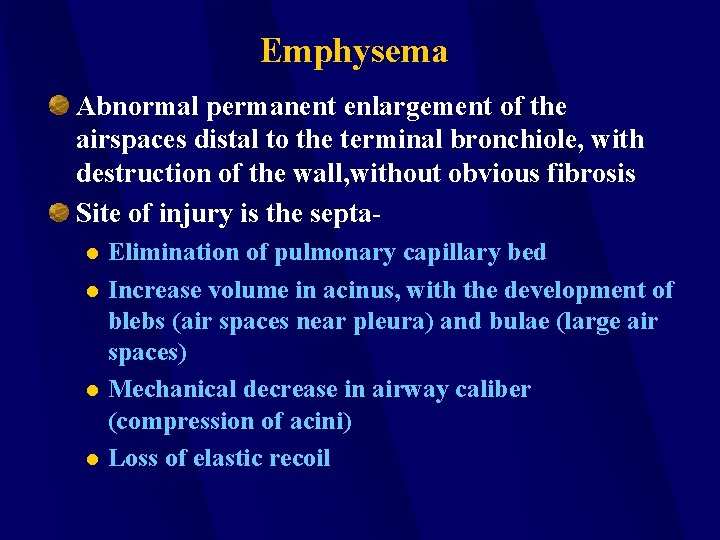
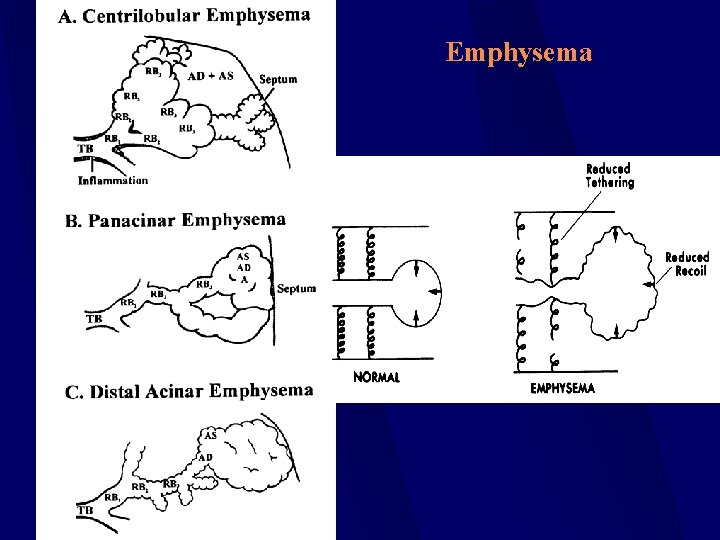
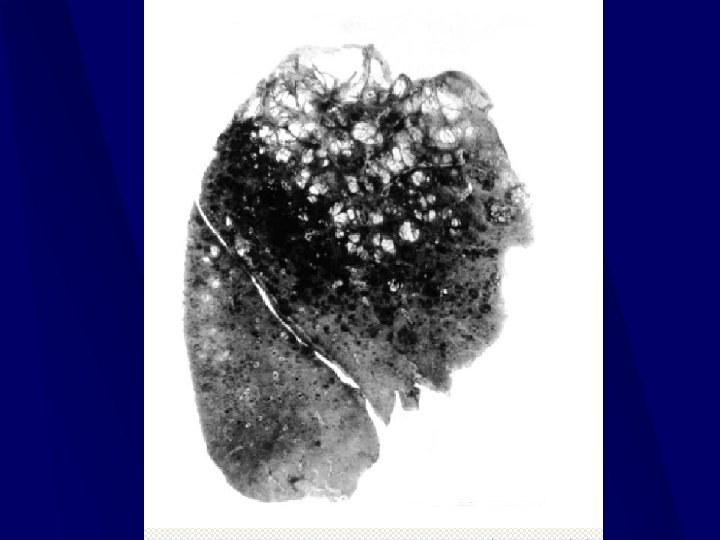
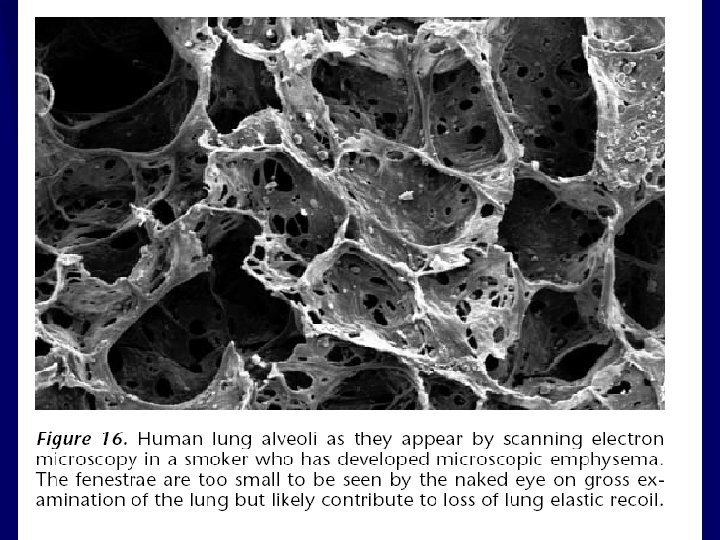
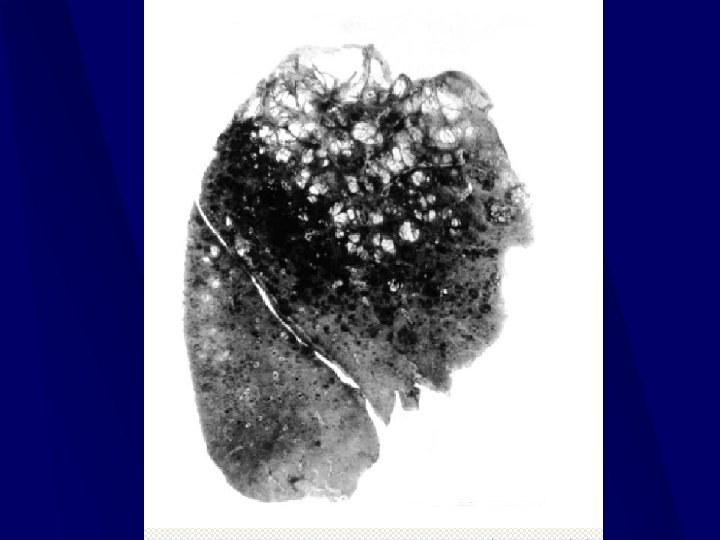
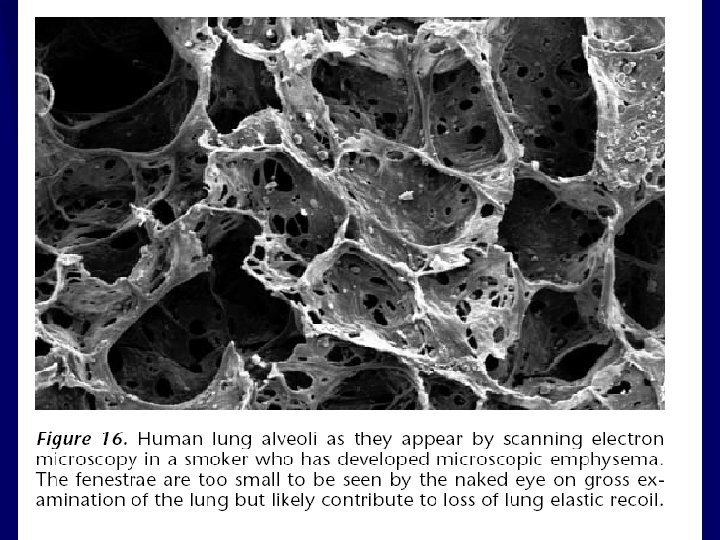
Emphysema Abnormal permanent enlargement of the airspaces distal to the terminal bronchiole, with destruction of the wall, without obvious fibrosis Site of injury is the septal l Elimination of pulmonary capillary bed Increase volume in acinus, with the development of blebs (air spaces near pleura) and bulae (large air spaces) Mechanical decrease in airway caliber (compression of acini) Loss of elastic recoil
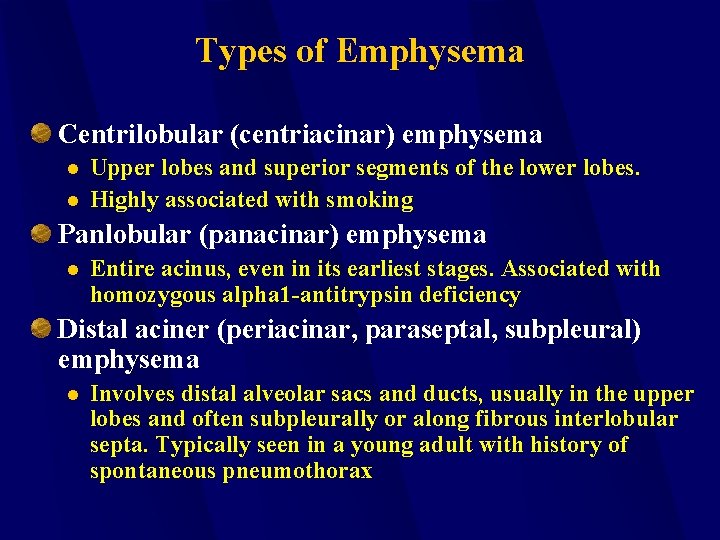
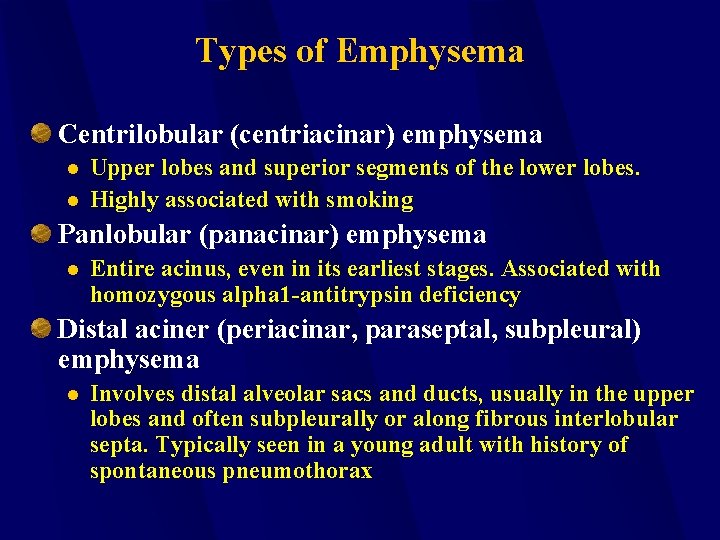
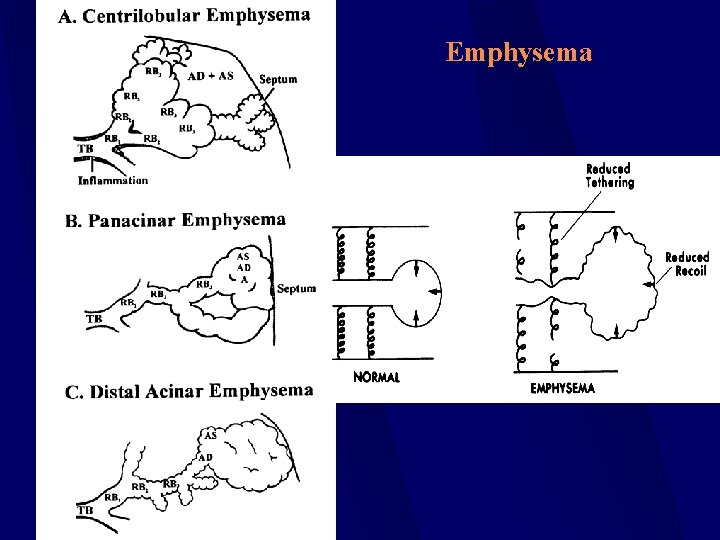
Types of Emphysema Centrilobular (centriacinar) emphysema l l Upper lobes and superior segments of the lower lobes. Highly associated with smoking Panlobular (panacinar) emphysema l Entire acinus, even in its earliest stages. Associated with homozygous alpha 1 -antitrypsin deficiency Distal aciner (periacinar, paraseptal, subpleural) emphysema l Involves distal alveolar sacs and ducts, usually in the upper lobes and often subpleurally or along fibrous interlobular septa. Typically seen in a young adult with history of spontaneous pneumothorax
Emphysema
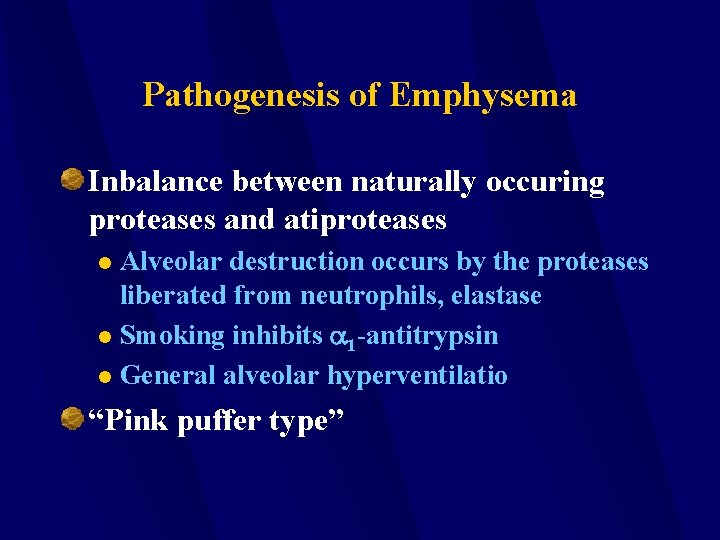
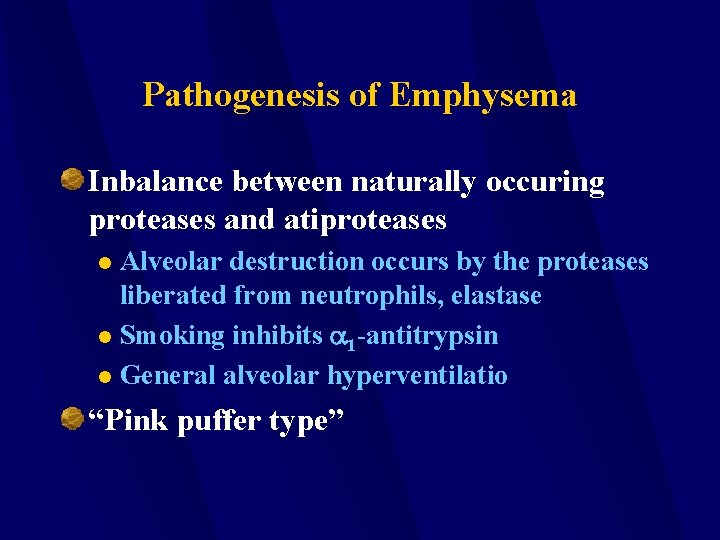
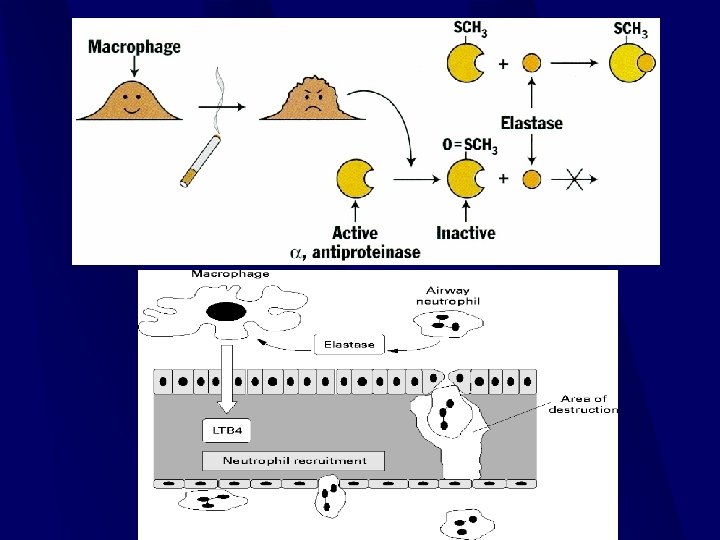
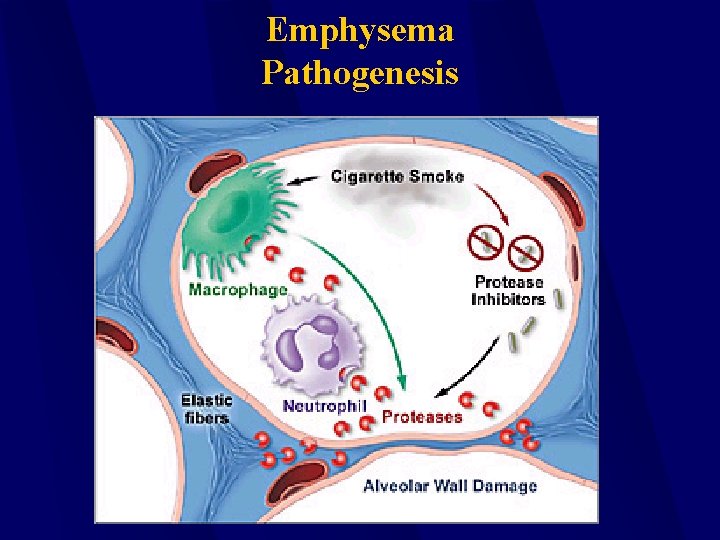
Pathogenesis of Emphysema Inbalance between naturally occuring proteases and atiproteases Alveolar destruction occurs by the proteases liberated from neutrophils, elastase l Smoking inhibits a 1 -antitrypsin l General alveolar hyperventilatio l “Pink puffer type”
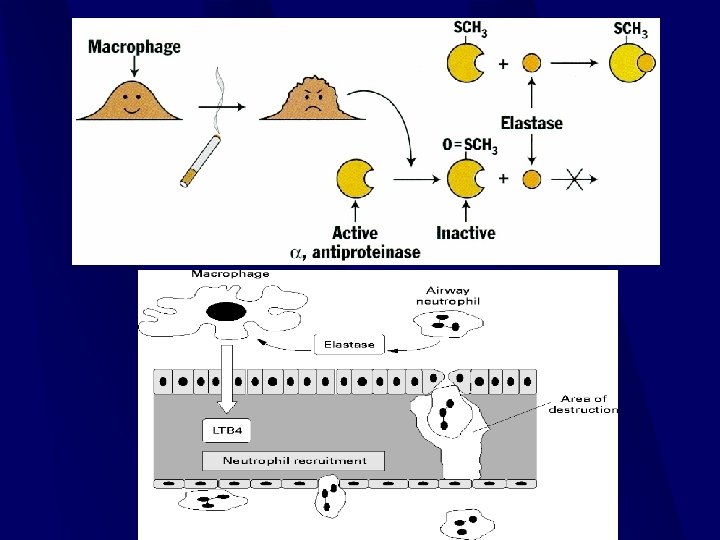
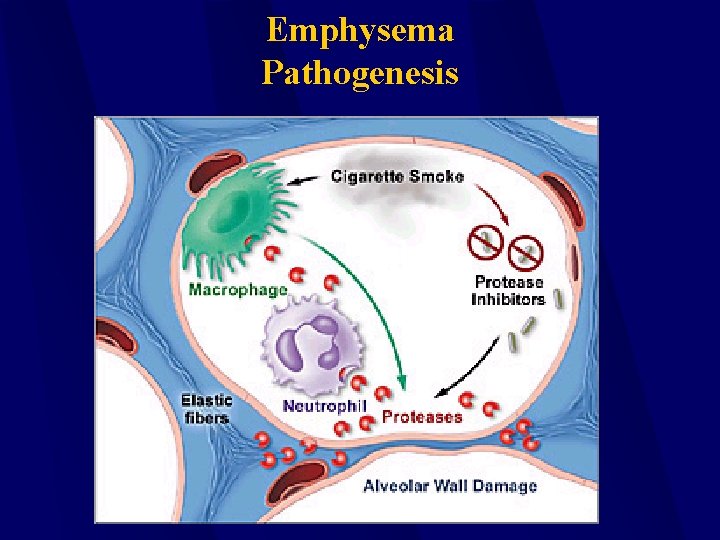
Emphysema Pathogenesis
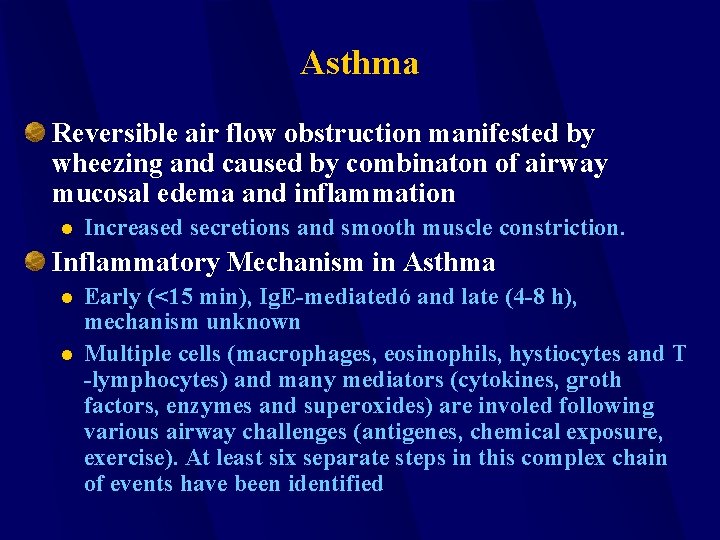
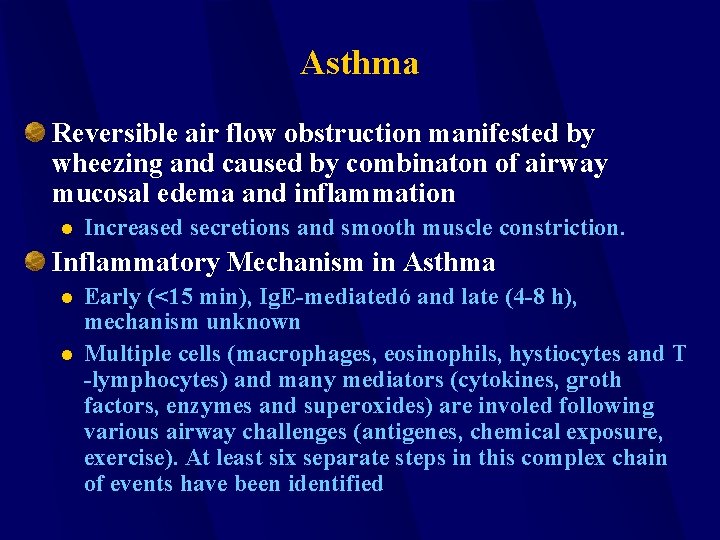
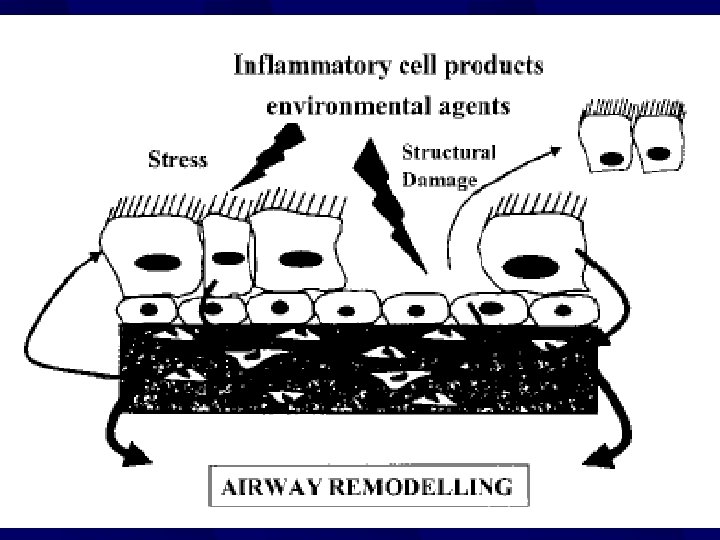
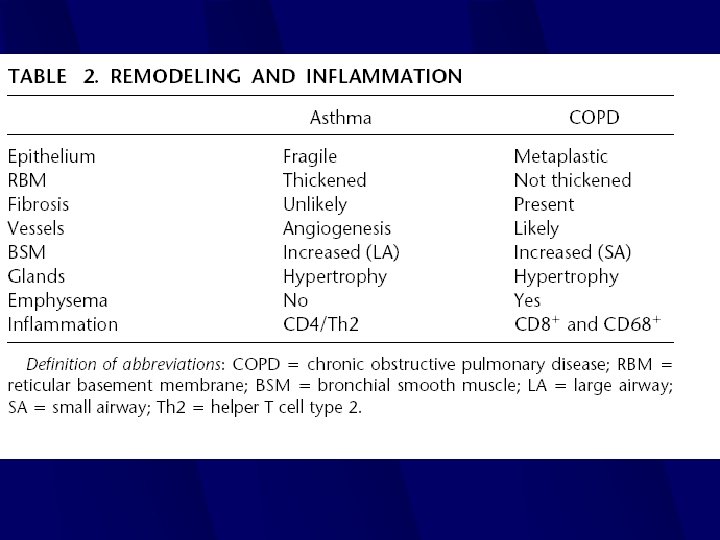
