Nutritional diseases Programs Dr Asif Rehman Nutrition Nutrition

- Slides: 39
Nutritional diseases & Programs Dr Asif Rehman
Nutrition • Nutrition may be defined as “The science of food and its relationship to health” (K Park, 2012) • The word Nutrient is used for specific dietary constituents and are organic and inorganic complexes contained in food such as: a) Proteins b) Vitamins c) Minerals etc
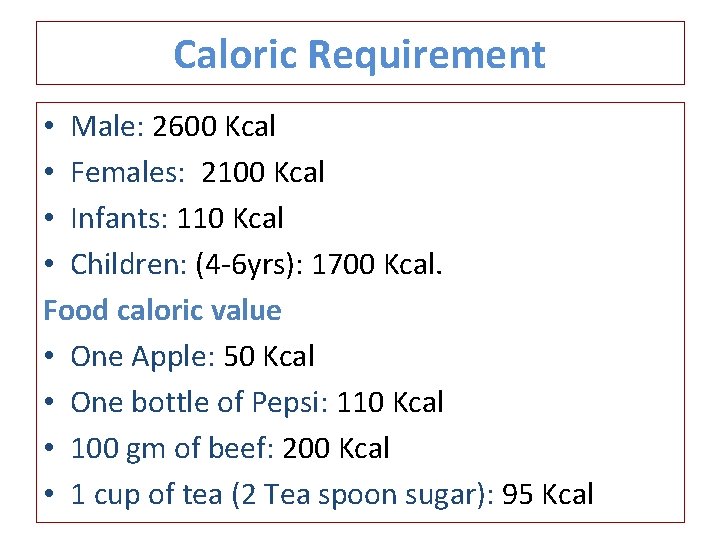
Caloric Requirement • Male: 2600 Kcal • Females: 2100 Kcal • Infants: 110 Kcal • Children: (4 -6 yrs): 1700 Kcal. Food caloric value • One Apple: 50 Kcal • One bottle of Pepsi: 110 Kcal • 100 gm of beef: 200 Kcal • 1 cup of tea (2 Tea spoon sugar): 95 Kcal
Nutrition • Poor nutrition – Can lead to reduced immunity, increased susceptibility to disease, impaired physical and mental development, and reduced productivity.
Nutrients • There about 50 different nutrients which are normally supplied through the foods we eat. Each nutrient has specific function in the body. These may be divided into • Macronutrients: (Proteins, Fats, Carbohydrates) • Micronutrients: ( Vitamins and Minerals)
Vitamins • Fat soluble: (Vitamin A, D, E, K) • Water soluble: (Vitamin B & C) • Each vitamin has specific function to perform and deficiency of any particular vitamin may lead to specific deficiency disease.
Vitamin A • In 1960 the term “Retinol” was introduced for Vitamin A. • The international unit (IU) of vitamin A is equivalent 0. 3 microgram of Retinol. • Sources: • Animal Food: (liver, eggs, butter, cheese, whole milk, fish & meat) • Plant Food: (spinach, mangos, carrots) • Fortified Food: ( Ghee, margarine, milk)
Vitamin A deficiency can causes: • Night blindness: • Conjunctional Xerosis: (Conjunctiva becomes dry and non wettable) • Corneal Xerosis: (cornea appears dull, dry and non wettable) • Keratomalacia: (Liquefaction of the cornea: one of the major cause of blindness in India)
Treatment & Prevention of Vitamin A Deficiency • Treatment: 1. Nearly all of the early stages of Xeropthalmia can be reversed by administration of massive dose of 200000 IU or 110 mg of Retinol orally on two successive days. • Prevention: 1. The recommended daily intake is 600 microgram for adults. 2. Diet improvement by regular and adequate intake of food rich in Vitamin A 3. Reducing contributory factors e. g Diarrhea Measles.
Vitamin D • The nutritionally important forms of vitamin D in man are Calciferol vitamin D 2 and cholecalciferol vitamin D 3. • Sources: 1. Vitamin D is found in animal fats and fish live oil. 2. It is also derived from exposure to UV rays of the sunlight. 3. Also found in Butter, Eggs and Milk
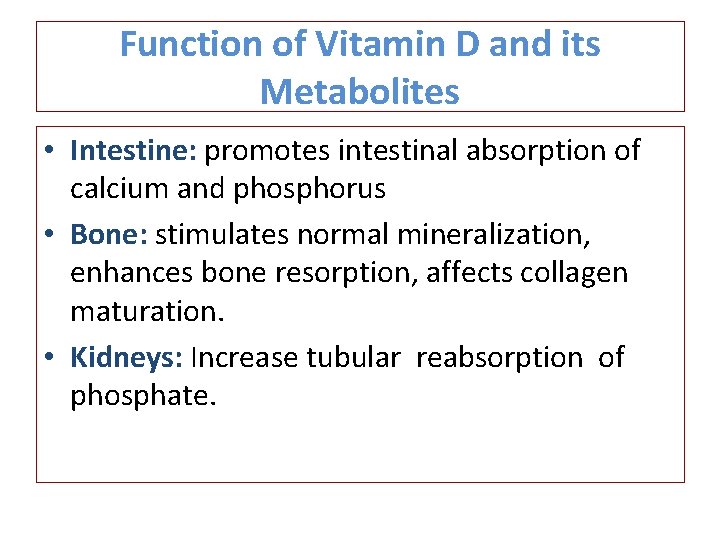
Function of Vitamin D and its Metabolites • Intestine: promotes intestinal absorption of calcium and phosphorus • Bone: stimulates normal mineralization, enhances bone resorption, affects collagen maturation. • Kidneys: Increase tubular reabsorption of phosphate.
