Nursing Care of the Client Sexually Transmitted Diseases

































![Herpes genitalis (herpes simplex virus, type 2 [HSV 2]) n Maternal effects – Primary Herpes genitalis (herpes simplex virus, type 2 [HSV 2]) n Maternal effects – Primary](https://slidetodoc.com/presentation_image/3b6cf42f332a9e68072b58a19c84a299/image-110.jpg)
- Slides: 111
Nursing Care of the Client: Sexually Transmitted Diseases (STDs)
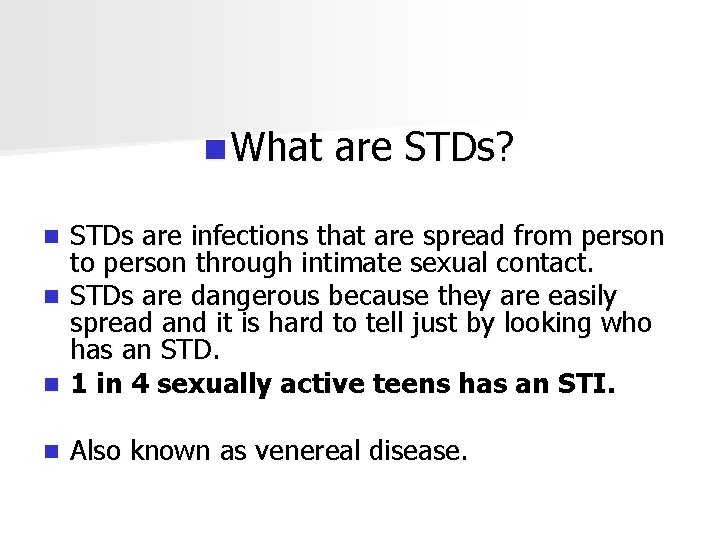
n What are STDs? STDs are infections that are spread from person to person through intimate sexual contact. n STDs are dangerous because they are easily spread and it is hard to tell just by looking who has an STD. n 1 in 4 sexually active teens has an STI. n n Also known as venereal disease.
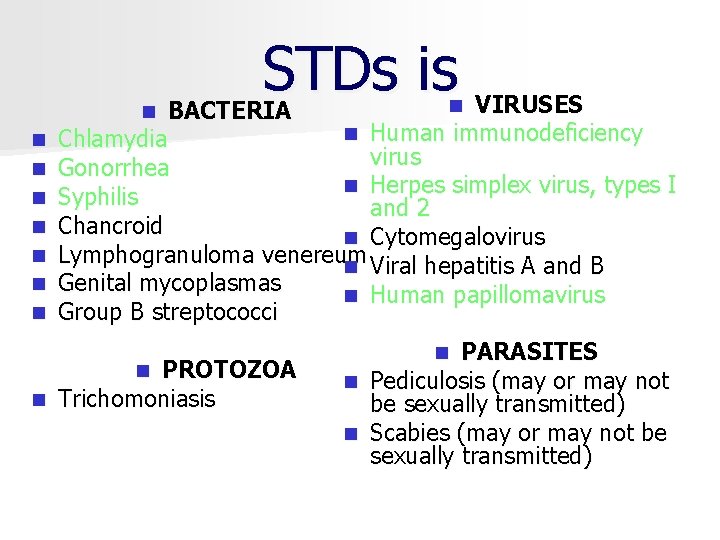
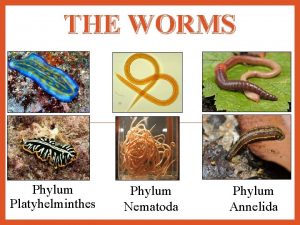
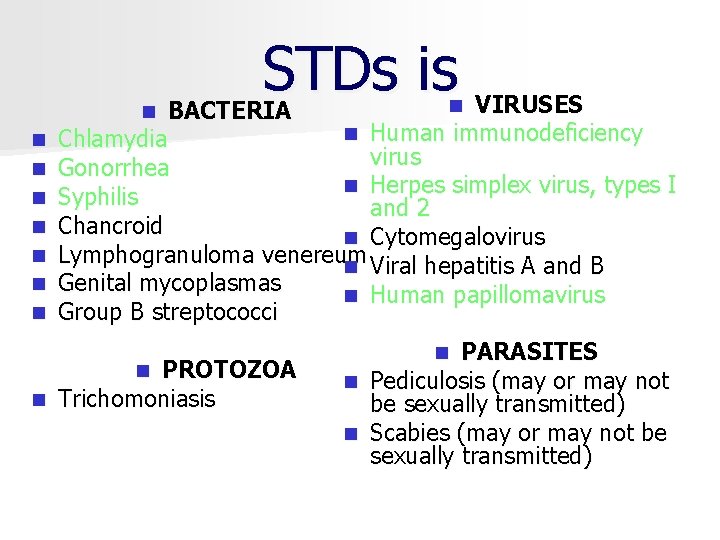
n VIRUSES BACTERIA n Human immunodeficiency Chlamydia virus Gonorrhea n Herpes simplex virus, types I Syphilis and 2 Chancroid n Cytomegalovirus Lymphogranuloma venereum n Viral hepatitis A and B Genital mycoplasmas n Human papillomavirus Group B streptococci n n n n STDs is PROTOZOA n Trichomoniasis n PARASITES n Pediculosis (may or may not be sexually transmitted) n Scabies (may or may not be sexually transmitted) n

PREVENTION n Preventing infection (primary) n Prompt diagnosis and treatment of current infections (secondary)

Prevention Change of behavior n Prevention counseling: n – Identification of risk factors (sexual history and behavior, drug related risk, blood related risk) – Techniques for effective counseling (using open ended questions, using understandable language, and reassuring the woman that treatment will be provided regardless of consideration such as ability to pay, language spoken, or lifestyle)

Prevention n Safer sex practices – Knowledge of partner – Condom use § Male compliance § Negotiation of use § Storage – Abstinence of activities with fluid exchange
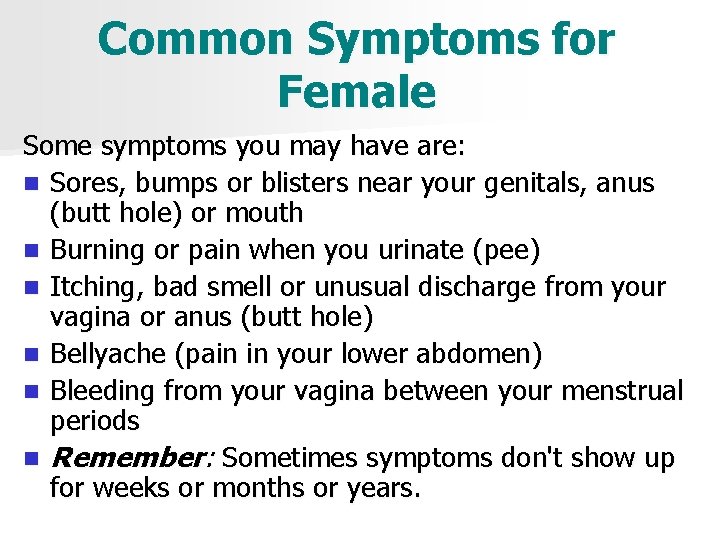
Common Symptoms for Female Some symptoms you may have are: n Sores, bumps or blisters near your genitals, anus (butt hole) or mouth n Burning or pain when you urinate (pee) n Itching, bad smell or unusual discharge from your vagina or anus (butt hole) n Bellyache (pain in your lower abdomen) n Bleeding from your vagina between your menstrual periods n Remember: Sometimes symptoms don't show up for weeks or months or years.

Common Symptoms for Male Some symptoms you may have are: n Sores, bumps or blisters near your genitals, anus (butt hole) or mouth n Burning or pain when you urinate (pee) n Drip or discharge from your penis n Itching, pain or discharge from your anus (butt hole) n Remember: Sometimes symptoms don't show up for weeks or months.
Bacterial Sexually Transmitted Infections

Chlamydia trachomatis

Chlamydia trachomatis – Most common and fastest spreading STI § Infections are often silent and highly destructive § Difficult to diagnose
Chlamydia trachomatis n Risk factors – – Age (younger than 20 years) Early onset of sexual activity Multiple partners Nonuse of barrier methods of birth control

Chlamydia trachomatis n Transmittal – Genital to genital – Oral to genital – Anal to genital – Vagina to rectum – Mother to newborn Infectivity: people can infect other when they have symptoms & some times when they do not, the partner is infected in approximately 33% of the sexual contacts with an infected partner

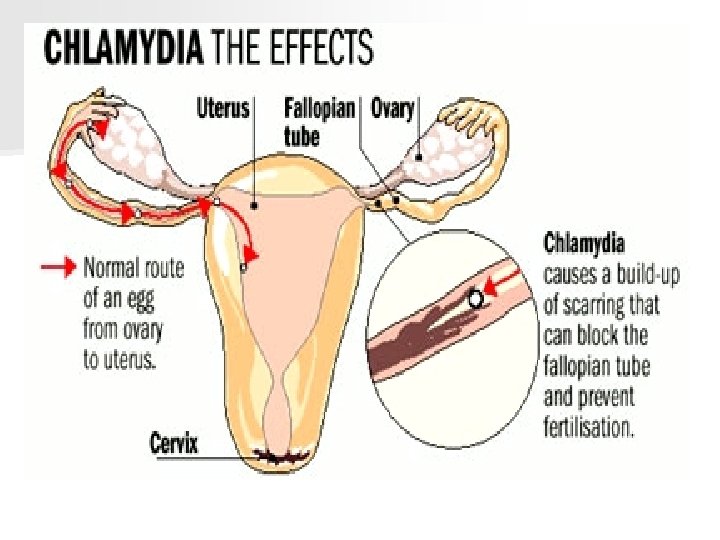
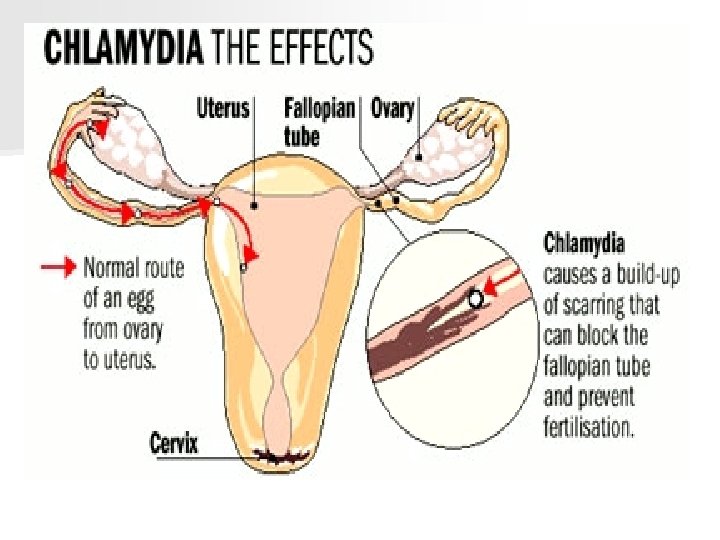
Chlamydia trachomatis n Untreated infectious lead to: – males - inflammation of testicles, infected prostate, infertility – females – acute salpingitis, pelvic inflammatory disease, ectopic pregnancies tubal infertility, cervical ulcaration increase risk of acquiring HIV infections – fetus/newborns – conjunctivitis, pneumonia, death, eye & ear infections

