Toxicology in the Pediatric Patient Adam Litroff DO









- Slides: 112
Toxicology in the Pediatric Patient Adam Litroff, DO Emergency Medicine Pediatric Emergency Medicine
General Toxicology • Except for life-saving antidotes, most poisonings only need supportive care • Know your general work up and toxidromes • Know when to give or not to give an antidote
General Toxicology • ALWAYS Start with your ABC’s • Good history and physical exam skills are essential • Be thorough • Is there a toxidrome? If yes, treat it! Don’t always need labs
General Considerations • Most laboratory analyses are not helpful in the ED setting • Specific assays may not be available at your institution • Results of tests may be delayed hours or days • Results of tests may be insensitive or non-specific • The absence of toxins on a toxicology screen does not mean that toxins are not present • Serum toxin levels may not correlate with the degree of toxicity

Epidemiology • Over 1 million poison control center calls annually for pediatrics • Majority under age 6 years • Very few fatalities comparatively • Most fatalities in adolescents • Most common ingestant is analgesics • Most common fatal exposure is fumes/gases
Considerations in Pediatrics • Higher body surface area more absorption of topical exposure • Exposure is same as medication – consider mg/kg • Relatively small exposures may be impactful • What is available to the child other than the offending agent • Adolescents will abuse what is common, popular, inexpensive, and readily available
GI Decontamination • Activated charcoal Binds intoxicant to prevent absorption 0. 5 -1 g/kg, Ideal dose 10: 1 Rarely is useful, is often harmful Never been proven to improve outcomes Consider if <1 hour post ingestion, with significantly dangerous ingestion – Beta Blocker, Calcium Channel Blocker, Tricyclic Anti-depressant • Do not use with seizures, AMS, CNS depression, metals, alcohols, caustics • • •
GI Decontamination • Gastric Lavage has also never been proven to improve outcome, use selectively and with caution • Recent ingestion of life-threatening medication or quantity that does not have good treatment or antidote available • Whole Bowel Irrigation • Use polyethylene glycol • Consider for Fe, Pb, Li, Sustained release preparations or Drug packets
Urine Alkalization • Traps weak acids • Administer D 5 W + 3 amps Na. HCO • Salicylates, chlorpropramide, chlorophenoxy herbicides
Hemodialysis • Failure to respond to standard therapy • Renal or hepatic dysfunction • Metabolic acidosis • Severe electrolyte abnormality • Drug must have a small volume of distribution, small molecular weight, be water soluble, and have low protein binding • Li, ASA, phenobarb, alcohols, theophylline
History • Exposure • • What substance/drug What amount What time What symptoms History of substance abuse PMHx for patient and all occupants of home Other medications or ingestants available at home
Physical Exam • Toxidromes will give you clues to ingestant/coingestant • Be aware of possible trauma, i. e. fall while intoxicated
Lab Orders • Consider testing based upon possible exposure, toxidrome or lack thereof, and physical exam findings • If intentional ingestion, need more broad evaluation • • CBC CMP Coags ASA APAP ETOH EKG UTOX
Naloxone • Competitive opioid antagonist • Dose: • Chronic opiate use: 0. 04 mg, titrate to effect up (0. 04, 0. 4, 2, to 10 mg) • Naïve: 0. 4 mg initial dose • Indication for use is respiratory depression • Goal is for normal respiratory status, NOT normal mental status if chronic abuser • Duration of action 20 -90 minutes • May require repeated doses or gtt (2/3 of dose that caused reversal) • May cause withdrawal in chronic users, may cause pulmonary edema • If short acting opiate, observe up to 4 hours, otherwise admit
Flumazenil • Competitive antagonist of benzodiazepine receptor – GABA • Use ONLY in patients who are benzo naïve with respiratory depression • Iatrogenic • Can always provide supportive care alone – may include intubation • Flumazenil in chronic benzodiazepine user will precipitate intractable seizures
Lead Poisoning • May be from paint, alloys, pottery, pipes, ammunition • Vague symptoms – weakness, irritability, weight loss, vomiting, personality changes, ataxia, headache, colic, developmental delay, seizures, coma • CBC shows hypochromic normocytic anemia, basophilic stippling
