Acute respiratory failure Definitions acute respiratory failure occurs





- Slides: 75
Acute respiratory failure
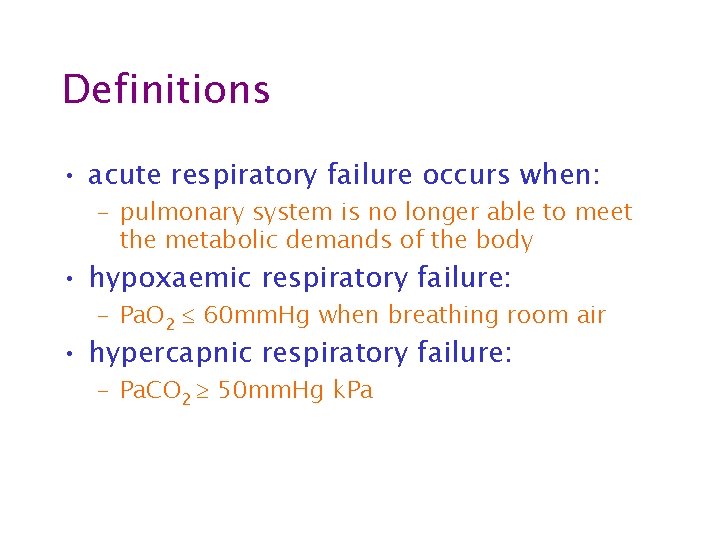
Definitions • acute respiratory failure occurs when: – pulmonary system is no longer able to meet the metabolic demands of the body • hypoxaemic respiratory failure: – Pa. O 2 60 mm. Hg when breathing room air • hypercapnic respiratory failure: – Pa. CO 2 50 mm. Hg k. Pa
Basic respiratory physiology
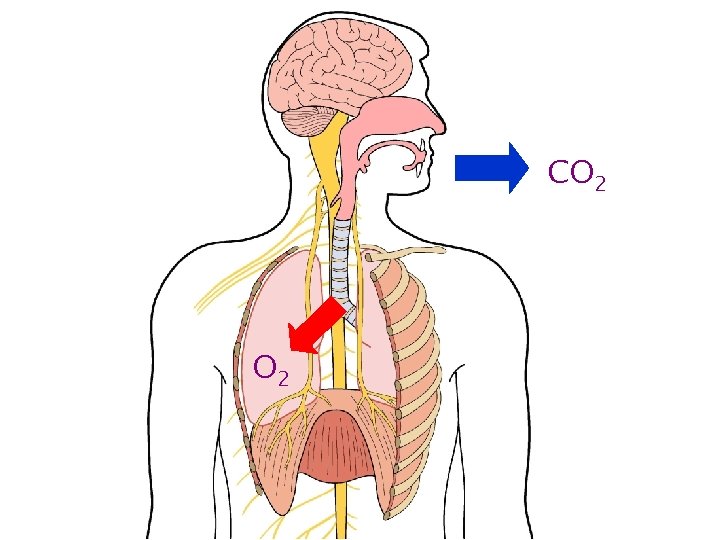
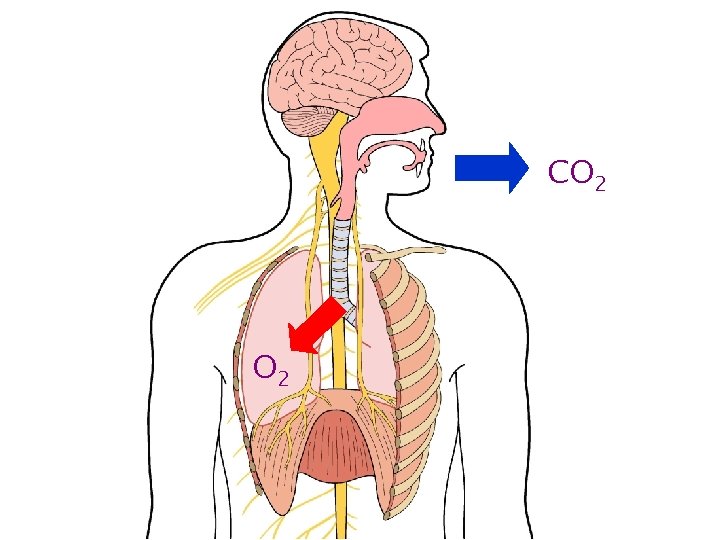
CO 2
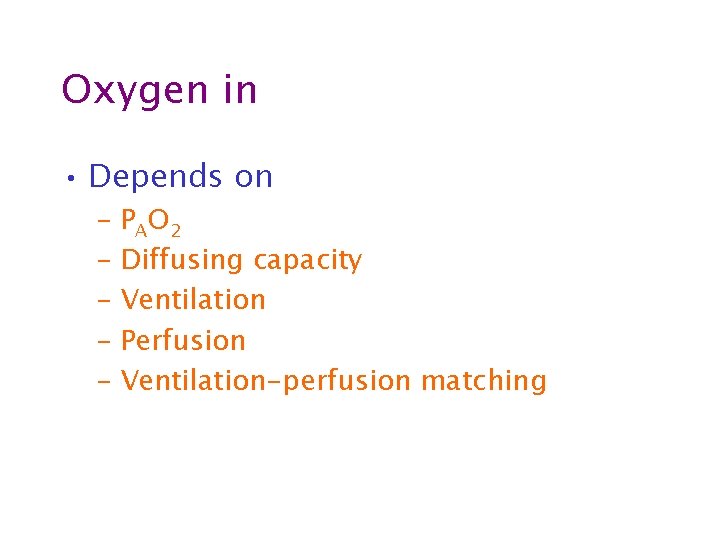
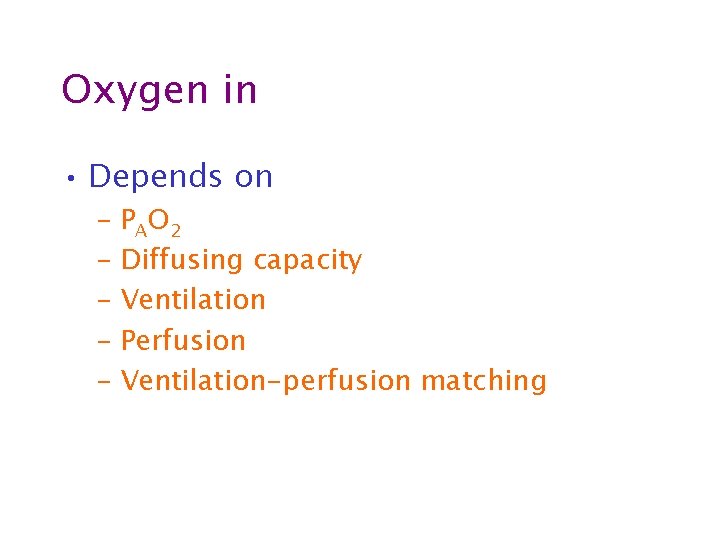
Oxygen in • Depends on – PAO 2 – Diffusing capacity – Ventilation – Perfusion – Ventilation-perfusion matching
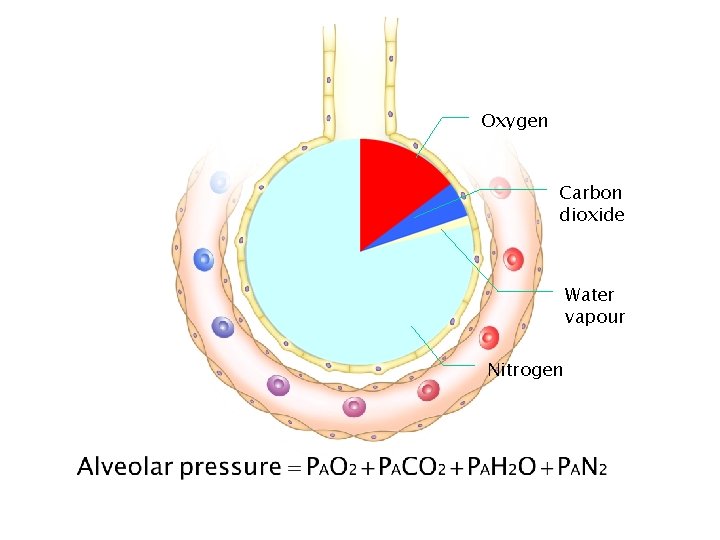
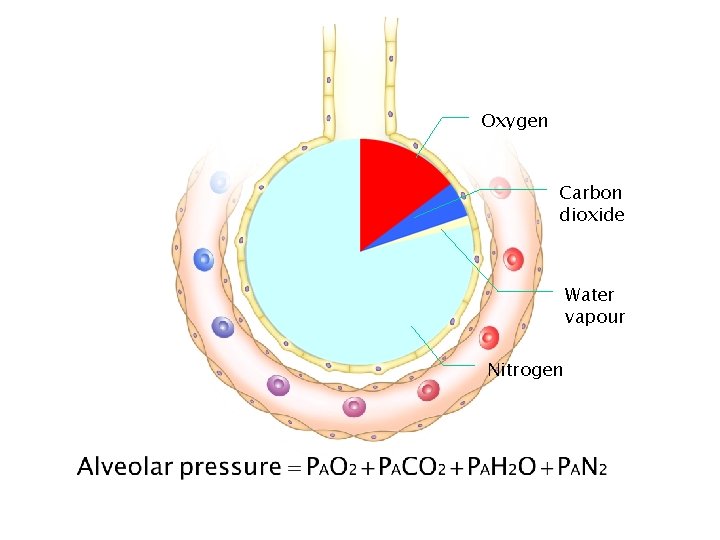
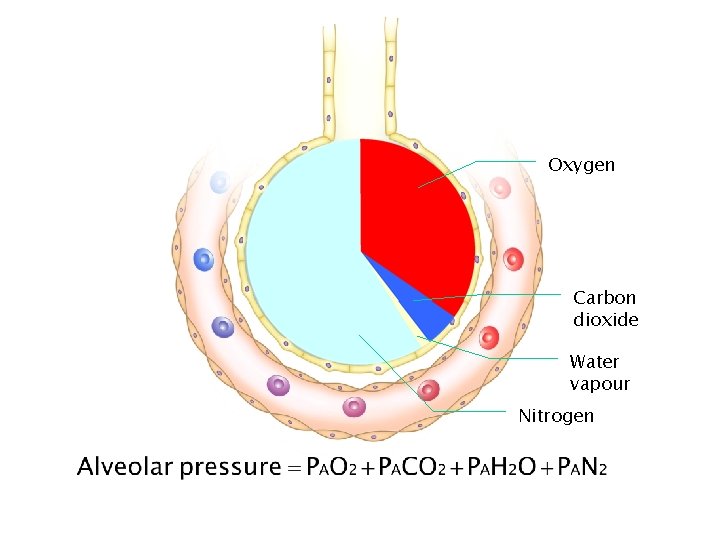
Oxygen Carbon dioxide Water vapour Nitrogen
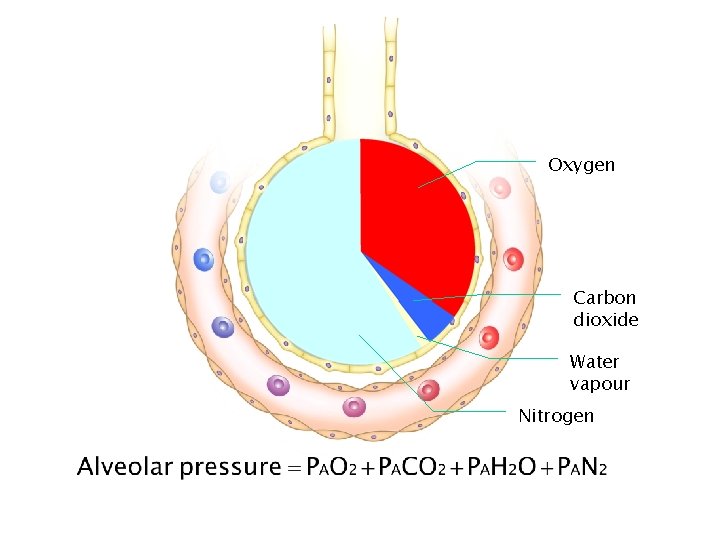
Oxygen Carbon dioxide Water vapour Nitrogen

Oxygen Carbon dioxide Water vapour Nitrogen
Oxygen in • Depends on – PAO 2 • F IO 2 • Alveolar pressure • PACO 2 • Ventilation – Ventilation-perfusion matching – Perfusion – Diffusing capacity
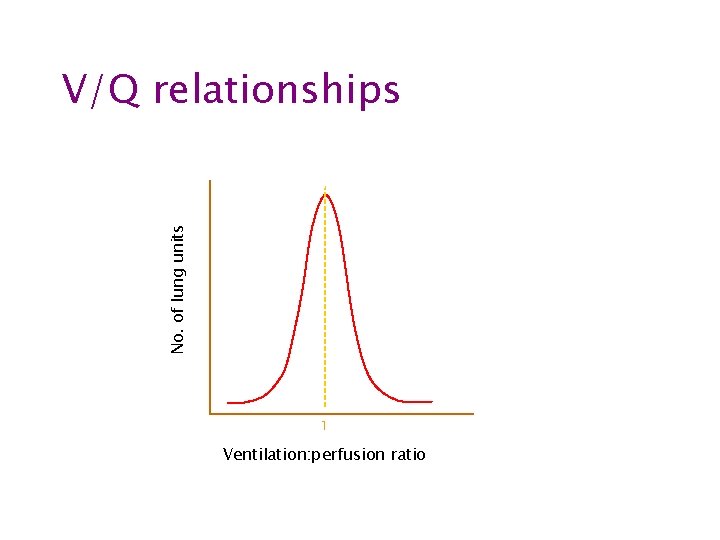
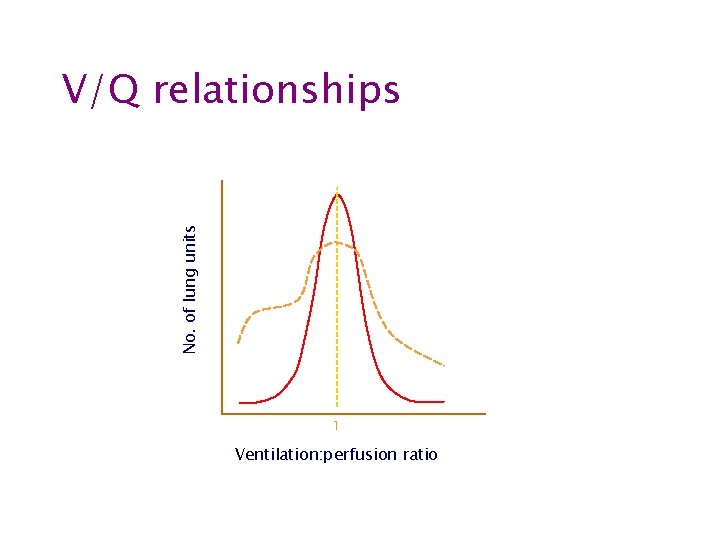
Ventilation-perfusion matching
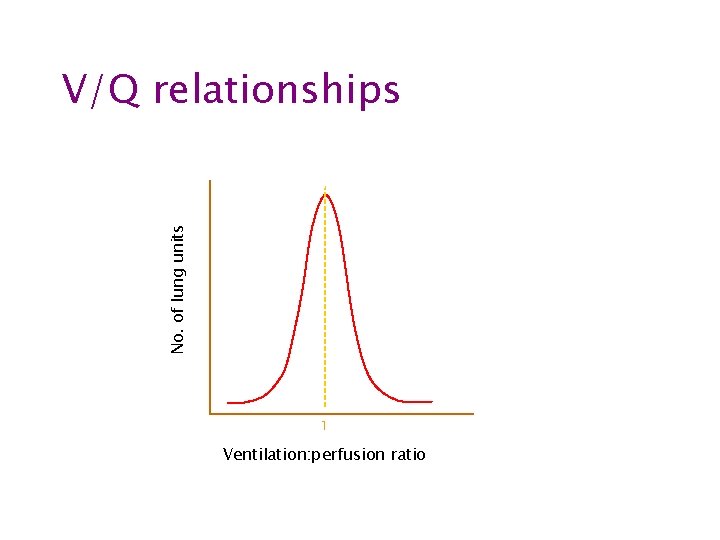
No. of lung units V/Q relationships 1 Ventilation: perfusion ratio
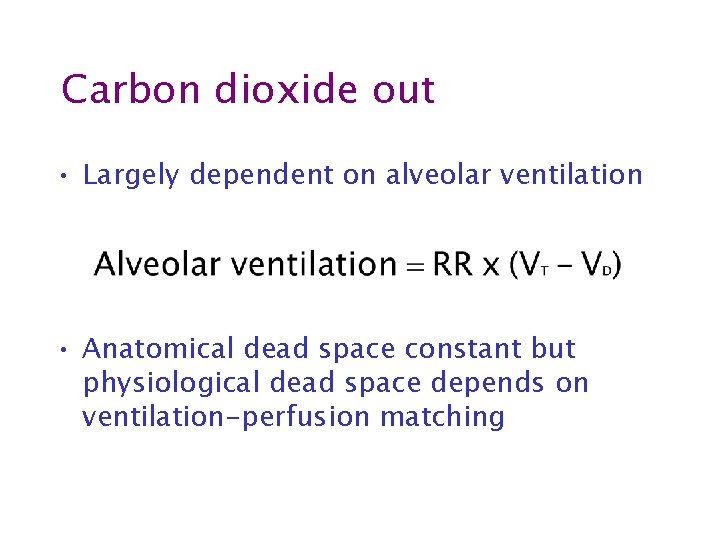
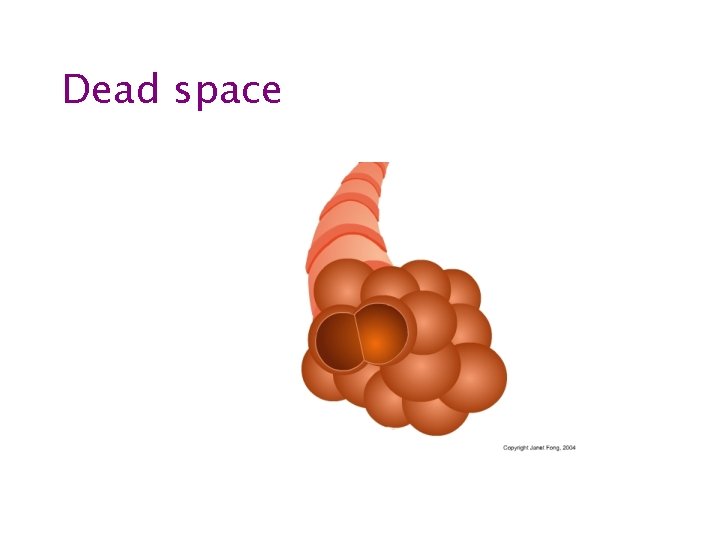
Carbon dioxide out • Largely dependent on alveolar ventilation • Anatomical dead space constant but physiological dead space depends on ventilation-perfusion matching
Carbon dioxide out • Respiratory rate • Tidal volume • Ventilation-perfusion matching
Pathophysiology
Pathophysiology • Low inspired Po 2 • Hypoventilation • Ventilation-perfusion mismatch – Shunting – Dead space ventilation • Diffusion abnormality
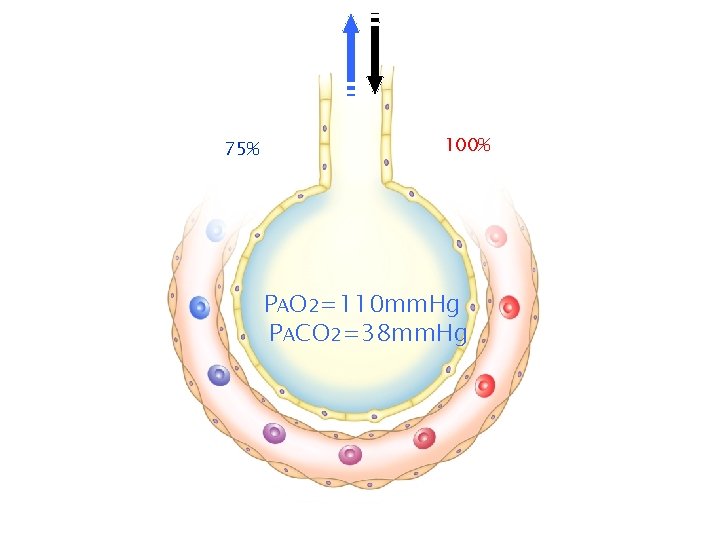
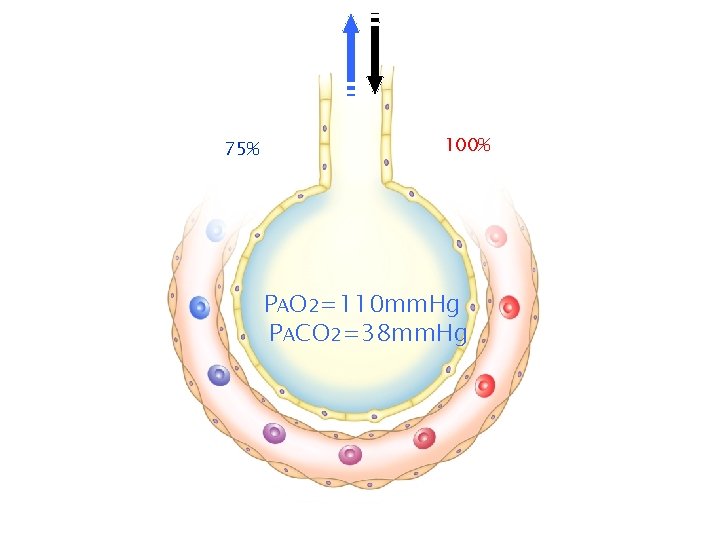
