Hemostasis Hemostasis Hemostasis or haemostasis from the Ancient



- Slides: 57
Hemostasis
Hemostasis • Hemostasis or haemostasis (from the Ancient Greek: αἱμόστασις haimóstasis ) is a process which causes bleeding to stop. • Purpose : to keep blood within the damaged blood vessel • It is the first stage of wound healing • The opposite of hemostasis is hemorrhage).
Platelets
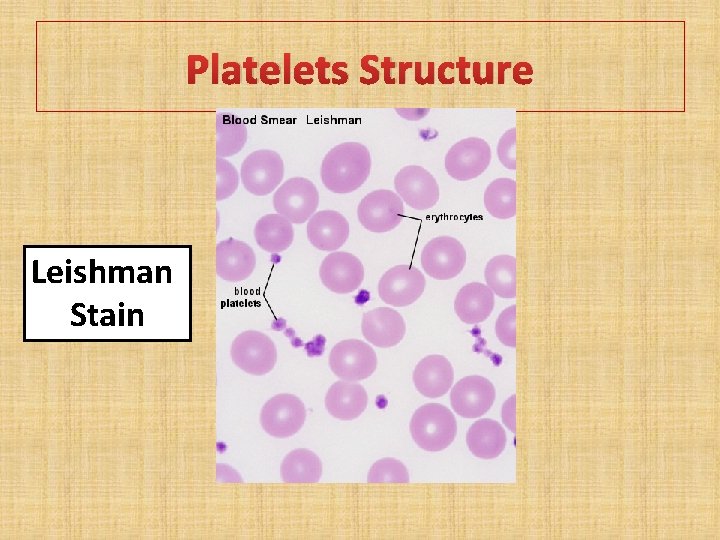
Platelets (Thrombocytes) • Is small, non-nucleated, granulated bodies • Reddish purple granules with Leishman stain • Size is between 2 and 4. • May be circular or oval shaped. • Normal count 1. 5 – 4 lakhs/cu mm of blood.
Platelets (Thrombocytes) • Life span is about 10 days. • The cells are produced by the megakaryocytes present in red bone marrow. • Thrombopoietein- regulate the synthesis of platelets • Site of destruction is mainly spleen, which contains reticulo-endothelial system (RES).
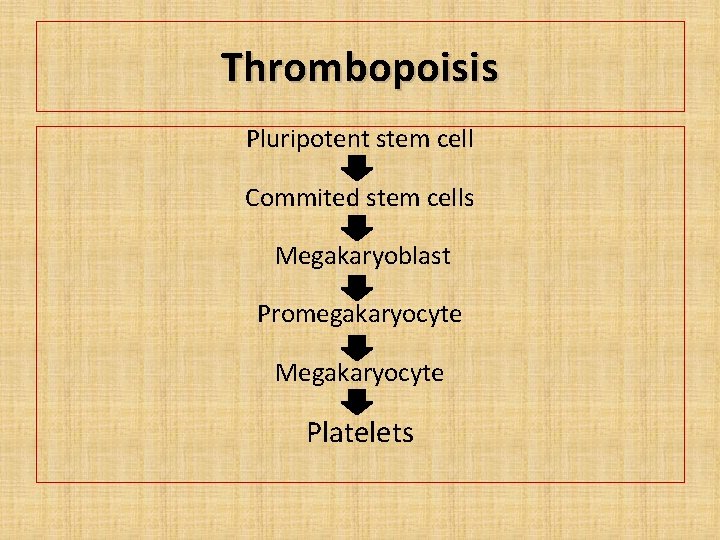
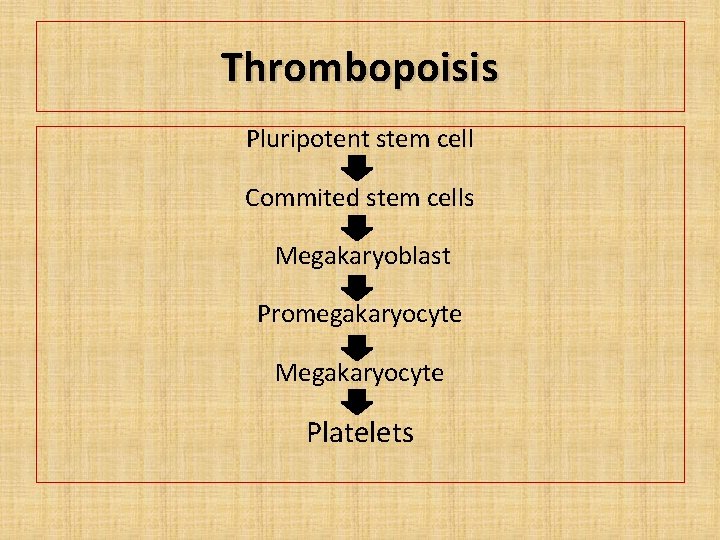
Thrombopoisis Pluripotent stem cell Commited stem cells Megakaryoblast Promegakaryocyte Megakaryocyte Platelets
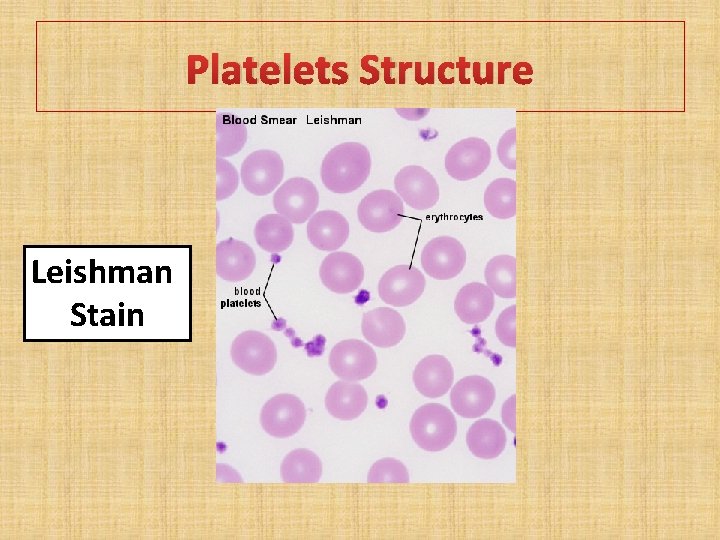
Platelets Structure Leishman Stain
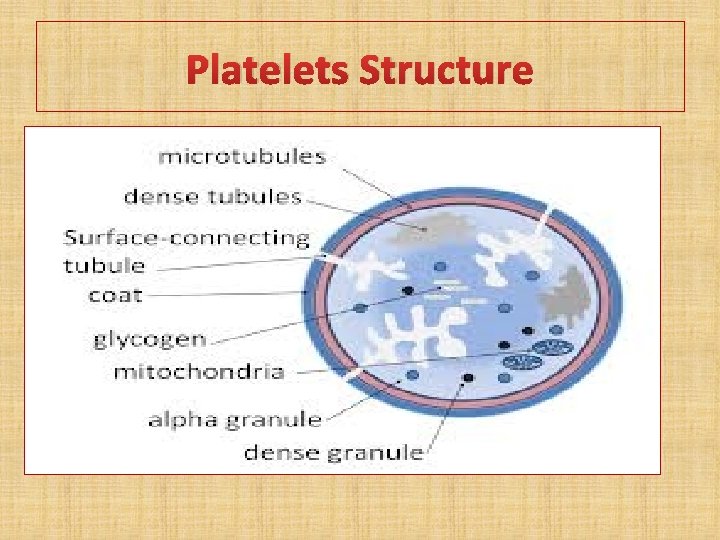
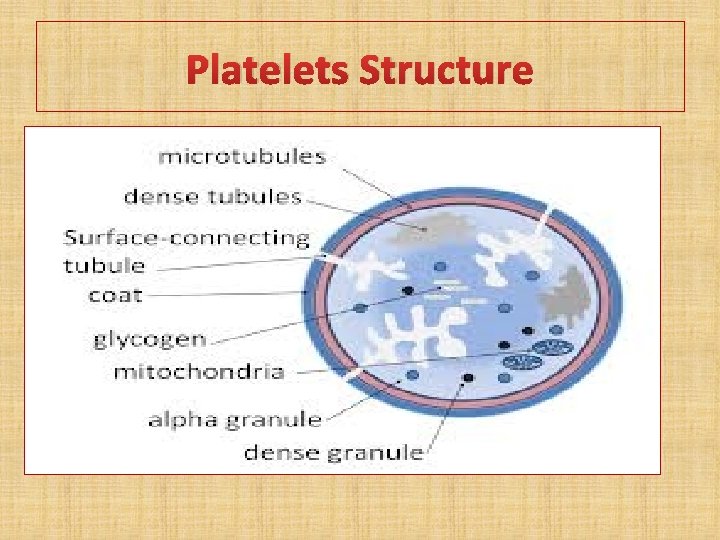
Platelets Structure
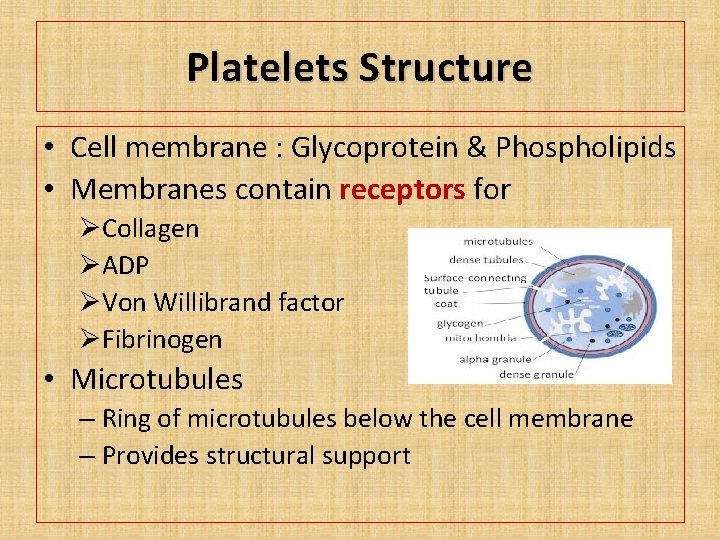
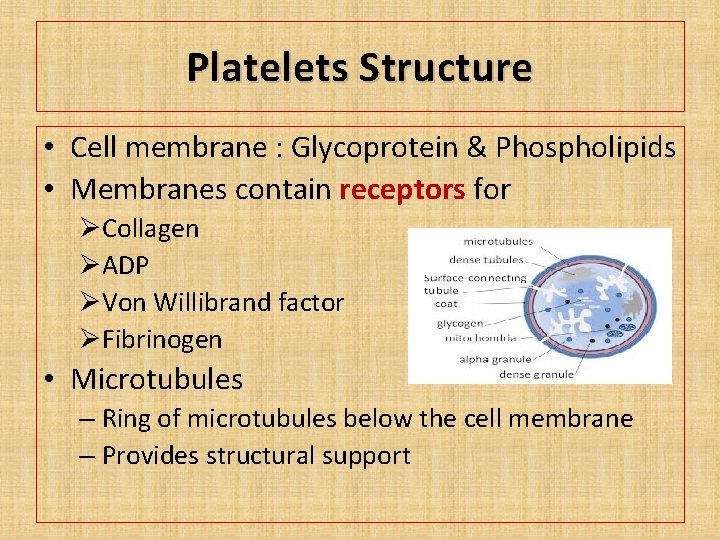
