Syncope and shock Dr Szathmri Mikls Semmelweis University
- Slides: 39
Syncope and shock Dr. Szathmári Miklós Semmelweis University First Department of Medicine 14. Nov. 2011.
Syncope • Definition: Transient loss of consciousness due to reduced cerebral blood flow • Symptoms: – Postural collapse and spontanous recovery – It may occur suddenly, or may be preceded by symptoms of faintness (presyncope: dizziness, a feeling of warmth, nausea, visual blurring) • Types: – Benign: Result of inadequate effects of normal cardiovascular reflexes on heart rate and vascular tone – Serious: Due to a life-threatening arrythmia • Recurrent unexplained syncope with structural heart disease is associated a high risk of death (40% mortality within 2 years)
Pathophysiology of syncope 1. • Sudden impairment of brain metabolism, usually brought about by hypotension with reduction of cerebral blood flow – Three-fourths of the systemic blood volume is contained in the venous bed, and any interference in venous return may lead to a reduction in cardiac output – Cerebral blood flow is maintained as long as systemic arterial vasoconstriction occurs – When this adjustment fails, the hypotension, with resultant cerebral underperfusion to less than half of normal, results in syncope
Syncope-patophysiology 2. • Normally, the pooling of blood in the lower parts of the body is prevented by: – Pressor reflexes that induce contsriction of peripheral arteriolas and venules – Reflex acceleration of the heart by means of aortic and carotid reflexes – Improvement of venous return to the heart by activity of the muscles of the limbs
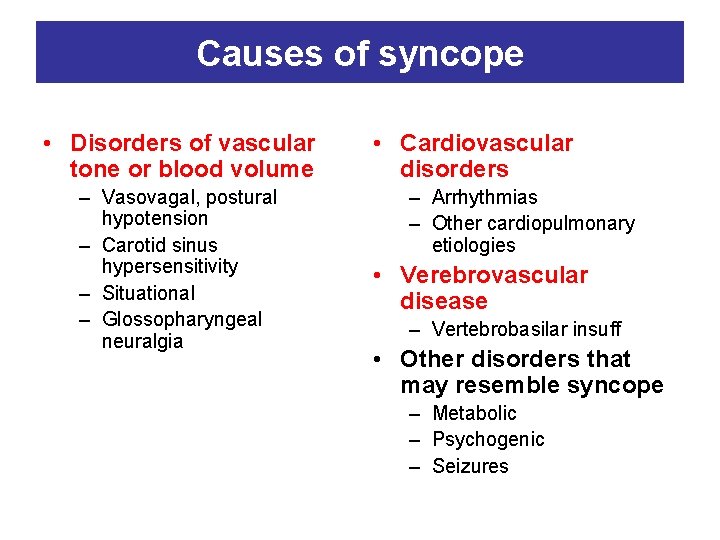
Causes of syncope • Disorders of vascular tone or blood volume – Vasovagal, postural hypotension – Carotid sinus hypersensitivity – Situational – Glossopharyngeal neuralgia • Cardiovascular disorders – Arrhythmias – Other cardiopulmonary etiologies • Verebrovascular disease – Vertebrobasilar insuff • Other disorders that may resemble syncope – Metabolic – Psychogenic – Seizures
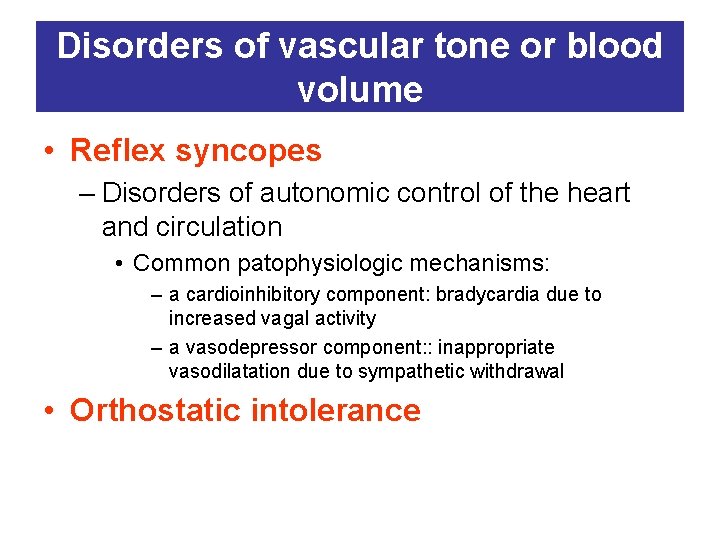
Disorders of vascular tone or blood volume • Reflex syncopes – Disorders of autonomic control of the heart and circulation • Common patophysiologic mechanisms: – a cardioinhibitory component: bradycardia due to increased vagal activity – a vasodepressor component: : inappropriate vasodilatation due to sympathetic withdrawal • Orthostatic intolerance
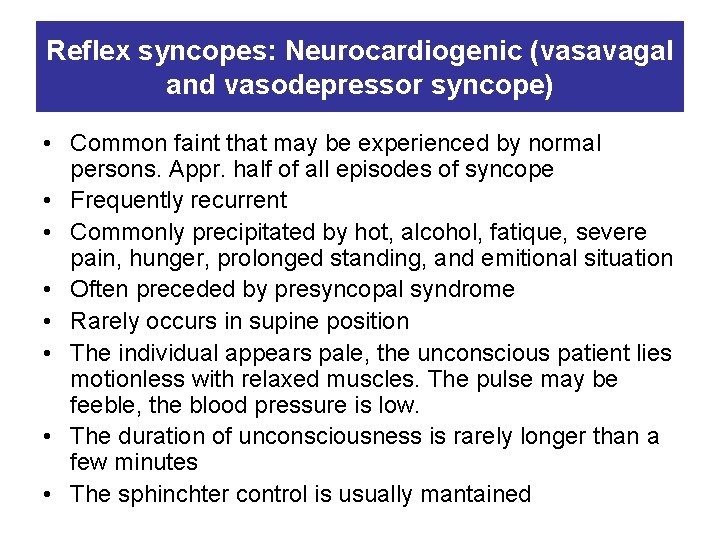
Reflex syncopes: Neurocardiogenic (vasavagal and vasodepressor syncope) • Common faint that may be experienced by normal persons. Appr. half of all episodes of syncope • Frequently recurrent • Commonly precipitated by hot, alcohol, fatique, severe pain, hunger, prolonged standing, and emitional situation • Often preceded by presyncopal syndrome • Rarely occurs in supine position • The individual appears pale, the unconscious patient lies motionless with relaxed muscles. The pulse may be feeble, the blood pressure is low. • The duration of unconsciousness is rarely longer than a few minutes • The sphinchter control is usually mantained