Lead Poisoning - Treatment • If level 45 -66 ug/dl • Succimer 700 -1050 mg/m 2/d oral • If level > 69 ug/dl or encephalopathic • Ca-Na-2 EDTA 1500 mg/m 2/d IV • Renal toxicity
Beta Blockers • β-1, β-2, α-1 • β-1: atenolol, esmolol, metoprolol, • Non-selective: Nadolol, propranolol • β & α: carvedilol, labetalol • Toxic at 2 -3 times therapeutic ingestion • Mostly hepatic clearance
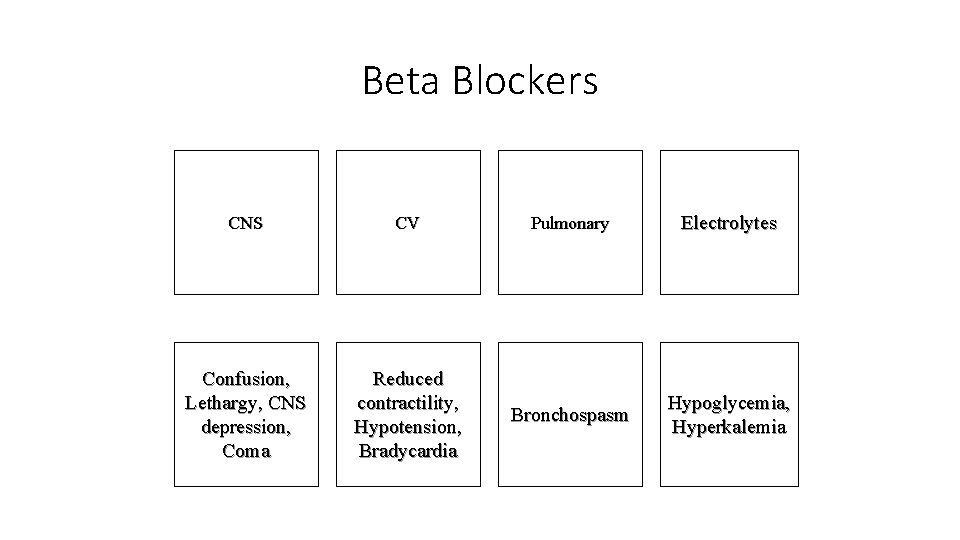
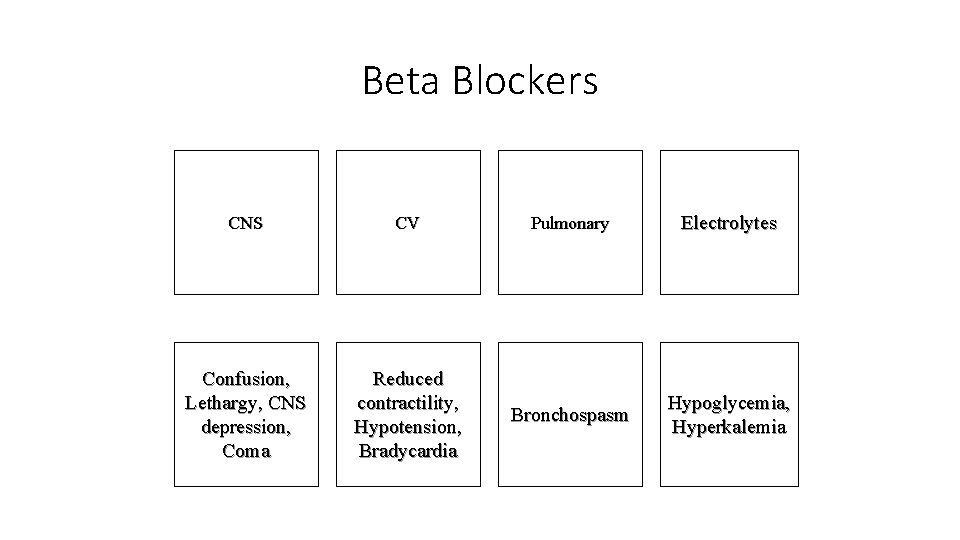
Beta Blockers CNS CV Pulmonary Electrolytes Confusion, Lethargy, CNS depression, Coma Reduced contractility, Hypotension, Bradycardia Bronchospasm Hypoglycemia, Hyperkalemia
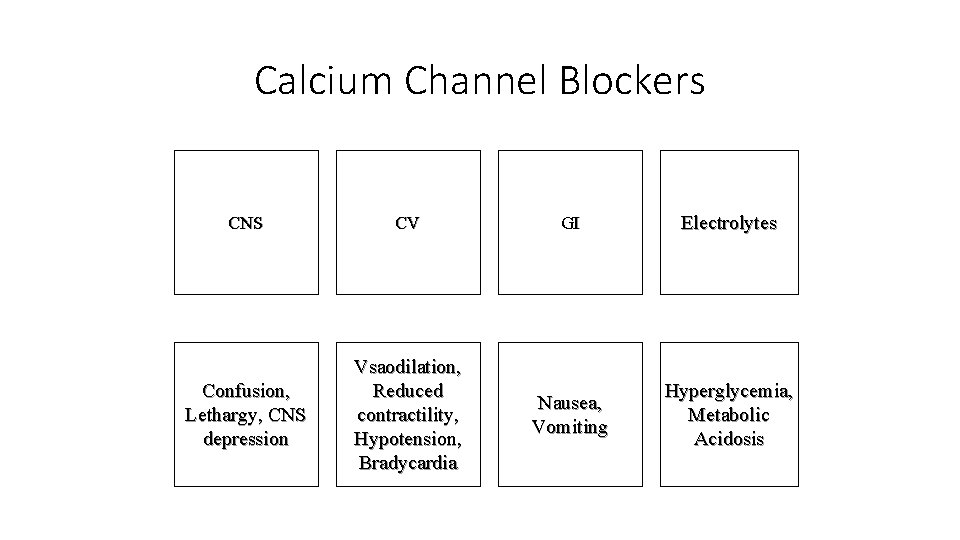
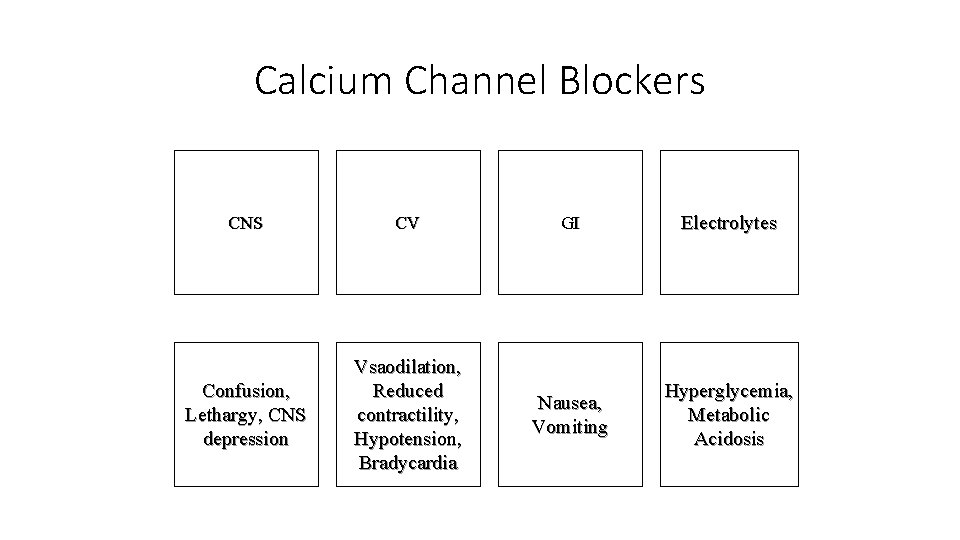
Calcium Channel Blockers CNS CV GI Electrolytes Confusion, Lethargy, CNS depression Vsaodilation, Reduced contractility, Hypotension, Bradycardia Nausea, Vomiting Hyperglycemia, Metabolic Acidosis
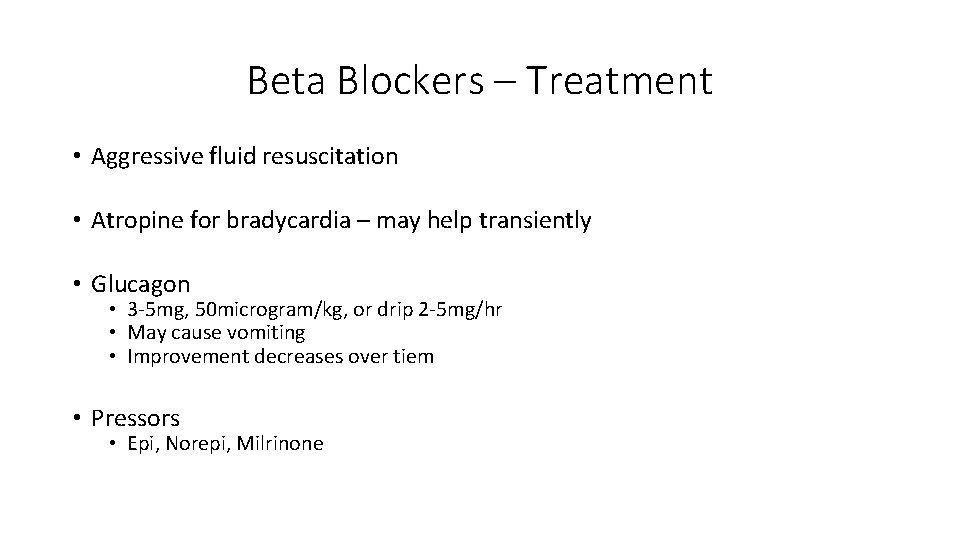
Beta Blockers – Treatment • Aggressive fluid resuscitation • Atropine for bradycardia – may help transiently • Glucagon • 3 -5 mg, 50 microgram/kg, or drip 2 -5 mg/hr • May cause vomiting • Improvement decreases over tiem • Pressors • Epi, Norepi, Milrinone
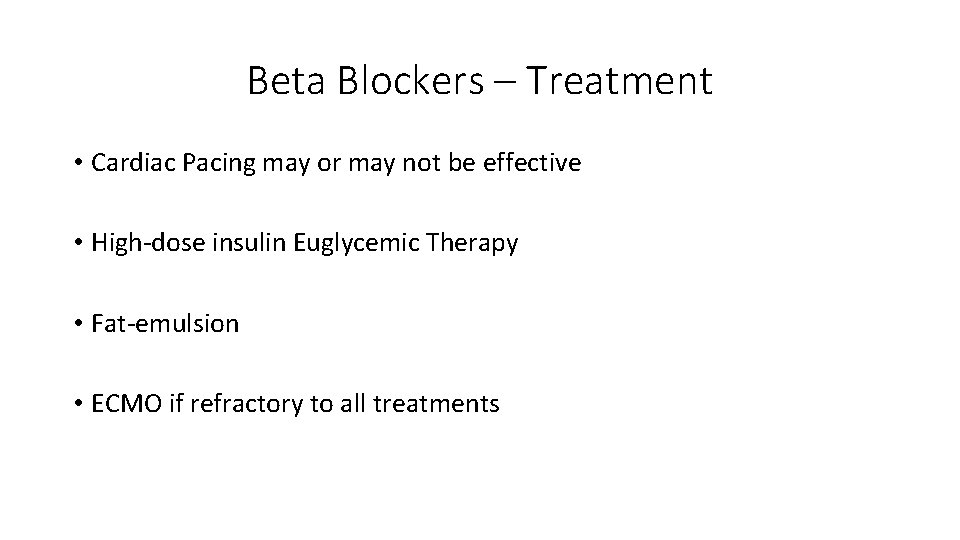
Beta Blockers – Treatment • Cardiac Pacing may or may not be effective • High-dose insulin Euglycemic Therapy • Fat-emulsion • ECMO if refractory to all treatments
Calcium Channel Blockers - Treatment • Same therapy essentially as beta blocker overdose • Calcium gluconate 0. 6 ml/kg • Calcium chloride 0. 2 ml/kg • 5 -7 mg/kg bolus
Sulfonylureas • Blyburide, Glipizide • Anti-hyperglycemic medications via increased insulin release • May result in severe and prolonged hypoglycemia • Must observe at least 12 -24 hours • Longer if sustained release, unknown time of ingestion, co-ingestants
Sulfonylureas - Treatment • Dextrose IV as needed • Octreotide • Reverses effect of sulfonylureas • 1 mcg/kg subcutaneous or IV • Max dose 50 micrograms SQ every 8 -12 hours
Anticholinergics • Antimuscurinic Acetylcholine receptors • Prototype: belladonna alkaloids • Atropa belladonna – Atropine • Datura stramonium (Jimson weed) – Scopolamine • Hyoscyamine
Anticholinergic Activity • Affect smooth muscles in the eye, gastrointestinal tract, bladder • Regulate sweat, salivary, and mucosal gland activity • Affect heart rate and cardiac conduction via AV node • Information storage, perception, cognitive function and motor coordination

Anticholinergic Toxicity • Hot as a Hare • Red as a Beet • Blind as a Bat • Dry as a Bone • Mad as a Hatter
Clinical Anticholinergics • Pupillary dilators (atropine) • Antispasmodics (dicyclomine) • Decrease gastric secretions (propantheline) • Motion sickness (scopolamine)
Clinical Anticholinergics • Asthma (ipratropium) • Bradycardia (atropine) • Parkinson’s (benztropine)
Anticholinergics in Overdose • Rarely result in death if supportive care is available • Thermoregulatory dysfunction may be lethal even at therapeutic doses • Heatstroke fatalities in people exercising • Jimson weed overdoses as hallucinogenic in various cultures and teenagers
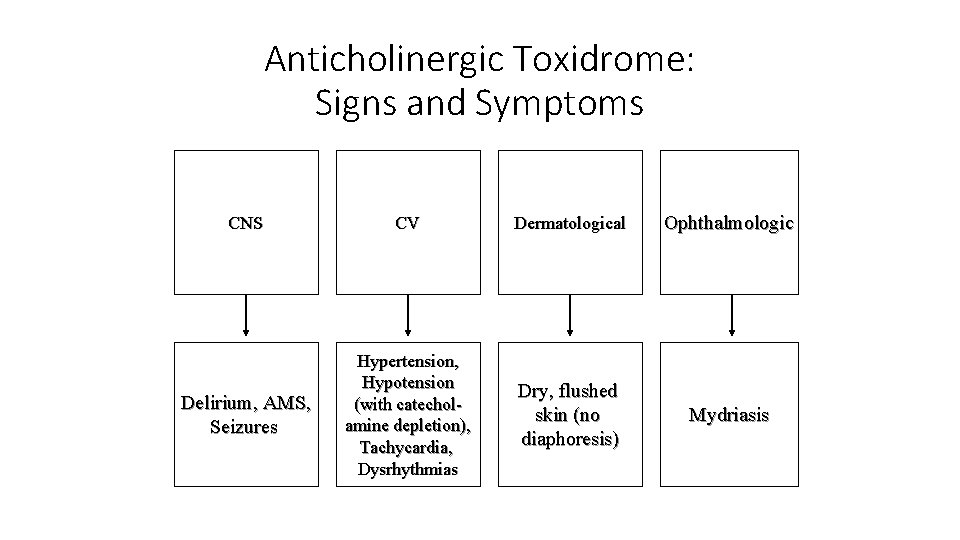
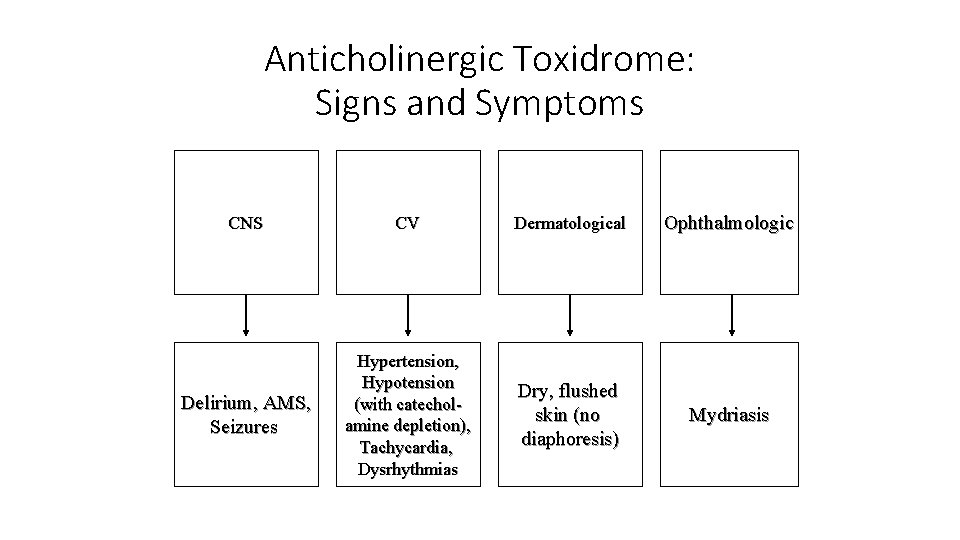
Anticholinergic Toxidrome: Signs and Symptoms CNS CV Dermatological Ophthalmologic Delirium, AMS, Seizures Hypertension, Hypotension (with catecholamine depletion), Tachycardia, Dysrhythmias Dry, flushed skin (no diaphoresis) Mydriasis
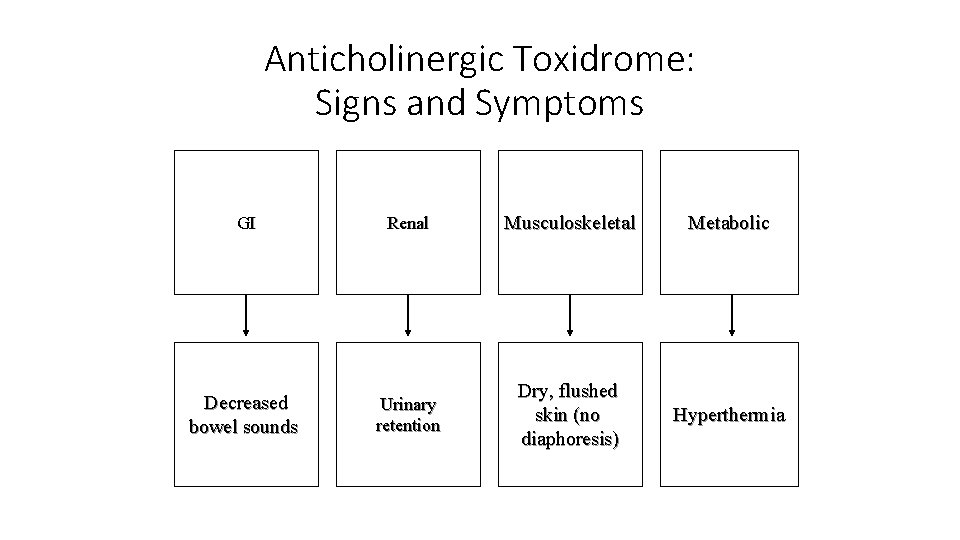
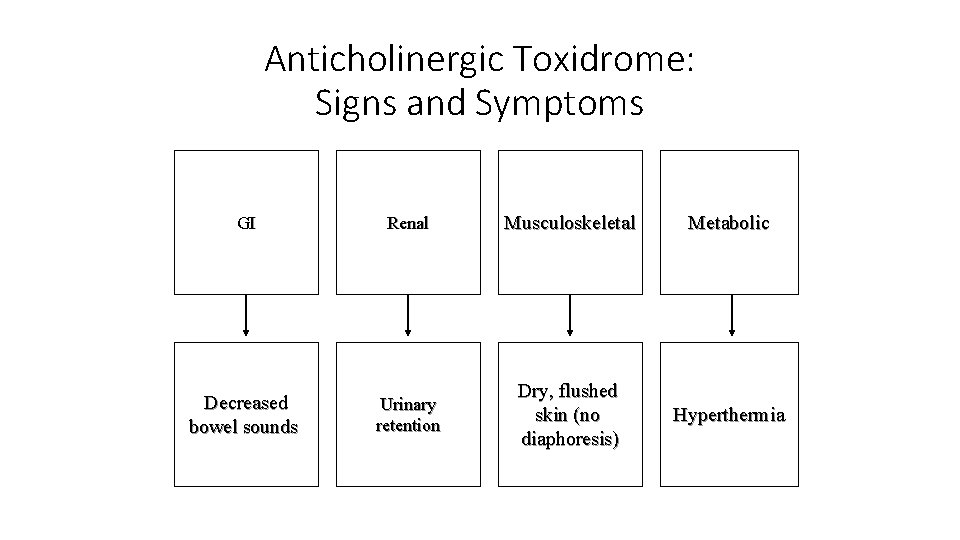
Anticholinergic Toxidrome: Signs and Symptoms GI Renal Musculoskeletal Metabolic Decreased bowel sounds Urinary retention Dry, flushed skin (no diaphoresis) Hyperthermia
Management • Treat agitation with benzodiazepines IV • Agitated patients may have altered mental status worsened by severe hyperthermia • Monitor core temperature with rectal probe • Ice water, evaporative cooling – NO antipyretics, cooling blankets
Management • Treat seizures with benzodiazepines IV or IM • Consider GI decontamination for large ingestions presenting early • No evidence that GI lavage improves outcome, may worsen • Activated charcoal will absorb diphenhydramine, TCA, phenothiazines, but no evidence it improves outcome
