STROKE ITS NO JOKE NURSING ASSESSMENT AND CARE


- Slides: 58
STROKE…. IT’S NO JOKE NURSING ASSESSMENT AND CARE Kate Holmes 4/4/2012 MSN 621
Logistics of the Tutorial Underlined, colored words indicate that the definition is available. To view these definitions in context, hover the link. Portions of the tutorial are interactive and will require the learner to click on the appropriate response which are colored choices located on the right side of the screen. Pay attention to the bolded information throughout the case study to help direct the correct response to these interactive sections. Links are available to review the case study.
Statistics Stroke ranks 3 rd among all causes of death; behind heart disease and cancer. The American Academy of Nurse Practitioners reports annually that 900, 000 patients are discharged from the hospital with a stroke diagnosis. Experts estimate that up to 30% of stroke patients will deteriorate within the first 24 hours. American Academy of Nurse Practitioners, 2011 Wild Iris Medical Education, 2010
Objectives Define a generalized stroke and an ischemic stroke. Review common stroke risk factors. Learn the pathophysiology of an ischemic stroke. Understand the use of the National Institute of Health (NIH) stroke scale. Acknowledge the possible Clinical Nurse Specialist (CNS) role with an acute stroke patient.
Stroke Review What is a stroke? A stroke is a disturbance in blood flow to the brain causing neurological deficits. Recently titled a “brain attack. ” Microsoft Clip Art, 2010
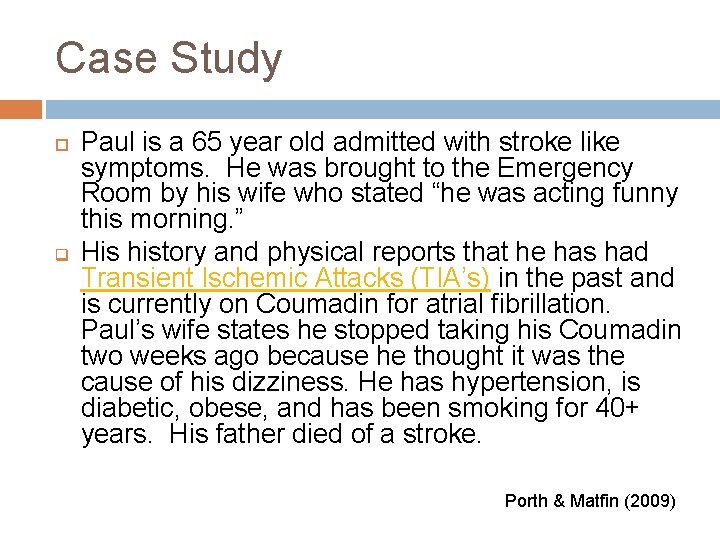
Case Study q Paul is a 65 year old admitted with stroke like symptoms. He was brought to the Emergency Room by his wife who stated “he was acting funny this morning. ” His history and physical reports that he has had Transient Ischemic Attacks (TIA’s) in the past and is currently on Coumadin for atrial fibrillation. Paul’s wife states he stopped taking his Coumadin two weeks ago because he thought it was the cause of his dizziness. He has hypertension, is diabetic, obese, and has been smoking for 40+ years. His father died of a stroke. Porth & Matfin (2009)
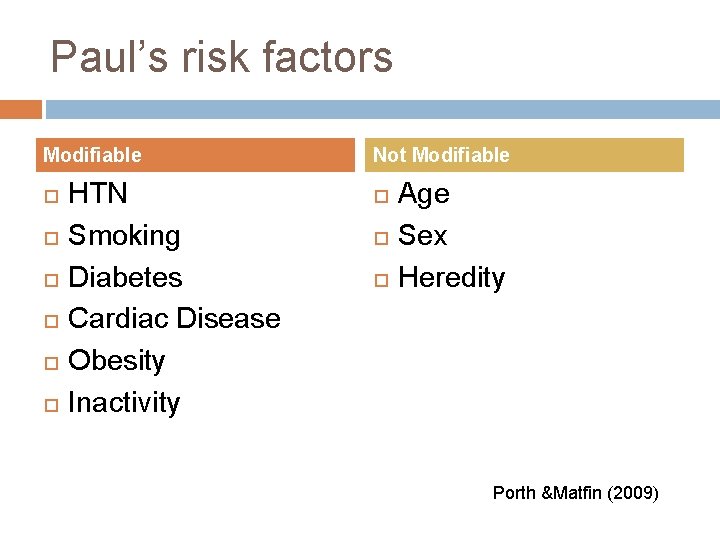