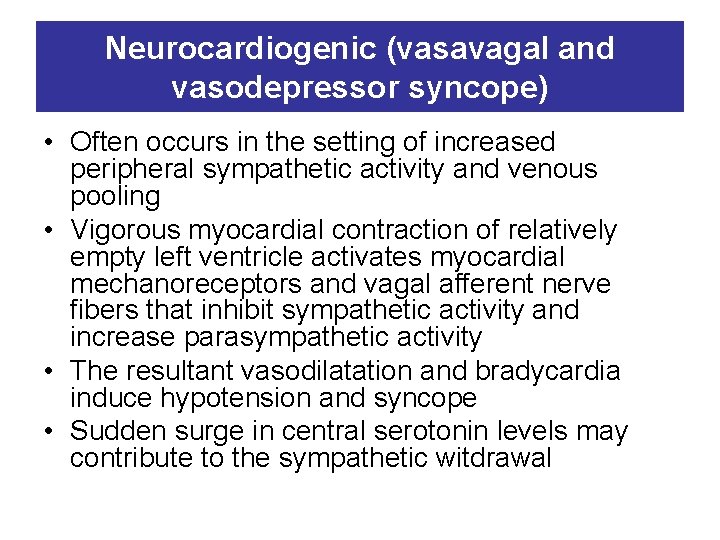
Neurocardiogenic (vasavagal and vasodepressor syncope) • Often occurs in the setting of increased peripheral sympathetic activity and venous pooling • Vigorous myocardial contraction of relatively empty left ventricle activates myocardial mechanoreceptors and vagal afferent nerve fibers that inhibit sympathetic activity and increase parasympathetic activity • The resultant vasodilatation and bradycardia induce hypotension and syncope • Sudden surge in central serotonin levels may contribute to the sympathetic witdrawal
Reflex syncopes: Situational syncope • These syndromes are caused by abnormal autonomic control and may involve a cardioinhibitory response, a vasodepressor response, or both – Cough (after prolonged coughing in men with COPD) – Micturition (in older men with prostatic hypertrophy and obstruction. Occurs at night during or after voiding) – Defecation (secondary to Valsalva’s maneuver in older individuals with constipation)
Reflex syncopes: Carotid sinus hypersensitivity • Precipitated by pressure on the carotid sinus baroreceptors • Typically occurs in the setting of shaving, a tight collar, or turning the head to one side • This occurs predominantly in men over 50 years • The afferent impulses (via a branch of glossopharyngeal nerve) activate cardiac vagal efferent nerve fibres. The response may cause sinus arrest or AV block (cardioinhibitory response) or/and vasodilation (vasodepressor response)
Postural (orthostatic) hypotension • This occurs in patients who have hypovolemia or a chronic defect in vasomotor reflexes • Systemic arterial blood pressure falls on assumption of upright position due to loss of vasoconstriction reflexes • Sudden rising from a recumbent position is precipitating circumstance • Orthostatic hypotension may be the cause of syncope in up to 30% of the elderly • Causes: – Drug induced – Idiopathic postural hypotension (often familial, more common in men, together with constipation, erectile dyfunction, inability to sweat, heat intolerance) – Autonom nervous system disorders (diabetic, nutritional, amyloid polyneuropathy – CNS disorders (parkinsonism, progressive cerebellar degneration)
Syncope because of cardiovascular disorders 1. • Cardiac syncope results from a sudden reduction in cardiac output, caused most commonly by a cardiac arrhythmia – As the heart rate decreases, ventricular filling time and stroke volume increase to maintain normal cardiac output – At rates less than 30/min, stroke volume can no longer increase. At rate more than 180/min ventricular filling time is inadequate to maintain adequate stroke volume. – Upright position, cerebrovascular disease, anemia, loss of atrioventricular synchrony, coronary, myocardial, or valvular disease all reduce the tolerance to alterations in rate.
