Anaemias I Makrocytic anaemias Dr Judit Demeter Semmelweis






















- Slides: 61
Anaemias I Makrocytic anaemias Dr. Judit Demeter Semmelweis Egyetem ÁOK. , I. sz. Belgyógyászati Klinika
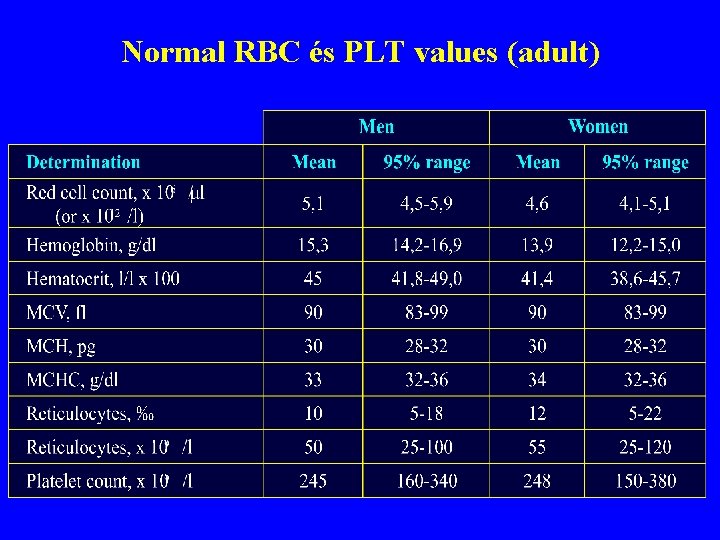
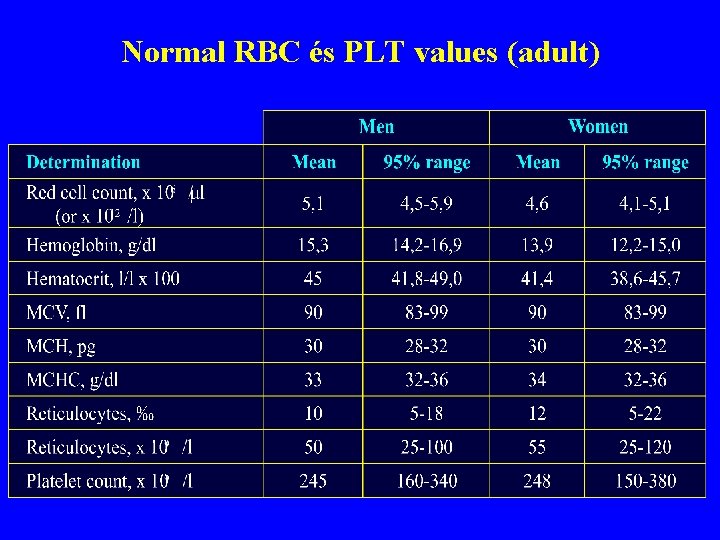
Normal RBC és PLT values (adult)

Normal peripheral blood smear, thin, homogenous part

Normal RBC morphology

Red blood cell maturation 1. 2. 3. 4. 5. 6. 1. : proerythroblast; 4. : oxyphil normoblast; 2. : basophil normoblast; 5. : polychromatophil RBC; 3. : polychromatophil normoblast; 6. : mature RBC
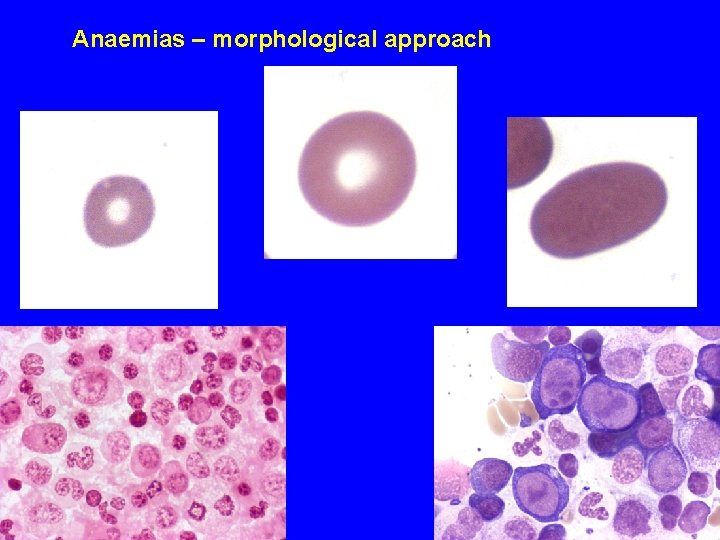
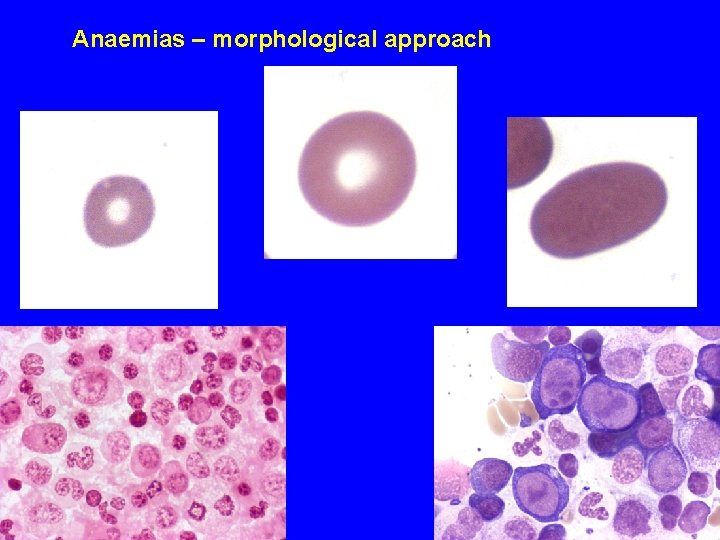
Anaemias – morphological approach
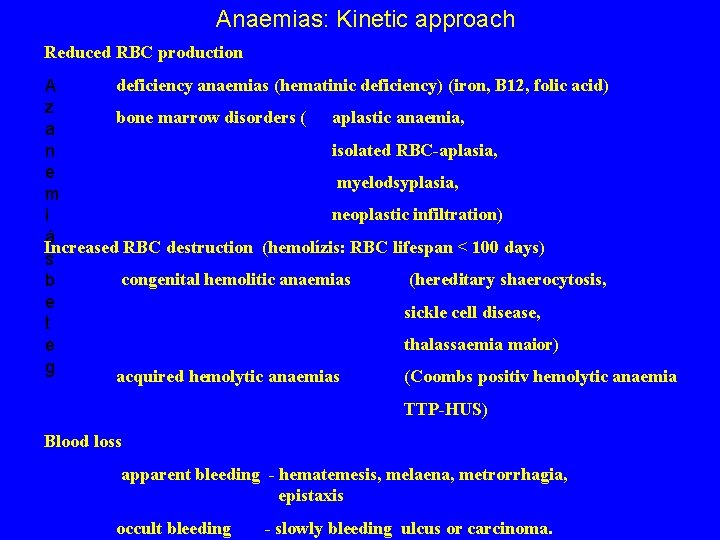
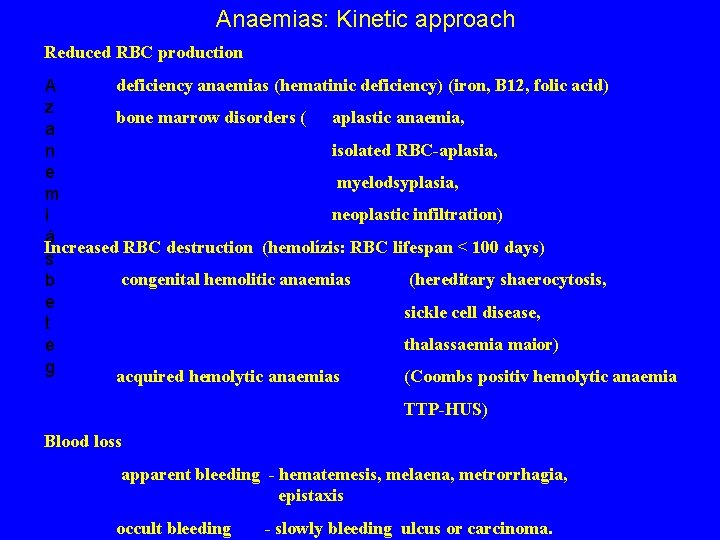
Anaemias: Kinetic approach Reduced RBC production deficiency anaemias (hematinic deficiency) (iron, B 12, folic acid) A z bone marrow disorders ( aplastic anaemia, a isolated RBC-aplasia, n e myelodsyplasia, m neoplastic infiltration) i á Increased RBC destruction (hemolízis: RBC lifespan < 100 days) s congenital hemolitic anaemias (hereditary shaerocytosis, b e sickle cell disease, t thalassaemia maior) e g acquired hemolytic anaemias (Coombs positiv hemolytic anaemia TTP-HUS) Blood loss apparent bleeding - hematemesis, melaena, metrorrhagia, epistaxis occult bleeding - slowly bleeding ulcus or carcinoma.
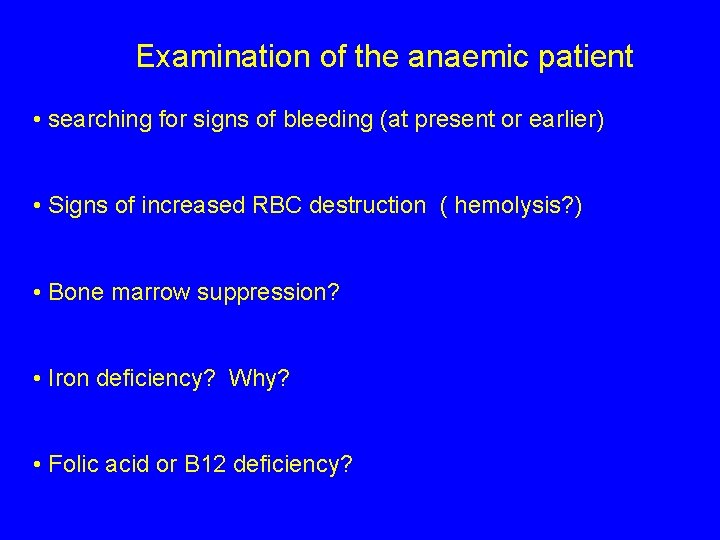
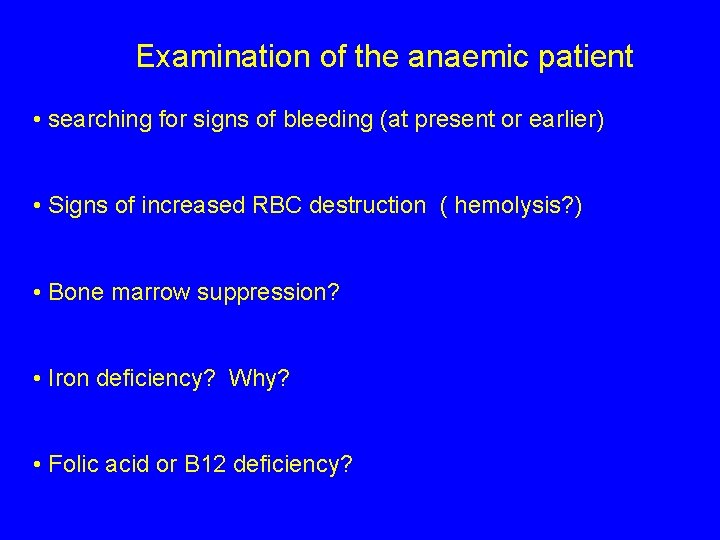
Examination of the anaemic patient • searching for signs of bleeding (at present or earlier) • Signs of increased RBC destruction ( hemolysis? ) • Bone marrow suppression? • Iron deficiency? Why? • Folic acid or B 12 deficiency?
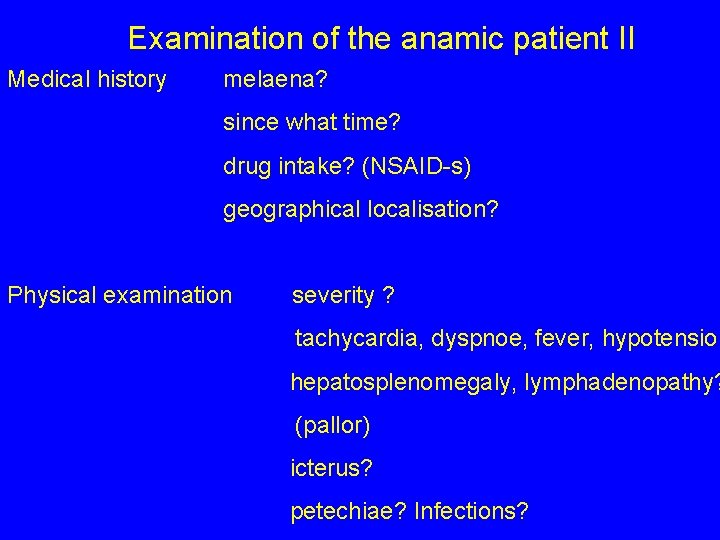
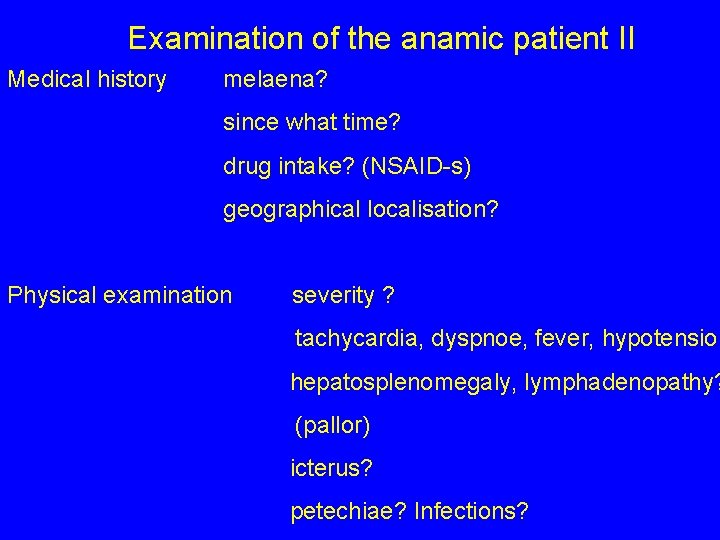
Examination of the anamic patient II Medical history melaena? since what time? drug intake? (NSAID-s) geographical localisation? Physical examination severity ? tachycardia, dyspnoe, fever, hypotension hepatosplenomegaly, lymphadenopathy? (pallor) icterus? petechiae? Infections?
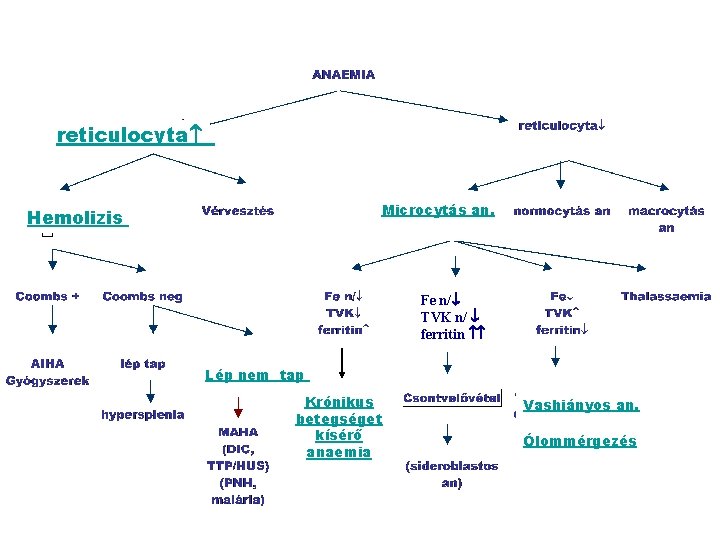
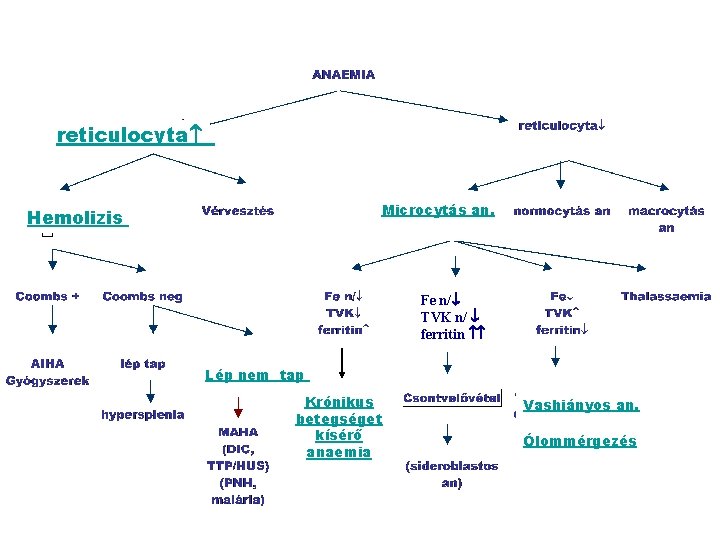
reticulocyta Microcytás an. E Hemolizis Fe n/ TVK n/ ferritin Lép nem tap Krónikus betegséget kísérő anaemia Vashiányos an. Ólommérgezés