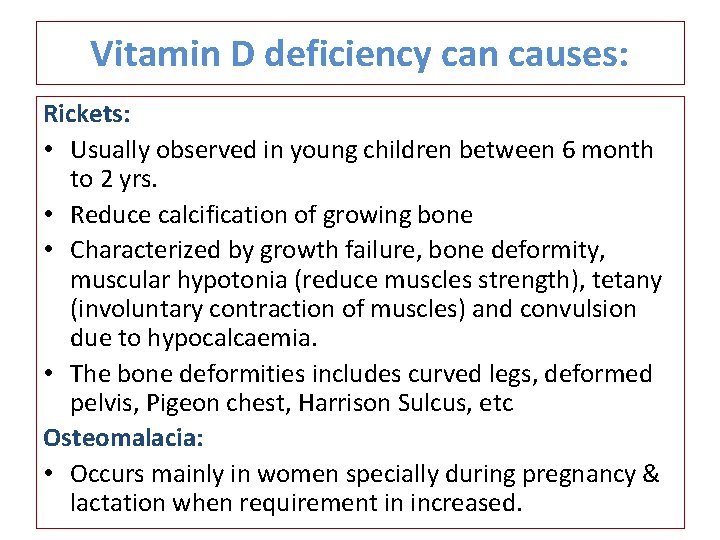
Vitamin D deficiency can causes: Rickets: • Usually observed in young children between 6 month to 2 yrs. • Reduce calcification of growing bone • Characterized by growth failure, bone deformity, muscular hypotonia (reduce muscles strength), tetany (involuntary contraction of muscles) and convulsion due to hypocalcaemia. • The bone deformities includes curved legs, deformed pelvis, Pigeon chest, Harrison Sulcus, etc Osteomalacia: • Occurs mainly in women specially during pregnancy & lactation when requirement in increased.
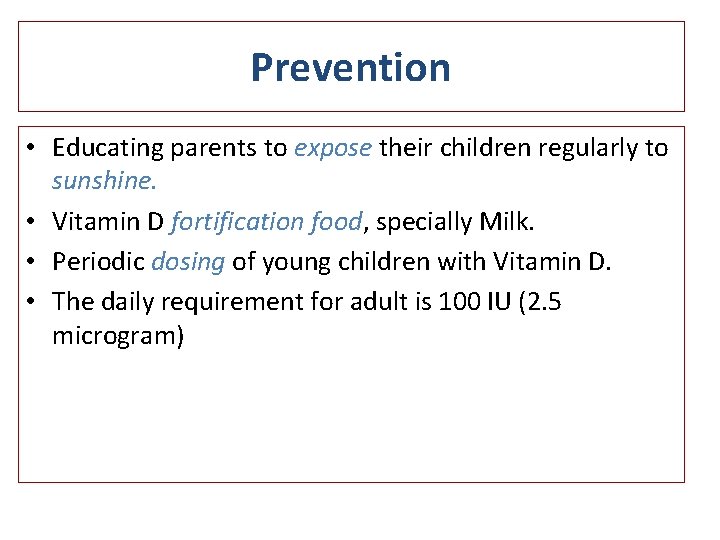
Prevention • Educating parents to expose their children regularly to sunshine. • Vitamin D fortification food, specially Milk. • Periodic dosing of young children with Vitamin D. • The daily requirement for adult is 100 IU (2. 5 microgram)
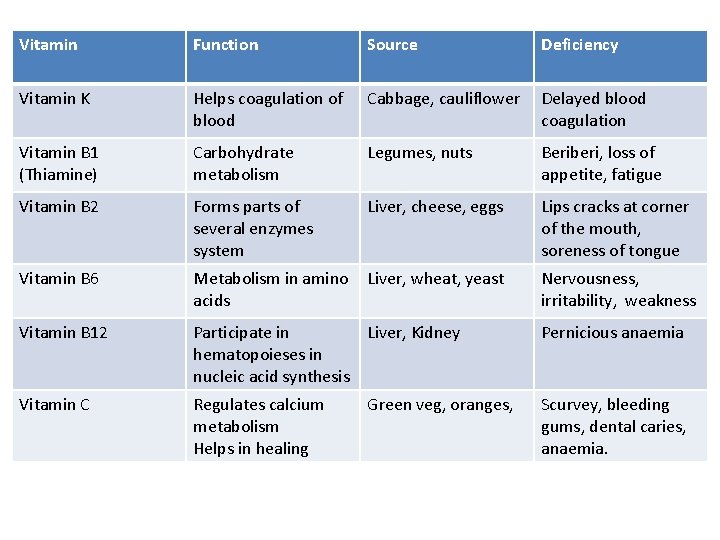
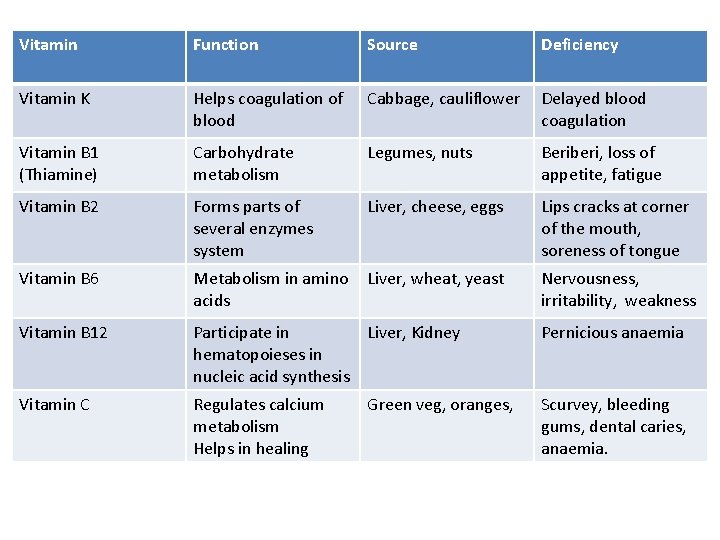
Vitamin Function Source Deficiency Vitamin K Helps coagulation of blood Cabbage, cauliflower Delayed blood coagulation Vitamin B 1 (Thiamine) Carbohydrate metabolism Legumes, nuts Beriberi, loss of appetite, fatigue Vitamin B 2 Forms parts of several enzymes system Liver, cheese, eggs Lips cracks at corner of the mouth, soreness of tongue Vitamin B 6 Metabolism in amino