Syncope because of cardiovascular disorders 2. • Bradyarrhythmias if the escape pacemaker rate is insufficient to maintain cardiac output – The syncope occurs abruptly without presyncopal symptoms – It recurs several times daily • Tachyarrhythmias, mostly ventricular tachycardia with structural heart disease – Usually preceded by palpitation or other presyncopal symptoms • Structural cardiovascular disorders – When the cardiac output cannot increase to compensate adequately for peripheral vasodilatation (such as following exercise) • Obstruction to forward flow is the most common reason that cardiac output can not increase (aortic stenosis or HOCM)
Syncope because of cerebrovascular disease • Alone rarely causes syncope but may lower the threshold for syncope in patients with other causes • The vertebrobasilar arteries (which supply the brainstem structures) are usually involved • Most patients with cerebrovascular syncope also have symptoms of focal neurological ischemia (arm or leg weakness, diplopia, ataxia, dysarthria etc. )
Differential diagnosis of syncope • Anxiety attacks and hyperventilation syndrome – The symptoms are not accompanied by facial pallor and are not relieved by recumbency – Typical associated symptoms: palpitation, air hunger, tingling of fingers etc. Attacks can often be reproduced by hyperventilation. • Seizure – – May be heralded by an aura Injury from falling is frequent Tonic-clonic movements The period of uncosciousness is longer than in syncope • Hypoglykaemia – Most common cause is the excessive administration of insulin • Acute haemorrhage – Gastrointestinal bleeding. Black stool.
Approach to the patient with syncope 1. • The cause may only be apparent at the time of the event, leaving few, if any, clues when the patient is seen later by the physician. • The physician should think first of those causes that constitute at therapeutic emergency: – Massive internal hemorrhage – Myocardial infarction (may be painless) – Cardiac arrhythmias
Approach to the patient with syncope 2. • Careful hystory – Loss of consciousness in particular situation – The position of patient at the time of the syncopal episode: • Syncope in supine position suggest arrhythmia or seizure • Syncope in upright position suggest neurocardiogenic, postural hypotension • When the individual wearing a shirt with a tight collar, or is turning to look while driving in reverse, suggest carotid hypersensitivity
Approach to the patient with syncope 3. • Physical examination – Heart rate, blood pressure in the supine, sitting, and standing position – An attempt to reproduce an attack (hyperventilation, or cough syncope induced by Valsalva’s maneuver) • Laboratory examinations – Electrolytes, blood glucose and hematocrit are usually indicated. – Cardiac enzymes if myocardial ischemia is suspected – Blood and urine toxicology screens may reveal the presence of alcohol or other drugs – In case of suspition of adrenal insufficiency measurements of the hormone levels
Approach to the patient with syncope 4. • ECG should be performed in all patients • Continuous electrocardiographic monitoring or Holter monitor for 24 to 48 h. • Invasive cardiac electrophysiologic testing provides information regarding sinus node function, AV conduction, and supraventricular and ventricular arrhythmias • Upright tilt table testing is indicated for recurrent syncope, or a single syncopal event in a high-risk setting (pilot, commercial vehicle driver etc) • To determine the presence of structural heart disease: echocardiogram with Doppler examination
Treatment of syncope 1. • The patient should avoid situation in which sudden loss of consciousness might result in injury (operating heavy machinery, driving, swimming alone etc. ) • Patients with vasovagal syncope should be instructed to avoid situations that have caused them to lose consciousness and to assume a recumbent position when premonitory symptoms occur • Patients with orthostatic hypotension should be intstructed to rise slowly and systematically (supine to seated, seated to standing) from the bed or a chair • Family members should be educated, this will ensure appropriate therapy and may prevent delivery of inappropriate therapy
In patients who are resistant to the preventive measures and in cases of recurrent episodes of syncope • In patients with vasovagal syncope: • • • β-adrenergic receptor antagonists Serotonin reuptake inhibitors Fludrocortisone (also in patients with postural hypotension) α-receptor agonist (proamatine) Disopyramid is a vagolytic antiarrhythmic drug Permanent dual chamber cardiac pacing • In patients with orthostatic hypotension: • Whenever possible, medications that aggravate the problem (vasodilatators, diuretics etc) should be discontinued • Use of compression stocking may help
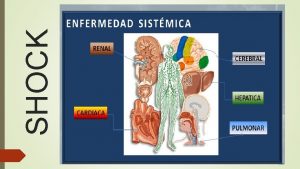
Shock • Definition: Shock is a clinical syndrome that results from inadequate tissue perfusion. • The hypoperfusion-induced imbalance between the delivery of and requirements for oxygen and substrate leads to cellular dysfunction. The inadequate oxygen supply induces the production and release of inflammatory mediators that further compromise perfusion through functional and structural changes within the microvasculature. The cellular hypoperfusion causes multiple organ failure. • If the process is not interrupted, leads to death of the patient • Clinical manifestation: result of sympathetic neuroendocrine responses to hypoperfusion and the breakdown in organ function
Classification of shock • Hypovolemic • Traumatic • Cardiogenic – Intrinsic – Compressive • Septic – Hyperdynamic – Hypodynamic • Neurogenic • Hypoadrenal
Pathogenesis and organ response 1. • Microcirculation – Systemic vascular resistance rises to maintain a level of systemic pressure that is adequate for perfusion of the heart and brain at the expense of other tissue. Arteriolar vascular smooth cells has both α- and β–adrenergic receptors. Norepinephrine release - acting on α 1 -receptors as vasocontsrictor - is the fundamental compensatory response in shock. – Reduced filtration because of decreased capillary surface area across which filtration occurs. Consequence: increased interstitial and intravascular volume at the expense of intracellular volume.