Asthma Reversible air flow obstruction manifested by wheezing and caused by combinaton of airway mucosal edema and inflammation l Increased secretions and smooth muscle constriction. Inflammatory Mechanism in Asthma l l Early (<15 min), Ig. E-mediatedó and late (4 -8 h), mechanism unknown Multiple cells (macrophages, eosinophils, hystiocytes and T -lymphocytes) and many mediators (cytokines, groth factors, enzymes and superoxides) are involed following various airway challenges (antigenes, chemical exposure, exercise). At least six separate steps in this complex chain of events have been identified
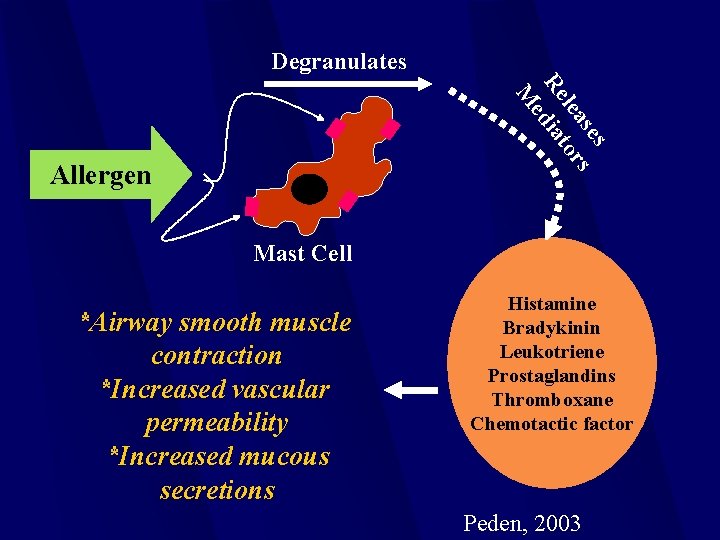
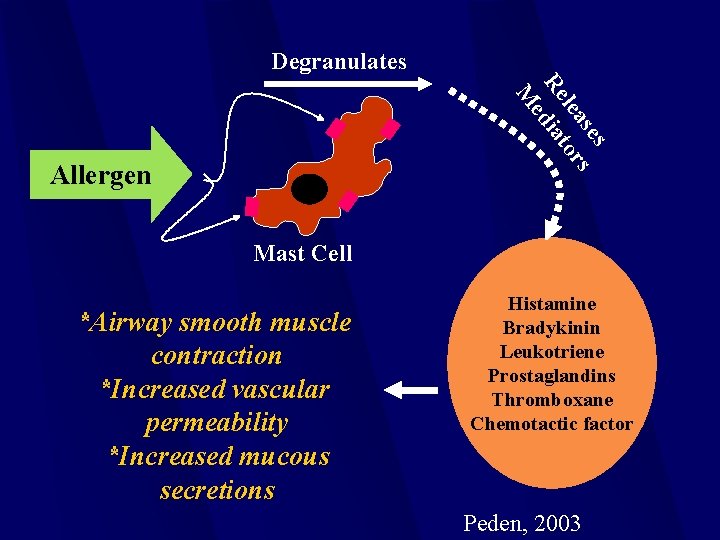
Degranulates s se s lea tor Re dia e M Allergen Mast Cell *Airway smooth muscle contraction *Increased vascular permeability *Increased mucous secretions Histamine Bradykinin Leukotriene Prostaglandins Thromboxane Chemotactic factor Peden, 2003
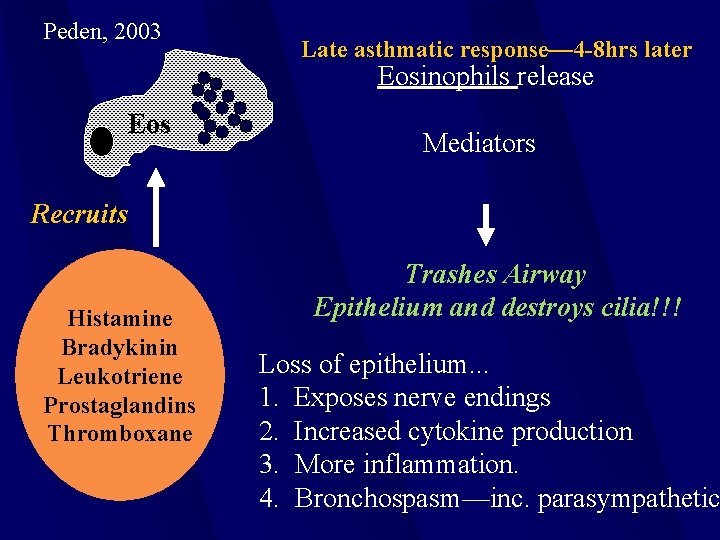
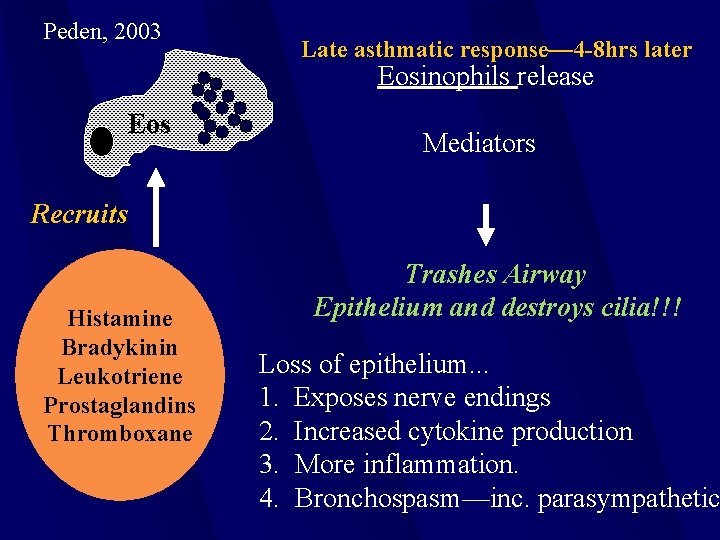
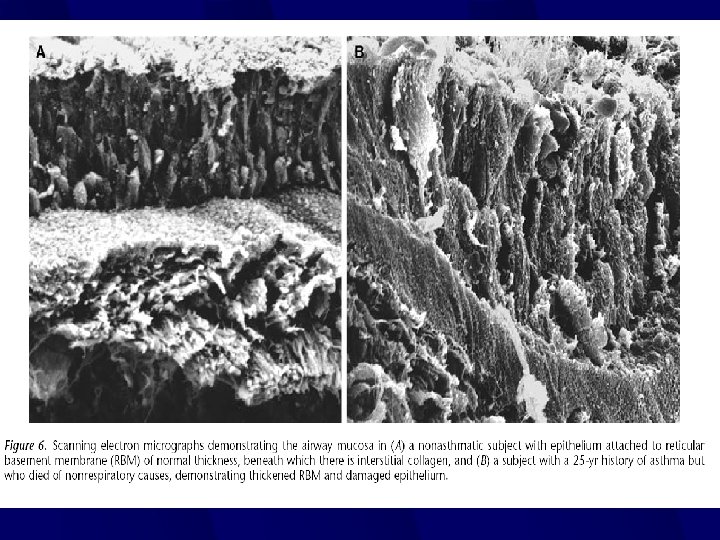
Peden, 2003 Late asthmatic response— 4 -8 hrs later Eosinophils release Eos Mediators Recruits Histamine Bradykinin Leukotriene Prostaglandins Thromboxane Trashes Airway Epithelium and destroys cilia!!! Loss of epithelium. . . 1. Exposes nerve endings 2. Increased cytokine production 3. More inflammation. 4. Bronchospasm—inc. parasympathetic