acids Liver, wheat, yeast Nervousness, irritability, weakness Vitamin B 12 Participate in Liver, Kidney hematopoieses in nucleic acid synthesis Pernicious anaemia Vitamin C Regulates calcium metabolism Helps in healing Scurvey, bleeding gums, dental caries, anaemia. Green veg, oranges,
Food Fortification • According to WHO Food Fortification is defined as “the process whereby nutrients are added to food (in relatively small amount) to maintain and improve the quality of diet of a group, a community or population” Food adulteration: • Mixing/substitution/concealing the quality/miss branding/adding toxicants
Malnutrition Definition • A pathological state resulting from a relative or absolute deficiency or excess of one or more essential nutrient. Primary Malnutrition: • due to external factor like Food non availability Secondary malnutrition: • due to abnormal digestion/absorbtion/utelization
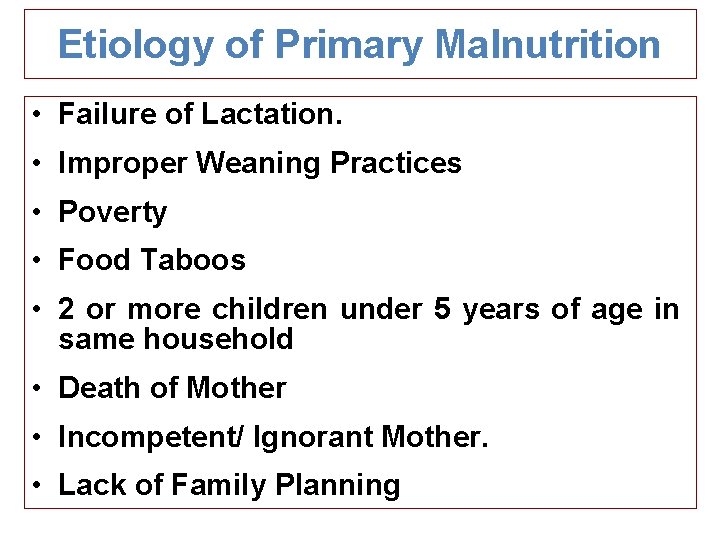
Etiology of Primary Malnutrition • Failure of Lactation. • Improper Weaning Practices • Poverty • Food Taboos • 2 or more children under 5 years of age in same household • Death of Mother • Incompetent/ Ignorant Mother. • Lack of Family Planning
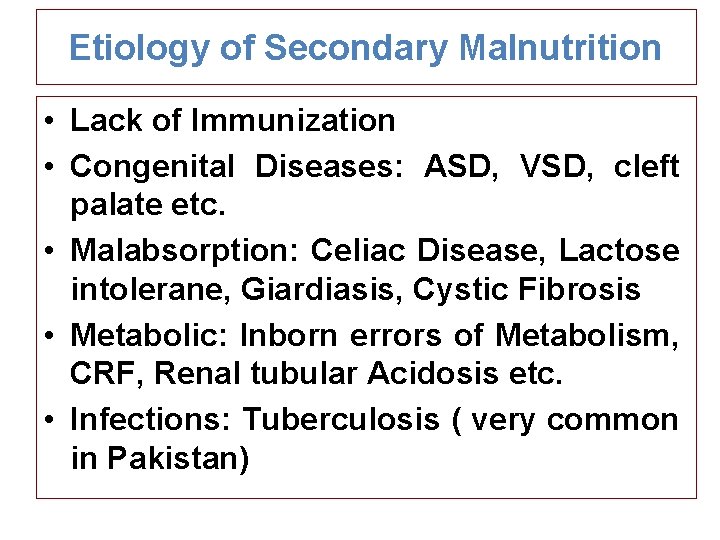