Vvs: 4. 83 Hgb: 138 Ht: 41 MCV: 86 T/l g/l % fl Vvs: 1. 51 T/l hgb: 64 g/l Ht: 17 % MCV: 113 fl
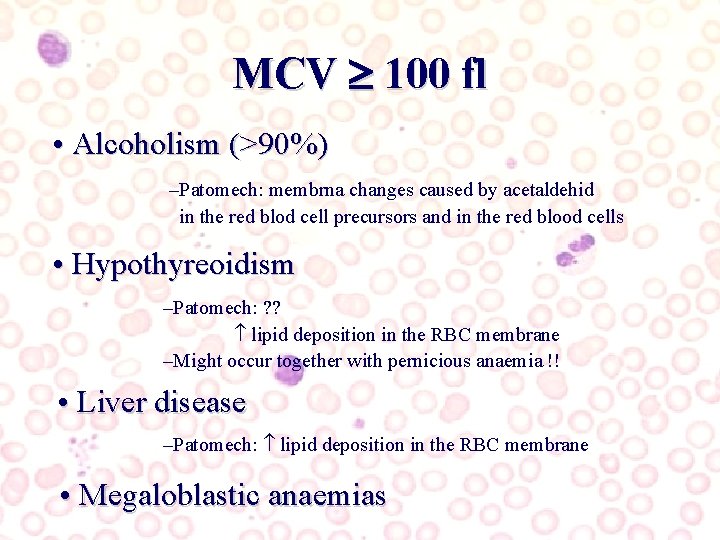
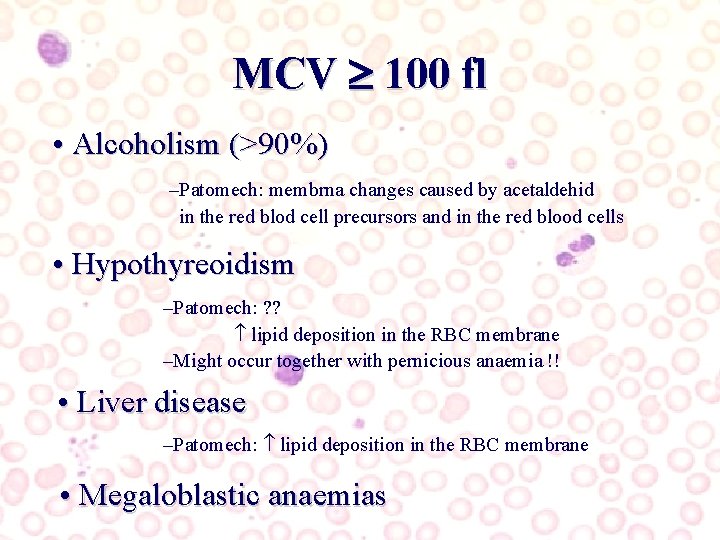
MCV 100 fl • Alcoholism (>90%) –Patomech: membrna changes caused by acetaldehid in the red blod cell precursors and in the red blood cells • Hypothyreoidism –Patomech: ? ? lipid deposition in the RBC membrane –Might occur together with pernicious anaemia !! • Liver disease –Patomech: lipid deposition in the RBC membrane • Megaloblastic anaemias
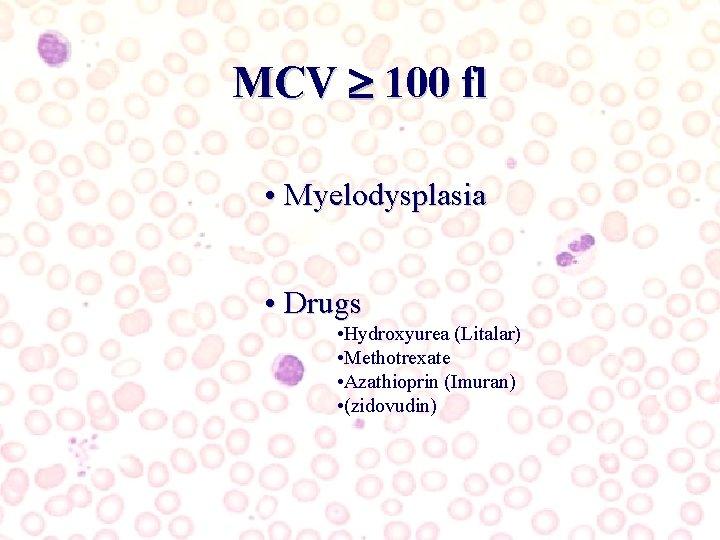
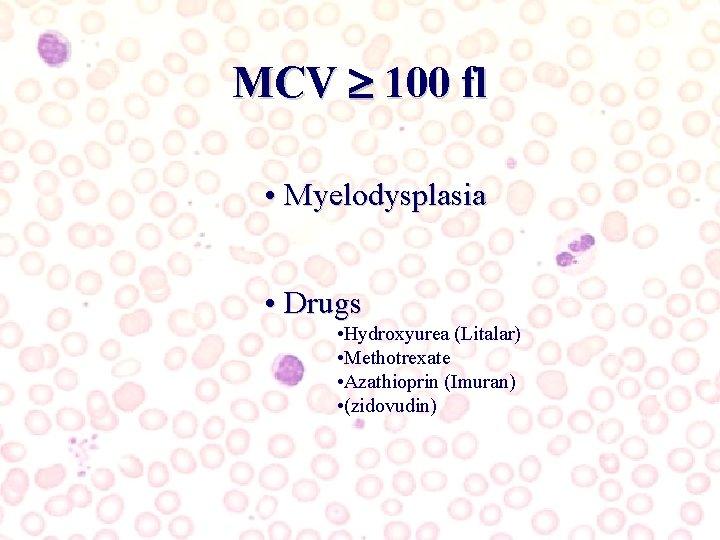
MCV 100 fl • Myelodysplasia • Drugs • Hydroxyurea (Litalar) • Methotrexate • Azathioprin (Imuran) • (zidovudin)
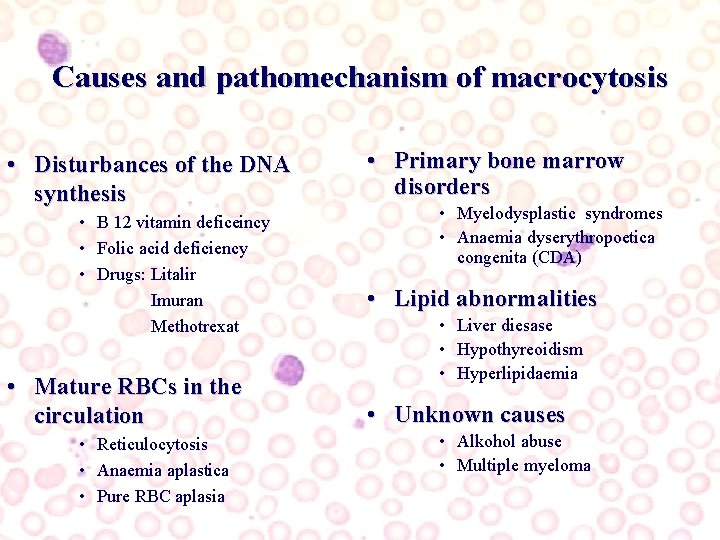
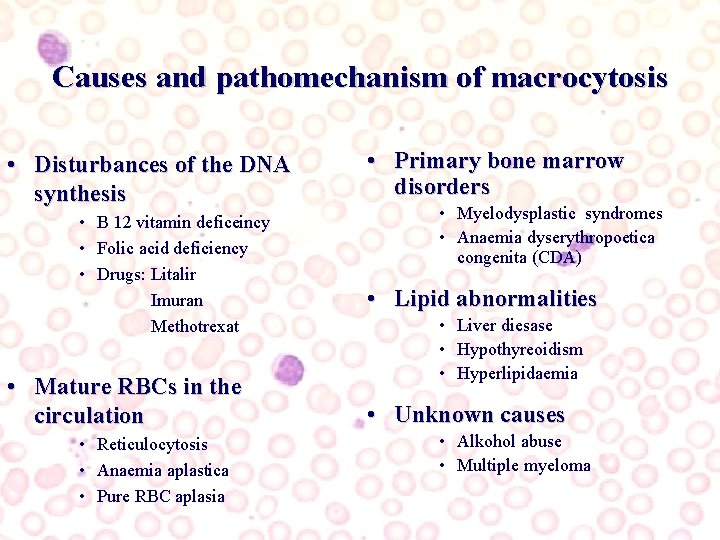
Causes and pathomechanism of macrocytosis • Disturbances of the DNA synthesis • B 12 vitamin deficeincy • Folic acid deficiency • Drugs: Litalir Imuran Methotrexat • Mature RBCs in the circulation • Reticulocytosis • Anaemia aplastica • Pure RBC aplasia • Primary bone marrow disorders • Myelodysplastic syndromes • Anaemia dyserythropoetica congenita (CDA) • Lipid abnormalities • Liver diesase • Hypothyreoidism • Hyperlipidaemia • Unknown causes • Alkohol abuse • Multiple myeloma
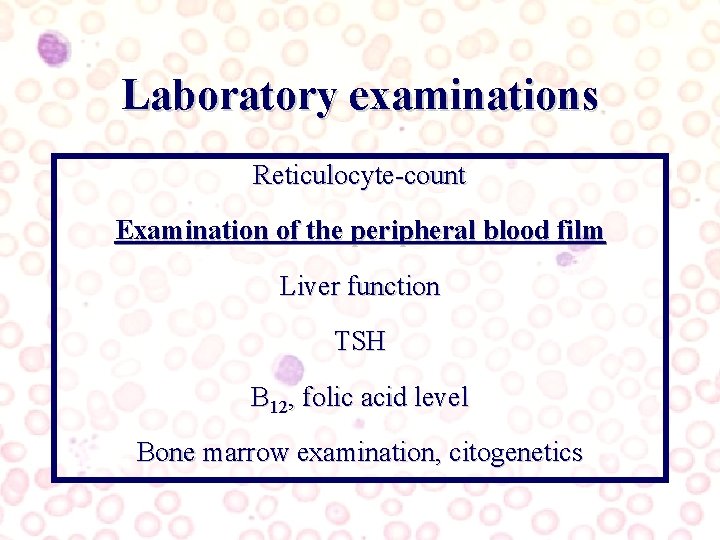
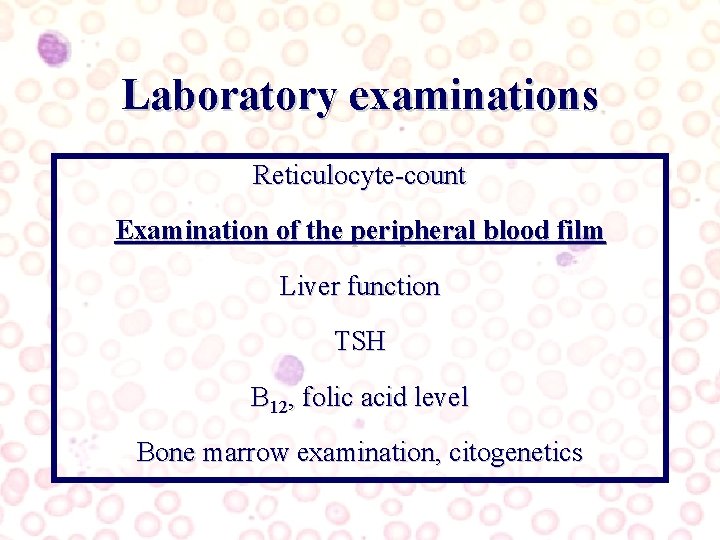
Laboratory examinations Reticulocyte-count Examination of the peripheral blood film Liver function TSH B 12, folic acid level Bone marrow examination, citogenetics