Platelets Structure • Cell membrane : Glycoprotein & Phospholipids • Membranes contain receptors for ØCollagen ØADP ØVon Willibrand factor ØFibrinogen • Microtubules – Ring of microtubules below the cell membrane – Provides structural support

Platelets Structure Cytoplasm– • Proteins: – – – • • Actin Myosin Thrombosthenin Lysosomes Granules
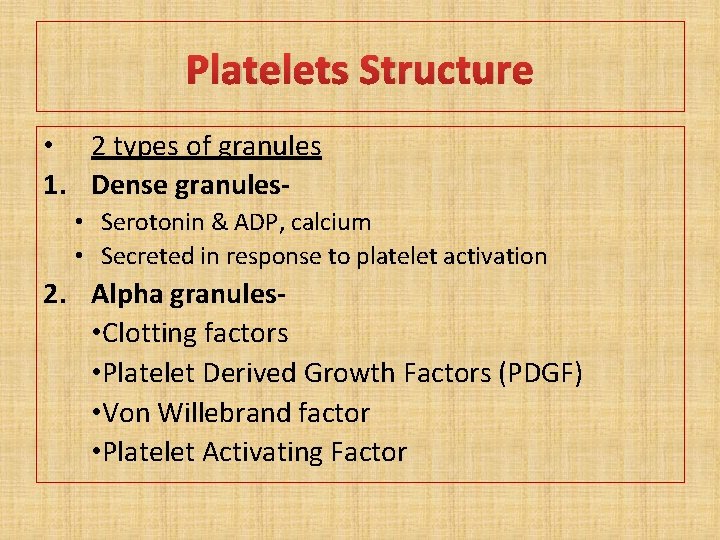
Platelets Structure • 2 types of granules 1. Dense granules • Serotonin & ADP, calcium • Secreted in response to platelet activation 2. Alpha granules • Clotting factors • Platelet Derived Growth Factors (PDGF) • Von Willebrand factor • Platelet Activating Factor
Functions of Platelets 1. 2. 3. 4. 5. Hemostasis (Platelet Plug Formation) Blood coagulation Clot retraction Repair of capillary endothelium. Phagocytosis.
Hemostasis • Hemostasis is the spontaneous arrest of bleeding. • By the process of forming clots in the walls of damaged blood vessels and maintaining blood in a fluid state in the vascular system
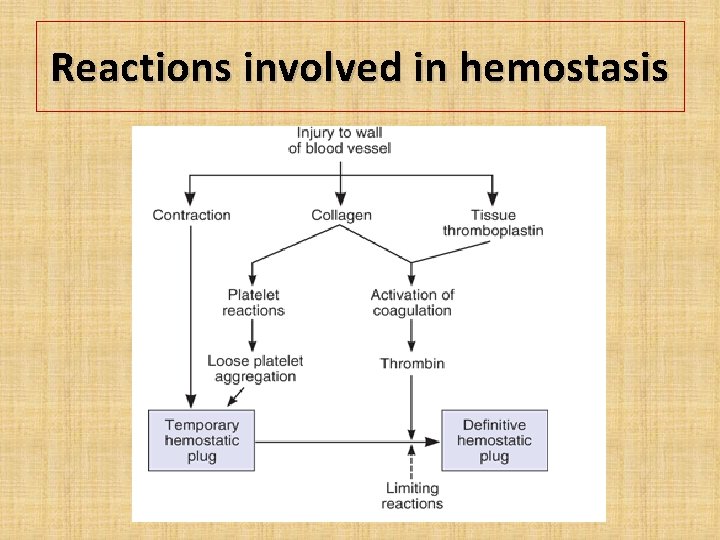
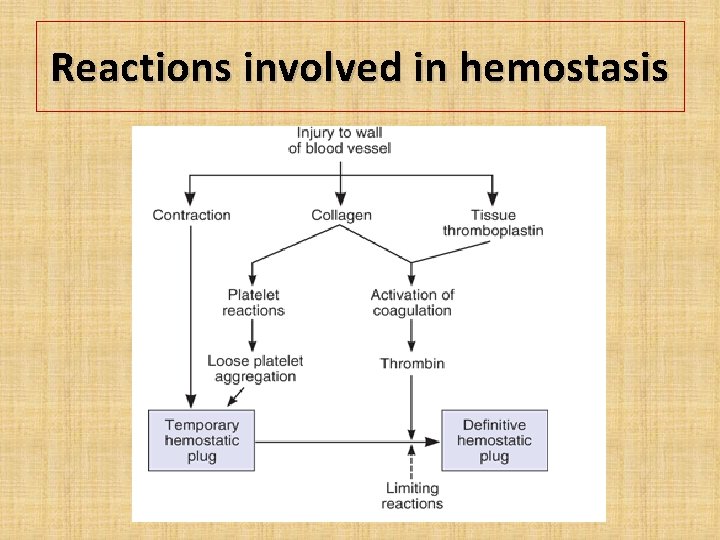
Hemostasis • Hemostasis is brought about by three mechanisms : 1. Vasoconstriction 2. Platelet plug formation 3. Coagulation of blood
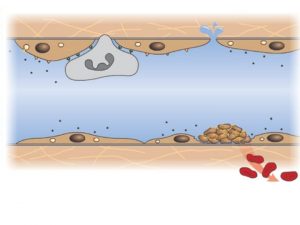
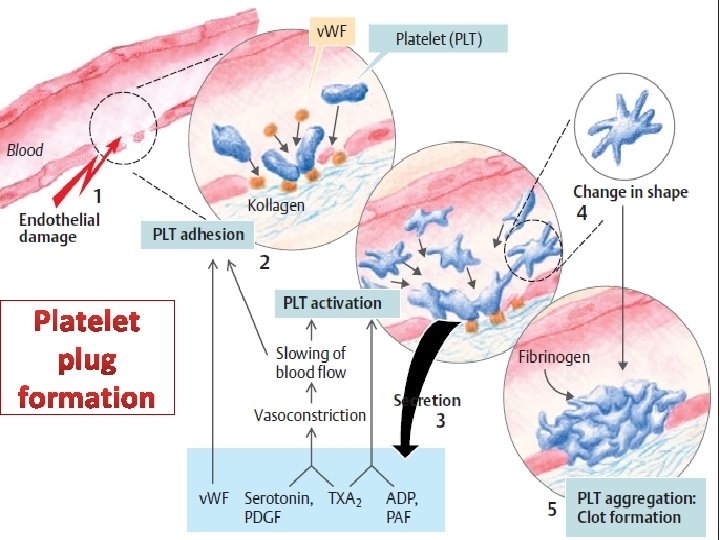
Vasoconstriction • Constriction of the blood vessel is a local phenomenon • The collagen fibers are exposed in a damaged blood vessel • Platelet Activation : The platelets adhere to the collagen and get activated (accelerated by von Willebrand factor) • Activated platelets secrete serotonin and other vasoconstrictors