Chlamydia trachomatis n Symptoms: – males 1 25% show no symptoms; watery or milky discharge from penis, burning sensation upon urination: – females 70% show no symptoms; mucoid or purulent vaginal discharge &/or bleeding (postcoital), dysuria, abnormal cramping, abdominal pain, fever, painful urination. – Oral sore throat – Rectal inflammation, itching n Incubation: 1 to 4 weeks
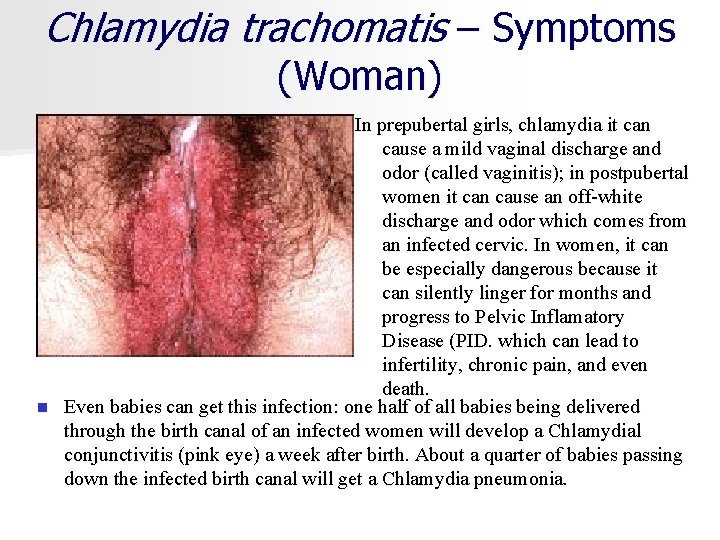
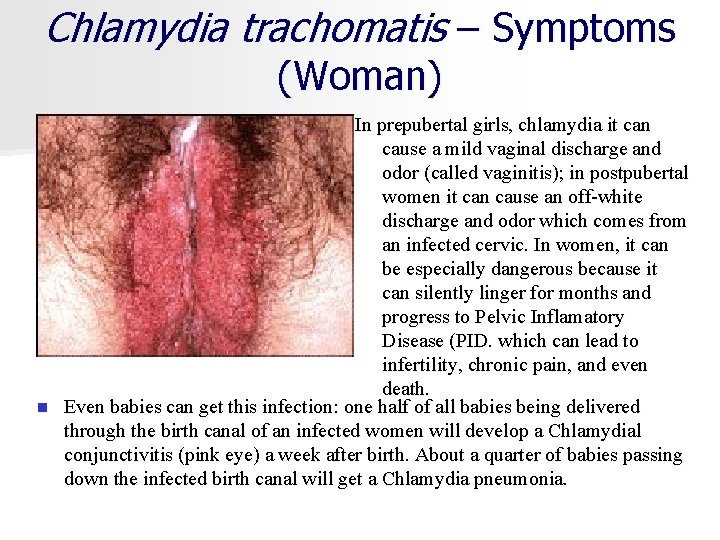
Chlamydia trachomatis – Symptoms (Woman) In prepubertal girls, chlamydia it can cause a mild vaginal discharge and odor (called vaginitis); in postpubertal women it can cause an off-white discharge and odor which comes from an infected cervic. In women, it can be especially dangerous because it can silently linger for months and progress to Pelvic Inflamatory Disease (PID. which can lead to infertility, chronic pain, and even death. n Even babies can get this infection: one half of all babies being delivered through the birth canal of an infected women will develop a Chlamydial conjunctivitis (pink eye) a week after birth. About a quarter of babies passing down the infected birth canal will get a Chlamydia pneumonia.
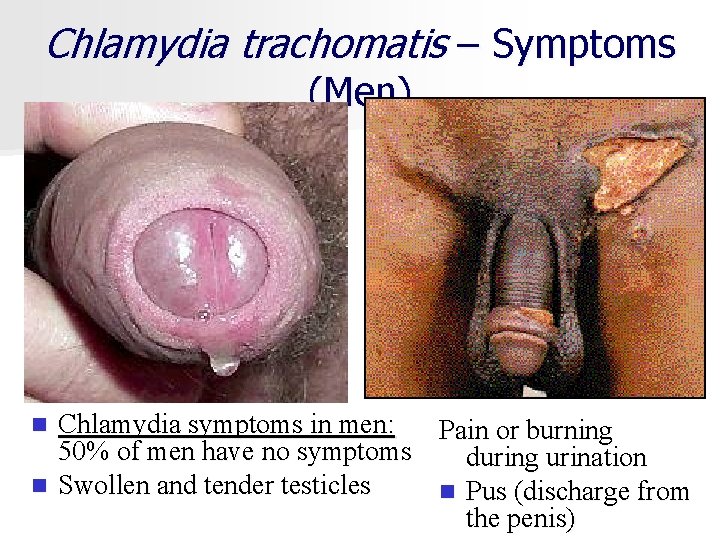
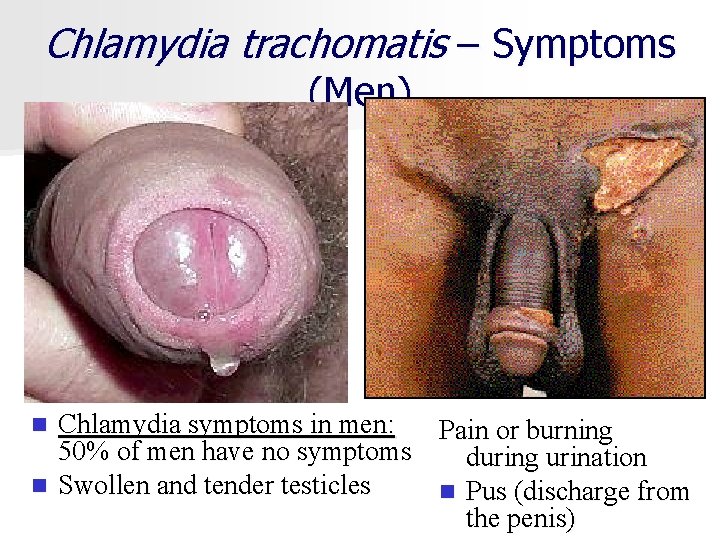
Chlamydia trachomatis – Symptoms (Men) Chlamydia symptoms in men: 50% of men have no symptoms n Swollen and tender testicles n Pain or burning during urination n Pus (discharge from the penis)
Chlamydia trachomatis n Screening – asymptomatic women at high risk in whom infection would otherwise go undetected – sexually active adolescents, – women between ages 20 and 25 years, – women older than 25 years who do not use barrier contraceptives, – women older than 25 years with new or multiple partners. – women with two or more of the risk factors for chlamydia should be cultured. – all pregnant women at the first prenatal visit and in the third trimester (36 weeks) if the woman was positive previously or if she is younger than 25 years or has a new sex partner or multiple sex partners.