75% 100% PAO 2=110 mm. Hg PACO 2=38 mm. Hg
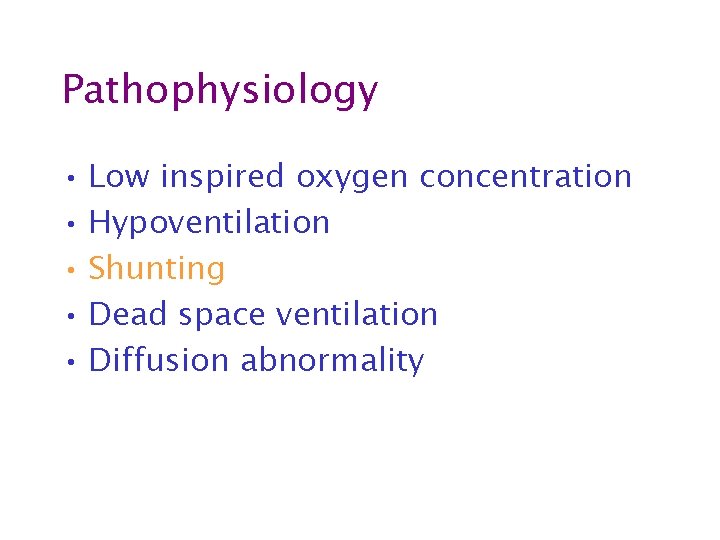
Pathophysiology • Low inspired oxygen concentration • Hypoventilation • Shunting • Dead space ventilation • Diffusion abnormality
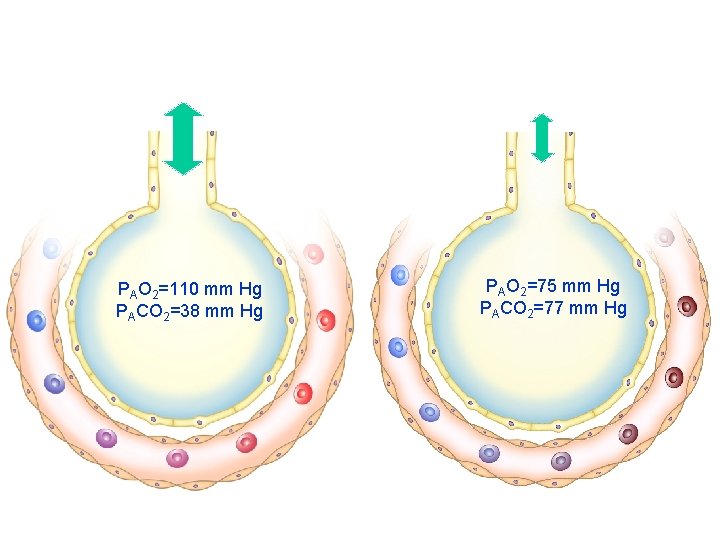
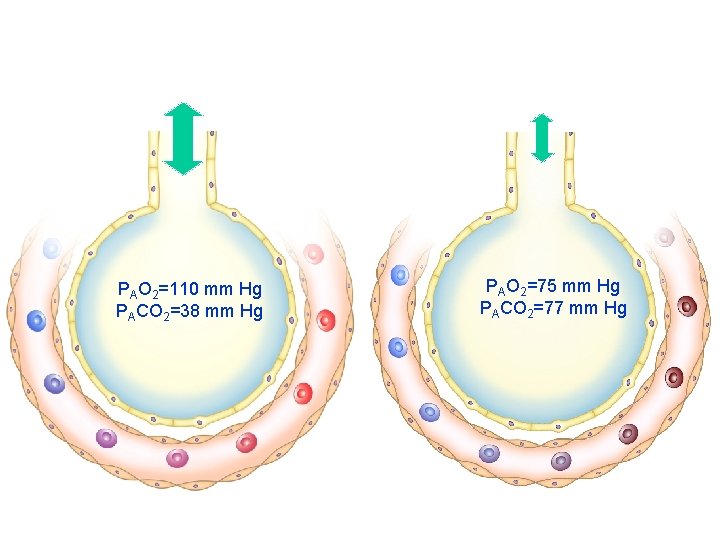
PAO 2=110 mm Hg PACO 2=38 mm Hg PAO 2=75 mm Hg PACO 2=77 mm Hg
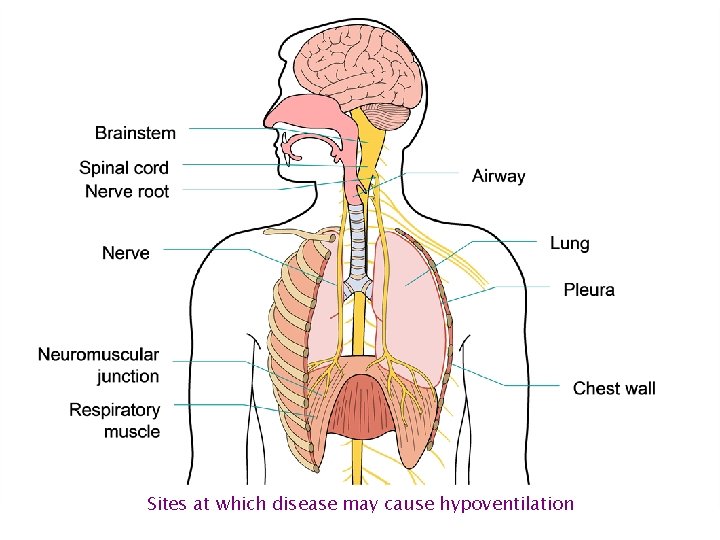
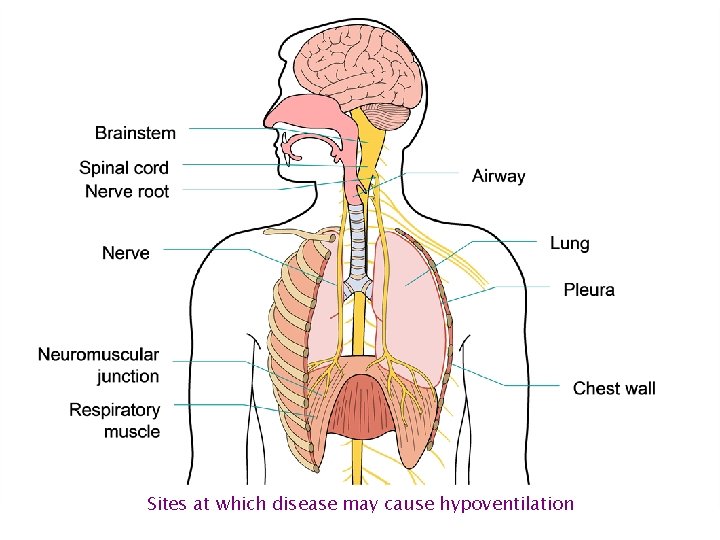
Sites at which disease may cause hypoventilation
Pathophysiology • Low inspired oxygen concentration • Hypoventilation • Shunting • Dead space ventilation • Diffusion abnormality
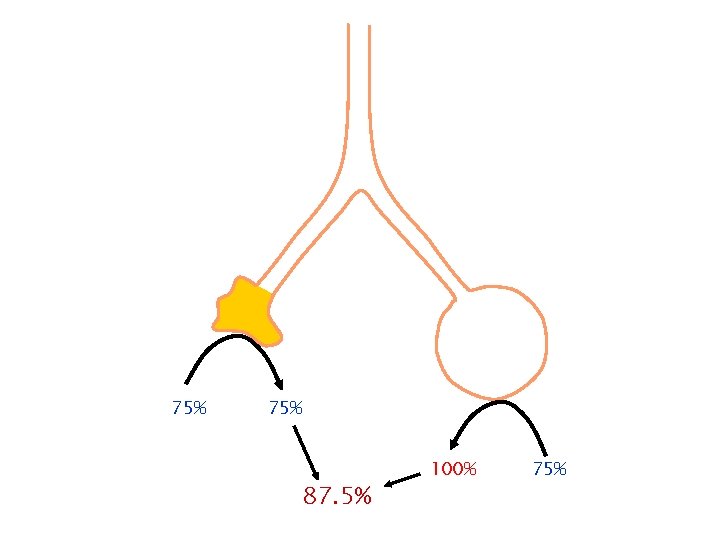
Shunt
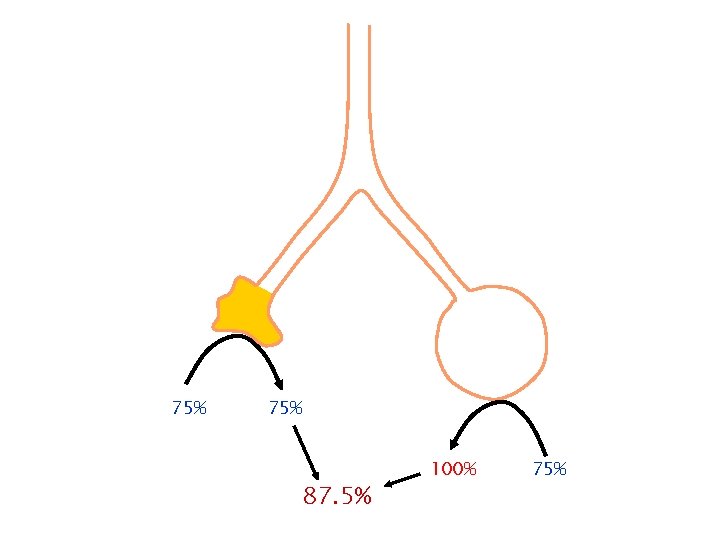
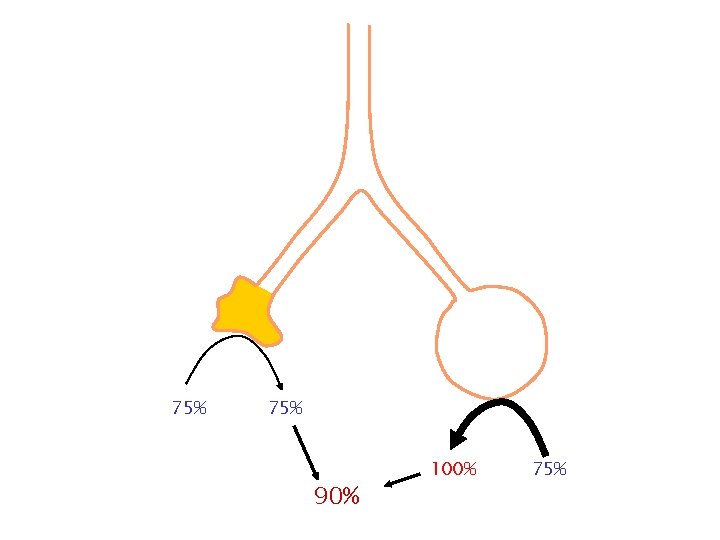
75% 87. 5% 100% 75%
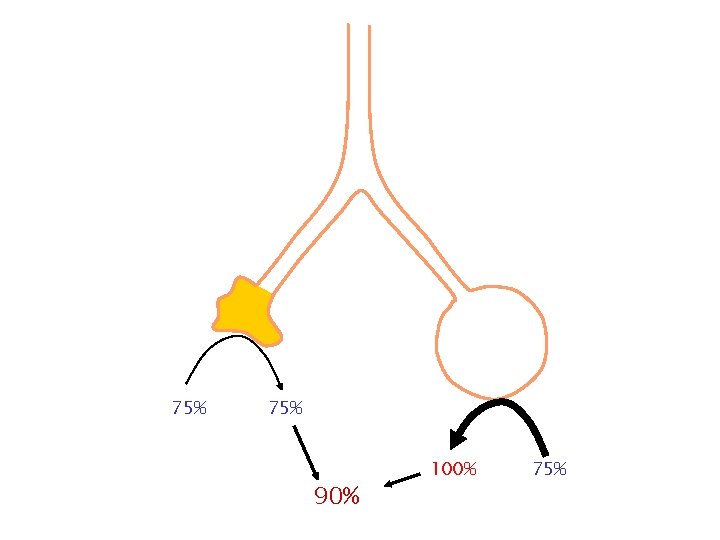
75% 90% 100% 75%
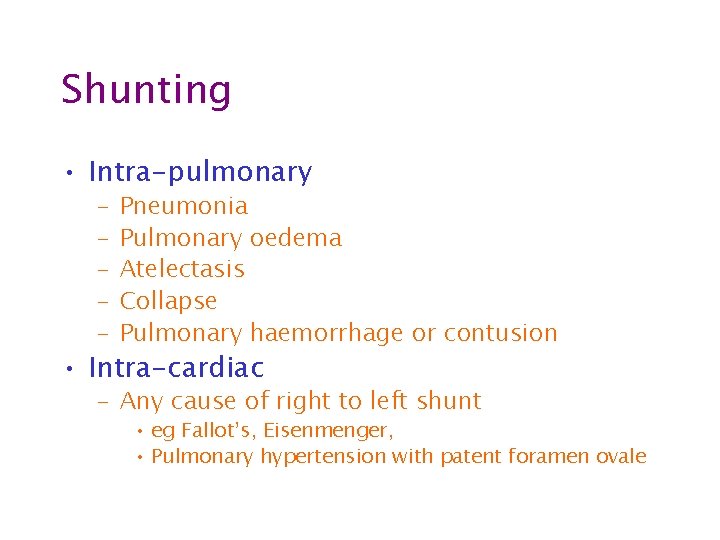
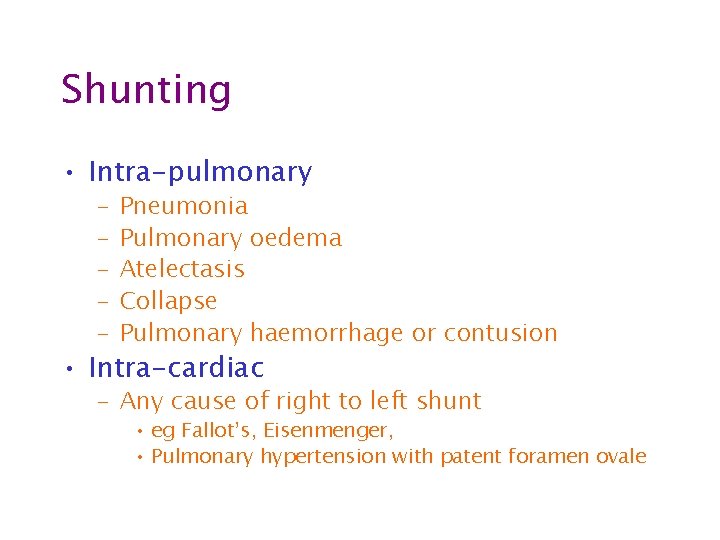
Shunting • Intra-pulmonary – – – Pneumonia Pulmonary oedema Atelectasis Collapse Pulmonary haemorrhage or contusion • Intra-cardiac – Any cause of right to left shunt • eg Fallot’s, Eisenmenger, • Pulmonary hypertension with patent foramen ovale
Pathophysiology • Low inspired oxygen concentration • Hypoventilation • Shunting • Dead space ventilation • Diffusion abnormality
Dead space
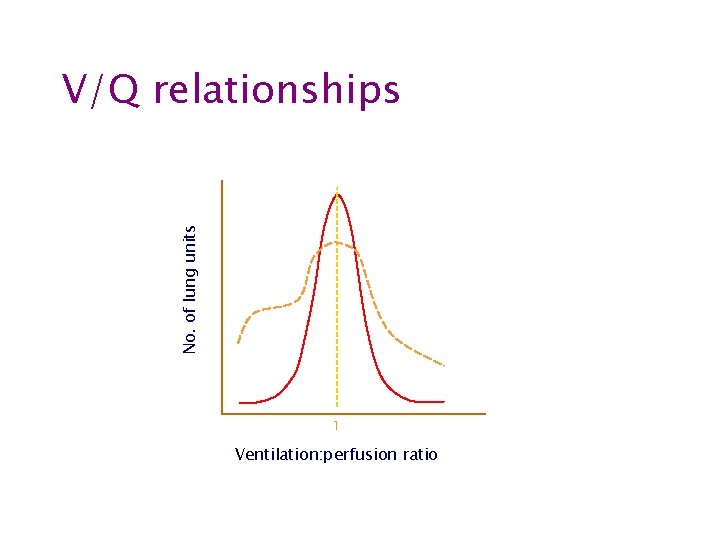
No. of lung units V/Q relationships Diseased Normal 1 Ventilation: perfusion ratio
Pathophysiology • Low inspired oxygen concentration • Hypoventilation • Shunting • Dead space ventilation • Diffusion abnormality
Respiratory monitoring
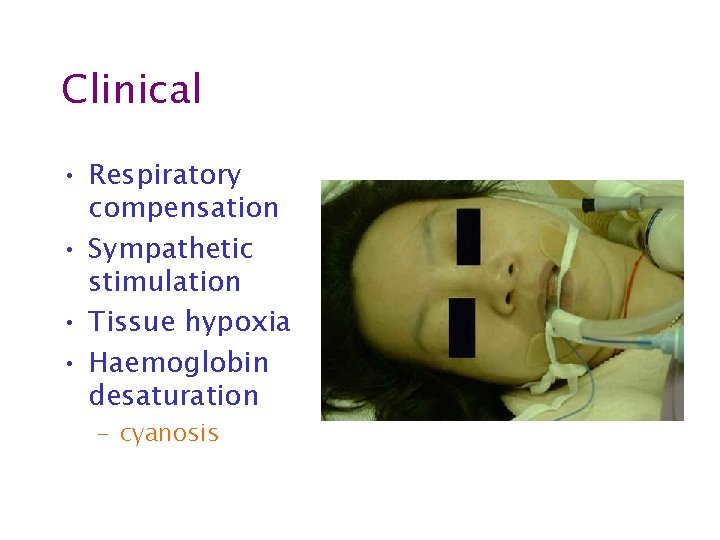
Clinical • Respiratory compensation • Sympathetic stimulation • Tissue hypoxia • Haemoglobin desaturation
Clinical • Respiratory compensation – Tachypnoea – Accessory muscles – Recesssion – Nasal flaring • Sympathetic stimulation • Tissue hypoxia • Haemoglobin desaturation
Clinical • Respiratory compensation • Sympathetic stimulation – HR – BP (early) – sweating • Tissue hypoxia • Haemoglobin desaturation