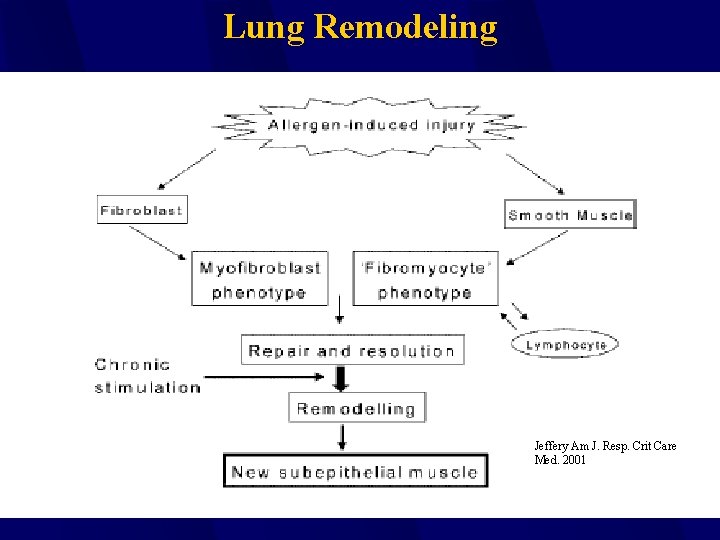
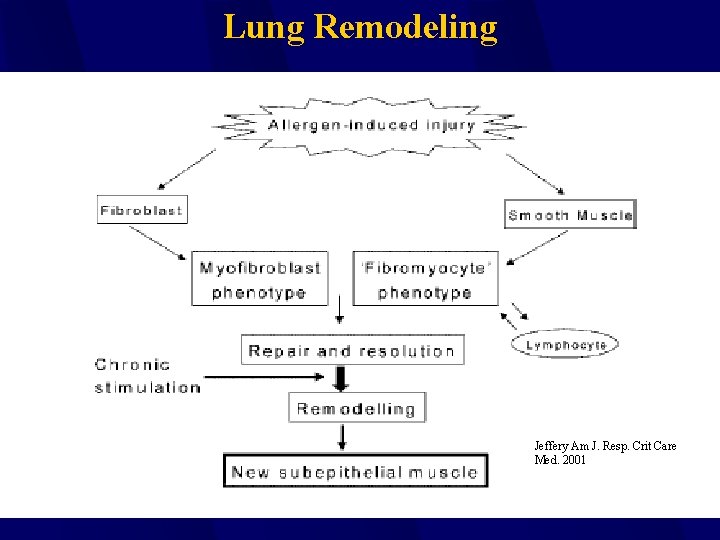
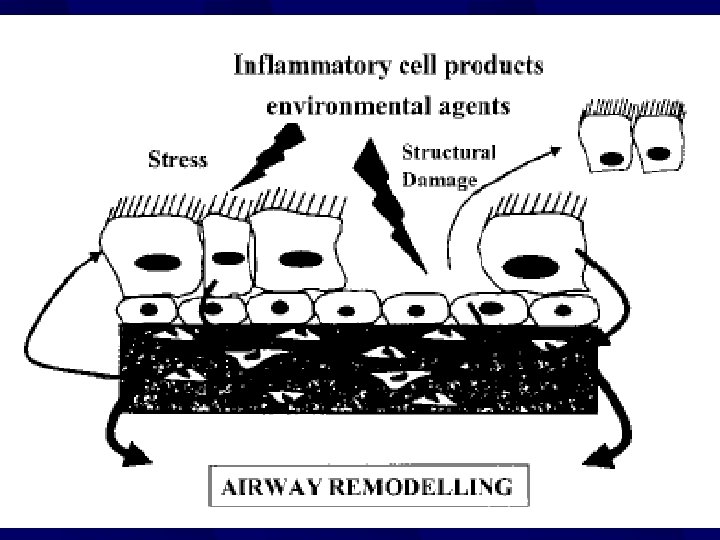
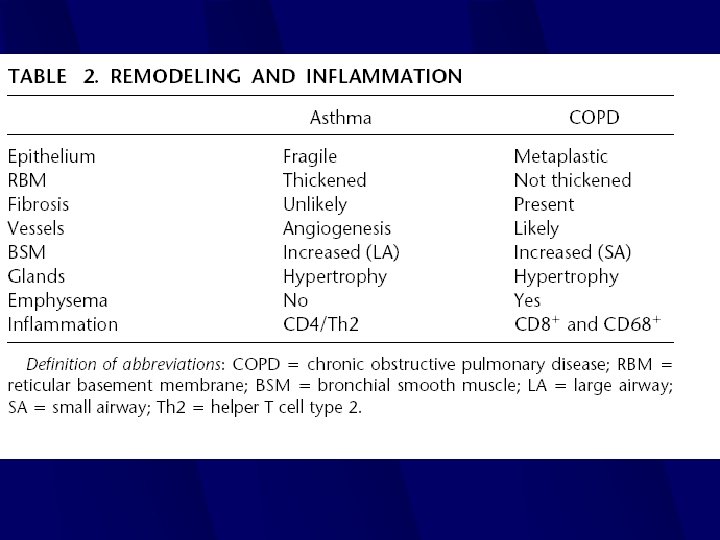
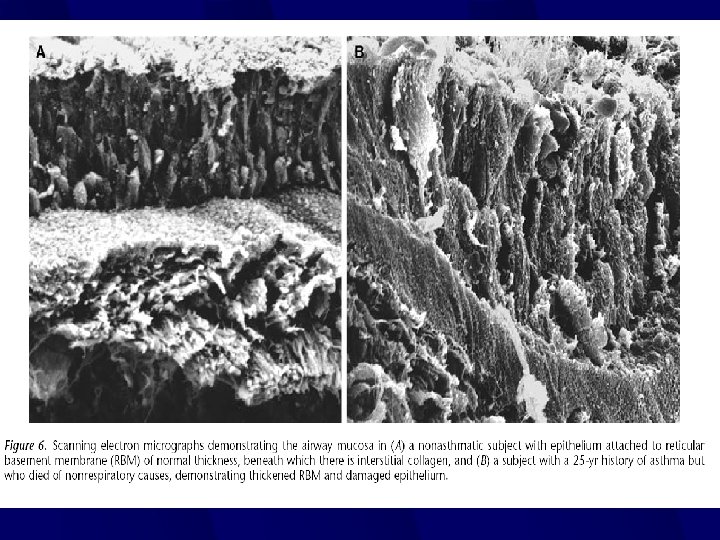
Lung Remodeling Jeffery Am J. Resp. Crit Care Med. 2001
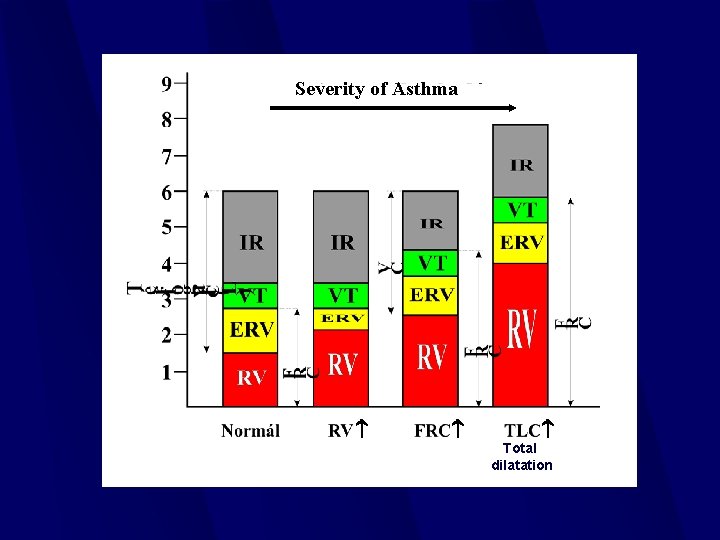
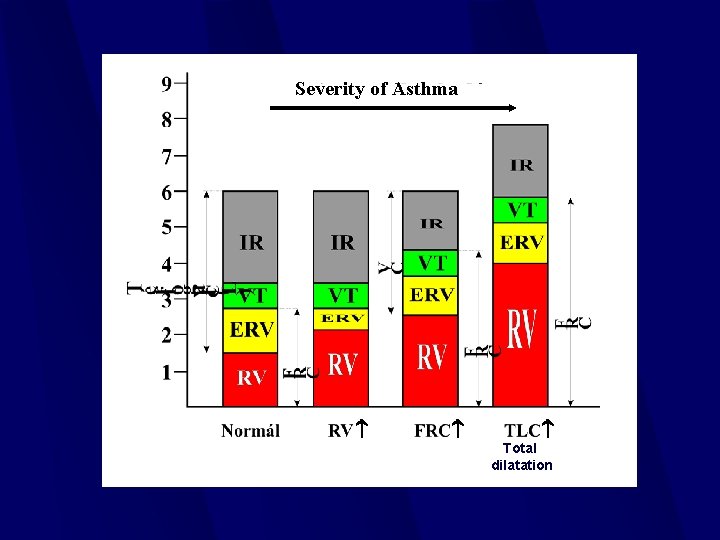
Severity of Asthma Total dilatation
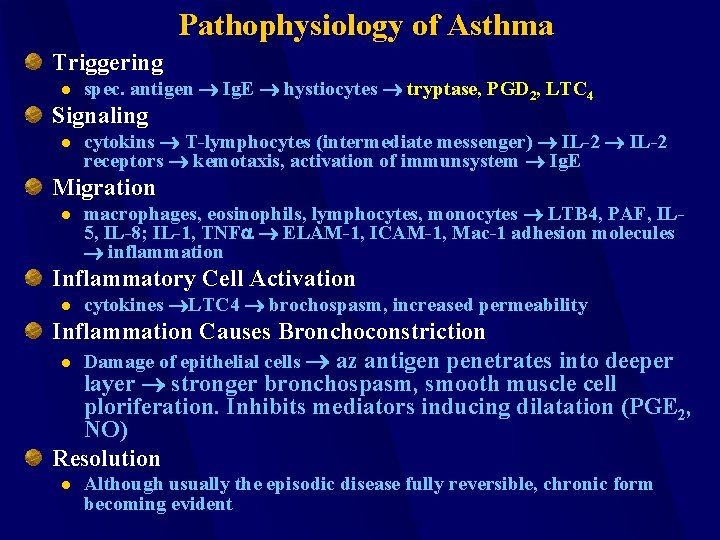
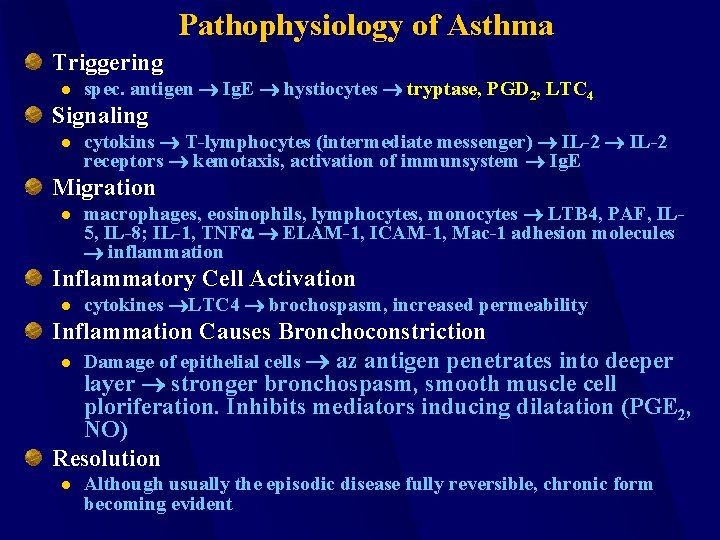
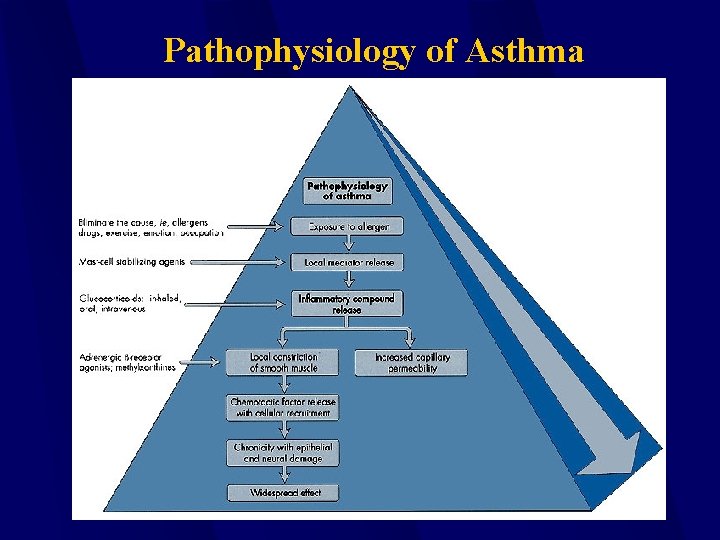
Pathophysiology of Asthma Triggering l spec. antigen Ig. E hystiocytes tryptase, PGD 2, LTC 4 Signaling l cytokins T-lymphocytes (intermediate messenger) IL-2 receptors kemotaxis, activation of immunsystem Ig. E Migration l macrophages, eosinophils, lymphocytes, monocytes LTB 4, PAF, IL 5, IL-8; IL-1, TNFa ELAM-1, ICAM-1, Mac-1 adhesion molecules inflammation Inflammatory Cell Activation l cytokines LTC 4 brochospasm, increased