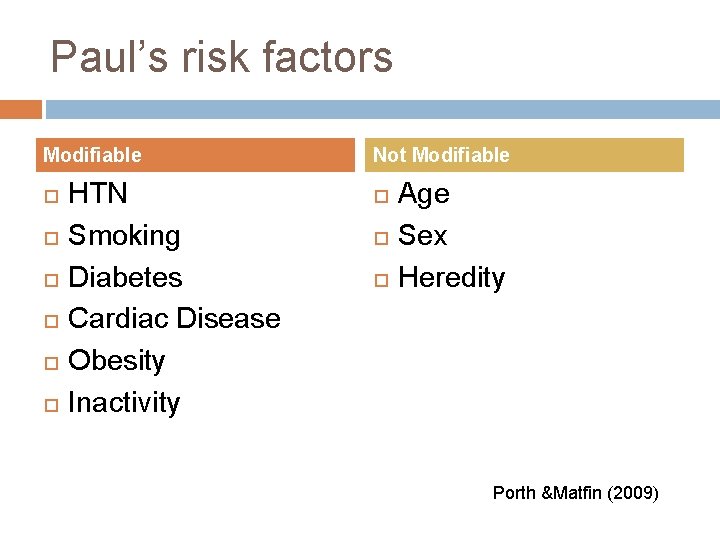
Paul’s risk factors Modifiable HTN Smoking Diabetes Cardiac Disease Obesity Inactivity Not Modifiable Age Sex Heredity Porth &Matfin (2009)
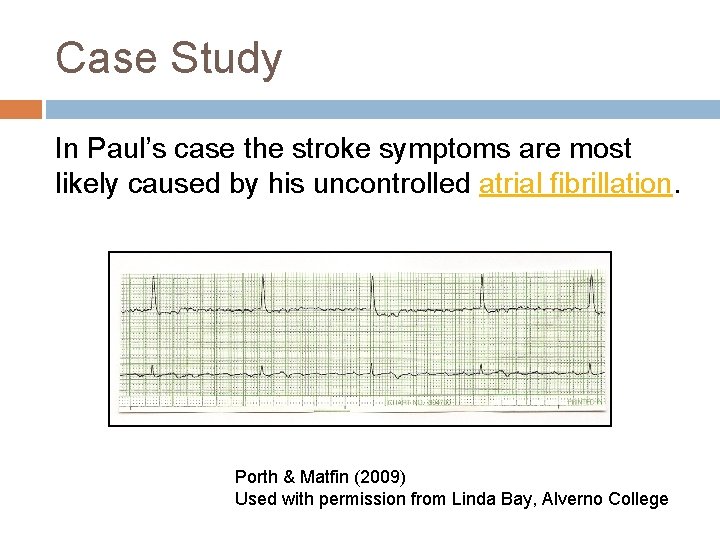
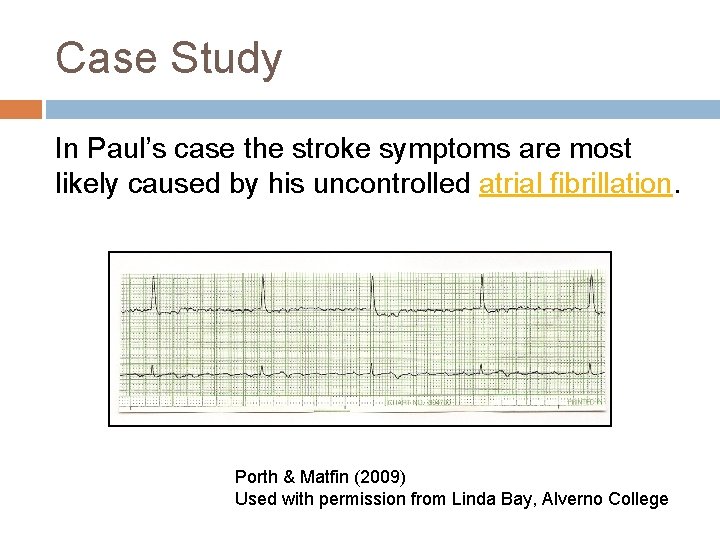
Case Study In Paul’s case the stroke symptoms are most likely caused by his uncontrolled atrial fibrillation. Porth & Matfin (2009) Used with permission from Linda Bay, Alverno College
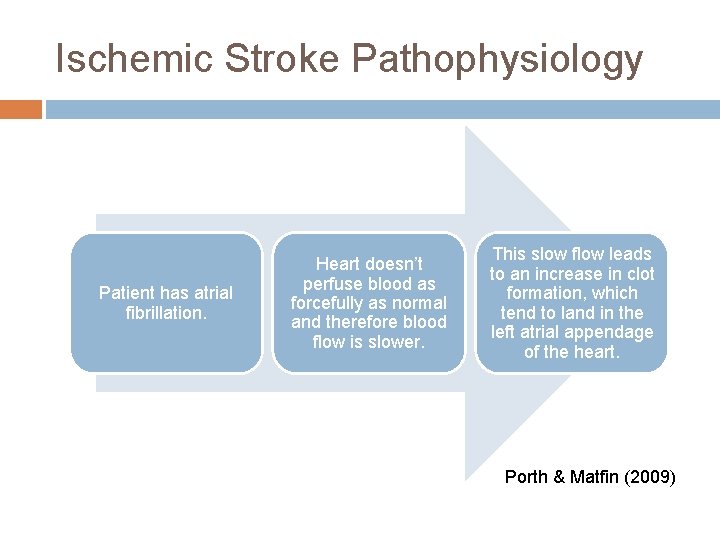
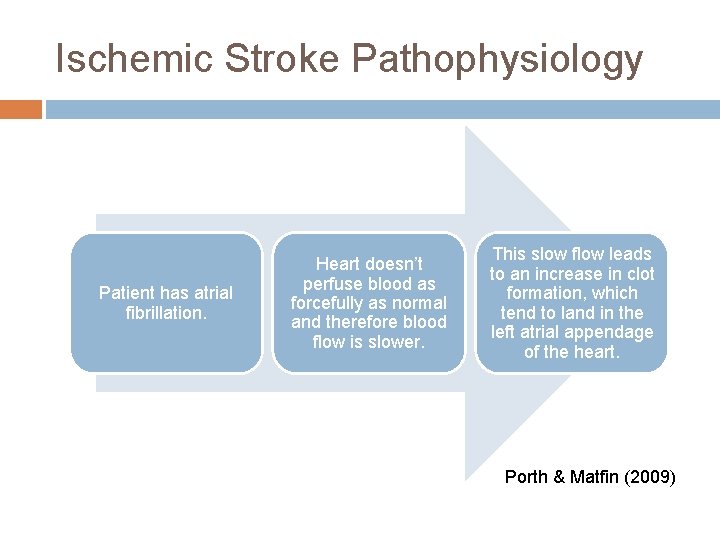
Ischemic Stroke Pathophysiology Patient has atrial fibrillation. Heart doesn’t perfuse blood as forcefully as normal and therefore blood flow is slower. This slow flow leads to an increase in clot formation, which tend to land in the left atrial appendage of the heart. Porth & Matfin (2009)
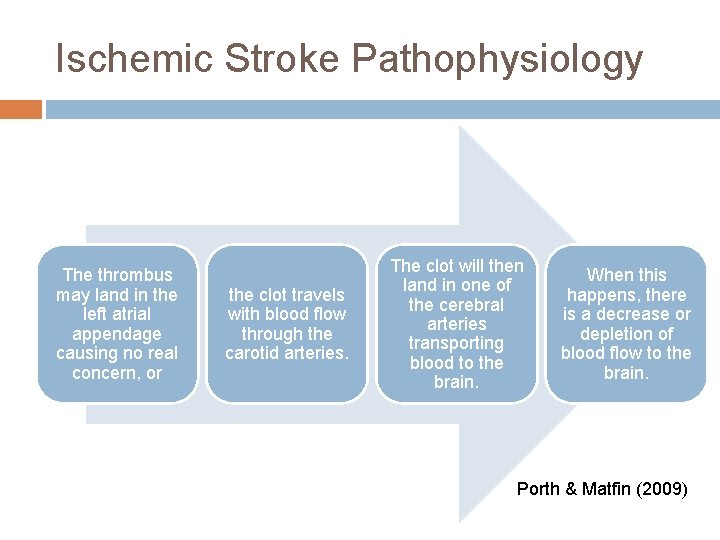
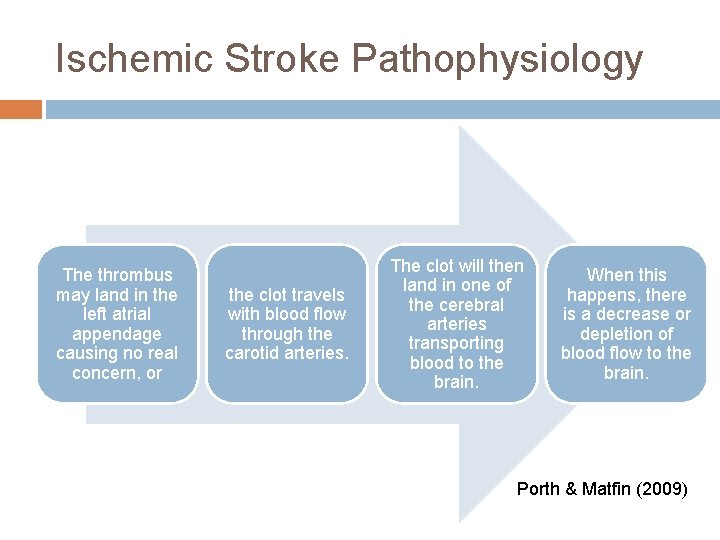
Ischemic Stroke Pathophysiology The thrombus may land in the left atrial appendage causing no real concern, or the clot travels with blood flow through the carotid arteries. The clot will then land in one of the cerebral arteries transporting blood to the brain. When this happens, there is a decrease or depletion of blood flow to the brain. Porth & Matfin (2009)
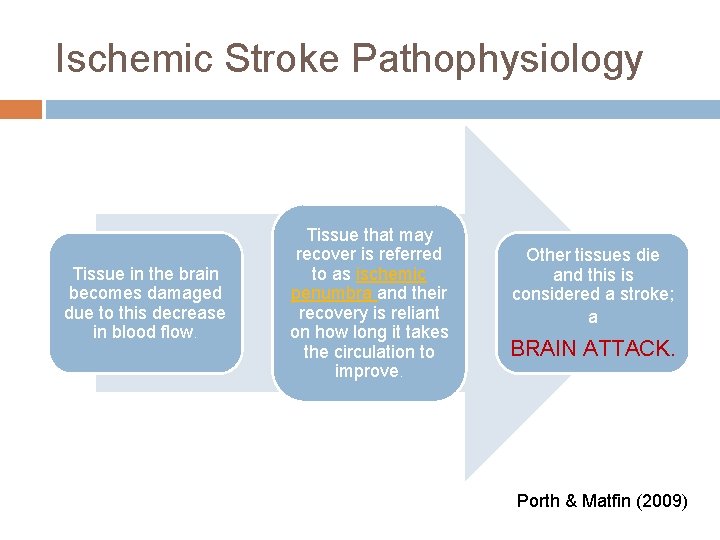
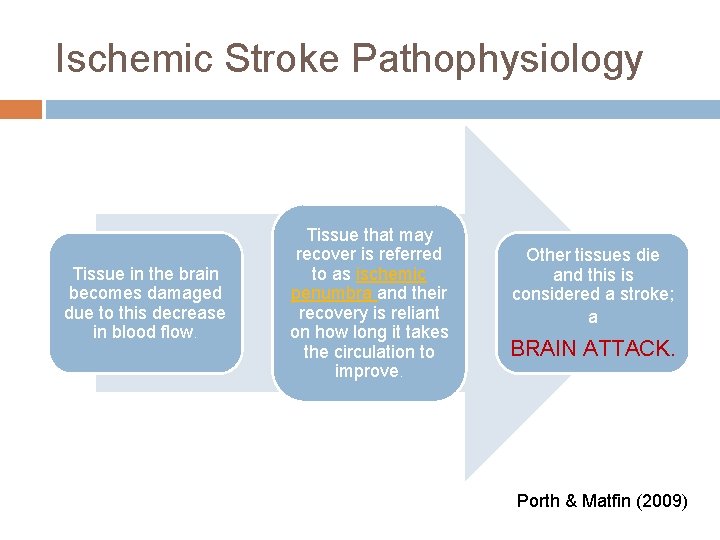
Ischemic Stroke Pathophysiology Tissue in the brain becomes damaged due to this decrease in blood flow. Tissue that may recover is referred to as ischemic penumbra and their recovery is reliant on how long it takes the circulation to improve. Other tissues die and this is considered a stroke; a BRAIN ATTACK. Porth & Matfin (2009)
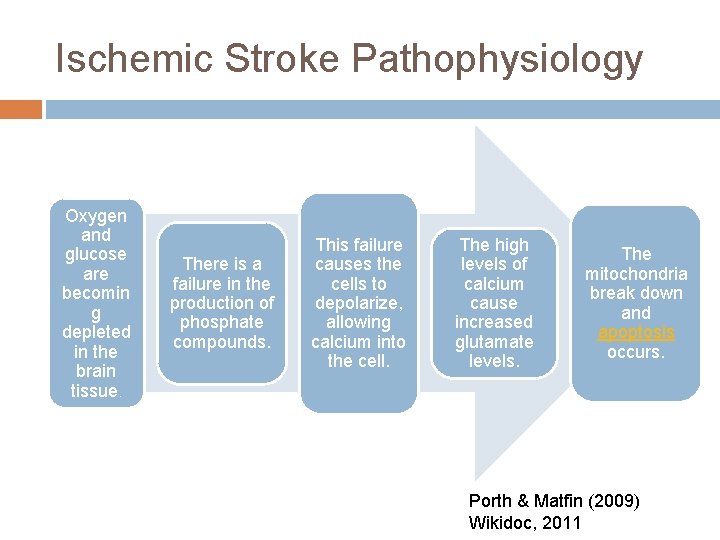
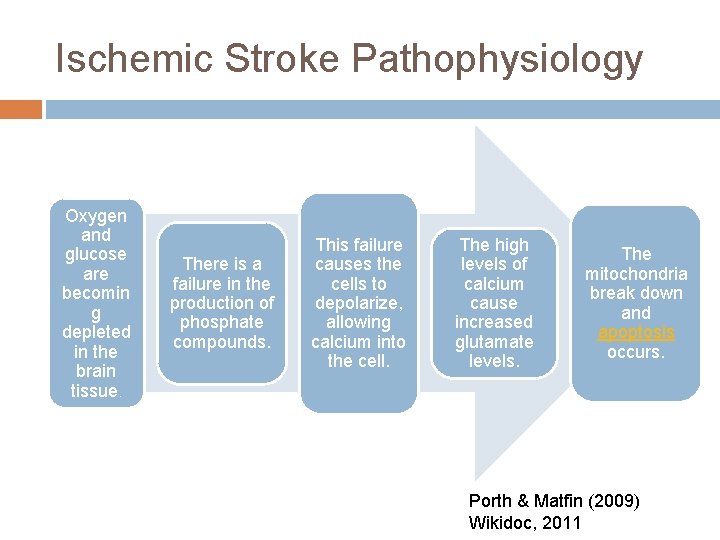
Ischemic Stroke Pathophysiology Oxygen and glucose are becomin g depleted in the brain tissue. There is a failure in the production of phosphate compounds. This failure causes the cells to depolarize, allowing calcium into the cell. The high levels of calcium cause increased glutamate levels. The mitochondria break down and apoptosis occurs. Porth & Matfin (2009) Wikidoc, 2011