reticulocytosis
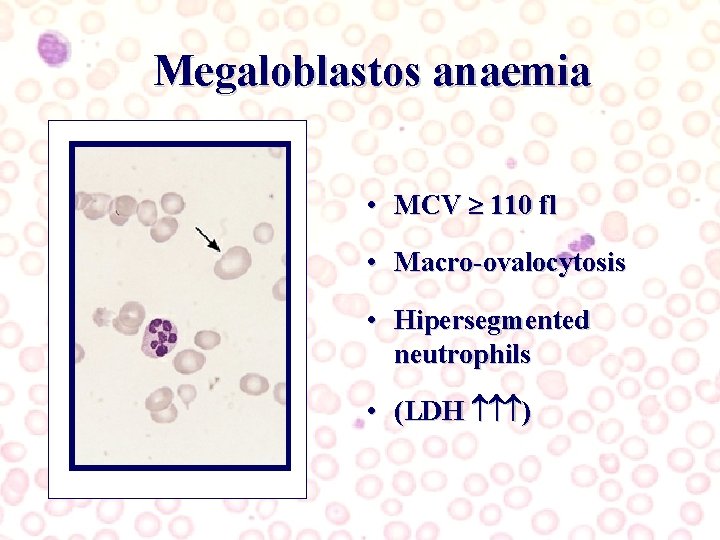
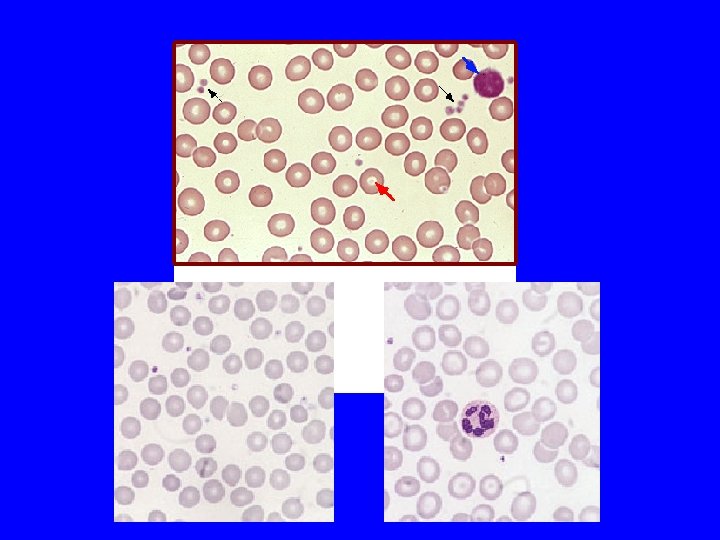
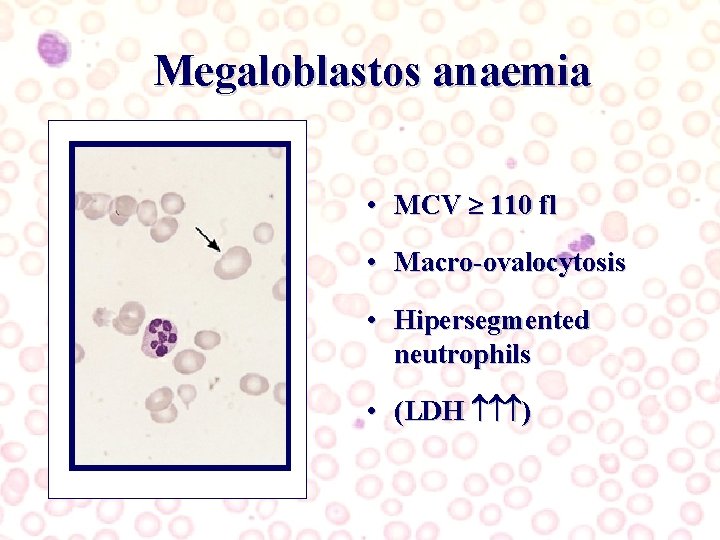
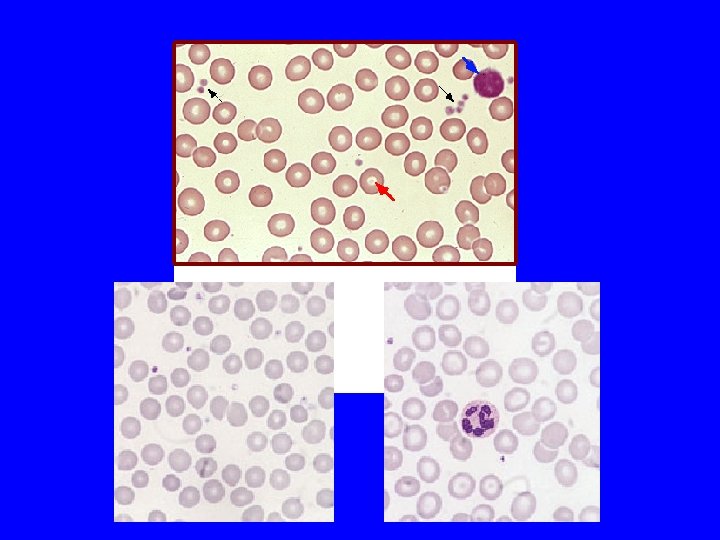
Megaloblastos anaemia • MCV 110 fl • Macro-ovalocytosis • Hipersegmented neutrophils • (LDH )
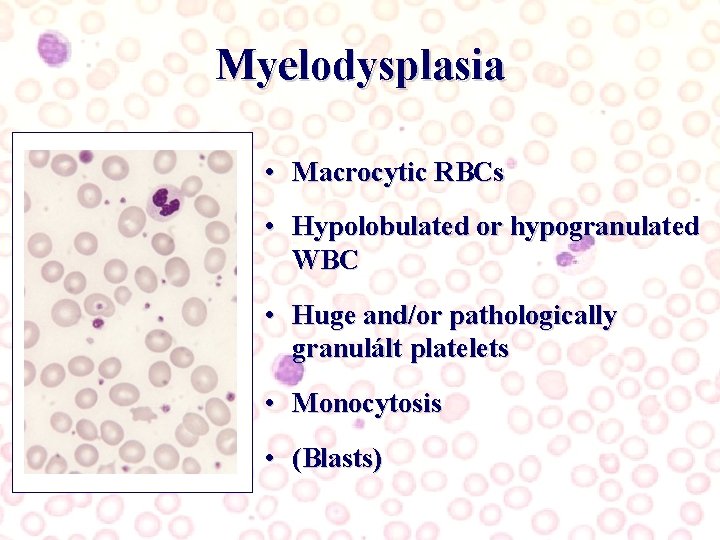
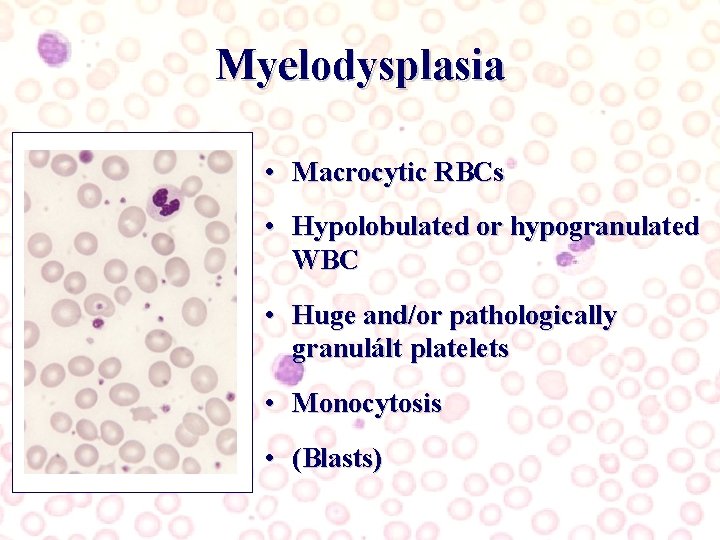
Myelodysplasia • Macrocytic RBCs • Hypolobulated or hypogranulated WBC • Huge and/or pathologically granulált platelets • Monocytosis • (Blasts)
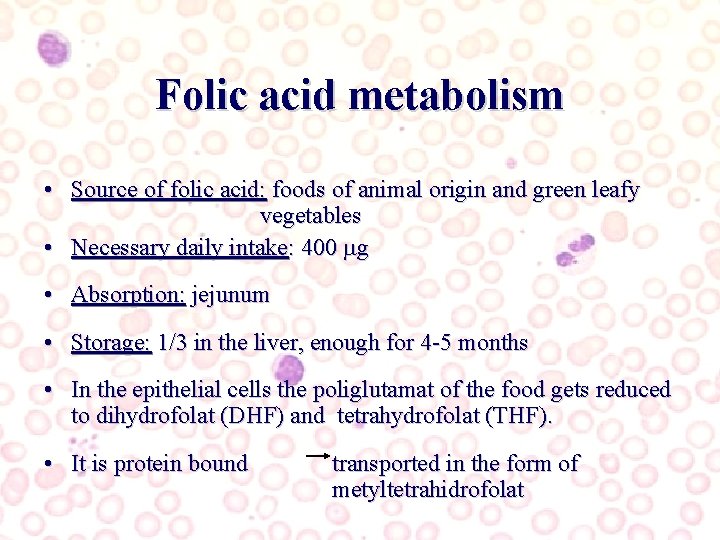
Folic acid metabolism • Source of folic acid: foods of animal origin and green leafy vegetables • Necessary daily intake: 400 g • Absorption: jejunum • Storage: 1/3 in the liver, enough for 4 -5 months • In the epithelial cells the poliglutamat of the food gets reduced to dihydrofolat (DHF) and tetrahydrofolat (THF). • It is protein bound transported in the form of metyltetrahidrofolat
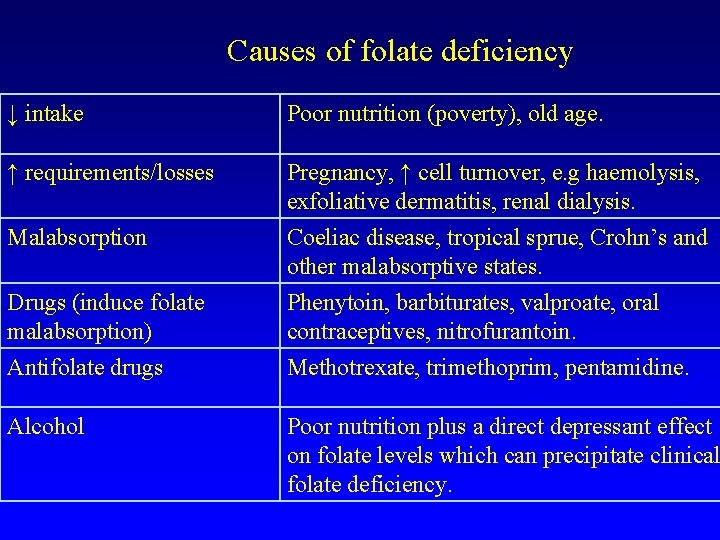
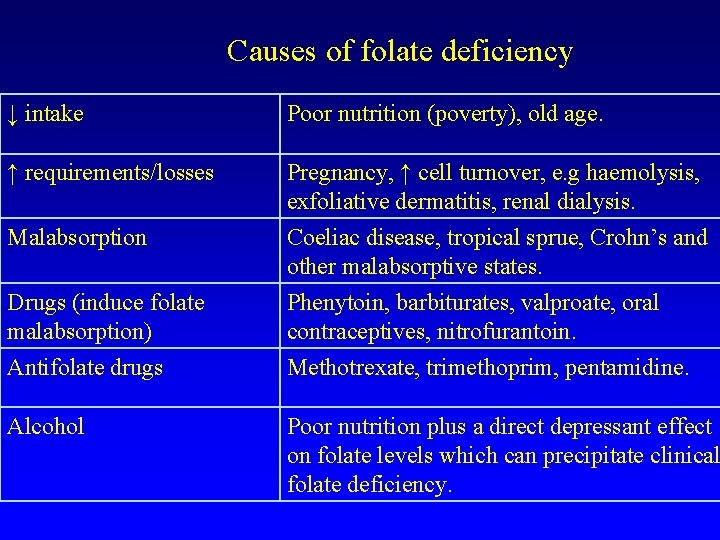
Causes of folate deficiency ↓ intake Poor nutrition (poverty), old age. ↑ requirements/losses Pregnancy, ↑ cell turnover, e. g haemolysis, exfoliative dermatitis, renal dialysis. Malabsorption Coeliac disease, tropical sprue, Crohn’s and other malabsorptive states. Drugs (induce folate malabsorption) Antifolate drugs Phenytoin, barbiturates, valproate, oral contraceptives, nitrofurantoin. Methotrexate, trimethoprim, pentamidine. Alcohol Poor nutrition plus a direct depressant effect on folate levels which can precipitate clinical folate deficiency.
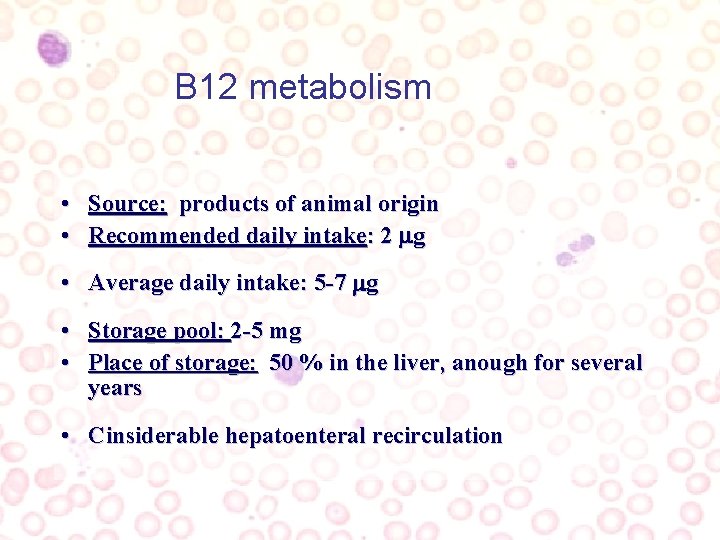
B 12 metabolism • Source: products of animal origin • Recommended daily intake: 2 g • Average daily intake: 5 -7 g • Storage pool: 2 -5 mg • Place of storage: 50 % in the liver, anough for several years • Cinsiderable hepatoenteral recirculation
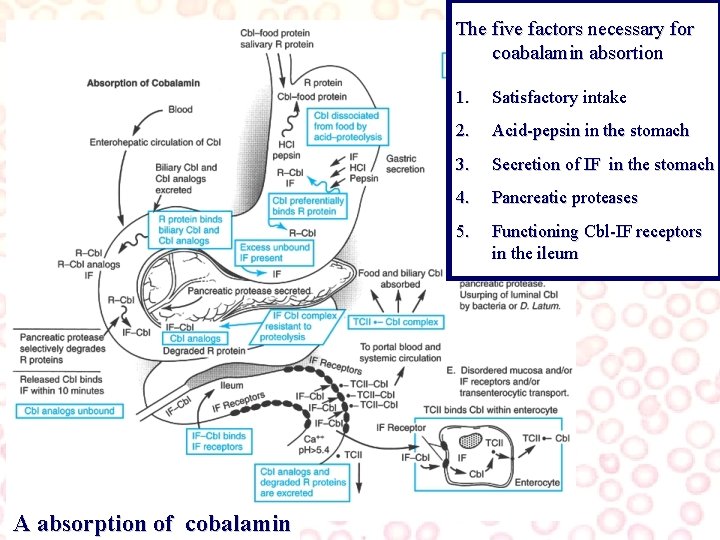
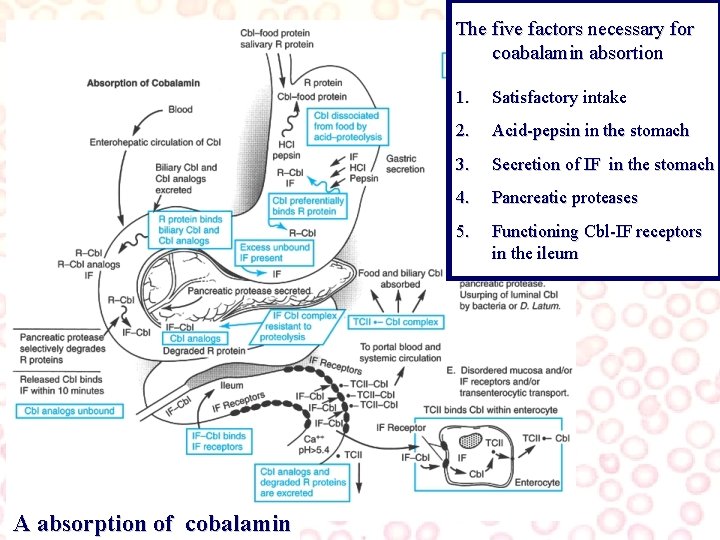
The five factors necessary for coabalamin absortion A absorption of cobalamin 1. Satisfactory intake 2. Acid-pepsin in the stomach 3. Secretion of IF in the stomach 4. Pancreatic proteases 5. Functioning Cbl-IF receptors in the ileum