Chlamydia trachomatis n Diagnosis is by n Obtain culture – – – culture (expensive and la bor intensive), DNA probe (less expensive but less sensi tivity), enzyme immunoassay (less expensive but less sen sitivity), – nucleic acid amplification (expensive but about 90% sensitivity) – – to remove mucus and discharge from the cervical os. the cervix should be swabbed with cotton or rayon swabs – contains many endocervical (columnar) cells
Chlamydia trachomatis n Treatment: – Doxycycline, 100 mg orally twice a day for 7 days – Azithromycin, 1 g orally once n Pregnant female – Erythromycin base, 500 mg orally qid for 7 days – Amoxicillin, 500 mg orally TID for 7 days
Chlamydia trachomatis n All exposed sexual partners should be treated. n Woman treated with doxycycline or azithromycin do not need to be retested unless symptoms continue. n Women treated with erythromycin may be retested 3 weeks after completing the medication
Gonorrhea
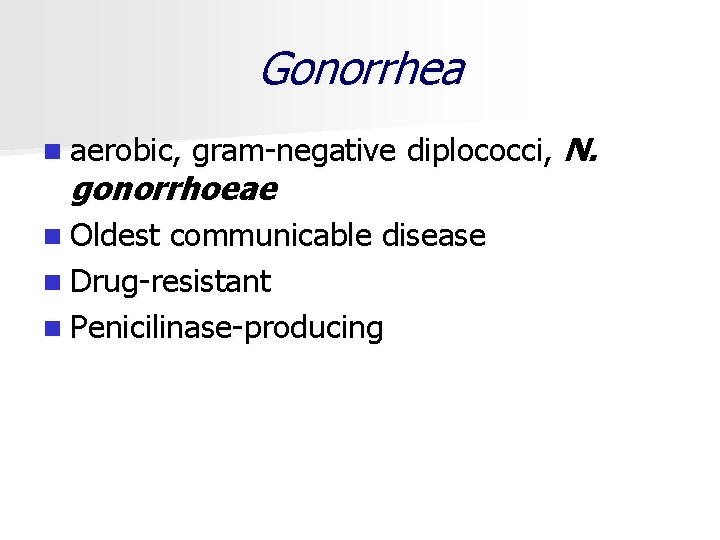
Gonorrhea n aerobic, gram negative diplococci, N. gonorrhoeae n Oldest communicable disease n Drug resistant n Penicilinase producing
Gonorrhea n Transmittal n Incubation: 2 to 7 days n Result – – – Genital to genital Oral to genital Anal to genital Vagina to rectum Mother to newborn – pelvic inflammatory disease (PID) – Infertility – ectopic or tubal pregnancy – blockage of urethra, problems with erection
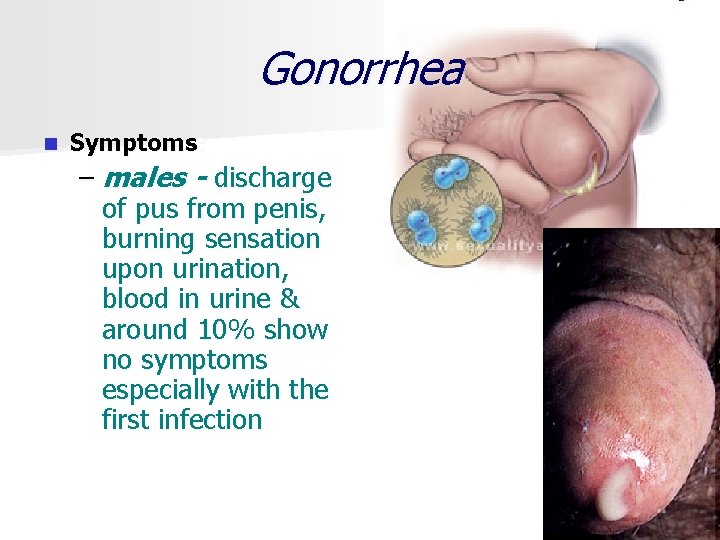
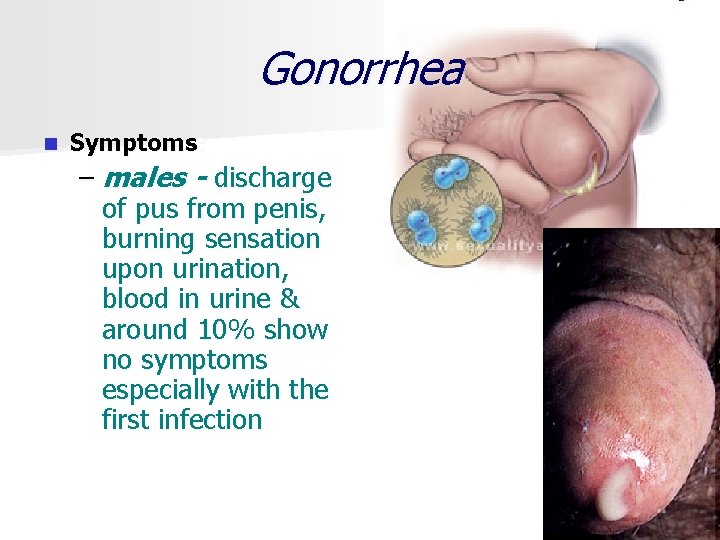
Gonorrhea n Symptoms: – males - discharge of pus from penis, burning sensation upon urination, blood in urine & around 10% show no symptoms especially with the first infection
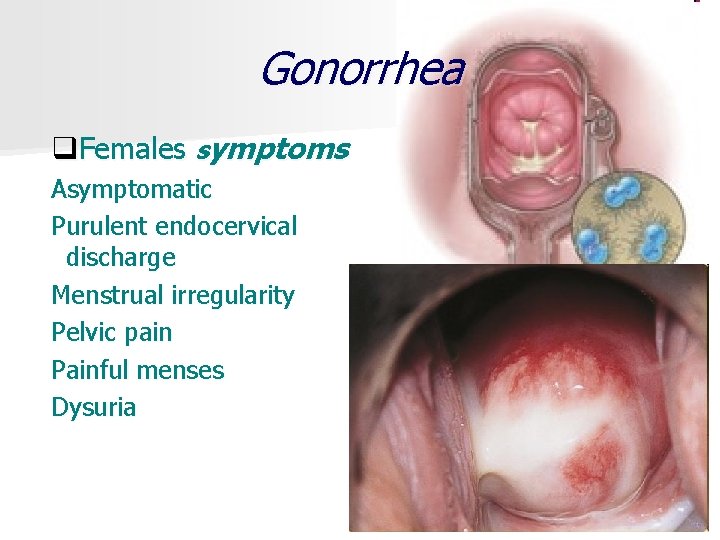
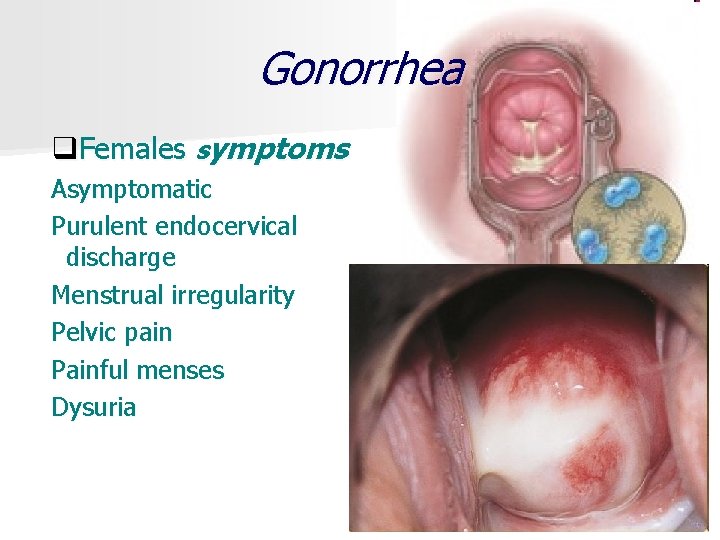
Gonorrhea q. Females symptoms Asymptomatic Purulent endocervical discharge Menstrual irregularity Pelvic pain Painful menses Dysuria
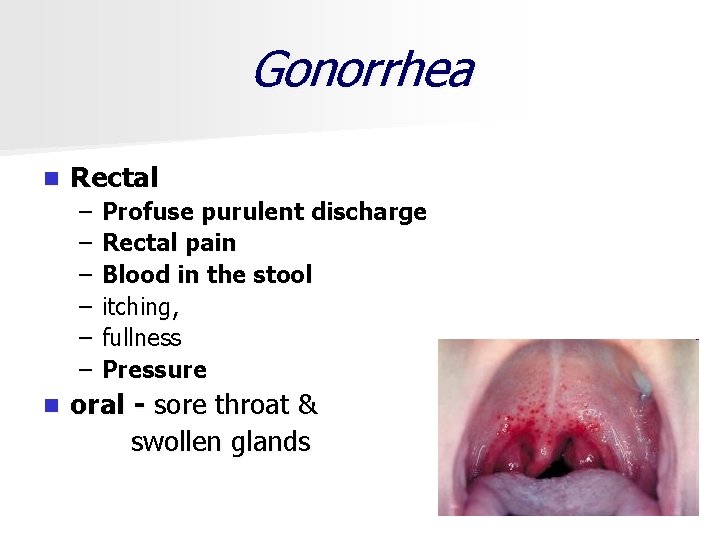
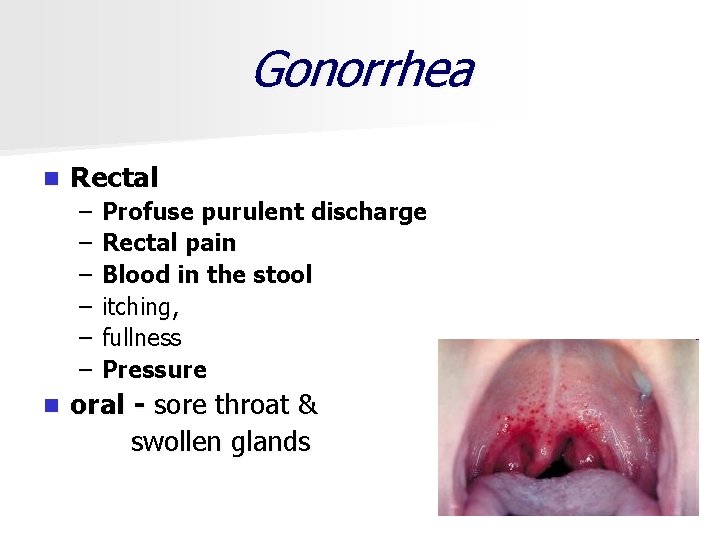
Gonorrhea n Rectal – – – Profuse purulent discharge Rectal pain Blood in the stool itching, fullness Pressure oral - sore throat & swollen glands n

Gonorrhea n Pregnancy § Premature rupture of membranes § Preterm birth § Chorioamnionitis § Neonatal sepsis § Intrauterine growth restriction § Maternal postpartum sepsis

Gonorrhea n Newborn § Ophthalmia neonatorum

Gonorrhea n Screening – – – n All women All pregnant at first prenatal visit Infected oa with risky behaviors – at 36 weeks Diagnosis – Cultures with selective media are considered the gold standard for diagnosis of gonorrhea. – Cultures should be obtained from the endocervix, rectum, and when indicated, the pharynx. – should have a chlamydial culture and serologic test for syphilis
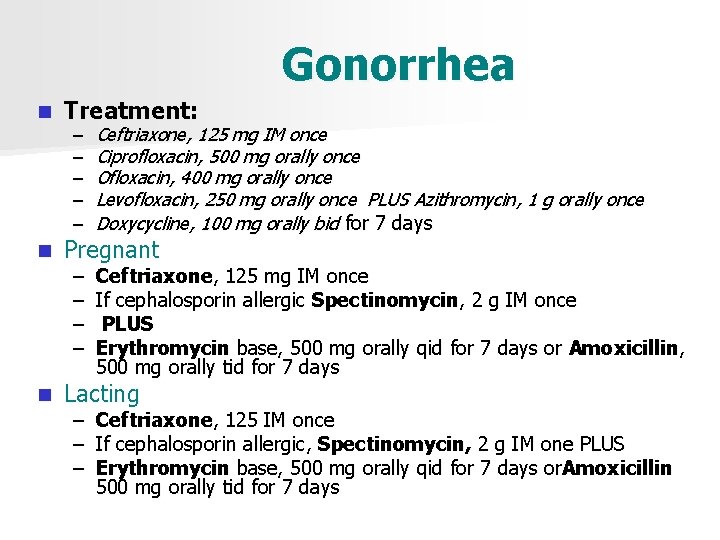
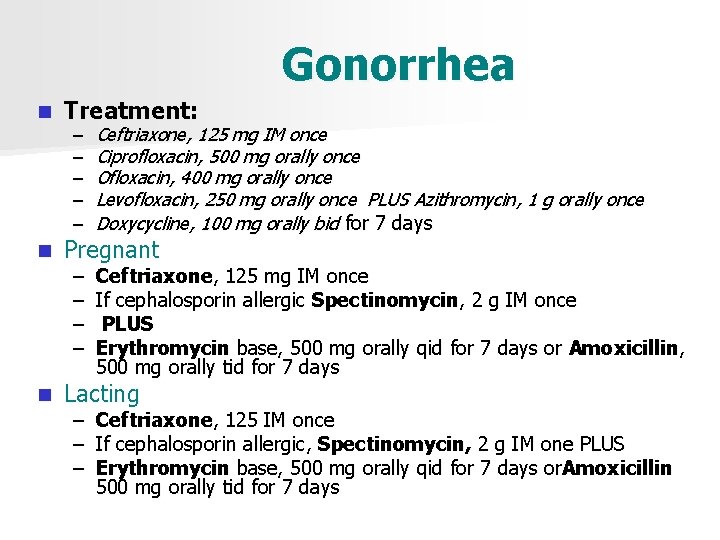
Gonorrhea n Treatment: n Pregnant n Lacting – – – Ceftriaxone, 125 mg IM once Ciprofloxacin, 500 mg orally once Ofloxacin, 400 mg orally once Levofloxacin, 250 mg orally once PLUS Azithromycin, 1 g orally once Doxycycline, 100 mg orally bid for 7 days – – Ceftriaxone, 125 mg IM once If cephalosporin allergic Spectinomycin, 2 g IM once PLUS Erythromycin base, 500 mg orally qid for 7 days or Amoxicillin, 500 mg orally tid for 7 days – Ceftriaxone, 125 IM once – If cephalosporin allergic, Spectinomycin, 2 g IM one PLUS – Erythromycin base, 500 mg orally qid for 7 days or. Amoxicillin 500 mg orally tid for 7 days

Syphilis Treponema pallidum
Syphilis – T. pallidum, a motile spirochete § Transmission by entry in subcutaneous tissue through microscopic abrasions that can occur during sexual intercourse § Also transmitted through kissing, biting, or oral genital sex – Transplacental transmission may occur at any time during pregnancy
Syphilis n Can lead to serious systemic disease and even death n Infection manifests itself in distinct stages § Primary § Secondary § Tertiary
Syphilis n Incubation: – primary stage - 10 to 70 days, 21 days in most people; – secondary stage - weeks to a year; – late stage – years
Primary Syphilis : n Symptoms Approximately 5 -90 days after sexual contact with an infected, contagious partner, a chancre (a painless papule which than eroded to form a nontender, swallow, indurated, clean ulcer with well-defined edges and an inflamed base up to 1 cm in diameter) appears at the site of the microbe’s entry. n The chancre is typically painless (this is in contrast with genital herpes which causes painful ulcers). n There may be associated swollen lymph nodes (small painless lumps that are centers of immune system activity) in the inguinal region (groin). It is contact with such a syphilitic chancre that the infection is transmitted. This initial chancre routinely heals itself spontaneously within three to eight weeks.

