The Core Concepts in the Doctor Patient Relationship


- Slides: 26
The Core Concepts in the Doctor- Patient Relationship & Conflicts of Interest Lead Faculty: Dr Suzanne Goh Dr Anupama Chowdhury Dr Lalit Krishna Slides adapted from Dr Rukshini Puvanendran and Prof Thirumoorthy, with thanks 11 October 2017
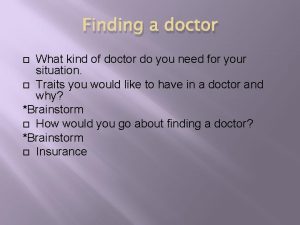
The Doctor-Patient Relationship • LESSON OBJECTIVES: • To examine and understand the ethical and legal nature of the Doctor-Patient Relationship. • To acquire the reasoning skills in resolving ethical and legal issues in the doctor-patient relationship esp. in the areas of: – Refusal of care. – Conscientious objectors. – Termination of Care. – Sexual relationships between patients and doctors. – Gifts from patients to physicians

The Doctor-Patient Relationship The Nature, Value and Principles of the Doctor Patient Relationship
The differing Roles of the Doctor in the Doctor-Patient Relationship • The Healer* – in a Therapeutic role of caring for the ill. • The Examiner – in the role of certification of health status or Assessing disability/prognosis – As a Medical expert witness • The Scientist – when conducting clinical research • The Educator – when conducting medical training involving patients
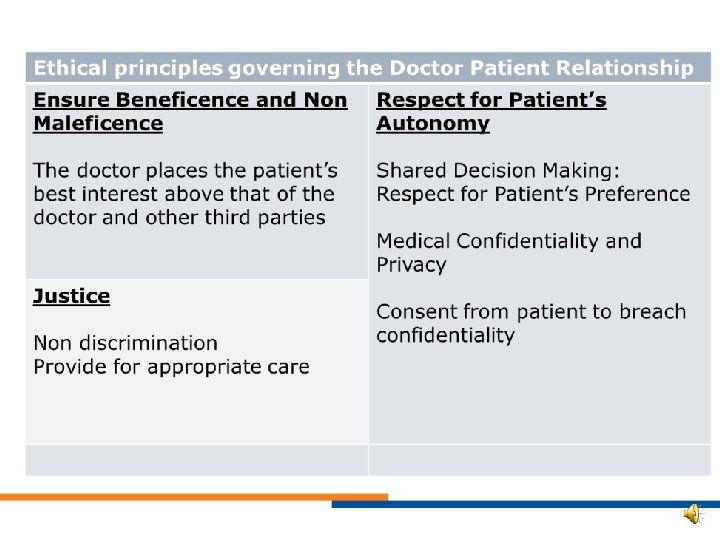
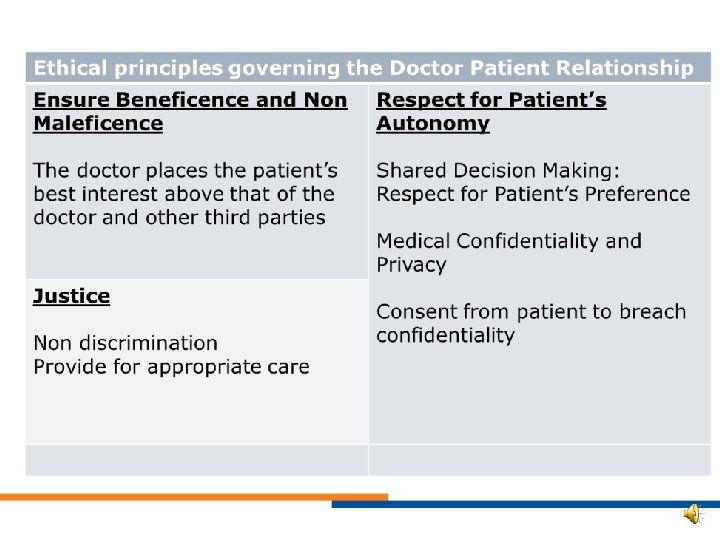
The Doctor-Patient Therapeutic Relationship is governed by: • Ethical principles of the Profession • Legal principles in Statute and Common Law
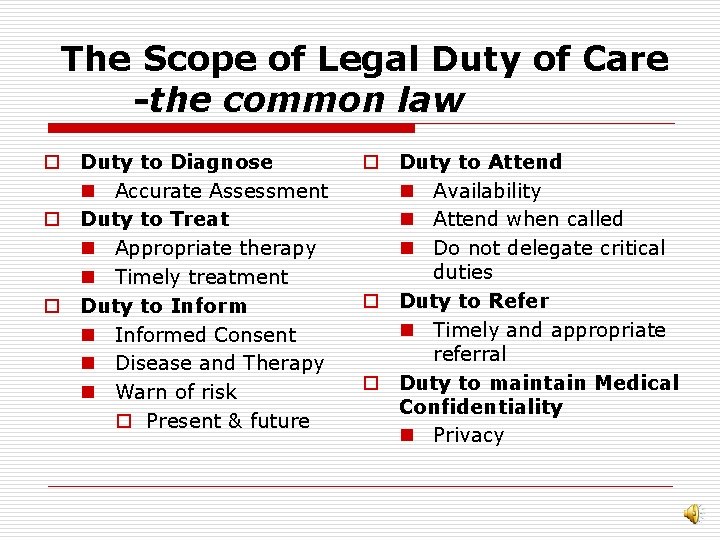
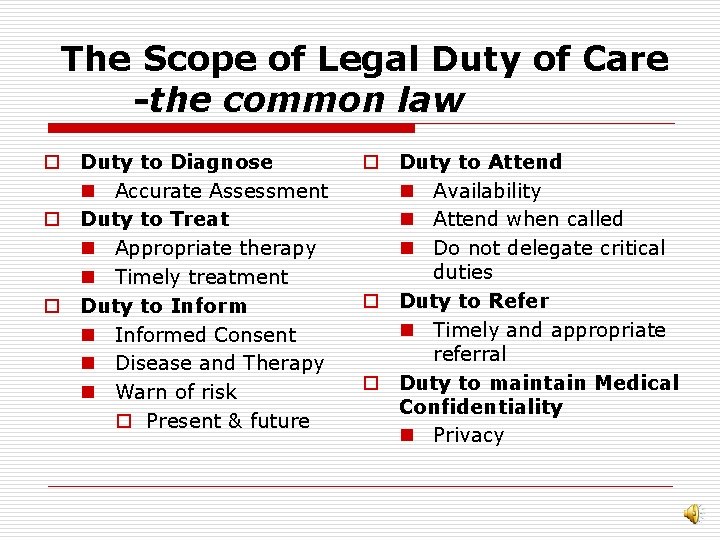
The Scope of Legal Duty of Care -the common law o Duty to Diagnose n Accurate Assessment o Duty to Treat n Appropriate therapy n Timely treatment o Duty to Inform n Informed Consent n Disease and Therapy n Warn of risk o Present & future o Duty to Attend n Availability n Attend when called n Do not delegate critical duties o Duty to Refer n Timely and appropriate referral o Duty to maintain Medical Confidentiality n Privacy
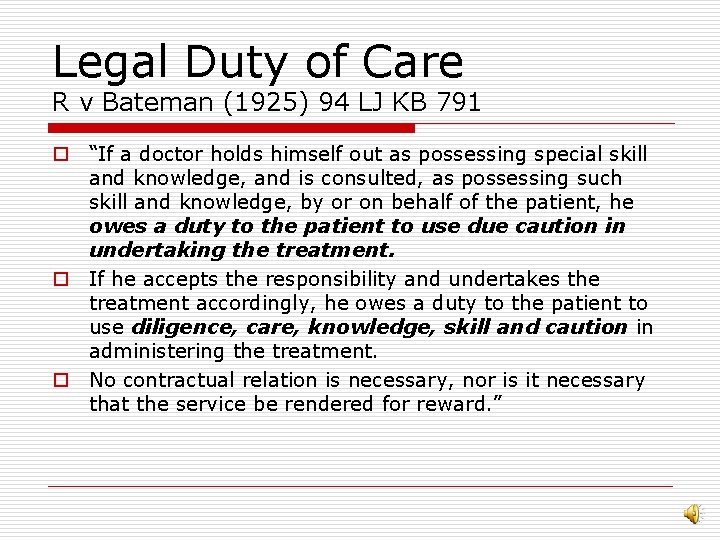
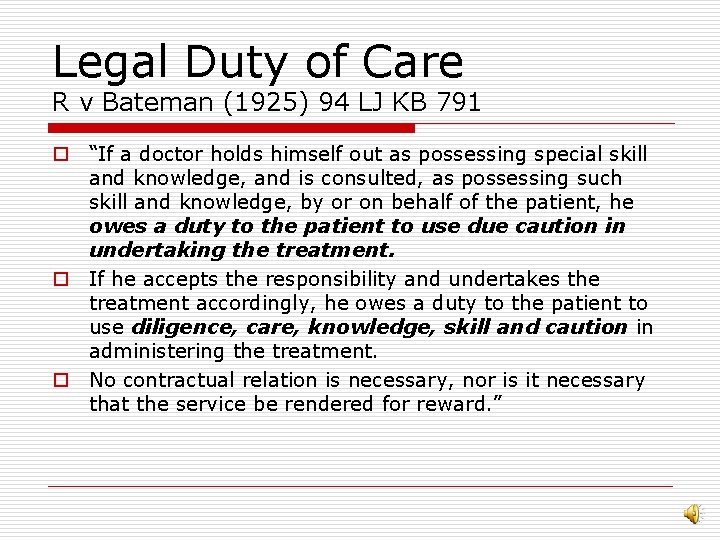
