General Approach in Investigation of Haemostasis Lecture 2


- Slides: 27
General Approach in Investigation of Haemostasis Lecture 2: Bleeding Time
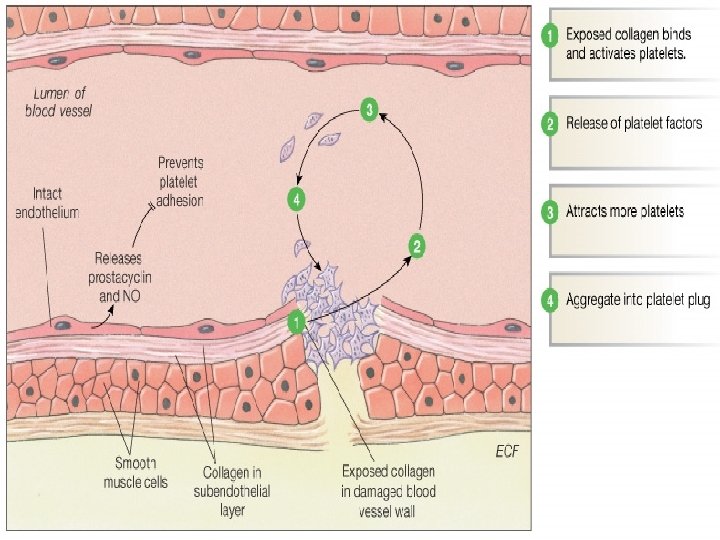
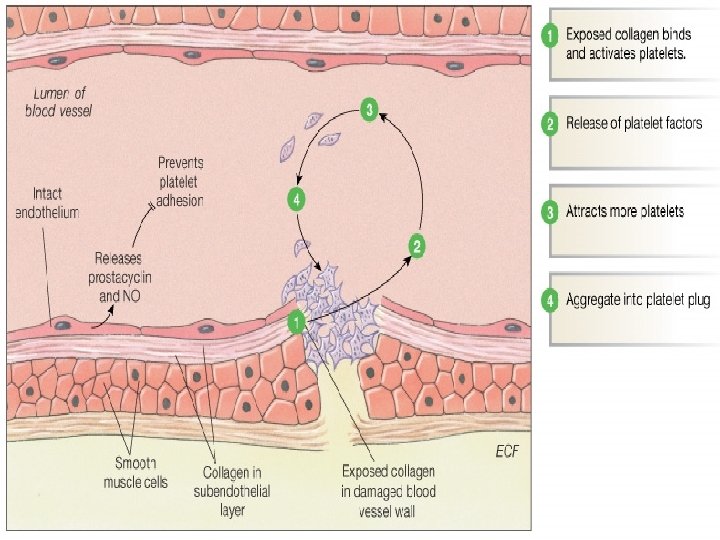
The process of haemostasis occurs in three phases : 1. The vascular platelet phase, which assures primary haemostasis 2. Activation of the coagulation cascade, which assures formation of the clot 3. And activation of a series of control mechanisms, which stop propagation of the clot and limit activation of the coagulation cascade to the region of endothelial rupture.
Coagulation Tests 1. Tests of the Vascular Platelet Phase of Haemostasis: q Bleeding Time (BT) 2. Tests of the Coagulation Cascade: q Clotting Time ( CT) or Coagulation time q Activated Partial Thromboplastin Time (APTT). q Prothrombin Time (PT). 3. Tests of Fibrinolysis and the Mechanisms That Control Hemostasis: q Fibrin Degradation Products (FDP)
Bleeding Time (BT) Principle: q q The bleeding time test is a useful tool to test for platelet plug formation and capillary integrity. Occasionally, the bleeding time test will be ordered on a patient scheduled for surgery. The bleeding time is dependent upon q q q The efficiency of tissue fluid in accelerating the coagulation process Capillary function and The number of blood platelets present and their ability to form a platelet plug.