Primary Syphilis
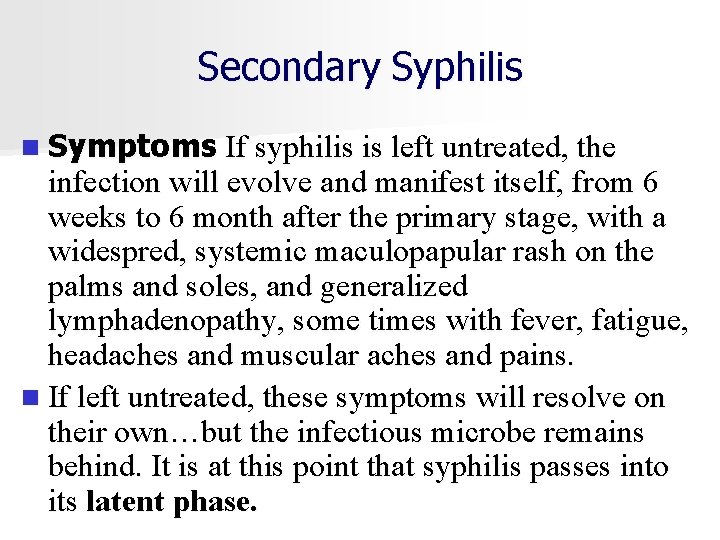
Secondary Syphilis n Symptoms If syphilis is left untreated, the infection will evolve and manifest itself, from 6 weeks to 6 month after the primary stage, with a widespred, systemic maculopapular rash on the palms and soles, and generalized lymphadenopathy, some times with fever, fatigue, headaches and muscular aches and pains. n If left untreated, these symptoms will resolve on their own…but the infectious microbe remains behind. It is at this point that syphilis passes into its latent phase.
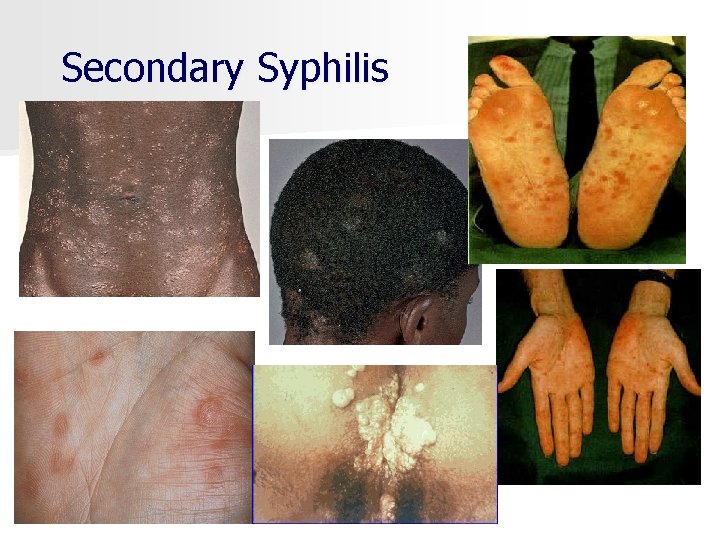
Secondary Syphilis
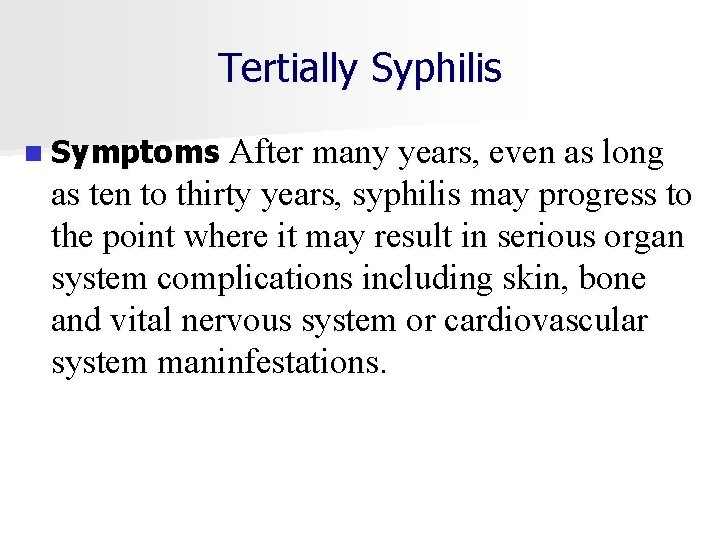
Tertially Syphilis n Symptoms After many years, even as long as ten to thirty years, syphilis may progress to the point where it may result in serious organ system complications including skin, bone and vital nervous system or cardiovascular system maninfestations.

Tertial Syphilis

Tertiary syphilis
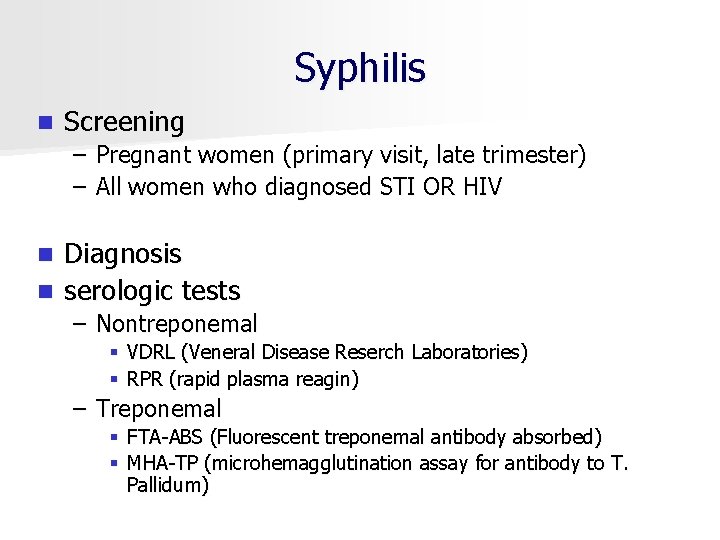
Syphilis n Screening – Pregnant women (primary visit, late trimester) – All women who diagnosed STI OR HIV Diagnosis n serologic tests n – Nontreponemal § VDRL (Veneral Disease Reserch Laboratories) § RPR (rapid plasma reagin) – Treponemal § FTA ABS (Fluorescent treponemal antibody absorbed) § MHA TP (microhemagglutination assay for antibody to T. Pallidum)
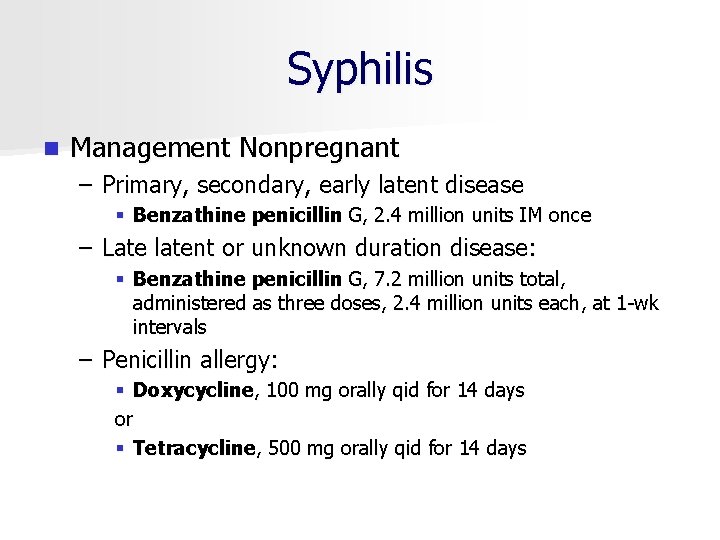
Syphilis n Management Nonpregnant – Primary, secondary, early latent disease § Benzathine penicillin G, 2. 4 million units IM once – Late latent or unknown duration disease: § Benzathine penicillin G, 7. 2 million units total, administered as three doses, 2. 4 million units each, at 1 wk intervals – Penicillin allergy: § Doxycycline, 100 mg orally qid for 14 days or § Tetracycline, 500 mg orally qid for 14 days
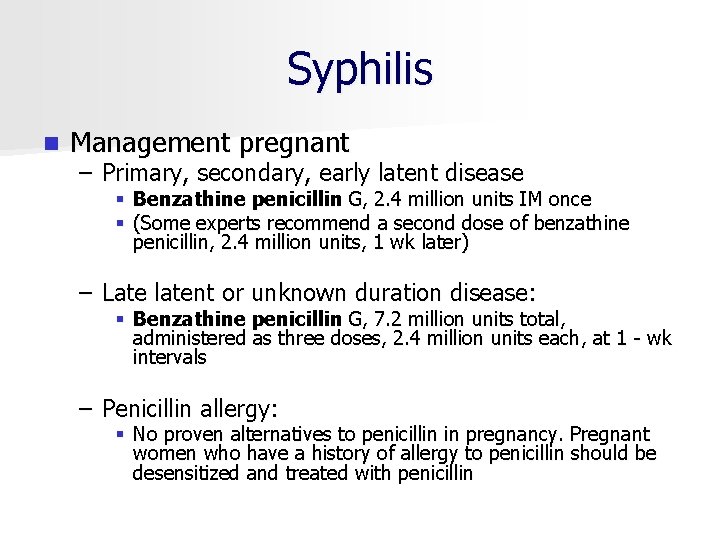
Syphilis n Management pregnant – Primary, secondary, early latent disease § Benzathine penicillin G, 2. 4 million units IM once § (Some experts recommend a second dose of benzathine penicillin, 2. 4 million units, 1 wk later) – Late latent or unknown duration disease: § Benzathine penicillin G, 7. 2 million units total, administered as three doses, 2. 4 million units each, at 1 wk intervals – Penicillin allergy: § No proven alternatives to penicillin in pregnancy. Pregnant women who have a history of allergy to penicillin should be desensitized and treated with penicillin
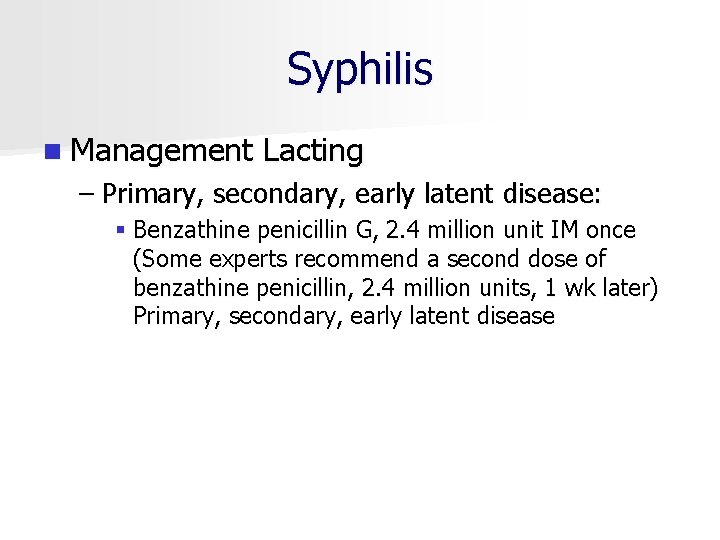
Syphilis n Management Lacting – Primary, secondary, early latent disease: § Benzathine penicillin G, 2. 4 million unit IM once (Some experts recommend a second dose of benzathine penicillin, 2. 4 million units, 1 wk later) Primary, secondary, early latent disease
Pelvic inflammatory disease (PID)
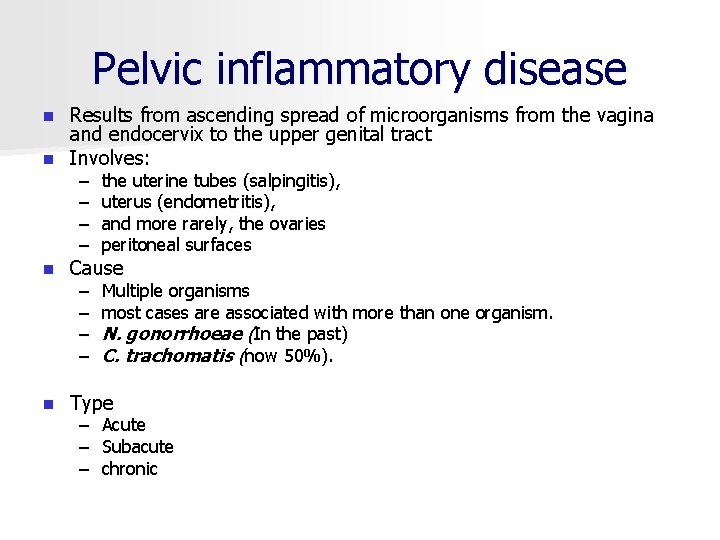
Pelvic inflammatory disease Results from ascending spread of microorganisms from the vagina and endocervix to the upper genital tract n Involves: n – – the uterine tubes (salpingitis), uterus (endometritis), and more rarely, the ovaries peritoneal surfaces – – Multiple organisms most cases are associated with more than one organism. N. gonorrhoeae (In the past) C. trachomatis (now 50%). n Cause n Type – – – Acute Subacute chronic
Pelvic inflammatory disease n Risk factors – young age, – multiple partners, – history of STIs. – IUDs – abortion – pelvic surgery – childbirth
Pelvic inflammatory disease n Results – ectopic pregnancy – Infertility – chronic pelvic pain – dyspareunia (painful intercourse), – pyosalpinx (pus in the uterine tubes), – tuboovarian abscess – pelvic adhesions
Pelvic inflammatory disease n Symptoms – pain § Dul, cramping, intermittent (subacute) § Severe, persistent, incapacitating (acute) n Physical examination § Adnexal tendernass swelling or thickening § uretral, cervical discharge – Intermenstrual bleeding – Fever n Lab data – Dispareunia – WBC – ESR – Menstrual irregularity – Urinary discomfort – constipation
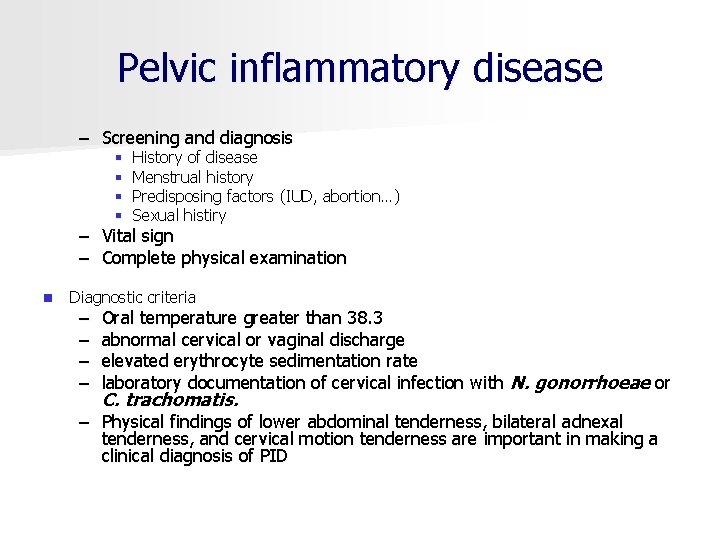
Pelvic inflammatory disease – Screening and diagnosis § § History of disease Menstrual history Predisposing factors (IUD, abortion…) Sexual histiry – Vital sign – Complete physical examination n Diagnostic criteria – – Oral temperature greater than 38. 3 abnormal cervical or vaginal discharge elevated erythrocyte sedimentation rate laboratory documentation of cervical infection with N. gonorrhoeae or C. trachomatis. – Physical findings of lower abdominal tenderness, bilateral adnexal tenderness, and cervical motion tenderness are important in making a clinical diagnosis of PID