Causes of B 12 deficiency PERNICIOUS ANAEMIA Commonest, due to autoimmune gastric atrophy resulting in loss of intrinsic factor production required for absorption of B 12. Often associated with other atoimmune problems. Following total gastrectomy Ileal disease May develop after major partial gastrectomy. Blind loop syndromes E. g. diverticulae or localised inflammatory bowel changes allowing bacterial overgrowth which then competes for available B 12. Malabsorptive disorders Tropical sprue, coeliac disease. Fish tapeworm Diphyllobothrium latum. Dietary deficiency Vegans. Resection of ileum, Crohn’s disease.
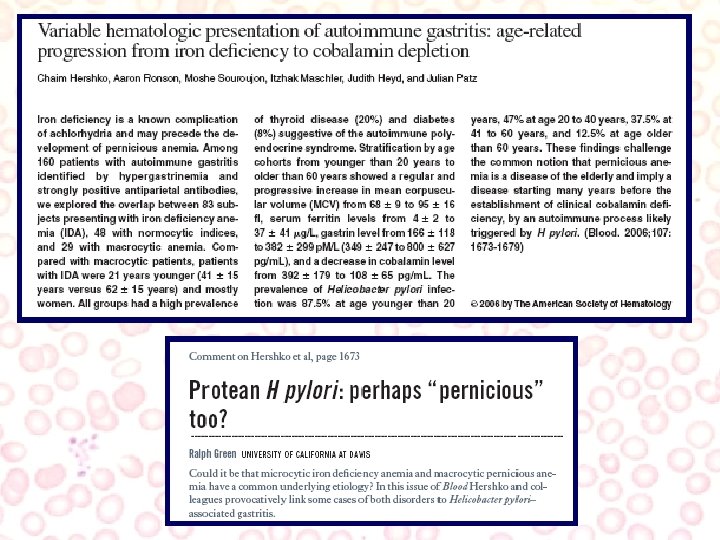
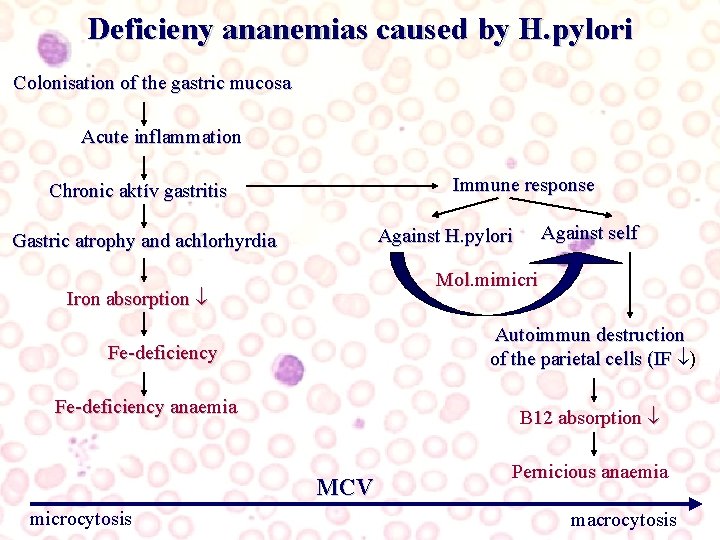
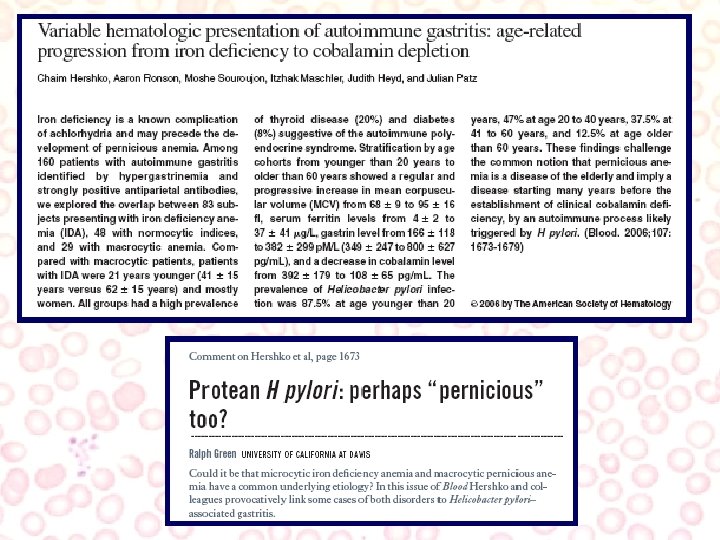
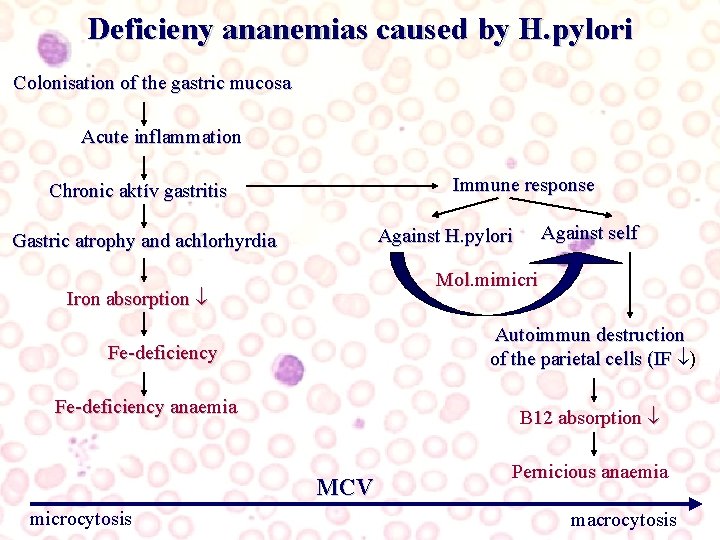
Deficieny ananemias caused by H. pylori Colonisation of the gastric mucosa Acute inflammation Immune response Chronic aktív gastritis Mol. mimicri Iron absorption Autoimmun destruction of the parietal cells (IF ) Fe-deficiency anaemia B 12 absorption MCV microcytosis Against self Against H. pylori Gastric atrophy and achlorhyrdia Pernicious anaemia macrocytosis
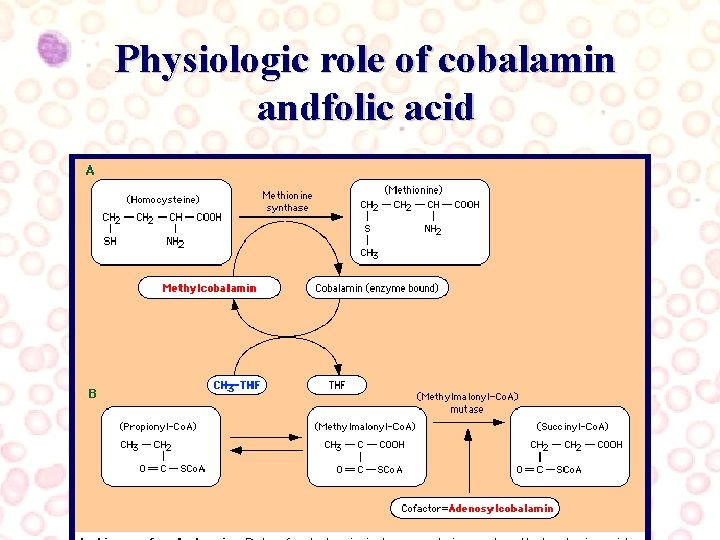
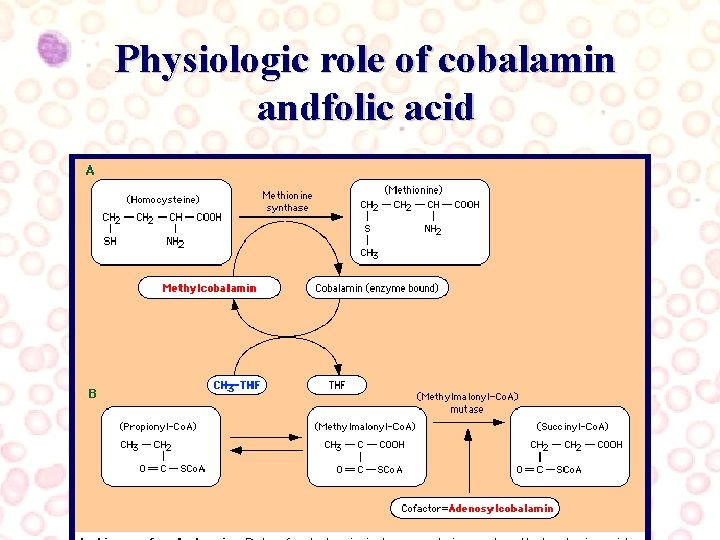
Physiologic role of cobalamin andfolic acid
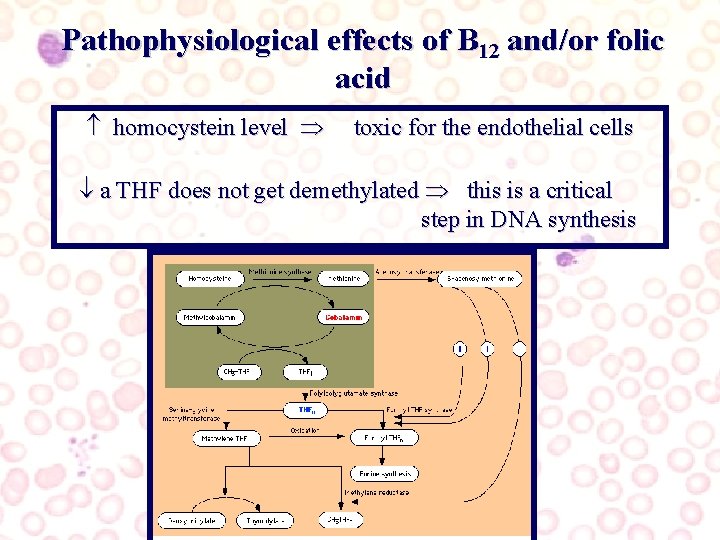
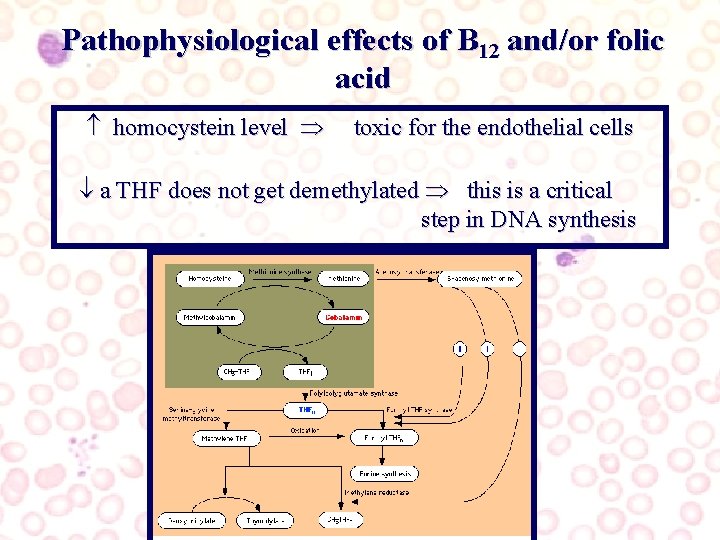
Pathophysiological effects of B 12 and/or folic acid homocystein level toxic for the endothelial cells a THF does not get demethylated this is a critical step in DNA synthesis
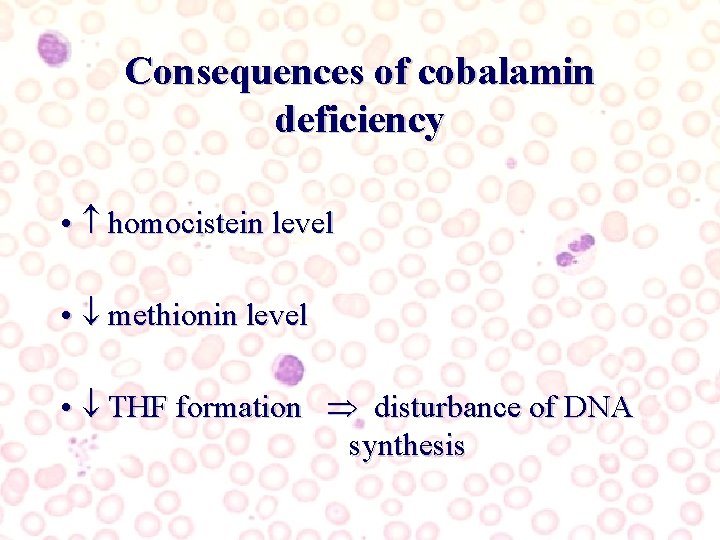
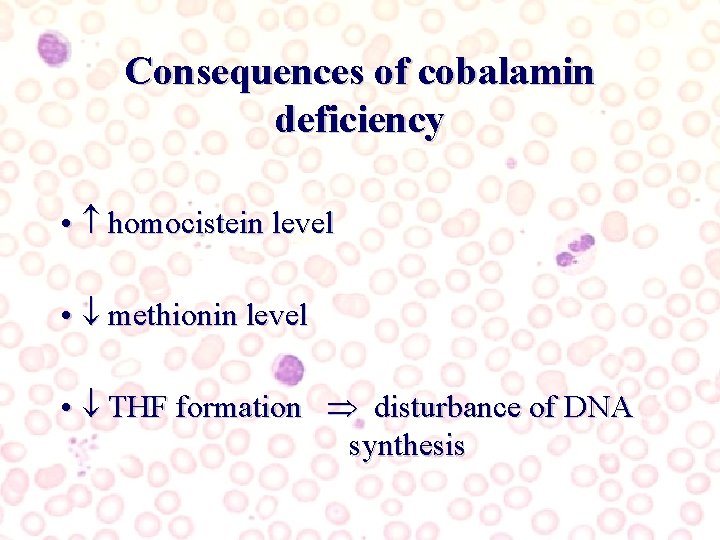
Consequences of cobalamin deficiency • homocistein level • methionin level • THF formation disturbance of DNA synthesis
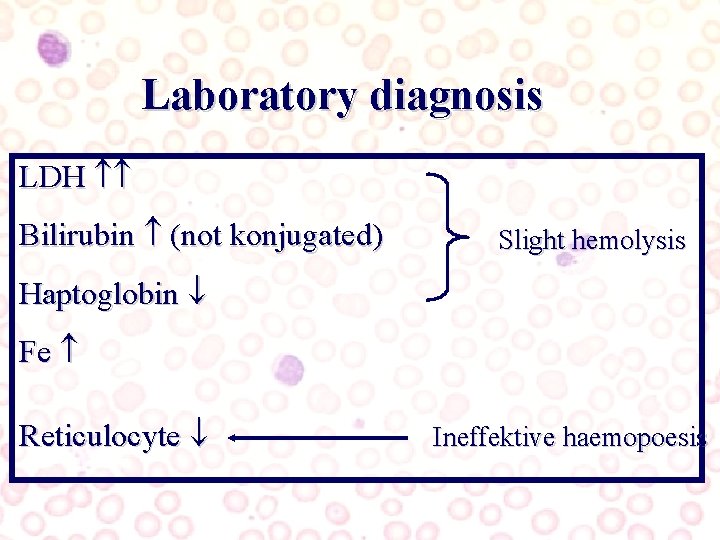
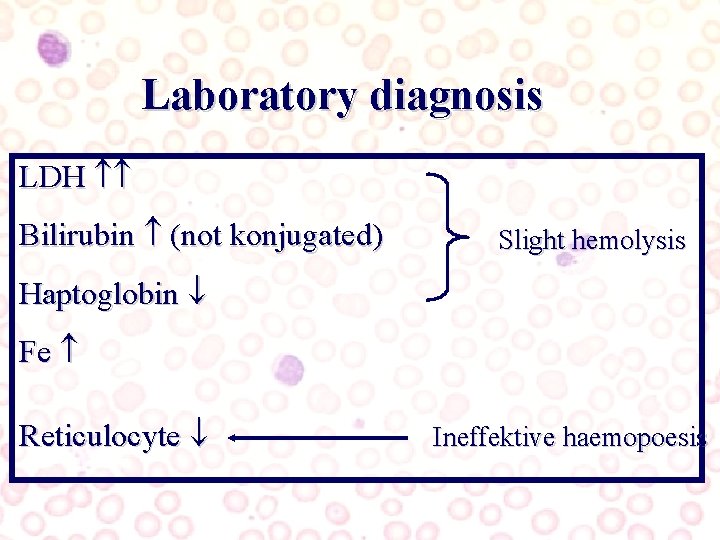
Laboratory diagnosis LDH Bilirubin (not konjugated) Slight hemolysis Haptoglobin Fe Reticulocyte Ineffektive haemopoesis
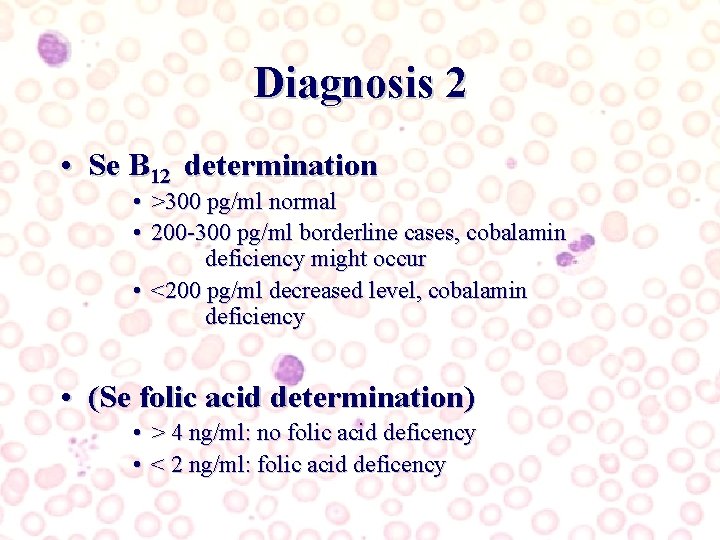
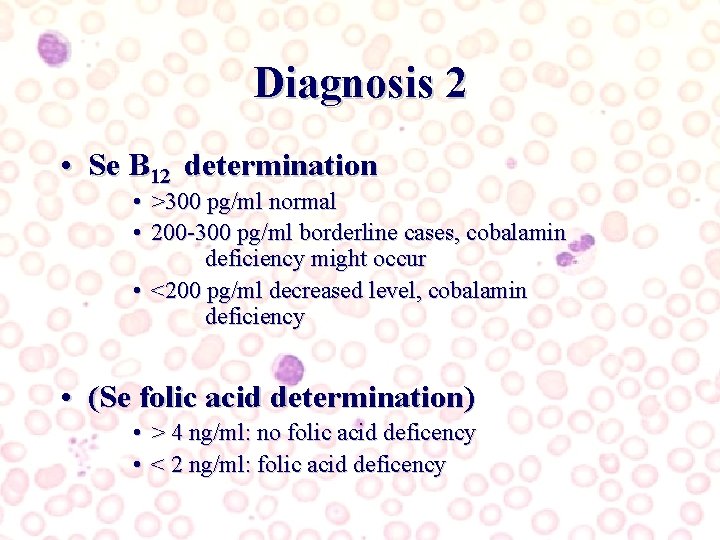
Diagnosis 2 • Se B 12 determination • >300 pg/ml normal • 200 -300 pg/ml borderline cases, cobalamin deficiency might occur • <200 pg/ml decreased level, cobalamin deficiency • (Se folic acid determination) • > 4 ng/ml: no folic acid deficency • < 2 ng/ml: folic acid deficency
Diagnosis 3 B 12 szint if no antibodies to IF present (Schilling teszt)
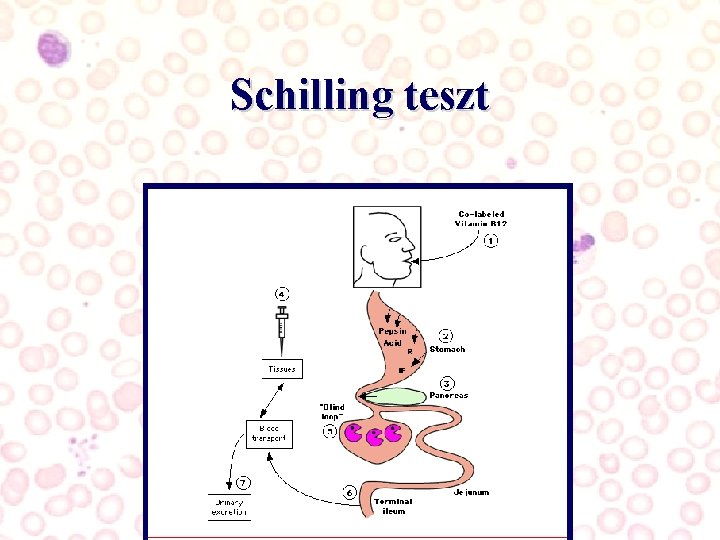
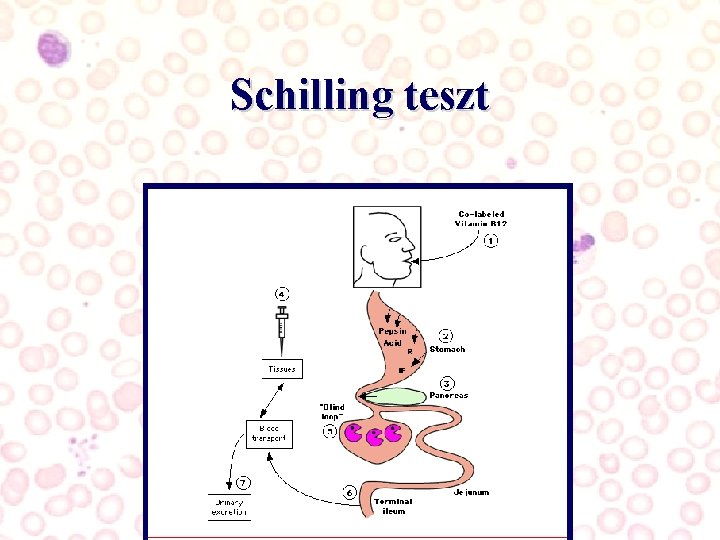
Schilling teszt

