Pediatric Failure to Thrive Michael Michener MD Major
- Slides: 29
Pediatric Failure to Thrive Michael Michener, MD Major, USAF 14 March 2007
Overview n n n n Definitions Case presentation Introduction Diagnosis Treatment Outcomes Top 6 things to remember about FTT
Definition n Failure to Thrive (FTT): • Weight below the 5 th percentile for age and sex • Weight for age curve falls across two major percentile lines n Other definitions exist, but are not superior in predicting problems or long term outcomes
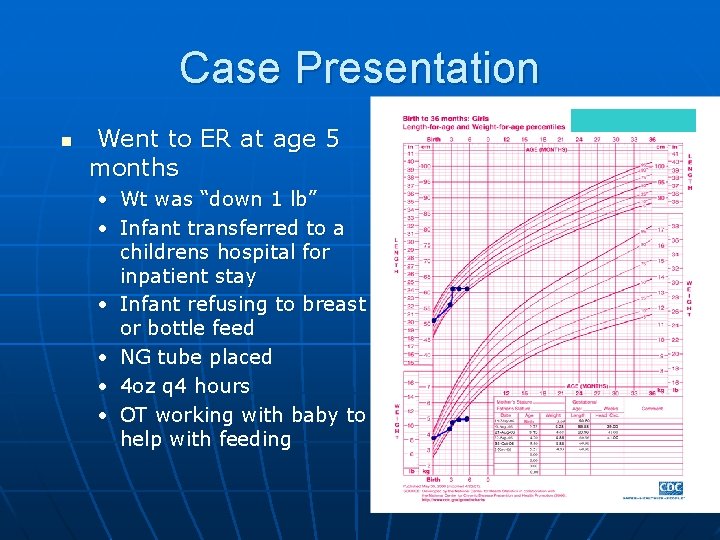
Case Presentation n 4 mo F, well child visit (Sept 06) • Mom complained about poor wt gain • Same problem with first child • Husband deployed • Parents small stature • Other development was normal • Mom alleged that feeding was going well (breastfeeding) • Wt = 10 lb 8 oz
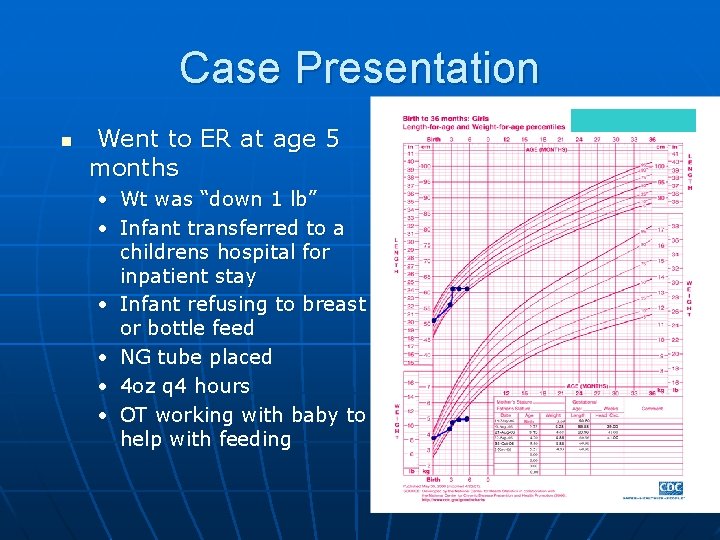
Case Presentation n Went to ER at age 5 months • Wt was “down 1 lb” • Infant transferred to a childrens hospital for inpatient stay • Infant refusing to breast or bottle feed • NG tube placed • 4 oz q 4 hours • OT working with baby to help with feeding
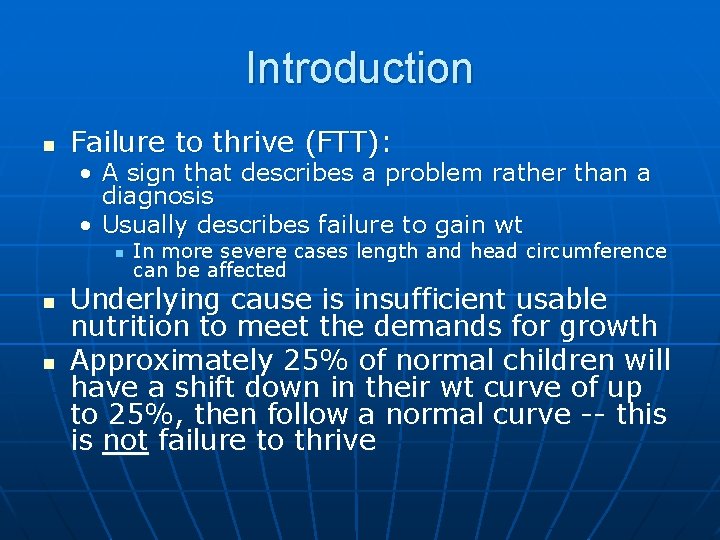
Introduction n Failure to thrive (FTT): • A sign that describes a problem rather than a diagnosis • Usually describes failure to gain wt n n n In more severe cases length and head circumference can be affected Underlying cause is insufficient usable nutrition to meet the demands for growth Approximately 25% of normal children will have a shift down in their wt curve of up to 25%, then follow a normal curve -- this is not failure to thrive
Introduction n Specific infant populations • Premature/IUGR – wt may be less than 5 th percentile, but if following the growth curve and normal interval growth then FTT should not be diagnosed • Modified growth charts exist for specific populations
Introduction n Historically has been divided into organic and nonorganic causes • Most cases have mixed etiologies • This classification system is out of favor n More useful classification system is: • Inadequate caloric intake • Inadequate fat or carbohydrate absorption • Increased energy requirements
Etiology n Inadequate Caloric Intake • • Incorrect preparation of formula Poor feeding habits (ex: too much juice) Poverty Mechanical feeding difficulties (reflux, cleft palate, oromotor dysfunction) • Neglect n Physicians are strongly encouraged to consider child abuse and neglect in cases of FTT that don’t respond to appropriate interventions* *(SOR – C, expert and consensus opinion, Ref 1)
Etiology n Inadequate absorption • Celiac disease • Cystic fibrosis • Milk allergy • Vitamin deficiency • Biliary Atresia • Necrotizing enterocolitis
Etiology n Increased metabolism • • n Hyperthyroidism Chronic infection Congenital heart disease Chronic lung disease Other considerations • Genetic abnormalities, congenital infections, metabolic disorders (storage diseases, amino acid disorders)
Diagnosis n n n Accurately plotting growth charts at every visit is recommended* Assess the trends H&P more important than labs • Most cases in primary care setting are psychosocial or nonorganic in etiology *(SOR – C, expert and consensus opinion, Ref 1)
History n Dietary n n PMH n n Who lives in the home, family stressors, poverty, drugs? Family n n Illnesses, hospitalizations, reflux, vomiting, stools? Social n n Keep a food diary If formula fed, is it being prepared correctly? When, where, with whom does the child eat? Medical condition (or FTT) in siblings, mental illness, stature? Pregnancy/Birth n Substance abuse? postpartum depression?
Physical n Accurate measurement of child’s height, weight, head circumference n n Single data point has limited usefulness Evaluate for dysmorphic features Mouth, palate Neurologic exam • Signs of spasticity or hypotonia n Cardiovascular/Lung exam
