Musculoskeletal Dysfunction In The Athlete The Shoulder John


- Slides: 23
Musculoskeletal Dysfunction In The Athlete (The Shoulder) John M. Lavelle DO Spine Physiatrist
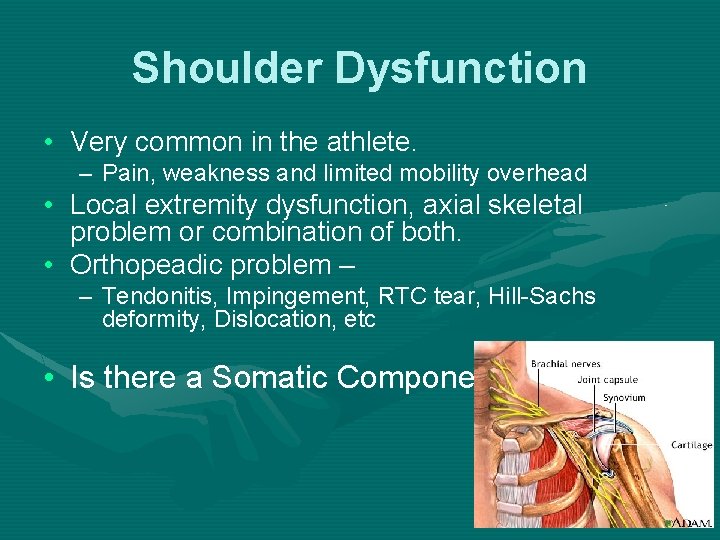
Shoulder Dysfunction • Very common in the athlete. – Pain, weakness and limited mobility overhead • Local extremity dysfunction, axial skeletal problem or combination of both. • Orthopeadic problem – – Tendonitis, Impingement, RTC tear, Hill-Sachs deformity, Dislocation, etc • Is there a Somatic Component?
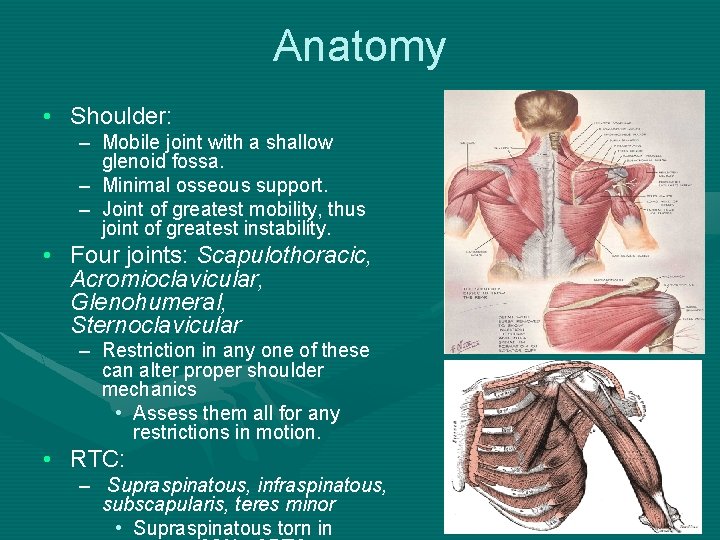
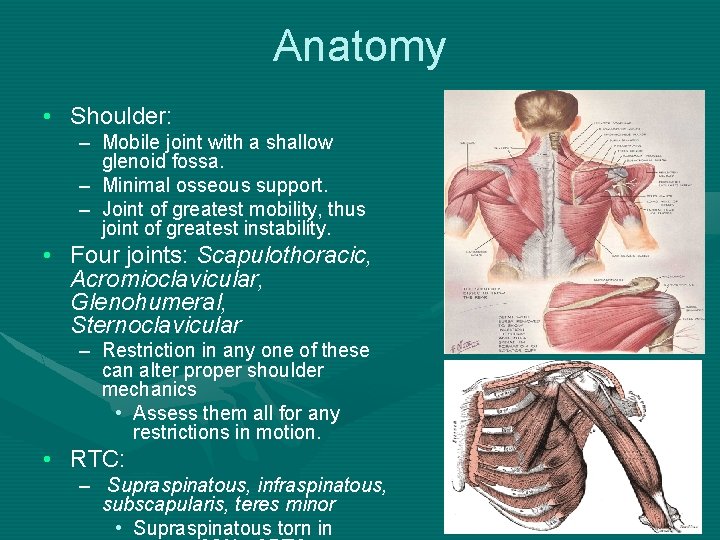
Anatomy • Shoulder: – Mobile joint with a shallow glenoid fossa. – Minimal osseous support. – Joint of greatest mobility, thus joint of greatest instability. • Four joints: Scapulothoracic, Acromioclavicular, Glenohumeral, Sternoclavicular – Restriction in any one of these can alter proper shoulder mechanics • Assess them all for any restrictions in motion. • RTC: – Supraspinatous, infraspinatous, subscapularis, teres minor • Supraspinatous torn in
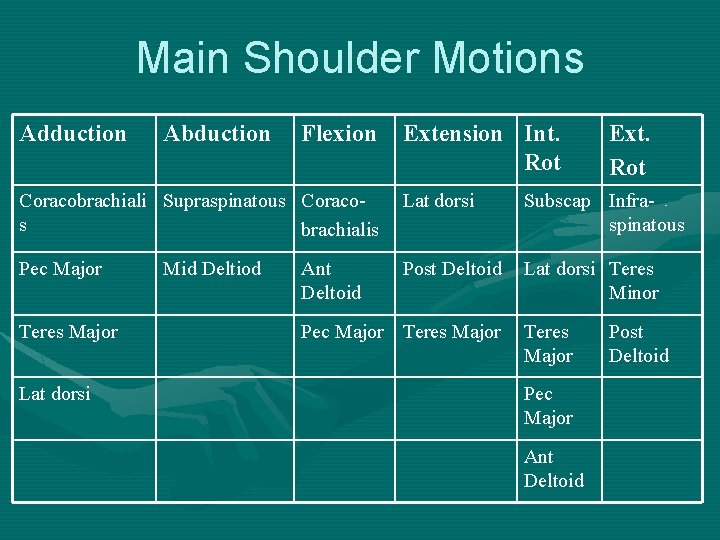
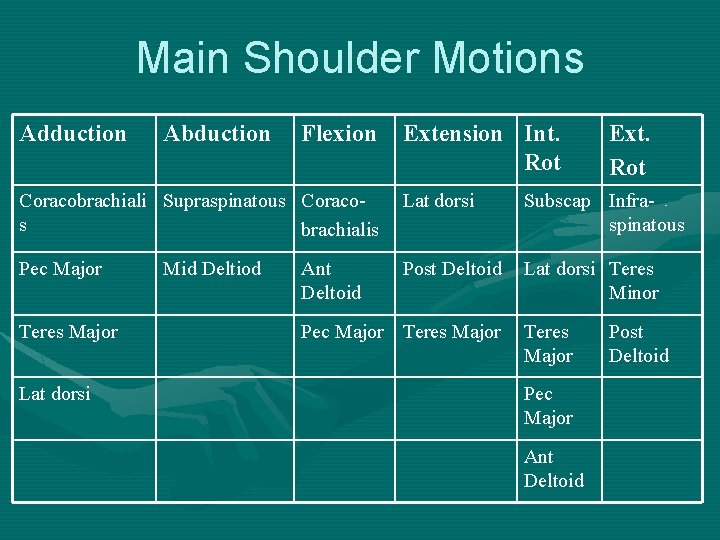
Main Shoulder Motions Adduction Abduction Flexion Extension Int. Rot Ext. Rot Coracobrachiali Supraspinatous Coracos brachialis Lat dorsi Subscap Infraspinatous Pec Major Post Deltoid Lat dorsi Teres Minor Teres Major Lat dorsi Mid Deltiod Ant Deltoid Pec Major Teres Major Pec Major Ant Deltoid Post Deltoid

History • Sport – – Pitching, Golf Rock climbing Tennis Gymnastics • How long season? , Level of play? , Equipment? • Why presenting now? : Improving? , Same? , Worse? • FOOSH injury/Collisions/Trauma - Macrotrauma • Repetitive Overuse (lifting, bending, twisting, etc) – Microtrauma
Thoracic Dysfunction • Somatic dysfunction of the thoracic spine/ribs may produce shoulder symptoms – Extended Type II dysfunction common • Segmental dysfunction alters the scapular stabilizing muscles, affecting the gliding movement of the scapula over the thoracic cage. • Only the first 20 -30° of shoulder abduction occurs without scapulothoracic motion. – RTC muscles become irritable and tender • The sympathetic autonomic outflow for the UE/neck: T 1 -T 4. – Somatic dysfunction in this region can lead to increased stimulation of the sympathetics.