Pathogenesis and organ response 2. • Cellular response – Decline of intracellular high energy phosphate stores (decreased amount of ATP) because of the mitochondrial dysfuction. – Consequences: • Accumulation of hydrogen ions, lactate (products of anaerobic metabolism) • As shock progresses, these vasodilatator metabolits cause further hypotension and hypoperfusion
Pathogenesis and organ response 3. • Neuroendocrine response – Hypovolemia are sensed by baro- and chemoreceptors • Increased adrenergic output – release of norepinephrine – vasocontriction and metabolic effects : increased glycolysis and gluconeogenesis • Reduced vagal activity – increased heart rate and cardiac output • Severe stress causes ACTH release – this stimulates cortisol secretion • Increased renin release because of the hypoperfusion of JGA. Renin induces the formation of angiotensin II, an extremely potent vasoconstrictor and stimulator of aldosterone release. Aldosterone enhances renal tubular reabsorption of sodium, resulting in low-volume, concentrated, sodium-free urine
Pathogenesis and organ response 4. • Cardiovascular response – Decreased ventricular filling (decreased preload). The increased heart rate is a useful but limited compensatory mechanism to maintain the adequate stroke volume – Impaired myocardial contractility which reduces the stroke volume – Elevated sytemic vascular resistance (except of hyperdynamic stage of septic shock) increases the afterload
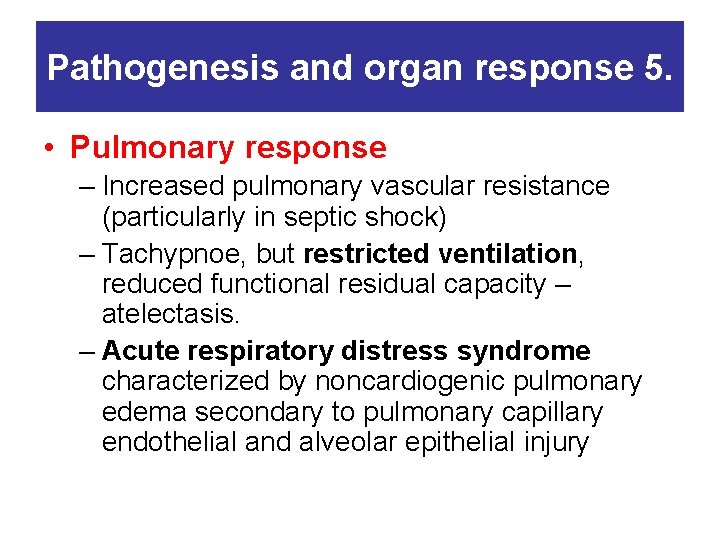
Pathogenesis and organ response 5. • Pulmonary response – Increased pulmonary vascular resistance (particularly in septic shock) – Tachypnoe, but restricted ventilation, reduced functional residual capacity – atelectasis. – Acute respiratory distress syndrome characterized by noncardiogenic pulmonary edema secondary to pulmonary capillary endothelial and alveolar epithelial injury
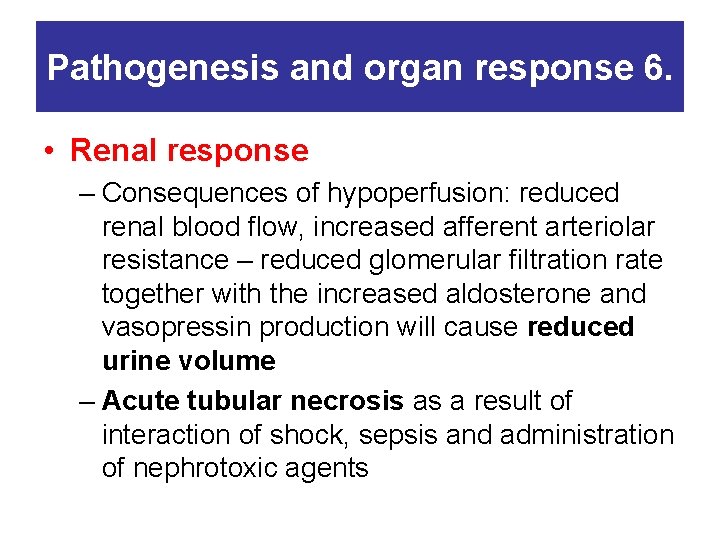
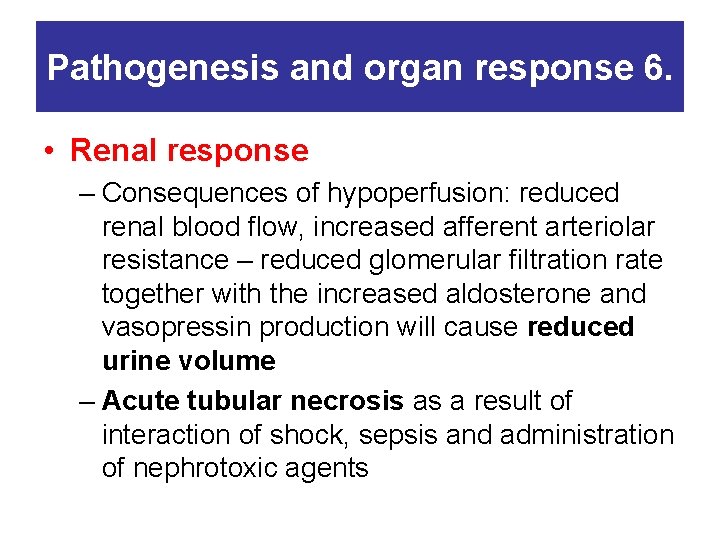
