Approach to a patient with ataxia Dr Rakesh



- Slides: 66
Approach to a patient with ataxia Dr Rakesh Shukla Professor Of Neurology
Definition v Ataxia (Gk. Taxis = Order; means lack of order) v Ataxia denotes a syndrome of imbalance and incoordination involving gait, limbs, and speech and usually results from the disorder of the cerebellum or its connections v It is characterized by dyssynergia, dysmetria, dysdiadochokinesia (Joseph Babinski). v It is a disorder of rate, range, direction and force of movements (Gordon Holmes).


Outline of today’s lecture v Clinical Scenario v Anatomy and Physiology v Is it Cerebellar Ataxia v History and Examination v Classification v Hereditary Ataxias v Acquired Ataxias v Treatment v Conclusion v MCQs
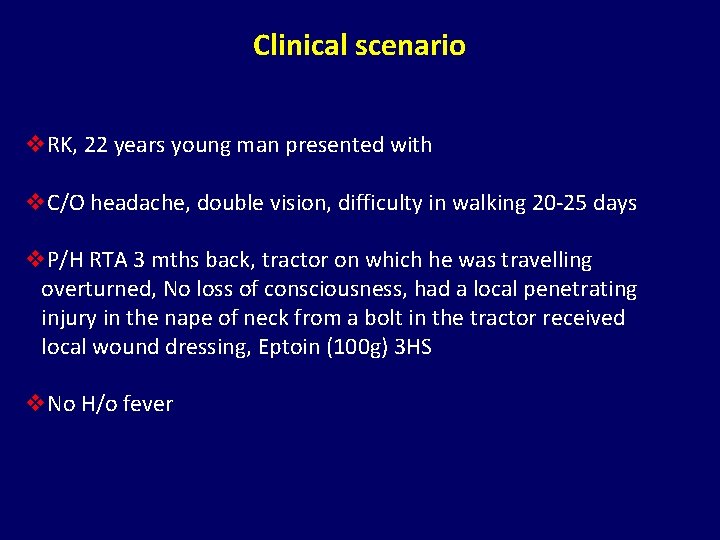
Clinical scenario v. RK, 22 years young man presented with v. C/O headache, double vision, difficulty in walking 20 -25 days v. P/H RTA 3 mths back, tractor on which he was travelling overturned, No loss of consciousness, had a local penetrating injury in the nape of neck from a bolt in the tractor received local wound dressing, Eptoin (100 g) 3 HS v. No H/o fever
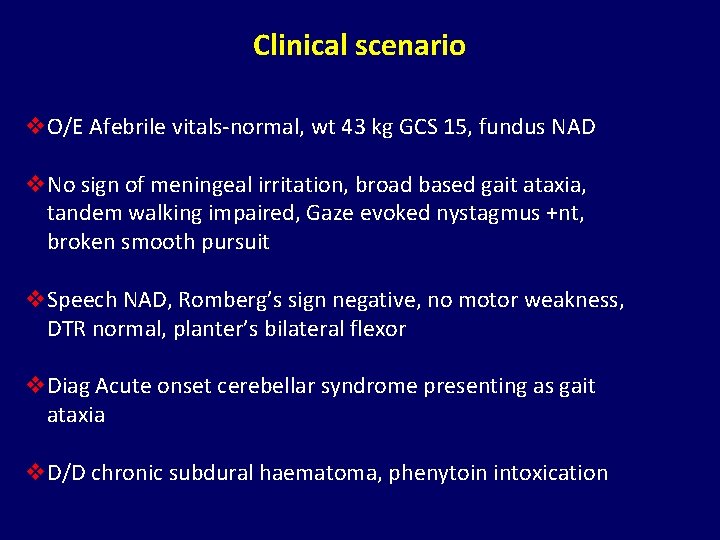
Clinical scenario v. O/E Afebrile vitals-normal, wt 43 kg GCS 15, fundus NAD v. No sign of meningeal irritation, broad based gait ataxia, tandem walking impaired, Gaze evoked nystagmus +nt, broken smooth pursuit v. Speech NAD, Romberg’s sign negative, no motor weakness, DTR normal, planter’s bilateral flexor v. Diag Acute onset cerebellar syndrome presenting as gait ataxia v. D/D chronic subdural haematoma, phenytoin intoxication
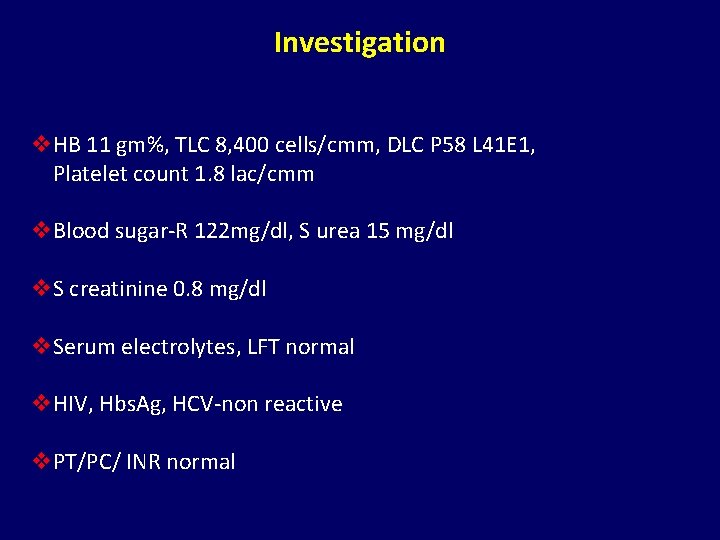
Investigation v. HB 11 gm%, TLC 8, 400 cells/cmm, DLC P 58 L 41 E 1, Platelet count 1. 8 lac/cmm v. Blood sugar-R 122 mg/dl, S urea 15 mg/dl v. S creatinine 0. 8 mg/dl v. Serum electrolytes, LFT normal v. HIV, Hbs. Ag, HCV-non reactive v. PT/PC/ INR normal
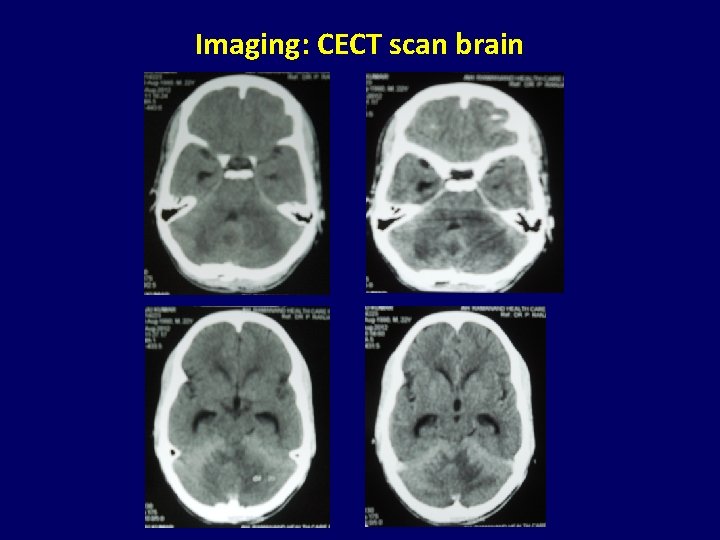
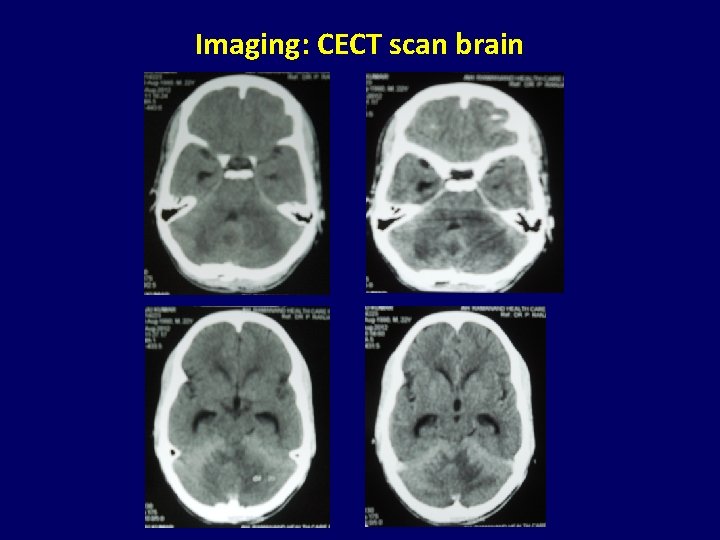
Imaging: CECT scan brain
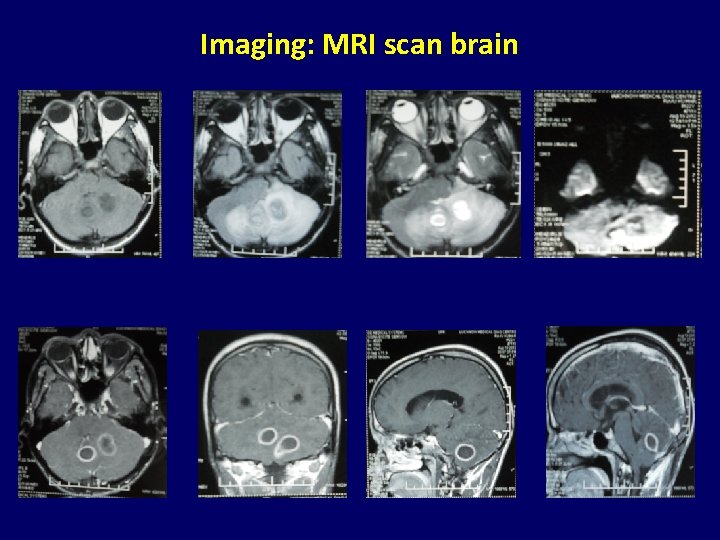
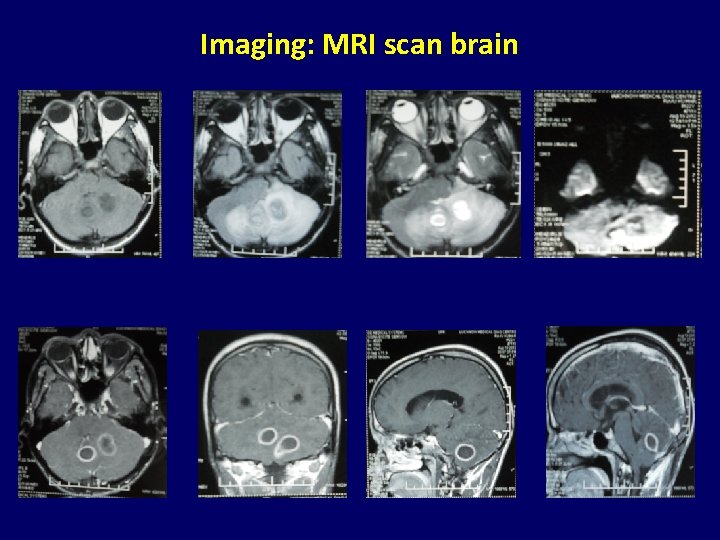
Imaging: MRI scan brain
Outline of today’s lecture v Clinical Scenario v Anatomy and Physiology v Is it Cerebellar Ataxia v History and Examination v Classification v Hereditary Ataxias v Acquired Ataxias v Treatment v Conclusion v MCQs
v Cerebellum has been recognised as a distinct division of the brain since Herophilus (335 -280 BC) and Galen (131 -200 AD) v Angevine et al. , (1961) listed 24 different nomenclatures, terminology used by Larsell (1972) is used commonly at present. v It has a volume of about 144 cm 3 and weighs 150 g (~10% of brain weight), but its surface area is about 40% that of the cerebellar cortex.