Legal Duty of Care R v Bateman (1925) 94 LJ KB 791 o “If a doctor holds himself out as possessing special skill and knowledge, and is consulted, as possessing such skill and knowledge, by or on behalf of the patient, he owes a duty to the patient to use due caution in undertaking the treatment. o If he accepts the responsibility and undertakes the treatment accordingly, he owes a duty to the patient to use diligence, care, knowledge, skill and caution in administering the treatment. o No contractual relation is necessary, nor is it necessary that the service be rendered for reward. ”
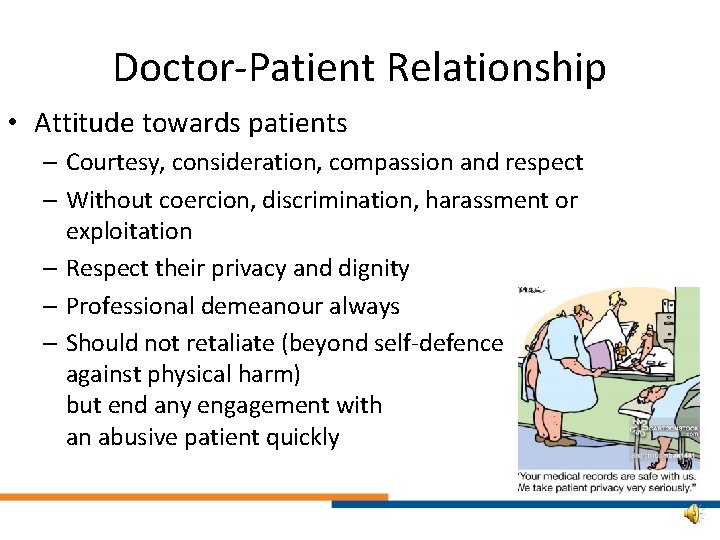
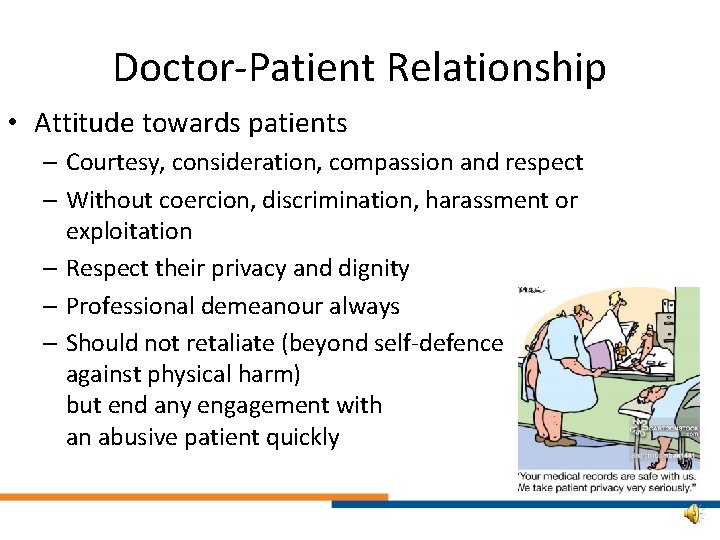
Doctor-Patient Relationship • Attitude towards patients – Courtesy, consideration, compassion and respect – Without coercion, discrimination, harassment or exploitation – Respect their privacy and dignity – Professional demeanour always – Should not retaliate (beyond self-defence against physical harm) but end any engagement with an abusive patient quickly
Doctor-Patient Relationship • COMMUNICATION • Good communication with patients is based on – to support patient openness, truthfulness autonomy, and honesty – facilitate decision • Must not communicate making by patients such that patients’ – maximize the potential welfare is compromised, for patient benefit. or they are deprived of autonomy or suffer harm
Doctor-Patient Relationship • Personal Beliefs – Remain personal • Conscientious objections need to be explained non-judgmentally • Ensure they are aware of their other options - Eg referrals
Occupational Risk • Determination of risk – By objective, scientific evidence – Not subjective judgement • Acknowledge, address own fears & limitations – Reflection • Reduce occupational risks – Measures to minimise risk, NOT avoid patients who may carry risks, eg HIV • Balance risks to Dr vs Benefits to patients
Conscientious Objectors • Conscience is a burden that belongs to the individual professional; patients should not have to shoulder it nor suffer its consequences • Patients should have access to all legal options in information, diagnosis, treatment and referral • Cantour JD N Engl J Med 2009; 360(15) 1484 -5