permeability Inflammation Causes Bronchoconstriction l Damage of epithelial cells az antigen penetrates into deeper layer stronger bronchospasm, smooth muscle cell ploriferation. Inhibits mediators inducing dilatation (PGE 2, NO) Resolution l Although usually the episodic disease fully reversible, chronic form becoming evident
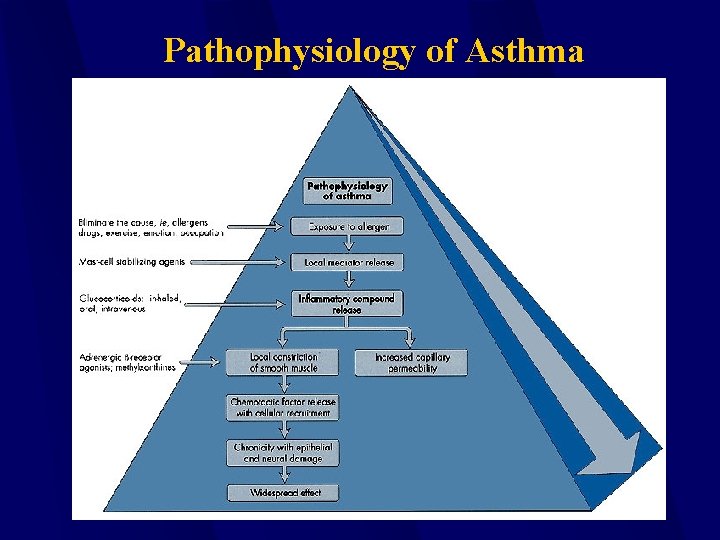
Pathophysiology of Asthma
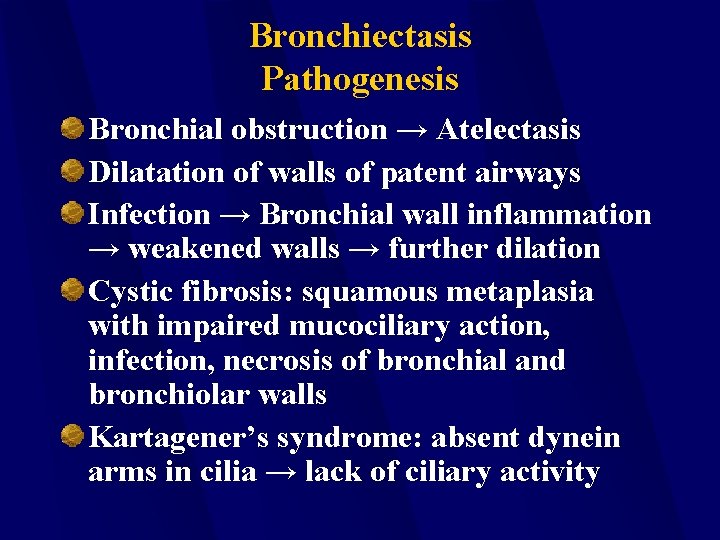
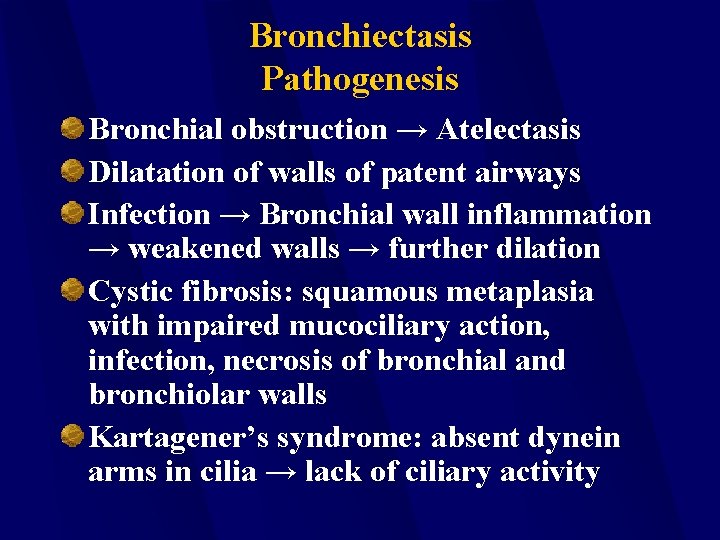
Bronchiectasis Pathogenesis Bronchial obstruction → Atelectasis Dilatation of walls of patent airways Infection → Bronchial wall inflammation → weakened walls → further dilation Cystic fibrosis: squamous metaplasia with impaired mucociliary action, infection, necrosis of bronchial and bronchiolar walls Kartagener’s syndrome: absent dynein arms in cilia → lack of ciliary activity
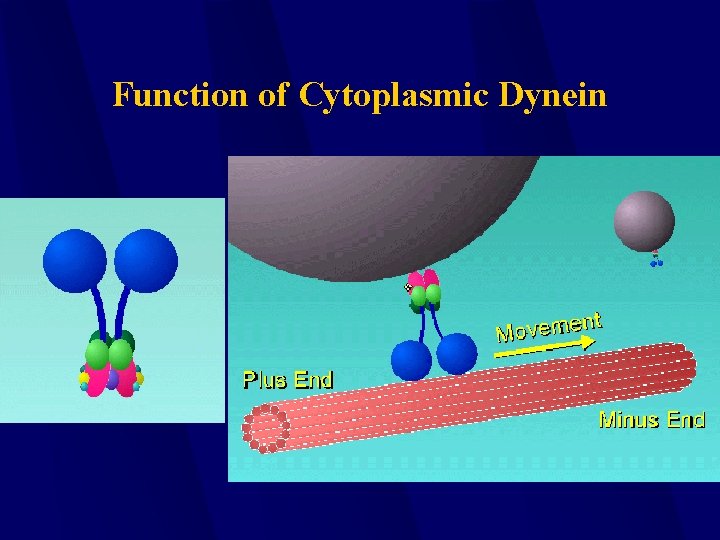
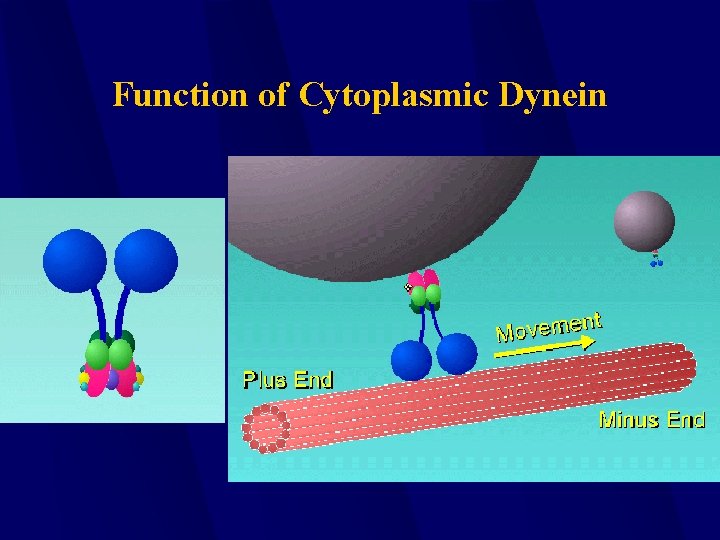
Function of Cytoplasmic Dynein
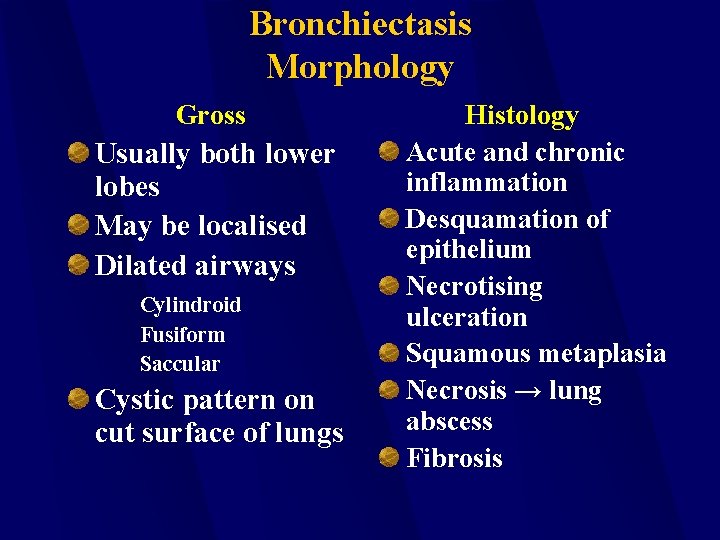
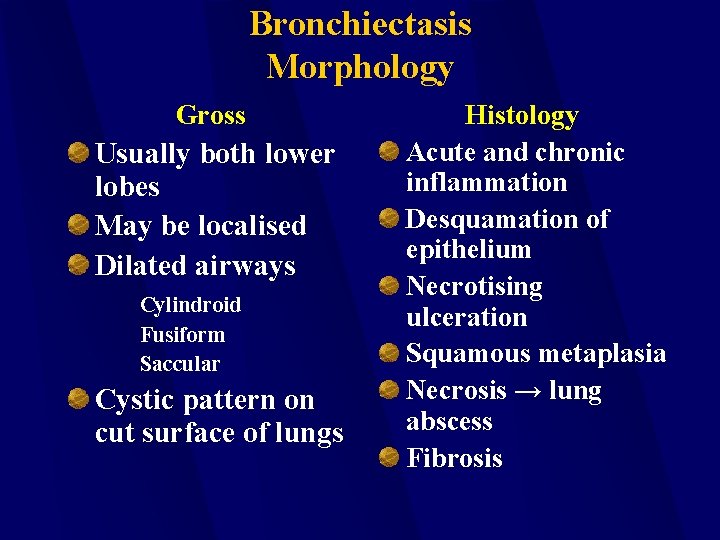
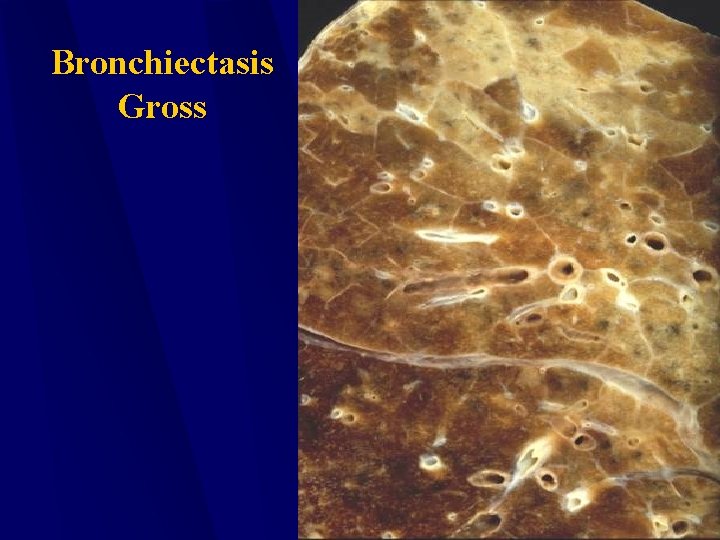