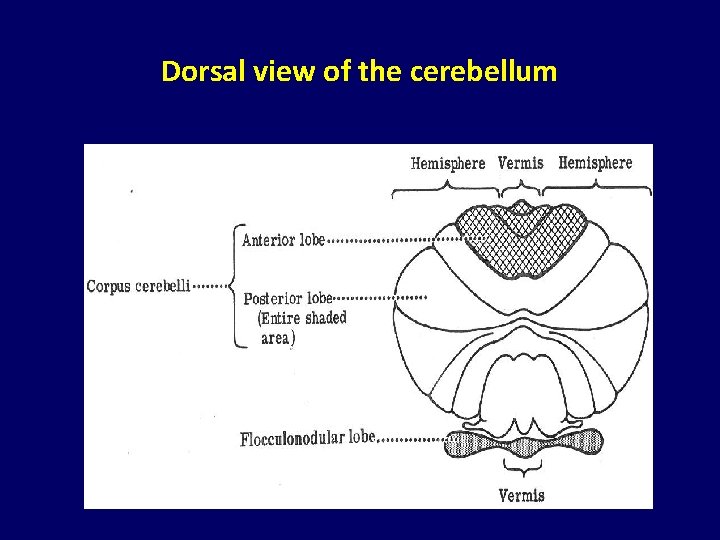
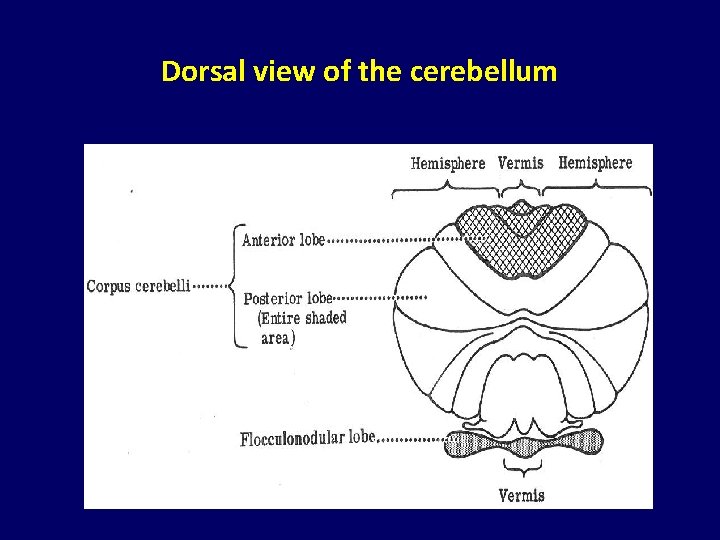
Dorsal view of the cerebellum
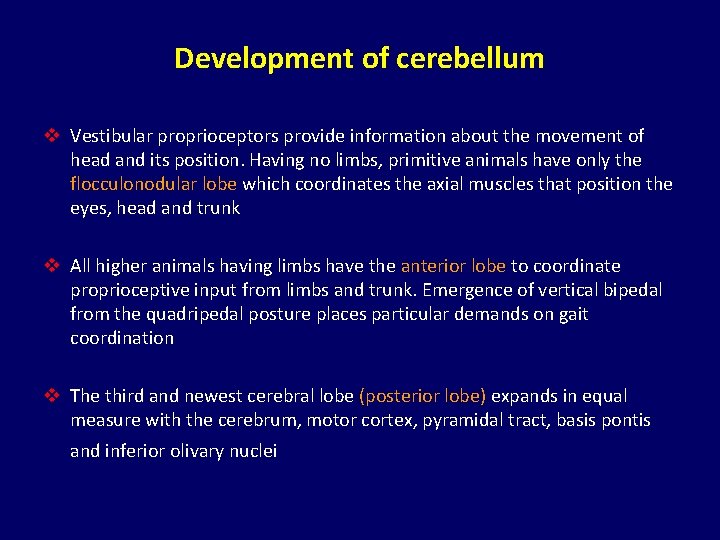
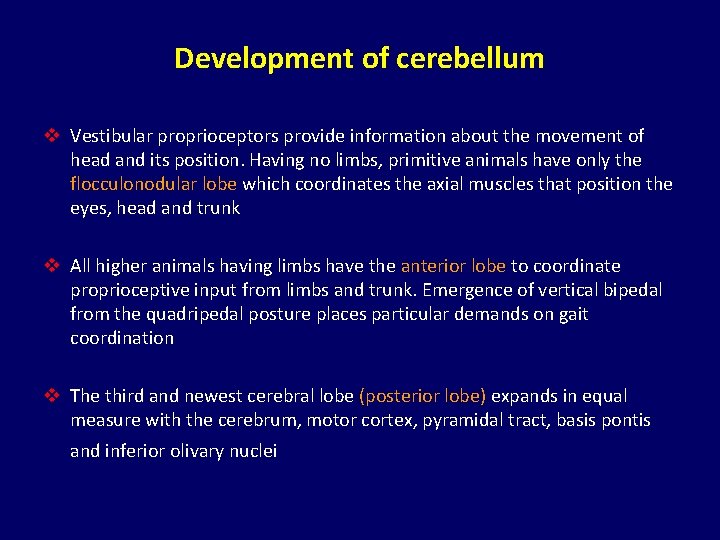
Development of cerebellum v Vestibular proprioceptors provide information about the movement of head and its position. Having no limbs, primitive animals have only the flocculonodular lobe which coordinates the axial muscles that position the eyes, head and trunk v All higher animals having limbs have the anterior lobe to coordinate proprioceptive input from limbs and trunk. Emergence of vertical bipedal from the quadripedal posture places particular demands on gait coordination v The third and newest cerebral lobe (posterior lobe) expands in equal measure with the cerebrum, motor cortex, pyramidal tract, basis pontis and inferior olivary nuclei
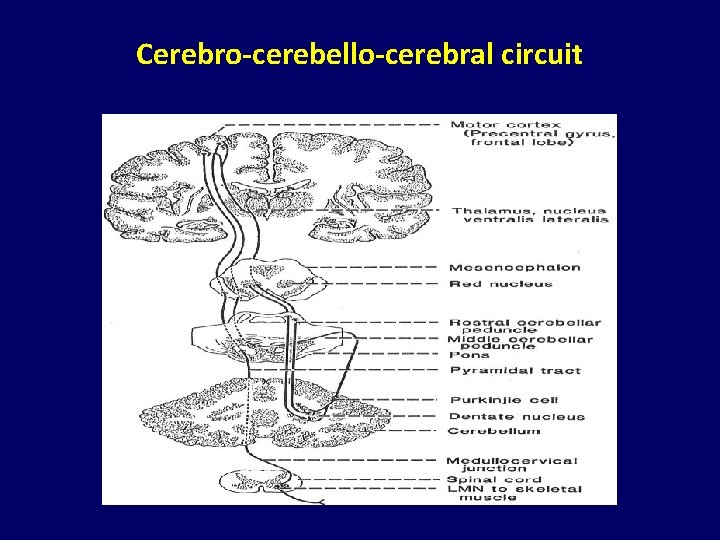
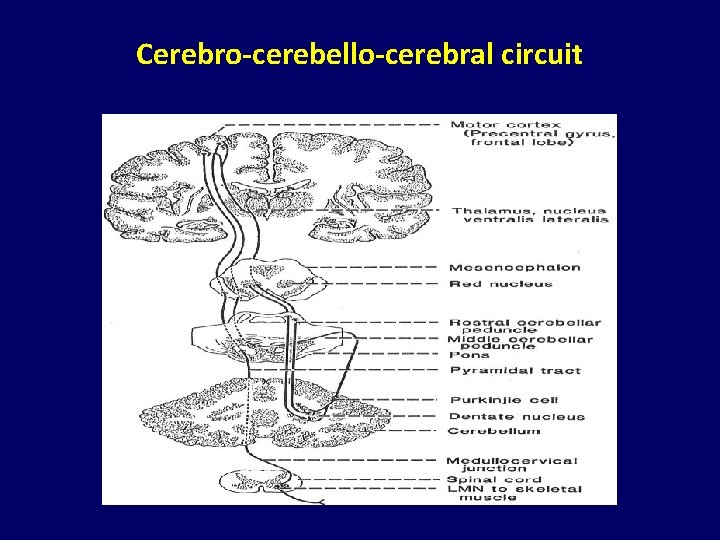
Cerebro-cerebello-cerebral circuit
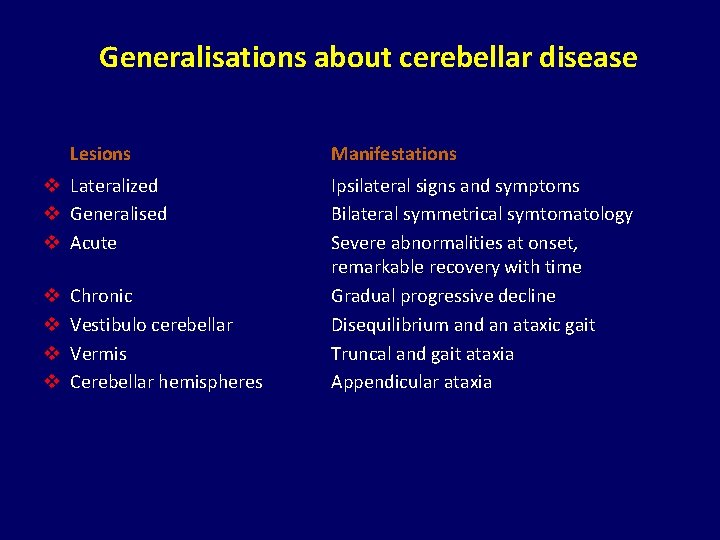
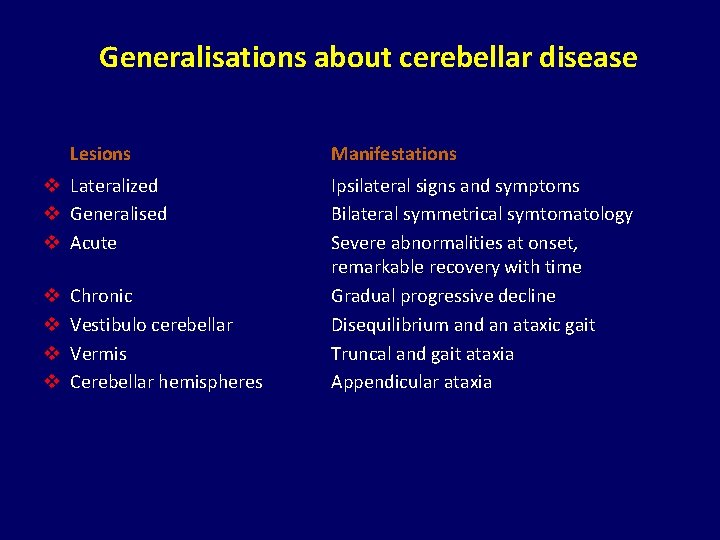
Generalisations about cerebellar disease Lesions v Lateralized v Generalised v Acute v v Chronic Vestibulo cerebellar Vermis Cerebellar hemispheres Manifestations Ipsilateral signs and symptoms Bilateral symmetrical symtomatology Severe abnormalities at onset, remarkable recovery with time Gradual progressive decline Disequilibrium and an ataxic gait Truncal and gait ataxia Appendicular ataxia
Outline of today’s lecture v Clinical Scenario v Anatomy and Physiology v Is it Cerebellar Ataxia v History and Examination v Classification v Hereditary Ataxias v Acquired Ataxias v Treatment v Conclusion v MCQs
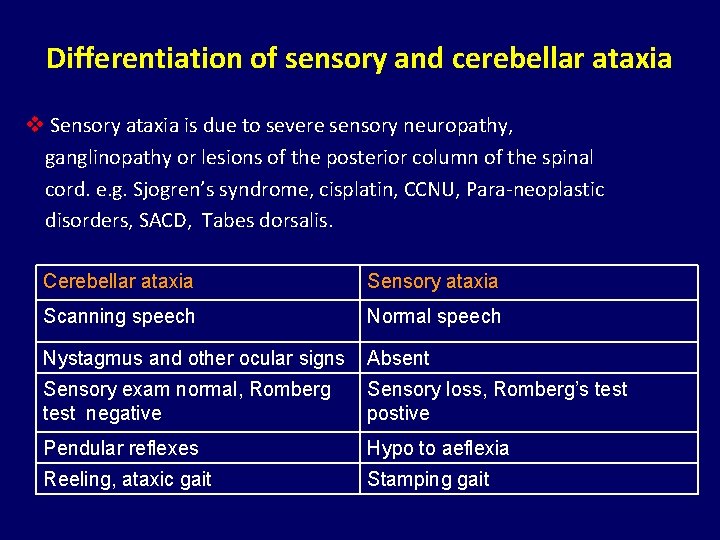
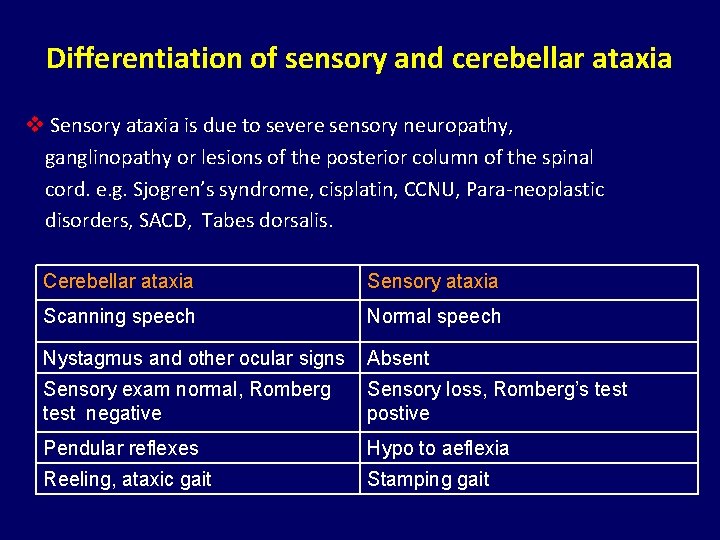
Differentiation of sensory and cerebellar ataxia v Sensory ataxia is due to severe sensory neuropathy, ganglinopathy or lesions of the posterior column of the spinal cord. e. g. Sjogren’s syndrome, cisplatin, CCNU, Para-neoplastic disorders, SACD, Tabes dorsalis. Cerebellar ataxia Sensory ataxia Scanning speech Normal speech Nystagmus and other ocular signs Absent Sensory exam normal, Romberg test negative Sensory loss, Romberg’s test postive Pendular reflexes Hypo to aeflexia Reeling, ataxic gait Stamping gait