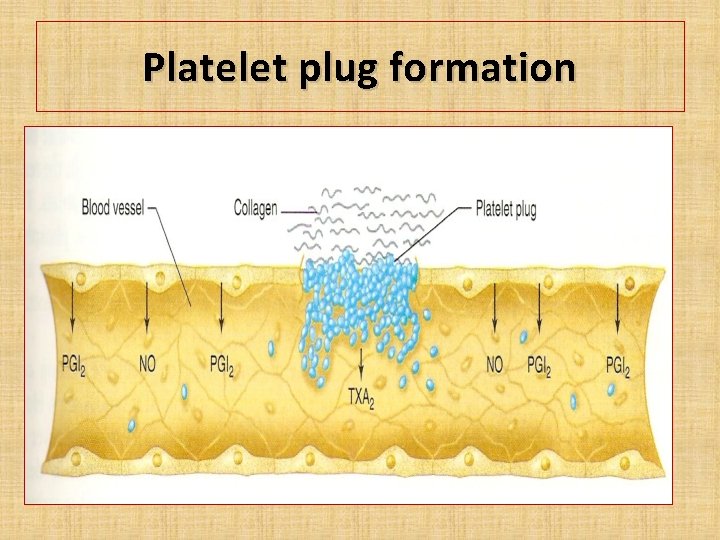
Platelet plug formation • Platelet Adhesion • Platelet Activation • Platelet Aggregation
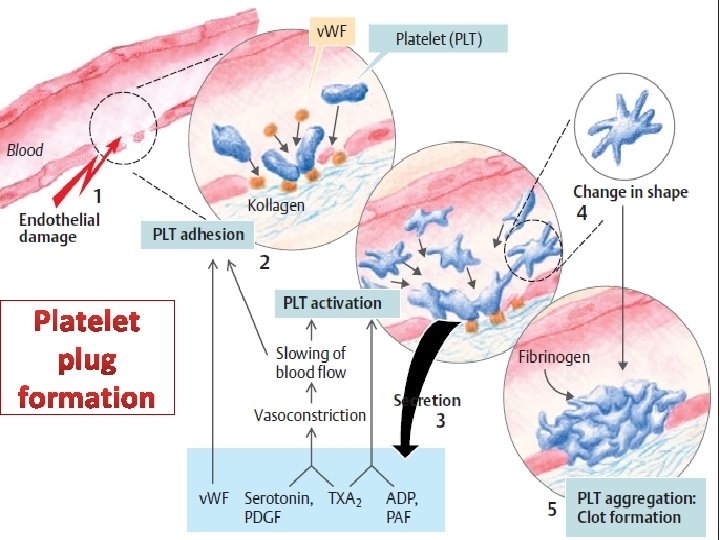
Platelet plug formation
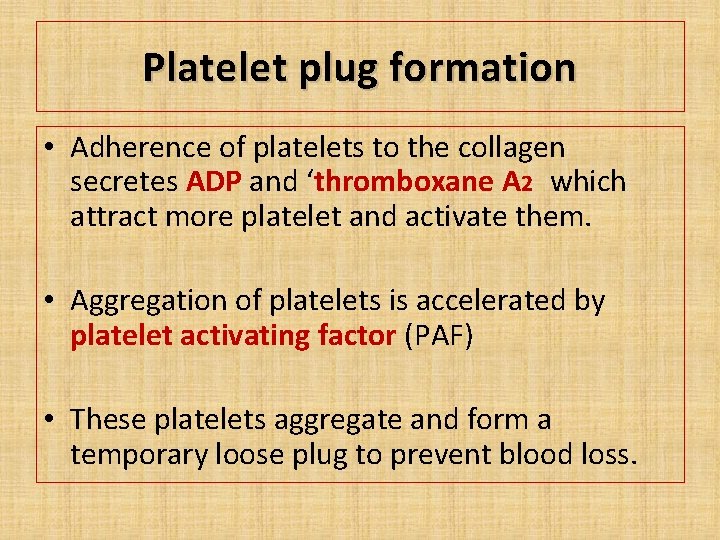
Platelet plug formation • Adherence of platelets to the collagen secretes ADP and ‘thromboxane A 2 which attract more platelet and activate them. • Aggregation of platelets is accelerated by platelet activating factor (PAF) • These platelets aggregate and form a temporary loose plug to prevent blood loss.
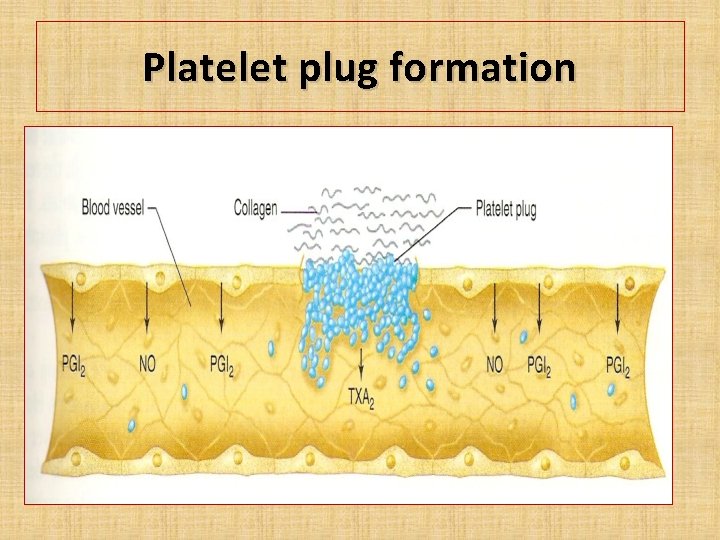
Platelet plug formation
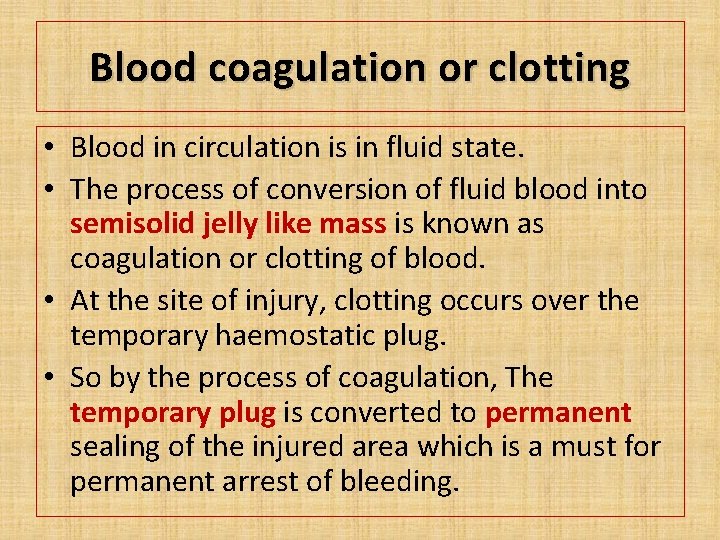
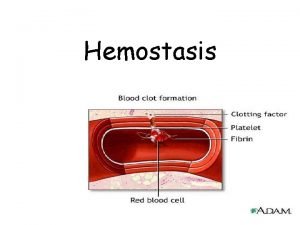
Blood coagulation or clotting • Blood in circulation is in fluid state. • The process of conversion of fluid blood into semisolid jelly like mass is known as coagulation or clotting of blood. • At the site of injury, clotting occurs over the temporary haemostatic plug. • So by the process of coagulation, The temporary plug is converted to permanent sealing of the injured area which is a must for permanent arrest of bleeding.
Blood coagulation or clotting Why should clotting occur on hemostatic plug? • Hemostatic plug is not stable one. • If clotting doesn’t take place on this plug, the hemostatic plug may get washed away. • This results in prolonged bleeding • Seen in certain coagulation disorder like hemophilia.