Bleeding Time (BT) q Prolonged bleeding times are generally found when q. The platelet count is below 50, 000/µL q When there is platelet dysfunction. q Four procedures are currently in use for determining the bleeding time: q. The Duke method. q. The Ivy Method. q. The Mielke Method. q. The Simplate or Surgicutt Method.
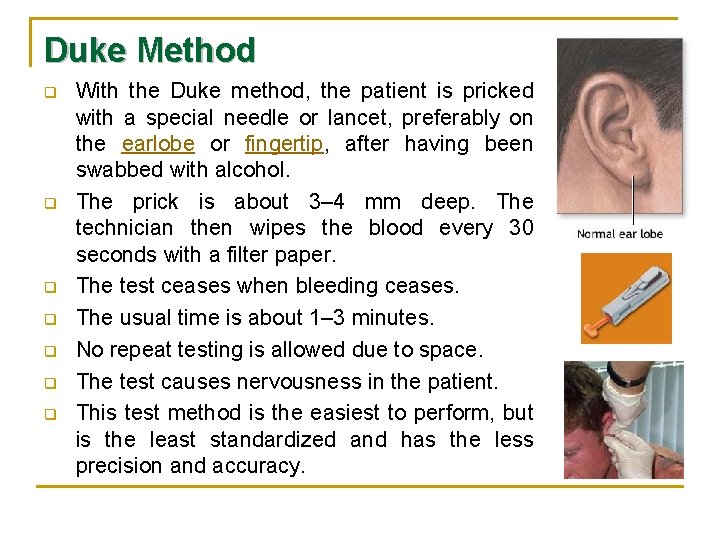
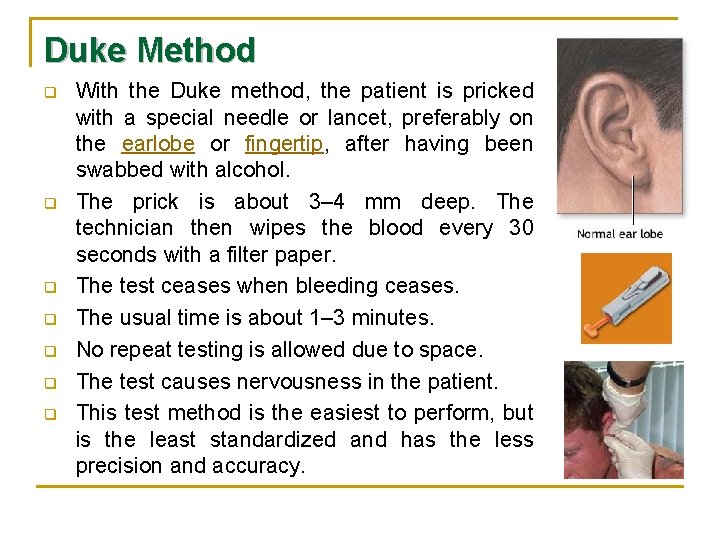
Duke Method q q q q With the Duke method, the patient is pricked with a special needle or lancet, preferably on the earlobe or fingertip, after having been swabbed with alcohol. The prick is about 3– 4 mm deep. The technician then wipes the blood every 30 seconds with a filter paper. The test ceases when bleeding ceases. The usual time is about 1– 3 minutes. No repeat testing is allowed due to space. The test causes nervousness in the patient. This test method is the easiest to perform, but is the least standardized and has the less precision and accuracy.