Diagnózis 4 • (determination of metilmalonate and homocistein in serum) • (multistep Schilling test)
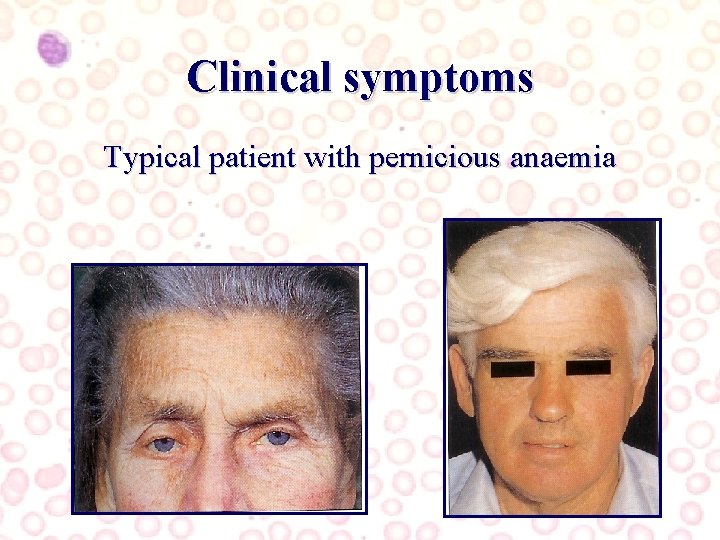
Clinical symptoms Typical patient with pernicious anaemia