Reactions involved in hemostasis

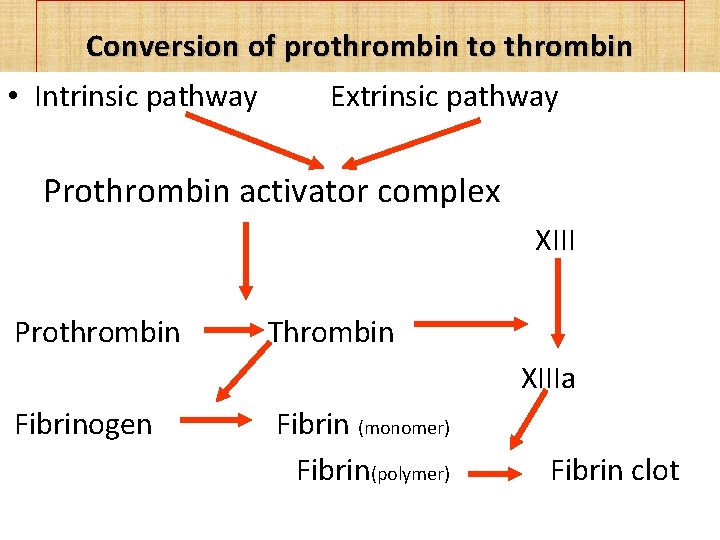
Clotting 1. Formation of Prothrombin Activator 1. Intrinsic system 2. Extrinsic system 2. Conversion of prothrombin to thrombin 3. Conversion of fibrinogen to fibrin and clot formation
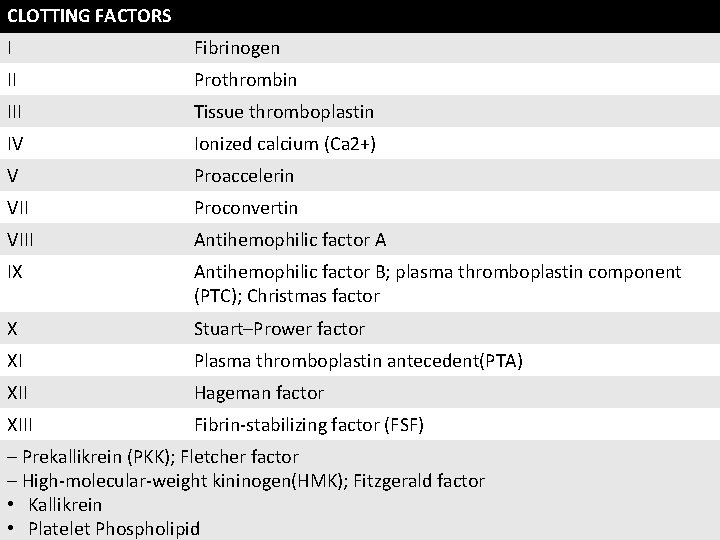
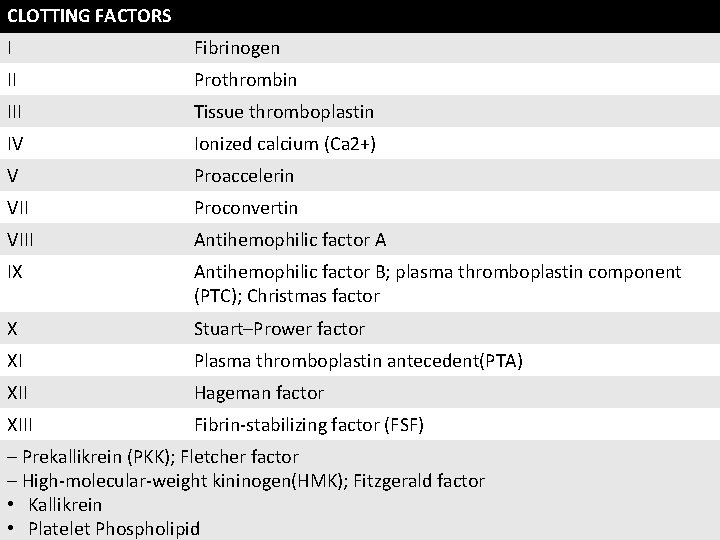
CLOTTING FACTORS I Fibrinogen II Prothrombin III Tissue thromboplastin IV Ionized calcium (Ca 2+) V Proaccelerin VII Proconvertin VIII Antihemophilic factor A IX Antihemophilic factor B; plasma thromboplastin component (PTC); Christmas factor X Stuart–Prower factor XI Plasma thromboplastin antecedent(PTA) XII Hageman factor XIII Fibrin-stabilizing factor (FSF) – Prekallikrein (PKK); Fletcher factor – High-molecular-weight kininogen(HMK); Fitzgerald factor • Kallikrein • Platelet Phospholipid
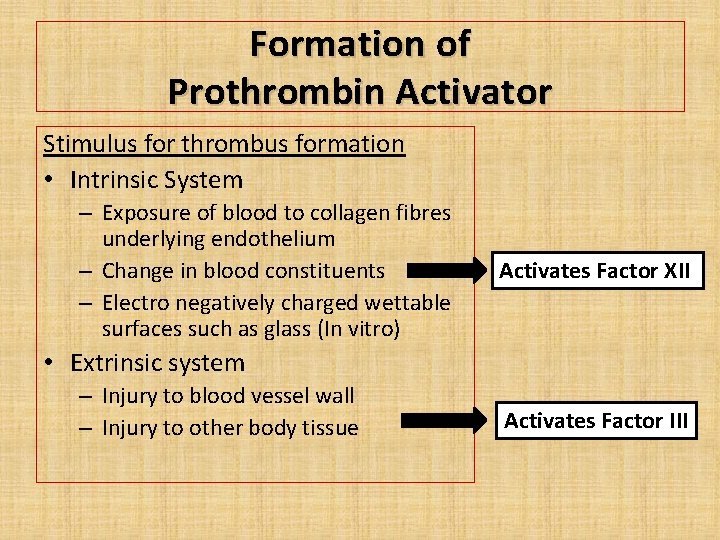
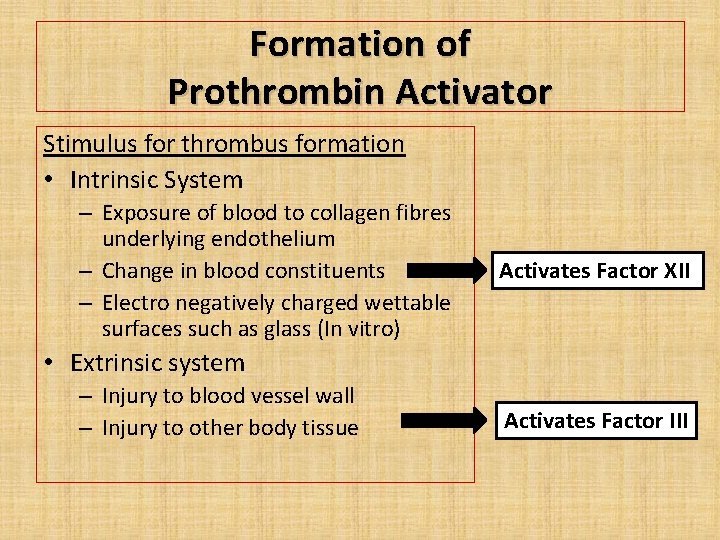
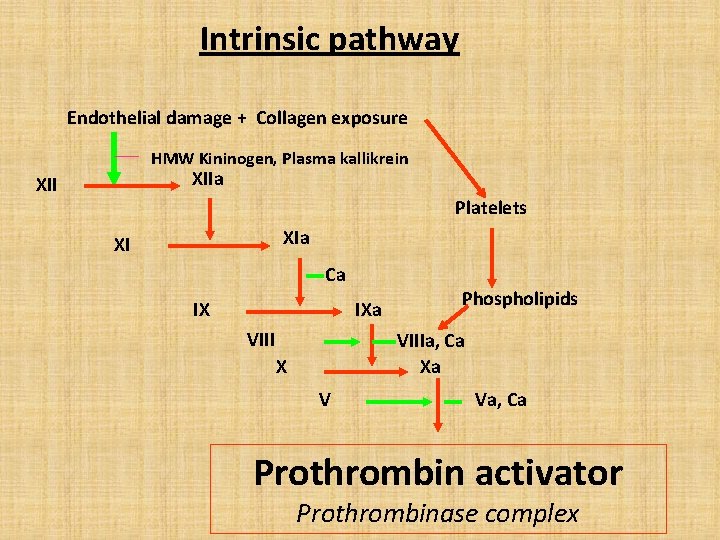
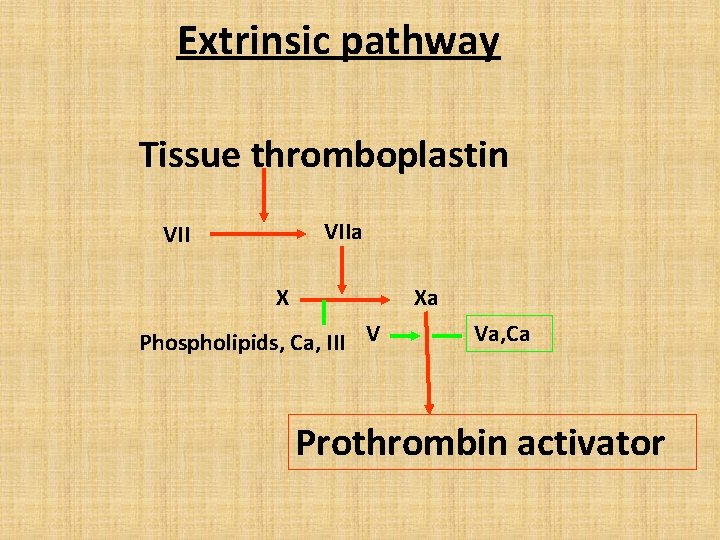
Formation of Prothrombin Activator Stimulus for thrombus formation • Intrinsic System – Exposure of blood to collagen fibres underlying endothelium – Change in blood constituents – Electro negatively charged wettable surfaces such as glass (In vitro) Activates Factor XII • Extrinsic system – Injury to blood vessel wall – Injury to other body tissue Activates Factor III
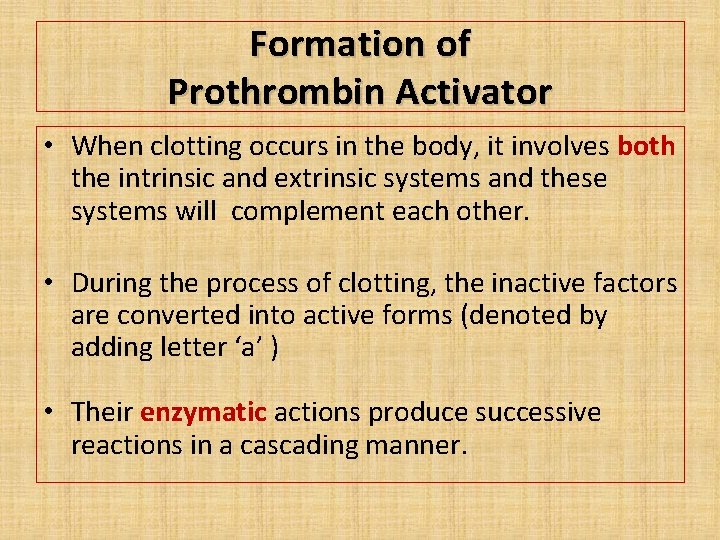
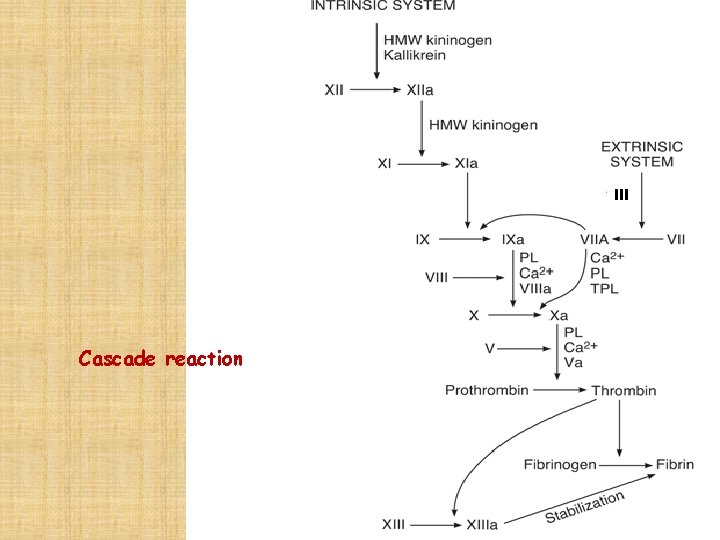
Formation of Prothrombin Activator • When clotting occurs in the body, it involves both the intrinsic and extrinsic systems and these systems will complement each other. • During the process of clotting, the inactive factors are converted into active forms (denoted by adding letter ‘a’ ) • Their enzymatic actions produce successive reactions in a cascading manner.