Clinical • Respiratory compensation • Sympathetic stimulation • Tissue hypoxia – Altered mental state – HR and BP (late) • Haemoglobin desaturation
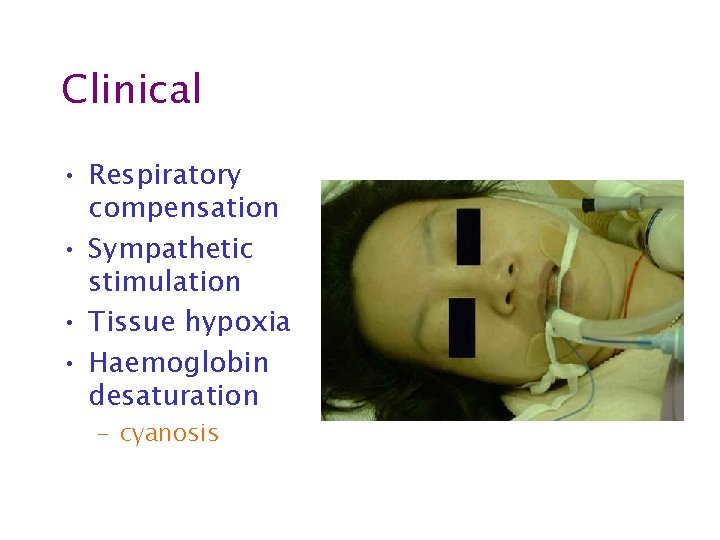
Clinical • Respiratory compensation • Sympathetic stimulation • Tissue hypoxia • Haemoglobin desaturation – cyanosis
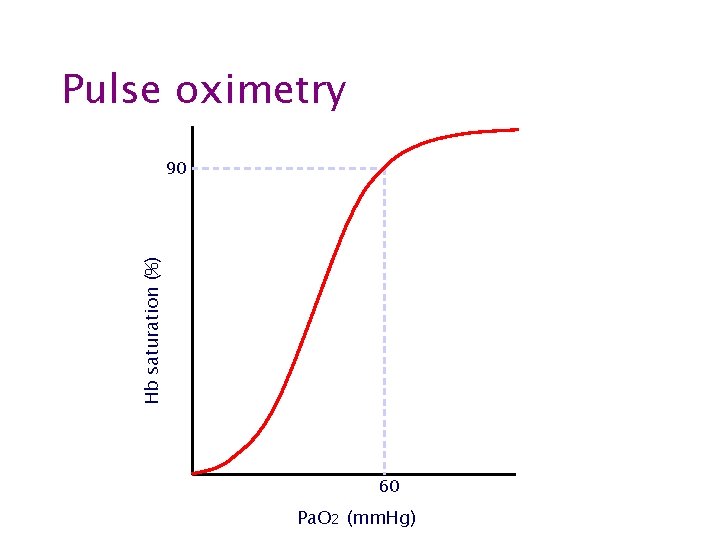
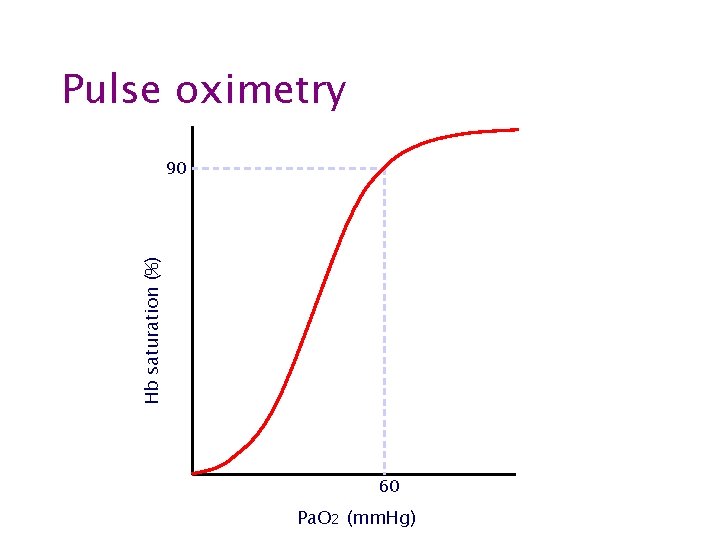
Pulse oximetry Hb saturation (%) 90 60 Pa. O 2 (mm. Hg)
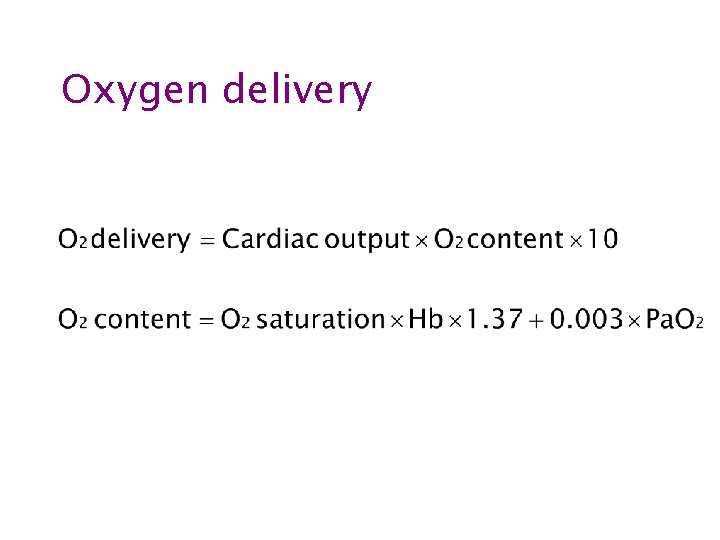
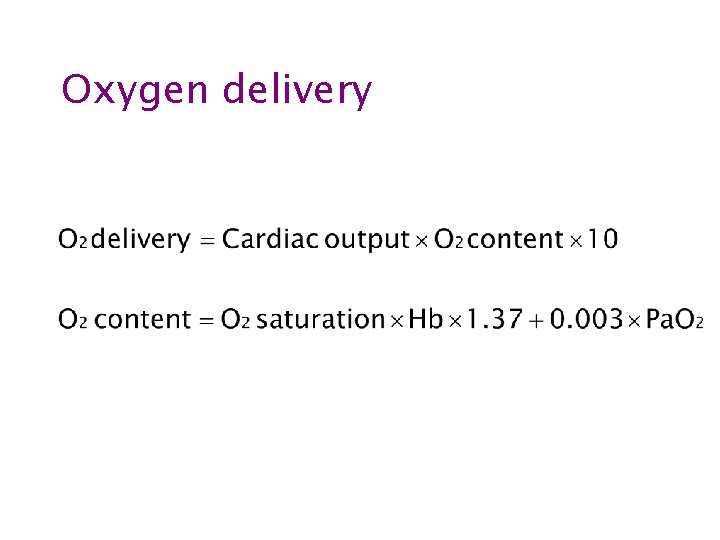
Oxygen delivery
Sources of error • • Poor peripheral perfusion Poorly adherent/positioned probe False nails or nail varnish Lipaemia Bright ambient light Excessive motion Carboxyhaemoglobin or methaemoglobin

123 80 40 87% HR=95
Summary • worry if • RR > 30/min (or < 8/min) • unable to speak 1/2 sentence without pausing • agitated, confused or comatose • cyanosed or Sp. O 2 < 90% • deteriorating despite therapy • remember • normal Sp. O 2 does not mean severe ventilatory problems are not present

Treatment
Treatment • Treat the cause • Supportive treatment – Oxygen therapy – CPAP – Mechanical ventilation
Oxygen therapy • Progressive hypercarbia due to loss of hypoxic drive is RARE • Hypoxia KILLS • The appropriate response to progressive hypercarbia is assisted ventilation NOT removal of oxygen
Oxygen therapy • Fixed performance devices • Variable performance devices
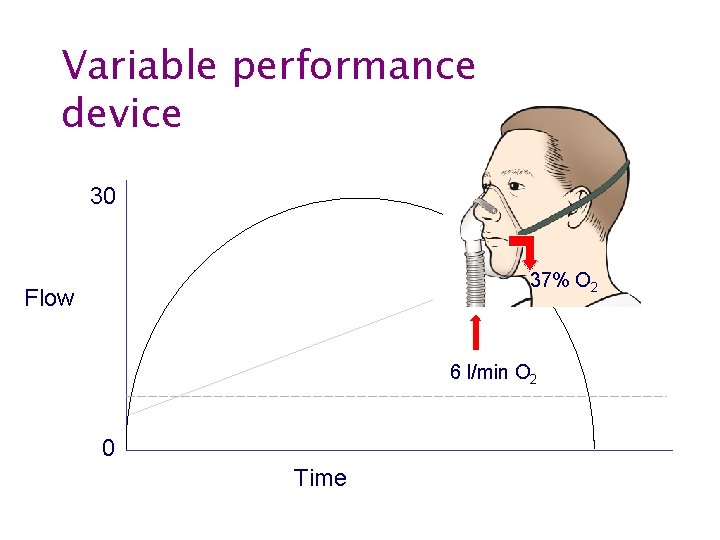
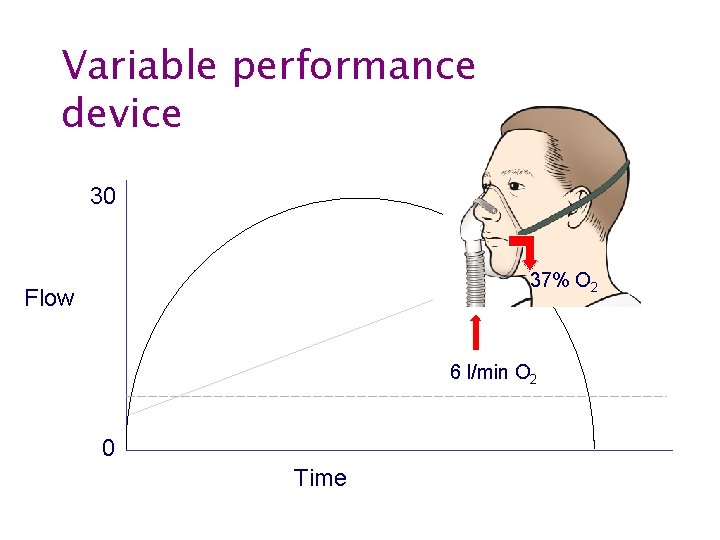
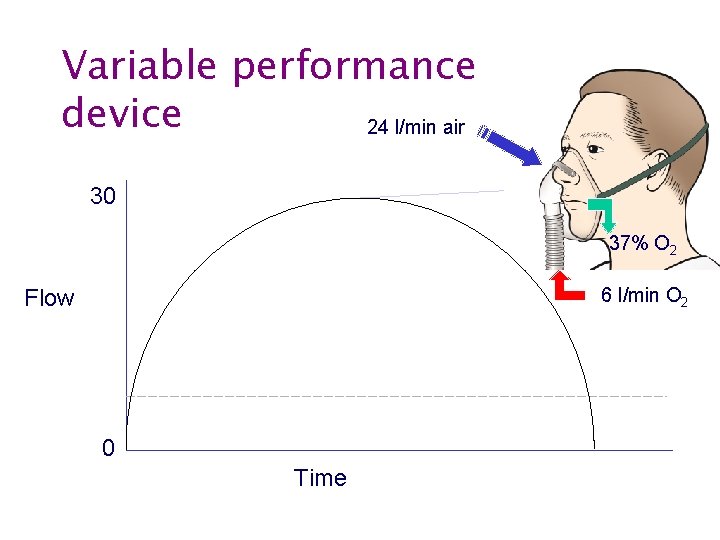
Variable performance device 30 37% O 2 Flow 6 l/min O 2 6 0 Time
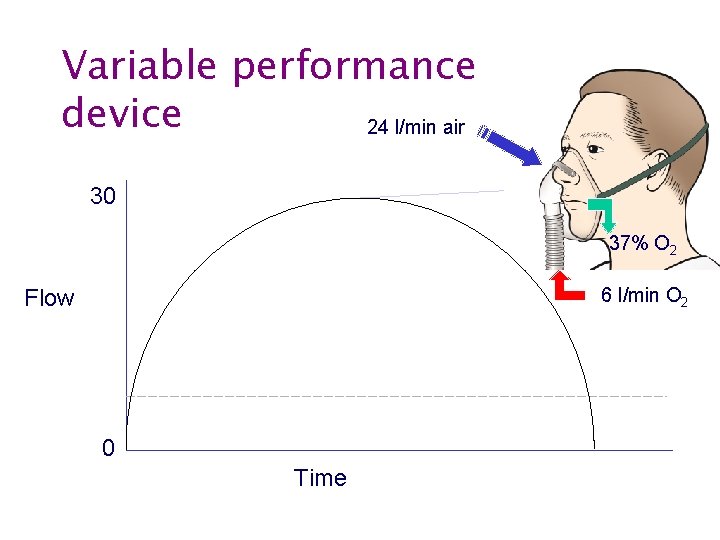
Variable performance device 24 l/min air 30 37% O 2 6 l/min O 2 Flow 6 0 Time
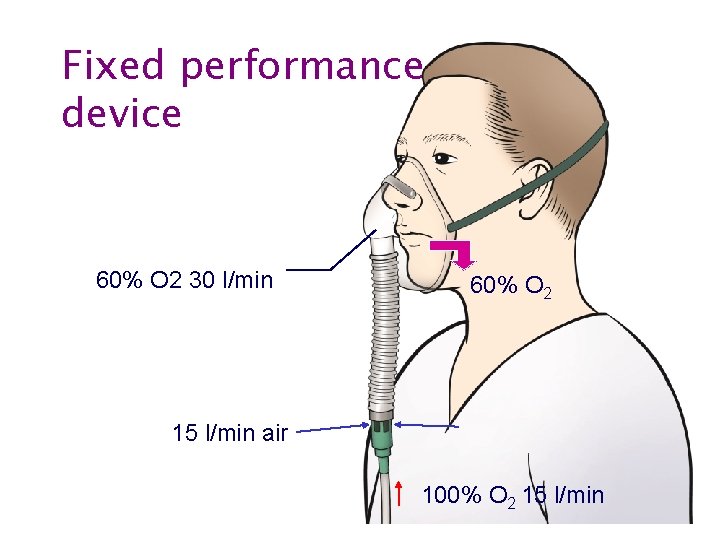
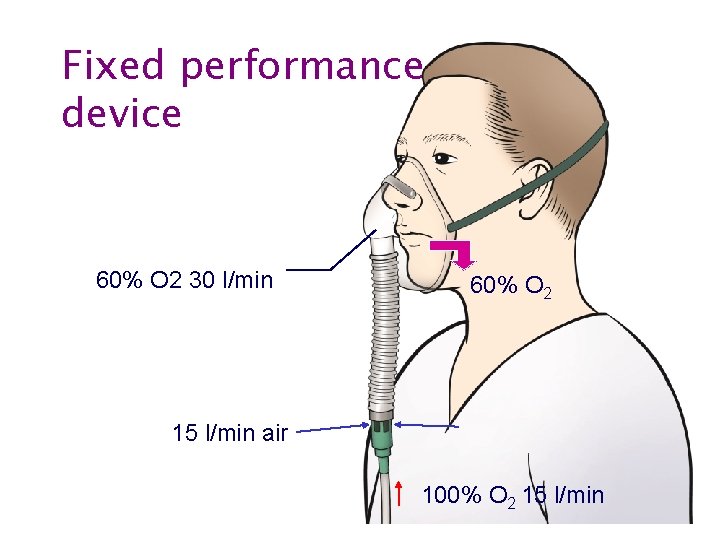
Fixed performance device 60% O 2 30 l/min 60% O 2 15 l/min air 100% O 2 15 l/min
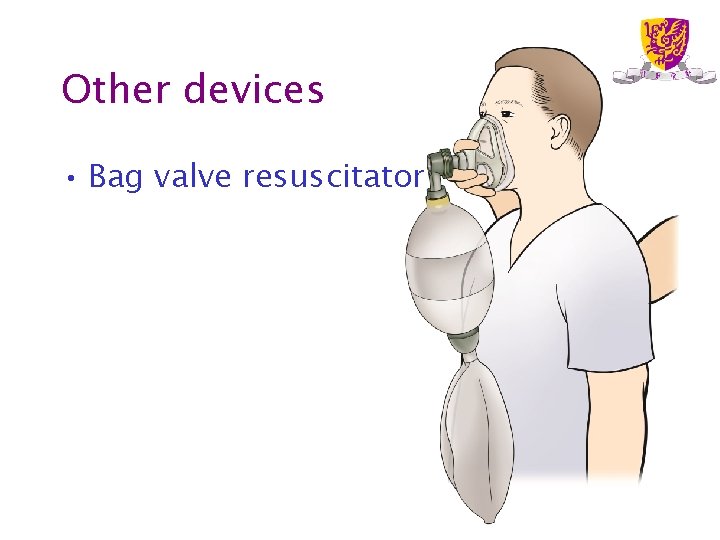
Other devices • Bag valve resuscitator
Other devices • Reservoir face mask