Clinical symptoms Cobalamin deficiency causes symptoms after several years Might occur in young people as well, usually associated with other autoimmune disorders(vitiligo, alopecia, autoimmun poliglandular insuff type 2: + Hashimoto thyreoiditis, Addison-disease) Folic acid deficiency manifestation after 4 -5 months

Clinical symptoms Hard to characterise neurological symptoms might be the earliest or only finding!!!! Symmetric, mainly lower extremity neuropathy, paresthesia, ataxia, weakness, spasticity Patom : degeneration of the posterior and oldalsó gerincvelői kötegek Disturbances of memory, demencia, irritability, personality disturbances Patom: CNS and perpheral nevous system axon degeneration

Clinical symptoms Impairment of cells with quick metabolism – Glossitis – Malabsorption – Vaginal atrophy – Frequent cystitis
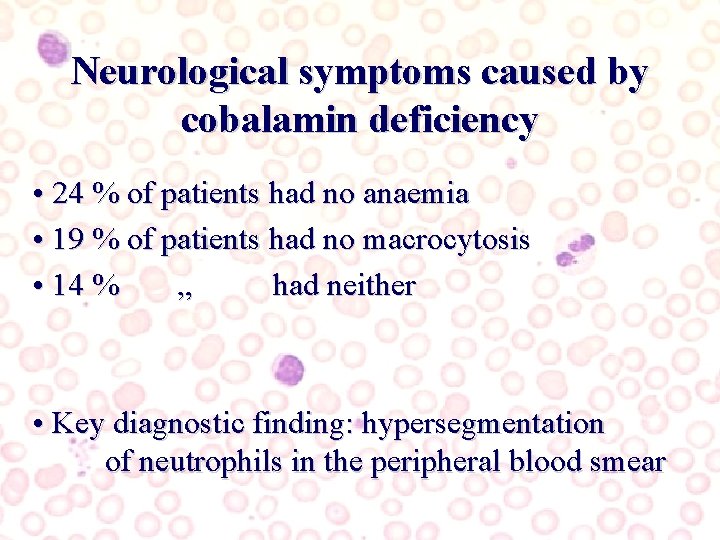
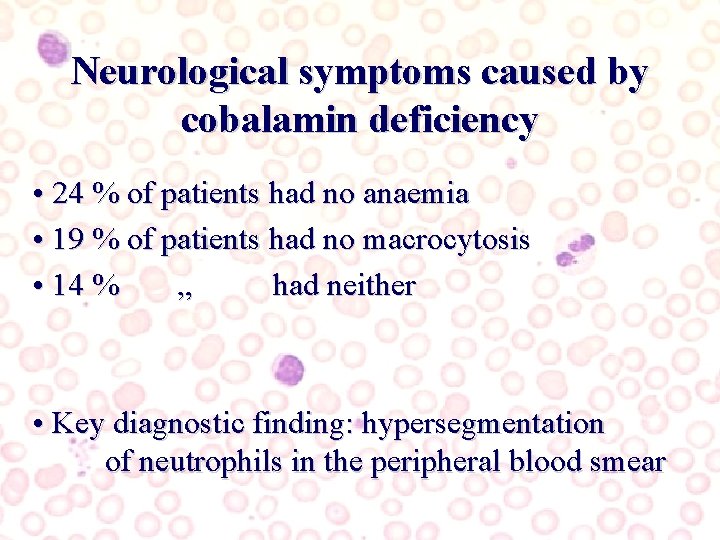
Neurological symptoms caused by cobalamin deficiency • 24 % of patients had no anaemia • 19 % of patients had no macrocytosis • 14 % „ had neither • Key diagnostic finding: hypersegmentation of neutrophils in the peripheral blood smear

Miért van neuropathia B 12 hiányban? • Propionil-Ko. A metilmalonil-Ko. A szukcinil Ko. A • Metionin hiány • toxikus NO gáz hatására neuropathia alakul ki (metionin szintáz gátlása révén) • metionin adása hatásos kobalaminhiány állatkísérleti modelljében • ? ? ?
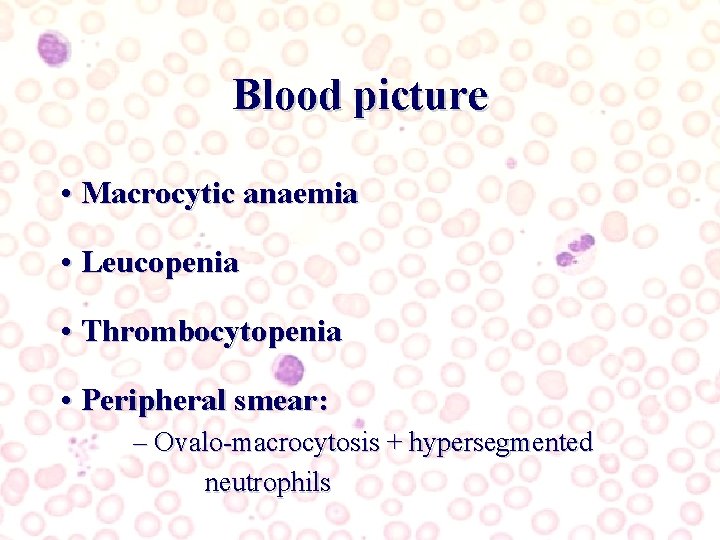
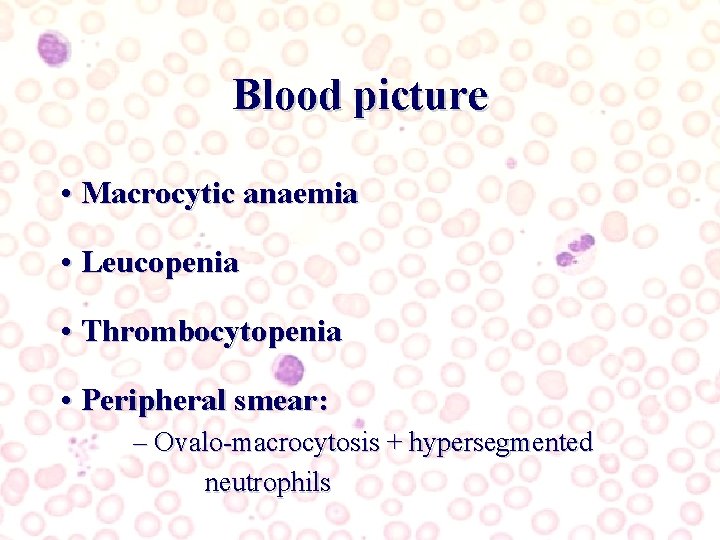
Blood picture • Macrocytic anaemia • Leucopenia • Thrombocytopenia • Peripheral smear: – Ovalo-macrocytosis + hypersegmented neutrophils