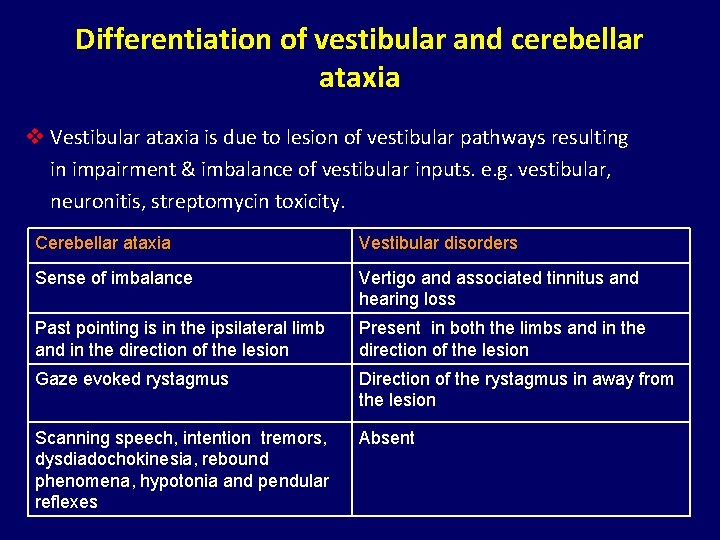
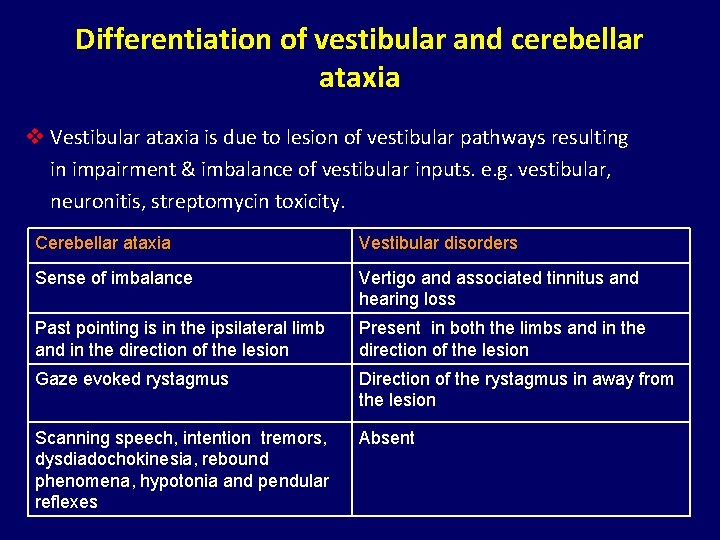
Differentiation of vestibular and cerebellar ataxia v Vestibular ataxia is due to lesion of vestibular pathways resulting in impairment & imbalance of vestibular inputs. e. g. vestibular, neuronitis, streptomycin toxicity. Cerebellar ataxia Vestibular disorders Sense of imbalance Vertigo and associated tinnitus and hearing loss Past pointing is in the ipsilateral limb and in the direction of the lesion Present in both the limbs and in the direction of the lesion Gaze evoked rystagmus Direction of the rystagmus in away from the lesion Scanning speech, intention tremors, dysdiadochokinesia, rebound phenomena, hypotonia and pendular reflexes Absent
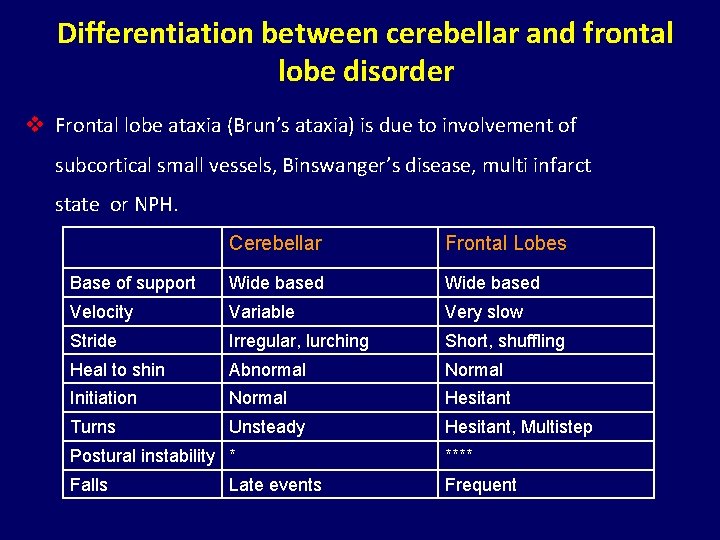
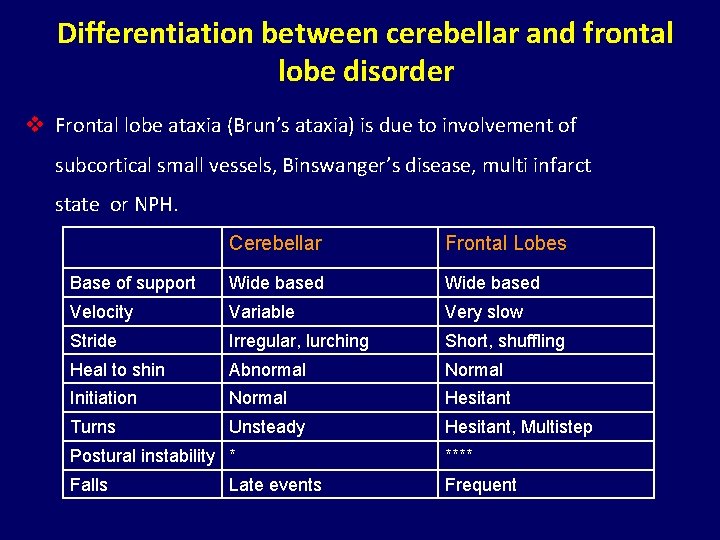
Differentiation between cerebellar and frontal lobe disorder v Frontal lobe ataxia (Brun’s ataxia) is due to involvement of subcortical small vessels, Binswanger’s disease, multi infarct state or NPH. Cerebellar Frontal Lobes Base of support Wide based Velocity Variable Very slow Stride Irregular, lurching Short, shuffling Heal to shin Abnormal Normal Initiation Normal Hesitant Turns Unsteady Hesitant, Multistep Postural instability * **** Falls Frequent Late events
Outline of today’s lecture v Clinical Scenario v Anatomy and Physiology v Is it Cerebellar Ataxia v History and Examination v Classification v Hereditary Ataxias v Acquired Ataxias v Treatment v Conclusion v MCQs
Important points in history v Age at onset v Mode of onset v Precipitating factors v Rate of progression v Symptoms of raised ICP v Presence of systemic symptoms v Drug history and toxin exposure v Family history
Examination v Neck tilt and titubation v Nystagmus and other ocular movement abnormalities v Dysarthria v Intention tremor v Hypotonia v Past pointing v Rebound phenomenon v Macrographia v Stance v Ataxic Gait v Pendular knee jerk