Physostigmine • Naturally occurring acetylcholinesterase inhibitor • Block degradation of Ach, overcomes effects of receptor blockade • Crosses blood-brain barrier • Physostigmine itself is toxic in otherwise healthy patients • Seizures, muscle weakness, bradycardia, bronchoconstriction, lacrimation, salivation, bronchorrhea, vomiting, diarrhea • Conduction delay or prolonged QRS or TCA is contraindication
Physostigmine • Useful in severe cases, 102 mg adults, 0. 02 mg/kg peds • Repeat in 10 -15 minutes if needed • Have atropine available if you get physostigmine toxicity
Disposition • Most patients recover rapidly, even with just supportive care • Alert, mildly symptomatic patients may be discharged after observation • Asymptomatic patients early in ingestion should be observed for at least 4 hours • Patients with hyperthermia, seizures, agitation, coma admission
Cholinergic Toxidrome • Usually results from environmental exposure to the following: • • • Organophosphate and carbamate insecticides Physostigmine Edrophonium (Tensilon ) Plants (mushrooms) Chemical nerve agents (i. e. VX, sarin gas)
Cholinergic Toxidrome: Mechanism • The toxins irreversibly bind to acetylcholinesterase • Degradation of acetylcholine is reduced • Results in an increase in acetylcholine at the terminal motor end plate and at the synapses of parasympathetic nerve ganglia • Unopposed muscarinic and nicotinic stimulation
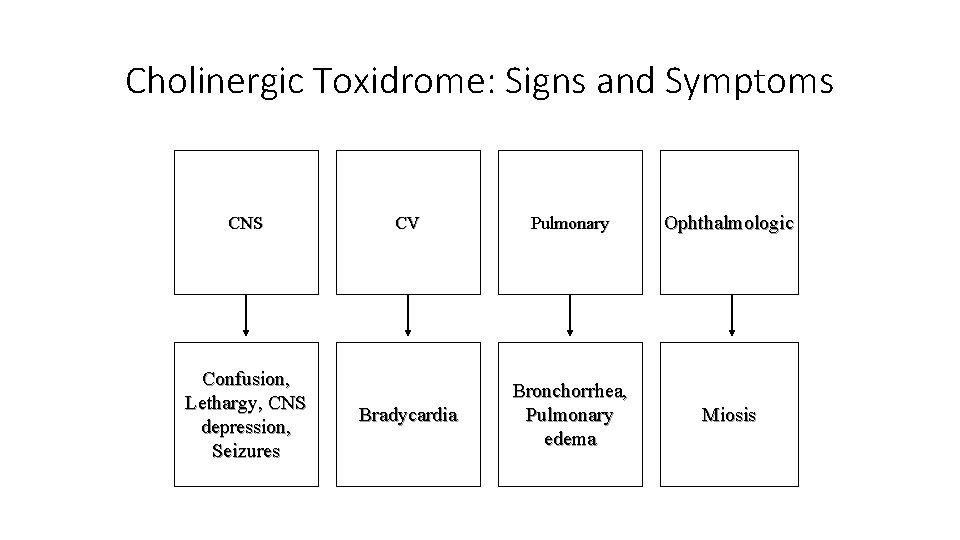
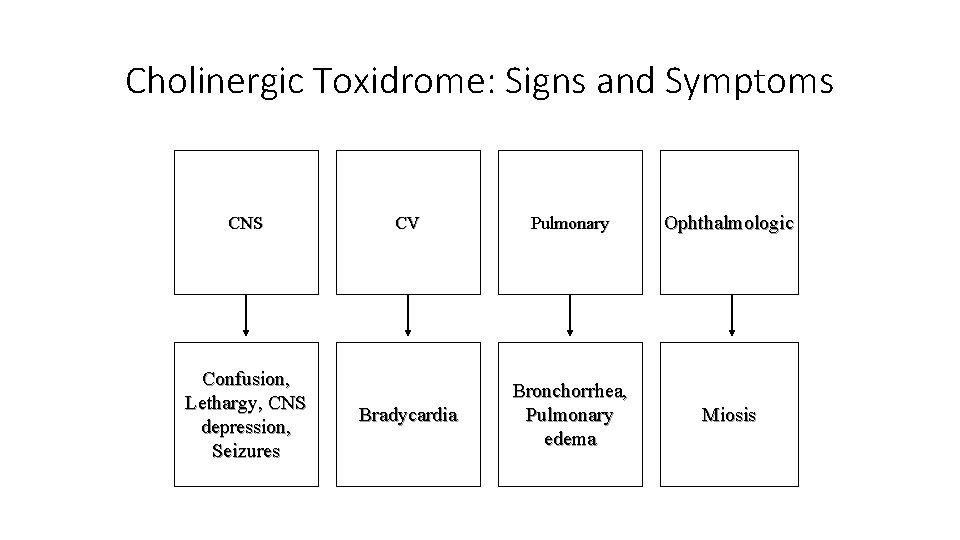
Cholinergic Toxidrome: Signs and Symptoms CNS Confusion, Lethargy, CNS depression, Seizures CV Pulmonary Ophthalmologic Bradycardia Bronchorrhea, Pulmonary edema Miosis
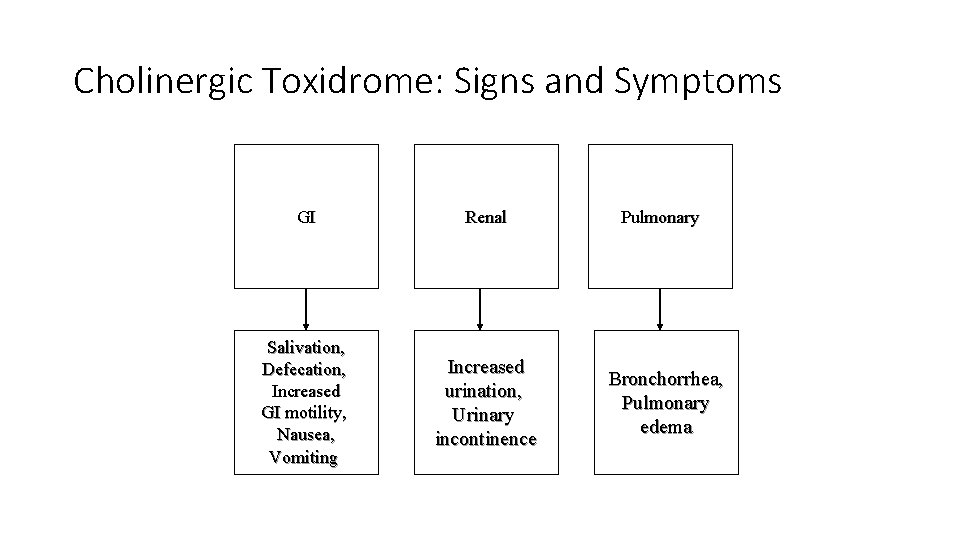
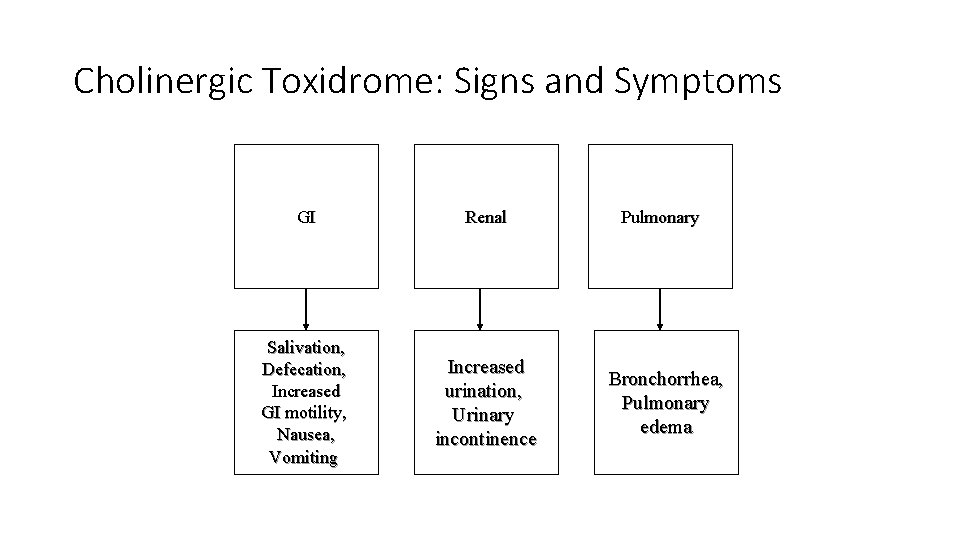
Cholinergic Toxidrome: Signs and Symptoms GI Renal Salivation, Defecation, Increased GI motility, Nausea, Vomiting Increased urination, Urinary incontinence Pulmonary Bronchorrhea, Pulmonary edema
Cholinergic Toxidrome: Signs and Symptoms • Summarized by the mnemonic “SLUDGE” • • • Salivation Lacrimation Urination/urinary incontinence Defecation/fecal incontinence Gastrointestinal distress Emesis
Cholinergic Toxidrome: Management • Supportive care • Management of altered mental status • "Coma cocktail" administration • Assess for other causes • Administration of atropine sulfate (in large quantities) • Will reverse/treat cholinergic symptoms, bronchorrhea, and bradycardia
Cholinergic Toxidrome: Management • Pralidoxime chloride (2 -PAM chloride, Protopam ) in severe cases • Cholinesterase-reactivating agent
Acetaminophen • One of the most commonly used antipyretic/analgesics globally • Found alone and in numerous products OTC and prescription • Toxicity is a leading cause of hospital admission, antidotal use, and patient fatalities
Acetaminophen • Inhibits PGE 2 synthesis, causing antipyresis and analgesia • Metabolized by conjugation with glucuronide (40 -67%) and sulfate (20 -46%) into nontoxic metabolites • Less than 5% via CYP-450 2 E 1 to N-acetyl-p-benzoquinonimine (NAPQI)
NAPQI • Toxic Metabolite • Normally rapidly combined with glutathione, other thiols to form nontoxic metabolites, excreted in urine • Large ingestions or repeated dosing… NAPQI levels overwhelm thiol reserves and liver’s ability to regenerate thiols • Initiates hepatocellular death upon binding with cells fulminant failure
NAC • NAC serves as a glutathione precursor to generate more • NAC also serves as sulfur-containing substitute to detoxify NAPQI • NAC may decrease NAPQI formation by enhancing acetaminophen conjugation with sulfate • NAC will act as free-radical scavenger to improve hepatic failure and prevent death in cases when no free acetaminophen is present
Presentation • Initially – and often – asymptomatic • Vague, nonspecific symptoms of nausea, vomiting, anorexia, malaise • Hepatic injury after 8 -36 hours, elevated AST, RUQ pain, jaundice • AST peaks in 2 -4 days; ALT, PT, Bilirubin rise and peak after AST • Severe: coagulopathy, metabolic acidosis, encephalopathy

Presentation • Resolution of transaminitis during recovery takes 5 -7 days • Repair of hepatic damage takes months • No long term sequelae
Diagnosis and Risk Assessment - Acute • Over 150 mg/kg must be consumed for toxicity in acute setting • Serum acetaminophen concentration at 4 hours post-ingestion • Use Rumack-Matthew nomogram for diagnosis of toxicity • If level is greater than treatment line, give NAC