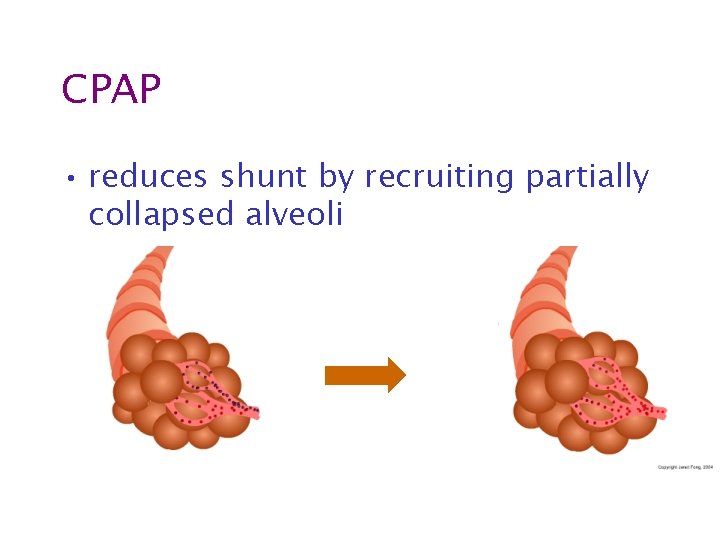
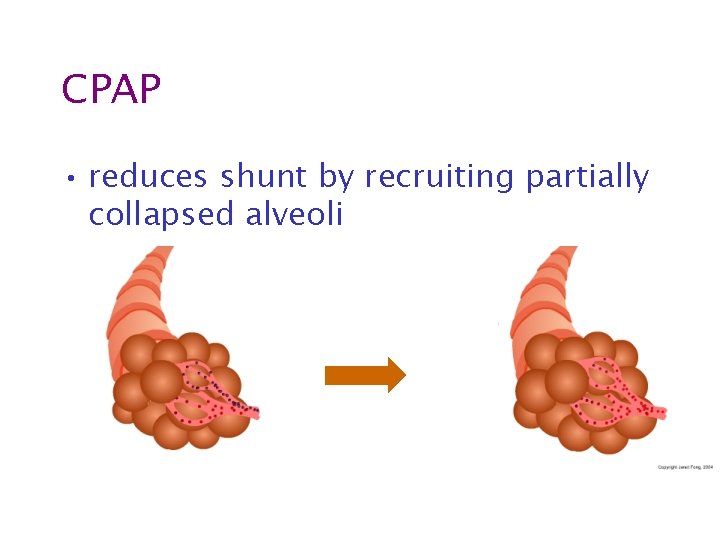
CPAP • reduces shunt by recruiting partially collapsed alveoli
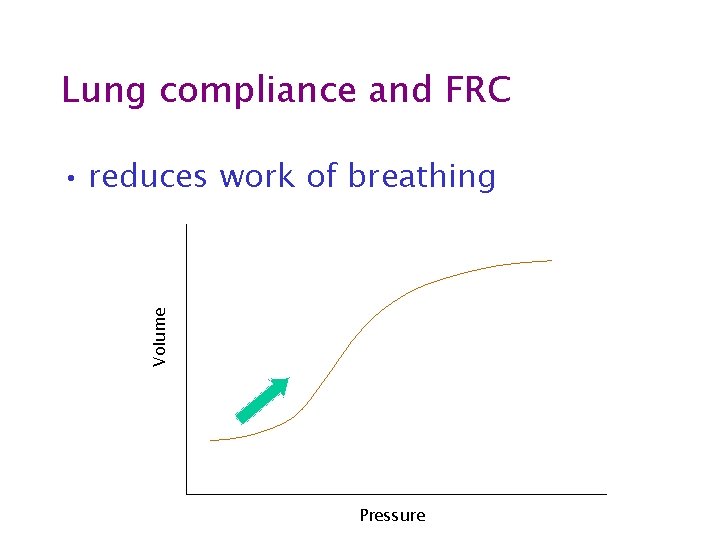
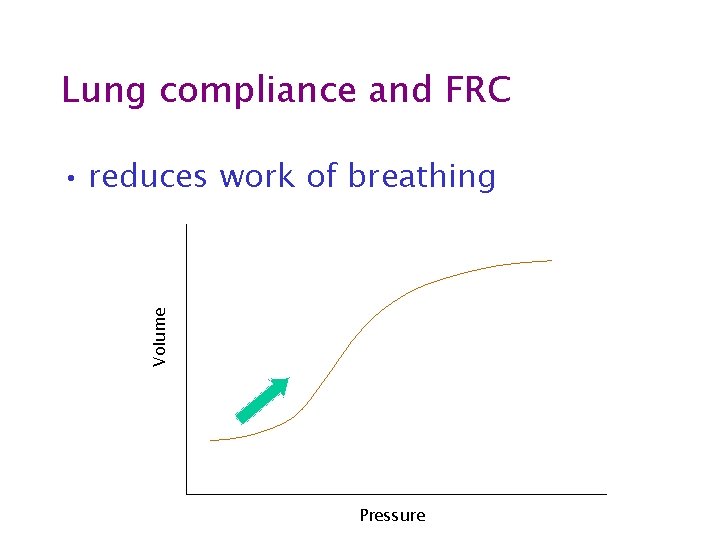
Lung compliance and FRC Volume • reduces work of breathing Pressure
Mechanical ventilation • Decision to ventilate – Complex – Multifactorial – No simple rules
Ventilate? • Severity of respiratory failure

Ventilate? • Severity of respiratory failure • Cardiopulmonary reserve
Ventilate? • Severity of respiratory failure • Cardiopulmonary reserve • Adequacy of compensation – Ventilatory requirement
Ventilate? • Severity of respiratory failure • Cardiopulmonary reserve • Adequacy of compensation – Ventilatory requirement • Expected speed of response – Underlying disease – Treatment already given
Ventilate? • Severity of respiratory failure • Cardiopulmonary reserve • Adequacy of compensation – Ventilatory requirement • Expected speed of response – Underlying disease – Treatment already given • Risks of mechanical ventilation
Ventilate? • Severity of respiratory failure • Cardiopulmonary reserve • Adequacy of compensation – Ventilatory requirement • Expected speed of response – Underlying disease – Treatment already given • Risks of mechanical ventilation • Non-respiratory indication for intubation

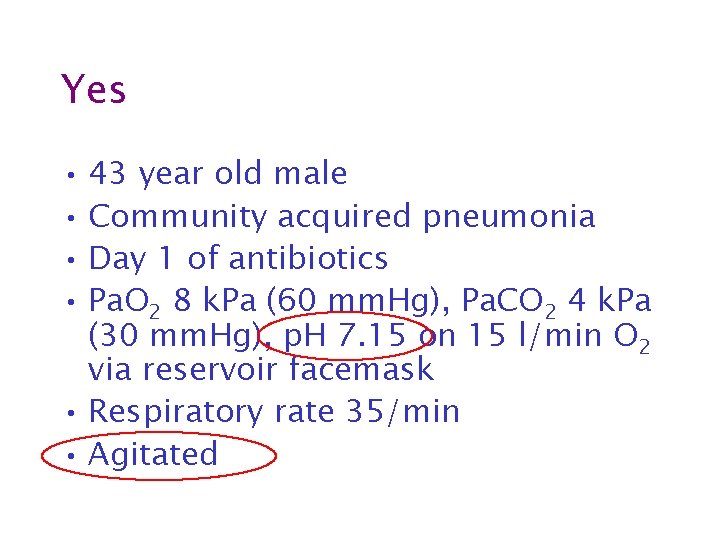
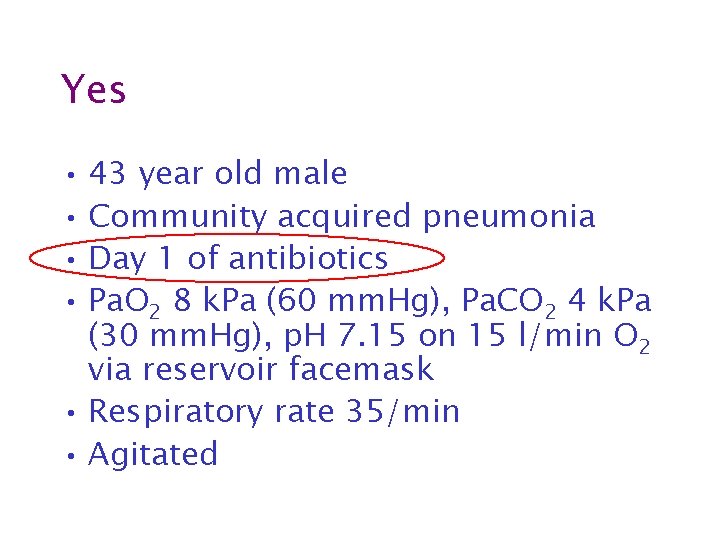
Ventilate? • 43 year old male • Community acquired pneumonia • Day 1 of antibiotics • Pa. O 2 60 mm. Hg, Pa. CO 2 30 mm. Hg, p. H 7. 15 on 15 l/min O 2 via reservoir facemask • Respiratory rate 35/min • Agitated
Yes • 43 year old male • Community acquired pneumonia • Day 1 of antibiotics • Pa. O 2 60 mm. Hg, Pa. CO 2 30 mm. Hg, p. H 7. 15 on 15 l/min O 2 via reservoir facemask • Respiratory rate 35/min • Agitated
Yes • 43 year old male • Community acquired pneumonia • Day 1 of antibiotics • Pa. O 2 60 mm. Hg, Pa. CO 2 30 mm. Hg, p. H 7. 15 on 15 l/min O 2 via reservoir facemask • Respiratory rate 35/min • Agitated