Maintaining Propriety • Keep sexual boundaries - Including physical contact, words and gestures • Explanation before asking intimate questions or intimate examination • Ensure reasonable patient feels safe and not taken advantage of when examining - Chaperone if necessary - Privacy during undressing • If patient exhibits sexualised behaviour towards you - Don’t reciprocate - Gently but firmly discourage - Consider need to formally end patient-doctor relationship
Sexual contact between Doctor and Patient • Sexual contact or romantic relationship with a patient concurrent with the physician-patient relationship is unethical. – Obscures objective judgment by physicians – Exploits vulnerability of patients • Trust & Dependency – Detracts from the goals of medicine – Erodes patients trust and public confidence
Gifts from patients • Patients who bear gifts – May have inappropriate expectations • Expectations of special services • Request for unlawful or unethical deeds – May have a hidden agenda • Satisfy patient’s own needs • Clinicians soliciting gifts – Unethical for clinicians to solicit from their patients for the hospital, charities, social or political causes
Gifts from patients • Well intentioned and appropriate gifts must be accepted graciously – Appropriate time – Appropriate value – Appropriate cultural context • Do not let gifts delude you – Exaggerated sense of their skills & importance • Conform to organizational policy • Share the gift with others in the clinic – Inform the patient
Termination of Doctor-Patient Relationship • If the patient-doctor relationship is so compromised or rendered so ineffective that you feel unable to continue to provide care for the patients, you must explain this to patients before terminating the relationship. • Must offer to refer them to other doctors and ensure a smooth handover / transition of care, with all the necessary relevant medical information, as well providing continued care until transition complete