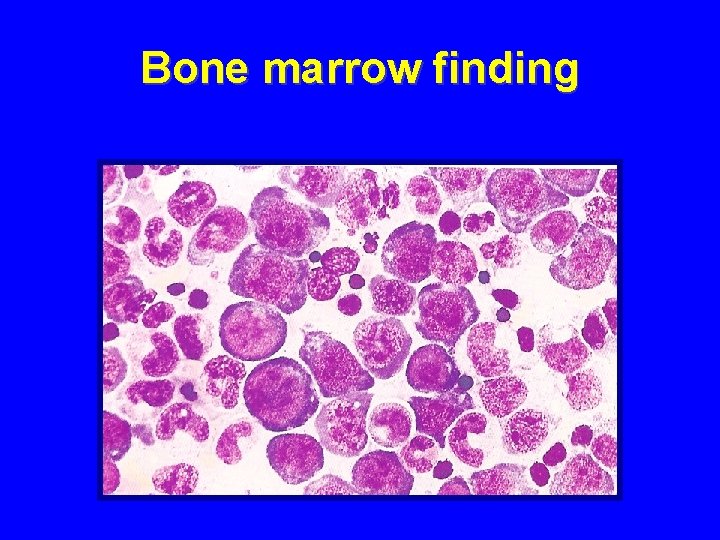
Bone marrow • Highly hypercellular • Megaloblastic erythroid hyperplasia – Mauration asynchrony of the nucleus and the cytoplasm – Nuclear anomalies: karyorrhexis, two nuclei stb • Huge metamyelocytes, stabs
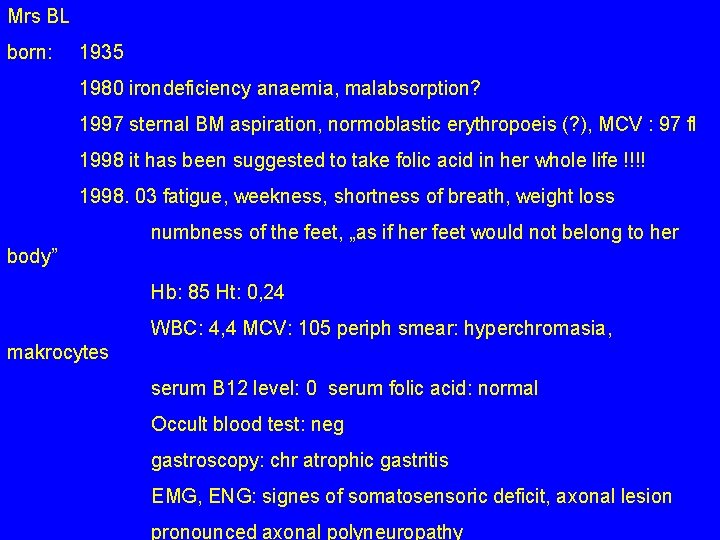
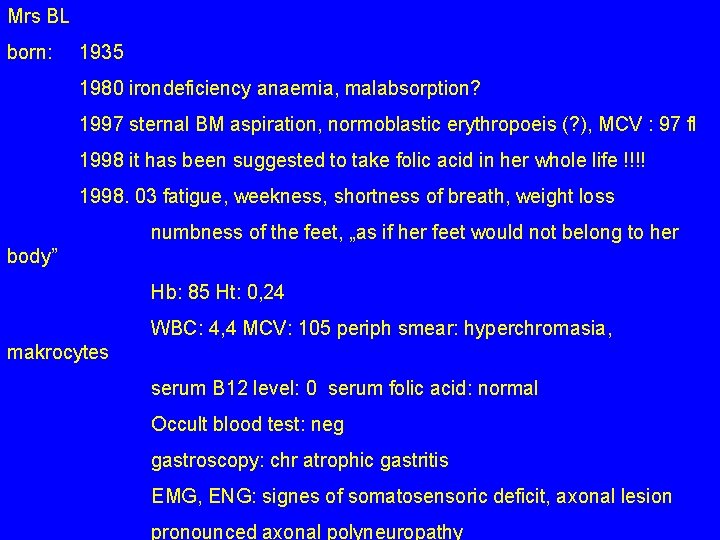
Mrs BL born: 1935 1980 irondeficiency anaemia, malabsorption? 1997 sternal BM aspiration, normoblastic erythropoeis (? ), MCV : 97 fl 1998 it has been suggested to take folic acid in her whole life !!!! 1998. 03 fatigue, weekness, shortness of breath, weight loss numbness of the feet, „as if her feet would not belong to her body” Hb: 85 Ht: 0, 24 WBC: 4, 4 MCV: 105 periph smear: hyperchromasia, makrocytes serum B 12 level: 0 serum folic acid: normal Occult blood test: neg gastroscopy: chr atrophic gastritis EMG, ENG: signes of somatosensoric deficit, axonal lesion pronounced axonal polyneuropathy

Mrs BL: 1998 Schilling test 1, 2% Correction of Schilling test with intrinsic factor: 10, 3 % treatment : monthly B 12 injections im. 1000 gamma Her sister: Mrs HL born: 1938 since many years her mouth, her tongue was painful and felt like burning. Hb: 130 g /L Ht: 39, WBC, PLT: norm BUT: Schilling test 2, 2 % !!!!! B 12 injection immediately effective, all symptoms ceased permanently !!!! treatment : monthly B 12 injections im. 100 gamma