Etiology of Secondary Malnutrition • Lack of Immunization • Congenital Diseases: ASD, VSD, cleft palate etc. • Malabsorption: Celiac Disease, Lactose intolerane, Giardiasis, Cystic Fibrosis • Metabolic: Inborn errors of Metabolism, CRF, Renal tubular Acidosis etc. • Infections: Tuberculosis ( very common in Pakistan)
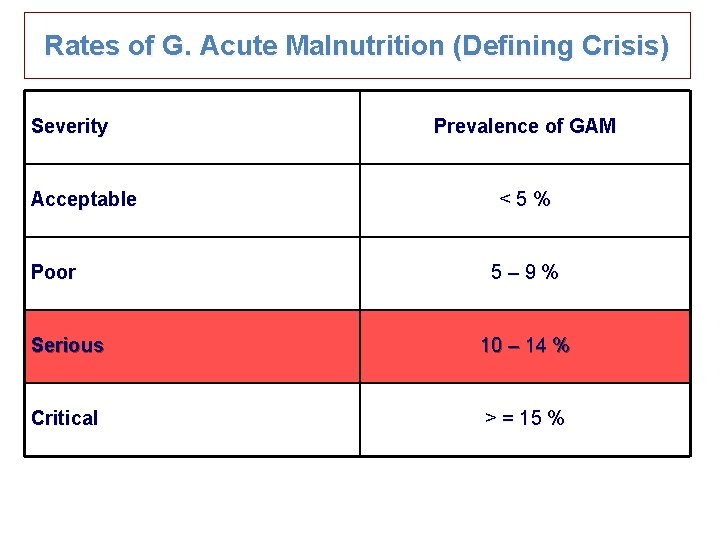
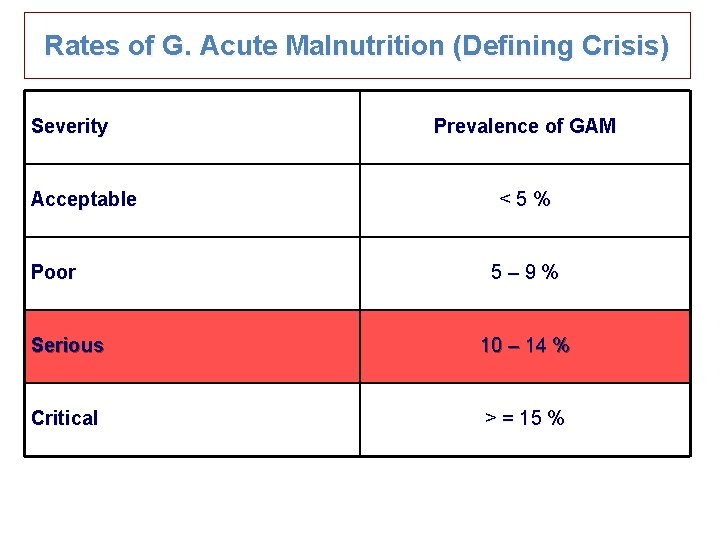
Rates of G. Acute Malnutrition (Defining Crisis) Severity Acceptable Poor Prevalence of GAM <5% 5– 9% Serious 10 – 14 % Critical > = 15 %
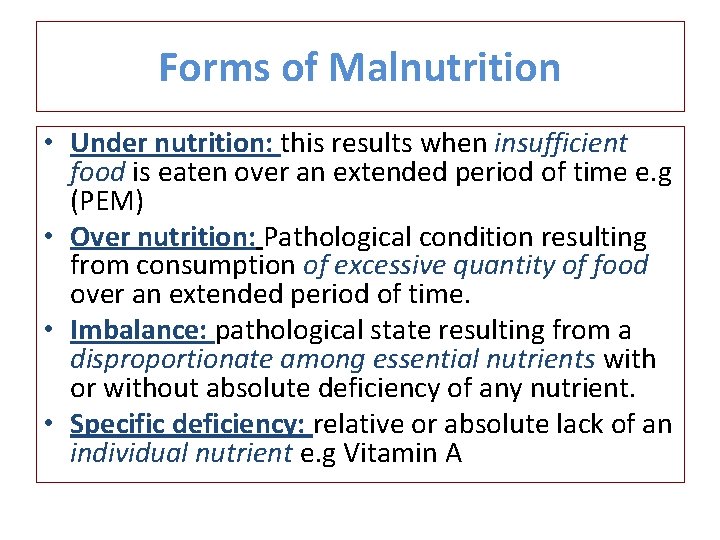
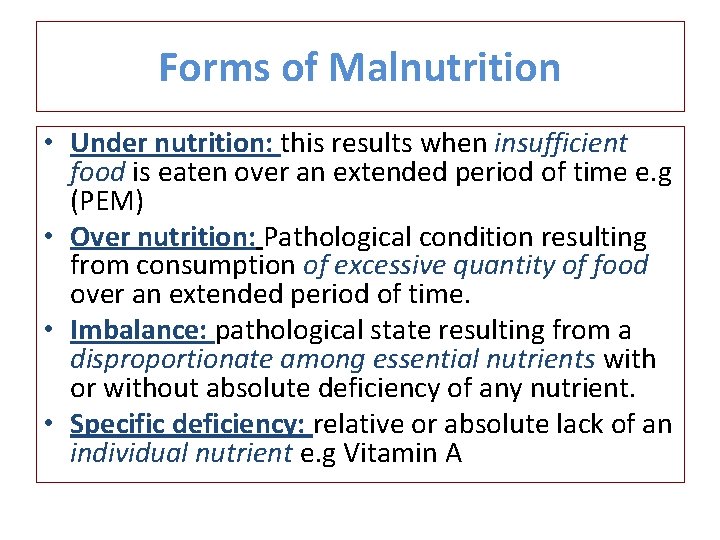
Forms of Malnutrition • Under nutrition: this results when insufficient food is eaten over an extended period of time e. g (PEM) • Over nutrition: Pathological condition resulting from consumption of excessive quantity of food over an extended period of time. • Imbalance: pathological state resulting from a disproportionate among essential nutrients with or without absolute deficiency of any nutrient. • Specific deficiency: relative or absolute lack of an individual nutrient e. g Vitamin A
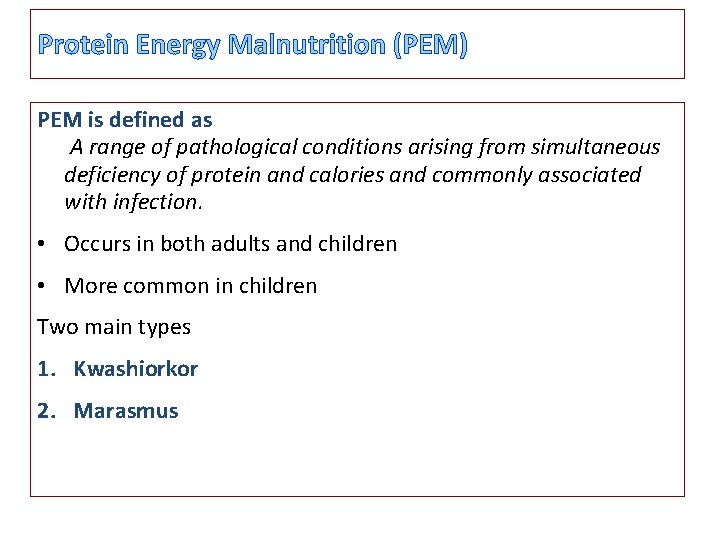
Protein Energy Malnutrition (PEM) PEM is defined as A range of pathological conditions arising from simultaneous deficiency of protein and calories and commonly associated with infection. • Occurs in both adults and children • More common in children Two main types 1. Kwashiorkor 2. Marasmus