Diagnosis and Risk Assessment - Chronic • Can’t use nomogram • Risk of hepatotoxicity increased with increasing total dose and longer duration of dosing • Lab tests should be done for any patient meeting chronic ingestion criteria

Diagnostics and Risk Assessment - Chronic • Chronic use of INH, Ethanol hav eincreased CYP 2 E 1 activity, high risk • Prolonged fasting and kids with febrile illness high risk • Chronic ingestions with elevations of AST should get NAC regardless of APAP levels • If AST normal but greater than expected APAP levels, start NAC
Diagnostic and Risk Assessment - Pregnancy • Fetal toxicity is rare • APAP crosses placenta, levels equal to or greater than mother’s • NAC is safe in pregnancy • Assess as for other acute or chronic presentations

Treatment Duration • 72 hour PO treatment • 21 hour IV treatment • Discontinue after course if AST normalized AND APAP level negative • If AST elevated or APAP present, continue treatment and retest
Aspirin • Peak concentrations in 2 -4 hours • In Intestines, Liver, RBC, hydrolyzed to free salicylic acid, reversibly binds albumin • In liver, conjugated with glucuronic acid & renal excretion • Many forms • Oil of wintergreen: 1 m. L = 1. 4 grams • Pepto-Bismol: 1 m. L = 8. 7 mg
Aspirin • At therapeutic doses, follows first-order kinetics • Excretion proportional to concentration • At toxic doses, follows zero-order kinetics • Metabolic pathways are saturated • Constant rate of metabolism • Mortality 25% for chronic ingestion, 1% for acute ingestion
Effects of Aspirin • Respiratory effects: stimulates respiratory center in medulla • Increases sensitivity to p. H & CO 2 • Causes hyperventilation, initially from stimulation, then as a compensation for metabolic acidosis • May be increased depth without increased rate • Metabolic Acidosis from uncoupled oxidative phosphorylation • Causes further hyperventilation to compensate for acidosis • Respiratory alkalosis causes dumping of bicarb, worsening acidosis • As p. H drops, ASA crosses BBB, worsens condition with CNS effects
Effects of Aspirin • Renal effects: • Increased potassium excretion from multiple factors • Non-oliguric renal failure from decreased RBF or direct toxicity • ASA induced SIADH • Pulmonary & CNS Effects: Edema for both • Unknown mechanism • All effects may be worse in the elderly and pediatric populations
Presentation • Toxicity at 200 -300 mg/kg, 500 mg/kg may be fatal • Tinnitus, impaired hearing, hyperventilation, vomiting, dehydration, hyperthermia • CNS manifestations from severe acidemia

Diagnostics • Serum levels 6 hours after ingestion, and if elevated, repeat in 2 hours • Frequent ABG to monitor p. H • Consider dialysis for any patient severely acidotic or with concern for respiratory failure/compromise • Do NOT intubate ASA patients unless no other choice – VERY difficult to maintain respiratory rate
Treatment • IV Fluids • replace dehydration, maintain urine output 2 -3 ml/kg/hr • Include dextrose – hypoglycemia correlates with death • Replete potassium • Alkalinize urine – increases urinary excretion • Urine p. H 7. 5 -8. 0 • Sodium Bicarbonate 1 -2 m. Eq/kg over 1 -2 hours • NO role forced diuresis
Treatment • Consider hemodialysis for patients with significant toxicity • • • ASA levels > 100 mg/d. L in acute ingestion, > 50 mg/d. L in chronic ingestion AMS Intubation other than for coingestants Coma Renal or hepatic failure Pulmonary Edema Severe acid-base disturbance Rapidly rising ASA level Failure to respond to other treatment
ASA and Pregnancy • ASA significantly more toxic to fetus than mother • If fetus is viable, consider delivery
NSAIDS • Cyclo-oxygenase Inhibitors • Nonspecific or Specific to COX-1, COX-2 • Almost complete absorption from GI tract • Large plasma protein binding
Presentation - Ibuprofen • Usually asymptomatic or with mild symptoms, but may have GI bleeding, AMS, coma, seizures, hypotension, hypothermia • Vast majority of Ibuprofen overdoses are benign and self-limited • 7% of children will develop symptoms • Toxicity requires at least 100 mg/kg ingestion, and symptoms appear within 4 hours • Reversible renal dysfunction • Seen with hypotension, hypovolemia • Responds to supportive care
Management • Supportive care • Kids • < 100 mg/kg ingestion: No evaluation necessary • > 300 mg/kg ingestion: evaluate for signs/symptoms & treat • 100 -300 mg/kg ingestion: evaluate for signs/symptoms and only treat if symptomatic • NO EVIDENCE of AC or GI Lavage being useful!