Physical n Signs of neglect or abuse • Lack of age appropriate eye contact, smiling, vocalization, or interest in environment • Chronic diaper rash • Impetigo • Flat occiput • Poor hygeine • Bruises • Scars
Physical n Observe parent-child interactions • Especially during a feeding session How is food or formula prepared? n Oral motor or swallowing difficulty? n Is adequate time allowed for feeding? n Do they cuddle the infant during feeds? n Is TV or anything else causing a distraction? n
Lab Evaluation n Unless suggested by H&P, no routine lab tests recommended initially* n n If problem persists, could consider: n n One study of hospitalized pts resulted in only 1. 4% of tests being of diagnostic assistance in FTT CBC, U/A, Electrolytes, TSH, ESR, Lead, HIV, Tb If not improving with adequate diet, consider: n n n Stool for fat, reducing substances, pathogens Celiac antibody testing CF testing *(SOR – B, historical, uncontrolled study, Ref 1, 2)
Management n n n Goal is “catch-up” weight gain Most cases can be managed with nutrition intervention and/or feeding behavior modification General principles: • High Calorie Diet • Close Follow-up n n Keep a prospective feeding diary-72 hour Assure access to WIC, food programs, other community resources
Management n Energy intake should be 50% greater than the basal caloric requirement Concentrate formula, add rice cereal to pureed foods n Add taste pleasing fats to diet (cheese, peanut butter, ice cream) n High calorie milk drinks (Pediasure has 30 cal/oz vs 19 cal per oz in whole milk) n Multivitamin with iron and zinc n Limit fruit juice to 8 -12 oz per day n
Management n Parental behavior • May need reassurance to help with their own anxiety • Encourage, but don’t force, child to eat • Make meals pleasant, regular times, don’t rush • May need to schedule meals every 2 -3 hours • Make the child comfortable • Encourage some variety and cover the basic food groups • Snacks between meals
Management n Do you hospitalize? • Rarely necessary • Consider if: n n the child has failed outpt management FTT is severe • Medical emergency if wt <60 -70% of ideal wt • Hypothermia, bradycardia, hypotension n safety is a concern
Management n For difficult cases: • Multidisciplinary team approach produces better outcomes Dietitians n Social workers n Occupational therapists n Psychologists n • NG tube supplementation may be necessary
Outcomes and Prognosis n Persistent disorders of growth • 6 of 7 studies showed statistically significant persistent poor growth (ht, wt, hc) in FTT group at up to 5 years from initial treatment. n Earlier intervention leads to better outcomes
Outcomes and Prognosis n FTT and Immunologic/Infectious Outcomes • FTT children have significantly increased susceptibility to infection Among hospitalized children – increased rates of bacteremia and mortality n Increased rates of upper and lower respiratory infections n
Outcomes and Prognosis n Concurrent Behavior disorders • FTT groups scored lower on reports describing affect and communications skills n Behavior disorders at follow-up • Various trials have demonstrated significant increase in behavioral problems n Cognitive Development • There is a consistent association between FTT and lower cognitive development test scores in preschool and primary school children
Top 6 take home points 1. 2. 3. Evaluation of Failure to Thrive involves careful H&P, observation of feeding session, and should not include routine lab or other diagnostic testing Nutritional deprivation in the infant and toddler age group can have permanent effects on growth and brain development Treatment can usually occur by the primary care physician in the outpatient setting.