Outline of today’s lecture v Clinical Scenario v Anatomy and Physiology v Is it Cerebellar Ataxia v History and Examination v Classification v Hereditary Ataxias v Acquired Ataxias v Treatment v Conclusion v MCQs
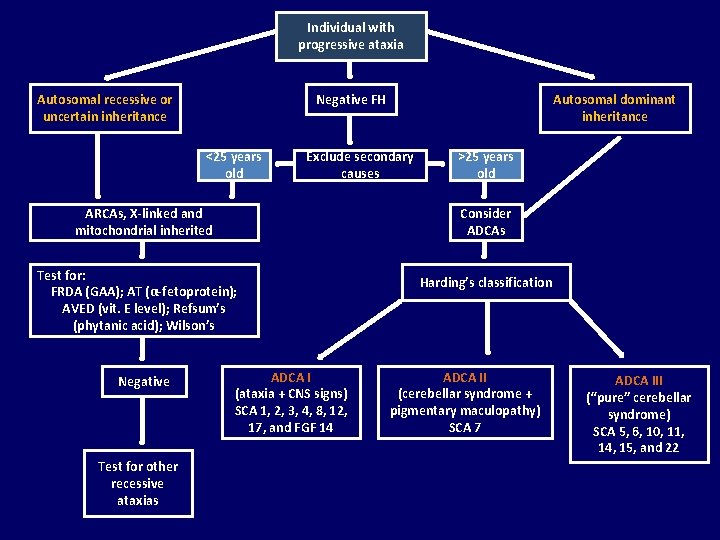
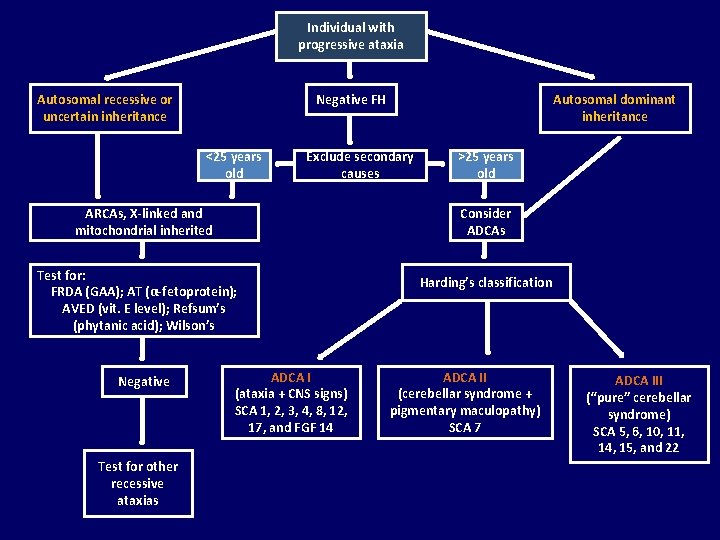
Individual with progressive ataxia Negative FH Autosomal recessive or uncertain inheritance <25 years old Exclude secondary causes ARCAs, X-linked and mitochondrial inherited Test for other recessive ataxias >25 years old Consider ADCAs Test for: FRDA (GAA); AT (α-fetoprotein); AVED (vit. E level); Refsum’s (phytanic acid); Wilson’s Negative Autosomal dominant inheritance ADCA I (ataxia + CNS signs) SCA 1, 2, 3, 4, 8, 12, 17, and FGF 14 Harding’s classification ADCA II (cerebellar syndrome + pigmentary maculopathy) SCA 7 ADCA III (“pure” cerebellar syndrome) SCA 5, 6, 10, 11, 14, 15, and 22
Outline of today’s lecture v Clinical Scenario v Anatomy and Physiology v Is it Cerebellar Ataxia v History and Examination v Classification v Hereditary Ataxias v Acquired Ataxias v Treatment v Conclusion v MCQs
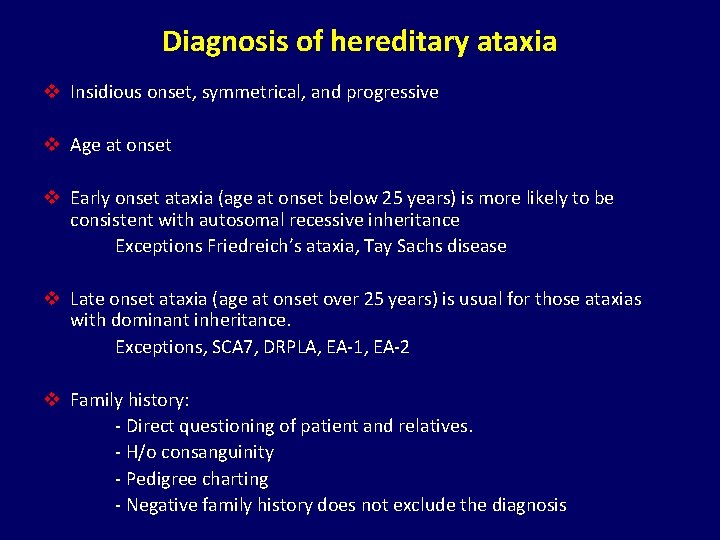
Diagnosis of hereditary ataxia v Insidious onset, symmetrical, and progressive v Age at onset v Early onset ataxia (age at onset below 25 years) is more likely to be consistent with autosomal recessive inheritance Exceptions Friedreich’s ataxia, Tay Sachs disease v Late onset ataxia (age at onset over 25 years) is usual for those ataxias with dominant inheritance. Exceptions, SCA 7, DRPLA, EA-1, EA-2 v Family history: - Direct questioning of patient and relatives. - H/o consanguinity - Pedigree charting - Negative family history does not exclude the diagnosis
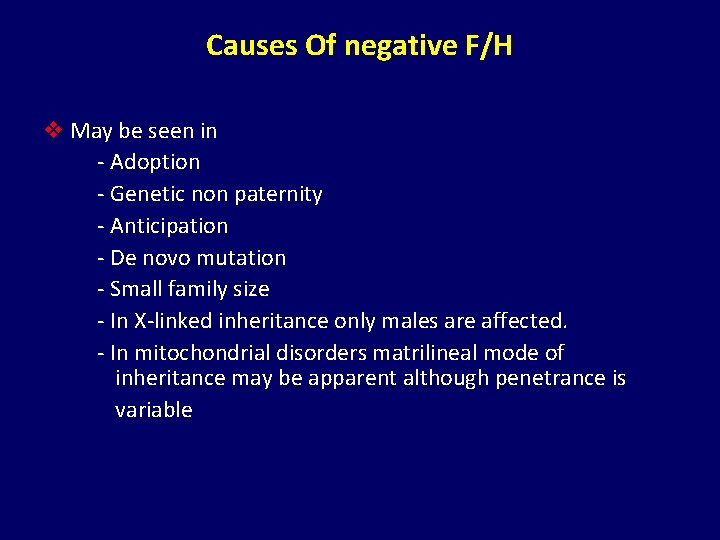
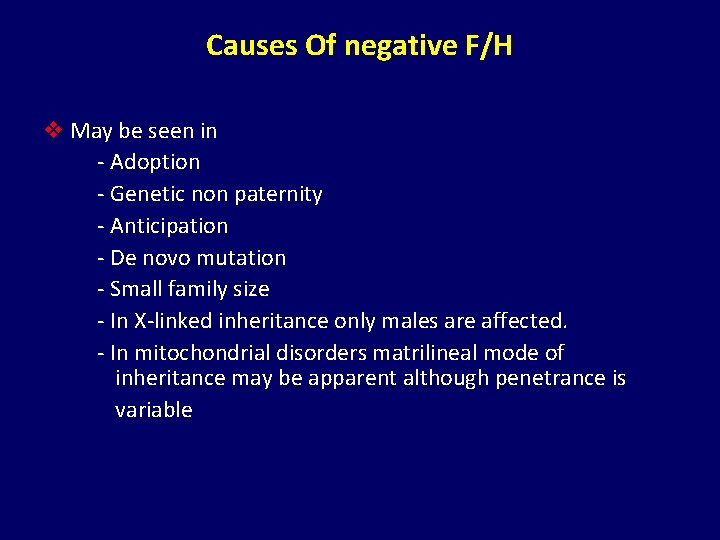
Causes Of negative F/H v May be seen in - Adoption - Genetic non paternity - Anticipation - De novo mutation - Small family size - In X-linked inheritance only males are affected. - In mitochondrial disorders matrilineal mode of inheritance may be apparent although penetrance is variable
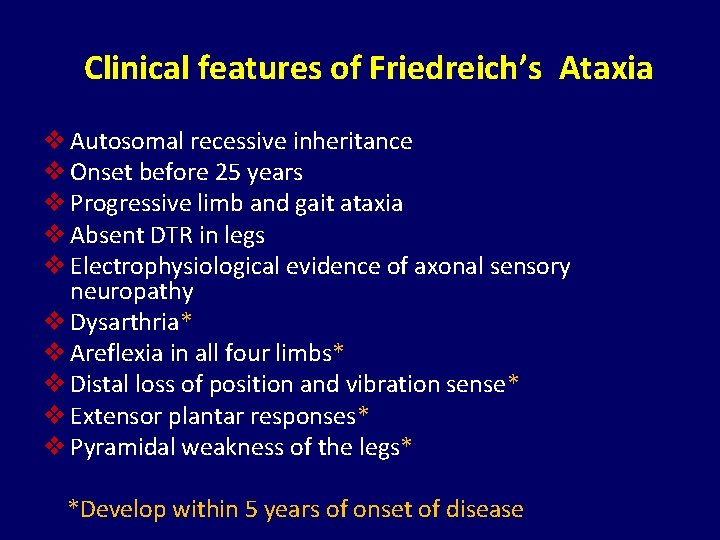
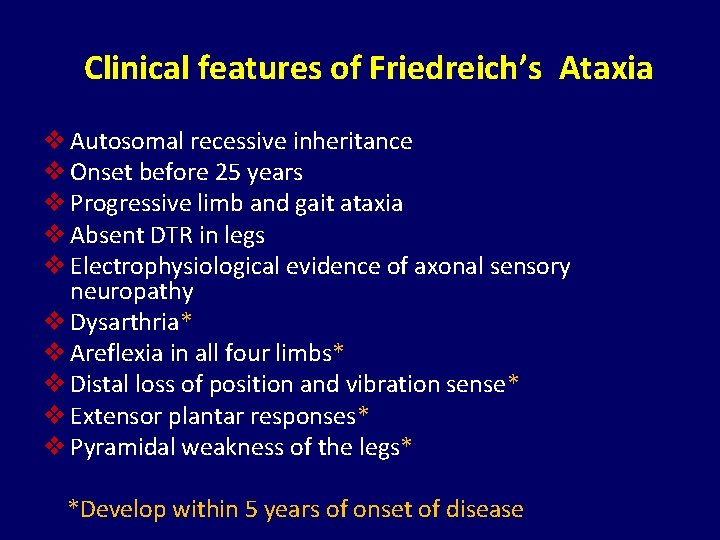