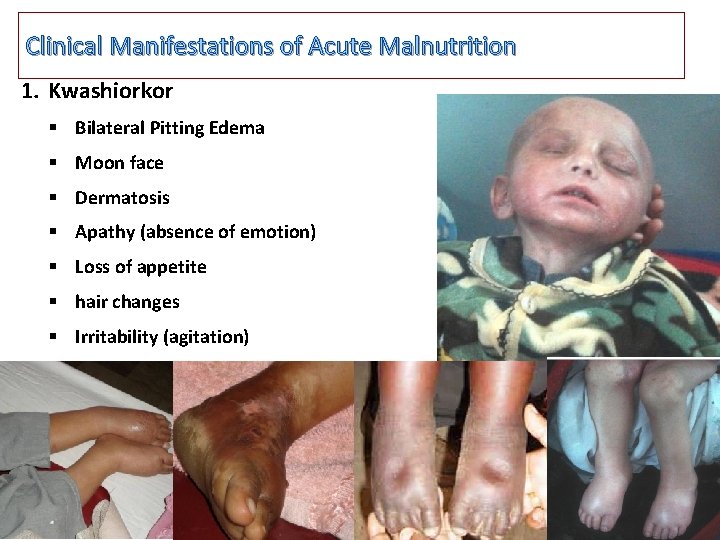
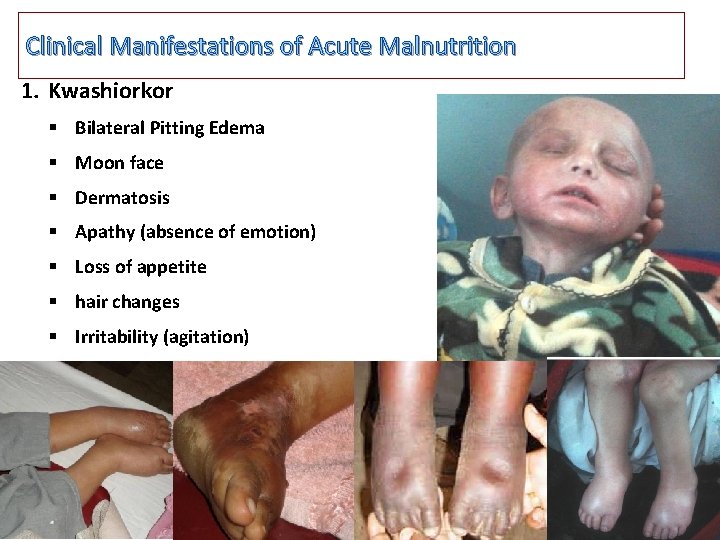
Clinical Manifestations of Acute Malnutrition 1. Kwashiorkor § Bilateral Pitting Edema § Moon face § Dermatosis § Apathy (absence of emotion) § Loss of appetite § hair changes § Irritability (agitation)
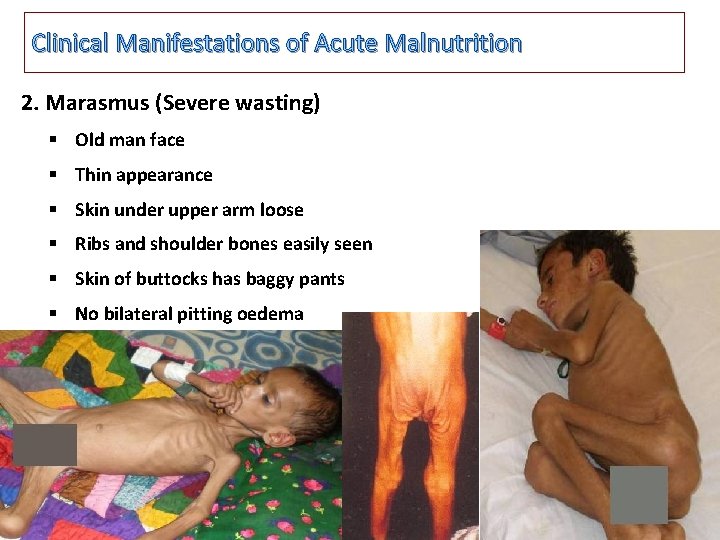
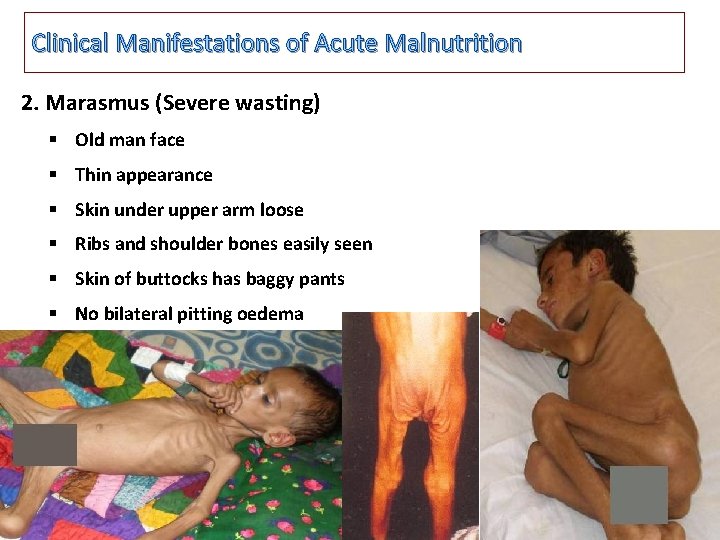
Clinical Manifestations of Acute Malnutrition 2. Marasmus (Severe wasting) § Old man face § Thin appearance § Skin under upper arm loose § Ribs and shoulder bones easily seen § Skin of buttocks has baggy pants § No bilateral pitting oedema
Prevention of Malnutrition • Primary Prevention • Health Education to mothers about good nutrition and food hygiene through Lady Health Workers • Immunization of children. • Growth monitoring on Growth Charts specially of all children under 5 years of age • Secondary Prevention • Mass Screening of high risk populations, using simple tools like Weight for age or MUAC. • Tertiary Prevention • Good Nutritional Care, supplementary feedings and rehabilitation, counseling of mothers.
Chronic malnutrition • It is the impair development of body function due to long term deficiency/excess in nutrient/energy intake. e. g. , stunting.