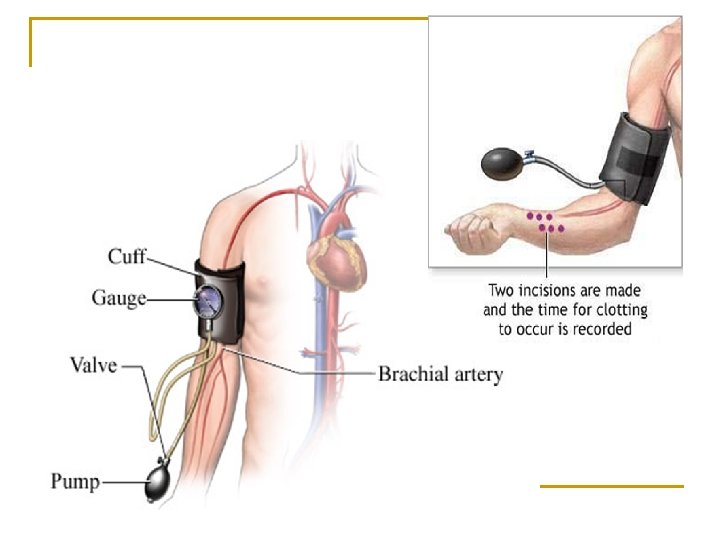
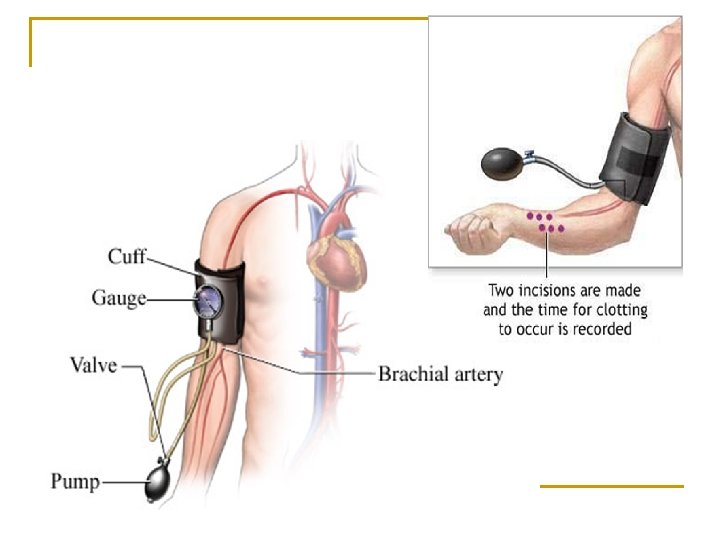
Ivy Method q q In the Ivy method, a blood pressure cuff is placed on the upper arm and inflated to 40 mm. Hg to control capillary tone and to improve the sensitivity and reproducibility– this will maintain constant pressure within the capillaries and help standardize the procedure-. A sterile, disposable blood lancet or scalpel blade is used to make a shallow incision that is 1 millimeter deep on the underside of the forearm. Every 30 seconds, filter paper is used to draw off the blood. The time from when the incision is made until all bleeding has stopped is measured.
Ivy Method q q The test is finished when bleeding has stopped completely. A prolonged bleeding time may be a result from decreased number of thrombocytes or impaired blood vessels. However, it should also be noted that the depth of the puncture or incision may be the source of error. Normal values fall between 2 – 7 minutes depending on the method used. The greatest source of variation in this test is largely due to difficulty in performing a standardized puncture. This usually leads to erroneously low results.
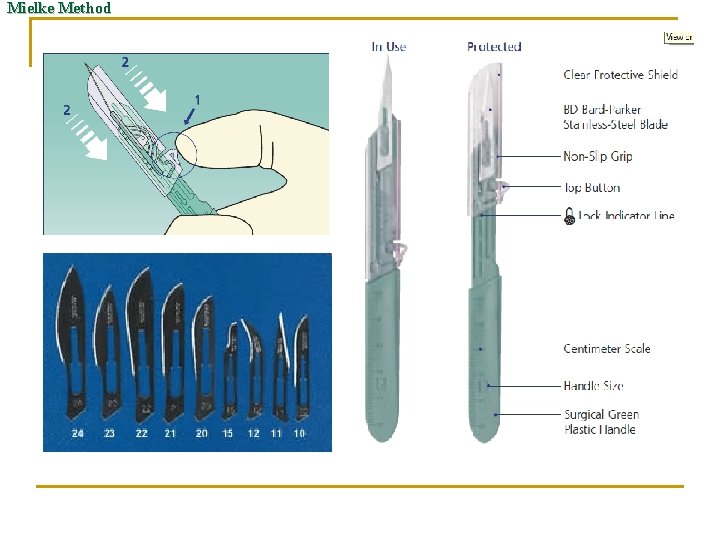
Mielke Method q q q A Modification of the Ivy Method. A Bard-Parker or similar disposable blade is used, along with a rectangular polystyrene or plastic template that contains a standardized slit. The blade is placed in a special handle containing a gauge in order to standardize the depth of the incision. The same procedure as described for the Surgicutt method is employed.