Yes • 43 year old male • Community acquired pneumonia • Day 1 of antibiotics • Pa. O 2 60 mm. Hg), Pa. CO 2 30 mm. Hg, p. H 7. 15 on 15 l/min O 2 via reservoir facemask • Respiratory rate 35/min • Agitated
Yes • 43 year old male • Community acquired pneumonia • Day 1 of antibiotics • Pa. O 2 8 k. Pa (60 mm. Hg), Pa. CO 2 4 k. Pa (30 mm. Hg), p. H 7. 15 on 15 l/min O 2 via reservoir facemask • Respiratory rate 35/min • Agitated
Yes • 43 year old male • Community acquired pneumonia • Day 1 of antibiotics • Pa. O 2 8 k. Pa (60 mm. Hg), Pa. CO 2 4 k. Pa (30 mm. Hg), p. H 7. 15 on 15 l/min O 2 via reservoir facemask • Respiratory rate 35/min • Agitated
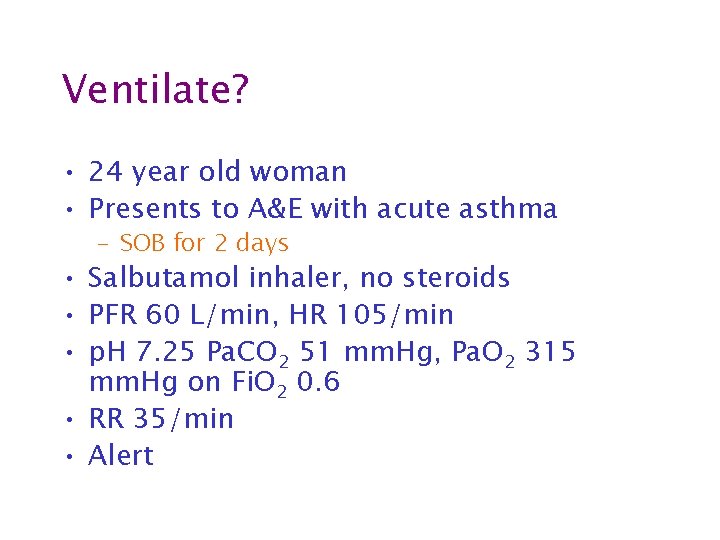
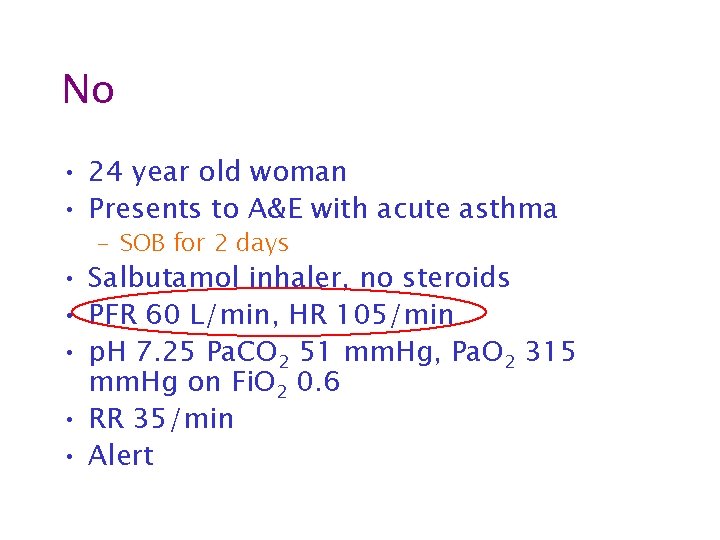
Ventilate? • 24 year old woman • Presents to A&E with acute asthma – SOB for 2 days • Salbutamol inhaler, no steroids • PFR 60 L/min, HR 105/min • p. H 7. 25 Pa. CO 2 51 mm. Hg, Pa. O 2 315 mm. Hg on Fi. O 2 0. 6 • RR 35/min • Alert
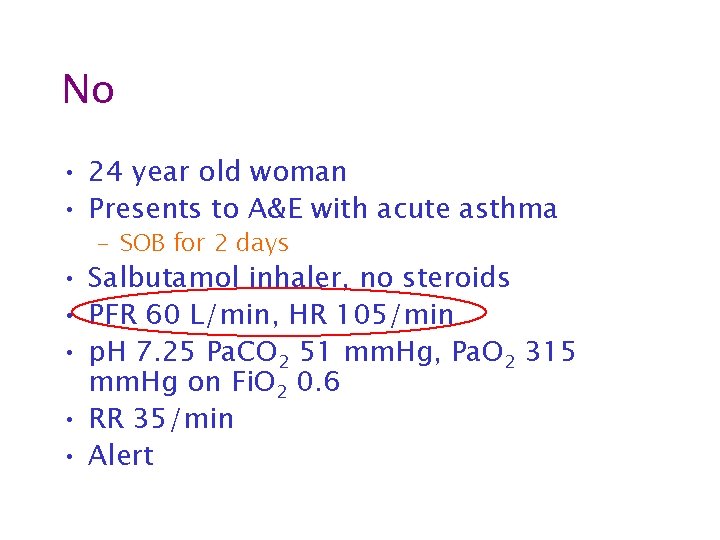
No • 24 year old woman • Presents to A&E with acute asthma – SOB for 2 days • Salbutamol inhaler, no steroids • PFR 60 L/min, HR 105/min • p. H 7. 25 Pa. CO 2 51 mm. Hg, Pa. O 2 315 mm. Hg on Fi. O 2 0. 6 • RR 35/min • Alert
No • 24 year old woman • Presents to A&E with acute asthma – SOB for 2 days • Salbutamol inhaler, no steroids • PFR 60 L/min, HR 105/min • p. H 7. 25, Pa. CO 2 51 mm. Hg, Pa. O 2 315 mm. Hg on Fi. O 2 0. 6 • RR 35/min • Alert
No • 24 year old woman • Presents to A&E with acute asthma – SOB for 2 days • Salbutamol inhaler, no steroids • PFR 60 L/min, HR 105/min • p. H 7. 25 Pa. CO 2 51 mm. Hg, Pa. O 2 315 mm. Hg on Fi. O 2 0. 6 • RR 35/min • Alert
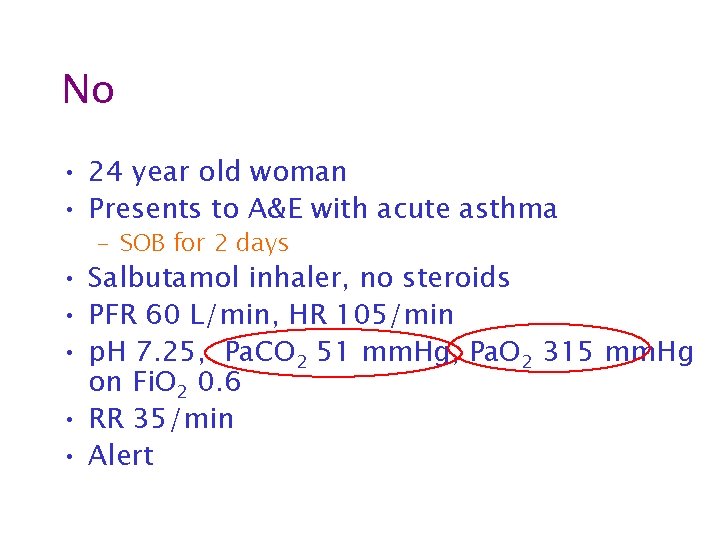
No • 24 year old woman • Presents to A&E with acute asthma – SOB for 2 days • Salbutamol inhaler, no steroids • PFR 60 L/min, HR 105/min • p. H 7. 25 Pa. CO 2 51 mm. Hg, Pa. O 2 315 mm. Hg on Fi. O 2 0. 6 • RR 35/min • Alert
