Improving the patient journey identifying and implementing interventions
- Slides: 1
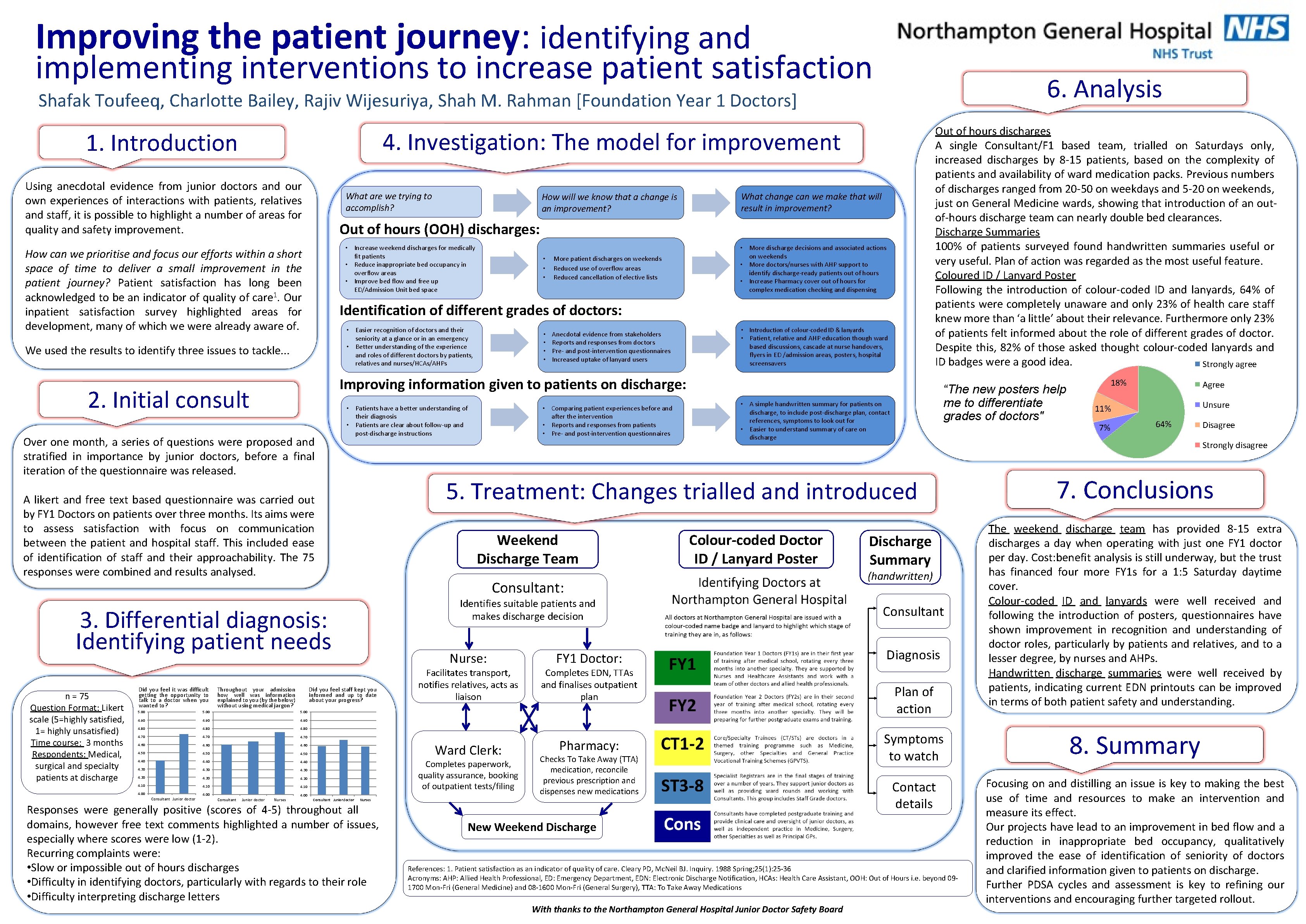
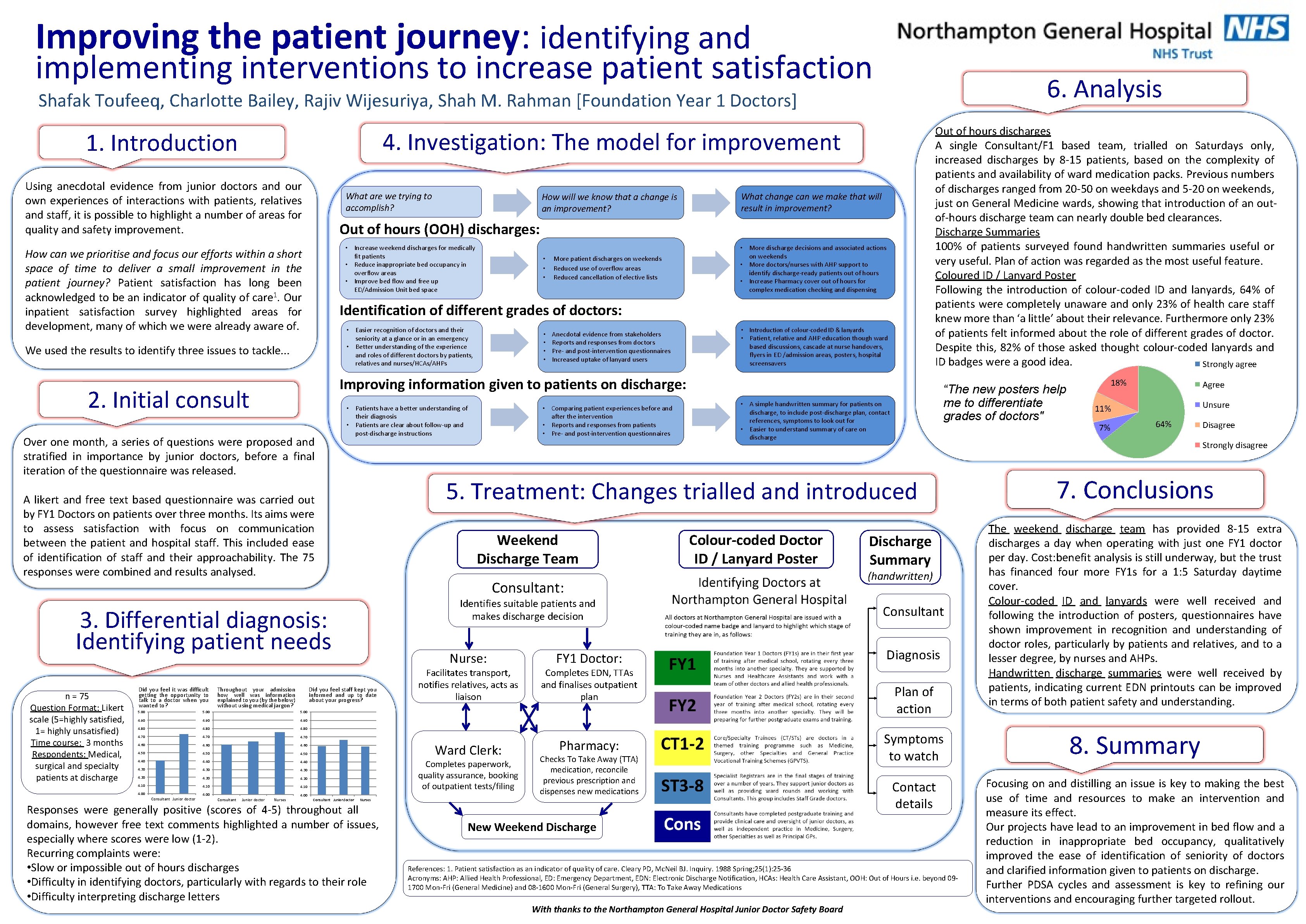
Improving the patient journey: identifying and implementing interventions to increase patient satisfaction 6. Analysis Shafak Toufeeq, Charlotte Bailey, Rajiv Wijesuriya, Shah M. Rahman [Foundation Year 1 Doctors] 4. Investigation: The model for improvement 1. Introduction Using anecdotal evidence from junior doctors and our own experiences of interactions with patients, relatives and staff, it is possible to highlight a number of areas for quality and safety improvement. • Increase weekend discharges for medically fit patients • Reduce inappropriate bed occupancy in overflow areas • Improve bed flow and free up ED/Admission Unit bed space • • • Patients have a better understanding of their diagnosis • Patients are clear about follow-up and post-discharge instructions Anecdotal evidence from stakeholders Reports and responses from doctors Pre- and post-intervention questionnaires Increased uptake of lanyard users • Introduction of colour-coded ID & lanyards • Patient, relative and AHP education though ward based discussions, cascade at nurse handovers, flyers in ED /admission areas, posters, hospital screensavers Throughout your admission how well was information explained to you (by the below) without using medical jargon? Weekend Discharge Team 5. 00 4. 90 4. 80 4. 70 4. 60 4. 50 4. 40 4. 30 4. 20 4. 10 4. 00 Nurses Colour-coded Doctor ID / Lanyard Poster Identifies suitable patients and makes discharge decision Nurse: Facilitates transport, notifies relatives, acts as liaison Ward Clerk: Completes paperwork, quality assurance, booking of outpatient tests/filing 4. 00 Consultant Junior doctor • A simple handwritten summary for patients on discharge, to include post-discharge plan, contact references, symptoms to look out for • Easier to understand summary of care on discharge Consultant: Did you feel staff kept you informed and up to date about your progress? 5. 00 • Comparing patient experiences before and after the intervention • Reports and responses from patients • Pre- and post-intervention questionnaires “The new posters help me to differentiate grades of doctors" FY 1 Doctor: Completes EDN, TTAs and finalises outpatient plan Pharmacy: Checks To Take Away (TTA) medication, reconcile previous prescription and dispenses new medications Nurses Responses were generally positive (scores of 4 -5) throughout all domains, however free text comments highlighted a number of issues, especially where