ACUTE MALNUTRITION Types 1. 2. 3. Moderate Severe (without Complication) Severe (with Complication)
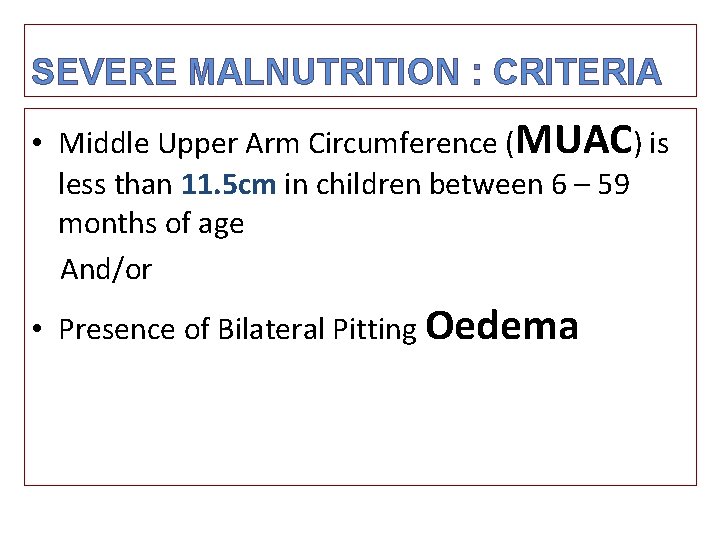
SEVERE MALNUTRITION : CRITERIA • Middle Upper Arm Circumference (MUAC) is less than 11. 5 cm in children between 6 – 59 months of age And/or • Presence of Bilateral Pitting Oedema
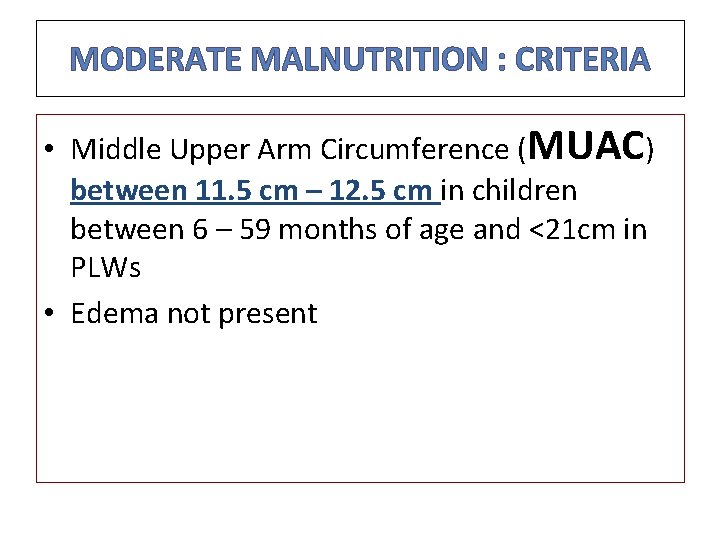
MODERATE MALNUTRITION : CRITERIA • Middle Upper Arm Circumference (MUAC) between 11. 5 cm – 12. 5 cm in children between 6 – 59 months of age and <21 cm in PLWs • Edema not present
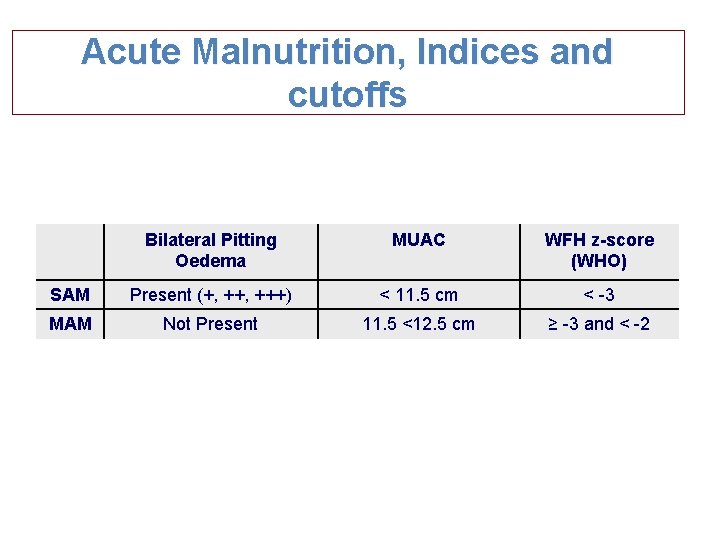
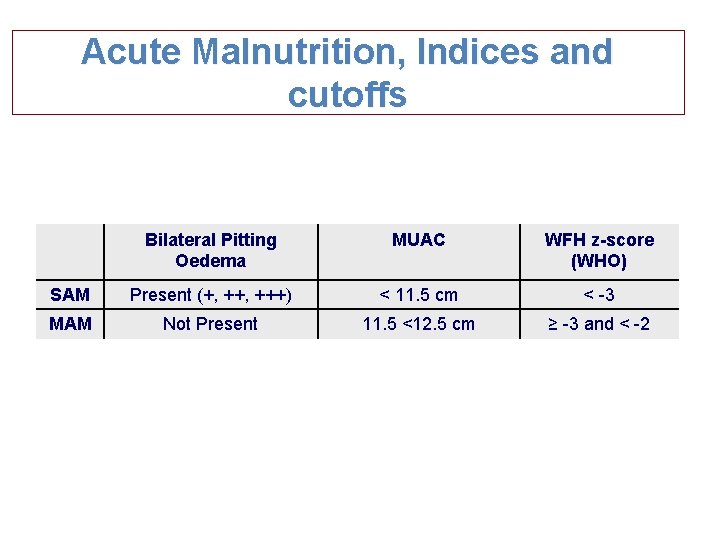
Acute Malnutrition, Indices and cutoffs Bilateral Pitting Oedema MUAC WFH z-score (WHO) SAM Present (+, +++) < 11. 5 cm < -3 MAM Not Present 11. 5 <12. 5 cm ≥ -3 and < -2
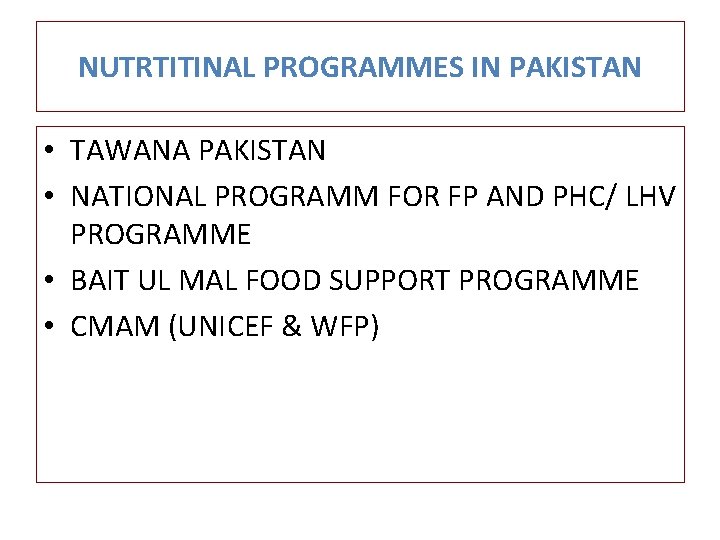
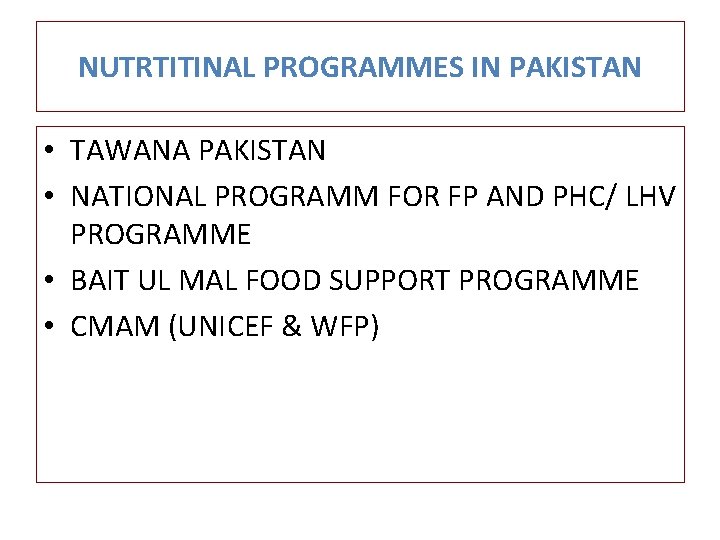
NUTRTITINAL PROGRAMMES IN PAKISTAN • TAWANA PAKISTAN • NATIONAL PROGRAMM FOR FP AND PHC/ LHV PROGRAMME • BAIT UL MAL FOOD SUPPORT PROGRAMME • CMAM (UNICEF & WFP)
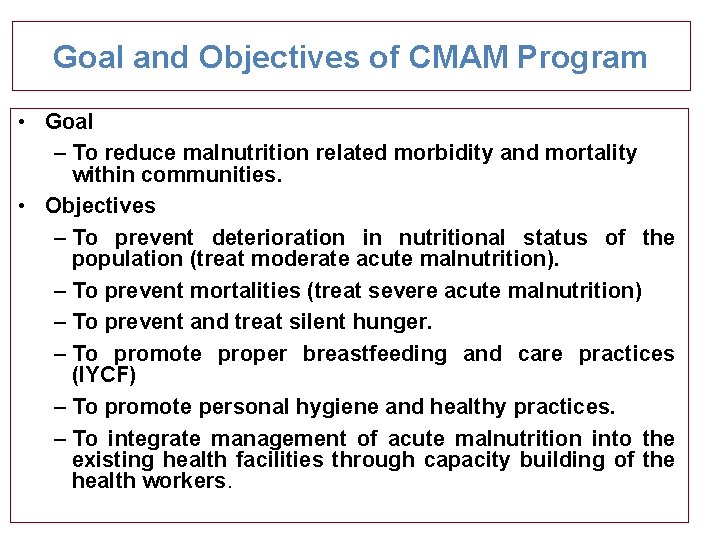