Cervical Dysfunction • The cervical spine also affects the shoulder. – C 5 -C 8 nerve roots exit the c-spine thru intervertebral foraminae and coalesce in the brachial plexus innervates the UE. – Somatic dysfunction of the neck. • Impingement at the nerve root. • Compression at the brachial plexus. – Anterior and middle scalenes, first rib and/or clavicular dysfunction, and myofascial strain – RTC patients tend to “hike” shoulder: • Scalene hypertonicity, upper trap tender points, type II cervical dysfunction, elevated 1 st rib, T 1 dysfunction
Latissimus Dorsi • Connection between the pelvis and the UE through latissimus dorsi muscle. – Attaches to the iliac crest, the spinous processes of the lumbar and lower thoracic vertebrae and the bicipital groove. – In addition, this muscle often attaches to the inferior angle of the scapula as it passes over the scapula. • Somatic dysfunction at the thoracolumbar junction can lead to dysfunction of the UE. UE
Functional Examination • Orthopeadic pathology vs Functional conditions – Evaluate performing sport specific movement – Musculoskeletal compensations • normal vs abnormal – Consider center of gravity, ground reaction forces, muscle firing patterns and postural patterns
Osteopathic Exam • Observation: – Osteopathic standing structural exam. • Any asymmetry by comparing the mastoid process, AC joint, spine of the scapula and inferior angle of the scapula bilaterally. • Muscle wasting? - focusing on the supraspinatous, infraspinatous, trapezius, deltoid muscles, rhomboids, biceps, triceps and levator scapulae muscles. – AROM: look at cervical’s and shoulder for restrictions
Osteopathic Exam • Palpation: – Compare both shoulders - healthy shoulder first. – Palpate the c-spine - restrictions of movement in PROM – Any segmental, Fryette type II, restrictions in the cspine. – Palpate thoracic spine - any somatic dysfunction within the thoracic vertebrae, ribs or musculature. • Remember that somatic dysfunction in this area will affect scapulothoracic motion and thus the motion of the entire shoulder joint.
Osteopathic Exam • Palpation: – Along supraspinatous and infraspinatous muscles – Subscapularis muscle tender point • Place your palpating finger anterior to the posterior axillary fold and palpate the anterior boarder of the scapula. – Biceps tendon • Place the patients hand in supination and arm in external rotation to open the bicipital groove and palpate along the biceps tendon for tenderness. – Any medial scapular winging - weakness in the serratus anterior • Ask the patient to elevate/flex the arm as you depress the arm with one hand palpate the scapula with the other.
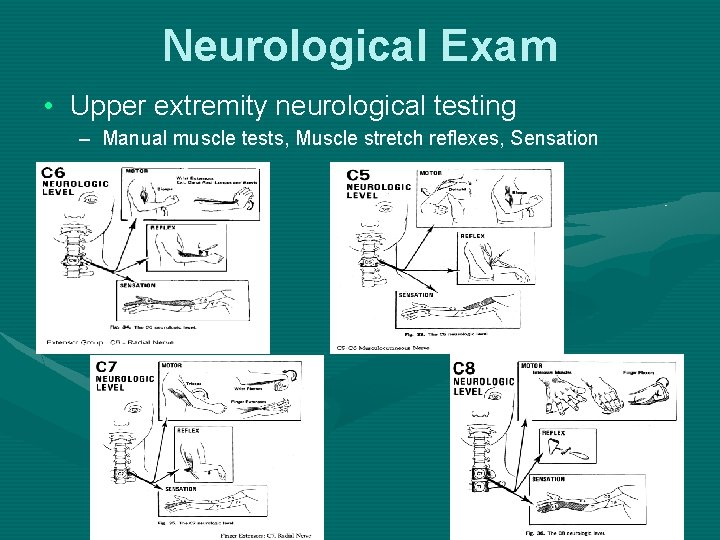
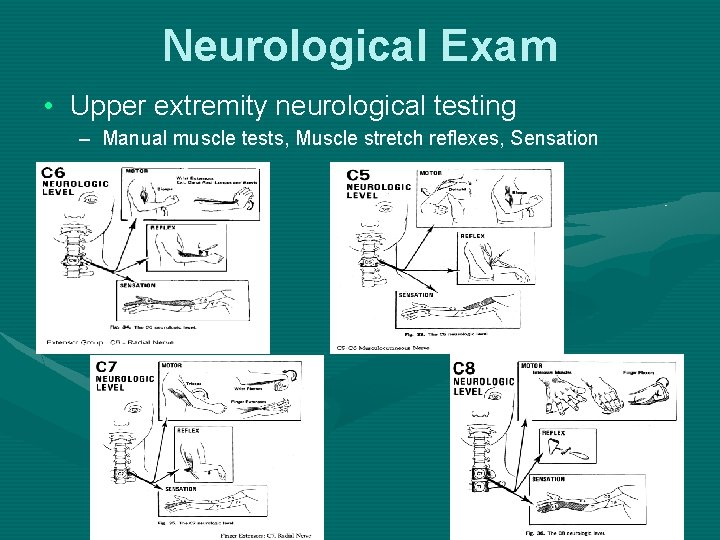
Neurological Exam • Upper extremity neurological testing – Manual muscle tests, Muscle stretch reflexes, Sensation
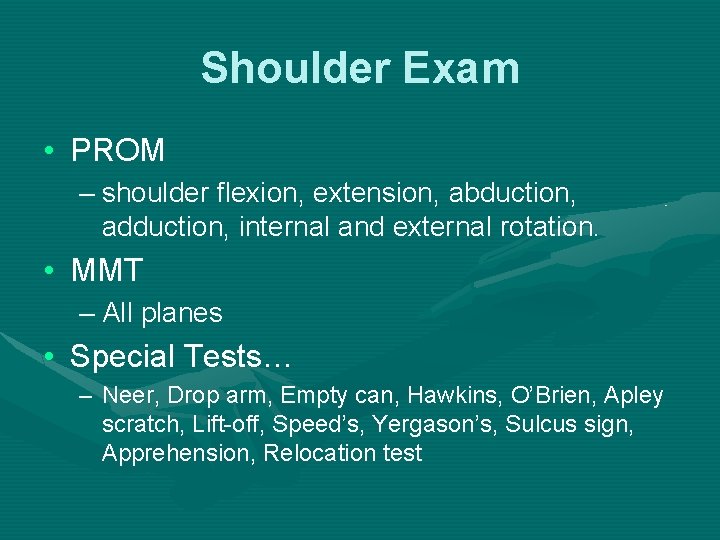
Shoulder Exam • PROM – shoulder flexion, extension, abduction, adduction, internal and external rotation. • MMT – All planes • Special Tests… – Neer, Drop arm, Empty can, Hawkins, O’Brien, Apley scratch, Lift-off, Speed’s, Yergason’s, Sulcus sign, Apprehension, Relocation test
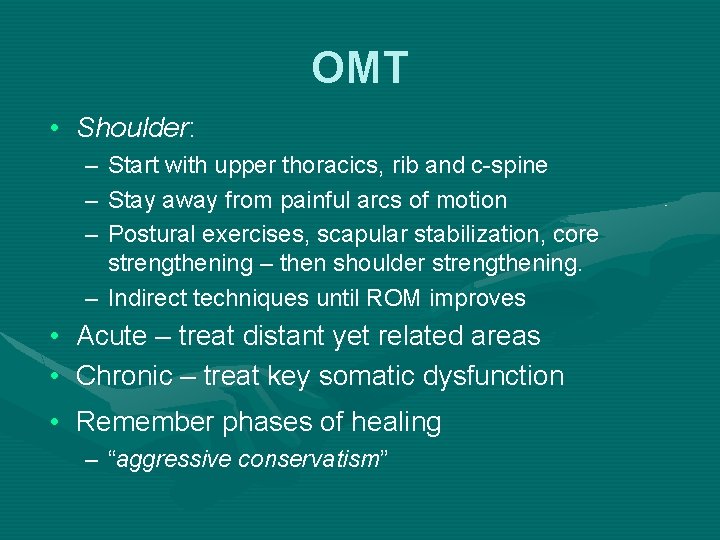
OMT • Shoulder: – – – Start with upper thoracics, rib and c-spine Stay away from painful arcs of motion Postural exercises, scapular stabilization, core strengthening – then shoulder strengthening. – Indirect techniques until ROM improves • Acute – treat distant yet related areas • Chronic – treat key somatic dysfunction • Remember phases of healing – “aggressive conservatism”
Conclusion • Clincal exam/history gives you most of the information. • Further work-up with radiographs. • Reserve MRI/Electrodiagnostics for when diagnosis is equivocal, management is in question or surgery is considered. • Begin treatment with conservative measures – OMT, NSAIDS, physical therapy.