Cascade
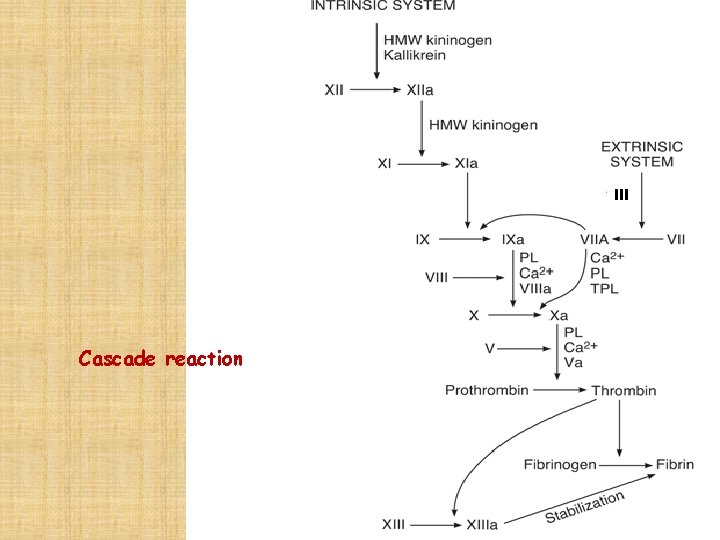
III Cascade reaction
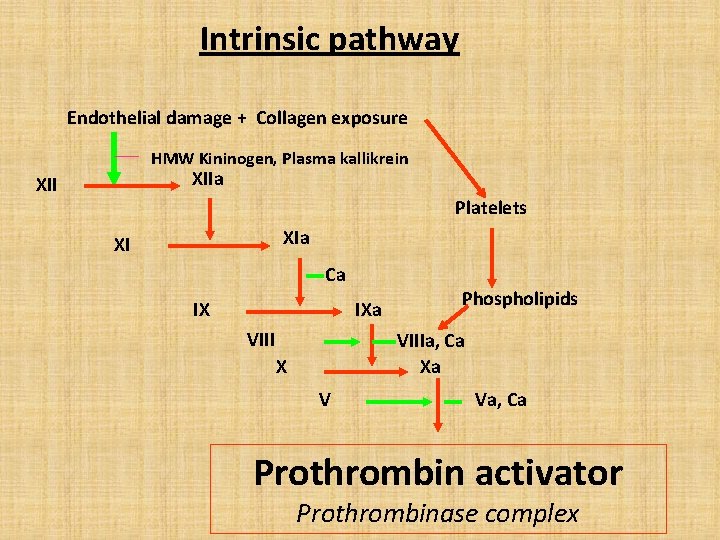
Intrinsic pathway Endothelial damage + Collagen exposure HMW Kininogen, Plasma kallikrein XIIa XII Platelets XIa XI Ca IX IXa VIII Phospholipids VIIIa, Ca Xa X V Va, Ca Prothrombin activator Prothrombinase complex
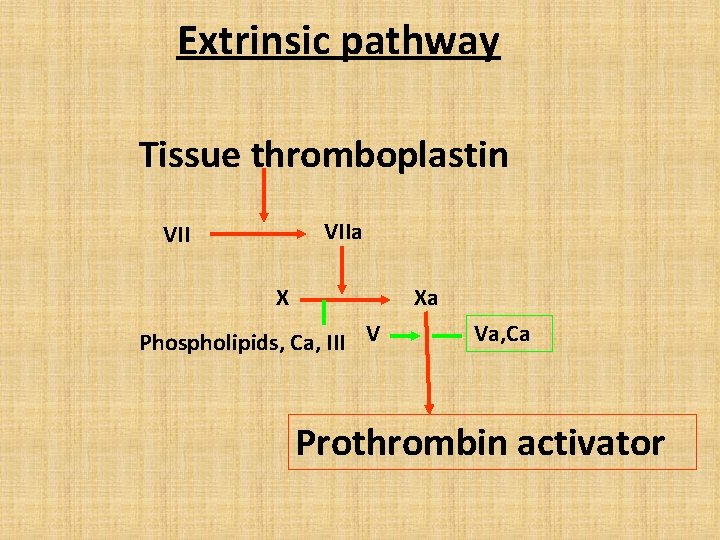
Extrinsic pathway Tissue thromboplastin VIIa VII X Xa Phospholipids, Ca, III V Va, Ca Prothrombin activator
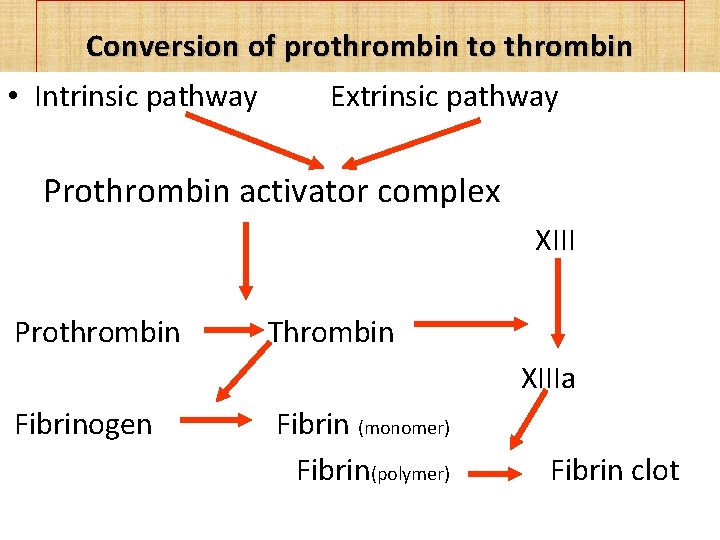
Conversion of prothrombin to thrombin • Intrinsic pathway Extrinsic pathway Prothrombin activator complex XIII Prothrombin Thrombin XIIIa Fibrinogen Fibrin (monomer) Fibrin(polymer) Fibrin clot
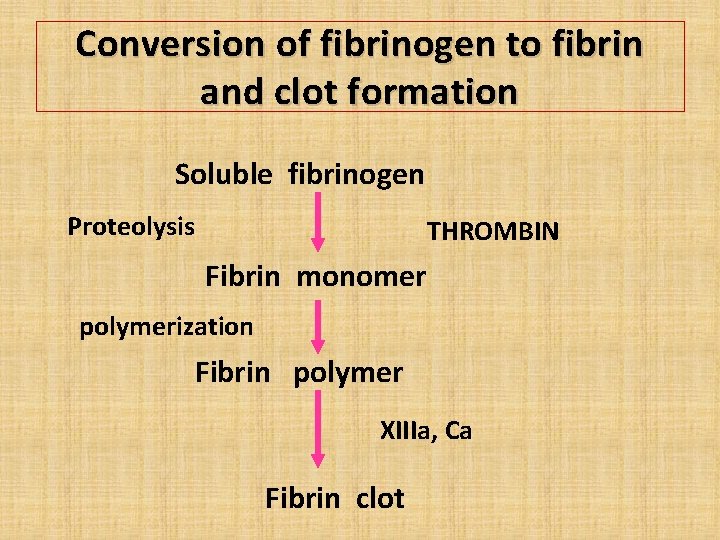
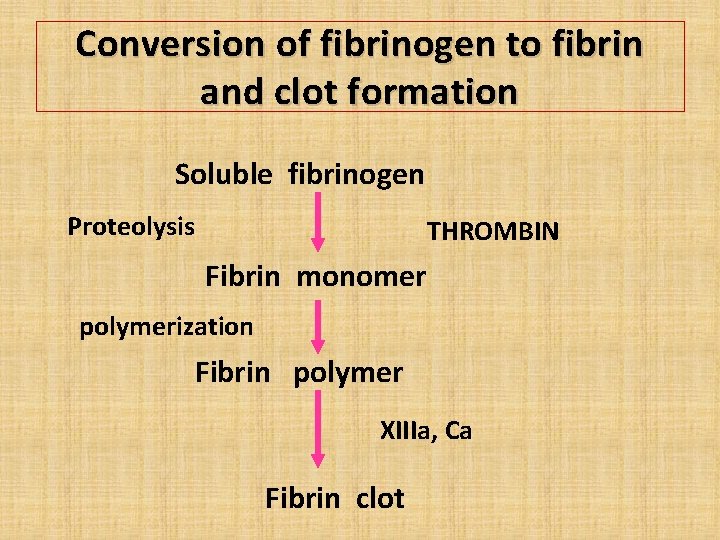
Conversion of fibrinogen to fibrin and clot formation Soluble fibrinogen Proteolysis THROMBIN Fibrin monomer polymerization Fibrin polymer XIIIa, Ca Fibrin clot
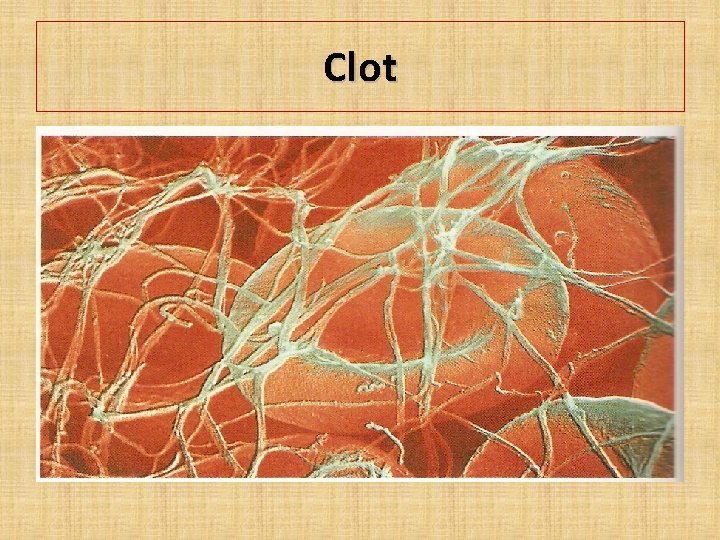
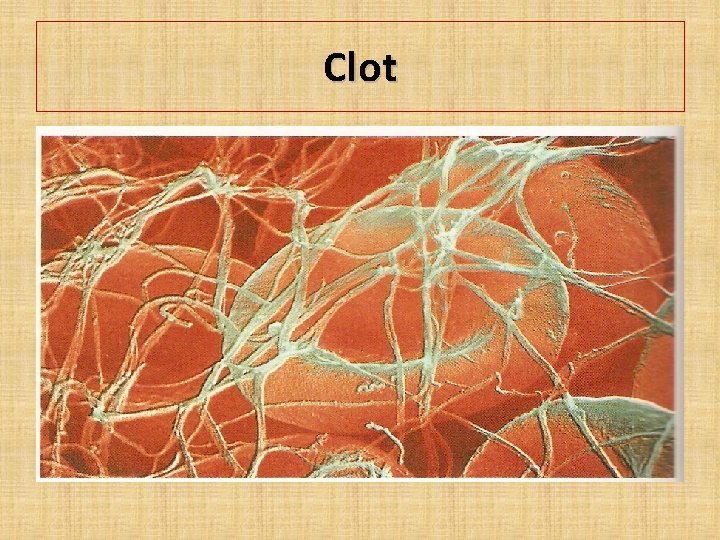
Clot
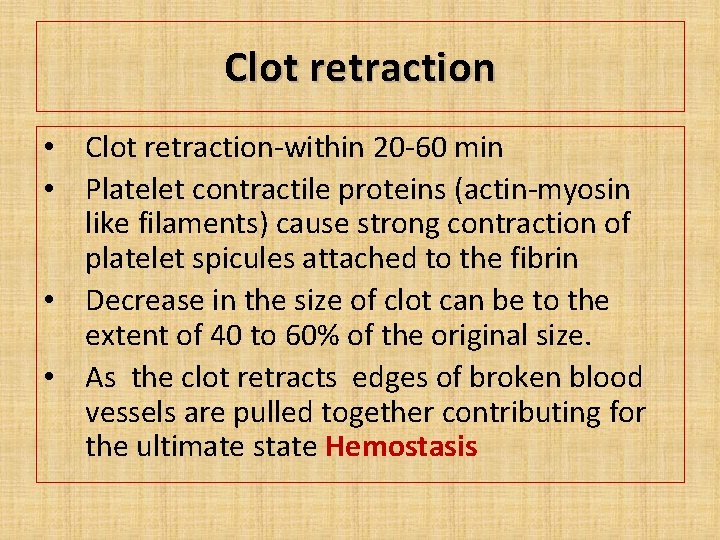