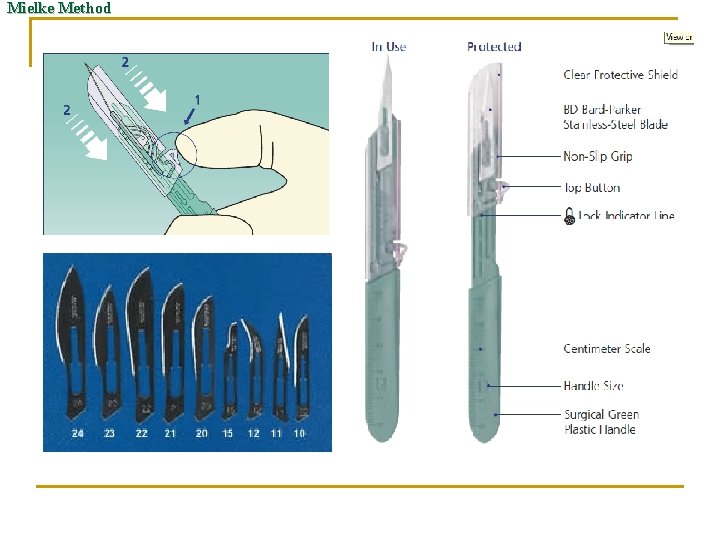
Mielke Method
Mielke Method q Advantages of this method include: q q q That the surgical incision more closely approximates the patient’s haemostatic response to surgery, when compared to the puncture in the Ivy Method. The depth of the incision can be controlled. Disadvantages of this method include: q q Patient anxiety, due to open blade. Small scars might form.
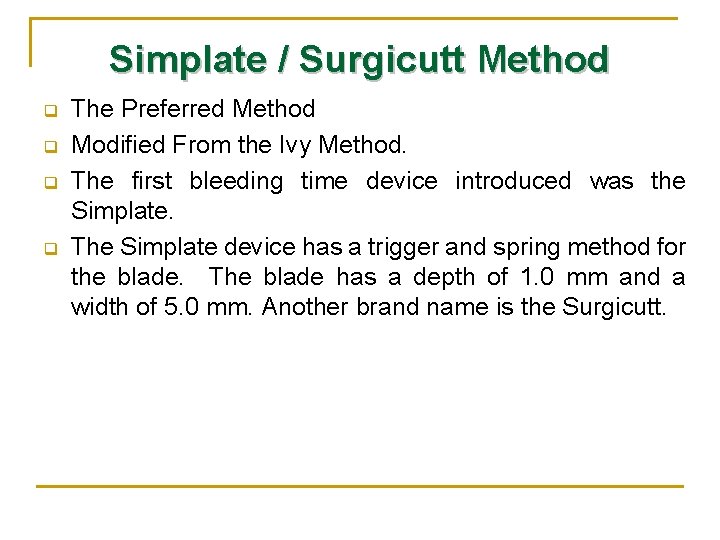
Simplate / Surgicutt Method q q The Preferred Method Modified From the Ivy Method. The first bleeding time device introduced was the Simplate. The Simplate device has a trigger and spring method for the blade. The blade has a depth of 1. 0 mm and a width of 5. 0 mm. Another brand name is the Surgicutt.

Simplate / Surgicutt Method q Advantages of this method include: q Instrument is a sterile, standardized, easy to use device that makes a uniform incision. q Instrument is a spring activated surgical steel blade which is housed in a plastic unit. This eliminates variability of blade incision. q This method is the most standardized method of all the bleeding time procedures. q Disadvantages of this method include: q Slight scarring can occur so patient should be informed.