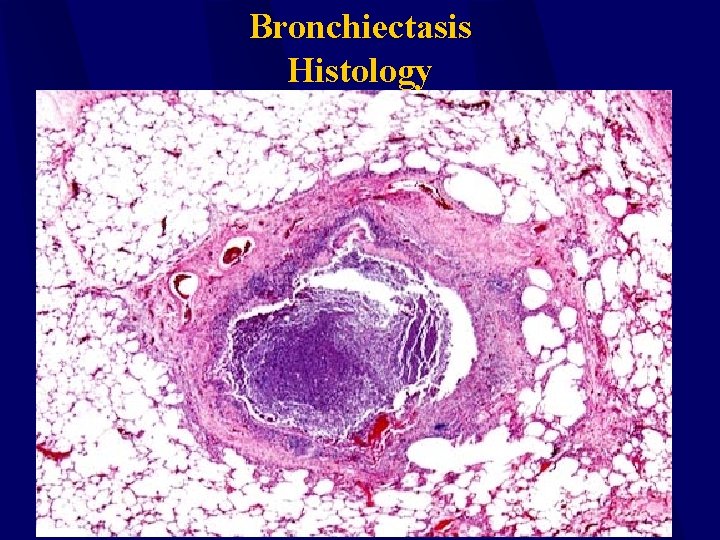
Bronchiectasis Morphology Gross Usually both lower lobes May be localised Dilated airways Cylindroid Fusiform Saccular Cystic pattern on cut surface of lungs Histology Acute and chronic inflammation Desquamation of epithelium Necrotising ulceration Squamous metaplasia Necrosis → lung abscess Fibrosis
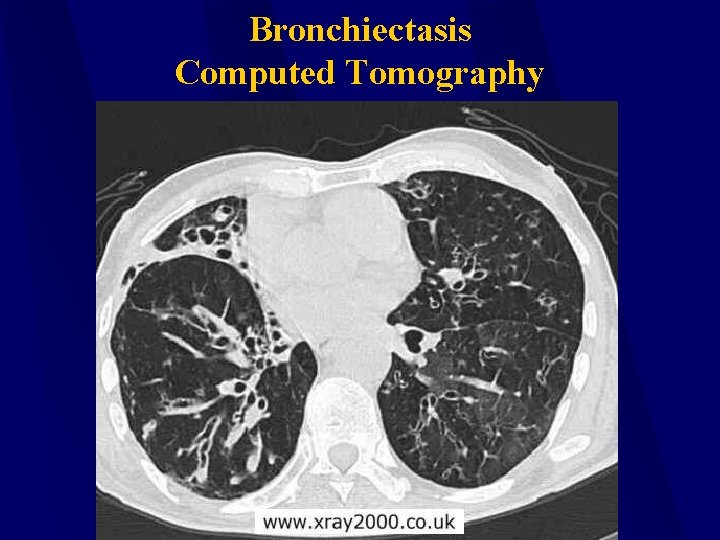
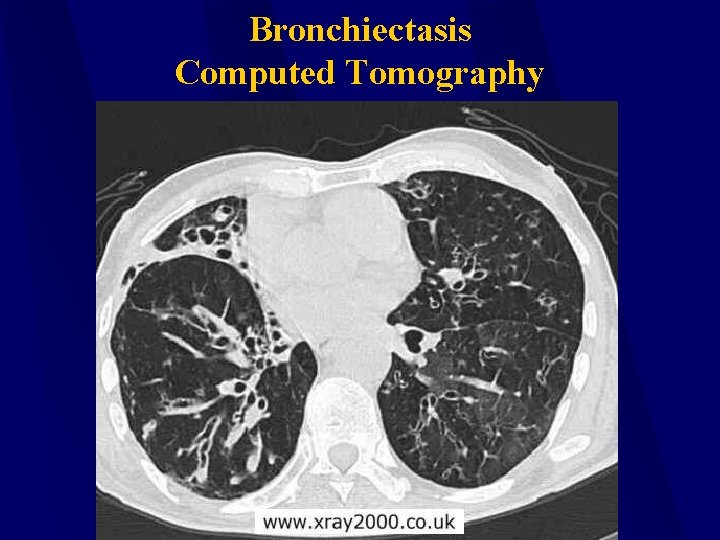
Bronchiectasis Computed Tomography
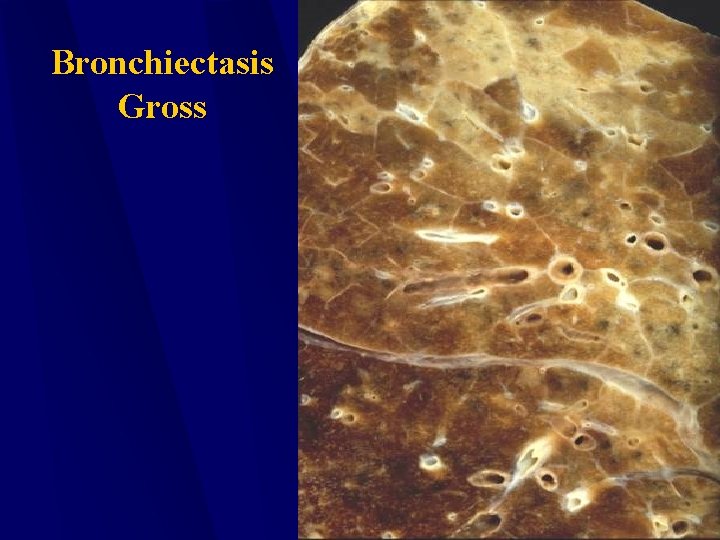
Bronchiectasis Gross
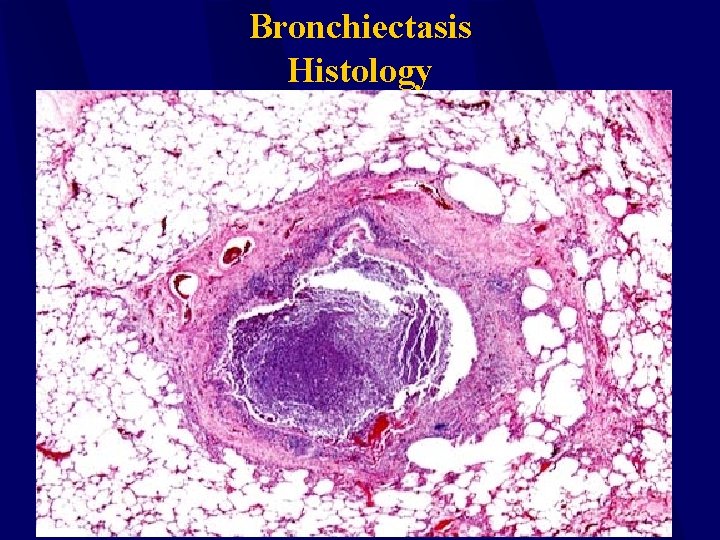
Bronchiectasis Histology
Bronchiectasis Complications Pneumonia Lung abscess Empyema Septicaemia Cor pulmonale Metastatic cerebral abscesses Secondary Amyloidosis
Cystic Fibrosis Genetic deficiency disease characterized by recurrent respiratory tract infections. Estimated 1 in 20 individuals carry trait for CF. Typically diagnosed by age of 6 months. Limits life expectancy to ~29 years.
Cystic Fibrosis Improper cellular retention of sodium chloride – lungs, pancreas. Na. Cl draws water from airways, resulting in dry mucus. Airway obstruction, resulting in respiratory infection and tissue damage.