Clinical features of Friedreich’s Ataxia v Autosomal recessive inheritance v Onset before 25 years v Progressive limb and gait ataxia v Absent DTR in legs v Electrophysiological evidence of axonal sensory neuropathy v Dysarthria* v Areflexia in all four limbs* v Distal loss of position and vibration sense* v Extensor plantar responses* v Pyramidal weakness of the legs* *Develop within 5 years of onset of disease
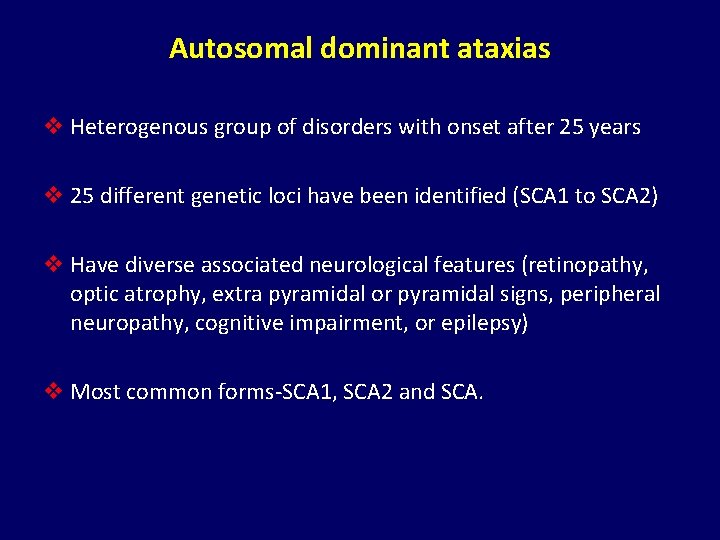
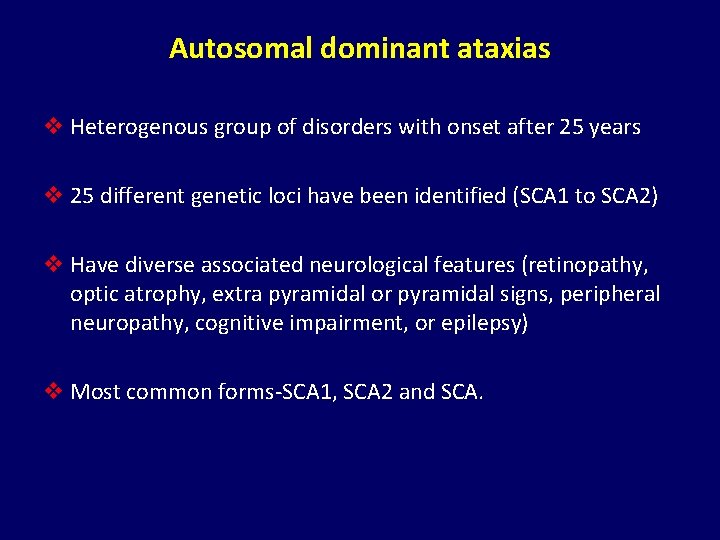
Autosomal dominant ataxias v Heterogenous group of disorders with onset after 25 years v 25 different genetic loci have been identified (SCA 1 to SCA 2) v Have diverse associated neurological features (retinopathy, optic atrophy, extra pyramidal or pyramidal signs, peripheral neuropathy, cognitive impairment, or epilepsy) v Most common forms-SCA 1, SCA 2 and SCA.
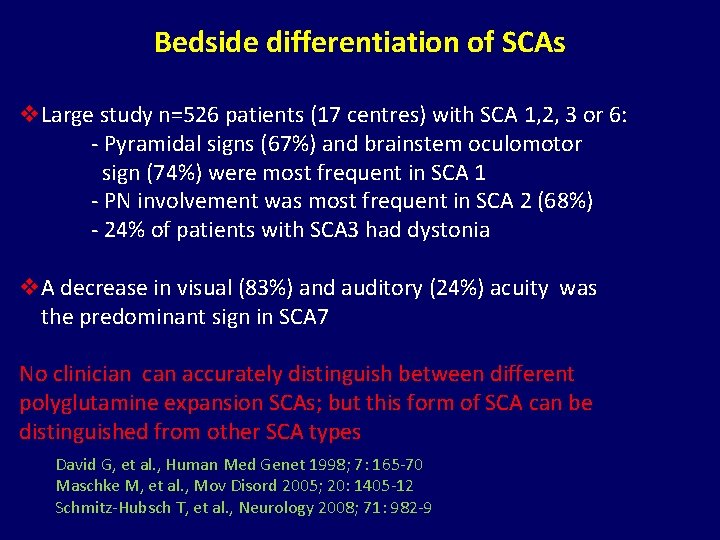
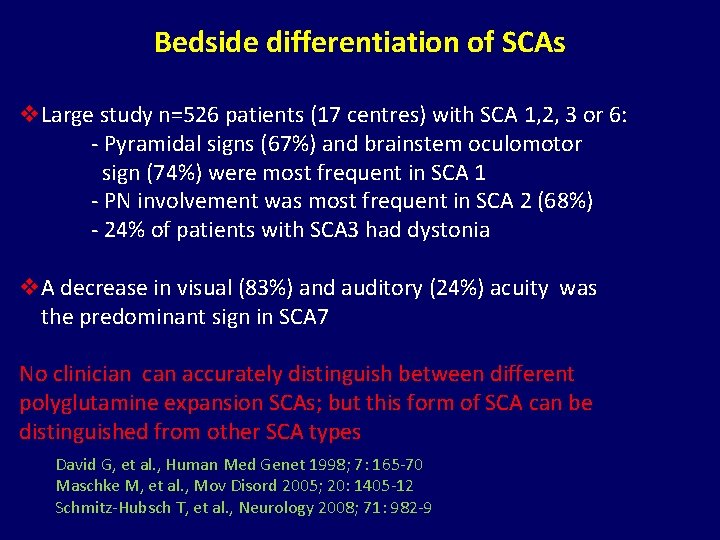
Bedside differentiation of SCAs v. Large study n=526 patients (17 centres) with SCA 1, 2, 3 or 6: - Pyramidal signs (67%) and brainstem oculomotor sign (74%) were most frequent in SCA 1 - PN involvement was most frequent in SCA 2 (68%) - 24% of patients with SCA 3 had dystonia v. A decrease in visual (83%) and auditory (24%) acuity was the predominant sign in SCA 7 No clinician can accurately distinguish between different polyglutamine expansion SCAs; but this form of SCA can be distinguished from other SCA types David G, et al. , Human Med Genet 1998; 7: 165 -70 Maschke M, et al. , Mov Disord 2005; 20: 1405 -12 Schmitz-Hubsch T, et al. , Neurology 2008; 71: 982 -9
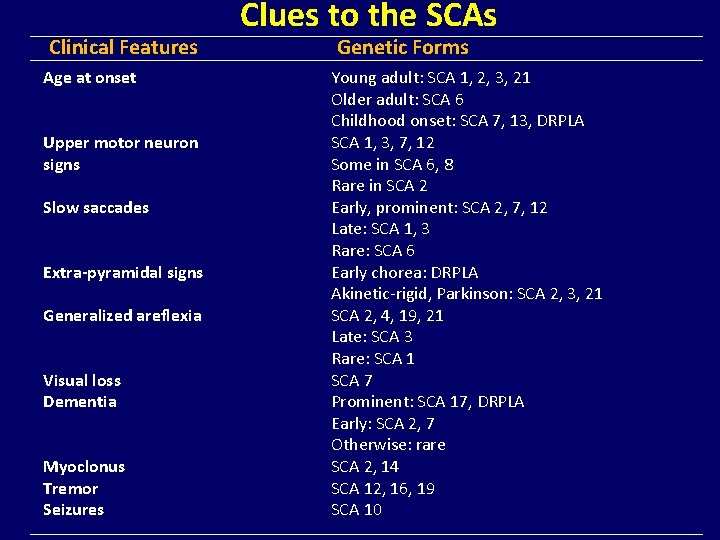
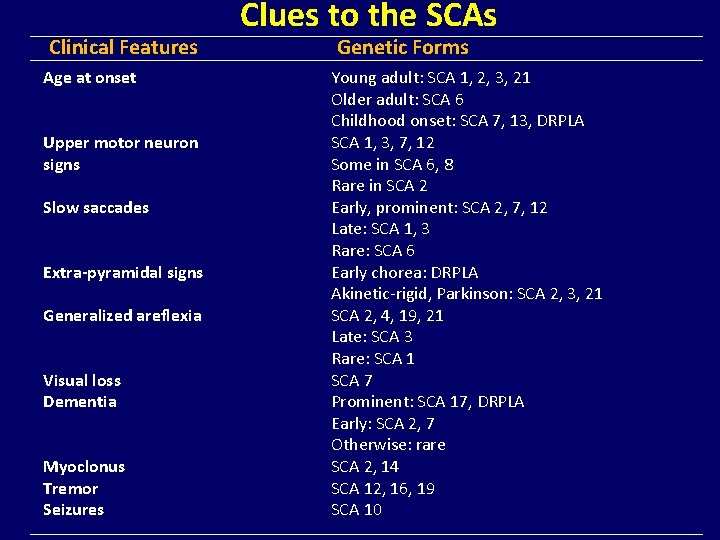
Clinical Features Age at onset Upper motor neuron signs Slow saccades Extra-pyramidal signs Generalized areflexia Visual loss Dementia Myoclonus Tremor Seizures Clues to the SCAs Genetic Forms Young adult: SCA 1, 2, 3, 21 Older adult: SCA 6 Childhood onset: SCA 7, 13, DRPLA SCA 1, 3, 7, 12 Some in SCA 6, 8 Rare in SCA 2 Early, prominent: SCA 2, 7, 12 Late: SCA 1, 3 Rare: SCA 6 Early chorea: DRPLA Akinetic-rigid, Parkinson: SCA 2, 3, 21 SCA 2, 4, 19, 21 Late: SCA 3 Rare: SCA 1 SCA 7 Prominent: SCA 17, DRPLA Early: SCA 2, 7 Otherwise: rare SCA 2, 14 SCA 12, 16, 19 SCA 10