Goal and Objectives of CMAM Program • Goal – To reduce malnutrition related morbidity and mortality within communities. • Objectives – To prevent deterioration in nutritional status of the population (treat moderate acute malnutrition). – To prevent mortalities (treat severe acute malnutrition) – To prevent and treat silent hunger. – To promote proper breastfeeding and care practices (IYCF) – To promote personal hygiene and healthy practices. – To integrate management of acute malnutrition into the existing health facilities through capacity building of the health workers.
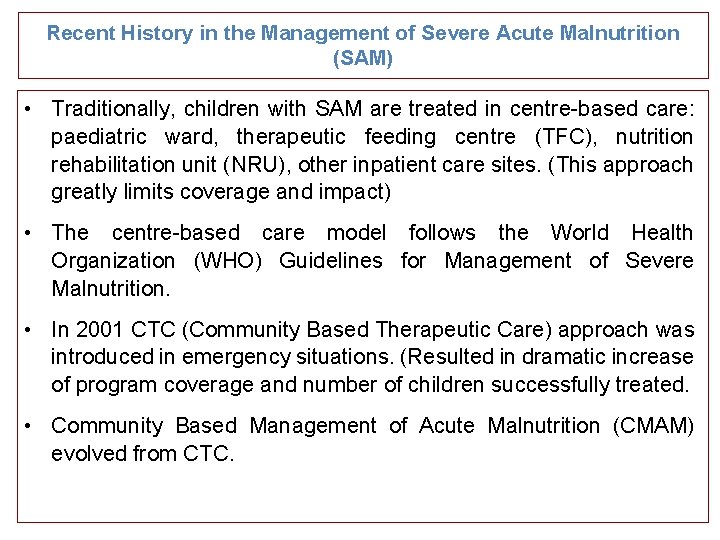
Recent History in the Management of Severe Acute Malnutrition (SAM) • Traditionally, children with SAM are treated in centre-based care: paediatric ward, therapeutic feeding centre (TFC), nutrition rehabilitation unit (NRU), other inpatient care sites. (This approach greatly limits coverage and impact) • The centre-based care model follows the World Health Organization (WHO) Guidelines for Management of Severe Malnutrition. • In 2001 CTC (Community Based Therapeutic Care) approach was introduced in emergency situations. (Resulted in dramatic increase of program coverage and number of children successfully treated. • Community Based Management of Acute Malnutrition (CMAM) evolved from CTC.