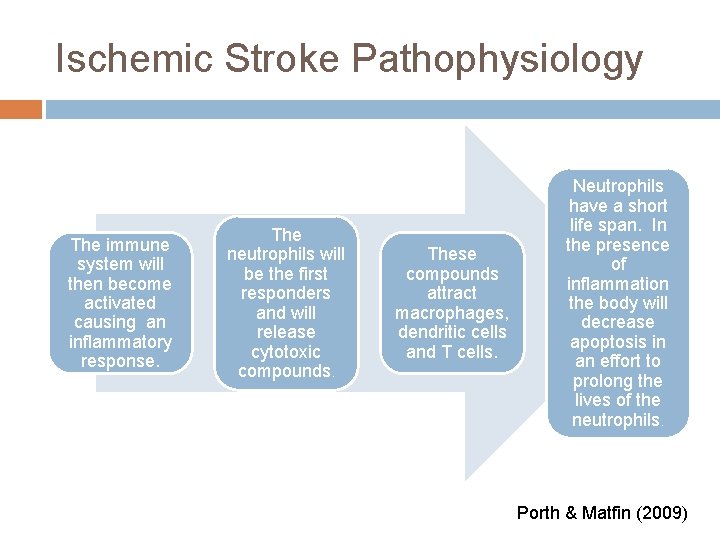
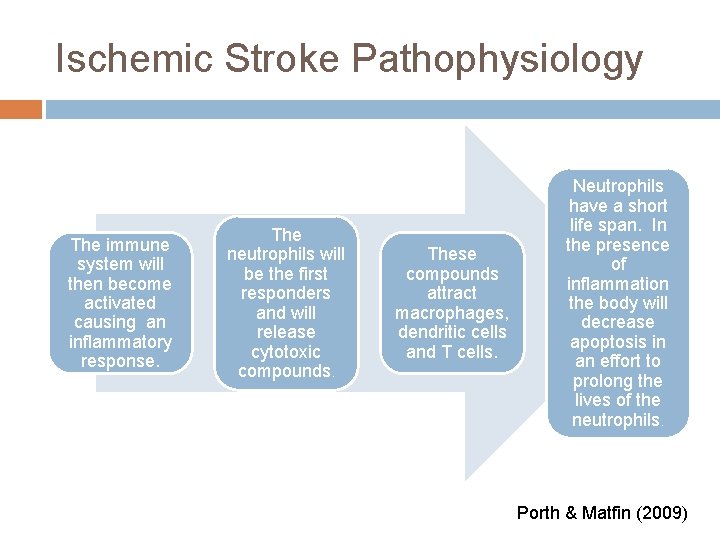
Ischemic Stroke Pathophysiology The immune system will then become activated causing an inflammatory response. The neutrophils will be the first responders and will release cytotoxic compounds. These compounds attract macrophages, dendritic cells and T cells. Neutrophils have a short life span. In the presence of inflammation the body will decrease apoptosis in an effort to prolong the lives of the neutrophils. Porth & Matfin (2009)
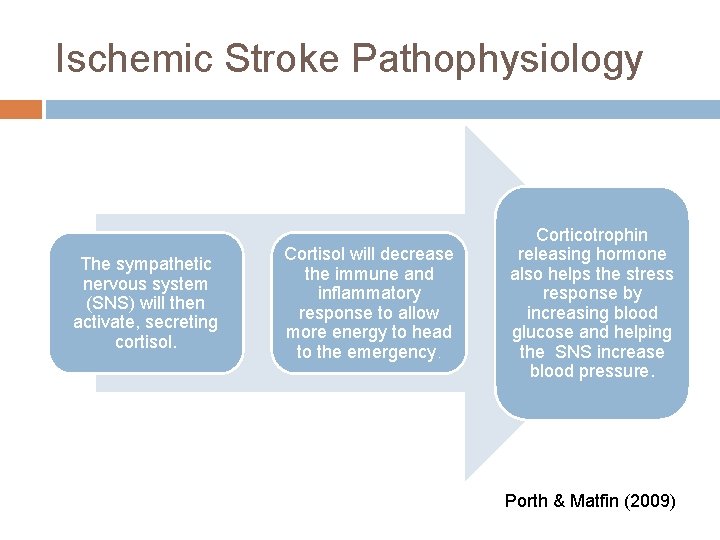
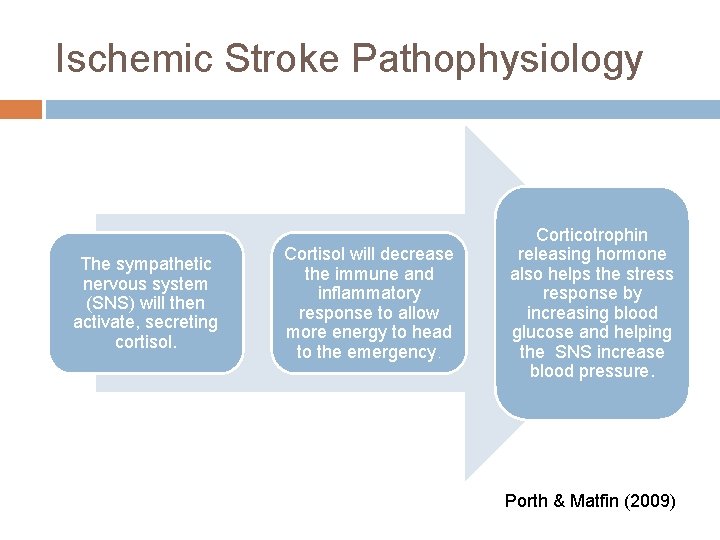
Ischemic Stroke Pathophysiology The sympathetic nervous system (SNS) will then activate, secreting cortisol. Cortisol will decrease the immune and inflammatory response to allow more energy to head to the emergency. Corticotrophin releasing hormone also helps the stress response by increasing blood glucose and helping the SNS increase blood pressure. Porth & Matfin (2009)
Ischemic Stroke Pathophysiology The longer the blood flow is absent or decreased, the more brain tissues die. This is why TIME IS BRAIN.
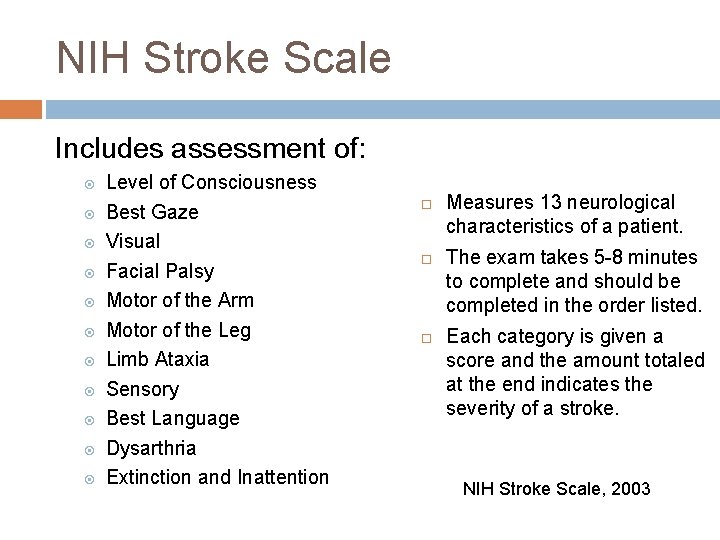
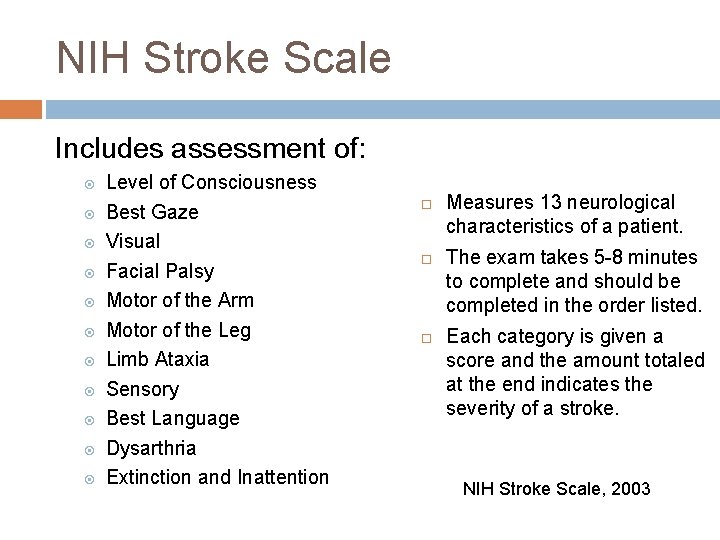
NIH Stroke Scale Includes assessment of: Level of Consciousness Best Gaze Visual Facial Palsy Motor of the Arm Motor of the Leg Limb Ataxia Sensory Best Language Dysarthria Extinction and Inattention Measures 13 neurological characteristics of a patient. The exam takes 5 -8 minutes to complete and should be completed in the order listed. Each category is given a score and the amount totaled at the end indicates the severity of a stroke. NIH Stroke Scale, 2003
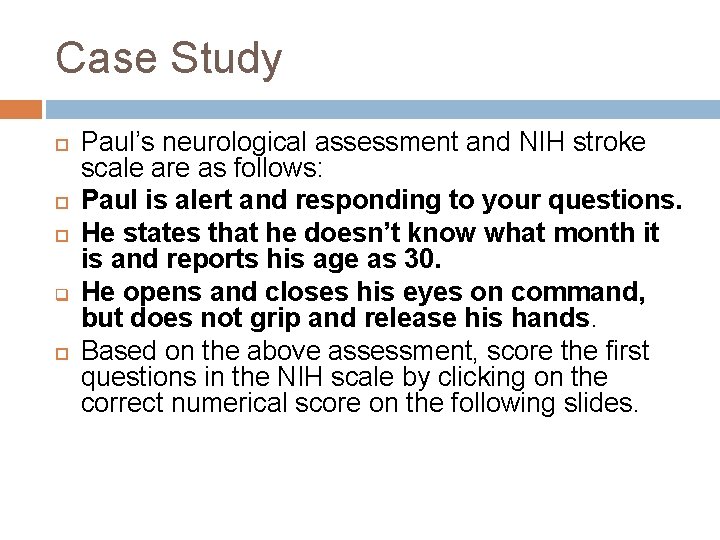
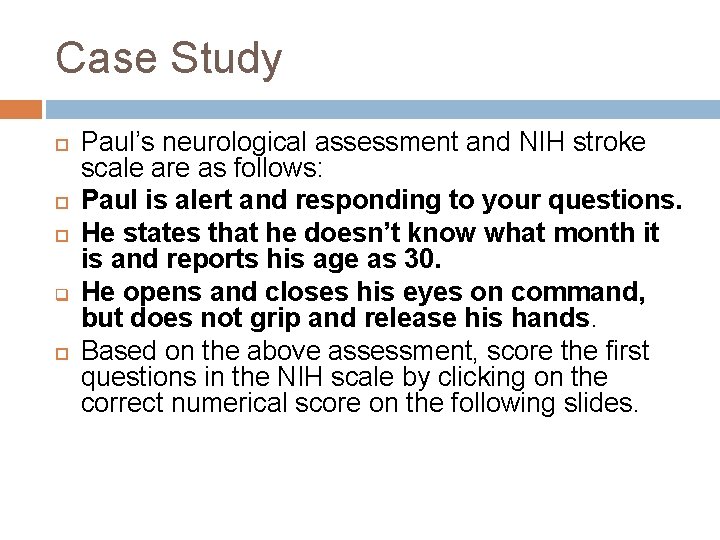
Case Study q Paul’s neurological assessment and NIH stroke scale are as follows: Paul is alert and responding to your questions. He states that he doesn’t know what month it is and reports his age as 30. He opens and closes his eyes on command, but does not grip and release his hands. Based on the above assessment, score the first questions in the NIH scale by clicking on the correct numerical score on the following slides.