Outline of today’s lecture v Clinical Scenario v Anatomy and Physiology v Is it Cerebellar Ataxia v History and Examination v Classification v Hereditary Ataxias v Acquired Ataxias v Treatment v Conclusion v MCQs

Classification of acquired cerebellar ataxias v Ataxias due to toxic reasons Alcoholic cerebellar degeneration (ACD) Ataxias due to other toxic reasons v Immune-mediated ataxias Paraneoplastic cerebellar degeneration (PCD) Other immune-mediated ataxias v Ataxias due to vitamin deficiency v Ataxias due to other rare causes
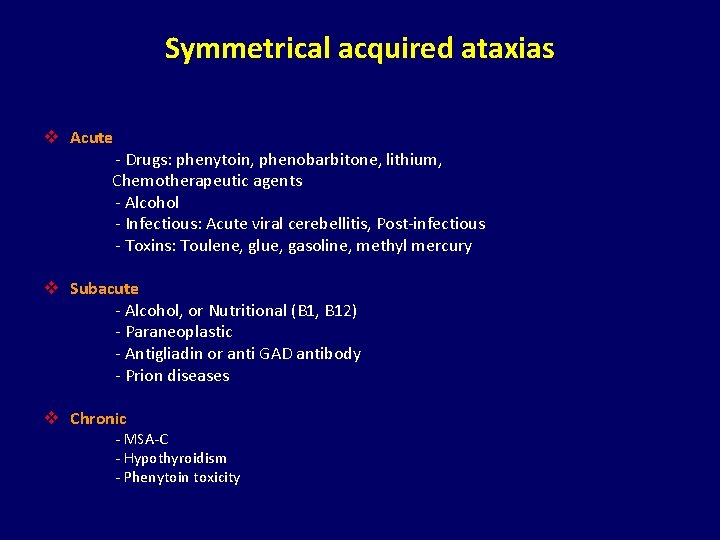
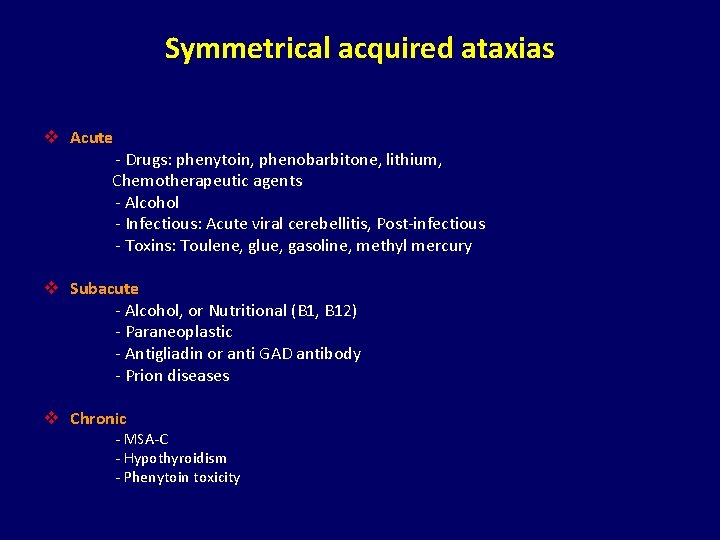
Symmetrical acquired ataxias v Acute - Drugs: phenytoin, phenobarbitone, lithium, Chemotherapeutic agents - Alcohol - Infectious: Acute viral cerebellitis, Post-infectious - Toxins: Toulene, glue, gasoline, methyl mercury v Subacute - Alcohol, or Nutritional (B 1, B 12) - Paraneoplastic - Antigliadin or anti GAD antibody - Prion diseases v Chronic - MSA-C - Hypothyroidism - Phenytoin toxicity
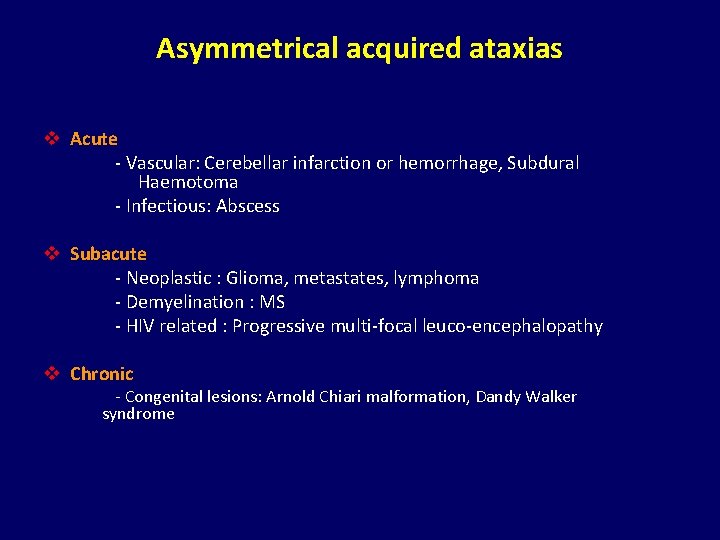
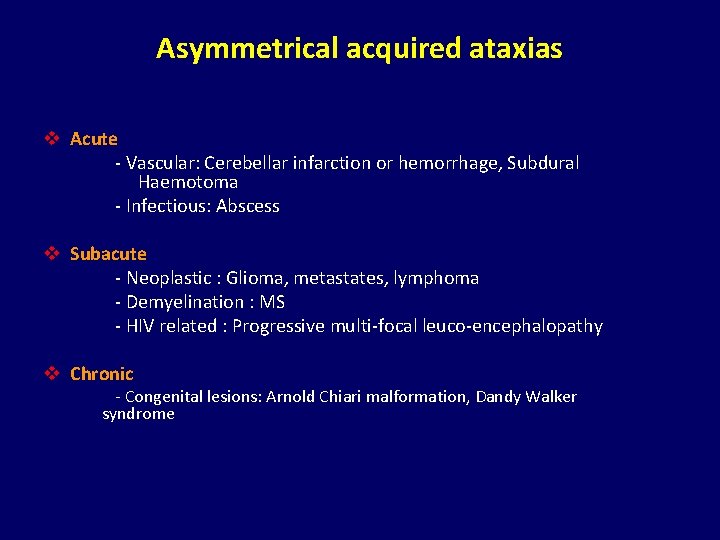
Asymmetrical acquired ataxias v Acute - Vascular: Cerebellar infarction or hemorrhage, Subdural Haemotoma - Infectious: Abscess v Subacute - Neoplastic : Glioma, metastates, lymphoma - Demyelination : MS - HIV related : Progressive multi-focal leuco-encephalopathy v Chronic - Congenital lesions: Arnold Chiari malformation, Dandy Walker syndrome
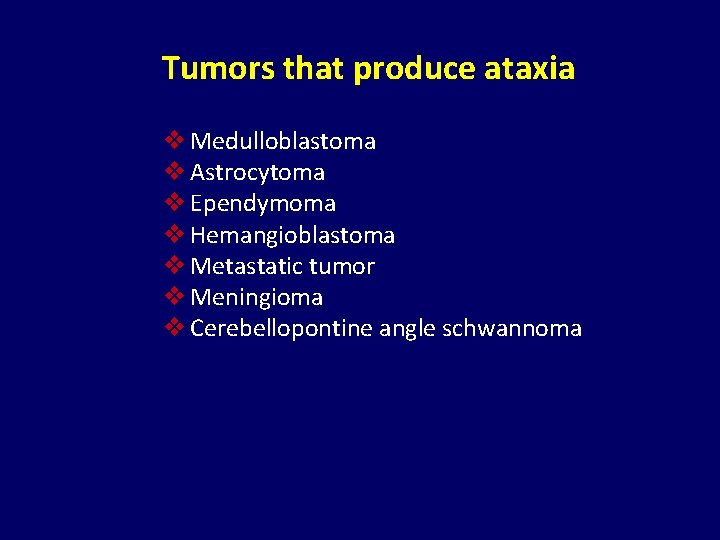
Tumors that produce ataxia v Medulloblastoma v Astrocytoma v Ependymoma v Hemangioblastoma v Metastatic tumor v Meningioma v Cerebellopontine angle schwannoma
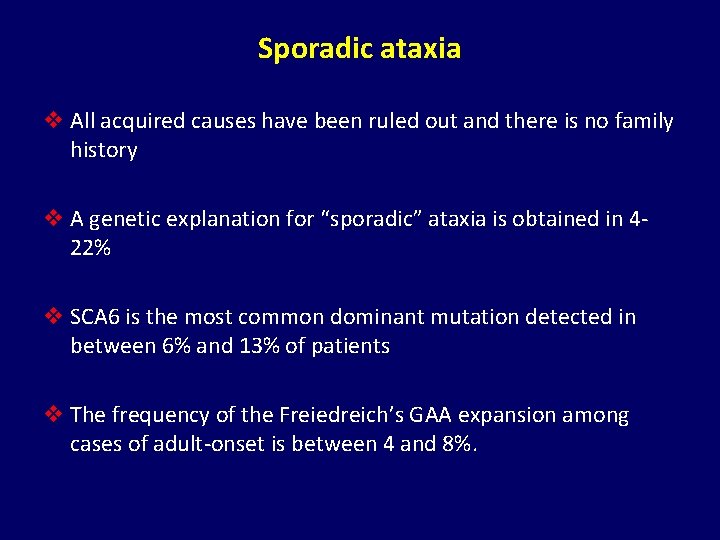
Sporadic ataxia v All acquired causes have been ruled out and there is no family history v A genetic explanation for “sporadic” ataxia is obtained in 422% v SCA 6 is the most common dominant mutation detected in between 6% and 13% of patients v The frequency of the Freiedreich’s GAA expansion among cases of adult-onset is between 4 and 8%.