Pelvic inflammatory disease n. Management – Prevention – Hospitalization § § § Surgical emergencies such as appendicitis cannot be excluded. The woman has a tuboovarian abscess. The woman is pregnant. Severe illness precludes outpatient management. The woman is unable to tolerate or follow an outpatient oral regimen. The woman has failed to respond to oral outpatient therapy – Education § Nature of disease § Necessity of treatment § prevention – Treatment – Antibiotics, analgetics

Viral Sexually transmitted infections
Human papillomavirus (HPV) Genital or veneral warts)
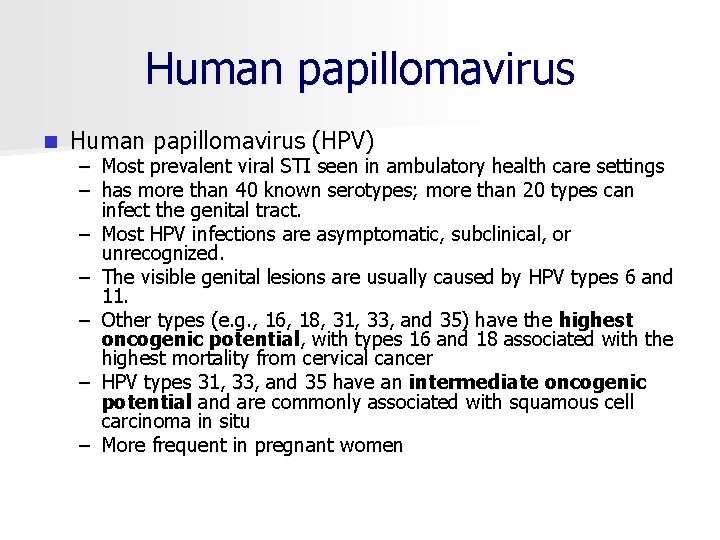
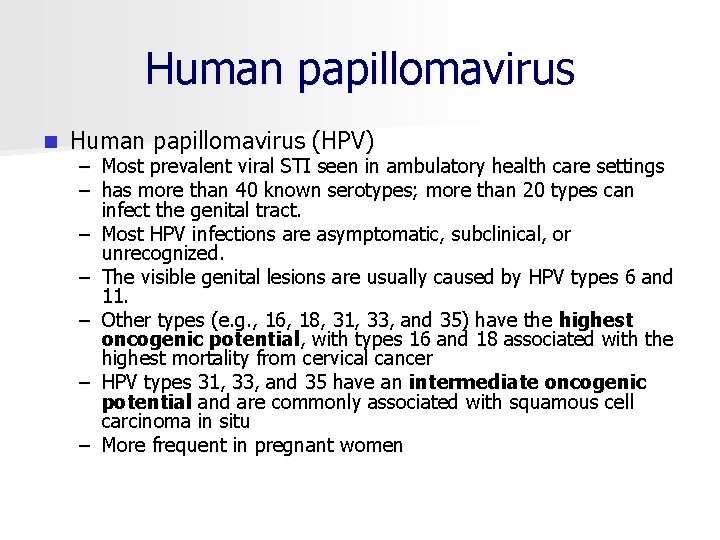
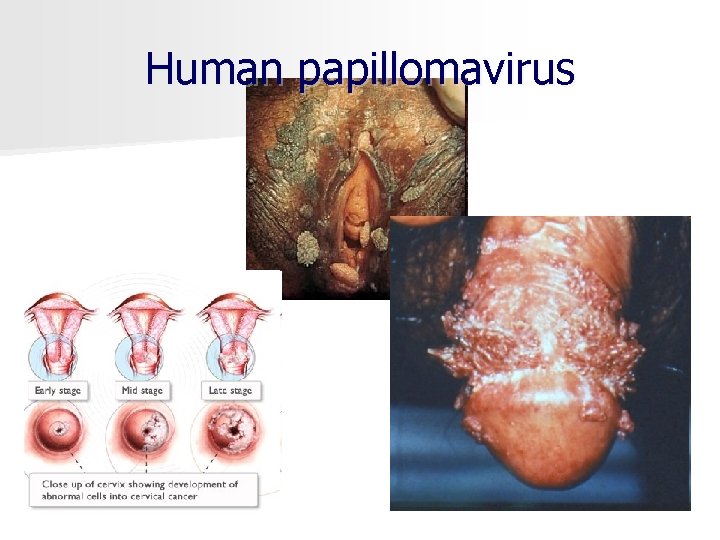
Human papillomavirus n Human papillomavirus (HPV) – Most prevalent viral STI seen in ambulatory health care settings – has more than 40 known serotypes; more than 20 types can infect the genital tract. – Most HPV infections are asymptomatic, subclinical, or unrecognized. – The visible genital lesions are usually caused by HPV types 6 and 11. – Other types (e. g. , 16, 18, 31, 33, and 35) have the highest oncogenic potential, with types 16 and 18 associated with the highest mortality from cervical cancer – HPV types 31, 33, and 35 have an intermediate oncogenic potential and are commonly associated with squamous cell carcinoma in situ – More frequent in pregnant women
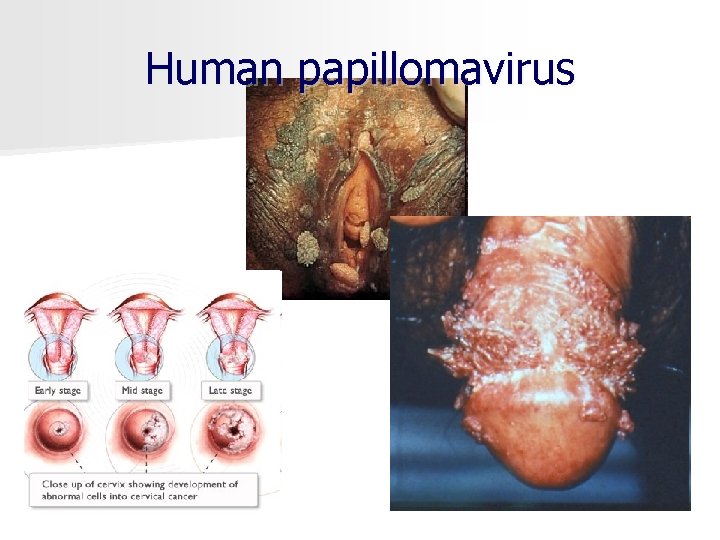
Human papillomavirus

Human papillomavirus www. skinchoice. com
Human papillomavirus Untreated: both sexes warts grow & obstruct infected body openings, pre cancerous lesions of the cervix, vulva, & penis have been linked to some types of HPV. n If

Human papillomavirus n Screening and diagnosis – Complains § § profuse, irritating vaginal discharge itching, dyspareunia, or postcoital bleeding "bumps" on her vulva or labia. – Physical inspection of the vulva, perineum, anus, vagina, and cervix – Colposcopy with biopsy – Pap smear – DNA testing for high risk types of HPV n Management § § § Removal (Imiquimod, podophyllin, and podofilox, cryotherapy) Medications (Acyclovir. Famciclovir, Valacyclovir) Counseling