Pathogenesis and organ response 6. • Renal response – Consequences of hypoperfusion: reduced renal blood flow, increased afferent arteriolar resistance – reduced glomerular filtration rate together with the increased aldosterone and vasopressin production will cause reduced urine volume – Acute tubular necrosis as a result of interaction of shock, sepsis and administration of nephrotoxic agents
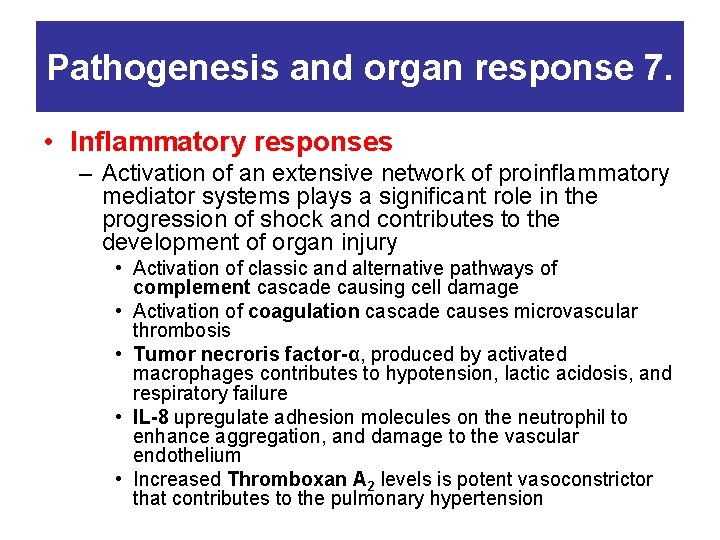
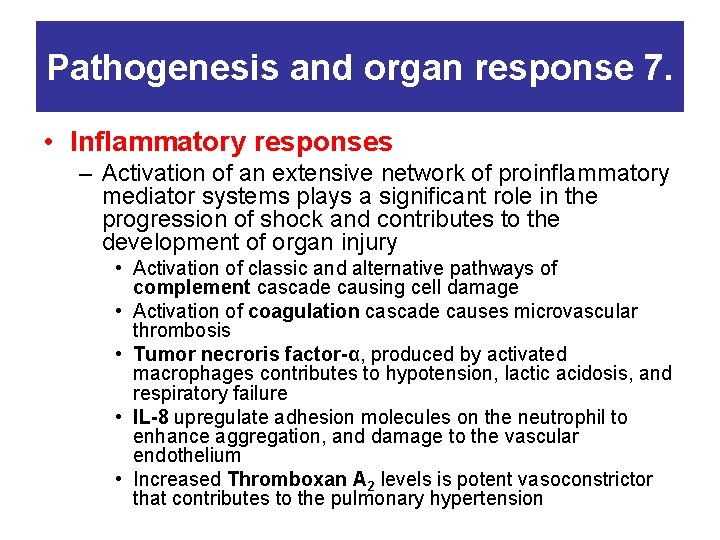
Pathogenesis and organ response 7. • Inflammatory responses – Activation of an extensive network of proinflammatory mediator systems plays a significant role in the progression of shock and contributes to the development of organ injury • Activation of classic and alternative pathways of complement cascade causing cell damage • Activation of coagulation cascade causes microvascular thrombosis • Tumor necroris factor-α, produced by activated macrophages contributes to hypotension, lactic acidosis, and respiratory failure • IL-8 upregulate adhesion molecules on the neutrophil to enhance aggregation, and damage to the vascular endothelium • Increased Thromboxan A 2 levels is potent vasoconstrictor that contributes to the pulmonary hypertension
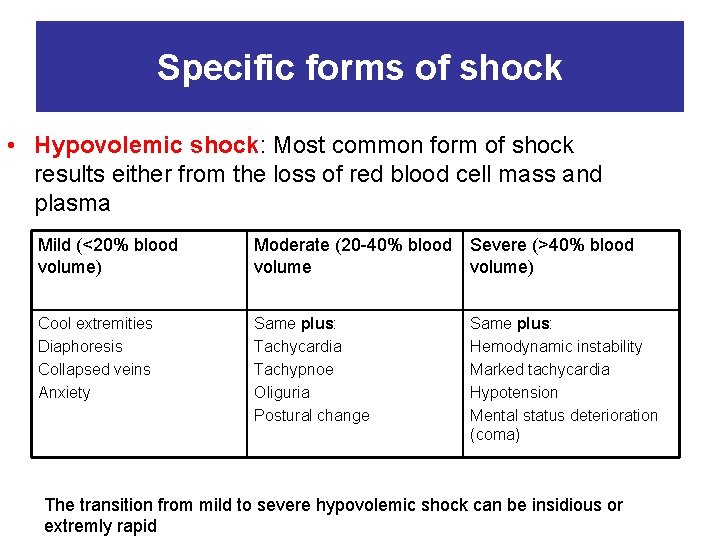
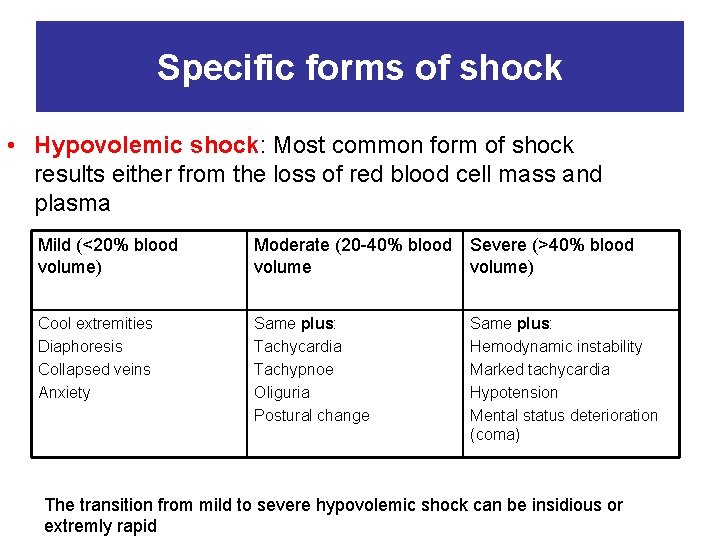
Specific forms of shock • Hypovolemic shock: Most common form of shock results either from the loss of red blood cell mass and plasma Mild (<20% blood volume) Moderate (20 -40% blood Severe (>40% blood volume) Cool extremities Diaphoresis Collapsed veins Anxiety Same plus: Tachycardia Tachypnoe Oliguria Postural change Same plus: Hemodynamic instability Marked tachycardia Hypotension Mental status deterioration (coma) The transition from mild to severe hypovolemic shock can be insidious or extremly rapid
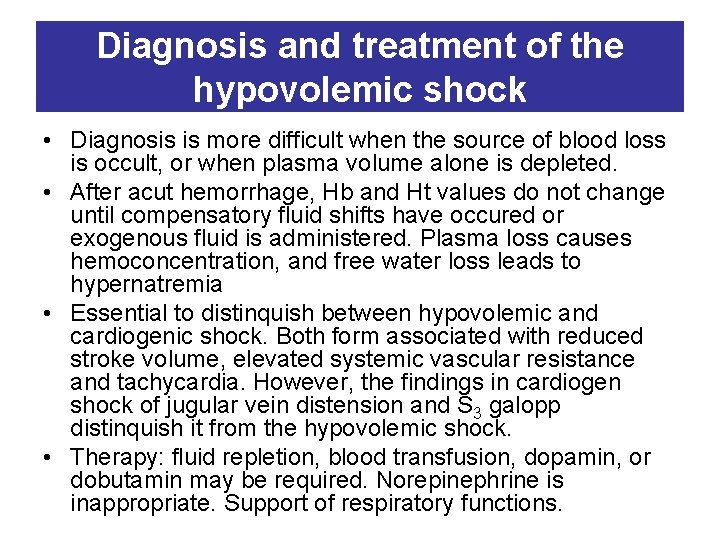