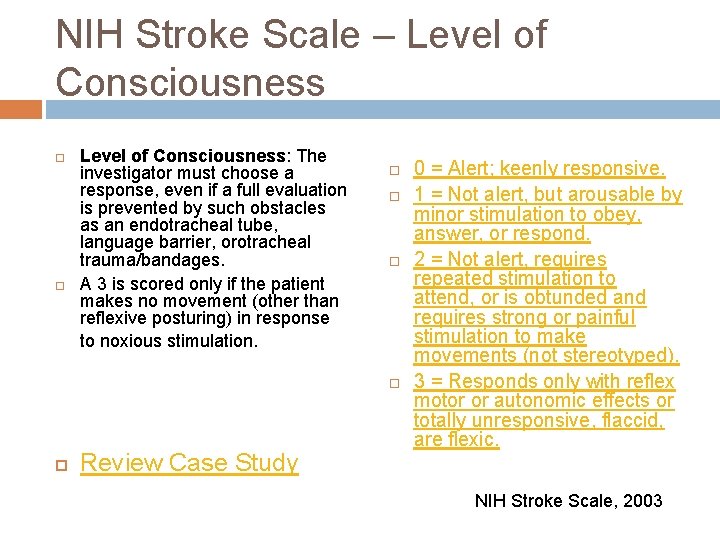
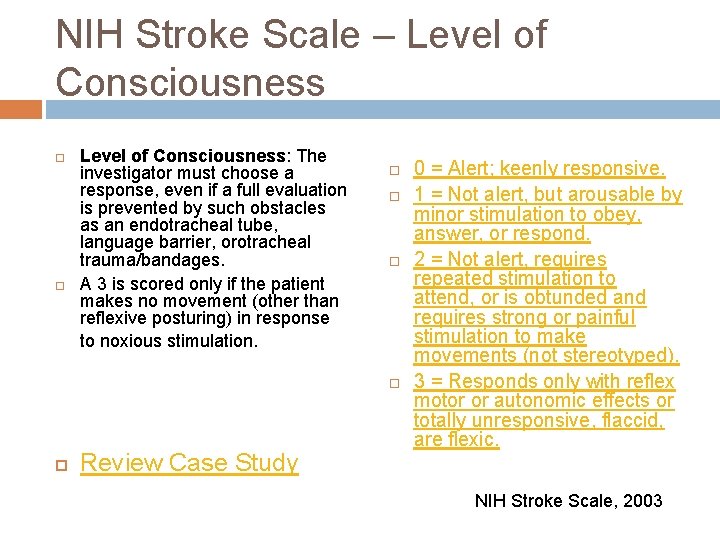
NIH Stroke Scale – Level of Consciousness: The investigator must choose a response, even if a full evaluation is prevented by such obstacles as an endotracheal tube, language barrier, orotracheal trauma/bandages. A 3 is scored only if the patient makes no movement (other than reflexive posturing) in response to noxious stimulation. Review Case Study 0 = Alert; keenly responsive. 1 = Not alert, but arousable by minor stimulation to obey, answer, or respond. 2 = Not alert, requires repeated stimulation to attend, or is obtunded and requires strong or painful stimulation to make movements (not stereotyped). 3 = Responds only with reflex motor or autonomic effects or totally unresponsive, flaccid, are flexic. NIH Stroke Scale, 2003
That’s right. His score is 0, he is alert and responding. Click here to continue.
Try again, Paul is alert and responding. Click here to try again.
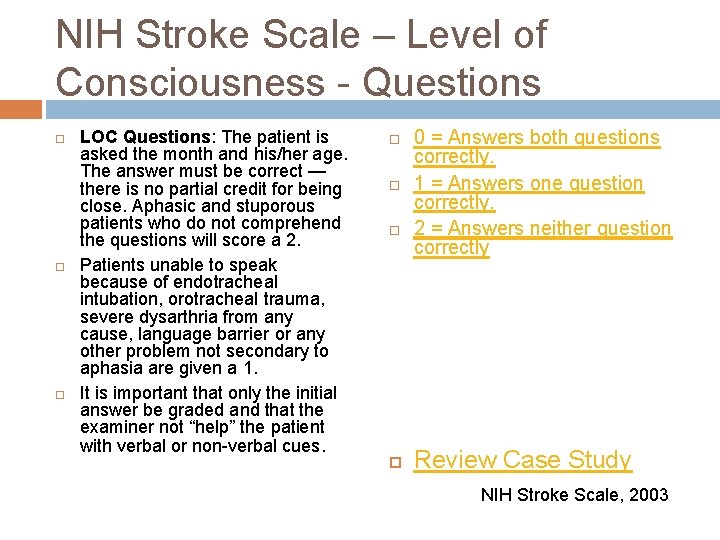
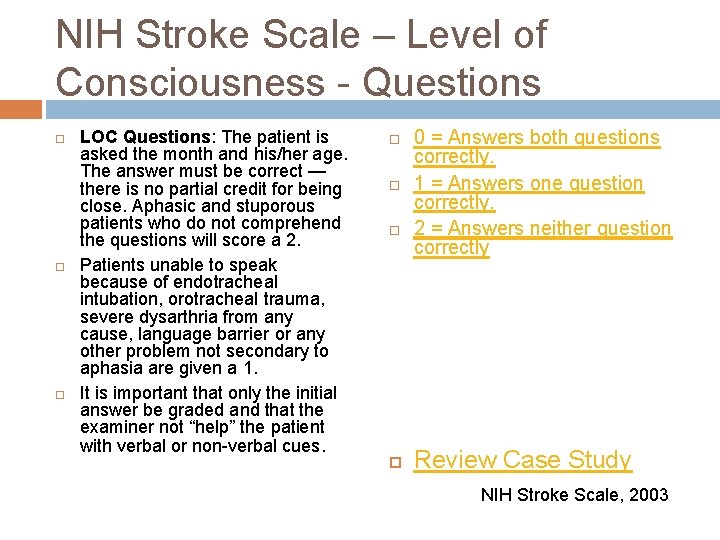
NIH Stroke Scale – Level of Consciousness - Questions LOC Questions: The patient is asked the month and his/her age. The answer must be correct — there is no partial credit for being close. Aphasic and stuporous patients who do not comprehend the questions will score a 2. Patients unable to speak because of endotracheal intubation, orotracheal trauma, severe dysarthria from any cause, language barrier or any other problem not secondary to aphasia are given a 1. It is important that only the initial answer be graded and that the examiner not “help” the patient with verbal or non-verbal cues. 0 = Answers both questions correctly. 1 = Answers one question correctly. 2 = Answers neither question correctly Review Case Study NIH Stroke Scale, 2003
Great Job, the answer is 2 because Paul couldn’t state his correct age or the month. Click here to continue.
Please try again, he was incorrect with his age and the month. Click here to try again.
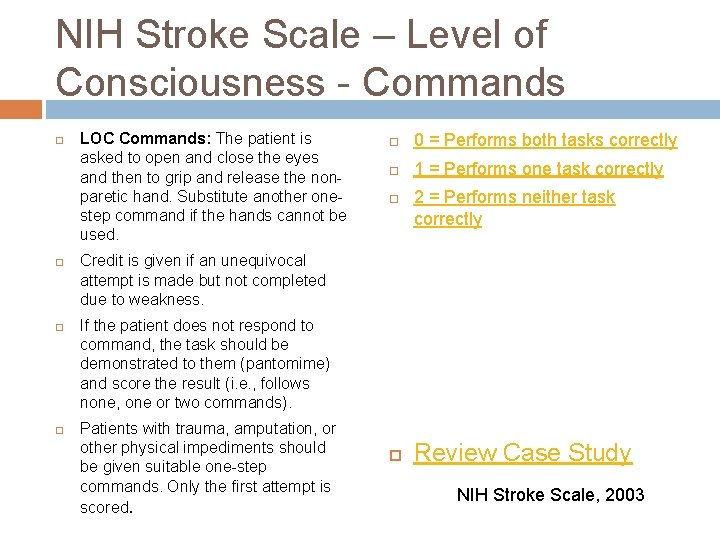
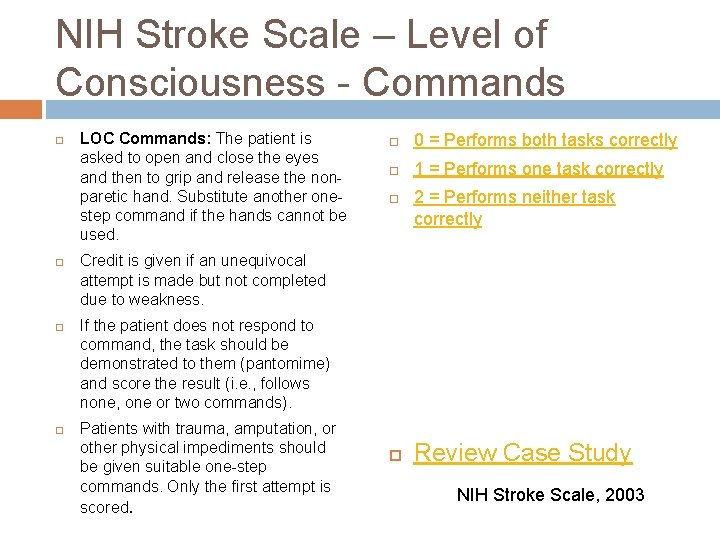
NIH Stroke Scale – Level of Consciousness - Commands LOC Commands: The patient is asked to open and close the eyes and then to grip and release the nonparetic hand. Substitute another onestep command if the hands cannot be used. 0 = Performs both tasks correctly 1 = Performs one task correctly 2 = Performs neither task correctly Credit is given if an unequivocal attempt is made but not completed due to weakness. If the patient does not respond to command, the task should be demonstrated to them (pantomime) and score the result (i. e. , follows none, one or two commands). Patients with trauma, amputation, or other physical impediments should be given suitable one-step commands. Only the first attempt is scored. Review Case Study NIH Stroke Scale, 2003

That’s correct. Good work. Click here to continue.
That’s incorrect. Paul opened his eyes, but did complete hand grasps on command. He performed 1 task correctly. Click here to try again.
Case Study Paul’s pupils are equal with a sluggish reaction. His gaze follows appropriately. Paul is unable to follow the visual acuity exam with both eyes. Paul raises his eyebrows and closes his eyes without difficulty. He follows the command to smile, but a profound right sided facial droop is noted. Based on the above assessment pieces, review the next set of slides to see how Paul would be scored.
NIH Stroke Scale – Best Gaze Based on the above assessment findings, Paul would score a 0 on the “best gaze” portion of the NIH stroke scale because his gaze follows appropriately. NIH Stroke Scale, 2003 Microsoft Clip Art, 2010
NIH Stroke Scale - Visual Paul was unable to follow the visual acuity exam with either eye and therefore his score for this section of the NIH stroke scale would be 2, indicating complete hemianopia. NIH Stroke Scale, 2003
NIH Stroke Scale – Facial Palsy Paul’s assessment indicates that he has some partial facial paralysis which would give him a score of 2 in this portion of the NIH stroke scale. At this point, Paul has a score of NIH Stroke Scale, 2003 Microsoft Clip Art, 2010
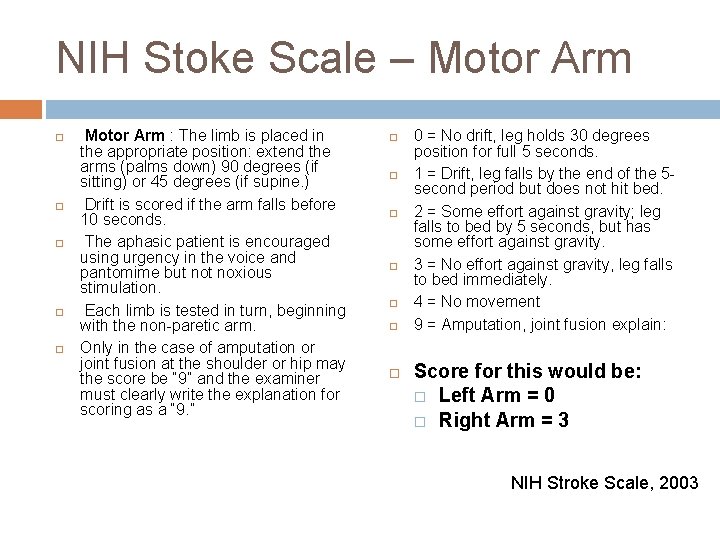
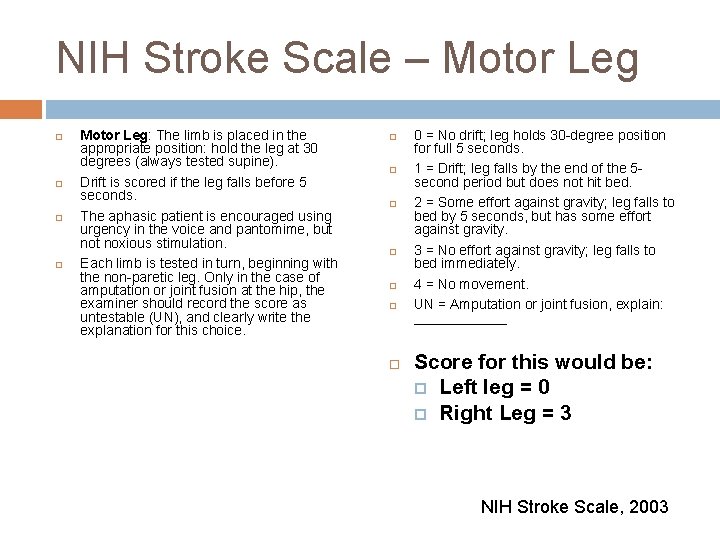
Case Study Paul’s arms are lifted to a 45 degree angle, his left arm maintains itself in that position, but his right arm immediately falls to the bed. His legs are also lifted and the same situation arises. He can maintain the lift in the left leg, but the right leg falls to the bed immediately. See the following two slides to see how Motor would be scored according the NIH Stroke Scale.
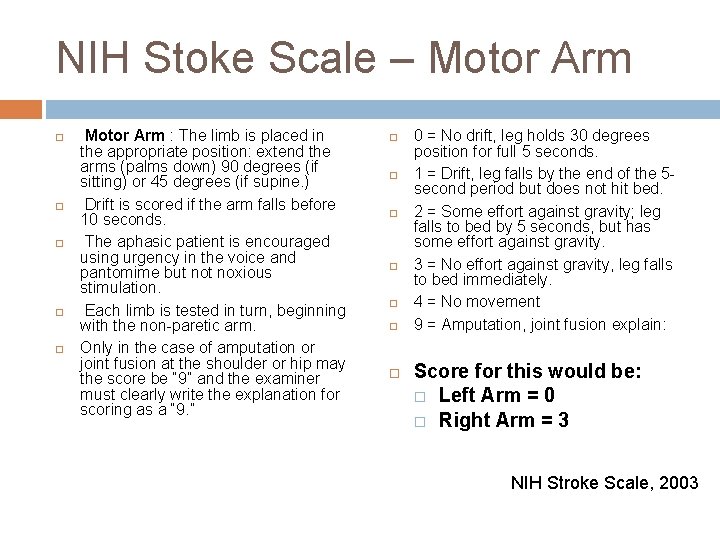
NIH Stoke Scale – Motor Arm Motor Arm : The limb is placed in the appropriate position: extend the arms (palms down) 90 degrees (if sitting) or 45 degrees (if supine. ) Drift is scored if the arm falls before 10 seconds. The aphasic patient is encouraged using urgency in the voice and pantomime but noxious stimulation. Each limb is tested in turn, beginning with the non-paretic arm. Only in the case of amputation or joint fusion at the shoulder or hip may the score be “ 9” and the examiner must clearly write the explanation for scoring as a “ 9. ” 0 = No drift, leg holds 30 degrees position for full 5 seconds. 1 = Drift, leg falls by the end of the 5 second period but does not hit bed. 2 = Some effort against gravity; leg falls to bed by 5 seconds, but has some effort against gravity. 3 = No effort against gravity, leg falls to bed immediately. 4 = No movement 9 = Amputation, joint fusion explain: Score for this would be: Left Arm = 0 Right Arm = 3 NIH Stroke Scale, 2003
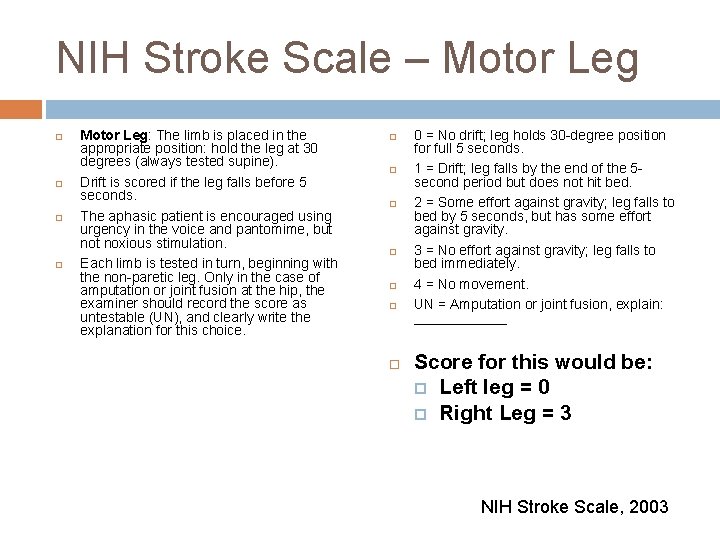
NIH Stroke Scale – Motor Leg Motor Leg: The limb is placed in the appropriate position: hold the leg at 30 degrees (always tested supine). Drift is scored if the leg falls before 5 seconds. The aphasic patient is encouraged using urgency in the voice and pantomime, but noxious stimulation. Each limb is tested in turn, beginning with the non-paretic leg. Only in the case of amputation or joint fusion at the hip, the examiner should record the score as untestable (UN), and clearly write the explanation for this choice. 0 = No drift; leg holds 30 -degree position for full 5 seconds. 1 = Drift; leg falls by the end of the 5 second period but does not hit bed. 2 = Some effort against gravity; leg falls to bed by 5 seconds, but has some effort against gravity. 3 = No effort against gravity; leg falls to bed immediately. 4 = No movement. UN = Amputation or joint fusion, explain: ______ Score for this would be: Left leg = 0 Right Leg = 3 NIH Stroke Scale, 2003
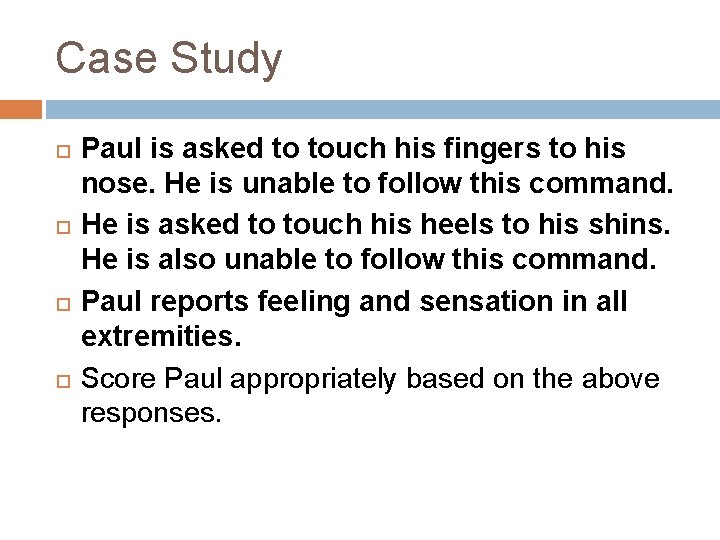
Case Study Paul is asked to touch his fingers to his nose. He is unable to follow this command. He is asked to touch his heels to his shins. He is also unable to follow this command. Paul reports feeling and sensation in all extremities. Score Paul appropriately based on the above responses.
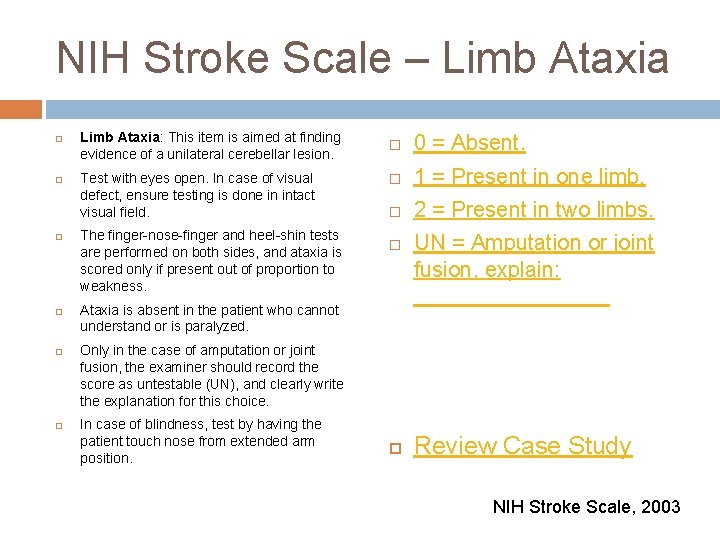
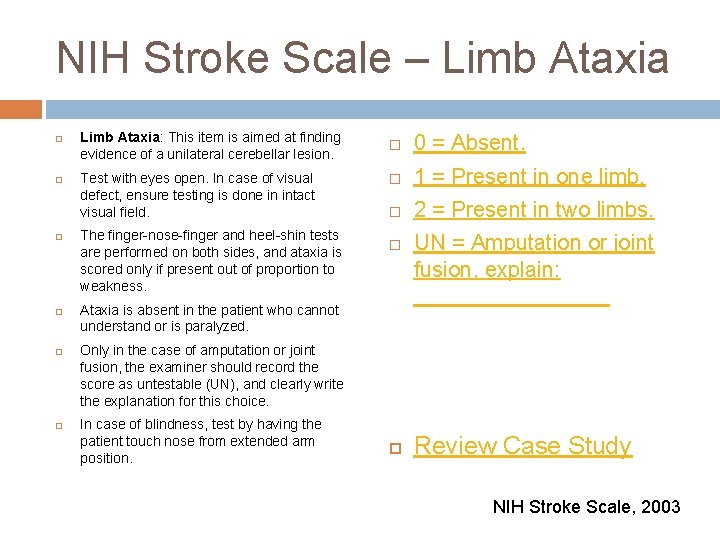
NIH Stroke Scale – Limb Ataxia Limb Ataxia: This item is aimed at finding evidence of a unilateral cerebellar lesion. Test with eyes open. In case of visual defect, ensure testing is done in intact visual field. The finger-nose-finger and heel-shin tests are performed on both sides, and ataxia is scored only if present out of proportion to weakness. 0 = Absent. 1 = Present in one limb. 2 = Present in two limbs. Ataxia is absent in the patient who cannot understand or is paralyzed. UN = Amputation or joint fusion, explain: ________ Only in the case of amputation or joint fusion, the examiner should record the score as untestable (UN), and clearly write the explanation for this choice. In case of blindness, test by having the patient touch nose from extended arm position. Review Case Study NIH Stroke Scale, 2003
Perfect Answer Click here to continue.
Try that one again. Paul was unable to do either exam. Click here to try again.
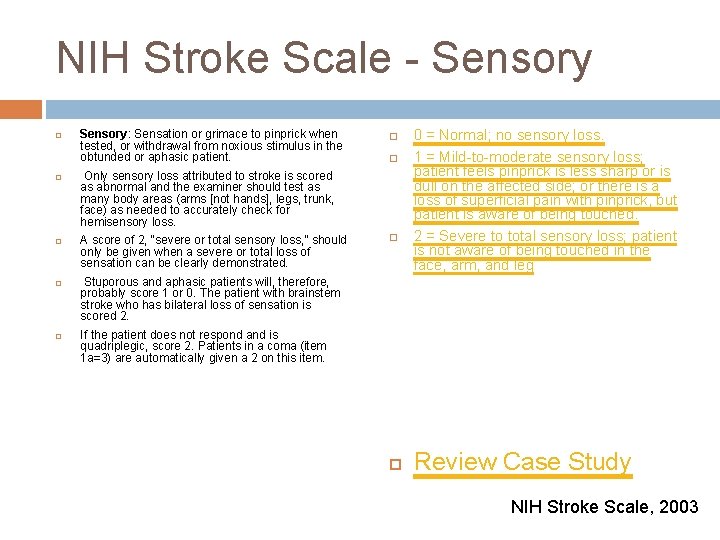
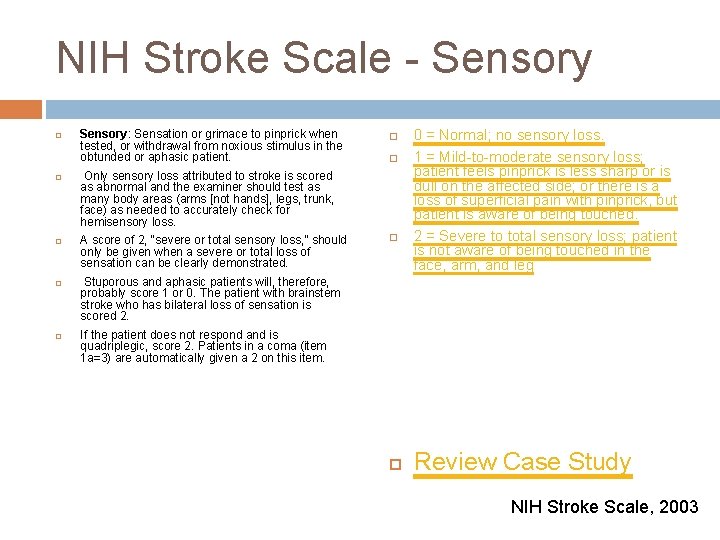
NIH Stroke Scale - Sensory Sensory: Sensation or grimace to pinprick when tested, or withdrawal from noxious stimulus in the obtunded or aphasic patient. Only sensory loss attributed to stroke is scored as abnormal and the examiner should test as many body areas (arms [not hands], legs, trunk, face) as needed to accurately check for hemisensory loss. A score of 2, “severe or total sensory loss, ” should only be given when a severe or total loss of sensation can be clearly demonstrated. 0 = Normal; no sensory loss. 1 = Mild-to-moderate sensory loss; patient feels pinprick is less sharp or is dull on the affected side; or there is a loss of superficial pain with pinprick, but patient is aware of being touched. 2 = Severe to total sensory loss; patient is not aware of being touched in the face, arm, and leg Stuporous and aphasic patients will, therefore, probably score 1 or 0. The patient with brainstem stroke who has bilateral loss of sensation is scored 2. If the patient does not respond and is quadriplegic, score 2. Patients in a coma (item 1 a=3) are automatically given a 2 on this item. Review Case Study NIH Stroke Scale, 2003
You’re an expert. Click here to continue.
That is the wrong score, Paul reported a feeling of sensation in all his extremities. Click here to try again.
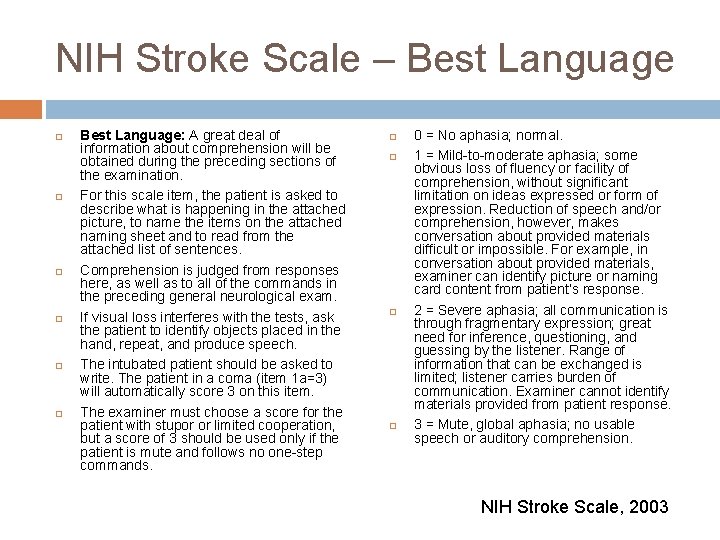
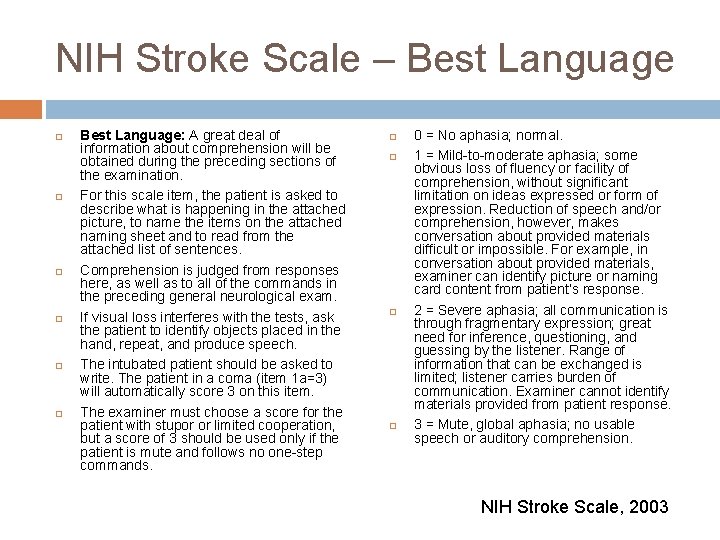
NIH Stroke Scale – Best Language Best Language: A great deal of information about comprehension will be obtained during the preceding sections of the examination. For this scale item, the patient is asked to describe what is happening in the attached picture, to name the items on the attached naming sheet and to read from the attached list of sentences. Comprehension is judged from responses here, as well as to all of the commands in the preceding general neurological exam. If visual loss interferes with the tests, ask the patient to identify objects placed in the hand, repeat, and produce speech. The intubated patient should be asked to write. The patient in a coma (item 1 a=3) will automatically score 3 on this item. The examiner must choose a score for the patient with stupor or limited cooperation, but a score of 3 should be used only if the patient is mute and follows no one-step commands. 0 = No aphasia; normal. 1 = Mild-to-moderate aphasia; some obvious loss of fluency or facility of comprehension, without significant limitation on ideas expressed or form of expression. Reduction of speech and/or comprehension, however, makes conversation about provided materials difficult or impossible. For example, in conversation about provided materials, examiner can identify picture or naming card content from patient’s response. 2 = Severe aphasia; all communication is through fragmentary expression; great need for inference, questioning, and guessing by the listener. Range of information that can be exchanged is limited; listener carries burden of communication. Examiner cannot identify materials provided from patient response. 3 = Mute, global aphasia; no usable speech or auditory comprehension. NIH Stroke Scale, 2003
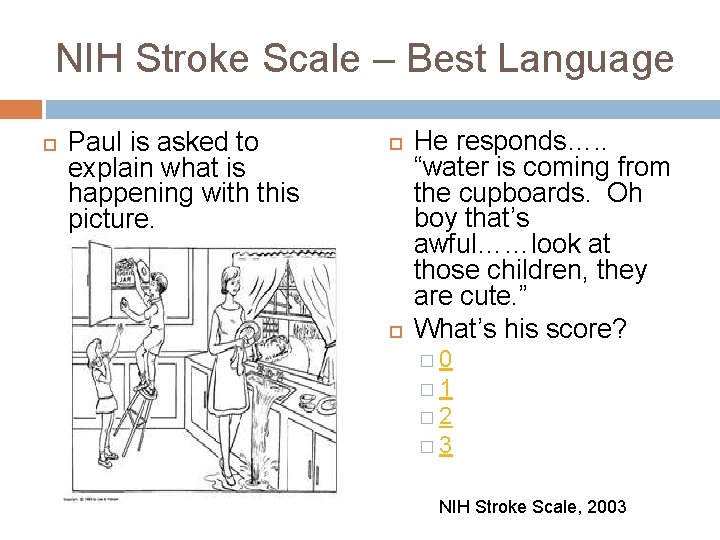
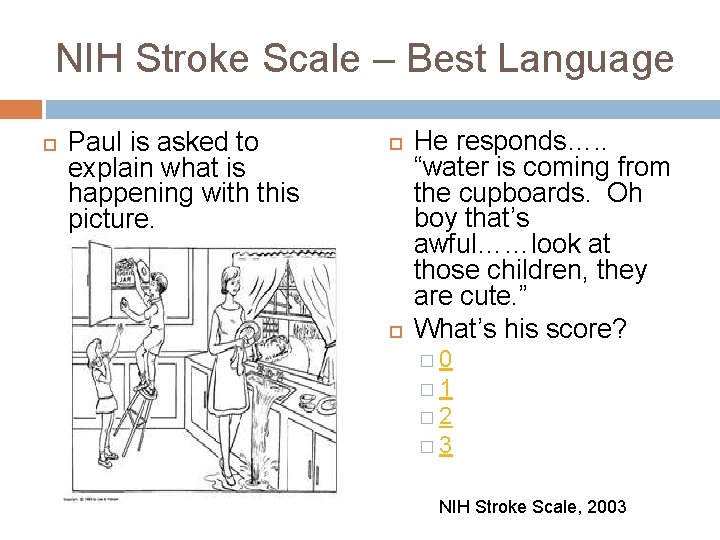
NIH Stroke Scale – Best Language Paul is asked to explain what is happening with this picture. He responds…. . “water is coming from the cupboards. Oh boy that’s awful……look at those children, they are cute. ” What’s his score? � 0 � 1 � 2 � 3 NIH Stroke Scale, 2003

Nice job!!!! Click here to continue.
Try again. Click here to try again.
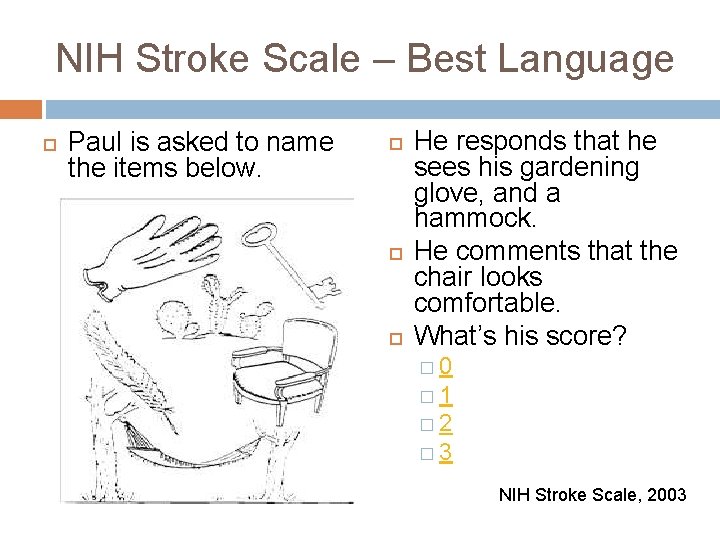
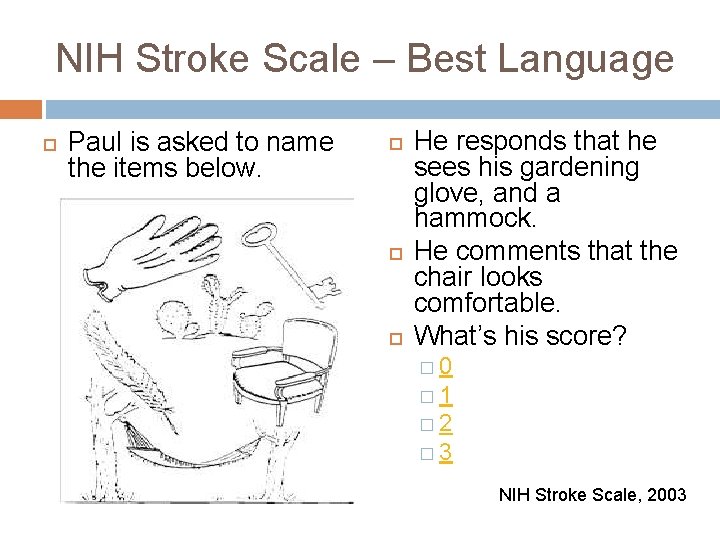
NIH Stroke Scale – Best Language Paul is asked to name the items below. He responds that he sees his gardening glove, and a hammock. He comments that the chair looks comfortable. What’s his score? � 0 � 1 � 2 � 3 NIH Stroke Scale, 2003
That’s right. Click here to continue.
Sorry, that’s incorrect. Click here to try again.