CMAM ? Ø Community based management of acute malnutrition. Ø Community based public health approach to treating malnutrition Ø Benefits at individual & population level Ø Improves access to care Ø Close liaison with community improves case coverage (proportion of diseased subjects receiving care) Ø Reduces opportunity costs to family Ø Supports family coping mechanisms and /or family unit
CMAM • A community-based approach to treating SAM – CMAM helps identify SAM in the community before the onset of complications (Screening in Community through LHWs/CHWs/ Volunteers) – Most children with SAM without medical complications (80%) can be treated as outpatients at accessible, decentralised sites with RUTF. – Children with SAM and medical complications are treated as inpatients in SC. – Community outreach for community involvement and early detection and referral of cases • Also known as community-based therapeutic care (CTC), ambulatory care, home-based care (HBC) for the management of SAM
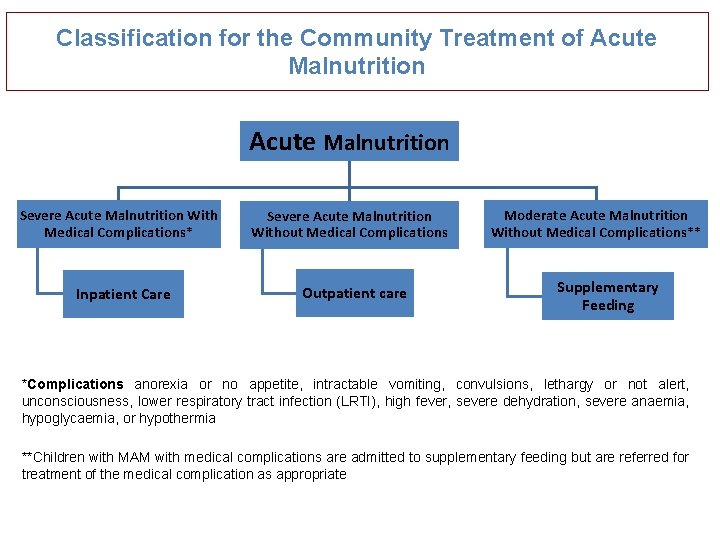
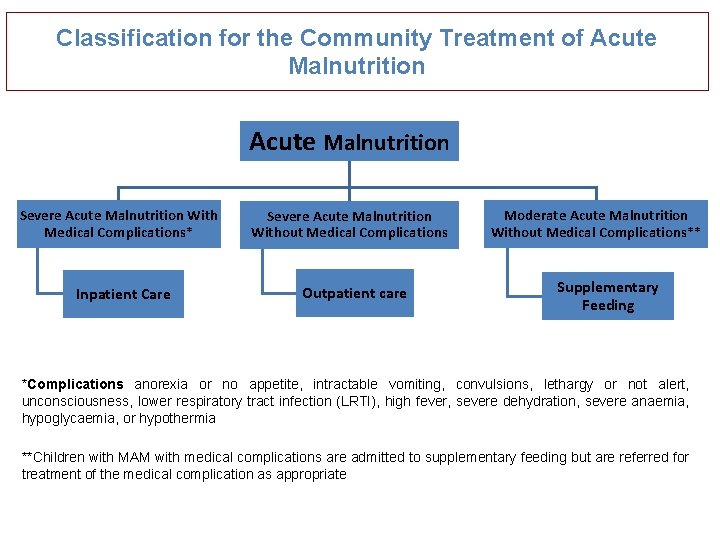
Classification for the Community Treatment of Acute Malnutrition Severe Acute Malnutrition With Medical Complications* Inpatient Care Severe Acute Malnutrition Without Medical Complications Outpatient care Moderate Acute Malnutrition Without Medical Complications** Supplementary Feeding *Complications anorexia or no appetite, intractable vomiting, convulsions, lethargy or not alert, unconsciousness, lower respiratory tract infection (LRTI), high fever, severe dehydration, severe anaemia, hypoglycaemia, or hypothermia **Children with MAM with medical complications are admitted to supplementary feeding but are referred for treatment of the medical complication as appropriate
4 Principles of CMAM 1. 2. 3. 4. Maximum access and coverage Timeliness Appropriate medical and nutrition care Care for as long as needed (Following these steps ensure maximum public health impact)

Timeliness (continued) • Find children before SAM becomes serious and medical complications arise • Good community outreach is essential • Screening and referral by outreach workers (e. g. , community health workers [CHWs], volunteers)
THANK YOU
 Hyperglyceremia
Hyperglyceremia Nutritional diseases
Nutritional diseases Nutritional diseases
Nutritional diseases Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Fasih ur rehman
Fasih ur rehman Ben rehman
Ben rehman Dr waheed rehman
Dr waheed rehman Tahira rehman
Tahira rehman Abdul rehman chughtai paintings
Abdul rehman chughtai paintings Asif əsgərov
Asif əsgərov Amir asif
Amir asif Minahil asif
Minahil asif Cremagliera tonda
Cremagliera tonda Ltad evreleri
Ltad evreleri Asif international
Asif international Barrel chest
Barrel chest Collection of programs written to service other programs.
Collection of programs written to service other programs. Civil rights in child nutrition programs
Civil rights in child nutrition programs Civil rights in child nutrition programs
Civil rights in child nutrition programs Child nutrition food buying guide
Child nutrition food buying guide Civil rights training child nutrition programs
Civil rights training child nutrition programs Enteral parenteral beslenme
Enteral parenteral beslenme How can we crack nature’s secret nutritional code?
How can we crack nature’s secret nutritional code? Common nutritional health problem in bangladesh
Common nutritional health problem in bangladesh Nutritional status assessment
Nutritional status assessment Ada 411
Ada 411 Chapter 28 nutritional support and iv therapy
Chapter 28 nutritional support and iv therapy Nutritional intervention
Nutritional intervention Nutritional management of diabetes mellitus
Nutritional management of diabetes mellitus Malnutrition definition
Malnutrition definition Hypnum sp nutritional habits
Hypnum sp nutritional habits Conclusion of malnutrition
Conclusion of malnutrition Mini nutritional assessment
Mini nutritional assessment Ruminant animals
Ruminant animals Nutritional requirements of plants
Nutritional requirements of plants Abcd of nutritional assessment
Abcd of nutritional assessment Define nutritional epidemiology
Define nutritional epidemiology Public health nutrition definition
Public health nutrition definition Culinary nutrition definition
Culinary nutrition definition Chapter 28 nutritional support and iv therapy
Chapter 28 nutritional support and iv therapy