Caustics • Acids or bases • In general, severity increases with p. H < 3 and p. H > 11 • Exception: Hydroflouric acid – weak acid, life-threatening • 85% of ingestions are accidental • Intentional ingestion has more oral sparing, but worse injuries • Concentrated forms generate heat and also cause thermal burns
Caustics • Liquid drain clearners: Base up to 30% KOH, Acid up to 93% H 2 SO 4 • Crystal and solids have higher degree of adherence and worse injury • Crystal drain cleaner: Lye up to 74% Na. OH • Household liquid bleach: Ha. HCl. O 5. 25% - rarely injures! • Toilet cleaner: up to 26% HCl
Factors Influencing Extent of Injury • Type of Agent • Concentration of Solution • Volume of Exposure • Viscosity • Duration of Exposure • p. H • Presence or Absence of Food in Stomach
Acid Ingestions • Cause coagulative necrosis • Eschar forms, limiting further penetration • Strong odor and immediate pain usually limit exposure • Less likely to cause severe esophageal and pharyngeal injur • Systemic absorption: metabolic acidosis, injury to spleen, liver, biliary tract, pancreas, kidneys
Alkali Ingestions • Liquefaction necrosis, fat saponification, protein disruption • Deeper injuries • Depth of injury dependent on concentration of chemical • 30% Na. OH with tissue contact for 1 second causes full-thickness burns • Colorless, odorless, no immediate pain on contact
Alkali Ingestions • Gastric necrosis & perforation • Burns below the pylorus carry worse prognosis than burns above • 50% mortality vs 9%
Degree of Damage • 1 st Degree (Grade 1): Edema, Hyperemia • 2 nd Degree (Grade 2): Ulcers, exudates, membranes • A: Non-circumferential • B: Circumferential • 3 rd Degree (Grade 3): Transmural involvement, necrosis, perforation • 15 -30% of all Grade 2 and 75% of Type B progress to stricture • 90% Grade 3 progress to stricture
Presentation • Airway edema & esophageal or gastric perforation are most urgent • Systemic toxicity, hypovolemic shock, hemodynamic instability all ominous • Oral pain, abdominal pain, vomiting, drooling • Wheezing, coughing, stridor, dysphonia, chest pain
Presentation • Prolonged drooling and dysphagia predict esophageal injury with 100% sensitivity, 90% specificity • Dysphagia usually subsides in 3 -4 days • Stricture formation in 2 -8 weeks
Other Information • Increased risk of cancer in 40 -50 years – 1000 -3000 fold • Significant ingestion of acid has higher mortality than alkali • Systemic effects may be cause
Diagnostics • CXR, ABD XR • CT Chest, Abdomen/Pelvis • ABG • Cardiac monitoring • Endoscopy in 12 -24 hours
Management • If hoarseness, throat pain, drooling, edema – Intubate immediately • Consider fiber-optics or cricothyrotomy if necessary • Vigorous fluid resuscitation • Do NOT induce vomiting or gastric lavage, NO AC • Immediate surgery if free air on x-ray

Sympathomimetic Toxidrome • Results from excessive alpha/beta adrenergic stimulation with the following: • • • Cocaine Caffeine MAO-I overdoses/interactions Amphetamine and related toxicities Hallucinogenic compounds (PCP, LSD, Ketamine)
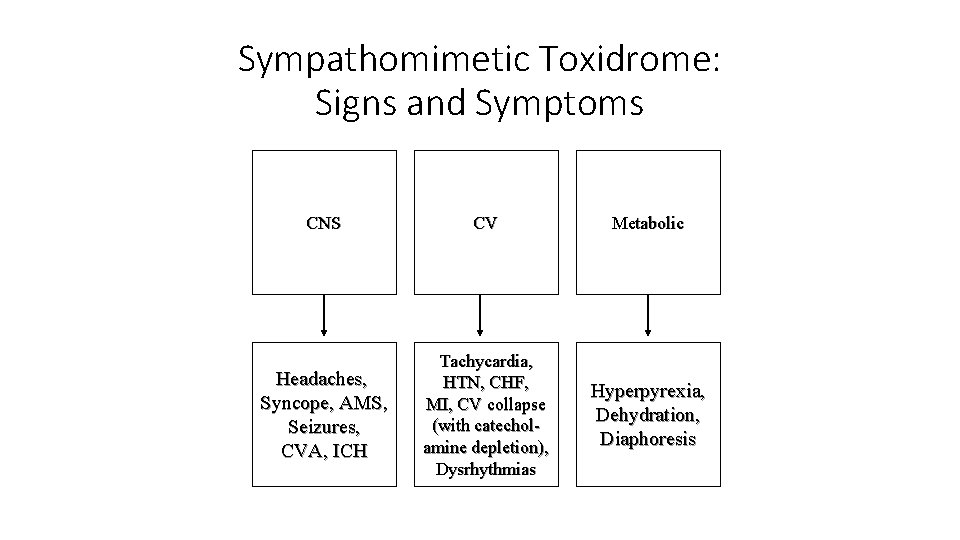
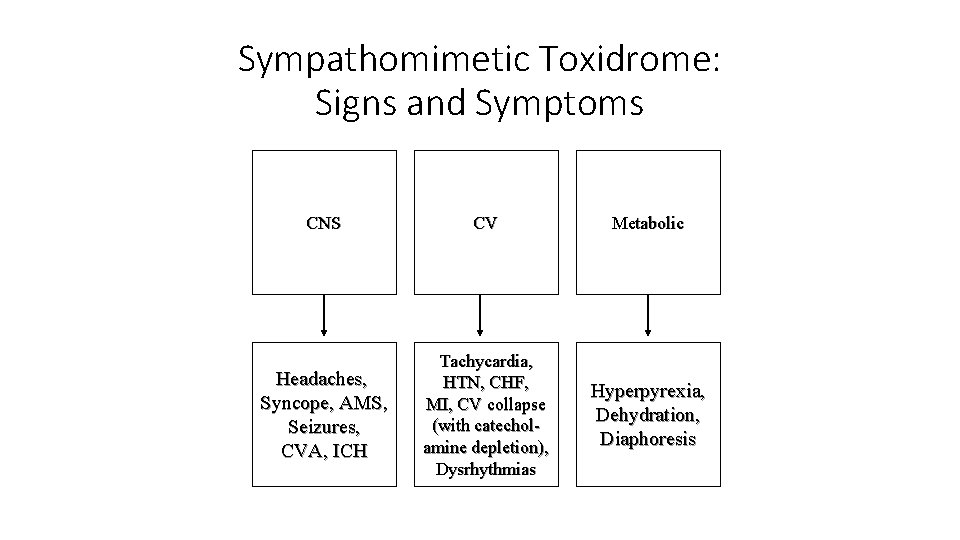
Sympathomimetic Toxidrome: Signs and Symptoms CNS CV Metabolic Headaches, Syncope, AMS, Seizures, CVA, ICH Tachycardia, HTN, CHF, MI, CV collapse (with catecholamine depletion), Dysrhythmias Hyperpyrexia, Dehydration, Diaphoresis
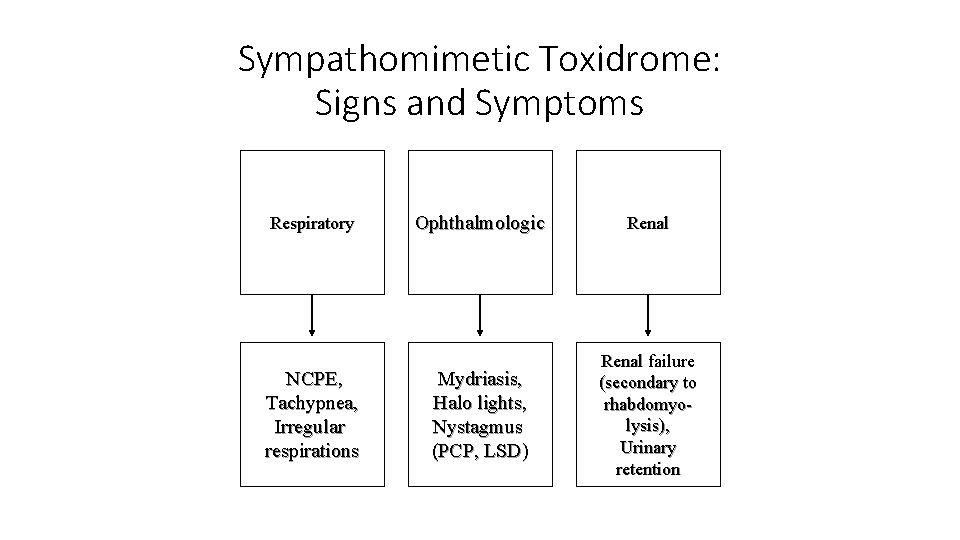
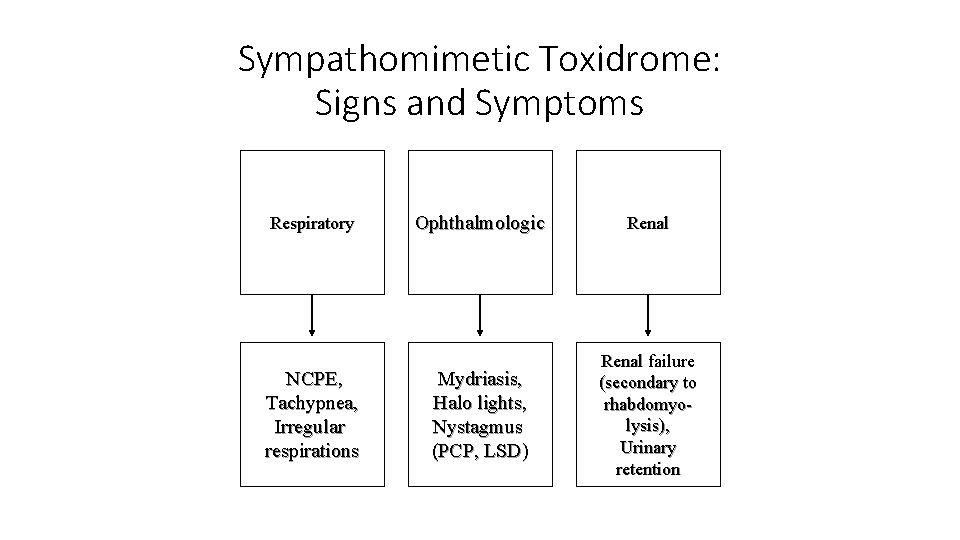
Sympathomimetic Toxidrome: Signs and Symptoms Respiratory NCPE, Tachypnea, Irregular respirations Ophthalmologic Renal Mydriasis, Halo lights, Nystagmus (PCP, LSD) Renal failure (secondary to rhabdomyolysis), Urinary retention
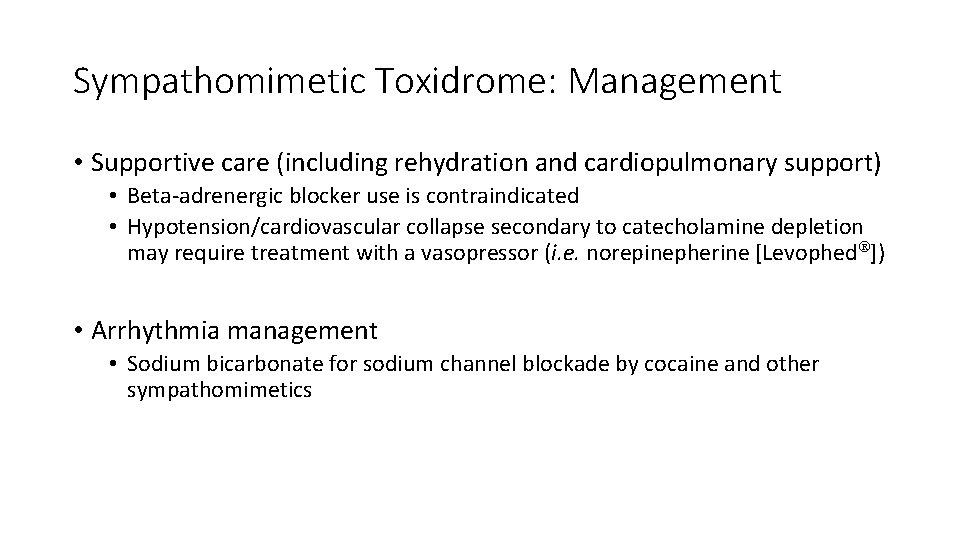
Sympathomimetic Toxidrome: Management • Supportive care (including rehydration and cardiopulmonary support) • Beta-adrenergic blocker use is contraindicated • Hypotension/cardiovascular collapse secondary to catecholamine depletion may require treatment with a vasopressor (i. e. norepinepherine [Levophed ]) • Arrhythmia management • Sodium bicarbonate for sodium channel blockade by cocaine and other sympathomimetics
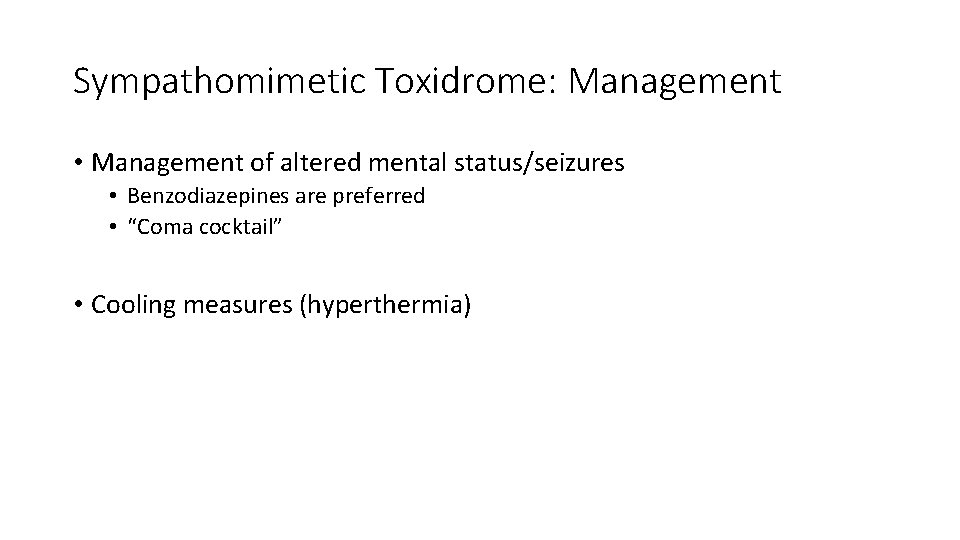
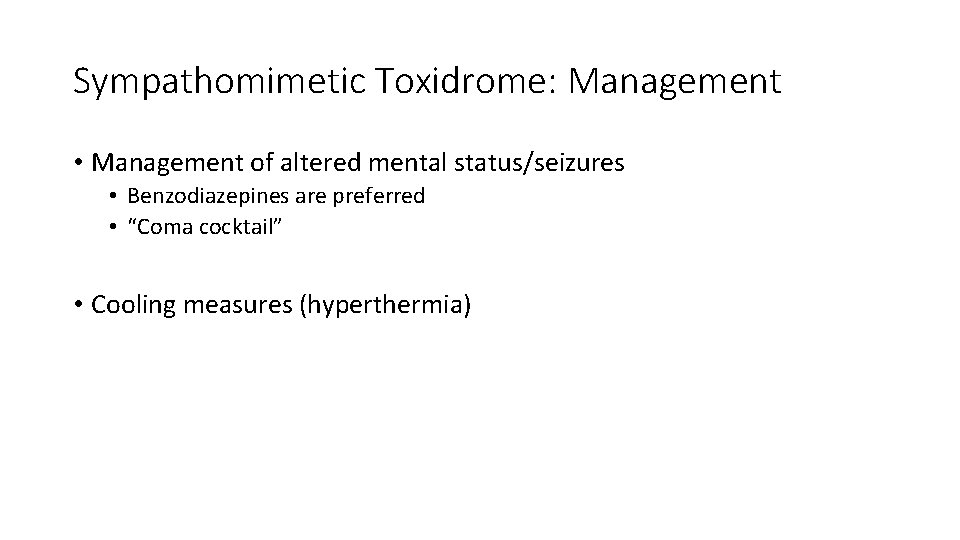
Sympathomimetic Toxidrome: Management • Management of altered mental status/seizures • Benzodiazepines are preferred • “Coma cocktail” • Cooling measures (hyperthermia)

Opioid Toxidrome • Results from stimulation of opioid receptors (kappa, mu, sigma, delta) • Commonly caused by some of the following: • • • Heroin Morphine sulfate Meperidine (Demerol ) Fentanyl (Sublimaze ) Hydrocodone/acetminophen (Vicodin ) Hydromorphone (Dilaudid )
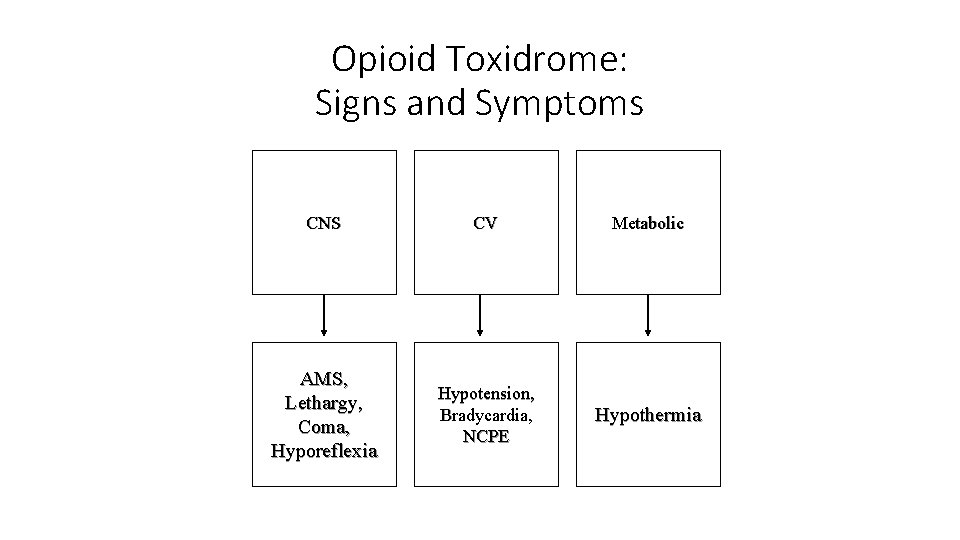
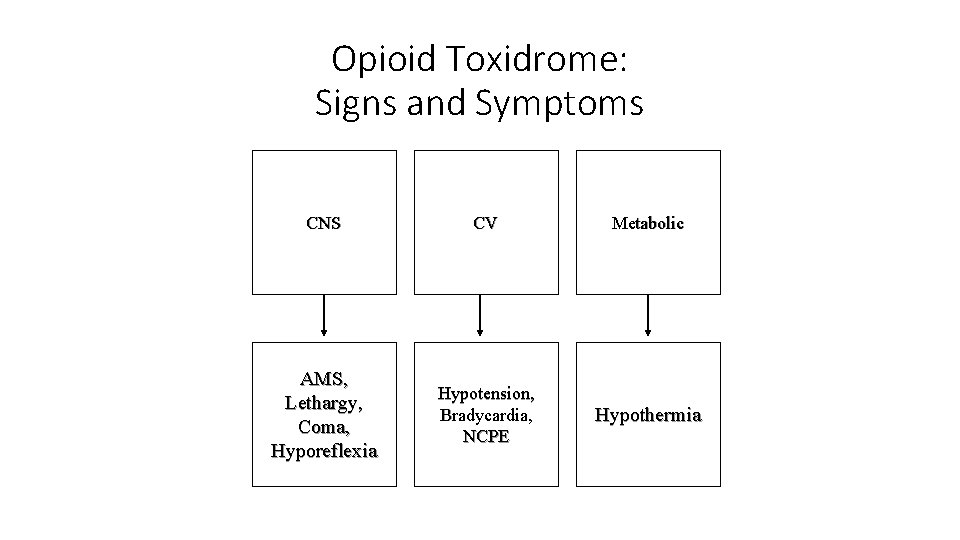
Opioid Toxidrome: Signs and Symptoms CNS CV Metabolic AMS, Lethargy, Coma, Hyporeflexia Hypotension, Bradycardia, NCPE Hypothermia
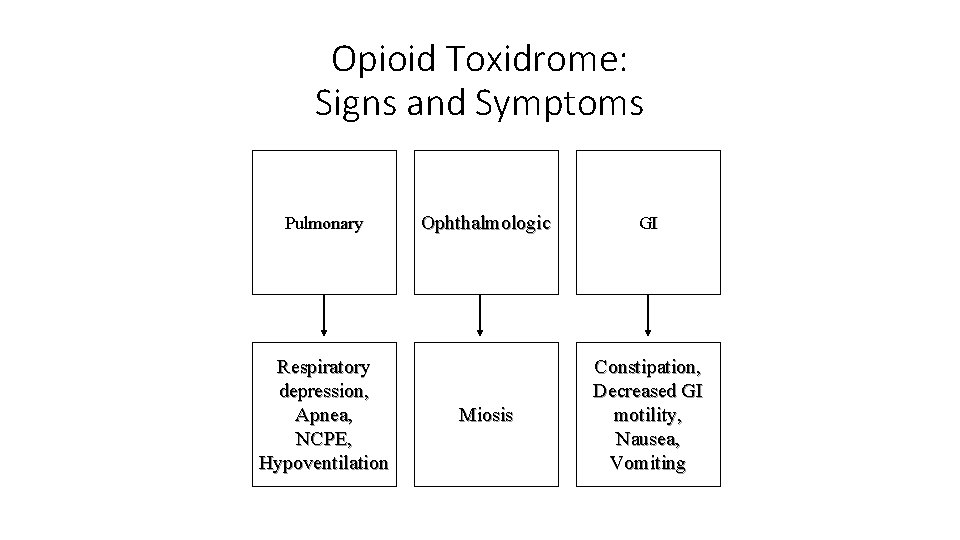
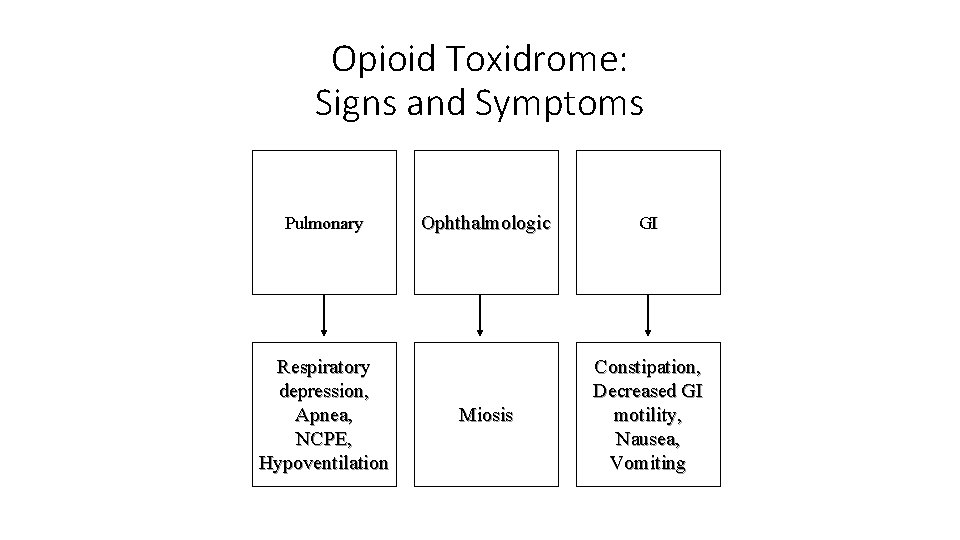
Opioid Toxidrome: Signs and Symptoms Pulmonary Respiratory depression, Apnea, NCPE, Hypoventilation Ophthalmologic GI Miosis Constipation, Decreased GI motility, Nausea, Vomiting
Opioid Toxidrome: Management • Supportive care (cardiopulmonary support) • Administration of naloxone hydrochloride (Narcan ) • Opioid antagonist • Naloxone may have a shorter half-life than the agent causing toxicity • Frequent, repeated doses may be required
Opioid Withdrawal Toxidrome • Signs and symptoms of the opioid withdrawal toxidrome similar to those expected with the withdrawal from any CNS depressant • Causes • Cessation of drug use by an individual • Cessation of drug exposure (i. e. neonates born to heroin-using mothers) • Iatrogenic use of opioid antagonists (naloxone)
Opioid Withdrawal Toxidrome: Signs and Symptoms • Signs and symptoms are the "inverse" of the toxidrome • Cardiovascular • Hypertension • Tachycardia • CNS • Normal mental status, hyperactivity • Ophthalmologic • Mydriasis
Opioid Withdrawal Toxidrome: Signs and Symptoms • Gastrointestinal • Increased gastrointestinal activity • Nausea and vomiting • Diarrhea • ENT • Rhinorrhea • Dermatologic • Piloerection ("gooseflesh") • Diaphoresis
Opioid Withdrawal Toxidrome: Management • Supportive care • Cardiopulmonary support • Admission to detoxification program • Agitation control • Psychiatric support/counseling • ? Benzodiazepines (risk of "rotating addictions")
Opioid Withdrawal Toxidrome: Management • Reversal of withdrawal symptoms • Clonidine (centrally acting alpha-agonist) • Methadone (saturates opioid receptors without producing intoxication)
Sedative-Hypnotic/Ethanol Toxidrome • Results from intoxication with or exposure to the following agents: • • Barbiturates Benzodiazepines Ethanol Gamma hydroxybutyrate Chloral hydrate Etomidate (Amidate ) Propofol (Diprivan )
Sedative-Hypnotic Agents: Mechanism of Action • • GABA = γ-aminobutyric acid Major inhibitory neurotransmitter in CNS Alcohol Barbiturates – Attach to barbiturate receptor • Benzodiazepines – Attach to BZD receptor (multiple)
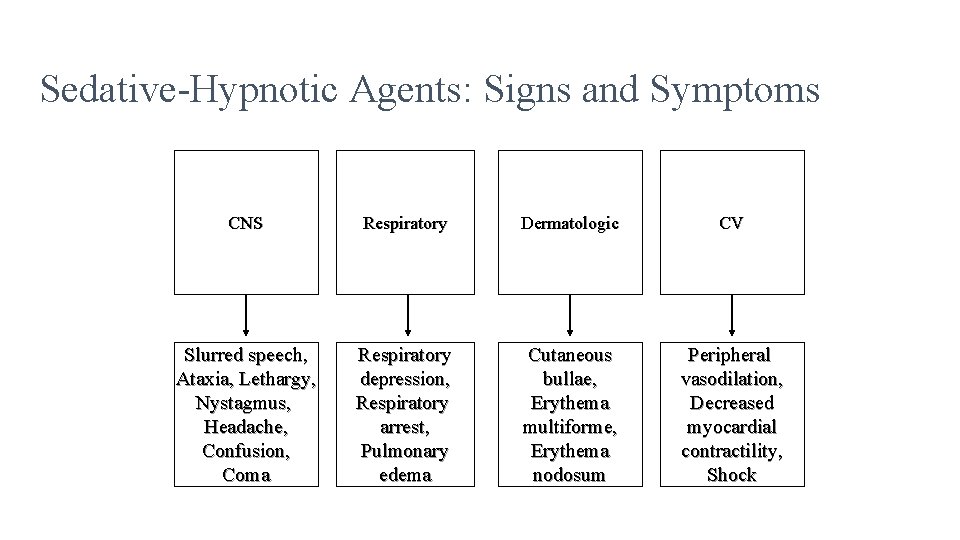
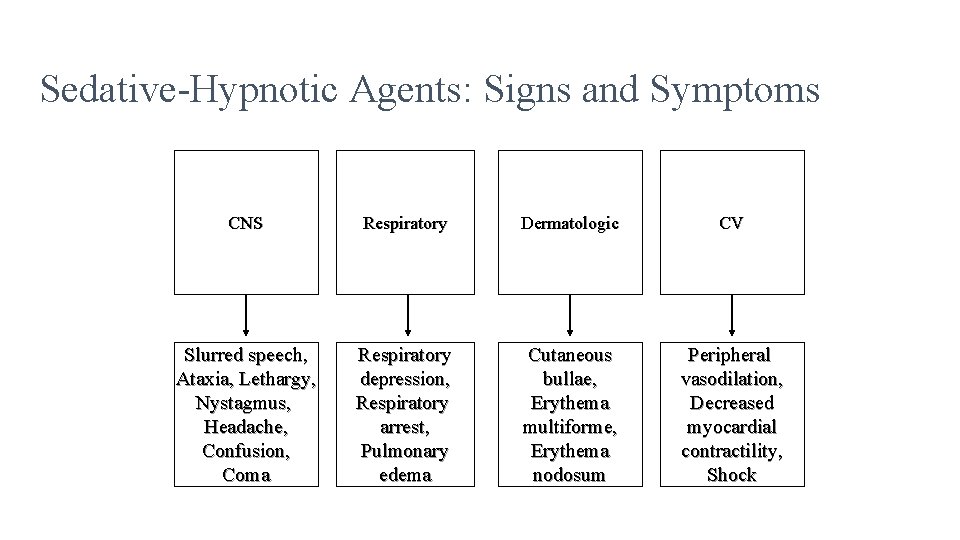