Herpes Simplex Virus (HSV) Type 1, 2

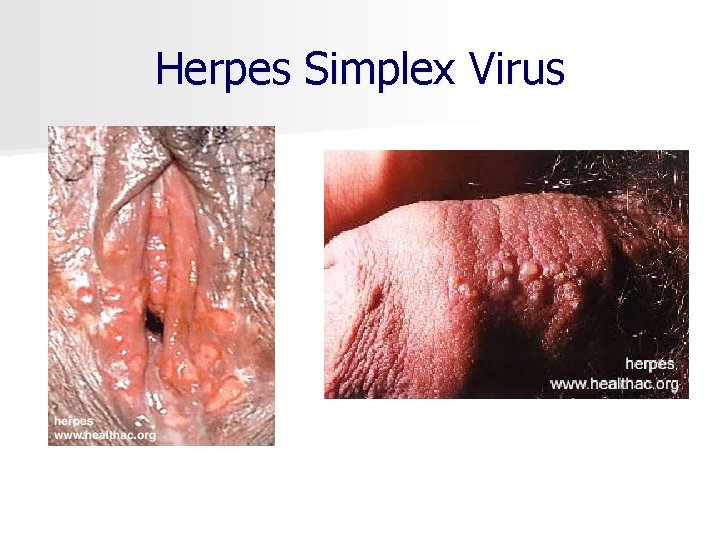
Herpes Simplex Virus n Herpes simplex virus (HSV) – Herpes simplex virus 1 (HSV 1) § Transmitted nonsexually – Herpes simplex virus 2 (HSV 2) § Transmitted sexually – Initial infection characterized by multiple painful lesions, fever, chills, malaise, and severe dysuria – Lesion progress from macules to papules, then forming vesicles, pustules, and ulcers that crust and heal without scarring
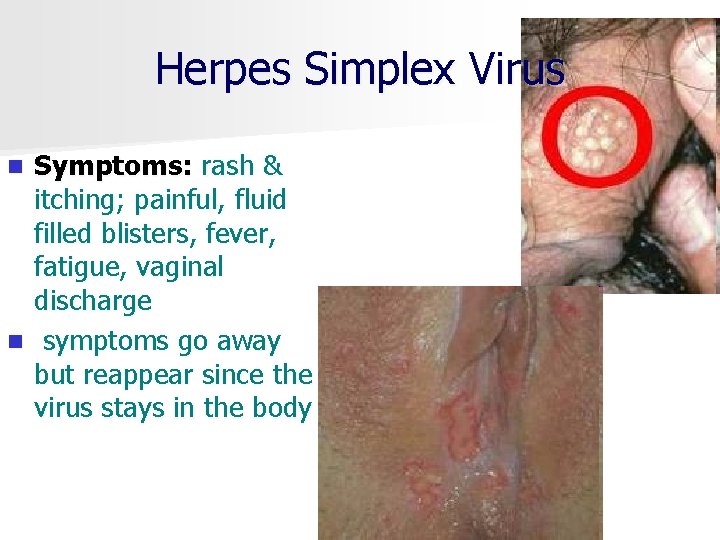
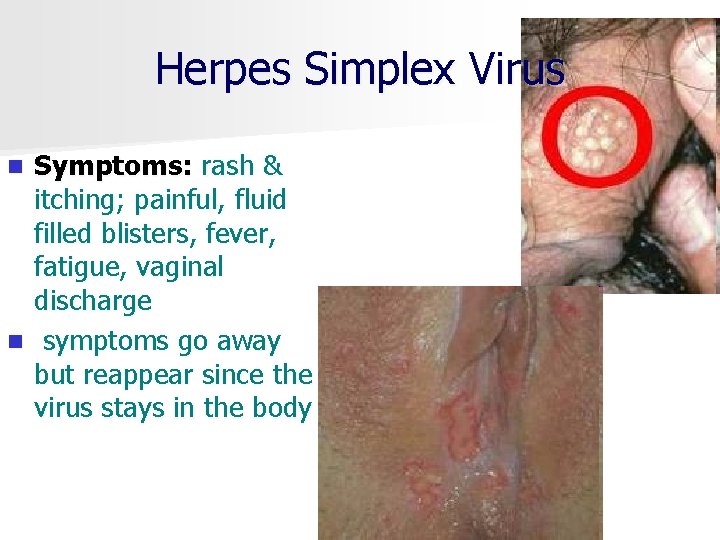
Herpes Simplex Virus Symptoms: rash & itching; painful, fluid filled blisters, fever, fatigue, vaginal discharge n symptoms go away but reappear since the virus stays in the body n
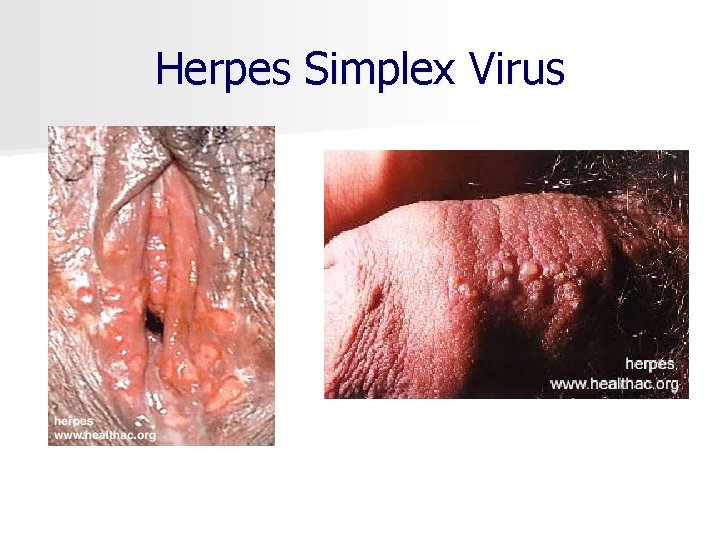
Herpes Simplex Virus
Herpes Simplex Virus n Maternal infection with HSV 2 can have adverse effects on both mother and fetus n Maternal herpes § increase miscarriage rate n Neonatal herpes § Fatal or severe disabling disease
Herpes Simplex Virus n Treatment: § § § n n Antiviral drug: acyclovir, valacyclovir, famciclovir Saline solution sitz bath Oral analgetics Counseling Education use Betadine on lesions to dry & prevent secondary infections, however, Acyclovir (Zovirax) eases symptoms & lessens reoccurrence but is not a cure n There is NO cure for the virus n If Untreated: in fetus/newborns there is a risk of spontaneous abortion; neonatal herpes; mental retardation, death n
Viral hepatitis
Viral hepatitis A
Viral hepatitis A Acquired primarily through a fecal oral route n Transmit during sexual intercourse n Clinical manifestation n – flulike symptoms with malaise, fatigue, anorexia, nausea, pruritis, fever, and right upper quadrant pain. n Lab test – detect the immunoglobulin M (Ig. M) antibody is done to confirm acute infections. The Ig. M antibody is detectable 5 to 10 days after exposure and can remain positive for up to 6 months n Serologic testing to – Hepatitis virus (HAV) n Vaccination is the most effective means of preventing HAV transmission
Viral hepatitis B

Viral hepatitis B n is a disease of the liver and is often a silent infection. n Symptoms are similar to those of hepatitis A: arthralgias, arthritis, lassitude, anorexia, nausea, vomiting, headache, fever, and mild abdominal pain. Later the woman may have clay colored stools, dark urine, increased abdominal pain, and jaundice. n is transmitted person to person through blood and body fluids. n There is no specific treatment for the virus after it has been contracted.
Viral hepatitis C
Viral hepatitis C n Chronic viral hepatitis n Asymptomatic or like hepatitis A n Blood testing n Interferon alfa 2 b
Human Immunodeficiency Virus (HIV)
HIV / AIDS n n HIV is NOT the same as having AIDS, it is only the virus that causes AIDS. Currently there is NO cure but drug therapies "show great promise in managing HIV infection". "HIV infected people are healthy and do not realize they have been infected. HIV primarily infects certain white blood cells that manage the operation of the immune system. Severe depression of the cellular immune system
HIV / AIDS Eventually, the virus can disable the immune system, leaving the person with HIV infection vulnerable to a number of life threatening illnesses. n People who have HIV infection may not have symptoms for many years, especially if they receive good medical care and effective therapies" (American College Health Association [ACHA] , 2001). n
HIV / AIDS n "When symptoms do develop, they are usually similar at first to those of common minor illnesses, such as the "flu", except that they last longer and are more severe. n Persistent tiredness, unexplained fevers, recurring night sweats, prolonged enlargement of the lymph nodes, and weight loss are all common.

HIV / AIDS n Screening and diagnosis – Antibody testing § Enzyme immunoassay (EIA) § Western blot – Counseling for HIV testing § HIV testing offered early in pregnancy § Perinatal transmission decrease § Consider confidentiality and documentation § Notification of results – Treatment
HIV / AIDS n n n People with HIV infection can transmit the virus to others even if they have no symptoms and even if they do not know they have been infected. HIV can be transmitted (1) by sexual contact (anal, vaginal, & oral); (2) by direct exposure to infected blood; and (3) from an HIV infected woman to her fetus during pregnancy or childbirth, or to her infant during breastfeeding" (ACHA, 2001).

Kaposi’s sarcoma (Cancer associated with AIDS) Oral Leukoplakia Oral Thrush (yeast infection) Common infection associated with AIDS