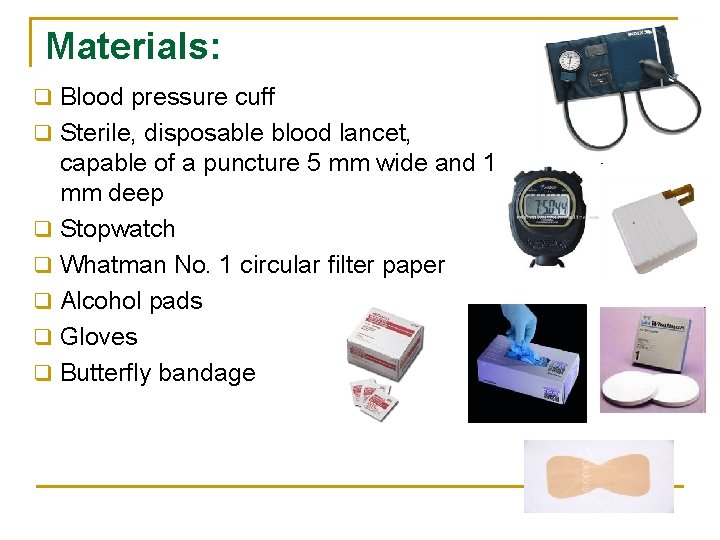
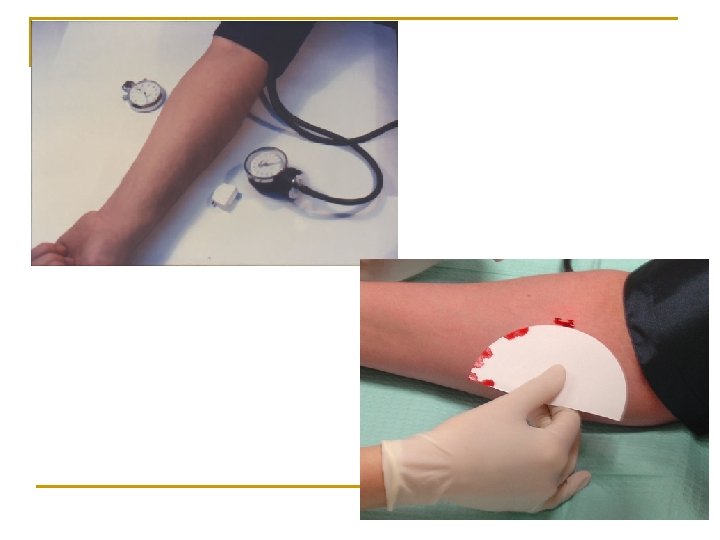
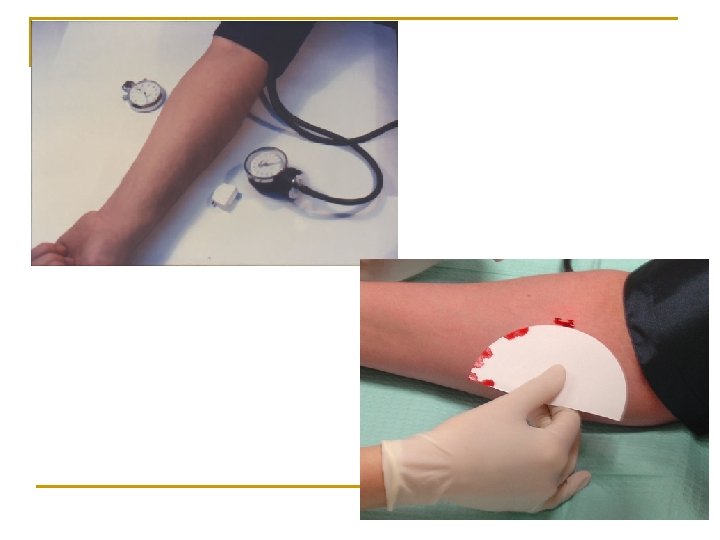
Materials: q Blood pressure cuff q Sterile, disposable blood lancet, q q q capable of a puncture 5 mm wide and 1 mm deep Stopwatch Whatman No. 1 circular filter paper Alcohol pads Gloves Butterfly bandage
Preparation of the Patient q After proper greeting and identification of the patient, explain the test for patient. q It is critical that you ask the patient whether or not they have taken aspirin, aspirin containing compounds (many over the counter medications contain aspirin) or blood thinners such as heparin or Coumadin recently. These drugs will cause a falsely abnormal bleeding time and the test should not be done.
Procedure: 1. 2. 3. 4. 5. 6. Greet and identify the patient. Explain the procedure to the patient. Obtain a history about aspirin or aspirin containing compounds taken within last 7 - 10 days. Select a site on the patient's forearm approximately three fingers widths below the bend in the elbow that is free of visible subcutaneous veins. Cleanse the outer surface of the patient's forearm by moving the alcohol pad in concentric circles from the incision site outward; allow to air dry. Place a blood pressure cuff on the patient's arm above the elbow. Turn the knob on the bulb of the sphygmomanometer until it stops. Squeeze the bulb to inflate the sphygmomanometer. Inflate the cuff and maintain pressure at 40 mm Hg.
Procedure: Remove the Surgicutt device from the blister pack, being careful not to contaminate or touch the blade-slot surface. Remove the safety clip. 8. Holding the skin tight, depress the “trigger” on the bleeding time device. The puncture must be performed within 30 to 60 seconds of inflation of the blood pressure cuff. Simultaneously start the stopwatch. 9. After 30 seconds have passed blot (do not wipe) the blood with the filter paper. The filter paper must not touch the wound on the arm. Blot the site at regular thirty second intervals. Rotate the filter paper after each 30 seconds. 10. When bleeding ceases and blood no longer is drawn to the filter paper, stop the watch and release the blood pressure cuff by turning the knob next to the bulb in the opposite direction used to inflate the cuff. Remove the blood pressure cuff. 11. Record the bleeding time. Bleeding time is determined to the nearest 30 seconds. 7.
Procedure: 12. If bleeding continues for more than 15 minutes, the procedure should be discontinued, and pressure applied to the wound sites. 13. After ensuring that the bleeding has stopped, carefully bandage the site. 14. Appropriately discard all used materials and wash hands.
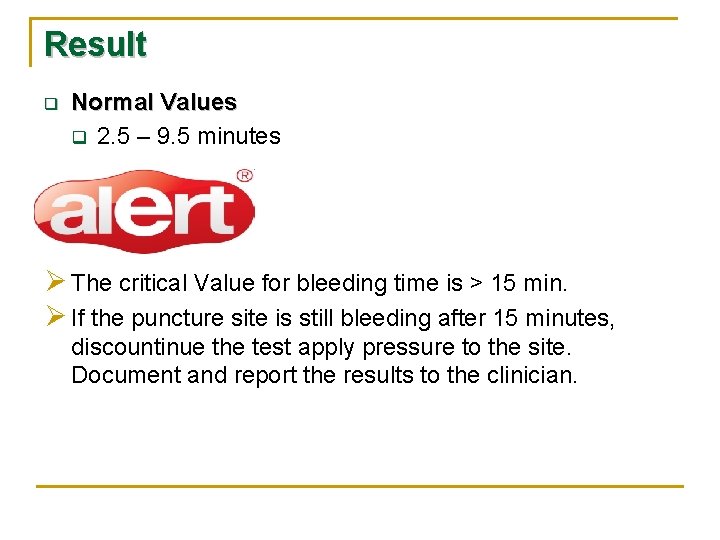
Result q Normal Values q 2. 5 – 9. 5 minutes Ø The critical Value for bleeding time is > 15 min. Ø If the puncture site is still bleeding after 15 minutes, discountinue the test apply pressure to the site. Document and report the results to the clinician.
Calibration , Quality Control: q Calibration: None q Quality Control: No external QC is available. Care must be taken to standardize the procedure. The protocol must followed exactly!
Sources of Error q If the patient has taken aspirin or aspirin-containing compounds 7 to 10 days prior to the procedure, the bleeding time may be prolonged. The technician must determine the patient's history concerning aspirin ingestion to ensure quality results. About 20 different medications, including antihistamines and nonsteroidal anti-inflammatory drugs such as aspirin and ibuprofen, impair the platelets' ability to stick to wounds, and therefore produce a longer bleeding time. q q Results may be affected by an improperly performed puncture. A puncture that is too shallow, too deep, or in an inappropriate location will adversely affect test results. The alcohol must be completely dried before making the puncture. If residual alcohol is on a puncture site, the bleeding time will be erroneously prolonged.
Sources of Error q q q If the technician does not initiate timing of the procedure simultaneously with the puncture, the results will be adversely affected. If the technician allows the filter paper to touch the wound, the platelet clot may be dislodged, causing falsely elevated results. If the stopwatch has not been appropriately calibrated, it may keep incorrect time. Stopwatches should be calibrated on a regular basis as a part of the quality assurance program. The direction of the incision should be consistent. A horizontal incision gives a longer bleeding time than a vertical incision The bleeding time is prolonged in thrombocytopenia, hereditary and acquired platelet dysfunctions, von Willebrand's disease, a fibrinogenemia, severe hypofibrinogenemia, and some vascular bleeding disorders
Sources of Error q Errors producing false positive results q q q Blood pressure cuff maintained too high (>40 mm Hg). Incision too deep, caused by excessive pressure on the incision device. Disturbing the clot with the filter paper. Low fibrinogen (<100 mg/dl) or platelet count (100, 00 /mm 3) Drug ingestion affecting platelet function (e. g. Asprin) Errors producing false negative results q q Blood pressure cuff maintained too low (<40 mm Hg) Incision too shallow.
 Duke and ivy method
Duke and ivy method Haemostasis
Haemostasis 01:640:244 lecture notes - lecture 15: plat, idah, farad
01:640:244 lecture notes - lecture 15: plat, idah, farad Security personnel definition
Security personnel definition Dyphilidium caninum
Dyphilidium caninum General medicine lecture
General medicine lecture General parasitology lecture notes
General parasitology lecture notes Differentiate between virtual circuit and datagram network
Differentiate between virtual circuit and datagram network Theoretical models of counseling
Theoretical models of counseling Waterfall approach in international marketing
Waterfall approach in international marketing Multiple conflict
Multiple conflict Cognitive approach vs behavioral approach
Cognitive approach vs behavioral approach What is research approach definition
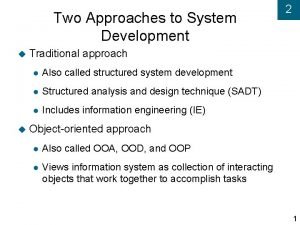
What is research approach definition Traditional approach vs object oriented approach
Traditional approach vs object oriented approach Deep learning approach and surface learning approach
Deep learning approach and surface learning approach How to write a discursive introduction
How to write a discursive introduction Aice general paper rubric
Aice general paper rubric Back detection
Back detection Aice general paper exam
Aice general paper exam Aice hand
Aice hand Diferencia entre gran plano general y plano general
Diferencia entre gran plano general y plano general Where did general lee surrender to general grant?
Where did general lee surrender to general grant? Extended investigation study design
Extended investigation study design Tems investigation
Tems investigation Seven s of crime scene
Seven s of crime scene Transformation in the creative process
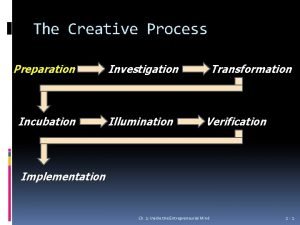
Transformation in the creative process System planning and initial investigation
System planning and initial investigation Surface area investigation
Surface area investigation