Cystic Fibrosis Individuals can go asymptomatic until adolescence. Later trigger, however, indicates more rapid decline in health. Typically will also involve heptatic system, including cirrhosis and jaundice.
Diagnosis PE and history of respiratory infections during infancy/childhood. Sweat test – increased sodium marker. DNA analysis. Currently, genetic engineering is attempting to develop way to modify gene.
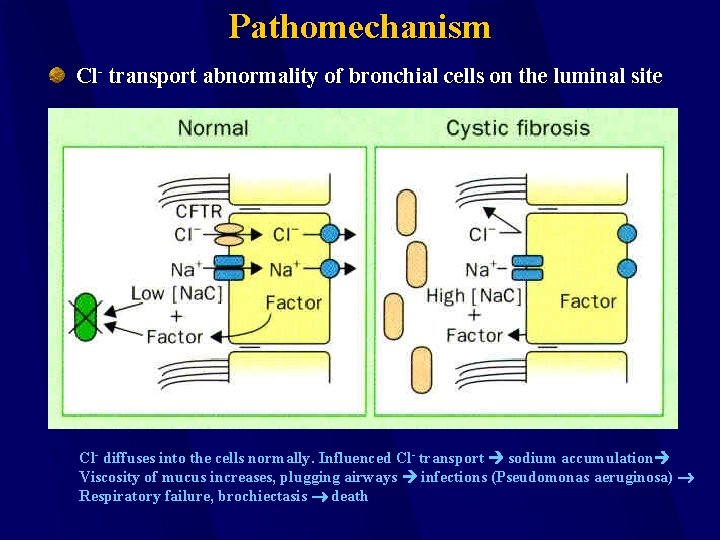
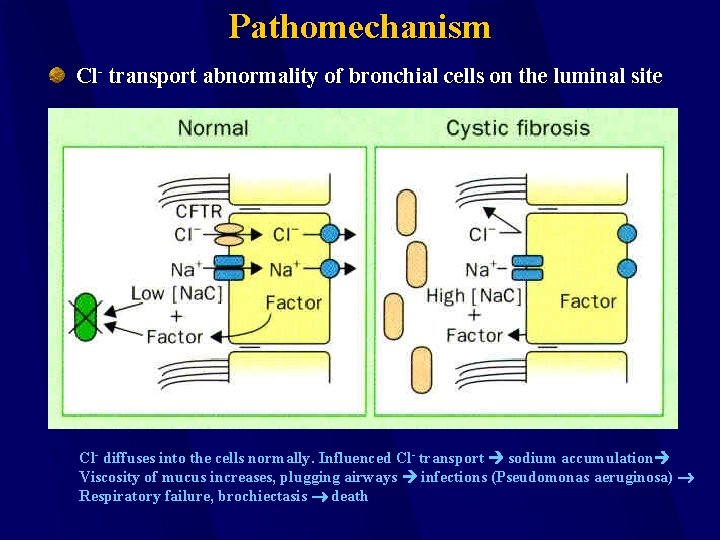
Pathomechanism Cl- transport abnormality of bronchial cells on the luminal site Cl- diffuses into the cells normally. Influenced Cl- transport sodium accumulation Viscosity of mucus increases, plugging airways infections (Pseudomonas aeruginosa) Respiratory failure, brochiectasis death
a 1 – antitrypsin Deficiency (AAT) Autosomal disease (more than 75 allels have been identified), decreased amount of antitrypsin produced. Antiprotease activity decreases elastase activity ↑ emphysema by age of 40, develops earlier in smokers.