Clot retraction • Clot retraction-within 20 -60 min • Platelet contractile proteins (actin-myosin like filaments) cause strong contraction of platelet spicules attached to the fibrin • Decrease in the size of clot can be to the extent of 40 to 60% of the original size. • As the clot retracts edges of broken blood vessels are pulled together contributing for the ultimate state Hemostasis
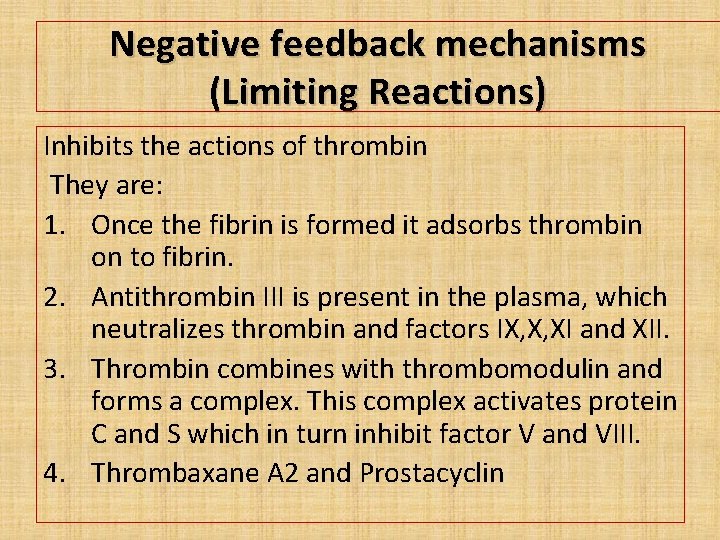
Negative feedback mechanisms (Limiting Reactions) Inhibits the actions of thrombin They are: 1. Once the fibrin is formed it adsorbs thrombin on to fibrin. 2. Antithrombin III is present in the plasma, which neutralizes thrombin and factors IX, X, XI and XII. 3. Thrombin combines with thrombomodulin and forms a complex. This complex activates protein C and S which in turn inhibit factor V and VIII. 4. Thrombaxane A 2 and Prostacyclin
Positive feedback mechanisms during coagulation Positive feed back mechanism comes into play to hasten the process. They are: 1. When once thrombin is formed it brings about conversion of prothrombin to thrombin by autocatalytic reaction. 2. Thrombin also activates factors V, VIII, IX, X, XII and also XIII.