Vaginal infections
Bacterial vaginosis nonspecific vaginitis

Bacterial vaginosis n n n Haemophilus vaginitis, or Gardnerella, Mobiluncus, but the exact etiology is unknown is associated with preterm labor and birth. syndrome in which normal H 2 O 2 producing lactobacilli are replaced with high concentrations of anaerobic bacteria With the proliferation of anaerobes, the level of vaginal amines is increased, and the normal acidic p. H of vagina is altered. Epithelial cells slough, and numerous bacteria attach to their surfaces (clue cells). When the amines are volatilized, the characteristic odor occurs
Bacterial vaginosis n Screening n Diagnosis – "fishy odor « – discharge is usually profuse; thin; and white, gray, or milky in appearance – mild irritation or pruritis. – Microscopic examination of vaginal secretions: clue cells (vaginal epithelial cells coated with bacteria) – Nitrazine paper p. H of 4. 5 or greater. – The fishy odor will be released when KOH is added to vaginal secretions on the lip of the withdrawn speculum.
Bacterial vaginosis n Management – Metronidazole, – Clindamycin
Candidiasis C. Albicans
Candidiasis Vulvovaginal candidiasis, or yeast infection, is second most common type of vaginal infection n Factors affecting predisposal n § § § § Antibiotic therapy Diabetes Pregnancy Obesity Diets high in refined sugars Use of corticosteroids Immunosuppressed states
Candidiasis n Common symptoms – vulvar and possibly vaginal pruritis – itching may be mild or intense, interfere with rest and activities and occur during or after intercourse – feeling of dryness – painful urination – the discharge is thick, white, lumpy, and cottage cheese like, may be found in patches on the vaginal walls, cervix, and labia – the vulva are red and the swollen, as are the labial folds, vagina, and cervix. – there is no characteristic odor with yeast infections, sometimes a yeasty or musty smell occurs.
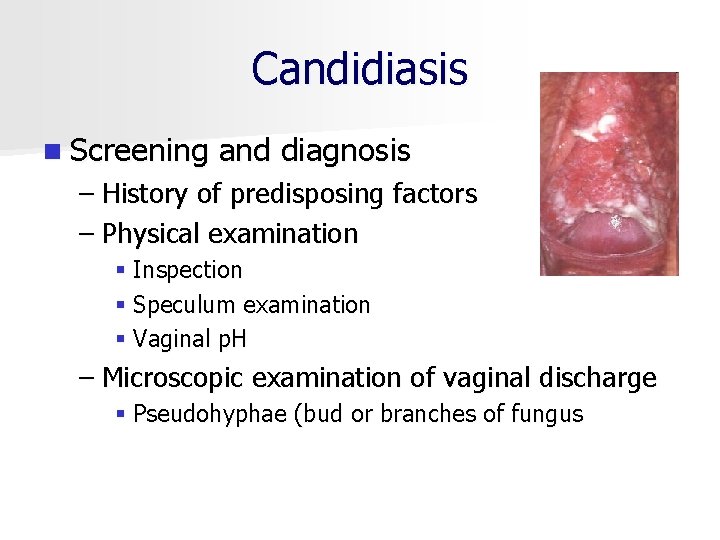
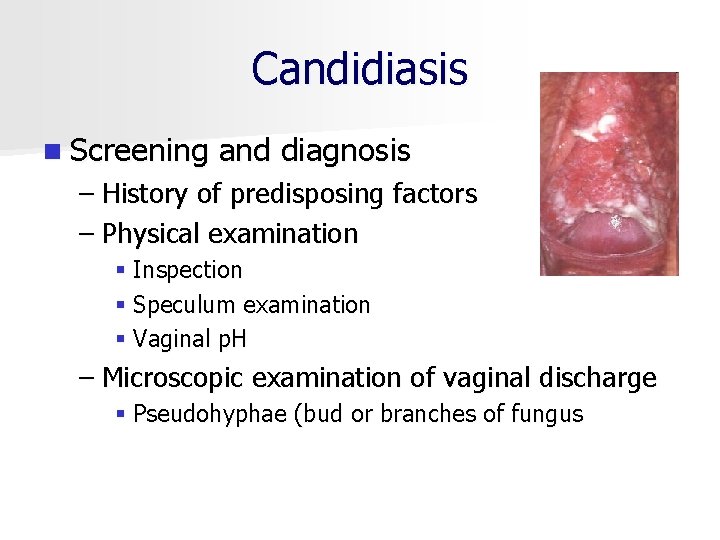
Candidiasis n Screening and diagnosis – History of predisposing factors – Physical examination § Inspection § Speculum examination § Vaginal p. H – Microscopic examination of vaginal discharge § Pseudohyphae (bud or branches of fungus
Candidiasis – Management § Antifungal drug § Method of comfort – Genital hygiene – Sitz bath – Cotton underpants – Not wearing underpants to bed – Not to use tampons – Avoiding intercorse
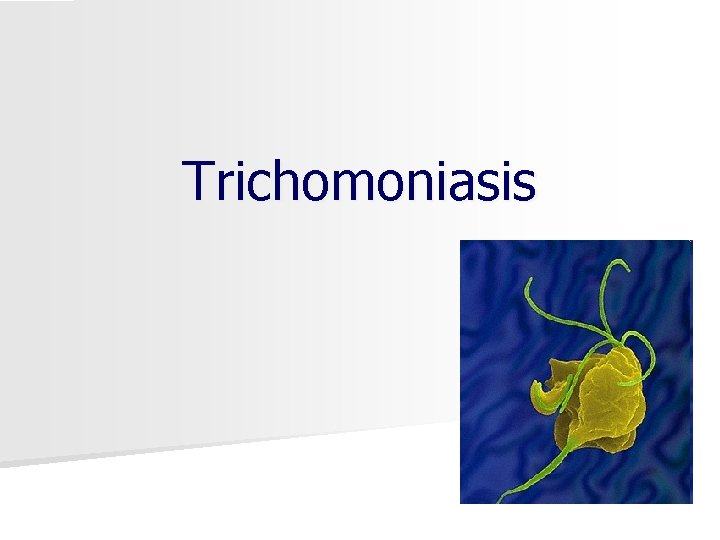
Trichomoniasis
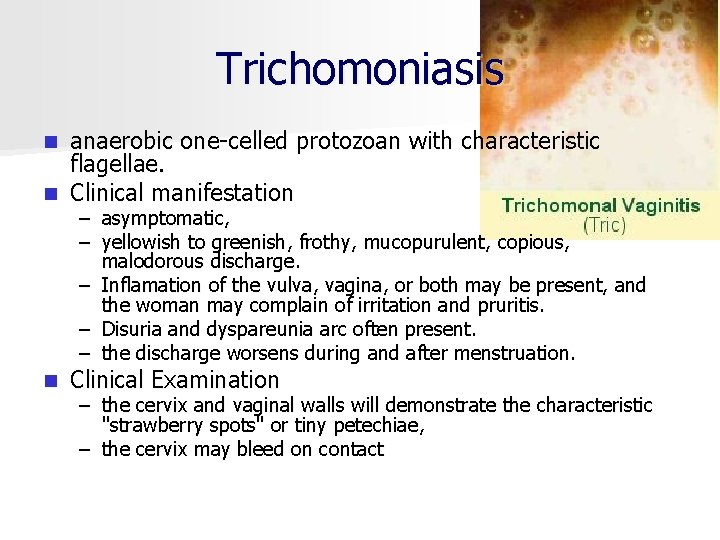
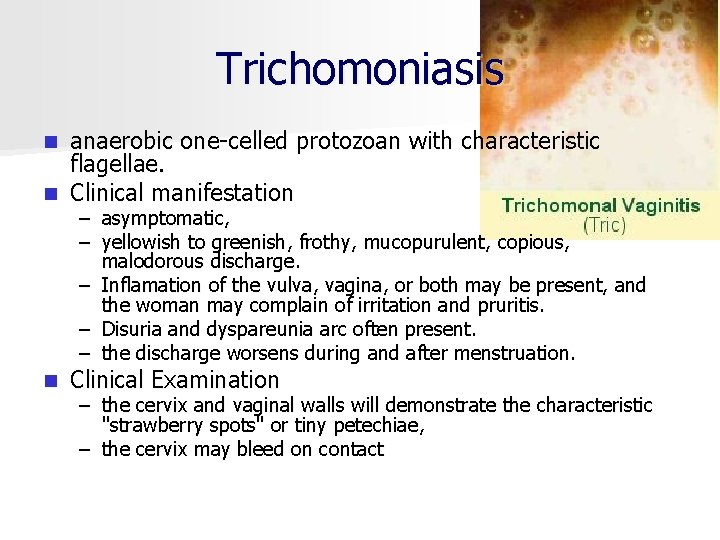
Trichomoniasis anaerobic one celled protozoan with characteristic flagellae. n Clinical manifestation n – asymptomatic, – yellowish to greenish, frothy, mucopurulent, copious, malodorous discharge. – Inflamation of the vulva, vagina, or both may be present, and the woman may complain of irritation and pruritis. – Disuria and dyspareunia arc often present. – the discharge worsens during and after menstruation. n Clinical Examination – the cervix and vaginal walls will demonstrate the characteristic "strawberry spots" or tiny petechiae, – the cervix may bleed on contact

Trichomoniasis n Screening and diagnosis § Speculum examination § Pap smear n Treatment: metronidazole, given by mouth in a single dose

Pubic Lice (Crabs)