scores were low (1 -2). Recurring complaints were: • Slow or impossible out of hours discharges • Difficulty in identifying doctors, particularly with regards to their role • Difficulty interpreting discharge letters Discharge Summary (handwritten) Consultant Diagnosis Plan of action Agree Unsure 11% 7% 64% Disagree 7. Conclusions The weekend discharge team has provided 8 -15 extra discharges a day when operating with just one FY 1 doctor per day. Cost: benefit analysis is still underway, but the trust has financed four more FY 1 s for a 1: 5 Saturday daytime cover. Colour-coded ID and lanyards were well received and following the introduction of posters, questionnaires have shown improvement in recognition and understanding of doctor roles, particularly by patients and relatives, and to a lesser degree, by nurses and AHPs. Handwritten discharge summaries were well received by patients, indicating current EDN printouts can be improved in terms of both patient safety and understanding. Symptoms to watch 8. Summary Contact details Focusing on and distilling an issue is key to making the best use of time and resources to make an intervention and measure its effect. Our projects have lead to an improvement in bed flow and a reduction in inappropriate bed occupancy, qualitatively improved the ease of identification of seniority of doctors and clarified information given to patients on discharge. Further PDSA cycles and assessment is key to refining our interventions and encouraging further targeted rollout. New Weekend Discharge References: 1. Patient satisfaction as an indicator of quality of care. Cleary PD, Mc. Neil BJ. Inquiry. 1988 Spring; 25(1): 25 -36 Acronyms: AHP: Allied Health Professional, ED: Emergency Department, EDN: Electronic Discharge Notification, HCAs: Health Care Assistant, OOH: Out of Hours i. e. beyond 091700 Mon-Fri (General Medicine) and 08 -1600 Mon-Fri (General Surgery), TTA: To Take Away Medications With thanks to the Northampton General Hospital Junior Doctor Safety Board 18% Strongly disagree 5. Treatment: Changes trialled and introduced 3. Differential diagnosis: Identifying patient needs Junior doctor More patient discharges on weekends Reduced use of overflow areas Reduced cancellation of elective lists • More discharge decisions and associated actions on weekends • More doctors/nurses with AHP support to identify discharge-ready patients out of hours • Increase Pharmacy cover out of hours for complex medication checking and dispensing Improving information given to patients on discharge: A likert and free text based questionnaire