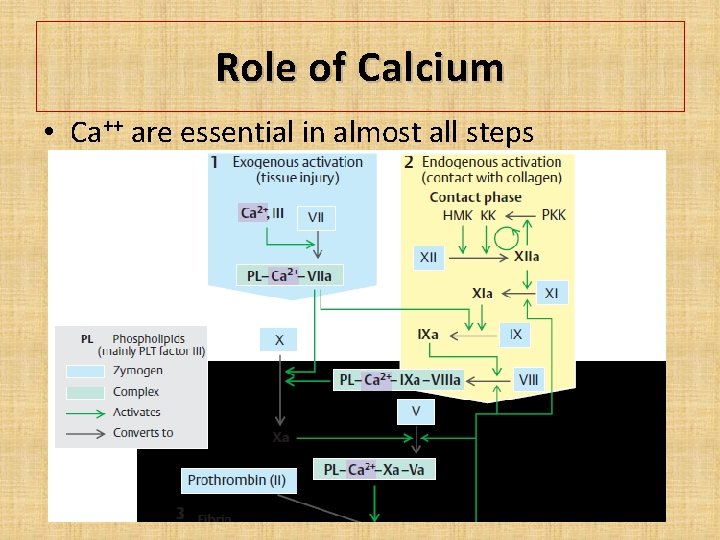
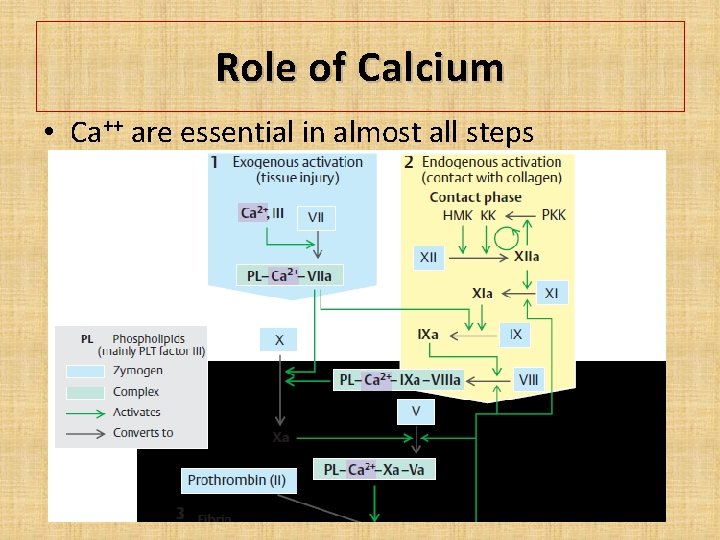
Role of Calcium • Ca++ are essential in almost all steps
Role of platelets in clotting • Platelets contribute for coagulation of blood by releasing substance like phospholipids • Phospholipids provide a surface for the cascade reactions • Required formation of prothrombin activator by intrinsic system.
Role of Vitamin K • Vitamin K is essential for the synthesis of coagulation factors II, VII, IX and X by the liver. • Post-translational γ-carboxylation of glutamate residues of these factors
Intravascular prevention of blood clotting 1. 2. 3. 4. 5. 6. Movement of blood Smoothness of endothelium Layer of glycocalyx-on the endothelium Secretion of prostacyclin Fibrin threads -85% of the thrombin adsorbed Antithrombin III-Heparin-blocks activity of thrombin & factor IX, X, XII. 7. Thrombomodulin on the surface of the endothelium-binds to thrombin
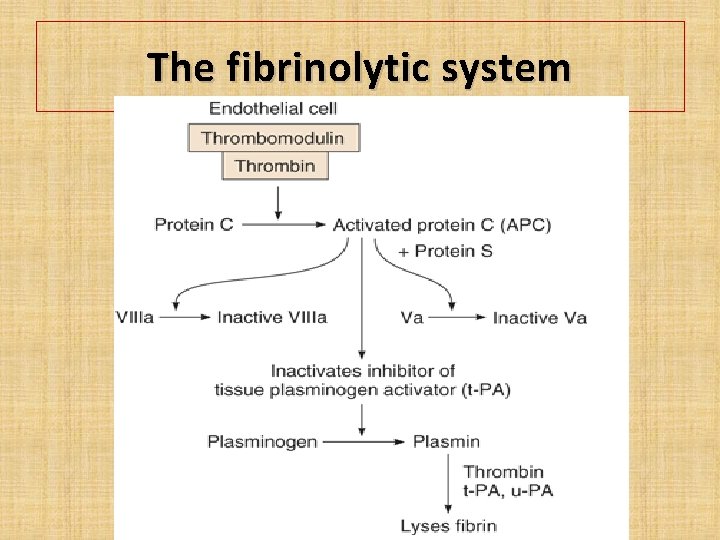
The fibrinolytic system • Fibrinolysis is a process by which the clot is broken down. It is essential to prevent clogging or blocking of capillary. • After the formation of clot, the fibrinolytic system becomes active. • It involves many factors that are present in circulation in inactive form and get activated during fibrinolysis.
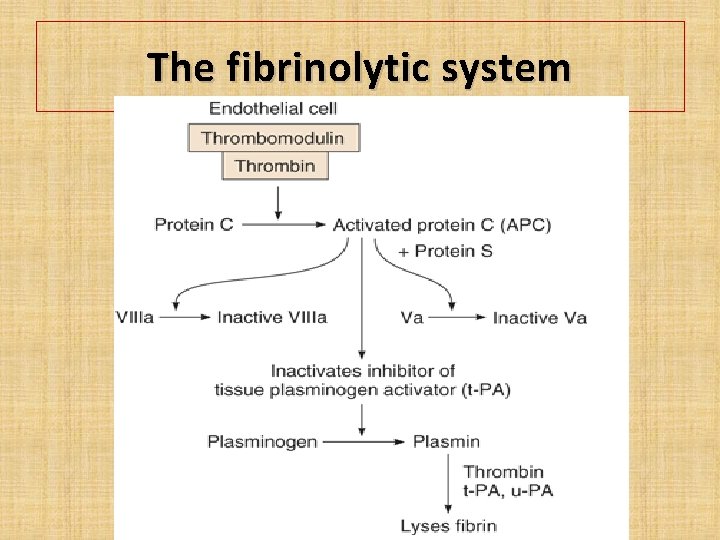
The fibrinolytic system
Plasmin • Plasmin is generated by proteolytic cleavage of plasminogen, a plasma protein synthesized in the liver. • This cleavage is catalyzed by tissue plasminogen activator (t-PA), which is synthesized and secreted by endothelium. • Plasmin is fibrinolytic • It proteolytically cleaves fibrin into fibrin degradation products that inhibit excessive fibrin formation.
Anticoagulants • Anticoagulants are substances that prevent clotting of blood. • They also have important role to play in maintaining the fluidity of blood in circulation. • They can be classified into in vivo and in vitro anticoagulants.
Anticoagulants In vivo anticoagulants are used to prevent coagulation of blood inside the body. • – Eg: heparin and dicoumarol. In vitro anticoagulants are used to prevent coagulation of blood outside the body. • – Eg: heparin, inorganic salts of sodium, potassium and ammonium.
Heparin • • • Produced by the mast cells & basophils. Mechanism of action Combines with Antithrombin III and it neutralizes the action of thrombin Prevents aggregation of platelets Therapeutically used for preventing intra vascular thrombosis, during dialysis, myocardial infarction etc
Dicoumarol • • • Exogenous administration. It can be taken orally. It acts as vitamin K antagonist. Vitamin K is essential for the synthesis of coagulation factors II, VII, IX and X by the liver. Therapeutically dicoumarol is used to prevent intra vascular clotting in long standing bedridden patients.
In vitro anticoagulants • • Heparin Sodium citrate solution (3. 8 %) Double oxalate (ammonium and potassium) EDTA (ethylene diamino tetra acetic acid). • Mechanism : The inorganic salts will remove the ionic calcium by precipitating calcium ions • In vitro anticoagulants are used - outside the body in laboratories and in blood banks.
Tests for hemostasis • • • Bleeding time It’s the time interval from oozing of blood till arrest of bleeding. Normal duration is 1 to 6 min. Clotting time Time interval from oozing of blood till formation of clot Normal duration is 2 to 8 min.