Doctor-Patient Relationship • Professional relationship – Not a social relationship • Gifts, Social media • Soliciting gifts – Not an economic relationship • Avoid business dealings • Contractual issues are secondary. • Relationship in force even if not paid. • Boundaries MUST BE GUARDED – Avoiding blurring the borders – Sexual relationships violate the boundaries
Conflicts of Interest (Co. I) • LESSON OBJECTIVES: • To identify and define potential conflicts of interest in medicine • To recognise misconceptions about Co. I • To learn how to address Co. I appropriately
Conflict of Interest • A set of circumstances which creates a risk that professional judgement or actions regarding a primary interest will be unduly influenced by a secondary interest. – For doctors, the patient’s health should be their primary interest, taking precedence over selfinterest or third party interests
Co. I in Medical Practice - Definitions • Compromise of physicians’ primary interest • Compromise of physicians’ judgement or the decision-making process • Potential for detrimental outcomes or compromised judgment (broad definition) – Secondary interests unduly influencing primary interests
Conflicts of Interest • May be perceived or apparent – Did not or has not happened, but MIGHT – Still has the potential to erode public trust • Financial Co. I – Flaws of reimbursement systems • Fee-for-service -> increase services whether indicated or not • Payment per capita -> reduces services or withholds beneficial care – May subtly influence Dr’s decisions (unintentional)
Consequences • Primacy of patient’s best interest subordinated – May lead to patient harm • Dr’s judgement/decision-making compromised – Irrespective of patient outcome – Eg ordering unnecessary tests, choosing treatment options that may not be indicated or are less evidence-based • Erosion of trust between doctor and patient • Undermining public trust in medical fraternity