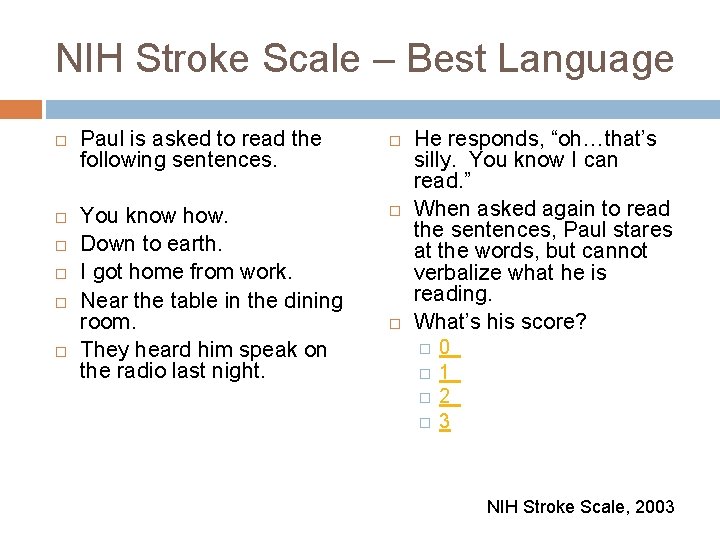
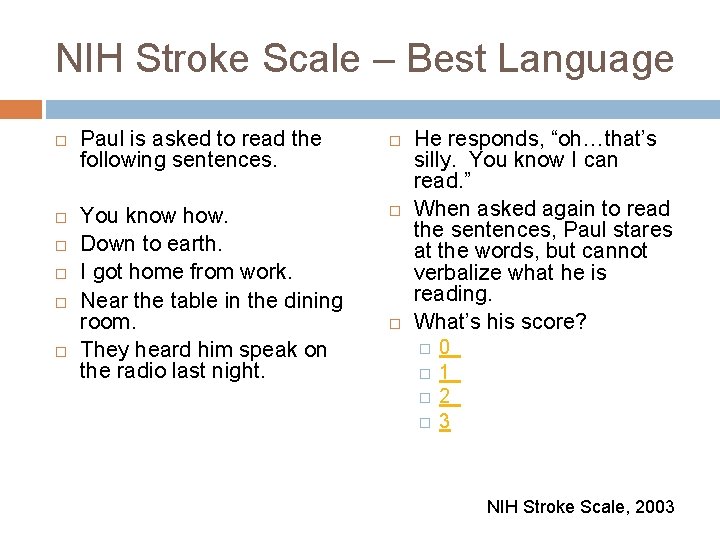
NIH Stroke Scale – Best Language Paul is asked to read the following sentences. You know how. Down to earth. I got home from work. Near the table in the dining room. They heard him speak on the radio last night. He responds, “oh…that’s silly. You know I can read. ” When asked again to read the sentences, Paul stares at the words, but cannot verbalize what he is reading. What’s his score? � � 0 1 2 3 NIH Stroke Scale, 2003
Perfect answer. Click here to continue.
Give it another shot. Click here to try again.
NIH Stroke Scale - Dysarthria Paul is asked to repeat the words below. Mama Tip –Top Fifty-Fifty Thanks Huckleberry Baseball Player He repeats some of the words clearly, but others are difficult to understand. Based on Paul’s response, he would be a given a 1 for this area of the NIH stroke scale. NIH Stroke Scale, 2003
NIH Stroke Scale – Extinction and Inattention The final category or the NIH stroke scale gave Paul a score of 1. After completing the NIH stroke scale, Paul has a total score of 18. What does this mean? NIH Stroke Scale, 2003
NIH Stroke Scale The NIH Stroke Scale is helpful in measuring the severity of a stroke and is also helpful in evaluating improvement or worsening of an acute stroke patient. The score can range from 0 -42. The higher the score, the more severe the neurological injury. A score of 10 or greater gives a patient a less likely chance for a good recovery. A score over 22 is considered a major stroke. NIH Stroke Scale, 2003 Wild Iris Medical Education, 2010
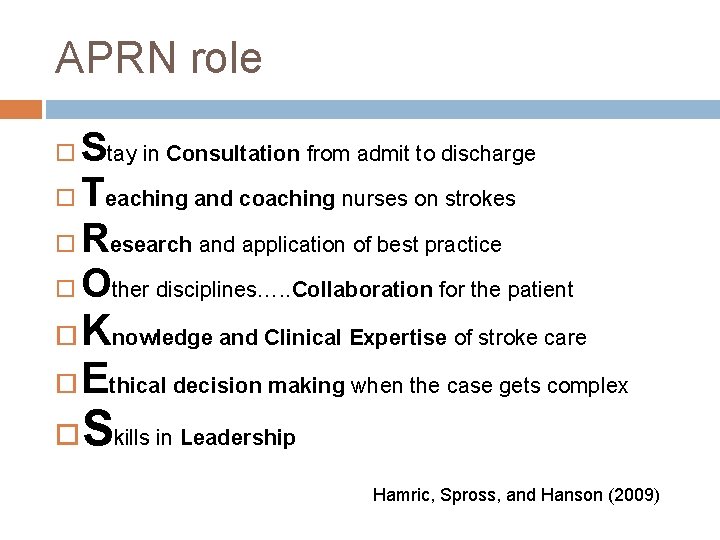
APN CNS Role Paul is admitted to the Intensive Care Unit for further monitoring. You, are a CNS on that unit and are aware of his arrival. As a CNS just spell out STROKES to put it all together. Microsoft Clip Art, 2010
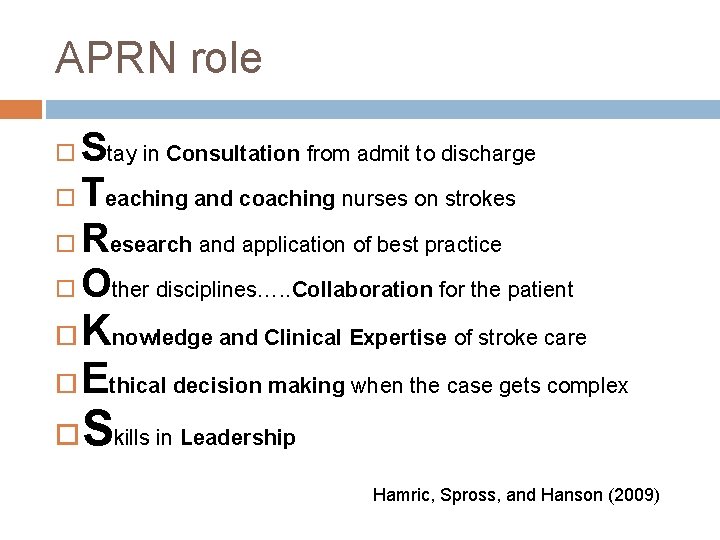
APRN role Stay in Consultation from admit to discharge Teaching and coaching nurses on strokes Research and application of best practice Other disciplines…. . Collaboration for the patient Knowledge and Clinical Expertise of stroke care Ethical decision making when the case gets complex Skills in Leadership Hamric, Spross, and Hanson (2009)
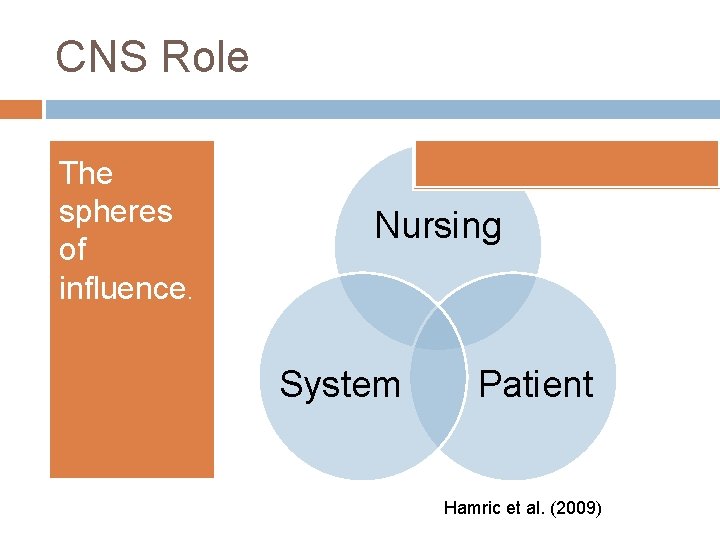
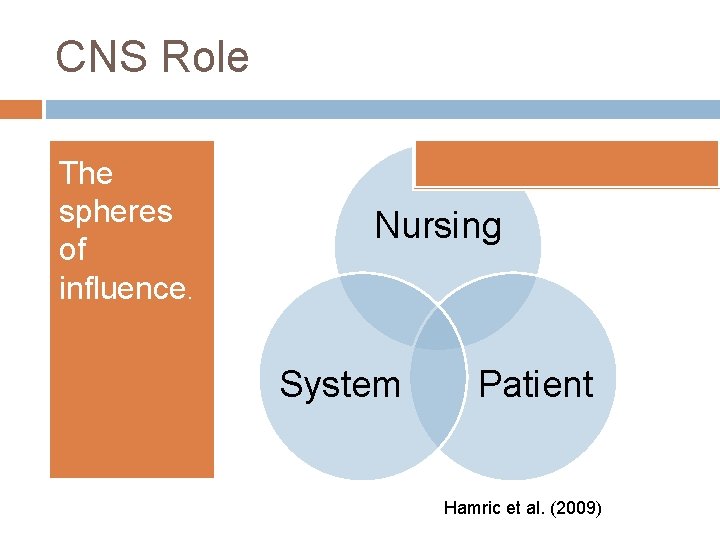
CNS Role The spheres of influence. Nursing System Patient Hamric et al. (2009)
Summary Throughout this tutorial you should have learned. � How to define a generalized and ischemic stroke. � What the risk factors of a stroke are. � The pathophysiology of an ischemic stroke. � Understanding of the NIH stroke scale. � Review of the CNS core competencies and spheres of influence.
Literature Cited Hamric, A. B. , Spross, J. A. , & Hanson, C. M. (2009). Advanced practice nursing: An integrative approach (4 th ed). St. Louis, MO: Elsevier Saunders. Bergman, D. (2011). Preventing recurrent cerebrovascular events in patients with stroke or transient ischemic attack: The current data. Journal of the American Academy of Nurse Practitioners, 23 (2011), 659 -666. doi: 10. 1037/0278 -6133. 24. 2. 225. Katz, M. J. (2010). Stroke ICU and potential complications. Wild Iris Medical Education. Retrieved from http: //www. nursingceu. com/courses/328/indexx_nceu. html Gibson, C. M. , (2011). Stroke Pathophysiology. Wikidoc. Retrieved from http: //www. wikidoc. org/index. php/Stroke_pathophysiology National Institute of Health Stroke Scale (NIHSS). (2003). NIH Stroke Scale. Retrieved from http: //www. nihstrokescale. org/ Porth, C. M. & Matfin, G. (2009). Pathophysiology: Concepts of altered health states (8 th ed). Philadelphia: Lippincott, Williams, & Wilkins.