Sedative-Hypnotic Agents: Signs and Symptoms CNS Respiratory Dermatologic CV Slurred speech, Ataxia, Lethargy, Nystagmus, Headache, Confusion, Coma Respiratory depression, Respiratory arrest, Pulmonary edema Cutaneous bullae, Erythema multiforme, Erythema nodosum Peripheral vasodilation, Decreased myocardial contractility, Shock
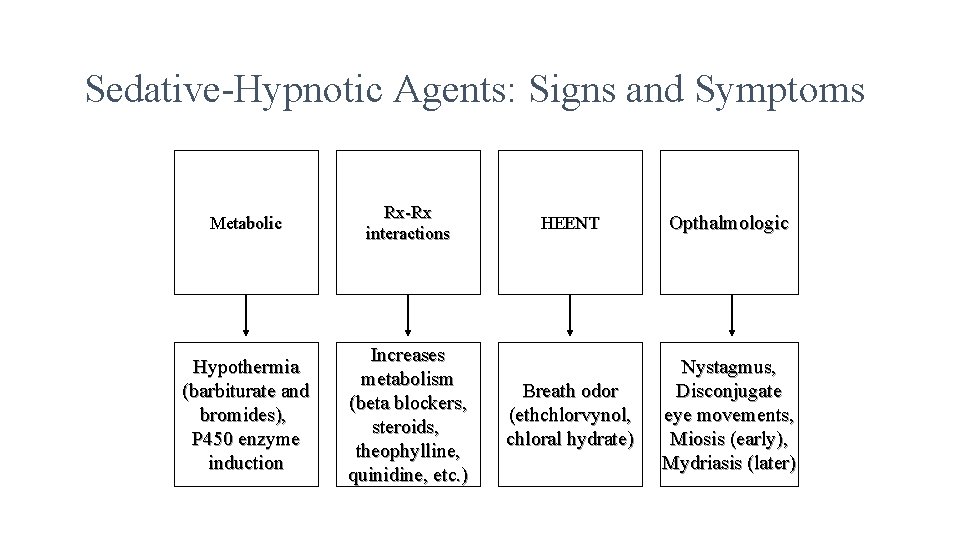
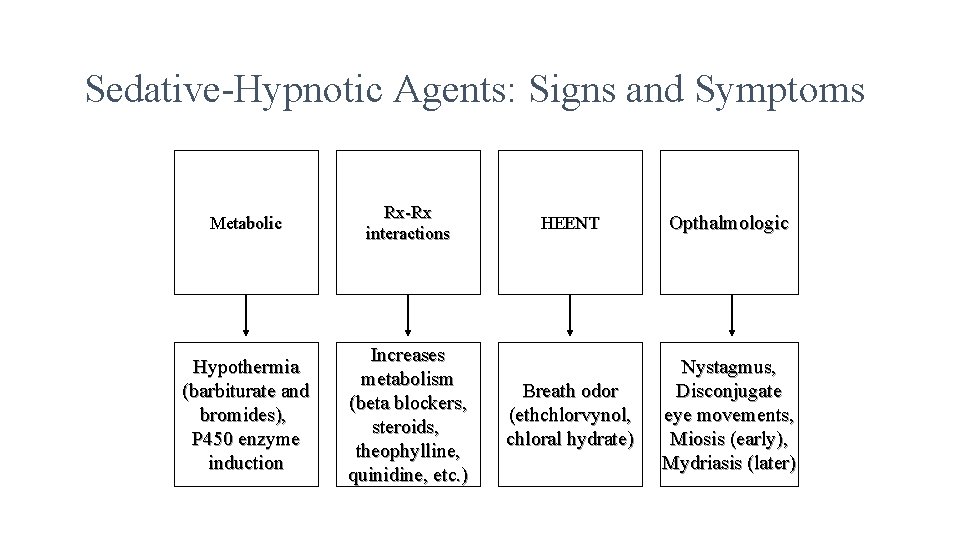
Sedative-Hypnotic Agents: Signs and Symptoms Metabolic Rx-Rx interactions Hypothermia (barbiturate and bromides), P 450 enzyme induction Increases metabolism (beta blockers, steroids, theophylline, quinidine, etc. ) HEENT Opthalmologic Breath odor (ethchlorvynol, chloral hydrate) Nystagmus, Disconjugate eye movements, Miosis (early), Mydriasis (later)
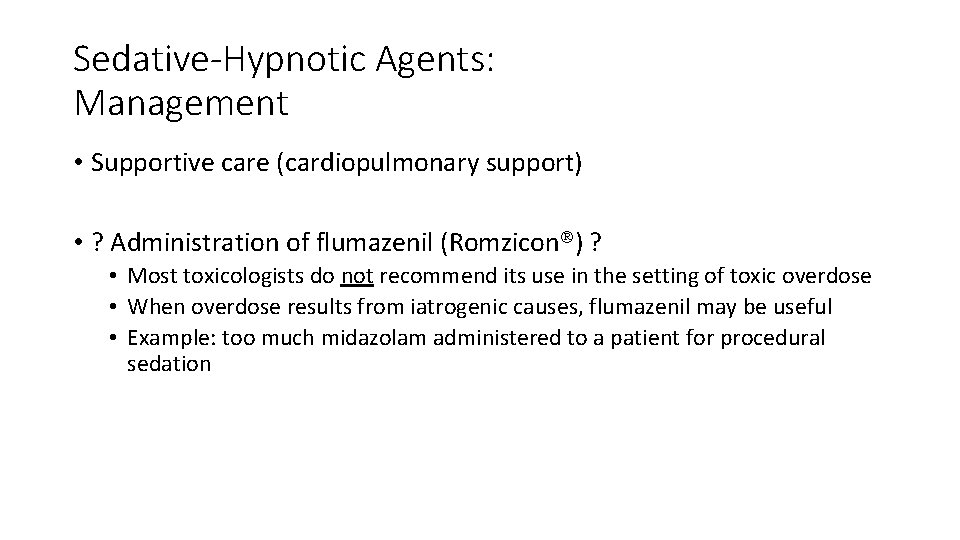
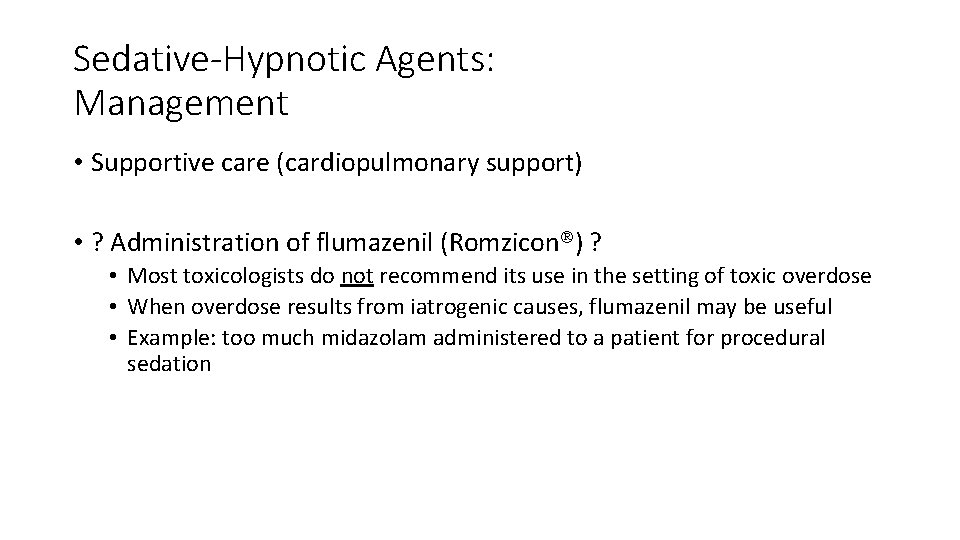
Sedative-Hypnotic Agents: Management • Supportive care (cardiopulmonary support) • ? Administration of flumazenil (Romzicon ) ? • Most toxicologists do not recommend its use in the setting of toxic overdose • When overdose results from iatrogenic causes, flumazenil may be useful • Example: too much midazolam administered to a patient for procedural sedation
Sedative-Hypnotic/Ethanol Withdrawal Toxidrome • Signs and symptoms of the Sedative-Hypnotic/Ethanol withdrawal toxidrome similar to those expected with the withdrawal from any CNS depressant • Severe ethanol withdrawal may lead to delirium tremens • The presence of "D. T. 's" is associated with an increased mortality rate
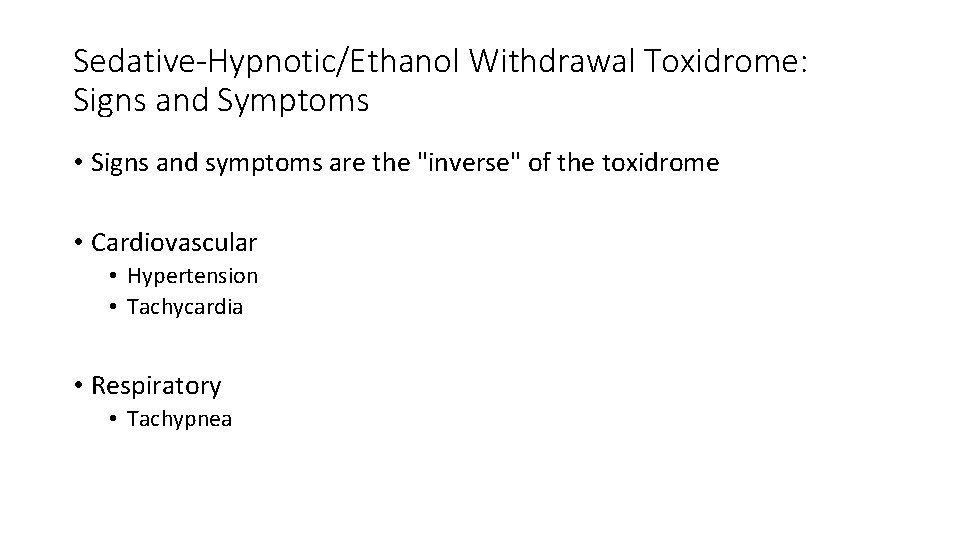
Sedative-Hypnotic/Ethanol Withdrawal Toxidrome: Signs and Symptoms • Signs and symptoms are the "inverse" of the toxidrome • Cardiovascular • Hypertension • Tachycardia • Respiratory • Tachypnea
Sedative-Hypnotic/Ethanol Withdrawal Toxidrome: Signs and Symptoms • Metabolic • Hyperthermia • CNS • • Altered mental status Tremor Seizures Hyperactivity
Sedative-Hypnotic/Ethanol Withdrawal Toxidrome: Signs and Symptoms • Opthalmologic • Mydriasis • Gastrointestinal • Normal to increased gastrointestinal activity • Nausea • Diaphoresis
Sedative-Hypnotic/Ethanol Withdrawal Toxidrome: Treatment • Supportive care • Cardiopulmonary support • Admission to detoxification program • Agitation control • Psychiatric support/counseling
Sedative-Hypnotic/Ethanol Withdrawal Toxidrome: Treatment • Reversal of withdrawal symptoms • Ethanol withdrawal: benzodiazepines (sometimes at high doses) should be used to blunt the initial symptoms (and prevent the onset of delirium tremens) • Sedative-hypnotic withdrawal: phenobarbital loading (for benzodiazepine withdrawal; controversial); benzodiazepines (for severe symptoms; controversial)
 Adam white facebook
Adam white facebook Patient 2 patient
Patient 2 patient Forensic toxicology lab activity
Forensic toxicology lab activity Toxicology effects
Toxicology effects Forensics toxicology definition
Forensics toxicology definition Examples of toxicology
Examples of toxicology Food safety and toxicology
Food safety and toxicology Toxicology types
Toxicology types Chapter 21 toxicology
Chapter 21 toxicology Accipitridae
Accipitridae Tera toxicology
Tera toxicology Toxicology and applied pharmacology
Toxicology and applied pharmacology Toxicology definition
Toxicology definition Forensic toxicology definition
Forensic toxicology definition Toxicology effects
Toxicology effects Toxicology
Toxicology Toxicology management
Toxicology management A small dose of toxicology
A small dose of toxicology Annual review of pharmacology and toxicology
Annual review of pharmacology and toxicology Who is regarded as the father of forensic science?
Who is regarded as the father of forensic science? Nc medical examiner and coroner guidelines