Pubic Lice (Crabs) n n n Pubic lice are tiny insects that can crawl from the pubic hair of one person to the pubic hair of another person during sex. You will be prescribed or told to buy medication that kills the lice and their eggs. You will also need to dry clean or use very hot water to wash all of your bedding, towels, or recently worn clothing to kill the lice. Tell your partner. Pubic lice can be spread even when you use a condom.
What Happens without treatment? n STD without treatment lead to some long term effects such as: – Infertility (Unable to have babies) – Cancer – Long term pain – Can pass disease from mother to baby – Death
Conclusion It is much easier to prevent an STD than to cure one. n The ONLY way to prevent STDs is to abstain from ALL types of sexual intercourse. n However, if you have sex, you must use a latex condom, EVERY TIME. However, condoms do not always protect you from STDs such as HSV 2, HPV, and Pubic Lice. n Remember, just because you and your partner may be monogamous with each other, the risk of getting an STD is increased by the number of previous sexual partners either partner has had. n
Prevention is the Key n Abstinence, or not having oral, vaginal or anal sex, is the best way to protect yourself. n It is possible to get an STD even without having intercourse through skin to skin contact. n Use latex condoms correctly for any type of sex (vaginal, oral or anal) from start to finish.
TORCH Infections T Toxoplasmosis O Other (HIV. . . ) R Rubella C Cytomegalovirus H Herpes
Toxoplasmosis n is a multisystem disease caused by the protozoan n Risk factors Toxoplasma gondii. – Eating cured, raw, or undercooked meat puts women at high risk for contracting toxoplasmosis. – contact with soil – travel outside the United States, Europe, and Canada – hand to mouth contact after disposal of cat litter is less of a risk factor. Approximately 30% of women who contract toxoplasmosis during gestation transmit the disease to their offspring. n Fetal infection occurs in 0. 07% to 0. 11% of all pregnancies n
Toxoplasmosis n Maternal effects n Fetal effects n Counseling: prevention, identification, and management – Acute infection similar to (protozoa) influenza, lymphadenopathy. Woman immune after first episode (except in immunocompromised patients) – With maternal acute infection, parasitemia – Less likely to occur with maternal chronic infection – Miscarriage likely with acute infection early in pregnancy – Use good handwashing technique – Avoid eating raw meat and exposure to litter used by infected cats; if cats in house, have toxoplasma titer checked – If titer is rising during early pregnancy, abortion may be considered an option
Rubella n Maternal effects n Fetal effects n Counseling: prevention, identification, and management – Rash, fever, mild symptoms; suboccipital lymph nodes may be swollen; some photophobia – Occasionally arthritis or encephalitis – Miscarriage – Incidence of congenital anomalies—first month 50%, second month 25%, third month 10%, fourth month 4% – Exposure during first 2 months—malformations of heart, eyes, ears, or brain, abnormal dermatoglyphics – Exposure after fourth month—systemic infection, hepatosplenomegaly. intrauterine growth restriction, rash – Vaccination of pregnant women contraindicated; pregnancy should be prevented for 3 months after vaccination; pregnant women nonreactive to hemagglutinin inhibition antigen can be safely vaccinated after birth
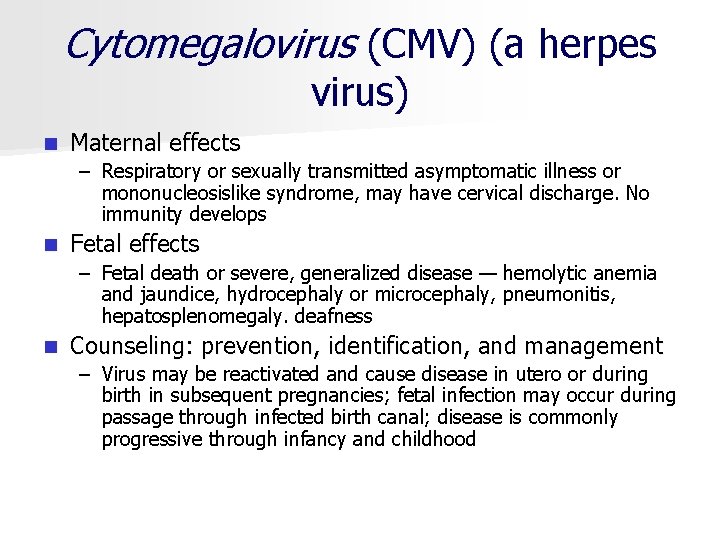
Cytomegalovirus (CMV) (a herpes virus) n Maternal effects – Respiratory or sexually transmitted asymptomatic illness or mononucleosislike syndrome, may have cervical discharge. No immunity develops n Fetal effects – Fetal death or severe, generalized disease — hemolytic anemia and jaundice, hydrocephaly or microcephaly, pneumonitis, hepatosplenomegaly. deafness n Counseling: prevention, identification, and management – Virus may be reactivated and cause disease in utero or during birth in subsequent pregnancies; fetal infection may occur during passage through infected birth canal; disease is commonly progressive through infancy and childhood
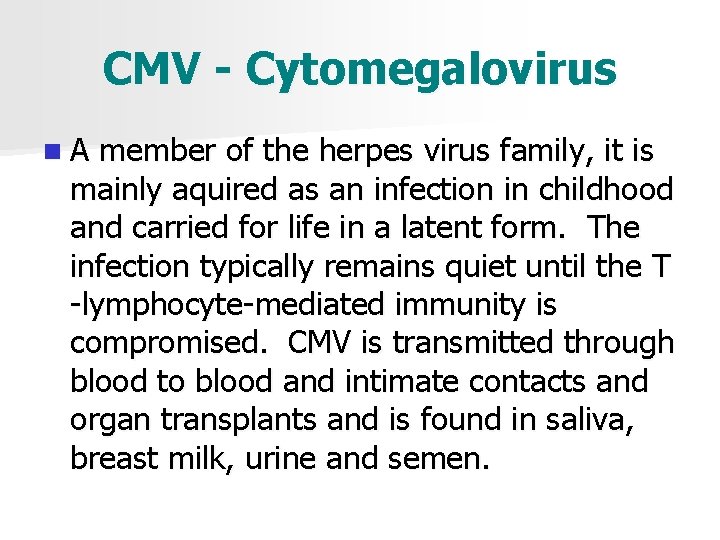
CMV - Cytomegalovirus n A member of the herpes virus family, it is mainly aquired as an infection in childhood and carried for life in a latent form. The infection typically remains quiet until the T lymphocyte mediated immunity is compromised. CMV is transmitted through blood to blood and intimate contacts and organ transplants and is found in saliva, breast milk, urine and semen.
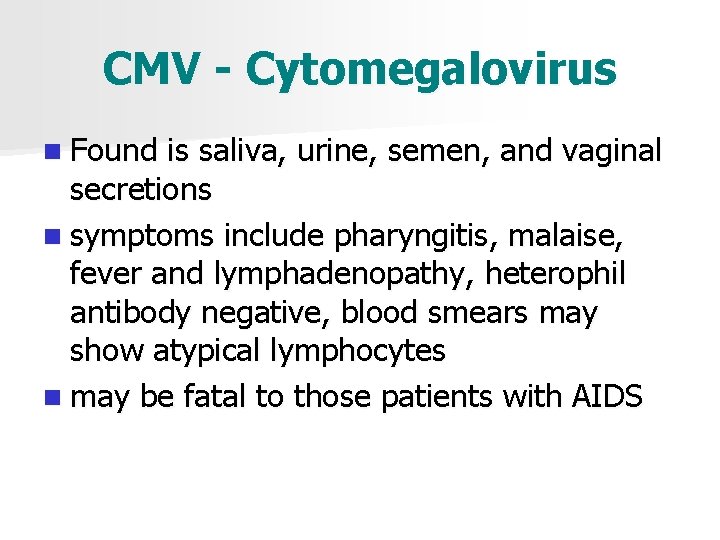
CMV - Cytomegalovirus n Found is saliva, urine, semen, and vaginal secretions n symptoms include pharyngitis, malaise, fever and lymphadenopathy, heterophil antibody negative, blood smears may show atypical lymphocytes n may be fatal to those patients with AIDS
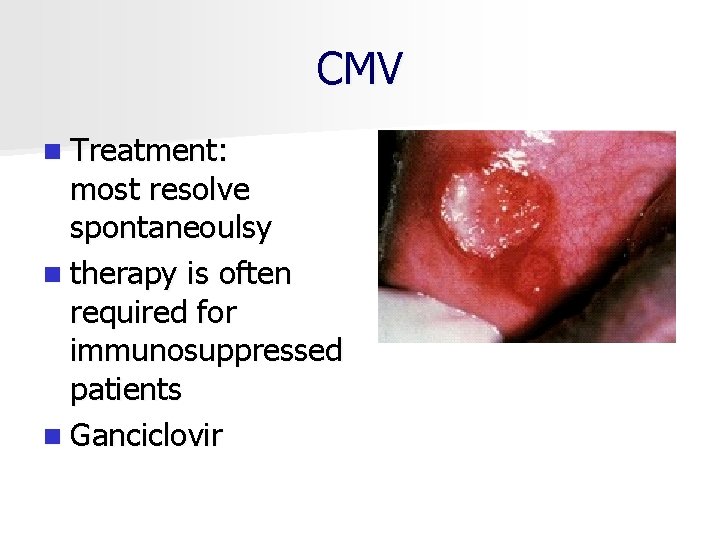
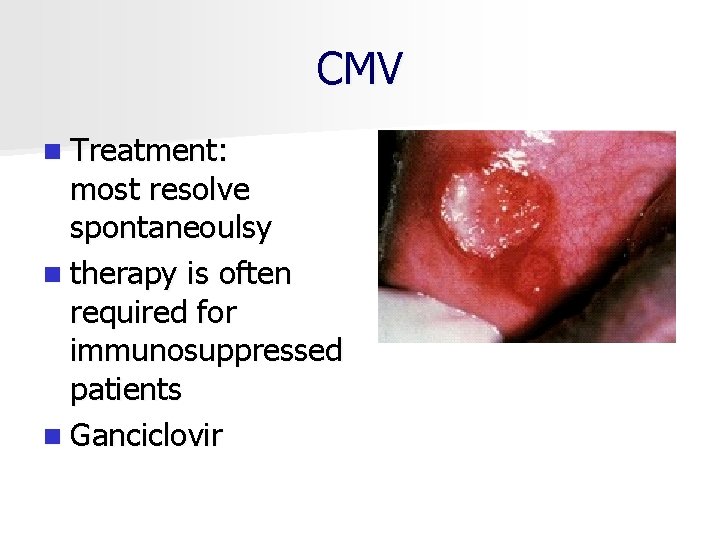
CMV n Treatment: most resolve spontaneoulsy n therapy is often required for immunosuppressed patients n Ganciclovir

Interstial keratitis causing blindness Mucous patches and skin lesions in an infant Rhagades facial disfigurement Hutchinson's teeth

Perforation of the hard palate (resulting from gummatous destruction) Runny nose (rhinitis) known as snuffles, a macular rash and mucus patches Hutchinson's teeth - peg-shaped upper incisors
![Herpes genitalis herpes simplex virus type 2 HSV 2 n Maternal effects Primary Herpes genitalis (herpes simplex virus, type 2 [HSV 2]) n Maternal effects – Primary](https://slidetodoc.com/presentation_image/3b6cf42f332a9e68072b58a19c84a299/image-110.jpg)
Herpes genitalis (herpes simplex virus, type 2 [HSV 2]) n Maternal effects – Primary infection with painful blisters, rash, fever, malaise, nausea, headache; pregnancy risks include miscarriage, preterm labor, stillbirths n Fetal effects – Transplacental infection is rare; congenital effects include skin lesions and scarring, IUGR, mental retardation, microcephaly n Counseling: prevention, identification, and management – Risk of transmission is greatest during vaginal birth if woman has active lesions – Acyclovir not recommended in pregnancy; treat symptomatically
Thanks for your attention!
 Chapter 24 lesson 1 sexually transmitted diseases
Chapter 24 lesson 1 sexually transmitted diseases Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Sti std
Sti std Sexually transmitted diseases
Sexually transmitted diseases A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Std
Std Obsessive compulsive disorder ncp
Obsessive compulsive disorder ncp Care plan for cataract
Care plan for cataract Vcloudpoint zero client price
Vcloudpoint zero client price Linux leger
Linux leger Example of two tier architecture
Example of two tier architecture Primary secondary tertiary care
Primary secondary tertiary care How do whales reproduce sexually
How do whales reproduce sexually Nematoda segmentation
Nematoda segmentation Do sea urchins reproduce sexually or asexually
Do sea urchins reproduce sexually or asexually What is sexually dimorphic mean
What is sexually dimorphic mean Rules of consent
Rules of consent Is mitosis asexual
Is mitosis asexual Sexual abuse quiz
Sexual abuse quiz Sea cucumber internal anatomy
Sea cucumber internal anatomy Protists habitat
Protists habitat Vasocongestion definition
Vasocongestion definition What is an annelid
What is an annelid Sexual harassment quiz
Sexual harassment quiz Sexual propagation
Sexual propagation Cnidaria class
Cnidaria class Bilateral symmetry
Bilateral symmetry Frustrated freight
Frustrated freight How do sponges reproduce sexually and asexually
How do sponges reproduce sexually and asexually How do birds mate diagram
How do birds mate diagram Sexually dimorphic meaning
Sexually dimorphic meaning Licensed sex offender treatment provider illinois
Licensed sex offender treatment provider illinois Oblique light examination in questioned document
Oblique light examination in questioned document A song transmitted orally which tells a story:
A song transmitted orally which tells a story: Flat pivot bearing
Flat pivot bearing Electronically transmitted postal ballot system
Electronically transmitted postal ballot system The totality of learned socially transmitted behavior
The totality of learned socially transmitted behavior Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Tư thế worm breton
Tư thế worm breton Chúa yêu trần thế
Chúa yêu trần thế Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Phép trừ bù
Phép trừ bù Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Ví dụ về giọng cùng tên
Ví dụ về giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Tia chieu sa te
Tia chieu sa te Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot Các số nguyên tố là gì
Các số nguyên tố là gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Hệ hô hấp
Hệ hô hấp Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Different types of diseases
Different types of diseases Which one is jurans three role model
Which one is jurans three role model Protein deficiency diseases
Protein deficiency diseases Natural history of disease
Natural history of disease Modern lifestyle and hypokinetic diseases
Modern lifestyle and hypokinetic diseases Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Odontogenic inflammation
Odontogenic inflammation Iceberg phenomenon definition
Iceberg phenomenon definition Human diseases a systemic approach
Human diseases a systemic approach Venn diagram of communicable and non-communicable diseases
Venn diagram of communicable and non-communicable diseases Classification of periapical diseases
Classification of periapical diseases Section 19-3 diseases caused by bacteria and viruses
Section 19-3 diseases caused by bacteria and viruses Define a primary skin lesion and list three types
Define a primary skin lesion and list three types Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Chapter 32 childhood communicable diseases bioterrorism
Chapter 32 childhood communicable diseases bioterrorism Chapter 23 communicable diseases
Chapter 23 communicable diseases Chapter 22 genetics and genetically linked diseases
Chapter 22 genetics and genetically linked diseases Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders What conditions do fungal organisms favor for growth
What conditions do fungal organisms favor for growth 10 diseases of lymphatic system
10 diseases of lymphatic system X linked diseases
X linked diseases Whats sex linked
Whats sex linked Perianal pruritus
Perianal pruritus Hyperglyceremia
Hyperglyceremia Nutritional diseases
Nutritional diseases Nutritional diseases
Nutritional diseases King of diseases
King of diseases Normal gingiva in child
Normal gingiva in child Non communicable diseases
Non communicable diseases Columbian exchange restaurant names
Columbian exchange restaurant names Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases