Chapter 33 The Child with Endocrine Dysfunction Copyright






- Slides: 90
Chapter 33 The Child with Endocrine Dysfunction Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved.
THE ENDOCRINE SYSTEM Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 2
Hormones A complex chemical substance produced and secreted into body fluids by a cell or group of cells that exert a physiologic controlling effect on other cells Local hormones General hormones Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 3
Control of Hormone Secretion “Tropic hormones” Anterior pituitary gland = “master gland” Releasing hormones Inhibitory hormones Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 4
Neuroendocrine Interrelationships Hemostasis is maintained by two regulatory systems Ø Ø Endocrine system Autonomic nervous system • Sympathetic system • Parasympathetic system Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 5
Disorders of Pituitary Function Pituitary gland is also called hypophysis Pituitary gland is the “master gland” Responsible for regulating other glands Two portions, each with unique functions Ø Ø Anterior Posterior Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 6
Hypopituitarism—Growth Hormone (GH) Deficiency Inhibits somatic growth Primary site of dysfunction appears to be in the hypothalamus Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 7
Diagnostic Evaluation of GH Deficiency Family history Growth patterns and health history Definitive diagnosis based on radioimmunoassay of plasma GH levels Hand x-rays to evaluate growth potential vs. ossification Endocrine studies to detect deficiencies Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 8
Therapeutic Management of GH Deficiency (Cont. ) Biosynthetic growth hormone (injections) Other hormone replacements as needed Ø Ø Ø Thyroid extract Cortisone Testosterone or estrogens and progesterone Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 9
Prognosis GH replacement successful in 80% of affected children Growth rate of 3. 5 to 4 cm/yr before treatment and increase to 8 to 9 cm/yr after treatment Response varies based on age, length of treatment, frequency of doses, dosage, weight, and GH receptor amount Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 10
Nursing Care Management Nurse is key in helping to establish diagnosis Identify growth problems Serial height/weight records Question parents about growth Prepare child and family for diagnostic tests Discuss administration of growth hormones Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 11
Creutzfeldt-Jakob Disease (CJD) Rare neurodegenerative condition reported in some patients after receiving human GH from cadavers Does not occur with biosynthetic GH Blood banks will not accept donation from former human GH recipients because of risk of infection with CJD Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 12
Nursing Considerations for GH Replacement Family members support needs Child’s body image Preparing child for daily injections Injections given at bedtime for best results Treatment very expensive ($20, 000 to $30, 000 per year) Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 13
Pituitary Hyperfunction Excess GH before closure of the epiphyseal shafts results in overgrowth of long bones Reach heights of 8 feet or more Vertical growth and increased muscle Weight is generally in proportion to height Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 14
Pituitary Hyperfunction—Acromegaly Excess GH after epiphyseal closure is called acromegaly Typical facial features Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 15
Diagnostic Evaluations Radiologic studies Endocrine studies Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 16
Therapeutic Management Surgical treatment to remove tumor Radiation and radioactive implants Hormone replacement therapy after surgery in some cases Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 17
Nursing Care Management Early identification of children with excessive growth rates Early treatment for improved outcomes Emotional support Body image concerns Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 18
Precocious Puberty Defined as sexual development before age 9 in boys or before age 8 in girls Occurs more frequently in girls Potential causes Disorder of the gonads, adrenal glands, or hypothalamic-pituitary-gonadal axis Ø No causative factor in 80% to 90% of girls and 50% boys Ø Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 19
Types of Precocious Puberty Central precocious puberty Peripheral precocious puberty Incomplete puberty Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 20
Therapeutic Management Treatment of specific cause if known May be treated with Lupron Ø Ø Slows prepubertal growth to normal rates Treatment is discontinued at age for normal pubertal changes to resume Psychologic support for child and family Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 21
Diabetes Insipidus (DI) The principal disorder of the posterior pituitary Results from hyposecretion of ADH Produces uncontrolled diuresis Primary causes—familial or idiopathic Secondary causes—trauma, tumors, CNS infection, aneurysm Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 22
Clinical Manifestations of DI Cardinal signs—polyuria and polydipsia First sign is often enuresis Infants—irritability that is relieved with feedings of water but not milk; dehydration often occurs Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 23
Therapeutic Management of DI Instruct parents in difference between diabetes insipidus and diabetes mellitus Daily hormone replacement of vasopressin Drug of choice—DDAVP Ø Ø Nasal spray or IM or SQ administration Requires treatment for life Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 24
Nursing Management of DI Identification of disorder Accurate I&O Observe for signs of fluid overload Seizure precautions Administer ADH-antagonizing meds Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 25

Syndrome of Inappropriate Antidiuretic Hormone (SIADH) Produced by hypersecretion of the posterior pituitary (increased ADH) Signs and symptoms—fluid retention and hypotonicity Kidneys unable to reabsorb water Anorexia, nausea/vomiting, irritability, personality changes Symptoms disappear when ADH is decreased Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 26
Disorders of Thyroid Function Thyroid hormone regulates BMR Thyroid secretes two types of hormones Thyroid hormone, which is made up of • Thyroxine (T 4) • Triiodothyronine (T 3) Ø Thyrocalcitonin Ø May have hypo- or hyperthyroidism May have disturbance in secretion of TSH Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 27
Juvenile Hypothyroidism Congenital Ø Congenital hypoplastic thyroid gland Acquired Partial or complete thyroidectomy for CA or thyrotoxicosis Ø Following radiation for Hodgkin or other malignancy Ø Rarely occurs from dietary insufficiency in United States Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 28
Clinical Manifestations of Juvenile Hypothyroidism Decelerated growth Constipation Sleepiness Myxedematous skin changes Ø Ø Ø Dry skin Sparse hair Periorbital edema Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 29
Therapeutic Management Oral thyroid hormone replacement Prompt treatment needed for brain growth in infant May administer in increasing amounts over 4 to 8 weeks to reach euthyroidism Compliance with medication regimen is crucial Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 30
Goiter Hypertrophy of the thyroid gland Congenital Ø Usually results from maternal ingestion of antithyroid drugs during pregnancy Acquired Ø Result of neoplasm, inflammatory disease, dietary deficiency (but rarely in children), or increased secretion of pituitary thyrotropic hormone Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 31
Nursing Considerations Thyroid enlargement at birth may compromise newborn’s airway May become noticeable during periods of rapid growth Large goiters may be obvious; smaller nodules evident only on palpation TH replacement is necessary for treatment of hypothyroidism Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 32
Lymphocytic Thyroiditis Hashimoto disease or juvenile autoimmune thyroiditis Most common cause of thyroid disease in children and teens Accounts for largest percentage of juvenile hypothyroidism Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 33
Pathophysiology of Lymphocytic Thyroiditis Genetic predisposition but specifics unclear Characterized by lymphocytic infiltration of the gland, inflammation, hyperplasia, which may be replaced with fibrous tissue Child usually is euthyroid, with some symptoms of hyperthyroidism Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 34
Therapeutic Management of Lymphocytic Thyroiditis Goiter may be transient, asymptomatic May resolve spontaneously within 1 to 2 years Oral TH often decreases the goiter significantly Surgery contraindicated for this disorder Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 35
Hyperthyroidism (Graves Disease) Most common cause of hyperthyroidism in childhood is Graves disease Believe caused by serum thyroid-stimulating immunoglobulin, but no specific etiology Enlarged thyroid gland exophthalmos Peak incidence at 12 to 14 years of age but may be present at birth Familial association Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 36
Symptoms of Graves Disease Manifestations develop gradually, often over 6 to 12 months Eyes—exophthalmos Excessive motion, irritability, hyperactivity, short attention span, tremors, insomnia, and emotional lability Ø GI hyperactivity Ø Ø Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 37
Symptoms of Graves Disease (Cont. ) Manifestations (Cont. ) Cardiac—rapid, pounding pulse even during sleep, widened pulse pressure, systolic murmurs, and cardiomegaly Ø Dyspnea occurs during slight exertion. Ø Skin is warm, flushed, and moist. Heat intolerance may be severe and is accompanied by diaphoresis. Ø Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 38
Graves Disease Management Diagnosis based on increased levels of T 4 and T 3 with suppressed TSH Therapy is controversial Goal of therapy—retard rate of hormone secretion Treatments Ø Ø Ø Antithyroid drugs (PTU and methimazole) Subtotal thyroidectomy Ablation with radioiodine Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 39
Thyrotoxicosis Thyroid “crisis” or “storm” May occur from sudden release of hormone Unusual in children but can be life threatening May be precipitated by infection, surgery, or discontinuation of antithyroid therapy Treatment of thyroid storm Ø Ø Antithyroid drugs Propranolol Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 40
Nursing Care Management Identify children with hypothyroidism Alert for signs and symptoms Child needs quiet environment, rest periods Help family cope with emotional lability associated with disorder Dietary requirements to meet the child’s increased metabolic rate Medications—side effects of ATD therapy Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 41
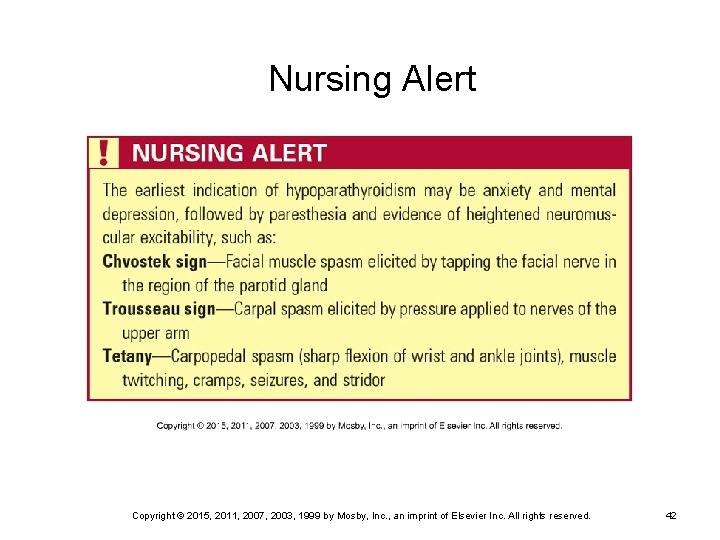
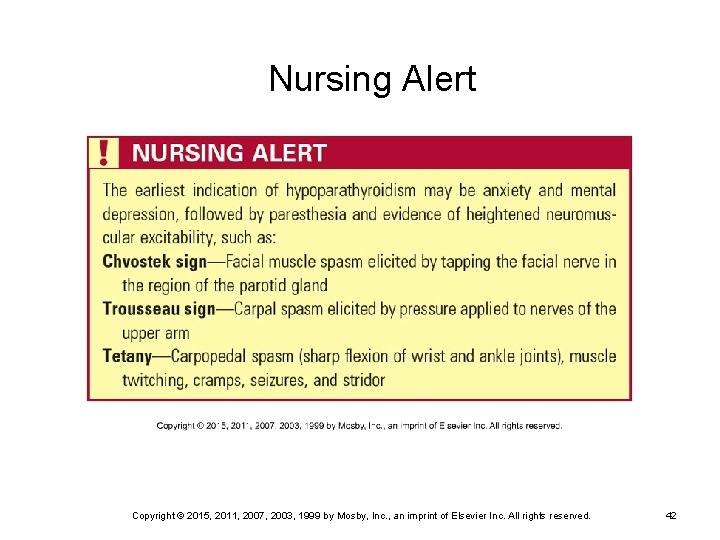
Nursing Alert Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 42
Disorders of Parathyroid Function Parathyroid glands secrete parathormone (PTH) Function of PTH—maintain serum calcium by Increasing the release of calcium and phosphate from bone demineralization Ø Increasing absorption of calcium and excretion of phosphate by the kidneys Ø Promoting calcium absorption in the GI tract Ø Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 43
Hypoparathyroidism Autoimmune hypoparathyroidism Ø Deficient production of PTH Pseudohypoparathyroidism Production of PTH is increased, but end organs are unresponsive to the hormone Ø Thought to be inherited as X-linked dominant trait with variable expressivity Ø Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 44
Clinical Manifestations Dry, scaly skin with eruptions Brittle hair, thin nails with transverse grooves Tetany, paresthesias, tingling, laryngeal stridor, and/or spasms Headache, seizures, emotional lability, depression, confusion, memory loss Positive Chvostek and/or Trousseau signs Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 45
Hyperparathyroidism Primary—adenoma of the gland Secondary—chronic renal disease, congenital anomalies of the urinary tract Common factor is hypercalcemia Rare in children Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 46

Hyperparathyroidism (Cont. ) Diagnostic evaluation Therapeutic management—surgical removal or treat underlying cause if possible Nursing considerations Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 47
Disorders of Adrenal Function Adrenal cortex secretes three groups of “steroids”: Ø Ø Ø Glucocorticoids (cortisol, corticosterone) Mineralocorticoids (aldosterone) Sex steroids (androgens, estrogens, and progestins) Altered levels of these produce significant dysfunction Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 48
Disorders of Adrenal Function (Cont. ) Adrenal medulla secretes catecholamines— epinephrine and norepinephrine Catecholamine-secreting tumors are the primary cause of adrenal medullary hyperfunction Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 49
Acute Adrenocortical Insufficiency “Adrenal crisis” Etiologic factors—hemorrhage into the gland from trauma, fulminating infections, abrupt withdrawal of exogenous cortisone, failure to increase cortisone during times of stress Diagnosis generally based on clinical symptoms Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 50
Acute Adrenocortical Insufficiency (Cont. ) Clinical symptoms Therapeutic management Nursing considerations Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 51
Chronic Adrenocortical Insufficiency —Addison Disease Rare in children When it occurs, usually result of neoplasm or lesion of adrenal glands or idiopathic cause Symptoms appear gradually after 90% of adrenal tissue is nonfunctional Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 52
Addison Disease Diagnosis Therapeutic management Nursing considerations Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 53
Cushing Syndrome A characteristic group of manifestations caused by excessive circulating free cortisol May be caused by excessive or prolonged steroid therapy Condition is reversible once steroids are discontinued Abrupt withdrawal of steroids may precipitate acute adrenal insufficiency Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 54
Etiologies of Cushing Syndrome Pituitary—excess ACTH Adrenal—hypersecretion of glucocorticoids Ectopic—extrapituitary neoplasm Iatrogenic—administration of excessive steroids Food dependent—inappropriate adrenal response to secretion of polypeptide Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 55
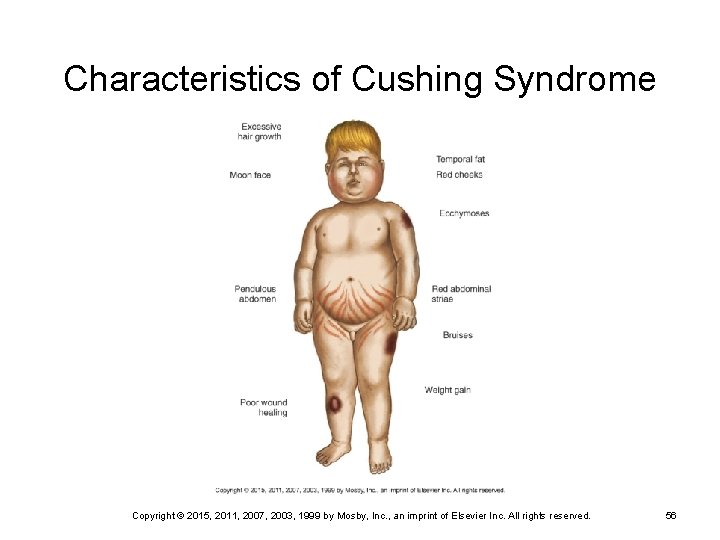
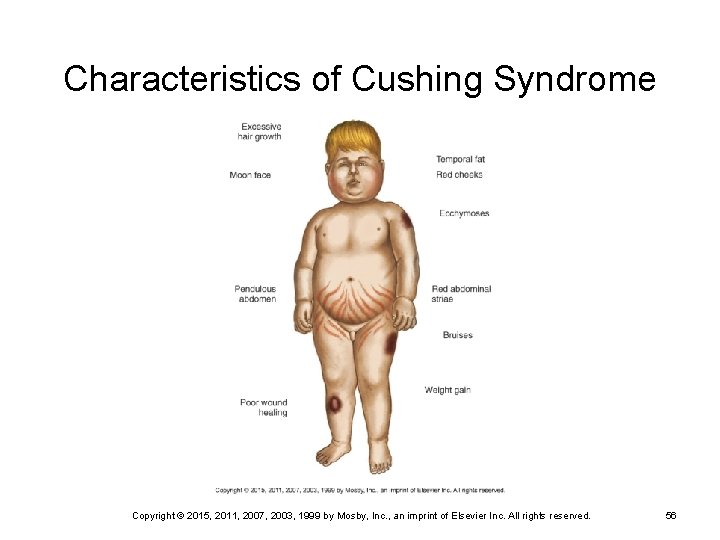
Characteristics of Cushing Syndrome Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 56
Cushingoid Appearance Excessive hair growth Moon face, red cheeks Weight gain Pendulous abdomen with red striae Poor wound healing Ecchymoses Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 57

Diagnostic Evaluation Confirm excess cortisol levels X-rays—evaluate for osteoporosis and skull films to look for enlargement of sella turcica Labs Ø Ø Ø Fasting blood glucose Serum electrolytes 24 -hour urine Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 58
Therapeutic Management Surgery Replacement of growth hormone, ADH, TH, gonadotropins, and steroids Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 59
Nursing Care Management Medication administration Postoperative complications Management of anorexia, nausea, and vomiting Parent education Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 60
Congenital Adrenal Hyperplasia (CAH) A family of disorders caused by decreased enzyme activity required for cortisol production in the adrenal cortex More than 90% of cases are 21 -hydroxylase deficiency 11 -hydroxylase deficiency Overproduction of adrenal androgens and results in virilization of female fetus Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 61

Clinical Manifestations Males—precocious genital development Females—may be born with varying degrees of ambiguous genitalia Enlarged clitoris appears as a small phallus Fused labia produce saclike structure without testes Ø Internal female sexual organs are intact Ø Ø Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 62
Diagnostic Evaluation Ultrasonography to visualize pelvic organs Chromosome typing for positive sex determination and to rule out any other genetic anomalies Newborn screening measurement of cortisol precursor Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 63
Therapeutic Management of CAH Confirm diagnosis and assign a sex to the infant according to genotype Cortisone to suppress abnormally high secretion of ACTH Reconstructive surgery as required Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 64
Nursing Care Management Parental anxiety Help parents learn how to explain disorder Teach parents signs and symptoms of dehydration and salt-losing crises Role of genetic counseling Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 65
Hyperaldosteronism May be caused by adrenal tumor May be caused by adrenogenital syndromes Results in hypertension, hypokalemia, and polyuria that fails to respond to ADH administration Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 66
Hyperaldosteronism (Cont. ) Therapeutic management Ø Ø Replacement of potassium Administration of spironolactone to block effects of aldosterone Nursing considerations Ø Alert for signs and symptoms of hypokalemia and hyperkalemia Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 67
Pheochromocytoma Adrenal tumor that secretes catecholamines May occur around adrenal medulla, along the paraganglia of the aorta, or the thoracolumbar sympathetic chain Children often have bilateral, multiple, benign tumors Increased production of catecholamines; may mimic other disorders Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 68
Therapeutic Management of Pheochromocytoma Do not palpate tumor (releases catecholamines) Surgical removal of tumor(s) May require bilateral adrenalectomy and lifelong glucocorticoid and mineralocorticoid therapy Nursing considerations Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 69
DISORDERS OF PANCREATIC HORMONE SECRETION Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 70
Diabetes Mellitus (DM) Characterized by a total or partial deficiency of the hormone insulin The most common endocrine disorder of childhood Peak incidence in early adolescence Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 71
Three Major Groups of DM Type 1 Type 2 Maturity-onset diabetes of the young (MODY) Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 72
Type 1 Diabetes Characterized by destruction of beta cells, usually leading to absolute insulin deficiency Onset typically in childhood and adolescence but can occur at any age Most DM of childhood is type 1 Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 73
Type 2 Diabetes Arises because of insulin resistance Onset usually after age 40 Native American, Hispanic, and African. American children are at increased risk of type 2 DM Affected people may require insulin injections Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 74
Maturity-Onset Diabetes of the Young (MODY) Transmitted as autosomal dominant disorder with formation of structurally abnormal insulin with decreased biologic activity Onset is generally before age 25 Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 75
Maturity-Onset Diabetes of the Young (MODY) (Cont. ) Similar to type 2 DM May be seen in obese teens May be controlled with oral hypoglycemic agents and diet modifications More benign disease but increasing frequency in pediatric population Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 76
Etiology Type 1 DM believed to be autoimmune disease arising when a person with a genetic predisposition is exposed to a precipitating event such as a viral infection Heredity is prominent factor in the etiology Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 77
Pathophysiology of DM With a deficiency of insulin, glucose is unable to enter the cell and remains in blood, causing hyperglycemia When serum glucose exceeds the renal threshold, glucose spills into urine (glycosuria) Cells break down protein for conversion to glucose by the liver (glucogenesis) Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 78
Ketoacidosis When glucose is unavailable for cellular metabolism, the body breaks down alternate sources of energy Ketones released and excess ketones eliminated in urine (ketonuria) or by the lungs (acetone breath) Ketones in blood are strong acids that lower serum p. H and produce ketoacidosis Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 79
Kussmaul Respirations Hyperventilation characteristic of metabolic acidosis resulting from the respiratory system’s attempt to eliminate excess CO 2 by increased depth and rate Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 80
Diabetic Ketoacidosis (DKA) Pediatric emergency Results from progressive deterioration with dehydration, electrolyte imbalance, acidosis, coma, and may cause death Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 81
Long-Term Complications of DM Microvascular complications, especially nephropathy and retinopathy Macrovascular disease, neuropathy Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 82
Therapeutic Management of Type 1 DM Insulin therapy Glucose monitoring—goal range 80 to 120 mg/dl Lab measurement of hemoglobin A 1 c Urine testing for ketones Ø Not routinely used except to test q 3 h during illness and whenever glucose is ≥ 240 mg/dl when illness not present Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 83
Therapeutic Management of Type 1 DM (Cont. ) Nutrition Exercise Teach patient and family how to manage hypoglycemic episodes Illness management Management of DKA Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 84
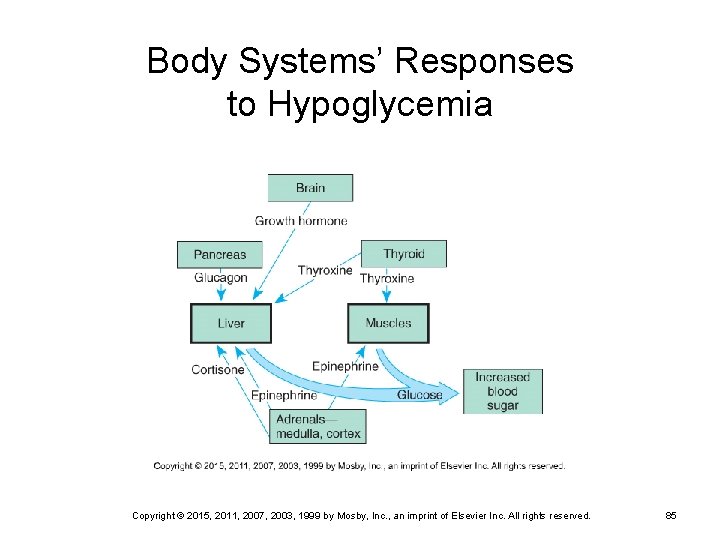
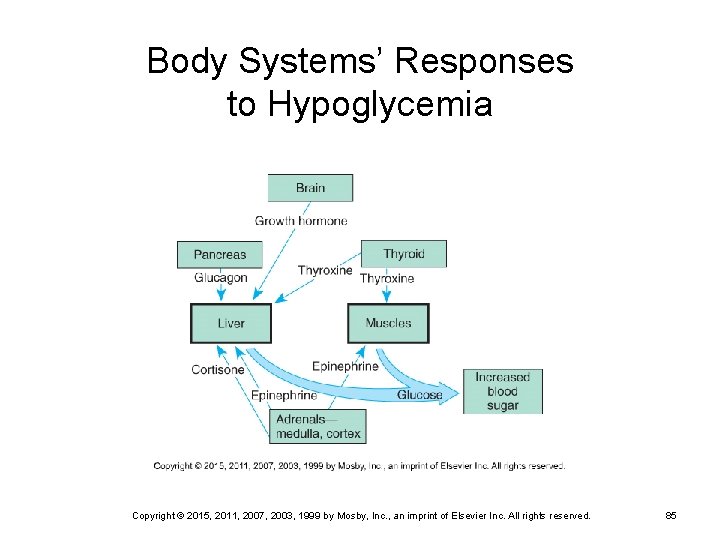
Body Systems’ Responses to Hypoglycemia Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 85
Patient Education—DM and Insulin Therapy Nature of the disease Meal planning Insulin therapy—types of insulin, duration, onset and peak action, mixing and administration, rotation of injection sites Insulin pump therapy in some cases Glucose monitoring Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 86

Child Administering Own Insulin Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 87
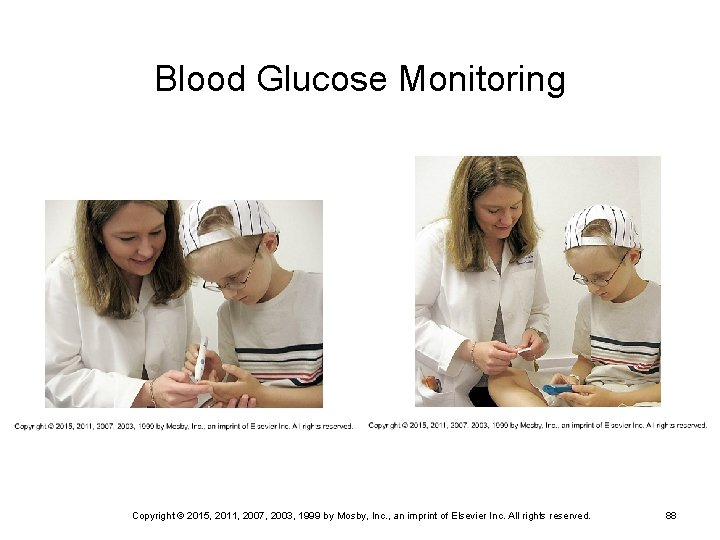
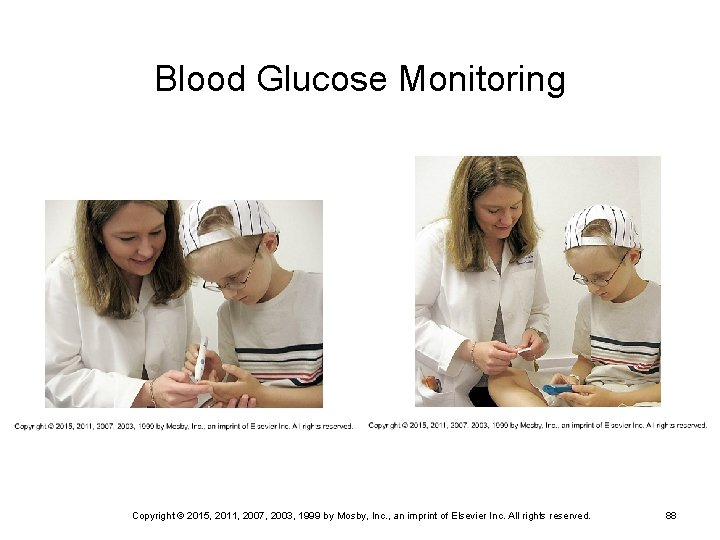
Blood Glucose Monitoring Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 88
Patient Education (Cont. ) Recognition and treatment of hypoglycemia and hyperglycemia Management of “minor” illnesses Record keeping Hygiene Family support Acute care Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 89

Possible Nursing Diagnoses for Pediatric Client with DM Risk for Injury related to insulin deficiency Risk for Injury related to hypoglycemia Deficient Knowledge (Diabetes Management) related to care of child with newly diagnosed diabetes mellitus Copyright © 2015, 2011, 2007, 2003, 1999 by Mosby, Inc. , an imprint of Elsevier Inc. All rights reserved. 90