Diagnosis and treatment of the hypovolemic shock • Diagnosis is more difficult when the source of blood loss is occult, or when plasma volume alone is depleted. • After acut hemorrhage, Hb and Ht values do not change until compensatory fluid shifts have occured or exogenous fluid is administered. Plasma loss causes hemoconcentration, and free water loss leads to hypernatremia • Essential to distinquish between hypovolemic and cardiogenic shock. Both form associated with reduced stroke volume, elevated systemic vascular resistance and tachycardia. However, the findings in cardiogen shock of jugular vein distension and S 3 galopp distinquish it from the hypovolemic shock. • Therapy: fluid repletion, blood transfusion, dopamin, or dobutamin may be required. Norepinephrine is inappropriate. Support of respiratory functions.
Specific forms of shock • Traumatic shock – Hypovolemia (fluid loss into the interstitum of injured tissues), and blood loss. These fluid losses are compounded by injury-induced inflammatory responses, leading to multiple organ failure. • Neurogenic shock – Interruption of sympatetic vasomotor input after high cervical spinal cord injury, severe head injury – Arteriolar dilatation and venodilatation, which decreases venous return and cardiac output. Warm extremities. Correction of the hypovolemia and norepinephrine may be necessery to augment vascular resistance
Specific forms of shock • Intrinsic cardiogenic shock – Caused by sudden failure of the heart as an effective pump. It occurs most commonly as a complication of acute myocardial infarction, but it may also be seen in patients with severe bradyor tachyarrhythmias, valvular heart disease, or in terminal stage of chronic heart failure (ischemic heart disease, or dilated cardiomyopathy) – Low cardiac output, reduced systemic perfusion, elevation of systemic vascular resistance and pulmonary vascular pressure. Absolute or relative hypovolemia is usually not present. Pulmonary edema, reduction in lung compliance – Treatment: The goal is to increase contractility without significant increases in heart rate (dopamine, dobutamine). Pulmonary congestion may be responsive to intravenous furosemid. In case of inadequate response intraaortic balloon-pump. Revascularization in patients with AMI, correction of anatomic defects such as rupture of the papillary muscles.