Interstitial Lung Disease Inflammation of the alveolar walls inside the lungs. Almost exclusively from industrial irritants and agricultural byproducts. Numerous conditions coined in occupational health to describe ILD.
Interstitial Lung Disease Black lung – coal dust from mining. Farmer’s lung – fungi exposure in moldy hay. Bird breeder’s lung – inhalation of avian proteins. Silicosis – inhalation of silicon dust. Asbestosis – inhalation of asbestos. Exposure to wood products, detergents, metals, and other animal proteins.
Diagnosis PE. Evaluation of job site. X-ray of lungs. Spirometry
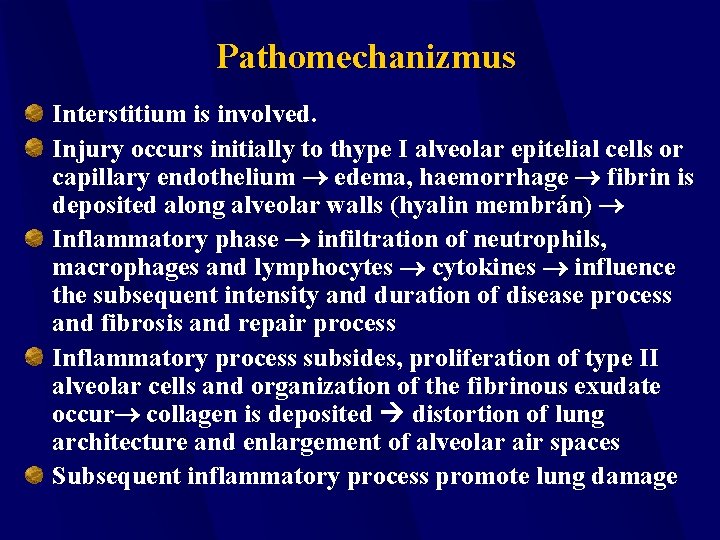
Pathomechanizmus Interstitium is involved. Injury occurs initially to thype I alveolar epitelial cells or capillary endothelium edema, haemorrhage fibrin is deposited along alveolar walls (hyalin membrán) Inflammatory phase infiltration of neutrophils, macrophages and lymphocytes cytokines influence the subsequent intensity and duration of disease process and fibrosis and repair process Inflammatory process subsides, proliferation of type II alveolar cells and organization of the fibrinous exudate occur collagen is deposited distortion of lung architecture and enlargement of alveolar air spaces Subsequent inflammatory process promote lung damage
This should be enough for to day
 Matematika ng egypt
Matematika ng egypt Paddestoel
Paddestoel Molnr
Molnr Molnr
Molnr Types of emphysema
Types of emphysema Pathophysiology semmelweis
Pathophysiology semmelweis Ontario mikls
Ontario mikls Mikls
Mikls Davis mikls
Davis mikls Eszéki híd felégetése
Eszéki híd felégetése Mikls
Mikls Mikls
Mikls Capture beat
Capture beat Failure to sense pacemaker
Failure to sense pacemaker Ductile fracture mechanism
Ductile fracture mechanism Type i respiratory failure
Type i respiratory failure Pink puffer
Pink puffer Patm disease
Patm disease Type 1 respiratory failure
Type 1 respiratory failure Respiratory failure type
Respiratory failure type Nursing management of dyspnea ppt
Nursing management of dyspnea ppt Solid thyroid nodule
Solid thyroid nodule Agnes csaki semmelweis
Agnes csaki semmelweis Semmelweis university faculty of medicine
Semmelweis university faculty of medicine What is the conducting zone of the respiratory system
What is the conducting zone of the respiratory system Doktori iskola sote
Doktori iskola sote Semmelweis itc
Semmelweis itc Retikulinfasern leber
Retikulinfasern leber Semmelweis
Semmelweis Orthodontics semmelweis
Orthodontics semmelweis Semmelweis
Semmelweis Semmelweis egyetem konzerváló fogászati klinika budapest
Semmelweis egyetem konzerváló fogászati klinika budapest Semmelweis egyetem szemészeti klinika budapest
Semmelweis egyetem szemészeti klinika budapest Határidősz
Határidősz Nasal vestibule
Nasal vestibule Semmelweis
Semmelweis Erasmus plus semmelweis
Erasmus plus semmelweis Itc semmelweis
Itc semmelweis Different between plasma and serum
Different between plasma and serum Semmelweis arc
Semmelweis arc Semmelweis
Semmelweis Konservierende zahnheilkunde semmelweis
Konservierende zahnheilkunde semmelweis Semmelweis egyetem bérosztály
Semmelweis egyetem bérosztály Itc.semmelweis
Itc.semmelweis Ignas semmelweis
Ignas semmelweis Gastrulation and neurulation
Gastrulation and neurulation Semmelweis portál
Semmelweis portál Pathophysiologie semmelweis
Pathophysiologie semmelweis Semmelweis reflex
Semmelweis reflex Tubulointerstitial nephritis
Tubulointerstitial nephritis Gsi semmelweis
Gsi semmelweis Semmelweis egyetem humán erőforrás
Semmelweis egyetem humán erőforrás Amnionüreg
Amnionüreg Weilaner
Weilaner Carpi volare
Carpi volare Se etk dse
Se etk dse Garatívek
Garatívek Institute of industrial science the university of tokyo
Institute of industrial science the university of tokyo Confucius institute at moscow state linguistic university
Confucius institute at moscow state linguistic university Lviv polytechnic university
Lviv polytechnic university George mason university english language institute
George mason university english language institute King abdulaziz university english language institute
King abdulaziz university english language institute Angli ruskin
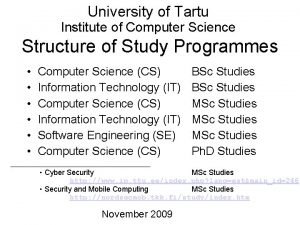
Angli ruskin University of tartu institute of computer science
University of tartu institute of computer science National technical university kharkiv polytechnic institute
National technical university kharkiv polytechnic institute Francisco de asis university institute
Francisco de asis university institute Addis ababa university institute of technology
Addis ababa university institute of technology 沈榮麟
沈榮麟 Theories of failure
Theories of failure Failure to sense
Failure to sense Long term memory
Long term memory Earthy look in chronic renal failure
Earthy look in chronic renal failure Internal failure costs examples
Internal failure costs examples Example of encoding failure
Example of encoding failure Fbi virtual case file case study
Fbi virtual case file case study Principles of information security 5th edition pdf
Principles of information security 5th edition pdf Failure to thrive definition
Failure to thrive definition Patriot missile failure case study
Patriot missile failure case study Patriot missile failure
Patriot missile failure Heart failure and frank starling law
Heart failure and frank starling law Treatments for acute renal failure
Treatments for acute renal failure Advantages and challenges of multigrade teaching
Advantages and challenges of multigrade teaching Example of encoding failure
Example of encoding failure Define market failure
Define market failure The failure of the league of nations
The failure of the league of nations Cardiomegay
Cardiomegay Power failure andrew forster
Power failure andrew forster Portal hypertension definition
Portal hypertension definition Hepatic encephalopathy symptoms
Hepatic encephalopathy symptoms Heart failure defined
Heart failure defined New york scale heart failure
New york scale heart failure Sod table in fmea
Sod table in fmea Partial failure meaning
Partial failure meaning Fatigue beach marks
Fatigue beach marks League of nations
League of nations Iap teaching slides
Iap teaching slides League of nations
League of nations Buck converter failure modes
Buck converter failure modes Failure point analysis
Failure point analysis Failure mode and effect analysis
Failure mode and effect analysis Bonding fail
Bonding fail Signal box failure
Signal box failure Roger boisjoly
Roger boisjoly Edema assessment
Edema assessment Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Heart failure complications
Heart failure complications Blind to failure summary
Blind to failure summary Chapter 24 heart failure drugs
Chapter 24 heart failure drugs Role of government in correcting market failure
Role of government in correcting market failure Brand extension definition
Brand extension definition Erp implementation failure a case study
Erp implementation failure a case study Principles of bpr
Principles of bpr Fhf
Fhf Cushings triad
Cushings triad Hepatic encephalopathy stages
Hepatic encephalopathy stages Example of encoding failure
Example of encoding failure Market failure definition ib
Market failure definition ib Indirect tax to correct market failure
Indirect tax to correct market failure Incidence of subsidy
Incidence of subsidy Design for flexure
Design for flexure Overcoming challenges essay
Overcoming challenges essay Failure of appeasement definition
Failure of appeasement definition Heart failure
Heart failure Simplifying and isolating failure-inducing input
Simplifying and isolating failure-inducing input Failure in ddbms
Failure in ddbms Factors of project success and failure
Factors of project success and failure Photo emission microscopy failure analysis
Photo emission microscopy failure analysis