Outline of today’s lecture v Clinical Scenario v Anatomy and Physiology v Is it Cerebellar Ataxia v History and Examination v Classification v Hereditary Ataxias v Acquired Ataxias v Treatment v Conclusion v MCQs
Treatment v Identify treatable causes of ataxia v No proven therapy for SCAs v Some patients with parameoplastic cerebellar syndrome improve following removal of tumour and immunotherapy v Preliminary evidence suggests that idebenone, a free radical scavenger improves myocardial hypertrophy v Genetic counselling can reduce risk in future generations
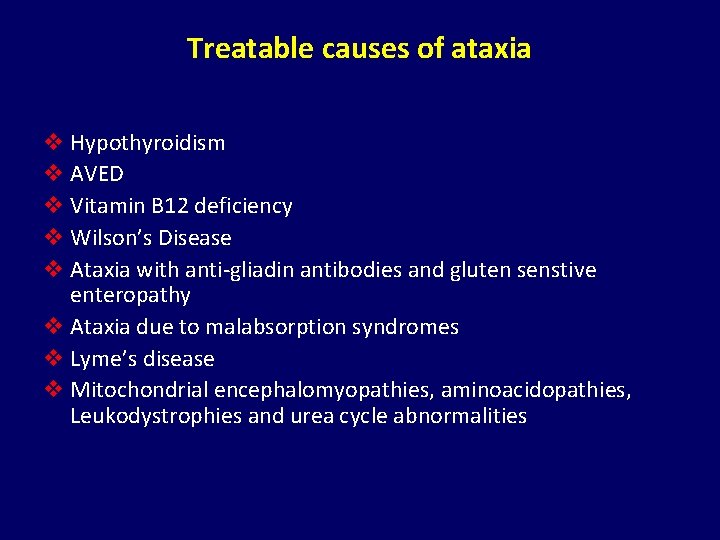
Treatable causes of ataxia v Hypothyroidism v AVED v Vitamin B 12 deficiency v Wilson’s Disease v Ataxia with anti-gliadin antibodies and gluten senstive enteropathy v Ataxia due to malabsorption syndromes v Lyme’s disease v Mitochondrial encephalomyopathies, aminoacidopathies, Leukodystrophies and urea cycle abnormalities
Outline of today’s lecture v Clinical Scenario v Anatomy and Physiology v Is it Cerebellar Ataxia v History and Examination v Classification v Hereditary Ataxias v Acquired Ataxias v Treatment v Conclusion v MCQs
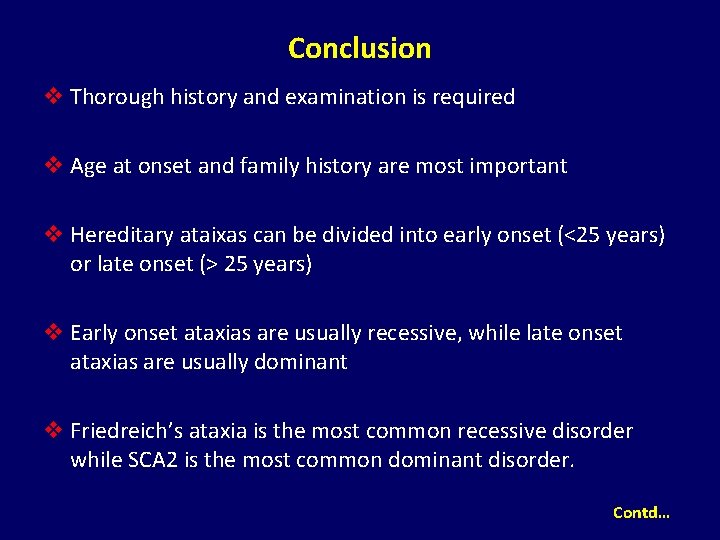
Conclusion v Thorough history and examination is required v Age at onset and family history are most important v Hereditary ataixas can be divided into early onset (<25 years) or late onset (> 25 years) v Early onset ataxias are usually recessive, while late onset ataxias are usually dominant v Friedreich’s ataxia is the most common recessive disorder while SCA 2 is the most common dominant disorder. Contd…
Conclusion contd… v. No single physical sign is specific for a single disorder v. Investigations should be performed in a logical order v. Treatable causes should be excluded
Outline of today’s lecture v Clinical Scenario v Anatomy and Physiology v Is it Cerebellar Ataxia v History and Examination v Classification v Hereditary Ataxias v Acquired Ataxias v Treatment v Conclusion v MCQs
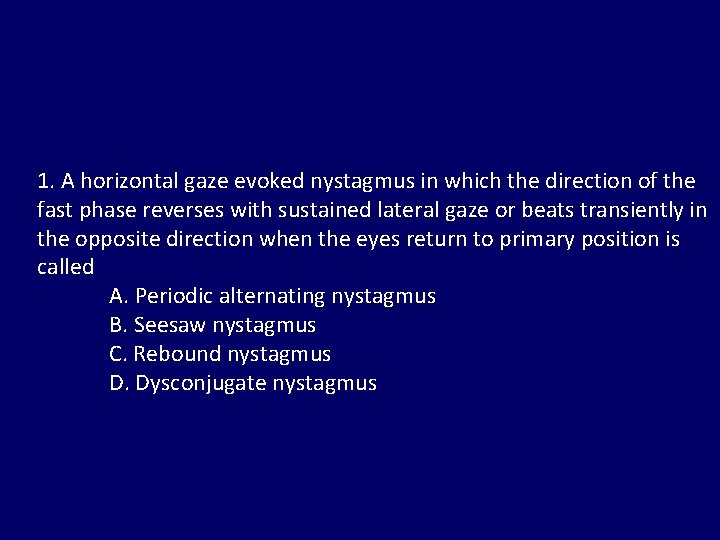
1. A horizontal gaze evoked nystagmus in which the direction of the fast phase reverses with sustained lateral gaze or beats transiently in the opposite direction when the eyes return to primary position is called A. Periodic alternating nystagmus B. Seesaw nystagmus C. Rebound nystagmus D. Dysconjugate nystagmus
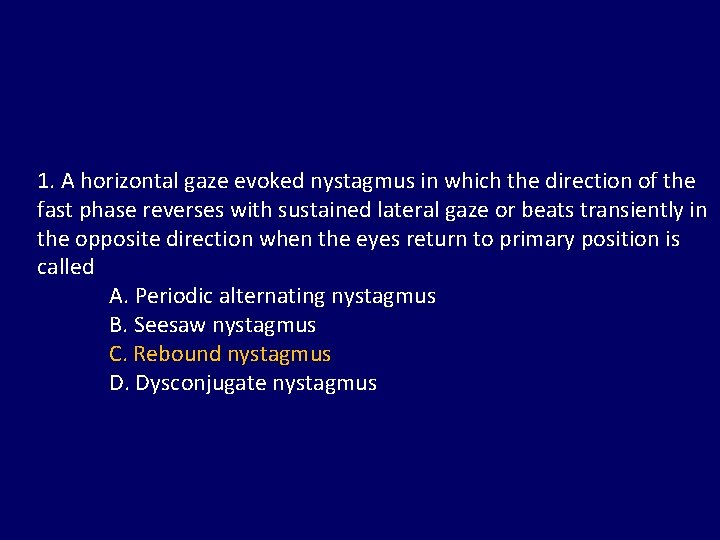
1. A horizontal gaze evoked nystagmus in which the direction of the fast phase reverses with sustained lateral gaze or beats transiently in the opposite direction when the eyes return to primary position is called A. Periodic alternating nystagmus B. Seesaw nystagmus C. Rebound nystagmus D. Dysconjugate nystagmus
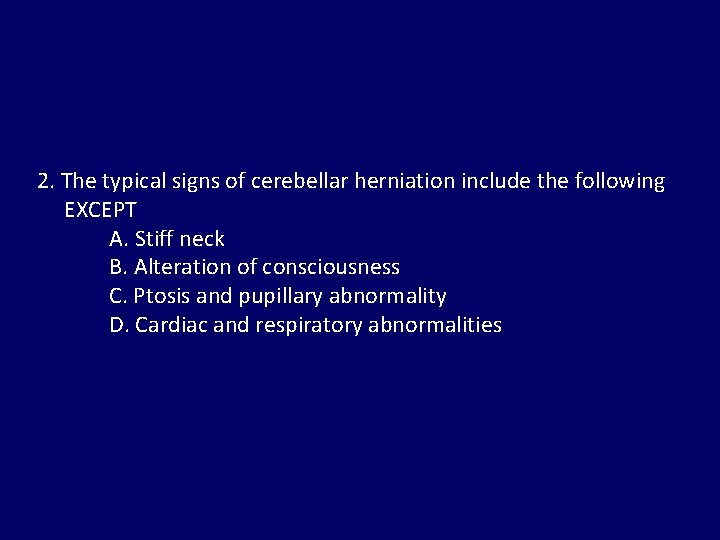
2. The typical signs of cerebellar herniation include the following EXCEPT A. Stiff neck B. Alteration of consciousness C. Ptosis and pupillary abnormality D. Cardiac and respiratory abnormalities
2. The typical signs of cerebellar herniation include the following EXCEPT A. Stiff neck B. Alteration of consciousness C. Ptosis and pupillary abnormality D. Cardiac and respiratory abnormalities
3. Romberg’s sign is positive in which type of lesion : A. Cerebellar B. Posterior column C. Hysterical D. Vestibular
3. Romberg’s sign is positive in which type of lesion : A. Cerebellar B. Posterior column C. Hysterical D. Vestibular
4. Harding’s classification of cerebellar ataxia is based upon : A. Mode of inheritance B. Site of involvement C. Chromosomal abnormality D. Metabolic abnormality
4. Harding’s classification of cerebellar ataxia is based upon : A. Mode of inheritance B. Site of involvement C. Chromosomal abnormality D. Metabolic abnormality
5. Which statement is not true of Friedreich’s ataxia? A. Recessive inheritance B. Dysarthria C. Flexor plantar response D. Absent ankle jerk
5. Which statement is not true of Friedreich’s ataxia? A. Recessive inheritance B. Dysarthria C. Flexor plantar response D. Absent ankle jerk
6. Alcoholic cerebellar degeneration is characterized by : A. Gaze evoked nystagmus B. Limb ataxia C. Gait ataxia D. Action myoclonus
6. Alcoholic cerebellar degeneration is characterized by : A. Gaze evoked nystagmus B. Limb ataxia C. Gait ataxia D. Action myoclonus
7. Cerebellar ataxia can result from intoxication with : A. Lead B. Mercury C. Manganese D. Gold
7. Cerebellar ataxia can result from intoxication with : A. Lead B. Mercury C. Manganese D. Gold
8. Wadia’s type of spinocerebellar degeneration is characterized by A. Limitation of downgaze B. Limitation of upgaze C. Slowing of saccadic movements D. Broken smooth pursuit
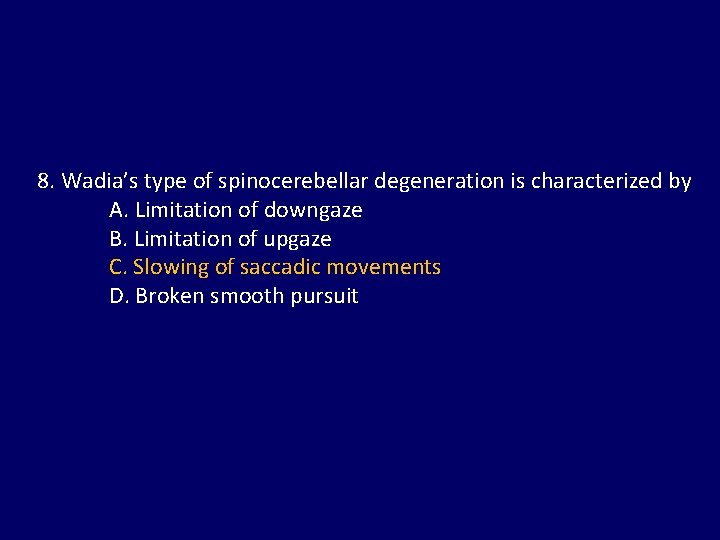