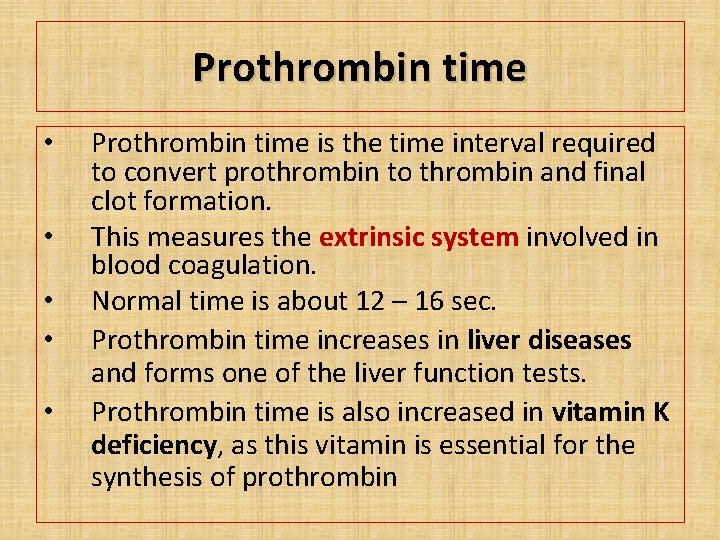
Prothrombin time • • • Prothrombin time is the time interval required to convert prothrombin to thrombin and final clot formation. This measures the extrinsic system involved in blood coagulation. Normal time is about 12 – 16 sec. Prothrombin time increases in liver diseases and forms one of the liver function tests. Prothrombin time is also increased in vitamin K deficiency, as this vitamin is essential for the synthesis of prothrombin
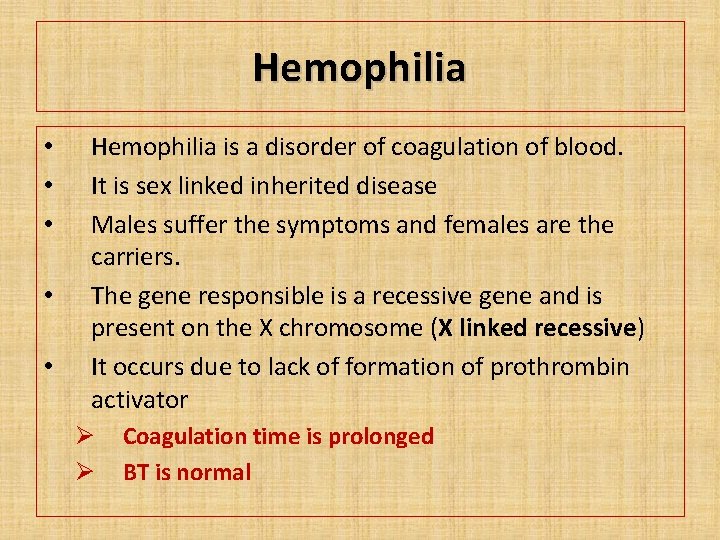
Hemophilia • • • Hemophilia is a disorder of coagulation of blood. It is sex linked inherited disease Males suffer the symptoms and females are the carriers. The gene responsible is a recessive gene and is present on the X chromosome (X linked recessive) It occurs due to lack of formation of prothrombin activator Ø Ø Coagulation time is prolonged BT is normal
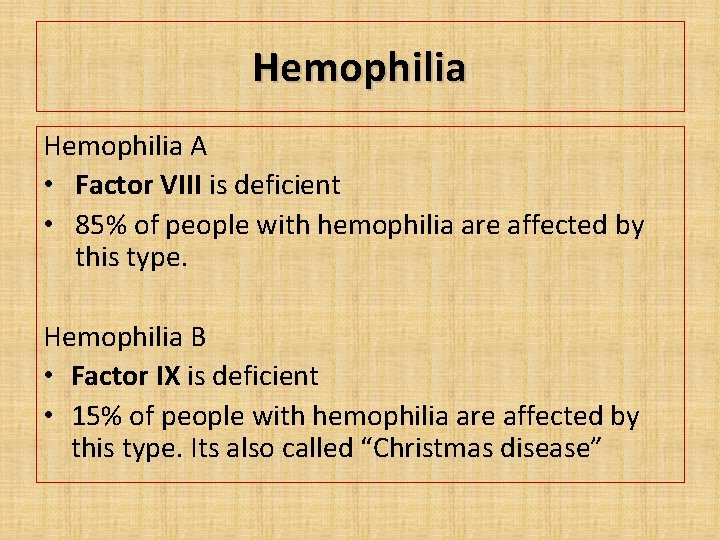
Hemophilia A • Factor VIII is deficient • 85% of people with hemophilia are affected by this type. Hemophilia B • Factor IX is deficient • 15% of people with hemophilia are affected by this type. Its also called “Christmas disease”
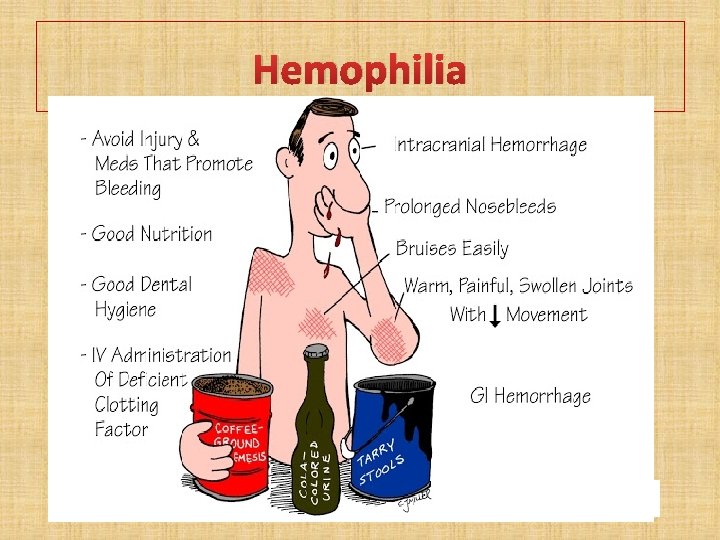
Hemophilia
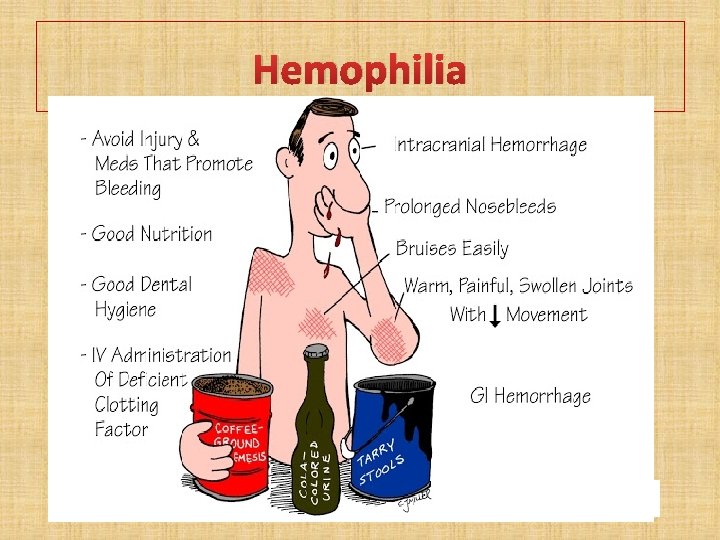
Hemophilia Complications • Deep internal bleeding • Joint damage from haemarthrosis • Transfusion transmitted infection • Intracranial haemorrhage
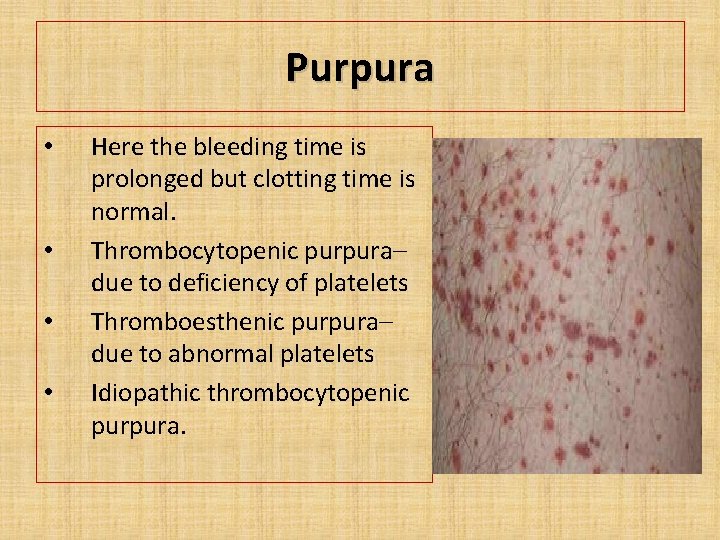
Purpura • • Here the bleeding time is prolonged but clotting time is normal. Thrombocytopenic purpura– due to deficiency of platelets Thromboesthenic purpura– due to abnormal platelets Idiopathic thrombocytopenic purpura.
Others • • Atherosclerosis Thrombus Emboli DIC

THANK YOU
 Ivy method
Ivy method Blood clotting factor
Blood clotting factor Primary hemostasis
Primary hemostasis Virchow triad
Virchow triad Thrombopoisis
Thrombopoisis Hemotasis
Hemotasis Skema hemostasis
Skema hemostasis Hemostasis definition
Hemostasis definition Hemostasis
Hemostasis Primary hemostasis
Primary hemostasis What is hemostasis
What is hemostasis 1ry hemostasis prescribed by:
1ry hemostasis prescribed by: Hemostasis definition
Hemostasis definition Hemostasis
Hemostasis Ancient and modern means of communication
Ancient and modern means of communication Ancient india vs ancient china
Ancient india vs ancient china Môn thể thao bắt đầu bằng chữ f
Môn thể thao bắt đầu bằng chữ f Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Dot
Dot điện thế nghỉ
điện thế nghỉ Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ độ dài liên kết
độ dài liên kết Chó sói
Chó sói Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Phối cảnh
Phối cảnh Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Ng-html
Ng-html Hệ hô hấp
Hệ hô hấp Số nguyên là gì
Số nguyên là gì đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Tư thế worm breton
Tư thế worm breton ưu thế lai là gì
ưu thế lai là gì Tư thế ngồi viết
Tư thế ngồi viết Thẻ vin
Thẻ vin Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Bổ thể
Bổ thể Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Tư thế ngồi viết
Tư thế ngồi viết Thế nào là giọng cùng tên
Thế nào là giọng cùng tên Thể thơ truyền thống
Thể thơ truyền thống 101012 bằng
101012 bằng Bài hát chúa yêu trần thế alleluia
Bài hát chúa yêu trần thế alleluia Hổ đẻ mỗi lứa mấy con
Hổ đẻ mỗi lứa mấy con Diễn thế sinh thái là
Diễn thế sinh thái là đại từ thay thế
đại từ thay thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Công thức tiính động năng
Công thức tiính động năng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra