Occupational Asthma ARSHAD EJAZI Occupational asthma Definition Occupational
- Slides: 45
Occupational Asthma ARSHAD EJAZI
Occupational asthma Definition “Occupational asthma is a form of work-related asthma characterized by variable airflow obstruction, airway hyperresponsiveness, and airway inflammation attributable to a particular exposure in the workplace and not due to stimuli encountered outside the workplace” Bernstein IL et al. Asthma in the workplace, 2006.
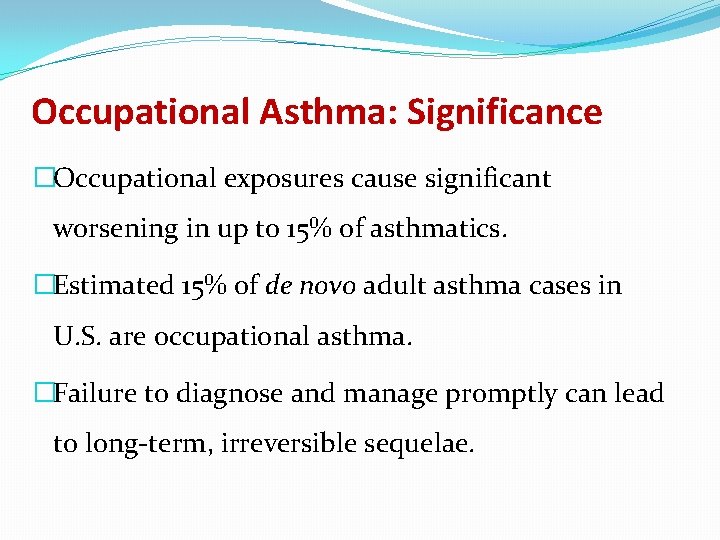
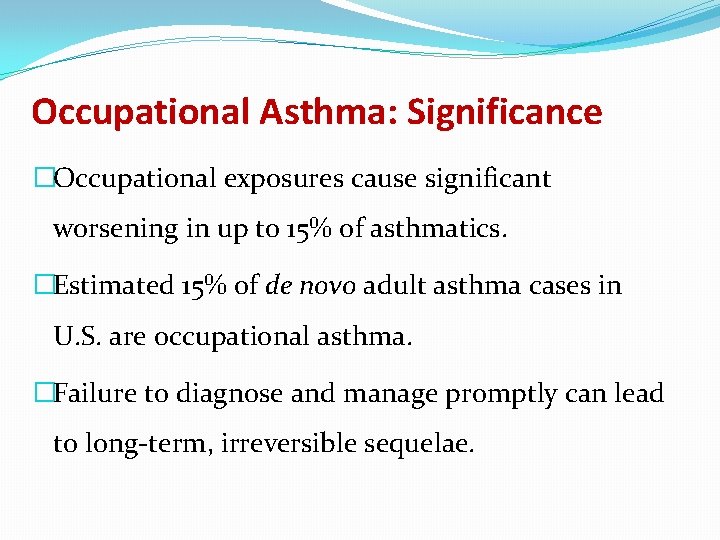
Occupational Asthma: Significance �Occupational exposures cause significant worsening in up to 15% of asthmatics. �Estimated 15% of de novo adult asthma cases in U. S. are occupational asthma. �Failure to diagnose and manage promptly can lead to long-term, irreversible sequelae.
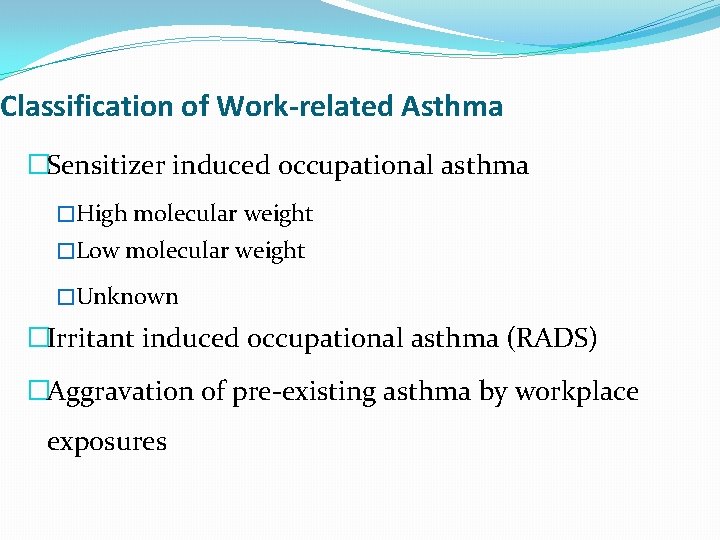
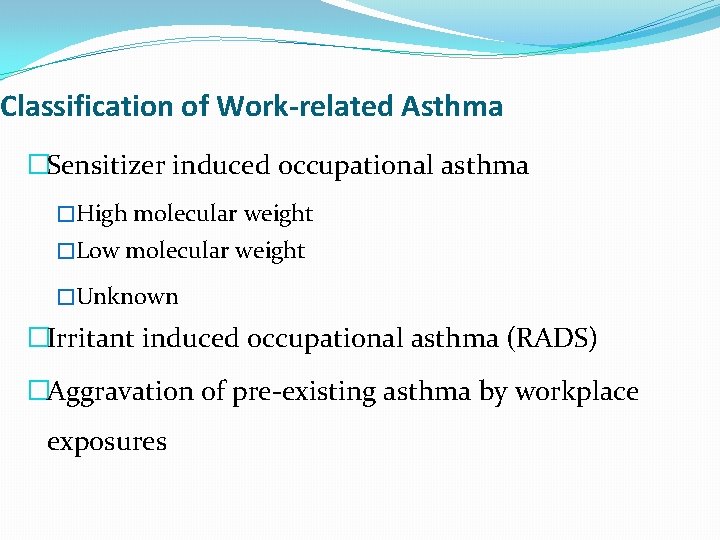
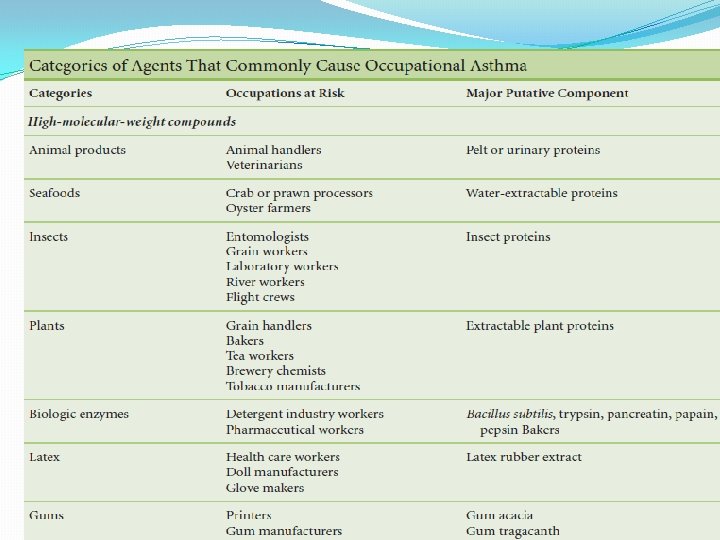
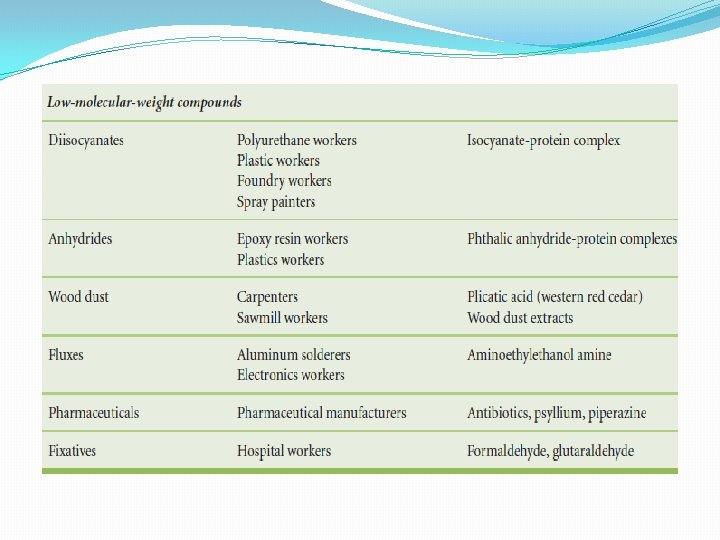
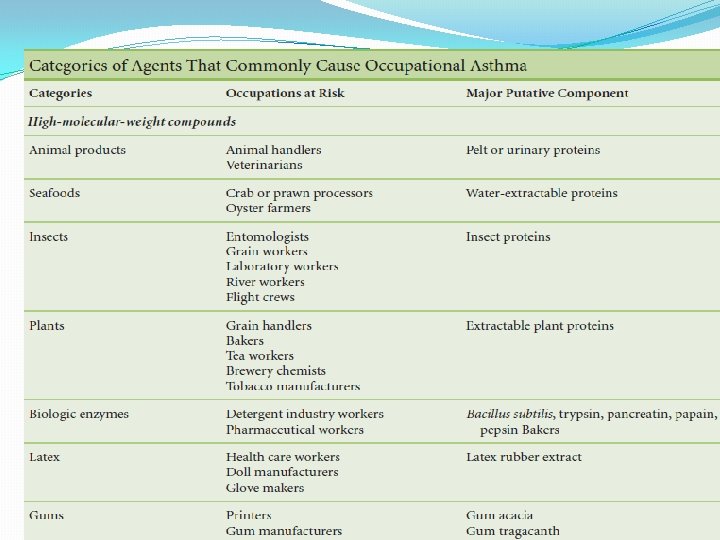
Classification of Work-related Asthma �Sensitizer induced occupational asthma �High molecular weight �Low molecular weight �Unknown �Irritant induced occupational asthma (RADS) �Aggravation of pre-existing asthma by workplace exposures
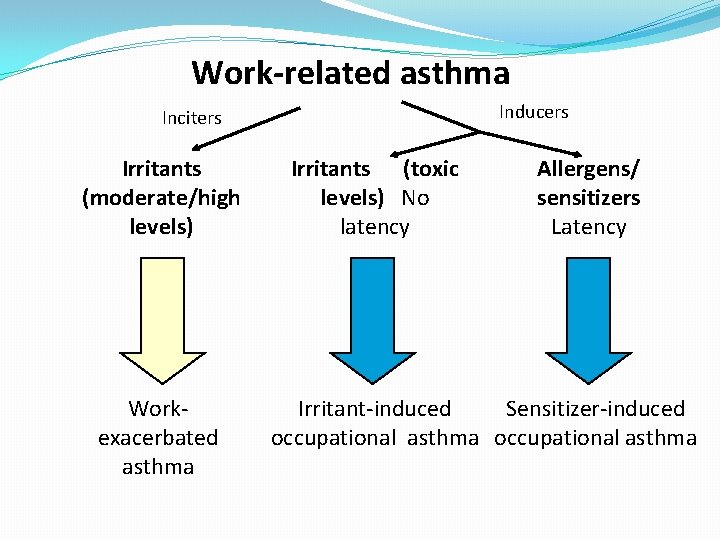
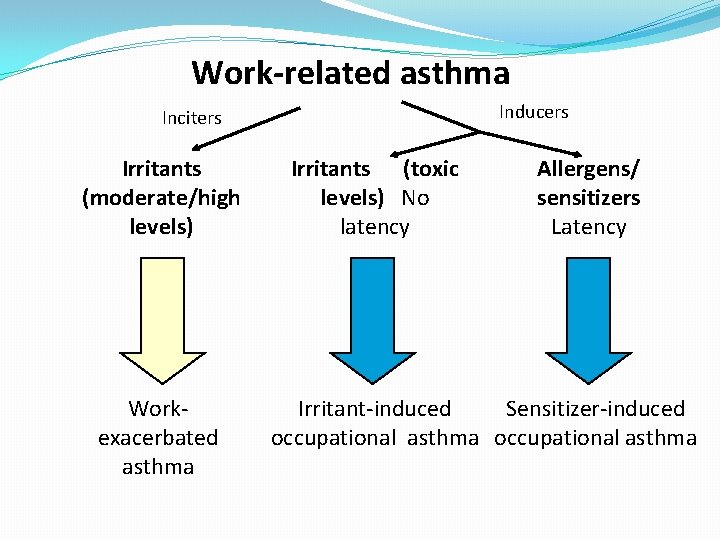
Work-related asthma Inducers Inciters Irritants (moderate/high levels) Workexacerbated asthma Irritants (toxic levels) No latency Allergens/ sensitizers Latency Irritant-induced Sensitizer-induced occupational asthma
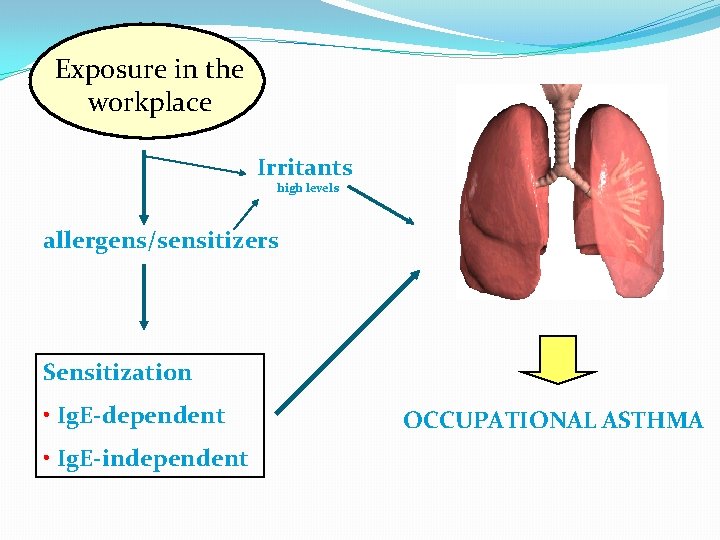
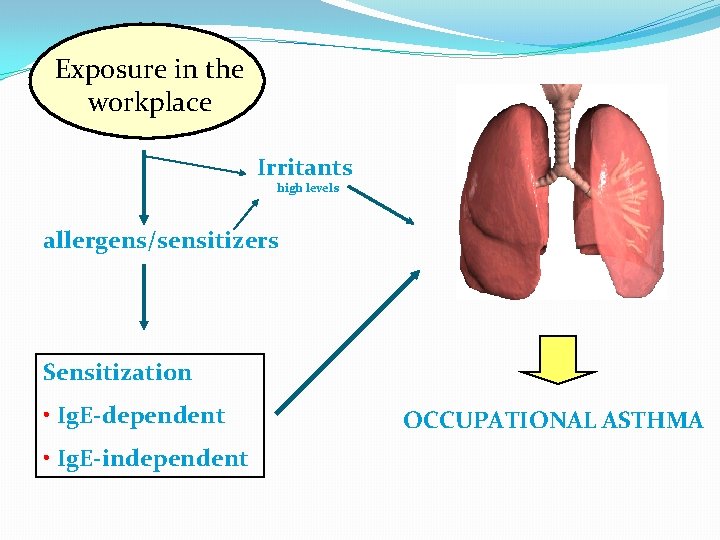
Exposure in the workplace Irritants high levels allergens/sensitizers Sensitization • Ig. E-dependent • Ig. E-independent OCCUPATIONAL ASTHMA
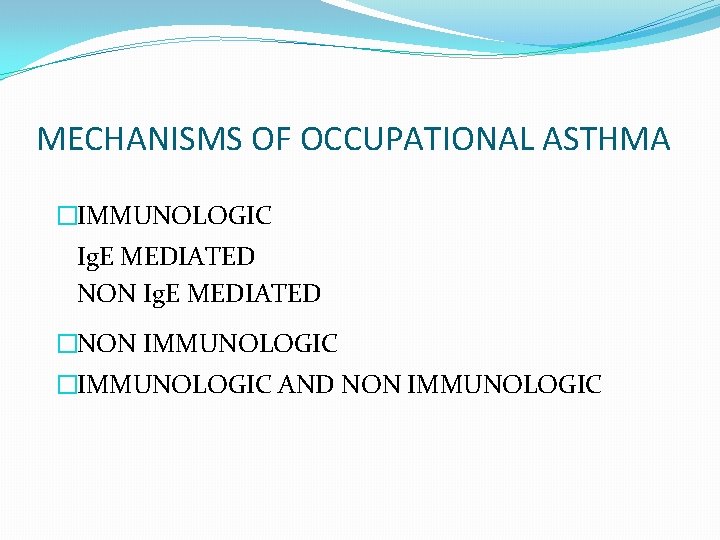
MECHANISMS OF OCCUPATIONAL ASTHMA �IMMUNOLOGIC Ig. E MEDIATED NON Ig. E MEDIATED �NON IMMUNOLOGIC �IMMUNOLOGIC AND NON IMMUNOLOGIC
MECHANISMS INVOLVED IN OCCUPATIONAL ASTHMA �T CELL RESPONSE �NONLINEAR EXPOSURE REPONSE �BASOPHILS AND MONCYTES ROLE �AIRWAY REMODELING WHEN ASYMPTOMATIC �POSSIBLE ROLE FOR IRRITANT EXPOSURE
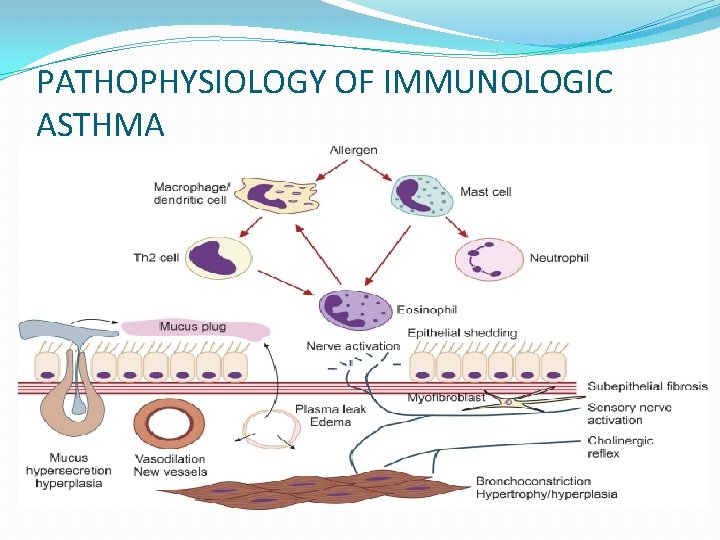
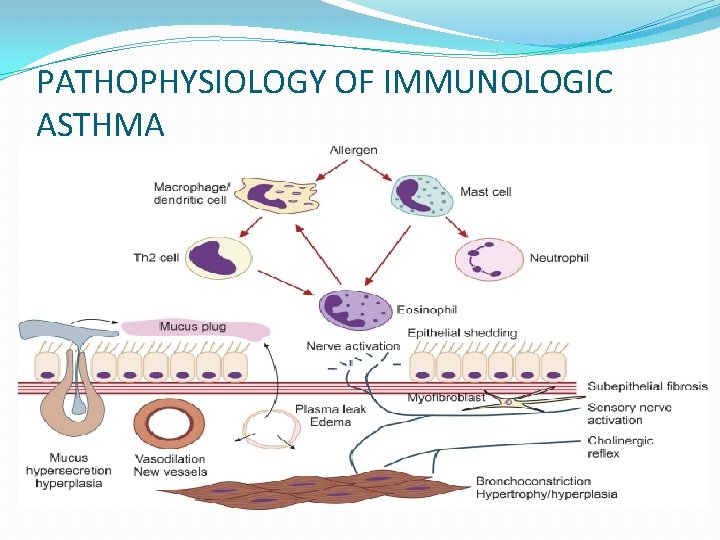
PATHOPHYSIOLOGY OF IMMUNOLOGIC ASTHMA
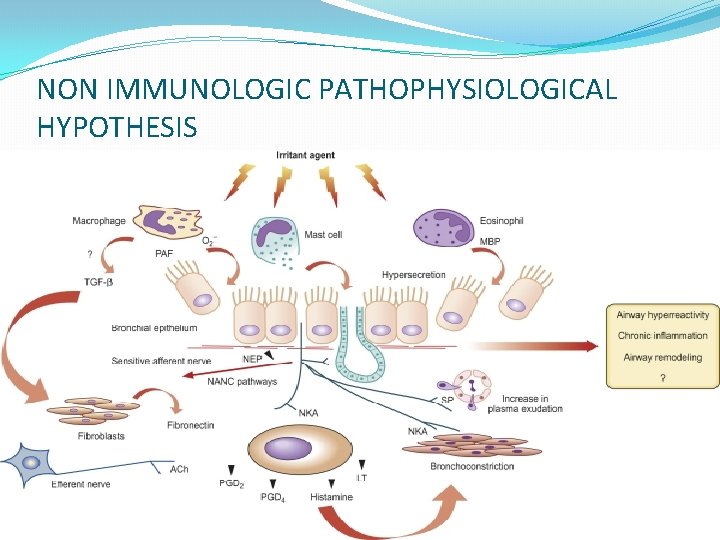
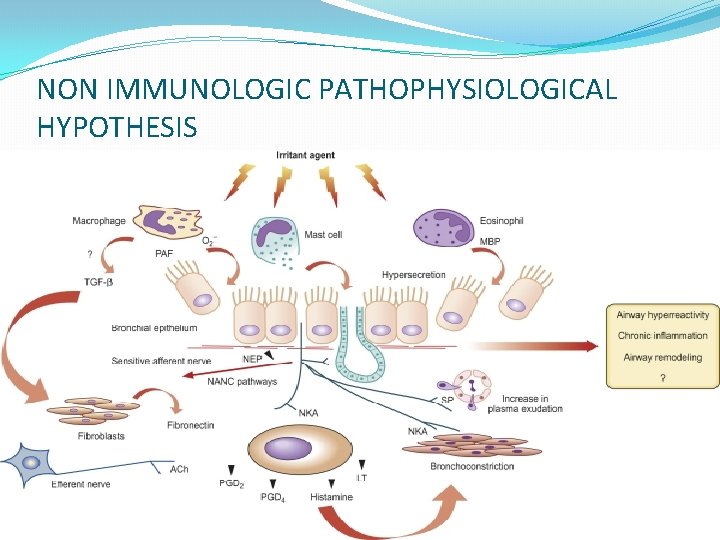
NON IMMUNOLOGIC PATHOPHYSIOLOGICAL HYPOTHESIS
RISK FACTORS RESULTS FROM THE INTERACTION HOST FACTORS GENETIC FACTORS LEVELS OF EXPOSURE ROUTE OF EXPOSURE
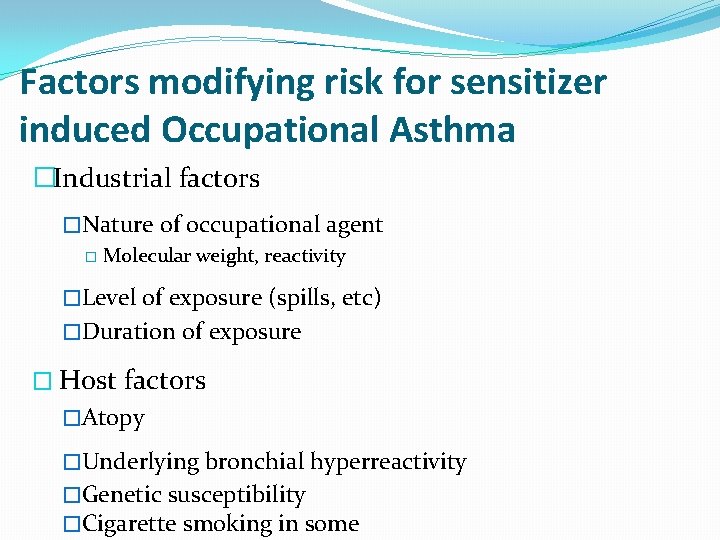
Factors modifying risk for sensitizer induced Occupational Asthma �Industrial factors �Nature of occupational agent � Molecular weight, reactivity �Level of exposure (spills, etc) �Duration of exposure � Host factors �Atopy �Underlying bronchial hyperreactivity �Genetic susceptibility �Cigarette smoking in some
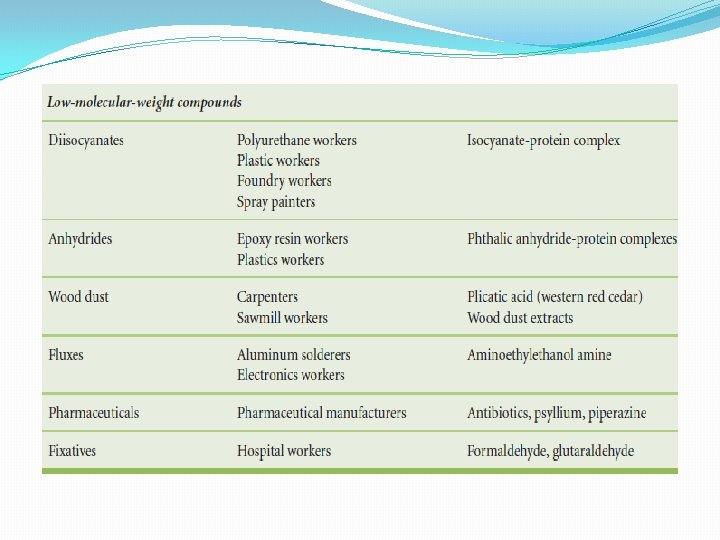
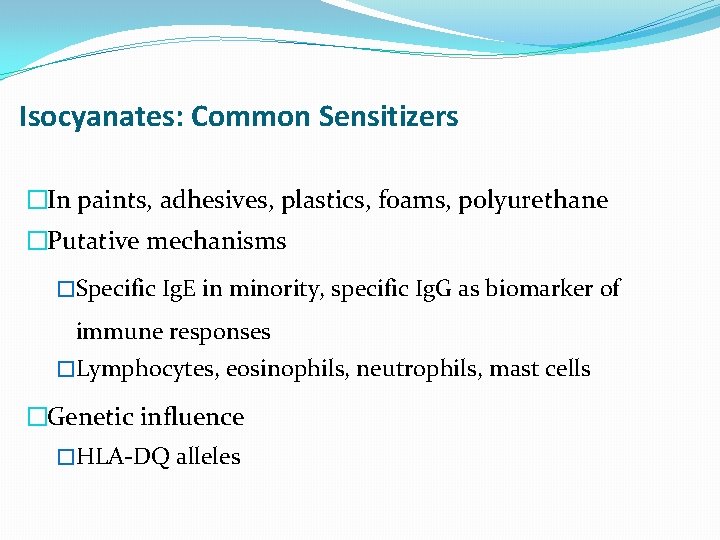
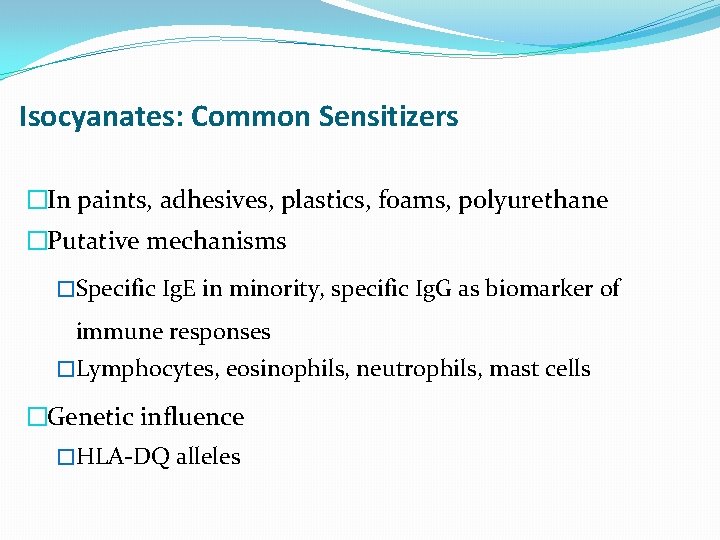
Isocyanates: Common Sensitizers �In paints, adhesives, plastics, foams, polyurethane �Putative mechanisms �Specific Ig. E in minority, specific Ig. G as biomarker of immune responses �Lymphocytes, eosinophils, neutrophils, mast cells �Genetic influence �HLA-DQ alleles
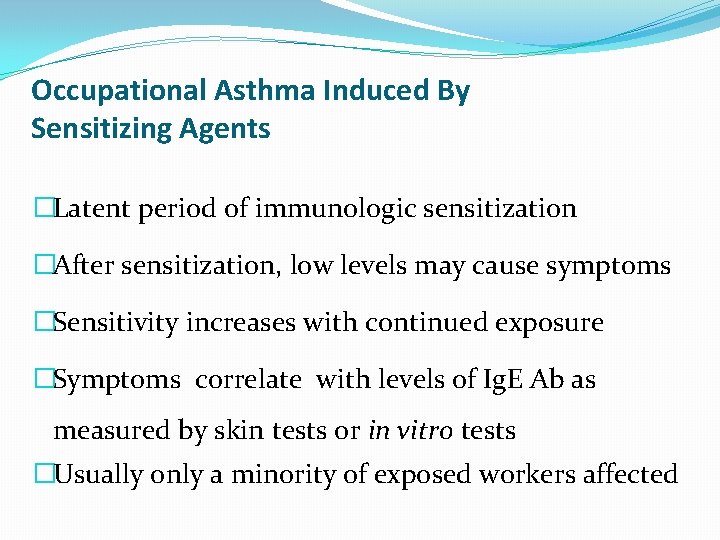
Occupational Asthma Induced By Sensitizing Agents �Latent period of immunologic sensitization �After sensitization, low levels may cause symptoms �Sensitivity increases with continued exposure �Symptoms correlate with levels of Ig. E Ab as measured by skin tests or in vitro tests �Usually only a minority of exposed workers affected
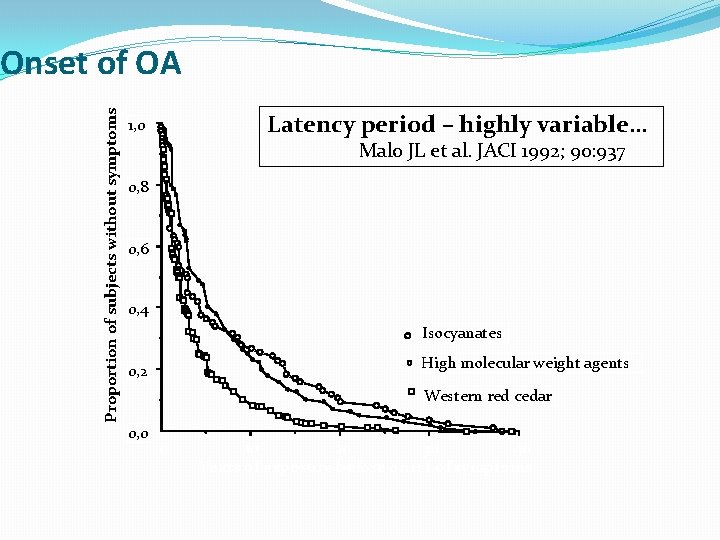
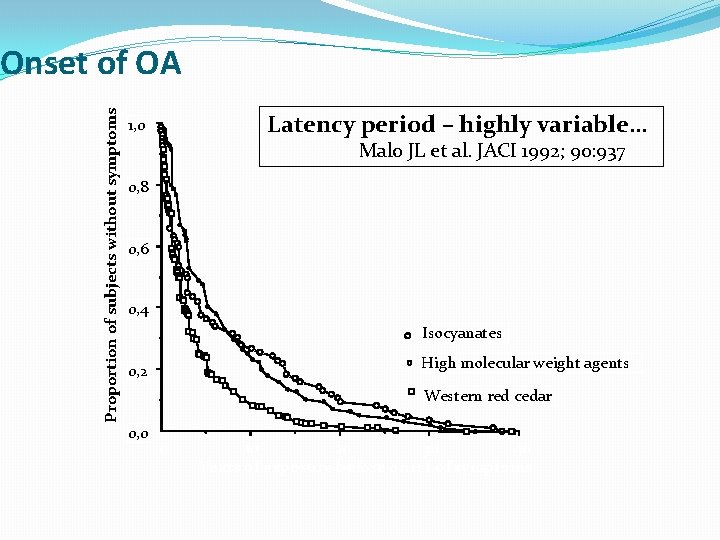
Proportion of subjects without symptoms Onset of OA Latency period – highly variable… 1, 0 Malo JL et al. JACI 1992; 90: 937 0, 8 0, 6 0, 4 Isocyanates High molecular weight agents 0, 2 Western red cedar 0, 0 0 10 20 30 40 Years of exposure before onset of symptoms
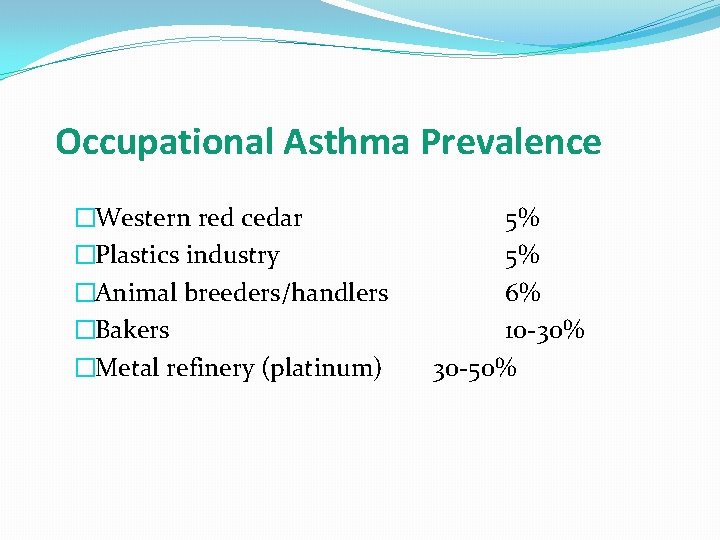
Occupational Asthma Prevalence �Western red cedar �Plastics industry �Animal breeders/handlers �Bakers �Metal refinery (platinum) 5% 5% 6% 10 -30% 30 -50%
Diverse industries associated with sensitizer induced Occupational Asthma �Plastics and paint manufacturing �Electronics, photography �Welding, metal refining �Health care, pharmaceutical manufacturing �Saw mills, forestry �Farming
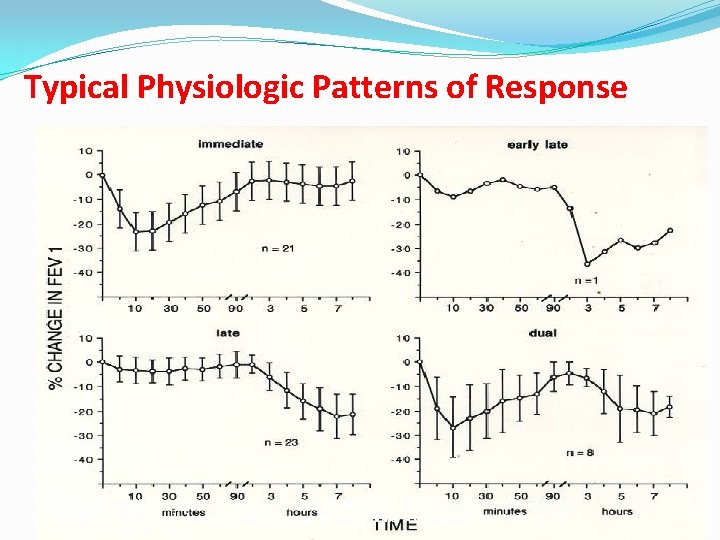
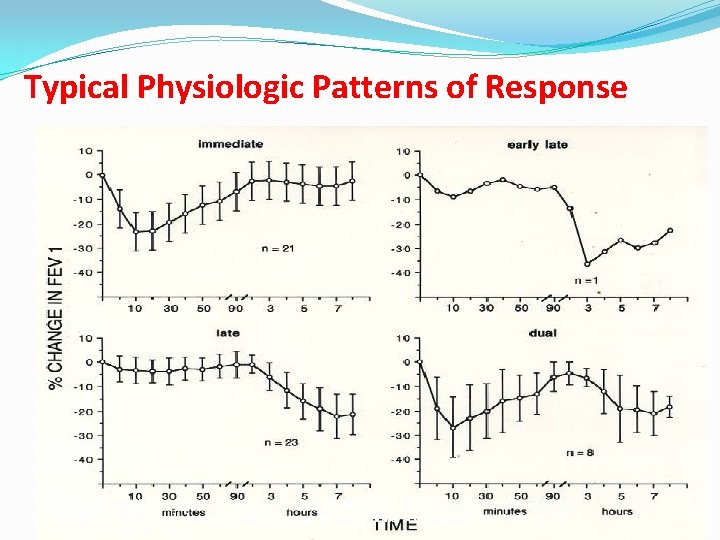
Typical Physiologic Patterns of Response Perrin B, Cartier A, Ghezzo H, Grammer L, Harris K, Chan H et. Al. Reassessment of the temporal patterns of bronchial obstruction after exposure to occupational sensitizing agents. J Allergy Clin Immunol 1991; 87: 630 -9.
Reactive Airways Dysfunction Syndrome (RADS) �No previous history of asthma �Acute, high level exposure to toxic/irritant �Respiratory symptoms within 24 hrs of exposure �Persistent respiratory symptoms, non-specific bronchial hyperreactivity �Pulmonary function may be normal or show reversible airway obstruction: � but obstruction are less reversible than sensitizer induced asthma �Eosinophilic infiltration not characteristic, subepithelial fibrosis �Worse outcome than sensitizer induced OA
Exacerbation of pre-existing asthma � Reported in > 20% of asthmatics in 1° care settings. � Asthma that preceded or started concurrently with the implicated work conditions, and worsened at work. � Causes include typical asthma triggers such as dusts or fumes at work, cold air and exercise. � If frequent or persistent, may mimic sensitizer OA. � Document with objective tests, especially when work-related symptoms are frequent or prolonged, � Management includes: � optimizing asthma control. � may require reducing work exposure to triggers � � (e. g. short-term use of respirators, or move to cleaner area.
Occupational History �Current and previous jobs �Employer, job names and descriptions, duration �Specific exposures �Adverse health effects �Control measures �Provision and use of personal protective equipment �Work place practices (e. g. procedures to follow if a spill occurs) �Engineering controls
Clinical history to be asked �Circumstances of the onset of asthma symptoms � Severity and persistence, clinical course of asthma �Temporal relationships between exposures at work and disease exacerbation: �Immediate (minutes), late (hours) or dual (both) �Known triggers and intercurrent factors of asthma �Identify risk factors: Atopy – Smoking habit �Focused occupational/environmental history
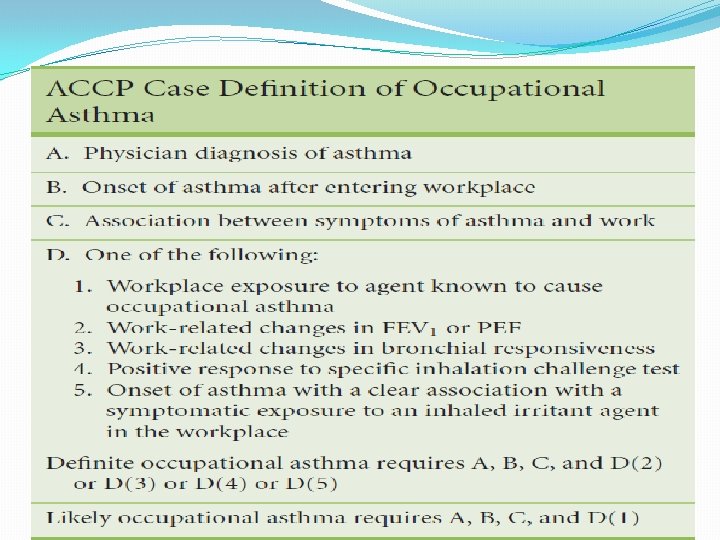
Diagnostic Approach to Occupational Asthma �Does the patient have asthma? �History, physical examination �Reversible airway obstruction (e. g. spirometry) �Non-specific airway hyperreactivity If absent while symptomatic and at work, may rule out diagnosis �Is the asthma caused by work or a non-occupational factor? – �History �Objective testing
Does History Suggest Occupational Basis? �Symptoms within months of job change? �(though may also take years to develop. ) �New agent introduced in workplace? �Are respirable agents in the workplace known to cause asthma? �Symptoms relieved on weekends or vacations? �Are other workers affected? �Have workers left because of similar symptoms?
Additional Information About Suspected Work Exposures �Information sources: employers, product manufacturers, labor unions. �Material safety data sheet (MSDS) (Bernstein JA, Material safety data sheets: are they reliable in identifying human hazards? JACI 2002; 110: 35 -8. ) �By law, employer must provide �Identity of workplace agents and information about adverse health effects �May be misleading �Contacts for additional information �Medical literature searches
Does History Suggest Non-Occupational Basis? �No relation between work and symptoms �Preexisting asthma / respiratory problems �Upper respiratory infection at onset of symptoms �Non-occupational allergies �Smoking �Medications (beta blockers, NSAIDs) �Gastroesophageal reflux symptoms �Review medical records
Occupational Hygiene Assessment �Occupational/industrial hygienists assess workplace environments. �Identify relevant exposures. �Measure concentrations to determine if suspect agents are present at harmful levels �Recommend changes in the work environment (e. g. product substitution, improved ventilation).
Tests for Occupational Asthma �History alone insufficient for diagnosis �Objective testing �Work-related changes in peak flows(repeated & >20% fall) �PEF coupled with nonspecific bronchial responsiveness to Methacholine increases sensitivity of diagnosis �Immunologic testing for occupational allergens(skin testing & In vitro tests for specific Ig. E) �Controlled inhalation challenge with suspect agent
Immunologic assessment • • • Skin prick tests (occasionally ID) to HMW agents In vitro tests – Measurements of specific Ig. E: RAST/CAP, ELISA – Immunoblotting, CRIE Reagents: – Whole “natural” extracts (not standardized, potency? ) – Purified allergens (e. g. enzymes, isolated proteins) – Recombinant allergens (e. g. latex allergens)
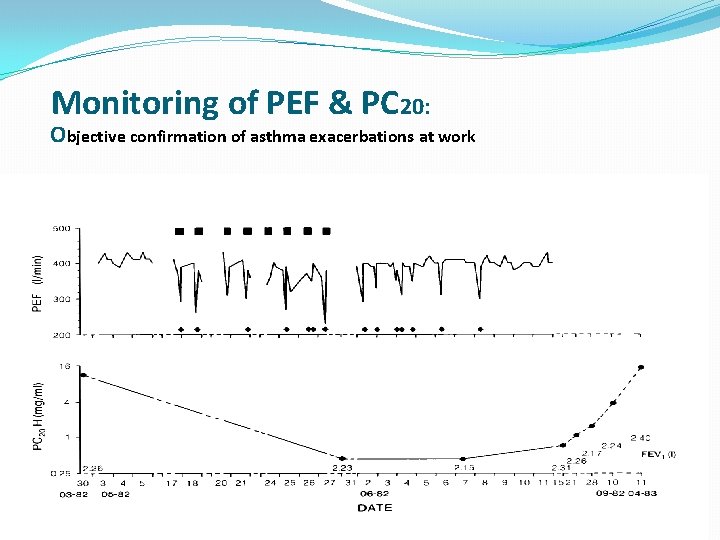
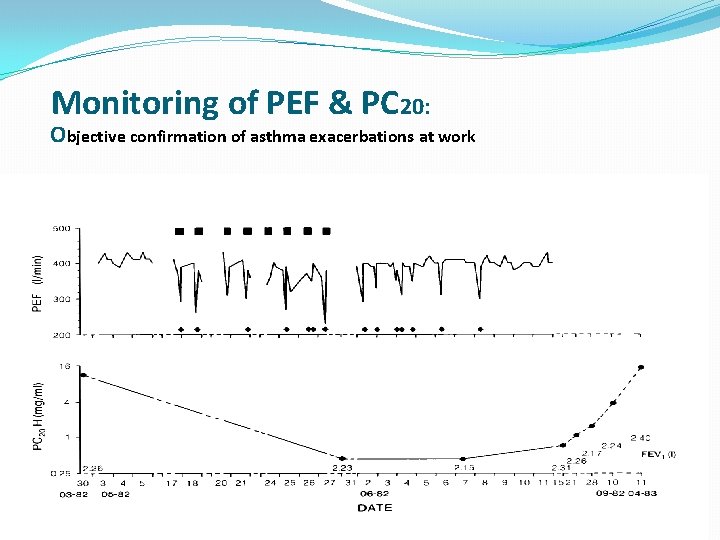
Monitoring of PEF & PC 20: Objective confirmation of asthma exacerbations at work Cartier A, Malo JL, Forest F, Lafrance M, Pineau L, St-Aubin JJ et al. Occupational asthma in snow crabprocessing workers. J Allergy Clin Immunol 1984; 74: 261 -9
Indications for Controlled Challenge with Suspect Agent �Diagnostic uncertainty �Poor history, confounding factors, work related changes in peak flows unavailable or equivocal, unknown etiology, can’t return to work for monitoring �Diagnostic dispute �Physicians, employers, insurance companies, attorneys �Research
Relative Contraindications for Specific Inhalation Challenge �Inability of worker to hold asthma medications before challenge �Unstable asthma and/or low FEV 1 �Severe underlying medical or psychological problem
Specific Inhalation Challenge in Occupational Asthma �Most often, these tests are done on an outpatient basis. �Multiple challenges required. �Tests are time consuming and expensive. �Informed consent and compliance needed. �In certain condition, these are done in workplace like- when the sensitizing agent at work is unknown, too many potential sensitizers.
Interpretation of positive challenge �A positive challenge is usually defined by a sustained fall in FEV 1 of ≥ 20%, compared to the control mock exposure day. �Other indices suggesting OA: �≥ 3 fold decrease post challenge in PC 20 �Increase in eosinophils in post challenge induced sputum compared to baseline pre-challenge.
Interpretation of negative challenge �A negative challenge, however, does not entirely exclude the diagnosis of occupational asthma: �Wrong agent (or sensitizing process not active) �Loss of sensitization over time out of exposure �Mixture of antigens at work not replicated in challenge �Took medication that blocked the test (e. g. bronchodilators)
Purpose of Immunosurveillance Programs � To periodically evaluate the health of workers in the workplace � Monitor clinical symptoms � Monitor changes in lung function � Monitor changes in Chest x-rays � Monitor specific antibody responses � Identification of workers demonstrating signs of sensitization and/or work related symptoms � Early removal from further exposure � Identify hazardous work conditions using group health information and environmental information � Implement appropriate interventions to prevent reoccurrences or new cases � Evaluation of the effectiveness of exposure controls
Medical Surveillance Methods �Itemized questionnaires � Respiratory responses to 22 irritants correlated with methacholine PC 20 �Spirometry �Testing for Nonspecific Bronchial Hyperresponsiveness � Methacholine, mannitol, histamine �Immunological tests � ELISAs (low and high molecular weight antigens) � Skin testing (enzymes, animal handlers, some LMW chemicals such as anhydrides and platinum salts)
Occupational Asthma Management �Reduce / avoid exposure in workplace. �Removal of worker in some cases, particularly if sensitizer present. �Surveillance measures: �Periodic monitoring of work place exposures, spirometry, tests for immunologic sensitization. �Medications. �Address any non-occupational factors. �The patient with OA should be considered a sentinel event in the workplace.
Occupational Asthma Prognosis �Timely removal should result in improvement. � Causes Residual disease: Isocyanates, red cedar, snow crab, some irritants, other agents. �Prognosis worse if: � longer duration of exposure, � greater severity / frequency of symptoms, � airway obstruction or hyper-reactivity, dual bronchial responses.
Occupational Asthma Prognosis �Restriction from exposure or removal from the job often has significant socioeconomic consequences for the worker: �Loss of income �Unemployment �Higher medication costs in those remaining in exposure � Be reasonably sure of the diagnosis and cause of OA before recommending job change.
Impairment and Disability from Occupational Asthma �Assess 2 yrs after removal from exposure �Respiratory impairment assessed by guidelines �Degree of airway obstruction, reversibility �Airway hyperresponsiveness �Medication requirements �Disability �Limitation in work tasks or activities of daily living, including future work restrictions
THANK YOU