Nc medical examiner and coroner guidelines Environmental toxicology definition
Environmental toxicology definition Forensic toxicology vocabulary
Forensic toxicology vocabulary Nst 110
Nst 110 Toxicology
Toxicology Washington state toxicology lab
Washington state toxicology lab Importance of toxicology
Importance of toxicology Forensics toxicology definition
Forensics toxicology definition Toxicology
Toxicology Hormesis
Hormesis Chapter 8 toxicology poisons and alcohol
Chapter 8 toxicology poisons and alcohol Drug identification and toxicology
Drug identification and toxicology Toxicology defination
Toxicology defination What is toxicology?
What is toxicology? Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Lp html
Lp html Sơ đồ cơ thể người
Sơ đồ cơ thể người Số.nguyên tố
Số.nguyên tố đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Tư thế worms-breton
Tư thế worms-breton ưu thế lai là gì
ưu thế lai là gì Tư thế ngồi viết
Tư thế ngồi viết Cái miệng xinh xinh thế chỉ nói điều hay thôi
Cái miệng xinh xinh thế chỉ nói điều hay thôi Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Bổ thể
Bổ thể Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Tư thế ngồi viết
Tư thế ngồi viết Ví dụ giọng cùng tên
Ví dụ giọng cùng tên Thẻ vin
Thẻ vin Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Chúa sống lại
Chúa sống lại Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Công thức tiính động năng
Công thức tiính động năng Phép trừ bù
Phép trừ bù Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Dot
Dot Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 độ dài liên kết
độ dài liên kết Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau điện thế nghỉ
điện thế nghỉ Một số thể thơ truyền thống
Một số thể thơ truyền thống Pediatric assessment triangle
Pediatric assessment triangle Pediatric diabetes consortium
Pediatric diabetes consortium Implox
Implox Pediatric vision screening guidelines
Pediatric vision screening guidelines Pediatric dysphagia goals
Pediatric dysphagia goals Unc hematology oncology fellows
Unc hematology oncology fellows Chapter 57 pediatric dentistry recall
Chapter 57 pediatric dentistry recall Emt 6 rights
Emt 6 rights Pediatric triangle
Pediatric triangle Pediatric coma scale
Pediatric coma scale Sick child introduction
Sick child introduction Pediatric equipment list
Pediatric equipment list Normal vital signs for adults
Normal vital signs for adults Trends in pediatric
Trends in pediatric Peylonephritis
Peylonephritis 421 rule
421 rule Pediatric nursing definition
Pediatric nursing definition Pediatric occupational therapy frames of reference
Pediatric occupational therapy frames of reference Pediatric seizures
Pediatric seizures Atraumatic care principles
Atraumatic care principles 21 audubon pediatric clinic
21 audubon pediatric clinic Amoxicillin dosage chart by weight
Amoxicillin dosage chart by weight Step 1 score percentiles 2021
Step 1 score percentiles 2021 Pediatric chalk mixture
Pediatric chalk mixture Trends in pediatric nursing
Trends in pediatric nursing National pediatric hospital cambodia
National pediatric hospital cambodia Vague questions examples
Vague questions examples Pediatric rn
Pediatric rn Ebtesam ahmed
Ebtesam ahmed Triage disaster
Triage disaster Mt washington pediatric hospital feeding clinic
Mt washington pediatric hospital feeding clinic Pediatric trach ties
Pediatric trach ties Tailwinds pediatric dentistry
Tailwinds pediatric dentistry Bactrim pediatric dosing
Bactrim pediatric dosing Pediatric urologist salary
Pediatric urologist salary Cap module 1
Cap module 1 Jennifer kean
Jennifer kean