Thank You! • References: – Nelson KE. Somatic Dysfunction in Osteopathic Family Medicine. LWW, Baltimore MD, 2007: 139 -151. – Malanga GA. Musculoskeletal Physical Examination. Elsevier, Philadelphia PA, 2006: 59 -115. – Griffin LY. Essentials of Musculoskeletal Care. AAOS, 2005: 145 -233

Myofascial Release (MFR): Scapulothoracic Release Technique Kristin Garlanger OMS III, OMM Fellow Chicago College of Osteopathic Medicine
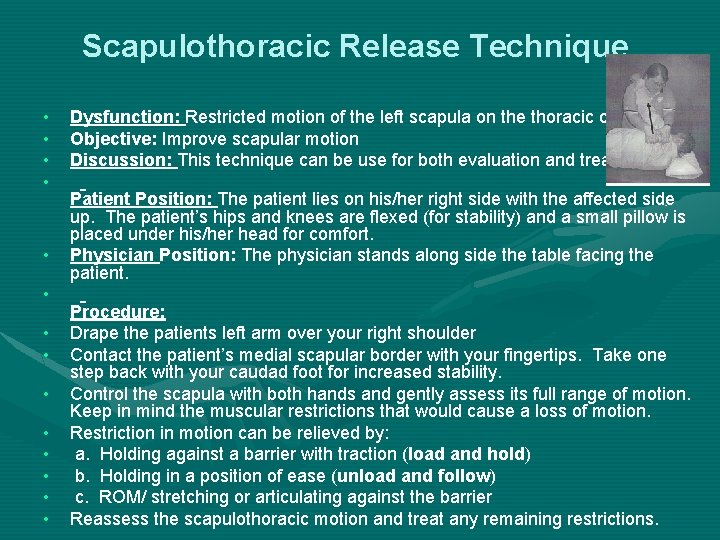
Scapulothoracic Release Technique • • • • Dysfunction: Restricted motion of the left scapula on the thoracic cage Objective: Improve scapular motion Discussion: This technique can be use for both evaluation and treatment Patient Position: The patient lies on his/her right side with the affected side up. The patient’s hips and knees are flexed (for stability) and a small pillow is placed under his/her head for comfort. Physician Position: The physician stands along side the table facing the patient. Procedure: Drape the patients left arm over your right shoulder Contact the patient’s medial scapular border with your fingertips. Take one step back with your caudad foot for increased stability. Control the scapula with both hands and gently assess its full range of motion. Keep in mind the muscular restrictions that would cause a loss of motion. Restriction in motion can be relieved by: a. Holding against a barrier with traction (load and hold) b. Holding in a position of ease (unload and follow) c. ROM/ stretching or articulating against the barrier Reassess the scapulothoracic motion and treat any remaining restrictions.