No • 24 year old woman • Presents to A&E with acute asthma – SOB for 2 days • Salbutamol inhaler, no steroids • PFR 60 L/min, HR 105/min • p. H 7. 25 Pa. CO 2 6. 8 k. Pa (51 mm. Hg), Pa. O 2 42 k. Pa (315 mm. Hg) on Fi. O 2 0. 6 • RR 35/min • Alert
No • 24 year old woman • Presents to A&E with acute asthma – SOB for 2 days • Salbutamol inhaler, no steroids • PFR 60 L/min, HR 105/min • p. H 7. 25, Pa. CO 2 51 mm. Hg, Pa. O 2 315 mm. Hg on Fi. O 2 0. 6 • RR 35/min • Alert
Summary • Shunting is the most common cause of acute respiratory failure in acutely ill patients – High concentrations of oxygen are required • Hypoventilation due to abolition of hypoxic drive is RARE
Summary • worry if • RR > 30/min (or < 8/min) • unable to speak 1/2 sentence without pausing • agitated, confused or comatose • cyanosed or Sp. O 2 < 90% • deteriorating despite therapy • remember • normal Sp. O 2 does not mean severe ventilatory problems are not present
Treatment • Treat the cause • Supportive treatment – Oxygen therapy – CPAP – Mechanical ventilation
Ventilation • Severity of respiratory failure • Cardiopulmonary reserve • Adequacy of compensation – Ventilatory requirement • Expected speed of response – Underlying disease – Treatment already given • Risks of mechanical ventilation • Non-respiratory indication for intubation
 Treatments for acute renal failure
Treatments for acute renal failure Acute vs chronic heart failure
Acute vs chronic heart failure Fhf
Fhf Acute brain failure
Acute brain failure Acute liver failure criteria
Acute liver failure criteria Acute liver failure
Acute liver failure Failure to pace vs failure to capture
Failure to pace vs failure to capture Site:slidetodoc.com
Site:slidetodoc.com Ventricular escape rhythm
Ventricular escape rhythm Broncheols
Broncheols Nursing management of dyspnea ppt
Nursing management of dyspnea ppt Types of respiratory failure
Types of respiratory failure Blue bloaters vs pink puffers
Blue bloaters vs pink puffers Wide a a gradient