was carried out by FY 1 Doctors on patients over three months. Its aims were to assess satisfaction with focus on communication between the patient and hospital staff. This included ease of identification of staff and their approachability. The 75 responses were combined and results analysed. Consultant • • Easier recognition of doctors and their seniority at a glance or in an emergency • Better understanding of the experience and roles of different doctors by patients, relatives and nurses/HCAs/AHPs Over one month, a series of questions were proposed and stratified in importance by junior doctors, before a final iteration of the questionnaire was released. Consultant Junior doctor What change can we make that will result in improvement? Identification of different grades of doctors: 2. Initial consult 4. 00 How will we know a change is anthat a change is animprovement? Out of hours (OOH) discharges: We used the results to identify three issues to tackle. . . n = 75 Question Format: Likert scale (5=highly satisfied, 1= highly unsatisfied) Time course: 3 months Respondents: Medical, surgical and specialty patients at discharge How will we know that What are we trying to accomplish? How can we prioritise and focus our efforts within a short space of time to deliver a small improvement in the patient journey? Patient satisfaction has long been acknowledged to be an indicator of quality of care 1. Our inpatient satisfaction survey highlighted areas for development, many of which we were already aware of. Did you feel it was difficult getting the opportunity to talk to a doctor when you wanted to? Out of hours discharges A single Consultant/F 1 based team, trialled on Saturdays only, increased discharges by 8 -15 patients, based on the complexity of patients and availability of ward medication packs. Previous numbers of discharges ranged from 20 -50 on weekdays and 5 -20 on weekends, just on General Medicine wards, showing that introduction of an outof-hours discharge team can nearly double bed clearances. Discharge Summaries 100% of patients surveyed found handwritten summaries useful or very useful. Plan of action was regarded as the most useful feature. Coloured ID / Lanyard Poster Following the introduction of colour-coded ID and lanyards, 64% of patients were completely unaware and only 23% of health care staff knew more than ‘a little’ about their relevance. Furthermore only 23% of patients felt informed about the role of different grades of doctor. Despite this, 82% of those asked thought colour-coded lanyards and ID badges were a good idea. Strongly agree