Top 6 take home points 4. 5. 6. Psychosocial problems predominate as the causes of FTT in the outpatient setting Treatment goal is to increase energy intake to 1. 5 times the basal requirement Earlier intervention may make it easier to break difficult behavior patterns and reduce sequelae from malnutrition
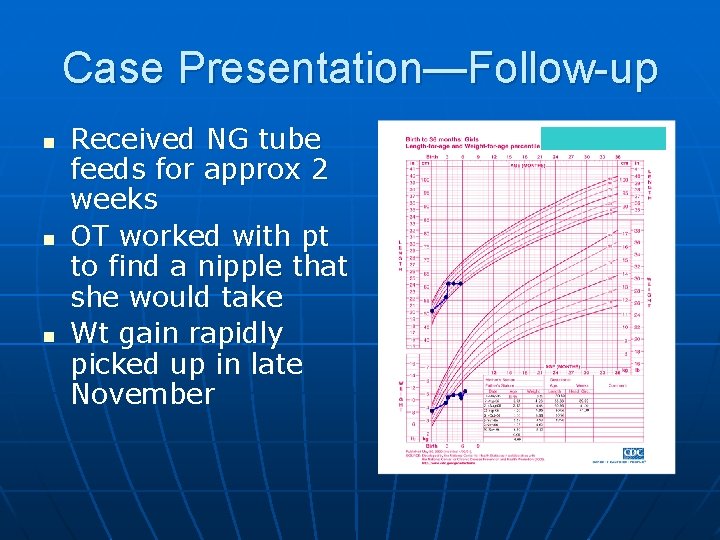
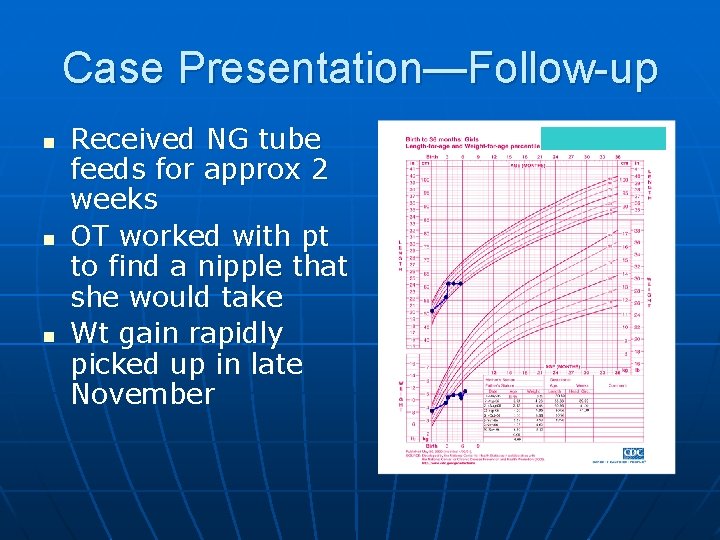
Case Presentation—Follow-up n n n Received NG tube feeds for approx 2 weeks OT worked with pt to find a nipple that she would take Wt gain rapidly picked up in late November
References 1. 2. 3. 4. 5. 6. 7. Block RW, Krebs NF. Failure to thrive as a manifestation of child neglect. Pediatrics 2005 Nov; 116(5): 1234 -7. From National Guidline Clearinghouse – www. guideline. gov Kirkland, RT. Failure to thrive in children under the age of two. Up to Date: http: //www. utdol. com/utd/content/topic. do? topic. Key=gen_pedi/2884&t ype=P&selected. Title=6~29 version 14. 2, april 2006: pgs 1 -8. Krugman SD, Dubowitz H. Failure to thrive. American Family Physician, sept 1 2003. Vol 68 (5). Kane, ML. Pediatric Failure to Thrive. Clinics in Family Practice. Vol 5, #2, June 2003, pages 293 -311. Agency for Healthcare Research and Quality (AHRQ); Evidence report: Criteria for Determining Disability in Infants and Children: Failure to thrive. #72, pages 1 -54. http: //www. ahrq. gov/clinic/ Bauchner, H. Failure to thrive, in Behrman: Nelson Textbook of Pediatrics, 17 th ed, chapter 35, 36 - 2004. Rudolf M, Logan S. What is the long term outcome for children who fail to thrive? A systematic review. In Arch Dis Child 2005; 90; 925 -931.