Specific forms of shock • Septic shock – Caused by the systemic response to a severe infection. Most frequently in elderly or immuncompromised patients and in those who have undergone an invasive procedure in which bacterial contamination has occured. – Clinical findings in septic shock are a consequence of metabolic and circulatory derangements driven by the systemic infection and the release of toxic components of the infectious organisms. – Organism toxins lead to the release of cytokines – Tissue factor expression and fibrin deposition are increased, and DIC may develop – NO-synthase is stimulated, and NO, a powerful vasodilatator is released.
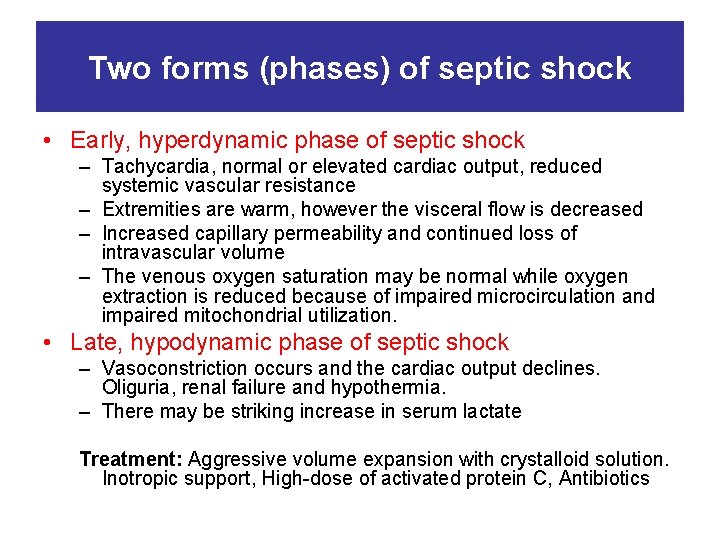
Two forms (phases) of septic shock • Early, hyperdynamic phase of septic shock – Tachycardia, normal or elevated cardiac output, reduced systemic vascular resistance – Extremities are warm, however the visceral flow is decreased – Increased capillary permeability and continued loss of intravascular volume – The venous oxygen saturation may be normal while oxygen extraction is reduced because of impaired microcirculation and impaired mitochondrial utilization. • Late, hypodynamic phase of septic shock – Vasoconstriction occurs and the cardiac output declines. Oliguria, renal failure and hypothermia. – There may be striking increase in serum lactate Treatment: Aggressive volume expansion with crystalloid solution. Inotropic support, High-dose of activated protein C, Antibiotics
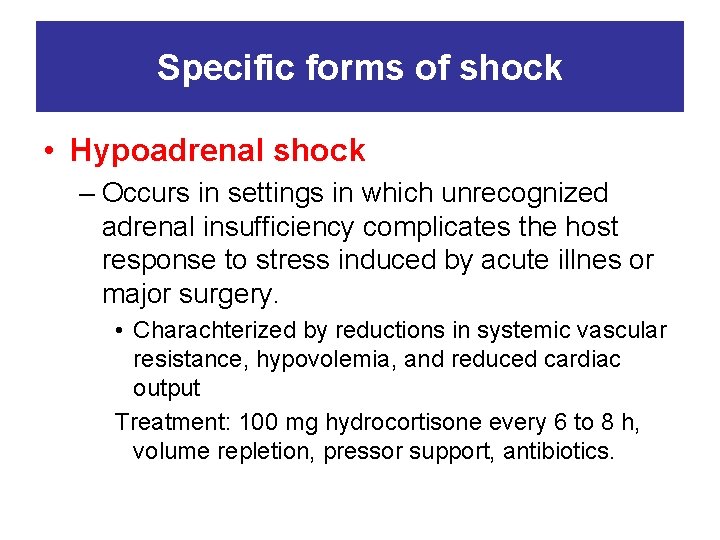
Specific forms of shock • Hypoadrenal shock – Occurs in settings in which unrecognized adrenal insufficiency complicates the host response to stress induced by acute illnes or major surgery. • Charachterized by reductions in systemic vascular resistance, hypovolemia, and reduced cardiac output Treatment: 100 mg hydrocortisone every 6 to 8 h, volume repletion, pressor support, antibiotics.
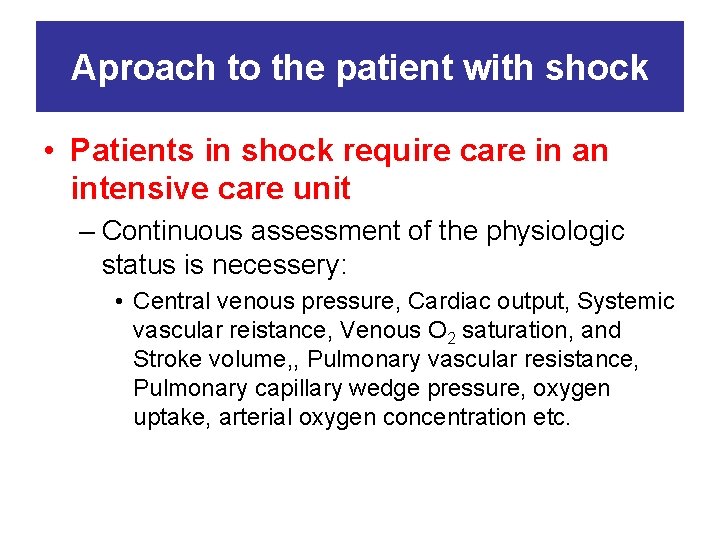
Aproach to the patient with shock • Patients in shock require care in an intensive care unit – Continuous assessment of the physiologic status is necessery: • Central venous pressure, Cardiac output, Systemic vascular reistance, Venous O 2 saturation, and Stroke volume, , Pulmonary vascular resistance, Pulmonary capillary wedge pressure, oxygen uptake, arterial oxygen concentration etc.