Bone marrow finding
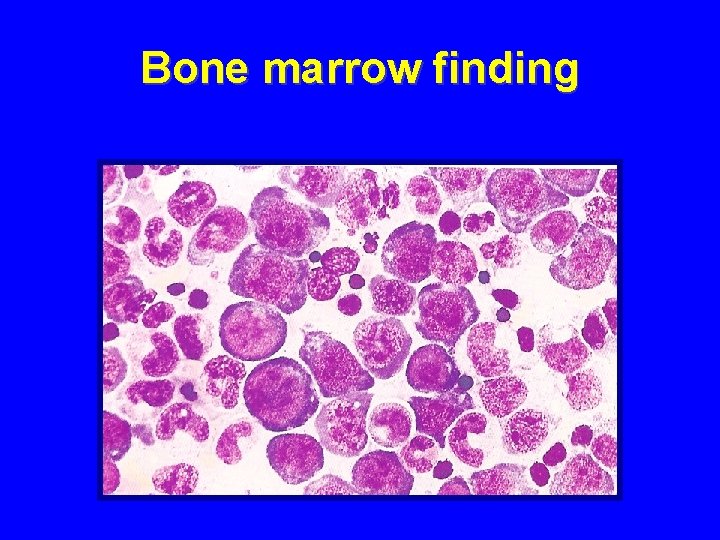
Bone marrow finding

Bone marrow finding

Bone marrow finding

Bone marrow finding

Bone marrow finding

Bone marrow finding
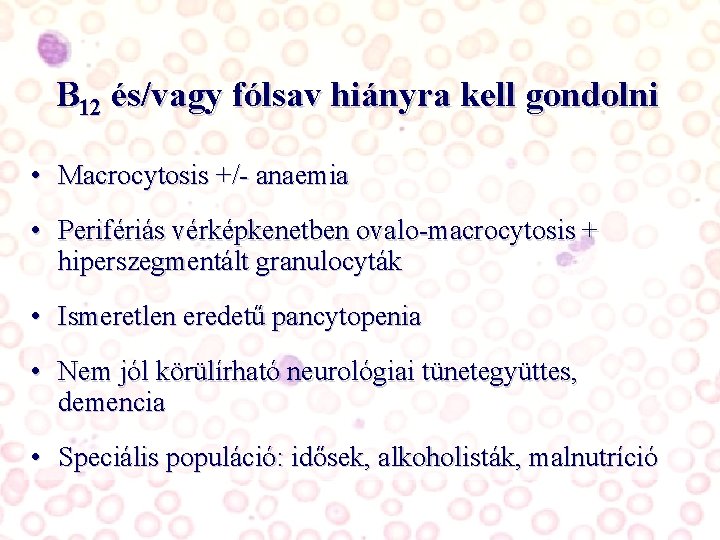
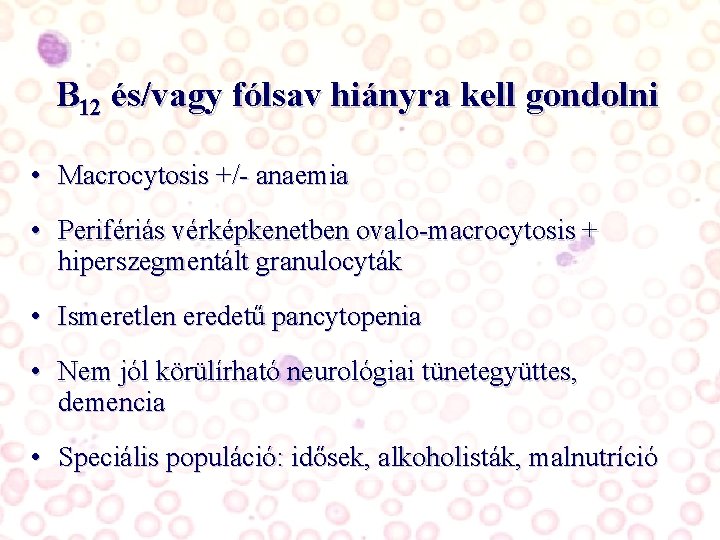
B 12 és/vagy fólsav hiányra kell gondolni • Macrocytosis +/- anaemia • Perifériás vérképkenetben ovalo-macrocytosis + hiperszegmentált granulocyták • Ismeretlen eredetű pancytopenia • Nem jól körülírható neurológiai tünetegyüttes, demencia • Speciális populáció: idősek, alkoholisták, malnutríció
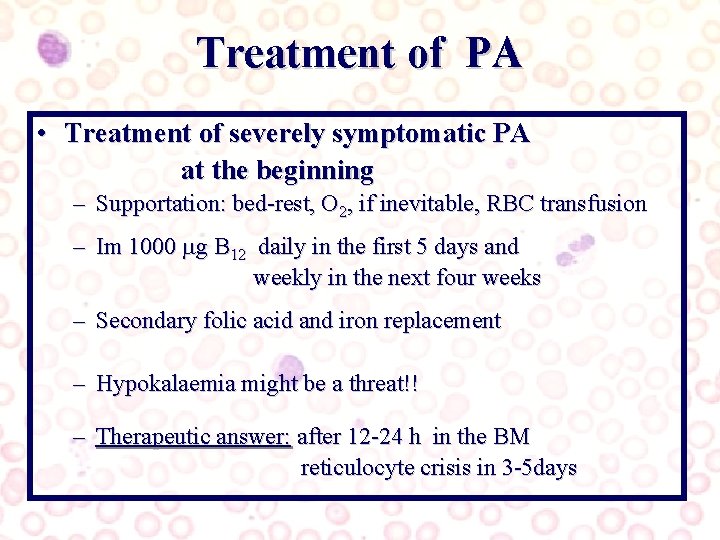
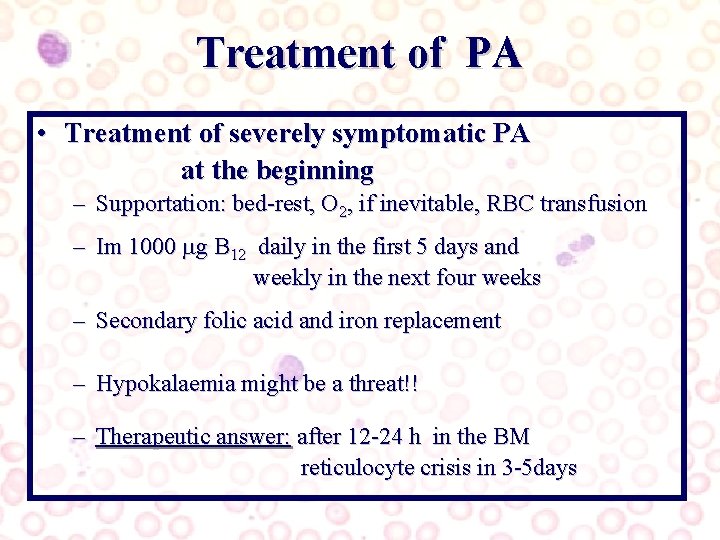
Treatment of PA • Treatment of severely symptomatic PA at the beginning – Supportation: bed-rest, O 2, if inevitable, RBC transfusion – Im 1000 g B 12 daily in the first 5 days and weekly in the next four weeks – Secondary folic acid and iron replacement – Hypokalaemia might be a threat!! – Therapeutic answer: after 12 -24 h in the BM reticulocyte crisis in 3 -5 days
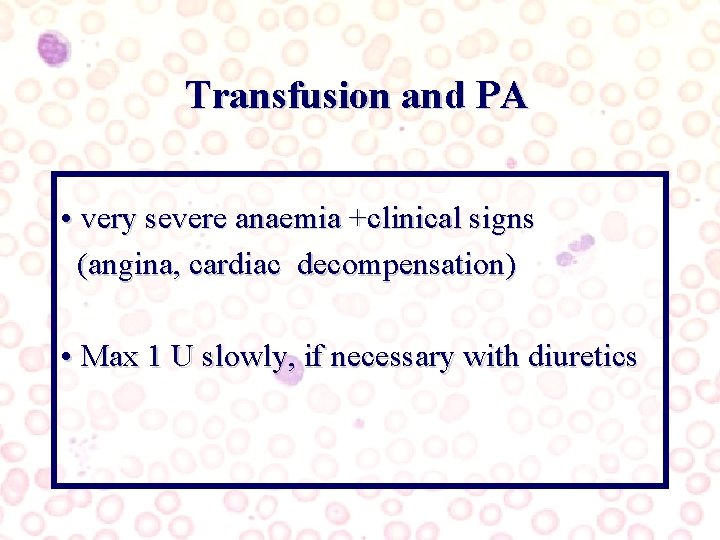
Transfusion and PA • very severe anaemia +clinical signs (angina, cardiac decompensation) • Max 1 U slowly, if necessary with diuretics
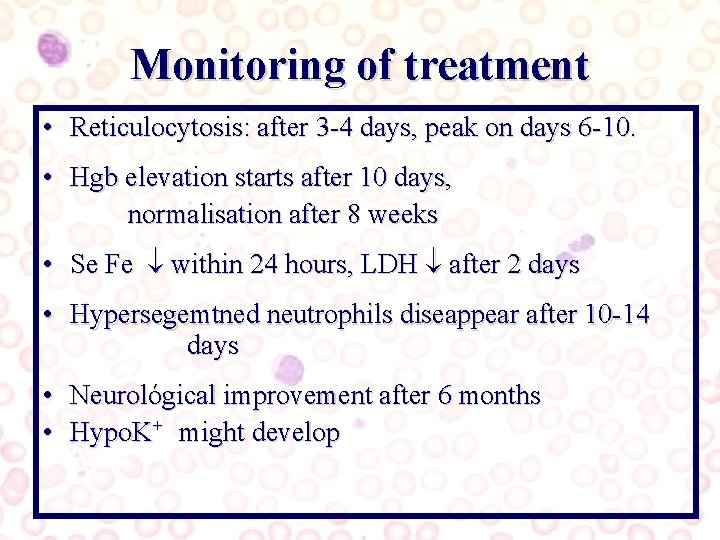
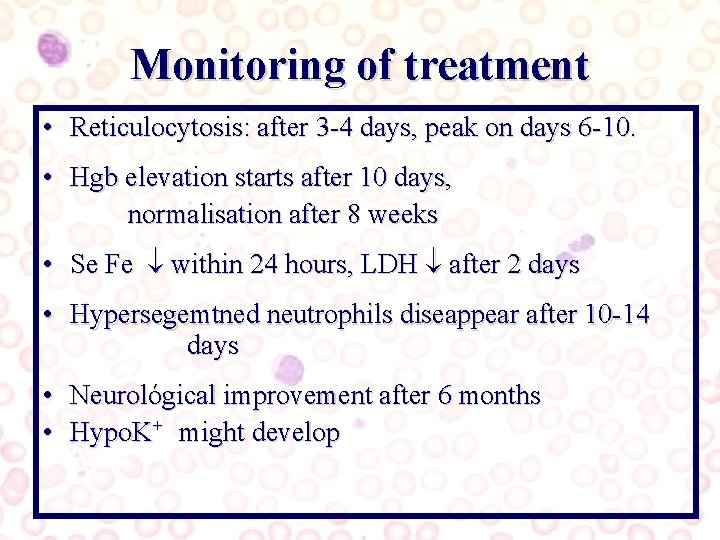
Monitoring of treatment • Reticulocytosis: after 3 -4 days, peak on days 6 -10. • Hgb elevation starts after 10 days, normalisation after 8 weeks • Se Fe within 24 hours, LDH after 2 days • Hypersegemtned neutrophils diseappear after 10 -14 days • Neurológical improvement after 6 months • Hypo. K+ might develop
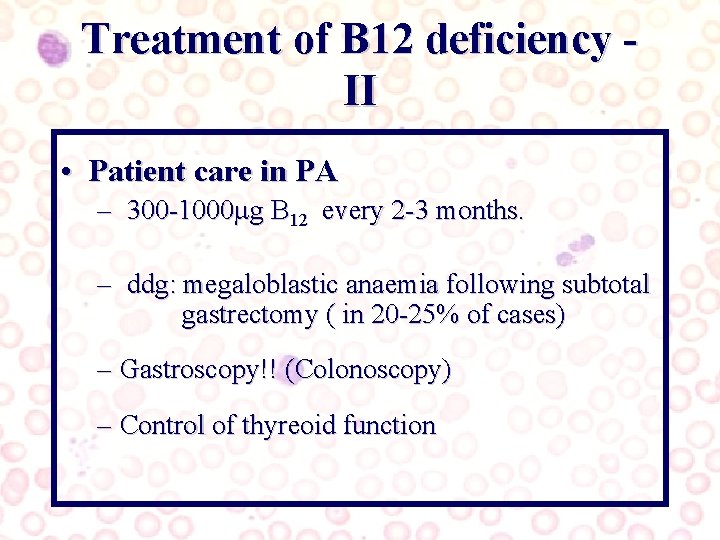
Treatment of B 12 deficiency II • Patient care in PA – 300 -1000 g B 12 every 2 -3 months. – ddg: megaloblastic anaemia following subtotal gastrectomy ( in 20 -25% of cases) – Gastroscopy!! (Colonoscopy) – Control of thyreoid function
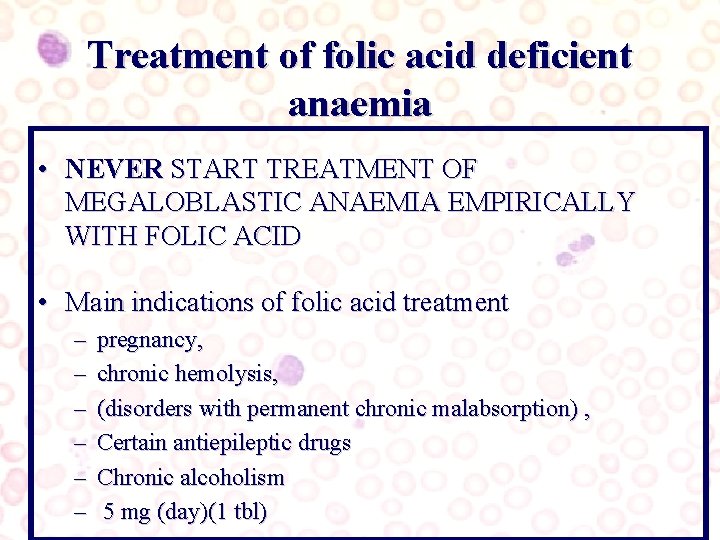
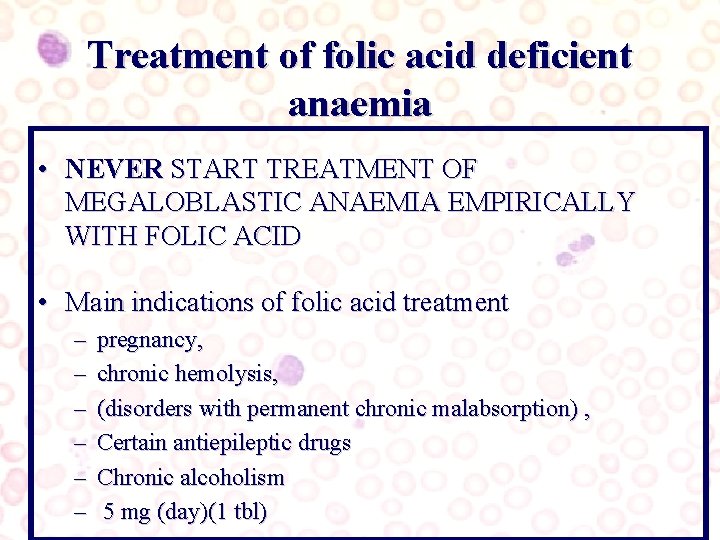
Treatment of folic acid deficient anaemia • NEVER START TREATMENT OF MEGALOBLASTIC ANAEMIA EMPIRICALLY WITH FOLIC ACID • Main indications of folic acid treatment – – – pregnancy, chronic hemolysis, (disorders with permanent chronic malabsorption) , Certain antiepileptic drugs Chronic alcoholism 5 mg (day)(1 tbl)
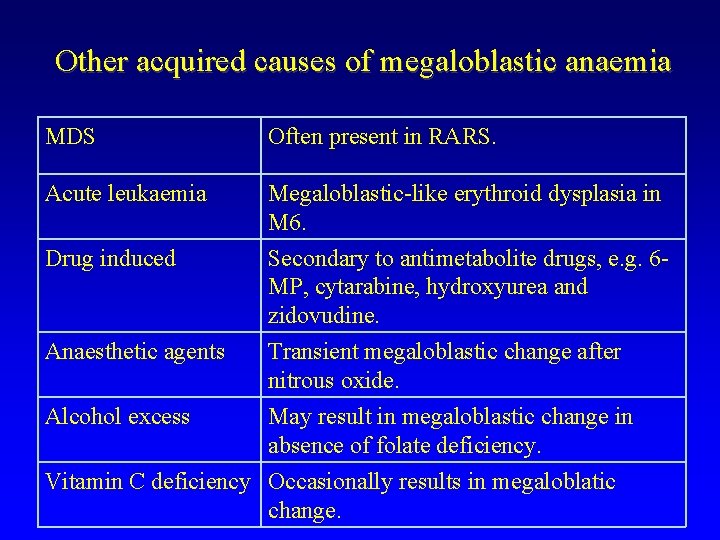
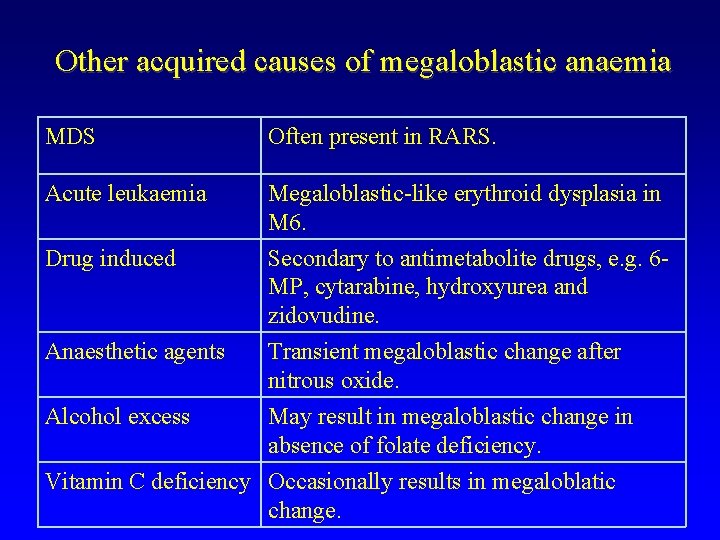
Other acquired causes of megaloblastic anaemia MDS Often present in RARS. Acute leukaemia Megaloblastic-like erythroid dysplasia in M 6. Drug induced Secondary to antimetabolite drugs, e. g. 6 MP, cytarabine, hydroxyurea and zidovudine. Anaesthetic agents Transient megaloblastic change after nitrous oxide. Alcohol excess May result in megaloblastic change in absence of folate deficiency. Vitamin C deficiency Occasionally results in megaloblatic change.


„Felhőkép segítség” Anaemia perniciosa Normális kép

„Felhőkép segítség” CDA RARS