8. Wadia’s type of spinocerebellar degeneration is characterized by A. Limitation of downgaze B. Limitation of upgaze C. Slowing of saccadic movements D. Broken smooth pursuit
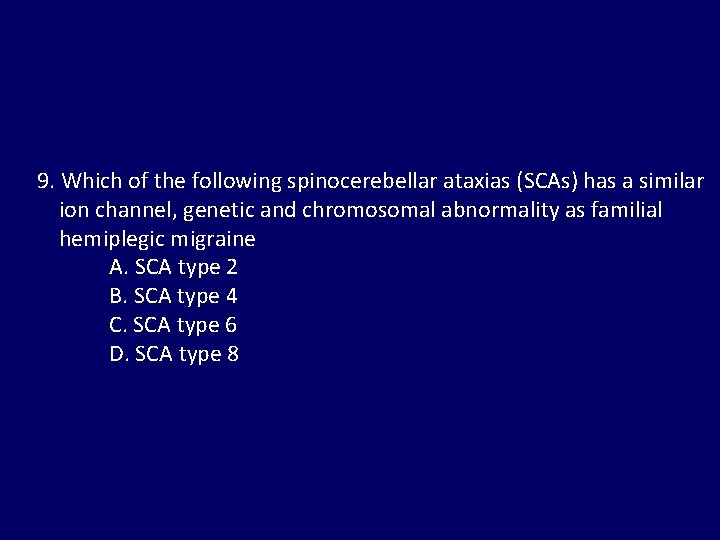
9. Which of the following spinocerebellar ataxias (SCAs) has a similar ion channel, genetic and chromosomal abnormality as familial hemiplegic migraine A. SCA type 2 B. SCA type 4 C. SCA type 6 D. SCA type 8
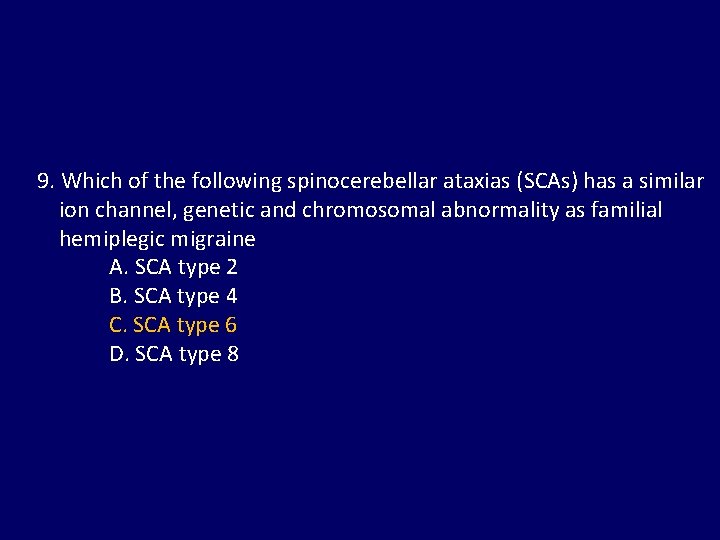
9. Which of the following spinocerebellar ataxias (SCAs) has a similar ion channel, genetic and chromosomal abnormality as familial hemiplegic migraine A. SCA type 2 B. SCA type 4 C. SCA type 6 D. SCA type 8
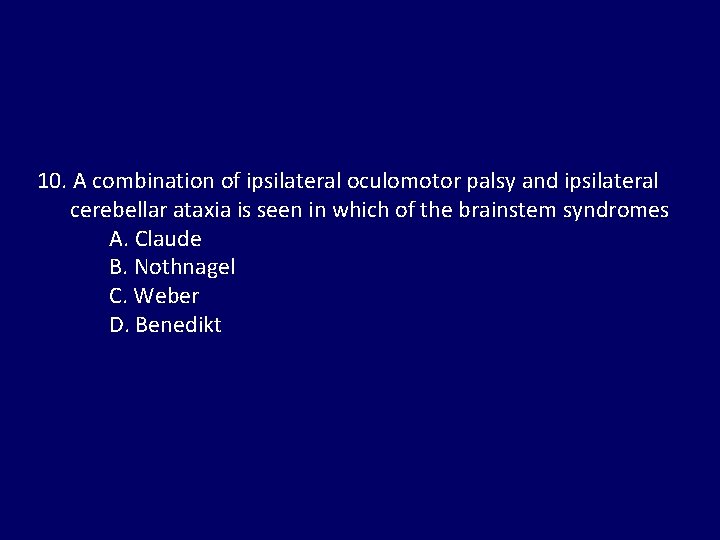
10. A combination of ipsilateral oculomotor palsy and ipsilateral cerebellar ataxia is seen in which of the brainstem syndromes A. Claude B. Nothnagel C. Weber D. Benedikt
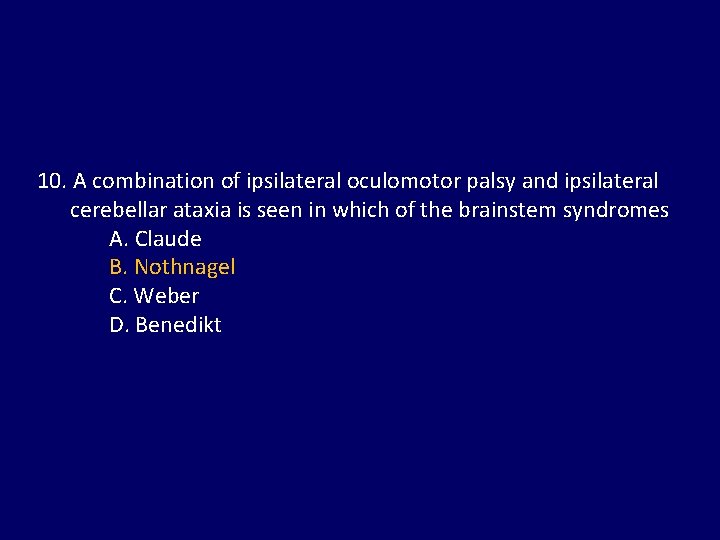
10. A combination of ipsilateral oculomotor palsy and ipsilateral cerebellar ataxia is seen in which of the brainstem syndromes A. Claude B. Nothnagel C. Weber D. Benedikt
 Sensory ataxia causes
Sensory ataxia causes Optic ataxia
Optic ataxia Spastic gait
Spastic gait Stroke assessment
Stroke assessment Causes of cerebellar dysfunction
Causes of cerebellar dysfunction Gait ataxia spokane
Gait ataxia spokane Exercises for ataxia
Exercises for ataxia Limb ataxia
Limb ataxia Ataxia
Ataxia Gait patterns with walker
Gait patterns with walker Cerebellopontine
Cerebellopontine Rakesh heer
Rakesh heer Uiuc cs 445
Uiuc cs 445 Smita biswas md
Smita biswas md Dr rakesh biswas
Dr rakesh biswas Ca rakesh agrawal
Ca rakesh agrawal Dr rakesh sharma ahmedabad
Dr rakesh sharma ahmedabad Dr rakesh biswas
Dr rakesh biswas Rakesh mehta nsdl
Rakesh mehta nsdl Rakesh kumar ntnu
Rakesh kumar ntnu Patient 2 patient
Patient 2 patient Waterfall approach vs shower approach
Waterfall approach vs shower approach Traditional approach to system development
Traditional approach to system development Multiple approach avoidance
Multiple approach avoidance Tony wagner's seven survival skills
Tony wagner's seven survival skills Virtual circuit and datagram
Virtual circuit and datagram Bandura's reciprocal determinism
Bandura's reciprocal determinism Theoretical models of counseling
Theoretical models of counseling Research design definition
Research design definition Appropriate patient selection
Appropriate patient selection Patient counselling for peptic ulcer disease
Patient counselling for peptic ulcer disease Patient scenarios examples
Patient scenarios examples Patient zone
Patient zone Chapter 53 care of the patient with a sensory disorder
Chapter 53 care of the patient with a sensory disorder Patient safety goals - awareness course
Patient safety goals - awareness course Nature metaphors for love
Nature metaphors for love Safe patient transfers
Safe patient transfers Interpersonal relations theory
Interpersonal relations theory Assessment of patient
Assessment of patient 2013 hospital national patient safety goals
2013 hospital national patient safety goals A noiseless patient spider paraphrase
A noiseless patient spider paraphrase Brenda milner patient hm
Brenda milner patient hm Christine andre
Christine andre Medically compromised patient meaning
Medically compromised patient meaning Bidirectional patient messaging
Bidirectional patient messaging Sacred 7 medical
Sacred 7 medical Meeting patient expectations in nursing
Meeting patient expectations in nursing Ros medical history
Ros medical history Care of critically ill surgical patient
Care of critically ill surgical patient Doctor patient relationship ethics
Doctor patient relationship ethics Patient hands
Patient hands Patient classification system
Patient classification system Complex patient populations
Complex patient populations Patient handout template
Patient handout template Patient safety evaluation system
Patient safety evaluation system Patient throughput definition
Patient throughput definition Paternalism in dentistry
Paternalism in dentistry Pre operative care
Pre operative care Theme of a noiseless patient spider
Theme of a noiseless patient spider Patient notification system
Patient notification system Role of nurse in maintaining records and reports
Role of nurse in maintaining records and reports Nursing interventions classification (nic)
Nursing interventions classification (nic) Patient
Patient Monocacy health partners patient portal
Monocacy health partners patient portal History taking of patient
History taking of patient The process of classifying and reviewing past due accounts
The process of classifying and reviewing past due accounts Improving the patient journey
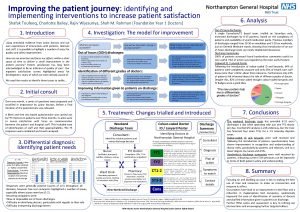
Improving the patient journey