HVLA: Knee in the Back Pratik Shah OMS IV, OMM Fellow Chicago College of Osteopathic Medicine
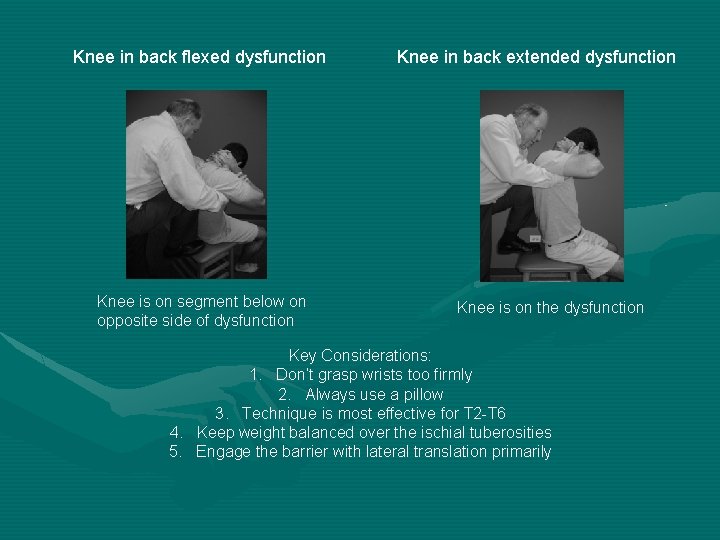
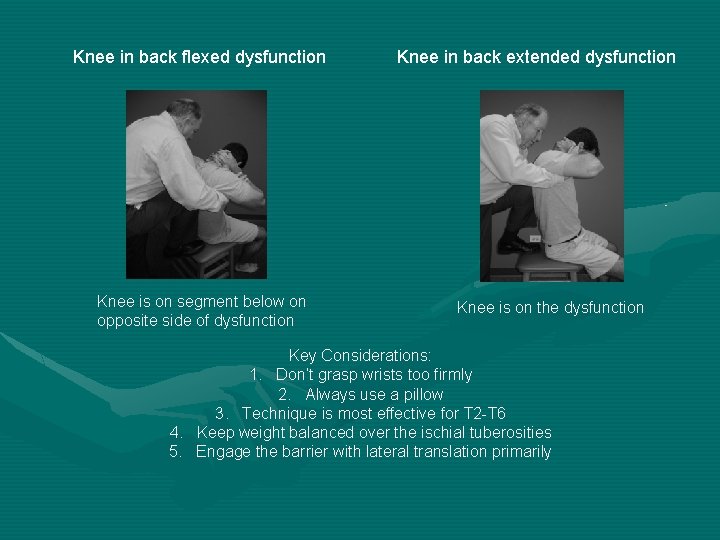
Knee in back flexed dysfunction Knee is on segment below on opposite side of dysfunction Knee in back extended dysfunction Knee is on the dysfunction Key Considerations: 1. Don’t grasp wrists too firmly 2. Always use a pillow 3. Technique is most effective for T 2 -T 6 4. Keep weight balanced over the ischial tuberosities 5. Engage the barrier with lateral translation primarily
Treating Rib Dysfunction with Functional Technique Paula Ackerman OMSV, OMM Fellow Ohio University College of Osteopathic Medicine
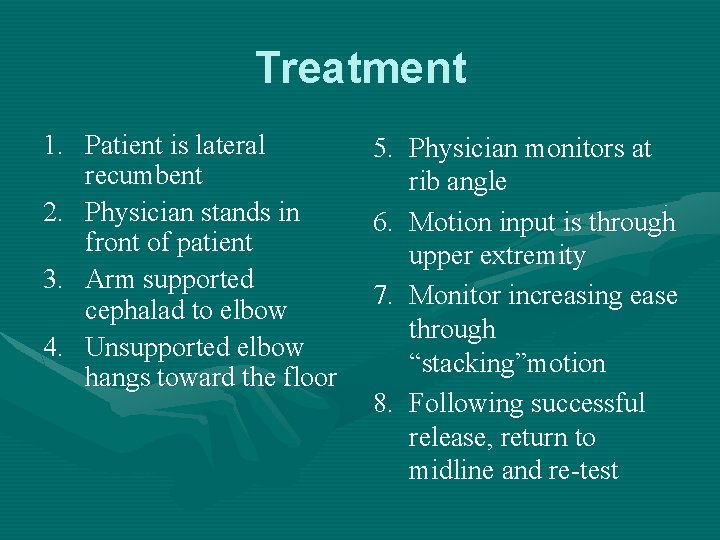
Treatment 1. Patient is lateral recumbent 2. Physician stands in front of patient 3. Arm supported cephalad to elbow 4. Unsupported elbow hangs toward the floor 5. Physician monitors at rib angle 6. Motion input is through upper extremity 7. Monitor increasing ease through “stacking”motion 8. Following successful release, return to midline and re-test