Managing Co. I • Avoid situations that offer significant possibility of a conflict of interest arising – Determination of whethere is a tendency to undue influence by secondary interest should be made by independent, reasonable observers • Reaffirm primacy of patient’s interests and doctor’s fiduciary responsibility to patient • Disclose conflicts of interest • Official regulatory bodies – Rules and laws to regulate and even prohibit certain actions & situations – Singapore laws, SMC, IRB

The End. Thank you!!
 Doctor-patient relationship ethics
Doctor-patient relationship ethics Doctor-patient relationship ethics
Doctor-patient relationship ethics Paternalism in dentistry
Paternalism in dentistry Doctor doctor google drive
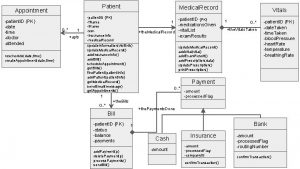
Doctor doctor google drive Uml vs erd
Uml vs erd Patient 2 patient
Patient 2 patient Phases of nurse-patient relationship ppt
Phases of nurse-patient relationship ppt Nurse-patient relationship phases
Nurse-patient relationship phases Phases of nurse patient relationship
Phases of nurse patient relationship Phases of nurse patient relationship
Phases of nurse patient relationship Relationship to patient 書き方
Relationship to patient 書き方 Safe space
Safe space Patient provider relationship
Patient provider relationship Chapter 8 communication and the nurse patient relationship
Chapter 8 communication and the nurse patient relationship A company's resources and capabilities represent
A company's resources and capabilities represent Marketing creating and capturing customer value
Marketing creating and capturing customer value Core concepts of management
Core concepts of management The core concepts of marketing
The core concepts of marketing Core database concepts
Core database concepts Core concepts
Core concepts Core concepts of accounting information systems
Core concepts of accounting information systems Payroll conference 2014
Payroll conference 2014 The brittle, rocky outer layer of earth
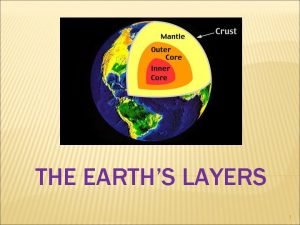
The brittle, rocky outer layer of earth Earth mantle definition
Earth mantle definition Layers of earth from most dense to least dense
Layers of earth from most dense to least dense Core rigidity
Core rigidity Customer relationship mangement
Customer relationship mangement