Wide a a gradient Priyanka breathing
Priyanka breathing Types of respiratory failure
Types of respiratory failure Conductive zone vs respiratory zone
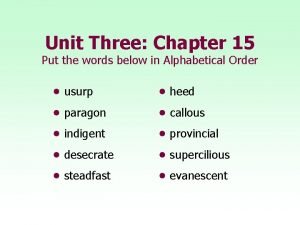
Conductive zone vs respiratory zone Use the words below
Use the words below Six essential elements of geography definitions
Six essential elements of geography definitions Meaning of financial management
Meaning of financial management Cash budgeting leaving cert
Cash budgeting leaving cert Interpret cartoon
Interpret cartoon Basic chemistry definitions
Basic chemistry definitions Extasy definitions
Extasy definitions What is architecture business cycle?
What is architecture business cycle? What is the definition of compare and contrast
What is the definition of compare and contrast Brighton collaboration level 1
Brighton collaboration level 1 Compound welds
Compound welds Material properties definitions
Material properties definitions Parts of a circle and their definitions
Parts of a circle and their definitions Whatshere
Whatshere Situational poverty definition
Situational poverty definition Parallel lines and transversals definitions
Parallel lines and transversals definitions Science whmis symbols
Science whmis symbols Film genres and definitions
Film genres and definitions Marketing management objectives
Marketing management objectives Elements of a story definition
Elements of a story definition The problem of concept drift: definitions and related work
The problem of concept drift: definitions and related work Gantt chart symbols
Gantt chart symbols Put a or an to the words below
Put a or an to the words below Atmosphere definition
Atmosphere definition Cyberdefinitions
Cyberdefinitions Treatment plan goals and objectives for adhd
Treatment plan goals and objectives for adhd Scope of psychology
Scope of psychology What are the parts of a play
What are the parts of a play Nursing definition by florence nightingale
Nursing definition by florence nightingale Eapg code list