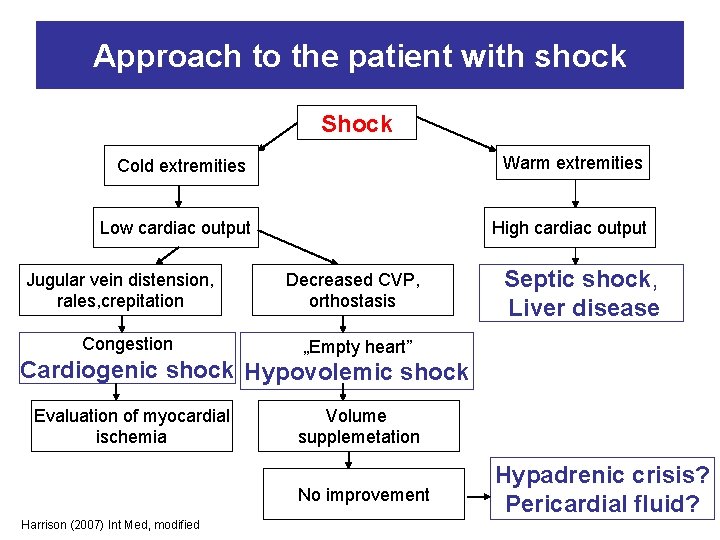
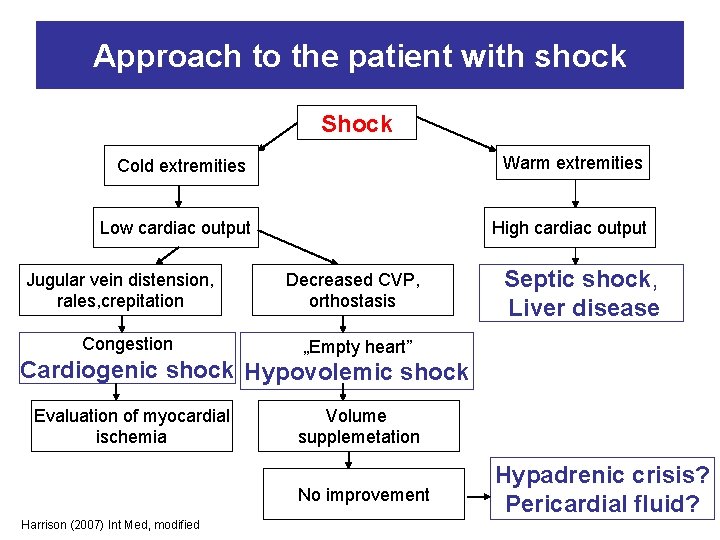
Approach to the patient with shock Shock Cold extremities Warm extremities Low cardiac output High cardiac output Jugular vein distension, rales, crepitation Congestion Decreased CVP, orthostasis Septic shock, Liver disease „Empty heart” Cardiogenic shock Hypovolemic shock Evaluation of myocardial ischemia Volume supplemetation No improvement Harrison (2007) Int Med, modified Hypadrenic crisis? Pericardial fluid?
 Mikls
Mikls Yazid saidi
Yazid saidi Davis mikls
Davis mikls Eszéki híd felégetése
Eszéki híd felégetése Mikls
Mikls Nkt 65§
Nkt 65§ Cauda equina vs conus medullaris
Cauda equina vs conus medullaris Shok neurogenico
Shok neurogenico Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Semmelweis
Semmelweis Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Syncope in the older patient is
Syncope in the older patient is Keppra loading dose
Keppra loading dose Seizure vs syncope
Seizure vs syncope Prodromen syncope
Prodromen syncope Carotid sinus hypersensitivity
Carotid sinus hypersensitivity Snycope
Snycope Nursing care plan for pulmonary embolism
Nursing care plan for pulmonary embolism Syncope
Syncope Syncope
Syncope Syncope
Syncope Sote doktori hivatal
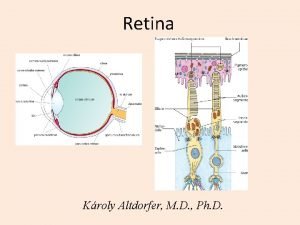
Sote doktori hivatal Kroly
Kroly Retikulinfasern leber
Retikulinfasern leber Vesicle fusion
Vesicle fusion Orthodontics semmelweis
Orthodontics semmelweis Semmelweis
Semmelweis Semmelweis egyetem konzerváló fogászati klinika budapest
Semmelweis egyetem konzerváló fogászati klinika budapest Semmelweis egyetem szemészeti klinika budapest
Semmelweis egyetem szemészeti klinika budapest Semmelweis egyetem doktori iskola
Semmelweis egyetem doktori iskola Nasal vestibule
Nasal vestibule Semmelweis
Semmelweis Erasmus plus semmelweis
Erasmus plus semmelweis Itc semmelweis
Itc semmelweis Semmelweis
Semmelweis Semmelweis arc
Semmelweis arc Semmelweis
Semmelweis