Eapg code list Standard definitions for techniques of supply chain finance
Standard definitions for techniques of supply chain finance Examples of reciprocal determinism
Examples of reciprocal determinism 2-2 statements conditionals and biconditionals
2-2 statements conditionals and biconditionals Plot elements definition
Plot elements definition Conceptualization operationalization and measurement
Conceptualization operationalization and measurement Historical and contemporary nursing practice
Historical and contemporary nursing practice 2-4 biconditional statements and definitions
2-4 biconditional statements and definitions What are the 7 love languages
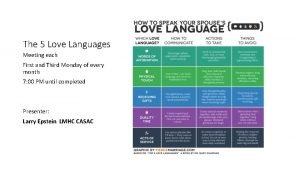
What are the 7 love languages Elements of plot definitions
Elements of plot definitions Formal definition examples
Formal definition examples Definition of public speaking
Definition of public speaking A multiwire circuit must consist of conductors connected to
A multiwire circuit must consist of conductors connected to With definitions
With definitions Reference angle example
Reference angle example Kairos rhetorical device
Kairos rhetorical device Heat? - definition
Heat? - definition Software architecture definition
Software architecture definition Goal for technical writing
Goal for technical writing Comparative of simply
Comparative of simply Dynamic discounting definition
Dynamic discounting definition Level g unit 1 antonyms
Level g unit 1 antonyms Poem meaning
Poem meaning Gothic literature meaning
Gothic literature meaning Definition of reading strategies
Definition of reading strategies Defining cybercrime
Defining cybercrime Artifacts nonverbal communication definition
Artifacts nonverbal communication definition Literary devices techniques
Literary devices techniques Miscible liquids
Miscible liquids Match the following terms with their definitions communism
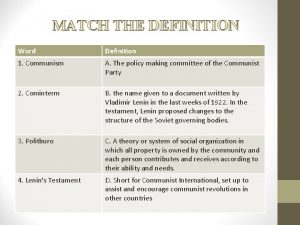
Match the following terms with their definitions communism